Abstract
The diagnostic criteria for silent sinus syndrome (SSS) are still controversial, especially for the post-traumatic/surgery cases that are, nowadays, excluded from the diagnosis of SSS because lacking of spontaneously. We present a systematic review of the last 10 years and our case series of SSS associated to previous trauma/surgery, proposing a new interpretation of SSS. In this work, following the PRISMA guide lines for systematic reviews, we collected 86 articles published on PubMed, Cochrane Library and Medline Plus since 2013 to 2023 about SSS. We divided them in six groups forming the structure of the review: (1) epidemiology, (2) clinical presentation, (3) imaging, (4) etiopathogenesis, (5) sss and craniofacial trauma and (6) treatment. We reported two explicative clinical cases: two men of 34 and 37 years old, involved in motorcycle accident in 2020 and 2014, respectively, and underwent surgery. They came back in 2023 referring diplopia documented by Hess-Lancaster test. CT-scan reported two clear cases of SSS. Basing on what is reported in literature, and basing on our experience, the post-traumatic/surgery SSS are more frequent than the idiopathic ones. Our proposal is to considered them as two individual entities. We propose to adopt the name of Post-traumatic sinus syndrome, or CDR syndrome (Catalfamo-De Rinaldis), for all cases that respect four specific diagnostic criteria reported into the text.
Keywords: Silent sinus syndrome, Chronic maxillary atelectasis, Maxillary sinus hypoplasia, Post-traumatic sinus, Enophthalmos, Diplopia, Hess-lancaster test, Maxillofacial trauma
Introduction
In 1964 montgomery described a case of enophthalmos associated to a mucocele of the maxillary sinus [1]. That was the first description of the entity known as “chronic maxillary atelectasis” (CMA) or “maxillary sinus hypoplasia” (MSH).
In 1994, Soparkar introduced the term “silent sinus syndrome” (SSS) to identify all clinical signs and symptoms correlated to CMA [2].
The scientific community is uncertain about diagnostic criteria of SSS. One of the main doubt is about its correlation with the chronic maxillary sinusitis even if, currently, an essential criterion for diagnosis of silent sinus syndrome is the absence of symptoms characteristic of Chronic RhinoSinusitis (CRS), as reported in the European Position Paper on Rhinosinusitis and Nasal Polyps 2020 (EPOS 2020) [3].
However, some authors disagree and suggest to include into the diagnosis of SSS also all cases of CMA associated with chronic rhinosinusitis [4].
The following criteria have been proposed for the diagnosis of Silent Sinus Syndrome [5]:
No episodes of acute rhinosinusitis and no history of chronic rhinosinusitis;
Remodeling and inferior bowing of the maxillary roof/orbital floor evident in a coronal CT scan;
No history of orbital trauma or orbital/sinus surgery;
No documented congenital deformity of sinus and/or nasal cavity.
Kass et al. [6], classified CMA in three stages based on radiological features:
Stage I: membranous deformity,
Stage II: bony deformity,
Stage III: clinical deformity (enophthalmos/hypoglobus/diplopia).
Still today it isn’t clear if SSS and CMA are the same pathological entity or if they are two distinct entities. In literature they are still described separately but several authors, based on the observation that the definition of the stage III of CMA meet, exactly, the same diagnostic criteria of SSS, propose to consider SSS and CMA the same entity, and propose to adopt Kass staging system to describe the natural evolution of SSS [7–10].
SSS is referred only to the involvement of the maxillary antrum but sporadic cases of “ethmoidal sinus syndrome” and “frontal sinus syndrome” are just mentioned in literature [11–15].
Materials and Methods
Following the rules of PRISMA guide lines, we propose a systematic review of the last 10 years, since 2013 to 2023, about the topic of Silent Sinus Syndrome and we present two of our representative clinical cases.
We used PubMed, Cochrane Library and Medline Plus as searching engines and we entered “silent sinus syndrome” as key words.
We found a total of 174 papers, forty-five of which were excluded by their title for one or more of the following reasons:
Duplication,
Different topic (ex. sick sinus syndrome),
Language different from English.
So, 129 papers were selected for the Abstract reading. With the following step, 98 papers were selected for the complete reading and, finally, 86 manuscripts were collected for the analysis programmed. We excluded all the articles that were only case report and that didn’t provide any further contribute more than already reported by the others just selected. After that, we divided the article in two main groups: the ones relative to SSS in adult patients (80 papers) and the others reported pediatric cases of SSS (6 papers).
Finally, we divided the articles in six subgroups basing on the main contribution each of them provided and those subgroups formed the structure of the review:
-
I.
Epidemiology.
-
II.
Clinical presentation.
-
III.
Imaging.
-
IV.
Etiopathogenesis.
-
V.
SSS and craniofacial trauma.
-
VI.
Treatment.
Each of these topics are described below.
Epidemiology
Silent Sinus Syndrome is a rare, but probably underdiagnosed, entity and data of its prevalence are still lacking [16].
An higher frequency in adult age is reported, between the 3rd and the 5th decade [17], although some pediatric cases are also reported [18–24].
Still today, no risk factor has been associated to SSS [25].
Sivrice et al. [8] estimated a prevalence of 0.92% for CMA, and of 0.11% for SSS.
D’Agostino et al. [26] found a prevalence of 6.17% for CMA and of 0.56% for SSS.
In conclusion, the exact prevalence of SSS isn’t still known, even if several cases report have been reported in literature [27–34], about 150 [35]. A CMA has even been find out under the wrappings of an Egyptian mummy [36].
Approximatively, the prevalence of CMA can be estimated about 0.9–6% while that one of SSS about 0.1–0.5%.
Clinical Presentation
Generally, patients with SSS first contact the ophthalmologist practitioner [37, 38]. Furthermore, the term “silent” just refers to the development of SSS which is totally without symptoms. However, in advanced cases, patients with SSS present evident facial deformities, as orbital asymmetry, enophthalmos and/or hypoglobus, sinking of the upper palpebral sulcus, palpebral retraction, and palpebral delay in the downward gaze [39].
Sometimes it’s possible to observe a “pseudopneumoortbita”, described as air trapped under the superior eyelid which gives the appearance of “air into the orbit” in CT scans [40].
