Abstract
Background
Predicting the outcome of blunt chest trauma by scoring systems is of utmost value.
We aimed to assess the role of the chest trauma scoring system (CTS) in predicting blunt chest trauma outcomes among Egyptians.
Methods
A prospective observational study included 45 patients admitted to the cardiothoracic emergency unit of Al-Azhar University hospitals. We documented their demographic data, history, cause and mode of trauma, vital parameters, and necessary investigations (e.g., chest X-ray and Computed Tomography) when the patient was admitted to the cardiothoracic department. All patients were assessed using the chest trauma scale (CTS) and followed up till death or discharge.
Results
The patient's age ranged between 18 to 76 years (mean 42.67 years). Eighty percent were males, and 48% needed mechanical ventilation (MV). The period of MV was ranged from 1 to 5 days (mean 2.81 days). Twenty-two patients had pneumonia. Eight patients died with a chest trauma scale ranging from 2 to 12 with a median of 6. About 87 percent of patients had unilateral lesions, and 5 had criminal causes. Road traffic accidents were the most typical cause of trauma (60%). There was a significant relation between mortality among the studied patients and each MV, length of ICU duration, chest trauma scale, laterality of trauma, and associated injuries. There was a statistically significant relation between the chest trauma scale and the need for MV, the timing of MV, the presence of pneumonia, and mortality.
Conclusion
CTS ≥ 6.5 can predict mortality with 100.0% sensitivity, specificity of 62.2%, and accuracy of 68.9%. However, a score of ≥ 5.5 can predict the development of pneumonia with a sensitivity of 81.8%, specificity of 78.3%, and accuracy of 80%.
Keywords: Chest Trauma, Blunt, Severity, Mortality, Intensive Care
↑What is “already known” in this topic:
Blunt chest trauma is a common health problem with marked morbidity and mortality. The prediction of outcome is of utmost importance; it could guide the treatment process. Different scores are assessed, including the Chest Trauma Scoring (CTS) System. However, the results are heterogeneous, and no consensus was reached for the best score.
→What this article adds:
To the available literature, the current study confirmed the value of CTS in the prediction of morbidity and mortality. thus, it could be considered as one of the best scores to guide the management plan. This could decrease the associated morbidity and mortality and reduce the time to initiate the treatment plan.
Introduction
There are two types of thoracic trauma: blunt and penetrating. Automobile accidents are the leading cause of blunt chest trauma. Assaults, blast injuries, falls, and vehicles striking pedestrians were also examples of such reasons. Gunshots and stabbings account for the majority of penetrating trauma (1).
Although numerous studies have evaluated factors that predict thoracic trauma-induced morbidity and mortality, few have established scoring systems. Patients can be managed with greater ease using a prognostic scoring system. Implementing scores and protocol-based interventions resulted in better outcomes and shorter hospital stays (2).
A widespread system for predicting thoracic trauma outcomes is necessary to identify risk factors, predict outcomes, and determine whether immediate management or intensive care is required (3).
The existing scores for the prediction of thoracic trauma outcome include the Wagner score, Abbreviated Injury Scale chest (AIS), Lung Injury Scale, Pulmonary Contusion score (PCS), or Rib Score, Thoracic Trauma Severity Score (TTSS), modified early warning signs (MEWS) scoring system (4-6).
There is no widespread scoring system because of the complex application of some scores, the lack of significance for outcome prediction, or the limited resources. However, there are global recognizing age systems, and the presence of rib fractures, pulmonary contusions, and bilateral injury is identified as the most significant factors predicting the prognosis of chest trauma in studies evaluating the scoring systems (6-8).
These factors, either alone or in combination, may assist in predicting outcomes. The aforementioned predicting factors were developed by Pressley et al. (7) and validated by Chen et al. (9) to create the Chest Trauma Score (CTS). The current study aimed to determine whether CTS was a factor in poor outcomes for Egyptian patients.
Methods
This was an observational prospective study of 45 patients. The current study included all patients admitted to the Cardiothoracic surgery departments at Al-Azhar University Hospitals who presented with blunt chest trauma. After obtaining their informed and appropriate consent, they were recruited between April 2018 and March 2022. The Institutional Ethics and Research Committee (Damietta Faculty of Medicine, Al-Azhar University, Damietta, Egypt) approved the protocol. Patients or legal guardians provided written informed consent. Criteria for rejection were subjects under 18, and patients with significant chest-related injuries were excluded.
