Abstract
Background: Chronic rhinosinusitis (CRS) is a syndrome with multifactorial aetiology. Amongst which, anatomical variations studied by computed tomography of paranasal sinuses (CT PNS) had a high incidence which varied between 64.0% and 99.8%10. Due to such high incidence, this study is undertaken to assess the various anatomical variations and their significant association in CRS. Method: A prospective observational study was conducted in 70 CRS patients and were subjected to CT PNS. CT PNS is studied to know the various anatomical variations & other CT findings causing CRS and then findings noted down, tabulated and statistical analysis done. Results: All 70 CRS patients evaluated by CT PNS had one or more anatomical variations along with other findings like fungal sinusitis in 6 patients, dentigerous cyst and inverted papilloma in 1 case each. The anatomical variations observed in our study were septal deviation(62.8%), concha bullosa(52.8%), agger nasi(51.4%), pneumatized crista galli(47.1%), hyperpneumatized bulla(40%), suprabullar cells(37%), septal spur(34.3%), paradoxically curved middle turbinate(34.2%), supra orbital cells(32.8%), haller cells(31.4%), septal pneumatization(17.1%), pneumatized uncinate(13%), interfrontal septal pneumatization(13%), maxillary septations(10%), maxillary sinus hypoplasia(7.1%), frontal hypoplasia(5.7%), uncinate attached to lamina papyracea(40%), uncinate to middle turbinate(11%), uncinate to skull base(7.9%), free uncinate(41%), frontal cells type 1;2;3;4 (36%);(30%);(20%);(38.5%), onodi cells(27.1%), pneumatized anterior clinoid process(18.5%), lateral recess(15.7%), sphenoid septations attached to optic nerve(10%) and carotid(2.8%), pneumatized superior turbinate(1.4%), Sellar; Pre sellar; Post sellar sphenoid(42.8%);(5.7%);(51.4%). In our study only anatomical variations around the maxillary & Frontal sinus showed significant association with CRS. Conclusion: Anatomical variations around the anterior group of sinuses have a significant association with CRS.
Keywords: Chronic Rhinosinusitis, EPOS 2020, CT Paranasal Sinuses, Anatomical Variation
Introduction
Chronic rhinosinusitis (CRS) is the chronic inflammation of the sinonasal mucosa. CRS represents a significant disease burden worldwide, affecting at least 11% of the population and consequently carrying with it a substantial economic burden to healthcare systems, to patients and to the economy [1]. The prevalence of CRS is 46.1% throughout the Indian subcontinent [2]. The European Position Paper on Rhinosinusitis and Nasal Polyps 2020 (EPOS 2020) has defined chronic rhinosinusitis as a diagnosis made on clinical grounds (characteristic symptoms) combined with objective evidence (characteristic signs in either nasal endoscopy or computed tomography) of mucosal inflammation for more than 12 weeks (Table 1 A) [3]. Chronic rhinosinusitis has multifactorial etiology [4]. Among the various causes, the incidence of anatomical variations in chronic rhinosinusitis varies between 64.0% and 99.8%10. In spite of their higher incidence, the association of anatomical variation with chronic sinusitis was not always significant in few of the previous studies conducted [5, 6]. Nevertheless, a considerable number of studies have found a significant association between few anatomical variations like deviated nasal septum, concha bullosa, hyperpneumatized ethmoid bulla, agger nasi cell, haller cell, frontal cells and sinusitis [4, 7–11]. Because of this disparity in data, our study is being conducted to analyze various anatomical variations in the sinonasal region that have association with CRS by computed tomography of paranasal sinuses.
Table 1.
