Abstract
The sino-nasal cavities represent an anatomical region affected by a variety of tumors with clinical, etiological, genetic and pathological features, which are distinct from tumors commonly encountered in the area of head and neck cancers. We have undertaken this study with the aim of assessing clinical profile, various treatment modalities and outcome of patients with malignant sino-nasal tumors. In this prospective study of two years, done in a rural tertiary care hospital of India, 40 patients with malignant neoplastic tumors of nasal cavity, sinuses and nasopharynx were analyzed for their clinic-pathological and radiological profile and surgical management. The age range found was 10–78 years. There was a significant male preponderance with 23 (57.5%) male patients. Most common histological type seen in our study was Squamous cell carcinoma amongst 32 (80%) of cases. Maximum number of patients were managed with combination therapy of Surgery and Radiotherapy i.e. in 21 patients (52.5%). Multimodality treatment has been deemed the most efficacious choice of treatment which would improve disease free survival for the patients.
Keywords: Sino-nasal tumors, Malignant neoplasm
Introduction
The sino-nasal cavities represent an anatomical region affected by a variety of tumors with clinical, etiological, genetic and pathological features, which are distinct from tumors commonly encountered in the area of head and neck cancers [1]. Sino-nasal carcinomas are rare entities originating from paranasal sinuses and the nasal cavity. Exposure to leather, wood and dust particles is implicated in development of Sino-nasal carcinoma. Sino-nasal carcinoma (SNC) is a rare disease that accounts for < 3% of all head and neck tumors, with a 5-year overall survival (OS) rate of 30% across all stages [1]. Sino-nasal tumors can have an epithelial (carcinomas) or mesenchymal (sarcomas) origin. Epithelial tumors are the most common form and originate from the epithelial lining, accessory salivary glands, neuroendocrine tissue, and olfactory epithelium. Conversely, mesenchymal tumors derive from the supporting tissue [2].
Sinonasal squamous cell carcinoma (SNSCC) is the most common subtype of sino-nasal malignancy, accounting for 60–75% of sino-nasal tumors [3, 4]. Others reported includes adenocarcinoma, esthesioneuroblastoma, minor salivary gland tumors, or sinonasal neuroendocrine carcinoma [SNEC]) [5]. Patients with SNC are often asymptomatic in early stages and are therefore commonly diagnosed at an advanced stage (T3-4), presenting with a large primary tumor that invades the surrounding bone structures and is associated with a high frequency of poor outcome and local failure [6]. But there is paucity of literature on clinical profile, various treatment modalities and outcome of patients with malignant sino-nasal tumors hence, we have undertaken this study.
Objective
To study clinical profile, various treatment modalities and outcome of patients with malignant sino-nasal tumors.
Materials and Methods
This was a facility based prospective observational study, protocol of which was approved by the Institutional Ethical committee of the medical college. Written informed consent was taken from all study subjects.
Present study included 40 Patients with malignant sino-nasal masses confirmed on clinical examination, radiological investigations and histopathology report who were willing to be part of the study. Sampling method used was universal. Study was carried out over a period of 2 years. Cases with benign sino-nasal masses and cases with non-neoplastic sino-nasal mass were excluded.
All cases were analyzed as regard to the history, clinical presentation, routine investigations were carried out in order to get fitness for surgery. A detailed history was asked in every case, general and systemic examination was performed followed by oto-rhinolaryngological examination. This was followed by computed tomographic examination of nose and paranasal sinuses and diagnostic nasal endoscopic examination. Details of every case was recorded in separate case proforma. All patients were treated by surgery either endoscopically or by combined approach. Management of the patient was depending on the nature of the nasal mass. It was Surgery/radiotherapy/chemotherapy/combined modality. All patients were followed up after discharge at 1 month, 3 month and 6 months for assessing disease outcome, complications and recurrences if any. Data was collected in pre-structured proforma which was pilot tested and after ensuring it’s validity. The data collected was then analyzed by using SPSS IBM version 20.
