Abstract
Background
This mini review aims to provide an overview of the role of telemedicine in preventing multi-drug resistant tuberculosis (MDR-TB) in Nigeria. The specific objectives include examining the potential benefits of telemedicine, identifying the challenges associated with its implementation, and highlighting the importance of addressing infrastructure limitations and data privacy concerns.
Methods
This minireview is based on a comprehensive analysis of existing literature, including scholarly articles, and reports,. A systematic search was conducted using electronic databases, such as PubMed and Google Scholar, to identify relevant publications related to telemedicine and MDR-TB prevention in Nigeria. The selected articles were assessed for their relevance, and key findings were synthesized to provide an overview of the role of telemedicine in addressing the challenges of MDR-TB in Nigeria.
Results
The review demonstrates that telemedicine has the potential to significantly contribute to MDR-TB prevention efforts in Nigeria. The benefits of telemedicine include improved access to specialized care, enhanced patient adherence to treatment, and potential cost savings. However, challenges such as infrastructure limitations and data privacy concerns need to be addressed for successful implementation. Integrating telemedicine into the healthcare system has the potential to strengthen MDR-TB prevention, particularly in underserved areas, including within Nigeria. Specifically, the integration of telemedicine into the healthcare system can enhance access to specialized care, improve patient adherence, and potentially reduce costs associated with MDR-TB management.
Conclusions
Addressing infrastructure challenges, ensuring data privacy and security, and fostering trust among healthcare providers and patients are critical for successful implementation of telemedicine. Further research and policy frameworks are needed to guide the effective implementation and scale-up of telemedicine in MDR-TB prevention efforts in Nigeria.
Keywords: Telemedicine, Tuberculosis, Multi-drug resistance tuberculosis, Nigeria, Healthcare
1. Introduction
Tuberculosis (TB) remains a significant public health challenge in Nigeria, with a high burden of both drug-susceptible TB and drug-resistant TB [1]. Nigeria is the country with the highest tuberculosis burden in Africa and the sixth highest in the world [2], [3]. In 2020, an estimated 108,000 people in Nigeria developed tuberculosis, and 23,000 died from the disease [4]. The emergence of drug-resistant tuberculosis (DR-TB) strains, including multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB), poses a growing threat. The prevalence of drug-resistant tuberculosis (DR-TB) in Nigeria is high, with an estimated 32 % of newly diagnosed cases and 53 % of previously treated cases being resistant to at least one anti-TB medication [5], [6]. MDR-TB is the most common form of DRTB, and it occurs in an estimated 6 % of newly diagnosed cases and 32 % of previously treated cases in Nigeria [4], [5]. This form of TB is difficult and costly to treat, increasing the economic and health burden in Nigeria [7], [8].
Despite progress in recent years, several key factors contribute to this ongoing challenge. The high incidence is primarily due to factors such as overcrowding, poverty, and inadequate healthcare infrastructure [9]. Access to TB diagnosis and treatment services remains limited in many regions of Nigeria, particularly in rural areas [10]. This lack of access exacerbates the spread of the disease and delays diagnosis and treatment initiation [7], [10]. Poverty, malnutrition, and inadequate living conditions contribute to the persistence of TB in Nigeria. These factors make individuals more vulnerable to infection and hinder adherence to treatment regimens [7]. Nigeria's healthcare infrastructure faces challenges such as a shortage of healthcare workers, insufficient diagnostic facilities, and inconsistent drug supply chains, further hampering efforts to combat TB.
The development of Information Communication Technology (ICT) has become an important factor in the socio-economic and educational development of many countries [11], [12], [13]. The number of healthcare practitioners serving over 200 million Nigerians has been reducing drastically over the years as a result of the exodus of doctors and nurses seeking alternate opportunities outside the country [14], [15]. Most of the available ones are situated in major cities, and the remaining few are arbitrarily and distributed elsewhere, often with inadequate infrastructure to work with [15]. Mobile phones could offer the opportunity to provide healthcare to populations across the country through telemedicine, with the potential to improve healthcare delivery in Nigeria.
A large portion of Nigeria's about 200 million inhabitants resides in rural regions with little or no access to urban healthcare infrastructure, in part due to difficulty with financial and logistical access to convenient transportation to these areas [14], [16], [17]. Over the years, healthcare in these far-flung rural areas has become a priority for federal, state, and local governments to ensure that people living in both urban and rural areas have equal access to medical services and clinical healthcare regardless of where they live, however, this effort has been met with mixed success [18], [19]. A healthcare system that could enable providers to access patients across space, such as telemedicine could enable providers to access patients in distant locales to achieve the national goal of universal healthcare coverage [20]. This would enable healthcare providers to deliver diagnostic, treatment and counselling services to patients remotely, thereby enhancing the quality, timeliness, and cost-effectiveness of healthcare services in rural and outlying regions.
Despite efforts to combat TB in Nigeria, the emergence of MDR-TB continues to threaten the population. To address this critical issue, it is imperative to explore innovative approaches, such as telemedicine, which has the potential to improve access to specialized care, enhance patient adherence, and reduce costs associated with TB management. This review seeks to evaluate the potential advantages of telemedicine in the context of TB prevention, particularly in addressing the challenges of MDR-TB in Nigeria. It assesses how telemedicine can improve access to specialized care, enhance patient adherence to treatment regimens, and potentially reduce healthcare costs associated with MDR-TB management. By reviewing the literature, we aim to provide valuable insights into the feasibility and potential impact of telemedicine in combating MDR-TB in Nigeria and similar resource-limited settings. This review seeks to contribute to the development of evidence-based policies and frameworks for the effective implementation and scale-up of telemedicine as a valuable tool in the fight against drug-resistant TB in Nigeria and beyond.
