Abstract
Hip arthroscopy continues to increase in popularity and has an ever-expanding range of indications; however, the steep learning curve introduces significant risk of iatrogenic chondrolabral injury when accessing the joint and establishing arthroscopic portals. This article presents a technique for establishing the modified midanterior portal and is particularly useful when the available space is tight. We present “the air-lift” as a safe and simple adjunct to standard portal creation when performing hip arthroscopy in the supine position.
Technique Video
We describe a technique called the air lift for improving safety and reducing risk of chondrolabral injury while establishing the modified midanterior portal. This is a simple technique that involves placing a minimum of 60 cc of air through the arthroscope to facilitate greater precision, efficiency, and safety of mid anterior portal placement. The anterolateral viewing portal has been created under fluoroscopic guidance and we are viewing through this with a 70° arthroscope (Stryker, Denver, CO). We illustrate this technique in the 3 distinct examples to follow. The first is a situation in which the ideal placement of the needle puts the femoral head at risk of iatrogenic injury, as shown by this arrow. Use of the air lift in this case creates substantial expansion of the anterior triangle. This amount of decreased exposure is common in patients with at least some baseline soft-tissue laxity. In patients like this, it is critical to preserve the hip capsule with a strong and complete capsule repair. One of the key technical steps in achieving this is making the interportal capsulotomy far enough from the acetabular rim to preserve enough capsule for optimal suture placement. This is one of our favorite applications of the air-lift technique. The next case is a more typical example of a small anterior triangle. Although midanterior portal placement is possible, the window for placement is small, which can lead to iatrogenic injury or prolonged access time. Here you can see the air lift creates less space than in the previous example but that incremental space is of high value, doubling the accessible space of the anterior triangle. This case required repeating the air lift to optimize needle placement. You can see here, where the air lift allowed to see that placement of the needle would have caused iatrogenic injury, and we then moved the needle to a more optimal, safer location. The final case, is a collegiate football lineman with a large cam morphology, and you can see the increased exposure the air lift generates. This example demonstrates how the air lift can generate resistance against the anterior capsule to make needle placement safer. This example also demonstrates optimal insertion depth of the needle; no further than is necessary to allow placement of the wire. The final series of images review these 3 cases before and after the air lift. We hope this simple but effective technique can be useful to you in your practice.
Since Ganz first described the phenomenon of femoroacetabular impingement in 2003,1 hip arthroscopy has grown in popularity and has emerged as an effective treatment for femoroacetabular impingement along with many other intra-articular and periarticular hip pathologies. From 2005 to 2010, the number of arthroscopic hip procedures increased by >600%.2 Hip arthroscopy has been shown to have excellent outcomes in the right patient groups, including competitive athletes3 and adolescents.4 Simultaneously, hip arthroscopy remains one of the most challenging procedures in orthopaedics and comes with a steep learning curve.2,5 A 2010 study showed that although the nature of complications changes with surgeon experience, there was no significant variation in incidence over a 9-year period.6 In a large systematic review, iatrogenic chondrolabral injury was reported as the most common minor complication along with transient neuropraxia.7 Furthermore, supine positioning for hip arthroscopy has been associated with a greater rate of labral penetration when compared with lateral decubitus positioning.8
It is important that as a community of surgeons we continue to refine our techniques to reduce iatrogenic complications. This technique offers a reproducible way of improving safe and efficacious access to the hip joint while creating the modified mid anterior portal during hip arthroscopy with a supine positioned patient.
Surgical Technique (With Video Illustration)
Placement of the midanterior portal can be challenging. While viewing from the anterolateral portal, the anterior triangle is visualized, with the borders consisting of the acetabular labrum, femoral head, and anterior capsule. The modified midanterior portal entry is through this window. Sometimes the anterior triangle is small secondary to synovitis, a hypertrophic labrum, or difficult distraction. Other times, the anterior triangle may be large enough, but placement of the needle and cannula could be easier with a little more space. Other times, the anterior capsule is laying against the femoral head and the optimal portal location and placement of the needle and cannula could create iatrogenic injury. We describe a technique called the air lift for improving safety and reducing risk of chondrolabral injury whilst establishing the modified midanterior portal, demonstrated in Video 1.
The patient is positioned supine using the Stryker Pivot Guardian hip distraction system (Stryker, Denver, CO; Fig 1). Surface anatomy is marked on the skin, including the profile of the greater trochanter and a line extending distally from the anterior superior iliac spine. An air arthrogram (Fig 2) is performed by injecting air into the hip joint through a distal anterior location under image intensifier guidance. After the joint has been insufflated, longitudinal traction is applied to the limb with approximately 75 lbs of force typically used to achieve distraction of the femoral head from the acetabulum.
