Abstract
Anterior cruciate ligament reconstructions are often performed with associated procedures, most commonly for associated meniscal tears. The lateral meniscal root tear is a commonly associated injury, which increases rotational instability and results in altered tibiofemoral biomechanics. Lateral meniscectomy results in poorer functional and long-term outcomes, making repair vital. The position of the lateral root tear makes its repair technique complicated. Because of the proximity to vessels posteriorly, the all-inside technique is considered potentially unsafe, and current transtibial repair techniques fail to appose the body with the root remnant. In the lineage of Laprade, who proclaimed the use of a transtibial suture for radial tears elsewhere in the knee in order to reduce the shear force, we describe a transtibial technique that optimizes meniscal apposition, theoretically improving the repair biomechanics and is technically easier to perform in comparison to suture hook techniques with one tunnel and one suture.
Technique Video
The Double Compressive Knot
Lateral meniscal root tears are commonly seen in conjunction with anterior cruciate ligament (ACL) tears, with an incidence of up to 12%.1 Lateral meniscus root tears increase rotational instability2 and lead to altered tibiofemoral contact pressures with decreased contact area by 32% and increased peak pressures in the lateral compartment by 49%,3 resulting in an increased incidence of osteoarthritis and a shortened athletic career.4
Therefore, there is a need to preserve the lateral meniscus.5 Side-to-side or pullout suture repair, the most common types of lateral meniscal root repairs. Side-to-side repairs involve either a suture hook, which is technically difficult, or an all-inside device, which is dangerous because of the proximity of the popliteal vascular structures and tibial nerve and relies on the thinner lateral joint capsule for fixation strength.6 Pullout suture repair involves a transtibial tunnel to pull the meniscal root back to the attachment site, and the suture is then fixed to the anterior tibia, commonly by a suture button. However, the pullout suture technique does not directly appose the torn remnant with the meniscal body and is typically reserved for root avulsions.1
Given that close to 80% of posterior horn lateral meniscal root tears extend more than 1 cm from the root attachment,1 we aimed to develop a suture technique that apposes the 2 torn ends of meniscal tissue and has the repair strength of a transtibial technique. This technique should also avoid passing an all-inside device through the posterior capsule in close proximity to the popliteal neurovascular structures.
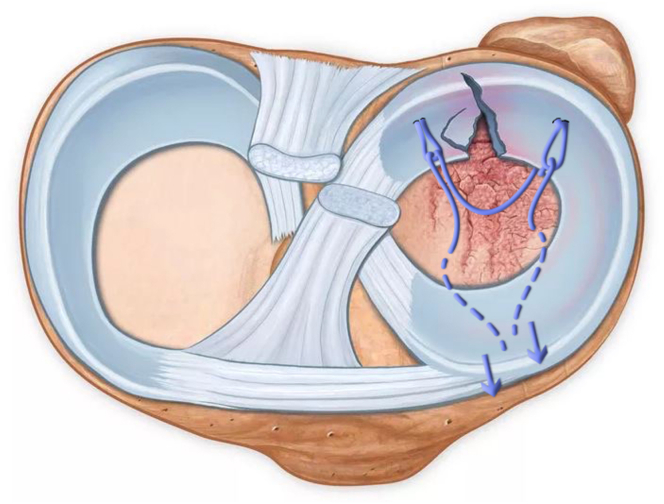
We describe a technique that involves using a meniscal suture passer device to place a horizontal mattress stitch with looped ends in each part of the torn meniscus to allow retensioning to appose the two torn meniscal ends before passing, and securing sutures through a separate transtibial tunnel (see Fig 1).
Fig 1.
Drawing of the double compression (DC) knot. Drawing of a left knee presenting a lateral meniscal root tear. DC knot, demonstrating the two cinched loops and the bridging thread (untensioned) of a single suture. The DC knot is designed to appose the torn meniscal ends and be tensioned via a transtibial tunnel.