2. Methods
This minireview synthesizes existing literature on the role of telemedicine in preventing multi-drug resistant tuberculosis (MDR-TB) in Nigeria. A systematic search was conducted using the electronic databases PubMed and Google Scholar to identify relevant publications related to telemedicine and MDR-TB prevention in Nigeria. Search terms included keywords such as “telemedicine,” “tuberculosis,” “multi-drug resistant tuberculosis,” “Nigeria,” “digital health” and so on. The search was conducted with a focus on peer-reviewed scholarly articles, and reports. Identified publications were screened based on predefined inclusion and exclusion criteria. To ensure relevance and reliability, predefined inclusion criteria were adhered to, emphasizing articles that distinctly addressed telemedicine's involvement in MDR-TB prevention in Nigeria. Conversely, exclusion criteria filtered out non-peer-reviewed publications, those focusing solely on general tuberculosis management without telemedicine context, and articles lacking a specific focus on Nigeria or MDR-TB prevention through telemedicine. The selection process prioritized credible, English-language sources to gather comprehensive insights into the subject matter.
2.1. What is Telemedicine?
Telemedicine, often known as telehealth or e-medicine, is the use of communications technology (textual, audio, and video) to offer healthcare services, such as consultations and laboratory studies, across long distances [21], [22], [23]. Advanced telecoms and information technologies have been the focus of investigation by doctors, health services academics, and others for over 30 years [24]. Telemedicine, which combines cutting-edge and established technologies, is at the centre of many of these initiatives. In this context, “telemedicine” refers to the practice of using information and communication tools online to facilitate medical treatment between geographically separated individuals. Patient treatment, teaching, research, management, and even public health are just a few of the areas where telemedicine can be useful [21].
There is a history of using telehealth for video-based direct observed therapy (v iDOT) for patients with active TB disease [25], even if this adoption of telehealth is still in its infancy and actively evolving based on the needs of patients and health system resources. VDOT is a practical and affordable substitute for daily in-person monitoring, which was particularly helpful during the COVID-19 pandemic [25], [26].
Telemedicine enables healthcare practitioners to examine, diagnose, and treat patients without the requirement for a face-to-face encounter with the patients [21], [27], [28]. The patient could download a telemedicine electronic application (app) like VIDOT or call a telemedicine number supplied by their primary care physician's office or their employer as part of their health insurance to have a telemedicine assessment from home [22]. The integration of home devices, particularly smartphones, into medical practices has revolutionized patient care and healthcare communication. These devices offer a unique advantage by enabling physicians to remotely monitor telemetry patients while concurrently managing other tasks. This might include reviewing medical records, responding to urgent messages or calls, consulting with colleagues, updating patient charts, accessing reference materials, or attending to administrative tasks [28]. The ability to multitask effectively using smartphones ensures that healthcare professionals can optimize their time and resources while maintaining a consistent level of patient care and responsiveness. Notably, these devices serve as a conduit for real-time interactions, allowing healthcare professionals to promptly address concerns or emergencies.
Furthermore, their utility in reducing liability is significant, primarily by providing a clear and instantaneous visualization of medical orders and test results. This eradicates potential errors associated with illegible handwriting or misunderstandings arising from verbal instructions. Misunderstandings due to language barriers, distractions, or misinterpretations may occur, potentially leading to medical errors [29]. The adoption of such technology not only enhances patient care but also streamlines the healthcare process, ensuring a more efficient and error-free system [28], [29]. Additionally, having a digital record of instructions can serve as a reference point for both patients and healthcare providers, ensuring adherence to prescribed protocols and treatments while minimizing potential miscommunication-related risks.
2.2. Challenges of telemedicine
There are still many impediments to the use of therapeutic telemedicine by most people. For instance, despite the efforts of many organizations to establish hardware and software standards, it is still difficult to assemble systems in which all of the parts function reliably and smoothly together, adapt well to new environments, and can be easily replaced if necessary [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32]. The complexities inherent in the healthcare system, encompassing the diverse needs and dynamics of doctors, patients, and decision-makers, have not been fully integrated into the design of technical systems dedicated to healthcare [33], [34]. This lack of integration means that the architecture of these technical systems might not align effectively with the actual work settings and preferences of healthcare professionals, patients, and key decision-makers. Additionally, current applications (Apps) used in healthcare often overlook the significance of incorporating organizational business goals and strategic plans essential for the successful implementation of telemedicine programs [33]. This oversight can result in a mismatch between the intended objectives of telemedicine initiatives and the broader organizational strategies, potentially hindering the seamless integration and long-term success of these programs within healthcare institutions.
In the current landscape of healthcare, tensions and rivalries emerge among various stakeholders due to the perception of telemedicine as an economic threat amid intensified competition, system reconfigurations, and an oversupply of certain healthcare professionals [35]. Clinicians, in particular, may view telemedicine as a disruptor that challenges traditional healthcare delivery models and potentially alters the balance of competitiveness among healthcare providers. Healthcare institutions and organizations are also significant stakeholders, with concerns centered around resource allocation, revenue streams, and operational changes influenced by the integration of telemedicine systems [36]. Additionally, patients and advocacy groups play a vital role, as some patients embrace the convenience of remote healthcare services while others express concerns about the quality of care and the loss of personal interaction with healthcare providers [36]. Regulatory bodies and government agencies are actively involved, grappling with jurisdictional complexities, data privacy, licensure, and quality standards in telehealth services. Furthermore, technology developers and telecommunication companies are deeply invested stakeholders, striving for market competitiveness, technological advancements, and compliance with evolving healthcare regulations [35].
