Abstract
Ankylosing spondylitis (AS) and diffuse idiopathic skeletal hyperostosis (DISH) are bone-forming spinal conditions which inherently increase spine rigidity and place patients at a higher risk for thoracolumbar fractures. Due to the long lever-arm associated with their pathology, these fractures are frequently unstable and may significantly displace leading to catastrophic neurologic consequences. Operative and non-operative management are considerations in these fractures. However conservative measures including immobilization and bracing are typically reserved for non-displaced or incomplete fractures, or in patients for whom surgery poses a high risk. Thus, first line treatment is often surgery which has historically been an open posterior spinal fusion. Recent techniques such as minimally invasive surgery (MIS) and robotic surgery have shown promising lower complication rates as compared to open techniques, however these methods need to be further validated.
Keywords: Ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis, thoracolumbar fractures
1. Introduction
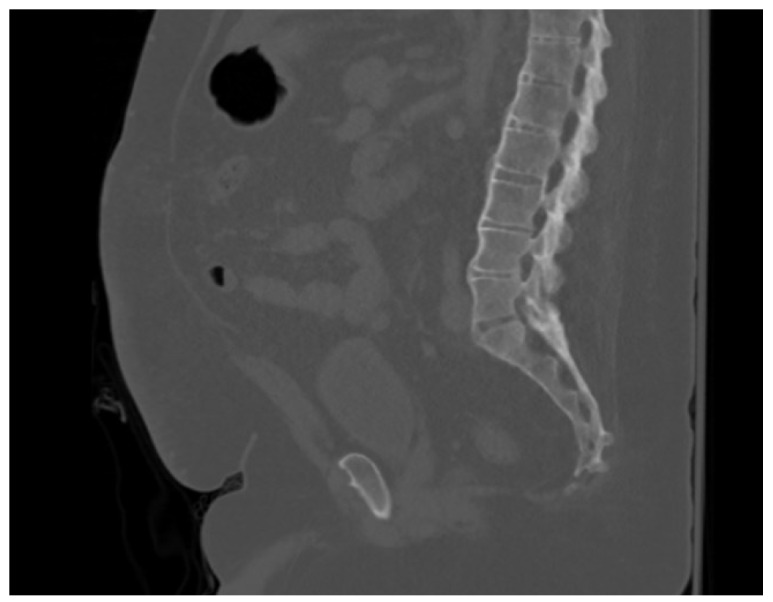
Ankylosing spondylitis (AS) and diffuse idiopathic skeletal hyperostosis (DISH) are bone-forming spinal diseases that increase spine rigidity, leading to functional and structural abnormalities with decreased quality of life.1–3 In AS, chronic inflammation causes the sacroiliac joints and spine to spontaneously fuse resulting in acute back pain followed by generalized spinal stiffness3 (Figure 1). The prevalence of this entity has a range of 0.1% to 1.4%.2
Figure 1. CT scan showing an intact spine in a patient with AS.
In DISH, a non-inflammatory disease, there is no degeneration of the sacroiliac or apophyseal joints, but the pathologic process is defined by four adjacent vertebral bodies bridged by osteophytes, forming new bone4 (Figure 2). The prevalence of this disease is higher, ranging from 2.9% to 25%.5,6 This multilevel bone fusion creates a long spinal lever arm, increasing susceptibility to injury even after low energy trauma.7–10 The risk of fractures is higher in patients with ankylosing conditions of the spine than in healthy individuals, particularly thoracolumbar fractures.11–13
Figure 2. CT scan showing an intact spine in a patient with DISH.

Dislocation events tend to be more common in AS and DISH due to the ossification of the elastic and supporting soft tissues creating a longer lever arm, creating severe instability and have an increased potential for neurologic impairment.3,14,15 To protect against the progression of neurological deficits, these patients should be managed with extreme caution such as using advanced and full spine imaging when a fracture is suspected.3,16–18 Like most spinal pathology, management can be either conservative or operative. Although surgical strategies can have a high rates of postoperative morbidity and mortality making nonoperative management a logical consideration, prolonged bed rest is associated with complications such as bedsores, pneumonia, and venous thrombosis; Additionally, non-operative management has an increased risk for pseudarthosis and subsequent nerve injury which is why operative treatment is usually favored in these patients.3,19,20
There is some debate surrounding the management of thoracolumbar fractures in patients with AS and DISH. Furthermore, there is a paucity of clear guidelines and algorithms to handle thoracolumbar fractures in these patients. Thus, the purpose of this article is to review the different management techniques of these fractures to help guide spine surgeons in treating these entities.
2. Conservative Management
In patients with AS and DISH, the instability of these fractures have prompted a move towards surgical treatment to avoid any risk of future displacements and subsequent neurologic injury.21 While conservative management can be successful in some cases, close monitoring is required in AS and DISH due to the high risk of deformity progression, neurologic injuries, and non-union.18 Non-surgical management is limited to rigid external orthoses including plaster jackets, thoracolumbosacral orthoses, halo vest, and cervical collars, depending on the location of the injury.18
Conservative treatment strategies date back as early as the mid-1900s when immobilization was reported to be successful for AS patients.22 This evolved to more rigid external immobilization, where in 1975, it was recommended that neurologically intact patients be placed in a plaster body-cast with regular follow-up.23 However, more recently, the efficacy of external orthoses has been questioned, with one case report describing successful conservative management with only observation and no brace in a neurologically intact patient suffering from a T5 3-column spinal fracture.24 The authors highlighted the role of the rib-sternum complex - the “fourth column” - in maintaining the stability of this fracture that was initially described as “unstable”.24 The high rate of kyphotic deformities makes bracing difficult for AS patients.18 Nevertheless, Faqeeh et al. reported a lumbar fracture in a neurologically intact AS patient that was successfully managed with a brace.25 However, one must note that in these two recent reports, conservative management was a second-line management since surgery was ruled out either due to patient refusal or medical comorbidities which placed the patient at increased surgical risk.24,25 Traction is rarely used as most of the fractures in AS patients are unstable and traction can risk even further displacement.18
As for DISH, bracing alone may be a feasible option if the fractures are stable.26 Three cases of conservative management were discussed by Taher et al. and included patients with hyperextension injuries and normal facet orientations without significant dislocation.26 The authors recommended that surgeons consider conservative treatment on a case-by-case basis and that the surgeon should consider the nature of the fracture to determine the appropriate orthosis strategy for fusion.26 Institutionally, we have experienced the same stability profile with bracing in certain pure extension-type fractures due to the relative stability in flexion, which tends to be the direction of displacement and deformity in AS and DISH patients.