Facial depression of the suborbital cutaneous area [41], laughter-induced transient vision loss [42], headache [43] and ipsilateral upper alveolar numbness [44] have been described too.
It’s known that modifications of the sinus wall and the orbital floor involve slowly and progressively and develop over years after the ostiomeatal obstruction but, sometimes, sinus collapse can be quickly progressive, so that signs and symptoms of SSS occur quickly since a known cause of an ostiomeatal obstruction [45], and some authors [46, 47] have described cases of SSS arises with acute diplopia.
Imaging
Although suspect of SSS is clinical, its confirmation must be based on radiology [48].
CT scan is considered the gold standard for diagnosis of SSS. Generally, Multi Detector Computed Tomography (MDCT) is required, however, the Cone-Beam Computed Tomography (CBCT) can produce images with sufficient high resolution but with much lower radiation burden (200–1200 μSv vs. 30 μSv) [49].
Radiographic signs of Silent Sinus Syndrome are pathognomonic [5, 50]:
Occlusion of the ethmoidal infundibulum,
Lateral retraction of the uncinate process,
Increase of orbital floor inward concavity,
Opacification of the antrum cavity,
Septal deviation to the affected maxillary sinus,
Decrease of the maxillary sinus volume,
Increase of the orbital cavity volume,
Enophthalmos and/or hypoglobus.
Opacification of the maxillary sinus cannot be considered a pathognomonic sign of SSS, because it is also present in several other sinus pathologies (for example odontogenic sinusitis) but it’s considered a consistent of SSS, as it’s present in almost all cases. However, several cases of SSS without opacification of the maxillary sinus are also reported [17, 51–53].
Both CT and MRI allow to obtain the diagnosis of SSS [54]. Observing the coronal plane, it is possible to recognize maxillary sinus atelectasis, orbital floor depression and the opacification of the antrum. However, CT-scan is considered the gold standard within the radiological exams for diagnosis of CMA/SSS [55].
Finally, SSS is a monolateral pathology but sporadic cases (about 5–6 cases) of bilateral SSS have been described [56–60] also as metachronous presentation [61].
Etiopathogenesis
The acquired obstruction of the ostiomeatal complex of Higmoro antrum is the primum movens for the onset of SSS. The obstruction results in an hypoventilation and a negative pressure into the sinus [43]. Although a chronic inflammatory process, consequent to mucosal stagnation, is inevitably present, pathogenesis of SSS is more likely due to anatomical/mechanical factors [62].
Kass et al. [63] measured the manometric pressures present into the antrum of patients affected by SSS finding an average value of − 8.4 ± 2.6 cmH2O, while the normal pressure should be isobaric.
SSS has also been associated to IgG4-related orbitopathy [64], to a mass in the deep masticatory space [65] and to a Small Lymphocytic Lymphoma [66].
SSS and Craniofacial Trauma
The traditional definition of SSS exclude the presence of a prior craniofacial trauma and/or sinus surgery. However, in literature, there are several cases report compatible with a diagnosis of SSS except for a previous trauma [67], so the recent literature suggests the possibility to include them into the traditional SSS [68–73].
Treatment
The treatment of SSS has two goals. The first is to restore the maxillary sinus aeration, the second aim is to recover the orbital architecture [74].
The ventilation of the maxillary sinus can be achieved endoscopically creating a rhinoantral access. In many cases, the orbital floor resumes spontaneously its original position as a result of the only aeration of the antrum [74] while sometimes the sinus antrostomy is not sufficient and becomes necessary an orbital floor surgical restoration [75, 76].
Some authors suggest to performe simultaneously the antrostomy and the orbital floor restoration [77, 78], others suggest to perform them deferring but some authors believe that, after antrostomy, there should be an observation period between 2 and 6 months before to procede with the correction of the orbital floor [79].
The gold standard for sinus access is FESS (Functional Endoscopic Sinus Surgery) with or without orbital floor reconstruction [80–82].
However, both the necessity and the timing of orbital surgery are debatable. There are three options: (1) FESS with simultaneous orbital reconstruction, (2) FESS with orbital reconstruction delayed of 2–6 months, and (3) FESS without orbital surgery [83].
Unconventional surgical procedures have also been described, for example it has been reported a case of SSS treated with balloon sinuplasty technique [84], or using a modified Foley catheter introduced into the pathological sinus and inflated [85], or with custom made prosthesis [86], or with HAG (Hyaluronic Acid Gel) intraorbital injection in extraconal position [87, 88], or by neuronavigation [89].
Our Experience
We present two explicative clinical cases, on 64 examined, on beyond 400 cases of orbital floor operated in the last 10 years.
Case 1
I.T., 34 year-old-man, white. He was involved in a motorcycle accident on 25th January 2020. After the impact, he was rescued by the passersby and suddenly conducted to G. Martino Hospital of Messina (Italy) where he underwent a Craniofacial CT scan.
The radiological examination denied the presence of brain lesion but proved the presence of multifragmentary fracture of the nasal bones, a fracture of the nasal septum, of the anterior, lateral and medial walls of the left maxillary sinus, of the left medial pteryogoid process and of the left orbital floor. It revealed, also, a plurifocal fracture of the left lamina papyracea and a fracture of the inferior orbital frame extended to the ascendent branch of the maxilla.