2.3. Benefits of telemedicine
Telemedicine is adaptable to patients living with Tuberculosis who need to follow strict protocols for taking their medications, ensuring that direct observation is achieved [37]. This type of care has the potential to reduce costs. It also has the potential to reduce risk of spread of disease that may occur when patients are transported to health care facilities [37], [38]. Additionally, telemedicine can help ensure healthcare access to care for elderly patients with impaired mobility who may have difficulty making their way to a medical facility. [39]. The use of telemedicine also has the potential to help patients become more involved in their healthcare plans and increase their autonomy [40], [41], [42], [43]. A Web-based solution for care coordination can integrate information from biometric measures and diagnostic tests and automatically alert clinicians of panic values [41], [44]. For instance, in the case of adverse events to TB medications, such as jaundice, visual and renal impairment, psychosis, or peripheral neuropathy, an appropriate ICT App like ViDot, using its video component, can be used to alert the managing physician on what instructions to give the patients [22], [45]. The fear of these side effects may make some patients stop medications halfway which is a major risk to the emergency of multi-drug resistant TB [21], [46].
2.4. Role of telemedicine in preventing multi-drug-resistant TB
Telemedicine, one of the digital health innovations and interventions, has the potential to strengthen each of the WHO’s three pillars of the End TB Strategy. These pillars include ensuring integrated, patient-centered care and prevention; bold policies and supportive systems; and intensified research and innovation. Also, telemedicine can significantly contribute to achieving the research pillar outlined by the World Health Organization (WHO) by facilitating improved access to healthcare, enhancing patient care, and supporting research initiatives [53]. Implementing telemedicine in MDR-TB care aligns with WHO's research pillar by fostering innovation, improving healthcare delivery, and promoting research collaborations [50]. It facilitates the generation of real-time data, promotes evidence-based practices, and supports ongoing research efforts to refine treatment strategies and control the spread of drug-resistant TB.
The various pillars are described in a digital health strategy agenda that the WHO has produced [53]. The use of cutting-edge technology through telemedicine can offer several potential applications such as video-observed therapy to enable a more patient-centered approach, applications for adherence support, remote patient consultations, and remote technical assistance, including consensus expert opinions for complex cases. [50], [53]. Through the administration of pharmaceuticals by qualified health department staff, directly observed therapy (DOT) ensures patient adherence [54]. This strategy has been widely used in the treatment of tuberculosis. Unfortunately, DOT programmes necessitate a significant investment of time and money from the limited public health budget [54]. The use of telemedicine in DOT is expected to result in significant time and cost savings [53].
The difficulties that TB patients encounter in finishing their treatment have been the subject of numerous research projects [48], [49], [50]. Language barriers, the severity of isoniazid and rifampin side effects, and transportation have all been mentioned in previous studies as obstacles to completing treatment [50], [55]. Treatment time has also been identified as a factor linked with treatment completion. Studies have revealed that a 4-month daily rifampin regimen (4R) for treatment of latent Tuberculosiswas more likely to result in treatment completion than a 9-month isoniazid regimen (9H) [50], [56], [57]. Missed appointments can result in incomplete and ineffective therapy, occasionally leading to the emergence of multi-drug resistant strains of TB.
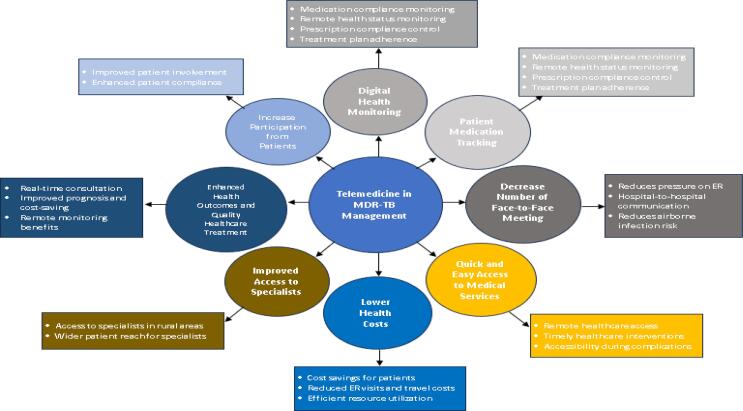
The management of patients with MDR-TB can benefit from the application of telemedicine in a variety of settings, including teleconsultation, medical response, tele-expertise, tele-monitoring, and tele-assistance. With increasing evidence and altering standards of treatment in MDR-TB predicted over the future decade, telemedicine will be an essential intervention in optimizing patient care and building local capacity and clinical partnerships in the management of MDR-TB in low-resourced settings [59]. Telemedicine has several potential roles in preventing MDR-TB (Fig. 1):
-
1.
Digital Health Monitoring.
Fig. 1.
Highlights of Roles of Telemedicine in Preventing MDR-TB. *ER- Emergency Room (Emergency Health Service).
More precise diagnoses and treatment options could be offered by telemedicine systems with digital health monitoring capabilities when paired with artificial intelligence and machine learning for MDR-TB patients [53], [58]. Through the use of networking technology, telemedicine allows healthcare providers in one region to treat patients in another. Applications for appointment scheduling, chart review, video conferences and photo transcripts provide an alternative to in-person meetings. It enables the safe expansion of medical services to regions without easy access to healthcare and the protection of medical professionals and patients.
-
2.
Patient Medication Tracking.
In the continuation phase of TB treatment which ranges from 4 months to up to 18 months in cases of the TB of the spine, patients will take their medications home to be taken daily and must return monthly for a refill. It is not always practical that all these patients would take the medications daily as prescribed [50]. The use of telemedicine will help to remind them and monitor the use via video directly observed therapy [54], [58]. The adverse effects of these medications could also be monitored for adherence to be achieved. Telemedicine use for patient medication tracking could also help in monitoring the use of other medications for common TB co-morbidities such as HIV and Hepatitis B, which can also constitute a barrier to treatment response [53], [60]. Telemedicine may be useful since elderly people are more prone to stop taking their medications as prescribed [61].
