Abstract
Purpose
We examined the utility of screening instruments to identify risk factors for suicidal ideation (SI) in a population of women with neuropsychiatric illnesses at high risk for postpartum depression.
Methods
Pregnant women with neuropsychiatric illness enrolled prior to 20 weeks gestation. Follow up visits at 4-8 week intervals through 13 weeks postpartum included assessment of depressive symptoms with both clinician and self-rated scales.
Results
A total of 842 women were included in the study. Up to 22.3% of postpartum women admitted SI on rating scales, despite the majority (79%) receiving active pharmacological treatment for psychiatric illness. Postpartum women admitting self-harm/SI were more likely to meet criteria for current major depressive episode (MDE), less than college education, an unplanned pregnancy, a history of past suicide attempt, and higher score on the Childhood Trauma Questionnaire.
Conclusions
In women with a history of neuropsychiatric illness over 20% admitted SI during the postpartum period despite ongoing psychiatric treatment. Patient-rated depression scales are more sensitive screening tools than a clinician-rated depression scale for +SI in the postpartum period.
Keywords: postpartum, risk factors, suicidal ideation
Introduction
Over the past 50 years, the rates of violent maternal deaths (suicide and homicide) have remained essentially unchanged in contrast to an overall decrease in maternal mortality secondary to advances in obstetrical care (Shadigian 2005). A metaanalysis released by the Agency for Healthcare Research and Quality (AHRQ) revealed up to 14.5% of women experience an episode of depression during pregnancy or first three months postpartum (Gaynes 2005).
The rates of SI during pregnancy and the postpartum period vary across different populations. Data from the RESPOND trial evaluating SI in postpartum women in a primary care setting revealed up to 9% had ‘any’ self-harm thoughts endorsed on the Edinburgh Postnatal Depression Scale (EPDS) (Howard 2011). Similarly, Wisner and colleagues (2013), examining a large sample (N = 10,000) from the general population, observed that overall 3.2% of postpartum women admitted SI and 19.3% of these women with EPDS scores greater than 10, recognized thoughts of self-harm. Studies of ‘thoughts of self-harm’ in women with a history of a mood or anxiety disorder have reported rates as high as 35% in pregnancy (Newport 2007) and almost 17% in the postpartum period (Pope 2013). In a non-clinical population of postpartum women with history of childhood maltreatment, up to 37% endorsed SI on the Postpartum Depression Screening Scale (Muzik 2016).
Our group previously examined the association of self-rated and clinician rated scales compared to diagnostic interviews for depression in a longitudinal study across pregnancy and the postpartum period (Ji 2011). Despite the highly significant correlation between the scales, there were significant variations in effects across the second and third trimesters of pregnancy and timing postpartum on determining the optimal screening tool. In clinical psychiatric populations of pregnant (Newport 2007) and postpartum (Pope 2013) women, the self-rated EPDS consistently yields a higher rate of self-harm endorsement than the clinician-rated Hamilton Rating Scale for Depression (HRSD).
In the current study, we sought to confirm and extend our previous investigations by addressing questions germane to clinical care, including: 1) Compare the sensitivity of self-rated and clinician-rated scales in identifying maternal thoughts of self-harm in the postpartum period; 2) Examine obstetrical and neonatal outcomes potentially associated with thoughts of self-harm; and 3) Examine prenatal and postnatal characteristics associated with postpartum SI as potential risk factors.
Materials and Methods
This secondary analysis is derived from prospective observational studies (1994-2012) of women in a clinical setting with neuropsychiatric illnesses presenting to Emory Women's Mental Health Program (WMHP) and/or the Emory Women's Epilepsy Program, tertiary referral centers specializing in the management of perinatal mental illness and perinatal epilepsy, respectively. All subjects were enrolled prior to 20 weeks gestation, based on last menstrual period, and followed at 4-8 week intervals throughout pregnancy and the first postnatal year. Medical, psychiatric, and life histories were obtained. At each visit, participants completed a series of rating scales examining depressive symptoms, perceived stress, and marital satisfaction. Obstetrical, labor/delivery, and pediatric records were obtained. All data was coded with a HIPAA compliant numbering system and entered into a relational database. Written informed consent was obtained prior to study enrollment and approved by the Emory University Institutional Review Board.
Inclusion criteria included: 1) At least one follow up visit during their first 13 weeks postpartum and completed at least one depression rating scale including Beck Depression Inventory (BDI) (Beck 1961), HRSD (Hamilton 1960; Williams 1988) and/or EPDS during that visit (Cox 1987); 2) Completed the Structured Clinical Interview for DSM-IV (SCID) (First 2002) at enrollment and a SCID mood module at identified postpartum visit. The subject's first visit within the 13 week period was analyzed. By convention, only an individual's first pregnancy within the duration of the study was included and women with a multiple gestation (i.e. twin pregnancy) were excluded.
