Abstract
Amyotrophic lateral sclerosis (ALS) is a fatal, severely debilitating and rapidly progressing disorder affecting motor neurons in the brain, brainstem, and spinal cord. Unfortunately, there are few effective treatments, thus there remains a critical need to find novel interventions that can mitigate against its effects. Whilst the aetiology of ALS remains unclear, ageing is the major risk factor. Ageing is a slowly progressive process marked by functional decline of an organism over its lifespan. However, it remains unclear how ageing promotes the risk of ALS. At the molecular and cellular level there are specific hallmarks characteristic of normal ageing. These hallmarks are highly inter-related and overlap significantly with each other. Moreover, whilst ageing is a normal process, there are striking similarities at the molecular level between these factors and neurodegeneration in ALS. Nine ageing hallmarks were originally proposed: genomic instability, loss of telomeres, senescence, epigenetic modifications, dysregulated nutrient sensing, loss of proteostasis, mitochondrial dysfunction, stem cell exhaustion, and altered inter-cellular communication. However, these were recently (2023) expanded to include dysregulation of autophagy, inflammation and dysbiosis. Hence, given the latest updates to these hallmarks, and their close association to disease processes in ALS, a new examination of their relationship to pathophysiology is warranted. In this review, we describe possible mechanisms by which normal ageing impacts on neurodegenerative mechanisms implicated in ALS, and new therapeutic interventions that may arise from this.
Keywords: Ageing, ALS, Neurodegenerative diseases, Molecular hallmarks
Introduction
Amyotrophic lateral sclerosis (ALS) is a relentlessly fatal and rapidly progressing disorder affecting motor neurons in the brain, brainstem, and spinal cord, resulting in gradual muscle paralysis. With a poor prognosis and severely debilitating symptoms it is important to identify the underlying mechanisms that trigger ALS. The average age of diagnosis of ALS is 55 years, and ageing is its biggest risk factor. Ageing is a slowly progressive, continuous decline in the normal function of an organism over its lifespan. It is also marked by an increased sensitivity to ageing-related diseases and increased risk of death. Importantly, the World Health Organization (WHO) estimates that the proportion of the global population over 60 years will nearly double (12% to 22%) from 2015 and 2050, implying that the incidence of age-related neurodegenerative diseases such as ALS will increase significantly in the coming decades. However, it is important to note that these estimations may be revised in the future due to the unique circumstances and challenges posed by the COVID-19 pandemic. We are currently living in the United Nations Decade of Healthy Ageing (2021–2030), a global collaboration led by the WHO, recognising the importance of ageing to health. It is also essential to note the difference between lifespan (total number of years an individual survives from birth until death) and healthspan (total number of years an individual remains healthy, without chronic disease). Thus, healthy ageing should also consider healthspan as well as lifespan.
It is well-established that changes in the morphology and function of the brain are present during ageing, involving weight and volume decreases, loss of white and grey matter, and the degeneration of neurites and synapses [1]. Whilst the effect of normal ageing on the spinal cord remains poorly studied in comparison, significant alterations have been described, including the loss of alpha motor neurons (α-MNs)[2], reminiscent of ALS. Muscle cells, like motor neurons, also display many of the classic hallmarks of ageing.
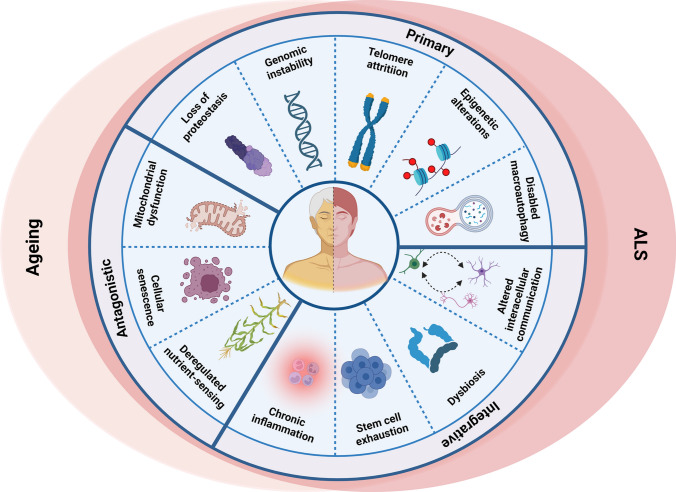
Whilst ageing itself is a normal process, there are striking similarities between neurodegeneration and normal ageing at the molecular and cellular level, because the specific ‘hallmarks’ associated with ageing [3] overlap significantly with pathophysiological mechanisms implicated in ALS (Fig. 1). However, it remains poorly defined how exactly ageing promotes the increased risk of ALS. The molecular and cellular hallmarks of ageing have been recently updated [3]. Hence, a new examination of the relationship between ageing and neurodegeneration in the pathophysiology of ALS is warranted and is the subject of this review.
Fig. 1.
Molecular hallmarks of ageing in ALS. The molecular hallmarks of ageing denote a collection of inter-connected molecular and cellular features that are widely linked to the ageing process in diverse tissues and organisms. These mechanisms offer a framework for comprehending the intricacies of ageing. Strikingly, the molecular hallmarks of ageing exhibit notable similarities and substantially overlap with the pathophysiological mechanisms described in ALS
Ageing and neurodegeneration
Ageing occurs with time in all organisms, although it progresses at different rates within a species. The differences between individuals are due to variations in genetic makeup, environment, lifestyle, and adaptation [4, 5] and are evident on an organismal, organ, cellular and molecular level. We provide below a brief overview of the major theories of ageing.
Theories of ageing
Whilst the factors that control human lifespan remain unclear, current theories of ageing mainly fall into two broad categories. The ‘Programmed Theory’ proposes that normal ageing follows a biological timetable (similar to that regulating childhood growth) that results in changes in expression of genes involved in cellular maintenance [6]. In contrast, the ‘Damage or Error’ theory suggests that ageing is the result of progressive damage to cells and organs over time [6]. However, currently there is no consensus on the causes of ageing in humans. Moreover, many of the cellular mechanisms implicated in ageing interact extensively and thus may act together to accelerate the underlying molecular processes.
The programmed theory of ageing
The programmed theory of ageing can be further divided into three subtypes. The ‘Programmed Longevity’ theory implies that ageing results from changes in gene expression, leading to age-associated deficits and a subsequent cellular senescent phenotype [7]. Secondly the ‘Endocrine Theory’ proposes that hormones act as biological clocks to control the rate of ageing [8]. Thirdly, the ‘Immunological Theory’ states that the function of the immune system is at its peak during puberty, but it declines thereafter, resulting in an increased susceptibility to inflammation [9].
Damage or error theory of ageing
The ‘Damage or Error’ Theory of ageing can be further divided into five subtypes. First, the ‘Wear and Tear’ theory proposes that cellular components naturally wear out over time from consistent repeated usage [6]. Second, the ‘Rate of Living’ theory states that the lifespan of an organism becomes shorter with higher rates of basal oxygen consumption [10, 11]. Third, the ‘Cross Linking Theory’ [12] proposes that proteins become cross-linked and then aggregate over time [12, 13]. The ‘Free Radical’ theory [14, 15] suggests that superoxide and other free radicals accumulate and damage cellular components (nucleic acids, lipids, sugars, and proteins) during ageing [15]. Whilst antioxidants counteract this to some extent, eventually this becomes ineffective during normal ageing [15]. Finally, the ‘Somatic DNA Damage’ theory proposes that DNA damage occurs continuously in cells. Whilst these lesions are initially repaired, increasing damage over time results in mutations, which impair genome integrity and thus cellular function. Damage to both nuclear and mitochondrial DNA is implicated in this process [16].
Genetics and ageing in ALS
It remains unclear how ageing increases the risk of ALS, but it probably involves a combination of genetic, environmental, and age-related factors [17]. Whilst most (~ 90%) ALS cases arise sporadically, the remaining proportion are familial, and can provide insights into the underlying pathophysiology [17]. Hexanucleotide repeat expansions (GGGGCC) in the first intron of chromosome 9 open reading frame 72 (C9ORF72) gene are the most common genetic cause of both familial (~ 40%) and sporadic ALS (~ 8–10%), as well as the related condition, frontotemporal dementia (FTD), both sporadic (~ 5–10%) and familial forms (~ 25–30%) [18]. FTD primarily affects the frontal and temporal lobes of brain and patients exhibit a combination of cognitive, behavioural, and/or motor symptoms, although these can vary widely [19]. Some individuals with FTD may also develop symptoms of ALS and vice versa, referred to as 'ALS-FTD' [20]. Hence, there is significant genetic and pathological overlap between ALS and FTD. Three main mechanisms are implicated in neurodegeneration induced by hexanucleotide C9ORF72 mutations; production of toxic RNA, non-AUG translation (RAN) to produce dipeptide repeat proteins (DPRs) and haploinsufficiency due to lack of C9ORF72 protein [21].
Mutations in the genes encoding superoxide dismutase 1 (SOD1) and TAR DNA-binding protein 43 (TDP-43) cause another ~ 20% and ~ 4% cases respectively of familial ALS cases [22–24]. TDP-43 is an RNA/DNA binding protein normally located primarily in the nucleus. However, the presence of pathological forms of TDP-43, involving its truncation, abnormal aggregation, and mislocalization to the cytoplasm, are the characteristic hallmark of almost all (~ 97%) ALS cases [25]. Fused in Sarcoma (FUS) is another RNA-binding protein with structural and functional similarities to TDP-43 and mutations in FUS also cause ~ 4% cases [26]. Over 30 other genes have been linked to familial ALS, though each account for a smaller proportion of cases. These genes include CCNF, CHCHD10, ATXN2, KIF5A, hnRNPA2/B1, UBQLN2, TBK1. OPTN, PRPH, NEK1, VCP, and PFN1, among others [17, 27, 28].
Whilst ALS involves the degeneration and death of motor neurons, glial cells, which provide important supportive roles to neurons, also contribute to pathophysiology via non-cell autonomous mechanisms. Astrocytes regulate blood flow within the CNS, recycle neurotransmitters, and form the blood brain barrier. Microglia function in phagocytosis, the immune response, neuroinflammation, and immune surveillance and activation. Thus they act as the immune cells of the CNS [29]. Oligodendrocytes myelinate neuronal axons within the CNS to facilitate synaptic transmission and provide metabolic support to neurons, and Schwann cells myelinate neuronal axons in the peripheral nervous system (PNS). The latter cells also perform important roles in maintaining the function of the neuromuscular junction (NMJ) [30].
The clinical manifestations in ALS are driven by loss of voluntary muscle function, facilitated normally by motor neurons at the NMJ [31, 32]. Previously, ALS was considered to affect motor neurons primarily, and the involvement of skeletal muscle was thought to be a secondary consequence. However, the role of muscle in the pathogenesis of ALS is gaining increasing recognition (reviewed recently [33]).
Molecular hallmarks of ageing in ALS
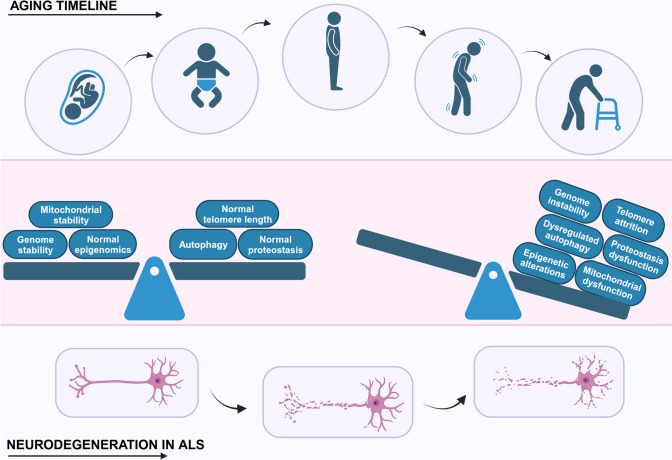
The molecular and cellular hallmarks of ageing are defined by specific criteria [3]; (a) a hallmark should alter in a time-dependent fashion during the ageing process, (b) it should be enhanced by experimental acceleration of ageing, and (c) modulating the hallmark should inhibit, halt or even reverse ageing. Nine ageing hallmarks were originally proposed (in 2013) [3]: genomic instability, loss of telomeres, senescence, epigenetic modifications, dysregulated nutrient sensing, loss of proteostasis, mitochondrial dysfunction, stem cell exhaustion, and altered intercellular communication. However, these hallmarks were recently (2023) [3] expanded to include dysregulation of autophagy, inflammation and dysbiosis. It is important to note however that these twelve age-related hallmarks overlap significantly and are highly inter-related, with much crosstalk between these pathways (Fig. 1). Several are implicated as ‘primary’ hallmarks and drivers of the ageing process [3], including genomic instability, telomere dysfunction, epigenetic dysregulation, and proteostasis dysregulation (Fig. 2). In contrast, the ‘antagonistic’ hallmarks refer to cellular reactions to damage, including nutrient-sensing, mitochondrial dysfunction, and senescence. Finally, the ‘integrative’ hallmarks reflect the lack of ability of the cell to cope with the age-associated damage, involving defects in inter-cellular communication, stem cell exhaustion and dysbiosis. Below, we detail each of the twelve hallmarks, and how these relate to mechanisms of neurodegeneration in ALS.
Fig. 2.
Primary drivers of ageing and ALS. Ageing and neurodegeneration in ALS are complex processes influenced by a combination of genetic, environmental, and cellular factors. Whilst the precise causes of both ageing and ALS are not fully understood, genomic instability, telomere attrition, epigenetic alterations, proteostasis dysfunction, dysregulated autophagy and mitochondrial dysfunction are thought to be primary drivers
Primary hallmarks of ageing and how they relate to ALS
Genomic instability
Genomic instability refers to the high frequency of mutations within the genome [34]. This can result from both exogenous and endogenous sources, such as environmental agents and DNA replication errors, respectively. The DNA damage response (DDR) refers to the signalling pathways that normally detect and repair DNA damage, and the efficiency of DNA repair decreases during ageing [3]. Genomic instability results from either alterations in the nuclear architecture, damage to nuclear and/or mitochondrial DNA, and defective DNA repair mechanisms [35]. However, whilst genomic instability increases significantly with ageing, direct evidence showing that it modulates ageing specially is lacking.
Nuclear architecture alterations
The architecture of the nucleus maintains multiple aspects of genome stability. This primarily involves the nuclear lamina, a filamentous scaffold mesh underneath the nuclear envelope that tethers proteins and chromatin. Nuclear lamin proteins are its main constituents, and they are strongly associated with ageing and genome stability. Importantly, mutations in the genes encoding several of these proteins cause accelerated ageing disorders such as Hutchinson–Gilford progeria syndrome (HGPS, or progeria) [36, 37], which results from an abnormal truncated form of Lamin A (progerin), that also accumulates normally with age [38]. Dysregulation of Lamin B1 disrupts the shelterin complex and drives telomere instability in human cells [39].
Defects to the nucleus and impairment of nucleocytoplasmic transport are well-described in ALS. Nuclear pore pathology is detected in brains of sporadic ALS, TDP-43 and C9ORF72 patients [40]. Pathological forms of TDP-43 disrupt the nuclear architecture and nuclear pore complexes in ALS [40]. ALS-associated variant FUSR521G interacts with nucleoporins, which form the nuclear pore complex, and disrupts nucleocytoplasmic transport [41]. The C9ORF72 RNA and DPRs also interact with and disrupt various components of the nuclear transport machinery such as nuclear transport receptors, Ran GTPase, nucleoporins and nuclear envelope proteins [42]. However, nuclear morphology is unaltered in C9ORF72 ALS/FTD [43]. Loss of the nucleoporin NUP50 has been implicated as a risk factor for ALS [44]. Mutations in loss of never-in-mitosis A (NIMA)-related kinase-1 (NEK1) in induced pluripotent stem cell (iPSC) derived motor neurons also disrupt the nuclear architecture and import of proteins [45].
Damage to nuclear DNA
Cells are highly prone to DNA damage and insults arise at a rate of tens of thousands per day per cell [34]. Somatic mutations normally accumulate over time and the rate of formation is inversely correlated with lifespan [3]. During normal ageing, the efficiency of DNA repair mechanisms declines, resulting in the accumulation of DNA damage [35]. Furthermore, mutations in several DNA repair proteins cause several human progeroid disorders, directly linking DNA repair deficiencies to ageing. Double-stranded DNA breaks (DSBs) are the most toxic type of damage, which in neurons are repaired primarily by the error-prone non-homologous end-joining (NHEJ) mechanism. Neurons are also prone to oxidative DNA damage, which is repaired by base excision repair (BER) [46].
There is now extensive evidence for DNA damage in the pathophysiology of ALS. Several proteins central to ALS, including C9ORF72, FUS, TDP-43, SOD1, NEK1, C21orf2, senataxin, and valosin containing protein 1 (VCP), are known to function in DNA repair [47]. We and others have shown that TDP-43 is recruited to γH2AX foci where it functions in NHEJ [48], interacts with Ku 70 and is implicated in the repair of R loops [49, 50]. FUS interacts with histone deacetylase 1 (HDAC1) to repair DSBs [51] and it also functions in BER by mediating PARP1-dependent recruitment of XRCC1/DNA Ligase IIIα (LigIII). C21orf72 interacts with NEK1 and is thought to be involved in DSB repair [52–54]. VCP and senataxin are also involved in the maintenance of genomic integrity by facilitating transcription, DNA replication and the DDR [55, 56].
DNA damage is also induced by pathological forms of the same proteins in ALS [57]. ALS-mutant TDP-43 displays impaired activity in NHEJ, which disrupts R-loop homeostasis and induces TDP-43 pathology [48, 58]. TDP-43 pathology is associated with genome instability, encompassing splicing changes, somatic mutations, and gene fusions [59]. Loss of TDP-43 in the nucleus correlates with increased accumulation of DSBs [60, 61]. Similarly, ALS-associated mutant FUSR521C induces DNA damage and RNA splicing defects [62]. Loss of nuclear FUS impairs DNA nick ligation by inhibiting recruitment of XRCC1/LigIII [63], inducing aggregate formation and neurodegeneration [64]. In addition, ALS-associated variants of other proteins implicated in ALS also induce DNA damage. DNA repair genes are activated in response to DNA damage caused by SOD1G93A mutations in iPSC-derived motor neurons [65]. Hexanucleotide mutations in C9ORF72 induce DNA damage in neuronal cells, and motor neurons of ALS patients [66]. This has been associated with deficiencies in DSB and R loop repair and H2A ubiquitylation [67]. The C9ORF72 DPRs poly-glycine arginine (poly-GA) and poly-proline-arginine (poly-PA) induce DSBs, and phosphorylation of ataxia telangiectasia mutated (pATM) [68]. There is also evidence linking DNA repair defects to motor neuron loss. Ercc1Δ/− mice lacking DNA repair mechanisms nucleotide excision repair (NER), inter-strand crosslink repair, NHEJ and homologous recombination (HR) display aberrant motor neuron loss, microglia and astrocyte activation, Golgi apparatus dysfunction, genotoxic stress and NMJ pathology [69]. However, neither TDP-43 nor FUS pathology were detected in motor neurons in these mice, indicating that loss of Ercc1 alone is enough to induce ALS-related pathology [69, 70]. Together these data imply there is a strong correlation between ALS and DNA damage, raising the possibility that normal ageing increases genomic instability and thus the risk of neurodegeneration. However, this has not been shown directly.
Damage to mitochondrial DNA
Mitochondrial DNA (mtDNA) is particularly vulnerable to age-associated somatic mutations because of its proximity to oxidative phosphorylation sites and lack of protection by histones [71]. It accumulates oxidative damage in an age-dependent manner [71]. Furthermore, whilst mtDNA repair mechanisms are not as well-studied as those of nuclear DNA, they appear to be less efficient [71].
Mutations in mDNA and increased oxidative stress are implicated in both ageing and the development of ALS [72, 73]. Both wildtype TDP-43 and mutant TDP-43Q331K localise to mitochondria and trigger the release of mtDNA through the mitochondrial permeability transition pore [74]. The mtDNA accumulation then activates the cGAS/STING pathway, inducing neuroinflammation and neurodegeneration [74]. Cytoplasmic mtDNA is also present in spinal cords of ALS patients and iPSC-derived motor neurons [74]. Therefore, together these studies imply that damage to mtDNA is present in ALS, although this is not well-characterised.
Telomere attrition
Telomeres are non-coding repetitive DNA sequences (TTAGGG)n found at the distal ends of chromosomes that protect the integrity of the genome during replication. During normal ageing, the length of telomeres decreases, and rodents with short or long telomeres display inhibition or extension of lifespan, respectively [3]. Telomere shortening is thus one of the major features of ageing that is implicated in many age-related diseases [75]. Telomerase reverse transcriptase (TERT) prevents telomere shortening by maintaining telomere length [75], and whilst telomere shortening induces genomic instability and DNA damage, it is recognised as a separate hallmark of ageing [3].
Dysregulation in the length of telomeres has also been described in ALS. Knockout of telomerase leads to telomere shortening and an accelerated ALS phenotype in the SOD1G93A mice model [76]. In addition, age-dependent telomere shortening was detected in iPSC motor neurons from C9ORF72 patients [77]. However, a recent whole genome sequencing study concluded that longer telomeres are a risk factor for ALS and worsen prognosis, including in the brain [78]. Similarly, longer telomere length is associated with FTD [79]. Hence, it is possible that maintaining a balanced telomere length is essential in ALS and that alterations in telomere length, both lengthening and shortening, are both relevant to neurodegeneration. In contrast, genome wide association studies found no association between telomere length and ALS in leukocytes, implying that telomere length is cell-type specific [80]. Thus, these contrasting findings imply that more studies are required to characterise telomere length and activity in ALS.
Epigenetic alterations
Epigenetics refers to heritable changes in the regulation of gene expression independent of the DNA sequence. Multiple epigenetic modifications are known to alter during ageing [81], including DNA methylation, histone acetylation, chromatin remodelling and regulation of non-coding RNAs [81]. These alterations affect DNA replication and repair, gene transcription and silencing, cell division, and maintenance of telomere length [81]. DNA methylation on cytosine is one the most studied epigenetic modifications.
Chromatin, containing both genomic DNA and histones, regulates accessibility of the transcription machinery and thus gene expression. During ageing, chromatin alterations occur, including structural remodelling and changes in chromatin architecture, loss of histones and histone post-translational modifications. Histone acetylation is regulated by histone acetyltransferases (HATs) and histone deacetylases (HDACs) [82, 83]. Decreased global histone acetylation results in dysregulated metabolic gene expression and metabolic homeostasis [82]. Hyper-or hypo-acetylation of histones is regulated by HAT/HDAC homeostasis, and imbalance in this process induces defects in the integrated stress response and DNA repair mechanisms [84]. HDAC inhibitors have been implicated as a therapeutic strategy to prevent ageing [85].
There is increasing evidence for a role for epigenetic modifications in the pathogenesis of ALS, particularly in relation to the C9ORF72 repeat expansion [86]. Increased methylation of a CpG island near the GGGGCC repeat in the C9ORF72 promoter decreases C9ORF72 protein expression [87]. Furthermore, age-accelerated DNA methylation in the CpG-island 5′ is associated with more severe disease phenotype, early onset, and short disease duration in C9ORF72 patients [88]. Histones H3 and H4 undergo hyper-methylation of the promoter CpG-island [89] in ALS and FTD patients [90–93]. Hypermethylation also inhibits the formation of RNA foci and DPR aggregation in ALS [94]. Less nuclear 5-methyl cytosine (5mC) and 5hmC methylation was detected in lower motor neurons displaying TDP-43 pathology compared to those lacking pathology [95]. In addition, iPSC-derived motor neurons from ALS-associated FUS variants express more DNA methyltransferases and display more methylation in the FUS promoter region [96]. Studies in SOD1G93A mice also identified aberrant DNA and RNA methylation (increased or decreased) in spinal cords and skeletal muscles compared to control mice [97].