All patients had their CTS estimated. In addition to vital signs and necessary tests, such as a chest X-ray or CT, that were required when patients were admitted to the cardiothoracic unit, demographic information, history, the type of trauma, and the cause were all recorded. CTS was calculated according to Harde et al.2 (Table 1). The CTS has four distinct parts, each of which is assigned a point system: age (45 years = 1, 45–65 years =2, >65 years =3) pulmonary contusion (none equals 0; unilateral minor equals 1, bilateral minor equals 2, unilateral primary equals 3, and bilateral significant equals 4)number of rib fractures (3 =1, 3-5 =2, and greater than 5 =3)and a bilateral rib fracture is present =2. Chest X-ray and CT revealed several rib fractures and pulmonary contusions. The sum of the scores for each parameter was used to determine the final score, which was determined by assigning a specific score to each parameter. Then, the final CTS, which ranges from 2 to 12, was calculated.
Table 1. Calculation of chest trauma score (CTS).
| Variable | Level | Score |
|---|---|---|
| Age score | <45 y | 1 |
| 45-65 y | 2 | |
| >65 y | 3 | |
| Pulmonary contusion score | None | 0 |
| Unilateral minor | 1 | |
| Bilateral minor | 2 | |
| Unilateral major | 3 | |
| Bilateral major | 4 | |
| Rib score | <3 RIBFX | 1 |
| 3-5 RIBFX | 2 | |
| >5 RIBFX | 3 | |
| Bilateral RIBFX | No | 0 |
| Yes | 2 |
RIBFX: Rib fractures
Chest complications (specific pneumonia), the requirement for ventilator support, or death were the primary outcomes. Pneumonia was diagnosed using standard clinical and radiographic criteria, and the clinician decided to start ventilator support. Hospital protocols for treating chest trauma were unaffected by this study.
SPSS version 20 (Statistical Package for the Social Sciences) was used for data analysis. Means and standard deviations were used to describe quantitative variables. The Chi-square test was used to compare categorical variables, and their absolute frequencies were used to describe them. The distribution-type Kolmogorov-Smirnov and homogeneity of variances Levene tests were used to validate assumptions for parametric tests. When the data were not normally distributed, the Mann-Whitney test was used to compare the means of the two groups. For normally distributed data, the independent sample t-test was used. The best cutoff of the studied parameters for diagnosing specific health issues was determined using the ROC curve. A p value lower than 0.05 was set as the level of statistical significance.
Results
The age of the studied patients ranged from 18 to 76 years, with a mean age of 42.67 ± 15.52 years. Eighty percent (36 subjects) of them were males. 21 (46.7%) underwent mechanical ventilation. Out of them, twelve patients (57.1%) needed early mechanical ventilation. The period of MV was ranged from 1 to 5 days, with a mean of 2.81 ± 1.33 days. Twenty-two patients (48.9%) had pneumonia. Eight patients (17.8%) had died by the end of the study. Chest trauma scale ranged from 2 to 12 with a median of 6. Twenty-six (57.8%) studied patients had been admitted to ICU for 1 to 10 days, with a mean of 4.19 ± 2.3 days. 39 patients (86.7%) had a unilateral lesion, and 11.1% (5 patients) had the criminal trauma mode. Road traffic accidents (RTA) were the most common cause of trauma, accounting for 60% (27 patients). Of these, 15.6% (n=7) were pedestrians, 24.4% (n=11) were drivers of motor vehicles, and 20% (n=9) were motorcyclists. Falls accounted for 22.2% (n=10) , and 11.1% (n=5) were due to assaults. Other causes included sports injuries (6.7%; n=3) (Table 2).
