Abstract
The second wave of COVID pandemic was associated with an outbreak of Mucormycosis. The mortality rate of Mucormycosis reaches 50–80% in cases with orbital and intracranial extension (Fadda in Acta Otorhinolaryngol Ital 41:43–50, 2021). In this outbreak we found that few of these patients had bacterial invasive sinusitis mimicking fungal sinusitis. Amphotericin the only effective drug against Mucormycosis is highly toxic and expensive and not indicated in bacterial sinusitis. Our aim was to determine the exact etiologic agent, predisposing factors and outcome of treatment of COVID associated invasive sinusitis presenting with orbital complications. It is a retrospective observational study done in 33 patients with orbital complications in COVID associated invasive sinusitis. Demographic details of the patients and clinical presentation were documented. Rhinological examination was done and a nasal swab was taken for KOH mount along with Gram`s stain and Culture and Sensitivity. All Patients underwent radiological evaluation by contrast enhanced computed tomography (CECT) or MRI. Liposomal Amphotericin B was started. Surgical debridement done. Amphotericin-B was stopped in cases reported negative for fungal elements and antibiotics administered for two weeks. Outcome of treatment was documented. A total of 33 patients were included in the study. 48.5% patients were found to have bacterial infection and 27.3% patient’s fungal infections and 24.2% mixed infections.Eschar formation, necrotic tissue, erosion of the lamina papyracea was seen in both Klebsiella (33.3%) and Staphylococcal infections (16.6%) similar to Mucor and mixed infections. Persistent opthalmoplegia and deterioration of vision was associated with Mucor and mixed infections. However improvement in proptosis, ptosis, ophthalmoplegia, and vision was observed in cases associated with bacterial invasive sinusitis. Invasive bacterial sinusitis was under diagnosed during second wave of COVID. Identification of invasive bacterial sinusitis can help in de-escalation of treatment.
Keywords: Invasive sinusitis, Orbital complications, Mucor mycosis, COVID, Debridement, Liposomal Amphotericin
Introduction
COVID is a multisystem disease with life threatening events like pneumonia, acute respiratory distress due to cytokine storm, cerebrovascular thrombosis, acute abdomen resulting from acute mesenteric artery thrombosis and probable transient altered immunity. The second wave of COVID pandemic was associated with an outbreak of Mucormycosis among patients who were undergoing treatment, or who were recently treated for COVID in various countries particularly tropical regions.The global prevalence of Mucormycosis is 0.005 to 1.7 per million population. India contributed approximately 45% of the new COVID cases and 34% of the deaths globally during the peak of second wave of COVID pandemic [1].India also ranked highest for Mucormycosis in the world [2].Literature showed that India contributed to approximately two thirds (71%) of the global cases of Mucormycosis in COVID patients[3]. During the second wave of COVID pandemic in 2019–2020 the prevalence of Mucor in India compared to developed countries, was 80 times higher (0.14 per 1000)[4].
Invasive fungal sinusitis (IFS) can extend into orbit and cranial cavity. It has high mortality rates if not treated adequately and aggressively. The reported mortality rate due to COVID associated IFS is 29.6% [5].The mortality rate reaches 50-80% in cases with orbital and intracranial extension[6]. Early diagnosis and treatment is necessary to minimise morbidity and prevent mortality.
The increase in the incidence of invasive sinusitis among COVID patients is attributed to various factors like immunosuppresion, high glycemic index with raised glycated haemoglobin levels, oxygen support, inadvertent use of steroids, warm humid conditions in tropical areas [6]. According to literature, COVID virus affects pancreatic islets of Langerhans, macrophages and alters glucose regulating protein (GRP 78) [1, 7]. However, in this outbreak of COVID associated Mucormycosis, we found that few of these patients had bacterial invasive sinusitis mimicking fungal sinusitis in clinical presentation. This can mislead a physician. Wrong diagnosis and improper management can have a negative impact on the outcome. Amphotericin the only effective drug against Mucormycosis is highly toxic and expensive and not indicated in bacterial sinusitis. Early diagnosis with prompt treatment is crucial for saving vision as well as preventing further spread of infection. The purpose of this study is to share our experience in terms of clinical presentation, microbiology and histopatholgical features, management, complications, and outcomes in COVID associated invasive sinusitis presenting with orbital complications.
Objectives
To determine the exact etiologic agent of COVID associated invasive sinusitis presenting with orbital complications in this rural area.
To identify predisposing factors for orbital complications in COVID associated invasive sinusitis.
To document the outcome of treatment in patients presenting with COVID associated invasive sinusitis presenting with orbital complications.
