Abstract
Weather and climate change are constant and ever-changing processes that impact allergy and asthma. The purpose of this report is to provide information since the last climate change review with focus on asthmatic disease. PubMed and internet searches for topics included climate and weather change, air pollution, particulate, greenhouse gasses, traffic, insect habitat, and mitigation, in addition to references contributed by the individual authors. Changes in patterns of outdoor aeroallergens due to increasing temperatures and amounts of carbon dioxide in the atmosphere are major factors linked to increased duration of pollen seasons, pollen production, and possibly increased allergenicity of pollen. Indoor air pollution threats anticipated from climate changes include microbial and mold growth secondary to flooding resulting in displacement of persons and need for respiratory protection of exposed workers. Air pollution from indoor burning of mosquito repellants is a potential anticipatory result of an increase in habitat regions. Air pollution from fossil fuel burning and traffic-related emissions can alter respiratory defense mechanisms and work synergistically with specific allergens to enhance immunogenicity to worsen asthma in susceptible individuals. Community efforts can significantly reduce air pollution, thereby reducing greenhouse gas emission and improving air quality. The allergist’s approach to weather pattern changes should be integrated and anticipatory to protect at-risk patients.
Keywords: weather, climate, allergy, asthma, pollution, pollen
INTRODUCTION
Global warming and climate change are observable phenomena. The earth’s climate is constantly changing and variable over time. Earth’s climate is dependent upon incoming solar radiation, outgoing thermal radiation and the composition of Earth’s atmosphere. Other influences of earth’s climate include the earth’s rotation, wind patterns, and ocean currents. Carbon dioxide, in addition to methane and mixed greenhouse gases, is accumulating in the atmosphere, largely due to fossil fuel use, to collectively influence warming. In addition, the effect of these pollutants on climate change must also account for geologic weather cycles that are occurring every 10 to 100,000 years and are often overlapping. Much of the climate change observations are based on observed trends beginning around 1870 as well as by complex computer modeling based on a number of assumptions. Unfortunately, climate change has become politicized, resulting in ongoing debate that may interfere in the enactment of policy toward mitigation and/or adaptation.
There is a considerable volume of scientifically compelling observations on the climate that has been collected over the past 150 years, including evidence from ice cores dating back over 600,000 years. This evidence, which has been analyzed by a group of scientists called the Intergovernmental Panel on Climate Change (www.ipcc.ch)*, is summarized and includes:
Globally averaged carbon dioxide (CO2) concentration has increased from 250 to 410 parts per million over the past 150 years.*
During the past 150 years, the oceans have had a 26% increase in acidity, measured as hydrogen ion concentration attributable to uptake of carbon dioxide.*
Recent records indicate Greenland and Antarctic ice sheets have been losing mass, the majority of glaciers worldwide have shrunk, permafrost is thawing and northern hemisphere spring snow cover has decreased.*
Over the past hundred years, global mean sea level has risen by 0.19 [0.17 to 0.21] m*.
In plants and animals, seasonal activities and species abundances have been altered in response to ongoing climate change, impacting biodiversity.*
Recorded observations indicate that worldwide the number of record cold days and nights has decreased and the number of record warm days and nights has increased. Seven of the last 10 years have been the hottest years on record.*
The number of frost-free days has increased and the dates for frost-off are coming earlier.*
The frequency of heat waves has increased in large parts of Europe, Asia and Australia.*
Observed warming has increased heat-related human mortality and decreased cold-related human mortality.* In addition to the IPCC report, the relationships between heat waves and mortality have been detailed for Russia(1) and India.(2) In more affluent regions, adaptation to climate changes is often more available whereas developing countries have increased challenges because of high vulnerabilities.(3)
In the last decade, climate driven changes in agriculture has threatened economic stability, leading to mass migration of humans from affected regions.*
These natural system changes may currently have minimal direct impact on many human populations; however, there are increasing observations where the results of climate changes are devastating individual populations.
It is important to distinguish between what is meant by the terms weather and climate. Whereas weather conditions refer to day-to-day fluctuations in temperature and precipitation, climate changes refer to changes in long-term averages of daily weather for an extended period of time. There are data to show that increasing levels of CO2 are associated with increased crop yields for wheat and rice; however, these increased yields are offset by the detrimental impact of rising temperatures, resulting in a net reduction in crop production when CO2 increases and temperature increases are both taken into account.(4–7) Moreover, in a meta-analyses, Myers and colleagues demonstrate that in higher CO2 environments there is a significant decrease in protein content of grains, including rice, wheat, and maize.(8) Thus, the overall negative impact of climate change on crop yields and ocean acidification is concerning because it is projected to impact the largest single primary food source chain contributing to human nutrition. Alterations in overall and regional precipitation events will be more difficult to predict, but it is anticipated that some land regions will experience an increase in heavy precipitation with precipitation events resulting in land erosion, while other land regions will experience a decrease in precipitation resulting in drought, both of which result in loss of life and population displacement. The results of extreme sea level changes that occur in conjunction with hurricanes, typhoons, and flooding resulting in devastating regional events are of concern to human safety and health. Demonstrating short-term weather fluctuations and their overall enumeration over prolonged periods of time will be necessary to demonstrate a concrete link to climate change and long-term trends.
As we continue through the 21st century, predictions that are largely based on current data and computer modeling propose that the Earth’s surface temperature will continue to rise, oceans will continue to get warmer and pick up more carbon dioxide, and sea level will continue to rise. It is also projected that the Arctic region will continue to warm more rapidly than the other parts of the globe. It has been detected that human influence is the principal driver of these changes. If the rate of human manufactured pollution continues, climate change is expected to further amplify current risks and create new, unanticipated risks for natural and human systems. Moreover, these risks will undoubtedly be unevenly distributed and generally greater for disadvantaged people and communities in underdeveloped countries. Vulnerable populations including children, elderly, and those with pre-existing conditions, especially pulmonary and cardiovascular diseases, will also be a greatest risk. As recent hurricanes have demonstrated, however, even countries with highly developed infrastructure will not be spared. The relationship between climate change and human migration is also of potential concern because the incidence rate of respiratory disease to geographic locations could be impacted, but this aspect depends on the differential vulnerability of population and places because if places and populations are not vulnerable, or susceptible, to climate change, then the climate-migration relationship may not materialize. (9) The exact future consequences of these trends are speculative, but the allergy community should be knowledgeable about the issues, understand the impact on allergy and asthma, and be well-versed in possible means to mitigate adverse health consequences. Ultimately, the approach to climate change should be integrated and anticipatory to protect and treat our patients with asthma, and other allergic and climate-sensitive diseases from constituents that are likely driving this phenomenon.