Table 2. Distribution of the studied patients according to patient characteristics and outcome.
| Variable | Measure | Value | |
|---|---|---|---|
| Age (years) | Mean ± SD; Min. – Max. | 42.67±15.52;
18.0-76.0 |
|
| Gender (n, %) | Male | 36 (80.0%) | |
| Female | 9(20.0%) | ||
| Cause of trauma (n, %) | Road traffic accident | Total | 27 (60.0%) |
| Pedestrians, drivers, motorcyclists | 7, 11,
9 |
||
| Falls | 10 (22.2%) | ||
| Assaults | 5 (11.1%) | ||
| Sport-related injury | 3 (6.7%) | ||
| Laterality of trauma | Unilateral | 39 (86.7%) | |
| Bilateral | 6 (13.3%) | ||
| Mode of trauma | Accidental | 40 (88.9%) | |
| Criminal | 5 (11.1%) | ||
| Presence of an associated injury | 7 (15.6%) | ||
| Mechanical ventilation | (n, %) | 21 (46.7%) | |
| Timing of MV (for 21 cases) (n, %) | Early | 12 (57.1%) | |
| Late | 9 (42.9%) | ||
| Duration of MV | Mean ± SD; Min. – Max. | 2.81±1.33;
1.0 – 5.0 |
|
| ICU stay duration | Mean ± SD; Min. – Max. | 4.19±2.3;
1.0 – 10.0 |
|
| Chest trauma score | Mean ± SD; median; Min. – Max. | 6.44±3.05;
6;
2.0- 12.0 |
|
| Pneumonia | (n, %) | 22 (48.9%) | |
| Mortality | (n, %) | 8 (17.8%) | |
Min: minimum, Max: Maximum, SD: standard deviation; MV: Mechanical Ventilation; ICU: Intensive Care unit.
There was a significant difference between the occurrence of mortality among the studied patients regarding mechanical ventilation (all patients who died underwent MV), length of ICU duration (patients who died stayed less in ICU), and chest trauma scale (higher in patients in patients who died by the end). There is a non-significant difference between the studied groups regarding gender, age, timing, period of ventilation, or mortality. There is a statistically significant association between mortality and the laterality of trauma (higher mortality in bilateral lesions) and associated injuries (high mortality in patients with associated injuries. There is a non-significant association between mortality and either the mode or mechanism of trauma. Traffic road accidents represented the highest mechanism of the lesion with a higher occurrence of mortality (62.5%) out of dead patients had traffic road accidents, two pedestrians, two motorcar drivers, and one motorcyclist (Table 3). There is a statistically significant relationship between the chest trauma scale and the need for mechanical ventilation, the timing of mechanical ventilation, the presence of pneumonia, and mortality (Table 4).
Table 3. Factors associated with mortality among the studied patients.
| Variables | Mortality | Statistical analysis | |||
|---|---|---|---|---|---|
| No (n=37) | Yes (n=8) | Test | P | ||
| Sex (n, %) | Male | 30(81.1%) | 6 (75.0%) | FE | 0.651 |
| Female | 7(18.9%) | 2 (25.0%) | |||
| Age | Mean ± SD | 42.54±14.9 | 43.25±19.31 | 0.12 | 0.910 |
| Cause of trauma | RTA | 22 (59.5%) | 5 (62.5%) | 2.762 | 0.430 |
| Falls | 9 (24.3%) | 1 (12.5%) | |||
| Assaults | 3 (8.1%) | 2 (25.0%) | |||
| Sport-related injury | 3 (8.1%) | 0 (0.0%) | |||
| Laterality | Unilateral | 37 (100.0%) | 2 (25.0%) | FE | <0.001* |
| Bilateral | 0 (0.0%) | 6 (75.0%) | |||
| Mode of trauma | Accidental | 34 (91.9%) | 6 (75.0%) | FE | 0.211 |
| Criminal | 3 (8.1%) | 2 (25.0%) | |||
| Presence of an associated injury | 1 (2.7%) | 6 (75.0%) | FE | <0.001* | |
| Mechanical ventilation (n, %) | 13 (35.1%) | 8 (100.0%) | FE | <0.001* | |
| Timing of MV | Early | 5(38.5%) | 7(58.5%) | FE | 0.067 |
| Late | 8(61.5%) | 1 (12.5%) | |||
| Duration of MV (day) | Mean ± SD | 3.0 ± 1.08 | 2.5 ± 1.69 | 1.039 | 0.299 |
| ICU stay duration (day) | Mean±SD | 4.94 ± 2.12 | 2.5 ± 1.69 | 2.645 | 0.008* |
| Chest trauma score | Mean±SD | 5.51 ± 2.5 | 10.75 ± 0.71 | 1.88 | <0.001* |
| Pneumonia | 19 (51.4%) | 3 (37.5%) | FE | 0.669 | |
FE: Fisher Exact test, MV: Mechanical Ventilation; * indicates significant differences; ICU: Intensive care unit.