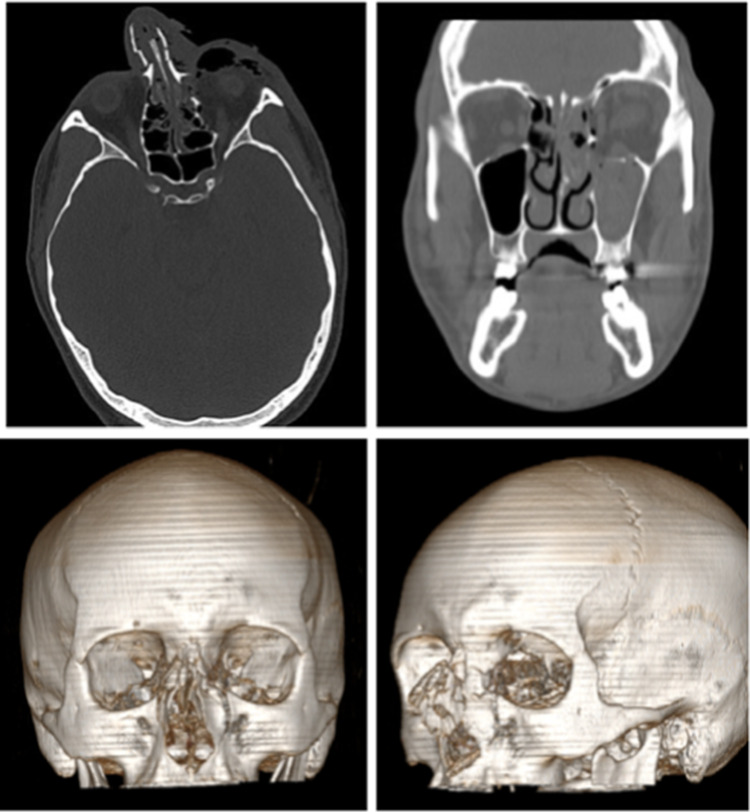
In Fig. 1 are reported an axial and a frontal scans and a 3-D reconstruction of the immediate post-traumatic event. In these images it’s possible to note that the volume of the maxillary sinus and of the orbital cavity involved are totally comparable to the contralateral ones, and no difference within right and left side of the skull is evident in the 3-D reconstruction too.
Fig. 1.
Axial and frontal scan and 3-D reconstruction of immediate post-traumatic event
The patient underwent surgery 4 days after the admission. Surgery was performed under general anesthesia and, through a subciliary approach, the fracture of the orbital frame was restored and a thin matrix of alloplastic material (Medpor, microporous polyethylene high-density) was placed above the collapsed orbital floor.
The fracture of the inferior orbital frame was fixed by a 5-hole microplate and four screws of 5 mm length.
The patient was discharged 7 days and no complication occurred during the first post-operative period.
The patient hadn’t any kind of complaint for the next 3 years until, in December 2022, he came back to our clinic reported a vertical and horizontal diplopia.
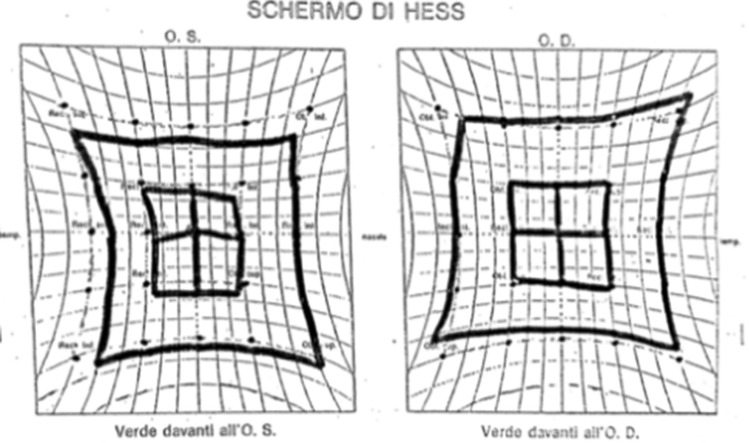
The patient underwent orthotic evaluation with Hess-Lancaster test (Fig. 2). The test proved the presence of a latent hypotropia and esotropia, indeed, the patient presented a diplopia looking up and towards the left side.
Fig. 2.
Hess-Lancaster test performed on December 2022
Our first hypothesis was that a dislocation of the titanium plate placed in January 2020 occured, so the patient underwent a Craniofacial CT-scan.
However, no dislocation of the titanium plate was reported in the images, but they clearly showed a reduction of left maxillary sinus volume and an increase of the ipsilateral orbital cavity volume.
The left antrum was totally obliterated by hyperdense tissue until the ostioinfundibular region; the ostiomeatal complex was flared and inverted, while the infundibulum appeared medially retracted. The left orbital floor was deflected on the sinus side with a concave upper profile.
The inferior rectus muscle was stretched downwards and verticalized, with prevalence of the longitudinal axis (7–8 mm) in comparison to the transverse axis (6 mm).
Observing the patient from the submental view (Fig. 3), enophthalmos of the left eye was quite evident while, observing him from the frontal view, the hypoglobus and down dislocation of the ipsilateral globe were unequivocal. However, any alteration was evident in the 3-D reconstruction.
Fig. 3.
December 2022 CT-scan: enophthalmos, hypoglobus and globes asymmetry
All the findings described seem to be an expression of a “silent sinus syndrome”, as was reported by the radiologist.
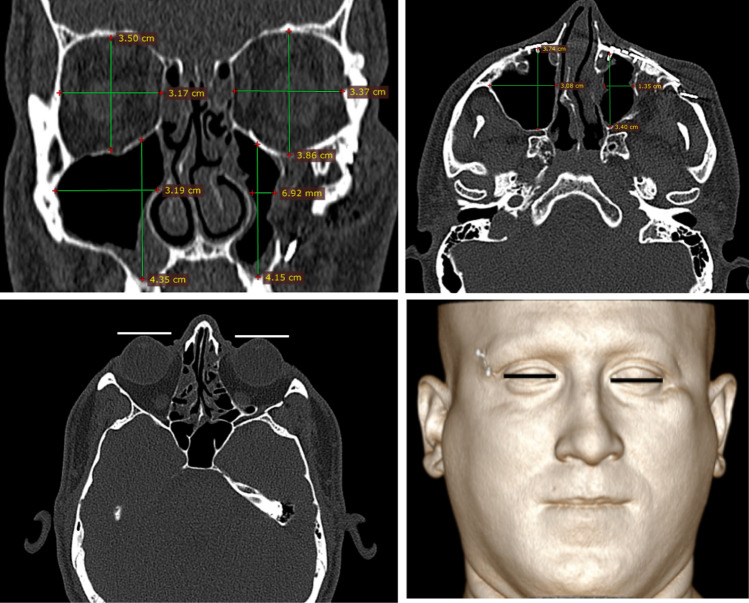
In Fig. 4 are reported the measures of the two orbital cavities and the two maxillary sinuses. It’s evident that the difference between the sagittal axis of the right and the left sinus is 7.4 mm (2.63 cm the right antrum and 1.89 cm the left one), the difference between the transversal axis of the two sinuses is 1.8 mm (2.63 cm the right antrum and 2.47 cm the left one).
Fig. 4.
