Abstract
Background
The identification of the determinants of health literacy is an essential prerequisite for developing health literacy promotion programs. While these factors have been reported in previous studies, there is a lack of a comprehensive review specifically focused on the Iranian population. Therefore, this review aimed to identify the factors related to health literacy in Iran.
Methods
This scoping review used the Arksey and O'Malley methodological framework and the Joanna Briggs Institute framework. A search was performed in English-language databases—Web of Science, Scopus, and PubMed—using the MeSH keyword of "health literacy," and in Persian-language databases—Magirean and SID—using the related keywords. A narrative synthesis was conducted to describe all included studies' characteristics and explore factors associated with health literacy.
Results
A total of 76 studies were included. Based on the results of the study, related factors included personal factors—including sex, age, education level, field of study, parents’ education level, marital status, occupation, work experience, employment status, ethnicity, income, socioeconomic status, medical history, duration of disease, addiction, number of children, media literacy, information literacy, computer literacy, and self-efficacy—situational factors—including use of the internet, use of social networks, social support, source of information, and participation in health education classes—and societal and environmental factors—including place of residence and type of insurance.
Conclusion
Modifiable factors identified in this study were self-efficacy, social support, information sources, media literacy, information literacy, computer literacy, internet or social networks, and participation in health education classes. Planners can consider these factors when developing interventions to promote health literacy.
Keywords: Health Literacy, Related Factors, Determinants, Iran
↑What is “already known” in this topic:
Recognizing influential and determining factors of health literacy is one of the most critical steps in implementing effective health strategies and programs to promote public health.
→What this article adds:
Three categories of factors were associated with health literacy: personal; situational; and societal and environmental factors. Education level was the most definitive health literacy factor.
Introduction
Health literacy is one type of literacy that people should possess (1). The World Health Organization (WHO) defines health literacy as cognitive and social skills that determine an individual's capacity and ability to acquire, process, understand, and use health information (2).
The prevalence of health literacy ranges from 6.1% to 94.2% across countries, indicating differences between studies (3). Health literacy is a critical and specific tool for societal health and is regarded as the top priority in improving the quality of health care (4). As a result, the WHO emphasizes that all societies should strive to achieve optimal health literacy and include health literacy improvement programs and strategies in their agenda to attain sustainable development goals (5). Recognizing influential and determining factors of health literacy is one of the most important steps in implementing effective health strategies and programs to promote public health (6).
Based on the Paasche-Orlow and Wolf's theory, health literacy is influenced by social and demographic features, social support, and individuals' cognitive and physical abilities (7). McCormack argues that demographic features, resources, prior knowledge, capabilities, and mediators affect health literacy (8). However, these theoretical explanations must be examined and proven in more accurate studies.
Accordingly, health literacy is a global issue that is considered one of the most fundamental health promotion tools because of its crucial role in health decision-making. However, a low level of health literacy has been reported in studies conducted on different groups in Iranian society, highlighting the need to address this issue. In this regard, the determinants of health literacy must be identified.
While several primary studies have reported factors associated with health literacy, review articles published in Iran have primarily focused on determining the levels of health literacy in the general population and various subgroups. Although each of these studies has focused on some of the factors associated with health literacy (4), there is a need for more comprehensive reviews that synthesize the available evidence on the different factors that affect health literacy. Such reviews can help identify gaps in knowledge and inform the development of interventions to improve health literacy and health outcomes by considering the relevant factors. To the best of our knowledge, no scoping review has been conducted to provide a comprehensive summary of the elements related to health literacy, specifically in the Iranian population. Therefore, this scoping review aimed to precisely identify the factors related to health literacy in Iranians.
Methods
Scoping reviews are a valuable research method that can identify and examine the various characteristics or factors associated with a particular concept (9). This scoping review was conducted based on the Arksey and O'Malley methodological framework (10), and the Joanna Briggs Institute's (JBI) updated guidance on scoping reviews (11). Additionally, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) were used as a checklist to report this scoping review (12).
Stage 1. Identifying the Research Question
The following research question was formulated based on the population, concept, and context strategy: which factors are associated with health literacy among Iranians aged 18 to 65 years?
Stage 2. Identifying Relevant Studies
The Persian-language databases of Magiran and SID were searched using the Persian equivalents for health literacy to obtain the research data. Similarly, using the keyword health literacy, a search was conducted in English-language databases such as PubMed, Web of Science, and Scopus, without any time limitation from April 1, 2021, to April 5, 2021. The article search process was performed independently by 2 researchers. If an article's full text was unavailable, its corresponding author was contacted. The search strategy in the PubMed database was as follows: ((“Health literacy”[mh] OR “Health literacy”[tiab] OR (health[tiab] AND literacy[tiab]) OR “literacy”[mh] OR literacy[tiab] OR “Information Literacy”[mh] OR Information Literacy[tiab] OR Health literate[tiab] OR Functional health literacy[tiab]) AND (iran*[tiab] OR iran[pl] OR iran[ad]).
Stage 3. Selecting Studies
The study selection process was such that the studies obtained from the Persian and English databases were first entered into Endnote software Version 6, and then duplicate studies were removed. In the next step, the titles and abstracts of the articles were reviewed, and articles unrelated to the aim of our research were deleted. Then, the full texts of the related articles were examined according to the inclusion and exclusion criteria and, finally, the eligible studies were included in the study. Two independent researchers performed the study selection to increase its validity. Table 1 shows the inclusion and exclusion criteria of the studies.
Table 1. Study Inclusion and Exclusion Criteria.
| Study Characteristics | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Studies focusing on individuals aged 18 to 65, including both males and females | Studies targeting the population below 18 years and above 65 years. |
| Concept: Factors | Studies that had identified one or more variables as factors associated with health literacy and had utilized standardized tools to determine health literacy. | Studies that did not analyze factors associated with health literacy and studies that utilized researcher-made tools |
| Context | Observational studies conducted in Iran. | Nonobservational studies. Studies that were not conducted in Iran. |
| Others | Written in Persian and English Without any time limitation | lack of access to the full text of the article. Duplicate studies. |
Stage 4. Charting the Data
Two independent researchers extracted the data using a researcher-made checklist. This checklist consisted of 3 parts as follows:
• Article information: name of authors, year of publication, place of research, type of research, sample size, sampling methods
• Participants characteristics: Population age range, participation class, number of participants by sex, and sex
• Investigated outcome: health literacy-related factors
Stage 5. Collating, Summarizing, and Reporting the Results
To summarize and report the results, a template with maps of tables and charts was developed. In addition, for reporting findings, factors related to health literacy among Iranian people were divided into 3 categories based on the integrated model of health literacy: societal and environmental factors; personal factors; and situational factors (13).
Results
Search and General Characteristics of Included Studies
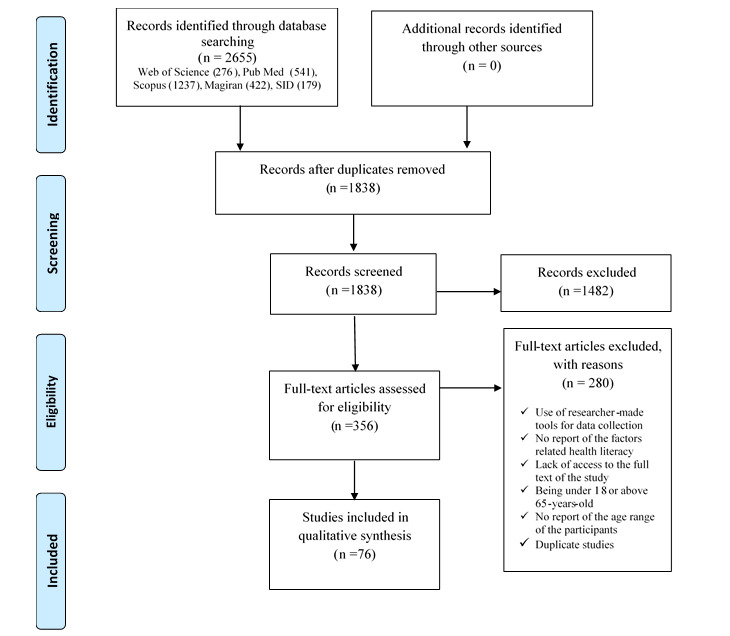
Figure 1 shows the selection process of the studies. In the initial investigation, 2655 articles were found. Then, after removing duplicate reports, the abstracts and titles of the studies were reviewed. Finally, after evaluating the full text of the remaining articles, 76 articles were included in the study, considering the inclusion and exclusion criteria.