Table 4. Relation between chest trauma scale and other variables.
| Variables | Chest trauma scale | t | P | |
|---|---|---|---|---|
| Mean ± SD | ||||
| Gender | Male | 6.56 ± 2.84 | 0.485 | 0.630 |
| Female | 6.0 ± 3.94 | |||
| MV | No | 4.0 ±1.25 | 11.12 | <0.001* |
| Yes | 9.24 ± 1.81 | |||
| Timing of MV | Early | 10.42 ± 1.31 | 5.24 | <0.001* |
| Late | 7.67 ± 1.0 | |||
| Pneumonia | No | 5.17 ± 3.23 | 3.131 | 0.003* |
| Yes | 7.77 ± 2.22 | |||
| Mortality | No | 5.51 ± 2.5 | 10.88 | <0.001* |
| Yes | 10.75 ± 0.71 | |||
MV: Mechanical ventilation; * indicates statistical differences.
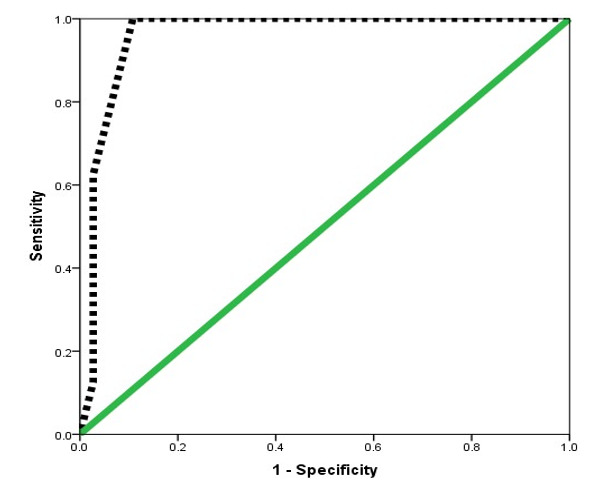
The best cutoff of chest trauma scale in the prediction of development of pneumonia among the studied patients≥5.5 with are under curve 0.776, sensitivity 81.8%, specificity 78.3%, positive predictive value 78.3%, negative predictive value 81.8%, positive likelihood ratio 3.78, negative likelihood ratio 0.23, accuracy 80% (p<0.05) (Table 5, Figure 1). The best cutoff of chest trauma scale in the prediction of mortality among the studied patients≥6.5 with are under curve 0.959, sensitivity 100%, specificity 62.2%, positive predictive value 36.4%, negative predictive value 100%, positive likelihood ratio 2.65, negative likelihood ratio 0, accuracy 68.9% (p<0.05) (Table 5, Figure 2).
Table 5. Performance of chest trauma scale in prediction of pneumonia and mortality among the studied patients.
| Cutoff | AUC | Sensitivity | Specificity | PPV | NPV | +LR | -LR | Accuracy | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| Pneumonia | ≥ 5.5 | 0.776 | 81.8 | 78.3 | 78.3 | 81.8 | 3.78 | 0.23 | 80.0 | 0.002* |
| Mortality | ≥ 6.5 | 0.959 | 100 | 62.2 | 36.4 | 100 | 2.65 | 0 | 68.9 | <0.001** |
Figure 1.
ROC curve showing performance of chest trauma scale in prediction of pneumonia development.

Figure 2.
ROC curve showing performance of chest trauma scale in prediction of mortality.
Discussion
For accurate management, expected outcome, complications, and establishing a clear prognosis for patients and their loved ones, prompt and precise evaluation of the severity of thoracic trauma is essential. Sorting, triage, and the implementation of treatment protocols can be completed quickly if the severity of the chest trauma is consistently assessed (2).
There are different scales for assessing chest trauma, including the Wagner score, Abbreviated Injury Scale chest (AIS), Lung Injury Scale, Pulmonary Contusion score (PCS), Rib Score, Thoracic Trauma Severity Score (TTSS), and modified early warning signs (MEWS) scoring system (5, 9, 10).