CT-scan of December 2022 with the measures of the antra and of the orbital cavities volume
Both the measures have been taken in the CT-scan slide in which the volume of the orbital cavities appeared greater.
In the same slide we measured the difference between the sagittal and the transversal axis of the right and left orbital cavity.
The difference between the left and the right sagittal axis of the orbital cavities is 7.6 mm (4.06 cm the left orbital cavity and 3.30 cm the right one), the difference between the transversal axis of the two orbital cavities is 5.4 mm (3.86 cm the left orbital cavity and 3.32 cm the right one).
We also measured the depth and the width of the antra on the axial view, considering the slide in which the two maxillary sinuses appeared greatest. The difference between the depth of the two sinuses is 2.4 mm (3.19 cm the depth of the right sinus and 2.95 cm the left one), while the difference between the width of the two sinuses is 2.1 mm (2.68 cm the width of the right sinus and 2.47 cm the left one).
After that, we measured the retrusion of the left eye, choosing the slide in which both the corneas were free from the superior eyelid. We drawn a line tangent to the most anterior point of the left and the right cornea and we measured the distance between the two lines, that is 5.62 mm, that is the measure of the left eye retrusion.
Another measure that we believed useful was the distance between the anterior wall of the maxillary sinuses and the cutaneous surface, that are 1.12 cm on the right and 1.19 cm on the left. This means that the anterior wall of the left sinus is further back of 7 mm in comparison to the left one.
Analyzing the pre-operative CT-scan we confirmed that the volume of the maxillary sinuses and of the orbital cavities of the patient were quite normal in 2020. As we can see in Fig. 1 there were any difference between the two sides of the orbital cavity and of the maxillary sinus.
Case 2
D.C., 37 years old, caucasian man. He was victim of a road accident in February 2014, when he was only 17 years old. In the incident he reported multiple fractures of the face, involving both the lower and the middle face.
The patient underwent urgent surgery during which the anatomy of the facial skull was well reconstructed (Fig. 5).
Fig. 5.
3-D reconstruction of the facial skull of patient that shows the presence of plate and screws
The patient was completely free of symptoms for almost 10 years, when he came back to our clinic in May 2023 referring a persistent vertical diplopia arises in the last 2 months.
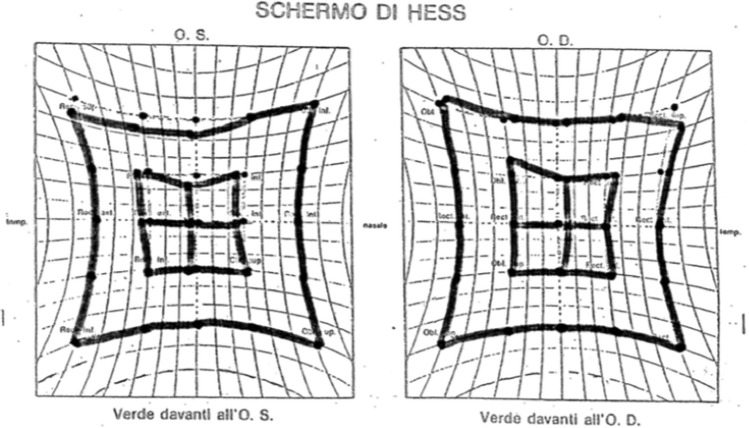
The Hess-Lancaster test (Fig. 6), performed in the same May 2023, proved a mild hypotropia of the left eye.
Fig. 6.
Hess-Lancaster test performed in May 2023
A few days later the patient underwent a CT-scan of the facial skull that proved a reduction of the volume of the left antrum, above all in its transversal diameter, just 6.92 mm in comparison to 3.19 cm of the contralateral one (Fig. 7) while the vertical diameter was quite preserved (4.15 vs. 4.35 of the contralateral one). The CT-scan proved also an increase of the volume of the left orbital cavity whose vertical diameter was 36 mm greater in comparison to the contralateral one (3.86 cm the left orbit and 3.50 the right one) and the horizontal diameter was 20 mm greater (3.37 cm the left in comparison to 3.17 of the right one). Observing the patient in frontal view, it’s possible to note an asymmetry of the eyes position with an evident downward position of the left globe, while the CT-scan showed, in the axial view, a retroposition of the eye.
Fig. 7.
CT-scan of May 2023
Discussion
In this work we would express the opinion that the same condition of ostiomeatal infundibulum obstruction can be idiopathic or induced by other causes, as trauma involving the nasal cavity, the orbit or, more generally, the middle face, with a clinical presentation similar to the idiopathic ones. Today they are out of diagnostic criteria of SSS but, in our opinion, they are the most frequent.
Conclusions
Based on that just exposed, we propose to keep separate the conditions of idiopathic CMA from those with previous trauma associated. We propose to continue to identify the idiopathic ones as silent sinus syndrome but to consider all the secondary cases as “Catalfamo-De Rinaldis Syndrome” (CDR Syndrome) if the following criteria are present:
Diplopia and/or evident globe eyes asymmetries.
Increase of horizontal and/or vertical diameters of the orbital cavity, in comparison to contralateral one, measured on the slide of a CT-scan in which the two cavities appeared greatest.
Reduction of horizontal and/or vertical diameters of the maxillary sinus, in comparison to contralateral one, measured on the slide of a CT-scan in which the two cavities appeared greatest.
Previous trauma involving the middle face bones.
