Abstract
Non-ossifying fibroma (NOF) of jaw bones are rare. While NOF is the most common benign bone tumor of long bones with pathognomonic radiological features and bear a tendency for self-regression, gnathic NOF appears to be comparatively larger in size and behave more aggressively. A 16 years old female patient reported with painless swelling of the right side of the face of 4 months duration. Radiographic analysis showed a unilocular radiolucent lesion of right angle of the mandible with ill-defined margins, cortical perforation and thinning of inferior border. The lesion was provisionally diagnosed as odontogenic keratocyst/unicystic ameloblastoma and incisional biopsy was performed. The histopathological features and immunohistochemical characteristics favored a diagnosis of NOF. The lesion was excised and reconstructed. The excised specimen confirmed the diagnosis. There are no signs of recurrence at 18 months follow-up. NOF should be considered in the differential diagnosis of uni-/multilocular radiolucencies of jaws particularly the posterior mandible.
Keywords: ER, FGFR1, Gnathic, Mandible, Non-ossifying fibroma, RAS
Introduction
Non-ossifying fibroma (NOF; ICD-O-8830/0) is considered to be a benign and generally self-limiting storiform spindle cell tumour of bone containing osteoclast-like giant cells (WHO-2020) [1]. NOF is explained in literature under various terminologies such as benign fibrous histiocytoma (BFH), fibrous cortical defect (FCD, for lesions confined to the cortex of bone) or metaphyseal fibrous defect; however, usage of these terms is not recommended in the latest WHO classification of soft tissue and bone tumors. Metaphysis of long bones of the lower limbs are affected in majority of the cases, most are usually asymptomatic and detected as incidental findings [2]. Multifocal lesions have been reported [3, 4].
Sontag and Pyle, first recognized non-ossifying fibroma (NOF) but the term ‘‘non-ossifying fibroma’’ was applied to describe a lesion of the mandible in the year 1979 [5, 6]. While NOF in other bones are common with characteristic radiological findings of lobulated well defined lesion of cortex, NOF of the gnathic bones are rare and lack these features. Thus, a variety of odontogenic and non-odontogenic lesions are usually considered in differential diagnoses. Here, we present a surgical case report of non-ossifying fibroma of right mandible in a 16 years old female with an updated review on the pathological findings and usage of terminologies.
Case report
A sixteen years old Dravidian (Tamil) female presented in February 2022 with painless swelling in right side of the lower jaw region of 4 months duration and for removal of partially erupted third molar. On extraoral examination, there was a slight asymmetry attributed to swelling at the right angle region (Fig. 1a). Intraorally, there was severe malocclusion and partially erupted 48 with obliteration of right posterior gingivobuccal sulcus in relation to 48 (Fig. 1b). The swelling was firm in consistency, mildly tender on palpation, non-fluctuant, non-pulsatile and non-compressible. The orthopantomogram revealed a unilocular radiolucency, measuring about 2 × 2 cm, on the right angle of mandible which extended to the mesial root of 46 anteriorly (Fig. 1c). The margins were ill-defined with thinning and breach of inferior border and perforation of cortical plates. The findings were confirmed by computed tomography (Fig. 1d). Based on clinical and imaging findings, a provisional diagnosis of unicystic ameloblastoma/odontogenic keratocyst was made, possibility of odontogenic malignancy was however, could not be ruled out completely.
Fig. 1.