-
3.
Patient Health Tracking.
With cutting-edge medical technology, the healthcare provider may also now monitor their patients’ health status from great distances [29]. By sending data from one system to another, this technology provides information such as pulse rhythm, blood pressure, glucose levels, and more. E-Prescribing technologies, which enable quick and precise monitoring of prescription compliance, are used in telemedicine [61]. In practical terms, this gives doctors more control over their patients' pharmaceutical regimens and progress monitoring.
-
4.
Decrease the number of face-to-face meetings.
Telemedicine allows for appointments and monitoring, which reduces pressure on emergency rooms and improves treatment for those in dire need [24], [27], [28]. With the use of telemedicine, Providers may communicate medical information to provide treatment more swiftly. It also helps lower overall health risks by treating individuals who require close monitoring [21]. Tuberculosis is an air-borne infection. Its spread in the hospital environment can be reduced by the use of telemedicine to prevent unnecessary hospitalizations and subsequent contact with other patients.
-
5.
Quick and easy access to medical services.
Telemedicine was developed to address issues like a lack of doctors and hospitals mostly in areas where there is a relatively lower number of healthcare providers thereby allowing for the remote delivery of medical treatment [16], [17], [40]. Remote patient monitoring technologies have allowed healthcare providers at larger hospitals to assist smaller, rural institutions in providing critical healthcare services [21]. Therefore, MDR-TB patients when confronted with an issue or complications could quickly access a healthcare provider when this otherwise may not be feasible.
-
6.
Lower Health Cost.
Numerous stakeholders within the healthcare system stand to gain significant advantages from the cost-effectiveness and efficiency facilitated by telemedicine. Patients, doctors, health insurance providers, and employers all stand to benefit from its implementation. Patients, for instance, can experience financial savings by reducing transportation expenses and doctor's fees through the utilization of telemedicine. Instead of making unnecessary visits to emergency rooms or undertaking physical consultations to rule out relatively common conditions like a cold or the flu, patients can opt for remote consultations via telemedicine [21]. This approach not only saves patients the expenses associated with travel and consultation fees but also offers convenience and flexibility in accessing healthcare services from the comfort of their homes. Additionally, by leveraging telemedicine, healthcare providers can focus on more critical cases that require in-person attention, thereby optimizing their resources and providing more efficient care to patients in need [28]. Health insurance providers and employers also stand to benefit from reduced healthcare costs and improved productivity among employees by encouraging the use of telemedicine, thereby potentially decreasing absenteeism due to minor illnesses that can be managed remotely [34]. This multifaceted advantage highlights how telemedicine can generate cost savings, enhance accessibility, and improve overall efficiency within the healthcare ecosystem, benefitting various stakeholders involved.
-
7.
Improved Access to specialists.
Data shows that less than 30 specialists per 100,000 patients are located in rural communities in most developing nations [62], [63]. People in outlying locations must travel farther to see experts and get potentially life-saving treatments. Due to the advancement brought by telemedicine, specialists are more easily accessible to patients. It also helps specialists access a wider range of patients, regardless of their location [59].
-
8.
Enhanced Health Outcomes and Quality Healthcare Treatment.
With urgent consultations in real-time, medical difficulties may be resolved in a matter of minutes. Getting a patient diagnosed and started on therapy soon after diagnosis may greatly improve their prognosis and save medical costs. Also, in areas where access to doctors or experts is limited, remote monitoring systems may improve the quality of treatment provided. Patients engaged in the remote monitoring programme were shown to have a 23 % reduced risk of hospitalisation, a 44 % lower risk of readmission within 30 days, and a 38 % lower risk of readmission within 90 days [61].
-
9.
Increase Participation from Patients.
The proliferation of telemedicine and the availability of several healthcare applications has helped patients become more comfortable with technology and more cognizant of their health. By making it easier for patients to keep their regular doctor's visits and other care commitments, telemedicine boosts patient involvement and compliance [21].
2.5. Causes of multidrug-resistant tuberculosis (MDR-TB)
-
1.
Incomplete adherence to prescribed drug schedules may occur when medication schedules are followed improperly, when drugs are not effective or of poor quality (e.g., when they expire), or when there are gaps in the regimen [47], [48], [49]. The spread of multidrug-resistant tuberculosis (MDR-TB) from one person to another is more common in vulnerable, crowded settings such as hospitals, prisons, refugee camps, and similar high-risk environments [43]. The greater the number of persons who disseminate MDR-TB without being diagnosed or successfully treated, the wider the spread of resistance and the greater the number of others who may become infected [46].
-
2.
Drug resistance can also be related to inadequate TB control policies at the national level, which may allow for ineffective TB treatment. TB control programmes are created to develop a system of supervision by health professionals that ensures completion of effective treatment [50]. However, nations with limited healthcare facilities and resources are unable to monitor every TB patient's course [51]. MDR TB treatment can be quite expensive and difficult to access. The treatment cycle can last up to two years and often involves daily injections for a minimum of six months. This regimen significantly raises the likelihood that patients won't complete the course of therapy compared to standard TB treatment [42], [43]. Patients who do not complete their treatment often develop resistance to second-line medications.
-
3.
Extremely drug-resistant, or XDR, TB strains are a new phenomenon. Less than 5 % of MDR TB cases are XDR TB cases [40]. XDR TB is defined as resistance to any fluoroquinolone, at least one of three second-line medications, and both first-line medications (rifampicins, isoniazid). The amount of direct XDR TB research and infrastructure is quite little and resource intensive [42], [52]. XDR TB is virtually untreatable in underdeveloped and least-developed nations because of the lack of available medical resources [52].