Epigenetic alterations to chromatin are also described in ALS. A chromatin remodelling complex, neuronal Brahma-related gene 1 (Brg1)-associated factor complex (nBAF), which in neurons regulates differentiation, dendritic expansion, and synaptic function, was lacking in cultured motor neurons expressing ALS-associated FUSR521G or TDP-43G348C [98]. Wildtype TDP-43 expression also disrupts chromatin dynamics due to impaired functioning of the chromatin remodelling enzyme CHD2 in Drosphilia [99]. HAT/HDAC homeostasis is altered in the brain and spinal cord of FUS-ALS patients [84]. HDAC inhibition using ACY-738 restores global histone acetylation, improves survival, and reduces metabolic abnormalities in a mouse model overexpressing wildtype FUS [100]. HDAC inhibitors have been examined extensively in ALS models (SOD1G93A mice, FUS and C9ORF72 mice models (detailed further in the "Therapeutic interventions for ageing and ageing-related diseases" section) [85, 101].
Loss of proteostasis
Protein homeostasis, or 'proteostasis', refers to the dynamic network of processes that regulate the protein synthesis, folding, trafficking and degradation machinery [102]. Proteostasis depends on the proper functioning of molecular chaperones, autophagy, the ubiquitin proteasome system (UPS), and endoplasmic reticulum (ER)-associated degradation (ERAD). Loss of proteostasis occurs if these protein quality control mechanisms fail and this can result in the accumulation of misfolded or aggregated proteins [103]. During normal ageing, the efficiency of proteostasis declines, and the consequent accumulation of damaged and aggregated misfolded proteins is a key hallmark of ageing and neurodegeneration. Lipofuscin aggregates—granules composed of misfolded proteins and lipids as a by-product of lysosomal digestion—also accumulate in motor neurons during normal ageing [104–106]. Proteins can also become post-translationally modified during ageing by oxidative damage from reactive oxygen species (ROS) or sugars, and the later modification results in the formation of advanced glycation end products (AGEs)[107]. The rate of protein translation decreases with age, and slowed translation elongation induces protein misfolding and ageing [108]. Proteostasis collapse refers to the breakdown or failure of the cellular machinery responsible for maintaining protein homeostasis and it is implicated as an important driver of cellular ageing in humans [103, 109].
The expression of protein chaperones such as the heat shock proteins (HSPs) decreases with ageing [110], implying that protein folding becomes impaired with increasing age. Administering recombinant human HSP70 to mice delays senescence, enhances proteasome activity and cognitive functions, reduces brain lipofuscin levels, and extends lifespan [111]. Feeding young fruit flies with AGEs and lipofuscin inhibits the UPS, which accelerates ageing and reduces lifespan [112]. Similarly, another chaperone, the oxidoreductase protein disulphide isomerase (PDI) is protective against cellular ageing in several models including replicative senescent human mesenchymal stem cells (RS hMSCs), HGPS hMSCs, Werner syndrome (WS) hMSCs and human primary hMSCs [113]. In addition, stabilising dysfunctional proteostasis using the chemical chaperone 4‐phenyl butyrate (PBA) improves cognitive behaviour and inhibits ageing [114].
The pathological ALS hallmark of misfolded protein aggregates strongly implicates proteostasis defects in pathophysiology [102]. Dysregulation of most proteostasis and protein quality control mechanisms are also well-described in ALS, including defects in autophagy, the UPS, ER-Golgi transport and ERAD [102]. Numerous molecular chaperones are also dysregulated in ALS including PDI proteins and HSPs [102]. PDI proteins have also been linked to ALS as a protective mechanism and as a genetic risk factor [115–118].
The formation of stress granules (SGs) is increasingly recognised in the maintenance of proteostasis [119]. SGs are cytoplasmic membrane-less organelles (also known as biomolecular condensates) composed of protein and RNA [120–123]. Functionally, they are implicated in the storage of biomolecules and as mRNA triage locations to regulate translation and the stability of mRNA [124, 125]. The formation of SGs is regulated by liquid phase separation (LLPS), the process by which proteins and nucleic acids in solution separate into liquid droplets (similar to droplets of oil forming in water) [126]. SGs assemble and disassemble in response to exogenous or environmental conditions, thus promoting survival during cellular stress [127]. LLPS is driven by proteins with intrinsically disordered domains, which includes misfolded proteins associated with ALS, including TDP-43 and FUS [128]. Recent studies have shown that SGs sequester misfolded proteins, preventing them from building up in the nucleus or cytoplasm, thus maintaining proteostasis [119]. However abnormal SGs disrupt proteostasis and during normal ageing defects in regulating the normal assembly/disassembly and dynamics of SGs is related to loss of proteostasis [33].
SGs are present in the pathological aggregates in ALS. Moreover, they are implicated in the formation of misfolded protein inclusions via nucleation of these aggregates [129]. TDP-43 localises in SGs in the presence of ER stress, oxidative stress, mitochondrial stress, osmotic stress, and inhibition of the proteasome [49, 130–134]. ALS-associated variant SOD1G93A colocalizes with SGs, unlike wildtype SOD1 [135, 136]. Co-localization of TDP-43 aggregates and SG markers has been detected in ALS patient tissues [120, 130, 137, 138], although cellular studies could not detect co-localization between mutant TDP-43 A315T, M337V and SGs under stress conditions [139, 140]. Similarly, colocalization between ALS-mutant FUS R495X and SGs has been reported in cell lines, primary neurons, human tissues [137, 141–145].
Dysregulated macroautophagy
Autophagy is a catabolic process responsible for the degradation and recycling of cellular components. Macroautophagy is the major type of autophagy, which involves the formation of double-membraned vesicles, or autophagosomes. Dysregulation of macroautophagy is well-described in ageing and was recently categorised as a separate hallmark from proteostasis, because organelles and non-protein cellular components are also subject to macroautophagy [3]. Expression of autophagy-related genes, including ATG5, ATG7, and OPTN, are known to decline with age [146, 147]. This results in the accumulation of protein aggregates and dysfunctional organelles during ageing [146]. In addition, stimulation or activation of autophagy increases healthspan and lifespan in humans and model organisms [146]. Autophagy is also reduced in muscle samples obtained from elderly patients [148]. Knocking out autophagy-related gene 7 (ATG7) in mice leads to increased muscle atrophy, muscular inflammation, abnormal structure, and reduced lifespan [148].
Dysregulated macroautophagy is implicated in neurodegeneration in ALS [149] and ALS-associated variants in C9ORF72, SOD1, TARDBP, TBK1, FUS, FIG4, OPTN, UBLN2, SQSTM1, CHMP2B, ALS2 dysregulate macroautophagy [150]. When autophagy is inhibited genetically or pharmacologically, ageing is accelerated and motor neuron toxicity is enhanced in ALS [146, 151]. Autophagy also plays a vital role in clearing protein aggregates associated with neurodegeneration in ALS [152]. Increased activation of autophagy proteins is detected in SOD1G93A transgenic mice [153]. Similarly, progesterone is neuroprotective through activation of autophagy in SOD1G93A mice [154]. C9ORF72 itself interacts with Rab1a and Unc-51-like kinase 1 (ULK1) complex to initiate autophagy via the formation of autophagosomes [155] and loss of C9ORF72 impairs autophagy [156, 157]. C9ORF72 DPRs co-localise with including p62-positive inclusions, suggesting that DPRs are targeted for clearance by the UPS and/or autophagy [158]. TDP-43A315T mutation activates ER stress and induces autophagy to clearance misfolded protein aggregates [159].
Antagonistic hallmarks of ageing in ALS
Cellular senescence
Senescence is implicated as an important characteristic and driver of the ageing process. Many studies have shown that senescence regulates age-associated phenotypes and is present in age-related diseases [160, 161]. Senescent cells were previously considered to be harmful because their elimination extends the lifespan of mice [162]. However, more recent studies in liver have reported that senescent cells positively impact on healthy ageing and lifespan and may have important functional roles in ageing [163]. In cycling cells, senescence is characterised by a state of eternal cell cycle arrest although they remain metabolically active [164]. DNA damage in the nucleus (mainly in the form of DSBs) and telomere shortening are key features of senescence [165–169]. The senescence-associated DDR involves ATR, ATM, and p53, which induces activation of cyclin-dependent kinase inhibitors p16, p21, and p27 and hyperphosphorylation of retinoblastoma protein (Rb), which results in withdrawal from the cell cycle [170]. Senescence is induced following diverse endogenous and exogenous stimulii, including oxidative stress, neuroinflammation, oncogenic activation, inactivation of tumour suppressor genes and mitochondrial dysfunction [168, 171]. During senescence, cells undergo several phenotypic modifications, including profound chromatin and secretome changes, and tumour-suppressor activation [172]. The senescence-associated secretory phenotype (SASP) is a prominent feature of senescence that induces inflammation via accumulation of pro-inflammatory cytokines, chemokines and growth factors [173]. Consequently, senescent cells can induce significant alterations in the cellular microenvironment through SASP, which can worsen inflammation [174]. Microglia in the white matter are thought to be the primary cell type undergoing senescence in the CNS during ageing [175].
As neurons are post-mitotic, they do not undergo classic ‘replicative’ senescence, so this mechanism was originally thought to be restricted to dividing cells. However, neurons express senescence markers, SASP is present in the ageing brain, and recent findings have revealed that neurons undergo a similar process as senescence in response to stress (‘stress-induced premature senescence’) [170, 176–179]. Hence, senescence in normal ageing neurons may compromise viability and increase their susceptibility to additional insults [180]. However, our understanding of senescence in neurons remains limited [181].
Senescence has been described in ALS, although this has been detected predominately in glial cells. In lumbar spinal cords of symptomatic SOD1G93A rats, microglia with characteristics of senescence were detected [174]. Senescence markers, including loss of nuclear lamin B1 expression and significantly increased p16INK4a, p53, matrix metalloproteinase-1 (MMP-1) were present compared to non-transgenic or asymptomatic transgenic rats [174]. Interestingly, other cell types in the degenerating lumbar spinal cord, including ChAT-positive motor neurons and GFAP-expressing astrocytes, also exhibited nuclear p16INK4a staining. Similarly, in astrocytes generated from iPSCs of individuals with sporadic ALS and ALS-C9ORF72 patients, there was a significant rise in expression of senescence markers [182]. The brains of ALS patients also display elevated numbers of senescent astrocytes [183].
Satellite cells are skeletal muscle adult stem cells that reside between muscles fibres and basement membranes and self-replicate and/or differentiate to new form new muscle fibres following injury [184]. Senescence has been reported in these cells in geriatric mice, resulting in halted muscle fibre regeneration [185]. B lymphoma Mo-MLV insertion region 1 homolog (Bmi1) knockdown results in senescence-like phenotypes in young satellite cells [185]. Protein arginine methyltransferase 7 (PRMT7) [186] is associated with muscle regeneration capacity and its expression decreases in an age-dependant manner [187]. Decreased skeletal muscle mass, impaired satellite cell regeneration and premature senescence, were detected in PRMT7 knockout mice [186]. Together these findings lend support to the idea that senescence plays a role in the development of ALS, although this is not well-characterised [182].
Mitochondrial dysfunction
Mitochondria are multi-functional organelles that have long been associated with ageing. They provide the primary sources of cellular energy, and also regulate innate immunity, inflammation and apoptosis [188]. During ageing, mitochondrial functions become impaired by defects in membrane potential, decreased respiratory capacity, increased free radical production, reduced turnover, and dynamics, as well as accumulation of mutations in mtDNA [73, 188].
Mitochondrial dysfunction is widely described in ALS [73, 188, 189]. Deficiencies in mitochondrial respiratory chain complex 1 are present in motor neurons obtained from lumbar spinal cord sections from sporadic ALS patients [106, 190]. Decreased mitochondrial membrane potential is present in C9ORF72 and mutant TDP-43M337V human iPSC-derived motor neurons [191] and fibroblasts [192]. C9ORF72 haploinsufficiency impairs mitochondrial bioenergetics and function, and expression of electron transport chain complexes [193, 194]. Overexpression of C9ORF72 DPRs (particularly poly-GR) induces mitochondrial DNA damage, disrupts mitochondrial membrane potential, and increases ROS production [195]. Poly-GR binds to mitochondrial ATP synthase Atp5a1, inducing defects in mitochondrial structure and morphology [196]. Abnormal accumulation of mitochondria is present in spinal cord motor neurons of mutant TDP-43A315T and SOD1G93A transgenic mice [197] and mitochondria dysfunction and transport abnormalities are present in cells expressing ALS mutant TDP-43Q331K, M337V [198–200] and mutant SOD1G93A, G85R [201]. Mutations in UBQLN2P497S [202] and FUSR514G also induce mitochondrial abnormalities [203]. ALS-linked oxidised SOD1 triggers mitochondrial dysfunction and cellular senescence, which further accelerates ageing, providing a more direct link between oxidative stress, ALS and ageing[204]. Together, these findings suggest that mitochondrial dysfunction is closely associated with the major ALS pathological proteins.
Dysregulated nutrient sensing
During ageing, there is a decline in key metabolic signaling pathways relevant to ageing and neurodegeneration [210], involving the adrenergic, dopamine, insulin/insulin-like growth factor 1 (IGF1), AMP-activated protein kinase (AMPK), sirtuin (SIRT) and mTOR pathways. IGF-1 is a primary mediator of the action of growth hormone (GH) that modulates carbohydrate metabolism via insulin. Ageing results in reduced IGF-1 and GH levels [205], including in the brain [206]. AMPK is a sensor of cellular energy status, and its activation restores energy balance. Moreover, reduced AMPK activity is implicated in ageing [207]. mTOR, a serine-threonine protein kinase, is a negative regulator of ageing that promotes SASP [208]. In yeast, worms, and flies, blocking mTORC1 prolongs lifespan [209].
Nicotinamide adenine dinucleotide (NAD +) is a coenzyme central to energy metabolism and an essential cofactor in cellular redox reactions and SIRT activities [211]. It influences DNA repair, chromatin remodelling, and senescence, and reduced NAD + levels are detected during ageing [212, 213]. SIRTs are a family of seven proteins that regulate cell/tissue survival and metabolism, and they possess many functions associated with ageing. This includes DNA repair and genome stability, senescence, and mitochondrial function, and they inhibit oxidative stress, inflammation, and apoptosis [214, 215]. SIRT-1, 2, 3 and 6 also increase lifespan in species ranging from fruit flies to mammals [216–218]. Expression of SIRT1 decreases during ageing, hence elevating expression of SIRTs may protect against age-related events [219].
Changes in metabolic pathways are associated with the heterogeneity and diverse clinical characteristics of ALS. mTOR inhibition in mutant SOD1G93A transgenic mice hastens disease progression and increases motor neuron degeneration [220]. However, mTOR inhibition is protective in a transgenic mouse model involving neuron-specific wildtype TDP-43 overexpression [221]. IGF-1 overexpression in primary motor neurons is protective against glutamate-induced toxicity in ALS [222]. AMPK activation has been detected in motor neurons of ALS patients as well as in the spinal cord of SOD1G93A mice [223]. Dysregulation of SIRT has been described in ALS [224–226] and SIRT1 sensitive lysine-136 acetylation drives LLPS and pathological aggregation of TDP-43 [227, 228]. SIRT-1 activation has been examined therapeutically using resveratrol, which initially displayed promising effects by improving motor impairment and extending lifespan in SOD1G93A mice [229]. However, it failed in clinical trials [230].
Integrative hallmarks and ALS
Impaired intercellular communication
Cells can communicate with each other by either direct physical interactions or by intermediates such as extracellular vesicles (EVs) that act as inter-cellular messengers. During normal ageing, there is a gradual decline in the quality of communication between cells, which impacts on several processes relevant to ALS. These are discussed in the sections below.
Senescence and intercellular communication
Senescent cells are metabolically active and can communicate with, and influence the behaviour of, neighbouring cells through paracrine signalling [231]. Senescence is also an important part of inter-cellular communication and ageing [232] via SASP [233]. As well as the secretion of pro-inflammatory molecules, senescent cells also communicate with other cells via membrane-bound intercellular bridges or ‘tunnelling nanotubes’, that facilitate direct physical connections between cells [234]. The role of senescence in ageing and ALS is described in the 'Integrative hallmarks and ALS' section.
Neuroinflammation and inter-cellular communication between glia and neurons
Within the CNS, neurons, astrocytes, microglia, and oligodendrocytes must normally communicate with each other and the surrounding environment to maintain homeostasis. Motor neuron health and viability relies on efficient communication with glial cells and skeletal muscles [235, 236].
ALS is a non-cell-autonomous disease, and extrinsic inter-cellular communication amongst motor neurons, microglia, oligodendrocytes, and astrocytes is implicated in pathophysiology. This occurs through alterations in trophic factor support to motor neurons, signalling factors that impact on glial cell receptors and changes in direct cell-to-cell interactions [236]. Intrathecal administration of CSF from ALS patients in mice reduces the expression of trophic factors BDNF, fibroblast growth factor 2 (FGF2), and IGF-1 [237]. Pro-inflammatory cytokines and apoptosis-triggering TNF-α and Fas ligand (FASL) produced by activated microglia and astrocytes induce damage to motor neurons [238, 239]. Mouse cortical neurons treated with iPSC-derived astrocytes from C9ORF72 patients show increased oxidative stress and neurotoxicity [182]. Degenerating and morphologically altered oligodendrocytes are dramatically increased in mutant SOD1G93A mice and are surrounded by clustered activated microglia [240]. Astrocytes derived from post-mortem familial ALS (SOD 1A4V) and sporadic ALS patient brains are toxic to motor neurons, but this is alleviated by reducing SOD1 expression in astrocytes [241]. In mutant SOD1G93A mice model, senescent astrocytes display less support to motor neurons. Furthermore, IL-6 levels increase in astrocytes of SOD1G93A rodent models which recruits immune cells to clear the senescent cells [242, 243].
Extracellular vesicles and intercellular communication
EVs are tiny membrane-bound structures, typically ranging in size from 50 to 1000 nm [244]. They contain both protein and nucleic acid and they are released by various cell types in both physiological and pathological conditions [244]. Extracellular RNAs (exRNAs) are important mediators of cell-to-cell communication that are secreted as either EVs or in a complex with RNA binding proteins (RBPs)[245]. Senescence-associated EVs are implicated in the DDR and SASP [246, 247]. The levels of EVs alter during senescence and ageing, although it is controversial whether they increase or decrease [248–250].
ExRNAs and EVs are also implicated in ALS pathogenesis. Some exRNAs, including mRNA, microRNA and circular RNA, are present in exosomes and as they are dysregulated in ALS they have been proposed as potential biomarkers [174, 175] [251] (RNA dysregulation in ALS is reviewed in more detail in the 'Defects in RNA dysfunction section). Transgenic SOD1G93A mice release astrocyte-derived EVs containing mutant SOD1G93A that transfer to spinal neurons and selectively trigger death [252]. Microvesicles isolated from ALS patients contain higher levels of pathological proteins (SOD1, TDP-43, FUS) compared to controls, unlike exosomes, despite the mean size for both EV types being larger in ALS than controls [253].
Misfolded proteins are known to transmit between cells in ALS and other neurodegenerative diseases, particularly SOD1 [254, 255]. Several studies have described ‘prion-like’ characteristics of misfolded SOD1, including its capacity to transfer between cells and cause the misfolding of wildtype SOD1 within cells [256] and in vivo [257]. The transmission of toxic aggregates via EVs is not well-understood [244]. Misfolded SOD1, whether wildtype or ALS-associated variants A4V, G93A, G127X, are secreted as EVs in NSC-34 and HEK cells [254]. Astrocytes and neurons constitute the primary sources of EVs in vivo containing misfolded SOD1 in spinal cords of both SOD1G93A transgenic mice and SOD1-ALS patients [258]. Similarly, ‘prion- like’ behaviour for TDP-43 has been described in mice [259, 260]. Further studies have demonstrated both exosome-dependent and independent mechanisms are involved in TDP-43 inter-cellular transmission [261]. Similarly, C9ORF72 DPRs, poly-GA, poly-GP, poly-GR, and poly-PA transmit from cell-to-cell by exosome dependent and independent mechanisms [262].
Neuroinflammation and ageing
Inflammation increases significantly during normal ageing, both systemically and in the nervous system (neuroinflammation). Senescent cells also contribute to the persistent inflammatory environment via SASP [162], and their accumulation leads to sustained inflammation [263]. Inflammasomes, multimeric protein complexes that activate inflammatory caspase 1, are integral components of the innate immune system that become activated during the ageing process [264]. This includes the nucleotide oligomerization domain (NOD)-like receptor protein 3 (NLRP3) inflammasome [265].
Neuroinflammation plays a significant role in ageing of the CNS and associated pathological conditions [266]. During ageing, activated microglia and astrocytes display altered morphologies and produce pro-inflammatory cytokines, leading to neuroinflammation [267–269]. When activated, astrocytes can display either neurotoxic, pro-inflammatory (A1) or neuroprotective, anti-inflammatory (A2) phenotypes. Similarly, microglia display both inflammatory and anti-inflammatory states, M1 and M2, respectively. RNA sequencing of brain-derived astrocytes throughout the lifespan of mice [270, 271] revealed up-regulation of A1-phenotype genes associated with neuroinflammation [271], linking astrocytes to cognitive impairment during ageing. Mice are protected from age-related reactive astrogliosis in the absence of microglial proinflammatory cytokines, suggesting that microglia are responsible for initiating the neuroinflammation that occurs with ageing [271]. However, astrocytes exert detrimental effects on microglia during ageing, impairing their phagocytic capabilities, resulting in a prolonged pro-inflammatory state [272].
Neuroinflammation is well-described in both human ALS and animal models [273]. Infiltration of peripheral lymphocytes, natural killer (NK) cells and macrophages, along with activation of astrocytes and microglia and the excessive production of inflammatory cytokines, is present in both humans and mice [274]. Interestingly, transcriptomic analysis of spinal cords of SOD1G93A mice revealed a significant overlap (90% shared transcripts) between gene expression patterns associated with normal ageing and ALS, particularly inflammation and immune system activation [219]. The NLRP3 inflammasome, along with expression of caspase-1, IL-1β, IL-18, and NFκB, is increased in the SOD1G93A transgenic rat [275]. In astrocytes of the spinal cord from SOD1G93A mice [276] and sporadic ALS patients, elevated levels of NLRP3, apoptosis-associated speck-like protein containing a caspase-1 recruitment domain (ASC), IL18, and active caspase 1, are present [277]. Microglia in mutant and wild-type SOD1G93A and TDP-43Q331K ALS mice express NLPR3, consistent with elevated expression of inflammasome components in vivo [265]. TDP-43 binds to CD14 receptors in microglia, macrophages, and monocytes, activating NFκB and stimulating the NLRP3 inflammasome [278]. In SOD1G93A rats, progression of paralysis was linked to neuroinflammation and motor neuron toxicity via microglia [174]. There is evidence for both neuroprotective and neurotoxic effects of astrocytes and microglia in ALS (reviewed in Clarke et al. 2020) [279, 280].
Stem cell exhaustion
Stem cells have self-renewal and multi-differentiation capabilities and thus regenerate tissue growth during ageing. Neural stem cells (NSCs) are responsible for producing neurons during prenatal development and maintaining the nervous system throughout adult life [281, 282]. However, during ageing, the functionality and regenerative capacity of NSCs deteriorates. This exhaustion of stem cells can be induced experimentally by upregulation of DNA damage, altered DNA repair mechanisms, decreased regenerative ability, epigenetic alterations, increased genomic instability, altered protein homeostasis, dysfunctional mitochondria, and senescence [290]. Several studies have identified possible ways to improve stem cell function during ageing, such as by increasing the levels of transcription factor FOXO4, HSP70 [290], or alternatively by exposing young blood to aged animals through heterochronic parabiosis [288].