Changing patterns of outdoor aeroallergens could impact asthma
Increasing temperatures and increasing amounts of CO2 in the atmosphere are major factors that have been linked to increased duration of pollen seasons, increased amount of pollen produced by plants, and possibly increased allergenicity of pollen. These changing events that impact patterns of pollen could impact allergic asthma. In various parts of the world, the duration of pollen seasons has been increasing. For example, Ziska et al. noted that, from 1995 to 2009, the duration of ragweed season in North America increased in association with an increasing delay in the first frost of the fall season.(10) Furthermore, this effect was most pronounced in more northern locations, such as certain cities in Canada experiencing a ragweed season prolonged by more than 3 weeks (e.g. Saskatoon, Canada experienced 44 days of ragweed season in 1995 and 71 days in 2009).(10) In addition to a prolonged fall pollen season, there is an earlier start of the spring tree pollen season. Data from pollen counting stations across the United States have revealed that the spring pollen season started earlier in the recent decade as compared to prior years.(11, 12) This lengthening of the pollen season demonstrated in North America has also been witnessed in Europe. Although not directly evaluating pollen counts, a 2002 British study of 385 plant species found that the average first flowering date advanced 4.5 days in the previous decade with 16% of species flowering significantly earlier by an average of 15 days and only 3% of species flowering significantly later.(13) In Poland, the fall weed season has increased in duration in recent decades due to a later end date to the season.(14) A study from Italy, evaluating the years 1981 to 2007, demonstrates a progressive increase in the duration of certain pollen seasons with an increased total pollen load.(15) Importantly, it was also noted that the rates of patients in that region sensitized to pollen increased during these years, whereas the percentage of individuals sensitized to dust mite remained stable.(15) In addition to increased duration of the pollen season, there have been studies demonstrating an increased amount of pollen released during these seasons. Pollen data from 1987 to 2016 in Oklahoma found significant increases in the seasonal pollen index over time, including the peak concentrations that are reached by eastern red cedar tree pollen.(16) When evaluating multiple common pollens, others have noted the average peak value and annual total production of airborne pollen has increased in the recent two decades.(11)
In addition to increased quantity, there is some evidence that higher temperatures affect IgE binding. Namely, it was demonstrated that birch pollen (Bet v 1) extracts from trees grown in warmer temperatures had stronger IgE binding intensity.(17) Singer and colleagues also demonstrated increasing Amb a1 in ragweed pollen as a function of rising CO2.(18) With increased pollen production and longer pollen seasons combined with the hypothesized increase in frequency of thunderstorms in some geographic areas with climate change, there is a potential heightened importance of thunderstorm-related asthma epidemics.(19) This phenomomen reflects the mechanical and/or osmotic rupture of pollen that allows for release of smaller particles and bioaerosol formation to be deposited in deeper airways resulting in asthma attacks.(19) Another contributing aspect is the change in geographic distribution of various allergenic plants in recent decades. These include range expansions for some species as well as latitudinal or altitudinal shifts for other species.(20, 21) Distribution changes have been documented in trees, shrubs, weeds, and grasses;(16, 20–23) however, the expansion of ragweed in Europe has the greatest implications for allergic asthma patients. Ragweed has become invasive through large areas of Central and Eastern Europe since the mid-20th century, and the pollen has become a major health issue in many areas.(24–27) The projected impact of climate change on ragweed has been perhaps the most well-studied (Table I).(28) Several studies in Europe have used computer simulations to predict the potential effects of future climate change on ragweed spread and pollen sensitization rates.(25–27) Simulation studies have demonstrated that the number of individuals sensitized to ragweed is expected to more than double in Europe within only a few decades.(27) The greatest proportional increases are expected to occur in countries where current ragweed sensitization rates are low. Associated with the increased sensitization rates, higher pollen counts and longer pollen seasons are expected to increase the severity of symptoms in those sensitized.(27) It is also noted that there is evidence that with extremely high temperatures, ragweed pollen release may be hindered.(29–31)
TABLE I.
Projected changes in the biology of ragweed and the consequences for aeroallergen production, distribution, and exposure from spatial and temporal studies. Adapted from Ziska and Beggs.(28)
| Methodology | Variables examined | Outcome | Implications |
|---|---|---|---|
| Glasshouses, growth chambers, single plants | Projected future CO2 concentrations, earlier springs | Bigger plants, more flowering, pollen production increases, more allergenic pollen | Pollen production and allergenicity might increase with climate change scenarios |
| Prairie grassland, plant mixture | 1°C-2°C increase, clipping to simulate herbivory | Significant increases in pollen production and diameter with warming | Warming and herbivory might stimulate pollen size and production |
| Disturbed soil in urban-rural transect, plant succession | Urban microclimate of warmer temperatures, more CO2, longer growing season | Larger plants, earlier flowering, reduced allergenicity | Microclimate changes, similar to near-term Intergovernmental Panel on Climate Change projections might already be stimulating pollen production and increased exposure in urban areas |
| National Allergy Bureau and Aerobiology Canada, pollen counts | Start and end of pollen season since 1990s from Texas to Canada | Duration of pollen season increasing as a function of latitude in North America | Warming might have already altered pollen exposure in North America |
Increasing CO2 is a crucial factor in the growth of plant species and increased pollen production. In environmentally controlled greenhouses, it has been demonstrated that increasing temperatures and increasing atmospheric CO2 concentrations results in enhanced ragweed pollen production.(32, 33) Similarly, controlled studies have shown that increased CO2 results in an increased amount of grass pollen production even in the setting of increased ozone levels, a repressor of pollen production.(34) Urban areas may be particularly susceptible to these environmental changes as the inner city is a place known for increased temperatures and increased CO2. Ziska et al. demonstrates that urban environments, when compared to rural environments, had higher temperatures and higher CO2 production that was associated with ragweed plants growing faster, flowering earlier, and producing more pollen.(35) This is supported by data from Europe detailing an increasing trend in yearly amount of airborne pollen that was more pronounced in urban areas.(36) Plants that grow in an enhanced CO2 environment have a higher carbon to nitrogen ratio in their leaves that can affect growth of organisms, such as Alternaria, which can become more abundant and produce more allergens in these environments.(37) Lake et al. demonstrates that an increase of CO2 from 400 ppm to 800 ppm increased established mycelia colonies 40%.(37)
Modeling efforts have recently been made to quantify the projected medical costs of current pollen trends. Anenberg et al. used different emission scenarios termed the Representative Concentration Pathways [RCP] of four greenhouse gas concentration trajectories adopted by the Intergovernmental Panel on Climate change (www.ipcc.ch) to analyze the future impact of projected oak pollen distributions on emergency department visits and healthcare costs.(38) Under their projections, “severe climate change (RCP8.5)”could increase oak pollen season length and associated asthma emergency department visits by 5% by 2050 and by 10% by 2090, whereas “moderate climate change (RCP4.5)” modeling would result in a 4% increase in emergency department visits by 2090.(38) Richter et al. simulates the future costs of treating ragweed allergy in Austria and southern Germany with predictive costs increasing in magnitude of 200% to 350% for 2050.(25) A similar analysis was performed for ozone exposure. This analysis demonstrated an increase in cost that was dependent on the various predicted climate model scenarios and regional differences within the United States.(39)
Recognizing these past regional changes in pollen trends toward longer pollen seasons, increased pollen quantity, and perhaps allergenicity of pollen as a result of weather and climate changes may be useful for allergy/asthma health care providers, researchers, and policy makers in anticipating future needs. The predictive models of climate change scenarios to date suggest that the numbers of allergic asthma patients seeking care will increase, and to meet this need, it is likely that enhanced early warning systems and effective training and preparation of existing and future health care providers will be necessary.