Figure 1.
The PRISMA-ScR diagram depicts the process of study selection
Detailed characteristics of the individual studies are summarized in Table 2. Among these articles, 21 studies were conducted on women and 55 others on both men and women. The papers were published from 2014 to 2022. The total sample size was 53,094 participants (31,360 female and 21,564 male participants; in 1 study, the sample size was not mentioned by sex). The sample size of the studies was between 60 and 20,571 people. Of the selected studies, 40 were published in Farsi, and 36 were published in English. Moreover, all analyses were cross-sectional.
Table 2. Characteristics of studies included in the scoping review.
| First author & year | Setting | Participant | Sample size |
|---|---|---|---|
| Tavousi, 2016 (14) | All provinces of the country* | General adult population | 20571 |
| Naghibi, 2017 (15) | Ten areas of Shahriar city | General adult population | 299 |
| Haghdoost, 2019 (16) | Sistan and Baluchestan, Kerman, Markazi, Mazandaran, Qom, Booshehr, Yazd, Isfahan, and Qazvin | General adult population | 8404 |
| Ravati, 2018 (17) | Alborz province | People living in Alborz province | 465 |
| Jahani, 2019 (18) | Health centers of Neishabour City | Adults covered by comprehensive health service centers | 385 |
| Ansari, 2018 (19) | Health network of Shemiranat City | Adults covered by health centers | 170 |
| Baraie, 2020 (20) | Health centers of Bijar City | Adults covered by comprehensive health service centers | 600 |
| Fouladi, 2017 (21) | Health centers of Ardabil City | Middle-aged people covered by comprehensive health service centers | 1049 |
| Joveini, 2019 (22) | Health centers of Bardsakan City | Adults covered by health centers | 700 |
| Nadi, 2020 (23) | Health centers of Arak City | Adults covered by health centers | 750 |
| Shahavandi, 2021 (24) | Health centers of Tehran City | Adults covered by health centers | 261 |
| Isaapare, 2020 (25) | Health centers of Dezfol City | Adults covered by health centers | 1575 |
| Abedini, 2021 (26) | Health centers of Hormozgan province | Adults covered by health centers | 812 |
| Askarian, 2018 (27) | Health centers of Bardsakan City | Adults covered by comprehensive health service centers | 428 |
| Zareban, 2016 (28) | Health centers of Iranshahr, Bampur, and Sarbaz cities in the Baluchistan region | Women covered by health centers | 247 |
| Sajadi, 2016 (29) | Health centers of Izadeh City | Women covered by health centers | 240 |
| Enjezab, 2021 (30) | Health centers of Yazd City | Women covered by health centers | 280 |
| Baghaei, 2017 (31) | Health centers of Orumieh City | Pregnant women | 400 |
| Zaree, 2017 (32) | Health centers of Minab City | Pregnant women | 361 |
| Moshki, 2018 (33) | Health centers of Gonabad City | Pregnant women | 400 |
| Akbarinejad, 2017 (34) | Health centers of Esfahan City | Pregnant women | 351 |
| Izadirad, 2019 (35) | Health centers of Balochistan | Pregnant women | 430 |
| Eslami, 2022 (36) | Health centers of Mashhad City | Pregnant women | 238 |
| Alinejad-Naeini, 2019 (37) | Educational hospitals affiliated with the Tehran University of Medical Sciences | Mothers with preterm infant | 200 |
| Morteza-Nejad, 2019 (38) | Health centers affiliated with Guilan University of Medical Sciences | Mothers with infants | 253 |
| Peyman, 2016 (39) | Health centers of Mashhad City |
Mothers with
children less than three months |
120 |
| Karimi, 2018 (40) | Addiction treatment centers in Tehran city | Women referring to the addiction treatment centers of Tehran | 141 |
| Rostami, 2018 (41) | Welfare Organization of Nourabad City | Women covered by the Welfare Organization | 149 |
| Afshari, 2017 (42) | Mehrkam Pars Automotive Company, Karaj city | Workers | 157 |
| Amini, 2017 (43) | Libraries of the UMS Tehran and the University of Tehran | Librarians | 79 |
| Moghadaszadeh, 2018 (44) | Regional Science and Technology Information Center of Shiraz city | Librarians | 80 |
| Mousavi, 2018 (45) | Province Public Libraries of Mazandaran City | Librarians | |
| Ansari, 2017 (46) | Libraries Foundation of Kerman City | Library users | 375 |
| Rahimi, 2019 (47) | Libraries of Public of Ilam City | Library users | 300 |
| Pashaeypoor, 2018 (48) | Schools of the University of Medical Sciences Tehran | Employees | 150 |
| Ghanbari, 2017 (49) | Schools of the University of Medical Sciences Guilan | Employees | 186 |
| Khoshravesh, 2018 (50) | Hamadan University of Medical Sciences | Employees | 188 |
| Baji, 2019 (51) | Education Culture & Research in Khuzestan | Employees | 209 |
| Zarezadeh, 2020 (52) | Kurdistan University of Medical Sciences | Employees | 202 |
| Solhi, 2017 (53) | Municipality Offices of Shemiranat city | Employees | 360 |
| Kahouei, 2015 (54) | Hospitals affiliated with the Semnan University of Medical Sciences | Employees | 389 |
| Mahdifar, 2021 (55) | Medical centers of Binalood city | Employees | 170 |
| Rahimi, 2019 (56) | Primary schools of Shahrekord city | Teachers | 60 |
| Yusefi, 2019 (57) | Educational hospitals affiliated with the Shiraz University of Medical Sciences | Nurses | 171 |
| Ramezankhani, 2015 (58) | Shahid Beheshti and Shahid Beheshti University of Medical Sciences, Tehran | Students | 370 |
| Barati, 2019 (59) | Schools of Hamadan University of Medical Sciences | Students | 382 |
| Moghaddam, 2019 (60) | Schools of Guilan University of Medical Sciences | Students | 583 |
| Mahdizadeh, 2019 (61) | Schools of Torbat Heydariyeh University of Medical Sciences | Students | 201 |
| Panahi, 2016 (62) | Shahid Beheshti University of Medical Sciences in Tehran | Students | 337 |
| Sajadi, 2020 (63) | Faculty of Isfahan University | Students | 376 |
| Ziaee, 2018 (64) | Islamic Azad University of Kazerun | Students | 200 |
| Khaleghi, 2019 (65) | Islamic Azad University, Shahreri Branch | Students | 278 |
| Dehghankar, 2019 (66) | Imam Khomeini International University of Qazvin | Students | 357 |
| Ahmadi, 2018 (67) | Campuses of Farhangian University | Students | 932 |
| Shekari, 2019 (68) | University Yazd | Students | 400 |
| Namazi, 2020 (69) | Islamic Azad University of Rasht | Students | 250 |
| Mahdizadeh, 2021 (70) | Torbat Heydariyeh University of Medical Sciences | Students | 201 |
| Mahmoudi, 2015 (71) | Postgraduate education Ferdowsi University of Mashhad | Students | 368 |
| Shirzad, 2019 (72) | Dormitory of Tarbiat Modares University of Tehran | Students | 183 |
| Taheri, 2020 (73) | Schools of Iran University of Medical Sciences | Students | 167 |
| Jahanieftekhari, 2018 (74) | Neishabour Health Centers | Health Volunteers | 250 |
| Seyedoshohadaee, 2016 (75) | Diabetes Research Center affiliated with the Tehran University of Medical Sciences | Patients | 200 |
| Shafiei, 2020 (76) | Diabetes Clinic of Imam Sadegh Hospital in Delijan | Patients | 150 |
| Fadaiyan Arani, 2018 (77) | Health Centers of Kaghzi and Hosseinabad in Aran and Bidgol cities | Patients | 120 |
| Taghi Sohrabi, 2020 (78) | Kazeroon Health Centers | Patients | 60 |
| Noroozi, 2019 (79) | Clinic affiliated to Golestan Hospital in Ahvaz | Patients | 362 |
| Izadkhah, 2020 (80) | Qom health centers | Patients | 300 |
| Saba Seif, 2018 (81) | Khorramabad teaching hospitals | Patients | 161 |
| Marzangi, 2018 (82) | Hospitals located in the southern cities of West Azerbaijan province | Patients | 374 |
| Imanian, 2017 (83) | Hospitals affiliated with the Shahid Beheshti University of Medical Sciences | Patients | 299 |
| Qobadi, 2015 (84) | Dialysis Center affiliated with the Tehran University of Medical Sciences | Patients | 204 |
| Yadollahi, 2018 (85) | A public center with breast cancer counseling and treatment in Shiraz | Patients | 196 |
| Roohi, 2020 (86) | Cancer Clinic of Imam Khomeini Hospital in Tehran | Patients | 265 |
