Abstract
Objective. To analyse the result of endoscopic endonasal dacryocystrhinostomy with or without preservation of nasal mucosal flap. Study design. Randomised prospective cohort design. Setting. Tertiary academic centre. Subjects and Methods. 100 patients who presented with epiphora and diagnosed as chronic dacryocystitis after syringing by ophthalmologist, were selected and randomised into two groups. Standard surgical procedure of endoscopic endonasal dacryocystorhinostomy was carried out except for the preservation of flap in group A and without preservation of flap in group B. Additional surgeries were done according to necessity. Postoperatively, patients were followed up on OPD-basis at the end of 1st week, 2nd week, 1st month, and 3rd month. Symptomatic improvement was assessed and patency checked by syringing by the ophthalmologist. Results. Nil intraoperative complications (p < 0.05) and nil postoperative complication noted (p < 0.05). Functional and anatomical patency found to be 100% at the end of 1st week in both groups, 96% at 3rd month in case group A and 98%, 92% and 82% respectively at the end of 2nd week, 1st month and 3rd month in group B. Nasal endoscopy of all surgical failures showed restenosis in both groups and synechiae in 2 patients in group B. Conclusions: Preservation of nasal mucosal flap with modification around stoma can be used to cover the bared bone with avoidance of granulation tissue formation reducing the risk of closure of ostium with large rhinostomy and improve success of endoscopic endonasal DCR.
Keywords: Dacryocystorhinostomy
Introduction
Anastomosis of the nasal mucosa and lacrimal sac in endonasal DCR can replicate external DCR closely [1–4]. Creation of U-shaped [2–4], Lshaped nasal mucosal flap [5], free nasal mucosal flap [6] and preservation of whole nasal mucosal flap appositing to lacrimal sac [7] were tried in the past. Exposure of bare bone at the end of surgical procedure might evoke granulation and scar formation and creation of a large bony ostium is necessitated by the increased risk of failure, if inadequate bony removal is attempted. For which, extensive removal of the frontal process of the maxilla is required. Central part of the flap is lost in the technique of U-shaped and L-shaped nasal mucosal flap, and wide area of bare bone resulted. Furthermore, the left behind flap, being small might tear and lost. Durvasula and Gatland reported that the formation of granulation tissue may be caused by the bare bone [8]. Free mucosal flap over the bare bone was tried by Mahendran et al. [6], but found it to be time-consuming,and factors like flap mobility and survival of free flap on the bared bone were stressed. Hence the present study was done to evaluate the benefit of preservation of nasal mucosal flap with modification around stoma site and its impact on success rate.
.
Materials and Methods
This randomised prospective cohort study was performed at the Department of Otorhinolaryngology and Head and Neck, Gandhi Medical College and Hamidia Hospital, Bhopal, India, ( November 2015 to December 2017). Ethical approval was obtained from the Institutional Review Board and informed consent was obtained from all subjects. A total of 100 patients, belonging to both sex groups with clinical evidence of epiphora with nasolacrimal duct obstruction on syringing, diagnosed as chronic dacryocystitis were included in the study. Patients with absent upper and lower punctum, previous lacrimal surgery, eyelid malposition including ectropion or entropion, and previous facial fractures and those not giving consent for endonasal DCR were excluded from the study.Endoscopic examination of nasal cavities was done for any nasal pathology especially mucosal disease, hypertrophied middle turbinate, deviated nasal septum.