Weather and climate changes impact the indoor built environment to affect asthma
Changes in short-time weather and longtime climate conditions also impact indoor built environment exposures that affect persons with allergic asthmatic disease. Some of these effects are predictable, and others might not be predictable. For example, as sea level rises and ocean temperatures warm, storms and hurricanes are predicted to increase in frequency and intensity,(40) increasing vulnerability and exposure to coastal flooding.(41) The catastrophic floods resulting from Hurricanes Katrina and Rita in New Orleans, Louisiana, in 2005 promoted heavy microbial and mold growth with levels of indoor molds, endotoxins, and fungal glucans similar to levels found in agricultural environments and at levels associated with adverse respiratory health effects.(42–44) The Head-Off Environmental Asthma in Louisiana Asthma (HEAL) study that enrolled families affected from the flooding found that 94% of the families had to move at least once with many moving more than 2 or even 4 times to find acceptable housing.(45) The HEAL study demonstrates that the remediation efforts coupled with moving families to safe homes decreased the airborne mold (except Alternaria) and dust allergens,(46) and moreover, after one year there were few associations found between mold and other allergen concentrations with asthma.(45)
Because extensive remediation and renovations of the built environments are required following massive storm damage, protection of exposed workers in these efforts is necessary. Survey data collected from persons who participated in the environmental and reconstruction efforts following Hurricane Sandy (2012; New Jersey/New York) demonstrated that more than one-third of participants (34.4%) reported post-Sandy lower respiratory symptoms.(47) Furthermore, there was a dose-response relationship between the number of types of Sandy-related exposures reported and post-Sandy lower respiratory symptoms.(47) During the recovery efforts following Hurricane Katrina, it was demonstrated that the use of elastomeric respirators (i.e. tight-fitting, air-purifying respirator with replaceable filters or cartridges attached to a rubber or silicone face piece) performed better than N95 respirators to reduce remediation worker exposure levels to endotoxins and molds,(42) which is valuable information that can be applied to future events. Most recently, in the aftermath of Hurricane Maria in Puerto Rico (2017), the Associated Press reported an increase in asthma and asthma severity that could be attributed to increased use of diesel- or gasoline- powered generators, high mold counts, and increased problems with rodents and cockroaches in damaged homes.(48) It is too early to know the asthmatic consequences ascribed to the 2018 weather events that included, but not limited to, the California wild-fires, Atlantic hurricanes, volcanic activity in Hawaii, and Venice, Italy flooding events.
A potential emerging indoor pollutant consequence as a result of climate change that might not be predictable, is the generation of indoor air pollution occurring predominately in developing countries as a result of burning mosquito repellants.(49) Under current and future climate projections, the distribution of mosquito habitat ranges that are defined as warm and humid climates associated with high rainfall is anticipated to change.(50, 51) Based on a recent Centers for Disease Control and Prevention report,(52) the incidence of vector borne disease has tripled in the United States between 2004 to 2016. Additionally, since 2004, nine new diseases have been introduced in the United States, including the chikungunya and Zika viruses.(52) To protect against mosquito-borne parasitic and viral disease,(49) pyrethrum-containing repellants (e.g. coils, mats or liquidators) are typically burned for six to eight hours, which results in very high levels of indoor air toxicants.(49) The pollutants induced include particulate matter (PM2.5) (53) and particulate-associated heavy metals (lead and cadmium),(49) polycyclic aromatic hydrocarbons, formaldehyde, benzene and carbon monoxide.(54) Furthermore, studies have demonstrated an increase in respiratory symptoms including asthma in persons exposed to mosquito coils.(53) Substitution with a charcoal base (which can also release toxic emissions) was shown to reduce this indoor air pollution by 5–10 fold.(54)
Whereas increased allergen and respiratory health hazards resulting from flooding of indoor environments following massive storms will impact persons with asthmatic disease and may affect incidence of asthma development, there are also potential unanticipated consequences as the mosquito habitat and use of repellent example provides. Another potential consequence from climate change that could impact asthma outcomes is the African dust events that have increased due to drought conditions and subsequently affect areas in the Caribbean, the southern United States, and other parts of the world.(55) In addition, there may likely be unanticipated consequences from weather changes leading to adaptions in the indoor built environment, for example, changes in architectural/construction techniques leading to tighter building, filtration systems, or external air-exchange systems.
Impact of climate change and air pollution interactions to affect asthma health
Weather changes closely interact with air pollution to represent a major challenge that can impact the health of asthmatics. Human-influenced air pollutants (i.e. anthropogenic) are predominately derived from burning of fossil fuels (e.g. power plants, vehicles) and biomass to include carbon dioxide (CO2), black carbon, sulfate (SO4), nitrogen oxides (NOx), volatile organic compounds (VOC), ozone precursors, and particulate organic matter.(56, 57) Agricultural emissions of methane and ammonia are also important anthropogenic air pollutants.(56) Naturally occurring air pollutants are recognized as smoke from wildfires, wind-blown mineral dust, and (VOCs) from trees. Whereas these aerosols affect weather and climate changes, these pollutants can be transformed by weather and climate factors such as temperature and humidity to modify composition and enhance toxicity and biological properties.(56, 58, 59) For example, higher temperatures favor rapid formation of ozone, and VOCs and NOx increase with temperature due to increased fossil fuel combustion of electricity generation during heat waves.(56, 60) Particulate matter, particularly PM2.5, which is a complex mixture of airborne particles emitted from a great variety of sources (e.g. vehicles, power plants, burning of fossil fuels, heating systems, wild fires, windblown dust), can be modified by weather systems to impact distribution and concentration as well as volatilize at higher temperatures.(55, 56, 61)
Air pollution can increase the frequency of emergency room visits and hospitalizations for asthma, increase the incidence and development of asthma, and act as an adjuvant to potentiate the development of allergy to pollen.(62–66) Mechanistic studies have demonstrated a role for pollutants in inducing airway inflammation, neutrophil influx, cytokine/chemokine release, production of white blood cells, oxygen free-radical production, endotoxin-mediated cellular and tissue responses, stimulation of irritant receptors, and covalent modification of key cellular enzymes.(66–69) Pollutant exposures can also alter mucus production, damage the airway epithelium, impair mucociliary ciliary clearance, and trigger airway hyper-reactivity.(59, 70–72) Importantly, pollutants (e.g. PM2.5 and ozone) can act as adjuvants and enhance allergy by skewing responses towards IgE production and allergic Th2-mediated responses as well as stimulation of Th17 responses.(58, 67, 72, 73) Ambient air pollution and polycyclic aromatic hydrocarbon exposure has also been shown to impair T-regulatory cell function in asthmatics,(74, 75) but it is also recognized that signaling through the aryl hydrocarbon receptor induces human regulatory T cells.(76) The generation of free radicals by these particulate components, in addition to a contribution from semivolatile organic components and gases such as ozone, nitrogen oxides and SO2 can induce oxidative stress, which can lead to further pro-inflammatory effects in the respiratory tract and lung.(63, 67, 73) Although the effect of individual air pollutants may be unique, the combined impact of exposure spikes or chronic low-level exposure to a mixture of airborne pollutants can result in a pronounced effect on individuals with underlying allergic or non-allergic asthmatic disease.(59, 65, 69, 77, 78)
Air pollution may also be an important risk factor affecting the progression of asthma to chronic obstructive pulmonary disease (COPD), which is referred to as asthma/COPD overlap (ACO). It was demonstrated in the Canadian Community Health Survey that individuals exposed to higher levels of air pollution had nearly threefold greater odds of developing ACOS.(79) Specifically, the adjusted hazard ratios of ACO and cumulative exposures to PM2.5 and ozone were 2.78 (95% confidence interval, 1.62–4.78) and 1.31 (95% confidence interval, 0.71–2.39), respectively.(79) Furthermore, the air quality health index, a composite air pollution index based on levels of ozone and fine particulate matter, was associated with an increased risk of concurrent COPD and asthma, with an adverse impact on mortality.(80)
There is mixed news regarding the current trends in air pollution parameters. The American Lung Association State of the Air 2017 report of levels of ozone and particle pollution from official monitoring sites encompassing years 2013–2015(66) found improvement in air quality in ozone and year round particle pollution compared to previous years, but found an increase in high spikes of particle pollution. Whereas trends toward improvement since the Clean Air Act of 1970 have been witnessed, the number of people exposed to unhealthy levels of air pollution remains at more than 125 million with 38.9% of people in the U.S. living in counties with unhealthy levels of either ozone or particle pollution.(66) A changing climate that includes increased wildfire smoke and extreme weather events led to a few cities reporting their worst number of unhealthy days since this reporting began. For example, cities in the West and Southwest dominate the most ozone-polluted list, Western states had the highest fine and ultrafine particle exposure, and short-term particle pollution spikes from burden of smoke from wildfires, brush fires, and wood-burning devices were found in the Western U.S. and Alaska.(66)
With new fossil fuel combustion technologies (e.g. gasoline direct injection engines for cars), it is likely that future particulate emissions could also change with evidence of health concerns increasing with ultrafine particles and secondary organic aerosols (SOA). Ultrafine particles that are generated as byproducts of fossil fuel combustion, condensation of semi-volatile substances, or industrial emissions represent health concerns to asthmatics.(81) These particles might be more dangerous than larger PM due to their chemical composition, small size, capability of generating reactive oxygen species, and deep penetration in the respiratory system.(81) Because these particles are concentrated in locations that are in proximity to busy traffic and are not being tracked, investigators will need to understand how these particulates are impacted by climate and weather changes and any resulting effect on asthma.(81) Lastly, SOA that are formed by oxidation and complex reactions of sunlight and volatile organic components from trees, plants, and petroleum-derived fuels account for two-thirds of the total organic aerosols in urban aerosols. Whereas the role of SOA in asthma has yet to be defined, studies show that SOA can impact lung responses including increasing gene expression profiling of the nuclear factor-like 2 (Nrf2) transcription factor network as well as TNF-α and IL-6 expression.(82–85) There should be continual awareness and research of not only the traditional fossil fuel combustion products, but other air pollutant sources such as ultrafine particles and SOA and their interplay with climate change and asthma.
