Abstract
Mucormycosis is a rare but serious angio-invasive infection caused by a group of fungi called mucormycetes. Mucormycosis is an aggressive, life-threatening infection requiring prompt diagnosis and early treatment. Wide spread use of steroid and higher antibiotics may cause immune irregulation in post covid patients. A hallmark of mucormycosis infection is the presence of extensive angioinvasion with resultant vessel thrombosis and tissue necrosis. We reported exponential rising cases of fungal infection in covid pandemic era. Here we published epidemiological data of 773 fungal infected cases operated in ENT department of PDU Medical college, Rajkot in 2021. We have documented patients demographic data with comorbidity, paranasal sinuses with orbital, palatal and cerebral involvement, evaluation method, surgical and post surgical management protocol which we followed in our institute to treat all cases. We got promising result in terms of survival and less morbidity. Early presentation, less comorbidity, proper evaluation and immediate debridement with systemic antifungal coverage for adequate duration proved to be mainstay treatment of fungal infection in covid pandemic era.
Keywords: Fungal infection, Exponential rise
Introduction
Mucormycosis is a rare but serious angio-invasive infection caused by a group of fungi called mucormycetes. Mucormycosis is not a contagious disease, it cannot be spread from one person to another. Clinical presentation is classified according to the organ involvement. It can be rhino-orbital cerebral, pulmonary, cutaneous, gastrointestinal, or disseminated. Mucormycosis is an aggressive, life-threatening infection requiring prompt diagnosis and early treatment. A hallmark of mucormycosis infection is the presence of extensive angioinvasion with resultant vessel thrombosis and tissue necrosis [1]. Treatment usually consists of antifungal medications and surgery. Fungal infections, including mucormycosis, aspergillosis and invasive candidiasis, have been reported in patients with severe COVID-19 or those recovering from the disease and have been associated with severe illness and death. India has reported a recent surge in mucormycosis cases. Prevention of COVID-19 associated mucormycosis needs to focus on aiming for better glycaemic control in COVID-19 patients and monitoring the use of systemic corticosteroids in treating severe cases. The incidence rate of mucormycosis globally varies from 0.005 to 1.7 per million population.In India, prevalence of mucormycosis is estimated as 140 per million population, which is about 80 times higher than the prevalence in developed countries [2].
Following the surge of COVID-19 associated mucormycosis and the Government of India directive, several states in India made mucormycosis a notifiable disease in May 2021. This will provide better insights into the disease burden, population characteristic, risk factors, clinical spectrum and outcomes of these patients.
We have observed sudden rise of mucormycosis cases in covid 19 era. Being an apex institute of Gujarat, we are publishing this article with the aim of understanding disease course, diagnosis and management protocol for future. Here we have reported data of 773 patient operated for fungal infection in our institute.
Material and Method
This was single center record based retrospective study of 773 operated cases of fungal infection till July 2021 either it was covid positive or non covid. All the patients of Rhino and/or orbital- palatal- cerebral fungal infection cases admitted under care of ENT department included in the study. In clinically suspecting cases, Nasal endoscopy done and tissue taken for fungal KOH examination. For further diagnosis, radiological investigation done. MRI PNS with MRI Brain with Orbit done to know the extent of diseases. Once the diseases confirmed, endoscopic sinus surgery with debridement done for only sinuses involvement. In initial stages of orbital involvement, cases treated with antibiotic eye drops and peribulber injection Amphotericin B given. In cases of extensive involvement like absent PL + PR and restricted eye movement, exenteration done. In palatal involvement cases, with proven radiological findings, maxillectomy done. In cases of limited skull base involvement, pterygopalatine fossa and infratemporal fossa clearance done. After debridement, tissue was sent for histopathological examination. Documentation done. Post operatively, Amphotericin B IV injection given in indoor patient either conventional or liposomal in patient having chronic kidney diseases. Patient was discharged on oral antifungal drugs. All the patient were kept for continuous surveillance by nasal endoscopy for 3 months with oral antifungal drugs.
Result
In study of 773 patients, common age group was 51–60 years followed by 41–50 years as shown in Table 1. We have 3 cases of pediatric age 13 years. Out of 773 patients, 495 were males, 278 were females. This ratio is of 1.78:1.
Table 1.