A meta-analysis of eleven studies demonstrated that isolating and transplanting NSCs from the CNS into the spinal cord of transgenic mutant SOD1G93A mice slowed disease progression [281]. This was related to improvement of neurotrophic factor production, reduced neuroinflammation, and preservation of neuromuscular function [281]. Regenerating and renewing aged stem cells may be beneficial therapeutically in neurodegenerative diseases including ALS, although this has not been well-studied.
Dysbiosis
The gut microbiome is now recognised to play a critical role in health and well-being [3] including ageing [4, 5], and it is shaped by genetics, age, stress, illness, medication, diet, and the environment. However, the microbiome is dysregulated in many pathological conditions, which is known as 'dysbiosis’ [3]. Most gut microorganisms are bacteria, and they are implicated in metabolism, defence against pathogens, development of the immune system, and synthesis of vitamins, short-chain fatty acids and other metabolites [3]. Importantly, the microbiome interacts with the CNS via the gut-brain axis, the bidirectional network linking the enteric nervous system to the CNS [2].
The gut microbiome is established during childhood. Whilst it displays significant diversity among individuals, [3] during normal ageing, changes in the composition of gut microbiota and reduced species diversity are associated with frailty, cognitive function, depressive symptoms, and inflammatory processes [3]. Furthermore, mouse models of progeria and progeria patients with HGPS or Nestor-Guillermo progeria syndrome (NGPS) display dysbiosis, characterised by loss and gain of specific species [36]. Transplantation of faecal microbiota between wildtype mice and progeria mice confirm the existence of a strong link to healthspan/lifespan [37, 38] and in the maintenance of brain health and immunity during ageing [11]. Similarly, administration of gut microbiota metabolites improves age-related pathologies in mice [2, 3]. Collectively, these findings suggest that ageing is closely associated with dysbiosis.
Dysbiosis is also linked to neurodegeneration in ALS. Dysregulation of the gut microbiome correlates with disease severity in both mutant SOD1G93A transgenic mice and human patients [283]. Sodium butyrate is a bacterial metabolite produced in the gut by Butyrivibrio fibrisolvens, and reduced levels of this organism were detected in the SOD1G93A mouse [284]. Increased intestinal permeability to toxins was also detected [284] and treatment of SOD1G93A mice with butyrate also delayed weight loss and improved survival [285], implying that interventions aimed at restoring the gut microbiome may extend lifespan and healthspan in ALS. Alterations in gut microbiota have also been detected in C9ORF72-mutant mice [286], and C9ORF72 itself was found to inhibit systemic and neural inflammatory responses induced by gut bacteria [286]. Together these studies imply that the gut microbiome contributes both to ageing and the pathogenesis of ALS.
Defects in RNA functions
Defects in RNA metabolism are not included as a hallmark of ageing [3], but it has been proposed they should be designated as one, given increasing evidence highlighting their importance to ageing [287]. Given that ageing cells lose their ability to maintain RNA metabolism [288], and dysfunctional RNA metabolism is strongly implicated in the pathophysiology of ALS [289], here we consider this as an ageing hallmark that is discussed in relation to ALS.
The RNA milieu within a cell consists of coding messenger RNAs (mRNAs) and non-coding RNAs (ncRNAs), both of which interact with RNA-binding proteins (RBPs) within ribonucleoprotein complexes (RNPs). RBPs play important roles in RNA metabolism, including alternative splicing of pre-mRNA, transport, and stability, which are fine-tuned by modulation of their own expression and that of other RBPs [290]. They are also involved in modulation of SG dynamics by interaction with cytoplasmic RNAs and other RBPs. Dysregulation of RBPs also induces metabolic dysfunction, ageing, and senescence [291].
The transcriptome of the ageing cell results in global changes in gene expression with down-regulation of genes related to oxidative respiration, protein translation and growth signalling, and up-regulation of genes related to innate immunity, inflammation and DNA damage [292–296]. The multiple layers of processing that determine gene expression, including mRNA modification such as splicing, capping and polyadenylation, RNA export, localization, turnover, and translation, are affected by ageing and ALS [297]. In multiple species, including humans and mice, ageing results in shorter RNA transcripts in nearly 80% of tissues, disrupting the balance of long and short RNA transcripts [297].
The signalling pathways that control alternative splicing are some of the most dysregulated processes in normal ageing [292, 298] and senescence [287, 299]. Higher rates of alternative splicing, including back-splicing and circular RNA formation, reduced transcript quality, and mismatches with genome sequences are also detected during ageing [296]. Furthermore, during natural ageing, cryptic splice sites become revealed. These are sequences within introns that incorporate into the transcript during splicing, resulting in a premature stop codon and loss of function of the associated protein [300].
The ageing transcriptome may further be influenced by altered RNA polymerase II (Pol II) activity [296, 301]. The speed of RNA polymerase II elongation within introns increases with age across multiple cellular and animal models and human samples [296]. In contrast, stalling of Pol II at DNA damage sites increases with age which results in transcriptional stress and shorter transcripts [301]. Cells have stringent RNA quality control systems to prevent these detrimental processes. Aberrantly spliced mRNA with premature stop codons are degraded by 'nonsense mediated decay (NMD)' in order to prevent translation into deleterious non-functional proteins [302]. This process is however dysregulated with ageing and it particularly affects post-mitotic neurons that are more dependent on strong RNA quality control and efficient NMD processes [302].
Chemical modifications to RNA regulate RNA metabolism and are known to contribute to at least eight of the classical hallmarks of ageing, including cellular senescence, epigenetic changes, immune and stem cell dysfunction, concomitant metabolic dysregulation and loss of proteostasis [303]. These RNA modifications include methylation and A-to-I editing. Decreased m6A modifications are present in aged human PBMCs [304], impairing synaptic protein synthesis and synaptic functions relevant to ageing and neurodegeneration [305], suggesting that m6A RNA methylation contributes to cognitive decline in ageing [305]. A-to-I editing also declines during ageing specifically in the human brain [306]. Similarly, mice lacking mRNA editing apolipoprotein B mRNA-editing enzyme catalytic polypeptide (APOBEC1) in microglia show acceleration of age-related neurodegeneration and motor deficiencies [307].
The expression of various ncRNAs is altered with ageing and influences its hallmarks. An array of ncRNAs, including long ncRNAs (lncRNAs), microRNAs (miRNAs), piwi-interacting RNAs (piRNAs), small nucleolar RNA (snoRNA), small nuclear RNA (snRNA), ribosomal RNA (rRNA), small Cajal body specific RNA (scaRNA), transfer RNA (tRNA) and tRNA derived fragments (tRFs), are differentially expressed in ageing tissues [308]. Of these, miRNAs were the most modified as a result of ageing [308]. Age-related changes in global gene expression also correlate with the corresponding miRNA expression [309], which is not surprising given that miRNAs regulate mRNA expression. LncRNAs regulate histone methyltransferases and other chromatin modifying enzymes and thus they epigenetically modify gene expression [310]. They may also protect cells from senescence, because the lncRNA senescence-associated noncoding RNA (SAN) was increased in aged adipose-derived stem cells (ASCs)[311] and another lncRNA, NEAT1 suppressed cellular senescence in hepatocellular carcinoma [312]. NEAT1 plays a crucial role in forming a flexible environment within cells, increasing LLPS and condensation of RBPs and nucleic acids [313]. CircRNAs, a more recently described class of mostly ncRNAs, are gaining recognition as potent regulators of gene expression via their interaction with miRNAs [314], and are emerging players in ageing [315] and age-related diseases [316], including ALS [317, 318].
There is now strong evidence that dysfunctional RNA metabolism is present in ALS. Interestingly, degenerating neurons in ALS show similar RNA metabolic defects (RNA processing, modifications and transport) to ageing neurons [298]. Some of the major proteins dysregulated in ALS are RBPs, including TDP43, FUS, TAF15 and hnRNPA1 [28, 291]. TDP43 and FUS mislocalise and aggregate in the cytoplasm in sporadic ALS [319], which reduces their expression in the nucleus [288], resulting in loss of essential functions, including splicing and regulation of transcription. Loss of nuclear TDP43 also leads to the emergence of cryptic splice sites, which are now increasingly recognised as contributors to ALS. This includes a cryptic splice site in the first intron of the stathmin-2 gene (STMN2), leading to loss of protein and inability to repair axons following motor neuron injury [320].
RNA modifications and quality control of RNA such as m6A methylation, A-to-I editing, NMD and RNA surveillance are also dysregulated in ALS [321–323]. The C9ORF72 expansion repeats sequester RNA export factors [324, 325] and inhibit NMD [326]. In contrast, NMD hyperactivation was detected in fibroblasts derived from ALS-associated FUS patients [327], which reduces protein biosynthesis and contributes to motor neuron death in ALS [328]. TDP-43 interacts with NEAT1 resulting in its condensation into nuclear bodies in response to stress and pathological features of ALS, such as phosphorylation and its mis-localisation [329].
These studies therefore provide significant evidence linking dysregulated RNA metabolism to ageing and ALS. However it is important to recognise that these events are intricately interconnected [330]. For example, loss of the RBP HuR causes a reduction in methylation (C106) of the lncRNA component of telomerase (TERC), impairing telomerase function and resulting in telomere attrition and accelerated ageing [331] (Table 1).
Table 1.
Hallmarks of ageing in ALS
| Hallmarks of ageing | Cellular pathways implicated in ALS | Pathological protein involved | References |
|---|---|---|---|
| Primary hallmarks | |||
| Genomic Instability | Nuclear architecture alterations, nuclear pore pathology, damage to nuclear DNA, damage to mitochondrial DNA | SOD1, TDP-43, C9ORF72 DPRs, FUS, NEK1 | [47, 48, 58, 60, 63, 64, 332, 333] |
| Telomere attrition | Both shorter and longer telomeres are described in ALS | SOD1, C9ORF72 DPRs | [77, 334, 335] |
| Epigenetic alterations |
DNA hyper- and hypo-methylation, hyper- or hypo-acetylation of histones |
SOD1, FUS, TDP-43, C9ORF72 DPRs | [88, 95–97, 100, 228, 336] |
| Loss of proteostasis | Defects in protein folding, disrupted UPS, defective ER-Golgi trafficking, ER stress, Golgi fragmentation and defects in ERAD | SOD1, TDP-43, C9ORF72 DPRs, FUS | [102, 103, 337–340] |
| Dysregulated macroautophagy | Increased or decreased activation of autophagy, impaired mitophagy, dysregulated autophagy initiation and impaired autophagic flux | C9ORF72 DPRs, SOD1, TDP-43, TBK1, FUS, FIG4, OPTN, UBLN2, SQSTM1, CHMP2B, ALS2 | [341–348] |
| Antagonistic hallmarks | |||
| Cellular senescence | Microglia senescence, abnormal expression of senescence markers | SOD1, C9ORF72 | [174, 285, 349] |
| Mitochondrial dysfunction | Defects in membrane potential, decreased respiratory capacity, increased free radical production, reduced turnover, and dynamics | SOD1, TDP-43, C9ORF72 DPRs, UBQLN2 and FUS | [74, 191, 196, 332, 350–354] |
| Dysregulated nutrient sensing | Dysregulated mTOR signaling, AMPK pathway and SIRT regulation | SOD1, C9ORF72 DPRs, TDP-43 | [210, 220, 355, 356] |
| Integrative hallmarks | |||
| Impaired intercellular communication | Dysregulated interaction between glia and neurons, dysregulated EV and intracellular communication | SOD1, TDP-43, FUS and C9ORF72 DPRs | [244, 253, 357, 358] |
| Neuroinflammation |
Hyperactivated astrocytes and microglia, increased pro-inflammatory cytokines Changes in glia to proinflammatory phenotypes |
SOD1, TDP-43 | [359–361] |
| Stem cell exhaustion | Decreased functionality and regenerative capacity of NSCs | SOD1 | [362] |
| Dysbiosis |
Increased intestinal permeability to toxins, altered gut microbiota |
SOD1, C9ORF72 DPRs | [283, 284, 286] |
| Defects in RNA dysfunction |
RNA metabolic defects (RNA processing, modifications and transport), splicing defects, cryptic exon inclusion, dysregulated quality control of RNA such as NMD and RNA surveillance |
TDP43, FUS, TAF15 and hnRNPA1 | [62, 317, 363–366] |
Ageing of motor neurons and non-neuronal cells in ALS
The hallmarks described above detail ageing-related events at the molecular and cellular level. Below, we also briefly discuss below how ageing specifically affects the cell types relevant to ALS; motor neurons, glia, and skeletal muscle cells.
Ageing of motor neurons and glial cells in ALS
Motor neurons
It is unclear whether motor neurons are lost during normal ageing because conflicting findings have been obtained. Some studies have concluded that the size and number of motor neurons remains constant [367], whereas others report that there is a progressive motor neuron loss during physiological ageing [105, 368], similar to ALS, leaving the remaining aged motor neurons under stress [369].
It is clear that during normal ageing there are alterations in the properties of spinal α-motor neurons and a decline in neurotransmitter function [370]. This impairs their membrane and electrical properties, rendering them more susceptible to degeneration. Voluntary movements require efficient intra-neuronal excitatory (glutamatergic and cholinergic) and inhibitory (GABAergic and glycinergic) signalling [105]. Decreased cholinergic and glutamatergic synaptic inputs terminating on motor neurons are present in the ventral horn of old rhesus monkeys and mice [105]. In mice, membrane depolarization and increased expression of voltage-gated sodium channel isoform Nav1.8 l are present in aged motor neuron axons [371]. In addition, as neurons age, they lose their excitatory synaptic connections across the cell body and dendritic branches. Consequently, older motor neurons possess a diminished balance of excitatory to inhibitory synapses, which could impair their ability to initiate motor movements [305]. The expression of matrix metalloproteinase 1 (dMMP1) rises during ageing, which leads to motor functional impairments that worsen with ageing Drosophila motor neurons [372].
Alterations in synaptic transmission and the excitability of motor neurons are one of the first events in ALS. Hyperexcitability of both upper and lower motor neurons is frequently observed in SOD1G93A mouse models, ALS-iPSC derived motor neurons, and ALS patients [373–375]. Excitotoxicity, referring to excessive activation of glutamate receptors and subsequent neuronal injury or death, is also commonly described in disease models [376]. During disease progression, however, motor neurons become hypo-excitable, although this could be a compensatory process [376]. In ALS patients, electrophysiological studies have identified abnormalities in sodium and potassium currents, implying that membrane depolarization and age-related changes in membrane excitability are present in median motor axons [377]. Increased expression of Drosophila dMMP1 in motor neurons contributes to the decline in motor function observed during ageing [372]. TDP-43 overexpression in neurons accelerates neuronal death by triggering dMMP1 expression, suggesting potential connections between ageing and ALS [372]. With ageing, motor neurons may become less efficient in transmitting signals to muscles, leading to slower response times and decreased motor control [378].
It remains unclear why motor neurons are selectively targeted in ALS. Neurons themselves display features that may render them more susceptible to the effects of ageing. Neurons rely on error-prone NHEJ for DSB repair [379], and being post-mitotic, they are unable to dilute the effect of DNA repair errors by cell division, unlike other cell types. Thus, they may be particularly vulnerable to DNA damage, as well as senescence [181, 379]. Post-mitotic neurons also may be more susceptible to the accumulation of misfolded proteins than other cell types, where the effect of protein aggregation can also be reduced by cell division. Hence, they are likely to be more susceptible to proteostasis dysfunction.
However, motor neurons possess distinctive characteristics compared to other neurons, which may render them uniquely vulnerable to neurodegeneration in ALS [1]. Motor neurons are large cells, with very long axons (up to 1m in an adult human), which may render them more prone to injury [380]. Also, they need to transmit signals over long distances and sustain constant firing and communication with muscles. Thus, the electrical activity of motor neurons may also contribute to their susceptibility in ALS, because this necessitates a significant amount of energy [380]. The constant firing of action potentials and the high metabolic rates required to maintain electrochemical gradients across neuronal membranes also increases oxidative stress [381]. Motor neurons are also highly susceptible to glutamate excitotoxicity compared to other neurons [382].
Within motor neurons, susceptibility to neurodegeneration in ALS is not uniform. Specific populations of motor neurons, including those in the oculomotor and Onuf's nuclei, remain relatively spared and do not degenerate until later stages of disease in humans [383] and mouse models [384–387]. Similarly, oculomotor neurons are not usually affected during ageing. In contrast, spinal motor neurons are targeted in both ALS and ageing, implying that ageing increases the susceptibility of spinal motor neurons to degeneration [388, 389]. Several studies have identified different gene expression profiles between oculomotor and spinal motor neurons. Microarray and laser capture microdissection of motor neurons isolated from oculomotor/trochlear nuclei, the hypoglossal nucleus, and the lateral column of the cervical spinal cord in humans and SOD1G93A rats have revealed unique expression patterns in pathways associated with the ageing hallmarks, including loss of proteostasis, mitochondrial impairment and dysregulated autophagy [390, 391].
Differential susceptibility among motor neuron subtypes, even within the same motor unit, is also observed in ALS. Fast-fatigable (FF) motor neurons degenerate early in disease course, and the fatigue-resistant (FR) types subsequently follow later. In contrast, the slow (S) MNs are resistant to degeneration and are retained, even up to late in disease course. The reasons for the selective vulnerability of motor neuron subtypes remain unclear. However, both FF and FR subtypes are affected first during normal ageing whereas the slow subtypes are affected later, implying that ageing increases the susceptibility of FF and FR motor neurons in ALS [392–394]. The motor neuron subtypes also display noticeable differences in their properties. FF motor neurons possess somas with large-diameter whereas S motor neurons contain much smaller soma [385]. Also, FF motor neurons are much less excitable than the FR subtype which in turn are less excitable than the S subtype, also linking motor neuron susceptibility to excitability. Different gene expression profiles are also evident between these subgroups [385].
The unique combination of features in motor neurons, including their long axons, high energy demands, increased DNA damage and error-prone DNA repair mechanisms, neuronal senescence, susceptibility to excitotoxicity, and heterogeneity in susceptibility among subtypes, may therefore collectively render them more vulnerable to the effects of ageing [395]. Further exploration of these aspects is crucial for understanding the mechanisms underlying age-related motor neuron degeneration. Characterising these events may pave the way for targeted interventions to promote motor neuronal health during the normal ageing process.
Glial cells
Age-related changes and the presence of the ageing hallmarks are also detected in glial cells, as detailed below. The role of neuroinflammation induced by reactive astrocytes and microglia is discussed in the 'Neuroinflammation and ageing' section.
Astrocytes
Ageing is associated with morphological changes to astrocytes, characterized by atrophy and shrinking of processes such as branches and leaflets, and a decline in their function [396]. More specifically during ageing there is a decrease in synaptic connections and plasticity [397]. Astrocyte marker glial fibrillary acidic protein (GFAP) is highly increased in the aged brain, representing activation and gliosis during neurodegeneration [398]. The blood brain barrier is also maintained by astrocytes which also becomes compromised and leaky during ageing [398]. Dysregulation of astrocyte function, leading to sustained release of pro-inflammatory molecules such as IL-8, IL-1β, IL-6, IL-18, TNF-α, is implicated in ageing and age-related neurogenerative diseases [399].
Many studies have implicated astrocytes in ALS pathogenesis. A meta-analysis of studies involving human iPSC-derived astrocytes with variations in SOD1, C9ORF72, and FUS, with those using mouse astrocyte models expressing the SOD1G93A mutation or TDP-43 deletion, or Tmem259 (membralin) deletion, revealed a consistent pattern of gene expression changes amongst these models [400], involving upregulation of genes associated with extracellular matrix dynamics, ER stress responses, and the immune system [400]. Reactive astrocytes induce neurofilament and SOD1 aggregation by disrupting autophagy via the action of TGF-β1, leading to motor neuron degeneration [401]. This occurs through the disruption of autophagy, primarily mediated by TGF-β1 [401]. Increased oxidative stress, reduced survival of motor neurons and neurotoxicity were observed in human iPSC-derived astrocytes from C9ORF72 ALS patients [182]. Similarly, iPSC-derived astrocytes from FUS R521H, P525L ALS patients impair motor neuron-neurite outgrowth, and formation and functionality of the NMJ formation [402].
Microglia
Microglia also undergo morphological changes with age [29]. In aged rats, microglia are characterized by shortened and less intricately branched structures containing nerve fibres and myelin sheets [403]. In the brains of aged individuals, a subset of microglia demonstrated elevated expression of activation markers, including MHC classII, CD45, and CD4. This expression pattern suggested that aged microglia exhibited increased inclusions, indicative of heightened phagocytosis activity [404]. Aged microglia cells also display altered mTOR signaling and increased oxidative stress [29].
There is debate whether microglial activation is present in ALS patients—transitioning from a ramified or stellate shape (inactive state) to an ameboid form (active state)—and whether there is increased proliferation and/or upregulation of inflammatory pathways in post-mortem ALS tissue [279, 405]. Evidence from mouse models including SOD1G93A, A4V, TDP-43WT, M337V, A315T, FUSWT and C9ORF72 knockouts revealed microglia activation and morphological changes compared to controls [279, 406–408]. Reactive microglia are neuroprotective in a TDP-43 mice model [409]. Monocyte-derived microglia-like cells display pathological hallmarks of ALS, including cytoplasmic aggregation and phosphorylation of TDP-43, DNA damage, and cell-specific impairment of phagocytosis associated with disease progression [410].
Oligodendrocytes
Whilst oligodendrocytes normally myelinate axons in the CNS [411], during ageing, myelin regeneration becomes slowed [411]. Ageing oligodendrocytes also display reduced expression of myelin-associated genes MOG, PLP, and CNP [412], and HMGCS1, which is associated with cholesterol synthesis [412]. Conversely, ageing oligodendrocytes display increased expression of genes related to ribosome biogenesis, RPl6, RPS29, and RPl23A, and upregulation of immune-related genes such as C4B and Il33 [412].
Selective removal of mutant SOD1 selectively from oligodendrocytes substantially delays disease onset and prolonged survival in SOD1G93A mice [413]. Oligodendrocytes supply energy to axons through glucose and lactose shuttling and blockage in these pathways is implicated in motor neuron degeneration in ALS [414]. Oligodendrocytes also induce motor neuron death via human SOD1-dependent mechanisms in ALS [415]. Morphological changes and the presence of TDP-43 inclusions were detected in oligodendrocytes in human sporadic ALS spinal cords [416].
Schwann cells
Schwann cells are peripheral myelin generating cells that have a remarkable capacity to regenerate and remyelinate but during ageing these abilities decline [417, 418]. The ageing process in Schwann cells is also linked to abnormalities in myelination in mice [418]. Moreover, older mice show a significant decrease in the number of myelinated nerve fibres [419].
The role of Schwann cells in ALS pathology is poorly understood. However, they induce peripheral nerve inflammation through expression of CSF1, IL-34, and SCF factors in ALS patients [420, 421] and transgenic SOD1G93A rodents [421, 422]. Reducing the levels of SOD1G37R from Schwann cells accelerated disease progression in mice [384]. Terminal and pre-terminal Schwann cells are lost in transgenic SOD1G93A mice, which impairs reinnervation following muscle denervation [422].