Fig 1.
Photograph of standard supine set up for hip arthroscopy using the Stryker Pivot Guardian hip distraction system and hip check (Stryker) with surface anatomy marked on the skin including the profile of the greater trochanter and a line extending distally from the anterior superior iliac spine. Patient's left side, supine position.
Fig 2.
An air arthrogram is performed injecting air into the hip joint through a distal anterior location under image intensifier guidance (needle is labeled). After the joint has been insufflated, longitudinal traction is applied to the limb with approximately 75 lbs of force typically used to achieve distraction of the femoral head from the acetabulum. Patient's right side, supine position.
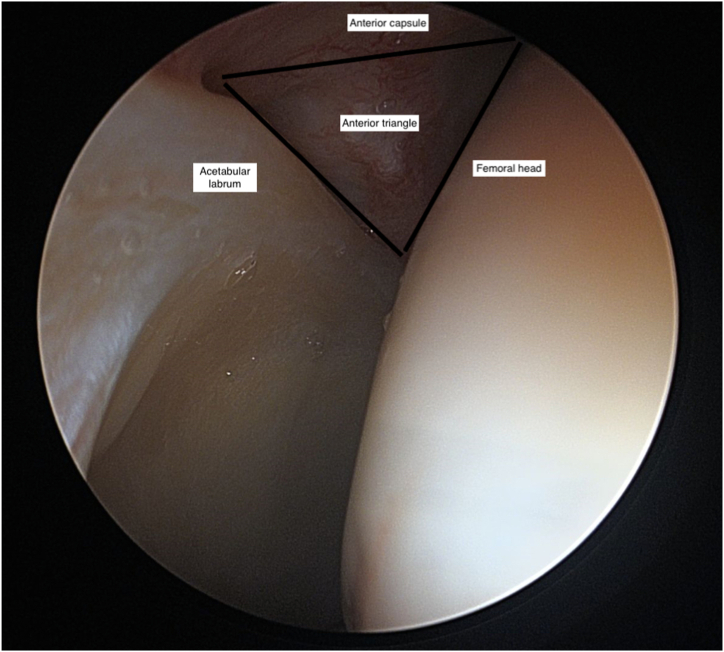
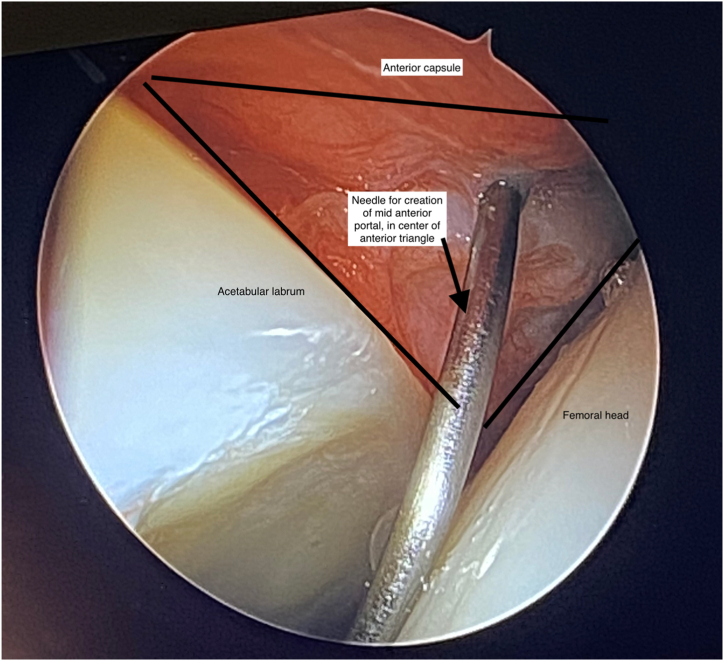
Under radiographic guidance, the initial anterolateral viewing portal is created with a needle followed by a wire positioned parallel to the sourcil of the acetabulum. Once the ideal position of the needle and wire is achieved (Fig 3), the portal is dilated and developed (Fig 4) and then a 70° arthroscope (Stryker) inserted. This is performed as a dry view, as fluid has not yet been introduced to the hip joint. While viewing from the anterolateral portal, the anterior triangle is visualized (Fig 5) with the borders consisting of the acetabular labrum, femoral head and anterior capsule. The desired entry point for the modified midanterior portal is in the center of this triangle, but the space can be tighter than ideal, with the needle and trocar risking chondral injury if we enter and then dilate in this location without sufficient space (Fig 6).