Surgical Technique
Patients were hospitalized 1 day prior to surgery. Antibiotic eye drops and nasal decongestents (xylometazoline) were administered. Before surgery, all patients were randomly divided into two groups.Surgical procedure was done under general anaesthesia in a slightly reversed Trendelenburg position (30°), along with decongestion of nasal mucosa with cotton pledgets placed in nasal cavity soaked in xylocaine 4% with adrenaline(1:30,000) for 10 min. Nasal cavities were examined by 0° endoscope(4 mm diameter,18 cm length).When septal and middle turbinate anatomical varients blocking access to lacrimal sac were present, such as deviation /spurs or concha bullosa, they underwent correction to get good operative field. The lateral nasal wall just anterior to the middle turbinate was injected with 2% Xylocaine with 1:1,00,000 adrenaline. A incision was given, about 5-10 mm anterior to attachment of middle turbinate with insulated microear surgical ball probe using monopolar diathermy (Fig. 1) and inferiorly based flap was elevated gently using a suction elevator. In cases where, prominent agger nasi was encountered, it was opened. Frontal process of maxilla (Fig. 2), was nibbled out with straight and curved Smith- Kerrison’s punch forceps along with frontal beak.The lacrimal bone also removed until complete and adequate exposition of lacrimal sac was obtained. Upon exposition, the sac was identified and its medial wall was put in tension by a probe inserted through the inferior canaliculus. Posterior vertical incision of the tented medial sac wall was performed (Fig. 3) with keratome, followed by removal of medial wall of sac with endoscopic DCR scissors, thus creating a stoma. Patency was confirmed by free flow on syringing of both upper and lower punctum, on table. In group A patients, the anterior lacrimal sac wall was cleanly punched in both superior and inferior aspect and the sac wall everted on to the bare bone anteriorly and the nasal mucosal flap repositioned in a modified way on to bare bone covering the anteriorly everted sac wall. Posterior wall of sac everted posteriorly, thus not closing the stoma. In group B patients, medial sac wall was removed along with the nasal mucosal flap. Stents were not used in the procedure. Nasal packing was done.
Fig. 1.
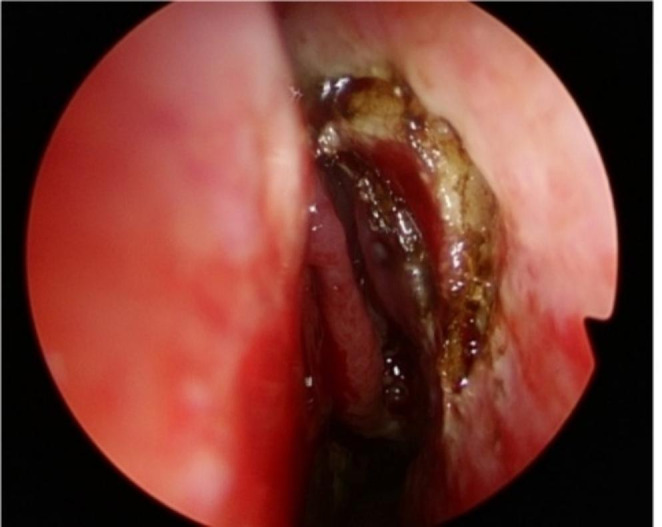
Incision over mucosa with cautery
Fig. 2.
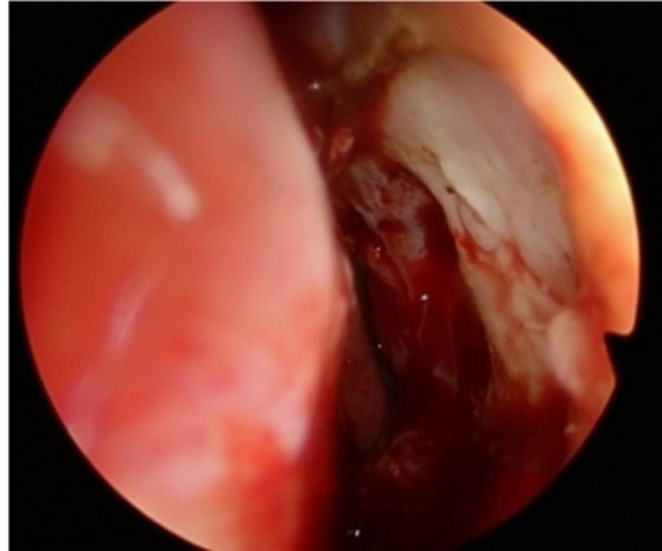
Frontal process of maxilla after inferiorly based flap creation
Fig. 3.