a Extraoral presentation showing mild facial asymmetry owing to swelling on the right side of the face, b Intraorally, there was slight obliteration of right gingivobuccal sulcus with severe malocclusion, c OPG revealing a well-defined unilocular radiolucency of right angle of the mandible with ill-defined margins, d 3D- reconstructed images of CT confirming the finding of plain radiography e Intra-operative view, showing solid tumor and exposed right inferior alveolar nerve, and f 3D- reconstructed images of CT after reconstruction
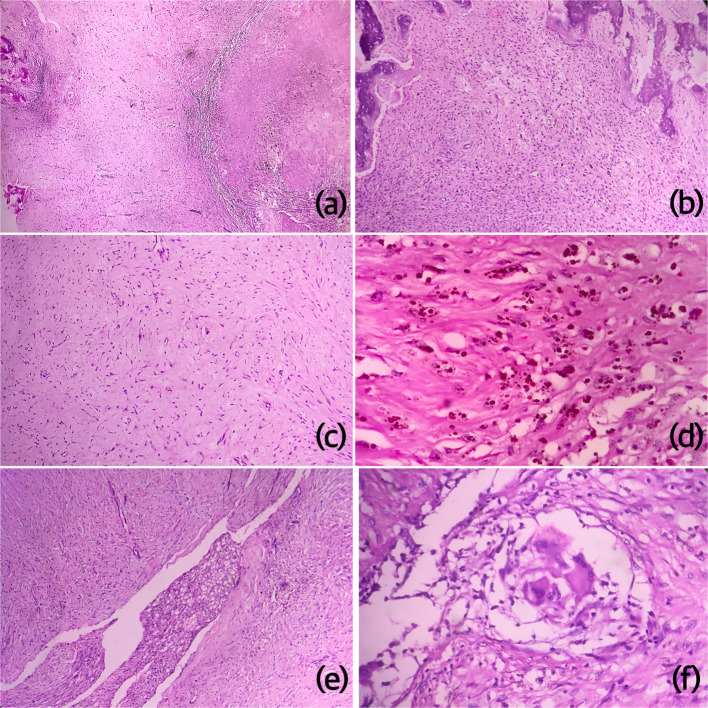
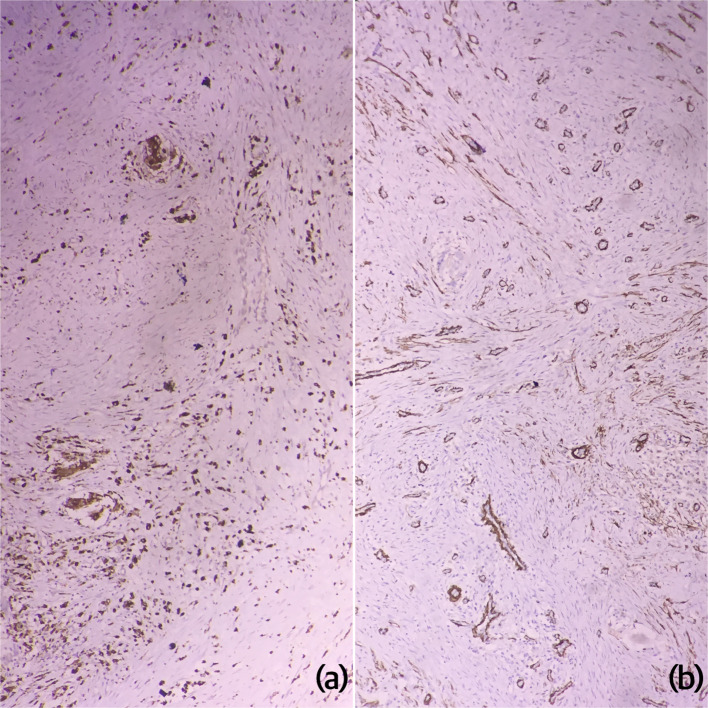
An incisional biopsy was taken with mandibular transoral modified Ward’s incision with extraction of 46, 47 and 48. The biopsied specimen was sent for histopathological examination in buffered 10% formalin. Multiple sections showed numerous bland spindle shaped fibroblasts arranged in storiform pattern in few areas, interspersed with few multinucleated giant cells, abundant hemosiderin pigment, hemosiderinophages and area of lipid laden macrophages. Some areas showed dense fibrosis with necrosis, mild lymphoplasmacytic cell infiltrate and hemorrhage. Peripheral resorbing bone and few areas of ossification were also evident (Fig. 2a–f). Van Gieson stain highlighted mature collagen. Diffuse cytoplasmic positivity for CD68 was noted in histiocytes/foam cells and giant cells, SMA and S100 were negative in lesional cells (SMA positivity was seen in background vasculature) and the proliferation index was < 1% (as demonstrated with Ki-67 immunostaining; low) (Fig. 3a–b). The histological features were suggestive of non-ossifying fibroma.
Fig. 2.
Photomicrographs of H&E stained sections showing proliferation of bland spindle to stellate shaped cells with rich vascularity and no ossification, peripheral bone is also evident (a-40X, b&c-100X), numerous hemosiderophages (d-400X), foci of foamy histiocytes (e-100X) and multinucleated giant cells, (f-400X)
Fig. 3.