Funding
This research received no funding grant from any funding agency in the public or commercial sectors.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Montgomery WW. Mucocele of the maxillary sinus causing enophthalmus. Eye Ear Nose Throat Mon. 1964;43:41–44. [PubMed] [Google Scholar]
- 2.Soparkar CN, Patrinely JR, Cuaycong MJ, Dailey RA, Kersten RC, Rubin PA, Linberg JV, Howard GR, Donovan DT, Matoba AY, Holds JB. The silent sinus syndrome. A cause of spontaneous enophthalmos. Ophthalmology. 1994;101(4):772–778. doi: 10.1016/s0161-6420(94)31267-x. [DOI] [PubMed] [Google Scholar]
- 3.Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology. 2020;58(Suppl S29):1–464. doi: 10.4193/Rhin20.600. [DOI] [PubMed] [Google Scholar]
- 4.Guillen DE, Pinargote PM, Guarderas JC. The silent sinus syndrome: protean manifestations of a rare upper respiratory disorder revisited. Clin Mol Allergy. 2013;11(1):5. doi: 10.1186/1476-7961-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Monis PL, Parikh MH, Bhowmick H, Pai K, Shetty S, Salins PC. Silent sinus syndrome: a case of sinking eyeball. J Maxillofac Oral Surg. 2021;20(4):577–580. doi: 10.1007/s12663-019-01262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kass ES, Salman S, Rubin PA, Weber AL, Montgomery WW. Chronic maxillary atelectasis. Ann Otol Rhinol Laryngol. 1997;106(2):109–112. doi: 10.1177/000348949710600204. [DOI] [PubMed] [Google Scholar]
- 7.de Dorlodot C, Collet S, Rombaux P, Horoi M, Hassid S, Eloy P. Chronic maxillary atelectasis and silent sinus syndrome: two faces of the same clinical entity. Eur Arch Otorhinolaryngol. 2017;274(9):3367–3373. doi: 10.1007/s00405-017-4622-8. [DOI] [PubMed] [Google Scholar]
- 8.Sivrice ME, Yasan H, Okur N, Okur E, Buyukcelik B, Kumbul YC. Prevalence of chronic maxillary atelectasis: a radiological study. J Larongol Otol. 2022;136(12):1240–1244. doi: 10.1017/S0022215122000056. [DOI] [PubMed] [Google Scholar]
- 9.Brandt MG, Wright ED. The silent sinus syndrome is a form of chronic maxillary atelectasis: a systematic review of all reported cases. Am J Rhinol. 2008;22(1):68–73. doi: 10.1017/S0022215122000056. [DOI] [PubMed] [Google Scholar]
- 10.Mangussi-Gomes J, Nakanishi M, Chalita MR, Damasco F, De Oliveira CA. Stage II chronic maxillary atelectasis associated with subclinical visual field defect. Int Arch Otorhinolaryngol. 2013;17(4):409–412. doi: 10.1055/s-0033-1351679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mc Ardle B, Perry C. Ethmoid silent sinus syndrome causing inward displacement of the orbit: case report. J Laryngol Otol. 2010;124(2):206–208. doi: 10.1017/S0022215109990521. [DOI] [PubMed] [Google Scholar]
- 12.Brown SJ, McNab AA. Ethmoid silent sinus syndrome following orbital trauma. Ophthalmic Plast Reconstr Surg. 2017;33(3):e60–e61. doi: 10.1097/IOP.0000000000000746. [DOI] [PubMed] [Google Scholar]
- 13.Naik RM, Khemani S, Saleh HA. Frontal silent sinus syndrome. Otolaringol Head Neck Surg. 2013;148(2):354–355. doi: 10.1177/0194599812466646. [DOI] [PubMed] [Google Scholar]
- 14.Ersan M, Özdemir A, Gultam SM. Silent sinus syndrome after rhinoplastic: a case report. Case Reports Plast Surg Hand Surg. 2020;7(1):73–79. doi: 10.1080/23320885.2020.1788947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ribeiro SPP, Loureiro RM, Gil JM, Dutra DL, Gomes RLE, Daniel MM. Ethmoidal silent sinus syndrome after nasal swab test. Neuroradiology. 2022;64(1):205–207. doi: 10.1007/s00234-021-02856-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Magalhães C, Baptista M, Lopes G, Duarte D. Silent sinus syndrome: an underdiagnosed entity. BMJ Case Rep. 2015 doi: 10.1136/bcr-2015-210548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee DS, Murr AH, Kersten RC, Pletcher SD. Silent sinus syndrome without opacification of ipsilateral maxillary sinus. Laryngoscope. 2018;128(9):2004–2007. doi: 10.1002/lary.27108. [DOI] [PubMed] [Google Scholar]
- 18.Chang DT, Truong MT. A child with silent sinus syndrome and spontaneous improvement after sinus surgery. Int J Pediatr Otorhinolaryngol. 2014;78(11):1993–1995. doi: 10.1016/j.ijporl.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Leidens N, Franco A, Santos MCJ, Makeeva IM, Fernandes A. Early-diagnosed silent sinus syndrome and cone-beam computed tomography in a pediatric patient: a case report. J Korean Assoc Oral Maxillofac Surg. 2020;46(2):155–159. doi: 10.5125/jkaoms.2020.46.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosa F, Figueirinhas R, Oliveira J, Sousa CAE. Silent sinus syndrome in children. Acta Otorrinolaringol Esp (Engl Ed) 2018;69(1):51–52. doi: 10.1016/j.otorri.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Sen D, Arora V, Adlakha S, Miglani H. The imploding antrum: an unusual case of nontraumatic painless enophthalmos. Indian J Ophthalmol. 2016;64(10):786–788. doi: 10.4103/0301-4738.195015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Freiser ME, McCoy J, Shaffer AD, Stapleton AL. Silent sinus syndrome in children. Int J Pediatr Otorhinolaryngol. 2020;134:110034. doi: 10.1016/j.ijporl.2020.110034. [DOI] [PubMed] [Google Scholar]
- 23.Petraroli M, Riscassi S, Panigari A, Maltese M, Esposito S. Silent sinus syndrome and williams syndrome: two rare diseases found in a pediatric patient. Front Pediatr. 2020;8:211. doi: 10.3389/fped.2020.00211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou S, Duncan K, Stefko ST. Nonhealing orbital floor fracture in a pediatric patient: a unique presentation of pseudo-silent sinus syndrome. Orbit. 2018;37(5):375–377. doi: 10.1080/01676830.2017.1423347. [DOI] [PubMed] [Google Scholar]
