Abstract
-
➤
Sagittal alignment of the spine has gained attention in the field of spinal deformity surgery for decades. However, emerging data support the importance of restoring segmental lumbar lordosis and lumbar spinal shape according to the pelvic morphology when surgically addressing degenerative lumbar pathologies such as degenerative disc disease and spondylolisthesis.
-
➤
The distribution of caudal lordosis (L4-S1) and cranial lordosis (L1-L4) as a percentage of global lordosis varies by pelvic incidence (PI), with cephalad lordosis increasing its contribution to total lordosis as PI increases.
-
➤
Spinal fusion may lead to iatrogenic deformity if performed without attention to lordosis magnitude and location in the lumbar spine.
-
➤
A solid foundation of knowledge with regard to optimal spinal sagittal alignment is beneficial when performing lumbar spinal surgery, and thoughtful planning and execution of lumbar fusions with a focus on alignment may improve patient outcomes.
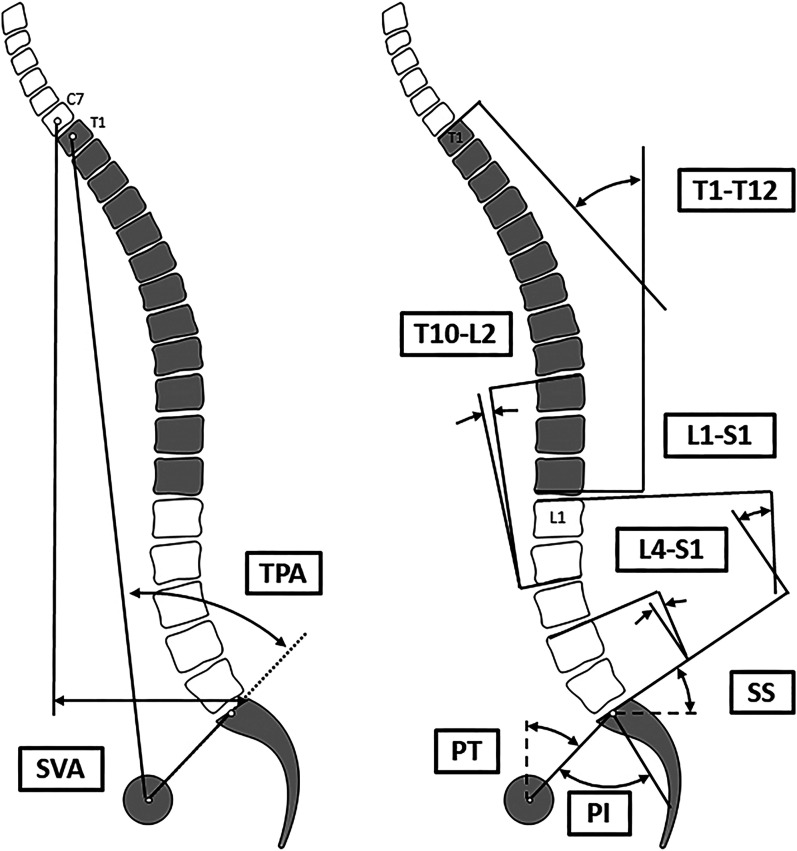
The concept of spinopelvic alignment was described by Jean Dubousset as a “cone of economy” where the axial skeleton balances in line above the pelvis, lower limbs, and feet1. From this idea, an understanding of multiple important sagittal alignment parameters (Fig. 1) emerged in the spinal deformity literature over the past few decades, and the importance of a harmonious spine is now well established2. However, in the degenerative spine realm, careful consideration of the sagittal plane was not widely considered when planning operations for degenerative pathology. Recently, this paradigm has begun to shift, and the importance of sagittal alignment in assessment and treatment of patients with degenerative spinal conditions is becoming increasingly recognized. With the increased volume of lumbar fusions, and the need for better short-term and long-term patient outcomes, alignment concepts are emerging to possibly provide solutions to improve the outcomes and longevity of short construct fusions3-5. This review will discuss the importance of sagittal plane alignment in the setting of degenerative lumbar disease based on recent literature, with the aim of assisting surgeons in improving outcomes following surgical management of degenerative spinal pathology.
Fig. 1.
Schematic representation of radiographic parameters used for sagittal alignment assessment. TPA = T1-pelvic angle, SVA = sagittal vertical axis, T1-T12 = thoracic kyphosis, T10-L2 = thoracolumbar junction, L1-S1 = LL, and L4-S1 = distal LL or lower LL.
Sagittal Alignment and Degenerative Lumbar Pathologies
The implications of abnormal spinopelvic alignment in degenerative lumbar pathologies have been recently investigated6-10. Patients with higher pelvic incidence (PI) are more prone to experiencing lumbar spondylolisthesis, and those with extremely high PI values have a greater likelihood of developing 2-level disease10-20. Although the literature has been conflicting with regard to the impact of degenerative spondylolisthesis on global lumbar lordosis (LL), a nuanced evaluation found that patients with degenerative spondylolisthesis have decreased LL in the caudal L4-S1 levels and increased LL in the cranial L1-L3 levels11,13,16,18.
Sagittal alignment is also a factor in the clinical presentation of patients with spinal stenosis. However, in comparison with degenerative spondylolisthesis, where the anatomy exacerbates the clinical symptoms, the opposite appears to be the case in spinal stenosis. The loss of LL and increased sagittal vertical axis in patients with spinal stenosis are, in some cases, a compensatory mechanism in the flexible spine in order to open the neural foramen, although it should be noted that spinal stenosis occurs at different rates in patients depending on spinopelvic morphology8,21. As malalignment progresses in spinal stenosis, these patients maintain their pelvic tilt (PT) and compensate by shifting the pelvis posteriorly, with pelvic retroversion considered a late finding in this cohort of patients22. This differs from patients with primary adult spinal deformity, who use pelvic retroversion as an earlier means of compensation22. For patients with lumbar spinal stenosis, simple lumbar decompression can potentially improve spinopelvic alignment, with Ham et al. demonstrating improvement in relative spinopelvic measures in patients with preoperative pain within 10 minutes of standing23. The application of sagittal alignment principles to lumbar degenerative disease may help to improve outcomes because one of the main issues facing degenerative spine surgery is the increased prevalence of overcorrected and undercorrected lordosis in patients with short-segment fusions24. This is partly due to the ambiguity in defining lordosis targets for any given lumbar disc-vertebral segment. Evaluating the contribution to lordosis from each segment is important, as it varies from one subject to another, even in the non-pathologic spine. The following sections will delve deeper into the normal lordosis and shape of the lumbar spine and the impact of age and degeneration on both.
LL, the Body, and the Disc
LL, a critical component of the sagittal plane for maintaining an upright posture, is primarily formed by a combination of wedging of the lumbar vertebral bodies and intervertebral discs25-28. Vaz et al. demonstrated that more lordosis is achieved by intervertebral disc wedging than by vertebral body wedging27. Been et al. confirmed these results and noted a progression from increased dorsal (lordotic) wedging of the vertebral bodies in the lower lumbar spine to slight ventral (kyphotic) wedging of the upper lumbar spine as LL transitions to thoracic kyphosis28. This transition usually occurs at the L2 vertebra, although this is influenced by normal variations in sagittal alignment among humans. Additionally, variations in sagittal alignment also influence the relative proportions of lordosis generated from the body and the disc.
Roussouly et al. was the first to describe different lumbar spinal shapes based on normal variations in sacral slope (SS)25. In this work, Roussouly et al.25 redemonstrated an earlier finding from Legaye et al.29, showing global LL to significantly correlate with SS and PI, although a weaker correlation was demonstrated with PI. PI describes the orientation of the sacrum within the ilium. PI increases throughout skeletal maturation, with anterior-posterior growth of the pelvis, before becoming fixed in adulthood, with a range from 20° to >80° in normative data30. PI is thought to remain unchanged in adulthood, even with degeneration31-33. However, recent data revealed that PI actually may change over time via increased stress over the sacroiliac joints and subsequent remodeling of these joints and the sacral end plate, a process evident in patients with long fusions involving S1 as the lower instrumented vertebra34,35. Nevertheless, given the relative stability of PI compared with SS, LL is often evaluated relative to PI25. In asymptomatic subjects, PI affects the magnitude and distribution of LL; subjects with a larger PI have a more horizontal sacrum, a higher SS, and a larger LL with a more proximal apex compared with those with a low PI34,36,37. LL is also correlated with thoracic kyphosis; in particular, the upper arch of the lordosis is often equal to the lower arch of the thoracic kyphosis38,39. Therefore, it is favorable to evaluate LL based on its relationship with PI and thoracic kyphosis.
