Abstract
Inverted follicular keratosis is a benign skin lesion that typically presents as an asymptomatic, solitary nodule that may mimic malignant lesions, especially squamous cell carcinoma, both clinically and pathologically. It is developed from the hair follicle infundibulum and can be considered a variant of seborrheic dermatitis. We present a case of a 26-year-old gentleman with a soft tissue mass at the external auditory canal which was later confirmed as inverted follicular keratosis and was treated by endoscopic transcanal excision of the mass with temporalis fascia graft reconstruction. He is currently under surveillance follow-up with no symptoms and signs of recurrence.
Keywords: Inverted follicular keratosis, External auditory canal, Benign tumour, Squamous cell carcinoma
Introduction
Inverted Follicular Keratosis (IFK) is a benign lesion which is more common in males and usually occurs in middle age and elderly individuals. It appears as an asymptomatic, firm, pinkish-brown solitary nodule and 85% of the cases were located in the facial region. However other sites like the chin, upper lip, head and neck region may be involved [1].
Histologically it may be classified as a benign tumour of the follicular infundibulum even though the cause of the lesion has not yet been explained [2]. It is characterized by an endophytic lesion that extends to the dermis, composed of basaloid cells in the periphery and squamous keratinized cells towards the centre with scaly twirls.
The most common treatment is complete surgical excision of the mass which shows a good prognosis without local recurrence observed. Another treatment option is topical 5% imiquimob cream however no previous case was reported using this topical cream for external auditory canal lesions.
Case Report
A case of a 26-year-old male presented with reduced hearing over the left ear for 1 month associated with otalgia. No other significant ear, nose and throat symptoms. Examination revealed granulation tissue covering the entire external auditory canal (EAC) obscuring the tympanic membrane with contact bleeding. Biopsy taken from the external auditory granulation tissue reported atypical squamous epithelial proliferation without the typical invasive growth pattern that is usually seen in invasive carcinoma. Audiology assessment showed moderate to severe left mixed hearing loss and normal hearing on the right ear. High Resolution Computed Tomography (HRCT) temporal reported as enhancing soft tissue density in the EAC with luminal narrowing causing obliteration of the left tympanic membrane, however no bony erosion (Fig. 1). Others ear structures were normal. He underwent transcanal excision of the left EAC mass and intraoperatively, the polypoidal mass occupied the entire lumen of EAC and arose from the anterosuperior aspect of the canal wall at the bony cartilaginous junction (Fig. 2). The mass was removed completely and the bare bone post-removal was covered with a temporalis fascia graft. The entire canal was then packed with roller gauze impregnated with Bisthmus Iodide Paraffin Paste (BIPP) and was removed two weeks post-surgery. He was reviewed again one week post removal of BIPP and noted the external canal slightly narrowed however no pus discharge and the graft site was taken well. Due to the narrowing of the canal, a silastic sheath was inserted to ensure the patency of the canal and was removed one month post-surgery. Follow-up showed a well-healed surgical site with the normal patency of the canal. Audiometry postoperatively was normal.
Fig. 1.
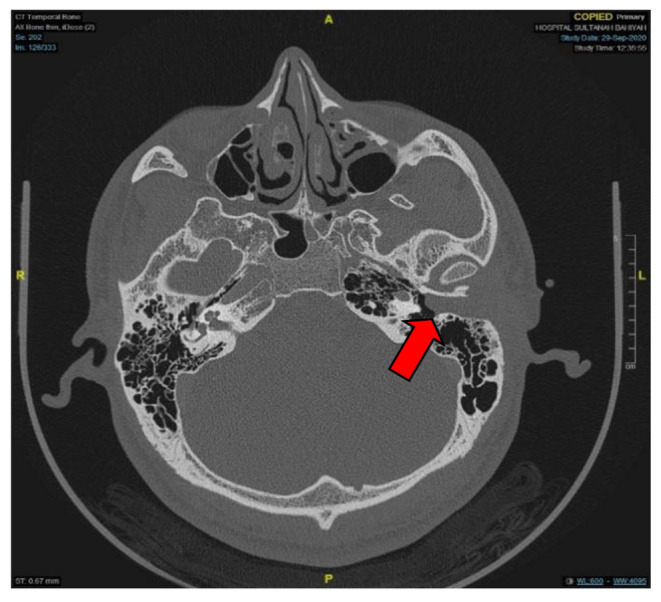
Axial HRCT temporal (bone window) showing soft tissue mass at EAC causing luminal narrowing without bony erosion (shown in red arrow)
Fig. 2.
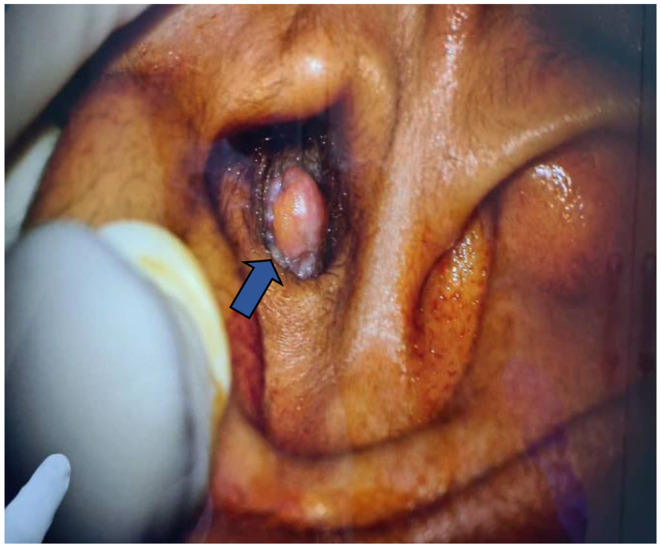
Intraoperative findings of polypoidal mass occupying entire EAC (shown in blue arrow)
Histopathology showed the endophytic lesion extending to the dermis (Fig. 3) with squamous cell proliferation in a downward growth pattern and thick trabeculae with mild nuclear pleomorphism, vesicular nuclei and prominent nucleoli (Fig. 4). Scattered mitosis with the squamous eddies was observed. The histological final interpretation was reported as inverted follicular keratosis.