- 25.Sheikhi M, Faranak J. The silent sinus syndrome. Dent Res J (Isfahan) 2013;10(2):264–267. doi: 10.4103/1735-3327.113369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.D’Agostino Fiorenza U, Spoldi C, Nekrasova L, Pipolo C, Lozza P, Scotti A, Maccari A, Felisati G, Saibene AM. Prevalence of maxillary sinus hypoplasia and silent sinus syndrome: a radiological cross-sectional retrospective cohort study. Am J Rhinol Allergy. 2022;36(1):123–128. doi: 10.1177/19458924211029418. [DOI] [PubMed] [Google Scholar]
- 27.Le GK. Case report: a rare case of silent sinus syndrome and vertical diplopia. Optom Vis Sci. 2020;97(7):485–488. doi: 10.1097/OPX.0000000000001539. [DOI] [PubMed] [Google Scholar]
- 28.Chavez-Montoya R, Araujo-Ramìrez O, Castillo-Lòpez IY, Govea-Camacho LH. Síndrome de implosión maxilar: tres casos y sus diferentes abordajes de tratamiento. Cirugía Cirujanos. 2017;85(6):529–534. doi: 10.1016/j.circir.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Varas G, Dolman PJ. Maxillary sinus wall thickening in silent sinus syndrome. JAMA Ophtalmol. 2017;135(5):e170637. doi: 10.1001/jamaophthalmol.2017.0637. [DOI] [PubMed] [Google Scholar]
- 30.Gaffuri M, di Furia D, Battilocchi L, Torretta S, Accorona R, Pignataro L. Unilateral silent sinus syndrome: a case report. Clin Case Rep. 2022;10(6):e05794. doi: 10.1002/ccr3.5794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gan WL. Silent sinus syndrome as a recognised cause of unilateral painless enophthalmos. BMJ Case Rep. 2014 doi: 10.1136/bcr-2014-203954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eisa N, Alraiyes AH, Alraies MC. Facial asymmetry: silent sinus syndrome. BMJ Case Rep. 2013 doi: 10.1136/bcr-2013-010377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bouchenna W, Delbarre M, Morfeq H, Audren F, Jani B, Froussart-Maille F. A rare cause of enophthalmos: silent sinus syndrome. J Fr Ophtalmol. 2020;43(10):e371–e374. doi: 10.1016/j.jfo.2020.05.007. [DOI] [PubMed] [Google Scholar]
- 34.Dumitrescu D, Fănuţă B, Stepan AE, Fronie AI, Dumitrescu CI, Mârţu MC, Şurlin P, Şurlin V, Popescu Silent sinus syndrome–report of a case. Rom J Morphol Embryol. 2015;56(1):229–237. [PubMed] [Google Scholar]
- 35.Jovančevic L, Čanadanović V, Savović S, Zvezdin B, Komazec Z. Silent sinus syndrome: One more reason for an ophthalmologist to have a rhinologist as a good friend. Vojnosanit Pregl. 2017;74(1):59–63. doi: 10.2298/VSP141118141J. [DOI] [PubMed] [Google Scholar]
- 36.Michailidis G, Kyriazi S, Maravelia A, Tourna E, Couvaris CM, Kalampoukas K, Pantazis I, Lazaris P, Geroulanos S, Kalogerakou K, Bontozoglou N. Chronic maxillary atelectasis under the wrappings of an Egyptian mummy. Ann Otol Rhinol Laryngol. 2019;128(12):1165–1169. doi: 10.1177/0003489419879716. [DOI] [PubMed] [Google Scholar]
- 37.Keren S, Sinclair V, Mc Callum E, Martinez-Devesa P, Norris JH. Silent sinus syndrome: potentially misleading features that should be recognized. Can J Ophthalmol. 2023;58(2):113–117. doi: 10.1016/j.jcjo.2021.09.018. [DOI] [PubMed] [Google Scholar]
- 38.Albadr FB. Silent sinus syndrome: interesting computed tomography and magnetic resonance imaging findings. J Clin Imaging Sci. 2020;10:38. doi: 10.25259/JCIS_62_2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gòmez L, Fontàn E, Leòn JC, Garrido J. Silent sinus syndrome. Clinical case. Arch Soc Esp Oftalmol. 2014;89(3):121–123. doi: 10.1016/j.oftal.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 40.Rullan-Oliver B, Del Toro-Diez E, Portela-Arraiza JC. Natural progression of bilateral maxillary silent sinus syndrome: a metachronous case report. SAGE Open Med Case Rep. 2020 doi: 10.1177/2050313X20902339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lim BW, Jung JH, Kim ST, Kim DH, Park JW, Cha HE, Kang IG. Autologous fat injection for the correction of facial depression resulting from silent sinus syndrome. J Craniofacial Surg. 2019;30(3):e191–e192. doi: 10.1097/SCS.0000000000005058. [DOI] [PubMed] [Google Scholar]
- 42.Reggie SN, Kalyam K, Holds JB, Chung SM. Laughter-induced transient vision loss in a patient with silent sinus syndrome. J Neuroophthalmol. 2018;38(1):30–31. doi: 10.1097/WNO.0000000000000536. [DOI] [PubMed] [Google Scholar]
- 43.Ferro A, Basyuni S, Santhanam V. Not so silent sinus syndrome: a case report. Int J Surg Case Rep. 2016;23:1–3. doi: 10.1016/j.ijscr.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lau HT, Lim KH. Isolated unilateral upper alveolar numbness in silent sinus syndrome. BMJ Case Rep. 2017 doi: 10.1136/bcr-2017-219322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jacobs JM, Chou EL, Tagg NT. Rapid remodeling of the maxillary sinus in silent sinus syndrome. Orbit. 2019;38(2):166–168. doi: 10.1080/01676830.2018.1473450. [DOI] [PubMed] [Google Scholar]
- 46.Singman EL, Matta NS, Silbert DI. Silent sinus syndrome presenting after a roller coaster ride: a case report. J Fr Ophtalmol. 2020;43(10):e371–e374. doi: 10.1016/j.jfo.2020.05.007. [DOI] [PubMed] [Google Scholar]
- 47.Saffra N, Rakhamimov A, Saint-Louis LA, Wolintz RJ. Acute diplopia as the presenting sign of silent sinus syndrome. Ophthalmic Plast Reconstr Surg. 2013;29(5):e130–e131. doi: 10.1097/IOP.0b013e31827bda92. [DOI] [PubMed] [Google Scholar]