Medial wall incised with keratome
Post Operative Care
Patients were hospitalized for 24-48 h, on intravenous antibiotic and topical anti-inflammatory eye drops. Nasal pack removed after 24-48 h and was discharged on 7 days of oral antibiotics and a topical mixture of antibiotic eye drops. Irrigation and spray of the nasal cavity with saline were performed to prevent crust formation and in helping to stop mucosal drying in the acute postoperative period. Follow-up reviews were 1 week, 2 weeks, 1 month, and 3 months after operation. At each follow-up appointment lacrimal irrigation by Ophthalmologist was used to confirm the patency of ostium. Weekly syringing and nasal douching were continued for initial 2 months of post operative period.
Surgical success was defined as absence of epiphora and purulent discharge together with a patent lacrimal system. If lacrimal obstruction was occurred at any time point during the follow-up period, the patient was considered a surgical failure.
To find out the cause of failure, post operative nasal endoscopy was performed. The patients with scar formation at osteotomy site were managed by endoscopic revision.
All statistical analysis was performed using SPSS. Success rates of Endoscopic Endonasal DCR, the scar tissue formation around the ostium were evaluated with Pearson’ χ –test, P<0.05 was considered as statistically significant.
Results
We randomly assigned 100 patients with unilateral chronic dacryocystitis into two groups with 50 patients each in group A and group B respectively. Between two groups, there were no differences statistically, in patient age, sex and history of symptoms. In group A, nasal mucosa was preserved in modified way around stoma and in group B, mucosa was removed.
In the present study, no intraoperative complications (p=<0.05) encountered and there was only single postoperative complication (p=<0.05).
Epiphora (100%) and associated mucocele (30%) were the symptoms. None of them had acute inflammation, history of epistaxis or features of chronic granulomatous diseases. The mean duration of symptoms was 32.3 months (Table 1). Additional surgeries were done, to get good access to the operative field, including septoplasty in 10 patients, submucosal resection in 7 patients. In the present study, no intraoperative complications (p=<0.05) encountered and there was only single postoperative complication (p=<0.05).
Table 1.
Demographics, Time to presentation
| Variables | Total |
|---|---|
| Age | 38 ± 15.27 years |
| Male-Female Ratio | 1:2.33 |
| Urban-Rural distribution | 1:1.5 |
| Mean duration of symptoms | 32.3 months |
Outcome measured in terms of subjective (functional) and objective (anatomical) assessments for follow up duration of 3 months and success rate evaluated.
Epiphora recurred in 2 patients at the end of 3rd month in group A and 1 patient at the end of 2nd week, 3 patients at the end of 1st month and 5 patients at the end of 3rd month in group B. Hence functional patency (subsidence of epiphora) documented in 100% patients at the end of 1st week, in 96%patients at the end of 3rd month in group A and in 98%of patients at the end of 2nd week and 92%of patients at the end of 1stmonth and 82% patients at the end of 3rd month in group B (Table 2).
Table 2.
Complication & Outcome
| Intraoperative complication | nil | ||||||
| Postoperative complication | 01 | ||||||
| Patency | 1st Week | 2nd Week | 1st Month | 3rd Month | X2 | p-value | |
| Group A |
Anatomical Functional |
100% | 100% | 100% | 96% | 5.0051 | 0.025 |
| Group B |
Anatomical Functional |
100% | 98% | 92% | 82% | ||
Anatomical patency was checked with syringing periodically and found regurgitation from the failure patients, who had recurrence of symptom.
Diagnostic nasal endoscopy revealed restenosis in 2 patients at the end of 3rd month in group A and all symptomatic patients in group B. 2 patients who had recurrence at the end of 3rd month had synechiae along with the restenosis.
Thus scar tissue was found only in 2 patients with mucosal flap preservation against 9 patients without mucosal flap preservation. Chi- square was 5.0051, p-value was 0.025 and was statistically significant at p < 0.05.