Results
In the present prospective study, there was no lost to follow up and we could analyze all 40 patients giving the response rate of 100%. Out of total 40 cases of malignant nasal tumors majority, 18 (45%) between 41 and 60 years followed by 16 (40%) from > 60 years, 04 (10%) from 21–40 years & least, 02 (5%) from < 20 years. The age range found was 10–78 years. There was a significant male preponderance with 23 (57.5%) male patients and 17 (42.5%) female patients. Most, 20 (50%) of the study subjects in our study had been addicted to smoking followed by 19 (47.5%) addicted to alcohol & 13 (32.5%) to tobacco chewing while 12 (30%) did not have any of this addiction. As per TNM staging, most common stage of disease at presentation was Stage IV seen in 21 patients (52.5%), followed by Stage III, 17 patients (42.5%) and Stage II seen in 2 patients (5%). As the symptoms are usually mild, easily confused with other diseases like sinusitis, nasal polyps, and go unnoticed by patients, because of which patients of sinonasal malignancy usually present at advanced stages. No patient presented to us in Stage I of disease. One patient (2.5%) of Olfactory Neuroblastoma was classified in Stage 3 disease, as per Dulguerov staging system [7] (Table 1).
Table 1.
Distribution of patients according to baseline characteristics
| Baseline characteristic | Cases | ||
|---|---|---|---|
| No | % | ||
| Age (years) | < 20 | 02 | 5 |
| 21–40 | 04 | 10 | |
| 41–60 | 18 | 45 | |
| > 60 | 16 | 40 | |
| Gender | Male | 23 | 57.5 |
| Female | 17 | 42.5 | |
| Addictions (n = 40) | Tobacco chewing | 13 | 32.5 |
| Smoking | 20 | 50 | |
| Alcohol | 19 | 47.5 | |
| No addiction | 12 | 30 | |
| Histopathological stage | Stage 1 | 0 | 0 |
| Stage II | 2 | 5 | |
| Stage III | 17 | 42.5 | |
| Stage IV | 21 | 52.5 | |
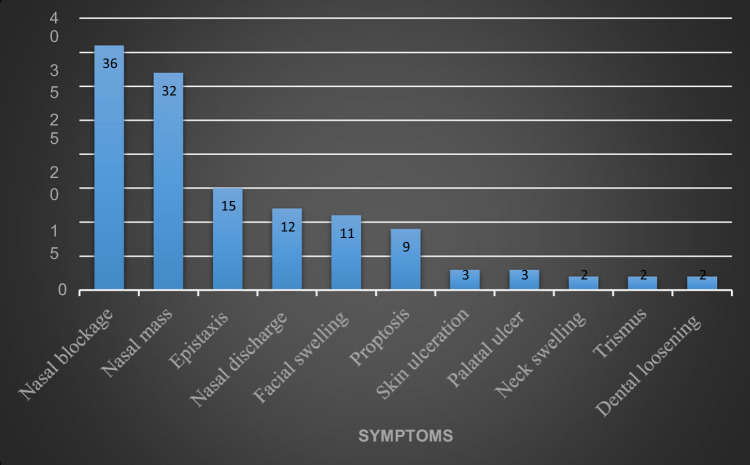
The commonest presenting complaint was Nasal blockage which was found in 36 (90%) cases. The other symptoms were Nasal mass in 32 patients (80%), Epistaxis in 15 patients (37.5%), Nasal discharge in 12 patients (30%), Facial swelling in 11 patients (27.5%) and Proptosis in 9 patients (22.5%). Other less frequent symptoms were Cheek skin ulceration, Palatal ulceration, Neck swelling, Trismus and Dental loosening. In patients presenting with trismus, skull base involvement was noted on radiology. Palatal ulceration indicates involvement of floor of maxillary sinus by the tumor. (Fig. 1).
Fig. 1.
Presenting complaints among patients
Most common histological type seen in our study was Squamous cell carcinoma amongst 32 (80%) of cases. There were 3 cases (7.5%) of Adenocarcinoma and one case (2.5%) each of Rhabdomyosarcoma, Adenoid Cystic, Olfactory Neuroblastoma, Sinonasal Terato-carcinosarcoma and Sinonasal Undifferentiated Carcinoma. (Table 2).
Table 2.
Histopathological types found in our study
| Histopathological type | No | % |
|---|---|---|
| Squamous cell carcinoma | 32 | 80 |
| Adenocarcinoma | 3 | 7.5 |
| Rhabdomyosarcoma | 1 | 2.5 |
| Olfactory neuroblastoma | 1 | 2.5 |
| Adenoid cystic carcinoma | 1 | 2.5 |
| Sinonasal undiffrentiated carcinoma | 1 | 2.5 |
| Sinonasal teratocarcinosarcoma | 1 | 2.5 |
| Total | 40 | 100 |
In present study, owing to late presentation and advanced stage of disease, multi-modality treatment approach was deemed most appropriate and used for managing most of the patients suffering from the disease. Maximum number of patients were managed with combination therapy of Surgery and Radiotherapy i.e. in 21 patients (52.5%). Only Surgical modality was used for one patient (2.5%). 10 (25%) patients were managed using a combination of Radiotherapy and Chemotherapy. Combined modality of Surgery, Chemotherapy and Radiotherapy was utilized in 3 patients (7.5%). 3 patients were given only Palliative care (7.5%) out of which one patient had non-resectable disease at presentation and 2 patients did not have medical fitness for any modality of treatment. Prosthesis/obturator was given for defect following ablative surgery (Fig. 2) (Table 3).