A: Diagnostic criteria B: CRS classification as per EPOS 2020 for CRS4
| A | B | |||
|
PRIMARY SYMPTOMS Nasal blockage/ Obstruction/congestion |
Primary CRS | Localized | Type 2 | AFRS |
| Non type 2 | Anatomical variation- Isolated sinusitis. | |||
|
ADDITIONAL SYMPTOMS Facial pain/pressure Olfactory dysfunction Hyposmia/Anosmia |
Diffuse | Type 2 |
eCRS AFRS CCAD |
|
| Non type 2 | Non eCRS | |||
|
DURATION Acute: >10 days to < 3 months. Chronic: > 3 months. |
Secondary CRS | Localized | local pathology |
Odontogenic Fungal ball Tumor |
|
ENDOSCOPY Nasal polyps Mucopurulent discharge in the middle meatus. Oedema/ obstruction in the middle meatus. |
Diffuse | Mechanical | PCD, CF | |
| Inflammatory | GPA, EGPA | |||
| Immunity |
HIV Selective IgA, IgG immunodeficiency |
|||
|
CT PNS Mucosal changes within the osteomeatal complex and / or sinuses | ||||
Table 1A: one primary + one additional symptom or two primary symptoms, along with signs either on endoscopy or CT PNS should be present for the diagnosis of CRS
Table 1B: CRS -chronic rhinosinusitis; eCRS - eosinophilic CRS; AFRS - allergic fungal rhinosinusitis; CCAD -central compartment allergic disease; PCD, primary ciliary dyskinesia.; CF - cystic fibrosis; GPA - granulomatosis with polyangiitis (Wegener’s disease); EGPA, eosinophilic granulomatosis with polyangiitis (Churg-Strauss disease), IgA, IgG – Immunoglobulin A and G
Materials and Methods/Methodology
This is a prospective observational study conducted in the department of ENT, Basaveshwara Teaching and General Hospital, attached to Mahadevappa Rampure Medical College, Kalaburagi. The duration of study is 18 months, from 1st march 2021–31st august 2022.
Inclusion Criteria
Patients with history suggestive of Chronic rhinosinusitis and who met the diagnostic criteria proposed by EPOS 2020 (Table 1 A); Patients more than 18 years of all genders; Patients giving consent for undergoing computed tomography of paranasal sinuses were included in our study.
Exclusion Criteria
Patients with history of prior nasal or paranasal surgeries and trauma were excluded from the study.
Study Method
In our study, patients more than 18 years of age attending ENT outpatient department with history suggestive of chronic rhino sinusitis and who met the diagnostic criteria based on EPOS 2020 were selected. After thorough Ear Nose Throat examination patients were subjected to Diagnostic Nasal Endoscopy to look for the signs indicating chronic inflammation of sinonasal mucosa. After taking informed and written consent from the patients, they were subjected to computed tomography of para nasal sinuses (CT PNS). CT PNS was then studied to know the various anatomical variations & other CT findings causing CRS. The findings were noted down, tabulated and statistical analysis done.
Statistical Analysis