| Sedghi, 2019 (87) | Iranian MS Association | Patients | 382 |
| Kazemi, 2019 (88) | Clinics of Shahid Sadoughi University of Medical Sciences in Yazd | Patients | 300 |
| Mollakhalili, 2014 (89) | Hospitals affiliated with Isfahan University of Medical Sciences | Patients | 384 |
The participants of the studies were the general population of men and women in 4 studies, adults (women or men) covered by health centers in 13 studies, pregnant women in 6 studies, mothers with infants and children in 3 studies, addict women in 1 study, women covered by the Welfare Organization in 1 study, workers in 1 study, employees in 13 studies, library users in 2 studies, university students in 16 studies, health volunteers in 1 study, and patients in 15 studies. The questionnaires of Health Literacy for Iranian Adults (54 studies), Test of Functional Health Literacy Adult (13 studies), Iranian Health Literacy Questionnaire (3 studies), Short Test of Functional Health Literacy Adult (3 studies), Newest Vital Sign (2 studies) and Functional, Communicative, and Critical Health Literacy Scale (1 study) were used in these studies.
Factors Affecting Health Literacy
Factors related to health literacy among Iranian people were divided into 3 categories based on the integrated model of health literacy. Accordingly, the most decisive factor related to health literacy is education. Appendix 1 provides a detailed list of factors associated with health literacy identified in each study included in this scoping review.
Personal Factors
Sex: Eighteen studies were significant, and 26 studies were not significant.In 12 studies (14, 16, 18, 20, 23, 51, 60, 62, 65, 67, 69, 71), the health literacy score was was significantly higher in women, and in 3 studies, this score was significantly higher in men (21, 77, 82). Three studies referred only to the significance of sex (48, 68, 75).
Age: A total of29 studies were significant, and 22 studies were not significant. One study reported a positive and statistically significant relationship between age and health literacy based on the correlation coefficient (57). Based on the correlation coefficient, 6 studies reported a statistically significant negative relationship between age and health literacy (34, 77, 80, 83, 88, 89). In 1 study, the literacy score decreased significantly for each year of age increase (61). In 3 studies, the literacy score increased significantly for each year of age increase (16, 50, 56). Based on the results of other studies, the health literacy score is lower at much younger and much older ages (15, 18-20, 22, 25-30, 42, 46, 53, 67, 74, 79, 82).
Education Level: A total of 43 studies were significant, and 8 were insignificant. In 41 studies, the level of health literacy was significantly higher in people with higher education levels (15-20, 22-31, 33-35, 38, 39, 41, 42, 45, 46, 49, 50, 52-54, 59, 71, 74, 77, 79, 80, 82-84, 88, 89). Conversely, in 2 studies, the level of health literacy was significantly lower in people with higher education levels (40, 75).
Field of Study: Two studies were significant, and 6 were insignificant. One study found that nonmedical students had significantly lower health literacy than medical students (58). Another study found that health literacy significantly differed in various medical disciplines (59). In other studies, health literacy was not very different in multiple nonmedical disciplines (43, 45, 65, 66, 69, 71).
Parents Education Level: Two studies were significant, and 2 studies were not significant. In 2 studies, a statistically significant relationship was observed between health literacy and father's education (60, 68).
Marital status: Twelve studies were significant, and 19 were insignificant. Inadequate health literacy was reported in 4 studies in singles (50, 65, 67, 80), in 3 studies in married (82, 88,89), and in 3 studies in widowed or divorced participants (22, 27, 79). Two studies referred only to the significance of marital status (68, 83).
Occupation: A total of 23 studies were significant, and 11 studies were not significant. The lowest level of health literacy was observed in 6 studies on housewives (23, 25, 28, 31, 46, 80), 6 studies on retirees (15, 22, 27, 40, 88, 89), 4 studies on workless people (16, 18, 38, 79), and 1 study on students (26). It was reported in 1 study that the health literacy of unemployed students was lower than that of employed students (66). Another study indicated that the health literacy of nonmedical staff was lower than that of medical staff (54). Two studies referred only to the significance of occupation (35, 68). Conversely, the highest level of health literacy was reported in 1 study on unemployed people (17). Accordingly, it can be concluded that occupation is one of the most important factors affecting health literacy and that unemployed people (unemployed students, homemakers, and workless people) and retirees have lower health literacy.
Work experience: One study was significant, and 3 were insignificant. One study found a significantly positive relationship between health literacy and work experience (57).
Employment status: In 1 study, there was a significantly positive correlation between employment status and health literacy (57).
Ethnicity: It was revealed in 1 study that Fars ethnicity had higher health literacy than non-Fars ethnic groups (17).
Income: Eight studies were significant, and 8 studies were not significant. It was indicated in 8 studies that health literacy was significantly lower in people with lower incomes (20, 28, 31, 32, 60, 62, 74, 83).
Socioeconomic Status: Five studies were significant, and 3 were insignificant. Five studies reported a statistically significant relationship between health literacy and socioeconomic status (23, 26, 51, 75, 82). People with better economic and social status had higher health literacy.
Self-efficacy: Four studies were significant, and 1 study was not. Four studies reported a positive correlation between health literacy and self-efficacy. People with higher self-efficacy had more health literacy (37, 76, 81, 86).
Addiction: In 1 study, a statistically significant relationship was found between health literacy and addiction (40).
Number of Children: In 2 studies, there was a statistically significant relationship between health literacy and the number of children (32, 67). In the Ahmadi et al study, the lowest mean health literacy score was reported in families without children (67). Two studies were not significant (38, 55).
Medical History: Three studies were significant, and 1 study was not. In 3 studies, a lower level of health literacy was observed among people with a history of underlying disease (22, 27, 82).
Duration of Disease: One study was significant, and 1 was not. In 1 study, there was a statistically significant relationship between health literacy and the time since the diagnosis of heart disease. The health literacy level was lower in patients who had been diagnosed with the disease for a longer period (82).
Media Literacy: In 2 studies, a significantly positive correlation was observed between health literacy and media literacy. People with higher levels of media literacy appeared to have higher levels of health literacy (34, 72).
Computer Literacy: A study on university students revealed a statistically significant relationship between health literacy and computer literacy. Based on the results of multivariate linear regression in this study, dimensions of computer literacy could predict up to 63% of changes in the health literacy score of the students (70).
Information Literacy: The results of 2 studies on students (71, 73) and 1 study on IT staff (44) indicated a statistically significant relationship between health literacy and information literacy. Thus, people with higher information literacy had better health literacy.