Surgical Technique
Patients Positioning and Anesthesia
The procedure is performed with the patient supine on the table with the knee flexed at 80°. A high tourniquet is applied, and the patient undergoes a general anesthetic. An examination under anesthesia is performed to confirm the diagnosis of ACL rupture. The operative limb is then prepared and draped in a standard sterile fashion.
Surgical Sequence
-
1.
Graft harvest
-
2.
Diagnostic arthroscopy, including identification of meniscal tear and freshening up of torn meniscal edges.
-
3.
ACL tunnel preparation
-
4.
Meniscal repair
-
5.
ACL graft passage and fixation
-
6.
Tie the meniscal suture over an Endobutton
-
7.
Wound closure
After graft harvest, standard anterolateral portal was established, 5 mm laterally to the patellar tendon, on the corner between patella and patellar tendon. The anteromedial portal was then established, under view control, in the same level as the anterolateral one and 1.5 cm medial to the patellar tendon.
An arthroscopic exploration is then performed, showing the lateral meniscal injury.
Meniscal Repair (Video 1)
Materials Needed
The entire repair is performed using a meniscal suture passer.
The following tools are needed:
-
-
ACL reconstruction tibial guide with a 40-45° angle
-
-
1.5-mm K-wire
-
-
4.5-mm drill
-
-
One nonabsorbable suture (no 2. UltraBraid; Smith and Nephew, London, UK)
-
-
One nonabsorbable Endobutton (Smith and Nephew, London, UK)
-
-
One meniscal suture passer (First Pass or Mini-Pass, Smith and Nephew, London, UK)
Step 1: Transtibial Tunnel
The first step of the procedure is to prepare the location of the exit point on the tibial plateau for the transtibial tunnel (Fig 2). Our preference is to use an elbow ACL reconstruction tibial guide, with a 40° to 45° angle, through the AM portal. The location of the fixation is chosen in accordance with the anatomical morphology of the lateral meniscus, between the meniscal tear, adjacent the lateral border of meniscal root remnant.
Fig 2.
Transtibial tunnel for lateral meniscal root tear repair, on a right knee sawbone model. Transtibial tunnel is performed using an elbow guide, at a 40-45° angle. The location of the articular tunnel aperture aims to restore the anatomical morphology of the lateral meniscus, by being between the two edges of the meniscal tear, adjacent to the lateral border of the meniscal root remnant.
A skin incision of 1 cm is made on the anterior lateral tibial border, 2 cm proximal, and lateral to the tibial ACL tunnel to avoid tunnel convergence.
A K-wire is then put in place using the guide. The exit point on the tibial plateau is confirmed arthroscopically before the tibial tunnel is drilled using the 4.5-mm cannulated drill.
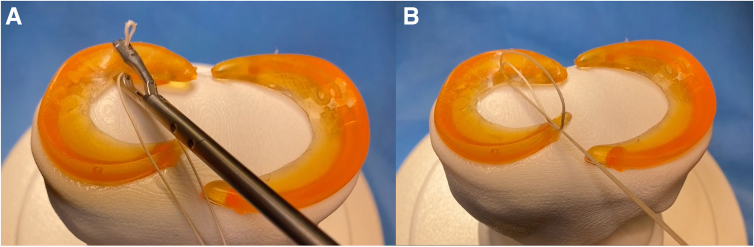
Step 2: First Loop
The suture thread (UltraBraid; Smith and Nephew, London, UK) is set up in the meniscal suture passer asymmetrically, leaving one limb of suture one-third of the total length and the other two-thirds of the total length (Table 1). The meniscal suture passer is then passed through the anteromedial portal. The suture is placed through the lateral part of the meniscal tear, and the loop (Fig 3) is retried through the same AM portal. Both limbs are then pulled through the loop, and tightened until the loop is snug against the meniscal body. A Kocher is then attached at the distal part of the short thread.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfall |
|---|---|
| Set suture ends at one-third and two-thirds initially to allow adequate length for second loop passage. | Tissue bridge. Avoid tissue bridge via passing the meniscal suture ends through the shuttling suture arthroscopically or grasp all suture ends and remove together at once. |
| Tunnel convergence. Avoid via replacing the ACL tibial tunnel drill to understand its trajectory and start the meniscal repair transtibial tunnel proximal and lateral to the ACL tibial tunnel. |
Fig 3.