Photomicrographs of IHC stained sections showing a CD68 positivity in histocytes and b SMA positivity in background vasculature and occasional spindle cells
To prevent pathological fracture and fast functional recovery rigid titanium- reconstruction plate was fixed across the surgically excised tumor (solid tumor intraoperatively) in toto where a part of inferior alveolar nerve was excised with tumor, both the remaining nerve ends were approximated, via extended submandibular incision (Fig. 1e). Autogenous cortico-cancellous bone graft harvested from the anterior iliac crest via incision superior to anterior superior iliac spine was used to fill the bony defect. No sign of recurrence, plate exposure, screw fracture, nerve paraesthesia or facial disfigurement were reported on 18 months follow-up (Fig. 1f).
The excised specimen confirmed the findings of incisional biopsy.
Discussion
In literature, NOF and FCD have been interchangeably used with marked histopathological resemblance of both with benign fibrous histiocytoma (BFH), and thus have been considered as non-ossifying fibroma in the latest classification. Conventionally, a cut off value of 3 cm is employed for distinction between FCD and NOF of long bones, former being smaller than 3 cm [3]. FCD/NOF of long bones are usually discovered incidentally and it has been estimated that about 30–40% of children have occult NOF with the highest incidence between 4 and 8 years of age, rendering them to be the commonest primary bone tumor [7].
The cause of sporadic cases is unknown however, germline or postzygotic mosaic mutations in NF1/KRAS have been postulated in the pathogenesis of NOF; not surprisingly patients with oculo-ectodermal syndrome (KRAS mutation) and Jaffe-Campanacci syndrome (NF1 mutation) develop multiple non-ossifying fibromas of bones and gnathic giant cell lesions [8, 9]. This further points a plausible link between NOF and giant cells lesions of jaws. Schematic representation of the signalling pathways involved in its pathogenesis is depicted in Fig. 4.
Fig. 4.
Schematic representation of the signalling pathways involved in the pathogenesis of NOF. FGFR-fibroblast growth factor, MEK-MAPK/ERK kinase, ERK-extracellular signal regulated kinase, M-CSF-macrophage colony stimulating factor, IL-1- interleukin-1, TNF-alpha- tumor necrosis factor-alpha, RANKL-receptor activator of nuclear factor kappa beta ligand, NF-neurofibromatosis-1
We search the literature regarding NOF/FCD [6, 10–31] and BFH [32–49] of gnathic bones, as these have been reported independently. The search terms included ‘non-ossifying fibroma’ or ‘benign fibrous histiocytoma’, or ‘fibrous cortical defect’, and ‘mandible/ maxilla/ jaws’ (Tables 1 and 2). Some interesting points were withdrawn. The mean age for non-ossifying fibroma of jaws was found to be 18.73 years (± 10.47; median: 16 years), with approximately 77% (20/26) of the cases were seen in the second and third decades of life. A similar peak incidence in the second decade has been reported in the non-ossifying fibromas of long bones. Contrary to NOF of other sites, jaw lesions were more commonly seen in female gender. The posterior mandible appears to be the commonest site for gnathic NOF. In contrast, BFH of jaws showed a comparative higher mean age of 37.3 years (± 15.82). The maximum number of cases were seen between 40 and 49 years (7/18), with equal predilection for both genders. NOF and BFH of the jaws are more commonly seen in mandible than maxilla.
Table 1.
Clinicodemographic profile of reported non-ossifying fibromas/fibrous cortical defect of gnathic bones; M-male, F-female, M/L-multilocular, U/L-unilocular, NM-not mentioned
| Sl. No. | Author and year | Number of cases | Age (years) | Gender | Location | Radiographic appearance | Treatment |
|---|---|---|---|---|---|---|---|
| 1. | Rudy and Scheingold [10] | 1 | 49 | F | Body/ramus | M/L | Curettage |
| 2. | Quinn JH et al. [11] | 1 | 21 | F | Angle of mandible | U/L | Curettage |
| 3. | Liaw et al. [6] | 1 | 17 | F | Mandible- posterior | U/L | Resection |
| 4. | Makek et al. [12] | 1 | 20 | M | Mandibular condyle | M/L | Resection |
| 5. | Ide et al. [13] | 1 | 37 | F | Body of mandible | M/L | Curettage |
| 6. | Mirra et al. [14] | 1 | 12 | F | Body of mandible | U/L | Curettage |
| 7. | Park et al. [15] | 1 | 21 | F | Body of mandible | U/L | Curettage |
| 8. | Elzay et al. [16] | 2 |
11 11 |
F F |
Ramus Ramus/Angle of mandible |
M/L M/L |
Curettage Curettage |
| 9. | Bessho et al. [17] | 1 | 28 | M | Body of mandible | U/L | Curettage |