All three depression rating scales include an item focusing on thoughts of self-harm or suicide (Table 1). Consistent with previous studies examining suicidal ideation during pregnancy and/or postpartum period, this analysis defined a priori the presence of SI or thoughts of self-harm as any response greater than 0 for each scale to maximize sensitivity (Newport 2007; Wisner 2013).
Table 1. Self-rated and clinician rated depression scales highlighting items related to suicidal ideation.
| EDINBURGH POSTNATAL DEPRESSION SCALE, ITEM 10 | |||
| In the past 7 days, the thought of harming myself has occurred to me: | |||
| 0 = Never | |||
| 1 = Hardly ever | |||
| 2 = Sometimes | |||
| 3 = Yes, quite often | |||
|
| |||
| BECK DEPRESSION INVENTORY, ITEM 9 | |||
|
| |||
| 0 = I don't have any thoughts of harming myself | |||
| 1 = I have thoughts of harming myself but I would not carry them out | |||
| 2a = I feel I would be better off dead | |||
| 2b = I have definitive plans about committing suicide | |||
| 2c = I feel my family would be better off if I were dead | |||
| 3 = I would kill myself if I could | |||
|
| |||
| HAMILTON RATING SCALE FOR DERPESSION, ITEM 3 | |||
|
| |||
| Suicide: Have you had any thoughts that life is not worth living? That you'd be better off dead? Even thoughts of hurting or killing yourself? If yes: What have you thought about? Have you done anything to hurt yourself? | |||
| 0 = Absent | |||
| 1 = Feels life is not worth living | |||
| 2 = Wishes he were dead or any thoughts of possible death to self | |||
| 3 = Suicidal ideas or gestures | |||
| 4 = Attempts at suicide | |||
The information was queried from the overall database and exported to SAS database for statistical analysis. For each scale, the data were categorized and proportion of non-zero versus zero answer was calculated using frequency table. Bivariate analysis was then performed looking at associations of positive SI with various sample characteristics. Women with pregnancy and/or delivery complications were combined into a categorical variable. Antepartum complications evaluated included gestational diabetes, abnormalities of amniotic fluid volume (oligohydramnios and polyhydramnios), hyperemesis gravidarum, placenta previa and hypertension (including chronic, pregnancy induced hypertension, preeclampsia, eclampsia and HELLP syndrome). Intrapartum complications evaluated included sub optimal anesthesia, placental abruption, precipitous labor, prolonged labor, mode of delivery, chorioamnionitis, postpartum hemorrhage, maternal hemodynamic instability, maternal Group B Streptococcus infection, other maternal infections, and maternal vaginal lacerations. Antepartum and intrapartum complications were obtained from the subjects, medical chart review, and the labor and delivery summary. Chi-square analysis was utilized for categorical variables and T-Test or Wilcoxon Test were utilized for continuous variables, based on the variable being normally distributed or not, respectively. All tests were two-tailed, and a p-value of 0.05 was used to determine statistical significance. After these associations were identified, logistic regression was performed to identify possible predictors of SI utilizing the EPDS specific item as this had highest proportion of women screening positive for SI. Variables that were significantly associated with EPDS-based SI in the bivariate analysis were selected for regression model fit. Some variables, though not significant in bivariate analysis, were included from a clinical significance standpoint including if the pregnancy was desired, gestational age at delivery, delivery complications, mode of delivery, neonatal complications, and infant NICU or special nursery admission. We achieved the most parsimonious model explaining maximum variance using R-Squared value. We also tested the predictive power of the fitted model using area under the ROC (Receiver Operating Characteristics) curve to assess relevant variables as potential markers for SI. A randomized selection of 70% of the subjects were selected using GLMSELECT procedure of SAS to train the model and remaining 30% sample was used to test the model. Area under the ROC curve was calculated as a measure of specificity and sensitivity. After ROC curve for this population was calculated the remaining 30% of the population was calculated using the same model to validate the results.
Results
The original study 868 women met inclusion criteria. 26 women were excluded due to twin gestation leaving a total of 842 included in analysis. They had a mean maternal age of 33.0 ± 4.8 years and 83% (n = 698) identified as White. A total of 2.6% (n = 22) reported Hispanic ethnicity. Mean duration of education was 15.9 ± 2.1 years and 83% were married (n =698). Obstetrical history revealed 37% were primigravid (n = 310) with 93% of pregnancies resulting in a live delivery (n = 787). Of the non-live deliveries (n = 55), 2 (3.6%) were elective abortions, 5 (9%) were stillbirths, and 28 (87.3%) were spontaneous abortions. The average gestational age at delivery was 36.9 ± 7 weeks (including spontaneous abortion or fetal demise deliveries). Almost one third of subjects (29%) reported that the pregnancy was not planned (n = 244).
