Abstract
Differentiated Thyroid carcinoma (DTC) with distant skeletal metastases is associated with a very poor prognosis and are unfortunately resistant to radioiodine therapy (RIT). Surgical removal of the metastases in such selected cases is a beneficial adjunct to RIT. We report two cases of DTC with sternal metastases whom we successfully managed with surgical resection of the sternal lesion with reconstruction of the chest wall defect using titanium mesh implant and myocutaneous flap.
Keywords: Differentiated thyroid carcinoma, Sternal metastases, Mesh, Myocutaneous flap
Introduction
Although the incidence of bone metastases from thyroid cancer is 4-23% [1], direct invasion or bone metastasis to the sternum is a very rare presentation. Patients with bone metastases are associated with a poor 10-year survival from 2 to 15% [2], however additional treatments may reduce the tumor burden in selected patients and thus offer them a survival or palliative benefit. Radioactive iodine (RAI) ablation is the treatment of choice for distant metastases but unfortunately this modality has a limitation of reduced iodine avidity in bone metastases [3, 4].
Other treatment modalities for patients with metastatic thyroid cancer include surgical excision, external beam radiotherapy, and recruitment to clinical trials.
Complete surgical resection of isolated symptomatic metastases is associated with effective uptake of RAI even in other distant metastases such as lung metastases, thus imparts an improved survival and should be considered especially for patients < 45 years old with slowly progressive diseases as well as in solitary sternal metastases [5, 6]. Therefore, if possible, surgical resection should be considered one of the treatments of choice for patients with bone metastases.
Our report describes two cases of thyroid carcinoma with sternal metastases, who were managed with surgical resection of metastases followed by reconstruction of the chest wall defect with titanium mesh. This report guides us to manage differentiated thyroid carcinoma (DTC) with distant bony metastases with a curative approach, with a provision of effective palliation as well as RAI uptake.
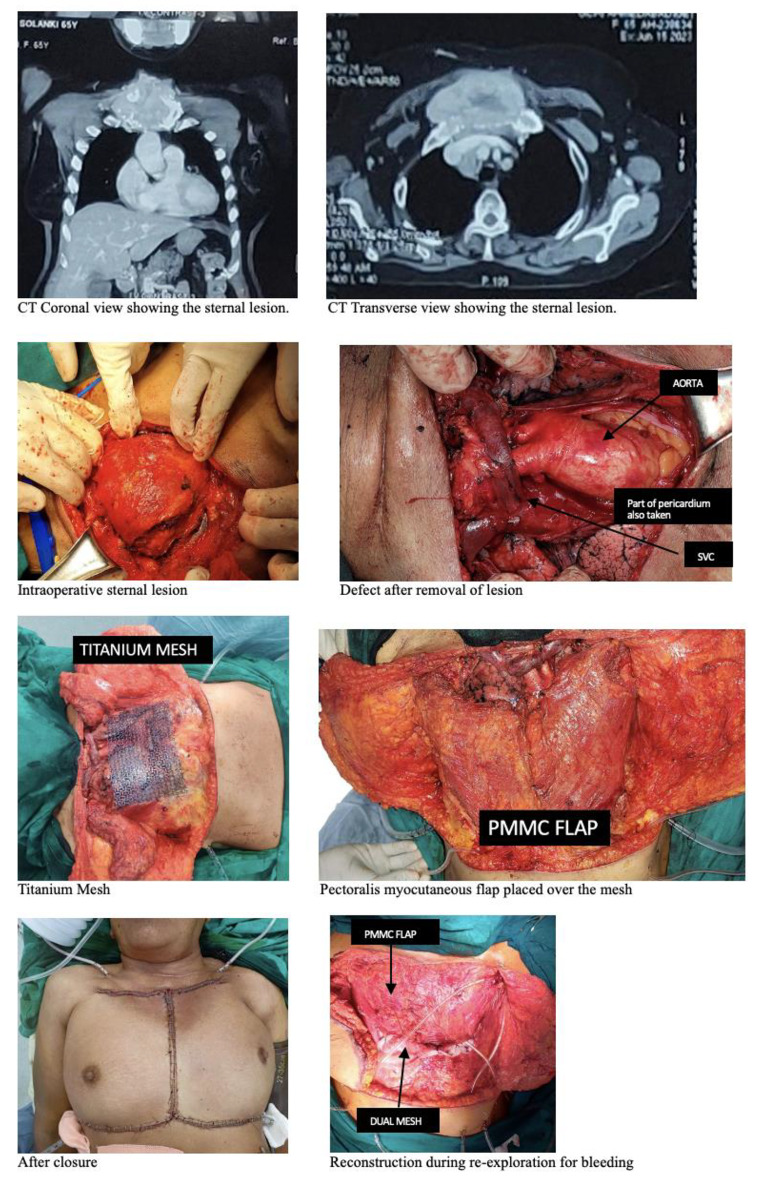
Case Report 1
A 50-year-old lady, a known case of follicular thyroid carcinoma (FTC) presented to us with anterior chest wall mass lesion and increase in the number and size of the lung & bony metastases. She had a history of right hemithyroidectomy in 2013 for FTC for which she did not take any adjuvant treatment. She then underwent completion thyroidectomy with bilateral neck dissection in 2019 for residual/recurrent disease and metastases to lung and bone, which on final histology was suggestive of FTC pT1bN0. She received radioactive iodine therapy in adjuvant setting with 200 mCi and then lost to follow up for 4 years. In 2023, she underwent wide local excision of the chest wall mass along with removal of part of clavicle with 1st and 2nd ribs along with the manubrium sterni and reconstruction with Pectoralis major myocutaneous flap (PMMC) and titanium mesh. Post operative recovery was good until post operative day10 when she developed thrombus in the right subclavian & axillary vein with anterior chest wall collection over the mesh detected on Computed tomography (CT) scan. Under all aseptic precautions, suction drain was placed inside the collection under local anesthesia. Patient was started on unfractionated heparin infusion followed by oral direct thrombin inhibitors. Patient recovered well with resolution of the right arm edema as well as the anterior chest wall collection. Patient is now on follow-up on thyroxine replacement dose for further treatment with RAI.
