Abstract
Background
Tympanoplasty is the most common operation performed by an Otolaryngologist worldwide.Type 1 tympanoplasty involves repair of pars tensa of tympanic membrane, when the middle ear is normal. The most widely used method is underlay technique using temporalis facia. In buttonhole tympanoplasty, the temporalis fascia is anchored to the handle of malleus through the buttonhole.
Objective
To compare and analyze graft uptake and hearing outcome in button hole technique and underlay technique.
Material and Method
It is a comparative study done at tertiary care center, where patients suffering from tubotympanic type of chronic otitis media with medium sized perforation with moderate conductive hearing loss, within age group of 18–60 years,were selected.
Results
In Button hole tympanoplasty group the mean hearing gain was 9.3dB, and 8.17 dB in Underlay tympanoplasty group which was statistically significant (p < 0.05) but P value between Button hole and Underlay tympanoplasty was not statistically significant.With regard to graft uptake 96.7% showed graft uptake in Buttonhole tympanoplasty group and in underlay tympanoplasty the graft uptake was 93.3%.
Interpretation and Conclusion
Buttonhole technique is better in terms of graft uptake since the graft is anchored to the handle of malleus, and postoperatively medialisation of graft and other complications like lateralization of graft, epithelial pearl formation and anterior blunting is prevented. Both techniques are good in terms of hearing improvement for chronic otitis media with medium sized perforation with moderateconductive hearing loss.
Keywords: Chronic Otitis Media, Tympanoplasty, Button hole Technique, Underlay Technique
Introduction
Chronic otitis media (COM) is an inflammatory process in the middle ear space that results in long term or permanent changes in the tympanic membrane including atelectasis, dimeric membrane formation, perforation, tympanosclerosis, retraction pocket or cholesteatoma [1]. The global burden of illness from COM involves 65–330 million individuals with draining ears, 60% of whom (39–200 million) suffer from significant hearing impairment [2]. Tympanoplasty is a commonly performed procedure in COM. It is defined as a surgical procedure to eradicate disease in the middle ear and to reconstruct the hearing mechanism, with or without mastoid surgery and with or without tympanic membrane grafting [3].
Type 1 tympanoplasty involves repair of pars tensa of tympanic membrane, when the middle ear is normal. The most widely used method is underlay technique using temporalis facia. In buttonhole tympanoplasty, the temporalis fascia is anchored to the handle of malleus through the buttonhole. The advantages of this technique intraoperative is that since the graft is anchored to the handle of malleus, all around movement of the graft is possible and the graft doesn’t fall back over the medial wall of middle ear, so this aids in the creation of neotympanum. The postoperative benefit is that, with the proper placement and anchoring, anterior retraction and blunting is prevented and since the graft is firmly held in position, chances of medial retraction and adherence to promontory are prevented [4].
Thus this study aims to compare the post-operative hearing improvement in buttonhole technique of myringoplasty with underlay technique and to compare the graft uptake in both.
Materials and Methods
It’s a Simple Prospective Study conducted at a tertiary care hospital from November 2017 to MAY 2019. 60 patients aged between 18 and 60 years with chronic otitis media, mucosal type with medium sized central perforation, with mild to moderate conductive hearing loss presented to ENT Out Patient Department were taken up for the study. CSOM with large perforation, CSOM with cholestaetoma, Otitis media with mixed hearing loss & sensorineural hearing loss, Patients with hearing loss of more than 60Db and Traumatic perforations of tympanic membrane were excluded from study.
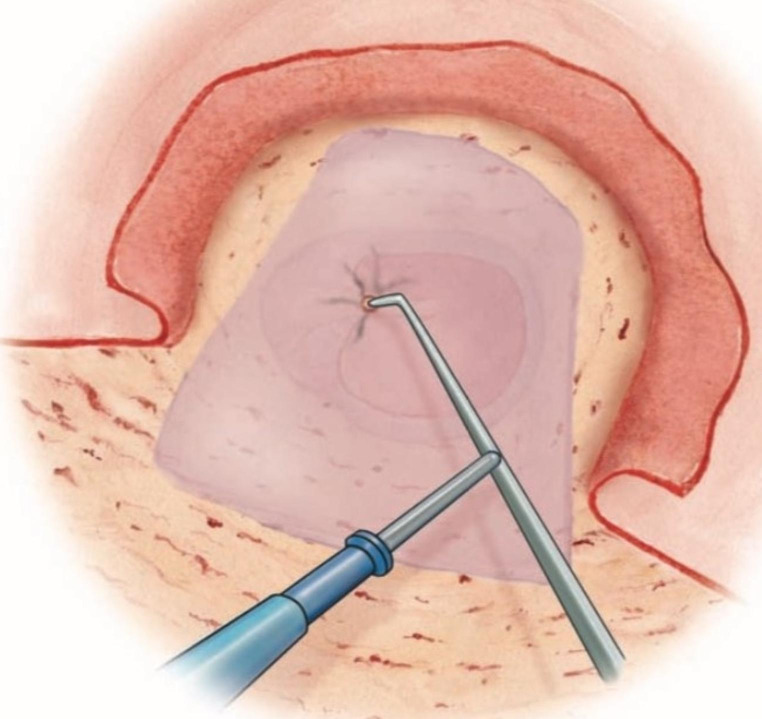
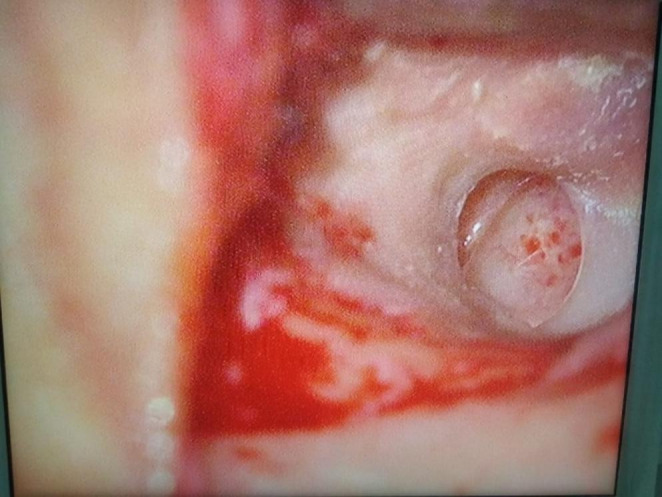