- 48.AlSaloom NS, Ashri NY. Silent sinus syndrome (first case report, Saudi Arabia with recommendation) Int J Surg Case Rep. 2020;74:104–108. doi: 10.1016/j.ijscr.2020.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Manila NG, Tahmasbi Arashlow M, Elhers S, Liang H, Nair MK. Cone-beam computed tomography imaging of silent sinus syndrome: a case series and a literature review. Imaging Sci Dent. 2020;50(4):365–371. doi: 10.5624/isd.2020.50.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Martìnez-Capoccioni G, Varela-Martìnez E, Martìn-Martìn C. Silent sinus syndrome an acquired condition and the essential role of otorhinolaryngologist consultation: a retrospective study. Eur Arch Otorhinolaryngol. 2016;273(10):3183–3188. doi: 10.1007/s00405-016-3965-x. [DOI] [PubMed] [Google Scholar]
- 51.Hunt SM, Tami TA. Sinusitis-induced enophthalmos: the silent sinus syndrome. Ear Nose Throat J. 2020;79(8):579–581. [PubMed] [Google Scholar]
- 52.Stryjewska-Makuch G, Kokoszka M, Goroszkiewicz K, Karlowska-Bijak, Kolebacz B, Misiolek M. What may surprise a rhinologist in everyday clinical practice: silent sinus syndrome or pneumosinus dilatans/pneumocele? Literature review and own experience. Eur Arch Oto-Rhino-Laryngol. 2023;280(2):519–527. doi: 10.1007/s00405-022-07697-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Serindere G, Belgin CA. An evaluation of the relationship between maxillary sinus anterior wall depression and maxillary sinus opacity by computed tomography and panoramic radiography. Oral Radiol. 2020;36(4):383–388. doi: 10.1007/s11282-020-00436-z. [DOI] [PubMed] [Google Scholar]
- 54.Eyigör H, Çekiç B, Çoban DT, Selçuk OT, Renda L, Şimşek EH, Yılmaz MD. Is there a correlation between the clinical findings and the radiological findings in chronic maxillary sinus atelectasis? J Craniomaxillofac Surg. 2016;44(7):820–826. doi: 10.1016/j.jcms.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 55.Gaudino S, Di Lella GM, Piludu F, Martucci M, Schiarelli C, Africa E, Salvolini L, Colosimo C. CT and RMI diagnosis of silent sinus syndrome. Radiol Med. 2013;118(2):265–275. doi: 10.1007/s11547-012-0822-x. [DOI] [PubMed] [Google Scholar]
- 56.Vahdani K, Rose GE. Bilateral silent sinus (imploding antrum) syndrome. Ophthalmic Plast Reconstr Surg. 2019;35(3):e67–e69. doi: 10.1097/IOP.0000000000001350. [DOI] [PubMed] [Google Scholar]
- 57.Ho JPK, Wong E, Gunaratne DA, Singh N. Chronic maxillary atelectasis (including silent sinus syndrome) can present bilaterally. J Laryngol Otol. 2019;133(3):251–255. doi: 10.1017/S0022215119000252. [DOI] [PubMed] [Google Scholar]
- 58.Trope M, Schwartz JS, Tajudeen BA, Kennedy DW. Bilateral silent sinus syndrome: a rare case and review of literature. Allergy Rhinol (Providence) 2017;8(2):100–102. doi: 10.2500/ar.2017.8.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shieh W-S, Huggins AB, Rabinowitz MR, Rosen MR, Rabinowitz MP. A case of concurrent silent sinus syndrome, thyroid eye disease, idiopathic orbital inflammatory syndrome, and dacryoadenitis. Orbit. 2017;36(6):462–464. doi: 10.1080/01676830.2017.1337194. [DOI] [PubMed] [Google Scholar]
- 60.Gunaratne DA, Hasan Z, Floros P, Singh N. Bilateral stage I chronic maxillary atelectasis: a case report. Int J Surg Case Rep. 2016;26:53–56. doi: 10.1016/j.ijscr.2016.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Farneti P, Bellusci A, Parmeggiani A, Pasquini E. Metachronous bilateral silent sinus syndrome: a case report. Iran J Otorhinolaryngol. 2020;32(110):175–179. doi: 10.22038/ijorl.2020.42809.2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zheng HD, Mecham JC, Abdel-Aty Y, Lal D, Marino MJ. Microbiology, histopathology, and radiographic findings in silent sinus syndrome. Am J Rhinol Allergy. 2021;35(5):685–692. doi: 10.1177/1945892421989161. [DOI] [PubMed] [Google Scholar]
- 63.Kass ES, Salman S, Montgomery WW. Manometric study of complete ostial occlusion in chronic maxillary atelectasis. Laryngoscope. 1996;106(10):1255–1258. doi: 10.1097/00005537-199610000-00017. [DOI] [PubMed] [Google Scholar]
- 64.Jurkov M, Olze H, Klaushen F, Bertelmann E, Schneider U, Arens P. IgG4-related orbitopathy as an important differential diagnosis of advanced silent sinus syndrome. HNO. 2020;68(11):864–868. doi: 10.1007/s00106-019-00798-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hura N, Ahmed OG, Rowan RN. Atypical presentation of silent sinus syndrome: a case report and literature review. Allergy Rino (Providence) 2020;11:2152656719899928. doi: 10.1177/2152656719899928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Deekonda P, Jones HS. Silent sinus syndrome secondary to lymphoma: an unusual case with radiological evidence of rapid progression. Ann Otol Rhinol Laryngol. 2022;131(8):918–922. doi: 10.1177/00034894211047103. [DOI] [PubMed] [Google Scholar]
- 67.Millis MC. A case of silent sinus syndrome following a history of multiple facial traumas. Clin Exp Optom. 2021;104(2):262–263. doi: 10.1111/cxo.13113. [DOI] [PubMed] [Google Scholar]
- 68.Canzi G, Morganti V, Novelli G, Bozzetti A, Sozzi D. Posttraumatic delayed enophthalmos: analogies with silent sinus syndrome? case report and literature review. Craniomaxillofac Trauma Reconstr. 2015;8(3):251–256. doi: 10.1055/s-0034-1399799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stryjewska-Makuch G, Goroszkiewicz K, Szymocha J, Lisowska G, Misiolek M. Etiology, early diagnosis and proper treatment of silent sinus syndrome based on review of the literature and our experience. J Oral Maxillofac Surg. 2022;80(1):113.e1–118.e8. doi: 10.1016/j.joms.2021.08.166. [DOI] [PubMed] [Google Scholar]