Examples of efforts to reduce adverse environmental conditions to improve health
Indoor and outdoor air pollution can be reduced through human influence and community efforts. The use of biomass fuels (animal dung, crop residues, wood, charcoal) is a major cause of both indoor and ambient air pollution, and it is widely recognized that exposure to smoke from the burning of biomass fuels is a major cause of global morbidity and mortality from respiratory diseases.(86–88) There are studies reporting an association of indoor cooking (either solid fuels or gas) with asthma in both adults and children and with asthma exacerbations.(86),(89, 90) Data from India’s Third National Family Health Survey of men and women aged 20–49 years observed a significantly higher risk of self-reported asthma in women (OR 1.26; 95% CI 1.06 – 1.49) exposed to cooking with solid fuels, but not in men, after adjusting for various confounding factors.(91) Furthermore, children in rural India observed a strong association (OR = 2.20; 95% CI: 1.16, 4.19) of physician-diagnosed asthma and decreased lung function with indoor cooking.(92) Due to adoption of safer cooking and heating fuels such as liquid petroleum gas (LPG) in developing countries, the recent global burden of disease report highlights a significant reduction (>40%) in the use of solid fuels from 1990 to 2016 in the world.(93) As further example of initiatives to improve health, the government of India launched the Ujjwala scheme in 2016 that provides the cleaner fuel (LPG) to below poverty line households.
An example of how community efforts worked to impact air quality, reduce greenhouse gases and improve respiratory disease conditions is from the Fairbanks North Star Borough in Alaska, which has some of the worst spikes in air pollutants due to increase in wildfires and the use of wood and coal for energy, heating and cooking.(66) Spikes in particulate matter (PM2.5) levels in Interior Alaska have been reported as almost double the next most-polluted area in the United States and nearly four times the recommended limit for unhealthy air. Man-made sources of PM2.5 in Fairbanks include outdoor burning, wood and/or coal burning heating devices, automobiles and other vehicles with combustion engines, and industrial facilities using coal-fired power plants. Alaska community groups joined together to demand that responsible officials address the air quality and related health concerns that North Star Borough residents and their families face when simply breathing in Fairbanks. As a result of grass-root community efforts, the Environmental Protection Agency (EPA) approved the state implementation plan revisions submitted by the State of Alaska to address the Clean Air Act, effective 10/10/2017 to improve air quality.(94, 95) Next, the Interior Gas Utility was established in 2012 by the Fairbanks North Star Borough to offer area residents a lower-cost alternative to heating oil, and a cleaner-burning fuel than either oil or firewood. Transporting LPG to Fairbanks is also being pursued.(96) Finally, alternative energy sources to successfully heat buildings using a ground-source heat pump buried deep in the earth are being pursued with 60 installed in homes in the Fairbanks area at time of this review.(97) It is also recognized that California put climate legislation AB 32 in place to target greenhouse gas reductions that set in motion a cascade of regulations, subsidies, and performance standards to promote a long-term approach to improving the environment. (98) These examples of efforts to reduce indoor and outdoor air pollutants to ultimately protect against adverse health effects, including asthma, might provide motivation to other communities needing to reduce pollutants.
The legislative efforts by governments to reduce atmospheric pollutants has been ongoing but are full of challenges due to differing opinions on economic and political priorities. The greatest sources of air particulates having the greatest impact on human respiratory health emanates from local emissions from wood stoves, burning distillate oil, industrial sources (power plants), and mobile emissions. The implementation of stringent air quality standards in the United States and Europe has had an impact on reducing air pollution and improving respiratory health in some regions more than others in the United States. Legislative efforts can be effective in combating air pollution to potentially reduce climate change patterns that have been observed over the past few decades.
CONCLUSION
The health impacts from weather and climate change with indoor and outdoor air quality as discussed in the report (summarized in Figure 1) are many and varied. Air pollution and climate change are closely related with air pollutants contributing to atmospheric temperature and increasing temperatures from climate change leading to increases in natural volatile organic compound emissions. In addition CO2 emissions primarily from burning of fossil fuels are not only an important driver of climate change, but also major sources of air pollutants. Larger and more frequent wildfires associated with climate change could also significantly reduce air quality. These related current event trends could have a devastating impact on our planet. In a recent Lancet article, the potential impact of current climate change trends we have been observing is described as the “biggest global health threat of the 21st century.”(99) Likewise, this challenge may provide the greatest opportunity to curtail the ensuing public health crisis.
Figure 1.