Data was analyzed by IBM SPSS 25.0 version software. Collected data were spread on excel sheet and master chart was prepared. Through the master chart tables and graphs were constructed. For quantitative data analysis of descriptive statistics, mean and standard deviation were done initially; independent samples “t-” test was used to compare the mean values between two variables for statistical significance. For qualitative data analysis chi-square test and Fisher exact probability tests were applied for statistical significance and P ≤ 0.05 was considered statistically significant for all comparisons.
Results
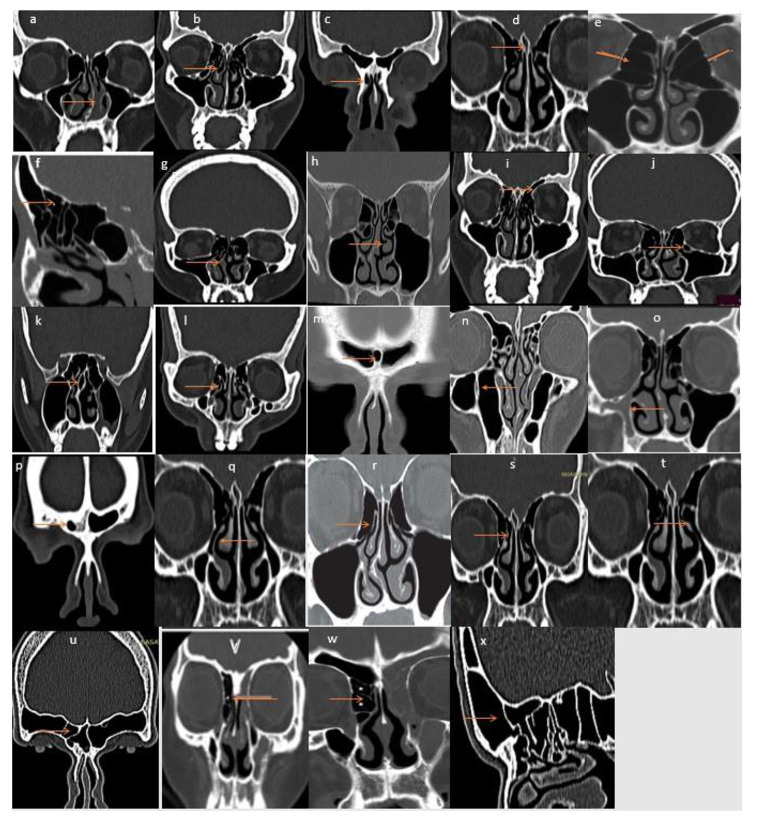
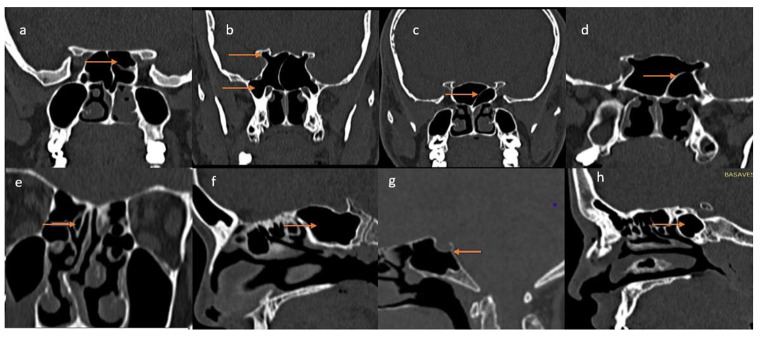
Of the 70 CRS patients in our study 28(40.0%) females and 42(60.0%) were males. Majority of patients i.e.,50 (71.4%) belongs to the age group of 21–40 years. Minimum age is 18 and maximum 70 years. Among the CT scan findings of 70 CRS patients, all had one or more anatomical variations, fungal sinusitis observed in 6 patients, dentigerous cyst and inverted papilloma in 1 case each. Out of 70, most common sinus involved with sinusitis were maxillary 38(54.2%), followed by frontal 32(46%), anterior ethmoid 24(34.2%), sphenoid 7(10%), posterior ethmoid 5(7.1%) and 10(14.2%) cases had pansinusitis. The individual anatomical variations on CT PNS seen in our study were deviated nasal septum (DNS) 44(62.8%), concha bullosa 37(52.8%), agger nasi cells 36(51.4%), pneumatized crista galli 33(47.1%), hyperpneumatized bulla 28(40%), suprabullar cells 26(37%), septal spur 24(34.3%), paradoxically curved middle turbinate 24(34.2%), supra orbital cells 23(32.8%), haller cells 22(31.4%), septal pneumatization 12(17.1%), pneumatized uncinate 9(13%), interfrontal septal pneumatization 9(13%), maxillary septations 7(10%), maxillary sinus hypoplasia 5(7.1%), frontal hypoplasia 4(5.7%), uncinate attached to lamina papyracea 56(40%), uncinate to middle turbinate 15(11%), uncinate to skull base 11(7.9%), free uncinate 58(41%), frontal type 4 cells 27(38.5%) type 1cells 25(36%), type 2 cells 21(30%), type 3 cells 14(20%) (Fig. 1a-x). Also, onodi cells 19(27.1%), pneumatized anterior clinoid process 13(18.5%), lateral recess 11(15.7%), sphenoid septations attached to optic nerve 7(10%) and carotid 2(2.8%), pneumatized superior turbinate 1(1.4%), Post sellar sphenoid 36(51.4%), Sellar sphenoid 30(42.8%), Pre sellar sphenoid 4 (5.7%) (Fig. 2a -h). In our study, anatomical variations on CT PNS that had a significant association with maxillary sinusitis were DNS, concha bullosa, hyperpneumatized ethmoid bulla, paradoxical middle turbinate, haller cell. Wherein frontal sinus mucosal disease had significant association with DNS, concha bullosa, type 1 and 2 frontal cells, agger nasi cells, suprabullar cells. Other findings like Allergic fungal sinusitis, dentigerous cyst, inverted papilloma also had significant association with sinusitis. Whereas ethmoid and sphenoid sinuses did not show any significant association with anatomical variation in CT PNS of CRS patients. (Table 2)
Fig. 1.