Methodology
This retrospective observational study included 33 patients with COVID associated invasive sinusitis who were treated for orbital complications in a tertiary rural hospital which was also a COVID referral centre from April to June 2021. Institutional Ethics Committee approval was obtained vide No.SDUMC/KLR/IEC/604/2021–22 for conducting the study. Informed consent was obtained from the patients, or their next of kin (in case the patients had expired), for inclusion in the study. The clinical data was collected from in-patient records and Out Patient Department (OPD) follow-up visits. Those patients who had other orbital conditions leading to loss of vision like glaucoma, diabetic retinopathy, age-related macular degeneration, retinal detachment, optic neuritis were excluded from the study.
Demographic details of the patients and predisposing factors like COVID status, diabetic status, diabetic ketoacidosis if any, usage of systemic steroids were recorded. Clinical presentation with regards to ocular and orbital as well as nasal and para nasal symptoms were documented. Headache, orbital pain and other ocular manifestations like eyelid swelling, ptosis, proptosis, ophthalmoplegia, loss of vision were documented. Rhinological examination was done which included diagnostic nasal endoscopy to look for the presence of ulceration, necrotic debris or eschar, and a nasal swab was taken for KOH mount for fungal elements along with Gram`s stain and Culture and Sensitivity. All Patients underwent radiological evaluation by contrast enhanced computed tomography (CECT) of nose and paranasal sinuses and the extent of disease was documented. Magnetic resonance imaging (MRI) brain with orbits was done when intraorbital infection or intracranial was seen on CECT scan. Determination of etiological agent by laboratory diagnosis included bacterial culture and sensitivity, culture on Sabouraud`s media for fungus and histopathological examination of the debrided necrotic tissue. An assessment by ophthalmologist in all cases and neurosurgeon in cases with intracranial extension was done. Liposomal Amphotericin B was started (3 to 5 mg/kg/day). All patients underwent surgical debridement of the necrotic material and devascularised tissue within the nose and paranasal sinuses by endoscopic or by open approach. Patients who had orbital involvement underwent orbital decompression. Orbital exenteration was done in one case who had extensive involvement of the globe with loss of vision. Neurosurgical intervention depending on intracranial extension if any was documented. Intraoperative nasal swabs and tissue sample from eschar and necrotic debris were sent for KOH mount, Gram`s stain and bacterial and fungal culture on Sabourauds`s agar and for histopathology and results were documented. Amphotericin-B was stopped in cases reported negative for fungal elements. In patients whose nasal swabs showed bacteria, antibiotics based on culture and sensitivity were administered for 2 weeks. A repeat negative swab taken after two weeks was considered as an indication to stop the antibiotic. A total cumulative dose of Amphotericin-B depending on the severity and extent of the disease was 5 to 7 g in patients who had Mucormycosis. Patients were administered oral Posaconazole 400 mg twice a day for two weeks following discharge from hospital after completion of systemic Amphotericin-B therapy. Recurrence if any on 2 weekly follow up by diagnostic endoscopy for a period of three months and repeat CT scan of paranasal sinuses three months after treatment, was documented. Outcome of treatment with regards to eye movements, ptosis/proptosis if any and visual acquity were documented on Microsoft excel sheet SPSS(Statistical package for Social sciences) version 20. An analysis of the results by descriptive statistics and correlation of etiological agent with risk factors and outcome was done.
Results
Among the 33 patients with orbital involvement in COVID associated invasive sinusitis in this study, 29(87.7%) had unilateral disease and four (12%) had bilateral. Eighteen(54.5%) patients were being treated for COVID at the time of presentation of orbital symptoms and 15(45.4%) had been treated for COVID two weeks to four weeks prior to presentation with orbital symptoms. Mean duration of onset after recovery from COVID was 17 ± 3 days. All patients were found to be diabetic and had history of systemic steroids and oxygen support during COVID treatment. Among them, 24(72.7%) patients were known diabetics of which four (12%) were in ketoacidosis at time of presentation, nine (27.2%) were newly detected diabetics at the time of admission. The mean Glycated Haemoglobin was found to be 8.4 (range 7.2–12.5).The duration of oxygen support during COVID treatment ranged from six to 20 days with a mean of 11 days. Depending on the oxygen saturation levels all these patients were on oxygen support either via face mask (19 patients), high flow nasal oxygen (11 patients) or ventilatory support(three patients). On laboratory investigations 16(48.5%) patients were found to have bacterial infection and nine (27.3%) patients fungal infections (other than Mucor species Aspergillus in one and Candida in three) and eight (24.2%) mixed infections and were treated based on culture sensitivity reports.The mixed infections were predominantly by Kleibsiella in association with either Candida(five), Rhizopus (two), Mucor(three).