Chen et al. (9) declared that this score could predict poor outcomes (e.g., complications and mortality) in thoracic trauma if CTS ≥5. This score was not examined on Egyptian patients according to the best of researchers' knowledge at starting this work. In addition, few studies evaluate CTS in the prediction of patient outcomes. The current study reported a significant relationship between the chest trauma scale and the need for mechanical ventilation, pneumonia occurrence, MV timing, and patient outcome. Patients with pneumonia who died by the end needed MV (especially early MV) and had significantly higher CTS). This denoted that achieving higher scores is associated with poor outcomes regarding the patients and an increasing burden on health resources. In the next step, CTS was examined as a predictor for poor outcomes, including pneumonia and mortality. At cutoff ≥5.5, the scale can point to the possibility of pneumonia with a sensitivity of 81.8%, specificity of 78.3%, and accuracy of 80%. At cutoff ≥ 6.5, mortality can be predicted with sensitivity 100%m specificity of 62.2% and 68.9% accuracy in a previous Indian study by Harde et al. (2), who studied 30 patients. They divided their patients according to CTS into both groups (Low CTS <5 and High CTS ≥ 5). Higher CTS was significantly associated with a high incidence of pneumonia, need for MV, and mortality in chest trauma. All of their findings agreed with the current study. They denoted that CTS ≥5.5 can predict mortality with a sensitivity of 87.5% and a specificity of 68%. Pressley et al. (7) and Chen et al. (9) revealed that increasing CTS scores have a more significant association with mortality in harmony with the current study.
A previous study by Veysi et al. (11) noted that RTA was the most common cause of injury overall, affecting 57.01% of patients, of which 19.4% were pedestrians.
RTA is considered one of Egypt's leading causes of trauma-related morbidity and mortality. Additionally, this is observed globally, with varying incidence rates attributed to the implementation of traffic laws and safety measures to reduce this high rate.
Khursheed et al. (12) found that road traffic accidents are the most common cause of chest injuries, accounting for more than half of all chest injuries (56.17 percent). Additionally, pedestrians were more likely to sustain blunt chest injuries than passengers, which is in line with our findings. It has been observed that the mechanism of chest injuries varies not only between nations but also within a nation. According to Liman et al. (13), motor vehicle accidents were the cause of 67.79 percent of chest trauma cases (n=1490). Other studies reported similar figures (14, 15).
According to an analysis of mortality, the overall mortality rate following blunt trauma was 20.84 percent, with a mortality rate of 13.7% (12).
Veysi et al. (11) reported an overall mortality rate of 18.7% for blunt chest trauma, while Lema et al. (14) found a mortality rate of 4.7 percent. In addition, a second study found that 20% of participants suffered blunt chest trauma due to RTA (16).
In Tsai et al. (17), patients with multiple traumas and associated blunt thoracic injuries had a mortality rate of 50%. In another study, 30%–75% of pulmonary contusions were attributed to vehicular motor accidents. The presence of associated extra-thoracic organ injury, which was noted in 25.5%, delayed presentation (>24 hours), and severe injury of the chest as defined by bilateral involvement positively correlated with mortality (6).
Conclusion
In conclusion, CTS is a simple, rapid scale that can help triage and treat patients. At scores≥ 5.5 and ≥6.5, it can significantly predict the possibility of pneumonia and mortality, respectively. Road traffic accidents represented the most common cause of blunt trauma to the chest and the leading cause of mortality. The existence of associated extra-thoracic lesions and bilateral chest lesions was associated with higher mortality. Good triage is needed to highlight such risk factors to improve patient outcomes.
The present study can be explained in the context of some limitations, including small sample size and being applied in a single study. Further prospective large-scale multi-centric studies should be used to verify the role of CTS in predicting poor outcomes among chest trauma.
Ethical approval
DFM-IRB 00012367-18-03-005.