Anatomical variations of anterior group of sinuses. a-deviated nasal septum, b-concha bullosa, c-agger nasi cell, d-pneumatized crista galli, e-hyperpneumatized bulla, f-suprabullar cell, g-septal spur, h-paradoxical middle turbinate, i-suprabullar cell, j-haller cell, k-nasal septum pneumatized, l-uncinate pneumatized, m-pneumatized interfrontal septum, n-maxillary septation, o-maxillary hypoplasia, p-frontal hypoplasia, q-uncinate attached to lamina papyracea, r-uncinate to middle turbinate, s-uncinate to skull base, t-free uncinate, u;v;w;x-frontal type4,1,2,3 cell
Fig. 2.
Anatomical variations of posterior group of sinuses. a-onodi cell, b-lateral recess, pneumatized anterior clinoid process, c-sphenoid septation attached to optic nerve, d-sphenoid septation attached to carotid, e-pneumatized superior turbinate, f-post sellar sphenoid, g-sellar sphenoid, h-pre sellar sphenoid
Table 2.
CT scan findings in crs patients
| No of cases Out of 70 |
CT paranasal sinuses findings in chronic rhinosinusitis patients | Anterior group of sinuses | Posterior group of sinuses | Significance (P < 0.05 is Significant) |
||||
|---|---|---|---|---|---|---|---|---|
| M* 38 |
F* 32 |
AE* 24 |
PE* 5 |
S* 7 |
||||
| 70/70 | Anatomical variation | Nasal septal deviation | 21 | 19 | 10 | 1 | 2 | P < 0.05 for M, F |
| Concha bullosa | 18 | 17 | 9 | P < 0.05 for M, F | ||||
| Paradoxical middle turbinate | 19 | 14 | 4 | P < 0.05 for M | ||||
| Hyperpneumatized bulla | 20 | 10 | 1 | P < 0.05 for M | ||||
| Haller cell | 18 | 12 | 1 | P < 0.05 for M | ||||
| Frontal cell type 1 | 20 | P < 0.05 for F | ||||||
| Frontal cell type 2 | 21 | P < 0.05 for F | ||||||
| Agger nasi cell | 24 | P < 0.05 for F | ||||||
| Suprabullar cell | 23 | P < 0.05 for F | ||||||
| Pneumatized nasal septum | 1 | 2 | 2 | P > 0.05 | ||||
| Septal spur | 4 | 10 | 9 | 1 | 3 | P > 0.05 | ||
| Uncinate attachment lamina papyracea | 3 | 5 | 1 | P > 0.05 | ||||
| Uncinate skull base attachment | 3 | 9 | 1 | P > 0.05 | ||||
| Uncinate middle turbinate attachment | 4 | 2 | P > 0.05 | |||||
| Pneumatized uncinate | 3 | 5 | 3 | P > 0.05 | ||||
| Frontal hypoplasia | P > 0.05 | |||||||
| Frontal cells type 3 | 6 | P > 0.05 | ||||||
| Frontal cells type 4 | 10 | P > 0.05 | ||||||
| Interfrontal septum pneumatization | 5 | P > 0.05 | ||||||
| Supraorbital cell | 4 | P > 0.05 | ||||||
| Pneumatized crista galli | 14 | 2 | P > 0.05 | |||||
| Onodi cell | 1 | 2 | P > 0.05 | |||||
| Maxillary sinus hypoplasia | 2 | P > 0.05 | ||||||
| Maxillary septations | 4 | P > 0.05 | ||||||
| Post sellar sphenoid | P > 0.05 | |||||||
| pre sellar sphenoid | P > 0.05 | |||||||
| Pneumatized anterior clinoid process | 4 | P > 0.05 | ||||||
| Lateral recess | 1 | P > 0.05 | ||||||
| Septations to optic nerve | P > 0.05 | |||||||
| Septations to internal carotid | P > 0.05 | |||||||
| 6/70 | Other causes | Allergic fungal sinusitis | 3 | 3 | 4 | 3 | 4 | P < 0.05 for M, F, AE, PE, S |
| 1/70 | Dentigerous cyst | 1 | P < 0.05 for M | |||||
| 1/70 | Inverted papilloma | 1 | P < 0.05 for M | |||||
M* -maxillary, F*-frontal, AE &PE *- anterior; posterior ethmoid & S*-sphenoid sinusitis
Discussion
Human beings are individualistic creatures therefore subjected to a large number of anatomical variations or deviations from the rule. The sinonasal anatomy is no different and shows numerous variations. With the advent of CT in 1972 by Hounsfield and Allan, considerable attention has been given to the detailed study of sinonasal anatomy and its variations [12].