The most common clinical presentation was history of ipsilateral pain in the eye and face in 30(90%) and headache in 21(63.3%).There was found to be eye lid swelling in 14 (42.4%) patients, ptosis in 23(69.6%) patients, proptosis in five (15%), ophthalmoplegia in 17(51.5%) and visual impairment in 12(36.3%) as shown in Table 1 and Fig. 1.Diagnostic nasal endoscopy revealed the presence of extensive crusting in 29 patients and mucopurulent discharge in 16(48.4%),black eschar in nine (27.2%), necrotic tissue in 19(57.7%),pale mucosa or bluish mucosal discolouration of the inferior and middle turbinate in 17(51.5%),congested or polypoidal mucosa in the lateral wall of the nose and turbinates in six (18%) and bony sequestrum in nine (27.2%) patients. The presence of pale mucosa or bluish mucosal discolouration was specific of mucor and congested polypoidal mucosa of bacterial sinusitis. Eschar formation, necrotic tissue, erosion of the lamina papyracea on imaging was seen in both Klebsiella(33.3%) and Staphylococcal infections (16.6%) similar to Mucor and mixed infections.
Table 1.
Distribution based on clinical presentation and causative organism
| Rhino-orbital mucormycosis (RCOM) n = 9 |
Bacteria sinusitis with orbital complications (BOC) n = 16 |
Mixed infections causing sinusitis with orbital complications n = 8 |
|
|---|---|---|---|
| Ophthalmoplegia | 9(100%) | 4(25%) | 4(50%) |
| Ptosis | 9(100%) | 6(37.5%) | 8(100%) |
| Proptosis | 3(33.3%) | – | 2(25%) |
| Visual impairment | 8(88.8%) | – | 4(50%) |
| Intracranial extension | 4(44.4%) | 1(6.25%) | – |
Fig. 1.

Pre-operative presentation with ptosis, proptosis and conjunctival chemosis
The most common finding on CT scan of nose and paranasal sinuses was mucosal thickening in at least one paranasal sinus or a heterogenous soft tissue density in the paranasal sinuses- maxillary sinus 27(87.8%), ethmoids 22(66.6%), sphenoid sinus11(33.3%) with obliteration of osteomeatal complex 30(90.9%). Pansinusitis was seen in eight (24.2%) patients. Erosion of the lamina papyracea along with floor of the orbit was seen in six (18%) patients. Erosion of the sphenoid till the pterygoid plate was seen in one (3%) patient with mucor. Among 16 patients who underwent MRI brain and orbit, the most common finding was periorbital fat stranding 16(48.4%) along with retro orbital fat pad stranding in five(15% Mucor), features of sinusitis involving maxillary, ethmoids sinus with extension to inferior and medial wall of the orbit mostly unilateral in 15(45.4%), increased bulk of medial rectus and intra orbital fat stranding 10(30.3%)).Erosion of the lamina papyracea along with periorbital fat stranding and retro orbital fat pad stranding was a classical feature of Mucormycosis as shown in Figs. 2 and 3.The five (15%) patients who presented with intracranial extension showed one or more of the following findings- cavernous sinus thrombosis in two(6%) patients and internal carotid thrombosis in two(6%) patients, brain abscess(15%) involving the temporal lobe in two, fronto-parietal region in two and occipital in one patient. Intraoperative findings of medial orbital wall dehiscence, necrotic fat in the medial wall of the orbit was seen in six patients out of which one patient was with Klebsiella, one patient was with Staphylococcus and four patients was with Mucor infection. Skull base dehiscence was seen in three Mucor patients.Encasement of internal carotid artery in the lateral wall of sphenoid by necrotic tissue was noted in one patient with Mucor. Results shown in Table 2 and Table 3.
Fig. 2.
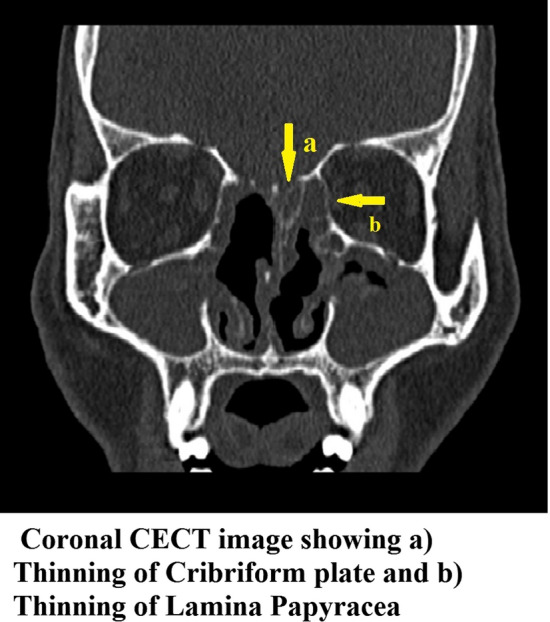
Coronal CECT image showing (a) thinning of cribriform plate and (b) thinning of lamina papyracea
Fig. 3.