| 10. | Aldred et al. [18] | 1 | 18 | F | Mandibular condyle | M/L | Resection |
| 11. | Roche et al. [19] | 1 | 26 | F | Mandible- posterior | U/L | Curettage |
| 12. | Mizukawa et al. [20] | 1 | 7 | M | Body of mandible | U/L | Curettage |
| 13. | Uçkan et al. [21] | 1 | 16 | F | Body of mandible | M/L | Curettage |
| 14. | Bailey et al. [22] | 1 | 6 | F | Angle of mandible | M/L | Curettage |
| 15. | Hudson et al. [23] | 1 | 13 | M | Mandibular condyle | U/L | Curettage |
| 16. | Chrcanovic et al. [24] | 1 | 15 | M | Angle of mandible | U/L | Curettage |
| 17. | Abdelsayed et al. [25] | 2 |
14 27 |
F M |
Ramus Ramus |
M/L M/L |
Curettage Curettage |
| 18. | Bowers et al. [26] | 1 | 22 | F | Ramus | M/L | Curettage |
| 19. | Jafari et al. [27] | 1 | 38 | F | Maxillary tuberosity | U/L | Curettage |
| 20. | Turki IM [28] | 1 | 12 | NM | Body of mandible | U/L | Conservative excision |
| 21. | Mannan et al. [29] | 1 | 15 | M | Body of mandible | U/L | Curettage with reconstruction |
| 22. | Hammad et al. [30] | 1 | 11 | M | Mandibular condyle | M/L | Excision and reconstruction |
| 23. | Khandaitkar et al. [31] | 1 | 4 | F | Angle of mandible | M/L | Curettage and peripheral ostectomy |
| 24. | Present case | 1 | 16 | F | Angle of mandible | U/L | Excision and reconstruction |
| Total | 26 |
Mean:18.73 ± 10.47 Median: 16 (Range: 4–49) |
17 F:8 M (1 NM) |
Commonest site: Body of mandible | Equal | ||
Table 2.
Clinicodemographic profile of reported benign fibrous histiocytoma of gnathic bones; M-male, F-female, M/L-multilocular, U/L-unilocular, RL-RO-radiolucent-radioopaque, NA-not available
| Sl. No. | Author and year | Number of cases | Age (years) | Gender | Location | Radiographic appearance | Treatment |
|---|---|---|---|---|---|---|---|
| 1. | White and Makar [32] | 1 | 29 | F | Mandible- posterior | U/L | Curettage |
| 2. | Remagen et al. [33] | 1 | 17 | M | Mandible- posterior | M/L | NA |
| 3. | Cale et al. [34] | 1 | 13 | M | Maxilla- posterior | U/L | Excision |
| 4. | Ertaş et al. [35] | 1 | 32 | M | Mandible- anterior | U/L | Curettage |
| 5. | Heo et al. [36] | 1 | 42 | M | Mandible- posterior | M/L | Segmental mandibulectomy |
| 6. | Kishino et al. [37] | 1 | 49 | F | Mandible- posterior, Mandibular condyle | M/L | Segmental mandibulectomy |
| 7. | Katagiri et al. [38] | 1 | 48 | M | Mandibular condyle | U/L | Curettage |
| 8. | Tanaka et al. [39] | 1 | 80 | F | Mandible- posterior | M/L | Excision (turned malignant in 6 months) |
| 9. | Wagner et al. [40] | 1 | 41 | M | Mandible- posterior | M/L | Excision |
| 10. | Gupta et al. [41] | 1 | 24 | F | Mandible- posterior | U/L | NA |
| 11. | Ou et al. [42] | 1 | 31 | M | Mandible- posterior | M/L | Segmental mandibulectomy |
| 12. | Saluja et al. [43] | 1 | 23 | F | Maxilla- posterior | M/L | Excision |
| 13. | Shoor et al. [44] | 1 | 30 | F | Mandible- posterior | M/L | Segmental mandibulectomy |
| 14. | Vylopilli et al. [45] | 1 | 46 | F | Mandible- posterior | M/L | Segmental mandibulectomy |
| 15. | Pattamparambath et al. [46] | 1 | 51 | F | Mandible- posterior | M/L, Mixed RL-RO | Segmental mandibulectomy |
| 16. | Mohanty et al. [47] | 1 | 24 | M | Maxilla- posterior | M/L, Mixed RL-RO | Excision |
| 17. | Chauhan et al. [48] | 1 | 45 | M | Maxilla | - | Maxillectomy |
| 18. | Wang et al. [49] | 1 | 46 | F | Mandible (anterior and posterior) | M/L |
Curettage (multiple recurrences) |
| Total | 18 |
Mean:37.3 ± 15.82 Median: 36.5 (Range:13–80) |
9 F: 9 M | Mandible > Maxilla | M/L > U/L | Excision | |
Unicystic ameloblastoma, odontogenic keratocyst, simple bone cyst, extrafollicular adenomatoid odontogenic tumor may be considered in the differential diagnoses of a unilocular radiolucency of posterior mandible in a young female with unassociated impacted tooth. Calcifying odontogenic cyst and glandular odontogenic cyst may also behave locally aggressive, however, these cysts show a predilection for the anterior parts of the jaw [50, 51]. Confirmatory diagnosis can be made only after histological examination, where storiform pattern of plump spindly cells are seen intermingling with osteoclast like giant cells, foamy macrophages, and hemosiderin pigment. The histological features of NOF of jaw bone are indistinguishable from the lesion of long bones, however, gnathic lesions do not appear to be self-limiting unlike metaphyseal lesions. Further, there is no clear distinction between NOF and BFH of jaws. Both show predilection for mandible than maxilla and similar histological features, thus these lesions may actually represent spectrum of the same disease process.
