Abstract
Trochlear dysplasia is the main anatomical risk factor for objective patellar instability. Surgical correction of trochlea dysplasia via a trochleoplasty has been described with good clinical results reported. Concerns remain for who have abnormal patellofemoral tracking post a trochleoplasty due to incongruence between the two articulating surfaces. We described a medial closing wedge patellar osteotomy to improve congruency of the patellofemoral joint post-trochleoplasty.
Technique Video
Medial patellar closing-wedge osteotomy in patellofemoral instability. Sedation and regional anesthesia with the patient placed in a supine position with 2 supports (lateral and distal) on the right knee. A 10-cm midline skin incision is used. After performing the sulcus deepening trochleoplasty patellofemoral tracking is tested. In case of persistence of maltracking the MCWPO is performed. A sterile marking pen is used to draw 2 medial dashed lines to set the thickness of the osteotomy. A third dashed line is drawn at the midline of the patella. With an oscillating saw, 2 osteotomies converging medially are performed and the cortical wedge of bone is removed. The osteotomy is closed with a grasper. A 1.7-mm drill is used to create two anterior to posterior transosseous holes. Two sutures no. 2 VICRYL (Ethicon, Somerville, NJ) are driven from anterior to posterior through the first hole and then with an opposite direction through the second hole. A knot is then carried out on the anterior patellar bone surface using the 4 ends of the suture. The new patellofemoral tracking is tested.
Despite being widely studied, patellofemoral dysplasia still represents a highly challenging condition. Trochlear dysplasia is the main anatomical risk factor for objective patellar instability (OPI), with an incidence of 96% in patients with OPI compared with 3% of patients without OPI.1 Surgical correction of trochlea dysplasia via a trochleoplasty has been described with good clinical results reported.2
Patellofemoral stability is determined not only by the trochlear morphology but also the patella, in agreement with the fundamental principle that the primary stability of a joint is determined by the congruence of the 2 articulating joint surfaces.3 Abnormal patellar shape can cause incongruency between the 2 articulating surfaces and play a role in patellofemoral dislocations.4,5
The patella has 2 main articulating surfaces, a medial and lateral facet. In patients with OPI and trochlear dysplasia, the patellar shape is modified. The medial facet is relatively smaller and the lateral facet relatively larger.5,6 The patellar shape was first classified by Wiberg in 1941.7 The classification uses axial radiographs at 30° of knee flexion to classify the patella into 3 types:
-
•
Type I: The medial facet is concave and has almost the same area as the lateral facet.
-
•
Type II: The medial facet is still concave but is smaller than the lateral facet.
-
•
Type III: The medial facet is convex and almost vertical.
A type IV patella was later added by Baumgartl and is when the medial facet is absent.8
A trochleoplasty increases the concavity of the trochlea groove, and as a result, there is the potential for a discrepancy between the angulation of the patellar articular facets with the trochlear groove.9 This incongruency is often seen in cases of high-grade patellar dysplasia (type III and IV) and can result in persistence of patellar maltracking and elevated point pressures post-trochleoplasty.
A patellar osteotomy aims to recreate medial and lateral patellar facets, forming an angle congruent with the reshaped trochlear groove. Patellar osteotomies in the case of OPI added to trochleoplasty, however, have scarcely been described.10,11 We present the surgical technique for performing a medial closing-wedge patellar osteotomy (MCWPO) to improve congruency of the patellofemoral joint post trochleoplasty.
Surgical Technique (With Video Illustration)
Indication for Surgery
The MCWPO is indicated in patients with a Wiberg type III or IV patella who have abnormal patellofemoral tracking post-trochleoplasty due to incongruence of the 2 articulating surfaces. The patellar osteotomy is contraindicated in cases of small patella or adequate patellofemoral tracking.
Preoperative Planning
The preoperative planning is the same as used for all patients with OPI, which includes appropriate plan radiographs and slice imaging.12 The standard radiographic views include an anteroposterior and true lateral of the knee, along with a skyline view at 30° of flexion.