In our study out of 70 patients with chronic rhinosinusitis majority were males 42(60.0%) and 28(40.0%) were females. This result is consistent with Prakash et al., Fadda GL et al. who also had more male cases 66%, 60% respectively [7, 8]. Majority in our study i.e.,50 (71.4%) patients belonged to the age group of 21–40 years.
Out of 70 CRS patients it was observed that commonest sinus involved in our study was maxillary 38(54.2%). This is similar to study by Rajneesh et al., Prakash. S et al. [5, 8]. This is followed by frontal 32(46%), anterior ethmoid 24(34.2%), posterior ethmoid 5(7.1%), 10(14.2%) pansinusitis and sphenoid 7 (10%).
Out of 70 CRS patients, anatomical variations on CT PNS were seen in all 70 (100%) cases, fungal sinusitis observed in 6(8.5%) patients, dentigerous cyst and inverted papilloma in 1 (1.4%) case each. Ufuk dasar et al. in their study stated the prevalence of anatomical variation in literature to be between 64% and 98.5%10. This wide range of variation in the incidence of anatomical variation may be simply due to the fact that the structural design of the facial skeleton varies greatly with each individual. Hence the incidence of anatomical variations varies with each study. Anna maria et al. in their meta-analysis concluded that sinus inflammation is caused by multiple factors, including anatomical variations, mucosal inflammation by upper respiratory tract infection, allergic rhinitis, adenoid hypertrophy, impaired immunity, gastroesophageal reflux disease and environmental factors. These factors will jointly determine the effect on the development of sinus pathology [13]. The EPOS 2020 has classified CRS as primary and secondary based on pathological characteristics (Table 1B) [3]. Although CT PNS has been extensively studied to determine the etiology in CRS patients, it cannot be used to diagnose all etiologies. Only structurally evident causes of CRS, like anatomical variations, allergic fungal sinusitis, dentigerous cyst or inverted papilloma, as seen in our study, can easily give the causes for CRS with the help of CT PNS. The diagnosis of other primary and secondary etiologies further requires other modalities of clinical evaluation and investigation.
The common anatomical variations observed in our study were deviated nasal septum 44 (62.8%), agger nasi cell 36 (51.4%), frontal cells type 1 25(36%); type 2 21(30%); type 3 14(20%); type 4 27(38.5), concha bullosa 37(52.8%), pneumatized crista galli 33 (47.1%), onodi cell 19 (27.1%), haller cell 22(31%), paradoxical middle turbinate 24(34%), hyper pneumatized ethmoid bulla 28(40%), septal spur 24 (34.3%). Among the anatomical variations noted in our study deviated nasal septum was commonly seen. This was comparable with Rashi et al., Devraj et al., M kaya et al. ;10, 11, 12]. On comparing literature, other most common variation observed in other studies were agger nasi cell, which was 84% in study by Allan keast et al., 78.3%Wenrol et al., 74.8% Ufukdasar et al. [4, 9, 14]. Concha bullosa was noted among 67.5% cases in the study by Ufukdasar et al., 51%M kaya et al. ,49.3% G.L Fadda et al. [7, 9, 11]. Septal spur was found in 60% patients in study by Allan keast et al., 49% in Devraj et al., 42.3%Ufukdasar et al. [9, 10, 14]. Incidence of haller cells in Wenrol et al., Allan keast et al., G.L Fadda et al. were 41.6%, 28%,22.8% respectively [4, 7, 14]. Incidence of onodi cells in the study by Ufukdasar et al., Allan keast et al. were 25.3% and 24% respectively.10,13 Frontal cells observed in studies like Ufukdasar et al., Rajneesh e al were 57.7%and 56%respectively.10,9 Hyperpneumatized bulla was observed as 32.8% ,31.3% in the studies conducted by G.L Fadda et al., Ahmet kaygusuz et al. [6, 7]. Paradoxical middle turbinate noted as 26%,15.8% in studies like M kaya et al. and Ufukdasar et al. [9, 11]. Pneumatized crista galli was observed in study by Ahmet kaygusuz et al. 22.2% and Devraj et al. 43% [6, 10].