Distribution according to age and sex
| Female | Male | Total | |
|---|---|---|---|
| Agegroup | |||
| 11–20 | 2 | 1 | 3 |
| 21–30 | 7 | 9 | 16 |
| 31–40 | 44 | 71 | 115 |
| 41–50 | 68 | 137 | 205 |
| 51–60 | 108 | 164 | 272 |
| 61–70 | 36 | 85 | 121 |
| 71–80 | 11 | 28 | 39 |
| 81–90 | 2 | 0 | 2 |
| Total | 278 | 495 | 773 |
84.9% cases had history of covid infection, while 15.1% had no such history.
74.6% cases were having type 2 diabetes mellitus while only 16.9% cases had hypertension.
KOH culture of representive tissue suggest positive report in 52.8% cases.
Out of 773 patients, 61.8% had diseases only limited to para nasal sinuses, 23.5% rhino-palatal cases, 9.1% rhino orbital cases. 5% patients found with rhino-orbito-palatal involvement. We had seen 0.5% rhino orbito cerebral involvement in our operated cases (Fig 1).
Fig. 1.

Distribution of patient according to site involvement
Biopsy suggestive of mucormycosis found in 69.6% cases. While in other cases we found fungal infection by other species like 3.5% with aspergillosis, 2.3% both mucormycosis with aspegillosis, 0.9% with candidiasis. 21.2% cases reported with chronic sinusitis and 2.5% cases with necrotizing inflammation as shown in Fig. 2.
Fig. 2.

Distribution of patient according to histopathological report
In operative procedure, we had done bilateral debridement in 88.6% cases in which fungal infection limited to para nasal sinuses only (Fig. 3).
Fig. 3.
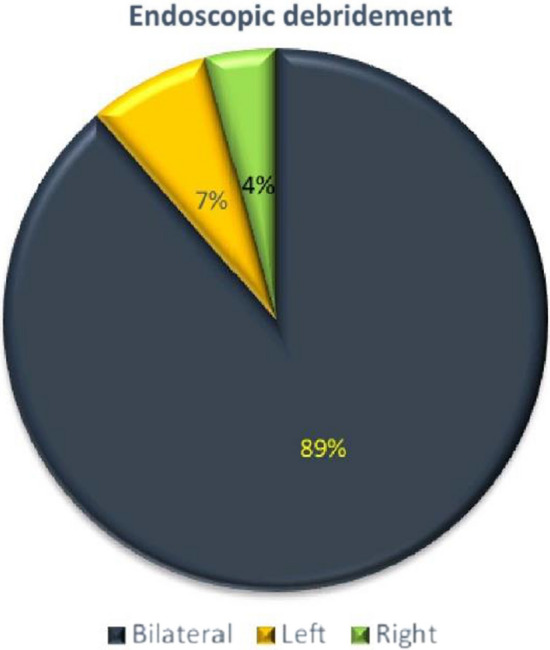
Distribution of patient according to endoscopic debridement
Among 14.6% cases with orbital involvement, in 4.1% cases treated with antibiotic eye drops, 4.3% cases with peribulbar injection Amphotericin B. In 6.2% cases exenteration done.
In 28.6% palate involvement cases, 20.8% treated by doing unilateral partial maxillectomy, 7.5% with bilateral partial maxillectomy and 0.3% with hemi maxillectomy.
In post operative period, we have given injection Amphotericin B and oral anti fungal drugs in all the cases with different duration as shown in Table 2.
Table 2.
Management protocol of our institute
| Fungal KOH report | HPE report | Site involvement | Amphotericin B IV | Oral Antifungal drug |
|---|---|---|---|---|
| Negative | Necrotizing inflammation/chronic sinusitis | Limited to para nasal sinuses | 14 days | Cap. Itraconazole for 3 months |
| Positive | Necrotizing inflammation/chronic sinusitis | Limited to or beyond para nasal sinuses | 21 days | Tab. Posaconazole for 14 days or 21 days then Cap. Itraconazole for total 3 months |
| Negative | Candidiasis/aspergillosis | Limited to para nasal sinuses | 14 days | |
| Positive | Candidiasis/aspergillosis | Limited to para nasal sinuses | 21 days | |
| Negative | Mucormycosis/mucormycosis + Aspergillosis | Limited to para nasal sinuses | 21 days | |
| Positive | Mucormycosis/mucormycosis + Aspergillosis | Limited to para nasal sinuses | 21 days | |
| Positive or negative | Mucormycosis/mucormycosis + Aspergillosis | Beyond para nasal sinuses | 28 days or 35 days |
In maxillectomy patient with oro antral fistula, patient was rehabilitated with palatal prosthesis to improve daily life.
We reported 14% mortality in our study.