Radiographs should be combined with slice imaging (computed tomography scan or magnetic resonance imaging) to determine the trochlear and patellar articular shape. The lateral radiograph and axial slice images allows the trochlear shape to be classified as per the Dejour classification.13 Patellar shape is then classified according to Wiberg and Baumgartl, allowing the physician to suspect cases in which a patellar osteotomy might be useful to improve patellar tracking.7,8
A sulcus deepening trochleoplasty is indicated at our institution in patients with OPI and high-grade trochlear dysplasia (Dejour type B or D) with a supratrochlear spur greater than 5 mm.12 A patellar osteotomy is then anticipated in trochleoplasties with high grade patellar dysplasia (type III and IV).11
The axial distance between the anterior tibial tubercle and the trochlear sulcus (tibial tuberosity-trochlear groove), along with the patellar height (Caton–Deschamps index) are also assessed to determine the need for adding additional procedures based on “menu à la carte” guidelines of the Lyon School of Knee Surgery.13
Step 1. Position and Examination Under Anesthesia
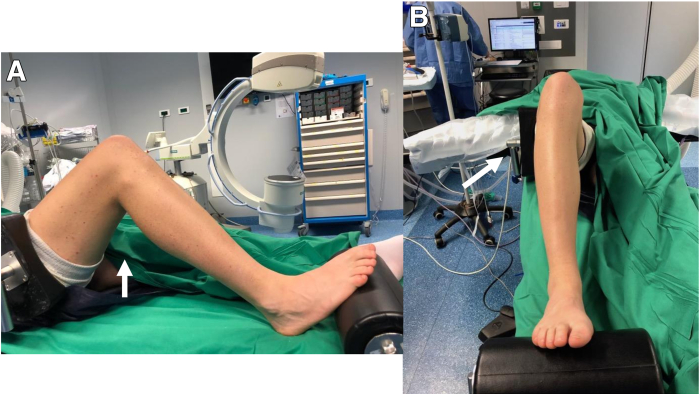
The patient is placed in the supine position under general or regional anesthesia (Video 1, Table 1). A padded tourniquet is placed proximally on the operative thigh. The affected knee is positioned at 90° of flexion with the contralateral limb in extension (Fig 1). Two supports, lateral and distal, are used to keep the knee in flexion. The lower extremity is prepped and draped in a sterile manner.
Table 1.
Step-by-Step Details of the Technique
| Step 1. Position |
|
| Step 2. Surgical approach and examination under anesthesia |
|
| Step 3. The osteotomy |
|
| Step 4. Fixation and closure |
|
MCWPO, medial closing-wedge patellar osteotomy; PF, patellofemoral.
Fig 1.
Patient position. The patient is placed in a supine position on the operating table. Two supports, lateral and distal, are used to keep the right knee in flexion. A high thigh tourniquet is placed to optimize the knee exposure during surgery. The knee is positioned at 90° of flexion.
Step 2. Surgical Approach
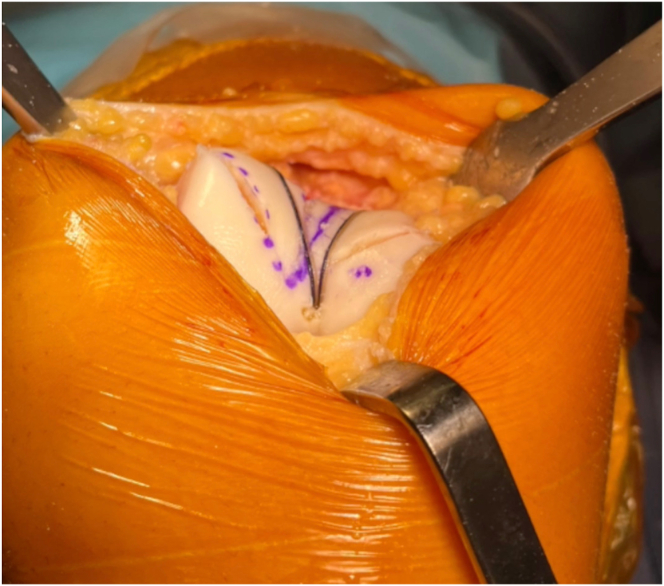
Beginning 5 cm proximal to the upper patellar pole, a 10-cm linear incision is made. A medial parapatellar approach is performed to expose the articular surface of the trochlea and patella. After performing the sulcus deepening trochleoplasty (Fig 2), the patellofemoral tracking and the congruence between the 2 articulating surfaces is evaluated. The MCWPO is then performed if there is persistence of PF maltracking due to incongruence between the newly shaped trochlea and patella.
