Abstract
Although microvascular free flaps are considered the first choice in head and neck cancer defect reconstruction, their use is limited in developing regions by availability of resources and the expertise .The Bipaddle pectoralis major myocutaneous flap (PMMC flap) is a commonly used flap in head and neck cancer reconstruction, but in literature flap is associated with high incidence of drawbacks including donor site morbidity and added bulk of the flap reducing cosmetics and function. The purpose of the study is to evaluate the Bipaddle PMMC flap reliability, operative technique and outcome in reconstructive head and neck cancer surgery in the era of microvascular free flaps. Its a prospective study in which the records of 50 patients treated with Bippadle PMMC flap reconstruction between January 2022 to July 2022 were systematically collected and reviewed. Data of recipient site, serum albumin, history of adjuvant, recurrence, defect dimension, type of donor site closure, length of hospital stay, postoperative complications and outcomes were analysed. There were 45 males and 5 females with a mean age of 41 years (31–60). Bipaddle PMMC flap reconstruction was done in all patients of advanced squamous cell carcinoma of oral cavity. There were two males with complete necrosis of flap salvaged with latissimus dorsi flap and forehead flap. Minor infections were noted in two female and one male patient, managed conservatively and recovered well with acceptable final outcome. The Bipaddle PMMC flap is reliable for large defects in head and neck reconstructive surgery, particularly when a bulky flap is required to reconstruct composite defects where the lesion is involving the skin. Placing the flap horizontally with inclusion of nipple and areola in most of the patients increased the reach and size of available flap.
Keywords: Full thickness cheek and oral defects, Operative technique, Bipaddle pectoralis major myocutaneous flap (PMMC flap)
Introduction
Oral cavity plays an important role in speech, deglutition, respiration and cosmesis of an individual. Since, majority of patients in India present with an advance disease stage [Fig. 1] which requires aggressive resection leading to large composite defects [Fig. 2] resulting in significant functional and aesthetic problems [1, 2]. Reconstruction of these defects should aim in restoring near normal form and function in individuals. Such composite defects of the head and neck region require reconstruction of several layers, including the intra-oral lining, osseous reconstruction of the mandible or maxilla and soft tissue/skin coverage. Free flaps are considered as ‘‘gold standard’’ for reconstructing such post-resection defects [3], but are not always available in all the centres managing head and neck malignancies mainly in developing countries, owing to higher costs and requirement of expertise in terms of refined microsurgical techniques [4].
Fig. 1.
Picture showing advance carcinoma buccal mucosa
Fig. 2.
Picture showing defect after surgical resection
The utility of pectoralis major myocutaneous flap (PMMC) still exists in advanced diseases with systemic co-morbidities and compromised vessel calibre which prevents use of free flaps. The pectoralis major myocutaneous flap (PMMC) has always been the workhorse flap of the head and neck reconstruction and has stood the test of time since its first description by Ariyan [5]. It carries the advantages of its determinate blood supply, excellent reach, robust size and bulk. Its advantages include reliable blood supply, excellent reach, robust size and bulk [6].
The purpose of the study is to evaluate the Bipaddle PMMC flap reliability, operative technique and outcome in reconstructive head and neck cancer surgery in the era of microvascular free flaps.
Materials and Methods
Its a prospective study in which the records of 50 patients treated with Bippadle PMMC flap reconstruction between January 2022 to July 2022 were included. Their data was systematically collected and reviewed. Data of recipient site, serum albumin, history of adjuvant, recurrence, defect dimension, type of donor site closure, length of hospital stay, postoperative complications and outcomes were analysed. All the patients underwent composite resection which included a wide local resection of primary tumour, segmental mandibulectomy and neck dissection. The neck dissection was modified radical neck dissection in all the cases. All the patients required postoperative adjuvant radiotherapy.
