Abstract
The use of bone marrow aspirate concentrate (BMAC) as a surgical augment to enhance biologic healing has been gaining popularity in a variety of sports medicine procedures. Due to its reliable availability from multiple sites, including the proximal tibia, proximal humerus, and anterior superior iliac spine, BMAC can be harvested at a location selected to be adjacent to the primary procedure. This Technical Note aims to highlight 3 different harvest sites for BMAC, allowing orthopaedic sports medicine surgeons to localize their harvest site based on the proximity of the planned procedure and ultimately increase efficiency.
Technique Video
In this Technical Note, we describe the surgical techniques for 3 common harvesting sites for bone marrow aspirate concentrate adjacent to the shoulder, hip, and knee as an adjunct to sports medicine procedures.
There has been increasing interest in the use of orthobiologic substances such as platelet-rich plasma (PRP) and bone marrow aspirate concentrate (BMAC) to augment surgical treatment and enhance biologic healing. BMAC and PRP both offer various benefits; however, BMAC may be associated with greater growth factor potential and anti-inflammatory properties.1,2 BMAC must be harvested at the time of surgery, and it is important to have reliable and easily accessible techniques to incorporate into the surgical workflow. The purpose of this Technical Note is to review BMAC-harvesting techniques and 3 common BMAC harvest sites that should be familiar to and accessible to orthopaedic sports medicine surgeons around the knee, shoulder, and hip (Video 1).
Surgical Technique (With Video Illustration)
General Principles of Harvesting
A number of harvest locations for BMAC have been described. Although the posterior superior iliac spine may yield one of the most cell-dense and proliferative harvests,3 access requires the patient being positioned in the lateral or prone position, which is not as common in routine sports medicine procedures. Although most studies demonstrate harvests from the ilium represent the gold standard, authors advocate for using locations local and adjacent to the primary joint, such as the proximal tibia for knee procedures, the proximal humerus for shoulder procedures, and anterior superior iliac spine (ASIS) for hip procedures, as there is still excellent yield of proliferative cells and colony-forming units,4,5 and it improves surgical efficiency.6
Regardless of the location used, the same general principles for harvest apply. In the authors’ surgical workflow, the BMAC harvest is performed at the beginning of the surgical case after sterile preparation and draping. Doing the harvest early in the procedure produces a time-efficient system in which the majority of the surgical procedure may be performed during the time for the processing portion of the BMAC preparation.
The harvesting needle (Arthrex, Naples, FL) is preflushed with diluted heparin (500 U/mL) (Fig 1 A and B). The inner trocar (Arthrex) is placed within the harvesting needle. The trocar and needle are placed orthogonal to the bone at the site of harvest. A stab incision may be created within the skin if desired, or the needle may be punctured directly through the skin. While keeping the trocar and needle held firmly, a mallet is used to impact the needle approximately 3 cm past the near bony cortex. The needle should end within cancellous bone and care should be taken to not penetrate the far cortex.
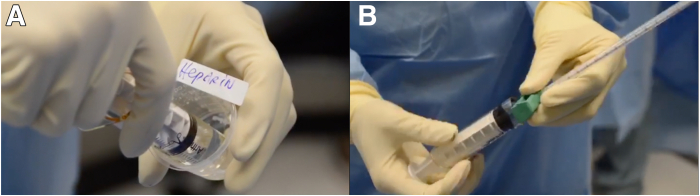
Fig 1.
Preflushing of harvesting trocar and needle with heparin. (A) Diluted heparin is drawn up into a syringe that is used to preflush the harvesting needle. (B) An outer sheath over the harvesting needle is used in order to thoroughly flush the needle with the diluted heparin solution. Equipment: Arthrex.
The inner trocar is then removed while the needle is held in place. The authors suggest a total aspiration volume of approximately 60 mL for each site and application, if possible. A 30-mL syringe preflushed with anticoagulant dextrose with or without heparin (Fig 2A) is applied to the end of the harvesting needle. Full suction is applied to the syringe (Fig 2B). An aspiration is performed until the 30 mL is filled with bone marrow aspirate. Five to 10 mL of aspirate, the authors rotate the harvesting needle 90° to break up more trabeculae to allow for greater access to marrow contents; in addition, while rotating, the needle is slightly withdrawn to expose the fenestrated tip to fresh trabeculae.