Ageing of skeletal muscle/NMJs
Physiological ageing can significantly affect skeletal muscles [423], both structurally and functionally. This can result in progressive loss of muscle mass or ‘sarcopenia’, leading to muscle weakness and motor control [423, 424]. The neuromuscular junction (NMJ) is a specialized tripartite chemical synapse that entails highly coordinated communication between the presynaptic motor neuron, postsynaptic skeletal muscle, and terminal Schwann cells. Muscle denervation is a major contributor to sarcopenia [425] and alterations in the NMJ during ageing play a pivotal role in this process [425–427]. In muscles, age-related decline in mitochondrial function [428] of 25–30% between the ages 30 and 70 years occurs [429]. Similarly, reduced oxygen consumption rates and elevated ROS production in muscles are present during normal ageing in mice [430].
Satellite cells display many classic hallmarks of ageing, and their capability to regenerate becomes compromised during normal ageing [185]. These are also similar to features detected in ALS, including increased DNA damage, mitochondrial dysfunction, loss of proteostasis, oxidative stress, and autophagy defects [351, 431]. Elderly satellite cells display disrupted antioxidant activity and increased membrane fluidity compared to those of young individuals [432], indicating age-dependent imbalance in the antioxidant system during ageing. Age related dysfunction of satellite cells and decreased regenerative capacity are also present in ALS [433].
Impaired NMJs are well-described in ALS although there is controversy whether this involves ‘dying forward’ (originating in the motor cortex before descending to the NMJ) or "dying back" (beginning at the NMJ and then propagating to the motor neuron cell body) mechanisms. Impairment in NMJs is detected in ALS patient tissues and disease models [434]. Transgenic SOD1G93A mice [435] and mutant FUSR521C mouse models exhibit changes in the NMJ early in disease course [387, 436]. Similarly, transgenic SOD1G93A zebrafish display early defects in motor neuron outgrowth, axonal branching and dysregulated NMJ with reduced postsynaptic volume [437, 438]. ALS transgenic mice displaying TDP-43 pathology that lack the nuclear localization signal, also exhibit substantial muscle denervation [439]. Similarly, inducible expression of the C9ORF72 hexanucleotide repeat expansion in mice result in structural abnormalities in NMJs. In addition, early inhibition of C9ORF72 expression leads to structural NMJ abnormalities and rapid muscle dystrophy [440]. It has been proposed that as NMJ impairment in ALS leads to motor neuron dysfunction [441], and degeneration of motor neurons results in further NMJ dysfunction, this creates a viscous cycle, resulting in the progressive loss of muscle control and strength [441].
Therapeutic interventions for ageing and ageing-related diseases
Whilst normal ageing is an inevitable consequence for all individuals, despite the increasing aged population, few therapeutic approaches have been developed for ageing itself. In contrast, there has been intense efforts to develop treatments for age-related diseases, including ALS [442]. There has been considerable progress in this area and there are now seven FDA-approved drugs for ALS. However, these treatments have limited efficacy or are restricted to specific groups of patients. Thus it is important to continue to develop new approaches.
During normal ageing there is a progressive decrease in functionality and in ALS this becomes accelerated. Thus, therapeutic approaches should aim to promote healthspan as well as lifespan. In humans, lifestyle interventions such as calorie restriction and exercise have been examined as approaches to prevent/delay ageing. Furthermore, numerous therapeutic studies have been performed in animal models, demonstrating that delayed ageing and prolonging longevity and healthspan are possible [442]. In particular, treatments that inhibit mTOR are showing promise [209]. In cells, senescence phenotypes such as size and granularity, β-galactosidase staining and fibroblastic spindle morphology are reversed by mTOR inhibition [443]. Rapamycin, an mTOR inhibitor, extends the lifespan of yeast, nematodes, fruit flies and mice [444]. Rapamycin is safe and well-tolerated in a randomised, double-blinded, placebo controlled ALS clinical trial, but further trials are necessary to understand the clinical and biological effects of the drug in ALS [445].
As the levels of NAD+ decline with normal ageing, NAD+ precursors that increase the levels of NAD+ have been examined therapeutically, including nicotinamide riboside (NR) and nicotinamide mononucleotide (NMN), NAD+ biosynthetic enzymes, and NAD+ degradation inhibitors [446]. NMN (CD38 inhibitor) and NR (PARP inhibitor) administration in transgenic SOD1G93A mice delay senescence, improve stem cell renewal, and enhance lifespan [447]. However, deletion of CD38 had no effect in survival in two hSOD1 ALS mouse models [448, 449]. These compounds are in various stages of human clinical trials for ALS [335, 449].
Compounds that enhance SIRT activity may also be protective against ageing given that this function is decreased with age [450]. These include polyphenols such as resveratrol, which activates SIRT1 NAD+-dependent histone deacetylase activity [451]. Administration of dietary resveratrol extends lifespan of several organisms including yeast, nematode and fruit flies [452] and mice models of ageing [453]. Resveratrol also enhances mitochondrial biogenesis and improves oxidative capacity in ageing mice models [454]. Resveratrol treatment also prevented motor neuron loss, relieved muscle atrophy, and improved mitochondrial function in muscles [455] and extended survival in SOD1G93A mice [229]. However, another study reported that in SOD1G93A mice it did not improve motor function or increase survival when given as a single dose, in contrast to these other studies [456].
Metformin, used in Europe as traditional medicine since the early nineteenth century, is also implicated as an anti-ageing treatment, because it suppresses cellular senescence phenotypes [457] and has been described as a possible protective factor against neurodegeneration [458, 459]. Metformin treatment of iPSCs generated from HGPS patients decreases progerin expression and reduces abnormalities in nuclear architecture, suggesting it has therapeutic potential to reduce ageing [460]. Lonafarnib is a farnesyltransferase inhibitor that reduces the effects of progerin on nuclear morphology in HGPS and is the only FDA approved treatment for HGPS [461]. FOXO4 peptide treatment and immunotherapy reverses senescence-associated loss of tissue by restoring the apoptotic role of p53 [462]. A small molecule telomerase activator, TA-65, inhibited telomere shortening and enhanced immune function [463], increased healthspan and rescued DNA damage defects in old adult mice [464]. Similarly, supplementation of TA-65 led to an improvement of healthspan indicators in several studies [465]. A recent RNA-seq analyses identified IGF1 and mitochondrial translation as longevity signatures common to 41 mammalian species and identified compounds that extended lifespan in mice [466]. However, none of these approaches have yet been tested in ALS (Table 2).
Table 2.
Therapeutic compounds targeting the ageing hallmarks
| Treatment | Properties/ Mechanism of action | Trial/ Study | Result | References |
|---|---|---|---|---|
| Vitamin E | Antioxidant | Randomized placebo-controlled human clinical trial (RCT) | No significant improvement in disease progression or survival | [467, 468] |
| Vitamin C and Carotenoids Supplementation | Antioxidant | Pooled results from 5 different cohort studies | Did not significantly reduce the risk of developing ALS | [469] |
| EH301, (PT and NR) | Combination of antioxidant and anti-aging agent | Pilot RCT | Slowed disease progression in an ALS patient | [470] |
| Rapamycin | mTOR inhibitor | Phase 1/II RCT | Treatment was safe and well-tolerated. Efficacy studies are required | [445] |
| NMN | CD38 inhibitor | Pre-clinical SOD1G93A mice study | Treatment delayed senescence, improved stem cell renewal, and enhanced lifespan | [448, 471] |
| NR | PARP inhibitor | Pre-clinical SOD1G93A mice study | Treatment delayed senescence, improved stem cell renewal, and enhanced lifespan | [471] |
| Resveratrol | SIRT 1 activation | Pre-clinical SOD1G93A mice study | Treatment prevented motor neuron loss, relieved muscle atrophy, and improved mitochondrial function in muscles and extended survival in SOD1G93A mice | [229, 230, 455] |
| Trichostatin A, scriptaid, tubastatin A | HDAC inhibitors | Pre-clinical SOD1G93A mice study | Improved lifespan, delayed disease onset and improved motor function in the SOD1G93A model | [85, 472] |
| Valproic acid, entinostat, sodium phenylbutyrate | HDAC inhibitors | Pre-clinical SOD1G93A mice study | Improved lifespan, delayed disease onset and improved motor function in the SOD1G93A model | [85, 472] |
| Sodium phenylbutyrate and valproic acid | HDAC inhibitors | Phase II RCT | Safe and tolerable | [85, 472] |
DNMTs, HDACs and HATs have also been examined in ageing. HDACs include the ‘classical’ Zn2+-dependent deacetylases (class I, II, and IV) and SIRT deacetylases (class III) that are also implicated in longevity [473]. Inactivating HDAC homologs in C. elegans and Drosophila improved lifespan, and delayed age-related physical decline [336]. HDAC inhibitors trichostatin A, scriptaid, tubastatin A, valproic acid, entinostat, sodium phenylbutyrate improved lifespan, delayed disease onset and improved motor function in SOD1G93A mice [101, 472]. HDAC inhibitors may therefore have potential in age-related diseases such as ALS [474]. However, whilst HDAC inhibitors sodium phenylbutyrate and valproic acid are safe and tolerable in human ALS phase II clinical trials, there was no difference in survival compared to placebo [101].Therapeutic strategies involving preventing protein aggregation and restoring proteostasis have been widely studied in ALS. Molecular chaperones such as HSPs [475] and PDI family members are neuroprotective against ALS mutant SOD1 and TDP-43-induced pathologies, including in vivo [115, 338, 476]. Compounds targeting neuroinflammation have largely been ineffective in ALS clinical trials, although a phase II study involving tyrosine kinase inhibitor masitinib with riluzole showed promising results in ALS patients [477].
Conclusion
The universal phenomenon of ageing is the largest risk factor for age-related neurodegenerative diseases, including ALS [335, 478]. Hence, therapeutic strategies that target ageing mechanisms may be beneficial in these conditions. However, to date, ageing has not been explored specifically as a drug development target in relation to ALS. Furthermore, the molecular links between ageing and neurodegeneration remain poorly understood. Normal ageing is a complex, multi-layered phenomenon that is difficult to separate from many age-associated diseases. Furthermore, the recognised molecular and cellular hallmarks of ageing overlap significantly and are strongly related to each other (Fig. 1). Moreover, there are numerous similarities between ageing and the pathophysiology of ALS. However, whilst most neurodegenerative mechanisms implicated in ALS are related to the key hallmarks of ageing, more studies are required to confirm a direct connection between dysfunction in these events and ageing in ALS. The pathophysiology underlying ALS involves a complex interaction between ageing, genetic, epigenetic, and environmental factors. As pathogenesis in ALS is thought to be multistep process requiring six steps [479], ageing may therefore be an important accelerator of neurodegeneration in ALS.
Given the complexity of ALS, it is important to employ a multifaceted approach to target age-associated molecular mechanisms. Maintenance of the integrity of both the genome and proteome is of central importance in this process and increasingly described links between these pathways are described [479, 480]. Similarly, restoring proteostasis and improving resilience to cellular stress will be essential to withstand the insults associated with ALS. The increasing recognition of skeletal muscle in the etiology of ALS must also be considered, particularly as many features of normal ageing in muscle are also described in ALS. However, understanding the primary mechanisms that drive ageing at molecular and cellular level will facilitate in unravelling the mysteries of why the risk of ALS increases with age. Normal ageing is an inevitable consequence for all individuals but it will be important to consider age-related molecular events when considering novel therapeutic approaches for ALS in the future to design more effective strategies to halt neurodegeneration [442].
Acknowledgements
Not applicable.
Authors contributions
CJJ and JDA conceptualized the structure of the manuscript. CJJ and JDA also conceived the article and edited the manuscript throughout for content and style consistency. SSH and SAK designed and created the figures with BioRender. All the authors wrote sections of the manuscript.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This work was supported by an Australian National Health and Medical Research Council (NHMRC) Dementia Teams Research Grant (1095215), Macquarie University Postgraduate Research Scholarship, and Motor Neuron Disease Research Australia (Peter Stearne Familial MND Research Grant and Linda Rynalski Bridge Funding Grant) and Fight MND Foundation.
Availability of data and materials
Not applicable.
Declarations
Conflict of interests
The authors declare that they have no financial or non-financial competing interests.
Ethical approval and consent to participate
Not applicable.
Consent for publication
All authors have agreed and provided consent for publication.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Blinkouskaya Y, et al. Brain aging mechanisms with mechanical manifestations. Mech Ageing Dev. 2021;200:111575. doi: 10.1016/j.mad.2021.111575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piekarz KM, et al. Molecular changes associated with spinal cord aging. GeroScience. 2020;42(2):765–784. doi: 10.1007/s11357-020-00172-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.López-Otín C, et al. Hallmarks of aging: an expanding universe. Cell. 2023;186(2):243–278. doi: 10.1016/j.cell.2022.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Carmona JJ, Michan S. Biology of healthy aging and longevity. Rev Invest Clin. 2016;68(1):7–16. [PubMed] [Google Scholar]
- 5.Khan SS, Singer BD, Vaughan DE. Molecular and physiological manifestations and measurement of aging in humans. Aging Cell. 2017;16(4):624–633. doi: 10.1111/acel.12601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jin K. Modern biological theories of aging. Aging Dis. 2010;1(2):72–74. [PMC free article] [PubMed] [Google Scholar]
- 7.Davidovic M, et al. Old age as a privilege of the "selfish ones". Aging Dis. 2010;1(2):139–146. [PMC free article] [PubMed] [Google Scholar]
- 8.van Heemst D. Insulin, IGF-1 and longevity. Aging Dis. 2010;1(2):147–157. [PMC free article] [PubMed] [Google Scholar]
- 9.Fulop T, et al. On the immunological theory of aging. Interdiscip Top Gerontol. 2014;39:163–176. doi: 10.1159/000358904. [DOI] [PubMed] [Google Scholar]
- 10.Brys K, Vanfleteren JR, Braeckman BP. Testing the rate-of-living/oxidative damage theory of aging in the nematode model Caenorhabditis elegans. Exp Gerontol. 2007;42(9):845–851. doi: 10.1016/j.exger.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Hulbert AJ, et al. Life and death: metabolic rate, membrane composition, and life span of animals. Physiol Rev. 2007;87(4):1175–1213. doi: 10.1152/physrev.00047.2006. [DOI] [PubMed] [Google Scholar]
- 12.Bjorksten J. The crosslinkage theory of aging. J Am Geriatr Soc. 1968;16(4):408–427. doi: 10.1111/j.1532-5415.1968.tb02821.x. [DOI] [PubMed] [Google Scholar]
- 13.Bjorksten J, Tenhu H. The crosslinking theory of aging–added evidence. Exp Gerontol. 1990;25(2):91–95. doi: 10.1016/0531-5565(90)90039-5. [DOI] [PubMed] [Google Scholar]
- 14.Gerschman R, et al. Oxygen poisoning and x-irradiation: a mechanism in common. Science. 1954;119(3097):623–626. doi: 10.1126/science.119.3097.623. [DOI] [PubMed] [Google Scholar]
- 15.Harman D. Aging: a theory based on free radical and radiation chemistry. J Gerontol. 1956;11(3):298–300. doi: 10.1093/geronj/11.3.298. [DOI] [PubMed] [Google Scholar]
- 16.Freitas AA, de Magalhães JP. A review and appraisal of the DNA damage theory of ageing. Mutat Res. 2011;728(1–2):12–22. doi: 10.1016/j.mrrev.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Taylor JP, Brown RH, Jr, Cleveland DW. Decoding ALS: from genes to mechanism. Nature. 2016;539(7628):197–206. doi: 10.1038/nature20413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Renton AE, et al. A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron. 2011;72(2):257–268. doi: 10.1016/j.neuron.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jellinger KA. The spectrum of cognitive dysfunction in amyotrophic lateral sclerosis: an update. Int J Mol Sci. 2023;24(19):14647. doi: 10.3390/ijms241914647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cividini C, et al. Amyotrophic lateral sclerosis-frontotemporal dementia: shared and divergent neural correlates across the clinical spectrum. Neurology. 2021;98(4):e402–e415. doi: 10.1212/WNL.0000000000013123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sattler R, et al. Roadmap for C9ORF72 in frontotemporal dementia and amyotrophic lateral sclerosis: report on the C9ORF72 FTD/ALS summit. Neurol Ther. 2023;12(6):1821–1843. doi: 10.1007/s40120-023-00548-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosen DR, et al. Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature. 1993;362(6415):59–62. doi: 10.1038/362059a0. [DOI] [PubMed] [Google Scholar]
- 23.Kabashi E, et al. TARDBP mutations in individuals with sporadic and familial amyotrophic lateral sclerosis. Nat Genet. 2008;40(5):572–574. doi: 10.1038/ng.132. [DOI] [PubMed] [Google Scholar]
- 24.Sreedharan J, et al. TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science. 2008;319(5870):1668–1672. doi: 10.1126/science.1154584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neumann M, et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314(5796):130–133. doi: 10.1126/science.1134108. [DOI] [PubMed] [Google Scholar]
- 26.Vance C, et al. Mutations in FUS, an RNA processing protein, cause familial amyotrophic lateral sclerosis type 6. Science. 2009;323(5918):1208–1211. doi: 10.1126/science.1165942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mead RJ, et al. Amyotrophic lateral sclerosis: a neurodegenerative disorder poised for successful therapeutic translation. Nat Rev Drug Discov. 2023;22(3):185–212. doi: 10.1038/s41573-022-00612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Akçimen F, et al. Amyotrophic lateral sclerosis: translating genetic discoveries into therapies. Nat Rev Genet. 2023;24(9):642–658. doi: 10.1038/s41576-023-00592-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Antignano I, et al. Aging microglia. Cell Mol Life Sci. 2023;80(5):126. doi: 10.1007/s00018-023-04775-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Snyder-Warwick AK, et al. Hypothalamic Sirt1 protects terminal Schwann cells and neuromuscular junctions from age-related morphological changes. Aging Cell. 2018;17(4):e12776. doi: 10.1111/acel.12776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Verma A (2021) Clinical manifestation and management of amyotrophic lateral sclerosis. In: Araki T (ED) Amyotrophic Lateral Sclerosis. Exon Publications Copyright: The Authors: Brisbane (AU) [PubMed]
- 32.Hobson EV, McDermott CJ. Supportive and symptomatic management of amyotrophic lateral sclerosis. Nat Rev Neurol. 2016;12(9):526–538. doi: 10.1038/nrneurol.2016.111. [DOI] [PubMed] [Google Scholar]
- 33.Cao X, Jin X, Liu B. The involvement of stress granules in aging and aging-associated diseases. Aging Cell. 2020;19(4):e13136. doi: 10.1111/acel.13136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jackson SP, Bartek J. The DNA-damage response in human biology and disease. Nature. 2009;461(7267):1071–1078. doi: 10.1038/nature08467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yousefzadeh M, et al. DNA damage-how and why we age? Elife. 2021;10:e62852. doi: 10.7554/eLife.62852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.De Sandre-Giovannoli A, et al. Lamin A truncation in Hutchinson–Gilford progeria. Science. 2003;300(5628):2055. doi: 10.1126/science.1084125. [DOI] [PubMed] [Google Scholar]
- 37.Eriksson M, et al. Recurrent de novo point mutations in lamin A cause Hutchinson-Gilford progeria syndrome. Nature. 2003;423(6937):293–298. doi: 10.1038/nature01629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Olive M, et al. Cardiovascular pathology in Hutchinson-Gilford progeria: correlation with the vascular pathology of aging. Arterioscler Thromb Vasc Biol. 2010;30(11):2301–2309. doi: 10.1161/ATVBAHA.110.209460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pennarun G, et al. Increase in lamin B1 promotes telomere instability by disrupting the shelterin complex in human cells. Nucleic Acids Res. 2021;49(17):9886–9905. doi: 10.1093/nar/gkab761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chou C-C, et al. TDP-43 pathology disrupts nuclear pore complexes and nucleocytoplasmic transport in ALS/FTD. Nat Neurosci. 2018;21(2):228–239. doi: 10.1038/s41593-017-0047-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin YC, et al. Interactions between ALS-linked FUS and nucleoporins are associated with defects in the nucleocytoplasmic transport pathway. Nat Neurosci. 2021;24(8):1077–1088. doi: 10.1038/s41593-021-00859-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chandra S, Lusk CP. Emerging connections between nuclear pore complex homeostasis and ALS. Int J Mol Sci. 2022;23(3):1329. doi: 10.3390/ijms23031329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coyne AN, Rothstein JD. Nuclear lamina invaginations are not a pathological feature of C9orf72 ALS/FTD. Acta Neuropathol Commun. 2021;9(1):45. doi: 10.1186/s40478-021-01150-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Megat S, et al. Loss of nucleoporin Nup50 is a risk factor for amyotrophic lateral sclerosis. MedRxiv. 2021 doi: 10.1101/2021.08.23.21262299. [DOI] [Google Scholar]
- 45.Mann JR, et al. Loss of function of the ALS-associated NEK1 kinase disrupts microtubule homeostasis and nuclear import. Sci Adv. 2023;9(33):eadi5548. doi: 10.1126/sciadv.adi5548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Narciso L, et al. The response to oxidative DNA damage in neurons: mechanisms and disease. Neural Plast. 2016;2016:3619274. doi: 10.1155/2016/3619274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Konopka A, Atkin JD. DNA damage, defective dna repair, and neurodegeneration in amyotrophic lateral sclerosis. Front Aging Neurosci. 2022;14:786420. doi: 10.3389/fnagi.2022.786420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Konopka A, et al. Impaired NHEJ repair in amyotrophic lateral sclerosis is associated with TDP-43 mutations. Mol Neurodegener. 2020;15(1):51. doi: 10.1186/s13024-020-00386-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Freibaum BD, et al. Global analysis of TDP-43 interacting proteins reveals strong association with RNA splicing and translation machinery. J Proteome Res. 2010;9(2):1104–1120. doi: 10.1021/pr901076y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hill SJ, et al. Two familial ALS proteins function in prevention/repair of transcription-associated DNA damage. Proc Natl Acad Sci U S A. 2016;113(48):E7701–e7709. doi: 10.1073/pnas.1611673113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang WY, et al. Interaction of FUS and HDAC1 regulates DNA damage response and repair in neurons. Nat Neurosci. 2013;16(10):1383–1391. doi: 10.1038/nn.3514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pelegrini AL, et al. Nek1 silencing slows down DNA repair and blocks DNA damage-induced cell cycle arrest. Mutagenesis. 2010;25(5):447–454. doi: 10.1093/mutage/geq026. [DOI] [PubMed] [Google Scholar]