In a study published in 2009 comparing surgical and nonsurgical outcomes for spinal fracture in AS and DISH, cases where there was a stable fracture (defined using the thoracolumbar injury classification system) and no associated deficits were managed conservatively using either a halo vest orthosis.27 The authors noted that patients placed in a halo vest died early within the postinjury time period, leading them to recommend that halo vest use be carefully considered in AS and DISH as they tend to be older with multiple medical comorbidities27. Data such as this support the recommendation that bracing be a second-line treatment with surgery the recommended treatment if medically safe.3
Complications after conservative management are common. While some complications are acceptable such as mild kyphosis, many complications can be catastrophic. These include complications such as pseudoarthrosis, displacement resulting in a nonrecoverable neurologic insult, or development of a spinal epidural hematoma.27–30 Epidural hematoma is not uncommon in these fractures and can even occur in non-displaced fractures due to the micromotion of the fractured segments injuring the epidural venous plexus.28 Other complications include the high risk of pulmonary complications and death associated with prolonged bed rest.31,32 Furthermore, external halo fixation has been associated with a high risk of respiratory insufficiency, loss of reduction, and pin-related complications such as pull-out or infection.18 Bracing is also associated with respiratory complications and high mortality rates.32,33 In a retrospective analysis done by Caron et al., bracing was used as the definitive treatment for 18% of patients; while for another 15% of patients, bracing was used when patients were considered too unstable for surgery.33 Among this nonoperative group treated with bracing alone, the mortality rate was higher at 51% compared to 23% in the surgically treated group.33 However, it was not clear if there were any baseline differences between cohorts which confounded these findings. Due to the potential for catastrophic outcomes we still prefer to reserve conservative management for non-operative candidates. Aoki et al. went further to suggest that even if the operative risk is high, surgery should still be considered as the first line treatment.28
3. Operative Management
3.1. Positioning
The ligaments and paraspinal muscles around a fractured and ankylosed spine are some of the only mechanical supports preventing further displacement. Thus, surgeons must be careful in positioning patients after the induction of general anesthesia due to the loss of muscular tone and subsequent structural spinal support.18,34,35 Surgeons must be careful when both moving and positioning patients in order to prevent any subsequent fractures or displacement and maintain proper spinal alignment.18,36,37 Furthermore, emergency intubation in AS and DISH was associated with the initiation or progression of neurological deficits.38 Thus, standard usage of fiberoptic intubation, in addition to suitable transportation and positioning while maintaining the spine under protection and avoiding sudden manipulations, is crucial especially in unstable cervical or cervicothoracic fractures.18,39,40
Additionally, utilizing fluoroscopy after positioning may help ensure appropriate alignment and avoid fusing patients in improper positions.34 Other recommendations include supplementing the operating table with pads/rolls which can help reduce the fracture by acting as a hypomochlion.18 In some cases, especially in hyperextension injuries, implementing an inclined upright sitting position is needed to reduce the fracture.18 Finally, applying a unilateral screw fixation system under local anesthesia before undergoing general anesthesia and extended instrumentation was shown to be effective in a small case series, preventing positioning and anesthesia-associated neurologic deterioration.35
3.2. Approach
A variety of surgical approaches have been suggested in the literature: posterior or combined anterior-posterior fixation.18,37 As for standalone anterior fixation, it is not recommended due to the long lever arm and lack of structural support without posterior fixation. In some cases, an anterior approach is necessary if the isolated posterior surgery was unsuccessful in aligning and/or approximating the fracture ends to an acceptable degree.18,41 However, a higher rate of pulmonary complications are noted when an anterior approach is used, especially in the cervicothoracic region.42
In AS patients, fusion can be performed effectively through a posterior or posterolateral approach using autologous bone or different forms of allograft or synthetic graft.41 In situations where posterolateral fusion cannot be achieved or the patient is at a high risk of pseudarthrosis, expandable cages or autologous bone grafts through an anterior approach for fusion may be useful.37,41 However, there is a high risk of cage subsidence which may be avoided by utilizing angular stable plating systems.18 Subsidence may be caused by escaped ossification in the concerned segment since AS is a multifocal and not a contiguous disease, and the altered biomechanics of the stiff spine result in endplate stress fractures.37