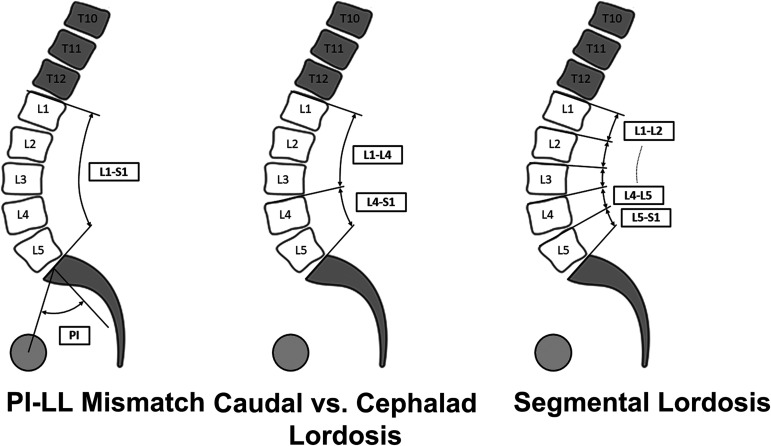
Defining Normal Global, Regional, and Segmental LL
Defining surgical targets for LL has evolved over the years. The historical target was “as much lordosis as possible.” This continued until several authors, including Schwab et al. and Lafage et al., proposed matching PI to LL within 10°, which has been shown to improve outcomes even in surgical procedures for degenerative pathology35,40-51. It has been suggested to correct LL to PI + 10° if the PI is low and to PI − 10° if the PI is high52. Since then, this simple concept of PI–LL has progressed into targeting the ideal lumbar apex and distribution of lordosis between the cephalad and caudal segments36,53. Those measurements are of particular importance in the degenerative lumbar spine because patients may have a poor distribution of LL even though global lordosis may appear normal. In one formative study, Pesenti et al. helped to define the regional distribution of lordosis in normal subjects34. The distribution of caudal lordosis (L4-S1) and cephalad lordosis (L1-L4) as a percentage of global lordosis varies by PI, with cephalad lordosis increasing its contribution to total lordosis as PI increases34. Their study also built on the work by Roussouly et al.25 and redemonstrated that, as PI increases, the apex of lordosis migrates to a more cephalad location, with a concomitant increase in the magnitude of proximal lordosis. Therefore, lordosis of the lumbar segments above and below the apex became better appreciated. It is important to note that authors have differed in their definitions of caudal and cephalad lordosis. Roussouly et al. defined cephalad lordosis as the lordosis proximal to the apex, which varies by PI25. However, to simplify the concept, Pesenti et al. analyzed lordosis within fixed boundaries of L1-L4 and L4-S1 (Fig. 2)34. The application of these measurements in degenerative spine diseases has been shown to reduce the risk of postoperative malalignment, adjacent segment disease, and revision surgery24,54-56. Recent studies have furthered the understanding of a harmonious sagittal plane, reporting the mean segmental lordosis values based on PI34,35. Table I includes the mean segmental lordosis per PI category; these values were extrapolated from recent normative segmental lordosis publications34,35. The table provides a general reference for surgical planning; however, surgical planning should be personalized for each patient’s spinopelvic anatomy. For example, in cases of low PI, it can be normal for the proximal lumbar vertebrae to be kyphotic, and aiming for a neutral T10-L2 alignment would be appropriate for most patients.
Fig. 2.
Evaluating global LL (left), regional LL (middle), and segmental LL (right).
TABLE I.
Mean Segmental Sagittal Alignment Values for the Lumbar and Thoracolumbar Spinal Regions*
| PI Category | T10-L2 | L1-L2 | L2-L3 | L3-L4 | L4-L5 | L5-S1 |
|---|---|---|---|---|---|---|
| 40° | −6.9° | 1.7° | 4.4° | 9.5° | 15° | 17.5° |
| 50° | −4.3° | 1.7° | 6.2° | 10.1° | 15° | 20° |
| 60° | −4.3° | 3.1° | 7.9° | 11.2° | 15° | 20° |
| 70° | 2.1° | 4.9° | 9.2° | 15.4° | 15° | 20° |
| 80° | 2.1° | 5.5° | 11.9° | 17° | 19° | 20° |
| 90° | 2.1° | 7.3° | 14.6° | 12.9° | 22° | 20° |
These data should be interpreted with caution, as the values are means and thus may not be prescriptive for every patient.
Impact of Age and Degeneration on LL
Prost et al. examined the correlation between age and sagittal alignment of the spine in asymptomatic volunteers57. They found that, in individuals with low PI, there was a global decrease in LL in both cephalad and caudal segments; in contrast, in individuals with high PI, more prominent loss of caudal lordosis was associated with increased PT and more prominent loss of cephalad lordosis was associated with increasing kyphosis and positive sagittal malalignment57. These findings have important implications and call for thorough assessment of PI and caudal and cephalad lordosis, with a surgical plan that aims to restore appropriate segmental lordosis based on spinopelvic anatomy58.
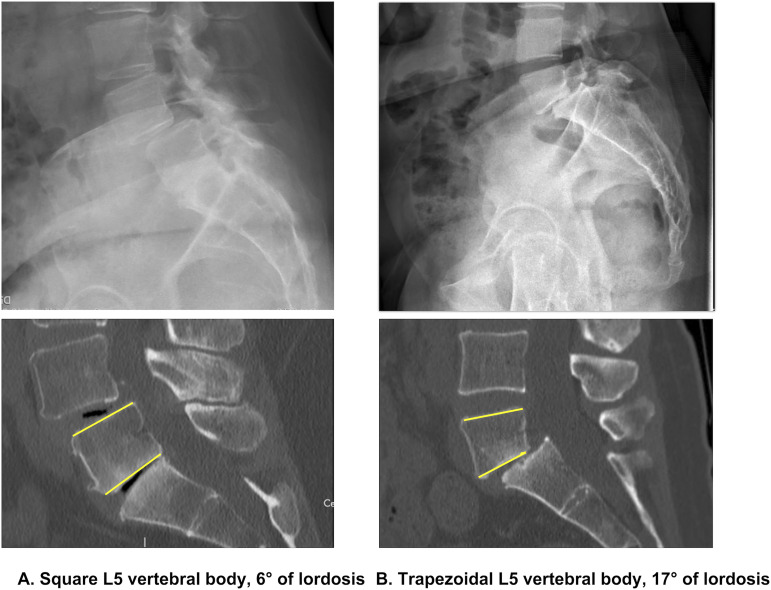
In the degenerative setting, decreased global LL (or flattening of the lumbar spine) can occur by squaring of the intervertebral discs from their previous dorsal wedging and degeneration of the intervertebral discs to a more kyphotic alignment, leading to alteration of segmental lordosis59-62. Thus, measurement of vertebral body wedging and intervertebral disc lordosis of the segment of interest will inform decisions with regard to the type of interbody device required in terms of magnitude of lordosis, height, location of the end-plate contact, and need for posterior compression of that segment25. For example, in isthmic spondylolisthesis, as the L5 vertebra translates anteriorly, the vertebral body has been shown to become more trapezoidal, the sacral dome becomes more dysplastic, and relative kyphosis develops at the intervertebral disc and lower lumbar segments59. Therefore, careful assessment of the L5 body and L5-S1 segmental alignment is important in surgical decision-making and choices of implants and techniques (Fig. 3). Overall, when performing a short-segment lumbar fusion, one should always be aware of the magnitude of lordosis in the level of interest, as well as in adjacent segments. Degenerative changes altering the magnitude of lordosis in 1 segment induce compensatory changes in other segments to maintain sagittal alignment. Thus, global lordosis may appear normal, but focused analysis will reveal the suboptimal lumbar distribution between cephalad and caudal segments63,64. The implications of this concept may explain some biomechanical failures in short lumbar fusions that include both pathologic segments and those in compensated positions; however, there have been no data yet to support this hypothesis. Similarly, fusion might be indicated for a hyperlordotic-compensated segment with resultant stenosis; recognizing this phenomenon enables surgeons to fuse in a proper segmental lordosis. In this scenario, the alignment goal might be to reduce (rather than increase) lordosis in that segment.
Fig. 3.
Two examples of L5 vertebral body shapes that could factor into restoring segmental lordosis. The yellow lines indicate L5 vertebral end plates.
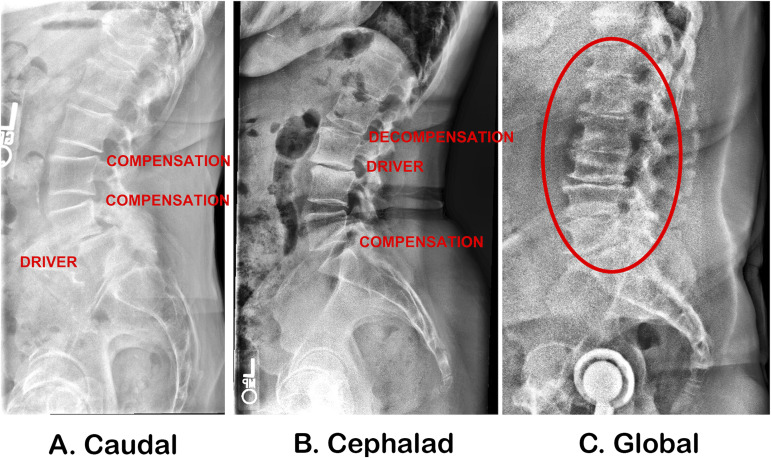
Although the prior argument emphasizes the importance of sagittal alignment in the degenerative spine, alignment itself is not an indication for surgical intervention. Patients’ physical examination, symptomology, and clinical correlation of radiographic findings to patient-reported outcome measures remain the first line to indicate patients for a surgical procedure. Therefore, it is imperative to note that we do not encourage fusing additional segments to optimize the sagittal plane, but rather encourage a critical analysis of segmental lordosis throughout the lumbar spine and an aim of restoring the surgically indicated levels to the normative targets. Figure 4 illustrates 3 types of degenerative spine conditions; note the associated loss of segmental lordosis, cephalad or caudal, and hyperlordotic compensation in adjacent segments65-67.