Discussion
Endoscopic endonasal dacryocystorhinostomy is considered as a highly successful procedure for chronic dacryocystitis due to nasolacrimal duct obstruction, with the advent of telescopes and newer instruments for functional endoscopic sinus surgery, from early 1990’s[9]. The present study done was to evaluate the impact on the success rate by the preservation of nasal mucosal flap with modification around stoma site.
The success rate of endonasal DCR was 96% (48/50) as opposed to control group 82% (41/50) (p-< 0.05). The study was in favour of preservation of nasal mucosal flap in modified way around stoma site, covering the bare bone reducing the scar formation and synechiae.
The study was consistent with the previous studies [1–3].Qing Shan Ji et al. study among asian population reported the similar result, introducing v- shaped flap[10]. In Mishra Sonkhyaet al. [11] study, the surgical technique involved the creation of nasal mucosal and large posterior lacrimal flaps at the medial lacrimal sac wall. The two flaps were placed in close apposition. The technique also involved creation of a large bony ostium. The described technique of endoscopic endonasal dacryocystorhinostomy had a success rate (92%) comparable to that of external dacryocystorhinostomy and also pointed out that the procedure is simple and cost-effective because it does not require sophisticated equipment such as lasers, optical fibres, silicone stents or a microdebrider.
Tsirbas and Wormald [2] also pointed out that the new technique of endonasal DCR involving creation of a large ostium and construction of nasal and lacrimal sac mucosal flaps had anatomic success rate(91% or 40 of 44 DCRs), was compared favourably with the success rate of other techniques for endonasal DCR and was also similar to the success of external dacryocystorhinostomy, which indicated that creation of lacrimal and nasal mucosal flap results in primary intention healing with minimal risk of granulation tissue formation. Experience in endoscopic nasal surgery is important in endonasal DCR surgery, as other ancillary procedures may be required within the nose at the time of surgery.
With the bare bone maximally covered by nasal and lacrimal mucosal flaps in this technique, more prompt epithelization of the bony ostium and primary healing can be achieved within a shorter period according to Wenyan Peng et al. [14]. Success rate of symptomatic cure was 92.6% (25/27). No significant complications occurred intraoperatively. In contrary, Ramakrishnan et al. [13] suggested that preservation of mucosal flap may not be essential in achieving successful outcomes. They removed the mucosal flap, raised early in the procedure and eliminated the redundant lacrimal sac edges at the conclusion of the procedure with anatomic success rate of 93%. These data suggested that successfully powered DCR may be performed without the preservation of mucosal flaps. Kansu et al. [12], evidenced that in endoscopic endonasal DCR, the closure of bare bone with a posteriorly based nasal mucosal flap that creates an anastomosis between the lacrimal sac mucosa and the nasal mucosa decreases the formation of granulation tissue. But, there was no significant difference of success rate between two groups. These limited effects observed with mucosal flap was explained by the large bony ostium and less portion of bared bone during EE-DCR in white people. Asians have a low nasal bridge and a thicker frontal process of the maxilla. The special characteristics restricted to create a large bony ostium and allowed to expose more portion of bared bone. Hence the technique of preservation of nasal mucosa and exact anastomosis of the nasal mucosa and lacrimal sac is more important for Asian patients to improve the success rate. In conclusion, the simple modification of fashioning a “V-shaped” nasal mucosal flap can easily manipulate in Asian patients and preserve most.
Conclusion
Preservation of inferior based nasal mucosal flap with modification around stoma can be used to cover the bared bone with avoidance of the flap mobility and loss, along with less synechiae and granulation tissue formation. Thus lessen the risk of closure of ostium with large rhinostomy and improve success of endoscopic endonasal DCR.
Good anatomical knowledge of intranasal structures allows accurate mucosa preserving surgery. Endoscopic skills are necessary to ensure accurate and reproducible surgery.
Funding
No funding.
Declarations
Was complied.
Conflict of interest
Author 1 and Author 2 declares that there no conflict of interest.