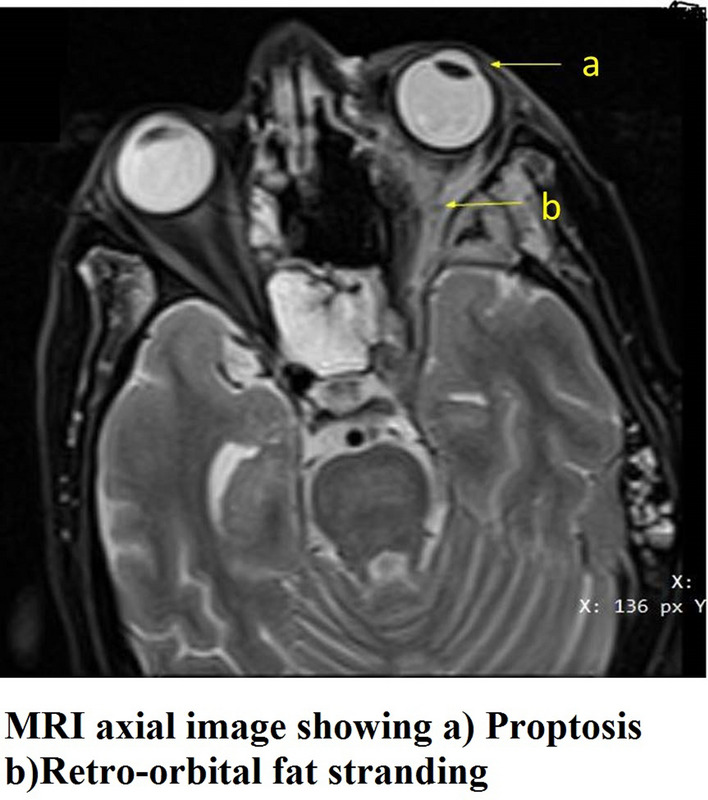
MRI axial image showing (a) proptosis, (b) retro-orbital fat stranding
Table 2.
Distribution of extent of Orbital involvement
| Rhino-orbital mucormycosis (ROM) n = 9 |
Bacteria sinusitis with orbital complications (BOC) n = 16 |
Mixed infections causing sinusitis with orbital complications n = 8 |
|
|---|---|---|---|
| Pre-septal cellulitis | 5(15%) | 6(18%) | 3(9%) |
| Orbital cellulitis | 4(12%) | 3(9%) | 3(9%) |
| Sub- periosteal abscess | 6(18%) | 5(15%) | 5(15%) |
| Orbital abscess | 2(6%) | 1(3%) | 2(6%) |
| Cavernous sinus thrombosis | 1(3%) | 1(3%) | – |
Table 3.
Organism- wise distribution of diagnostic nasal endoscopy features and imaging findings. Note K- Klebsiella, S- Staphylococuss, A- Acinetobacter, P-Pseudomonas)
| Features | Bacteria sinusitis with orbital complications | Rhino-orbital mucormycosis | Total |
|---|---|---|---|
| Diagnostic nasal endoscopy | |||
| Black eschar | 4(K -2, S- 2) | 5 | 9(27.2%) |
| Necrotic tissue | 12(K- 4, S- 4, A- 2, P-2) | 7 | 19(57.7%) |
| Pale /Bluish mucosa | 8(S-5, P- 3) | 11 | 17(51.5%) |
| Congested / polypoidal mucosa | 5 K | – | 5(15%) |
| Bony sequestrum | 4 K | 5 | 9(27.2%) |
| Imaging | |||
| Erosion of lamina papyracea and floor of the orbit | 3(K-2,S-1) | 3 | 6(18%) |
| Periorbital fat stranding | 6 (K-3,S-2,P-1) | 10 | 16(48.4%) |
| Retro orbital fat pad stranding | – | 5 | 5(15%) |
| Extension to inferior and medial wall of the orbit | 5(K-2,S-2,P-1) | 10 | 15(45.4%) |
| Increased bulk of medial rectus and intra orbital fat stranding | 1 K | 9 | 10(30.3%) |
| Intracranial extension | 1 K | 4 | 5(15%) |
| Cavernous sinus thrombosis | 1 K | 1 | 2(6%) |
| Internal carotid thrombosis | – | 2 | 2(6%) |
| Brain abscess | 1 K | 4 | 5(15%) |
Orbital decompression was done in 29(87.7%) patients, orbital exentration in one (3%) patient and total maxillectomy in three (9%) patients. One patient developed optic neuritis during the course of treatment. An additional intracranial intervention like craniotomy and debridement was done for five (15%) patients. Of the 14 (42.4%) patients who had eye lid swelling, pre-septal cellulitis was found in six patients, conjunctival chemosis was seen in three patients and peri-orbital oedema in four patients and visual impairment in 12(36.3%) with perception of light present in four (12%) patients, and absent in three (3%) patients, and fixed eye with total loss of vision in three(9%) patients. The features of pre-septal cellulitis and peri-orbital oedema was predominantly associated with bacterial type of invasive sinusitis.