Fig. 4.
Three types of degenerative lumbar disease from a sagittal alignment standpoint: loss of lordosis in caudal segments (Fig. 4-A), cephalad segments (Fig. 4-B), and globally throughout the lumbar spine (Fig. 4-C). L2-L3 and L3-L4 compensatory hyperlordosis is noted in Figure 4-A, L2-L3 decompensation (rotational failure) and L5-S1 compensatory hyperlordosis are noted in Figure 4-B, and no compensation due to regional degeneration (red oval) is noted in Figure 4-C.
Why Should Surgeons Preserve or Restore the Sagittal Plane in Degenerative Lumbar Surgery?
The decision to fuse the lumbar spine for degenerative pathology can be challenging. We believe that there are 3 important concepts to which to adhere (Table II).
TABLE II.
Recommendations for Restoring the Sagittal Plane in Degenerative Lumbar Surgery
| Benefits of Ideal Segmental Lordosis | Grade of Recommendation* |
|---|---|
| No creation of lumbar segmental malalignment during spinal fusion surgery | B |
| Prevention of adjacent segment disease | B |
| Reduction of the incidence of low back pain | B |
According to Wright112, grade A indicates good evidence (Level-I studies with consistent findings) for or against recommending intervention; grade B, fair evidence (Level-II or III studies with consistent findings) for or against recommending intervention; grade C, poor-quality evidence (Level-IV or V studies with consistent findings) for or against recommending intervention; and grade I, insufficient or conflicting evidence not allowing a recommendation for or against intervention.
The first concept is to not create malalignment. The spinal surgery community remains poor at restoring alignment, with 1 study showing that 28% of patients remained malaligned following short-segment fusion for degenerative lumbar pathologies68. Despite advances in segmental fixation and the power of newer interbody devices, there remains a high prevalence of iatrogenic sagittal plane deformity following short-segment fusions69-72. Subsequent management of these patients can include the need for invasive procedures such as pedicle subtraction osteotomies, with complication rates as high as 60%. This indicates the importance of careful preoperative planning at the index surgical procedure68.
Specific approaches to the spine and the use of selected interbody devices can profoundly impact spinopelvic parameters and regional alignment. Anterior lumbar interbody fusion (ALIF) is a reliable procedure that can provide powerful correction exceeding 30° of segmental lordosis; this may be vital at the L5-S1 segment. However, moving cranially in the spine can make the approach for ALIF cage placement challenging. Lateral approach techniques such as lateral lumbar interbody fusion (LLIF) and oblique lumbar interbody fusion (OLIF) can provide access to upper lumbar disc spaces and provide a substantial increase in segmental lordosis when combined with an anterior column realignment approach, compared with posterior-based approaches73-77. LLIF and OLIF can be combined with a posterior approach for posterior-column osteotomies to further improve segmental and global alignment78,79. Posterior-based approaches include transforaminal lumbar interbody fusion (TLIF) and posterior lumbar interbody fusion (PLIF). Multiple studies have shown that surgeons and implants vary in their ability to achieve lordosis at an individual segmental level utilizing TLIF44,80,81. Successful restoration (or retention) of segmental lordosis can be challenging via TLIF, but may be achieved with the aid of dedicated spinal tables, anteriorly placed TLIF cages, posterior column osteotomies, and compression posteriorly before the final tightening of the set screws82,83. Therefore, after the ideal segmental lordosis and the overall lumbar shape and apex have been chosen, choosing the proper surgical technique and implant may optimize achievement of alignment goals for the individual lumbar segments84.
In vertebral levels that already have substantial disc height and segmental lordosis, it can be challenging to further increase lordosis, and interbody device placement may induce kyphosis without appropriate attention to technical detail85. Bilateral facetectomy, anterior cage placement with compression across the posterior pedicle screws, and the use of expandable cages have been shown to mitigate these risks, although surgeons should be aware of the increased risk of subsidence with expandable cage placement86,87. Furthermore, iatrogenic foraminal stenosis and inadequate restoration of foraminal height are potential issues with lordosis restoration that need to be carefully considered. In general, and regardless of the approach and type of interbody device utilized, targeting segmental lordosis ideals should be the goal from an alignment perspective. It is important to note that restoring the segmental lordosis or achieving ideal alignment does not mean fusing an additional level, but rather ensuring that the indicated segment has adequate lordosis by increasing it, maintaining it, or sometimes decreasing it (Table I).
The second concept is to aim to prevent the development of adjacent segment disease. Sagittal malalignment may be a risk factor for developing adjacent segment disease, even following short-segment lumbar fusion for degenerative pathology. This is likely due to altered spinal biomechanics and stress concentration at the adjacent disc segments. This point was exemplified by Herrington et al., who showed that surgically reducing lordosis at L4-L5 led to increased focal lordosis at L3-L4 and a higher reoperation rate for adjacent segment disease at that location55. Similarly, Bari et al.24 and Zheng et al.56 demonstrated that, postoperatively, patients in whom <50% of the total lordosis was generated at L4-S1 experienced higher revision rates compared with patients with an adequate distribution of lordosis. Other studies have corroborated these findings, demonstrating the importance of sagittal alignment in lowering the risk of adjacent segment disease after lumbar fusion for degenerative pathology88-93. Although multiple studies have found an association between adjacent segment disease and sagittal alignment, Toivonen et al. found no association in their study with 10-year clinical outcome follow-up but only 3-month postoperative radiographic follow-up94. Hsieh et al. reported similar findings in a smaller study sample without a control group95. Furthermore, Hsieh et al. focused on global LL using PI–LL, instead of assessing segmental lordosis, which may have misclassified patients with compensatory changes adjacent to the indicated levels95.
The goal should not simply be to obtain as much disc height or segmental lordosis as possible, but to follow segmental lordosis targets96. Thus, harmonious restoration of level-specific sagittal parameters may help to reduce the risk of adjacent segment disease after lumbar fusion. Other factors that may contribute to the development of adjacent segment disease include preexisting facet degeneration cranial to the fusion, increased preoperative PT that does not correct after fusion, inadequate restoration of lordosis, advanced age, osteoporosis, higher body mass index, and longer fusion length97-102.
The third concept is to decrease the incidence of low back pain and spine-related disability by improving spinopelvic alignment parameters. In cases where spinopelvic alignment improves after isolated decompression, the associated back pain experienced by patients also improves103. This finding has carried over into cases of fusion, where restoration of both segmental lordosis and PT has resulted in decreased low back pain104. More globally, the correction of PI–LL as well as a positive sagittal vertical axis have also been shown to aid in the reduction of back pain for degenerative pathologies105. Back pain and fatigue in patients with spinopelvic malalignment may be driven by compensatory changes that occur outside of the fusion construct due to flattening of the thoracic kyphosis, elevated PT and posterior shift, knee flexion, cervical alignment compensation, and muscle fatigue due to increased energy expenditure106-108.
Case Example
Brief History
A 73-year-old patient presented with progressive low back pain, unresponsive to conservative measures, and bilateral lower-extremity radiculopathy. Magnetic resonance imaging (MRI) scans revealed moderate central and neuroforaminal stenosis bilaterally at the L4-L5 and L5-S1 levels. The preoperative patient-reported outcome measures were an Oswestry Disability Index (ODI) of 40, EuroQol Index Score (estimated health utility) of 0.60, Patient-Reported Outcomes Measurement Information System (PROMIS) Global Mental Health (GMH) of 50.80 and Global Physical Health (GPH) of 37.40, and Moderate to Vigorous Physical Activity (MVPA), determined from the Exercise Vital Sign (EVS), of 90.00.