First loop of the lateral meniscal root tear repair using the double compression (DC) knot, on a right knee sawbone. (A) Place the first suture in the lateral part of the meniscal tear using a meniscal suture passer (First Pass or Mini-Pass; Smith and Nephew, London, UK) through the anteromedial portal. (B) The two suture limbs are pulled through the loop to create the first part of the DC knot, cinched snug against the meniscal body.
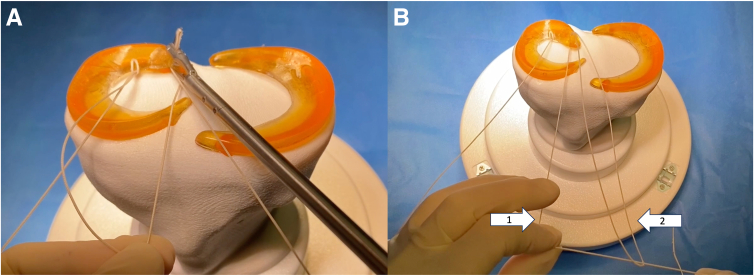
Step 3: Second Loop (Fig 4)
Fig 4.
Second loop of the lateral meniscal root tear repair using the double compression (DC) knot, on a right knee sawbone. (A) Place the second suture in the medial part of the meniscal tear using a meniscal suture passer (First Pass or Mini-Pass; Smith and Nephew, London, UK) through the anteromedial portal. (B) Once the new loop is outside (white arrow, no. 1), place the long thread through the loop (white arrow, no. 2), and slide until the loop disappears into the anteromedial portal.
The longest thread is then set up in the meniscal suture passer. The 2 limbs are maintained in tension to be sure to slide on thread and use the same route to minimize a suture bridge. Attention is now drawn to the medial part of the meniscal tear, the root remnant. The root remnant is penetrated with the meniscal suture passer, and the loop of suture is withdrawn through the same AM portal.
Once the new loop is outside, keep the loop in one hand and the distal part of the long thread in the other, and then slide the newly retrieved loop to make the first outside loop disappear into the AM portal. The long remaining thread is placed through the newly retrieved loop and pulled to tighten and cinch the new loop against the root remnant. Pulling on this medial thread also allows you to apply tension and increase the apposition of the 2 ends of the torn meniscus.
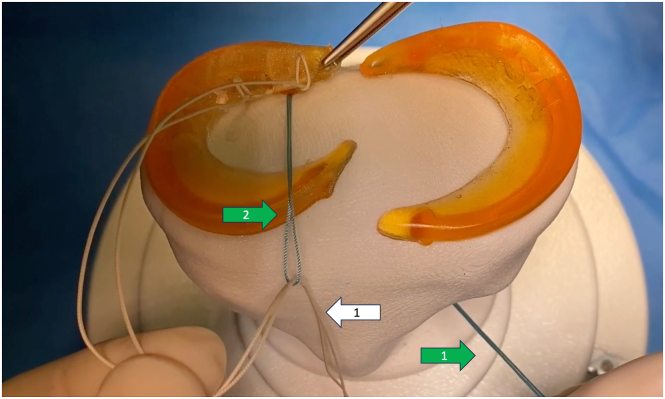
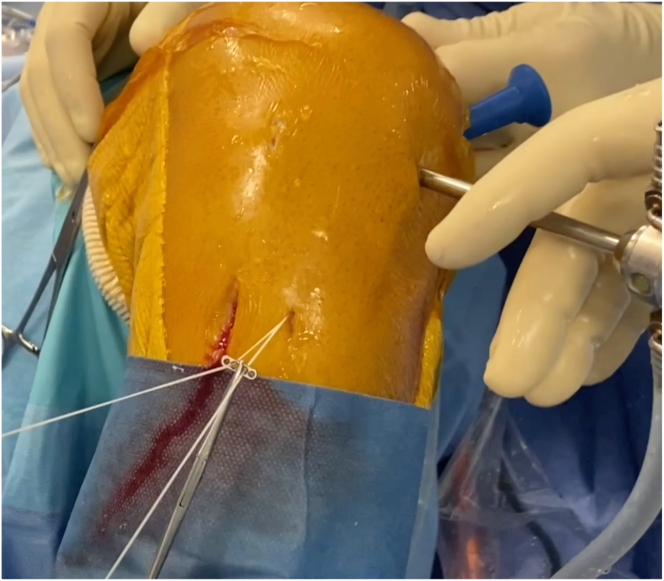
Step 4: Shuttle Meniscal Sutures Through Transtibial Tunnel
A shuttling suture is then introduced from the outside the transtibial tunnel into the knee joint and retrieved arthroscopically. The 2 threads of the meniscal suture are then passed into the loop of the shuttling suture, before the shuttling suture, along with the meniscal sutures are drawn back down the transtibial tunnel (Fig 5).
Fig 5.
Shuttle the meniscal sutures through transtibial tunnel, on a right knee sawbone.A shuttling suture is introduced from the outside of the transtibial tunnel into the knee joint (green arrow, no. 1). The thread is retrieved arthroscopically and exits via the anteromedial portal as a loop (green arrow, no. 2). The 2 threads of the meniscal suture are then passed into the loop (white arrow, no. 1). The 2 meniscal suture threads are then drawn back down through the tibial tunnel.