Pansinusitis and intra cranial extension was seen in association with one patient with Klebsiella associated invasive sinusitis. Optic neuritis was seen in mixed infection—Klebsiella with Candida, which was managed conservatively and showed response to treatment. At the end of three months of follow-up period, the symptoms of opthalmoplegia, ptosis, pre-septal cellulitis and peri-orbital oedema showed good response with improvement of ptosis (nine out of 23, 39%), eye lid edema (10 of 14, 71%), ophthalmoplegia (six of 17, 35%) and vision(six of 12, 50%) as shown in Table 4 and Fig. 4. Patients who had fixed eye with total loss of vision in three patients showed no improvement and one patient had to undergo orbital exentration. At the end of three months of follow up it was noted that persistent opthalmoplegia and deterioration of vision was associated with Mucor and mixed infections. However improvement in proptosis, ptosis, ophthalmoplegia, and vision was observed in cases associated with bacterial invasive sinusitis caused by Klebsiella and Staphylococcus.
Table 4.
Correlation of etiological agent with outcome
| Etiological agent | Outcome of treatment | ||||||
|---|---|---|---|---|---|---|---|
| Ptosis recovered | Ocular motility improved | Vision improved | Total | ||||
| Yes | No | Yes | No | Yes | No | ||
| Pseudomonas | 2 | 1 | – | 3 | – | 3 | 3 |
| 67% | 33% | 100% | 100% | ||||
| Klebsiella | 2 | 3 | 2 | 3 | 2 | 3 | 5 |
| 40% | 60% | 40% | 60% | 40% | 60% | ||
| Staphylococcus | 4 | 1 | 3 | 2 | 3 | 2 | 5 |
| 80% | 20% | 60% | 40% | 60% | 40% | ||
| Acinetobacter | 1 | 2 | 1 | 2 | 1 | 2 | 3 |
| 33% | 67% | 33% | 67% | 33% | 67% | ||
| Mucorales | – | 8 | – | 8 | – | 8 | 8 |
| 100% | 100% | 100% | |||||
| Aspergillus | – | 1 | – | – | – | 1000% | 1 |
| 100% | |||||||
| Mixed infections | 3 | 5 | – | 8 | – | 8 | 8 |
| 38% | 62% | 100% | 100% | ||||
Fig. 4.

Image showing post operative residual ptosis
Discussion
The second wave of COVID was associated with sudden outbreak of invasive sinusitis.This morbid infection was seen not only in active but also in recently recovered patients of COVID in association with co-morbid medical conditions like uncontrolled diabetes, high oxygen flow dependence and treatment with large doses of steroids. Life threatening opportunistic infections following COVID are predisposed to immune dysfunction due to lymphopenia, thrombocytopenia, ACE 2 mediated multi organ damage [7].
COVID induces an increase in serum ferritin levels due to altered iron metabolism. Raised intracellular iron concentration generates reactive oxygen resulting in tissue damage [3]. Hyperglycemic state, mild acidic environment, endothelial receptor GRP (78) induced endothelial dysfunction, hyper-ferritinemic state with an affinity of mucor to free iron provide a perfect milieu for the development of Mucormycosis [7, 7]
An increased adhesion and penetration of Mucorales into the endothelium of blood vessels triggers thrombosis [1].Endothelial cell injury and thrombotic events are considered as the possible factors that promote the growth and spread of fungus. The rapidly spreading arteritis and wide spread thrombosis results in ischemia, necrosis and ischemic infarction leading to necrosis and an eschar formation [8]. Poorly controlled diabetes mellitus, decrease in the iron binding capacity and phagocyte dysfunction, promote growth and virulence of the fungi [10, 11].Invasive sinusitis in immunocompromised is not only a threat to vision but also to life [11]. Patients with invasive sinusitis succumb from extensive disease as a result of rapid invasion resulting in intracranial extension. A major challenge for early diagnosis and treatment is lack of access to microbiological and histopathological supporting evidence due to fear and stigma in a highly contagious and deadly pandemic [1].