The uncommon anatomical variations observed in our study were pneumatized nasal septum 12(17.1%), Supra orbital cell 23(32.8%), Suprabullar cell 26(37%), pneumatized anterior clinoid 13(18.5%), lateral recess 11(15.7%), pneumatized uncinate 9(13%), inter frontal septal pneumatization 9(13%), maxillary hypoplasia 5(7.1%), maxillary septation 7(10%), sphenoid septations attached to optic nerve 7(10%) and carotid 2(2.8%), frontal hypoplasia 4(5.7%) and pneumatized superior turbinate 1(1.4%). Type of sphenoid pneumatization noted in our study were sellar sphenoid 30(42.8%), pre sellar 4 (5.7%) sphenoid, post sellar sphenoid 36(51.4%). Various types of Uncinate attachment observed in our study were to lamina 56(40%) cases, skull base 11(7.9%) cases, middle turbinate 15(11%) cases.
Incidence of pneumatized nasal septum observed in other studies were 27.1% in Devraj et al., 9.3% G L Fadda [10, 7]. Pneumatized uncinate observed as 13.8% in Ufuk dasar et al. [9]. Pneumatized anterior clinoid process was observed as 25.5% and 27.1% in Ufukdasar et al. and Devraj et al. respectively [9, 10]. Lateral recess seen in Ufukdasar et al. was 18.2%10. Pneumatized superior turbinate was noted as 13%,6.3%,3.9% in Ufukdasar et al., Regina et al., Devraj et al. [9, 10, 15]. Incidence of frontal hypoplasia, supra orbital cell, supra bullar cell observed in Ufukdasar et al. was 21.8%, 9% ,2.5%respectively10. Maxillary hypoplasia and septations seen in Ufukdasar et al., G L Fadda were 8%,8% and 5.3%,7% respectively [9, 7]. Ufukdasar et al. in their study noted septations attached to carotid to be 13%.10 Types of sphenoid pneumatization was studied by Devraj et al. and found that conchal type seen in 5%, pre sellar49%, sellar 14%, post sellar 83%.11 The superior attachment of uncinate seen in Rajneesh et al. were as follows 54% attached to lamina ,33% to skull base, middle turbinate in 13%.9 None of the anatomical variations in our study, be it common or uncommon, were comparable in terms of incidence with other studies. This is due to the fact that the developmental design of the nose and paranasal sinuses is not uniform and varies greatly with each individual. Hence, the incidence of each anatomical variations varies with each study.
In our study anatomical variations like DNS, concha bullosa, hyperpneumatized ethmoid bulla, paradoxical middle turbinate, haller cell had significant impact on maxillary sinus mucosal disease. Wherein frontal sinus mucosal disease had significant association with DNS, concha bullosa, type 1 and 2 frontal cells, agger nasi cells & suprabullar cells. Similarly, G. L Fadda et al. also observed in their study that anatomical variations like DNS, Concha bullosa, haller cell had association with maxillary sinusitis whereas medial deviation of uncinate, hyperpneumatized ethmoid bulla had association with anterior ethmoidal sinusitis. Also, significant association was observed between agger nasi cells and frontal sinusitis [7]. Devaraj et al. in their study found association of DNS, concha bullosa with maxillary sinus mucosal disease [10]. Prakash et al. in their study observed association between concha bullosa and multiple bilateral sinuses, haller cell and maxillary sinusitis [8]. These Anatomical variations in and around the narrow drainage pathways of osteomeatal complex of the anterior group of sinuses had significant association with chronic mucosal disease in our study. This significant association of anatomical variations at the osteomeatal complex level with chronic mucosal disease with respect to the respective draining sinus can be explained by mucosal contact theory of Messerklinger. Messerklinger in his study on secretion transport and its pathology found that, When the opposing mucosal surfaces in the narrow clefts or prechambers come into intense contact or are firmly pressed against each other as a result of mucosal swelling, the drainage and ventilation of the larger dependent sinuses may be seriously interfered with because the ciliary beat is immobilized and consequently the mucus is no longer transported away. These areas of contact may not be visible clinically but they can disturb nasal cycle, cause reactive hypersecretion and retention of mucus. When infection occurs, retained mucus serves as an ideal nutrient source for the organisms creating a vicious cycle [16].