Fig 2.
The sulcus deepening trochleoplasty is performed first.
Step 3. The Osteotomy
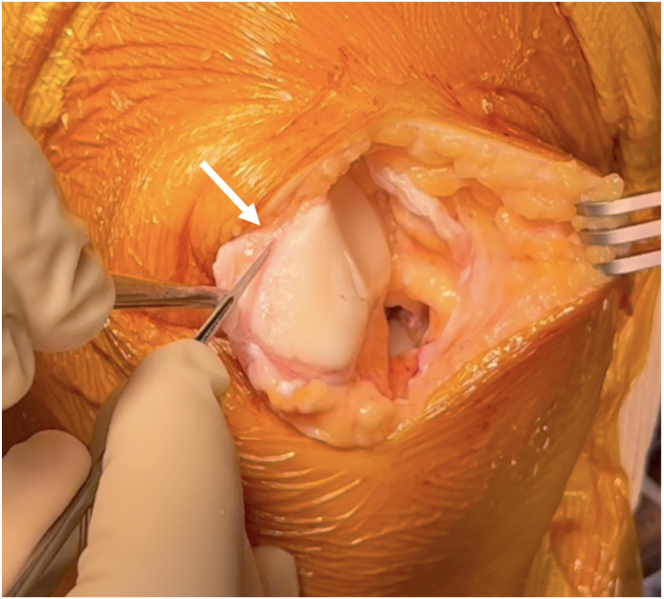
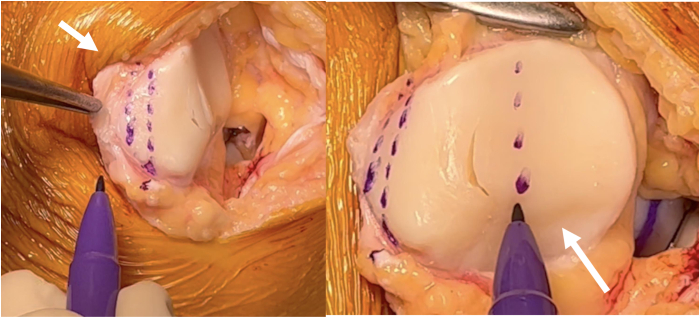
The medial patellar edge is completely exposed by releasing any remaining soft tissue (Fig 3). The osteotomy is then planned with a sterile marking pen (Fig 4). Two dashed lines are drawn on the medial edge of the patella to set the thickness of the bone wedge to be removed. Another dashed line is drawn on the articular surface indicating the desired articular ridge; this is also the medial to lateral depth of the osteotomy. With an oscillating saw the first osteotomy is performed at least 5 mm anterior and parallel to the articular surface to avoid any damages to the cartilage (Fig 5). A second, more anterior osteotomy, converging medially with the first cut at the level of the planned new articular ridge, is then made: the tip of the wedge should end at the midline of the patella. This cortical wedge of bone is then removed, and the osteotomy is closed with a grasper (Figs 6 and 7).
Fig 3.
Medial patellar soft-tissue release is performed to expose the cortical bone.
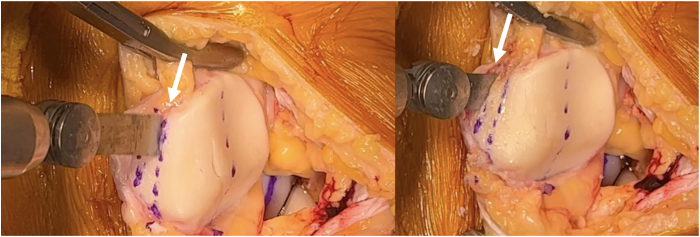
Fig 4.
A sterile marking pen is used to draw 2 dashed lines to set the thickness of the bone wedge to be removed (left). Another dashed line is drawn on the articular surface indicating the desired articular ridge (right).
Fig 5.