The meta-analysis done by Hussain S et al. showed that the global prevalence of COVID acquired Mucormycosis was 0.7%.The analysis also showed a statistically significant difference in the prevalence of fungal co-infections between Asian and European populations(15:7 cases per 1000 patients).The prevalence of Mucormycosis among the diabetic patients was also found to be 50 times higher in Indians (0.14 cases per 1000 patients).The mean age for COVID associated Mucormycosis was 62.12 ± 9.69 years[5]. Our study population in comparison were found to involve patients who were a decade younger (mean age 47.3%).The mean duration of Mucormycosis onset was 14.59 ± 6.88 days after the COVID-19 diagnosis which was similar to our study where the onset of invasive sinusitis was 17 ± 3 days after recovery from COVID.
The prevalence of associated factors like diabetes was 74.5% and exposure to steroids was 94.3% in the study by Hussain S et al. whereas a multicenteric study by Prakash et al. showed 50% of Mucormycosis cases had diabetes mellitus [5, 9]. However all patients (100%) in our study were diabetics at presentation and 12% of the patients were in diabetic ketoacidosis (DKA).
As per the systematic review by AK Singh, COVID associated Mucormycosis was predominant in males (78.9%) either active (59.4%) or recovered (40.6%) with 80% of cases with diabetes mellitus (DM) and 15% in diabetic ketoacidosis (DKA) and 76.3% of cases were on corticosteroid [9].
Contrary to the other studies in literature which reported headache and pansinusitis as the common presentation, our patients presented with ipsilateral pain in the eye and face in 30(90%) apart from headache in 21(63.3%) and pansinusitis was seen in only 24.2% [5].
All our patients (100%) were on oxygen support for an average of 11 days. Mucosal injury resulting from high flow oxygen under pressure, mechanical ventilation with a possible bacterial and fungal contamination of the oxygen humidifiers and usage of non-sterile/ tap water in humidifiers are considered as the risk factors for invasive sinusitis and Mucormycosis among COVID patients [7, 12]. Indian council of Medical Research (ICMR) national task force for COVID recommended using clean, sterile water for humidifiers during oxygen therapy [13].
The outbreak of COVID associated invasive fungal sinusitis showed a tendency for specific tropical areas resulting in endemic like situation in these areas. The possibility is local practices, excessive occupational exposure to fungal spores as in agricultural and food processing professions. The vulnerable factors are history of exposure to dust and fodder, and traumatic inoculation during procedures like lacrimal syringing [13, 14]. In contrast to this only 27% (nine of the 33 patients) in our study were farmers and none of them had any history of trauma.A study conducted by Amanati et al. found that orbital Mucormycosis can develop even in the absence of risk factors.
The study done by Cayir and Ozkurt et al. showed that orbital complications are predominantly associated with ethmoid sinusitis but can also be seen in the presence of maxillary, frontal and rarely with sphenoid sinusitis [15]. In 80% of the cases rapid spread of infection from acute ipsilateral bacterial ethmoiditis results in devastating complications like ophthalmoplegia and proptosis [17].The various modes of spread of infection to orbit is by direct, venous, lymphatic or perineural spread.The mechanism of direct regional spread is by osteitis in compact bones and osteomyelitis in diploic bones.The predominant causative organism is mainly Staphylococcus or Streptococcus species apart from Haemophilus Influenza and anaerobes [15, 17].
In our series KOH Studies and histopathological confirmatory studies showed evidence of fungi like Rhizopus, Mucor, Aspergillus and Candida in 51.5%(17 out of 33) of our patients. In contrast to COVID related Global surge in the incidence of Mucormycosis we found that 48.4%(16 of 33 patients) had bacterial invasive sinusitis mimicking as fungal sinusitis.The bacteria was predominantly Klebsiella, Pseudomonas followed by Methicillin resistant staphylococcus(MRSA). The features of pre-septal cellulitis and peri-orbital oedema, pansinusitis and intra cranial extension (3.03%) was seen in association with Klebsiella associated infections. A similar study done by Twu KH et al. also confirmed bacterial co-infection with Fungal rhinosinusitis [16]. He reported that predominant fungal agent was Aspergillus followed by Mucor and the bacterial agents were Hemophilus influenza and Staphylococcus aureus. This microbial spectrum differed from our study. Bacterial tendency for either biofilm formation or complement resistance in the setting of impaired host immunity and breach in mucosal barrier facilitates fungal invasion in both immunocompromised and immunocompetent patients [16].