The treatment regimen for multidrug-resistant tuberculosis (MDR-TB) in Nigeria typically followed international guidelines set forth by organizations like the World Health Organization (WHO) [50], [62]. The standard treatment for MDR-TB involves a combination of multiple antibiotics over an extended period, often ranging from 9 to 24 months or even longer [63]. These medications are typically more expensive, have more potential side effects, and require strict adherence to the regimen for successful treatment outcomes [62]. The treatment regimen generally includes a combination of second-line anti-TB drugs, such as fluoroquinolones (e.g., moxifloxacin, levofloxacin), injectable agents (e.g., kanamycin, amikacin), and other drugs like linezolid, bedaquiline, and clofazimine [50]. The exact combination and duration of these drugs can vary based on factors like drug susceptibility testing, individual patient circumstances, and any pre-existing medical conditions [63].
However, in Nigeria, challenges related to medication availability, quality, and patient adherence have been significant hurdles in effectively implementing these treatment regimens [64]. There have been concerns regarding drug stockouts, inconsistent drug supply chains, and limitations in accessing newer, more effective drugs due to cost and availability issues [65]. Additionally, ensuring proper adherence to the treatment schedule has been a persistent challenge, leading to treatment failure and the potential for the development of extensively drug-resistant TB (XDR-TB) [64]. Efforts have been made to improve the situation, including initiatives to strengthen healthcare infrastructure, enhance drug procurement and distribution systems, and provide education and support to healthcare providers and patients [66], [67]. Moreover, the introduction of newer medications like bedaquiline and delamanid has provided additional options for MDR-TB treatment in the country [66], [68].
3. Conclusion
Telemedicine as a healthcare tool could revolutionize healthcare services delivery. Telemedicine is capable of solving issues related to insufficient healthcare providers in rural areas. As MDR-TB is frequently influenced by non-adherence to TB medication and transmission from person to person, telemedicine can be an effective tool in enhancing adherence to MDR-TB medication through Digital Health Monitoring, Patient Medication Tracking, and a decrease in the need for in-person services. Leveraging this, TB patients may gain a great deal from this technological advancement in treating this potentially fatal illness, which may result in serious adverse effects on their health. Their medications have to be used daily for a considerable length of time, failure to which may lead to resistant TB. The monthly visits to the health care centres for review and refill of medications can be hampered by long distances, bad roads, and the high cost of transportation. With the appropriate use of telemedicine, all these barriers could be circumvented, and therefore, quality health care will be delivered to TB patients, also saving the community from exposure to multi-drug resistant mycobacterium tuberculosis.
Additionally, telemedicine holds the potential for a broad range of uses, such as; a) online databases and tools to ensure standards of care; b) monitoring patient outcomes; c) computer-assisted diagnosis; d) efficient drug information and electronic prescription filling; and e) improved access to research data. With improved access and a more connected level of care, doctors and patients can collaborate to achieve their therapeutic goals, especially in home and hospice care situations. Clinicians are also able to manage more patients than traditional care models would generally permit.
4. Recommendations
While telemedicine has the potential to revolutionize care in Nigeria, there are several challenges that need to be addressed (Table 1).
-
1.
Several changes would need to be made to effectively implement telemedicine in Nigeria. First, efforts should be geared by stakeholders towards adopting telemedicine to a large extent in Nigeria by expanding the telecommunication network coverage and also improving digital literacyGovernment and healthcare administrators should provide facilities needed for telemedicine such as tablets, laptop Wi-Fi and internet services. This should be free or at subsidized rates so that the devices would be affordable and available to all. Health care practitioners should be trained in the usage of telemedicine. This is not limited to them. The other end users, the patients, should also be trained on the use of the devices, including maintenance. There should be provision for increased capacity building for the local electronic engineers on how to repair these devices. This will also serve as a means of income generation.
-
2.
MDR-TB patients should be monitored through telemedicine to tackle the problem of adherence to medications. This is the basis for the introduction of telemedicine into the care of TB patients so as to reduce the incidence of MDR-TB. This can be achieved by strengthening the DOT principles at reduced costs. MDR-TB patients should be encouraged to use telemedicine so as to prevent its transmission. There has to be an attitudinal change. It is often challenging to implement new methods of treatment. Using the behavioral wheel of change principles will help in the acceptance of new devices that will help to curb the spread of MDR-TB in our society.
Table 1.
Telemedicine Implementation Challenges and Solutions in Nigeria.
| Telemedicine implementation challenge | Suggested solution |
|---|---|
| Infrastructure limitations | The government should invest in improving the telecommunications infrastructure in Nigeria. This could include expanding the reach of mobile networks and improving internet connectivity. |
| Data privacy concerns | The government should develop and implement strong data privacy laws and regulations. These laws should protect the privacy of patient data when it is transmitted through telemedicine. |
| Cost | The government and private sector should work together to make telemedicine more affordable. This could include providing subsidies for telemedicine services or making it easier for health insurance companies to cover telemedicine costs. |
| Lack of trained healthcare providers | The government should train more healthcare providers in the use of telemedicine. This could be done through educational programs or by providing financial incentives for healthcare providers to learn about telemedicine. |
| Patient acceptance | The government and healthcare providers should educate patients about the benefits of telemedicine. This could be done through public awareness campaigns or by providing information about telemedicine to patients during their initial consultations. |
CRediT authorship contribution statement
Kikelomo S. Olowoyo: . Deborah T. Esan: . Benedict T. Adeyanju: . David B. Olawade: . Babatunji E. Oyinloye: . Paul Olowoyo: Writing – review & editing, Resources, Methodology, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Ugwu K.O., Agbo M.C., Ezeonu I.M. Prevalence of tuberculosis, drug-resistant tuberculosis and HIV/TB co-infection in Enugu. Nigeria African Journal of Infectious Diseases. 2021 Jul 26;15(2):24–30. doi: 10.21010/ajid.v15i2.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adewole O.O. Impact of COVID-19 on TB care: experiences of a treatment Centre in Nigeria. Int J Tuberc Lung Dis. 2020 Sep 1;24(9):981–982. doi: 10.5588/ijtld.20.0418. [DOI] [PubMed] [Google Scholar]
- 3.Olaleye S.A., Balogun O.S., Adusei-Mensah F. Bibliometric structured review of tuberculosis in Nigeria. Afr Health Sci. 2023 Jul 13;23(2):139–160. doi: 10.4314/ahs.v23i2.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Tuberculosis Fact Sheet. 2020. Retrieved on 05/09/2023 from https://www.who.int/news-room/factsheets/detail/tuberculosis.