Situational Factors
Source of Information: Ten studies were significant, and 3 were not. Based on the results of 10 studies, there was a statistically significant relationship between health literacy and the source of information. The highest level of literacy belonged to books and brochures in 4 studies (23, 28, 54, 60), friends and physicians in 2 studies (19, 30), radio and television in 1 study (23), and the internet in 1 study (53). The lowest level of literacy was observed in 3 studies in people who used books and brochures (19, 30, 53), in 2 studies in those who used friends (23, 52), and in 1 study in those who gained information from their colleagues (45).
Participation in Health Education Classes: According to the results of 1 study, there was a statistically significant relationship between health literacy and health education classes (45).
Use of the Internet: A significantly positive correlation was reported between health literacy and internet use in 1 study. Health literacy was higher in people who used more internet (60)
Use of Social Networks: The results of 2 studies on library users revealed a statistically significant relationship between health literacy and the use of social networks; thus, the greater the use of social networks was, the higher the level of health literacy of users (47, 48).
Social Support: In 3 studies, a significantly positive correlation was found between health literacy and social support. People with more social support had better health literacy (37, 64, 86).
Societal and Environmental Factors
Place of Residence: Three studies were significant, and 4 were not. Health literacy in 1 study was significantly lower in rural areas than in urban areas (79), whereas it was significantly higher in 2 studies (16, 32).
Type of Insurance: One study was significant, and 4 were not. A statistically significant relationship was reported between health literacy and kind of insurance, as moderate health literacy in people with regular insurance was higher than in those with supplemental insurance (49).
Discussion
This study aimed to determine the factors related to health literacy in the Iranian population. Based on the results of the study, related factors include personal factors (sex, age, education level, field of study, education of parent, marital status, occupation, work experience, employment status, ethnicity, income, socioeconomic status, medical history, duration of disease, addiction, number of children, media literacy, information literacy, computer literacy, self-efficacy), situational factors (use of internet, use of social network, social support, source of information, participation in health education classes), and societal and environmental factors (place of residence, type of insurance).
Based on the study's results, education level is the most decisive factor related to health literacy; thus, the higher the education level is, the higher one's health literacy (15-20, 22-31, 33-35, 38-42, 45, 46, 49, 50, 52-54, 59, 71, 74, 75, 77, 79, 80, 82-84, 88-90). According to a systematic review, education strongly predicts health literacy. Low education level, difficulty in written communication, and limited familiarity with medical terms probably impair one's ability to interact with the health care system (91) successfully. These findings are consistent with the results of the present study. Furthermore, the results of this study indicated that health literacy is higher in medical disciplines than in nonmedical fields (58). There was no statistically significant difference in health literacy among different nonmedical disciplines (43, 45, 65, 66, 69, 71).
In the present scoping review, 18 studies revealed a relationship between health literacy and sex (14, 16, 18, 20, 21, 23, 48, 51, 60, 62, 65, 67-69, 71, 75, 77, 82). It was found in most of these studies that the health literacy of women was significantly higher than that of men (14, 16, 18, 20, 23, 48, 51, 60, 62, 65, 67-69, 71, 75). The need to care for sick family members gives them a better chance to gain health-related knowledge and, consequently, women have a higher level of literacy in this regard (92). This study's results align with the study conducted by Lee et al (93).
According to the results of 29 studies, there was a statistically significant relationship between health literacy and age (15, 16, 18, 19, 22, 25-30, 34, 42, 46, 50, 53, 56, 57, 59, 61, 67, 74, 75, 77, 79, 80, 82, 83, 88, 89).
Inadequate health literacy seems more prevalent at much younger and much older ages. With increasing age, deficiencies occur in one's literacy, caused by reduced cognitive function, distance from formal school years, and decreased sensory ability. Age was determined to be a health literacy-related factor in the systematic review conducted by Paasche-Orlow et al (94).
As shown in our study, marital status was considered one of the factors related to health literacy in 12 studies (22, 27, 50, 65, 67, 68, 79, 80, 82, 83, 88, 89). Eight studies reported inadequate and low health literacy among unmarried people (4 studies in single people [50, 65, 67, 80], 3 studies in widowed or divorced people [22, 27, 79]) and 3 studies in married people (82, 88, 89). These contradictions can be due to different types of tools, places and times of the study, types of participants, and other characteristics. Generally, it can be claimed that people who have the support of their spouse during their life are more likely to have a higher level of health literacy. Marriage enhances social interactions, the development of social networks, and economic support, thereby improving health literacy skills (50, 95). These results align with the study conducted by Rikard et al (95).
Based on the results of 23 studies, there was a statistically significant relationship between job and health literacy (15-18, 22, 23, 25-28, 30, 31, 35, 38, 40, 46, 54, 66, 68, 79, 80, 88, 89). Generally, in most of these studies, inadequate health literacy was more prevalent among unemployed and retired people (15-18, 22, 23, 25, 27, 28, 31, 38, 40, 46, 66, 79, 80, 88, 89, 96).
In the present scoping review, the results of 5 studies indicated a relationship between health literacy and socioeconomic status (23, 26, 51, 75, 82); this result aligns with the study of Coraline Stormacq et al. In their systematic review, these researchers argued that, as one of the most critical factors, unfavorable socioeconomic conditions are associated with low levels of health literacy (97).
In our review, 8 studies revealed a statistically significant relationship between health literacy and income level to the extent that people with higher income had a higher literacy level (20, 28, 31, 32, 60, 62, 83). The results of these studies are in line with the results of 2 other systematic reviews. Optimal socioeconomic conditions and a reasonable income level can promote health literacy by providing better access to information resources (3, 97).
In the present study, Zaree et al's results showed that health literacy was higher in the urban population (32). In contrast, Haghdoost et al (16) and Noroozi et al (79) indicated that the rural population had higher health literacy. Haghdoost et al attributed the higher health literacy of the rural population to more and easier access of villagers to doctors and health care workers, as well as the implementation of the family doctor program (at the time of the study, this program was implemented only in rural areas)(16). Being rural alone does not explain the difference between rural and urban health literacy, and demographic and social factors also play an important role (98). This has also been confirmed by Shayakhmetov et al (99).
According to the results of our study, people with a history of disease had lower health literacy (22, 27, 82). These results align with the study conducted by Charoghchian Khorasani et al (100). People with low health literacy are less likely to adhere to health guidelines because they have limited access to and difficulty comprehending oral and written health information (22).
As revealed in the present study, having skills and abilities such as using the internet (60), using social networks(47, 48), media literacy (34, 72), information literacy (44, 71, 73), and computer literacy (70), can help people to search for information and understand it better; thus, these factors are associated with higher health lit
eracy (47).
In the present review, the results of 4 studies introduced self-efficacy as one of the factors related to health literacy (37, 76, 81, 86). These results align with the findings of a systematic review conducted by Xu XY et al. One possible reason could be that people with higher self-efficacy value their ability to understand and interpret health information; therefore, they may mentally overestimate their health literacy (101).
In the present study, the results of 3 studies indicated a relationship between health literacy and social support (37, 64, 86). These results are in line with the study of Lee et al. The researchers found that supporting people's social networks could improve their ability to receive and understand health information (102).
Conclusions about other factors, including number of children (32, 67), addiction (40), type of insurance (49), work experience (57), employment status (57), duration of illness (82), and education of the parents (60, 68), were not adequate due to the small number of studies.
Limitations
All included studies were cross-sectional studies (descriptive-analytical or correlational). These studies have inherent potential limitations, such as weak identification of causal relationships between variables and the effect of confounding variables on the primary outcomes, limiting the possibility of more accurate conclusions and identifying the related factors.
Conclusion
Based on the results of this study, education level was the most decisive factor affecting health literacy. This study's strength lies in identifying the relevant modifiable factors. These factors were not mentioned in previous systematic reviews conducted in Iran. Thus, by considering initiatives such as boosting self-efficacy, social support, media literacy, information literacy, computer literacy, and easy access to health information via the internet or social networks, this study helps researchers and health policymakers create interventions for promoting health literacy.