- 53.Lai CK, et al. Functional characterization of putative cilia genes by high-content analysis. Mol Biol Cell. 2011;22(7):1104–1119. doi: 10.1091/mbc.e10-07-0596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fang X, et al. The NEK1 interactor, C21ORF2, is required for efficient DNA damage repair. Acta Biochim Biophys Sin (Shanghai) 2015;47(10):834–841. doi: 10.1093/abbs/gmv076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhu C, et al. Phospho-Ser(784)-VCP is required for DNA damage response and is associated with poor prognosis of chemotherapy-treated breast cancer. Cell Rep. 2020;31(10):107745. doi: 10.1016/j.celrep.2020.107745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rawal CC, et al. Senataxin ortholog Sen1 limits DNA:RNA hybrid accumulation at DNA double-strand breaks to control end resection and repair fidelity. Cell Rep. 2020;31(5):107603. doi: 10.1016/j.celrep.2020.107603. [DOI] [PubMed] [Google Scholar]
- 57.Shadfar S, et al. Redox dysregulation as a driver for DNA damage and its relationship to neurodegenerative diseases. Transl Neurodegener. 2023;12(1):18. doi: 10.1186/s40035-023-00350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Giannini M, et al. TDP-43 mutations link Amyotrophic Lateral Sclerosis with R-loop homeostasis and R loop-mediated DNA damage. PLoS Genet. 2020;16(12):e1009260. doi: 10.1371/journal.pgen.1009260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ziff OJ, et al. Integrated transcriptome landscape of ALS identifies genome instability linked to TDP-43 pathology. Nat Commun. 2023;14(1):2176. doi: 10.1038/s41467-023-37630-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mitra J, et al. Motor neuron disease-associated loss of nuclear TDP-43 is linked to DNA double-strand break repair defects. Proc Natl Acad Sci U S A. 2019;116(10):4696–4705. doi: 10.1073/pnas.1818415116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kawaguchi T, et al. Changes to the TDP-43 and FUS interactomes induced by DNA damage. J Proteome Res. 2020;19(1):360–370. doi: 10.1021/acs.jproteome.9b00575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Qiu H, et al. ALS-associated mutation FUS-R521C causes DNA damage and RNA splicing defects. J Clin Invest. 2014;124(3):981–999. doi: 10.1172/JCI72723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang H, et al. Mutant FUS causes DNA ligation defects to inhibit oxidative damage repair in amyotrophic lateral sclerosis. Nat Commun. 2018;9(1):3683. doi: 10.1038/s41467-018-06111-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Naumann M, et al. Impaired DNA damage response signaling by FUS-NLS mutations leads to neurodegeneration and FUS aggregate formation. Nat Commun. 2018;9(1):335. doi: 10.1038/s41467-017-02299-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Barbosa LF, et al. Increased SOD1 association with chromatin, DNA damage, p53 activation, and apoptosis in a cellular model of SOD1-linked ALS. Biochim Biophys Acta. 2010;1802(5):462–471. doi: 10.1016/j.bbadis.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 66.Farg MA, et al. The DNA damage response (DDR) is induced by the C9orf72 repeat expansion in amyotrophic lateral sclerosis. Hum Mol Genet. 2017;26(15):2882–2896. doi: 10.1093/hmg/ddx170. [DOI] [PubMed] [Google Scholar]
- 67.Walker C, et al. C9orf72 expansion disrupts ATM-mediated chromosomal break repair. Nat Neurosci. 2017;20(9):1225–1235. doi: 10.1038/nn.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nihei Y, et al. Poly-glycine-alanine exacerbates C9orf72 repeat expansion-mediated DNA damage via sequestration of phosphorylated ATM and loss of nuclear hnRNPA3. Acta Neuropathol. 2020;139(1):99–118. doi: 10.1007/s00401-019-02082-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.de Waard MC, et al. Age-related motor neuron degeneration in DNA repair-deficient Ercc1 mice. Acta Neuropathol. 2010;120(4):461–475. doi: 10.1007/s00401-010-0715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shadfar S, Brocardo M, Atkin JD. The complex mechanisms by which neurons die following DNA damage in neurodegenerative diseases. Int J Mol Sci. 2022;23(5):2484. doi: 10.3390/ijms23052484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Druzhyna NM, Wilson GL, LeDoux SP. Mitochondrial DNA repair in aging and disease. Mech Ageing Dev. 2008;129(7–8):383–390. doi: 10.1016/j.mad.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lin MT, Beal MF. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature. 2006;443(7113):787–795. doi: 10.1038/nature05292. [DOI] [PubMed] [Google Scholar]
- 73.Kudryavtseva AV, et al. Mitochondrial dysfunction and oxidative stress in aging and cancer. Oncotarget. 2016;7(29):44879–44905. doi: 10.18632/oncotarget.9821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yu CH, et al. TDP-43 Triggers Mitochondrial DNA release via mPTP to Activate cGAS/STING in ALS. Cell. 2020;183(3):636–649.e18. doi: 10.1016/j.cell.2020.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yu X, et al. Telomerase reverse transcriptase and neurodegenerative diseases. Front Immunol. 2023;14:1165632. doi: 10.3389/fimmu.2023.1165632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Linkus B, et al. Telomere shortening leads to earlier age of onset in ALS mice. Aging (Albany NY) 2016;8(2):382–393. doi: 10.18632/aging.100904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Robinson H, et al. Telomere attrition in induced pluripotent stem cell-derived neurons from ALS/FTD-related C9ORF72 repeat expansion carriers. Front Cell Dev Biol. 2022;10:874323. doi: 10.3389/fcell.2022.874323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Al Khleifat A, et al. Telomere length analysis in amyotrophic lateral sclerosis using large-scale whole genome sequence data. Front Cell Neurosci. 2022;16:1050596. doi: 10.3389/fncel.2022.1050596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kim EJ, et al. Increased telomere length in patients with frontotemporal dementia syndrome. J Neurol Sci. 2021;428:117565. doi: 10.1016/j.jns.2021.117565. [DOI] [PubMed] [Google Scholar]
- 80.Gao Y, et al. Mendelian randomization implies no direct causal association between leukocyte telomere length and amyotrophic lateral sclerosis. Sci Rep. 2020;10(1):12184. doi: 10.1038/s41598-020-68848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gonzalo S. Epigenetic alterations in aging. J Appl Physiol (1985) 2010;109(2):586–597. doi: 10.1152/japplphysiol.00238.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Eberharter A, Becker PB. Histone acetylation: a switch between repressive and permissive chromatin. EMBO Rep. 2002;3(3):224–229. doi: 10.1093/embo-reports/kvf053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lazo-Gómez R, et al. Histone deacetylases and their role in motor neuron degeneration. Front Cell Neurosci. 2013;7:243. doi: 10.3389/fncel.2013.00243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tejido C, Pakravan D, Bosch LVD. Potential therapeutic role of HDAC inhibitors in FUS-ALS. Front Mol Neurosci. 2021;14:686995. doi: 10.3389/fnmol.2021.686995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pasyukova EG, Vaiserman AM. HDAC inhibitors: a new promising drug class in anti-aging research. Mech Ageing Dev. 2017;166:6–15. doi: 10.1016/j.mad.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 86.Xi Z, et al. The C9orf72 repeat expansion itself is methylated in ALS and FTLD patients. Acta Neuropathol. 2015;129(5):715–727. doi: 10.1007/s00401-015-1401-8. [DOI] [PubMed] [Google Scholar]
- 87.Gijselinck I, et al. The C9orf72 repeat size correlates with onset age of disease, DNA methylation and transcriptional downregulation of the promoter. Mol Psychiatry. 2016;21(8):1112–1124. doi: 10.1038/mp.2015.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhang M, et al. DNA methylation age-acceleration is associated with disease duration and age at onset in C9orf72 patients. Acta Neuropathol. 2017;134(2):271–279. doi: 10.1007/s00401-017-1713-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Belzil VV, et al. Characterization of DNA hypermethylation in the cerebellum of c9FTD/ALS patients. Brain Res. 2014;1584:15–21. doi: 10.1016/j.brainres.2014.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Xi Z, et al. Hypermethylation of the CpG-island near the C9orf72 G4C2-repeat expansion in FTLD patients. Hum Mol Genet. 2014;23(21):5630–5637. doi: 10.1093/hmg/ddu279. [DOI] [PubMed] [Google Scholar]
- 91.Xi Z, et al. Hypermethylation of the CpG island near the G4C2 repeat in ALS with a C9orf72 expansion. Am J Hum Genet. 2013;92(6):981–989. doi: 10.1016/j.ajhg.2013.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Morahan JM, et al. A genome-wide analysis of brain DNA methylation identifies new candidate genes for sporadic amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2009;10(5–6):418–429. doi: 10.3109/17482960802635397. [DOI] [PubMed] [Google Scholar]
- 93.Figueroa-Romero C, et al. Identification of epigenetically altered genes in sporadic amyotrophic lateral sclerosis. PLoS ONE. 2012;7(12):e52672. doi: 10.1371/journal.pone.0052672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Liu EY, et al. C9orf72 hypermethylation protects against repeat expansion-associated pathology in ALS/FTD. Acta Neuropathol. 2014;128(4):525–541. doi: 10.1007/s00401-014-1286-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Appleby-Mallinder C, et al. TDP43 proteinopathy is associated with aberrant DNA methylation in human amyotrophic lateral sclerosis. Neuropathol Appl Neurobiol. 2021;47(1):61–72. doi: 10.1111/nan.12625. [DOI] [PubMed] [Google Scholar]
- 96.Hartung T, et al. Methylation and expression of mutant FUS in motor neurons differentiated from induced pluripotent stem cells from ALS patients. Front Cell Dev Biol. 2021;9:774751. doi: 10.3389/fcell.2021.774751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Martin LJ, et al. Aberrant DNA and RNA methylation occur in spinal cord and skeletal muscle of human SOD1 mouse models of ALS and in human ALS: targeting DNA methylation is therapeutic. Cells. 2022;11(21):3448. doi: 10.3390/cells11213448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tibshirani M, et al. Dysregulation of chromatin remodelling complexes in amyotrophic lateral sclerosis. Hum Mol Genet. 2017;26(21):4142–4152. doi: 10.1093/hmg/ddx301. [DOI] [PubMed] [Google Scholar]
- 99.Berson A, et al. TDP-43 promotes neurodegeneration by impairing chromatin remodeling. Curr Biol. 2017;27(23):3579–3590.e6. doi: 10.1016/j.cub.2017.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rossaert E, et al. Restoration of histone acetylation ameliorates disease and metabolic abnormalities in a FUS mouse model. Acta Neuropathol Commun. 2019;7(1):107. doi: 10.1186/s40478-019-0750-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Klingl YE, Pakravan D, Van Den Bosch L. Opportunities for histone deacetylase inhibition in amyotrophic lateral sclerosis. Br J Pharmacol. 2021;178(6):1353–1372. doi: 10.1111/bph.15217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Shahheydari H, et al. Protein quality control and the amyotrophic lateral sclerosis/frontotemporal dementia continuum. Front Mol Neurosci. 2017;10:119. doi: 10.3389/fnmol.2017.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Santra M, Dill KA, de Graff AMR. Proteostasis collapse is a driver of cell aging and death. Proc Natl Acad Sci. 2019;116(44):22173–22178. doi: 10.1073/pnas.1906592116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Moreno-García A, et al. An overview of the role of lipofuscin in age-related neurodegeneration. Front Neurosci. 2018;12:464. doi: 10.3389/fnins.2018.00464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Maxwell N, et al. α-Motor neurons are spared from aging while their synaptic inputs degenerate in monkeys and mice. Aging Cell. 2018;17(2):12726. doi: 10.1111/acel.12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rygiel KA, Grady JP, Turnbull DM. Respiratory chain deficiency in aged spinal motor neurons. Neurobiol Aging. 2014;35(10):2230–2238. doi: 10.1016/j.neurobiolaging.2014.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Nowotny K, et al. Advanced glycation end products and oxidative stress in type 2 diabetes mellitus. Biomolecules. 2015;5(1):194–222. doi: 10.3390/biom5010194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gerashchenko MV, et al. Translation elongation rate varies among organs and decreases with age. Nucleic Acids Res. 2020;49(2):e9–e9. doi: 10.1093/nar/gkaa1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Watanabe Y, Taguchi K, Tanaka M. Roles of stress response in autophagy processes and aging-related diseases. Int J Mol Sci. 2023;24(18):13804. doi: 10.3390/ijms241813804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Koga H, Kaushik S, Cuervo AM. Protein homeostasis and aging: The importance of exquisite quality control. Ageing Res Rev. 2011;10(2):205–215. doi: 10.1016/j.arr.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bobkova NV, et al. Exogenous Hsp70 delays senescence and improves cognitive function in aging mice. Proc Natl Acad Sci. 2015;112(52):16006–16011. doi: 10.1073/pnas.1516131112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Tsakiri EN, et al. Diet-derived advanced glycation end products or lipofuscin disrupts proteostasis and reduces life span in Drosophila melanogaster. Free Radical Biol Med. 2013;65:1155–1163. doi: 10.1016/j.freeradbiomed.2013.08.186. [DOI] [PubMed] [Google Scholar]
- 113.Cheng F, et al. Reducing oxidative protein folding alleviates senescence by minimizing ER-to-nucleus H(2) O(2) release. EMBO Rep. 2023;24(8):e56439. doi: 10.15252/embr.202256439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hafycz JM, Strus E, Naidoo N. Reducing ER stress with chaperone therapy reverses sleep fragmentation and cognitive decline in aged mice. Aging Cell. 2022;21(6):e13598. doi: 10.1111/acel.13598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Parakh S, et al. The redox activity of protein disulfide isomerase inhibits ALS phenotypes in cellular and Zebrafish models. iScience. 2020;23(5):101097. doi: 10.1016/j.isci.2020.101097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Parakh S, et al. Protein disulphide isomerase (PDI) is protective against amyotrophic lateral sclerosis (ALS)-related mutant Fused in Sarcoma (FUS) in in vitro models. Sci Rep. 2021;11(1):17557. doi: 10.1038/s41598-021-96181-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kwok CT, et al. Association studies indicate that protein disulfide isomerase is a risk factor in amyotrophic lateral sclerosis. Free Radical Biol Med. 2013;58:81–86. doi: 10.1016/j.freeradbiomed.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 118.Woehlbier U, et al. ALS-linked protein disulfide isomerase variants cause motor dysfunction. EMBO J. 2016;35(8):845–865. doi: 10.15252/embj.201592224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Xu S, et al. Cytosolic stress granules relieve the ubiquitin-proteasome system in the nuclear compartment. EMBO J. 2023;42(3):e111802. doi: 10.15252/embj.2022111802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Aulas A, Vande Velde C. Alterations in stress granule dynamics driven by TDP-43 and FUS a link to pathological inclusions in ALS? Front Cell Neurosci. 2015;9:423. doi: 10.3389/fncel.2015.00423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kedersha NL, et al. RNA-binding proteins TIA-1 and TIAR link the phosphorylation of eIF-2 alpha to the assembly of mammalian stress granules. J Cell Biol. 1999;147(7):1431–1442. doi: 10.1083/jcb.147.7.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Anderson P, Kedersha N. Stress granules: the Tao of RNA triage. Trends Biochem Sci. 2008;33(3):141–150. doi: 10.1016/j.tibs.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 123.Protter DSW, Parker R. Principles and properties of stress granules. Trends Cell Biol. 2016;26(9):668–679. doi: 10.1016/j.tcb.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kedersha N, et al. Dynamic shuttling of TIA-1 accompanies the recruitment of mRNA to mammalian stress granules. J Cell Biol. 2000;151(6):1257–1268. doi: 10.1083/jcb.151.6.1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kedersha N, et al. Evidence that ternary complex (eIF2-GTP-tRNA(i)(Met))-deficient preinitiation complexes are core constituents of mammalian stress granules. Mol Biol Cell. 2002;13(1):195–210. doi: 10.1091/mbc.01-05-0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Li Z, Liu X, Liu M. Stress granule homeostasis, aberrant phase transition, and amyotrophic lateral sclerosis. ACS Chem Neurosci. 2022;13(16):2356–2370. doi: 10.1021/acschemneuro.2c00262. [DOI] [PubMed] [Google Scholar]
- 127.Moujaber O, et al. Dissecting the molecular mechanisms that impair stress granule formation in aging cells. Biochim Biophys Acta Mol Cell Res. 2017;1864(3):475–486. doi: 10.1016/j.bbamcr.2016.12.008. [DOI] [PubMed] [Google Scholar]
- 128.Carey JL, Guo L. Liquid-liquid phase separation of TDP-43 and FUS in physiology and pathology of neurodegenerative diseases. Front Mol Biosci. 2022;9:826719. doi: 10.3389/fmolb.2022.826719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Moreno-Gonzalez I, Soto C. Misfolded protein aggregates: mechanisms, structures and potential for disease transmission. Semin Cell Dev Biol. 2011;22(5):482–487. doi: 10.1016/j.semcdb.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Liu-Yesucevitz L, et al. Tar DNA binding protein-43 (TDP-43) associates with stress granules: analysis of cultured cells and pathological brain tissue. PLoS ONE. 2010;5(10):e13250. doi: 10.1371/journal.pone.0013250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Dewey CM, et al. TDP-43 is directed to stress granules by sorbitol, a novel physiological osmotic and oxidative stressor. Mol Cell Biol. 2011;31(5):1098–1108. doi: 10.1128/MCB.01279-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.McDonald KK, et al. TAR DNA-binding protein 43 (TDP-43) regulates stress granule dynamics via differential regulation of G3BP and TIA-1. Hum Mol Genet. 2011;20(7):1400–1410. doi: 10.1093/hmg/ddr021. [DOI] [PubMed] [Google Scholar]
- 133.Colombrita C, et al. TDP-43 is recruited to stress granules in conditions of oxidative insult. J Neurochem. 2009;111(4):1051–1061. doi: 10.1111/j.1471-4159.2009.06383.x. [DOI] [PubMed] [Google Scholar]
- 134.Parker SJ, et al. Endogenous TDP-43 localized to stress granules can subsequently form protein aggregates. Neurochem Int. 2012;60(4):415–424. doi: 10.1016/j.neuint.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 135.Mateju D, et al. An aberrant phase transition of stress granules triggered by misfolded protein and prevented by chaperone function. EMBO J. 2017;36(12):1669–1687. doi: 10.15252/embj.201695957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gal J, et al. ALS mutant SOD1 interacts with G3BP1 and affects stress granule dynamics. Acta Neuropathol. 2016;132(4):563–576. doi: 10.1007/s00401-016-1601-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Bentmann E, et al. Requirements for stress granule recruitment of fused in sarcoma (FUS) and TAR DNA-binding protein of 43 kDa (TDP-43) J Biol Chem. 2012;287(27):23079–23094. doi: 10.1074/jbc.M111.328757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Volkening K, et al. Tar DNA binding protein of 43 kDa (TDP-43), 14–3–3 proteins and copper/zinc superoxide dismutase (SOD1) interact to modulate NFL mRNA stability. Implications for altered RNA processing in amyotrophic lateral sclerosis (ALS) Brain Res. 2009;1305:168–182. doi: 10.1016/j.brainres.2009.09.105. [DOI] [PubMed] [Google Scholar]
- 139.Ayala V, et al. Cell stress induces TDP-43 pathological changes associated with ERK1/2 dysfunction: implications in ALS. Acta Neuropathol. 2011;122(3):259–270. doi: 10.1007/s00401-011-0850-y. [DOI] [PubMed] [Google Scholar]
- 140.Meyerowitz J, et al. C-Jun N-terminal kinase controls TDP-43 accumulation in stress granules induced by oxidative stress. Mol Neurodegener. 2011;6:57. doi: 10.1186/1750-1326-6-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Andersson MK, et al. The multifunctional FUS, EWS and TAF15 proto-oncoproteins show cell type-specific expression patterns and involvement in cell spreading and stress response. BMC Cell Biol. 2008;9:37. doi: 10.1186/1471-2121-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Sama RR, et al. FUS/TLS assembles into stress granules and is a prosurvival factor during hyperosmolar stress. J Cell Physiol. 2013;228(11):2222–2231. doi: 10.1002/jcp.24395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Vance C, et al. ALS mutant FUS disrupts nuclear localization and sequesters wild-type FUS within cytoplasmic stress granules. Hum Mol Genet. 2013;22(13):2676–2688. doi: 10.1093/hmg/ddt117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Lenzi J, et al. ALS mutant FUS proteins are recruited into stress granules in induced pluripotent stem cell-derived motoneurons. Dis Model Mech. 2015;8(7):755–766. doi: 10.1242/dmm.020099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Dormann D, et al. ALS-associated fused in sarcoma (FUS) mutations disrupt Transportin-mediated nuclear import. Embo j. 2010;29(16):2841–2857. doi: 10.1038/emboj.2010.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Barbosa MC, Grosso RA, Fader CM. Hallmarks of aging: an autophagic perspective. Front Endocrinol (Lausanne) 2018;9:790. doi: 10.3389/fendo.2018.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Metaxakis A, Ploumi C, Tavernarakis N. Autophagy in age-associated neurodegeneration. Cells. 2018;7(5):37. doi: 10.3390/cells7050037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Carnio S, et al. Autophagy impairment in muscle induces neuromuscular junction degeneration and precocious aging. Cell Rep. 2014;8(5):1509–1521. doi: 10.1016/j.celrep.2014.07.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ramesh N, Pandey UB. Autophagy dysregulation in ALS: when protein aggregates get out of hand. Front Mol Neurosci. 2017 doi: 10.3389/fnmol.2017.00263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Nassif M, Woehlbier U, Manque PA. The enigmatic role of C9ORF72 in autophagy. Front Neurosci. 2017;11:442. doi: 10.3389/fnins.2017.00442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Madeo F, et al. Essential role for autophagy in life span extension. J Clin Invest. 2015;125(1):85–93. doi: 10.1172/JCI73946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Cuervo AM, Dice JF. Age-related decline in chaperone-mediated autophagy. J Biol Chem. 2000;275(40):31505–31513. doi: 10.1074/jbc.M002102200. [DOI] [PubMed] [Google Scholar]
- 153.Morimoto N, et al. Increased autophagy in transgenic mice with a G93A mutant SOD1 gene. Brain Res. 2007;1167:112–117. doi: 10.1016/j.brainres.2007.06.045. [DOI] [PubMed] [Google Scholar]
- 154.Kim J, et al. Autophagy activation and neuroprotection by progesterone in the G93A-SOD1 transgenic mouse model of amyotrophic lateral sclerosis. Neurobiol Dis. 2013;59:80–85. doi: 10.1016/j.nbd.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 155.Webster CP, et al. The C9orf72 protein interacts with Rab1a and the ULK1 complex to regulate initiation of autophagy. EMBO J. 2016;35(15):1656–1676. doi: 10.15252/embj.201694401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Sellier C, et al. Loss of C9ORF72 impairs autophagy and synergizes with polyQ Ataxin-2 to induce motor neuron dysfunction and cell death. EMBO J. 2016;35(12):1276–1297. doi: 10.15252/embj.201593350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Farg MA, et al. C9ORF72, implicated in amytrophic lateral sclerosis and frontotemporal dementia, regulates endosomal trafficking. Hum Mol Genet. 2014;23(13):3579–3595. doi: 10.1093/hmg/ddu068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Al-Sarraj S, et al. p62 positive, TDP-43 negative, neuronal cytoplasmic and intranuclear inclusions in the cerebellum and hippocampus define the pathology of C9orf72-linked FTLD and MND/ALS. Acta Neuropathol. 2011;122(6):691–702. doi: 10.1007/s00401-011-0911-2. [DOI] [PubMed] [Google Scholar]