In our study anatomical variations nearby posterior group of sinuses did not show any association with chronic mucosal disease. Because, the variations associated with posterior group of sinuses did not affect their drainage pathway. Rather, anatomical variations near the posterior group of sinuses like onodi cell, sphenoid septations attaching to optic nerve or internal carotid artery, lateral recess, carotico-optic recess are all important during endoscopic sinus surgery to avoid complications. Also, anatomical variations did not show significant association with ethmoid sinus mucosal disease in our study. This may be due to multiple drainage pathways of frontal and ethmoid sinuses. In the study by Toru et al. on anterior ethmoid and frontal sinus drainage pathways it was found that few anterior ethmoid cells drain between basal lamella of ethmoid bulla and basal lamella of middle turbinate (via hiatus semilunaris superioris) [17]. On contrary, Rajnesh et al. & Ahmet et al. [5, 6] in their study did not find any significant association between anatomical variations and sinusitis. Rajnesh et al. concluded that mere presence of variations in sinonasal region does not indicate a predisposition to sinus pathology. But these variations may predispose patients to increased risk of intra operative complications & Ahmet et al. recommended that a more scientific study would include, not only the rate of variations but also size, shape and type of specific variations and their interaction with sinus drainage [5, 6].
The CT findings other than anatomical variations found in our study, like allergic fungal sinusitis affected both the anterior and posterior groups of sinuses, whereas for maxillary sinus, the dentigerous cyst and inverted papilloma had a significant association with sinusitis. Anna maria et al., Prakash et al. in their study claimed CRS is a multifactorial disease and so the combination of these risk factors have effect on the development of sinus pathology [8, 13]. Although there is no significant association of anatomical variation and mucosal disease of posterior group of sinuses, inflammatory etiology like allergic fungal sinusitis as seen in our study has association with sinusitis of posterior group of sinuses.
So, studying anatomical variations by CT PNS in a CRS patient not only helps in identifying their possible association with mucosal inflammation but also gives preoperative knowledge about sinonasal anatomy and its numerous variations and helps the surgeon navigate the anatomy and its variations during FESS surgeries, avoiding the impending complications at the time of surgery.
Conclusion
Though anatomical variations seen in the CT PNS is high, not all anatomical variation show significant association with CRS. Anatomical variations around the narrow drainage pathways of the osteomeatal complex of the anterior group of sinuses, like maxillary and frontal favor the development of CRS rather than posterior sinuses, which have got non-narrow drainage pathways. CRS is a multifactorial disease, and so the combination of the risk factors can also have an effect on the development of sinus pathology.
Author Contributions
C.B Nandyal (CB) and Aslin Benola (AB) designed the Study concept. CB and AB helped in Analysis and Interpretation of data, Drafting of Manuscript, Critical revision of manuscript for important intellectual content, Literature research and analysis, statistical analysis. All authors equally contributed in writing the manuscript. All authors read and approved the submitted version.
Data Availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
Declarations
Financial Support and Sponsorship
This research is not funded by any resource.
Competing Interests
The authors declare that they have no competing interest.
Conflict of Interest
There is no conflict of interest.
Ethical Approval and Consent to Participate
The study was approved by the institutional Ethics Committee of Mahadevappa Rampure Medical College Kalaburagi, Karnataka under number HKES/MRMCK/IEC/202303 and informed written consent to participate in the study was provided by all participants.