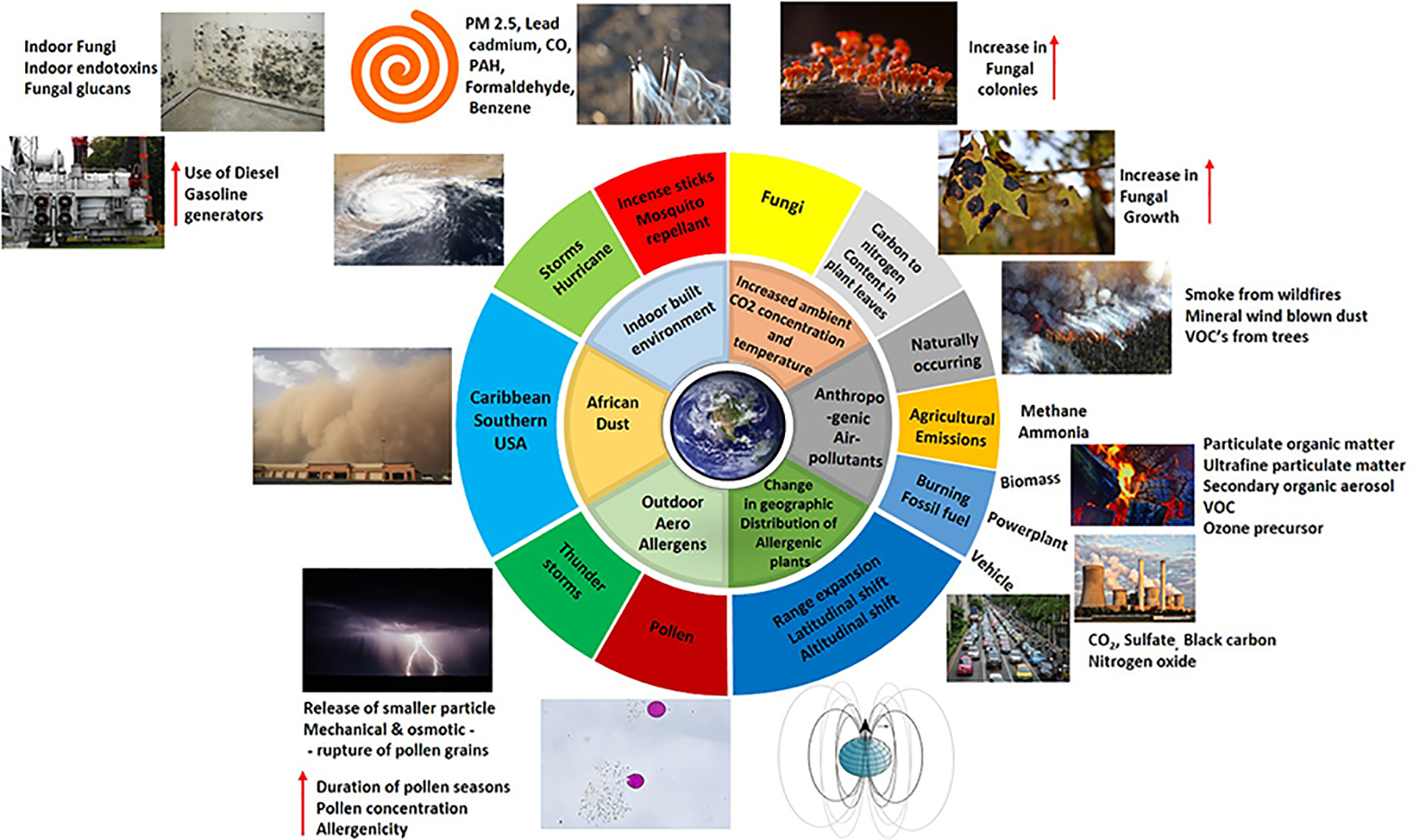
Overview figure summarizing impact of weather and climate change with indoor and outdoor air quality in asthma. Fungus on indoor home wall image following Hurricane Katrina in New Orleans, Louisiana, 2005, and image of pollen releasing content due to osmotic stress (Amaranthus retroflexus releasing starch granules) are courtesy of Rosa Codina.
We in the allergy and scientific community should be knowledgeable on how atmospheric conditions impact increases in air pollutants and aeroallergens and their impact on allergic and respiratory health, and how such exposures can be meaningfully reduced. We should continue to adapt our practices to meet the needs of our patients in the face of ever changing patterns and presentation of disease that might result from weather and climate changes. Moreover, we can take steps to expand coordinated research monitoring of climate impact on pollen trends, allergic sensitization, and asthma severity. We can also advocate for prevention measures and/or become involved in policy debates. A recent review of studies investigating the effects of nutrition on air pollution and various chronic respiratory diseases including asthma suggested that dietary and/or nutritional supplements might be somewhat beneficial with helping protect against air pollution induced respiratory damage; however, more robust evidence is needed. Climate and weather patterns will continue to change, and new difficulties will likely emerge that could impact asthma and allergies. As physicians and scientists, there should be a strong commitment to develop strategies for taking actions that will protect vulnerable persons at risk for adverse respiratory health outcomes.
Acknowledgements:
The authors would like to thank Sangeetha Vishweswaraiah, PhD, Department of Obstetrics and Gynecology, Oakland University William Beaumont School of Medicine, Royal Oak, Michigan, U.S, for assistance in figure graphic design with images for figure 1. Images not detailed in figure legend obtained from free use website (pixabay.com). We thank Lisa Chudomelka for assistance in manuscript submission.
Funding:
No funding source supported this manuscript.
Abbreviations:
- CO2
Carbon dioxide
- CO
Carbon monoxide
- DEP
Diesel exhaust particle
- DALY
Disability-Adjusted Life Years
- EPA
Environmental protection agency
- LPG
Liquid propane gas
- NOx
Nitrogen oxide
- PM
Particulate matter
- PAH
Polycyclic aromatic hydrocarbons
- SOA
Secondary organic aerosols
- SO2
Sulfur dioxide
- SO4
Sulfate
- U.S.
United States
- VOC
Volatile organic compounds
Footnotes
Disclosure of interest: Intellectual property developed by AN and others was licensed to Westwood Bioscience by the Regents of the Univertity of California. AN is co-founder, equity holder, and SAB chair of Westwood Bioscience, Inc. All others authors confirm that they have no conflicts of interest to disclose. This report is submitted by the AAAAI EERH Working Group and has been approved by the AAAAI Board of Directors.
References
- 1.Shaposhnikov D, Revich B, Bellander T, Bedada GB, Bottai M, Kharkova T, et al. Mortality related to air pollution with the moscow heat wave and wildfire of 2010. Epidemiology. 2014. May;25(3):359–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mazdiyasni O, AghaKouchak A, Davis SJ, Madadgar S, Mehran A, Ragno E, et al. Increasing probability of mortality during indian heat waves. Sci Adv. 2017. Jun 7;3(6):e1700066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mertz O, Halsnaes K, Olesen JE, Rasmussen K. Adaptation to climate change in developing countries. Environ Manage. 2009. May;43(5):743–52. [DOI] [PubMed] [Google Scholar]
- 4.Long SP, Ainsworth EA, Leakey AD, Nosberger J, Ort DR. Food for thought: Lower-than-expected crop yield stimulation with rising CO2 concentrations. Science. 2006. Jun 30;312(5782):1918–21. [DOI] [PubMed] [Google Scholar]
- 5.Cai C, Yin X, He S, Jiang W, Si C, Struik PC, et al. Responses of wheat and rice to factorial combinations of ambient and elevated CO2 and temperature in FACE experiments. Glob Chang Biol. 2016. Feb;22(2):856–74. [DOI] [PubMed] [Google Scholar]
- 6.Dubey SK, Tripathi SK, Pranuthi G. Effect of elevated CO2 on wheat crop: Mechanism and impact. Crit Rev Environ Sci Technol. 2015;45(21):2283–304. Available from: 10.1080/10643389.2014.1000749. [DOI] [Google Scholar]
- 7.Zhao C, Liu B, Piao S, Wang X, Lobell DB, Huang Y, et al. Temperature increase reduces global yields of major crops in four independent estimates. Proc Natl Acad Sci U S A. 2017. Aug 29;114(35):9326–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myers SS, Zanobetti A, Kloog I, Huybers P, Leakey AD, Bloom AJ, et al. Increasing CO2 threatens human nutrition. Nature. 2014. Jun 5;510(7503):139–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grecequet M, DeWaard J, Hellmann JJ, Abel GJ. Climate vulnerability and human migration in global perspective. Sustainability. 2017. May;9(5): 10.3390/su9050720. Epub 2017 Apr 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ziska L, Knowlton K, Rogers C, Dalan D, Tierney N, Elder MA, et al. Recent warming by latitude associated with increased length of ragweed pollen season in central north america. Proc Natl Acad Sci U S A. 2011. Mar 8;108(10):4248–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y, Bielory L, Mi Z, Cai T, Robock A, Georgopoulos P. Allergenic pollen season variations in the past two decades under changing climate in the united states. Glob Chang Biol. 2015. Apr;21(4):1581–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Y, Bielory L, Georgopoulos PG. Climate change effect on betula (birch) and quercus (oak) pollen seasons in the united states. Int J Biometeorol. 2014. Jul;58(5):909–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fitter AH, Fitter RS. Rapid changes in flowering time in british plants. Science. 2002. May 31;296(5573):1689–91. [DOI] [PubMed] [Google Scholar]
- 14.Bogawski P, Grewling L, Nowak M, Smith M, Jackowiak B. Trends in atmospheric concentrations of weed pollen in the context of recent climate warming in poznan (western poland). Int J Biometeorol. 2014. Oct;58(8):1759–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ariano R, Canonica GW, Passalacqua G. Possible role of climate changes in variations in pollen seasons and allergic sensitizations during 27 years. Ann Allergy Asthma Immunol. 2010. Mar;104(3):215–22. [DOI] [PubMed] [Google Scholar]
- 16.Flonard M, Lo E, Levetin E. Increasing juniperus virginiana L. pollen in the tulsa atmosphere: Long-term trends, variability, and influence of meteorological conditions. Int J Biometeorol. 2018. Feb;62(2):229–41. [DOI] [PubMed] [Google Scholar]
- 17.Ahlholm JU, Helander ML, Savolainen J. Genetic and environmental factors affecting the allergenicity of birch (betula pubescens ssp. czerepanovii [orl.] hamet-ahti) pollen. Clin Exp Allergy. 1998. Nov;28(11):1384–8. [DOI] [PubMed] [Google Scholar]