Fig. 2.

Image of patient presenting with right cheek swelling, Firm to hard in consistency
Table 3.
Distribution of patients according treatment to modalities
| Treatment modalities | Cases | |
|---|---|---|
| No | % | |
| Surgery only | 1 | 2.5% |
| Surgery + Radiotherapy | 21 | 52.5% |
| Surgery + Chemotherapy | 1 | 2.5% |
| Surgery + Radiotherapy + Chemotherapy | 3 | 7.5% |
| Radiotherapy only | 1 | 2.5% |
| Radiotherapy + Chemotherapy | 10 | 25% |
| Palliative | 3 | 7.5% |
In present study, out of 40 patients, 8 (20%) patients developed some kind of complications. Two patients developed Radiation Mucositis (5%). Two patients developed Xerostomia (5%) and two patients developed Surgical site Infection (5%). One patient developed Osteoradionecrosis after post operative radiotherapy (2.5%). One patient developed Neutropenia (2.5%). 32 patients (80%) however developed no complication during the course of follow up of this study (Fig. 3) (Table 4).
Fig. 3.
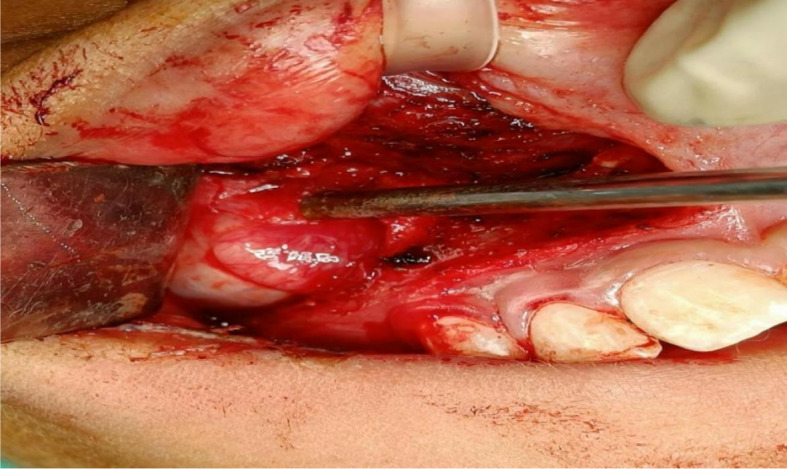
Sublabial approach as a part of combined approach for tumour removal showing right nasal mass
Table 4.
Distribution of patients according to complications
| Complications | No | % |
|---|---|---|
| Radiation mucositis | 2 | 5 |
| Xerostomia | 2 | 5 |
| Surgical site infection | 2 | 5 |
| Osteoradionecrosis | 1 | 2.5 |
| Neutropenia | 1 | 2.5 |
| No complications | 32 | 80 |
In present study,
Post operative radiotherapy:-
With high risk features (T3/T4, extracapsular extension, Close/positive margins, high grade,vascular invasion)-60 Gy in 30 fractions,
Low risk- 54 Gy in 27 fractions
Chemotherapy regimens:-
In most patients Inj Cisplatin 100 mg/m2 was administered- epithelial type.
Inj Paclitaxel 175mg/m2+ inj Carboplatin AUC 5 was administered–non epithelial variants
For Rhabdomyosarcoma:-
Inj Ifosfamide 1.5-2 g/m2 + Inj Doxorubicin 60 mg/m2
In this study, at the end of 6 months, 14 (35%) patients were alive with no evidence of disease (ANED) while 16 (40%) patients were Alive with residual/recurrent disease (AED) and 10 patients (25%) succumbed to disease. (Table 5).
Table 5.