With an oscillating saw the first osteotomy is performed at least 5 mm anterior and parallel to the articular surface to avoid any damages to the cartilage (left). A second, more anterior osteotomy, converging medially with the first cut at the level of the planned new articular ridge is then made (right).
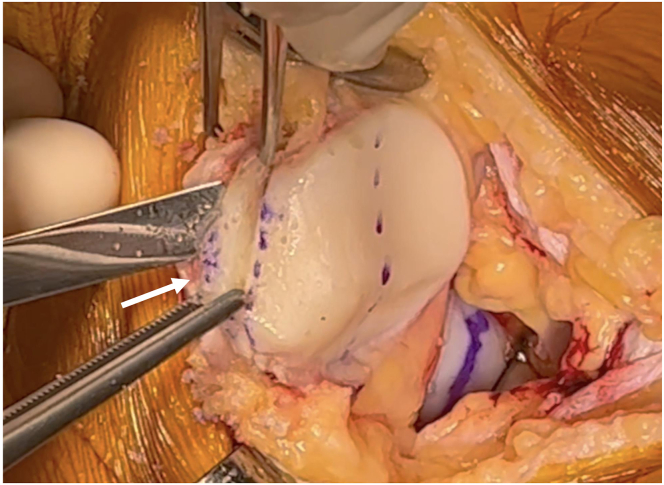
Fig 6.
The cortical wedge of bone is removed.
Fig 7.
The osteotomy is closed with a grasper.
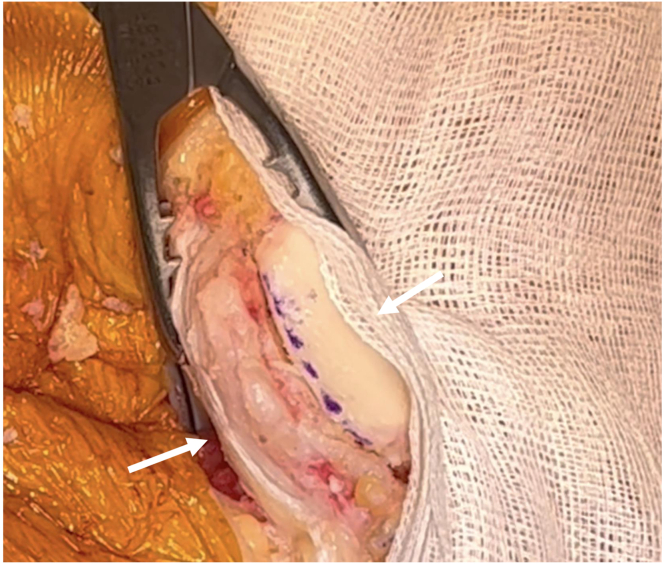
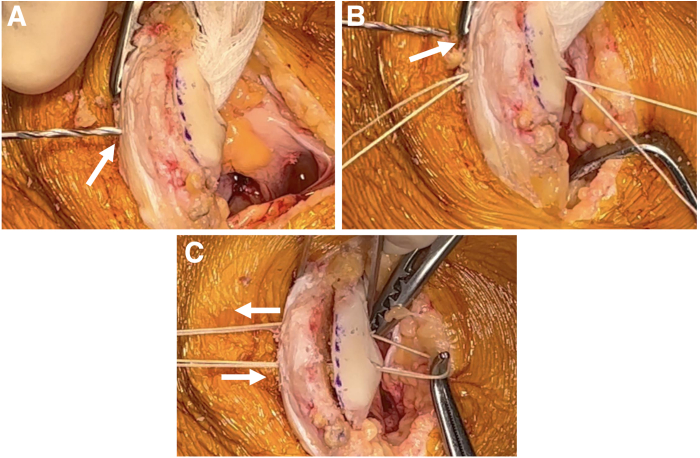
Step 4. Fixation and Closure
A 1.7-mm drill is used to create 2 anterior-to-posterior transosseous holes through the patella, slightly lateral to the medial patellar edge. Two no. 2 VICRYL sutures (Ethicon, Somerville, NJ) are driven from anterior to posterior through the first hole and then with an opposite direction through the second hole (Fig 8). A knot is then carried out on the anterior patellar bone surface using the 4 ends of the suture (Fig 9). The improved patellofemoral tracking is then confirmed by taking the knee through a range of motion.