Technique of Harvesting PMMC Flap
All the flaps were harvested according to the standard technique. Various techniques have been mentioned in literature including Freeman technique [7]. The flap design and the skin island were dependent on the site, size and shape of the defects with the skin island being usually below and medial to the nipple about the level of sixth rib. The surface marking was done by drawing a line from acromion process to the xiphisternum and another line drawn from midpoint of clavicle vertically intersecting the first line. Skin paddle was designed in a way that it lies over the pectoralis major muscle for reliable blood supply. The skin paddle was bevelled to avoid undercutting and to include more of myocutaneous perforators. The skin paddle was sutured to the underlying.
Muscle to avoid any shearing forces and insult to the perforators. The plane between pectoralis minor and pectoralis major was reached by dissecting the lateral border of pectoralis major muscle. The flap was elevated carefully keeping in view the vascular paddle at all times. The pectoralis major muscle was divided laterally and medially to the vascular pedicle, releasing it from the humerus and sternum. The flap was passed into the neck under the subcutaneous tunnel over the clavicle. The compression of the flap was avoided by sufficiently widening the tunnel. 3 − 0 vicryl was used to suture the flap and reconstruct the intra-oral defect. The flap was de-epithelialised at the junction of intra-oral and extra-oral defect for separate compartmental reconstruction. The donor site was closed primarily. Negative Suction drains were placed in neck and chest. Wounds closed in layers after hemostasis [Fig. 3].
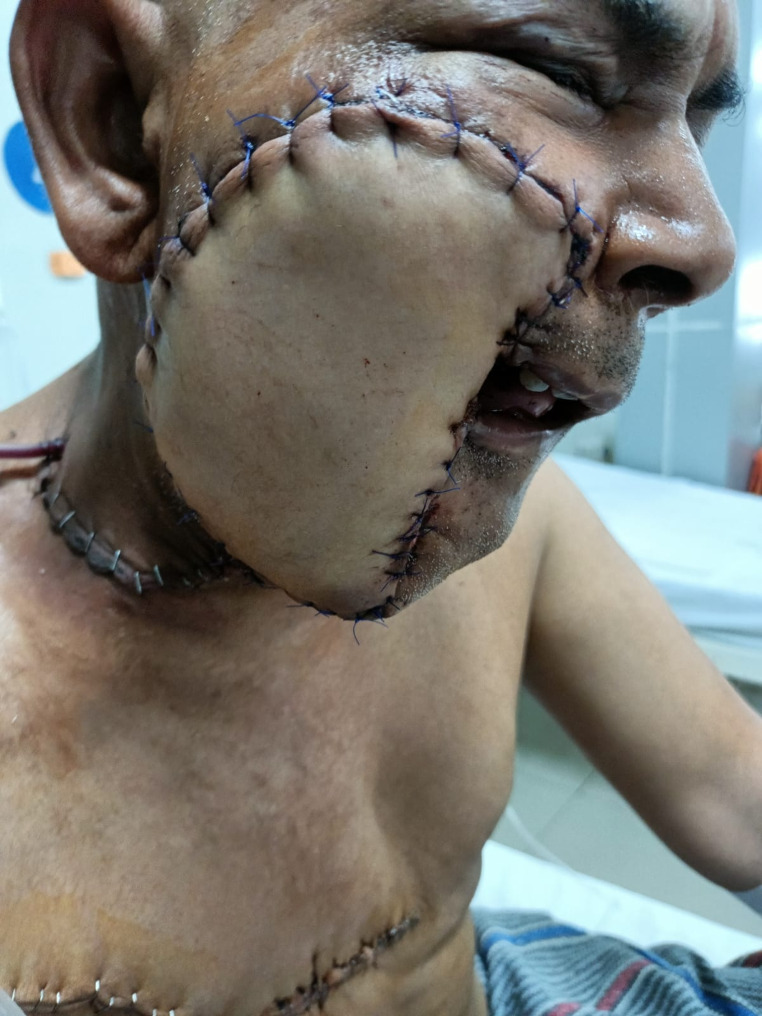
Fig. 3.
Picture showing closure of defect with large PMMC flap
Results
On analysing the data Table 1, we found that amongst 50 patients, 45 were males and 5 were females. The age group was between 31 and 60 years, with a mean age of 41. All the patients had biopsy proven malignancy. Resection of primary lesion, neck dissection and PMMC flap reconstruction was done for all patients.