- 159.Wang X, et al. Activation of ER stress and autophagy induced by TDP-43 A315T as pathogenic mechanism and the corresponding histological changes in skin as potential biomarker for ALS with the mutation. Int J Biol Sci. 2015;11(10):1140–1149. doi: 10.7150/ijbs.12657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kritsilis M, et al. Ageing, cellular senescence and neurodegenerative disease. Int J Mol Sci. 2018;19(10):2937. doi: 10.3390/ijms19102937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Sahu MR, et al. Cellular senescence in the aging brain: a promising target for neurodegenerative diseases. Mech Ageing Dev. 2022;204:111675. doi: 10.1016/j.mad.2022.111675. [DOI] [PubMed] [Google Scholar]
- 162.Childs BG, et al. Cellular senescence in aging and age-related disease: from mechanisms to therapy. Nat Med. 2015;21(12):1424–1435. doi: 10.1038/nm.4000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Grosse L, et al. Defined p16(High) senescent cell types are indispensable for mouse healthspan. Cell Metab. 2020;32(1):87–99.e6. doi: 10.1016/j.cmet.2020.05.002. [DOI] [PubMed] [Google Scholar]
- 164.Liao Z, et al. Cellular senescence: mechanisms and therapeutic potential. Biomedicines. 2021;9(12):1769. doi: 10.3390/biomedicines9121769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ovadya Y, et al. Impaired immune surveillance accelerates accumulation of senescent cells and aging. Nat Commun. 2018;9(1):5435. doi: 10.1038/s41467-018-07825-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.d'Adda di Fagagna F, et al. A DNA damage checkpoint response in telomere-initiated senescence. Nature. 2003;426(6963):194–198. doi: 10.1038/nature02118. [DOI] [PubMed] [Google Scholar]
- 167.Herbig U, et al. Telomere shortening triggers senescence of human cells through a pathway involving ATM, p53, and p21(CIP1), but not p16(INK4a) Mol Cell. 2004;14(4):501–513. doi: 10.1016/S1097-2765(04)00256-4. [DOI] [PubMed] [Google Scholar]
- 168.Di Micco R, et al. Cellular senescence in ageing: from mechanisms to therapeutic opportunities. Nat Rev Mol Cell Biol. 2021;22(2):75–95. doi: 10.1038/s41580-020-00314-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Rossiello F, et al. Telomere dysfunction in ageing and age-related diseases. Nat Cell Biol. 2022;24(2):135–147. doi: 10.1038/s41556-022-00842-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Gorgoulis V, et al. Cellular senescence: defining a path forward. Cell. 2019;179(4):813–827. doi: 10.1016/j.cell.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 171.Martínez-Cué C, Rueda N. Cellular senescence in neurodegenerative diseases. Front Cell Neurosci. 2020;14:16. doi: 10.3389/fncel.2020.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.van Deursen JM. The role of senescent cells in ageing. Nature. 2014;509(7501):439–446. doi: 10.1038/nature13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Limbad C, et al. Astrocyte senescence promotes glutamate toxicity in cortical neurons. PLoS ONE. 2020;15(1):e0227887. doi: 10.1371/journal.pone.0227887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Trias E, et al. Emergence of microglia bearing senescence markers during paralysis progression in a rat model of inherited ALS. Front Aging Neurosci. 2019;11:42. doi: 10.3389/fnagi.2019.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Matsudaira T, et al. Cellular senescence in white matter microglia is induced during ageing in mice and exacerbates the neuroinflammatory phenotype. Commun Biol. 2023 doi: 10.1038/s42003-023-05027-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.von Zglinicki T, Wan T, Miwa S. Senescence in post-mitotic cells: a driver of aging? Antioxid Redox Signal. 2021;34(4):308–323. doi: 10.1089/ars.2020.8048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Sah E, et al. The cellular senescence stress response in post-mitotic brain cells: cell survival at the expense of tissue degeneration. Life (Basel) 2021;11(3):229. doi: 10.3390/life11030229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Ishikawa S, Ishikawa F. Proteostasis failure and cellular senescence in long-term cultured postmitotic rat neurons. Aging Cell. 2020;19(1):e13071. doi: 10.1111/acel.13071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Ohashi M, et al. Loss of MECP2 leads to activation of P53 and neuronal senescence. Stem Cell Rep. 2018;10(5):1453–1463. doi: 10.1016/j.stemcr.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Pandya VA, Patani R. Region-specific vulnerability in neurodegeneration: lessons from normal ageing. Ageing Res Rev. 2021;67:101311. doi: 10.1016/j.arr.2021.101311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Sikora E, et al. Cellular senescence in brain aging. Front Aging Neurosci. 2021;13:646924. doi: 10.3389/fnagi.2021.646924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Birger A, et al. Human iPSC-derived astrocytes from ALS patients with mutated C9ORF72 show increased oxidative stress and neurotoxicity. EBioMedicine. 2019;50:274–289. doi: 10.1016/j.ebiom.2019.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Turnquist C, et al. p53 isoforms regulate astrocyte-mediated neuroprotection and neurodegeneration. Cell Death Differ. 2016;23(9):1515–1528. doi: 10.1038/cdd.2016.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Morgan JE, Partridge TA. Muscle satellite cells. Int J Biochem Cell Biol. 2003;35(8):1151–1156. doi: 10.1016/S1357-2725(03)00042-6. [DOI] [PubMed] [Google Scholar]
- 185.Sousa-Victor P, Perdiguero E, Muñoz-Cánoves P. Geroconversion of aged muscle stem cells under regenerative pressure. Cell Cycle. 2014;13(20):3183–3190. doi: 10.4161/15384101.2014.965072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Blanc RS, et al. PRMT7 preserves satellite cell regenerative capacity. Cell Rep. 2016;14(6):1528–1539. doi: 10.1016/j.celrep.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 187.Jeong HJ, et al. Prmt7 deficiency causes reduced skeletal muscle oxidative metabolism and age-related obesity. Diabetes. 2016;65(7):1868–1882. doi: 10.2337/db15-1500. [DOI] [PubMed] [Google Scholar]
- 188.Amorim JA, et al. Mitochondrial and metabolic dysfunction in ageing and age-related diseases. Nat Rev Endocrinol. 2022;18(4):243–258. doi: 10.1038/s41574-021-00626-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Bustamante-Barrientos FA, et al. Mitochondrial dysfunction in neurodegenerative disorders: potential therapeutic application of mitochondrial transfer to central nervous system-residing cells. J Transl Med. 2023;21(1):613. doi: 10.1186/s12967-023-04493-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Sasaki S, Iwata M. Mitochondrial alterations in the spinal cord of patients with sporadic amyotrophic lateral sclerosis. J Neuropathol Exp Neurol. 2007;66(1):10–16. doi: 10.1097/nen.0b013e31802c396b. [DOI] [PubMed] [Google Scholar]
- 191.Dafinca R, et al. Impairment of mitochondrial calcium buffering links mutations in C9ORF72 and TARDBP in iPS-derived motor neurons from patients with ALS/FTD. Stem Cell Rep. 2020;14(5):892–908. doi: 10.1016/j.stemcr.2020.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Onesto E, et al. Gene-specific mitochondria dysfunctions in human TARDBP and C9ORF72 fibroblasts. Acta Neuropathol Commun. 2016;4(1):47. doi: 10.1186/s40478-016-0316-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Wang T, et al. C9orf72 regulates energy homeostasis by stabilizing mitochondrial complex I assembly. Cell Metab. 2021;33(3):531–546.e9. doi: 10.1016/j.cmet.2021.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Mehta AR, et al. Mitochondrial bioenergetic deficits in C9orf72 amyotrophic lateral sclerosis motor neurons cause dysfunctional axonal homeostasis. Acta Neuropathol. 2021;141(2):257–279. doi: 10.1007/s00401-020-02252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lopez-Gonzalez R, et al. Poly(GR) in C9ORF72-related ALS/FTD compromises mitochondrial function and increases oxidative stress and DNA damage in iPSC-derived motor neurons. Neuron. 2016;92(2):383–391. doi: 10.1016/j.neuron.2016.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Choi SY, et al. C9ORF72-ALS/FTD-associated poly(GR) binds Atp5a1 and compromises mitochondrial function in vivo. Nat Neurosci. 2019;22(6):851–862. doi: 10.1038/s41593-019-0397-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Magrané J, et al. Abnormal mitochondrial transport and morphology are common pathological denominators in SOD1 and TDP43 ALS mouse models. Hum Mol Genet. 2014;23(6):1413–1424. doi: 10.1093/hmg/ddt528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Lu J, et al. Mitochondrial dysfunction in human TDP-43 transfected NSC34 cell lines and the protective effect of dimethoxy curcumin. Brain Res Bull. 2012;89(5–6):185–190. doi: 10.1016/j.brainresbull.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 199.Wang W, et al. The ALS disease-associated mutant TDP-43 impairs mitochondrial dynamics and function in motor neurons. Hum Mol Genet. 2013;22(23):4706–4719. doi: 10.1093/hmg/ddt319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Wang W, et al. The inhibition of TDP-43 mitochondrial localization blocks its neuronal toxicity. Nat Med. 2016;22(8):869–878. doi: 10.1038/nm.4130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Magrané J, et al. Mutant SOD1 in neuronal mitochondria causes toxicity and mitochondrial dynamics abnormalities. Hum Mol Genet. 2009;18(23):4552–4564. doi: 10.1093/hmg/ddp421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Lin BC, et al. ALS/FTD mutations in UBQLN2 are linked to mitochondrial dysfunction through loss-of-function in mitochondrial protein import. Hum Mol Genet. 2021;30(13):1230–1246. doi: 10.1093/hmg/ddab116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Ho WY, et al. Dysfunction in nonsense-mediated decay, protein homeostasis, mitochondrial function, and brain connectivity in ALS-FUS mice with cognitive deficits. Acta Neuropathol Commun. 2021;9(1):9. doi: 10.1186/s40478-020-01111-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Guo Y, et al. ALS-linked SOD1 mutations impair mitochondrial-derived vesicle formation and accelerate aging. Redox Biol. 2024;69:102972. doi: 10.1016/j.redox.2023.102972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Yang L, et al. The role of insulin/IGF-1/PI3K/Akt/GSK3beta signaling in Parkinson's disease dementia. Front Neurosci. 2018;12:73. doi: 10.3389/fnins.2018.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ogundele OM, et al. A putative mechanism of age-related synaptic dysfunction based on the impact of IGF-1 Receptor Signaling on synaptic CaMKIIalpha phosphorylation. Front Neuroanat. 2018;12:35. doi: 10.3389/fnana.2018.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Toyama EQ, et al. Metabolism AMP-activated protein kinase mediates mitochondrial fission in response to energy stress. Science. 2016;351(6270):275–281. doi: 10.1126/science.aab4138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Herranz N, et al. mTOR regulates MAPKAPK2 translation to control the senescence-associated secretory phenotype. Nat Cell Biol. 2015;17(9):1205–1217. doi: 10.1038/ncb3225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Mannick JB, Lamming DW. Targeting the biology of aging with mTOR inhibitors. Nat Aging. 2023;3(6):642–660. doi: 10.1038/s43587-023-00416-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Mazucanti CH, et al. Longevity pathways (mTOR, SIRT, Insulin/IGF-1) as key modulatory targets on aging and neurodegeneration. Curr Top Med Chem. 2015;15(21):2116–2138. doi: 10.2174/1568026615666150610125715. [DOI] [PubMed] [Google Scholar]
- 211.Jagaraj CJ, Parakh S, Atkin JD. Emerging evidence highlighting the importance of redox dysregulation in the pathogenesis of amyotrophic lateral sclerosis (ALS) Front Cell Neurosci. 2020;14:581950. doi: 10.3389/fncel.2020.581950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Chen C, et al. SIRT1 and aging related signaling pathways. Mech Ageing Dev. 2020;187:111215. doi: 10.1016/j.mad.2020.111215. [DOI] [PubMed] [Google Scholar]
- 213.Fang EF, et al. NAD(+) in aging: molecular mechanisms and translational implications. Trends Mol Med. 2017;23(10):899–916. doi: 10.1016/j.molmed.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Michan S, Sinclair D. Sirtuins in mammals: insights into their biological function. Biochem J. 2007;404(1):1–13. doi: 10.1042/BJ20070140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Grabowska W, Sikora E, Bielak-Zmijewska A. Sirtuins, a promising target in slowing down the ageing process. Biogerontology. 2017;18(4):447–476. doi: 10.1007/s10522-017-9685-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Taylor JR, et al. Sirt6 regulates lifespan in Drosophila melanogaster. Proc Natl Acad Sci U S A. 2022 doi: 10.1073/pnas.2111176119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Burnett C, et al. Absence of effects of Sir2 overexpression on lifespan in C. elegans and Drosophila. Nature. 2011;477(7365):482–485. doi: 10.1038/nature10296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Park S, Mori R, Shimokawa I. Do sirtuins promote mammalian longevity? A critical review on its relevance to the longevity effect induced by calorie restriction. Mol Cells. 2013;35(6):474–480. doi: 10.1007/s10059-013-0130-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Herskovits AZ, et al. SIRT1 deacetylase in aging-induced neuromuscular degeneration and amyotrophic lateral sclerosis. Aging Cell. 2018;17(6):e12839. doi: 10.1111/acel.12839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Granatiero V, et al. Modulation of the IGF1R-MTOR pathway attenuates motor neuron toxicity of human ALS SOD1(G93A) astrocytes. Autophagy. 2021;17(12):4029–4042. doi: 10.1080/15548627.2021.1899682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Wang IF, et al. Autophagy activators rescue and alleviate pathogenesis of a mouse model with proteinopathies of the TAR DNA-binding protein 43. Proc Natl Acad Sci U S A. 2012;109(37):15024–15029. doi: 10.1073/pnas.1206362109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Vincent AM, et al. Adeno-associated viral-mediated insulin-like growth factor delivery protects motor neurons in vitro. Neuromolecular Med. 2004;6(2–3):79–85. doi: 10.1385/NMM:6:2-3:079. [DOI] [PubMed] [Google Scholar]
- 223.Perera ND, et al. Mutant TDP-43 deregulates AMPK activation by PP2A in ALS models. PLoS ONE. 2014;9(4):e95549. doi: 10.1371/journal.pone.0095549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Pasinetti GM, Bilski AE, Zhao W. Sirtuins as therapeutic targets of ALS. Cell Res. 2013;23(9):1073–1074. doi: 10.1038/cr.2013.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Buck E, et al. Comparison of Sirtuin 3 levels in ALS and Huntington's disease-differential effects in human tissue samples vs Transgenic Mouse Models. Front Mol Neurosci. 2017;10:156. doi: 10.3389/fnmol.2017.00156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Tang BL. Could sirtuin activities modify ALS onset and progression? Cell Mol Neurobiol. 2017;37(7):1147–1160. doi: 10.1007/s10571-016-0452-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Garcia Morato J, et al. Sirtuin-1 sensitive lysine-136 acetylation drives phase separation and pathological aggregation of TDP-43. Nat Commun. 2022;13(1):1223. doi: 10.1038/s41467-022-28822-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Morato JG, et al. Sirtuin-1 sensitive lysine-136 acetylation drives phase separation and pathological aggregation of TDP-43. BioRxiv. 2021 doi: 10.1101/2020.05.26.104356v3.full. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Mancuso R, et al. Resveratrol improves motoneuron function and extends survival in SOD1(G93A) ALS mice. Neurotherapeutics. 2014;11(2):419–432. doi: 10.1007/s13311-013-0253-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Hendouei F, et al. Resveratrol as adjunctive therapy in treatment of irritability in children with autism: a double-blind and placebo-controlled randomized trial. J Clin Pharm Ther. 2020;45(2):324–334. doi: 10.1111/jcpt.13076. [DOI] [PubMed] [Google Scholar]
- 231.Biran A, et al. Senescent cells communicate via intercellular protein transfer. Genes Dev. 2015;29(8):791–802. doi: 10.1101/gad.259341.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Fafian-Labora JA, O'Loghlen A. Classical and nonclassical intercellular communication in senescence and ageing. Trends Cell Biol. 2020;30(8):628–639. doi: 10.1016/j.tcb.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 233.Dhirachaikulpanich D, et al. Intercellular communication analysis of the human retinal pigment epithelial and choroidal cells predicts pathways associated with aging, cellular senescence and age-related macular degeneration. Front Aging Neurosci. 2022;14:1016293. doi: 10.3389/fnagi.2022.1016293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Walters HE, Cox LS. Intercellular transfer of mitochondria between senescent cells through cytoskeleton-supported intercellular bridges requires mTOR and CDC42 signalling. Oxid Med Cell Longevity. 2021;2021:6697861. doi: 10.1155/2021/6697861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Phatnani HP, et al. Intricate interplay between astrocytes and motor neurons in ALS. Proc Natl Acad Sci USA. 2013;110(8):E756–E765. doi: 10.1073/pnas.1222361110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Brites D, Vaz AR. Microglia centered pathogenesis in ALS: insights in cell interconnectivity. Front Cell Neurosci. 2014;8:117. doi: 10.3389/fncel.2014.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Deepa P, et al. Down regulation of trophic factors in neonatal rat spinal cord after administration of cerebrospinal fluid from sporadic amyotrophic lateral sclerosis patients. J Neural Transm (Vienna) 2011;118(4):531–538. doi: 10.1007/s00702-010-0520-6. [DOI] [PubMed] [Google Scholar]
- 238.Gandelman M, et al. Extracellular ATP and the P2X7 receptor in astrocyte-mediated motor neuron death: implications for amyotrophic lateral sclerosis. J Neuroinflammation. 2010;7:33. doi: 10.1186/1742-2094-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Glass CK, et al. Mechanisms underlying inflammation in neurodegeneration. Cell. 2010;140(6):918–934. doi: 10.1016/j.cell.2010.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Philips T, et al. Oligodendrocyte dysfunction in the pathogenesis of amyotrophic lateral sclerosis. Brain. 2013;136(Pt 2):471–482. doi: 10.1093/brain/aws339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Haidet-Phillips AM, et al. Astrocytes from familial and sporadic ALS patients are toxic to motor neurons. Nat Biotechnol. 2011;29(9):824–U79. doi: 10.1038/nbt.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Das MM, Svendsen CN. Astrocytes show reduced support of motor neurons with aging that is accelerated in a rodent model of ALS. Neurobiol Aging. 2015;36(2):1130–1139. doi: 10.1016/j.neurobiolaging.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 243.Das MM, et al. Human neural progenitors differentiate into astrocytes and protect motor neurons in aging rats. Exp Neurol. 2016;280:41–49. doi: 10.1016/j.expneurol.2016.03.023. [DOI] [PubMed] [Google Scholar]
- 244.Kim G, Chen X, Yang Y. Pathogenic extracellular vesicle (EV) signaling in amyotrophic lateral sclerosis (ALS) Neurotherapeutics. 2022;19(4):1119–1132. doi: 10.1007/s13311-022-01232-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Mateescu B, et al. Phase 2 of extracellular RNA communication consortium charts next-generation approaches for extracellular RNA research. Iscience. 2022;25(8):104653. doi: 10.1016/j.isci.2022.104653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Takahashi A, et al. Exosomes maintain cellular homeostasis by excreting harmful DNA from cells. Nat Commun. 2017;8:15287. doi: 10.1038/ncomms15287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Dluzen DF, Noren Hooten N, Evans MK. Extracellular RNA in aging. Wiley Interdiscip Rev RNA. 2017;8(2):96–98. doi: 10.1002/wrna.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Eitan E, et al. Age-related changes in plasma extracellular vesicle characteristics and internalization by leukocytes. Sci Rep. 2017;7(1):1342. doi: 10.1038/s41598-017-01386-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Alibhai FJ, et al. Cellular senescence contributes to age-dependent changes in circulating extracellular vesicle cargo and function. Aging Cell. 2020;19(3):e13103. doi: 10.1111/acel.13103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Jeon OH, et al. Senescence cell-associated extracellular vesicles serve as osteoarthritis disease and therapeutic markers. JCI Insight. 2019 doi: 10.1172/jci.insight.125019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Hosaka T, et al. Extracellular RNAs as biomarkers of sporadic amyotrophic lateral sclerosis and other neurodegenerative diseases. Int J Mol Sci. 2019;20(13):3148. doi: 10.3390/ijms20133148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Basso M, et al. Mutant copper-zinc superoxide dismutase (SOD1) induces protein secretion pathway alterations and exosome release in astrocytes implications for disease spreading and motor neuron pathology in amyotrophic lateral sclerosis. J Biol Chem. 2013;288(22):15699–15711. doi: 10.1074/jbc.M112.425066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Sproviero D, et al. Pathological proteins are transported by extracellular vesicles of sporadic amyotrophic lateral sclerosis patients. Front Neurosci. 2018;12:487. doi: 10.3389/fnins.2018.00487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Grad LI, et al. Intercellular propagated misfolding of wild-type Cu/Zn superoxide dismutase occurs via exosome-dependent and -independent mechanisms. Proc Natl Acad Sci U S A. 2014;111(9):3620–5. doi: 10.1073/pnas.1312245111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Munch C, O'Brien J, Bertolotti A. Prion-like propagation of mutant superoxide dismutase-1 misfolding in neuronal cells. Proc Natl Acad Sci U S A. 2011;108(9):3548–53. doi: 10.1073/pnas.1017275108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Furukawa Y, et al. Intracellular seeded aggregation of mutant Cu, Zn-superoxide dismutase associated with amyotrophic lateral sclerosis. FEBS Lett. 2013;587(16):2500–5. doi: 10.1016/j.febslet.2013.06.046. [DOI] [PubMed] [Google Scholar]
- 257.Ekhtiari Bidhendi E, et al. Mutant superoxide dismutase aggregates from human spinal cord transmit amyotrophic lateral sclerosis. Acta Neuropathol. 2018;136(6):939–953. doi: 10.1007/s00401-018-1915-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Silverman JM, et al. CNS-derived extracellular vesicles from superoxide dismutase 1 (SOD1)(G93A) ALS mice originate from astrocytes and neurons and carry misfolded SOD1. J Biol Chem. 2019;294(10):3744–3759. doi: 10.1074/jbc.RA118.004825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Mishra PS, et al. Transmission of ALS pathogenesis by the cerebrospinal fluid. Acta Neuropathol Commun. 2020;8(1):65. doi: 10.1186/s40478-020-00943-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Porta S, et al. Patient-derived frontotemporal lobar degeneration brain extracts induce formation and spreading of TDP-43 pathology in vivo. Nat Commun. 2018;9(1):4220. doi: 10.1038/s41467-018-06548-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Iguchi Y, et al. Exosome secretion is a key pathway for clearance of pathological TDP-43. Brain. 2016;139(Pt 12):3187–3201. doi: 10.1093/brain/aww237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Westergard T, et al. Cell-to-cell transmission of dipeptide repeat proteins linked to C9orf72-ALS/FTD. Cell Rep. 2016;17(3):645–652. doi: 10.1016/j.celrep.2016.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Aquino-Martinez R, et al. Senescent cells exacerbate chronic inflammation and contribute to periodontal disease progression in old mice. J Periodontol. 2021;92(10):1483–1495. doi: 10.1002/JPER.20-0529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Brahadeeswaran S, Sivagurunathan N, Calivarathan L. Inflammasome signaling in the aging brain and age-related neurodegenerative diseases. Mol Neurobiol. 2022;59(4):2288–2304. doi: 10.1007/s12035-021-02683-5. [DOI] [PubMed] [Google Scholar]
- 265.Deora V, et al. The microglial NLRP3 inflammasome is activated by amyotrophic lateral sclerosis proteins. Glia. 2020;68(2):407–421. doi: 10.1002/glia.23728. [DOI] [PubMed] [Google Scholar]