Fig 8.
A 1.7-mm drill is used to create 2 anterior-to-posterior transosseous holes through the patella, slightly lateral to the medial patellar edge (A-B). Two no. 2 VICRYL sutures (Ethicon, Somerville, NJ) are driven from anterior to posterior through the first hole and then with an opposite direction through the second hole (B-C).
Fig 9.
A knot is then carried out on the anterior patellar bone surface using the 4 ends of the suture
The medial patellofemoral ligament reconstruction is then added at the end of the operation using a patellar soft-tissue fixation. The tourniquet is then released, hemostasis is confirmed, and a layered closure is performed.
Postoperative Rehabilitation
The postoperative protocol for patellar medial closing-wedge osteotomy is the same used for sulcus-deepening trochleoplasty. Physical therapy begins the day after surgery. The patient is allowed to bear weight as tolerated using crutches. Early muscle activation with isometric strengthening exercises and passive knee flexion from 0 to 90° is encouraged immediately. This applies compression to the patellar and trochlear osteomized bone, helping to promote healing of the osteotomized bone and re-model the articulating surfaces. At day 45 postoperatively, the patient is allowed to start closed kinetic chain strengthening exercises (e.g., cycling). At 3 months, light jogging may be performed. Full activity and return to sport are delayed until 6 months after surgery.
Discussion
Osteotomy of the patella is an unusual procedure that has been described previously to mainly address patellofemoral pain, not instability.14, 15, 16, 17 In cases of a highly dysplastic patella when an isolated sulcus-deepening trochleoplasty does not result in a congruent patellofemoral joint intraoperatively, a patellar osteotomy may be required. Nevertheless, patellar osteotomy for treating patients with OPI is uncommon, and only a few authors consider it in association with a trochleoplasty.
Albee18 proposed a dorsal closing-wedge patellar osteotomy associated with an opening-wedge lateral femoral distal osteotomy. However, this procedure has fallen out of favor, as the lateral facet elevation resulted in elevated patellofemoral pressures and caused residual pain.19
Koch et al.20 presented 2 cases of a dorsal closing-wedge patellar osteotomy in association with a Bereiter’s trochleoplasty. The osteotomy was fixed with 2 metallic screws from lateral to medial. They reported no complications with excellent patient satisfaction and patellofemoral congruence.
Morscher, described an opening-wedge patellar osteotomy, adding a wedge of bone graft dorsally to improve patellofemoral congruence and redistribute pressures. It has not been described in combination with trochleoplasty in human studies, and worse results were reported when combined with a tibial tubercle osteotomy.21
Choufani et al.22 published a case report of a lateral closing-wedge patellar osteotomy in a patient with OPI fixed with nonabsorbable transosseous sutures. After 12 months, no pain or instability recurrence was reported, with excellent improvements to patient-reported outcome scores. Larger series have not been published.
Compared with the aforementioned procedures, our technique offers some advantages (Table 2). The same surgical approach is used for sulcus deepening trochleoplasty and MCWPO. Using the same approach preserves the anterior nutrient foramina and does not compromise the principal blood supply to this sesamoid bone, reducing concern for avascular necrosis. Also, this osteotomy technique allows the patellar articular surface to be reshaped achieving a wider medial facet than before mentioned techniques. A wider osteotomy leads to a larger contact area, which can improve bone healing and reduce complications.
Table 2.
Advantages and Disadvantages of the Medial Patellar Closing-Wedge Osteotomy
| Advantages |
|
| Disadvantages |
|
Finally, the improved congruence of the patellofemoral joint allows adequate contact pressure at the osteotomy site to be stable when combined with a simple transosseous absorbable suture. This removes the need for any expensive or nonabsorbable fixation.
Although complications such as fracture and avascular necrosis are possible, none were reported in a MCWPO series of 21 cases with an average follow-up of 35 months. In this series, good clinical results with no further patellar dislocation were reported.11
In conclusion, the MCWPO associated with sulcus deepening trochleoplasty is a reproducible technique with promising clinical outcomes. Nevertheless, the indication should be restricted to patients with unsatisfactory intraoperative patellofemoral tracking after trochleoplasty.