Conflict of Interests
The authors declare that they have no competing interests.
Funding
This study was supported by Shahid Beheshti University of Medical Sciences (research project number: 30155).
Acknowledgment
This study was extracted from a PhD thesis in reproductive health from Shahid Beheshti University of Medical Sciences in Tehran, Iran. The authors would like to express their gratitude to the Vice Chancellor for Research of Shahid Beheshti University of Medical Sciences.
Ethical Approval
The study was approved by the ethics committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.PHARMACY.REC.1400.194).
Appendix 1.
Health literacy related factors in included studies.
| First author & year | Gender | Age | Education | Field of study | Education of parent | Marital status | Occupation | Work experience | Employment status | Ethnicity | Income | Socioeconomic status | Place of residence | Medical history | Duration of disease | Type of insurance | Media literacy | Computer literacy | Information literacy | Source of information | Education classes | Use of Internet | Use of social network | Social support | Self-efficacy | Addiction | Number of children | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Tavousi, 2016 (12) | |||||||||||||||||||||||||||
| 2. | Naghibi, 2017 (13) | |||||||||||||||||||||||||||
| 3. | Haghdoost, 2019 (14) | |||||||||||||||||||||||||||
| 4. | Ravati, 2018 (15) | |||||||||||||||||||||||||||
| 5. | Jahani, 2019 (16) | |||||||||||||||||||||||||||
| 6 | Ansari, 2018 (17) | |||||||||||||||||||||||||||
| 7 | Baraie, 2020 (18) | |||||||||||||||||||||||||||
| 8 | Fouladi, 2017 (19) | |||||||||||||||||||||||||||
| 9 | Joveini, 2019 (20) | |||||||||||||||||||||||||||
| 10 | Nadi , 2020 (21) | |||||||||||||||||||||||||||
| 11 | Shahavandi, 2021 (22) | |||||||||||||||||||||||||||
| 12 | Isaapare, 2020 (23) | |||||||||||||||||||||||||||
| 13 | Abedini, 2021 (24) | |||||||||||||||||||||||||||
| 14 | Askarian, 2018 (25) | |||||||||||||||||||||||||||
| 15 | Zareban, 2016 (26) | |||||||||||||||||||||||||||
| 16 | Sajadi, 2016 (27) | |||||||||||||||||||||||||||
| 17 | Enjezab, 2021 (28) | |||||||||||||||||||||||||||
| 18 | Baghaei, 2017 (29) | |||||||||||||||||||||||||||
| 19 | Zaree, 2017 (30) | |||||||||||||||||||||||||||
| 20 | Moshki, 2018 (31) | |||||||||||||||||||||||||||
| 21 | Akbarinejad, 2017 (32) | |||||||||||||||||||||||||||
| 22 | Izadirad, 2019 (33) | |||||||||||||||||||||||||||
| 23 | Eslami, 2022 (34) | |||||||||||||||||||||||||||
| 24 | Alinejad-Naeini, 2019 (35) | |||||||||||||||||||||||||||
| 25 | Morteza-Nejad, 2019 (36) | |||||||||||||||||||||||||||
| 26 | Peyman, 2016 (37) | |||||||||||||||||||||||||||
| 27 | Karimi, 2018 (38) | |||||||||||||||||||||||||||
| 28 | Rostami, 2018 (39) | |||||||||||||||||||||||||||
| 29 | Afshari, 2017 (40) | |||||||||||||||||||||||||||
| 30 | Amini, 2017 (41) | |||||||||||||||||||||||||||
| 31 | Moghadaszadeh, 2018 (42) | |||||||||||||||||||||||||||
| 32 | Mousavi, 2018 (43) | |||||||||||||||||||||||||||
| 33 | Ansari, 2017 (44) | |||||||||||||||||||||||||||
| 34 | Rahimi, 2019 (45) | |||||||||||||||||||||||||||
| 35 | Pashaeypoor, 2018 (46) | |||||||||||||||||||||||||||
| 36 | Ghanbari, 2017 (47) | |||||||||||||||||||||||||||
| 37 | Khoshravesh, 2018 (48) | |||||||||||||||||||||||||||
| 38 | Baji, 2019 (49) | |||||||||||||||||||||||||||
| 39 | Zarezadeh, 2020 (50) | |||||||||||||||||||||||||||
| 40 | Solhi, 2017 (51) | |||||||||||||||||||||||||||
| 41 | Kahouei, 2015 (52) | |||||||||||||||||||||||||||
| 42 | Mahdifar, 2021 (53) | |||||||||||||||||||||||||||
| 43 | Rahimi, 2019 (54) | |||||||||||||||||||||||||||
| 44 | Yusefi, 2019 (55) | |||||||||||||||||||||||||||
| 45 | Ramezankhani, 2015 (56) | |||||||||||||||||||||||||||
| 46 | Barati, 2019 (57) | |||||||||||||||||||||||||||
| 47 | Moghaddam, 2019 (58) | |||||||||||||||||||||||||||
| 48 | Mahdizadeh, 2019 (59) | |||||||||||||||||||||||||||
| 49 | Panahi, 2016 (60) | |||||||||||||||||||||||||||
| 50 | Sajadi, 2020 (61) | |||||||||||||||||||||||||||
| 51 | Ziaee, 2018 (62) | |||||||||||||||||||||||||||
| 52 | Khaleghi, 2019 (63) | |||||||||||||||||||||||||||
| 53 | Dehghankar, 2019 (64) | |||||||||||||||||||||||||||
| 54 | Ahmadi, 2018 (65) | |||||||||||||||||||||||||||
| 55 | Shekari, 2019 (66) | |||||||||||||||||||||||||||
| 56 | Namazi, 2020 (67) | |||||||||||||||||||||||||||
| 57 | Mahdizadeh, 2021 (68) | |||||||||||||||||||||||||||
| 58 | Mahmoudi, 2015 (69) | |||||||||||||||||||||||||||
| 59 | Shirzad, 2019 (70) | |||||||||||||||||||||||||||
| 60 | Taheri, 2020 (71) | |||||||||||||||||||||||||||
| 61 | Jahanieftekhari, 2018 (72) | |||||||||||||||||||||||||||
| 62 | Seyedoshohadaee, 2016 (73) | |||||||||||||||||||||||||||
| 63 | Shafiei, 2020 (74) | |||||||||||||||||||||||||||
| 64 | Fadaiyan Arani, 2018 (75) | |||||||||||||||||||||||||||
| 65 | Taghi Sohrabi, 2020 (76) | |||||||||||||||||||||||||||
| 66 | Noroozi, 2019 (77) | |||||||||||||||||||||||||||
| 67 | Izadkhah, 2020 (78) | |||||||||||||||||||||||||||
| 68 | Saba Seif, 2018 (79) | |||||||||||||||||||||||||||
| 69 | Marzangi, 2018 (80) | |||||||||||||||||||||||||||
| 70 | Imanian, 2017 (81) | |||||||||||||||||||||||||||
| 71 | Qobadi, 2015 (82) | |||||||||||||||||||||||||||
| 72 | Yadollahi, 2018 (83) | |||||||||||||||||||||||||||
| 73 | Roohi, 2020 (84) | |||||||||||||||||||||||||||
| 74 | Sedghi, 2019 (85) | |||||||||||||||||||||||||||
| 75 | Kazemi, 2019 (86) | |||||||||||||||||||||||||||
| 76 | Mollakhalili, 2014 (87) |
Cite this article as: Shahrahmani H, Kariman N, Ahmadi A, Nasiri M, Keshavarz Z. Factors Related to Health Literacy Among the Iranian Population: A Scoping Review. Med J Islam Repub Iran. 2023 19 Dec);37:138 https://doi.org/10.47176/mjiri.37.138
References
- 1.Kanj M, Mitic W, editors. Health literacy and health promotion: Definitions, concepts, and examples in the Eastern Mediterranean region. 7th Global Conference on Health Promotion Promoting Health and Development: Closing the Implementation Gap;; 7th Global Conference on Health Promotion; 26-30 October 2009; Kenya. [Google Scholar]
- 2.Nutbeam D. Health promotion glossary. Health Promot Int. 1998;13(4):349. doi: 10.1093/heapro/dal033. [DOI] [PubMed] [Google Scholar]
- 3.Rajah R, Hassali MAA, Murugiah MK. A systematic review of the prevalence of limited health literacy in Southeast Asian countries. Public Health. 2019;167:8–15. doi: 10.1016/j.puhe.2018.09.028. [DOI] [PubMed] [Google Scholar]
- 4.Sørensen K, Van den, Fullam J, Doyle G, Pelikan J, Slonska Z. et al. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health. 2012;12(80):1–13. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health. Promoting health in the SDGs: Report on the 9th Global conference for health promotion, Shanghai, China, 21–24 November 2016: all for health, health for all; World Health Organization;; 21–24 November 2016; Shanghai, China. [Google Scholar]