Contrary to the belief that black eschar and pale and bluish discolouration of turbinates is a cardinal feature of Mucormycosis we found it was present (44.4% of and 47% respectively) in patients with bacterial sinusitis. Klebsiella sinusitis was found to erode lamina papyracea in 33.3% of patients of bacterial invasive sinusitis. Intracranial extension and cavernous sinus thrombosis was also seen in bacterial sinusitis but at a lesser extent compared to Mucor. After completion of treatment all patients who had invasive fungal sinusitis did not have improvement in ptosis, vision or ocular motility. But bacterial invasive sinusitis except for Pseudomonas showed improvement in vision. However mixed infections did not show any significant improvement. In bacterial invasive sinusitis the orbital symptoms and vision improved probably due to reduction in oedema and drainage of pus. The persistence of sequelae of orbital complications in bacterial sinusitis may be due to thrombosis, devascularisation and extensive erosion.
As per the systematic review for Mucormycosis by Turner JH, orbital invasion was present in 49.6%, intracranial extension in 21.2% and cavernous sinus thrombosis in 8.6% [17].Our study also showed similar results with intracranial extension more with Mucor that is in four (12%) patients. Only one patient with Klebsiella presented with intracranial abscess which resolved with antibiotics. Cavernous sinus thrombosis was seen both in bacterial as well as Mucor (one patient in each group).Ischaemic necrosis and necrotising arteritis due to intraluminal spread of the organism secondary to septic thrombosis is considered for invasive bacterial sinusitis similar to angio-invasion by Mucorales. The outcome in terms of improvement in vision and ocular motility in those who had bacterial invasive sinusitis was good following surgical debridement and administration of antimicrobials in comparison with Mucor associated and mixed infections where the orbital sequelae persisted after treatment.
We also found that limited disease restricted anatomically to paranasal sinuses had good prognosis both with bacterial as well as fungal invasive sinusitis. The imminent spread of infection to the orbit even with aggressive surgical debridement did not benefit salvage of vision in Mucormycosis.
The other important factor for conservation of orbit and vision is aggressive correction of underlying metabolic derangement. Total ophthalmoplegia with loss of vision is either due to central retinal artery occlusion or thrombosis of posterior ciliary arteries or infarction of intraorbital part of optic nerve resulting in frozen eye [19].This is the indication for orbital exenteration which is lifesaving. Intracranial extension occurs mainly through cribriform plate and orbital apex. Cavernous sinus thrombosis and carotid artery occlusion leads to hemiplegia, hemiparesis and even death [17–19]. One patient in our study who had developed hemiplegia due to internal carotid artery thrombosis and one patient who had skull base dehiscence and exposure of internal carotid artery died at two half months of follow up. The remaining three patients post craniotomy for intracranial extension had no residual neurological deficits. A systematic review on Mucormycosis showed loss of vision in 32% which is almost similar to our results (36%) [9].
Study by Hussain S etal. has shown the overall mortality rate in COVID associated Mucormycosis as 29.6% [3]. Mortality rates for IFS reported in literature ranged from 17.8 to 85.7% and overall mortality rate due to invasive bacterial sinusitis was found to be 2.6%.In our study the mortality was due to IFS (6%) and was not related to bacterial orbital extension. The lower mortality for IFS in our series may be due to aggressive surgical debridement and antifungal therapy. Surgical debridement is the mainstay of treatment. Combination therapy with two antifungal agents either Liposomal Amphotericin B and Isavuconazole or Posaconazole has been recommended for all rhino–orbital–cerebral Mucormycosis [4]. Our strict adherence to this protocol which included aggressive surgical debridement and liposomal Amphotericin B based antifungal therapy and two weeks of Posaconazole after discharge, probably reduced the mortality in our study. Only 12% of the patients in our study had residual disease and underwent a second debridement.
Conclusion
Invasive fungal sinusitis is associated with threat to vision and life and has high mortality rates if inadequately treated particularly in diabetics.Orbital invasion and intracranial spread increase morbidity and mortality.Invasive bacterial sinusitis was under diagnosed during second wave of COVID due to outbreak of COVID associated Mucormycosis and similarity in clinical and radiological features. High index of suspicion, early and accurate diagnosis, aggressive surgical debridement in mucor, and appropriate antimicrobial treatment can minimise mortality and morbidity and save the vision in invasive sinusitis patients.Though the clinical and radiological features of Mucormycosis and invasive bacterial sinusitis can overlap, congested and polypoidal mucosa and absence of pale and blanched mucosa should indicate invasive bacterial sinusitis. Identification of invasive bacterial sinusitis in cases of suspected Mucor can help in de-escalation of treatment particularly stopping toxic Amphotericin. It also carries better prognosis.
Funding
None.
Declarations
Conflict of interest
The Authors declare that there is no conflict of interest.
Ethical Approval
Institutional Ethics Committee approval was obtained vide No.SDUMC/KLR/IEC/604/2021–22 for conducting the study.