Fig. 1.
Clinical photographs of case
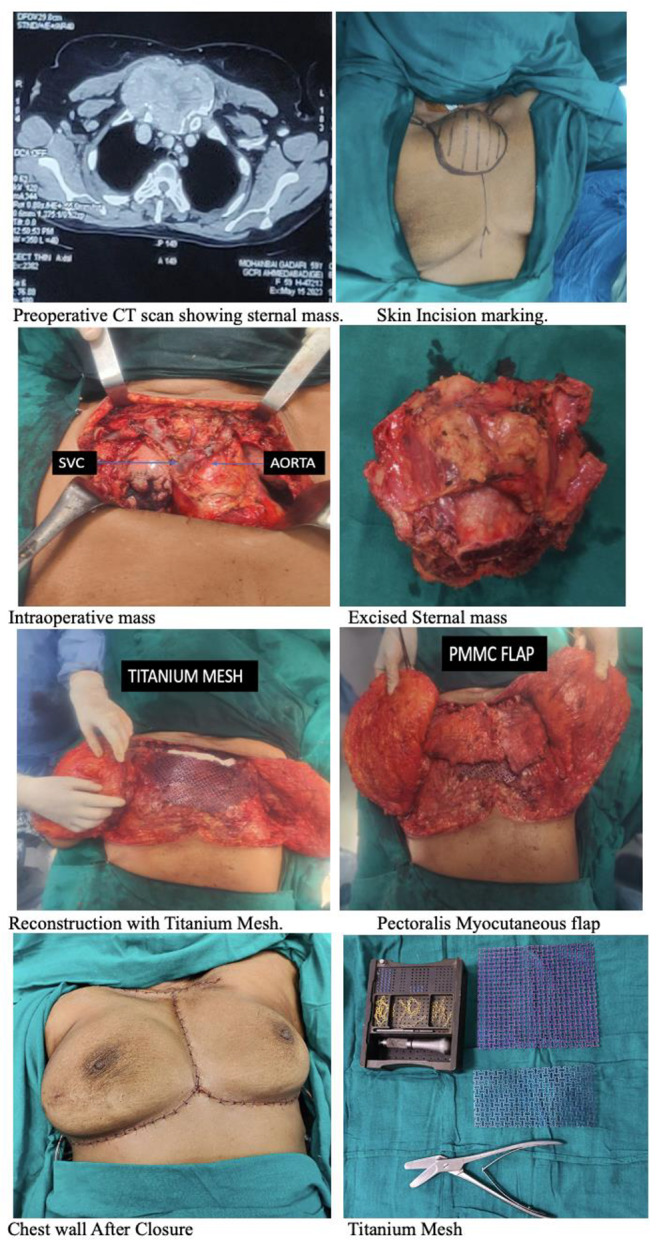
Case Report 2
A 65-year-old lady underwent left hemithyroidectomy in January 2023 and was reported with follicular variant of papillary thyroid carcinoma (PTC) on histological examination. She presented to us after 4 months when she developed an anterior chest wall swelling which was increasing in size. Chest CT scan showed 46 × 66 × 70 mm lytic bony lesion involving upper sternum and 1st costal cartilages with multiple lung metastasis and cervical & mediastinal lymphadenopathy with residual lesion of right lobe of thyroid gland. She underwent completion thyroidectomy with neck dissection and sternal resection with reconstruction using titanium mesh and PMMC flap. She was re-explored on post operative day 3 for a 5 mm tear at the root of brachiocephalic trunk which was repaired with the remaining pericardium and reconstruction was done using the poly-propylene dual mesh and covered with the PMMC flap.
Fig. 2.