- 6.Flottorp SA, Oxman AD, Krause J, Musila NR, Wensing M, Godycki-Cwirko M. et al. A checklist for identifying determinants of practice: A systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement Sci. 2013;8(35):1–11. doi: 10.1186/1748-5908-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 8.McCormack L, editor. Measures of health literacy: Workshop summary; 2009: Washington, DC: National Academy of Sciences. [DOI] [Google Scholar]
- 9.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review. Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 11.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L. et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119. doi: 10.11124/JBIES-20-00167. [DOI] [PubMed] [Google Scholar]
- 12.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D. et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 13.Sørensen K, Van den, Fullam J, Doyle G, Pelikan J, Slonska Z. et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tavousi M, Haeri Mehrizi, Rafiefar S, Solimanian A, Sarbandi F, Ardestani M. et al. Health literacy in Iran: Findings from a national study. Payesh. 2016;15(1):95–102. [Google Scholar]
- 15.Naghibi A, Chaleshgar M, Kazemi A, Hosseini M. Evaluation of health literacy level among 18-65 year-old adults in Shahriar, Iran. J Health Res Community. 2017;3(2):17–25. [Google Scholar]
- 16.Haghdoost AA, Karamouzian M, Jamshidi E, Sharifi H, Rakhshani F, Mashayekhi N. et al. Health literacy among Iranian adults: Findings from a nationwide population-based survey in 2015. East Mediterr Health J. 2019;25(11):828. doi: 10.26719/emhj.19.017. [DOI] [PubMed] [Google Scholar]
- 17.Ravati S, Farid M. The health literacy of adults in Alborz province in Iran. J Community Health Res. 2018;7(4):222. [Google Scholar]
- 18.Jahani Eftekhari, Rahimnia M, Esfahanian H, Bazoobandi B, Shams M. Health Literacy level of Adults in Neyshabur City: A Cross-Sectional Study. J Educ Community Health. 2019;6(3):161. [Google Scholar]
- 19.Ansari M, Mohammad-Moradi F, Khaledian M, Shekofteh M. Assessment of health literacy level in 18-30 year-old adults, an Iranian experience. Libr Philos Pract. 2018;1850:1–15. [Google Scholar]
- 20.Baraie B, Pashaei T, Kakemam E, Mahmoodi H. Health literacy and its predictors among urban and rural adults in Bijar County. J Educ Health Promot. 2020;9(181):1–6. doi: 10.4103/jehp.jehp_116_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fouladi N, Hazrati S, Shabani M, Nejaddadgar N. Investigating middle-aged health literacy in Ardabil. J Health Lit. 2017;2(1):39–44. [Google Scholar]
- 22.Joveini H, Rohban A, Askarian P, Maheri M, Hashemian M. Health literacy and its associated demographic factors in 18–65-year-old, literate adults in Bardaskan, Iran. J Educ Health Promot. 2019;8(244):1–8. doi: 10.4103/jehp.jehp_26_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nadi T, Poorolajal J, Doosti-Irani A. Socioeconomic status and health literacy as the important predictors of general health in Iran: a structural equation modeling approach. Epidemiol Biostat Public Health. 2020;17(2):e13312. [Google Scholar]
- 24.Shahavandi M, Ghorbaninejad P, Mohammadpour S, Djafari F, Shahinfar H, Sheikhhossein F. et al. Higher health literacy score is associated with better healthy eating index in Iranian adults. Nutrition. 2021;90(111262) doi: 10.1016/j.nut.2021.111262. [DOI] [PubMed] [Google Scholar]
- 25.Isaapare O, Ehsanbakhsh H, Kassani A, Najafi Fard, Poraein R, Gholami M. Evaluation of Health Literacy and Some of Its Associated Factors among 18-65 Years Old. J Health Lit. 2020;4(4):30. [Google Scholar]
- 26.Abedini S, Nooradin S, Mohseni S, Daryafti H, Ezati-rad R. Health literacy and health-promoting behaviors in southern Iran. J Health Lit. 2021;6(2):53–60. [Google Scholar]
- 27.Askarian P, Hashemian M, Joveini H, Solimanian A, Rastaghi S. A Survey on the Level of Health Literacy among the Women in Bardaskan City, Iran, in Year 2016: A Cross-Sectional Study. J Health Syst Res. 2018;14(1):35–40. [Google Scholar]
- 28.Zareban I, Izadirad H. Evaluation of health literacy, health status and health services utilization in women in Baluchistan region of Iran. J Health Lit. 2016;1(2):71–82. [Google Scholar]
- 29.Sajadi H, Hosseinpour N, Sharifian Sani, Mahmoodi Z. Association between health literacy and life style in married rural women in Izeh, Iran. J Health. 2016;7(4):479. [Google Scholar]
- 30.Enjezab B, Zarehosseinabadi F, Tafti AD, Zarehosseinabadi M. The relationship between health literacy dimensions and perceived risk of cardiovascular disease in middle-aged Iranian women. Iran J Nurs Midwifery Res. 2021;26(3):279. doi: 10.4103/ijnmr.IJNMR_104_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baghaei R, Najarzadeh M, Saei M, Mohamadi N. Functional health literacy in pregnant women in health centers of Urmia city-2015. Nurs Midwifery Res J. 2017;15(5):368. [Google Scholar]
- 32.Zaree F, Karimi F, Mohseni S, Mdani S, Dadipoor S, Mdani AH. Health literacy of pregnant women and some related factors in pregnant women referred to Minab health centers. J Prev Med. 2017;4(2):40. [Google Scholar]
- 33.Moshki M, Mirzania M, Kharazmi A. The relationship of health literacy to quality of life and demographic factors in pregnant women: a cross-sectional study. J Health Lit. 2018;2(4):203. [Google Scholar]
- 34.Akbarinejad F, Soleymani MR, Shahrzadi L. The relationship between media literacy and health literacy among pregnant women in health centers of Isfahan. J Educ Health Promot. 2017;6(17):1–6. doi: 10.4103/2277-9531.204749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Izadirad H, Ali Ahmadi, Niknami S. Predicting factors influencing prenatal care based on Health Literacy in Balochistan primigravida Women. J Health Lit. 2019;3(4):16–24. [Google Scholar]
- 36.Eslami V, Tavakkoli-Sani S, Ghavami V, Peyman N. The Relationship of Health literacy with Preventive Behaviors of Urinary Tract Infection in Pregnant Women. J Health Lit. 2022;6(4):22–31. [Google Scholar]
- 37.Alinejad-Naeini M, Razavi N, Sohrabi S, Heidari-Beni F. The association between health literacy, social support and self-efficacy in mothers of preterm neonates. J Matern Fetal Neonatal Med. 2019;34(11):1703. doi: 10.1080/14767058.2019.1644620. [DOI] [PubMed] [Google Scholar]
- 38.Morteza-Nejad SHRF, Yektakooshali M, Moshtaghikojal S, Salmalian Z, Ramezani A, Esmaeilpourbandboni M. Health Literacy and its Related Factors in Infant's Mothers. J Commut Med Health Educ. 2019;6(4):239. [Google Scholar]
- 39.Peyman N, Abdollahi M. The relationship between health literacy and self-efficacy physical activity in postpartum women. J Health Lit. 2016;1(1):5–12. [Google Scholar]
- 40.Karimi M, Jalili Z, Mahmoodi M. Relationship between Health Literacy and Addiction among Women of Reproductive Age Referring to Addiction Treatment Centers in Tehran, Iran. J Commut Med Health Educ. 2018;5(1):36–41. [Google Scholar]