Ethics approval and consent to participate
Ethical Approval was obtained.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wormald PJ. Powered endoscopic dacryocystorhinostomy. Laryngoscope. 2002;112(1):69–72. doi: 10.1097/00005537-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Tsirbas A, Wormald PJ. Endonasal dacryocystorhinostomy with mucosal flaps. Am J Ophthalmol. 2003;135(1):76–83. doi: 10.1016/S0002-9394(02)01830-5. [DOI] [PubMed] [Google Scholar]
- 3.Tsirbas A, Wormald PJ. Mechanical endonasal dacryocystorhinostomy with mucosal flaps. Br J Ophthalmol. 2003;87(1):43–47. doi: 10.1136/bjo.87.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsirbas A, Wormald PJ. Mechanical endonasal dacryocystorhinostomy with mucosal flaps. Otolaryngol Clin North Am. 2006;39(5):1019–1036. doi: 10.1016/j.otc.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Trimarchi M, Giordano Resti A, Bellini C, Forti M, Bussi M. Anastomosis of nasal mucosal and lacrimal sac flaps in endoscopic dacryocystorinostomy. Eur Arch Otorhinolaryngol. 2009;266(11):1747–1752. doi: 10.1007/s00405-009-1002-z. [DOI] [PubMed] [Google Scholar]
- 6.Mahendran S, Stevens-King A, Yung MW. How we do it: the viability of free mucosal grafts on exposed bone in lacrimal Surgery a prospective study. Clin Otolaryngol. 2006;31(4):324–327. doi: 10.1111/j.1749-4486.2006.01170.x. [DOI] [PubMed] [Google Scholar]
- 7.Codère F, Denton P, Corona J. Endonasal dacryocystorhinostomy: a modified technique with preservation of the nasal and lacrimal mucosa. Ophthal Plast Reconstr Surg. 2010;26(3):161–164. doi: 10.1097/IOP.0b013e3181b80af6. [DOI] [PubMed] [Google Scholar]
- 8.Durvasula VS, Gatland DJ (2004) Endoscopic dacrocystorhinostomy: long-term results and evolution of surgical technique. The Journal of laryngology and otology;118: 628–632. [DOI] [PubMed]
- 9.Kennedy DW Functional endoscopic sinus surgery technique. Arch Otolaryngol Head Neck Surg 1985;111(10):643–649 [DOI] [PubMed]
- 10.Qing-Shan Ji, Jing-Xiang Zhong, Yun-Hai Tu, and Wen-Can Wu New mucosal flap modification for endonasal endoscopic dacryocystorhinostomy in Asians. Int J Ophthalmol. 2012; 5(6): 704–707 [DOI] [PMC free article] [PubMed]
- 11.Sonkhya N, Mishra P. Endoscopic transnasal dacryocystorhinostomy with nasal mucosal and posterior lacrimal sac flap. J Laryngol Otol. 2009;123(3):320–326. doi: 10.1017/S0022215108003897. [DOI] [PubMed] [Google Scholar]
- 12.Kansu L, Aydin E, Axci S, Kal A, Gedik S. Comparison of surgical out comes of endonasal dacryocystorhinostomy with or without mucosal flaps. Auris Nasus Larynx. 2009;36(5):555–559. doi: 10.1016/j.anl.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 13.Ramakrishnan VR, Hink EM, Durairaj VD, Kingdom TT. Outcomes after endoscopic dacryocystorhinostomy without mucosal flap preservation. Am J Rhinol. 2007;21(6):753–757. doi: 10.2500/ajr.2007.21.3095. [DOI] [PubMed] [Google Scholar]
- 14.Wenyan Peng B, Tan Y, Wang H, Wang (2017) Zhonghao Wang & Xuanwei Liang A Modified Preserved Nasal and Lacrimal Flap Technique in Endoscopic Dacryocystorhinostomy Scientific Reports volume 7, Article number: 6809 [DOI] [PMC free article] [PubMed]