Preoperative Radiographic Alignment
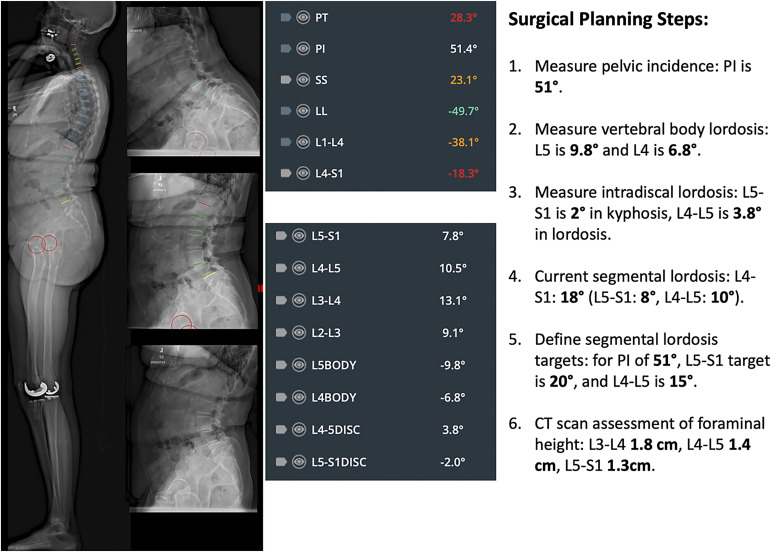
Obtaining imaging that captures the entire spine and the lower extremities is preferred to assess any compensatory changes that have occurred. Lumbar and full-body lateral free-standing radiographs revealed L4-L5 and L5-S1 grade-2 spondylolisthesis, dynamic in nature when compared between flexion and extension radiographs. In addition, compensatory L3-L4 lordosis and L2-L3 hyperlordosis were noted. The patient had an L1-L4 lordosis of 38.1° and an L4-S1 lordosis of 18.3°, indicating a maldistribution of lordosis (Fig. 5). The PT was 28°, indicating compensatory pelvic retroversion.
Fig. 5.
Preoperative sagittal alignment, with spinopelvic parameters. CT = computed tomography.
Surgical Planning
Preoperatively
To obtain 20° of lordosis at L5-S1, an ALIF device with 18° of lordosis was provisionally planned, pending confirmation of a preserved shape rather than plastic deformation of the L5 body intraoperatively (the preoperative L5 body lordosis was approximately 10°, but it was mostly driven by the concavity of the inferior end plate). A 12° ALIF device was planned at L4-L5 to obtain the segmental goal of 15°, pending intraoperative assessment of end-plate contact, as L4 vertebral body lordosis was only 7°. Finally, the baseline height difference between the L4-L5 and L5-S1 foramina was expected to factor into the heights of the cages (a 14-mm cage at L5-S1 compared with a 12-mm cage at L4-L5). We perform intraoperative measurements to ensure the achievement of segmental lordosis targets. Interbody device plans can be modified according to end-plate contact, reduction of spondylolisthesis, the impact on segmental lordosis, and lordosis gained from the cage. The decision was made to perform posterior instrumentation and fusion from L4 to the pelvis, and the plan was simulated via dedicated software; 5.5-mm titanium rods that could be prebent were requested.
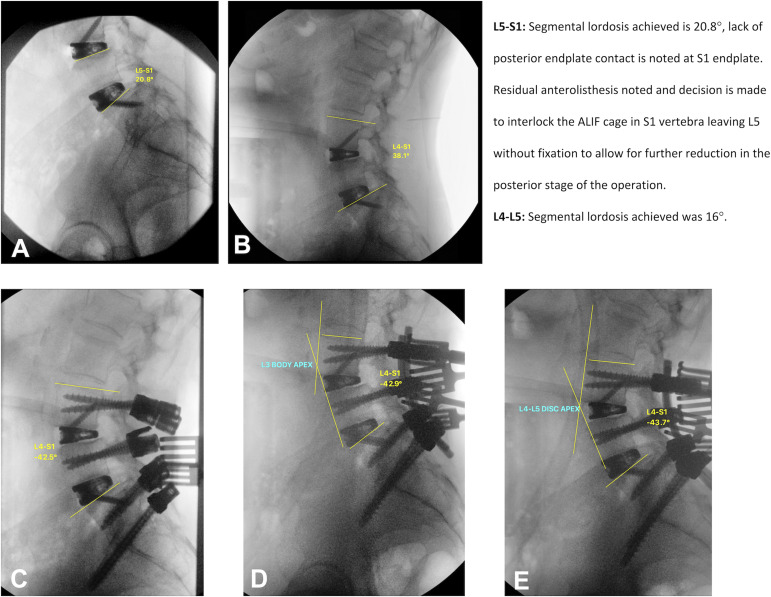
Intraoperatively
During the anterior stage of the operation, the anterior edge of the inferior end plate of the L5 body had plastically deformed, necessitating an 18° L5-S1 ALIF cage, whereas the L4-L5 plan remained a 12° cage. During the second stage, and in a prone position, intraoperative fluoroscopy revealed that 39° of L4-S1 lordosis was achieved, which was the ideal target based on the PI that the patient had. Following instrumentation, L4-S1 increased to 42°, which remained within an acceptable range of the target. To achieve better end-plate contact of the ALIF cages, the decision was made to compress the screws posteriorly by the final tightening of the L4 pedicle screws and the compression of the L5 and S1 screws (our preferred method of compression), which migrated the apex from the L4 body to the L4-L5 disc. Subsequently, S2-alar-iliac fixation was performed because of the magnitude of spondylolisthesis and lordosis correction (Fig. 6).
Fig. 6.
Intraoperative fluoroscopy during the anterior stage (Figs. 6-A and 6-B) and the posterior stage (Figs. 6-C, 6-D, and 6-E) of the surgical procedure.
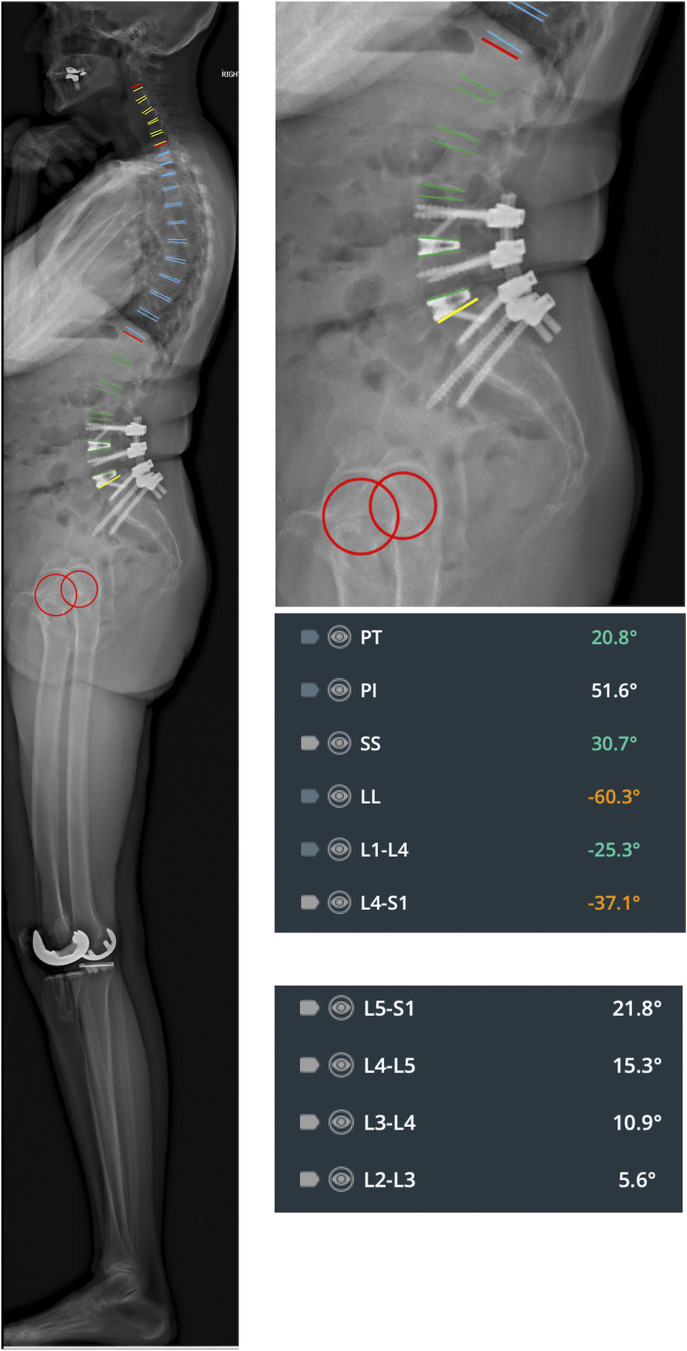
Postoperatively
Full-body standing EOS radiographs (EOS Imaging) revealed restoration of caudal and cephalad lordosis and relaxation of adjacent segment compensation at L2-L3 and L3-L4. Imaging also revealed relaxation of the PT. At the 1-year follow-up (Fig. 7), the patient was satisfied with the surgical procedure, and the postoperative patient-reported outcome measures were an ODI of 3, a EuroQol Index Score of 0.81, a GMH of 62.50, a GPH of 50.80, and an MVPA of 210.00.
Fig. 7.
Postoperative sagittal alignment, with spinopelvic parameters.
Future Directions
Sagittal alignment in degenerative spine disease will probably be the focus of numerous future studies. Future research could explore the impact of PI-adjusted relative spinopelvic measurements on outcomes following short-segment lumbar fusion, given their demonstrated benefits in adult spinal deformity correction109-111. Specifically, and more tailored to patients with spinal degeneration, there remains the need to investigate the impact of segmental lordosis surgical targets on patient-reported outcomes and rates of long-term complications and revision surgery. Restoring the shape of the lumbar spine requires carefully planning each lumbar fusion operation and tailoring interbody selection, rod contouring, and segmental correction to the patient’s need, primarily driven by the morphology of the pelvis.