Disclosure
The authors report the following potential conflicts of interest or sources of funding: D.H.D. reports royalties from Arthrex. All other authors (T.P., A.G., M.J.D., E.G.d.S.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Medial patellar closing-wedge osteotomy in patellofemoral instability. Sedation and regional anesthesia with the patient placed in a supine position with 2 supports (lateral and distal) on the right knee. A 10-cm midline skin incision is used. After performing the sulcus deepening trochleoplasty patellofemoral tracking is tested. In case of persistence of maltracking the MCWPO is performed. A sterile marking pen is used to draw 2 medial dashed lines to set the thickness of the osteotomy. A third dashed line is drawn at the midline of the patella. With an oscillating saw, 2 osteotomies converging medially are performed and the cortical wedge of bone is removed. The osteotomy is closed with a grasper. A 1.7-mm drill is used to create two anterior to posterior transosseous holes. Two sutures no. 2 VICRYL (Ethicon, Somerville, NJ) are driven from anterior to posterior through the first hole and then with an opposite direction through the second hole. A knot is then carried out on the anterior patellar bone surface using the 4 ends of the suture. The new patellofemoral tracking is tested.
References
- 1.Dejour H., Walch G., Nove-Josserand L., Guier C. Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 2.Ntagiopoulos P.G., Byn P., Dejour D. Midterm results of comprehensive surgical reconstruction including sulcus-deepening trochleoplasty in recurrent patellar dislocations with high-grade trochlear dysplasia. Am J Sports Med. 2013;41:998–1004. doi: 10.1177/0363546513482302. [DOI] [PubMed] [Google Scholar]
- 3.Clark D., Stevens J.M., Tortonese D., Whitehouse M.R., Simpson D., Eldridge J. Mapping the contact area of the patellofemoral joint: The relationship between stability and joint congruence. Bone Joint J. 2019;101-B:552–558. doi: 10.1302/0301-620X.101B5.BJJ-2018-1246.R1. [DOI] [PubMed] [Google Scholar]
- 4.Panni A.S., Cerciello S., Maffulli N., Di Cesare M., Servien E., Neyret P. Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc. 2011;19:663–670. doi: 10.1007/s00167-010-1329-4. [DOI] [PubMed] [Google Scholar]
- 5.Fucentese S.F., von Roll A., Koch P.P., Epari D.R., Fuchs B., Schottle P.B. The patella morphology in trochlear dysplasia—a comparative MRI study. Knee. 2006;13:145–150. doi: 10.1016/j.knee.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Barnett A.J., Gardner R.O., Lankester B.J., Wakeley C.J., Eldridge J.D. Magnetic resonance imaging of the patella: A comparison of the morphology of the patella in normal and dysplastic knees. J Bone Joint Surg Br. 2007;89:761–765. doi: 10.1302/0301-620X.89B6.18995. [DOI] [PubMed] [Google Scholar]
- 7.Wibeeg G. Roentgenographs and anatomic studies on the femoropatellar joint: With special reference to chondromalacia patellae. Acta Orthop Scand. 1941;12:319–410. [Google Scholar]
- 8.Baumgartl F. Anatomical and clinical importance of the femoropatellar joint. Zentralbl Chir. 1966;91:506–516. [in German] [PubMed] [Google Scholar]
- 9.Giovannetti de Sanctis E., Guarino A., Pineda T., Demey G., Dejour D.H. The femoral sulcus deepening trochleoplasty of Lyon. Arthrosc Tech. 2023;12:e687–e695. doi: 10.1016/j.eats.2023.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dejour D., Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev. 2007;15:39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 11.Giovannetti de Sanctis E., Dejour D.H. Patellar medial closing-wedge osteotomy in patello-femoral instability: Indications and outcomes. J Orthop. 2022;32:156–159. doi: 10.1016/j.jor.2022.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giovannetti de Sanctis E., Mesnard G., Dejour D.H. Trochlear dysplasia: when and how to correct. Clin Sports Med. 2022;41:77–88. doi: 10.1016/j.csm.2021.09.001. [DOI] [PubMed] [Google Scholar]