Out of the women included, 59 women were recruited from the epilepsy clinic with a known primary diagnosis of epilepsy; additionally, women recruited from the WMHP may have also had comorbid epilepsy. For the purposes of this analysis, these two groups were not separated. For all women, 64% met lifetime criteria for Major Depressive Disorder (n = 543), 19% for Bipolar I (n= 132) and/or II (n = 28) Disorder, 1% for a psychotic disorder (n = 12), 14% for Obsessive Compulsive Disorder (n = 119), 18% for Posttraumatic Stress Disorder (n = 156), 23% for Generalized Anxiety Disorder (n = 195) and 20% for a history of substance use disorder (n = 167). Pharmacological treatment data was available on majority of participants (n = 626) with more than two-thirds (n = 495) of these women taking an anti-depressant.
Women had higher rates of endorsement to specific self-harm/suicidal ideation items on EPDS compared to BDI or HRSD (Table 2). Considering only women who completed all three scales (n = 505), 14.6% (n = 74) consistently answered positive SI on all three with only 2.9% (n = 15) of these women being “missed” if the EPDS was the only scale utilized. When comparing patient rated scales (BDI and EPDS) against clinician-rated scales (HRSD), patient rated scales appear more sensitive with 13.8% subjects endorsing suicidal thoughts only on the BDI and/or EPDS and 2.4% endorsed thoughts of self-harm only on HRSD. Bivariate analysis of psychiatric, life events, sociodemographic, obstetrical, and neonatal variables on the three rating scales revealed multiple significant associations with SI (Table 3). For all three scales, SI was significantly more likely among women with a current major depressive episode (MDE), increased mean number of comorbid mental illnesses, higher Childhood Trauma Questionnaire scores, lower Dyadic Adjustment Scale (DAS) scores (a measure of marital satisfaction), unplanned pregnancy, and non-college graduates. A positive response on the clinician-rated instrument was also associated with past suicide attempt, non-desired pregnancy (p = 0.005), and lower estimated gestational age at delivery (p =0.032). Being non-Caucasian (p = 0.004, 0.01) was associated on the patient rated scales but not on the clinician rated scale. Other variables that showed no association with +SI, were: use of SSRI, conception method (including natural versus artificial reproductive technologies), infant gender, gestational age at delivery, term birth weight < 2500 grams, low APGAR score at 5 minutes, intrapartum complications, perinatal/neonatal death, fetal/neonatal structural anomalies, and neonatal NICU admission.
Table 2.
Reponses to self-harm/suicidal ideation items on Edinburgh Postnatal Depression Scale (EPDS), Beck Depression Inventory (BDI) and the Hamilton Rating Scale for Depression (HRSD).
| EPDS #10 | BDI #9 | HRSD #3 | |
|---|---|---|---|
| Patient Rated | Patient Rated | Clinician Rated | |
| Total Score, Mean | 8.47 + 6.1 | 10.81 ±8.7 | 9.64 + 5.1 |
| N (completed): | 577 | 818 | 738 |
| N (+SI): | 129 (22.3%) | 132 (16.1%) | 85 (11.5%) |
| Distribution of + SI scores: | |||
| 1 | 50.4%, N = 65 | 78.0%,N = 103 | 42.4%, N = 36 |
| 2 | 37.2%, N = 48 | 17.4%, N = 23 | 37.6%, N = 32 |
| 3 | 12.4%, N = 16 | 4.5%, N = 6 | 20.0%, N = 17 |
| 4 | N/A | N/A | 0%, N = 0 |
SI suicidal ideation
Total Score, Mean refers to total score on the full scale. For EPDS, score ≥ 10 indicates possible depression. For BDI, score 0-13 indicates minimal depression, 14-19 mild depression, 20-28 moderate depression and ≥29 indicates severe depression. For HRSD, score 8-13 indicates mild depression, 14-18 moderate depression, 19-22 severe depression and ≥23 indicates very severe depression.
Table 3.
Bivariate analysis of pre-pregnancy, pregnancy and postpartum characteristics and self-harm or suicidal thoughts in postpartum women up to 13 weeks.