- 5.Oladimeji O., Othman Y., Oladimeji K.E., Atiba B.P., Adepoju V.A., Odugbemi B.A. Patterns of presentation of drug-resistant tuberculosis in Nigeria: a retrospective file review. Microbiol Res. 2022 Aug 21;13(3):609–619. [Google Scholar]
- 6.Odume B, Sheshi M, Chukwuogo O, Sani U, Ogbudebe C, Aniwada E, Emperor U, Nongo D, Eneogu R, Oyelaran O, Efo E. Drug resistant tuberculosis treatment service alignment with health seeking behaviour in selected states in Nigeria.
- 7.Adebisi Y.A., Agumage I., Sylvanus T.D., Nawaila I.J., Ekwere W.A., Nasiru M., et al. Burden of tuberculosis and challenges facing its eradication in West Africa. international. J Infect. 2019 Jul 31;6(3) [Google Scholar]
- 8.Oshi D., Chukwu J., Nwafor C., Chukwu N.E., Meka A.O., Anyim M., et al. Support and unmet needs of patients undergoing multidrug-resistant tuberculosis (MDR-TB) treatment in southern Nigeria. Int J Health Plann Manage. 2020 Jul;35(4):832–842. doi: 10.1002/hpm.2929. [DOI] [PubMed] [Google Scholar]
- 9.Obioma A., Ngozika W.G. Investigation of prevalence of tuberculosis infection outcome in two government owned hospitals in Port Harcourt, Niger Delta. J Tuberc Ther. 2018;3(114):2. [Google Scholar]
- 10.Ukwaja K.N., Alobu I., Lgwenyi C., Hopewell P.C. The high cost of free tuberculosis services: patient and household costs associated with tuberculosis care in Ebonyi state, Nigeria. PLoS One. 2013 Aug 27;8(8):e73134. doi: 10.1371/journal.pone.0073134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roztocki N., Soja P., Weistroffer H.R. The role of information and communication technologies in socioeconomic development: towards a multi-dimensional framework. Inf Technol Dev. 2019;25(2):171–183. doi: 10.1080/02681102.2019.1596654. [DOI] [Google Scholar]
- 12.Doong S.H., Ho S.C. The impact of ICT development on the global digital divide. Electron Commer Res Appl. 2012;11(5):518–533. doi: 10.1016/j.elerap.2012.02.002. [DOI] [Google Scholar]
- 13.Karaman Aksentijević N., Ježić Z., Zaninović P.A. The effects of information and communication technology (ICT) use on human development—A macroeconomic approach. Economies. 2021;9(3):128. doi: 10.3390/economies9030128. [DOI] [Google Scholar]
- 14.Adebayo A., Akinyemi O.O. “What are you really doing in this country?”: emigration intentions of nigerian doctors and their policy implications for human resource for health management. J Int Migr Integr. 2021;23(3):1377–1396. doi: 10.1007/s12134-021-00898-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Onah C.K., Azuogu B.N., Ochie C.N., et al. Physician emigration from Nigeria and the associated factors: the implications to safeguarding the Nigeria health system. Hum Resour Health. 2022;20(85) doi: 10.1186/s12960-022-00788-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gizaw Z., Astale T., Kassie G.M. What improves access to primary healthcare services in rural communities? a systematic review. BMC. Prim Care. 2022;23(313) doi: 10.1186/s12875-022-01919-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Shorbaji N. Improving healthcare access through digital health: the use of information and communication technologies. Healthcare Access Published online. 2022 doi: 10.5772/intechopen.99607. [DOI] [Google Scholar]
- 18.Obubu M., Chuku N., Ananaba A., et al. Evaluation of healthcare facilities and personnel distribution in Lagos state: implications on universal health coverage. Hosp Pract. 2023;51(2):1–12. doi: 10.1080/21548331.2023.2170651. [DOI] [PubMed] [Google Scholar]
- 19.Adeloye D., David R.A., Olaogun A.A., et al. Health workforce and governance: the crisis in Nigeria. Hum Resour Health. 2017;15(32) doi: 10.1186/s12960-017-0205-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Universal Health Coverage Partnership Annual Report 2019. In Practice: Bridging Global Commitments with Country Action to Achieve Universal Health Coverage. Geneva: World Health Organization; 2020:11-75. Accessed June 30, 2023. https://apps.who.int/iris/bitstream/handle/10665/341433/9789240012950-eng.pdf?sequence=1.