Summary
Sagittal alignment of the degenerative lumbar spine is important for spinal surgeons to measure and assess prior to the surgical procedure. A detailed examination of segmental (level-specific) lordosis is likely more important in degenerative conditions than in spinal deformity, due to the performance of short fusions for degenerative conditions rather than long-segment deformity fusion crossing the spinal junctions. Importantly, sagittal realignment, in itself, is not an indication for longer fusions. Our preferred approach is foundational and focuses on proper LL distribution in the indicated levels, which may include maintenance, restoration, or even reduction of lordosis. The subtle deterioration of the sagittal profile in revision surgery is often overlooked. Chasing adjacent segment failure without analyzing the sagittal plane can lead to avoidable revisions. Thus, optimizing caudal lordosis, avoiding fusing cephalad segments with too much lordosis, and ensuring a proper thoracolumbar inflection point are integral concepts in realignment of the degenerative lumbar spine.
Footnotes
Investigation performed at Brown Spine Research Laboratory, Department of Orthopaedic Surgery, Warren Alpert Medical School, Brown University, Providence, Rhode Island
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/H867).
Contributor Information
Bassel G. Diebo, Email: dr.basseldiebo@gmail.com.
Mariah Balmaceno-Criss, Email: mariah_balmaceno-criss@brown.edu.
Renaud Lafage, Email: renaud.lafage@gmail.com.
Christopher L. McDonald, Email: christopher_mcdonald@brown.edu.
Daniel Alsoof, Email: alsoofd@gmail.com.
Sereen Halayqeh, Email: sereenhalaika99@gmail.com.
Kevin J. DiSilvestro, Email: kjdiso@gmail.com.
Eren O. Kuris, Email: eokuris@gmail.com.
Virginie Lafage, Email: virginie.lafage@gmail.com.
References
- 1.Hasegawa K, Dubousset JF. Cone of economy with the chain of balance-historical perspective and proof of concept. Spine Surg Relat Res. 2022. Apr 20;6(4):337-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iyer S, Sheha E, Fu MC, Varghese J, Cunningham ME, Albert TJ, Schwab FJ, Lafage VC, Kim HJ. Sagittal spinal alignment in adult spinal deformity: an overview of current concepts and a critical analysis review. JBJS Rev. 2018. May;6(5):e2. [DOI] [PubMed] [Google Scholar]
- 3.Cowan JA, Jr, Dimick JB, Wainess R, Upchurch GR, Jr, Chandler WF, La Marca F. Changes in the utilization of spinal fusion in the United States. Neurosurgery. 2006. Jul;59(1):15-20, discussion: 15-20. [DOI] [PubMed] [Google Scholar]
- 4.Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res. 2006. Feb;443(443):139-46. [DOI] [PubMed] [Google Scholar]
- 5.O’Lynnger TM, Zuckerman SL, Morone PJ, Dewan MC, Vasquez-Castellanos RA, Cheng JS. Trends for spine surgery for the elderly: implications for access to healthcare in North America. Neurosurgery. 2015. Oct;77(Suppl 4):S136-41. [DOI] [PubMed] [Google Scholar]
- 6.Mehta VA, Amin A, Omeis I, Gokaslan ZL, Gottfried ON. Implications of spinopelvic alignment for the spine surgeon. Neurosurgery. 2015. Mar;76(Suppl 1):S42-56, discussion S56. [DOI] [PubMed] [Google Scholar]
- 7.Pratali RR, Battisti R, Oliveira CEAS, Maranho DAC, Herrero CFPS. Correlation between the severity of the lumbar degenerative disease and sagittal spinopelvic alignment. Rev Bras Ortop (Sao Paulo). 2022. Feb 18;57(1):41-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zárate-Kalfópulos B, Reyes-Tarrago F, Navarro-Aceves LA, García-Ramos CL, Reyes-Sánchez AA, Alpízar-Aguirre A, Rosales-Olivarez LM. Characteristics of spinopelvic sagittal alignment in lumbar degenerative disease. World Neurosurg. 2019. Jun;126:e417-21. [DOI] [PubMed] [Google Scholar]
- 9.Lv X, Liu Y, Zhou S, Wang Q, Gu H, Fu X, Ding Y, Zhang B, Dai M. Correlations between the feature of sagittal spinopelvic alignment and facet joint degeneration: a retrospective study. BMC Musculoskelet Disord. 2016. Aug 15;17(1):341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007. Sep;16(9):1459-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai Q, Gao T, Lv X, Liu X, Wan Z, Dai M, Zhang B, Nie T. Correlation between the sagittal spinopelvic alignment and degenerative lumbar spondylolisthesis: a retrospective study. BMC Musculoskelet Disord. 2018. May 16;19(1):151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lim JK, Kim SM. Comparison of sagittal spinopelvic alignment between lumbar degenerative spondylolisthesis and degenerative spinal stenosis. J Korean Neurosurg Soc. 2014. Jun;55(6):331-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Funao H, Tsuji T, Hosogane N, Watanabe K, Ishii K, Nakamura M, Chiba K, Toyama Y, Matsumoto M. Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis. Eur Spine J. 2012. Nov;21(11):2181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferrero E, Ould-Slimane M, Gille O, Guigui P; French Spine Society (SFCR). Sagittal spinopelvic alignment in 654 degenerative spondylolisthesis. Eur Spine J. 2015. Jun;24(6):1219-27. [DOI] [PubMed] [Google Scholar]
- 15.Lim JK, Kim SM. Difference of sagittal spinopelvic alignments between degenerative spondylolisthesis and isthmic spondylolisthesis. J Korean Neurosurg Soc. 2013. Feb;53(2):96-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schuller S, Charles YP, Steib JP. Sagittal spinopelvic alignment and body mass index in patients with degenerative spondylolisthesis. Eur Spine J. 2011. May;20(5):713-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barrey C, Jund J, Perrin G, Roussouly P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery. 2007. Nov;61(5):981-6. [DOI] [PubMed] [Google Scholar]
- 18.Aono K, Kobayashi T, Jimbo S, Atsuta Y, Matsuno T. Radiographic analysis of newly developed degenerative spondylolisthesis in a mean twelve-year prospective study. Spine (Phila Pa 1976). 2010. Apr 15;35(8):887-91. [DOI] [PubMed] [Google Scholar]
- 19.Kobayashi H, Endo K, Sawaji Y, Matsuoka Y, Nishimura H, Murata K, Takamatsu T, Suzuki H, Aihara T, Yamamoto K. Global sagittal spinal alignment in patients with degenerative low-grade lumbar spondylolisthesis. J Orthop Surg (Hong Kong). 2019. Sep-Dec;27(3):2309499019885190. [DOI] [PubMed] [Google Scholar]
- 20.Ferrero E, Simon AL, Magrino B, Ould-Slimane M, Guigui P. Double-level degenerative spondylolisthesis: what is different in the sagittal plane? Eur Spine J. 2016. Aug;25(8):2546-52. [DOI] [PubMed] [Google Scholar]
- 21.Buckland AJ, Ramchandran S, Day L, Bess S, Protopsaltis T, Passias PG, Diebo BG, Lafage R, Lafage V, Sure A, Errico TJ. Radiological lumbar stenosis severity predicts worsening sagittal malalignment on full-body standing stereoradiographs. Spine J. 2017. Nov;17(11):1601-10. [DOI] [PubMed] [Google Scholar]
- 22.Buckland AJ, Vira S, Oren JH, Lafage R, Harris BY, Spiegel MA, Diebo BG, Liabaud B, Protopsaltis TS, Schwab FJ, Lafage V, Errico TJ, Bendo JA. When is compensation for lumbar spinal stenosis a clinical sagittal plane deformity? Spine J. 2016. Aug;16(8):971-81. [DOI] [PubMed] [Google Scholar]
- 23.Ham CH, Park YK, Kim JH, Kwon WK, Kim DW, Moon HJ. Characteristics of sagittal spinopelvic alignment changes after symptom relief after simple lumbar decompression. Neurosurgery. 2022. Aug 1;91(2):331-8. [DOI] [PubMed] [Google Scholar]
- 24.Bari TJ, Heegaard M, Bech-Azeddine R, Dahl B, Gehrchen M. Lordosis Distribution Index in short-segment lumbar spine fusion - can ideal lordosis reduce revision surgery and iatrogenic deformity? Neurospine. 2021. Sep;18(3):543-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). 2005. Feb 1;30(3):346-53. [DOI] [PubMed] [Google Scholar]
- 26.Gracovetsky SA, Iacono S. Energy transfers in the spinal engine. J Biomed Eng. 1987. Apr;9(2):99-114. [DOI] [PubMed] [Google Scholar]