Step 5: Fixation
The ACL graft is now passed, cycled, and appropriately tensioned and secured (Fig 6). The surgeon can now adjust the tension in both threads, with an arthroscopic view of the apposition of the meniscal tear before the meniscal sutures are tied over an Endobutton (Smith and Nephew, London, UK) flush against the anterior tibia with the knee in flexion.
Fig 6.
Fixation technique of the meniscal suture. The meniscal suture is tied over an Endobutton (Smith and Nephew, London, UK), after adjusting the tension using both threads (UltraBraid; Smith and Nephew). The Endobutton is placed flush against the anterior tibial cortex, via a separate 1-cm scar, on the anteromedial tibial crest.
Discussion
We described a meniscal repair technique for posterior lateral meniscal root tears, combining the benefits of side-to-side repair with transtibial pull-out techniques; namely, it allows apposition of the meniscal tear without the technical difficulties of the suture hook or the potential neurovascular dangers associated with penetrating the posterior joint capsule with an all-inside device.
A number of authors advocate using the same transtibial tunnel as the ACL7; however, this means transtibial techniques are only possible with complete root avulsions, and tears that extend laterally would otherwise place the repaired meniscus in a nonanatomical position, removing the biomechanical benefits of the repair and potentially increasing the risk of repair failure.8, 9, 10 Using a separate tibial tunnel, we are able to use the transtibial technique regardless of how far laterally the tear begins and still place the meniscus in an anatomical position (Table 2).
Table 2.
Advantages and Disadvantages
| Advantage | Disadvantage |
|---|---|
| Allows apposition of torn meniscal ends | Requires accurate placement to the transtibial tunnel to ensure anatomical reduction of the meniscal repair |
| Optimal repair strength with transtibial technique | |
| Avoids penetrating posterior joint capsule and the risk of neurovascular injury | |
| One tunnel, one suture. Easy and economical |
Given the technique can both appose the torn ends and utilize a transtibial technique, it is effective for all posterior lateral root tears requiring repair, as described by Krych et al.1 Transtibial repair techniques have been advocated for radial tears elsewhere because of their improved resistance to shear stress compared to capsular repairs alone11 and have resulted in improved healing rates of meniscal repair for radial tears.12
We have been using this repair technique since December 2022, and while we have not had any failures to date, clinical follow-up at 24 months and peer review will now be required to confirm the clinical effectiveness of the technique.