- 21.Haleem A., Javaid M., Singh R.P., Suman R. Telemedicine for healthcare: capabilities, features, barriers, and applications. Sensors International. 2021;2 doi: 10.1016/j.sintl.2021.100117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Binder W.J., Cook J.L., Gramze N., Airhart S. Telemedicine in the intensive care unit. Crit Care Nurs Clin North Am. 2018;30(2):289–296. doi: 10.1016/j.cnc.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 23.Parajuli R., Doneys P. Exploring the role of telemedicine in improving access to healthcare services by women and girls in rural Nepal. Telematics Inform. 2017;34(7):1166–1176. doi: 10.1016/j.tele.2017.05.006. [DOI] [Google Scholar]
- 24.Grigsby J., Kaehny M.M., Sandberg E.J., Schlenker R.E., Shaughnessy P.W. Effects and effectiveness of telemedicine. Health Care Financ Rev. 1995;17(1):115–131. [PMC free article] [PubMed] [Google Scholar]
- 25.Mirsaeidi M., Farshidpour M., Banks-Tripp D., Hashmi S., Kujoth C., Schraufnagel D. Video directly observed therapy for treatment of tuberculosis is patient-oriented and cost-effective. Eur Respir J. 2015;46(3):871–874. doi: 10.1183/09031936.00011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lippincott C.K., Perry A., Munk E., Maltas G., Shah M. Tuberculosis treatment adherence in the era of COVID-19. BMC Infect Dis. 2022;22(800) doi: 10.1186/s12879-022-07787-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shawwa L. The use of telemedicine in medical education and patient care. Cureus. 2023;15(4):e37766. doi: 10.7759/cureus.37766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alotaibi Y., Federico F. The impact of health information technology on patient safety. Saudi Med J. 2019;38(12):1173–1180. doi: 10.15537/smj.2017.12.20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gonçalves-Bradley D.C., Maria J., AR, Ricci-Cabello I,, et al. Mobile technologies to support healthcare provider to healthcare provider communication and management of care. Cochrane Database Syst Rev. 2020;2020(8):CD012927 doi: 10.1002/14651858.cd012927.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alarabyat I.A., Al-Nsair N., Alrimawi I., Al-Yateem N., Shudifat R.M., Saifan A.R. Perceived barriers to effective use of telehealth in managing the care of patients with cardiovascular diseases: a qualitative study exploring healthcare professionals’ views in Jordan. BMC Health Serv Res. 2023;23(452) doi: 10.1186/s12913-023-09368-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Physiopedia. Barriers to Telehealth. Physiopedia. Published 2023. Accessed July 3, 2023. https://www.physio-pedia.com/Barriers_to_Telehealth.
- 32.Kruse C.S., Karem P., Shifflett K., Vegi L., Ravi K., Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(3):4–12. doi: 10.1177/1357633x16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thimbleby H. Technology and the future of healthcare. Journal of Public Health Research. 2013;2(3):e28. doi: 10.4081/jphr.2013.e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dash S., Shakyawar S.K., Sharma M., Kaushik S. Big data in healthcare: management, analysis and future prospects. Journal of Big Data. 2019;6(54):1–25. doi: 10.1186/s40537-019-0217-0. [DOI] [Google Scholar]
- 35.Kane C.K., Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff. 2018;37(12):1923–1930. doi: 10.1377/hlthaff.2018.05077. [DOI] [PubMed] [Google Scholar]
- 36.Nittari G., Khuman R., Baldoni S., et al. Telemedicine practice: review of the current ethical and legal challenges. Telemedicine and e-Health. 2020;26(12):1427–1437. doi: 10.1089/tmj.2019.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Donahue M.L., Eberly M.D., Rajnik M. Tele-TB: using TeleMedicine to increase access to directly observed therapy for latent tuberculosis infection. Mil Med. 2021;186(Supplement 1):25–31. doi: 10.1093/milmed/usaa300. [DOI] [PubMed] [Google Scholar]
- 38.Snoswell C.L., Taylor M.L., Comans T.A., Smith A.C., Gray L.C., Caffery L.J. Determining if telehealth can reduce health system costs: scoping review. J Med Internet Res. 2020;22(10):e17298. doi: 10.2196/17298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Margineanu I., Louka C., Akkerman O., Stienstra Y., Alffenaar J.-W. eHealth in TB clinical management. Int J Tuberc Lung Dis. 2022;26(12):1151–1161. doi: 10.5588/ijtld.21.0602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alvandi M. Telemedicine and its Role in Revolutionizing Healthcare Delivery. The American Journal of Accountable Care. 2017;5(1): e1-e5. Accessed July 4, 2023. https://www.ajmc.com/view/telemedicine-and-its-role-in-revolutionizing-healthcare-delivery.
- 41.Parsons J.A. The telemedical imperative. Bioethics. 2021;35(4):298–306. doi: 10.1111/bioe.12847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.World Health Organization. Global Tuberculosis Report 2022. Geneva: World Health Organization; 2022:15-67. Accessed July 4, 2023. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022.
- 43.Chakaya J., Khan M., Ntoumi F., et al. Global tuberculosis report 2020 – reflections on the global TB burden, treatment and prevention efforts. Int J Infect Dis. 2021;113(Supplement 1):S7–S12. doi: 10.1016/j.ijid.2021.02.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baghaei P., Tabarsi P., Javanmard P., et al. Impact of diabetes mellitus on tuberculosis drug resistance in new cases of tuberculosis. Journal of Global Antimicrobial Resistance. 2016;4:1–4. doi: 10.1016/j.jgar.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 45.Nguyen L. Antibiotic resistance mechanisms in M. tuberculosis: an update. Arch Toxicol. 2016;90(7):1585–1604. doi: 10.1007/s00204-016-1727-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liebenberg D., Gordhan B.G., Kana B.D. Drug resistant tuberculosis: implications for transmission, diagnosis, and disease management. Front Cell Infect Microbiol. 2022;12 doi: 10.3389/fcimb.2022.943545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nigerian Federal Ministry of Health. National Tuberculosis and Leprosy Control Programme. Federal Ministry of Health Department of Public Health; 2019:7-43. Accessed July 4, 2023. https://www.health.gov.ng/doc/Draft-2019-NTBLCP-Annual-report-22032020.pdf.