- 41.Rostami F, Mohaqeqi Kamal, Sajjadi H, Nosrati Nejad, Hosseinzadeh S, Ghaedamini Harouni. Does mothers' health literacy affect their children's quality of life. Koomesh. 2018;20(3):432. [Google Scholar]
- 42.Afshari M, Teimori G, Kohnavard B, Pour H, Kangavari M. Workers' health literacy in a car spare parts factory: A cross-sectional study. Iran Occup. Health. 2017;14(2):147. [Google Scholar]
- 43.Amini M, Mostafavizade M. Survey on health literacy of librarians in Tehran University and Tehran University of Medical Sciences. Depict Health. 2017;7(4):37–45. [Google Scholar]
- 44.Moghadaszadeh H. The Relationship between Information Literacy and Health Literacy: A Case Study of the Staff of Shiraz Regional Center for Information Science and Technology. J Librariansh Inf Sci. 2018;7(2):144. [Google Scholar]
- 45.Mousavi Chalak, Riahi A. Evaluation of health literacy and resources to achieve them among librarians of Mazandaran public library. J Inflamm. 2018;21(6):73. [Google Scholar]
- 46.Ansari M, Shahdadneghad E, Khaledian M, Salajegheh M. Survey of health literacy of people referred to the libraries of public libraries foundation. Health Inf Manage. 2017;14(5):224. [Google Scholar]
- 47.Rahimi S, Fattahi M. The Relationship between the Use of Social Networks and the Health Literacy of Ilam Public Library Users in 2018. J Payavard Salamat. 2019;13(3):201. [Google Scholar]
- 48.Pashaeypoor S, Salemi N, Ansari M. The relationship between health literacy and the use of social networking in administrative staff of Tehran university of medical sciences. Iran J Nurs Res. 2018;13(2):67–73. [Google Scholar]
- 49.Ghanbari A, Rahmatpour P, Khalili M, Mokhtari N. Health literacy and its relationship with cancer screening behaviors among the employees of Guilan University of Medical Sciences. J Health Care. 2017;18(4):306. [Google Scholar]
- 50.Khoshravesh S, Moeini B, Rezapur-Shahkolai F, Taheri-Kharameh Z, Bandehelahi K. Health literacy of employees of Hamadan University of medical sciences and related demographic factors. J Commut Med Health Educ. 2018;5(1):19–26. [Google Scholar]
- 51.Baji Z, Shakerinejad G, Jarvandi F, Hajinajaf S. Health Literacy Level and its Related Demographic Factors among Employees of Iranian Academic Center for Education, Culture & Research (ACECR)-Khuzestan Branch. J Health Lit. 2019;3(4):46–54. [Google Scholar]
- 52.Zarezadeh Y, Eskandari N, Moradi M, Abdi N. The relationship between health literacy and quality of life of employees in campus of Kurdistan University of Medical Sciences. J Health Lit. 2020;4(4):38–45. [Google Scholar]
- 53.Solhi M, Jormand H. Assessment of health literacy of municipal employees in Shemiranat, Iran. Electron Physician. 2017;9(12):6072. doi: 10.19082/6072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kahouei M, Roghani PS, Zadeh JM, Firouzeh M. The determinants of nursing, allied health and non medical staffs’health literacy in hospitals of a developing country. Mater Sociomed. 2015;27(6):421. doi: 10.5455/msm.2015.27.421-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mahdifar M, Ghavami V, Vahedian-Shahroodi M. Health Literacy and Body Image Concern Among Healthcare Employees in Binaloud, Iran. J Health Lit. 2021;6(1):31–40. [Google Scholar]
- 56.Rahimi B, Tavassoli E. Measuring health literacy of elementary school teachers in Shahrekord. J Health Lit. 2019;4(1):25–32. [Google Scholar]
- 57.Yusefi A, Ebrahim Z, Bastani P, Najibi M, Radinmanesh M, Mehrtak M. Health literacy status and its relationship with quality of life among nurses in teaching hospitals of Shiraz University of Medical Sciences. Iran J Nurs Midwifery Res. 2019;24(1):73. doi: 10.4103/ijnmr.IJNMR_205_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ramezankhani A, Ghafari M, Rakhshani F, Ghanbari S, Azimi S. Comparison of health literacy between medical and non-medical students in Shahid Beheshti Universities in the academic. J Intellect Cap. 2015;20(2):78–85. [Google Scholar]
- 59.Barati M, Fathi N, Aahmadpur E, Jormand H. Investigate the Relationship Between Health Literacy and Health Promoting Behavior in Students. J Health Lit. 2019;4(3):56–65. [Google Scholar]
- 60.Moghaddam R, Mokhtari Lakeh, Rahebi SM, Kazemnezhad Leili. Health literacy and its relationship with body mass index. J Holist Nurs. 2019;29(3):8–14. [Google Scholar]
- 61.Mahdizadeh F, Tatari M, Sheykhotayefeh M. Study of health literacy and its related factors in Torbat Heydarieh students of medical sciences in 2019. J Health Lit. 2019;4(2):44. [Google Scholar]
- 62.Panahi R, Ramezankhani A, Tavousi M, Osmani F, Ghazanfari E, Niknami S. Evaluation of Health Literacy and its influencing factors on dormitory students of Shahid Beheshti University of Medical Sciences in Tehran. J Commut Med Health Educ. 2016;3(3):30. [Google Scholar]
- 63.Sajadi FA, Sajadi HS, Panahi R. Health literacy of university students and its influential factors: A case study at Isfahan University. J Commut Med Health Educ. 2020;7(1):23. [Google Scholar]
- 64.Ziaee S. Predictors of health promotion behavior of female students of azad islamic university, kazerun branch: role of social support and health literacy. J Health Lit. 2018;2(4):223. [Google Scholar]
- 65.Khaleghi M, Amin SF, Peyman N. The relationship between health literacy and health-related quality of life in students. J Educ Health Promot. 2019;7(1):66–73. [Google Scholar]
- 66.Dehghankar L, Hajikarimbaba M, Panahi R. Health literacy and factors related to it among female students of Imam Khomeini international university in Qazvin, Iran. J Public Health Res. 2019;17(3):295–306. [Google Scholar]
- 67.Ahmadi FZ, Mehrmohammadi M, Talaee E, Fardanesh H, Paknahad M, Taghizadeh S. et al. Health literacy among students of Farhangian University. Iran J Health Sci. 2018;17(3):257. [Google Scholar]
- 68.Shekari H. Investigating and prioritizing factors affecting health literacy in university students of Yazd using artificial neural network technique. J Community Health Res. 2019;8(1):29–37. [Google Scholar]
- 69.Namazi A. Health Literacy and Its Related Factors in Non-medical College Students. J Holist Nurs. 2020;30(4):233. [Google Scholar]
- 70.Mahdizadeh f, mahdizadeh f, tatari m, sheykhtayefeh m. The Relationship between Health Literacy and Computer Literacy among Torbat Heydarieh Students of Medical Sciences. Payavard Salamat. 2021;15(2):118. [Google Scholar]
- 71.Mahmoudi H, Taheri A. Relation between information literacy and health literacy of students in Ferdowsi University of Mashhad. Human Information Interaction. 2015;2(2):31–41. [Google Scholar]
- 72.Shirzad M, Taraghi Khah, Lafte A. The role of media literacy in health literacy and Internet addiction among female postgraduate students. J Res Health. 2019;9(3):254. [Google Scholar]