Table 1.
Incidence of patient factors
| PATIENT FACTORS | NUMBER OF CASES (N = 50) | PERCENTAGE % |
|---|---|---|
| ENE PRESENT | 4 | 8% |
| RECURRENCE | 2 | 4% |
| CHEST CLOSURE WITH STSG | 1 | 2% |
| ADJUVANT RECIEVED WITHIN 5 WEEKS POST-OPERATIVELY | 37 | 74% |
| HOSPITAL STAY > 10 DAYS | 4 | 8% |
| OCF | 4 | 8% |
| OSMF | 41 | 82% |
Majority of cases showed squamous cell carcinoma involving gingivobuccal complex and buccal mucosa (96%) followed by malignancy of lower alveolus (4%). Out of 50 patients two patients were recurrent cases. All patients had History of tobacco consumption in smokeless form with and without smoking. OSMF was present in 82% of patients. Out of 50 patients 9 patients didn’t have oral sub mucous fibrosis. Out of 50 patients, 8 patients were T4B. Out of 50 patients 94% of the patients had lymph node metastasis and 4 patients had extra nodal extension. All patients had extra-oral skin involvement. 26% patients did not take adjuvant treatment as required. The average serum albumin was 3.5. and average hemoglobin was 12.5. Out of 50 patients four patients had serum albumin < 2.5 which was not significant for infection or wound dehiscence.
There were two males with complete necrosis of flap [Fig. 4] salvaged with latissimus dorsi flap and forehead flap. Minor infections were noted in two female and one male patient, managed conservatively and recovered well with acceptable final outcome. On analysis of our data, we found the most common post-operative complication to be wound dehiscence Table 2 which was seen in 5 patients (10%), orocutaneous fistula in 4 (8%) followed by 3 patients with wound infection (6%) and partial skin margin necrosis which was seen in one patient (2%), donor site wound dehiscence in one patient (2%) four patients underwent re-suturing of wound. Out of 50 patients, 37 patients underwent radiotherapy two to three weeks post-operatively as per the indications and remaining 13 patients refused to undergo radiotherapy and chemotherapy because of financial constraints. A total of 32 patients tolerated radiotherapy with minimal toxicity, and there was no evidence of flap necrosis in the neck, nor any case of carotid blow out. The average hospital stay was of 5 days. Out of 50 patients four patients had hospital stay > 10 days.
Fig. 4.
Picture showing flap necrosis
Table 2.
Flap related complications incidence
| FLAP RELATED COMPLICATIONS | NUMBER OF CASES (N = 50) | PERCENTAGE % |
|---|---|---|
| TOTAL NECROSIS | 2 | 4% |
| INFECTION | 3 | 6% |
| WOUND DEHISCENCE | 5 | 10% |
| PARTIAL NECROSIS | 1 | 2% |
Discussion
Pectoralis major myocutaneous flap is one of the most versatile flaps available in literature and documented as workhorse flap for reconstruction of head and neck cancer defects. Our study has evaluated the Bipaddle PMMC flap reliability, operative technique and outcome in reconstructive head and neck cancer surgery in the era of microvascular free flaps. There is a variable flap complication rate in literature due lack of sample size for bipaddle PMMC flap. Free flaps have distinctive advantages over pedicled flap like better cosmesis, less bulk of the flap and better rehabilitation options, although one important finding that we noted in present study is the ability of the PMMC flap to be used as salvage procedure after failure of free flaps. This forms an important option in cases where use of vascularised flaps is not possible or in patients with vessels abnormalities, extremes of ages, patients with medical co-morbidities. [3]