Data pertaining to mutations in KRAS and FGFR1 in NOF and BFH in gnathic lesions is puny, owing to the fact that most lesion are diagnosed on clinical and radiographic backgrounds and biopsied material is usually not available for testing. Recent literature supports the fact that NOF should be considered as true neoplasm in contrast to the prevailing concept in favor of a reactive process. Along with many other tumors, NOF has now been added in ‘RASopathy family’ [52]. Most reported cases of gnathic NOF have been treated by curettage [10, 11, 13–17, 19–27, 31], with few managed by excision followed by reconstruction depending on the size and behavior. BFH cases were reported to be excised or aggressively resected. No malignisation has been reported in gnathic NOF, a single case of BFH, howbeit, showed malignant transformation [39]. Another case of BFH which was treated by curettage showed multiple recurrences [49].
Conclusion
Non-ossifying fibroma of the mandible may present as a unilocular radiolucency with clinical and radiographic features indistinguishable from other odontogenic pathologies. There are characteristic radiographic and clinical appearance of the NOF/FDC of the long bones and don’t require any active intervention, the gnathic lesions however, behave aggressively. The diagnosis relies upon histological examination of biopsied material; in ambiguous cases, KRAS and FFGR1 mutation may be considered which also might shed light on the pathogenesis of the jaw lesion. The larger lesions may require wider excision.
Acknowledgements
None.
Funding
No funding was received for the research, authorship, and/or publication of this article.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The manuscript presents a case of non-ossifying fibroma with no additional psychological, physical and financial burden for the patient.
Informed Consent
Further, the informed and written consents were taken from the patients at the time of admission for treatment.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO Classification of Tumours Editorial Board . Soft tissue and bone tumours. WHO classification of tumours series. 5. Lyon: International Agency for Research on Cancer; 2020. pp. 447–448. [Google Scholar]
- 2.Alshehri K, Fadil AA. Non-ossifying fibroma pathological fracture in a patient with Lactose Intolerance. Cureus. 2021;13(8):e17225. doi: 10.7759/cureus.17225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blau RA, Zwick DL, Westphal RA. Multiple non-ossifying fibromas. A case report. J Bone Joint Surg Am. 1988;70:299–304. doi: 10.2106/00004623-198870020-00022. [DOI] [PubMed] [Google Scholar]
- 4.Jamshidi K, Motaghi P, Bagherifard A, Eigi M, Al-Baseesee HH, Mirzaei A. Comparison of characteristic features and local recurrence in syndromic versus non-syndromic multifocal non-ossifying fibroma. J Orthop Sci. 2021;26(4):655–659. doi: 10.1016/j.jos.2020.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Sontag LW, Pyle DI. The appearance and nature of cyst-like areas in distal femoral metaphyses of children. Am J Roentgenol Radiat Ther. 1941;46:185–188. [Google Scholar]
- 6.Liaw WJ, So TK, Yao YT. Non-ossifying fibroma of mandible. A case report. J Formos Med Assoc. 1979;78:795–802. [PubMed] [Google Scholar]
- 7.Mallet JF, Rigault P, Padovani JP, Touzet P, Nezelof C. Le fibrome non ossifiant chez l’enfant: une affection chirurgicale? [Non-ossifying fibroma in children: a surgical condition?] Chir Pediatr. 1980;21(3):179–189. [PubMed] [Google Scholar]