| Predictors | EPDS | BDI | HRSD |
|---|---|---|---|
| Sociodemographics | |||
|
| |||
| Maternal age, years (mean, SD): + SI | 32.4 + 5.0 | 32.1 +4.75* | 32.2 + 4.63 |
|
|
|||
| Maternal age, years (mean, SD): No SI | 33.2 + 4.5 | 33.1 +4.77* | 33.1 +4.94 |
|
| |||
| Married | 21.5%, n = 484 p = 0.19 | 14.9%, n = 685 p = 0.03 | 10.7%, n = 609 p = 0.07 |
|
| |||
| White | 20.6%, n = 510 p = 0.004 | 14.8%, n = 715 p = 0.01 | 10.9%, n = 640 p = 0.12 |
|
| |||
| Non-College Graduate | 18.9%, n = 417 p = 0.001 | 12.9%, n = 583 p = <.0001 | 10.0%, n = 522 p = 0.02 |
|
| |||
| Pre-Pregnancy Factor | |||
|
| |||
| Past Suicide Attempt | 32.7%, n =55 p = 0.057 | 32.6%, n =86 p = <0.0001 | 39.6%, n = 78 p = 0.0009 |
|
| |||
| Number of comorbid mental illness (mean, SD): + SI | 5.2 ± 2.13*** | 5.4 + 2.13*** | 5.5 + 2.03*** |
|
| |||
| Number of comorbid mental illness (mean, SD): No SI | 4.5 + 1.79*** | 4.5 + 1.82*** | 4.5 + 1.90*** |
|
| |||
| Childhood Trauma Questionnaire score (mean, SD): + SI | 44.9 ± 14.20*** | 46.5+16.57*** | 47.8+16.01*** |
|
|
|||
| Childhood Trauma Questionnaire score (mean, SD): No SI | 38.9 + 13.48*** | 38.9+13.13*** | 39.5 + 13.88*** |
|
| |||
| Nulliparous | 20.0%, n = 329 p = 0.19 | 12.1%, n = 456 p = 0.001 | 9.5%, n = 400 p = 0.045 |
|
| |||
| Hollingshead Scale (mean, SD): + SI | 48.3 ± 12.42 | 46.2 + 13.76** | 47.3 + 12.21* |
|
|
|||
| Hollingshead Scale (mean, SD): No SI | 51.1 ±9.10 | 51.1 +9.59** | 50.8 + 10.13* |
|
| |||
| Pregnancy Factor | |||
| Unplanned Pregnancy | 27.6%, n = 156 p = 0.026 | 20.1%, n = 234* p = 0.01 | 16.2%, n = 222 p = 0.0046 |
|
| |||
| Non-Desired Pregnancy | 19.0%, n = 415 p = 0.96 | 20.5%, n = 112 p = 0.06 | 18.4%, n = 109 p = 0.006 |
|
|
|||
| Pregnancy Complication | 19.6%, n = 133 p. 0.18 | 17.6%, n = 182* p = 0.03 | 13.5%, n = 171 p = 0.16 |
|
| |||
| Postnatal Factor | |||
|
| |||
| SCID: Current MDE, + SI | 46.8%, n = 62*** p = <0.0001 | 39.1%, n = 87*** p = <0.0001 | 39.6%, n = 91 p = <0.0001 |
|
| |||
| Not Breastfeeding/Bottle Fed | 28.8%, n = 52 p = 0.47 | 18.0%, n = 78* p = 0.03 | 16.0%, n = 94* p = 0.013 |
|
|
|||
| Pittsburgh Sleep Scale (mean, SD): + SI | 8.4 ± 3.53 | 9.4 ± 3.25*** | 10.4 + 2.95*** |
|
| |||
| Pittsburg Sleep Scale (mean, SD): No SI | 7.1 +3.80 | 7.2 + 3.68*** | 7.2 + 3.67*** |
|
|
|||
| Dyadic Adjustment Scale (mean, SD): + SI | 109.4 ± 21.14*** | 107.1 +26.91*** | 102.4 + 29.5*** |
|
| |||
| Dyadic Adjustment Scale (mean, SD): No SI | 118.4 + 17.83*** | 117.8 + 17.31*** | 117.5 + 17.96*** |
|
| |||
| Social Adjustment Scale (mean, SD): + SI | 2.2 + 0.32* | 2.3 + 0.34 | 2.2 + 0.25 |
|
|
|||
| Social Adjustment Scale (mean, SD): No SI | 1.9 + 0.35* | 1.9 + 0.35 | 1.9 + 0.36 |
|
| |||
| Estimated gestational age at delivery (weeks): + SI | 37.8 + 4.96 | 36.2 + 7.88 | 36.3 + 7.94* |
|
|
|||
| Estimated gestational age at delivery (weeks): No SI | 37.1 ±6.88 | 37.0 + 6.90 | 37.0 + 6.90* |
|
| |||
| APGAR 1 minute: + SI | 7.6 + 1.30 | 7.5 + 1.30 | 7.7 + 1.30 |
|
|
|||
| APGAR 1 minute: No SI | 7.5 + 1.53 | 7.5 + 1.56 | 7.5 + 1.56 |
Bold = statistically significant;
<0.05;
<0.01,
<0.001
EPDS, Edinburgh Postnatal Depression Scale; BDI, Beck Depression Inventory; HRSD, Hamilton
Rating Scale for Depression SI, suicidal ideation; SCID, Structured Clinical Interview for DSM-IV; MDE, Major Depressive Episode
The logistic procedure using the EPDS based SI revealed that women with current MDE were almost 7 times more likely to have suicidal thoughts and those without college degree were 3 times more likely (Table 4). The Hosmer and Lemeshow goodness-of-fit statistic was 8.06 (df = 8, p = 0.42), therefore showing a good fit.