- 70.Araslanova R, Allen L, Rotenberg BW, Sowerby LJ. Silent sinus syndrome after facial trauma: a case report and literature review. Laringoscope. 2017;127(7):1520–1524. doi: 10.1002/lary.26527. [DOI] [PubMed] [Google Scholar]
- 71.Brown SJ, Hardy TG, McNab AA. “Silent sinus syndrome” following orbital trauma: a case series and review of the literature. Ophthalmic Plast Reconstr Surg. 2017;33(3):209–212. doi: 10.1097/IOP.0000000000000713. [DOI] [PubMed] [Google Scholar]
- 72.Rosso C, Saibene AM, Felisati G, Pipolo C. Silent sinus syndrome: systematic review and proposal of definition, diagnosis and management. Acta Otorhinolaryngol Ital. 2022;42(4):305–316. doi: 10.14639/0392-100X-N1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Février E, Vandersteen C, Castillo L, Savoldelli C. Silent sinus syndrome: a traumatic case. J Stomatol Oral Maxillofac Surg. 2017;118(3):187–190. doi: 10.1016/j.jormas.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 74.Cardesìn A, Escamilla Y, Romera M, Molina JA. Single surgical step for endoscopic surgery and orbital reconstruction of a silent sinus syndrome. Acta Otorrinolaringol Esp. 2013;64(4):297–299. doi: 10.1016/j.otorri.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 75.Wladis EJ, Kersten RC, Vagefi MR, Pinheiro-Neto C, Schinder R, Kim J. Clinical features and outcomes of post-traumatic silent sinus syndrome. Ophthalmic Plast Reconstr Surg. 2018;34(4):378–380. doi: 10.1097/IOP.0000000000001025. [DOI] [PubMed] [Google Scholar]
- 76.Lin GC, Sedaghat AR, Bleier BS, Holbrook EH, Busaba NY, Yoon MK, Gray ST. Volumetric analysis of chronic maxillary atelectasis. Am J Rhinol Allergy. 2015;29(3):166–169. doi: 10.2500/ajra.2013.27.4173. [DOI] [PubMed] [Google Scholar]
- 77.Claròs P, Sobolewska AZ, Cardesa A, Lopez-Fortuny M, Claros A. Silent sinus syndrome: combined sinus surgery and orbital reconstruction—report of 15 cases. Acta Otolaryngol. 2019;139(1):64–69. doi: 10.1080/00016489.2018.1542161. [DOI] [PubMed] [Google Scholar]
- 78.Tieghi R, Malagutti N, Valente L, Carnevali G, Clauser LC. Combined endoscopic and trans palpebral orbital reconstruction for silent sinus syndrome. J Craniofac Surg. 2017;28(4):955–958. doi: 10.1097/SCS.0000000000003421. [DOI] [PubMed] [Google Scholar]
- 79.Kram YA, Pletcher SD. Maxillary sinus posterior wall remodeling following surgery for silent sinus syndrome. Am J Otolaryngol. 2014;35(5):623–625. doi: 10.1016/j.amjoto.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 80.Hernaiz-Leonardo JC, Alqunaee M, Moghimi S, Alim BM, Javadian F, Vafaei-Nodeh S, Pascual A, Javer A. Maxillary sinus volume changes after functional endoscopic sinus surgery in patients with chronic maxillary atelectasis and silent sinus syndrome. Int Forum Allergy Rhinol. 2022;12(9):1212–1215. doi: 10.1002/alr.22985. [DOI] [PubMed] [Google Scholar]
- 81.Kim S-H. Successful treatment of silent sinus syndrome with combined endoscopic sinus surgery and blepharoplasty without orbital floor reconstruction. J Craniofac Surg. 2016;27(6):e586–e588. doi: 10.1097/SCS.0000000000002998. [DOI] [PubMed] [Google Scholar]
- 82.Mantsopoulos K, Thimsen V, Karkos P, Sievert M, Hiro H, Constantinidis J. Silent sinus syndrome: reduction of surgical invasiveness in an underdiagnosed clinical entity. Am J Otolaryngol. 2022;43(5):103541. doi: 10.1016/j.amjoto.2022.103541. [DOI] [PubMed] [Google Scholar]
- 83.Bhalla N, Rosenstein J, Dym H. Silent sinus syndrome: interesting clinical and radiologic findings. J Oral Maxillofac Surg. 2019;77(10):2040–2043. doi: 10.1016/j.joms.2019.03.042. [DOI] [PubMed] [Google Scholar]
- 84.Kilty SJ. Maxillary sinus atelectasis (silent sinus syndrome): treatment with ballon sinuplasty. J Laryngol Otol. 2014;128(2):189–191. doi: 10.1017/S0022215113003538. [DOI] [PubMed] [Google Scholar]
- 85.Kashima T, Goldberg RA, Kohn JC, Rootman DB. One-stage bone strip reconstruction technique with balloon sinus dilatation surgery for chronic maxillary atelectasis. Clin Ophthalmol. 2016;10:2363–2368. doi: 10.2147/OPTH.S103809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Baig MZ, Weber JF, Bhora F, Al Shetawi AH. Surgical advances in the management of the silent sinus syndrome: our experience and review of the literature. J Oral Maxillofac Surg. 2020;78(12):2289–2295. doi: 10.1016/j.joms.2020.07.026. [DOI] [PubMed] [Google Scholar]
- 87.Mavrikakis I, Detorakis ET, Yiotakis I, Kandiloros D. Nonsurgical management of silent sinus syndrome with hyaluronic acid gel. Ophthalmic Plast Reconstr Surg. 2012;28(1):e6–7. doi: 10.1097/IOP.0b013e31820d8840. [DOI] [PubMed] [Google Scholar]
- 88.Grusha Y, Khrovin V, Stoyukhina A, Sheptulin V. Hyaluronic acid gel re-injection for enophthalmos correction in silent sinus syndrome. Orbit. 2015;34(6):351–353. doi: 10.3109/01676830.2015.1078376. [DOI] [PubMed] [Google Scholar]
- 89.Chariba I, Lazard DS, Sain-Oulhen C, Lecanu JB. Correlation between the rate of asymmetry volume of maxillary sinuses and clinical symptomatology in the silent sinus syndrome: a retrospective study about 13 cases. Rev Laryngol Otol Rhinol (Bord) 2014;135(4–5):197–200. [PubMed] [Google Scholar]