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as : Hussein MHE, Mahmoud IF, Eita YMS, Aglan MAA, Esmaiel MSA, Farag GAI, Abdelmottaleb NA, Elkahely M, Mansour MA. A Prospective Study of Chest Trauma Scoring System as A Morbidity and Mortality Predictor in Patients with Blunt Chest Trauma. Med J Islam Repub Iran. 2024 (16 Jan);38:4. https://doi.org/10.47176/mjiri.38.4
References
- 1.Jones KA, Sadri S, Ahmad N, Weintraub JR, Reis SP. Thoracic Trauma, Nonaortic Injuries. Semin Intervent Radiol. 2021 Mar;38(1):75–83. doi: 10.1055/s-0041-1726005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harde M, Aditya G, Dave S. Prediction of outcomes in chest trauma patients using chest trauma scoring system: A prospective observational study. Indian J Anaesth. 2019;63(3):194–199. doi: 10.4103/ija.IJA_750_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valderrama-Molina CO, Giraldo N, Constain A, Puerta A, Restrepo C, León A. et al. Validation of trauma scales: ISS, NISS, RTS and TRISS for predicting mortality in a Colombian population. Eur J Orthop Surg Traumatol. 2017 Feb;27(2):213–220. doi: 10.1007/s00590-016-1892-6. [DOI] [PubMed] [Google Scholar]
- 4.Gupta AK, Ansari A, Gupta N, Agrawal H, B M, Bansal LK, Durga C. Evaluation of risk factors for prognosticating blunt trauma chest. Pol Przegl Chir. 2021 Jul 19;94(1):12–19. doi: 10.5604/01.3001.0015.0427. [DOI] [PubMed] [Google Scholar]
- 5.Chapman BC, Herbert B, Rodil M, Salotto J, Stovall RT, Biffl W. et al. RibScore: A novel radiographic score based on fracture pattern that predicts pneumonia, respiratory failure, and tracheostomy. J Trauma Acute Care Surg. 2016 Jan;80(1):95–101. doi: 10.1097/TA.0000000000000867. [DOI] [PubMed] [Google Scholar]
- 6.Ekpe EE, Eyo C. Determinants of mortality in chest trauma patients. Niger J Surg. 2014;20(1):30. doi: 10.4103/1117-6806.127107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pressley CM, Fry WR, Philp AS, Berry SD, Smith RS. Predicting outcome of patients with chest wall injury. Am J Surg. 2012;204(6):910. doi: 10.1016/j.amjsurg.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 8.Omar A, Winkelmann M, Liodakis E, Clausen JD, Graulich T, Omar M. et al. Applicability of Anatomic and Physiologic Scoring Systems for the Prediction of Outcome in Polytraumatized Patients with Blunt Aortic Injuries. Diagnostics (Basel) 2021;11(11):2156. doi: 10.3390/diagnostics11112156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen J, Jeremitsky E, Philp F, Fry W, Smith RS. A chest trauma scoring system to predict outcomes. Surgery. 2014;156(4):988. doi: 10.1016/j.surg.2014.06.045. [DOI] [PubMed] [Google Scholar]
- 10.Hildebrand F, Griensven MV, Garapati R, Krettek C, Pape HC. Diagnostics and scoring in blunt chest trauma. Eur J Trauma. 2002;28(3):157–167. doi: 10.1007/s00068-002-1192-1. [DOI] [Google Scholar]
- 11.Veysi VT, Nikolaou VS, Paliobeis C, Efstathopoulos N, Giannoudis PV. Prevalence of chest trauma, associated injuries and mortality: A level I trauma centre experience. Int Orthop. 2009;33:1425. doi: 10.1007/s00264-009-0746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khursheed SQ, Ashraf W, Rather AA, Bari SU. Clinical profile and outcome of chest trauma-A four-year retrospective analysis at a tertiary care centre. Int Surg J. 2019;6(7):2519. [Google Scholar]
- 13.Liman ST, Kuzucu A, Tastepe AI, Ulasan GN, Topcu S. Chest injury due to blunt trauma. Eur J Cardiothorac Surg. 2003;23(3):374. doi: 10.1016/s1010-7940(02)00813-8. [DOI] [PubMed] [Google Scholar]
- 14.Lema MK, Chalya PL, Mabula JB, Mahalu W. Pattern and outcome of chest injuries at Bugando Medical Centre in Northwestern Tanzania. J Cardiothorac Surg. 2011;6:7. doi: 10.1186/1749-8090-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dehgan N, de Mestral, McKee MD, Schemitsch EH, Nathens A. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76(2):462. doi: 10.1097/TA.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 16.El-Menyar A, Latifi R, AbdulRahman H, Zarour A, Tuma M, Parchani A. et al. Age and traumatic chest injury: a 3-year observational study. Eur J Trauma Emerg Surg. 2013;39(4):397–403. doi: 10.1007/s00068-013-0281-7. [DOI] [PubMed] [Google Scholar]
- 17.Tsai YU, Lin KH, Huang TW, Chen CY, Hong ZJ, Hsu SD. Outcomes of patients with blunt chest trauma encountered at emergency department and possible risk factors affecting mortality. J Med Sci. 2017;37(3):97–101. [Google Scholar]