Table 4. Logistic regression results of risk factors of suicidal ideation (EPDS Item 10 > 0).
| Predictor | Parameter Estimate | Odds Ratio (95% CI) | p-value |
|---|---|---|---|
| SCID: Current MDE | 1.932 | 6.90 (3.51-13.58) | <0.0001 |
| Non - College graduate | 1.089 | 2.97 (1.55-5.70) | 0.001 |
| Not Married | 0.648 | 1.91 (0.75-4.87) | 0.17 |
| Past suicide attempt | 0.439 | 1.55 (0.67-3.62) | 0.31 |
| Number of comorbid illnesses | 0.037 | 1.04 (0.88-1.22) | 0.65 |
| CTQ score | 0.014 | 1.01 (0.99-1.04) | 0.22 |
| Planned pregnancy | -0.532 | 0.59 (0.29-1.18) | 0.13 |
| Caucasian | -0.547 | 0.58 (0.24-1.38) | 0.22 |
EPDS Edinburgh Postnatal Depression Scale SCID Structure Clinical
To test whether the variables used in the logistic regression may be useful diagnostic tests for suicidal ideation, the sample using only the EPDS was divided into a test group including 70% of the subject and validation group including 30% of subjects and an ROC curve was calculated. For the test group, AUC was 0.81 (95% confidence interval [CI], 0.73-0.88 [P = <.0001], suggesting these variable are adequate predictors. For the validation group, AUC remained significant at 0.77 (Fig.1).
Figure 1.
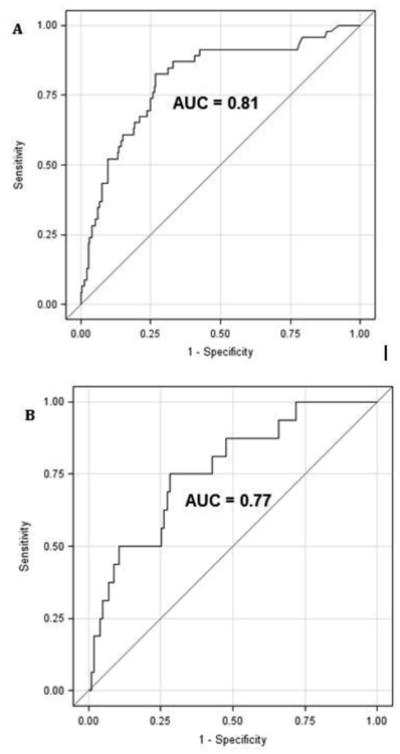
Receiver operating characteristics [ROC) curve (A) for test group population and validation group (B) for variables from logistic regression model. AUC indicates area under the ROC curve.
Discussion and Conclusion
The prevalence of self-harm and/or suicidal ideation in the postpartum period ranged from 11.5-22.3% depending on the rating scale in a clinical population of women with pre-existing neuropsychiatric illnesses. These rates are higher than those reported in community derived samples (Howard 2011) and only slightly higher than previous data from women with known mood disorders (Pope 2013; Wisner 2013); however, slightly lower than women with histories of childhood maltreatment (Muzik 2016). It is concerning, that despite active treatment, a high percentage of women acknowledged positive SI. This underscores the importance of ongoing symptom assessment in postpartum women who may or may not be receiving psychiatric care.
The self-rated scales, both the EPDS and BDI, had higher proportions of women endorsing self-harm thoughts than the clinician-rated instrument (HRSD), suggesting greater sensitivity. There are many possible reasons for variations in amount of women endorsing positive on each scale, most notably differences in wording of the questions. The EPDS question can be viewed as more conservative as the question asks about “self-harm” and this may not always be interpreted as “suicidal”. Many women may have higher rates of self-harm behavior without wishing to take one's life, albeit this remains a concerning health risk (Fliege 2009; Sansone 2000). Patient-rated scales may elicit increased responses to SI as patients may be more likely to endorse this on a piece of paper rather than verbalize this to a clinician out of fear of possible consequences. The reasons for the differential endorsement remain obscure, though it is reasonable to conclude that no single rating scale identifies all cases. In our population, only 15 women endorsing thoughts of self-harm and/or suicide were missed by the EPDS.