- 27.Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002. Feb;11(1):80-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Been E, Barash A, Marom A, Kramer PA. Vertebral bodies or discs: which contributes more to human-like lumbar lordosis? Clin Orthop Relat Res. 2010. Jul;468(7):1822-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Odland K, Yson S, Polly DW, Jr. Wide anatomical variability of PI normative values within an asymptomatic population: a systematic review. Spine Deform. 2023. May;11(3):559-66. [DOI] [PubMed] [Google Scholar]
- 31.Mac-Thiong JM, Berthonnaud E, Dimar JR, 2nd, Betz RR, Labelle H. Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976). 2004. Aug 1;29(15):1642-7. [DOI] [PubMed] [Google Scholar]
- 32.Abelin-Genevois K, Idjerouidene A, Roussouly P, Vital JM, Garin C. Cervical spine alignment in the pediatric population: a radiographic normative study of 150 asymptomatic patients. Eur Spine J. 2014. Jul;23(7):1442-8. [DOI] [PubMed] [Google Scholar]
- 33.Hou C, Chen K, Chen Y, Zhou T, Yang M, Li M. Assessment of sagittal spinopelvic alignment in asymptomatic Chinese juveniles and adolescents: a large cohort study and comparative meta-analysis. J Orthop Surg Res. 2021. Nov 2;16(1):656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pesenti S, Lafage R, Stein D, Elysee JC, Lenke LG, Schwab FJ, Kim HJ, Lafage V. The amount of proximal lumbar lordosis is related to pelvic incidence. Clin Orthop Relat Res. 2018. Aug;476(8):1603-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Charles YP, Bauduin E, Pesenti S, Ilharreborde B, Prost S, Laouissat F, Riouallon G, Wolff S, Challier V, Obeid I, Boissière L, Ferrero E, Solla F, Le Huec JC, Bourret S, Faddoul J, Abi Lahoud GN, Fière V, Vande Kerckhove M, Campana M, Lebhar J, Giorgi H, Faure A, Sauleau EA, Blondel B; French Spine Surgery Society (SFCR). Variation of global sagittal alignment parameters according to gender, pelvic incidence, and age. Clin Spine Surg. 2022. Aug 1;35(7):E610-20. [DOI] [PubMed] [Google Scholar]
- 36.Anwar HA, Butler JS, Yarashi T, Rajakulendran K, Molloy S. Segmental pelvic correlation (SPeC): a novel approach to understanding sagittal plane spinal alignment. Spine J. 2015. Dec 1;15(12):2518-23. [DOI] [PubMed] [Google Scholar]
- 37.Mendoza-Lattes S, Ries Z, Gao Y, Weinstein SL. Natural history of spinopelvic alignment differs from symptomatic deformity of the spine. Spine (Phila Pa 1976). 2010. Jul 15;35(16):E792-8. [DOI] [PubMed] [Google Scholar]
- 38.Berthonnaud E, Labelle H, Roussouly P, Grimard G, Vaz G, Dimnet J. A variability study of computerized sagittal spinopelvic radiologic measurements of trunk balance. J Spinal Disord Tech. 2005. Feb;18(1):66-71. [DOI] [PubMed] [Google Scholar]
- 39.Sebaaly A, Silvestre C, Rizkallah M, Grobost P, Chevillotte T, Kharrat K, Roussouly P. Revisiting thoracic kyphosis: a normative description of the thoracic sagittal curve in an asymptomatic population. Eur Spine J. 2021. May;30(5):1184-9. [DOI] [PubMed] [Google Scholar]
- 40.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010. Dec 1;35(25):2224-31. [DOI] [PubMed] [Google Scholar]
- 41.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 2009. Aug 1;34(17):1828-33. [DOI] [PubMed] [Google Scholar]
- 42.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009. Aug 1;34(17):E599-606. [DOI] [PubMed] [Google Scholar]
- 43.Ames CP, Smith JS, Scheer JK, Bess S, Bederman SS, Deviren V, Lafage V, Schwab F, Shaffrey CI. Impact of spinopelvic alignment on decision making in deformity surgery in adults: a review. J Neurosurg Spine. 2012. Jun;16(6):547-64. [DOI] [PubMed] [Google Scholar]
- 44.Youn YH, Cho KJ, Na Y, Kim JS. Global sagittal alignment and clinical outcomes after 1-3 short-segment lumbar fusion in degenerative spinal diseases. Asian Spine J. 2022. Aug;16(4):551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eun IS, Son SM, Goh TS, Lee JS. Sagittal spinopelvic alignment after spinal fusion in degenerative lumbar scoliosis: a meta-analysis. Br J Neurosurg. 2020. Apr;34(2):176-80. [DOI] [PubMed] [Google Scholar]
- 46.Kakadiya DG, Gohil DK, Soni DY, Shakya DA. Clinical, radiological and functional results of transforaminal lumbar interbody fusion in degenerative spondylolisthesis. N Am Spine Soc J. 2020. Jun 13;2:100011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vazifehdan F, Karantzoulis VG, Igoumenou VG. Sagittal alignment assessment after short-segment lumbar fusion for degenerative disc disease. Int Orthop. 2019. Apr;43(4):891-8. [DOI] [PubMed] [Google Scholar]
- 48.Oikonomidis S, Meyer C, Scheyerer MJ, Grevenstein D, Eysel P, Bredow J. Lumbar spinal fusion of low-grade degenerative spondylolisthesis (Meyerding grade I and II): Do reduction and correction of the radiological sagittal parameters correlate with better clinical outcome? Arch Orthop Trauma Surg. 2020. Sep;140(9):1155-62. [DOI] [PubMed] [Google Scholar]
- 49.Bai H, Li Y, Liu C, Zhao Y, Zhao X, Lei W, Feng Y, Wu Z. Surgical management of degenerative lumbar scoliosis associated with spinal stenosis: does the PI-LL matter? Spine (Phila Pa 1976). 2020. Aug 1;45(15):1047-54. [DOI] [PubMed] [Google Scholar]
- 50.Kong LD, Zhang YZ, Wang F, Kong FL, Ding WY, Shen Y. Radiographic restoration of sagittal spinopelvic alignment after posterior lumbar interbody fusion in degenerative spondylolisthesis. Clin Spine Surg. 2016. Mar;29(2):E87-92. [DOI] [PubMed] [Google Scholar]
- 51.Phan K, Nazareth A, Hussain AK, Dmytriw AA, Nambiar M, Nguyen D, Kerferd J, Phan S, Sutterlin C, 3rd, Cho SK, Mobbs RJ. Relationship between sagittal balance and adjacent segment disease in surgical treatment of degenerative lumbar spine disease: meta-analysis and implications for choice of fusion technique. Eur Spine J. 2018. Aug;27(8):1981-91. [DOI] [PubMed] [Google Scholar]
- 52.Berjano P, Langella F, Ismael MF, Damilano M, Scopetta S, Lamartina C. Successful correction of sagittal imbalance can be calculated on the basis of pelvic incidence and age. Eur Spine J. 2014. Oct;23(Suppl 6):587-96. [DOI] [PubMed] [Google Scholar]
- 53.Kalidindi KKV, Sangondimath G, Bansal K, Vishwakarma G, Chhabra HS. Introduction of a novel “segmentation line” to analyze the variations in segmental lordosis, location of the lumbar apex, and their correlation with spinopelvic parameters in asymptomatic adults. Asian Spine J. 2022. Aug;16(4):502-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang M, Xu L, Chen X, Zhou Q, Du C, Yang B, Zhu Z, Wang B, Qiu Y, Sun X. Optimal reconstruction of sagittal alignment according to global alignment and proportion score can reduce adjacent segment degeneration after lumbar fusion. Spine (Phila Pa 1976). 2021. Feb 15;46(4):E257-66. [DOI] [PubMed] [Google Scholar]
- 55.Herrington BJ, Fernandes RR, Urquhart JC, Rasoulinejad P, Siddiqi F, Bailey CS. L3-L4 hyperlordosis and decreased lower lumbar lordosis following short-segment L4-L5 lumbar fusion surgery is associated with L3-L4 revision surgery for adjacent segment stenosis. Global Spine J. 2023. Jul 24:21925682231191414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zheng G, Wang C, Wang T, Hu W, Ji Q, Hu F, Li J, Chaudhary SK, Song K, Song D, Zhang Z, Hao Y, Wang Y, Li J, Zheng Q, Zhang X, Wang Y. Relationship between postoperative lordosis distribution index and adjacent segment disease following L4-S1 posterior lumbar interbody fusion. J Orthop Surg Res. 2020. Apr 3;15(1):129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Prost S, Blondel B, Bauduin E, Pesenti S, Ilharreborde B, Laouissat F, Riouallon G, Wolff S, Challier V, Obeid I, Boissière L, Ferrero E, Solla F, Le Huec JC, Bourret S, Faddoul J, Abi Lahoud GN, Fière V, Vande Kerckhove M, Campana M, Lebhar J, Giorgi H, Faure A, Sauleau EA, Charles YP; French Spine Surgery Society (SFCR). Do age-related variations of sagittal alignment rely on spinopelvic organization? An observational study of 1540 subjects. Global Spine J. 2023. Oct;13(8):2144-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lafage R, Obeid I, Liabaud B, Bess S, Burton D, Smith JS, Jalai C, Hostin R, Shaffrey CI, Ames C, Kim HJ, Klineberg E, Schwab F, Lafage V; International Spine Study Group. Location of correction within the lumbar spine impacts acute adjacent-segment kyphosis. J Neurosurg Spine. 2018. Oct 26;30(1):69-77. [DOI] [PubMed] [Google Scholar]