- 48.Mekonnen H.S., Azagew A.W. Non-adherence to anti-tuberculosis treatment, reasons and associated factors among TB patients attending at Gondar town health centers. Northwest Ethiopia BMC Research Notes. 2018;11:691. doi: 10.1186/s13104-018-3789-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Silva D.R., Rendon A., Alffenaar J.W., et al. Global TB network: working together to eliminate tuberculosis. J Bras Pneumol. 2018;44(5):347–349. doi: 10.1590/s1806-37562018000000279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.World Health Organization . World Health Organization; Geneva: 2022. WHO consolidated guidelines on tuberculosis. module 4: treatment - drug-resistant tuberculosis treatment 2022 update. Accessed July 4, 2023. [PubMed] [Google Scholar]
- 51.World Health Organization. World bank and WHO: Half the world lacks access to essential health services, 100 million still pushed into extreme poverty because of health expenses. World Health Organization. Published 2017. Accessed July 4, 2023. https://www.who.int/news/item/13-12-2017-world-bank-and-who-half-the-world-lacks-access-to-essential-health-services-100-million-still-pushed-into-extreme-poverty-because-of-health-expenses.
- 52.Bu Q., Qiang R., Fang L., Peng X., Zhang H., Cheng H. Global trends in the incidence rates of MDR and XDR tuberculosis: findings from the global burden of disease study 2019. Front Pharmacol. 2023;14:1156249. doi: 10.3389/fphar.2023.1156249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.World Health Organization & European Respiratory Society. Digital Health for the End TB Strategy: An Agenda for Action. World Health Organization; 2015:1-24. Accessed July 4, 2023. .
- 54.World Health Organization. What Is DOTS? A Guide to Understanding the WHO-Recommended TB Control Strategy Known as DOTS. World Health Organization; 1999:6-30. Accessed July 4, 2023. https://apps.who.int/iris/bitstream/handle/10665/65979/WHO_CDS_CPC_TB_99.270.pdf.
- 55.Muture B.N., Keraka M.N., Kimuu P.K., Kabiru E.W., Ombeka V.O., Oguya F. Factors associated with default from treatment among tuberculosis patients in Nairobi province, Kenya: a case control study. BMC Public Health. 2011;11(696) doi: 10.1186/1471-2458-11-696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Menzies D., Adjobimey M., Ruslami R., et al. Four months of rifampin or nine months of isoniazid for latent tuberculosis in adults. N Engl J Med. 2018;379(5):440–453. doi: 10.1056/nejmoa1714283. [DOI] [PubMed] [Google Scholar]
- 57.Oh C.E., Menzies D. Four months of rifampicin monotherapy for latent tuberculosis infection in children. Clinical and Experimental Pediatrics. 2021;65(5):214–221. doi: 10.3345/cep.2021.01186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huang G.K.L., Pawape G., Taune M., et al. Telemedicine in resource-limited settings to optimize Care for Multidrug-Resistant Tuberculosis. Front Public Health. 2019;7:222. doi: 10.3389/fpubh.2019.00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gashu K.D., Gelaye K.A., Mekonnen Z.A., Lester R., Tilahun B. Does phone messaging improve tuberculosis treatment success? a systematic review and meta-analysis. BMC Infect Dis. 2020;20(1):42. doi: 10.1186/s12879-020-4765-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Warshaw R. Health Disparities Affect Millions in Rural U.S. Communities.; 2017. Accessed July 4, 2023. .
- 61.Cyr M.E., Etchin A.G., Guthrie B.J., Benneyan J.C. Access to specialty healthcare in urban versus rural US populations: a systematic literature review. BMC Health Serv Res. 2019;19(1):974. doi: 10.1186/s12913-019-4815-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ohiengbomwan O.T., Oguzie J., Eromon P., Kayode A.T., Afolabi T.S., Komolafe I.O. Gene mutation patterns of mycobacterium tuberculosis complex and associated factors among suspected multidrug-resistant tuberculosis patients in Osun state, south-west, Nigeria. Scientific African. 2023 Nov;1(22):e01968. [Google Scholar]
- 63.Lange C., Aarnoutse R.E., Alffenaar J.W., Bothamley G., Brinkmann F., Costa J., et al. Management of patients with multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2019 Jun 1;23(6):645–662. doi: 10.5588/ijtld.18.0622. [DOI] [PubMed] [Google Scholar]
- 64.Adagba K.O., Aliyu A.A., Ejembi C.L., Olorukooba A.A., Joshua I.A. Comparative study of patients' adherence between hospital-based and communitybased treatment for multidrug resistant tuberculosis (MDR-TB) in Kaduna state. Journal of Community Medicine and Primary Health Care. 2023 Apr 6;35(1):112–124. [Google Scholar]
- 65.Ogbuabor DC, Onwujekwe OE. Governance of tuberculosis control programme in Nigeria. Infectious diseases of poverty. 2019 Dec. 8. 1-1. [DOI] [PMC free article] [PubMed]
- 66.Bada F.O., Okpokoro E., Blok N., Meribole E., Dutt S., Dakum P., et al. Cost of three models of care for drug-resistant tuberculosis patients in Nigeria. BMC Infect Dis. 2019 Dec;19(1):1. doi: 10.1186/s12879-018-3636-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Oluwasanu M.M., Hassan A., Adebayo A.M., Ogbuji Q.C., Adeniyi B.O., Adewole D.A., et al. General and tuberculosis-specific service readiness in two states in Nigeria. BMC Health Serv Res. 2020 Dec;20(1):1–5. doi: 10.1186/s12913-020-05626-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dayyab F.M., Iliyasu G., Ahmad B.G., Habib A.G. Early safety and efficacy of linezolid-based combination therapy among patients with drug-resistant tuberculosis in North-Western Nigeria. The International Journal of Mycobacteriology. 2021 Apr 1;10(2):129–135. doi: 10.4103/ijmy.ijmy_57_21. [DOI] [PubMed] [Google Scholar]