Postpartum women endorsing suicidal ideation were associated with current MDE, increased number of comorbid psychiatric illnesses, higher scores on the childhood trauma questionnaire, unplanned pregnancy, lower DAS scores, and non-college graduates. The association with major depression is consistent with previous studies in postpartum populations using the EPDS (Gold 2012; Pope 2013; Wisner 2013). Consistent with data from non-obstetric populations, history of past suicide attempts, psychiatric comorbidity and childhood trauma have been linked to suicidal behavior (Dube 2001; Kessler 1999; Read 2001). There are conflicting reports regarding unplanned pregnancy being associated with postpartum depression although this was associated with suicidal ideation in our study; however, marital discord measured by DAS has been associated with postpartum depression and thus may also contribute to SI (Gotlib 1991; O'Hara 1990, Stowe 1995). Lower education level has been associated with increased risk of depression in the postpartum population, and our data found an association with SI that remained an independent risk factor based on logistic regression (Gotlib 1991). Women, who did not breastfeed, were nulliparous and having more difficulty sleeping were significantly more likely to endorse SI on both the BDI and HRSD. Previous studies have suggested that women who breastfeed and have multiple children are less likely to experience postnatal depression, which could explain these results (Hatton 2005; Kendall-Tackett 2007; Warner 1996). These findings may contribute to theories regarding decreased suicide attempts and completions during the perinatal period. The impact of breastfeeding on suicidal behaviors is understudied. It is feasible that breastfeeding women may have a heightened sense of responsibility as the primary nutrition source for the infant serving as a potential protective factor against suicide (Kendall-Tackett 2007).
This study does have several limitations that warrant discussion. The homogeneity of the population precluded our ability to more closely examine other sociodemographic factors such as minority races, lower socioeconomic status women, and women who may have more negative life experiences. This clinical derived sample also lacked evaluation of teen pregnancies and non-English speaking mothers. This limits generalizability, though the results and associations are in good agreement and extend previous reports. The analysis of potential associations and predictors was limited to the finite data set collected under the auspices of the original prospective study design. This study design aimed at enrolling and following women during pregnancy and the postpartum period. The group of women included in our group's previous publication examining suicidal ideation during pregnancy (Newport 2007) would have also been eligible for inclusion in this current study. Due to change in database systems, it is difficult to delineate the exact number of women included in the previous study in these analyses. For education, the data was arbitrally dichotomized at college education based on the demographics of the population. This split may have impacted the findings. The delineation of self-harm from thoughts of suicide as well as examination of the contribution of a history of self-harm or mutilation was not possible with the data available. Considering the high rate of thoughts of self-harm, consideration of Borderline Personality Disorder as part of the psychiatric diagnosis warrants attention. The original study did not include structured measures for this diagnosis; therefore, the potential of including women in this analysis with BPD is likely although unclear how this impacts finding of the study.
Our data indicate a high rate of suicidal ideation in women with a history of neuropsychiatric illness despite ongoing clinical care. With self-harm being a leading cause of maternal mortality, it would be prudent to continue psychiatric assessments and/or discussions of SI with pregnant and postpartum women despite current level of mental health treatment (Metz 2016). Association of suicidal ideation and psychotropic medication in the postpartum period has not been previously explored to the best of our knowledge; therefore, additional studies evaluating associations between neuropsychiatric care and suicidal ideation are needed to support these findings in various populations. History of psychiatric illness has been shown to be a strong predictor of suicidal behavior during pregnancy and the postpartum period (Newport 2007; Wisner 2013) and additional work exploring outcomes of those with and without treatment would benefit clinicians in guiding clinical intervention strategies. There was no evidence that antepartum, intrapartum and perinatal complications had an independent association with postpartum maternal suicidal ideation. The data indicate that the majority of risk factors are present prior to delivery (history of attempt, psychiatric co-morbidity, early life trauma, lower education, marital status, unplanned pregnancy) and that like previous studies the presence of depression are major determinants in the endorsement of suicidal thoughts. Beyond screening and additional historical information collection, there may be value in discussing the importance of the physical health of the mother and well-being of the child, such as breastfeeding and sleep hygiene in women who are at higher risk of postpartum depression.
With the self-reported questionnaires showing higher sensitivity than the HDRS in identifying women with suicidal thoughts, instituting patient-rated scales such as the EPDS in clinical practice may not only be time efficient but allow identification of at risk groups. It is recommended by the American College of Obstetrics and Gynecologists to screen every patient “at least once during the perinatal period for depression and anxiety symptoms using a standardized, validated tool” with coupling of appropriate follow-up and treatment when indicated (ACOG 2015). Universal screening for maternal depression in the postpartum period is a laudable goal, and prenatal screening for women at risk for depression would be ideal. While it may not be practical to screen for maternal depression and/or suicidal ideation at every peripartum visit, existing data, albeit limited, provides evidence that the first 2 months postpartum pose the highest risk for completed suicide (Appleby 1991; Gissler 1996) underscoring the potential value of screening during windows of heightened vulnerability.