- 266.Gudkov SV, et al. An emerging role of astrocytes in aging/neuroinflammation and gut-brain axis with consequences on sleep and sleep disorders. Ageing Res Rev. 2023;83:101775. doi: 10.1016/j.arr.2022.101775. [DOI] [PubMed] [Google Scholar]
- 267.Di Benedetto S, et al. Contribution of neuroinflammation and immunity to brain aging and the mitigating effects of physical and cognitive interventions. Neurosci Biobehav Rev. 2017;75:114–128. doi: 10.1016/j.neubiorev.2017.01.044. [DOI] [PubMed] [Google Scholar]
- 268.Rothhammer V, et al. Microglial control of astrocytes in response to microbial metabolites. Nature. 2018;557(7707):724–728. doi: 10.1038/s41586-018-0119-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Adrover JM, Nicolas-Avila JA, Hidalgo A. Aging: a temporal dimension for neutrophils. Trends Immunol. 2016;37(5):334–345. doi: 10.1016/j.it.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 270.Boisvert MM, et al. The aging astrocyte transcriptome from multiple regions of the mouse brain. Cell Rep. 2018;22(1):269–285. doi: 10.1016/j.celrep.2017.12.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Clarke LE, et al. Normal aging induces A1-like astrocyte reactivity. Proc Natl Acad Sci USA. 2018;115(8):E1896–E1905. doi: 10.1073/pnas.1800165115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Lana D, et al. Microglial distribution, branching, and clearance activity in aged rat hippocampus are affected by astrocyte meshwork integrity: evidence of a novel cell-cell interglial interaction. FASEB J. 2019;33(3):4007–4020. doi: 10.1096/fj.201801539R. [DOI] [PubMed] [Google Scholar]
- 273.Liu E, Karpf L, Bohl D. Neuroinflammation in amyotrophic lateral sclerosis and frontotemporal dementia and the interest of induced pluripotent stem cells to study immune cells interactions with neurons. Front Mol Neurosci. 2021;14:767041. doi: 10.3389/fnmol.2021.767041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Liu J, Wang F. Role of neuroinflammation in amyotrophic lateral sclerosis: cellular mechanisms and therapeutic implications. Front Immunol. 2017;8:1005. doi: 10.3389/fimmu.2017.01005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Gugliandolo A, et al. NLRP3 inflammasome activation in a transgenic amyotrophic lateral sclerosis model. Inflammation. 2018;41(1):93–103. doi: 10.1007/s10753-017-0667-5. [DOI] [PubMed] [Google Scholar]
- 276.Bellezza I, et al. Peroxynitrite activates the NLRP3 inflammasome cascade in SOD1(G93A) mouse model of amyotrophic lateral sclerosis. Mol Neurobiol. 2018;55(3):2350–2361. doi: 10.1007/s12035-017-0502-x. [DOI] [PubMed] [Google Scholar]
- 277.Johann S, et al. NLRP3 inflammasome is expressed by astrocytes in the SOD1 mouse model of ALS and in human sporadic ALS patients. Glia. 2015;63(12):2260–73. doi: 10.1002/glia.22891. [DOI] [PubMed] [Google Scholar]
- 278.Zhao W, et al. TDP-43 activates microglia through NF-kappaB and NLRP3 inflammasome. Exp Neurol. 2015;273:24–35. doi: 10.1016/j.expneurol.2015.07.019. [DOI] [PubMed] [Google Scholar]
- 279.Clarke BE, Patani R. The microglial component of amyotrophic lateral sclerosis. Brain. 2020;143(12):3526–3539. doi: 10.1093/brain/awaa309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Pehar M, et al. Role and therapeutic potential of astrocytes in amyotrophic lateral sclerosis. Curr Pharm Des. 2017;23(33):5010–5021. doi: 10.2174/1381612823666170622095802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Teng YD, et al. Multimodal actions of neural stem cells in a mouse model of ALS: a meta-analysis. Sci Transl Med. 2012;4(165):165ra164–165ra164. doi: 10.1126/scitranslmed.3004579. [DOI] [PubMed] [Google Scholar]
- 282.Carpentier PA, Palmer TD. Immune influence on adult neural stem cell regulation and function. Neuron. 2009;64(1):79–92. doi: 10.1016/j.neuron.2009.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Blacher E, et al. Potential roles of gut microbiome and metabolites in modulating ALS in mice. Nature. 2019;572(7770):474–480. doi: 10.1038/s41586-019-1443-5. [DOI] [PubMed] [Google Scholar]
- 284.Wu S, et al. Leaky intestine and impaired microbiome in an amyotrophic lateral sclerosis mouse model. Physiol Rep. 2015;3(4):e12356. doi: 10.14814/phy2.12356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Zhang Y, et al. A new role for oxidative stress in aging: The accelerated aging phenotype in Sod1(-/)(-) mice is correlated to increased cellular senescence. Redox Biol. 2017;11:30–37. doi: 10.1016/j.redox.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Burberry A, et al. C9orf72 suppresses systemic and neural inflammation induced by gut bacteria. Nature. 2020;582(7810):89–94. doi: 10.1038/s41586-020-2288-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Harries LW. Dysregulated RNA processing and metabolism: a new hallmark of ageing and provocation for cellular senescence. FEBS J. 2023;290(5):1221–1234. doi: 10.1111/febs.16462. [DOI] [PubMed] [Google Scholar]
- 288.Nussbacher JK, et al. Disruption of RNA metabolism in neurological diseases and emerging therapeutic interventions. Neuron. 2019;102(2):294–320. doi: 10.1016/j.neuron.2019.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Butti Z, Patten SA. RNA dysregulation in amyotrophic lateral sclerosis. Front Genet. 2018;9:712. doi: 10.3389/fgene.2018.00712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Fu X-D, Ares M. Context-dependent control of alternative splicing by RNA-binding proteins. Nat Rev Genet. 2014;15(10):689–701. doi: 10.1038/nrg3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Varesi A, et al. RNA binding proteins in senescence: a potential common linker for age-related diseases? Ageing Res Rev. 2023;88:101958. doi: 10.1016/j.arr.2023.101958. [DOI] [PubMed] [Google Scholar]
- 292.Harries LW, et al. Human aging is characterized by focused changes in gene expression and deregulation of alternative splicing. Aging Cell. 2011;10(5):868–78. doi: 10.1111/j.1474-9726.2011.00726.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Jung S, Arcos Hodar J, del Sol A. Measuring biological age using a functionally interpretable multi-tissue RNA clock. Aging Cell. 2023;22(5):13799. doi: 10.1111/acel.13799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Ren X, Kuan PF. RNAAgeCalc: a multi-tissue transcriptional age calculator. PLoS ONE. 2020;15(8):e0237006. doi: 10.1371/journal.pone.0237006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Souliotis VL, et al. DNA damage response and oxidative stress in systemic autoimmunity. Int J Mol Sci. 2019;21(1):55. doi: 10.3390/ijms21010055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Debès C, et al. Ageing-associated changes in transcriptional elongation influence longevity. Nature. 2023;616(7958):814–821. doi: 10.1038/s41586-023-05922-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Stoeger T, et al. Aging is associated with a systemic length-associated transcriptome imbalance. Nature Aging. 2022;2(12):1191–1206. doi: 10.1038/s43587-022-00317-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Tollervey JR, et al. Analysis of alternative splicing associated with aging and neurodegeneration in the human brain. Genome Res. 2011;21(10):1572–82. doi: 10.1101/gr.122226.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Holly AC, et al. Changes in splicing factor expression are associated with advancing age in man. Mech Ageing Dev. 2013;134(9):356–66. doi: 10.1016/j.mad.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Ward AJ, Cooper TA. The pathobiology of splicing. J Pathol. 2010;220(2):152–63. doi: 10.1002/path.2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Gyenis A, et al. Genome-wide RNA polymerase stalling shapes the transcriptome during aging. Nat Genet. 2023;55(2):268–279. doi: 10.1038/s41588-022-01279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Son HG, et al. RNA surveillance via nonsense-mediated mRNA decay is crucial for longevity in daf-2/insulin/IGF-1 mutant C. elegans. Nat Commun. 2017;8(1):14749. doi: 10.1038/ncomms14749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.McMahon M, Forester C, Buffenstein R. Aging through an epitranscriptomic lens. Nature Aging. 2021;1(4):335–346. doi: 10.1038/s43587-021-00058-y. [DOI] [PubMed] [Google Scholar]
- 304.Min K-W, et al. Profiling of m6A RNA modifications identified an age-associated regulation of AGO2 mRNA stability. Aging Cell. 2018;17(3):e12753. doi: 10.1111/acel.12753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Castro-Hernández R, et al. Conserved reduction of m6A RNA modifications during aging and neurodegeneration is linked to changes in synaptic transcripts. Proc Natl Acad Sci. 2023;120(9):e2204933120. doi: 10.1073/pnas.2204933120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Nicholas A, et al. Age-related gene-specific changes of A-to-I mRNA editing in the human brain. Mech Ageing Dev. 2010;131(6):445–7. doi: 10.1016/j.mad.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Cole DC, et al. Loss of APOBEC1 RNA-editing function in microglia exacerbates age-related CNS pathophysiology. Proc Natl Acad Sci. 2017;114(50):13272–13277. doi: 10.1073/pnas.1710493114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Wagner V, et al. Characterizing expression changes in noncoding RNAs during aging and heterochronic parabiosis across mouse tissues. Nat Biotechnol. 2023;42:109–118. doi: 10.1038/s41587-023-01751-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Somel M, et al. MicroRNA, mRNA, and protein expression link development and aging in human and macaque brain. Genome Res. 2010;20(9):1207–18. doi: 10.1101/gr.106849.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Butler AA, et al. Long noncoding RNA NEAT1 mediates neuronal histone methylation and age-related memory impairment. Sci Signal. 2019;12(588):9277. doi: 10.1126/scisignal.aaw9277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Xiong H, et al. Knockdown of long noncoding RNA SAN rejuvenates aged adipose-derived stem cells via miR-143-3p/ADD3 axis. Stem Cell Res Ther. 2023;14(1):213. doi: 10.1186/s13287-023-03441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Gurkar AU, et al. Spatial mapping of cellular senescence: emerging challenges and opportunities. Nat Aging. 2023;3(7):776–790. doi: 10.1038/s43587-023-00446-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Srinivas T, et al. Roles of lncRNAs in brain development and pathogenesis: emerging therapeutic opportunities. Mol Ther. 2023;31(6):1550–1561. doi: 10.1016/j.ymthe.2023.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Memczak S, et al. Circular RNAs are a large class of animal RNAs with regulatory potency. Nature. 2013;495(7441):333–8. doi: 10.1038/nature11928. [DOI] [PubMed] [Google Scholar]
- 315.Niu R, Liu J. Circular RNA involvement in aging and longevity. Curr Genomics. 2022;23(5):318–325. doi: 10.2174/1389202923666220927110258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Cai H, et al. Circular RNA involvement in aging: an emerging player with great potential. Mech Ageing Dev. 2019;178:16–24. doi: 10.1016/j.mad.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 317.Errichelli L, et al. FUS affects circular RNA expression in murine embryonic stem cell-derived motor neurons. Nat Commun. 2017;8(1):14741. doi: 10.1038/ncomms14741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Colantoni A, et al. FUS Alters circRNA metabolism in human motor neurons carrying the ALS-Linked P525L mutation. Int J Mol Sci. 2023;24(4):3181. doi: 10.3390/ijms24043181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Aksoy YA, et al. "STRESSED OUT": The role of FUS and TDP-43 in amyotrophic lateral sclerosis. Int J Biochem Cell Biol. 2020;126:105821. doi: 10.1016/j.biocel.2020.105821. [DOI] [PubMed] [Google Scholar]
- 320.Baughn MW, et al. Mechanism of STMN2 cryptic splice-polyadenylation and its correction for TDP-43 proteinopathies. Science. 2023;379(6637):1140–1149. doi: 10.1126/science.abq5622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Li Y, et al. Globally reduced N6-methyladenosine (m6A) in C9ORF72-ALS/FTD dysregulates RNA metabolism and contributes to neurodegeneration. Nat Neurosci. 2023;26(8):1328–1338. doi: 10.1038/s41593-023-01374-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Hideyama T, et al. Profound downregulation of the RNA editing enzyme ADAR2 in ALS spinal motor neurons. Neurobiol Dis. 2012;45(3):1121–8. doi: 10.1016/j.nbd.2011.12.033. [DOI] [PubMed] [Google Scholar]
- 323.Zhang X, et al. Small RNA modifications in Alzheimer's disease. Neurobiol Dis. 2020;145:105058. doi: 10.1016/j.nbd.2020.105058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Lee Y-B, et al. Hexanucleotide repeats in ALS/FTD Form length-dependent RNA foci, sequester RNA binding proteins, and are neurotoxic. Cell Rep. 2013;5(5):1178–1186. doi: 10.1016/j.celrep.2013.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Cooper-Knock J, et al. Sequestration of multiple RNA recognition motif-containing proteins by C9orf72 repeat expansions. Brain. 2014;137(7):2040–2051. doi: 10.1093/brain/awu120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Xu W, et al. Reactivation of nonsense-mediated mRNA decay protects against C9orf72 dipeptide-repeat neurotoxicity. Brain. 2019;142(5):1349–1364. doi: 10.1093/brain/awz070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Kamelgarn M, et al. ALS mutations of FUS suppress protein translation and disrupt the regulation of nonsense-mediated decay. Proc Natl Acad Sci U S A. 2018;115(51):E11904–e11913. doi: 10.1073/pnas.1810413115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Dobrowolny G, et al. A longitudinal study defined circulating microRNAs as reliable biomarkers for disease prognosis and progression in ALS human patients. Cell Death Discov. 2021;7(1):4. doi: 10.1038/s41420-020-00397-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Wang C, et al. Stress induces dynamic, cytotoxicity-antagonizing TDP-43 nuclear bodies via Paraspeckle LncRNA NEAT1-mediated liquid–liquid phase separation. Mol Cell. 2020;79(3):443–458.e7. doi: 10.1016/j.molcel.2020.06.019. [DOI] [PubMed] [Google Scholar]
- 330.Li P, et al. Identification and characterization of N6-methyladenosine CircRNAs and methyltransferases in the lens epithelium cells from age-related cataract. Invest Ophthalmol Vis Sci. 2020;61(10):13–13. doi: 10.1167/iovs.61.10.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Tang H, et al. HuR regulates telomerase activity through TERC methylation. Nat Commun. 2018;9(1):2213. doi: 10.1038/s41467-018-04617-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Wang P, et al. TDP-43 induces mitochondrial damage and activates the mitochondrial unfolded protein response. PLoS Genet. 2019;15(5):e1007947. doi: 10.1371/journal.pgen.1007947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Konopka A, Atkin JD. The emerging role of DNA damage in the pathogenesis of the C9orf72 repeat expansion in amyotrophic lateral sclerosis. Int J Mol Sci. 2018;19(10):3137. doi: 10.3390/ijms19103137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Sengupta D, Sengupta K. Lamin A and telomere maintenance in aging: two to Tango. Mut Res Fundam Mol Mech Mutagen. 2022;825:111788. doi: 10.1016/j.mrfmmm.2022.111788. [DOI] [PubMed] [Google Scholar]
- 335.Hou Y, et al. Ageing as a risk factor for neurodegenerative disease. Nat Rev Neurol. 2019;15(10):565–581. doi: 10.1038/s41582-019-0244-7. [DOI] [PubMed] [Google Scholar]
- 336.Yu R, et al. Inactivating histone deacetylase HDA promotes longevity by mobilizing trehalose metabolism. Nat Commun. 2021;12(1):1981. doi: 10.1038/s41467-021-22257-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Parakh S, et al. Rab-dependent cellular trafficking and amyotrophic lateral sclerosis. Crit Rev Biochem Mol Biol. 2018;53(6):623–651. doi: 10.1080/10409238.2018.1553926. [DOI] [PubMed] [Google Scholar]
- 338.Parakh S, et al. ERp57 is protective against mutant SOD1-induced cellular pathology in amyotrophic lateral sclerosis. Hum Mol Genet. 2018;27(8):1311–1331. doi: 10.1093/hmg/ddy041. [DOI] [PubMed] [Google Scholar]
- 339.Haase G, Rabouille C. Golgi fragmentation in ALS motor neurons. new mechanisms targeting microtubules, tethers, and transport vesicles. Front Neurosci. 2015;2015(9):448. doi: 10.3389/fnins.2015.00448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Soo KY, et al. Rab1-dependent ER-Golgi transport dysfunction is a common pathogenic mechanism in SOD1, TDP-43 and FUS-associated ALS. Acta Neuropathol. 2015;130(5):679–97. doi: 10.1007/s00401-015-1468-2. [DOI] [PubMed] [Google Scholar]
- 341.Valenzuela V, Nassif M, Hetz C. Unraveling the role of motoneuron autophagy in ALS. Autophagy. 2018;14(4):733–737. doi: 10.1080/15548627.2018.1432327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Evans CS, Holzbaur ELF. Autophagy and mitophagy in ALS. Neurobiol Dis. 2019;122:35–40. doi: 10.1016/j.nbd.2018.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Nguyen DKH, Thombre R, Wang J. Autophagy as a common pathway in amyotrophic lateral sclerosis. Neurosci Lett. 2018 doi: 10.1016/j.neulet.2018.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Ho WY, et al. The ALS-FTD-linked gene product, C9orf72, regulates neuronal morphogenesis via autophagy. Autophagy. 2019;15:1–16. doi: 10.1080/15548627.2019.1569441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Rudnick ND, et al. Distinct roles for motor neuron autophagy early and late in the SOD1(G93A) mouse model of ALS. Proc Natl Acad Sci U S A. 2017;114(39):E8294–e8303. doi: 10.1073/pnas.1704294114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Chen T, et al. Mutant UBQLN2(P497H) in motor neurons leads to ALS-like phenotypes and defective autophagy in rats. Acta Neuropathol Commun. 2018;6(1):122. doi: 10.1186/s40478-018-0627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Chitiprolu M, et al. A complex of C9ORF72 and p62 uses arginine methylation to eliminate stress granules by autophagy. Nat Commun. 2018;9(1):2794. doi: 10.1038/s41467-018-05273-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Madill M, et al. Amyotrophic lateral sclerosis patient iPSC-derived astrocytes impair autophagy via non-cell autonomous mechanisms. Mol Brain. 2017;10(1):22. doi: 10.1186/s13041-017-0300-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Ma Y, Farny NG. Connecting the dots: neuronal senescence, stress granules, and neurodegeneration. Gene. 2023;871:147437. doi: 10.1016/j.gene.2023.147437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Miwa S, et al. Mitochondrial dysfunction in cell senescence and aging. J Clin Invest. 2022;132(13):158447. doi: 10.1172/JCI158447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Zhao J, et al. The impact of mitochondrial dysfunction in amyotrophic lateral sclerosis. Cells. 2022;11(13):2049. doi: 10.3390/cells11132049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Delic V, et al. Discrete mitochondrial aberrations in the spinal cord of sporadic ALS patients. J Neurosci Res. 2018;96(8):1353–1366. doi: 10.1002/jnr.24249. [DOI] [PubMed] [Google Scholar]
- 353.Deng J, et al. FUS interacts with ATP synthase beta subunit and induces mitochondrial unfolded protein response in cellular and animal models. Proc Natl Acad Sci U S A. 2018;115(41):E9678–e9686. doi: 10.1073/pnas.1806655115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Khalil B, Lievens JC. Mitochondrial quality control in amyotrophic lateral sclerosis: towards a common pathway? Neural Regen Res. 2017;12(7):1052–1061. doi: 10.4103/1673-5374.211179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Perera ND, et al. Rilmenidine promotes MTOR-independent autophagy in the mutant SOD1 mouse model of amyotrophic lateral sclerosis without slowing disease progression. Autophagy. 2018;14(3):534–551. doi: 10.1080/15548627.2017.1385674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Ugolino J, et al. Loss of C9orf72 enhances autophagic activity via deregulated mTOR and TFEB signaling. PLoS Genet. 2016;12(11):e1006443. doi: 10.1371/journal.pgen.1006443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Di Giorgio FP, et al. Non-cell autonomous effect of glia on motor neurons in an embryonic stem cell-based ALS model. Nat Neurosci. 2007;10(5):608–14. doi: 10.1038/nn1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Rodriguez MJ, Mahy N. Neuron–microglia interactions in motor neuron degeneration. The inflammatory hypothesis in amyotrophic lateral sclerosis revisited. Curr Med Chem. 2016;23(42):4753–4772. doi: 10.2174/0929867324666161123091314. [DOI] [PubMed] [Google Scholar]
- 359.Parisi C, et al. Dysregulated microRNAs in amyotrophic lateral sclerosis microglia modulate genes linked to neuroinflammation. Cell Death Dis. 2013;4:e959. doi: 10.1038/cddis.2013.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Frakes AE, et al. Microglia induce motor neuron death via the classical NF-kappaB pathway in amyotrophic lateral sclerosis. Neuron. 2014;81(5):1009–1023. doi: 10.1016/j.neuron.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Radford RA, et al. The established and emerging roles of astrocytes and microglia in amyotrophic lateral sclerosis and frontotemporal dementia. Front Cell Neurosci. 2015;9:414. doi: 10.3389/fncel.2015.00414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Lee HJ, et al. Human motor neurons generated from neural stem cells delay clinical onset and prolong life in ALS mouse model. PLoS ONE. 2014;9(5):e97518. doi: 10.1371/journal.pone.0097518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Hoye ML, et al. MicroRNA profiling reveals marker of motor neuron disease in ALS models. J Neurosci. 2017;37(22):5574–5586. doi: 10.1523/JNEUROSCI.3582-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Zhou Y, et al. FUS-regulated RNA metabolism and DNA damage repair: Implications for amyotrophic lateral sclerosis and frontotemporal dementia pathogenesis. Rare Dis. 2014;2:e29515. doi: 10.4161/rdis.29515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Droppelmann CA, et al. RNA metabolism in ALS: when normal processes become pathological. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15(5–6):321–36. doi: 10.3109/21678421.2014.881377. [DOI] [PubMed] [Google Scholar]
- 366.Alami NH, et al. Axonal transport of TDP-43 mRNA granules is impaired by ALS-causing mutations. Neuron. 2014;81(3):536–543. doi: 10.1016/j.neuron.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Lee J, Kim HJ. Normal aging induces changes in the brain and neurodegeneration progress: review of the structural, biochemical, metabolic, cellular, and molecular changes. Front Aging Neurosci. 2022;14:931536. doi: 10.3389/fnagi.2022.931536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Tomlinson BE, Irving D. The numbers of limb motor neurons in the human lumbosacral cord throughout life. J Neurol Sci. 1977;34(2):213–9. doi: 10.1016/0022-510X(77)90069-7. [DOI] [PubMed] [Google Scholar]
- 369.Jacob JM. Lumbar motor neuron size and number is affected by age in male F344 rats. Mech Ageing Dev. 1998;106(1–2):205–16. doi: 10.1016/S0047-6374(98)00117-1. [DOI] [PubMed] [Google Scholar]
- 370.Maxwell N, et al. α-Motor neurons are spared from aging while their synaptic inputs degenerate in monkeys and mice. Aging Cell. 2018;17(2):e12726. doi: 10.1111/acel.12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Moldovan M, et al. Aging-associated changes in motor axon voltage-gated Na(+) channel function in mice. Neurobiol Aging. 2016;39:128–39. doi: 10.1016/j.neurobiolaging.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 372.Azpurua J, Mahoney RE, Eaton BA. Transcriptomics of aged Drosophila motor neurons reveals a matrix metalloproteinase that impairs motor function. Aging Cell. 2018;17(2):12729. doi: 10.1111/acel.12729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Wainger BJ, et al. Intrinsic membrane hyperexcitability of amyotrophic lateral sclerosis patient-derived motor neurons. Cell Rep. 2014;7(1):1–11. doi: 10.1016/j.celrep.2014.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Menon P, Kiernan MC, Vucic S. Cortical hyperexcitability precedes lower motor neuron dysfunction in ALS. Clin Neurophysiol. 2015;126(4):803–9. doi: 10.1016/j.clinph.2014.04.023. [DOI] [PubMed] [Google Scholar]