Disclosure
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The Double Compressive Knot
References
- 1.Krych A.J., LaPrade M.D., Cook C.S., et al. Lateral meniscal oblique radial tears are common with ACL injury: A classification system based on arthroscopic tear patterns in 600 consecutive patients. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120921737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Forkel P., von Deimling C., Lacheta L., et al. Repair of the lateral posterior meniscal root improves stability in an ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc. 2018;26:2302–2309. doi: 10.1007/s00167-018-4949-8. [DOI] [PubMed] [Google Scholar]
- 3.Schillhammer C.K., Werner F.W., Scuderi M.G., Cannizzaro J.P. Repair of lateral meniscus posterior horn detachment lesions: A biomechanical evaluation. Am J Sports Med. 2012;40:2604–2609. doi: 10.1177/0363546512458574. [DOI] [PubMed] [Google Scholar]
- 4.Brophy R.H., Gill C.S., Lyman S., Barnes R.P., Rodeo S.A., Warren R.F. Effect of anterior cruciate ligament reconstruction and meniscectomy on length of career in National Football League athletes: A case control study. Am J Sports Med. 2009;37:2102–2107. doi: 10.1177/0363546509349035. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade R.F., Geeslin A.G., Chahla J., et al. Posterior lateral meniscal root and oblique radial tears: The biomechanical evidence supports repair of these tears, although long-term clinical studies are necessary. Arthrosc J Arthrosc Relat Surg. 2022;38:3095–3101. doi: 10.1016/j.arthro.2022.09.015. [DOI] [PubMed] [Google Scholar]
- 6.Mao D.W., Upadhyay U., Thalanki S., Lee D.Y.H. All-inside lateral meniscal repair via anterolateral portal increases risk of vascular injury: A cadaveric study. Arthrosc J Arthrosc Relat Surg. 2020;36:225–232. doi: 10.1016/j.arthro.2019.07.023. [DOI] [PubMed] [Google Scholar]
- 7.Feucht M.J., Salzmann G.M., Bode G., et al. Posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2015;23:119–125. doi: 10.1007/s00167-014-2904-x. [DOI] [PubMed] [Google Scholar]
- 8.LaPrade C.M., Foad A., Smith S.D., et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43:912–920. doi: 10.1177/0363546514566191. [DOI] [PubMed] [Google Scholar]
- 9.Kamatsuki Y., Furumatsu T., Hiranaka T., et al. Accurate placement of a tibial tunnel significantly improves meniscal healing and clinical outcomes at 1 year after medial meniscus posterior root repair. Knee Surg Sports Traumatol Arthrosc. 2021;29:3715–3723. doi: 10.1007/s00167-020-06376-9. [DOI] [PubMed] [Google Scholar]
- 10.Gupta A., Sanchez M., Storaci H.W., Rohde M.S., Sherman S.L., Shea K.G. Transtibial repair of lateral meniscus posterior root tears improves contact biomechanics in pediatric cadavers. Arthrosc Sports Med Rehabil. 2022;4:e2011–e2018. doi: 10.1016/j.asmr.2022.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhatia S., Civitarese D.M., Turnbull T.L., et al. A novel repair method for radial tears of the medial meniscus: Biomechanical comparison of transtibial 2-tunnel and double horizontal mattress suture techniques under cyclic loading. Am J Sports Med. 2016;44:639–645. doi: 10.1177/0363546515615565. [DOI] [PubMed] [Google Scholar]
- 12.Cinque M.E., Geeslin A.G., Chahla J., Dornan G.J., LaPrade R.F. Two-tunnel transtibial repair of radial meniscus tears produces comparable results to inside-out repair of vertical meniscus tears. Am J Sports Med. 2017;45:2253–2259. doi: 10.1177/0363546517704425. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Double Compressive Knot
The Double Compressive Knot