Fig. 3.

Endophytic lesion that extends to dermis
Fig. 4.

Basaloid cells in the periphery and squamous keratinized cells towards centre
Discussion
Inverted Follicular Keratosis (IFK) in the EAC incidence is rare and often the aetiology remains unknown. Although it was reported that it might be related to viral warts or seborrheic keratosis, few authors reported that it is of a different entity [3–5]. Another study reported that IFK is a neoplasm of follicular origin thus it could be differentiated from seborrheic keratosis [2]. The association between Human Papilloma Virus (HPV) and IFK is still debatable. There is a study that relates the association between IFK with HPV infection, detected mainly by immunohistochemistry staining (IHC) using antibodies against HPV antigen. However recent studies using Polymerase Chain Reaction (PCR) test showed no significant relationship between both entities [3, 4, 6]. We have not proceeded with the HPV test in our patient as there was no indication to do so.
Diagnosis of IFK is generally established via histopathology as its clinical features might resemble more commonly seen diseases such as viral warts, seborrheic keratosis, actinic keratosis, basal cell carcinoma (BCC), and squamous cell carcinoma (SCC). Histologically IFK is characterized by the endophytic lesion that extends to the dermis composed of the basaloid cells in the periphery and squamous keratinized cells towards the centre with scaly twirls [1].
Clinically IFK of the EAC manifests as an expansive type of polypoidal mass occupying the entire canal with no bony erosion. HRCT Temporal will aid in the evaluation of the lesion and extension of the disease while audiometry pre-operatively will give us the baseline hearing before the operation. It is expected to have a conductive component of hearing loss as the lesion only affects the EAC.
The treatment of choice is complete surgical excision of the mass via transcanal approach. There was no recurrence reported in the previously reported literature [9]. Another literature proposed treatment of the IFK using Imiquimod which is an immunomodulatory drug that belongs to the imidazoquinolone group [1]. Its action is by induction of the cytokine production from the antigen-presenting cells and inhibits vascular tumour development by causing a decrease in tumour cell proliferation, increase in apoptosis, and decrease in matrix metalloproteinase 1 and 9 activity [7, 8]. In this case, 5% of the imiquimod cream was administered and near complete regression was seen after 2 months of treatment [1]. However, no other literature reported a similar IFK case that was successfully treated with Imiquimob. Thus, surgical excision remains as the mainstay of treatment in this disease.
Conclusion
IFK of the external auditory canal is a very rare benign epithelial tumour that arises from the infundibulum of the hair follicle. Histopathological examination is the gold standard for diagnosis of IFK. Complete surgical excision of the mass is the treatment of choice with no recurrence reported.
Declarations
Conflict of Interest
None to be declared.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Battistella M, Peltre B, Cribier B. Composite tumours associating trichoblastoma and benign epidermal/follicular neoplasm: another proof of the follicular nature of inverted follicular keratosis. J Cutan Pathol. 2010;37(10):1057–1063. doi: 10.1111/J.1600-0560.2009.01341.X. [DOI] [PubMed] [Google Scholar]
- 2.C C, B B. Safety, efficacy, and patient acceptability of imiquimod for topical treatment of actinic keratoses. Clin Cosmet Invest Dermatology. 2011;4:35. doi: 10.2147/CCID.S14109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kambiz KH, Kaveh D, Maede D, Hossein A, Nessa A, Ziba R, Alireza G. Human papillomavirus deoxyribonucleic acid may not be detected in non-genital Benign Papillomatous skin lesions by polymerase chain reaction. Indian J Dermatology. 2014;59(4):334–338. doi: 10.4103/0019-5154.135475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karadag AS, Ozlu E, Uzuncakmak TK, Akdeniz N, Cobanoglu B, Oman B. Inverted follicular keratosis successfully treated with imiquimod. Indian Dermatology Online Journal. 2016;7(3):177. doi: 10.4103/2229-5178.182354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehregan AH. Inverted follicular keratosis is a distinct follicular tumor. Am J Dermatopathol. 1983;5(5):467–470. doi: 10.1097/00000372-198310000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Ruhoy SM, Thomas D, Nuovo GJ. Multiple inverted follicular keratoses as a presenting sign of Cowden’s syndrome: case report with human papillomavirus studies. J Am Acad Dermatol. 2004;51(3):411–415. doi: 10.1016/J.JAAD.2003.12.049. [DOI] [PubMed] [Google Scholar]
- 7.Sidbury R, Neuschler N, Neuschler E, Sun P, Wang XQ, Miller R, Tomai M, Puscasiu E, Gugneja S, Paller AS. Topically applied imiquimod inhibits vascular tumor growth in vivo. J Invest Dermatol. 2003;121(5):1205–1209. doi: 10.1046/J.1523-1747.2003.12521.X. [DOI] [PubMed] [Google Scholar]
- 8.Spielvogel RL, Austin C, AcKerman AB. Inverted follicular keratosis is not a specific keratosis but a verruca vulgaris (or seborrheic keratosis) with squamous eddies. Am J Dermatopathol. 1983;5(5):427–442. doi: 10.1097/00000372-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Thom GA, Quirk CJ, Heenan PJ (2004) Inverted follicular keratosis simulating malignant melanoma. Australas J Dermatol 45. 10.1111/j.1440-0960.2004.00032. :55 – 7 [DOI] [PubMed]