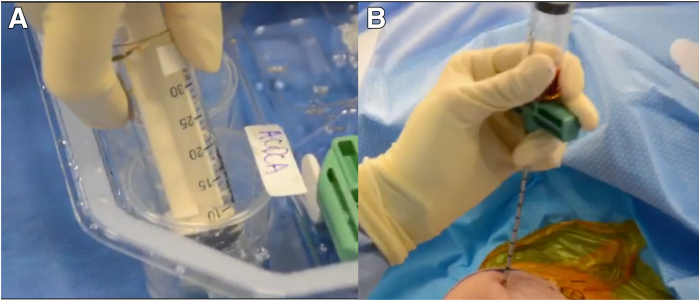
Fig 2.
Preparation and application of syringes to the harvesting needle. (A) The 30-mL syringes that are used for harvesting are preflushed with anticoagulant dextrose. (B) Once attached to the harvesting needle, full suction is applied to the syringe to efficiently aspirate bone marrow. Equipment: Arthrex.
Once the first 30-mL syringe is filled, the syringe is disconnected, and the second 30-mL syringe is applied, and aspirate is withdrawn in a similar manner. If there is difficulty obtaining bone marrow contents even with twisting the needle, the trocar may be reinserted and the needle redirected to obtain aspirate from a new location. Once 60 mL is obtained, the inner trocar is removed, and the needle is withdrawn manually. The filled syringes are handed off from the sterile field and sent to the processing system thereafter (Angel cPRP and Bone Marrow Processing System; Arthrex). The harvest incision, if not incorporated into another incision or portal, may be closed by applying an adhesive, sterile strip bandage.
The selected harvest site may vary based on the surgical procedure performed. The authors review the harvest sites of the proximal tibia, proximal humerus, and ASIS for ease of access for knee-, shoulder-, and hip-related arthroscopic and sports medicine procedures, respectively. These sites facilitate BMAC harvest and collection by using sites easily accessible with standard patient positioning and draping due to their proximity to the most common sports medicine procedure surgical sites.
Harvest Site: Proximal Tibia—for Knee-Related Procedures
A proximal tibial BMAC harvest is useful for arthroscopic and open knee procedures. The tibial crest, posteromedial tibia, and tibial tubercle border are palpated. The needle entry location is at a location halfway between the tibial crest and posteromedial tibial border, at the level of or 1 cm proximal to the tibial tubercle (Fig 3A). The needle is inserted angling in a direction aimed toward the fibular head (Fig 3B) (Video 1).
Fig 3.
Proximal tibia BMAC harvest. (A) The patient is in the supine position with the right leg in a leg holder. The right proximal tibia is being used as a BMAC harvest site. The border of the tibial tubercle as well as the posteromedial tibial border are palpated and marked. (B) The harvesting needle is inserted aimed towards the fibular head. (BMAC, bone marrow aspirate concentrate.)
The tourniquet should not be inflated during the harvest. If proximal tibial harvest yields insufficient volume or if there are bone tunnels from previous surgeries around the knee, a harvest also may be performed through an intra-articular approach via the femoral intercondylar notch nearby.7 Gerdy’s tubercle may also be used.
Harvest Site: Proximal Humerus—for Shoulder-Related Procedures
The lateral acromial border is palpated, including its anterior and posterior aspects. The needle entry point is typically just anterior to the halfway point between the anterior and posterior acromion, at a location 3 cm distal to the lateral acromial border (Fig 4A). The needle should be aimed inferiorly, medially, and anteriorly (Fig 4B) (Video 1). Care should be taken to feel bone with the needle before puncturing skin, ensuring that the mallet is used only to direct the needle directly into bone. Alternative sites may be used for harvest depending on surgeon preference for portal placement, such as via an anterolateral approach (Fig 4C). If the harvest location is too distal, there is danger of injuring the axillary nerve (which runs 5-7 cm distal to the lateral border of the acromion from posterior to anterior).
Fig 4.
Proximal humerus BMAC harvest. (A) The patient is in the beach-chair position and the right proximal humerus is being used as a BMAC harvest site. The lateral acromial border is palpated and marked, and then a small stab incision is made approximately 3 cm distal to this halfway between the anterior and posterior acromial borders. This is at the location of the commonly used direct lateral shoulder arthroscopic portal. (B) The harvesting needle should be aimed inferiorly, medially, and anteriorly to ensure correct positioning for insertion into bone and proper harvest. (C) An anterolateral approach can also be utilized to harvest BMAC successfully and safely from the proximal humerus. (BMAC, bone marrow aspirate concentrate.)