Also PMMC flap is a economic and reliable option for salvaging free flap failures, with better chances of patient to receive adjuvant treatment on time, as its very crucial for prognosis of patient. Same results were reflected by Schneider et al. [5] who stated PMMC flap was used as salvage procedure in 38% of their case series and another study done by Saito et al. [8] stated that 75% of cases operated for PMMC flaps were only used as salvage procedure supporting our findings. There were two males with complete necrosis of flap salvaged with latissimus dorsi flap and forehead flap. Minor infections were noted in two female and one male patient, managed conservatively and recovered well with acceptable final outcome. One of the most important advantages of PMMC flap is its ability to be used for reconstruction of extensivee composite defects, while avoiding need of free flaps, this is possible by using of bilobed or bipaddle flap by dividing the skin in two parts for extraoral and intraoral lining both via de-epithelialization. In a study done by Bhola et al. [9] where after resection of oral cancer, 62 cases of through-and-through defects of the oral cavity were reconstructed using bilobed PMMC flap. No patient developed a major complication and most common complication was wound dehiscence. The disadvantages of bipaddle flap include loss of nipple and areola complex (NAC) seen in most patients and technical difficulty in obese patients and females with heavy breasts. In female patients, the skin island extended below the seventh rib and the skin paddle was small in one patient that probably did not encompass a sufficient number of skin perforator vessels, thus resulting in unstable blood circulation. Another complication in literature was, the incidence of carotid blow out as per different authors ranges from 2.6 to 25% in head and neck irradiated region [10, 11]. In our study we did not encounter any carotid blow out. One disadvantage of the PMMC flap that we encountered in our study was bulky nature of the flap that gave the patient oedematous appearance. We used a special technique intra-operatively to de-bulk the flap over the clavicle to reduce the contracture and increase the range of flap. In most of our cases we achieved primary closure of the chest donor site inspite of large size of the skin paddle, due to the wide undermining of skin flaps. Most authors performed a primary closure but in some cases, different techniques have been described like buttons or Ventrofil®, a special tension- relief bridging device [12]. Closed suction drains are used to drain the donor site as well as the neck. A good success rate of PMMC flap was observed in our study (82.14%), and this rate was comparable with several papers in the literature [13–16]. The present study did not observe any cases of total flap loss and rate of partial loss was acceptable, with good final outcome observed in four such cases. In females there is intervening extra fatty tissue in breasts as compared to males.
Conclusion
The Bipaddle / Bilobed PMMC flap is reliable for large defects in head and neck reconstructive surgery, particularly when a bulky flap is required to reconstruct composite defects where the lesion is involving the skin. Placing the flap horizontally with inclusion of nipple and areola in most of the patients increased the reach and size of available flap. Hence, PMMC flap will always be a workhorse flap due to its advantages like versatility, local availability, ease of harvesting, excellent blood supply with reliable pedicle, with very good reach to all the corners of oral cavity and with minimal morbidity forms still remains workhorse for reconstruction of oral cavity defects.
Acknowledgements
We are grateful to the Departments of Pathology at SMS Medical College, SDM Hospital, contributions and support.
List of Abbreviations
- PMMC
Pectoralis Major Myocutaneous Flap
- SMS
Sawai Man Singh
- SDM
Santokba Durlabhji Memorial
Author Contributions
BGS and PP conceived the idea. PMS and AB designed the study and laid the framework for data collection. PP, SS and BGS did data collection and data entry. KKL and SS supervised data entry and did data analyses. AB and BGS laid down the framework for the paper and supervised data analysis. SS, PP, KKL wrote the manuscript. BGS, AB and SS helped review literature. PP, and NKA helped in editing and formation of the final draft.
Funding
No external sources of funding to declare. This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics Approval
Approval from the Institutional Ethics Committee of SMS medical college, Jaipur was taken for the conduct of this study.
Consent for Publication
Not Applicable.
Competing Interests
No competing interests to declare.