With these recommendations in place, effective screening has become a creditable goal. Adding a patient rated scale to intake packets can easily be completed in the waiting room of the clinic and addressed in detail by health care provider if needed.
Acknowledgments
Presented in part at the 167th annual American Psychiatric Association meeting 2014. New York City, New York. May 3-7, 2014
Funding: This study was funded by a grant from the NIH including (TRCBS P50 MH-77928, SCOR P50 MH 68036). The first author also received support from UAMS NIDA T32 grant (UL1TR000039).
Footnotes
Conflict of Interest Statement: Drs. Coker and Magann and Mr. Tripathi have no conflicts of interest.
Dr. Pennell has received research support from the National Institutes of Health (NIH), Epilepsy Foundation, and the Epilepsy Therapy Project, and speaker's honoraria from the American Academy of Neurology, American Epilepsy Society, the India Academy of Neurology, and the University of Maryland.
Dr. Newport has received research support from NARSAD and the National Institutes of Health (NIH), as well as Eli Lilly, GlaxoSmithKline (GSK), Janssen, and Wyeth Corporations, and speaker's honoraria from Astra-Zeneca Pharmaceuticals (AZP), Eli Lilly, GSK, and Pfizer Corporations
Dr. Stowe has received research support from NIH, SAGE therapeutics and Janssen, and consulted to GlaxoSmithKline, Pfizer, and Wyeth Corporations, and received speakers' honoraria from the GlaxoSmithKline, Pfizer, Wyeth, Eli Lilly and Forest Corporations.
Ms. Knight's adult son is employed by GlaxoSmithKline and has stock options as part of his employment.
No other coauthor or any family member holds equity positions in pharmaceutical or biomedical corporations.
Compliance with Ethical Standards: Ethical Approval: The original study was approved by the Emory University Institutional Review Board (IRB) on 7/11/2007, #4249.
Informed Consent: Informed consent was obtained from all individual participants included in the study
Contributor Information
Jessica L. Coker, Department of Psychiatry, University of Arkansas for Medical Sciences, 4301 W. Markham Street, Little Rock, AR 72205, Phone: (501) 472-09707.
Mr Shanti P. Tripathi, Email: shantpt26@gmail.com, Psychiatric Research Institute, University of Arkansas for Medical Sciences, 4301 W. Markham Street, Little Rock, AR 72205.
Ms Bettina T. Knight, Email: btknight@uams.edu, Psychiatric Research Institute, University of Arkansas for Medical Sciences, 4301 W. Markham Street, Little Rock, AR 72205, Phone: (501) 526-8201.
Page B. Pennell, Email: ppennell@partners.org, Harvard Medical School, Director of Research, Division of Epilepsy, Department of Neurology, 75 Francis Street, Brigham and Women's Hospital, Boston, MA 02115, Phone: 617-732-6531.
Everett F Magann, Email: EFMagann@uams.edu, Department of Obstetrics & Gynecology, Division Director, Maternal-Fetal Medicine Department, University of Arkansas for Medical Sciences, 4301 W. Markham Street, Little Rock, AR 72205.
D. Jeffrey Newport, Email: jeff.newport@miami.edu, Women's Reproductive Mental Health, University of Miami Miller School of Medicine, 1120 NW 14 th Street, Suite 1446, Miami, FL 33136.
Zachary N. Stowe, Email: znstowe@uams.edu, Women's Mental Health Program, Psychiatric Research Institute, University of Arkansas for Medical Sciences, 4301 W. Markham Street, #843, Little Rock, AR 72205-7199, Voice: (501) 526-8201, Fax: (501) 526-7816.