Harvest Site: Anterior Superior Iliac Spine—for Hip-Related Procedures
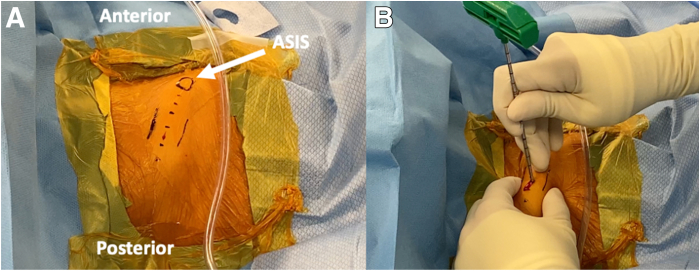
Although the posterior superior iliac spine also may be used around the hip,8 the authors tend to use the ASIS, as patients are more commonly positioned supine. The ASIS is palpated, in addition to the inner and outer tables of the pelvis. From the tip of the ASIS, the harvest site is typically 3 cm proximal (Fig 5A). The authors use a stab incision for this location before placing the needle.
Fig 5.
Anterior superior iliac spine BMAC harvest. (A) The patient is in the supine position and the right ASIS is being used as a BMAC harvest site. The ASIS, inner table, and outer table of the pelvis are identified and marked out in preparation of the stab incision for harvest. (B) The harvesting needle is inserted in between the markings of the inner and outer table of the pelvis approximately 3 cm proximal to the ASIS, taking care to remain within the iliac crest. The needle may also be reinserted for the second syringe harvest through the same skin stab incision by translating the skin proximally, or the needle may be rotated and advanced farther to break into deeper trabeculae. (ASIS, anterior superior iliac spine; BMAC, bone marrow aspirate concentrate.)
The needle is inserted between the inner and outer tables of the pelvis, and when impacting the needle, care should be taken to remain within the iliac crest and not penetrate through the inner table in particular (Fig 5B).
Once the first 30-mL syringe is filled, the authors remove the entire needle with trocar. The skin may then be moved proximally, and the needle re-entered through the same skin penetration site, but in a different bone entry site proximally9 (Video 1). Alternatively, the needle may be maintained in the same bone entry site, rotated, and advanced farther to break into deeper trabeculae. The second 30-mL syringe is then filled in the standard fashion. If advancing the needle farther into the crest, care should be taken to not go too deep as the bone continues to thin. In addition to its utility for hip-adjacent procedures due to ease of access, the ilium also may be used as a harvest site in cases when the highest cell quantity and proliferative quality is desired (eg, older patients).
Processing Postharvest
Once ultimately obtained, the bone marrow aspirate is prepared and centrifuged using a standard commercially available BMAC centrifuge system (Angel cPRP and Bone Marrow Processing System; Arthrex), at the 7% setting typically yielding up to 2 to 5 mL of concentrate. The automated centrifuge system rapidly concentrates cellular contents and growth factors in bone marrow aspirate.
BMAC Application
Once processed, the concentrate is transferred in a sterile fashion back to the surgical field and placed into a sterile syringe. The BMAC is applied or injected directly into the surgical field or tissue of choice.
Pearls and pitfalls of harvesting BMAC are summarized in Table 1. Advantages and disadvantages are summarized in Table 2.
Table 1.
Pearls and Pitfalls of BMAC Harvesting and Delivery
| Pearls |
|
|
|
|
|
|
| Pitfalls |
|
|
|
ASIS, anterior superior iliac spine; BMAC, bone marrow aspirate concentrate.
Table 2.
Advantages and Disadvantages of BMAC Harvest from the Proximal Tibia, Proximal Humerus, and Anterior Superior Iliac Spine
| Advantages |
|
|
|
|
|
|
|
|
| Disadvantages |
|
|
|
|
|
ASIS, anterior superior iliac spine; BMAC, bone marrow aspirate concentrate.
Discussion
The described techniques for harvesting BMAC in the operating room are useful for the sports medicine surgeon, given their proximity to the joints on which these surgeons frequently operate (ie, knee, shoulder, and hip). Furthermore, the authors advocate for these harvest sites for simplicity in surgical draping and positioning, requiring minimal changes to standard surgical setup and preparation. For those performing procedures around the elbow and ankle, the harvest sites of the proximal humerus and proximal tibia may still be used, respectively, with ease of access in the already draped operative limb.