Discussion
In study of 773 patients, common age group was 51–60 years. Similar result were noted by Desai et al. [3] in study of 100 patient and White et al. [4] study of 135 patients. We have 3 cases of pediatric age 13 years only. It can be attributed to less incidence of comorbidity and their immunity.
Out of 773 patients, 495 were males, 278 were females. This ratio is of 1.78:1 which was similar to study of Desai et al. [3] and nearer to study of White et al. [4] in which it was 2.2/1.
84.9% cases had history of covid infection, while 15.1% had no such history.
We found diabetes mellitus as most common risk factor in 74.6% cases as similar to study of Ferry et al. [5] and Desai et al. [3] Only 16.9% cases had hypertention. It proves that immunocompromised status is responsible for fungal infection.
In our study we reported palatal involvemet 28.6% while Desai et al. [3] reported this 45% and Sharma et al. [6] reported this 39% in post covid fungal infection patients. Goswami et al. [7] reported site wise incidence of mucormycosis. Bilateral Nasal cavity was most commonly involved (77.44%), followed by maxillary involvement (20.94%). Eye ball was also received in the section, which was almost 4.15%.
In early presentation, orbital involvement is less so we can manage it conservatively by eye drops or peribulbar injection Amphotericin B. In case of extensive disease, when there is no light perception and restricted eye movement, exenteration was done in 6.2% cases.
Biopsy suggestive of mucormycosis found in 69.6% cases. While in other cases we found fungal infection by other species like 3.5% with aspergillosis, 2.3% both mucormycosis with aspegillosis, 0.9% with candidiasis. 21.2% cases reported with chronic sinusitis and 2.5% cases with necrotizing inflammation. Biopsy proved to be a gold standard for diagnosis of various fungal species.
Amphotericin B is the gold standard in the treatment of mucormycosis. The survival rate of patients dramatically has increased to the 60% after the introduction of Amphotericin B [8].
In post operative period, we have given injection Amphotericin B during hospitalization and oral anti fungal drugs as maintenance therapy in all the cases with different duration according to KOH report, HPE report and clinical intra operative findings and recovery of patient in regular follow up.
Patient who presented early stage of diseases, gave us promising results with less morbidity. 14% patient didn’t survived due to comorbidity and advanced stage of diseases.
Conclusion
Epidemiology of mucormycosis is evolving. In light of new evidence, diabetes mellitus remains the main underlying disease globally. In this covid pandemic era one should always keep in mind of fungal infection due to wide spread use of steroid and higher antibiotics. This aids a higher chances for fungal infection in comorbid patients. Now a days awareness in both doctor and patient needed regarding early presentation of this rising cases of rare disease for better management and outcome. Hence early presentation, less comorbidity, proper evaluation and immediate debridement with systemic antifungal coverage for adequate duration proved to be mainstay treatment of fungal infection in covid pandemic era.
Funding
No funding sources.
Declarations
Conflict of interest
The author declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bouchara J, Oumeziane N, Lissitzky J, et al. Attachment of spores of the human pathogenic fungus Rhizopus oryzae to extracellular matrix components. Eur J Cell Biol. 1996;70(1):76–83. [PubMed] [Google Scholar]
- 2.https://www.who.int/india/emergencies/coronavirus-disease-(covid-19)/mucormycosis
- 3.Desai E, Pandya A, et al. Epidemiology, clinical features and management of rhino orbital mucormycosis in post COVID 19 patients. Indian J Otolaryngol Head Neck Surg. 2021 doi: 10.1007/s12070-021-02807-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.White PL, Dhillon R, Cordey A, et al. A national strategy to diagnose COVID-19 associated invasive fungal disease in the ICU. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferry A, Abedi S. Diagnosis and managementof rhino orbito-cerebral mucormycosis (phycomycosis)—a report of 16 personally observed cases. Ophthalmology. 1983;90:1096–1104. doi: 10.1016/S0161-6420(83)80052-9. [DOI] [PubMed] [Google Scholar]
- 6.Sharma S, Grover M, Bhargava S, et al. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol. 2021;135(5):442–447. doi: 10.1017/S0022215121000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goswami HM, Parikh UR, et al. Exponential rise in incidence of mucormycosis in the month of April and May 2021. Bjkines. 2021;13(1):61–67. [Google Scholar]
- 8.Furco A, Mouchet B, Carbonnelle M, et al. Pulmonary mucormycosis: benefit of aerosol amphotericin B. Rev Mal Respir. 2001;18(3):309–313. [PubMed] [Google Scholar]