- 59.Hanson DS, Bridwell KH, Rhee JM, Lenke LG. Correlation of pelvic incidence with low- and high-grade isthmic spondylolisthesis. Spine (Phila Pa 1976). 2002. Sep 15;27(18):2026-9. [DOI] [PubMed] [Google Scholar]
- 60.Protopsaltis TS, Soroceanu A, Tishelman JC, Buckland AJ, Mundis GM, Jr, Smith JS, Daniels A, Lenke LG, Kim HJ, Klineberg EO, Ames CP, Hart RA, Bess S, Shaffrey CI, Schwab FJ, Lafage V; International Spine Study Group (ISSG). Should sagittal spinal alignment targets for adult spinal deformity correction depend on pelvic incidence and age? Spine (Phila Pa 1976). 2020. Feb 15;45(4):250-7. [DOI] [PubMed] [Google Scholar]
- 61.Aoki Y, Kubota G, Inoue M, Takahashi H, Watanabe A, Nakajima T, Sato Y, Nakajima A, Saito J, Eguchi Y, Orita S, Fukuchi H, Sakai T, Ochi S, Yanagawa N, Nakagawa K, Ohtori S. Age-specific characteristics of lumbopelvic alignment in patients with spondylolysis: how bilateral L5 spondylolysis influences lumbopelvic alignment during the aging process. World Neurosurg. 2021. Mar;147:e524-32. [DOI] [PubMed] [Google Scholar]
- 62.Asai Y, Tsutsui S, Oka H, Yoshimura N, Hashizume H, Yamada H, Akune T, Muraki S, Matsudaira K, Kawaguchi H, Nakamura K, Tanaka S, Yoshida M. Sagittal spino-pelvic alignment in adults: the Wakayama Spine Study. PLoS One. 2017. Jun 6;12(6):e0178697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhou Z, Hou C, Li D, Si J. The pelvic radius technique in the assessment of spinopelvic sagittal alignment of degenerative spondylolisthesis and lumbar spinal stenosis. J Orthop Sci. 2018. Nov;23(6):902-7. [DOI] [PubMed] [Google Scholar]
- 64.Chuang CY, Liaw MY, Wang LY, Huang YC, Pong YP, Chen CW, Wu RW, Lau YC. Spino-pelvic alignment, balance, and functional disability in patients with low-grade degenerative lumbar spondylolisthesis. J Rehabil Med. 2018. Nov 7;50(10):898-907. [DOI] [PubMed] [Google Scholar]
- 65.Wang Q, Sun CT. Characteristics and correlation analysis of spino-pelvic sagittal parameters in elderly patients with lumbar degenerative disease. J Orthop Surg Res. 2019. May 9;14(1):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yang X, Kong Q, Song Y, Liu L, Zeng J, Xing R. The characteristics of spinopelvic sagittal alignment in patients with lumbar disc degenerative diseases. Eur Spine J. 2014. Mar;23(3):569-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ogon I, Takashima H, Morita T, Oshigiri T, Terashima Y, Yoshimoto M, Takebayashi T, Yamashita T. Association between spinopelvic alignment and lumbar intervertebral disc degeneration quantified with magnetic resonance imaging T2 mapping in patients with chronic low back pain. Spine Surg Relat Res. 2019. Nov 1;4(2):135-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Leveque JA, Segebarth B, Schroerlucke SR, Khanna N, Pollina J, Jr, Youssef JA, Tohmeh AG, Uribe JS. A multicenter radiographic evaluation of the rates of preoperative and postoperative malalignment in degenerative spinal fusions. Spine (Phila Pa 1976). 2018. Jul 1;43(13):E782-9. [DOI] [PubMed] [Google Scholar]
- 69.Wiggins GC, Ondra SL, Shaffrey CI. Management of iatrogenic flat-back syndrome. Neurosurg Focus. 2003. Sep 15;15(3):E8. [DOI] [PubMed] [Google Scholar]
- 70.Boody BS, Rosenthal BD, Jenkins TJ, Patel AA, Savage JW, Hsu WK. Iatrogenic flatback and flatback syndrome: evaluation, management, and prevention. Clin Spine Surg. 2017. May;30(4):142-9. [DOI] [PubMed] [Google Scholar]
- 71.Potter BK, Lenke LG, Kuklo TR. Prevention and management of iatrogenic flatback deformity. J Bone Joint Surg Am. 2004. Aug;86(8):1793-808. [DOI] [PubMed] [Google Scholar]
- 72.Gottfried ON, Daubs MD, Patel AA, Dailey AT, Brodke DS. Spinopelvic parameters in postfusion flatback deformity patients. Spine J. 2009. Aug;9(8):639-47. [DOI] [PubMed] [Google Scholar]
- 73.Nakashima H, Kanemura T, Satake K, Ishikawa Y, Ouchida J, Segi N, Yamaguchi H, Imagama S. Changes in sagittal alignment following short-level lumbar interbody fusion: comparison between posterior and lateral lumbar interbody fusions. Asian Spine J. 2019. Dec 31;13(6):904-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nakashima H, Kanemura T, Satake K, Ishikawa Y, Ouchida J, Segi N, Yamaguchi H, Imagama S. Comparative radiographic outcomes of lateral and posterior lumbar interbody fusion in the treatment of degenerative lumbar kyphosis. Asian Spine J. 2019. Jun;13(3):395-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Baghdadi YMK, Larson AN, Dekutoski MB, Cui Q, Sebastian AS, Armitage BM, Nassr A. Sagittal balance and spinopelvic parameters after lateral lumbar interbody fusion for degenerative scoliosis: a case-control study. Spine (Phila Pa 1976). 2014. Feb 1;39(3):E166-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Leveque JA, Drolet CE, Nemani V, Krause KL, Shen J, Rathore A, Baig Y, Louie PK. The impact of surgical approach on sagittal plane alignment in patients undergoing one- or two- level fusions for degenerative pathology: a multicenter radiographic evaluation 6 months following surgery. World Neurosurg. 2022. Aug;164:e311-7. [DOI] [PubMed] [Google Scholar]
- 77.Saadeh YS, Joseph JR, Jr, Smith BW, Kirsch MJ, Sabbagh AM, Park P. Comparison of segmental lordosis and global spinopelvic alignment after single-level lateral lumbar interbody fusion or transforaminal lumbar interbody fusion. World Neurosurg. 2019. Jun;126:e1374-8. [DOI] [PubMed] [Google Scholar]
- 78.Wu J, Ge T, Zhang N, Li J, Tian W, Sun Y. Posterior fixation can further improve the segmental alignment of lumbar degenerative spondylolisthesis with oblique lumbar interbody fusion. BMC Musculoskelet Disord. 2021. Feb 23;22(1):218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ahlquist S, Thommen R, Park HY, Sheppard W, James K, Lord E, Shamie AN, Park DY. Implications of sagittal alignment and complication profile with stand-alone anterior lumbar interbody fusion versus anterior posterior lumbar fusion. J Spine Surg. 2020. Dec;6(4):659-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pan W, Zhao JL, Xu J, Zhang M, Fang T, Yan J, Wang XH, Zhou Q. Lumbar alignment and patient-reported outcomes after single-level transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis with and without local coronal imbalance. J Neurosurg Spine. 2020. Dec 4;34(3):464-70. [DOI] [PubMed] [Google Scholar]
- 81.Zhu C, Qiu X, Zhuang M, Cheng D, Liu Z. Surgical outcomes of single-level transforaminal lumbar interbody fusion for degenerative spondylolisthesis with and without kyphotic alignment. World Neurosurg. 2018. Sep;117:e396-402. [DOI] [PubMed] [Google Scholar]
- 82.Toop N, Viljoen S, Baum J, Hatef J, Maggio D, Oosten J, Deistler K, Gilkey T, Close L, Farhadi HF, Grossbach AJ. Radiographic and clinical outcomes in one- and two-level transforaminal lumbar interbody fusions: a comparison of bullet versus banana cages. J Neurosurg Spine. 2021. Dec 17;36(6):918-27. [DOI] [PubMed] [Google Scholar]
- 83.Miyazaki M, Ishihara T, Abe T, Kanezaki S, Notani N, Kataoka M, Tsumura H. Effect of intraoperative position in single-level transforaminal lumbar interbody fusion at the L4/5 level on segmental and overall lumbar lordosis in patients with lumbar degenerative disease. Medicine (Baltimore). 2019. Sep;98(39):e17316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sabou S, Tseng THJ, Stephenson J, Siddique I, Verma R, Mohammad S. Correction of sagittal plane deformity and predictive factors for a favourable radiological outcome following multilevel posterior lumbar interbody fusion for mild degenerative scoliosis. Eur Spine J. 2016. Aug;25(8):2520-6. [DOI] [PubMed] [Google Scholar]