- 18.Singer BD, Ziska LH, Frenz DA, Gebhard DE, Straka JG Increasing amb a 1 content in common ragweed (ambrosia artemisiifolia) pollen as a function of rising atmospheric CO2 concentration. Functional Plant Biology. 2005;32(7):667–670. Available from: 10.1071/FP05039. [DOI] [PubMed] [Google Scholar]
- 19.Cecchi L, D’Amato G, Annesi-Maesano I. External exposome and allergic respiratory and skin diseases. J Allergy Clin Immunol. 2018. Mar;141(3):846–57. [DOI] [PubMed] [Google Scholar]
- 20.Beggs PJ. Impacts of climate change on allergens and allergic diseases. Beggs PJ, editor. Cambridge: Cambridge University Press; 2016. [Google Scholar]
- 21.Bertin RI. Plant phenology and distribution in relation to recent climate change. The Journal of the Torrey Botanical Society. 2008;135:126–46. Available from: 10.3159/07-RP-035R.1. [DOI] [Google Scholar]
- 22.Briggs JM, Hoch GA, Johnson LC. Assessing the rate, mechanisms, and consequences of the conversion of tallgrass prairie to juniperus virginiana forest. Ecosystems. 2002;5(6):578–86. Available from: https://www.jstor.org/stable/3658764. [Google Scholar]
- 23.Morgan JA, Milchunas DG, LeCain DR, West M, Mosier AR. Carbon dioxide enrichment alters plant community structure and accelerates shrub growth in the shortgrass steppe. Proc Natl Acad Sci U S A. 2007. Sep 11;104(37):14724–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katelaris CH, Beggs PJ. Climate change: Allergens and allergic diseases. Intern Med J. 2018. Feb;48(2):129–34. [DOI] [PubMed] [Google Scholar]
- 25.Richter Rl, Berger UE, Dullinger S, et al. Spread of invasive ragweed:Climate change, management and how to reduce costs. Journal of Applied Ecology. 2013;50:1422–30. [Google Scholar]
- 26.Hamaoui-Laguel L, Vautard R, Liu L, et al. Effects of climate change and seed dispersal on airborne ragweed pollen loads in europe. Nature Climate Change. 2015;5:766–71. [Google Scholar]
- 27.Lake IR, Jones NR, Agnew M, Goodess CM, Giorgi F, Hamaoui-Laguel L, et al. Climate change and future pollen allergy in europe. Environ Health Perspect. 2017. Mar;125(3):385–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ziska LH, Beggs PJ. Anthropogenic climate change and allergen exposure: The role of plant biology. J Allergy Clin Immunol. 2012. Jan;129(1):27–32. [DOI] [PubMed] [Google Scholar]
- 29.Shrestha A, Roman ES, Gordon Thomas A, Swanton CJ. Modeling germination and hoot-radicle elongation of ambroisa artemisiifolia. Weed Science. 1999. [cited 09-20-2018];47(5):557–62. Available from: https://www.jstor.org/stable/4046110. [Google Scholar]
- 30.Howard LE, Levetin E. Ambrosia pollen in tulsa, oklahoma: Aerobiology, trends, and forecasting model development. Ann Allergy Asthma Immunol. 2014. Dec;113(6):641–6. [DOI] [PubMed] [Google Scholar]
- 31.Makra L, Matyasovsky I, Paldy A, Deak AJ. The influence of extreme high and low termperatures and precipitation totals on pollen seasons of ambrosia, poaceae and populus in szeged, southern hungary. Grana. 2012. [cited 9-20-2018];51(3):215–27. Available from: 10.1080/00173134.2012.661764. [DOI] [Google Scholar]
- 32.Rogers CA, Wayne PM, Macklin EA, Muilenberg ML, Wagner CJ, Epstein PR, et al. Interaction of the onset of spring and elevated atmospheric CO2 on ragweed (ambrosia artemisiifolia L.) pollen production. Environ Health Perspect. 2006. Jun;114(6):865–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wayne P, Foster S, Connolly J, Bazzaz F, Epstein P. Production of allergenic pollen by ragweed (ambrosia artemisiifolia L.) is increased in CO2-enriched atmospheres. Ann Allergy Asthma Immunol. 2002. Mar;88(3):279–82. [DOI] [PubMed] [Google Scholar]
- 34.Albertine JM, Manning WJ, DaCosta M, Stinson KA, Muilenberg ML, Rogers CA. Projected carbon dioxide to increase grass pollen and allergen exposure despite higher ozone levels. PLoS One. 2014. Nov 5;9(11):e111712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ziska LH, Gebhard DE, Frenz DA, Faulkner S, Singer BD, Straka JG. Cities as harbingers of climate change: Common ragweed, urbanization, and public health. J Allergy Clin Immunol. 2003. Feb;111(2):290–5. [DOI] [PubMed] [Google Scholar]
- 36.Ziello C, Sparks TH, Estrella N, Belmonte J, Bergmann KC, Bucher E, et al. Changes to airborne pollen counts across europe. PLoS One. 2012;7(4):e34076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lake JA, Wade RN. Plant-pathogen interactions and elevated CO2: Morphological changes in favour of pathogens. J Exp Bot. 2009;60(11):3123–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Anenberg SC, Weinberger KR, Roman H, et al. Impacts of oak pollen on allergic asthma in the united states and potential influence of future climate change. GeoHealth. 2017;1:80–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fann N, Nolte CG, Dolwick P, Spero TL, Brown AC, Phillips S, et al. The geographic distribution and economic value of climate change-related ozone health impacts in the united states in 2030. J Air Waste Manag Assoc. 2015. May;65(5):570–80. [DOI] [PubMed] [Google Scholar]
- 40.Lane K, Charles-Guzman K, Wheeler K, Abid Z, Graber N, Matte T. Health effects of coastal storms and flooding in urban areas: A review and vulnerability assessment. J Environ Public Health. 2013;2013:913064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Impacts and predictions of coastal change during hurricanes. U.S. geological survey (USGS)fact sheet 2010–3012 [homepage on the Internet] U.S. Department of the Interior/U.S. Geological Survey. 2016 2016. November [cited April 6 2018]. Available from: https://pubs.usgs.gov/fs/2010/3012/. [Google Scholar]
- 42.Chew GL, Wilson J, Rabito FA, Grimsley F, Iqbal S, Reponen T, et al. Mold and endotoxin levels in the aftermath of hurricane katrina: A pilot project of homes in new orleans undergoing renovation. Environ Health Perspect. 2006. Dec;114(12):1883–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rao CY, Riggs MA, Chew GL, Muilenberg ML, Thorne PS, Van Sickle D, et al. Characterization of airborne molds, endotoxins, and glucans in homes in new orleans after hurricanes katrina and rita. Appl Environ Microbiol. 2007. Mar;73(5):1630–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Adhikari A, Jung J, Reponen T, Lewis JS, DeGrasse EC, Grimsley LF, et al. Aerosolization of fungi, (1-->3)-beta-D glucan, and endotoxin from flood-affected materials collected in new orleans homes. Environ Res. 2009. Apr;109(3):215–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grimsley LF, Wildfire J, Lichtveld M, Kennedy S, El-Dahr JM, Chulada PC, et al. Few associations found between mold and other allergen concentrations in the home versus skin sensitivity from children with asthma after hurricane katrina in the head-off environmental asthma in louisiana study. Int J Pediatr. 2012;2012:427358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grimsley LF, Chulada PC, Kennedy S, White L, Wildfire J, Cohn RD, et al. Indoor environmental exposures for children with asthma enrolled in the HEAL study, post-katrina new orleans. Environ Health Perspect. 2012. Nov;120(11):1600–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gargano LM, Locke S, Jordan HT, Brackbill RM. Lower respiratory symptoms associated with environmental and reconstruction exposures after hurricane sandy. Disaster Med Public Health Prep. 2018. Jan 21:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Puerto rico struggles with jump in asthma cases post-maria [homepage on the Internet]. AP News: Associated Press. 2018. June 18, 2018 [cited September 5, 2018]. Available from: https://www.apnews.com/23793064cc954c69a176cb094e6c96aa/Puerto-Rico-struggles-with-jump-in-asthma-cases-post-Maria. [Google Scholar]