The standard surgical approach for thoracolumbar spine fracture with hyperextension in patients with DISH involves an open posterior fixation with spinal instrumentation that extends three levels above and below the fracture site.3 In a retrospective review of 122 patients with AS and DISH, Caron et al. found that in the 58 patients (77% of the surgical treatment group) who received posterior segmental fixation with instrumentation three levels above and below the injury, no patients required reoperation for fixation failure.33 Within the posterior only surgical group, the lack of fixation failure with the multi-level segmental posterior fixation led them to recommend that there was no need for an additional anterior column fixation despite the increased occurrence of anterior column defects after correction in this cohort.33,43
3.3. Techniques
3.3.1. Open
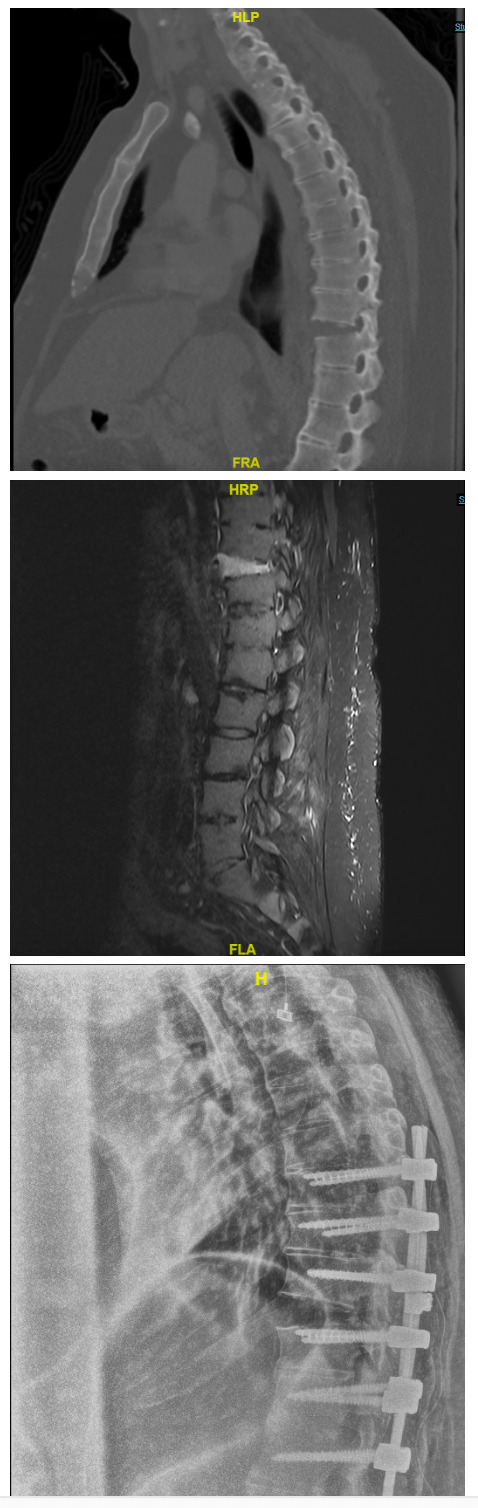
Trent et al. were one of the first to recommend operative treatment in shearing fractures using contoured Luque rods placed in a rectangular configuration with segmental wiring three levels below and above the injured level and contraindicated the usage of Harrington distraction rods.30 The rods utilized have changed to a pedicle screw-rod construct while maintaining the fixation to three segments above and below the injured vertebra in both AS and DISH (Figure 3).33,35 However, other recent literature has demonstrated efficacy with constructs that only extend two segments above and below the fracture instead of three.18,41
Figure 3. (A) CT scan (B) and MRI of a T10-11 fracture in a patient with AS. (C) Post-operative plain radiograph showing posterior instrumentation 3 levels above and below the T10-11 fracture.
Due to the high rate of associated osteoporosis in patients with AS and DISH, using polymethylmethacrylate (PMMA) to augment the screws can be effective.18,41,44 However, caution must be taken due to the risk of cement embolism especially in patients with a long thoracic instrumentation or patients with pre-operative pulmonary restriction due to the rib-cage stiffness associated especially with AS.45 Furthermore, open/closed wedge osteotomy for kyphosis correction is not recommended in the acute setting due to its association with a higher rate of complications, especially hematologic.18 If the deformity is severe, then concomitant osteotomy can be considered after discussing risks and benefits with the patient.18,46
Open posterior fixation three levels above and below the injury increases the length and invasiveness of the procedure which has been postulated to contribute to the high mortality rate associated with these surgical interventions. This has led to more recent attempts to utilize percutaneous pedicle screws in minimally invasive surgeries (MIS).
3.3.2. Minimally Invasive
The gradually emerging minimally invasive surgery (MIS) approaches are promising.47 Many studies have been carried out to examine the efficacy of MIS in AS and DISH and report similar outcomes with a lower perioperative complication rate when MIS was compared to open surgery.11,44,48–50 It was also shown that MIS decreases blood loss and shortens both operative time and hospital stay.32,44,47,50–54 These findings support MIS as another highly effective approach since it can achieve similar outcomes to open procedures with lower rates of perioperative complications.
One complication associated with MIS, as described by Yeoh et al., is the difficulty of identifying landmarks using fluoroscopy to correctly position pedicle screws.47 For this reason, some studies have advised the use of a CT guided navigation as an alternative, which improves the screw position accuracy.55–57 Choi et al. reported an 87.3% accuracy of computer-tomography image guided system (IGS) screw placement in comparison to 82.1% for fluorotactic guidance system (FGS). IGS also had a significantly lower mean registration and operational time of 6:50 minutes in contrast to 14:34 minutes of FGS operational time.57
3.3.3. Vertebroplasty & kyphoplasty
Due to the fact that AS patients often have other comorbidities and a high risk of mortality with surgery, posterior instrumentation can sometimes have unacceptably high surgical risk.58 In such patients, Kulkarni et al. demonstrated that vertebroplasty can be an effective alternative.58 This procedure should be performed with caution and cement must be placed anteriorly to avoid any cement leakage into the spinal canal.58 Kyphoplasty was also shown to be an effective procedure and resulted in satisfactory outcomes in AS patients.59,60 To avoid cement leakage, a graded infusion of cement is recommended.59 Late-stage cement should be added first to cover the fracture line, followed by cement in the paste or dough-phase which will diffuse evenly in the vertebral body.59
As for DISH, vertebroplasty improved the patients’ ambulatory status and reduced back pain to the patients pre-operative levels.61 The authors argue that this technique was safe and effective at reducing back pain and re-establishing gait in affected patients.61 Vertebroplasty may even be a suitable option after unsuccessful open surgeries.62 These results were also demonstrated when kyphoplasty was used instead of vertebroplasty.63,64 Additionally, bracing with anti-osteoporotic treatment is believed to contribute to improved quality of life for the patient.63 However, Tsuchikawa et al. recommend avoiding this technique in patients with a difference ≥ 10° in the wedge angle of the fractured vertebrae between the supine and sitting positions as it was associated with delayed healing.