- 8.Vannelli S, Buganza R, Runfola F, Mussinatto I, Andreacchio A, de Sanctis L. Jaffe-Campanacci syndrome or neurofibromatosis type 1: a case report of phenotypic overlap with detection of NF1 gene mutation in non-ossifying fibroma. Ital J Pediatr. 2020;46(1):58. doi: 10.1186/s13052-020-0813-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peacock JD, Dykema KJ, Toriello HV, Mooney MR, Scholten DJ, II, Winn ME, et al. Oculoectodermal syndrome is a mosaic RASopathy associated with KRAS alterations. Am J Med Genet A. 2015;167(7):1429–1435. doi: 10.1002/ajmg.a.37048. [DOI] [PubMed] [Google Scholar]
- 10.Rudy HN, Scheingold SS. Solitary xanthogranuloma of the mandible; report of a case. Oral Surg Oral Med Oral Pathol. 1964;18:262–271. doi: 10.1016/0030-4220(64)90436-0. [DOI] [PubMed] [Google Scholar]
- 11.Quinn JH, Graves LR, Leonard GL. Unusual histiocytic lesion of the mandible: report of case. J Oral Surg. 1970;28(7):528–530. [PubMed] [Google Scholar]
- 12.Makek M. Non ossifying fibroma of the mandible. A common lesion with unusual location. Arch Orthop Trauma Surg. 1980;96(3):225–227. doi: 10.1007/BF00457787. [DOI] [PubMed] [Google Scholar]
- 13.Ide F, Kusuhara S, Onuma H, Miyake T, Umemura S. Xanthic variant of non-ossifying fibroma (so-called xanthofibroma) of the mandible. An ultrastructural study. Acta Pathol Jpn. 1982;32(1):135–142. doi: 10.1111/j.1440-1827.1982.tb02034.x. [DOI] [PubMed] [Google Scholar]
- 14.Mirra JM, Gold RH, Rand F. Disseminated nonossifying fibromas in association with café-au-lait spots (Jaffe-Campanacci syndrome) Clin Orthop Relat Res. 1982;168:192–205. doi: 10.1097/00003086-198208000-00036. [DOI] [PubMed] [Google Scholar]
- 15.Park JK, Levy BA, Hanley JB., Jr Non-ossifying fibroma of the mandible: report of a case. J Baltim Coll Dent Surg. 1982;35(2):1–5. [PubMed] [Google Scholar]
- 16.Elzay RP, Mills S, Kay S. Fibrous defect (nonossifying fibroma) of the mandible. Oral Surg Oral Med Oral Pathol. 1984;58(4):402–407. doi: 10.1016/0030-4220(84)90333-5. [DOI] [PubMed] [Google Scholar]
- 17.Bessho K, Murakami K, Nishida M, et al. Non-ossifying fibroma of the mandible: case report and review of literature. Jpn J Oral Maxillofac Surg. 1986;32:291–296. doi: 10.5794/jjoms.32.291. [DOI] [Google Scholar]
- 18.Aldred MJ, Breckon JJ, Holland CS. Non-osteogenic fibroma of the mandibular condyle. Br J Oral Maxillofac Surg. 1989;27(5):412–416. doi: 10.1016/0266-4356(89)90082-X. [DOI] [PubMed] [Google Scholar]
- 19.Roche WC, Krishnan V, McDaniel RK. Fibrous defect of the mandible: a case report and literature review. J Oral Maxillofac Surg. 1993;51(7):809–811. doi: 10.1016/S0278-2391(10)80430-6. [DOI] [PubMed] [Google Scholar]
- 20.Mizukawa N, Nishijima Y, Nishijima K. Metaphyseal fibrous defect (nonossifying fibroma) in the mandible. A case report. Int J Oral Maxillofac Surg. 1997;26(2):129–130. doi: 10.1016/S0901-5027(05)80834-3. [DOI] [PubMed] [Google Scholar]
- 21.Uçkan S, Gürol M, Mutlu N, Güngör S. Non-ossifying fibroma of the mandible: report of a case. Br J Oral Maxillofac Surg. 1999;37(2):152–154. [PubMed] [Google Scholar]
- 22.Bailey JS, Nikitakis NG, Lopes M, Ord RA. Nonossifying fibroma of the mandible in a 6-year-old girl: a case report and review of the literature. J Oral Maxillofac Surg. 2001;59(7):815–818. doi: 10.1053/joms.2001.24303. [DOI] [PubMed] [Google Scholar]
- 23.Hudson JW, Livesay KW, McCoy JM. Condylar lesion. J Oral Maxillofac Surg. 2003;61(7):824–826. doi: 10.1016/S0278-2391(03)00157-5. [DOI] [PubMed] [Google Scholar]