- 73.Taheri A, Langarizadeh M, Dehkordi JG, Yousefianzadeh O. Development of health literacy among postgraduate students: From information literacy perspective. J Educ Health Promot. 2020;9(338):1–6. doi: 10.4103/jehp.jehp_340_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jahanieftekhari M, Peyman N, Doosti H. Health literacy and health-promoting lifestyle among health volunteers in neyshabour. J Ilam Univ Med Sci. 2018;26(3):7–15. [Google Scholar]
- 75.Seyedoshohadaee M, Barasteh S, Jalalinia F, Eghbali M, Nezami M. The relationship between health literacy and self-care behaviors in patients with type 2 diabetes. Iran. J Nurs. 2016;10(4):43–51. [Google Scholar]
- 76.Shafiei H, Nasiri S. The role of health literacy, psychological well-being and self–efficacy in prediction the quality of life of patients with type 2 diabetes. J Health Psychol. 2020;9(33):7–22. [Google Scholar]
- 77.Fadaiyan Arani, Amin Shokravi, Tavakoli Ghouchani. The Relationship between Health Literacy and Nutrition Behaviors in Patients with Type 2 Diabetes Mellitus. J North Khorasan Univ Med Sci. 2018;9(4):49–55. [Google Scholar]
- 78.Taghi Sohrabi, Nourafkan F, Fathimard F, Mazarei R. Relationship between Self-efficacy and Mental Health with Health Literacy in Patients with Diabetes in Kazerun City, Fars, Iran. J Community Health Res. 2020;9(4):256. [Google Scholar]
- 79.Noroozi M, Madmoli Y, Derikvand M, Saki M. Investigating health literacy level and its relation with some factors in patients with type 2 diabetes in Ahvaz-2018. J Health Lit. 2019;4(1):43–52. [Google Scholar]
- 80.Izadkhah F, Mohebi S, Rahbar A, Sharifirad G. Health literacy in type 2 diabetic women in Qom province in 2019. Jf Health Lit. 2020;5(1):50–60. [Google Scholar]
- 81.Saba Seif, Gholami M, Tarrahi MJ, Hossein Pour, Valiniaei S, Bazgir Z. The relationship between health literacy and perceived self-efficacy in cardiovascular patients hospitalized in Khorramabad educational hospitals. J Nurs Educ. 2018;7(3):14–21. [Google Scholar]
- 82.Marzangi A, Ahangarzadeh Rezaei, Ghareagaji Asl. Health literacy in heart disease community that covered by health services centers in south of west Azarbaijan province. Nurs Midwifery Res J. 2018;16(1):45–54. [Google Scholar]
- 83.Imanian M, Hosseini M, Torab TA, Shakeri N, Matbouei M. Relationship between health literacy and health-promoting behaviors in patients with heart failure referred to clinics of Shahid Beheshti University of Medical Sciences. An International Peer Reviewed Open Access Journal For Rapid Publication. 2017;10(1):116. [Google Scholar]
- 84.Qobadi M, Besharat MA, Rostami R, Rahiminezhad A, Pourgholami M. Health literacy, negative emotional status, and self-care behaviors in dialysis. J Fund Mental Health. 2015;17(1):46–51. [Google Scholar]
- 85.Yadollahi M, Siavashi E, Mostaghim S. The relationship between health literacy and patient participation in medical decision making among breast cancer patients. Arch Breast Cancer. 2018;5(4):183. [Google Scholar]
- 86.Roohi S, Salehi J, Mahmoodzadeh H, Morovati Z. Relationship of Social Support and Coping Strategies with Post-Traumatic Growth and Functional Disability Among Patients with Cancer: Meditating Role of Health Literacy. Iran Red Crescent Med J. 2020;22(3) [Google Scholar]
- 87.Sedghi S, Ashoori mhranani, Asadzandi S. Health literacy among Iranian MS patients. J Health Administ. 2019;22(1):78–90. [Google Scholar]
- 88.Kazemi M, Barkhordari-Sharifabad M, Nasiriani K, Fallahzadeh H. The Correlation of Health Literacy with Quality of Life in Asthmatic Patients. Iran J Nurs. 2019;32(121):54–67. [Google Scholar]
- 89.Mollakhalili H, Papi A, Zare-Farashbandi F, Sharifirad G, HasanZadeh A. A survey on health literacy of inpatient's educational hospitals of Isfahan University of Medical Sciences in 2012. J Educ Health Promot. 2014;11(4):464. doi: 10.4103/2277-9531.134804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Safari Morad, Agha Molaei, Ramezankhani A, Dadipoor S. The health literacy of pregnant women in Bandar Abbas, Iran. J Public Health Res. 2017;15(2):121. [Google Scholar]
- 91.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Viera A, Crotty K. et al. Health literacy interventions and outcomes: an updated systematic review. Evidence Report/Technology Assessment. 2011;199(199):1–941. [PMC free article] [PubMed] [Google Scholar]
- 92.Kun G, Xiaoye Z, Minhat HS, Jing O, Saliluddin SM, Malaysia P. The relevant factors of the limited health literacy among Chinese elderly adults: A systematic review. Eur J Mol Clin Med. 2020;7(6):2020. [Google Scholar]
- 93.Lee HY, Lee J, Kim NK. Gender Differences in Health Literacy Among Korean Adults: Do Women Have a Higher Level of Health Literacy Than Men. Am J Mens Health. 2015;9(5):370. doi: 10.1177/1557988314545485. [DOI] [PubMed] [Google Scholar]
- 94.Paasche‐Orlow MK, Parker RM, Gazmararian JA, Nielsen‐Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20(2):175. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rikard R, Thompson MS, McKinney J, Beauchamp A. Examining health literacy disparities in the United States: a third look at the National Assessment of Adult Literacy (NAAL) BMC Public Health. 2016;16(1):1–11. doi: 10.1186/s12889-016-3621-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ghanbari S, Majlessi F, Ghaffari M, Mahmoodi Majdabadi. Evaluation of health literacy of pregnant women in urban health centers of Shahid Beheshti Medical University. Daneshvar Medicine. 2012;19(6):1–12. [Google Scholar]
- 97.Stormacq C, Van den, Wosinski J. Does health literacy mediate the relationship between socioeconomic status and health disparities. Integrative review. Health Promot Int. 2019;34(5):e1–e17. doi: 10.1093/heapro/day062. [DOI] [PubMed] [Google Scholar]
- 98.Aljassim N, Ostini R. Health literacy in rural and urban populations: A systematic review. Patient Educ Couns. 2020;103(10):2142. doi: 10.1016/j.pec.2020.06.007. [DOI] [PubMed] [Google Scholar]
- 99.Shayakhmetov SS, Toguzbayeva KK, Ismailova AA, Tabibi R, Derbishalieva ZK, Dzhusupov KO. Health Literacy of Rural Population of Kazakhstan. Iran J Public Health. 2020;49(7):1269. doi: 10.18502/ijph.v49i7.3580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Charoghchian Khorasani, Tavakoly Sany, Orooji A, Ferns G, Peyman N. Health Literacy in Iranian Women: A Systematic Review and Meta-Analysis. Iran J Public Health. 2020;49(5):860. [PMC free article] [PubMed] [Google Scholar]
- 101.Xu XY, Leung AYM, Chau PH. Health literacy, self-efficacy, and associated factors among patients with diabetes. Health Lit Res Pract. 2018;2(2):e67–e77. doi: 10.3928/24748307-20180313-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lee SYD, Arozullah AM, Cho YI. Health literacy, social support, and health: a research agenda. Soc Sci Med. 2004;58(7):1309. doi: 10.1016/S0277-9536(03)00329-0. [DOI] [PubMed] [Google Scholar]