Distribution of patients according to outcome of malignant sino-nasal carcinoma
| Outcome | No | % |
|---|---|---|
| ANED | 14 | 35 |
| AED | 16 | 40 |
| Death | 10 | 25 |
As the duration of study and thereby follow-up of the patients was for a short duration of time, Overall survival rate was not considered as a parameter. However, Disease Free Survival was considered as the parameter to assess the efficacy of our treatment protocol. As per the above mentioned observations, Disease Free Survival is calculated to be 35% (Fig. 4).
Fig. 4.

Endoscopic view post tumour resection, dura covered with fascia lata
Discussion
The present study is a prospective study, conducted for two years from 1st October 2020 to 30th September 2022, where 40 patients fulfilling the study criterion attended ENT department with malignant mass in the nasal cavity and paranasal sinuses were studied. The varied age and gender distribution, radiological and histopathological features, management protocol used for different malignant nasal masses and outcomes and complications encountered were studied (Fig. 5).
Fig. 5.
Endoscopic resection of tumour in right nasal cavity piecemeal
In present study, the age range found was 10–78 years, which is similar to that of studies conducte The mean age in present study is 54 years which is similar with studies conducted by Rutkowska et al.[8] (56 years), Khademi et al.[6] (55 years) and Maliha et al.[9] (50 years). d by Khademi et al. [6] (5–80 years) and Maliha et al.[9] (23–88 years) (Fig. 6) (Table 6).
Fig. 6.
Axial cuts of CT scan of rhabdomyosarcoma patient showing infratemporal and nasopharyngeal extension
Table 6.
Comparison of age distribution in different studies
In the present study, there was Male preponderance with 57.5% patients Males and 42.5% were Females which is comparable with that of the studies conducted by Rutkowska et al. [8] (M- 66.7%, F- 33.3%) and Khademi et al. [6] (M- 50.7%, F- 49.3%). Maximum percentage of patients seen addicted to smoking either singly or in combination with other addictions amounting to 50% which is comparable to the study conducted by Rutkowska et al. [8] (64.3%). Most commonly patients presented with Stage IV disease (52.5%) followed by stage III disease in 40% patients which is comparable to the study conducted by Khademi et al. [6]
In current study, nasal blockage was found in 90% patients which is similar to the study conducted by Bashir A Khan et al. [10] (95.7%) and in contrast to the study conducted by Maliha et al. [9] (41%). Nasal mass was found in 80% patients which is contrast to the result seen in study conducted by Danesh sanil et.al [11] (11.1%). Epistaxis was seen in 37.5% patients which is in contrast to the study conducted by Bashir A Khan et al. [10] (80%). Proptosis was seen in22.5% patients which however was seen in 12.2% in the study conducted by Danesh sanil et.al. [11]
In our study, Squamous Cell Carcinoma was the most common histopathological variant seen in 80% cases which is comparable to the findings seen in study conducted by Rutkowska et al.[8] (59.5%) while it is in contrast with the finding in study of Khademi et al.[6] (26.76%).
In present study as patients presented in late stages of disease and elderly age group was common at presentation with associated comorbidities, and subject to anesthetic fitness, treatment modality was tailored as per individual patient. Combined modality of treatment was deemed the most appropriate for the patients in this study. 52.5% patients were managed by Surgery and Radiotherapy combined which is comparable to the study conducted by Maliha et al. [9] (34.8%). 25% patients were managed by Radiotherapy and Chemotherapy which is similar to the study conducted by Khademi et al. [6] (19.7%). 2.5% patients were managed by Surgery only which is in contrast to the study conducted by Dhanani et al. [12] (47.3%) and Maliha et al. [9] Prosthesis/obturator was given for defect following ablative surgery.
In present study, Radiation Mucositis was found in 5% which is in contrast to study conducted by Tejal Gupta et al. [13] (20%). In present study Xerostomia was seen in 5%, osteoradionecrosis in 2.5% and Neutropenia in 2.5%. These complications were not reported in the study by Tejal Gupta et al. [13] 70% patients showed ocular complications in the study conducted by Tejal Gupta et al. [13] At the end of 6 months, patients alive with no evidence of disease were 35%, which is comparable to the study conducted by Khademi et al. [6] (46.4%). However, in present study, patients alive with evidence of disease is 40% which is in contrast to that of Khademi et al. [6] (11.3%). In our study, 25% patients died during the course of follow up, while Khademi et al. [6] reported death in 42.3% of patients.