Clinical photographs of case 2
Discussion
Distant metastases occur in 10% of PTC and 25% of FTC and is the principal cause of death from DTC [7]. Bone metastases occur in almost 2–15% cases of DTC and approximately 19% patients develop sternal metastases [1]. Although the 10-year survival rate in DTC is approximately 98%, sternal metastases is associated with 2–15% of survival rate only [2], thus worsening the prognosis. This may be attributed to the reduced sensitivity to radioiodine in bone metastases, likely due to lesser absorption by poorly differentiated tumor cells [5].
Various therapeutic options include chemotherapy, I-131 treatment (if the whole-body scan is positive), considering dosimetry to maximize dosing and/or external-beam radiotherapy and surgical palliation. Surgical option is indicated in solitary metastases and resectable lesions. However, cytoreductive resection in cases with multiple metastases may provide an efficient radioiodine treatment, thus improving the prognosis in such cases.
Studies done by Stojadinovic et al. and Zettinig et al. have also reported the effect of metastatectomy in distant bony metastases and the associated improved survival [8, 9].
In our case report, to achieve optimal results, completion thyroidectomy with a composite resection of the metastatic sternal lesion was warranted in case 2 while in case 1 it was a staged procedure. Radical removal of the metastatic sternum, including the adjacent clavicle and ribs, was necessary to obtain clear margins in both the cases.
Reconstruction of the chest wall after sternal resection can be done either by autoplastic reconstruction in a small size defect or by using autologous flaps like myocutaneous flaps or alloplastic materials like titanium mesh, marlex mesh, Gore-Tex, dual mesh steel mesh in a wider defect. In our patients, we have used dual technique of titanium mesh and soft tissue coverage using PMMC flap.
Post operative complications like cardio-vascular instability, bleeding, vascular thrombosis, infection, implant related complications, wound related morbidity, pain management should be addressed promptly. Long term follow up is needed to prove survival advantage in any for these cases.
Conclusion
In summary, wide composite resection with appropriate reconstruction for advanced DTCs with sternal metastases can be performed safely and may offer these patients a palliative or survival benefit. Appropriate patient selection with a multidisciplinary approach may reduce the morbidity and mortality in such surgical procedures.
Funding
No funds received.
Declarations
Ethical Approval
Compliance with ethical standards has been maintained and approval from institutional ethical committee received.
Conflict of Interest
None.
Consent
Informed Consent was taken from both the patients.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Osorio M, Sami P, et al. Systematic review of site distribution of bone metastases in differentiated thyroid cancer. Head Neck. 2016;39(4):812–818. doi: 10.1002/hed.24655. [DOI] [PubMed] [Google Scholar]
- 2.Muresan MM, Olivier P, Leclère J, et al. Bone metastases from differentiated thyroid carcinoma. Endocr Relat Cancer. 2008;15:37–49. doi: 10.1677/ERC-07-0229. [DOI] [PubMed] [Google Scholar]
- 3.Marcocci C, Pacini F, et al. Clinical and biologic behavior of bone metastases from differentiated thyroid carcinoma –. Surgery. 1989;106(6):960–966. [PubMed] [Google Scholar]
- 4.Brown AP, Greening WP, et al. Radioiodine treatment of metastatic thyroid carcinoma: the Royal Marsden Hospital experience. Br J Radiol. 1983;57(676):323–327. doi: 10.1259/0007-1285-57-676-323. [DOI] [PubMed] [Google Scholar]
- 5.Mishra A, Mishra SK, et al. Surgical Treatment of Sternal metastases from thyroid carcinoma: report of two cases. Surg Today. 2001;31(9):799–802. doi: 10.1007/s005950170050. [DOI] [PubMed] [Google Scholar]
- 6.Haraguchi S, Yamashita Y, et al. Sternal resection for Metastasis from thyroid carcinoma and reconstruction with the sandwiched marlex and stainless steel mesh. Japanese J Thorac Cardiovasc Surg. 2004;52(4):209–212. doi: 10.1007/s11748-004-0111-2. [DOI] [PubMed] [Google Scholar]
- 7.Yanagawa J, Abtin F, Lai CK et al (2009) Resection of thyroid Cancer metastases to the Sternum. J Thorac Oncol • 4. 10.1097/JTO.0b013e3181adef20. [DOI] [PubMed]
- 8.Stojadinovic A, Ronald A, et al. The role of operations for distantly metastatic well-differentiated thyroid carcinoma. Surgery. 2002;131(6):636–643. doi: 10.1067/msy.2002.124732. [DOI] [PubMed] [Google Scholar]
- 9.Zetting G, Barbara J, et al. Long-term follow-up of patients with bone metastases from differentiated thyroid carcinoma - Surgery or conventional therapy? Clin Endocrinol. 2001;56(3):377–382. doi: 10.1046/j.1365-2265.2002.01482.x. [DOI] [PubMed] [Google Scholar]