- 49.Salvi D, Limaye S, Muralidharan V, Londhe J, Madas S, Juvekar S, et al. Indoor particulate matter < 2.5 mum in mean aerodynamic diameter and carbon monoxide levels during the burning of mosquito coils and their association with respiratory health. Chest. 2016. Feb;149(2):459–66. [DOI] [PubMed] [Google Scholar]
- 50.Samy AM, Elaagip AH, Kenawy MA, Ayres CF, Peterson AT, Soliman DE. Climate change influences on the global potential distribution of the mosquito culex quinquefasciatus, vector of west nile virus and lymphatic filariasis. PLoS One. 2016. Oct 3;11(10):e0163863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rochlin I, Ninivaggi DV, Hutchinson ML, Farajollahi A. Climate change and range expansion of the asian tiger mosquito (aedes albopictus) in northeastern USA: Implications for public health practitioners. PLoS One. 2013;8(4):e60874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Centers for disease control and prevention. national center for emerging and zoonotic infectious diseases (NCEZID). division of vector-borne diseases (DVBD ).[homepage on the Internet]. May 1, 2018. [cited May 5, 2018]. Available from: https://www.cdc.gov/ncezid/dvbd/index.html.
- 53.Liu W, Zhang J, Hashim JH, Jalaludin J, Hashim Z, Goldstein BD. Mosquito coil emissions and health implications. Environ Health Perspect. 2003. Sep;111(12):1454–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang L, Jiang Z, Tong J, Wang Z, Han Z, Zhang J. Using charcoal as base material reduces mosquito coil emissions of toxins. Indoor Air. 2010. Apr;20(2):176–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Prospero JM, Lamb PJ. African droughts and dust transport to the caribbean: Climate change implications. Science. 2003. Nov 7;302(5647):1024–7. [DOI] [PubMed] [Google Scholar]
- 56.Kinney PL. Interactions of climate change, air pollution, and human health. Curr Environ Health Rep. 2018. Mar;5(1):179–86. [DOI] [PubMed] [Google Scholar]
- 57.Provencal S, Kishcha P, da Silva AM, Elhacham E, Alpert P. AOD distributions and trends of major aerosol species over a selection of the world’s most populated cities based on the 1st version of NASA’s MERRA aerosol reanalysis. Urban Clim. 2017. Jun;20:168–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Orellano P, Quaranta N, Reynoso J, Balbi B, Vasquez J. Effect of outdoor air pollution on asthma exacerbations in children and adults: Systematic review and multilevel meta-analysis. PLoS One. 2017. Mar 20;12(3):e0174050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Spann K, Snape N, Baturcam E, Fantino E. The impact of early-life exposure to air-borne environmental insults on the function of the airway epithelium in asthma. Ann Glob Health. 2016. Jan–Feb;82(1):28–40. [DOI] [PubMed] [Google Scholar]
- 60.Fiore AM, Naik V, Leibensperger EM. Air quality and climate connections. J Air Waste Manag Assoc. 2015. Jun;65(6):645–85. [DOI] [PubMed] [Google Scholar]
- 61.Sapkota A, Symons JM, Kleissl J, Wang L, Parlange MB, Ondov J, et al. Impact of the 2002 canadian forest fires on particulate matter air quality in baltimore city. Environ Sci Technol. 2005. Jan 1;39(1):24–32. [DOI] [PubMed] [Google Scholar]
- 62.Finkelman FD. Diesel exhaust particle exposure during pregnancy promotes development of asthma and atopy. J Allergy Clin Immunol. 2014. Jul;134(1):73–4. [DOI] [PubMed] [Google Scholar]
- 63.Bernstein JA, Alexis N, Barnes C, Bernstein IL, Bernstein JA, Nel A, et al. Health effects of air pollution. J Allergy Clin Immunol. 2004. Nov;114(5):1116–23. [DOI] [PubMed] [Google Scholar]
- 64.Gilmour MI, Jaakkola MS, London SJ, Nel AE, Rogers CA. How exposure to environmental tobacco smoke, outdoor air pollutants, and increased pollen burdens influences the incidence of asthma. Environ Health Perspect. 2006. Apr;114(4):627–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Balmes JR, Earnest G, Katz PP, Yelin EH, Eisner MD, Chen H, et al. Exposure to traffic: Lung function and health status in adults with asthma. J Allergy Clin Immunol. 2009. Mar;123(3):626–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.American Lung Association. American lung association state of the air 2017. www.Lung.org: American Lung Association; 2017. Report No.: http://www.lung.org/assets/documents/healthy-air/state-of-the-air/state-of-the-air-2017.pdf. [Google Scholar]
- 67.Nel A. Atmosphere. air pollution-related illness: Effects of particles. Science. 2005. May 6;308(5723):804–6. [DOI] [PubMed] [Google Scholar]
- 68.Clifford RL, Jones MJ, MacIsaac JL, McEwen LM, Goodman SJ, Mostafavi S, et al. Inhalation of diesel exhaust and allergen alters human bronchial epithelium DNA methylation. J Allergy Clin Immunol. 2017. Jan;139(1):112–21. [DOI] [PubMed] [Google Scholar]
- 69.Brandt EB, Biagini Myers JM, Acciani TH, Ryan PH, Sivaprasad U, Ruff B, et al. Exposure to allergen and diesel exhaust particles potentiates secondary allergen-specific memory responses, promoting asthma susceptibility. J Allergy Clin Immunol. 2015. Aug;136(2):295, 303.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gasana J, Dillikar D, Mendy A, Forno E, Ramos Vieira E. Motor vehicle air pollution and asthma in children: A meta-analysis. Environ Res. 2012. Aug;117:36–45. [DOI] [PubMed] [Google Scholar]
- 71.Romeo E, De Sario M, Forastiere F, Compagnucci P, Stafoggia M, Bergamaschi A, et al. PM 10 exposure and asthma exacerbations in pediatric age: A meta-analysis of panel and time-series studies. Epidemiol Prev. 2006. Jul–Oct;30(4–5):245–54. [PubMed] [Google Scholar]
- 72.Bowatte G, Lodge C, Lowe AJ, Erbas B, Perret J, Abramson MJ, et al. The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: A systematic review and a meta-analysis of birth cohort studies. Allergy. 2015. Mar;70(3):245–56. [DOI] [PubMed] [Google Scholar]
- 73.Nel AE, Diaz-Sanchez D, Ng D, Hiura T, Saxon A. Enhancement of allergic inflammation by the interaction between diesel exhaust particles and the immune system. J Allergy Clin Immunol. 1998. Oct;102(4 Pt 1):539–54. [DOI] [PubMed] [Google Scholar]