Fig 3.
An anterior posterior view of the hip joint showing the initial needle for creation of the anterolateral viewing portal. Under radiograph guidance the initial anterolateral viewing portal is created with a needle followed by a wire positioned parallel to the sourcil of the acetabulum. Patient's right side, supine position.
Fig 4.
An anterior posterior view of the hip joint showing the initial needle for creation of the anterolateral viewing portal. The initial needle is removed and the portal is dilated and developed. Following this a 70° arthroscope (Stryker, Denver, CO) is inserted. Patient's right side, supine position.
Fig 5.
Surgeon’s view through the anterolateral portal with a 70° arthroscope visualizing the anterior triangle with the borders consisting of the acetabular labrum, femoral head and anterior capsule (labeled). This is performed as a dry view, as fluid has not yet been introduced to the hip joint. The desired entry point for the modified mid anterior portal is in the center of this triangle but this space can be tighter than ideal, with the needle and trocar risking chondral injury if we enter and then dilate in this location without sufficient space. Patient's left side, supine position.
Fig 6.
Surgeon’s view through the anterolateral viewing portal with the 70° arthroscope screen as the needle is inserted for creation of the mid anterior portal. The needle is in the center of the anterior triangle with the borders consisting of the acetabular labrum, femoral head and anterior capsule (labeled). Patient's left side, supine position.
At this point, we attach a 60-cc syringe (Luer-Lok syringe [Franklin Lakes, NJ, USA] included with the Stryker Portal Entry Kit, although any BD 60-cc Luer-Lok syringe would suffice) to the 3-way mechanism on the arthroscope portal, as seen in Figure 7. Air is used to insufflate the joint and expand the potential space. The needle is then advanced into the space and we proceed to dilate the portal from there using the Stryker flow port cannulae and capsule punch (Stryker), placing traction sutures into the capsule as per our standard technique to maintain a single pathway into the joint for our instrumentation.
Fig 7.
Photograph of the setup for insufflation of the joint for the air-lift technique during supine hip arthroscopy. The arthroscope is in the anterolateral viewing portal with a 60-cc syringe attached to the 3-way mechanism on the arthroscope. This is then used to inflate the joint before creation of the modified midanterior portal. Please see related video for more information relating to this technique. Patient's right side, supine position.
Discussion
The air-lift technique presented here is a simple adjunct to the creation of standard hip arthroscopy portals. The primary advantage is that it increases the space available for portal creation and thus reduces the risk of chondrolabral injury when entering the hip joint. The advantages and disadvantages of the airlift technique are presented in Table 1. The technique does require a dry scope technique, and we would typically introduce fluid into the joint immediately after the modified mid anterior portal has been established. Pearls and pitfalls are outlined in Table 2.
Table 1.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Avoidance of iatrogenic chondral injury in the setting of limited space | Requires use of a dry scope technique |
| Does not require specific instrumentation or equipment | Adds a small amount of operative time to the case |
| Does not require learning a new skill set or technique; simple addition to the case |
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Begin the case with a dry scope technique and introduce fluid into the joint after creation of the midanterior portal | The anterolateral viewing portal must be in an adequate position to visualize the anterior triangle adequately |
| Time the insufflation of the joint with the introduction of the needle, so that the joint is maximally expanded as the needle is introduced through the anterior triangle | The air lift may be less useful in revision settings in which the capsule is less pliable |
There are some minor limitations to this technique, in that it may be less useful in the revision setting when the capsule is less pliable and may not insufflate as well. In addition, the anterolateral viewing portal needs to be in an adequate position to enable the anterior triangle to be visualized for placement of the modified mid anterior portal. The use of intra-articular air to expand the available space may be able to be extrapolated to other portals; however, the technique would necessitate that this is done before the introduction of fluid into the joint and in an enclosed space so that pressure can be generated. While we have not performed a quantitative study, it is our experience that the incidence of iatrogenic chondrolabral injury is reduced using this technique.