3.3.4. Robot-Assisted
Another surgical treatment option, studied in AS patients, is the robot-assisted minimally invasive procedure which may further decrease blood loss and the operative period while reducing the complication rate.65,66 A study by Shi et al. investigated the efficacy of robot assisted internal fixation in the lateral decubitus position for the treatment of AS in comparison to conventional MIS.67 They found superior screw accuracy in the robot-assisted MIS surgery (96.9%) when compared to conventional MIS (81.5%).67 The use of robotic MIS for AS could be especially advantageous since these patients have a high potential to develop intra- and post-operative complications.65 Nevertheless, more studies are needed before implementing this approach in the management armamentarium of thoracolumbar fractures in AS and DISH.
4. Conclusion
Management of thoracolumbar fractures in patients with AS and DISH remains debated. Conservative management (immobilization, halo, bracing etc), which may be more suitable for neurologically intact patients with stable fractures, needs to be carefully justified as it may confer complications such as respiratory insufficiency and loss of reduction leading to potentially catastrophic neurological injury. Close monitoring is incumbent to facilitate early recognition of complications. As for surgical intervention, a traditional prone position posterior-only open approach with fusion carried three levels above and below the fractured level remains an excellent option with high rates of fusion and good outcomes. Other MIS techniques have recently shown a promising perioperative complication profile with similar outcomes, and increased experience may optimize results. However, more studies are needed before implementing these approaches as the standard of care.
Competing interests
MD, AR, MBC, JG, MB, JRM, and CLM declare no competing interests.
BGD declares consulting fees for clariance and spinevision. However, none of them is relevant to this manuscript.
AHD declares grants from stryker and Medtronic, royalties from stryker and spineart, consulting fees from stryker, spineart, and Medtronic, receiving payment for expert testimony from multiple law firms. However, none of them is relevant to this manuscript.
Corresponding Author
Alan H. Daniels, MD
1 Kettle Point Ave
East Providence, RI 02914
Email: alandanielsmd@gmail.com
Funding Statement
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- Spinal fractures complicating ankylosing spondylitis. Hunter T., Dubo H. Apr 1;1978 Annals of Internal Medicine. 88(4):546–9. doi: 10.7326/0003-4819-88-4-546. doi: 10.7326/0003-4819-88-4-546. [DOI] [PubMed] [Google Scholar]
- Ankylosing spondylitis. Braun Jürgen, Sieper Joachim. Apr;2007 The Lancet. 369(9570):1379–1390. doi: 10.1016/s0140-6736(07)60635-7. doi: 10.1016/s0140-6736(07)60635-7. [DOI] [PubMed] [Google Scholar]
- Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Westerveld L. A., Verlaan J. J., Oner F. C. 2009European Spine Journal. 18(2):145–156. doi: 10.1007/s00586-008-0764-0. doi: 10.1007/s00586-008-0764-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick Donald, Niwayama Gen. Radiology. 3. Vol. 119. Radiological Society of North America (RSNA); Radiographic and Pathologic Features of Spinal Involvement in Diffuse Idiopathic Skeletal Hyperostosis (DISH) pp. 559–568. [DOI] [PubMed] [Google Scholar]
- The prevalence of diffuse idiopathic skeletal hyperostosis in Korea. Kim S.K., Choi B.R., Kim C.G.., et al. 2004J Rheumatol. 31(10):2032–2035. http://www.ncbi.nlm.nih.gov/pubmed/15468371 [PubMed] [Google Scholar]
- The prevalence of diffuse idiopathic skeletal hyperostosis (DISH) in two large American Midwest metropolitan hospital populations. Weinfeld R. M., Olson Paul N., Maki Daniel D., Griffiths H. J. Apr 16;1997 Skeletal Radiology. 26(4):222–225. doi: 10.1007/s002560050225. doi: 10.1007/s002560050225. [DOI] [PubMed] [Google Scholar]
- Taggard Derek A., Traynelis Vincent C. Spine. 16. Vol. 25. Ovid Technologies (Wolters Kluwer Health); Management of cervical spinal fractures in ankylosing spondylitis with posterior fixation; pp. 2035–2039. [DOI] [PubMed] [Google Scholar]
- Spinal fractures complicating ankylosing spondylitis. A long-term followup study. Hunter Thomas, Dubo Hyman I. Jun;1983 Arthritis & Rheumatism. 26(6):751–759. doi: 10.1002/art.1780260608. doi: 10.1002/art.1780260608. [DOI] [PubMed] [Google Scholar]
- Injuries of the cervical spine in patients with ankylosing spondylitis: experience at two trauma centers. Einsiedel Thomas, Schmelz Andreas, Arand Markus, Wilke Hans-Joachim, Gebhard Florian, Hartwig Erich, Kramer Michael, Neugebauer Rainer, Kinzl Lothar, Schultheiss Markus. Jul;2006 Journal of Neurosurgery: Spine. 5(1):33–45. doi: 10.3171/spi.2006.5.1.33. doi: 10.3171/spi.2006.5.1.33. [DOI] [PubMed] [Google Scholar]