Conclusion
In this study, most of the cases of malignant sino-nasal tumours presented with advanced stage of disease as initial symptoms were missed and confused with other common disease entities by patients and general practitioners, so it is prudent to increase vigilance amongst people and general practitioners which could help in early diagnosis and more effective management for these patients. There is association of malignant sino-nasal masses with various addictions like Smoking, Tobacco chewing, alcoholism, so public awareness programmes should be implemented to refrain people from such addictions. Multimodality treatment has been deemed the most efficacious choice of treatment which would improve disease free survival for the patients.
Declarations
Conflict of Interest
There was no source of funding in our study and there was no any conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Llorente J, López F, Suárez C, Hermsen M. Sinonasal carcinoma: clinical, pathological, genetic and therapeutic advances. Nat Rev Clin Oncol. 2014;11(8):460–472. doi: 10.1038/nrclinonc97. [DOI] [PubMed] [Google Scholar]
- 2.Rosenthal DI, Barker JL, Jr, El-Naggar AK, Glisson BS, Kies MS, Diaz EM, Clayman GL, Demonte F, Selek U, Morrison WH, et al. Sinonasal malignancies with neuroendocrine differentiation: patterns of fail-ure according to histologic phenotype. Cancer. 2004;101:2567–2573. doi: 10.1002/cncr.20693. [DOI] [PubMed] [Google Scholar]
- 3.Turner JH, Reh DD. Incidence and survival in patients with sinonasal cancer: a historical analysis of population-based data. Head Neck. 2012;34:877–885. doi: 10.1002/hed.21830. [DOI] [PubMed] [Google Scholar]
- 4.Jain S, Li Y, Kuan EC, Tajudeen BA, Batra PS. Prognostic factors in paranasal sinus squamous cell carcinoma and adenocarcinoma: a seer database analysis. J Neurol Surg B Skull Base. 2019;80:258–263. doi: 10.1055/s-0038-1669420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma, D. , Sharma, N. , Sharma, V. (2019). Sinonasal cancers: diagnosis and management. In: Wang, T. , editor. Challenging Issues on Paranasal Sinuses [Internet]. London: IntechOpen; [cited 2023 Jan 15]. Available from: https://www.intechopen.com/chapters/64095 doi: 10.5772/intechopen.81161
- 6.Khademi B, Moradi A, Hoseini S, Mohammadianpanah M. Malignant neoplasms of the sinonasal tract: report of 71 patients and literature review and analysis. Oral Maxillofac Surg. 2009;13:191–199. doi: 10.1007/s10006-009-0170-8. [DOI] [PubMed] [Google Scholar]
- 7.Dulguerov P, Calcaterra T. Esthesioneuroblastoma: the UCLA experience 1970–1990. Laryngoscope. 1992;102:843–849. doi: 10.1288/00005537-199208000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Rutkowska M, Hnitecka S, Dominiak M (2020). Sinonasal malignancies–clinico-pathological characteristics and difficulties in diagnostics. Advances in biomedical research–from cancer prevention to treatment. Edited by: Bialy L, Mlynarczuk-Bialy I. Lubin: Wydawnictwo Naukowe Tygiel. 143–56.
- 9.Kazi M, et al. Management of sinonasal tumours: prognostic factors and outcomes: a 10 year experience at a tertiary care hospital. Indian j Otolaryngol head neck surg official public Assoc Otolaryngol India. 2013;65(1):155–159. doi: 10.1007/s12070-013-0650-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bashir A, Khan ZA, Maqsood A, Prabhu N, Saleem MM, Alzarea BK, et al. The evaluation of clinical signs and symptoms of malignant tumors involving the maxillary sinus: recommendation of an examination sieve and risk alarm score. Healthcare [Internet] 2023;11(2):194. doi: 10.3390/healthcare11020194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danesh-Sunil SA, Sarafraz A, Chamani M, Derakhshandeh H. Paranasal sinuses malignancies: a 12-year review of clinical characteristics. Med Oral Patol Oral Cir Bucal. 2016;21(5):e626–e630. doi: 10.4317/medoral.21170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dhanani R, Faisal M, Shahid H, Malik KI, Jamshed A, Hussain R. Outcomes of management of sinonasal malignancies at a dedicated cancer institution: a retrospective study. Ann Maxillofac Surg. 2021;11:115–120. doi: 10.4103/ams.ams_16_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta T, Wadasadawala T, Phurailatpam R, et al. Early clinical outcomes in midline sinonasal cancers treated with helical tomotherapy-based image- guided intensity-modulated radiation therapy. Int J Head Neck Surg. 2013;4(1):6–12. doi: 10.5005/jp-journals-10001-1128. [DOI] [Google Scholar]