Informed Consent
Informed consent was obtained from the patients, or their next of kin (in case the patients had expired), for participation in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Raut A, Huy NT. Rising incidence of Mucormycosis in patients with COVID-19: another challenge for India amidst the second wave? Lancet Respir Med. 2021;9(8):E77. doi: 10.1016/S2213-2600(21)00265-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prakash H, Chakrabarthi A. Global epidemiology of Mucormycosis. J Fungi. 2019;5(1):26. doi: 10.3390/jof5010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.John TM, Jacob CN, Kontoyiannis DP. When uncontrolled diabetes mellitus and severe COVID-19 converge: the perfect storm for Mucormycosis. J Fungi. 2021;7:298. doi: 10.3390/jof7040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar A, Verma M, Hakim A, et al. Epidemiology of Mucormycosis during second wave of COVID-19 in a tertiary care institute in western Rajasthan, India. Cureus. 2022;14(3):e22973. doi: 10.7759/cureus.22973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hussain S, Riad A, Singh A, Klugarová J, Antony B, Banna H, Klugar M. Global prevalence of COVID-19-associated Mucormycosis(CAM): living systematic review and meta-analysis. J Fung. 2021;7:985. doi: 10.3390/jof7110985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fadda GL, Martino F, Andreani G, Succo G, Catalani M, Di Girolamo S, Cavallo G. Definition and management of invasive fungal rhinosinusitis: a single-centre retrospective study. Acta Otorhinolaryngol Ital. 2021;41:43–50. doi: 10.14639/0392-100X-N0848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sabirli R, Koseler A, Goren T, Turkcuer I, Kurt O. High GRP78 levels in Covid-19 infection: a case-control study. Life Sci. 2021;265:118781. doi: 10.1016/j.lfs.2020.118781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pandiar D, Kumar NS, Anand R, Kamboj M, Narwal A, Shameena PM. Does COVID19 19 generate a milieu for propagation of Mucormycosis? Med Hypo. 2021;152:110613. doi: 10.1016/j.mehy.2021.110613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wali U, Balkhairb A, Al-Mujainia A. Cerebro-rhino orbital Mucormycosis: an update. J Infec Public Health. 2012;5:116–126. doi: 10.1016/j.jiph.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Prakash H, Ghosh AK, Rudramurthy SM, Singh P, Xess I, Savio J, Pamidimukkala U, Jillwin J, Varma S, Das A, et al. A prospective multicenter’ study on Mucormycosis in India: epidemiology, diagnosis, and treatment. Med Mycol. 2019;57:395–402. doi: 10.1093/mmy/myy060. [DOI] [PubMed] [Google Scholar]
- 11.Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. 2021;15(4):102146. doi: 10.1016/j.dsx.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mukherjee B, Raichura ND, Alam MS. Fungal infections of the orbit. Ind J Oph. 2016;64:337–345. doi: 10.4103/0301-4738.185588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakipoglu Y, Erturan Z, Buyukbaba-Boral O, Aksozek A, Aydin S, Derbentli S. Evaluation of the contaminant organisms of humidifier reservoir water and investigation of the source of contamination in a university hospital in Turkey. Am J Infect Control. 2005;33:62–63. doi: 10.1016/j.ajic.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 14.Indian Council of Medical Research, New Delhi. https://www.icmr.gov
- 15.Amanati A, Barzegar H, Pouladfar G, Dashti AS, Abtahi MB, Khademi B, Ashraf MJ, et al. Orbital Mucormycosis in immunocompetent children; review of riskfactors, diagnosis, and treatment approach. BMC Inf Dis. 2020 doi: 10.1186/s12879-020-05460-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Skaria J, John TM, Varkey S, Kontoyiannis DP. Are unique regional factors the missing link in India’s COVID-19-associated Mucormycosis crisis? MBio. 2022;13(2):e00473. doi: 10.1128/mbio.00473-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Çayir S, Kayabaşi S. An approach to orbital complications in rhinosinusitis. ENT Updates. 2019;9(3):180–184. [Google Scholar]
- 18.Saltagi MZ, Rabbani CC, Patel KS, Wannemuehler TJ, Chundury RV, Illing EA, Ting JY. Orbital complications of acute sinusitis in pediatric patients: management of chandler III patients. Allergy Rhinol. 2022;13:1–9. doi: 10.1177/21526575221097311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turner JH, Soudry E, Nayak JV, Hwang PH. Survival outcomes in acute invasive fungal sinusitis: a systematic review and quantitative synthesis of published evidence. Laryngoscope. 2013;123:1112–1118. doi: 10.1002/lary.23912. [DOI] [PubMed] [Google Scholar]