- Broom MICHAEL J., Raycroft JOHN F. Spine. 7. Vol. 13. Ovid Technologies (Wolters Kluwer Health); Complications of fractures of the cervical spine in ankylosing spondylitis; pp. 763–766. [DOI] [PubMed] [Google Scholar]
- Percutaneous instrumentation with cement augmentation for traumatic hyperextension thoracic and lumbar fractures in ankylosing spondylitis: a single-institution experience. Trungu Sokol, Ricciardi Luca, Forcato Stefano, Miscusi Massimo, Raco Antonino. Oct;2021 Neurosurgical Focus. 51(4):E8. doi: 10.3171/2021.7.focus21308. doi: 10.3171/2021.7.focus21308. [DOI] [PubMed] [Google Scholar]
- Fractures of the spine in diffuse idiopathic skeletal hyperostosis. Paley D., Schwartz M., Cooper P., Harris W.R., Levine A.M. 1991Clin Orthop Relat Res. (267):22–32. http://www.ncbi.nlm.nih.gov/pubmed/2044283 [PubMed]
- Diffuse idiopathic skeletal hyperostosis: musculoskeletal manifestations. Belanger Theodore A., Rowe Dale E. Jul;2001 Journal of the American Academy of Orthopaedic Surgeons. 9(4):258–267. doi: 10.5435/00124635-200107000-00006. doi: 10.5435/00124635-200107000-00006. [DOI] [PubMed] [Google Scholar]
- Fractures of the cervical spine in patients with ankylosing spondylitis. Surin Valdemar V. Jan;1980 Acta Orthopaedica Scandinavica. 51(1):79–84. doi: 10.3109/17453678008990772. doi: 10.3109/17453678008990772. [DOI] [PubMed] [Google Scholar]
- [Operative management of cervical spine injuries in patients with Bechterew’s disease] Lange U., Pape H.-C., Bastian L., Krettek C. Jan;2005 Der Unfallchirurg. 108(1):63–68. doi: 10.1007/s00113-004-0793-z. doi: 10.1007/s00113-004-0793-z. [DOI] [PubMed] [Google Scholar]
- Ankylosing spondylitis and spinal cord injury: origin, incidence, management, and avoidance. Jacobs W. Bradley, Fehlings Michael G. Jan;2008 Neurosurgical Focus. 24(1):E12. doi: 10.3171/foc/2008/24/1/e12. doi: 10.3171/foc/2008/24/1/e12. [DOI] [PubMed] [Google Scholar]
- Ankylosing Spondylitis: Patterns of Spinal Injury and Treatment Outcomes. Altun Idiris, Yuksel Kasım Zafer. 2016Asian Spine Journal. 10(4):655–62. doi: 10.4184/asj.2016.10.4.655. doi: 10.4184/asj.2016.10.4.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spine Fractures in Ankylosing Diseases: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU) Reinhold Maximilian, Knop Christian, Kneitz Christian, Disch Alexander. Sep;2018 Global Spine Journal. 8(2Suppl):56S–68S. doi: 10.1177/2192568217736268. doi: 10.1177/2192568217736268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Management of spinal fractures in patients with ankylosing spondylitis. El Tecle Najib E., Abode-Iyamah Kingsley O., Hitchon Patrick W., Dahdaleh Nader S. Dec;2015 Clinical Neurology and Neurosurgery. 139:177–182. doi: 10.1016/j.clineuro.2015.10.014. doi: 10.1016/j.clineuro.2015.10.014. [DOI] [PubMed] [Google Scholar]
- A retrospective study of treating thoracolumbar spine fractures in ankylosing spondylitis. Lu Meng-Ling, Tsai Tsung-Ting, Lai Po-Liang, Fu Tsai-Sheng, Niu Chi-Chien, Chen Lih-Huei, Chen Wen-Jer. 2014European Journal of Orthopaedic Surgery & Traumatology. 24(Suppl1):S117–123. doi: 10.1007/s00590-013-1375-y. doi: 10.1007/s00590-013-1375-y. [DOI] [PubMed] [Google Scholar]
- Spinal Fractures in Patients With Ankylosing Spondylitis: Etiology, Diagnosis, and Management. Werner Brian C., Samartzis Dino, Shen Francis H. Apr;2016 Journal of the American Academy of Orthopaedic Surgeons. 24(4):241–249. doi: 10.5435/jaaos-d-14-00149. doi: 10.5435/jaaos-d-14-00149. [DOI] [PubMed] [Google Scholar]
- Fractures of the thoracic and lumbar spine in ankylosing spondylitis. Thorngren Karl-Gran, Liedberg Einar, Aspelin Peter. Apr;1981 Archives of Orthopaedic and Traumatic Surgery. 98(2):101–107. doi: 10.1007/bf00460796. doi: 10.1007/bf00460796. [DOI] [PubMed] [Google Scholar]
- Multiple spine fractures in ankylosing spondylitis. Osgood CARROLL P., Abbasy MUNIR, Mathews THOMAS. Feb;1975 The Journal of Trauma: Injury, Infection, and Critical Care. 15(2):163–166. doi: 10.1097/00005373-197502000-00011. doi: 10.1097/00005373-197502000-00011. [DOI] [PubMed] [Google Scholar]
- Shen Francis H., Samartzis Dino. Spine. 15. Vol. 32. Ovid Technologies (Wolters Kluwer Health); Successful nonoperative treatment of a three-column thoracic fracture in a patient with ankylosing spondylitis: existence and clinical significance of the fourth column of the spine; pp. E423–E427. [DOI] [PubMed] [Google Scholar]