- 24.Chrcanovic BR, Albanese AL, Freire-Maia B, Nunes FC, Souza PE, Gomez RS. Non-ossifying fibroma (metaphyseal fibrous defect) of the mandible. Oral Maxillofac Surg. 2011;15(4):233–237. doi: 10.1007/s10006-010-0244-7. [DOI] [PubMed] [Google Scholar]
- 25.Abdelsayed RA, Sharma S, Ferguson H. Fibrous cortical defect (nonossifying fibroma) of the mandibular ramus: report of 2 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(4):504–508. doi: 10.1016/j.tripleo.2010.04.047. [DOI] [PubMed] [Google Scholar]
- 26.Bowers LM, Cohen DM, Bhattacharyya I, Pettigrew JC, Jr, Stavropoulos MF. The non-ossifying fibroma: a case report and review of the literature. Head Neck Pathol. 2013;7(2):203–210. doi: 10.1007/s12105-012-0399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jafari AA, Langaroodi AJ, Shokri A, Yazdani N, Dehghan A, Jafari MA, et al. Maxillary non-ossifying Fibroma: a Case Report and Review of the literature. J Dentomaxillofac Radiol Pathol Surg. 2013;2:32–37. doi: 10.18869/acadpub.3dj.2.1.6. [DOI] [Google Scholar]
- 28.Turki IM. Le fibrome non ossifiant mandibulaire: différences par rapport aux localisations orthopédiques et implications thérapeutiques. Méd Buccale Chirurgie Buccale. 2014;20:185–188. doi: 10.1051/mbcb/2014017. [DOI] [Google Scholar]
- 29.Mannan AA, Singh NG, Al-Waheeb S, Taher TN, Mohammed Eel D. Nonossifying fibroma (metaphyseal fibrous defect) of the mandible in a 15-year-old boy. Ear Nose Throat J. 2015;94(6):E41–E44. doi: 10.1177/014556131509400620. [DOI] [PubMed] [Google Scholar]
- 30.Hammad Y, Schlieve T. Metachronous odontogenic keratocyst and non-ossifying fibroma of the mandible. Oral Maxillofac Surg Cases. 2021;7:100221. doi: 10.1016/j.omsc.2021.100221. [DOI] [Google Scholar]
- 31.Khandaitkar S, Lamba G, Kolte V, Shenoi R, Shukla D. Non-ossifying Fibroma of Mandible in a four-year-old girl: a Case Report. Cureus. 2023;15(3):e36470. doi: 10.7759/cureus.36470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.White RD, Makar J., Jr Xanthofibroma of the mandible. J Oral Maxillofac Surg. 1986;44(12):1010–1014. doi: 10.1016/S0278-2391(86)80058-1. [DOI] [PubMed] [Google Scholar]
- 33.Remagen W, Nidecker A, Prein J. Case report 359: gigantic benign fibrous histiocytoma (nonossifying fibroma) Skeletal Radiol. 1986;15(3):251–253. doi: 10.1007/BF00354071. [DOI] [PubMed] [Google Scholar]
- 34.Cale AE, Freedman PD, Kerpel SM, Lumerman H. Benign fibrous histiocytoma of the maxilla. Oral Surg Oral Med Oral Pathol. 1989;68(4):444–450. doi: 10.1016/0030-4220(89)90143-6. [DOI] [PubMed] [Google Scholar]
- 35.Ertaş U, Büyükkurt MC, Ciçek Y. Benign fibrous histiocytoma: report of case. J Contemp Dent Pract. 2003;4(2):74–79. doi: 10.5005/jcdp-4-2-74. [DOI] [PubMed] [Google Scholar]
- 36.Heo MS, Cho HJ, Kwon KJ, Lee SS, Choi SC. Benign fibrous histiocytoma in the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(2):276–280. doi: 10.1016/j.tripleo.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 37.Kishino M, Murakami S, Toyosawa S, Nakatani A, Ogawa Y, Ishida T, Ijuhin N. Benign fibrous histiocytoma of the mandible. J Oral Pathol Med. 2005;34(3):190–192. doi: 10.1111/j.1600-0714.2004.00274.x. [DOI] [PubMed] [Google Scholar]
- 38.Katagiri W, Nakazawa M, Kishino M. Benign fibrous histiocytoma in the condylar process of the mandible: case report. Br J Oral Maxillofac Surg. 2008;46(1):e1–2. doi: 10.1016/j.bjoms.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 39.Tanaka T, Kobayashi T, Iino M. Transformation of benign fibrous histiocytoma into malignant fibrous histiocytoma in the mandible: case report. J Oral Maxillofac Surg. 2011;69(7):e285–e290. doi: 10.1016/j.joms.2011.02.067. [DOI] [PubMed] [Google Scholar]