References
- American College of Obstetricians and Gynecologists Committe on Obstetric Practiec. ACOG Committee Opinon No. 630: Screening for Perinatal Depression. Obstet Gynecol. 2015 May;125:1268–71. doi: 10.1097/01.AOG.0000465192.34779.dc. [DOI] [PubMed] [Google Scholar]
- Appleby L. Suicide during pregnancy and in the first postnatal year. BMJ. 1991;302(6769):137–140. doi: 10.1136/bmj.302.6769.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Ward C, Mendelson M. Beck depression inventory (BDI) Arch Gen Psychiatry. 1961;4(6):561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British journal of psychiatry. 1987;150(6):782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span. JAMA. 2001;286(24):3089–96. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. SCID-I/P; 2002. [Google Scholar]
- Fliege H, Lee JR, Grimm A, Klapp BF. Risk factors and correlates of deliberate self-harm behavior: A systematic review. Journal of Psychosomatic Research. 2009;66(6):477–493. doi: 10.1016/j.jpsychores.2008.10.013. [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, et al. Perinatal depression: prevalence, screening accuracy, and screening outcomes: summary. 2005 doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gissler M, Hemminki E, Lonnqvist J. Suicides after pregnancy in Finland, 1987-94: register linkage study. BMJ. 1996;313:1431–1434. doi: 10.1136/bmj.313.7070.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold KJ, Singh V, Marcus SM, Palladino CL. Mental health, substance use and intimate partner problems among pregnant and postpartum suicide victims in the National Violent Death Reporting System. General hospital psychiatry. 2012;34(2):139–145. doi: 10.1016/j.genhosppsych.2011.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotlib IH, Whiffen VE, Wallace PM, Mount JH. Prospective investigation of postpartum depression: factors involved in onset and recovery. Journal of Abnormal Psychology. 1991;2:122–132. doi: 10.1037//0021-843x.100.2.122. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of neurology, neurosurgery, and psychiatry. 1960;23(1):56. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatton DC, Hohner-Harrison J, Coste S, Dorato V, Curet LB, McCarron DA. Symptoms of postpartum depression and breastfeeding. Journal of Human Lactation. 2005;21(4):444–449. doi: 10.1177/0890334405280947. [DOI] [PubMed] [Google Scholar]
- Howard LM, Flach C, Mehay A, Sharp D, Tylee A. The prevalence of suicidal ideation identified by the Edinburgh Postnatal Depression Scale in postpartum women in primary care: findings from the RESPOND trial. BMC pregnancy and childbirth. 2011;11(1):57. doi: 10.1186/1471-2393-11-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji S, Long Q, Newport DJ, Na H, Knight B, Zach E, et al. Validity of Depression Rating Scales in Women with a History of Major Depression during Pregnancy and the Postpartum Period: Impact of Trimester and Parity. Journal of Psychiatric Research. 2011;45(2):213–9. doi: 10.1016/j.jpsychires.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall-Tackett K. A new paradigm for depression in new mothers: the central role of inflammation and how breastfeeding and antiinflammatory treatments protect maternal mental health. International Breastfeeding Journal. 2007;2:6. doi: 10.1186/1746-4358-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Metz TD, Rovner P, Allshouse AA, Beckwith K, Hoffman MC, Binnswanger I. 210: Maternal deaths from suicide and drug overdose in Colorado. American Journal of Obstetrics and Gynecology. 2016;1(214):S126–S127. doi: 10.1097/AOG.0000000000001695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Brier Z, Menke RA, Davis MT, Sexton MB. Longitudinal suicidal ideation across 18-months postpartum in mothers with childhood maltreatment histories. Journal of Affective Disorders. 2016;204:138–145. doi: 10.1016/j.jad.2016.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newport DJ, Levey LC, Pennell PB, Ragan K, Stowe ZN. Suicidal ideation in pregnancy: assessment and clinical implications. Archives of women's mental health. 2007;10(5):181–187. doi: 10.1007/s00737-007-0192-x. [DOI] [PubMed] [Google Scholar]
- O'Hara MW, Zekoski EM, Philipps LH, Wright EJ. Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. Journal of Abnormal Psychology. 1990;1:3–15. doi: 10.1037//0021-843x.99.1.3. [DOI] [PubMed] [Google Scholar]
- Pope CJ, Xie B, Sharma V, Campbell MK. A prospective study of thoughts of self-harm and suicidal ideation during the postpartum period in women with mood disorders. Archives of women's mental health. 2013;16(6):483–488. doi: 10.1007/s00737-013-0370-y. [DOI] [PubMed] [Google Scholar]
- Read J, Agar K, Barker-Collo S, Davies E, Moskowitz A. Assessing Suicidality in Adults: Integrating childhood trauma as a major risk factor. Professional Psychology. 2001;32(4):367–372. [Google Scholar]
- Sansone RA, Wiederman MW, Sansone LA, Monteith D. Patterns of self-harm behavior among women with Borderline Personality Symptomatology: psychiatric versus primary care samples. General Hospital Psychiatry. 2000;22:174–178. doi: 10.1016/s0163-8343(00)00074-8. [DOI] [PubMed] [Google Scholar]
- Shadigian EM, Bauer ST. Pregnancy-associated death: a qualitative systematic review of homicide and suicide. Obstetrical & gynecological survey. 2005;60(3):183–190. doi: 10.1097/01.ogx.0000155967.72418.6b. [DOI] [PubMed] [Google Scholar]
- Stowe ZN, Nemeroff CB. Women at risk for postpartum-onset major depression. Am J Obstet Gynecol. 1995;173:639–645. doi: 10.1016/0002-9378(95)90296-1. [DOI] [PubMed] [Google Scholar]
- Warner R, Appleby L, Whitton A, Faragher B. Demographic and obstetric risk factors for postnatal psychiatric morbidity. British Journal of Psychiatry. 1996;168:607–611. doi: 10.1192/bjp.168.5.607. [DOI] [PubMed] [Google Scholar]
- Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry. 1988;45(8):742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70(5):490–498. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]