- 13.Dejour D.H., Mesnard G., Giovannetti de Sanctis E. Updated treatment guidelines for patellar instability: "Un menu a la carte.". J Exp Orthop. 2021;8:109. doi: 10.1186/s40634-021-00430-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arnoldi C.C., Lemperg K., Linderholm H. Intraosseous hypertension and pain in the knee. J Bone Joint Surg Br. 1975;57:360–363. [PubMed] [Google Scholar]
- 15.Hejgaard N., Arnoldi C.C. Osteotomy of the patella in the patellofemoral pain syndrome. The significance of increased intraosseous pressure during sustained knee flexion. Int Orthop. 1984;8:189–194. doi: 10.1007/BF00269915. [DOI] [PubMed] [Google Scholar]
- 16.Vaquero J., Arriaza R. The patella thinning osteotomy. An experimental study of a new technique for reducing patellofemoral pressure. Int Orthop. 1992;16:372–376. doi: 10.1007/BF00189622. [DOI] [PubMed] [Google Scholar]
- 17.Deliss L. Coronal patellar osteotomy: Preliminary report of its use in chondromalacia patellae. Proc R Soc Med. 1977;70:257–259. doi: 10.1177/003591577707000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Albee F. Bone graft wedge in the treatment of habitual dislocation of the patella. Med Rec. 1915;88:257–259. [Google Scholar]
- 19.Badhe N.P., Forster I.W. Patellar osteotomy and Albee’s procedure for dysplastic patellar instability. Eur J Orthop Surg Traumatol. 2003;13:43–47. [Google Scholar]
- 20.Koch P.P., Fuchs B., Meyer D.C., Fucentese S.F. Closing wedge patellar osteotomy in combination with trochleoplasty. Acta Orthop Belg. 2011;77:116–121. [PubMed] [Google Scholar]
- 21.Pecina M., Ivkovic A., Hudetz D., Smoljanovic T., Jankovic S. Sagittal osteotomy of the patella after Morscher. Int Orthop. 2010;34:297–303. doi: 10.1007/s00264-009-0923-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choufani C., Barbier O., Versier G. Patellar lateral closing-wedge osteotomy in habitual patellar dislocation with severe dysplasia. Orthop Traumatol Surg Res. 2015;101:879–882. doi: 10.1016/j.otsr.2015.07.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Medial patellar closing-wedge osteotomy in patellofemoral instability. Sedation and regional anesthesia with the patient placed in a supine position with 2 supports (lateral and distal) on the right knee. A 10-cm midline skin incision is used. After performing the sulcus deepening trochleoplasty patellofemoral tracking is tested. In case of persistence of maltracking the MCWPO is performed. A sterile marking pen is used to draw 2 medial dashed lines to set the thickness of the osteotomy. A third dashed line is drawn at the midline of the patella. With an oscillating saw, 2 osteotomies converging medially are performed and the cortical wedge of bone is removed. The osteotomy is closed with a grasper. A 1.7-mm drill is used to create two anterior to posterior transosseous holes. Two sutures no. 2 VICRYL (Ethicon, Somerville, NJ) are driven from anterior to posterior through the first hole and then with an opposite direction through the second hole. A knot is then carried out on the anterior patellar bone surface using the 4 ends of the suture. The new patellofemoral tracking is tested.
Medial patellar closing-wedge osteotomy in patellofemoral instability. Sedation and regional anesthesia with the patient placed in a supine position with 2 supports (lateral and distal) on the right knee. A 10-cm midline skin incision is used. After performing the sulcus deepening trochleoplasty patellofemoral tracking is tested. In case of persistence of maltracking the MCWPO is performed. A sterile marking pen is used to draw 2 medial dashed lines to set the thickness of the osteotomy. A third dashed line is drawn at the midline of the patella. With an oscillating saw, 2 osteotomies converging medially are performed and the cortical wedge of bone is removed. The osteotomy is closed with a grasper. A 1.7-mm drill is used to create two anterior to posterior transosseous holes. Two sutures no. 2 VICRYL (Ethicon, Somerville, NJ) are driven from anterior to posterior through the first hole and then with an opposite direction through the second hole. A knot is then carried out on the anterior patellar bone surface using the 4 ends of the suture. The new patellofemoral tracking is tested.