Research does not involve animal study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carl Philpott. rhinosinusitis: definitions, classification and diagnosis. scott brown’s s otorhinolaryngology and head and neck surgery: basic sciences, endocrine surgery, rhinology 8th edi 2018 pages 1025–1034
- 2.Tanvi rekhade AZ, nitnaware, Seema patel RT, Pawar Ashish Keche clinical profile of chronic rhinosinusitis: a study in central India. Indian J Res | Volume – 10 | Issue – 04 |April – 2021
- 3.Wytske J, Fokkens VJ, Lund C, Hopkins PW, Hellings R, Kern S, Reitsma et al European position paper on Rhinosinusitis and nasal polyps 2020. Rhinol Suppl 29 vol 58: 1–464
- 4.Wenrol Espinosa R, Genito, Rachel Zita Ramos Anatomic variations of the nasal cavity and paranasal sinus and their correlation with chronic rhinosinusitis using Harvard staging system. J Otolaryngol ENT Res. 2018;10(4):190–193. [Google Scholar]
- 5.Rajneesh R (2017jul) Study of anatomical variations in osteomeatal complex in patients with chronic rhinosinusistis. Int J Otorhinolaryngol Head Neck Surg 3(3):528–533
- 6.Ahmet Kaygusuz M, Haksever D, Akduman S, Aslan Z, Sayar Sinonasal anatomical variations: their relationship with chronic Rhinosinusitis and Effect on the severity of Disease—A computerized tomography assisted anatomical and clinical study. Indian J Otolaryngol Head Neck Surg. 2014;66(3):260–266. doi: 10.1007/s12070-013-0678-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fadda L, Rosso S, Aversa S, Petrelli A, Ondolo C. Succo. Multiparametric statistical correlations between paranasal sinus anatomic variations and chronic rhinosinusitis. Acta Otorhinolaryngol Ital. 2012;32:244–251. [PMC free article] [PubMed] [Google Scholar]
- 8.Prakash S, Handi1, Mallikarjun N, Patil (2017) Evaluation of nose and paranasal sinus Disease, anatomical variations by computerized tomography. Int J Otorhinolaryngol Head Neck Surg 3(4):898–903
- 9.Dasar U, Gokce E Evaluation of variations in sinonasal region with computed tomography World J Radiol 2016 January 28; 8(1): 98–108 [DOI] [PMC free article] [PubMed]
- 10.Devaraja K, Doreswamy SM, Pujary K, Ramaswamy B, Pillai S. Anatomical variations of the nose and paranasal sinuses: a computed Tomographic Study. Indian J Otolaryngol Head Neck Surg (November. 2019;71(Suppl 3):S2231–S2240. doi: 10.1007/s12070-019-01716-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaya M, Çankal F, Gumusok M, Apaydin N. Role of anatomic variations of Paranasal sinuses on the prevalence of Sinusitis: computed tomography findings of 350 patients Niger. J Clin Pract. 2017;20:1481–1488. doi: 10.4103/njcp.njcp_199_16. [DOI] [PubMed] [Google Scholar]
- 12.Tiwari R, Rashmi Goyal Study of anatomical variations on CT in chronic sinusitis. Indian J Otolaryngol Head Neck Surg (Jan–Mar. 2015;67(1):18–20. doi: 10.1007/s12070-014-0734-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Papadopoulou A-M, Bakogiannis N, Skrapari I, Bakoyiannis C. Anatomical variations of the Sinonasal Area and their clinical impact on Sinus Pathology: a systematic review. Int Arch Otorhinolaryngol. 2022;26(3):e491–e49. doi: 10.1055/s-0042-1742327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allan Keast S, Yelavich P, Dawes, Lyons B. Anatomical variations of the paranasal sinuses in Polynesian and New Zealand European computerized tomography scans. Otolaryngology–Head and Neck Surgery. 2008;139:216–221. doi: 10.1016/j.otohns.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 15.Regina Chinwe Onwuchekwa, Nengi Alazigha (2016) Computed tomography anatomy of the paranasal sinuses and anatomical variants of clinical relevants in Nigerian adults. EgyptJ Ear Nose Throat Allied Sci
- 16.Heinz stammberger, wolfgang kopp. Secretion transportation. Stammberger’s functional endoscopic sinus Surgery 1st edi 1990, pages 17–46
- 17.Toru, Kikawada Yasutomo Araki1, Takuya Okamoto. Anterior ethmoid and frontal sinus drainage pathways: five patterns formed and defined by their bony walls. Eur Arch Otorhinolaryngol. 2023;280:199–206. doi: 10.1007/s00405-022-07517-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article and its supplementary information files.