- 74.Hew KM, Walker AI, Kohli A, Garcia M, Syed A, McDonald-Hyman C, et al. Childhood exposure to ambient polycyclic aromatic hydrocarbons is linked to epigenetic modifications and impaired systemic immunity in T cells. Clin Exp Allergy. 2015. Jan;45(1):238–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nadeau K, McDonald-Hyman C, Noth EM, Pratt B, Hammond SK, Balmes J, et al. Ambient air pollution impairs regulatory T-cell function in asthma. J Allergy Clin Immunol. 2010. Oct;126(4):845, 852.e10. [DOI] [PubMed] [Google Scholar]
- 76.Tousa S, Semitekolou M, Morianos I, Banos A, Trochoutsou AI, Brodie TM, et al. Activin-A co-opts IRF4 and AhR signaling to induce human regulatory T cells that restrain asthmatic responses. Proc Natl Acad Sci U S A. 2017. Apr 4;114(14):E2891–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Carracedo-Martinez E, Taracido M, Tobias A, Saez M, Figueiras A. Case-crossover analysis of air pollution health effects: A systematic review of methodology and application. Environ Health Perspect. 2010. Aug;118(8):1173–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Brandt EB, Kovacic MB, Lee GB, Gibson AM, Acciani TH, Le Cras TD, et al. Diesel exhaust particle induction of IL-17A contributes to severe asthma. J Allergy Clin Immunol. 2013. Nov;132(5):1194, 1204.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.To T, Zhu J, Larsen K, Simatovic J, Feldman L, Ryckman K, et al. Progression from asthma to chronic obstructive pulmonary disease. is air pollution a risk factor? Am J Respir Crit Care Med. 2016. Aug 15;194(4):429–38. [DOI] [PubMed] [Google Scholar]
- 80.To T, Zhu J, Carlsten C, Larsen K, Ryckman K, Feldman LY, et al. Do community demographics, environmental characteristics and access to care affect risks of developing ACOS and mortality in people with asthma? Eur Respir J. 2017. Sep 11;50(3): 10.1183/13993003.00644,2017. Print 2017 Sep. [DOI] [PubMed] [Google Scholar]
- 81.Li N, Georas S, Alexis N, Fritz P, Xia T, Williams MA, et al. A work group report on ultrafine particles (american academy of allergy, asthma & immunology): Why ambient ultrafine and engineered nanoparticles should receive special attention for possible adverse health outcomes in human subjects. J Allergy Clin Immunol. 2016. Aug;138(2):386–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yang B, Ma P, Shu J, Zhang P, Huang J, Zhang H. Formation mechanism of secondary organic aerosol from ozonolysis of gasoline vehicle exhaust. Environ Pollut. 2018. Mar;234:960–8. [DOI] [PubMed] [Google Scholar]
- 83.Holopainen JK, Kivimaenpaa M, Nizkorodov SA. Plant-derived secondary organic material in the air and ecosystems. Trends Plant Sci. 2017. Sep;22(9):744–53. [DOI] [PubMed] [Google Scholar]
- 84.Lin YH, Arashiro M, Clapp PW, Cui T, Sexton KG, Vizuete W, et al. Gene expression profiling in human lung cells exposed to isoprene-derived secondary organic aerosol. Environ Sci Technol. 2017. Jul 18;51(14):8166–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Niu X, Ho SSH, Ho KF, Huang Y, Cao J, Shen Z, et al. Indoor secondary organic aerosols formation from ozonolysis of monoterpene: An example of d-limonene with ammonia and potential impacts on pulmonary inflammations. Sci Total Environ. 2017. Feb 1;579:212–20. [DOI] [PubMed] [Google Scholar]
- 86.Behera D, Chakrabarti T, Khanduja KL. Effect of exposure to domestic cooking fuels on bronchial asthma. Indian J Chest Dis Allied Sci. 2001. Jan–Mar;43(1):27–31. [PubMed] [Google Scholar]
- 87.McCracken JP, Wellenius GA, Bloomfield GS, Brook RD, Tolunay HE, Dockery DW, et al. Household air pollution from solid fuel use: Evidence for links to CVD. Glob Heart. 2012. Sep;7(3):223–34. [DOI] [PubMed] [Google Scholar]
- 88.Gordon SB, Bruce NG, Grigg J, Hibberd PL, Kurmi OP, Lam KB, et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med. 2014. Oct;2(10):823–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Diette GB, Accinelli RA, Balmes JR, Buist AS, Checkley W, Garbe P, et al. Obstructive lung disease and exposure to burning biomass fuel in the indoor environment. Glob Heart. 2012. Sep 1;7(3):265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wong GW, Brunekreef B, Ellwood P, Anderson HR, Asher MI, Crane J, et al. Cooking fuels and prevalence of asthma: A global analysis of phase three of the international study of asthma and allergies in childhood (ISAAC). Lancet Respir Med. 2013. Jul;1(5):386–94. [DOI] [PubMed] [Google Scholar]
- 91.Agrawal S Effect of indoor air pollution from biomass and solid fuel combustion on prevalence of self-reported asthma among adult men and women in india: Findings from a nationwide large-scale cross-sectional survey. J Asthma. 2012. May;49(4):355–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Padhi BK, Padhy PK. Domestic fuels, indoor air pollution, and children’s health. Ann N Y Acad Sci. 2008. Oct;1140:209–17. [DOI] [PubMed] [Google Scholar]
- 93.GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet. 2017. Sep 16;390(10100):1345–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Air plan approval; AK, fairbanks north star borough; 2006 PM2.5 [homepage on the Internet] United States Environmental Protection Agency. 2017 2017. September 8 [cited 2018 April 2]. Available from: https://www.federalregister.gov/documents/2017/09/08/2017-18768/air-plan-approval-ak-fairbanks-north-star-borough-2006-pm25. [Google Scholar]
- 95.EPA in alaska: Fairbanks air quality plan [homepage on the Internet]. United States Environmental Protection Agency. 2017 2017. October 24 [cited 2018 April 2]. Available from: https://www.epa.gov/ak/fairbanks-air-quality-plan. [Google Scholar]
- 96.Three IGU candidates’ top priority: Speeding efforts to bring natural gas to fairbanks [homepage on the Internet]. Alaska Public Media/National Public Radio. 2017 2017. October 2 [cited 2018 January 6]. Available from: https://www.alaskapublic.org/2017/10/02/three-igu-candidates-top-priority-speeding-efforts-to-bring-natural-gas-to-fairbanks/. [Google Scholar]
- 97.Alternative heating system shows promise for reducing fuel costs in interior alaska [homepage on the Internet]. Anchorage Daily News. 2016 2016. September 28 [cited 2018 January 6]. Available from: https://www.adn.com/energy/article/after-full-year-operation-alternative-heat-source-fairbanks-proves-successful/2015/04/23/. [Google Scholar]
- 98.Assembly bill 32 overview [homepage on the Internet]. State of California. 2014. August 5, 2014 [cited January 30, 2019]. Available from: https://www.arb.ca.gov/cc/ab32/ab32.htm. [Google Scholar]
- 99.Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. Managing the health effects of climate change: Lancet and university college london institute for global health commission. Lancet. 2009. May 16;373(9676):1693–733. [DOI] [PubMed] [Google Scholar]