- 85.Alahmari A, Thornley P, Glennie A, Urquhart JC, Al-Jahdali F, Rampersaud R, Fisher C, Siddiqi F, Rasoulinejad P, Bailey CS. Preoperative disc angle is an important predictor of segmental lordosis after degenerative spondylolisthesis fusion. Global Spine J. 2022. Aug 10:21925682221118845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chang CC, Chou D, Pennicooke B, Rivera J, Tan LA, Berven S, Mummaneni PV. Long-term radiographic outcomes of expandable versus static cages in transforaminal lumbar interbody fusion. J Neurosurg Spine. 2020. Nov 13;34(3):471-80. [DOI] [PubMed] [Google Scholar]
- 87.Shiga Y, Orita S, Inage K, Sato J, Fujimoto K, Kanamoto H, Abe K, Kubota G, Yamauchi K, Eguchi Y, Inoue M, Kinoshita H, Aoki Y, Nakamura J, Matsuura Y, Hynes R, Furuya T, Koda M, Takahashi K, Ohtori S. Evaluation of the location of intervertebral cages during oblique lateral interbody fusion surgery to achieve sagittal correction. Spine Surg Relat Res. 2017. Nov 27;1(4):197-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001. Aug;10(4):314-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kiss L, Szoverfi Z, Bereczki F, Eltes PE, Szollosi B, Szita J, Hoffer Z, Lazary A. Impact of patient-specific factors and spinopelvic alignment on the development of adjacent segment degeneration after short-segment lumbar fusion. Clin Spine Surg. 2023. Aug 1;36(7):E306-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kim KH, Lee SH, Shim CS, Lee DY, Park HS, Pan WJ, Lee HY. Adjacent segment disease after interbody fusion and pedicle screw fixations for isolated L4-L5 spondylolisthesis: a minimum five-year follow-up. Spine (Phila Pa 1976). 2010. Mar 15;35(6):625-34. [DOI] [PubMed] [Google Scholar]
- 91.Rothenfluh DA, Mueller DA, Rothenfluh E, Min K. Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J. 2015. Jun;24(6):1251-8. [DOI] [PubMed] [Google Scholar]
- 92.Tempel ZJ, Gandhoke GS, Bolinger BD, Khattar NK, Parry PV, Chang YF, Okonkwo DO, Kanter AS. The influence of pelvic incidence and lumbar lordosis mismatch on development of symptomatic adjacent level disease following single-level transforaminal lumbar interbody fusion. Neurosurgery. 2017. Jun 1;80(6):880-6. [DOI] [PubMed] [Google Scholar]
- 93.Matsumoto T, Okuda S, Maeno T, Yamashita T, Yamasaki R, Sugiura T, Iwasaki M. Spinopelvic sagittal imbalance as a risk factor for adjacent-segment disease after single-segment posterior lumbar interbody fusion. J Neurosurg Spine. 2017. Apr;26(4):435-40. [DOI] [PubMed] [Google Scholar]
- 94.Toivonen LA, Mäntymäki H, Häkkinen A, Kautiainen H, Neva MH. Postoperative sagittal balance has only a limited role in the development of adjacent segment disease after lumbar spine fusion for degenerative lumbar spine disorders: a subanalysis of the 10-year follow-up study. Spine (Phila Pa 1976). 2022. Oct 1;47(19):1357-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hsieh MK, Kao FC, Chen WJ, Chen IJ, Wang SF. The influence of spinopelvic parameters on adjacent-segment degeneration after short spinal fusion for degenerative spondylolisthesis. J Neurosurg Spine. 2018. Oct;29(4):407-13. [DOI] [PubMed] [Google Scholar]
- 96.Kaito T, Hosono N, Mukai Y, Makino T, Fuji T, Yonenobu K. Induction of early degeneration of the adjacent segment after posterior lumbar interbody fusion by excessive distraction of lumbar disc space. J Neurosurg Spine. 2010. Jun;12(6):671-9. [DOI] [PubMed] [Google Scholar]
- 97.Lee CS, Hwang CJ, Lee SW, Ahn YJ, Kim YT, Lee DH, Lee MY. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J. 2009. Nov;18(11):1637-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yamasaki K, Hoshino M, Omori K, Igarashi H, Nemoto Y, Tsuruta T, Matsumoto K, Iriuchishima T, Ajiro Y, Matsuzaki H. Risk factors of adjacent segment disease after transforaminal inter-body fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 2017. Jan 15;42(2):E86-92. [DOI] [PubMed] [Google Scholar]
- 99.Ahn DK, Park HS, Choi DJ, Kim KS, Yang SJ. Survival and prognostic analysis of adjacent segments after spinal fusion. Clin Orthop Surg. 2010. Sep;2(3):140-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Min JH, Jang JS, Jung BJ, Lee HY, Choi WC, Shim CS, Choi G, Lee SH. The clinical characteristics and risk factors for the adjacent segment degeneration in instrumented lumbar fusion. J Spinal Disord Tech. 2008. Jul;21(5):305-9. [DOI] [PubMed] [Google Scholar]
- 101.Ankrah NK, Eli IM, Magge SN, Whitmore RG, Yew AY. Age, body mass index, and osteoporosis are more predictive than imaging for adjacent-segment reoperation after lumbar fusion. Surg Neurol Int. 2021. Sep 6;12:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sears WR, Sergides IG, Kazemi N, Smith M, White GJ, Osburg B. Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J. 2011. Jan;11(1):11-20. [DOI] [PubMed] [Google Scholar]
- 103.Ikuta K, Masuda K, Tominaga F, Sakuragi T, Kai K, Kitamura T, Senba H, Shidahara S. Clinical and radiological study focused on relief of low back pain after decompression surgery in selected patients with lumbar spinal stenosis associated with grade I degenerative spondylolisthesis. Spine (Phila Pa 1976). 2016. Dec 15;41(24):E1434-43. [DOI] [PubMed] [Google Scholar]
- 104.He S, Zhang Y, Ji W, Liu H, He F, Chen A, Yang H, Pi B. Analysis of spinopelvic sagittal balance and persistent low back pain (PLBP) for degenerative spondylolisthesis (DS) following posterior lumbar interbody fusion (PLIF). Pain Res Manag. 2020. Jan 11;2020:5971937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Li J, Zhang D, Shen Y, Qi X. Lumbar degenerative disease after oblique lateral interbody fusion: sagittal spinopelvic alignment and its impact on low back pain. J Orthop Surg Res. 2020. Aug 14;15(1):326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Barrey C, Roussouly P, Le Huec JC, D’Acunzi G, Perrin G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J. 2013. Nov;22(Suppl 6)(Suppl 6):S834-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Pourtaheri S, Sharma A, Savage J, Kalfas I, Mroz TE, Benzel E, Steinmetz MP. Pelvic retroversion: a compensatory mechanism for lumbar stenosis. J Neurosurg Spine. 2017. Aug;27(2):137-44. [DOI] [PubMed] [Google Scholar]
- 108.Takahashi S, Hoshino M, Ohyama S, Hori Y, Yabu A, Kobayashi A, Tsujio T, Kotake S, Nakamura H. Relationship of back muscle and knee extensors with the compensatory mechanism of sagittal alignment in a community-dwelling elderly population. Sci Rep. 2021. Jan 26;11(1):2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yucekul A, Ozpinar A, Kilickan FDB, Dalla M, Muthiah N, Zulemyan T, Yavuz Y, Pizones J, Obeid I, Kleinstück F, Pérez-Grueso FJS, Pellisé F, Yilgor C, Alanay A; European Spine Study Group (ESSG). Relationship between pelvic incidence-adjusted relative spinopelvic parameters, global sagittal alignment and lower extremity compensations. Eur Spine J. 2023. Oct;32(10):3599-607. [DOI] [PubMed] [Google Scholar]
- 110.Yilgor C, Yavuz Y, Sogunmez N, Haddad S, Mannion AF, Abul K, Boissiere L, Obeid I, Kleinstück F, Pérez-Grueso FJS, Acaroglu E, Pellise F, Alanay A; European Spine Study Group (ESSG). Relative pelvic version: an individualized pelvic incidence-based proportional parameter that quantifies pelvic version more precisely than pelvic tilt. Spine J. 2018. Oct;18(10):1787-97. [DOI] [PubMed] [Google Scholar]
- 111.Cawley DT, Boissiere L, Yilgor C, Larrieu D, Fujishiro T, Kieser D, Alanay A, Kleinstück F, Pérez-Grueso FS, Pellisé F, Obeid I; European Spine Study Group (ESSG). Relative pelvic version displays persistent compensatory measures with normalised sagittal vertical axis after deformity correction. Spine Deform. 2021. Sep;9(5):1449-56. [DOI] [PubMed] [Google Scholar]
- 112.Wright JG. Revised grades of recommendation for summaries or reviews of orthopaedic surgical studies. J Bone Joint Surg Am. 2006. May;88(5):1161-2. [DOI] [PubMed] [Google Scholar]