- Successful Nonoperative Treatment of a Lumbar Spine Extension Injury with Disruption of all Three Bony Columns in a Patient with Ankylosing Spondylitis – A Case Report. Faqeeh Ali, Yen David. Dec 29;2017 The Open Neurology Journal. 11(1):92–97. doi: 10.2174/1874205x01711010092. doi: 10.2174/1874205x01711010092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinal fractures in the setting of diffuse idiopathic skeletal hyperostosis conservatively treated via orthosis: illustrative cases. Taher Ayman W., Page Paul S., Greeneway Garret P., Ammanuel Simon, Bunch Katherine M., Meisner Lars, Hanna Amgad, Josiah Darnell. May 16;2022 Journal of Neurosurgery: Case Lessons. 3(20):14–17. doi: 10.3171/case21689. doi: 10.3171/case21689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The management of spinal injuries in patients with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis: a comparison of treatment methods and clinical outcomes. Whang Peter G., Goldberg Grigory, Lawrence James P., Hong Joseph, Harrop James S., Anderson David Greg, Albert Todd J., Vaccaro Alexander R. Apr;2009 Journal of Spinal Disorders & Techniques. 22(2):77–85. doi: 10.1097/bsd.0b013e3181679bcb. doi: 10.1097/bsd.0b013e3181679bcb. [DOI] [PubMed] [Google Scholar]
- Failure of conservative treatment for thoracic spine fracture in ankylosing spondylitis: delayed neurological deficit due to spinal epidural hematoma. Aoki Yasuchika, Yamagata Masatsune, Ikeda Yoshikazu, Nakajima Fumitake, Nakajima Arata, Nakagawa Koichi, Ohtori Seiji, Inaoka Tsutomu, Takahashi Kazuhisa. Sep;2013 Modern Rheumatology. 23(5):1008–1012. doi: 10.3109/s10165-012-0726-6. doi: 10.3109/s10165-012-0726-6. [DOI] [PubMed] [Google Scholar]
- Clinical features and outcomes of spine surgery in patients with ankylosing spondylitis. Nakao Yuki, Sakuraba Koji, Harimaya Katsumi, Terada Kazuo, Kobara Nobuo, Kawaguchi Ken-Ichi, Hayashida Mitsumasa, Iida Keiichiro, Nakashima Yasuharu, Fukushi Jun-Ichi. Dec 5;2022 Modern Rheumatology. 34(1):208–213. doi: 10.1093/mr/roac142. doi: 10.1093/mr/roac142. [DOI] [PubMed] [Google Scholar]
- Thoracolumbar fractures in ankylosing spondylitis: High-risk injuries. Trent G., Armstrong G. W. D., O'Neil J. Feb;1988 Clinical Orthopaedics and Related Research. 227:61–66. doi: 10.1097/00003086-198802000-00009. doi: 10.1097/00003086-198802000-00009. [DOI] [PubMed] [Google Scholar]
- Fracture in ankylosing spondylitis after minor trauma: radiological pitfalls and treatment by percutaneous instrumentation. A case report. Charles Y.P., Buy X., Gangi A., Steib J.-P. Feb;2013 Orthopaedics & Traumatology: Surgery & Research. 99(1):115–119. doi: 10.1016/j.otsr.2012.09.018. doi: 10.1016/j.otsr.2012.09.018. [DOI] [PubMed] [Google Scholar]
- Minimally Invasive Surgery for Traumatic Fractures in Ankylosing Spinal Diseases. Nayak Nikhil R., Pisapia Jared M., Abdullah Kalil G., Schuster James M. Jan 7;2015 Global Spine Journal. 5(4):266–273. doi: 10.1055/s-0034-1397341. doi: 10.1055/s-0034-1397341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caron Troy, Bransford Richard, Nguyen Quynh, Agel Julie, Chapman Jens, Bellabarba Carlo. Spine. 11. Vol. 35. Ovid Technologies (Wolters Kluwer Health); Spine fractures in patients with ankylosing spinal disorders; pp. E458–E464. [DOI] [PubMed] [Google Scholar]
- Iatrogenic fractures in ankylosing spondylitis—a report of two cases. Ruf Michael, Rehm Sascha, Poeckler-Schoeniger Christiane, Merk Harry R., Harms Juergen. 2006European Spine Journal. 15(1):100–104. doi: 10.1007/s00586-005-0973-8. doi: 10.1007/s00586-005-0973-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surgical Management Thoracolumbar Fractures in Patients with Ankylosing Spondylitis: Technical Note with Case Series. Börekci Ali, Kuru Bektaşoğlu Pınar, Ramazanoğlu Ali Fatih, Hazneci Jülide, Gürer Bora, Hakan Tayfun, Çelikoğlu Erhan. Aug;2023 World Neurosurgery. 176:3–9. doi: 10.1016/j.wneu.2023.04.054. doi: 10.1016/j.wneu.2023.04.054. [DOI] [PubMed] [Google Scholar]
- Surgical management of lower cervical spine fracture in ankylosing spondylitis. Shen Francis H., Samartzis Dino. Oct;2006 The Journal of Trauma: Injury, Infection, and Critical Care. 61(4):1005–1009. doi: 10.1097/01.ta.0000208125.63010.04. doi: 10.1097/01.ta.0000208125.63010.04. [DOI] [PubMed] [Google Scholar]
- Surgical treatment of lumbar hyperextension injury in ankylosing spondylitis. Lee Jung Keun, Park Ki Seok, Park Moon Sun, Kim Seong Min, Chung Seung Young, Lee Do Sung. 2013Korean Journal of Spine. 10(3):195–9. doi: 10.14245/kjs.2013.10.3.195. doi: 10.14245/kjs.2013.10.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neurological complications of ankylosing spondylitis. Fox Mark W., Onofrio Burton M., Kilgore John E. Jun;1993 Journal of Neurosurgery. 78(6):871–878. doi: 10.3171/jns.1993.78.6.0871. doi: 10.3171/jns.1993.78.6.0871. [DOI] [PubMed] [Google Scholar]