- 375.Tankisi H, et al. Early diagnosis of amyotrophic lateral sclerosis by threshold tracking and conventional transcranial magnetic stimulation. Eur J Neurol. 2021;28(9):3030–3039. doi: 10.1111/ene.15010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Dong XX, Wang Y, Qin ZH. Molecular mechanisms of excitotoxicity and their relevance to pathogenesis of neurodegenerative diseases. Acta Pharmacol Sin. 2009;30(4):379–87. doi: 10.1038/aps.2009.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Bae JS, et al. Effects of age on excitability properties in human motor axons. Clin Neurophysiol. 2008;119(10):2282–6. doi: 10.1016/j.clinph.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 378.Hunter SK, Pereira HM, Keenan KG. The aging neuromuscular system and motor performance. J Appl Physiol (1985) 2016;121(4):982–995. doi: 10.1152/japplphysiol.00475.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Wang H, et al. DNA damage and repair deficiency in ALS/FTD-associated neurodegeneration: from molecular mechanisms to therapeutic implication. Front Mol Neurosci. 2021;14:784361. doi: 10.3389/fnmol.2021.784361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Kanning KC, Kaplan A, Henderson CE. Motor neuron diversity in development and disease. Annu Rev Neurosci. 2010;33:409–40. doi: 10.1146/annurev.neuro.051508.135722. [DOI] [PubMed] [Google Scholar]
- 381.Singh A, et al. Oxidative stress: a key modulator in neurodegenerative diseases. Molecules. 2019;24(8):1583. doi: 10.3390/molecules24081583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Urushitani M, et al. Mechanism of selective motor neuronal death after exposure of spinal cord to glutamate: involvement of glutamate-induced nitric oxide in motor neuron toxicity and nonmotor neuron protection. Ann Neurol. 1998;44(5):796–807. doi: 10.1002/ana.410440514. [DOI] [PubMed] [Google Scholar]
- 383.Schrøder H, Reske-Nielsen E. Preservation of the nucleus X-pelvic floor motosystem in amyotrophic lateral sclerosis. Clin Neuropathol. 1984;3(5):210–216. [PubMed] [Google Scholar]
- 384.Lobsiger CS, et al. Schwann cells expressing dismutase active mutant SOD1 unexpectedly slow disease progression in ALS mice. Proc Natl Acad Sci U S A. 2009;106(11):4465–70. doi: 10.1073/pnas.0813339106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Pun S, et al. Selective vulnerability and pruning of phasic motoneuron axons in motoneuron disease alleviated by CNTF. Nat Neurosci. 2006;9(3):408–419. doi: 10.1038/nn1653. [DOI] [PubMed] [Google Scholar]
- 386.Spiller KJ, et al. Selective motor neuron resistance and recovery in a new inducible mouse model of TDP-43 proteinopathy. J Neurosci. 2016;36(29):7707–7717. doi: 10.1523/JNEUROSCI.1457-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Sharma A, et al. ALS-associated mutant FUS induces selective motor neuron degeneration through toxic gain of function. Nat Commun. 2016;7(1):10465. doi: 10.1038/ncomms10465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Hashizume K, Kanda K, Burke RE. Medial gastrocnemius motor nucleus in the rat: age-related changes in the number and size of motoneurons. J Comp Neurol. 1988;269(3):425–30. doi: 10.1002/cne.902690309. [DOI] [PubMed] [Google Scholar]
- 389.Swash M, Fox KP. The effect of age on human skeletal muscle. Studies of the morphology and innervation of muscle spindles. J Neurol Sci. 1972;16(4):417–32. doi: 10.1016/0022-510X(72)90048-2. [DOI] [PubMed] [Google Scholar]
- 390.Hedlund E, et al. Global gene expression profiling of somatic motor neuron populations with different vulnerability identify molecules and pathways of degeneration and protection. Brain. 2010;133(Pt 8):2313–30. doi: 10.1093/brain/awq167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Comley L, et al. Motor neurons with differential vulnerability to degeneration show distinct protein signatures in health and ALS. Neuroscience. 2015;291:216–29. doi: 10.1016/j.neuroscience.2015.02.013. [DOI] [PubMed] [Google Scholar]
- 392.Kadhiresan VA, Hassett CA, Faulkner JA. Properties of single motor units in medial gastrocnemius muscles of adult and old rats. J Physiol. 1996;493:543–52. doi: 10.1113/jphysiol.1996.sp021402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Kanda K, Hashizume K. Changes in properties of the medial gastrocnemius motor units in aging rats. J Neurophysiol. 1989;61(4):737–46. doi: 10.1152/jn.1989.61.4.737. [DOI] [PubMed] [Google Scholar]
- 394.Foran E, Trotti D. Glutamate transporters and the excitotoxic path to motor neuron degeneration in amyotrophic lateral sclerosis. Antioxid Redox Signal. 2009;11(7):1587–602. doi: 10.1089/ars.2009.2444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Arnold WD, Clark BC. Faster, higher, farther: outpacing age-related motor neuron losses. J Physiol. 2019;597(19):4867–4868. doi: 10.1113/JP278735. [DOI] [PubMed] [Google Scholar]
- 396.Palmer AL, Ousman SS. Astrocytes and aging. Front Aging Neurosci. 2018;10:337. doi: 10.3389/fnagi.2018.00337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Popov A, et al. Astrocyte dystrophy in ageing brain parallels impaired synaptic plasticity. Aging Cell. 2021;20(3):e13334. doi: 10.1111/acel.13334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Verkerke M, Hol EM, Middeldorp J. Physiological and pathological ageing of astrocytes in the human brain. Neurochem Res. 2021;46(10):2662–2675. doi: 10.1007/s11064-021-03256-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Li X, et al. Inflammation and aging: signaling pathways and intervention therapies. Signal Transduct Target Ther. 2023;8(1):239. doi: 10.1038/s41392-023-01502-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Ziff OJ, et al. Meta-analysis of human and mouse ALS astrocytes reveals multi-omic signatures of inflammatory reactive states. Genome Res. 2022;32(1):71–84. doi: 10.1101/gr.275939.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Tripathi P, et al. Reactive astrocytes promote als-like degeneration and intracellular protein aggregation in human motor neurons by disrupting autophagy through TGF-β1. Stem Cell Rep. 2017;9(2):667–680. doi: 10.1016/j.stemcr.2017.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Stoklund Dittlau K, et al. FUS-ALS hiPSC-derived astrocytes impair human motor units through both gain-of-toxicity and loss-of-support mechanisms. Mol Neurodegener. 2023;18(1):5. doi: 10.1186/s13024-022-00591-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Perry VH, Matyszak MK, Fearn S. Altered antigen expression of microglia in the aged rodent CNS. Glia. 1993;7(1):60–7. doi: 10.1002/glia.440070111. [DOI] [PubMed] [Google Scholar]
- 404.Vaughan DW, Peters A. Neuroglial cells in the cerebral cortex of rats from young adulthood to old age: an electron microscope study. J Neurocytol. 1974;3(4):405–29. doi: 10.1007/BF01098730. [DOI] [PubMed] [Google Scholar]
- 405.Tam OH, et al. Postmortem cortex samples identify distinct molecular subtypes of ALS: retrotransposon activation, oxidative stress, and activated glia. Cell Rep. 2019;29(5):1164–1177.e5. doi: 10.1016/j.celrep.2019.09.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Funikov SY, et al. FUS(1–359) transgenic mice as a model of ALS: pathophysiological and molecular aspects of the proteinopathy. Neurogenetics. 2018;19(3):189–204. doi: 10.1007/s10048-018-0553-9. [DOI] [PubMed] [Google Scholar]
- 407.Maniatis S, et al. Spatiotemporal dynamics of molecular pathology in amyotrophic lateral sclerosis. Science. 2019;364(6435):89–93. doi: 10.1126/science.aav9776. [DOI] [PubMed] [Google Scholar]
- 408.Zhou Q, et al. Active poly-GA vaccination prevents microglia activation and motor deficits in a C9orf72 mouse model. EMBO Mol Med. 2020;12(2):e10919. doi: 10.15252/emmm.201910919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Spiller KJ, et al. Microglia-mediated recovery from ALS-relevant motor neuron degeneration in a mouse model of TDP-43 proteinopathy. Nat Neurosci. 2018;21(3):329–340. doi: 10.1038/s41593-018-0083-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Quek H, et al. ALS monocyte-derived microglia-like cells reveal cytoplasmic TDP-43 accumulation, DNA damage, and cell-specific impairment of phagocytosis associated with disease progression. J Neuroinflammation. 2022;19(1):58. doi: 10.1186/s12974-022-02421-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Rawji KS, Neumann B, Franklin RJM. Glial aging and its impact on central nervous system myelin regeneration. Ann N Y Acad Sci. 2023;1519(1):34–45. doi: 10.1111/nyas.14933. [DOI] [PubMed] [Google Scholar]
- 412.Ximerakis M, et al. Single-cell transcriptomic profiling of the aging mouse brain. Nat Neurosci. 2019;22(10):1696–1708. doi: 10.1038/s41593-019-0491-3. [DOI] [PubMed] [Google Scholar]
- 413.Kang SH, et al. Degeneration and impaired regeneration of gray matter oligodendrocytes in amyotrophic lateral sclerosis. Nat Neurosci. 2013;16(5):571–579. doi: 10.1038/nn.3357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Allaman I, Bélanger M, Magistretti PJ. Astrocyte-neuron metabolic relationships: for better and for worse. Trends Neurosci. 2011;34(2):76–87. doi: 10.1016/j.tins.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 415.Ferraiuolo L, et al. Oligodendrocytes contribute to motor neuron death in ALS via SOD1-dependent mechanism. Proc Natl Acad Sci. 2016;113(42):E6496–E6505. doi: 10.1073/pnas.1607496113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Niebroj-Dobosz I, et al. Myelin composition of spinal cord in a model of amyotrophic lateral sclerosis (ALS) in SOD1G93A transgenic rats. Folia Neuropathol. 2007;45(4):236–41. [PubMed] [Google Scholar]
- 417.Painter MW, et al. Diminished Schwann cell repair responses underlie age-associated impaired axonal regeneration. Neuron. 2014;83(2):331–343. doi: 10.1016/j.neuron.2014.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Painter MW. Aging Schwann cells: mechanisms, implications, future directions. Curr Opin Neurobiol. 2017;47:203–208. doi: 10.1016/j.conb.2017.10.022. [DOI] [PubMed] [Google Scholar]
- 419.Fuertes-Alvarez S, Izeta A. Terminal schwann cell aging: implications for age-associated neuromuscular dysfunction. Aging Dis. 2021;12(2):494–514. doi: 10.14336/AD.2020.0708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Bruneteau G, et al. Endplate denervation correlates with Nogo-A muscle expression in amyotrophic lateral sclerosis patients. Ann Clin Transl Neurol. 2015;2(4):362–72. doi: 10.1002/acn3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Trias E, et al. Schwann cells orchestrate peripheral nerve inflammation through the expression of CSF1, IL-34, and SCF in amyotrophic lateral sclerosis. Glia. 2020;68(6):1165–1181. doi: 10.1002/glia.23768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Carrasco DI, Seburn KL, Pinter MJ. Altered terminal Schwann cell morphology precedes denervation in SOD1 mice. Exp Neurol. 2016;275(1):172–81. doi: 10.1016/j.expneurol.2015.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Marzetti E, et al. Sarcopenia: an overview. Aging Clin Exp Res. 2017;29(1):11–17. doi: 10.1007/s40520-016-0704-5. [DOI] [PubMed] [Google Scholar]
- 424.Clegg A, et al. Frailty in elderly people. Lancet. 2013;381(9868):752–62. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Rudolf R, et al. Degeneration of neuromuscular junction in age and dystrophy. Front Aging Neurosci. 2014;6:99. doi: 10.3389/fnagi.2014.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Gonzalez-Freire M, et al. The neuromuscular junction: aging at the crossroad between nerves and muscle. Front Aging Neurosci. 2014;6:208. doi: 10.3389/fnagi.2014.00208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Manini TM, Hong SL, Clark BC. Aging and muscle: a neuron's perspective. Curr Opin Clin Nutr Metab Care. 2013;16(1):21–6. doi: 10.1097/MCO.0b013e32835b5880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Seo DY, et al. Age-related changes in skeletal muscle mitochondria: the role of exercise. Integr Med Res. 2016;5(3):182–186. doi: 10.1016/j.imr.2016.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Power GA, Dalton BH, Rice CL. Human neuromuscular structure and function in old age: a brief review. J Sport Health Sci. 2013;2(4):215–226. doi: 10.1016/j.jshs.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Valentine JM, et al. NFκB regulates muscle development and mitochondrial function. J Gerontol A Biol Sci Med Sci. 2020;75(4):647–653. doi: 10.1093/gerona/gly262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Van Damme P, Robberecht W, Van Den Bosch L. Modelling amyotrophic lateral sclerosis: progress and possibilities. Dis Model Mech. 2017;10(5):537–549. doi: 10.1242/dmm.029058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Fulle S, et al. Age-dependent imbalance of the antioxidative system in human satellite cells. Exp Gerontol. 2005;40(3):189–97. doi: 10.1016/j.exger.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 433.Scaramozza A, et al. Skeletal muscle satellite cells in amyotrophic lateral sclerosis. Ultrastruct Pathol. 2014;38(5):295–302. doi: 10.3109/01913123.2014.937842. [DOI] [PubMed] [Google Scholar]
- 434.Cappello V, Francolini M. Neuromuscular junction dismantling in amyotrophic lateral sclerosis. Int J Mol Sci. 2017;18(10):2092. doi: 10.3390/ijms18102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Wong M, Martin LJ. Skeletal muscle-restricted expression of human SOD1 causes motor neuron degeneration in transgenic mice. Hum Mol Genet. 2010;19(11):2284–302. doi: 10.1093/hmg/ddq106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Picchiarelli G, et al. FUS-mediated regulation of acetylcholine receptor transcription at neuromuscular junctions is compromised in amyotrophic lateral sclerosis. Nat Neurosci. 2019;22(11):1793–1805. doi: 10.1038/s41593-019-0498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Sakowski SA, et al. Neuromuscular effects of G93A-SOD1 expression in zebrafish. Mol Neurodegener. 2012;7:44. doi: 10.1186/1750-1326-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Ramesh T, et al. A genetic model of amyotrophic lateral sclerosis in zebrafish displays phenotypic hallmarks of motoneuron disease. Dis Model Mech. 2010;3(9–10):652–62. doi: 10.1242/dmm.005538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Walker AK, et al. Functional recovery in new mouse models of ALS/FTLD after clearance of pathological cytoplasmic TDP-43. Acta Neuropathol. 2015;130(5):643–60. doi: 10.1007/s00401-015-1460-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 440.Iyer SR, Shah SB, Lovering RM. The neuromuscular junction: roles in aging and neuromuscular disease. Int J Mol Sci. 2021;22(15):8058. doi: 10.3390/ijms22158058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Verma S, et al. Neuromuscular junction dysfunction in amyotrophic lateral sclerosis. Mol Neurobiol. 2022;59(3):1502–1527. doi: 10.1007/s12035-021-02658-6. [DOI] [PubMed] [Google Scholar]
- 442.Partridge L, Fuentealba M, Kennedy BK. The quest to slow ageing through drug discovery. Nat Rev Drug Discov. 2020;19(8):513–532. doi: 10.1038/s41573-020-0067-7. [DOI] [PubMed] [Google Scholar]
- 443.Walters HE, Deneka-Hannemann S, Cox LS. Reversal of phenotypes of cellular senescence by pan-mTOR inhibition. Aging (Albany NY) 2016;8(2):231. doi: 10.18632/aging.100872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 444.Garay RP. Investigational drugs and+ nutrients for human longevity Recent clinical trials registered in ClinicalTrials.gov and clinicaltrialsregister.eu. Expert Opin Investig Drugs. 2021;30(7):749–758. doi: 10.1080/13543784.2021.1939306. [DOI] [PubMed] [Google Scholar]
- 445.Mandrioli J, et al. Randomized, double-blind, placebo-controlled trial of rapamycin in amyotrophic lateral sclerosis. Nat Commun. 2023;14(1):4970. doi: 10.1038/s41467-023-40734-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.Trammell SA, et al. Nicotinamide riboside is uniquely and orally bioavailable in mice and humans. Nat Commun. 2016;7:12948. doi: 10.1038/ncomms12948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.Zhang H, et al. NAD+ repletion improves mitochondrial and stem cell function and enhances life span in mice. Science. 2016;352(6292):1436–43. doi: 10.1126/science.aaf2693. [DOI] [PubMed] [Google Scholar]
- 448.Harlan BA, et al. Evaluation of the NAD(+) biosynthetic pathway in ALS patients and effect of modulating NAD(+) levels in hSOD1-linked ALS mouse models. Exp Neurol. 2020;327:113219. doi: 10.1016/j.expneurol.2020.113219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Zhou Q, et al. Nicotinamide riboside enhances mitochondrial proteostasis and adult neurogenesis through activation of mitochondrial unfolded protein response signaling in the brain of ALS SOD1(G93A) Mice. Int J Biol Sci. 2020;16(2):284–297. doi: 10.7150/ijbs.38487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Rajman L, Chwalek K, Sinclair DA. Therapeutic potential of NAD-boosting molecules: the in vivo evidence. Cell Metab. 2018;27(3):529–547. doi: 10.1016/j.cmet.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451.Biala A, et al. Resveratrol induces mitochondrial biogenesis and ameliorates Ang II-induced cardiac remodeling in transgenic rats harboring human renin and angiotensinogen genes. Blood Press. 2010;19(3):196–205. doi: 10.3109/08037051.2010.481808. [DOI] [PubMed] [Google Scholar]
- 452.Vaiserman AM, Lushchak OV, Koliada AK. Anti-aging pharmacology: promises and pitfalls. Ageing Res Rev. 2016;31:9–35. doi: 10.1016/j.arr.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 453.Baur JA, et al. Resveratrol improves health and survival of mice on a high-calorie diet. Nature. 2006;444(7117):337–42. doi: 10.1038/nature05354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454.Lagouge M, et al. Resveratrol improves mitochondrial function and protects against metabolic disease by activating SIRT1 and PGC-1alpha. Cell. 2006;127(6):1109–22. doi: 10.1016/j.cell.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 455.Song L, et al. Resveratrol ameliorates motor neuron degeneration and improves survival in SOD1(G93A) mouse model of amyotrophic lateral sclerosis. Biomed Res Int. 2014;2014:483501. doi: 10.1155/2014/483501. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 456.Markert CD, et al. A single-dose resveratrol treatment in a mouse model of amyotrophic lateral sclerosis. J Med Food. 2010;13(5):1081–5. doi: 10.1089/jmf.2009.0243. [DOI] [PubMed] [Google Scholar]
- 457.Moiseeva O, et al. Metformin inhibits the senescence-associated secretory phenotype by interfering with IKK/NF-κB activation. Aging Cell. 2013;12(3):489–98. doi: 10.1111/acel.12075. [DOI] [PubMed] [Google Scholar]
- 458.Patrone C, Eriksson O, Lindholm D. Diabetes drugs and neurological disorders: new views and therapeutic possibilities. Lancet Diabetes Endocrinol. 2014;2(3):256–62. doi: 10.1016/S2213-8587(13)70125-6. [DOI] [PubMed] [Google Scholar]
- 459.Ng TP, et al. Long-term metformin usage and cognitive function among older adults with diabetes. J Alzheimers Dis. 2014;41(1):61–8. doi: 10.3233/JAD-131901. [DOI] [PubMed] [Google Scholar]
- 460.Egesipe A-L, et al. Metformin decreases progerin expression and alleviates pathological defects of Hutchinson-Gilford progeria syndrome cells. NPJ Aging Mech Dis. 2016;2(1):16026. doi: 10.1038/npjamd.2016.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461.Abutaleb NO, et al. Lonafarnib and everolimus reduce pathology in iPSC-derived tissue engineered blood vessel model of Hutchinson-Gilford Progeria Syndrome. Sci Rep. 2023;13(1):5032. doi: 10.1038/s41598-023-32035-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 462.Krimpenfort P, Berns A. Rejuvenation by therapeutic elimination of senescent cells. Cell. 2017;169(1):3–5. doi: 10.1016/j.cell.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 463.Harley CB, et al. A natural product telomerase activator as part of a health maintenance program: metabolic and cardiovascular response. Rejuvenation Res. 2013;16(5):386–395. doi: 10.1089/rej.2013.1430. [DOI] [PubMed] [Google Scholar]
- 464.de Jesus BB, et al. The telomerase activator TA-65 elongates short telomeres and increases health span of adult/old mice without increasing cancer incidence. Aging Cell. 2011;10(4):604–621. doi: 10.1111/j.1474-9726.2011.00700.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465.Reichert S, et al. Experimental increase in telomere length leads to faster feather regeneration. Exp Gerontol. 2014;52:36–38. doi: 10.1016/j.exger.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 466.Tyshkovskiy A, et al. Distinct longevity mechanisms across and within species and their association with aging. Cell. 2023;186(13):2929–2949.e20. doi: 10.1016/j.cell.2023.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467.Graf M, et al. High dose vitamin E therapy in amyotrophic lateral sclerosis as add-on therapy to riluzole: results of a placebo-controlled double-blind study. J Neural Transm (Vienna) 2005;112(5):649–60. doi: 10.1007/s00702-004-0220-1. [DOI] [PubMed] [Google Scholar]
- 468.Galbussera A, et al. Vitamin E intake and quality of life in amyotrophic lateral sclerosis patients: a follow-up case series study. Neurol Sci. 2006;27(3):190–3. doi: 10.1007/s10072-006-0668-x. [DOI] [PubMed] [Google Scholar]
- 469.Fitzgerald KC, et al. Intakes of vitamin C and carotenoids and risk of amyotrophic lateral sclerosis: pooled results from 5 cohort studies. Ann Neurol. 2013;73(2):236–45. doi: 10.1002/ana.23820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.de la Rubia JE, et al. Efficacy and tolerability of EH301 for amyotrophic lateral sclerosis: a randomized, double-blind, placebo-controlled human pilot study. Amyotroph Lateral Scler Frontotemporal Degener. 2019;20(1–2):115–122. doi: 10.1080/21678421.2018.1536152. [DOI] [PubMed] [Google Scholar]
- 471.Yoshino J, Baur JA, Imai SI. NAD(+) intermediates: the biology and therapeutic potential of NMN and NR. Cell Metab. 2018;27(3):513–528. doi: 10.1016/j.cmet.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Ganai SA, Ramadoss M, Mahadevan V. Histone Deacetylase (HDAC) Inhibitors—emerging roles in neuronal memory, learning, synaptic plasticity and neural regeneration. Curr Neuropharmacol. 2016;14(1):55–71. doi: 10.2174/1570159X13666151021111609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 473.McIntyre RL, et al. From molecular promise to preclinical results: HDAC inhibitors in the race for healthy aging drugs. EMBO Mol Med. 2019;11(9):e9854. doi: 10.15252/emmm.201809854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Gomez-Sanchez JA, et al. Emerging role of HDACs in regeneration and ageing in the peripheral nervous system: repair schwann cells as pivotal targets. Int J Mol Sci. 2022;23(6):2996. doi: 10.3390/ijms23062996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Kalmar B, Lu C-H, Greensmith L. The role of heat shock proteins in amyotrophic lateral sclerosis: the therapeutic potential of Arimoclomol. Pharmacol Ther. 2014;141(1):40–54. doi: 10.1016/j.pharmthera.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 476.Bilches Medinas D, et al. Mutation in protein disulfide isomerase A3 causes neurodevelopmental defects by disturbing endoplasmic reticulum proteostasis. Embo j. 2022;41(2):e105531. doi: 10.15252/embj.2020105531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.Mora JS, et al. Masitinib as an add-on therapy to riluzole in patients with amyotrophic lateral sclerosis: a randomized clinical trial. Amyotroph Lateral Scler Frontotemporal Degener. 2020;21(1–2):5–14. doi: 10.1080/21678421.2019.1632346. [DOI] [PubMed] [Google Scholar]
- 478.Azam S, et al. The ageing brain: molecular and cellular basis of neurodegeneration. Front Cell Dev Biol. 2021;9:683459. doi: 10.3389/fcell.2021.683459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 479.Al-Chalabi A, et al. Analysis of amyotrophic lateral sclerosis as a multistep process: a population-based modelling study. Lancet Neurol. 2014;13(11):1108–1113. doi: 10.1016/S1474-4422(14)70219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.Gumeni S, et al. Proteome stability as a key factor of genome integrity. Int J Mol Sci. 2017;18(10):2036. doi: 10.3390/ijms18102036. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.