The air lift can help to reduce the incidence of one of the most common preventable complications in hip arthroscopy5 (iatrogenic chondrolabral injury) while adding minimally to the overall time and complexity of the surgical procedure as a whole. A recent study9 has shown that there is no significant reduction in cartilage thickness on magnetic resonance imaging following successful arthroscopic cam resection with labral repair, which emphasizes the importance of avoiding any iatrogenic injury to the chondrolabral complex. In addition, a 2023 study10 has shown no significant morphologic change in labral size after arthroscopic repair, with patients with hypertrophic labrums achieving more favorable clinical outcomes than those with a normal size labrum. Although the implications of these findings require further study, the suggestion is that loss of labral volume secondary to iatrogenic injury would have a negative effect on outcome of labral repair. The air lift is a simple, yet effective, technique with the potential to benefit patients and avoid unwanted complications. We hope it is a useful adjunct to your practice.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: E.J.S. reports editorial board for Arthroscopy. R.C.M. reports personal fees from and other from Stryker, other from SCA Health, and nonfinancial support and other from American Academy of Orthopaedic Surgeons and North Carolina Orthopaedic Association, outside the submitted work. All other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
We describe a technique called the air lift for improving safety and reducing risk of chondrolabral injury while establishing the modified midanterior portal. This is a simple technique that involves placing a minimum of 60 cc of air through the arthroscope to facilitate greater precision, efficiency, and safety of mid anterior portal placement. The anterolateral viewing portal has been created under fluoroscopic guidance and we are viewing through this with a 70° arthroscope (Stryker, Denver, CO). We illustrate this technique in the 3 distinct examples to follow. The first is a situation in which the ideal placement of the needle puts the femoral head at risk of iatrogenic injury, as shown by this arrow. Use of the air lift in this case creates substantial expansion of the anterior triangle. This amount of decreased exposure is common in patients with at least some baseline soft-tissue laxity. In patients like this, it is critical to preserve the hip capsule with a strong and complete capsule repair. One of the key technical steps in achieving this is making the interportal capsulotomy far enough from the acetabular rim to preserve enough capsule for optimal suture placement. This is one of our favorite applications of the air-lift technique. The next case is a more typical example of a small anterior triangle. Although midanterior portal placement is possible, the window for placement is small, which can lead to iatrogenic injury or prolonged access time. Here you can see the air lift creates less space than in the previous example but that incremental space is of high value, doubling the accessible space of the anterior triangle. This case required repeating the air lift to optimize needle placement. You can see here, where the air lift allowed to see that placement of the needle would have caused iatrogenic injury, and we then moved the needle to a more optimal, safer location. The final case, is a collegiate football lineman with a large cam morphology, and you can see the increased exposure the air lift generates. This example demonstrates how the air lift can generate resistance against the anterior capsule to make needle placement safer. This example also demonstrates optimal insertion depth of the needle; no further than is necessary to allow placement of the wire. The final series of images review these 3 cases before and after the air lift. We hope this simple but effective technique can be useful to you in your practice.
References
- 1.Ganz R., Parvizi J., Beck M., Leunig M., Notzli H., Siebenrock K.A. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 2.Maldonado D.R., Rosinsky P.J., Shapira J., Domb B.G. Stepwise safe access in hip arthroscopy in the supine position: Tips and pearls from A to Z. J Am Acad Orthop Surg. 2020;28:651–659. doi: 10.5435/JAAOS-D-19-00856. [DOI] [PubMed] [Google Scholar]
- 3.Jimenez A.E., Monahan P.F., Owens J.S., Maldonado D.R., Curley A.J., Domb B.G. Earlier treatment yields superior outcomes in competitive athletes undergoing primary hip arthroscopy. Arthroscopy. 2021;38:2183–2191. doi: 10.1016/j.arthro.2021.11.053. [DOI] [PubMed] [Google Scholar]
- 4.Maldonado D.R., Kufta A.Y., Krych A.J., et al. Primary hip arthroscopy for femoroacetabular impingement syndrome in adolescents improves outcomes and clinical benefit achievement rates at short term follow: A multicenter analysis. Arthroscopy. 2023;39:1211–1219. doi: 10.1016/j.arthro.2022.11.020. [DOI] [PubMed] [Google Scholar]
- 5.Mehta N., Chamberlin P., Marx R.G., et al. Defining the learning curve for hip arthroscopy. Am J Sports Med. 2018;46:1285–1293. doi: 10.1177/0363546517749219. [DOI] [PubMed] [Google Scholar]
- 6.Schröder e Souza B.G., Solatu Dani W., Kiyoshi Honda E., et al. Do complications in hip arthroscopy change with experience? Arthroscopy. 2010;26:1053–1057. doi: 10.1016/j.arthro.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 7.Harris J.D., McCormick F.M., Abrams G.D., et al. Complications and reoperations during and after hip arthroscopy: A systematic review of 92 studies and more than 6000 patients. Arthroscopy. 2013;29:589–595. doi: 10.1016/j.arthro.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 8.de Sa D., Stephens K., Parmar D., Phillippon M.J. A comparison of supine and lateral decubitus positions for hip arthroscopy: A systematic review of outcomes and complications. Arthroscopy. 2016;32:716–725. doi: 10.1016/j.arthro.2015.12.028. [DOI] [PubMed] [Google Scholar]