- McVeigh Claire M, Cairns Andrew P. BMJ. 7568. Vol. 333. BMJ; Diagnosis and management of ankylosing spondylitis; pp. 581–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anesthesia for ankylosing spondylitis patients undergoing transpedicle vertebrectomy. Lin B.C., Chen I.H. 1999Acta Anaesthesiol Sin. 37(2):73–78. http://www.ncbi.nlm.nih.gov/pubmed/10410406 [PubMed] [Google Scholar]
- Ankylosing Spinal Disease—Diagnosis and Treatment of Spine Fractures. Vazan Martin, Ryang Yu-Mi, Barz Melanie, Török Elisabeth, Gempt Jens, Meyer Bernhard. Mar;2019 World Neurosurgery. 123:e162–e170. doi: 10.1016/j.wneu.2018.11.108. doi: 10.1016/j.wneu.2018.11.108. [DOI] [PubMed] [Google Scholar]
- Kurucan Etka, Bernstein David N., Mesfin Addisu. Journal of Spine Surgery. 3. Vol. 4. AME Publishing Company; Surgical management of spinal fractures in ankylosing spondylitis; pp. 501–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoracic hyperextension injury with opening wedge distraction fracture in DISH -consideration of surgical strategy based on intraoperative pathological findings- Kanematsu Ryo, Hanakita Junya, Takahashi Toshiyuki, Tomita Yosuke, Minami Manabu. May;2020 Journal of Clinical Neuroscience. 75:231–234. doi: 10.1016/j.jocn.2020.03.012. doi: 10.1016/j.jocn.2020.03.012. [DOI] [PubMed] [Google Scholar]
- Spinal fractures in diffuse idiopathic skeletal hyperostosis: Advantages of percutaneous pedicle screw fixation. Okada Eijiro, Shiono Yuta, Nishida Mitsuhiro, Mima Yuichiro, Funao Haruki, Shimizu Kentaro, Kato Masanori, Fukuda Kentaro, Fujita Nobuyuki, Yagi Mitsuru, Nagoshi Narihito, Tsuji Osahiko, Ishii Ken, Nakamura Masaya, Matsumoto Morio, Watanabe Kota. May;2019 Journal of Orthopaedic Surgery. 27(2):1–8. doi: 10.1177/2309499019843407. doi: 10.1177/2309499019843407. [DOI] [PubMed] [Google Scholar]
- Risk of cement leakage and pulmonary embolism by bone cement-augmented pedicle screw fixation of the thoracolumbar spine. Janssen Insa, Ryang Yu-Mi, Gempt Jens, Bette Stefanie, Gerhardt Julia, Kirschke Jan S., Meyer Bernhard. Jun;2017 The Spine Journal. 17(6):837–844. doi: 10.1016/j.spinee.2017.01.009. doi: 10.1016/j.spinee.2017.01.009. [DOI] [PubMed] [Google Scholar]
- Li Bo, Guo Rui, Jiang Xu, Wu Jionglin, Zhang Di, Yang Canchun, Zhao Qiancheng, Zhang Chi, Yan Haolin, Wang Zheyu, Wang Qiwei, Huang Renyuan, Zhang Zhilei, Hu Xumin, Gao Liangbin. Annals of Palliative Medicine. 6. Vol. 10. AME Publishing Company; Posterior wedge osteotomy assisted by O-arm navigation for treating ankylosing spondylitis with thoracolumbar fractures: an early clinical evaluation; pp. 6694–6705. [DOI] [PubMed] [Google Scholar]
- Yeoh David, Moffatt Tapiwa, Karmani Shuiab. Injury. 10. Vol. 45. Elsevier BV; Good outcomes of percutaneous fixation of spinal fractures in ankylosing spinal disorders; pp. 1534–1538. [DOI] [PubMed] [Google Scholar]
- Wänman Johan, Burmeister Fabian, Thorell David, Kyrk Tobias, Blixt Simon, Gerdhem Paul, Mukka Sebastian, Bobinski Lukas. International Journal of Spine Surgery. 4. Vol. 17. International Journal of Spine Surgery; Minimally Invasive Surgery for Thoracolumbar Spinal Fractures in Patients With Ankylosing Spondylitis; pp. 526–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Percutaneous surgery for thoraco-lumbar fractures in ankylosing spondylitis: Study of 31 patients. Bredin S., Fabre-Aubrespy M., Blondel B., Falguières J., Schuller S., Walter A., Fuentes S., Tropiano P., Steib J.-P., Charles Y.-P. Dec;2017 Orthopaedics & Traumatology: Surgery & Research. 103(8):1235–1239. doi: 10.1016/j.otsr.2017.07.023. doi: 10.1016/j.otsr.2017.07.023. [DOI] [PubMed] [Google Scholar]
- Kai Kazuhiro, Ikuta Ko, Masuda Keigo, Kitamura Takahiro, Senba Hideyuki, Shidahara Satoshi. Asian Spine Journal. 3. Vol. 12. Asian Spine Journal (ASJ); Surgical Outcomes of Minimally Invasive Stabilization for Spinal Fractures in Patients with Ankylosing Spinal Disorders; pp. 434–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedney Cara L., Daffner Scott D., Obafemi-Afolabi Abimbola, Gelb Daniel, Ludwig Steven, Emery Sanford E., France John C. International Journal of Spine Surgery. 23. Vol. 10. International Journal of Spine Surgery; A Comparison of Open and Percutaneous Techniques in the Operative Fixation of Spinal Fractures Associated with Ankylosing Spinal Disorders; p. 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Open versus Minimally Invasive Fixation Techniques for Thoracolumbar Trauma: A Meta-Analysis. McAnany Steven J., Overley Samuel C., Kim Jun S., Baird Evan O., Qureshi Sheeraz A., Anderson Paul A. 2016Global Spine Journal. 6(2):186–194. doi: 10.1055/s-0035-1554777. doi: 10.1055/s-0035-1554777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perioperative complications in open versus percutaneous treatment of spinal fractures in patients with an ankylosed spine. Moussallem Charbel D., McCutcheon Brandon A., Clarke Michelle J., Cui Quanqi, Currier Bradford L., Yaszemski Michael J., Huddleston Paul M., Rose Peter S., Freedman Brett, Dekutoski Mark B., Bydon Mohamad, Nassr Ahmad. Aug;2016 Journal of Clinical Neuroscience. 30:88–92. doi: 10.1016/j.jocn.2016.01.020. doi: 10.1016/j.jocn.2016.01.020. [DOI] [PubMed] [Google Scholar]