In addition to ease of positioning and access, advantages of the proposed techniques include quick harvest time with minimal impact to the overall surgical workflow. By harvesting BMAC at the beginning of the operative case, processing can occur simultaneously to the procedure. Furthermore, the incision sites proposed are familiar and can be placed to be incorporated into other incisions or can be placed with safe distance from more invasive, open incisions. The small stab incisions for harvest typically heal well and do not require additional time for closure. In contrast, not all cases may be optimal for harvest from the suggested sites. Data demonstrate that BMAC derived from both iliac crest and proximal tibia may have similar chondrogenic and osteogenic capacity, but BMAC from the iliac crest may produce greater mononucleated cells relative to the proximal tibia.4 Furthermore, in older patients, the mononucleated cell number is significantly lower; therefore, surgeons may consider in older patients using iliac crest as the site of harvest to maximize the mononucleated cell count, regardless of the primary procedure site, especially since harvest from the anterior iliac crest has been shown to have similar quality regardless of demographic factors such as age, sex, and body mass index.4,10 It is important to note that incorporating BMAC requires preplanning, with a preoperative informed consent discussion with the patient. Currently in many health systems, the harvest and application of BMAC is not covered by routine health insurance, thereby often resulting in out-of-pocket costs to patients. The authors advocate for honest, open conversations about potential costs as a part of the risk versus benefit discussion of adding BMAC to a procedure.
Promising results of BMAC augmentation have been seen in a variety of sports medicine–related procedures. For the knee, BMAC in the setting of allograft bone–patellar tendon–bone anterior cruciate ligament reconstruction may enhance the ligamentization of the allograft.11 BMAC is being heavily studied in osteochondral allografts and may enhance incorporation of the graft as seen on imaging.12 In the shoulder, randomized trial data exist suggesting those having rotator cuff repairs augmented with BMAC have lower retear rates on magnetic resonance imaging at 1-year postoperatively.13 For the hip, those with symptomatic labral tears with early degenerative radiographic changes may perform similarly to those without arthritis, if they have intra-articular injection of iliac-crest derived BMAC.14 Furthermore, those with full-thickness acetabular chondral flaps have better outcome scores after treatment with BMAC as opposed to microfracture.15 Many other applications of BMAC exist and are undergoing ongoing investigation.
Although ongoing data and research will clarify the optimal uses of BMAC, having the skillset to harvest and apply BMAC to various tendon, ligament, and cartilage/joint pathologies is useful to optimize healing and outcomes.
Disclosure
The authors report the following potential conflicts of interest or sources of funding: J.C. reports board member/owner/officer/committee appointments: American Orthopaedic Society for Sports Medicine, Arthroscopy Association of North America, and International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine; and paid consultant or employee: Arthrex and Smith & Nephew. N.N.V. reports board member/owner/officer/committee appointments: American Orthopaedic Society for Sports Medicine, Arthroscopy Association of North America, and American Shoulder and Elbow Surgeons; royalties from Smith & Nephew; paid consultant or employee for Arthrex, Smith & Nephew, and Stryker; research or institutional support from SLACK Inc; and research or institutional support from (data generated from such studies must be unrestricted) Breg, Ossur, Smith & Nephew, and Stryker. B.J.C. reports board member/owner/officer/committee appointments: Arthroscopy Association of North America, American Journal of Sports Medicine, and Journal of the American Academy of Orthopaedic Surgeons; research or institutional support from Elsevier Publishing and Operative Techniques in Sports Medicine; research or institutional support (data generated from such studies must be unrestricted) from Aesculap/B. Braun, Arthrex, JRF Ortho; and stock or stock options from BandGrip and Ossio. All other authors (S.A., H.J., Z.A.K., C.M.B.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Footnotes
Institution where the work was performed: Rush University Medical Center, Chicago, Illinois, U.S.A.
Supplementary Data
In this Technical Note, we describe the surgical techniques for 3 common harvesting sites for bone marrow aspirate concentrate adjacent to the shoulder, hip, and knee as an adjunct to sports medicine procedures.