- 9.Forster-Hovarth C., Unterreithmeier U., Fries S., et al. Midterm follow and assessment of cartilage thickness by arthro-magnetic resonance imaging after arthroscopic cam resection, labral repair and rim trimming without labral detachment. Arthroscopy. 2021;37:541–551. doi: 10.1016/j.arthro.2020.10.012. [DOI] [PubMed] [Google Scholar]
- 10.Liu R., Gao G., Wu R., Dong H., Zhang S., Xu Y. Changes in hip labral size two years after arthroscopic repair are correlated with preoperative measurements on magnetic resonance imaging. Arthroscopy. 2023;39:1440–1450. doi: 10.1016/j.arthro.2022.12.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
We describe a technique called the air lift for improving safety and reducing risk of chondrolabral injury while establishing the modified midanterior portal. This is a simple technique that involves placing a minimum of 60 cc of air through the arthroscope to facilitate greater precision, efficiency, and safety of mid anterior portal placement. The anterolateral viewing portal has been created under fluoroscopic guidance and we are viewing through this with a 70° arthroscope (Stryker, Denver, CO). We illustrate this technique in the 3 distinct examples to follow. The first is a situation in which the ideal placement of the needle puts the femoral head at risk of iatrogenic injury, as shown by this arrow. Use of the air lift in this case creates substantial expansion of the anterior triangle. This amount of decreased exposure is common in patients with at least some baseline soft-tissue laxity. In patients like this, it is critical to preserve the hip capsule with a strong and complete capsule repair. One of the key technical steps in achieving this is making the interportal capsulotomy far enough from the acetabular rim to preserve enough capsule for optimal suture placement. This is one of our favorite applications of the air-lift technique. The next case is a more typical example of a small anterior triangle. Although midanterior portal placement is possible, the window for placement is small, which can lead to iatrogenic injury or prolonged access time. Here you can see the air lift creates less space than in the previous example but that incremental space is of high value, doubling the accessible space of the anterior triangle. This case required repeating the air lift to optimize needle placement. You can see here, where the air lift allowed to see that placement of the needle would have caused iatrogenic injury, and we then moved the needle to a more optimal, safer location. The final case, is a collegiate football lineman with a large cam morphology, and you can see the increased exposure the air lift generates. This example demonstrates how the air lift can generate resistance against the anterior capsule to make needle placement safer. This example also demonstrates optimal insertion depth of the needle; no further than is necessary to allow placement of the wire. The final series of images review these 3 cases before and after the air lift. We hope this simple but effective technique can be useful to you in your practice.
We describe a technique called the air lift for improving safety and reducing risk of chondrolabral injury while establishing the modified midanterior portal. This is a simple technique that involves placing a minimum of 60 cc of air through the arthroscope to facilitate greater precision, efficiency, and safety of mid anterior portal placement. The anterolateral viewing portal has been created under fluoroscopic guidance and we are viewing through this with a 70° arthroscope (Stryker, Denver, CO). We illustrate this technique in the 3 distinct examples to follow. The first is a situation in which the ideal placement of the needle puts the femoral head at risk of iatrogenic injury, as shown by this arrow. Use of the air lift in this case creates substantial expansion of the anterior triangle. This amount of decreased exposure is common in patients with at least some baseline soft-tissue laxity. In patients like this, it is critical to preserve the hip capsule with a strong and complete capsule repair. One of the key technical steps in achieving this is making the interportal capsulotomy far enough from the acetabular rim to preserve enough capsule for optimal suture placement. This is one of our favorite applications of the air-lift technique. The next case is a more typical example of a small anterior triangle. Although midanterior portal placement is possible, the window for placement is small, which can lead to iatrogenic injury or prolonged access time. Here you can see the air lift creates less space than in the previous example but that incremental space is of high value, doubling the accessible space of the anterior triangle. This case required repeating the air lift to optimize needle placement. You can see here, where the air lift allowed to see that placement of the needle would have caused iatrogenic injury, and we then moved the needle to a more optimal, safer location. The final case, is a collegiate football lineman with a large cam morphology, and you can see the increased exposure the air lift generates. This example demonstrates how the air lift can generate resistance against the anterior capsule to make needle placement safer. This example also demonstrates optimal insertion depth of the needle; no further than is necessary to allow placement of the wire. The final series of images review these 3 cases before and after the air lift. We hope this simple but effective technique can be useful to you in your practice.