- Surgical treatment of thoracolumbar fracture in ankylosing spondylitis: A comparison of percutaneous and open techniques. Ye Jing Yao, Jiang Ping, Guan Hua Peng, Wei Chuan Fu, Li Sen, Jia Meng Long, Li Nian Hu. Nov 24;2022 Journal of Orthopaedic Surgery and Research. 17(1):1–11. doi: 10.1186/s13018-022-03378-w. doi: 10.1186/s13018-022-03378-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Percutaneous management of thoracolumbar burst fractures: Evolution of techniques and strategy. Blondel B., Fuentes S., Pech-Gourg G., Adetchessi T., Tropiano P., Dufour H. Sep;2011 Orthopaedics & Traumatology: Surgery & Research. 97(5):527–532. doi: 10.1016/j.otsr.2011.03.020. doi: 10.1016/j.otsr.2011.03.020. [DOI] [PubMed] [Google Scholar]
- Pedicle screw insertion accuracy with different assisted methods: a systematic review and meta-analysis of comparative studies. Tian Nai-Feng, Huang Qi-Shan, Zhou Ping, Zhou Yang, Wu Rui-Kai, Lou Yi, Xu Hua-Zi. 2011European Spine Journal. 20(6):846–859. doi: 10.1007/s00586-010-1577-5. doi: 10.1007/s00586-010-1577-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi William W., Green Barth A., Levi Allan D. O. Neurosurgery. 4. Vol. 47. Ovid Technologies (Wolters Kluwer Health); Computer-assisted fluoroscopic targeting system for pedicle screw insertion; pp. 872–878. [DOI] [PubMed] [Google Scholar]
- Kulkarni ARVIND G., Agarwal VARUN K., Kumar NANDISH KC, Kumar AVINASH, Patel ANKIT. International Journal of Spine Surgery. 2. Vol. 13. International Journal of Spine Surgery; Is Long-Segment Fixation a Rule in Fractures Associated With Ankylosing Spondylitis? pp. 215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Hao, Zhou Quan, Zhang Junxin, Deng Lei, Hu Xiayu, He Wei, Liu Tao, Yang Huilin. Frontiers in Surgery. July. Vol. 9. Frontiers Media SA; Kyphoplasty for thoracic and lumbar fractures with an intravertebral vacuum phenomenon in ankylosing spondylitis patients; pp. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Gang Deuk, Chae Soo Uk, Kim Yeung Jin, Choi Deok Hwa. Journal of Bone Metabolism. 1. Vol. 20. Korean Society for Bone and Mineral Research; Osteoporotic Lumbar Compression Fracture in Patient with Ankylosing Spondylitis Treated with Kyphoplasty; p. 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OSTEOPOROTIC VERTEBRAL FRACTURE IN DISH REQUIRES VERTEBROPLASTY COMBINED WITH POSTERIOR LONG FUSION: GP248. Terai H, Toyoda H, Suzuki A, Dozono S, Nakamura H. 2011
- Hartman Jason, Granville Michelle, Berti Aldo, Jacobson Robert E. Cureus. Springer Science and Business Media LLC; An Unusual Vertical T12 Fracture Extending into the T12-L1 Disc in a Patient with Diffuse Idiopathic Spondylotic Hyperostosis: A Case Study Using Vertebroplasty to Stabilize the Fracture. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Wenhao, Huang Yixue, Zhang Linlin, Yang Huilin. Frontiers in Surgery. July. Vol. 9. Frontiers Media SA; Percutaneous kyphoplasty for the treatment of diffuse idiopathic skeletal hyperostosis with vertebral fractures: A case report and treatment review; pp. 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prognostic factors of balloon kyphoplasty for osteoporotic vertebral fractures with diffuse idiopathic skeletal hyperostosis. Tsuchikawa Yuji, Kamei Naosuke, Yamada Kiyotaka, Nakamae Toshio, Adachi Nobuo, Fujimoto Yoshinori. Mar 1;2023 Journal of Neurosurgery: Spine. 39(1):75–81. doi: 10.3171/2023.2.spine2392. doi: 10.3171/2023.2.spine2392. [DOI] [PubMed] [Google Scholar]
- Robotic-assisted device in posterior spinal fusion for a high risk thoraculombar fracture in ankylosing spondylitis. Suliman Ali, Wollstein Ronit, Bernfeld Benjamin, Bruskin Alexander. 2014Asian Spine Journal. 8(1):64–68. doi: 10.4184/asj.2014.8.1.64. doi: 10.4184/asj.2014.8.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Combined pedicle screw fixation at the fracture vertebrae versus conventional method for thoracolumbar fractures: A meta-analysis. Zhang Conghui, Liu Yang. May;2018 International Journal of Surgery. 53:38–47. doi: 10.1016/j.ijsu.2018.03.002. doi: 10.1016/j.ijsu.2018.03.002. [DOI] [PubMed] [Google Scholar]
- [Treatment of ankylosing spondylitis with thoracolumbar fractures by robot-assisted internal fixation in lateral decubitus position] Shi Y F, Shen Z K, Chen B, Zhou X, Dai J P. 202235(2):113–117. doi: 10.12200/j.issn.1003-0034.2022.02.004. [DOI] [PubMed] [Google Scholar]