References
- 1.Sugaya H., Yoshioka T., Kato T., et al. Comparative analysis of cellular and growth factor composition in bone marrow aspirate concentrate and platelet-rich plasma. Bone Marrow Res. 2018;2018:1–9. doi: 10.1155/2018/1549826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ziegler C.G., Van Sloun R., Gonzalez S., et al. Characterization of growth factors, cytokines, and chemokines in bone marrow concentrate and platelet-rich plasma: A prospective analysis. Am J Sports Med. 2019;47:2174–2187. doi: 10.1177/0363546519832003. [DOI] [PubMed] [Google Scholar]
- 3.Anz A., Sherman B. Concentrated bone marrow aspirate is more cellular and proliferative when harvested from the posterior superior iliac spine than the proximal humerus. Arthroscopy. 2022;38:1110–1114. doi: 10.1016/j.arthro.2021.10.011. [DOI] [PubMed] [Google Scholar]
- 4.Cavallo C., Boffa A., De Girolamo L., et al. Bone marrow aspirate concentrate quality is affected by age and harvest site. Knee Surg Sports Traumatol Arthrosc. 2023;31:2140–2151. doi: 10.1007/s00167-022-07153-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hyer C.F., Berlet G.C., Bussewitz B.W., Hankins T., Ziegler H.L., Philbin T.M. Quantitative assessment of the yield of osteoblastic connective tissue progenitors in bone marrow aspirate from the iliac crest, tibia, and calcaneus. J Bone Joint Surg Am. 2013;95:1312–1316. doi: 10.2106/JBJS.L.01529. [DOI] [PubMed] [Google Scholar]
- 6.LaPrade R.F., Murray I.R. Editorial Commentary: Bone marrow aspirate concentrate: Time to harvest locally? Arthroscopy. 2020;36:2412–2414. doi: 10.1016/j.arthro.2020.07.015. [DOI] [PubMed] [Google Scholar]
- 7.Youn G.M., Woodall B.M., Elena N., et al. Arthroscopic bone marrow aspirate concentrate harvesting from the intercondylar notch of the knee. Arthrosc Tech. 2018;7:e1173–e1176. doi: 10.1016/j.eats.2018.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chahla J., Mannava S., Cinque M.E., Geeslin A.G., Codina D., LaPrade R.F. Bone marrow aspirate concentrate harvesting and processing technique. Arthrosc Tech. 2017;6:e441–e445. doi: 10.1016/j.eats.2016.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piuzzi N.S., Mantripragada V.P., Sumski A., Selvam S., Boehm C., Muschler G.F. Bone marrow-derived cellular therapies in orthopaedics: Part I: Recommendations for bone marrow aspiration technique and safety. JBJS Rev. 2018;6:e4. doi: 10.2106/JBJS.RVW.18.00007. [DOI] [PubMed] [Google Scholar]
- 10.Huddleston H.P., Tauro T., Credille K., et al. Patient demographic factors are not associated with mesenchymal stromal cell concentration in bone marrow aspirate concentrate. Arthrosc Sports Med Rehabil. 2023;5:e559–e567. doi: 10.1016/j.asmr.2023.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Forsythe B., Chahla J., Korrapati A., et al. Bone marrow aspirate concentrate augmentation may accelerate allograft ligamentization in anterior cruciate ligament reconstruction: A double-blinded randomized controlled trial. Arthroscopy. 2022;38:2255–2264. doi: 10.1016/j.arthro.2022.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Oladeji L.O., Stannard J.P., Cook C.R., et al. Effects of autogenous bone marrow aspirate concentrate on radiographic integration of femoral condylar osteochondral allografts. Am J Sports Med. 2017;45:2797–2803. doi: 10.1177/0363546517715725. [DOI] [PubMed] [Google Scholar]
- 13.Cole B.J., Kaiser J.T., Wagner K.R., et al. Prospective randomized trial of biologic augmentation with bone marrow aspirate concentrate in patients undergoing arthroscopic rotator cuff repair. Am J Sports Med. 2023;51:1234–1242. doi: 10.1177/03635465231154601. [DOI] [PubMed] [Google Scholar]
- 14.Day M.A., Hancock K.J., Selley R.S., et al. Hip arthroscopy with bone marrow aspirate injection for patients with symptomatic labral tears and early degenerative changes shows similar improvement compared with patients undergoing hip arthroscopy with symptomatic labral tears without arthritis. Arthroscopy. 2023;39:1429–1437. doi: 10.1016/j.arthro.2022.12.012. [DOI] [PubMed] [Google Scholar]
- 15.Kucharik M.P., Abraham P.F., Nazal M.R., et al. Treatment of full-thickness acetabular chondral flaps during hip arthroscopy: bone marrow aspirate concentrate versus microfracture. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211059170. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
In this Technical Note, we describe the surgical techniques for 3 common harvesting sites for bone marrow aspirate concentrate adjacent to the shoulder, hip, and knee as an adjunct to sports medicine procedures.
In this Technical Note, we describe the surgical techniques for 3 common harvesting sites for bone marrow aspirate concentrate adjacent to the shoulder, hip, and knee as an adjunct to sports medicine procedures.