Conflict of Interest
Authors would like to declare there is no funding from institution or commercial company with regard to this study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ariyan S. Further experiences with the pectoralis major myocutaneous flap for the immediate repair of defects from excisions of head and neck cancers. Plast Reconstr Surg. 1979;64(5):605–612. doi: 10.1097/00006534-197911000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Sharma S, Murty P, Hazarika P, Nayak D, Sharma S. The indications and complications of pectoralis major myocutaneous flap reconstruction in head and neck surgery-our experience. Indian J Otolaryngol Head Neck Surg. 1998;50(4):362–367. doi: 10.1007/bf03000688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pinto F, Malena C, Vanni C, Capelli F, Matos L, Kanda J. Pectoralis major myocutaneous flaps for head and neck recon- struction: factors influencing occurrences of complications and the final outcome. Sao Paulo Med J. 2010;128(6):336–341. doi: 10.1590/s1516-31802010000600005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petruzzelli GJ, Brockenbrough JM, Vandevender D, Creech SD. The influence of reconstructive modality on cost of care in head and neck oncologic surgery. Arch Otolaryngol Head Neck Surg. 2002;128(12):1377–1380. doi: 10.1001/archotol.128.12.1377. [DOI] [PubMed] [Google Scholar]
- 5.Ariyan S. The pectoralis major myocutaneous flap. A versatile flap for reconstruction in the head and neck. Plast Reconstr Surg. 1979;63:73–81. doi: 10.1097/00006534-197901000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Wood JE. Reconstruction in head and neck cancer: a place for conservatism. Ann Plast Surg. 1987;18:209–211. doi: 10.1097/00000637-198703000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Freeman JL, Walker EP, Wilson JS, Shaw HJ. Te vascular anatomy of the pectoralis major myocutaneous flap. Br J Plast Surg. 1981;34:3–10. doi: 10.1016/0007-1226(81)90086-2. [DOI] [PubMed] [Google Scholar]
- 8.Saito A, Minakawa H, Saito N, Nagahashi T. Indications and outcomes for pedicled pectoralis major myocutaneous flaps at a primary microvascular head and neck reconstructive center. Mod Plast Surg. 2012;02(04):103–107. doi: 10.4236/mps.2012.24025. [DOI] [Google Scholar]
- 9.Bhola N, Jadhav A, Borle R, Khemka G, Kumar S, Shrivastava H. Is there still a role for bilobed/bipaddled pectoralis major myocutaneous flap for single- stage immediate reconstruction of post ablative oncologic full-thickness defects of the cheek? Oral Maxillofac Surg. 2014;19(2):125–131. doi: 10.1007/s10006-014-0458-1. [DOI] [PubMed] [Google Scholar]
- 10.Chen Y, Wang C, Wang C, Jiang R, Lin J, Liu S. Carotid blowout in patients with head and neck cancer: associated factors and treatment outcomes. Head Neck. 2014;37(2):265–272. doi: 10.1002/hed.23590. [DOI] [PubMed] [Google Scholar]
- 11.McDonald M, Moore M, Johnstone P. Risk of carotid blowout after reirradiation of the head and neck: a systematic review. Int J Radiat Oncol Biol Phys. 2012;82(3):1083–1089. doi: 10.1016/j.ijrobp.2010.08.029. [DOI] [PubMed] [Google Scholar]
- 12.Kruse AL, Luebbers HT, Gratz KW, Bredell M (2010) : A new method for closure of large donor side defects after raising the pectoralis major flap. Oral MaxillofacSurg [DOI] [PubMed]
- 13.Milenović A, Virag M, Uglesić V, Aljinović-Ratković N. The pectoralis major flap in head and neck reconstruction: first 500 patients. J Craniomaxillofac Surg. 2006;34(6):340–343. doi: 10.1016/j.jcms.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 14.El-Marakby HH. The reliability of pectoralis major myocutaneous flap in head and neck reconstruction. Egypt NatlCancInst. 2006;18:41–50. [PubMed] [Google Scholar]
- 15.Liu R, Gullane P, Brown D, Irish J. Pectoralis major myocutaneouspedicled flap in head and neck reconstruction: retrospective review of indications and results in 244 consecutive cases at the Toronto General Hospital. J Otolaryngol. 2001;30:34–40. doi: 10.2310/7070.2001.21011. [DOI] [PubMed] [Google Scholar]
- 16.Vartanian JG, Carvalho AL, Carvalho SM, Mizobe L, Magrin J, Kowalski LP. Pectoralis major and other myofascial/myocutaneous flaps in head and neck cancer reconstruction: experience with 437 cases at a single institution. Head Neck. 2004;26:1018–1023. doi: 10.1002/hed.20101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.