- 40.Wagner ME, Rana M, Traenkenschuh W, Kokemueller H, Eckardt AM, Gellrich NC. Piezoelectric-assisted removal of a benign fibrous histiocytoma of the mandible: an innovative technique for prevention of dentoalveolar nerve injury. Head Face Med. 2011;7:20. doi: 10.1186/1746-160X-7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gupta P, Godhi SS, Kukreja P, Bhatnagar S, Lall AB, Singh A, et al. Fibrous histiocytoma of the Mandible-a case report. J Indian Dent Assoc. 2011;5:994–995. [Google Scholar]
- 42.Ou DM, Zheng GS, Liao GQ, Su YX, Liu HC, Liang YJ. Clinical and pathologic characteristics and surgical management of benign fibrous histiocytoma of the mandible: a case report. J Oral Maxillofac Surg. 2012;70(11):2719–2723. doi: 10.1016/j.joms.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 43.Saluja H, Kasat VO, Rudagi BM, Dehane V, Kalburge JV, Nikam A. Benign fibrous histiocytoma of the maxilla: a case report and review of literature. Indian J Dent Res. 2014;25(1):115–118. doi: 10.4103/0970-9290.131160. [DOI] [PubMed] [Google Scholar]
- 44.Shoor H, Pai KM, Shergill AK, Kamath AT. Benign fibrous histiocytoma: a rare case involving jaw bone. Contemp Clin Dent. 2015;6(Suppl 1):S266–S268. doi: 10.4103/0976-237X.166828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vyloppilli S, Joseph B, Manoj Kumar KP, Kurian SD, Anirudhan A, Kumar N. Benign spindle cell tumour of mandible and points of modification in reconstruction with nonvascularised iliac crest graft. J Maxillofac Oral Surg. 2016;15(Suppl 2):262–265. doi: 10.1007/s12663-015-0775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pattamparambath M, Sathyabhama S, Khatri R, Varma S, Narayanan NM. Benign Fibrous Histiocytoma of Mandible: a case report and updated review. J Clin Diagn Res. 2016;10(6):ZD24–ZD26. doi: 10.7860/JCDR/2016/19067.8056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mohanty A, Mishra P, Kumar H, Panda A. A rare presentation of benign fibrous histiocytoma in the maxilla. J Oral Maxillofac Pathol. 2020;24(Suppl 1):S73–S76. doi: 10.4103/jomfp.JOMFP_321_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Singh Chauhan JP, Kumar A, Porwal PK, Thakur RK, Mittal K, Singh H. Benign fibrous histiocytoma of the maxilla: a rare case report and literature review. Natl J Maxillofac Surg. 2020;11(2):298–301. doi: 10.4103/njms.NJMS_85_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang Y, Huang Y, Cai WX, Tao Q. Multiple benign fibrous histiocytomas of the mandible: a case report and review of the literature. Exp Ther Med. 2022;24(3):593. doi: 10.3892/etm.2022.11530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li TJ, Yu SF. Clinicopathologic spectrum of the so-called calcifying odontogenic cysts: a study of 21 intraosseous cases with reconsideration of the terminology and classification. Am J Surg Pathol. 2003;27(3):372–384. doi: 10.1097/00000478-200303000-00011. [DOI] [PubMed] [Google Scholar]
- 51.Fowler CB, Brannon RB, Kessler HP, Castle JT, Kahn MA. Glandular odontogenic cyst: analysis of 46 cases with special emphasis on microscopic criteria for diagnosis. Head Neck Pathol. 2011;5:364–375. doi: 10.1007/s12105-011-0298-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bovée JV, Hogendoorn PC. Non-ossifying fibroma: a RAS-MAPK driven benign bone neoplasm. J Pathol. 2019;248(2):127–130. doi: 10.1002/path.5259. [DOI] [PMC free article] [PubMed] [Google Scholar]