Informed written consent for the study was obtained from all the patients. Patients were randomly selected for either of the techniques; Type 1 Tympanoplasty by buttonhole technique and underlay technique. The participants were allocated into two groups using computer based table of random numbers. Group A contained 30 patients who underwent Type I tympanoplasty by buttonhole technique method and Group B contained 30 patients who underwent Type I tympanoplasty by underlay method. In both these methods temporalis fascia graft was used. Detailed clinical history was taken and examination was carried out as per the proforma prepared. Relevant Laboratory investigations was done. All patients were subjected to pre-operative Otoendoscopy (Fig. 1) and Pure Tone Audiometry (PTA). They were followed up at third month post operatively (Fig. 2).The success of graft uptake was assessed by otoendoscopic examination. Postoperative improvement in hearing was assessed by Pure Tone Audiometry. The success of surgery was defined as complete closure of tympanic membrane perforation and post- operative improvement in hearing.
Fig. 1.
Preoperative otoendoscopy
Fig. 2.

Endoscopic picture of 3rd month otoendoscopy
All 60 cases were done by a single surgeon.
The data was statistically analyzed using the student’s t test, Chi square test and Fisher Exact Test.
Technique
Tympanoplasty can be performed using local or general anesthesia. Local injection of 1% lidocaine with epinephrine (1:100,000) provides excellent vasoconstriction for transcanal procedures. A 26 gauge needle mounted on a 2 mL syringe is recommended for ear canal injections. The canal injections consist of infiltrating slowly 1 mL of solution in 3, 6, 9 and 12 O’ clock positions each at the bony cartilaginous junction of EAC till the entire skin blanches. Slow infiltration will avoid the formation of a bleb beneath the canal skin that may obscure the surgical field. Half ml of the solution is injected each in the helico-tragal junction and anterior to tragus for additional block to the auriculotemporal nerve. Post auricular infiltration consists of injection along the post auricular sulcus, in the temporalis region and under the periosteum over the mastoid cortex. A sub periosteal injection will dissect freely under the skin and provide excellent vasoconstriction and anesthesia [5]. A post auricular incision is made about 3 mm behind the post auricular crease using a No.15 scalpel blade. Temporalis fascia graft is harvested and teased out to a thin layer.Middle ear is exposed by making a T-shaped incision is made through the subcutaneous tissue & periosteum to the bone overlying the mastoid & linea temporalis. A posterior meatotomy is done just below the Spine of Henle. The pinna is retracted forward with the help of ribbon gauze and a mastoid retractor is placed. The margin of the perforation is freshened, the undersurface of the drum remnant is then denuded of squamous epithelium using a sickle knife & a cupped forceps (Fig. 1). The manubrium of the malleus is denuded, preserving the fibrous annulus. In underlay technique same intial steps are followed and that middle ear is packed with gel foam and the graft material is placed medial to the perforation after trimming the graft to its required size and shape. The vascular strip is replaced into ear canal [6].
Button Hole Technique
Using a needle the position of the graft is adjusted to cover the denuded bone of the meatus with a minimum overlap of 5 mm. A mark is made on the graft with an electocautery needle at the level of the superior half of the malleus handle (Fig. 3) [7]. The graft is removed and placed on a wooden tongue depressor.
Fig. 3.
Making mark on the graft at the level of superior half of malleus handle
A small buttonhole is cut on the cauterized mark (Fig. 4). The graft is then replaced and the tip of the manubrium is passed through the buttonhole using micro suction and a needle (Fig. 5) [7]. The graft is positioned to cover the annulus and a denuded bone of the meatus with a minimum overlap of 5 mm all around to avoid blunting. (Fig. 6). The conical aspect of the tympanic membrane must be restored (Fig. 7) [7]. After inspecting the middle ear for the ossicular integrity, the entire tympanomeatal flap is placed back into its original position, fine adjustments made and the graft placement is checked all around. The same medicated gel foam is placed over the graft in the bony canal.The post aural incision is closed by mattress sutures using 3 − 0 Ethilon in a single layer. Finally the external auditory canal is packed with medicated gelfoam and mastoid dressing is applied.
Fig. 4.

Temporalis fascia with button hole
Fig. 5.
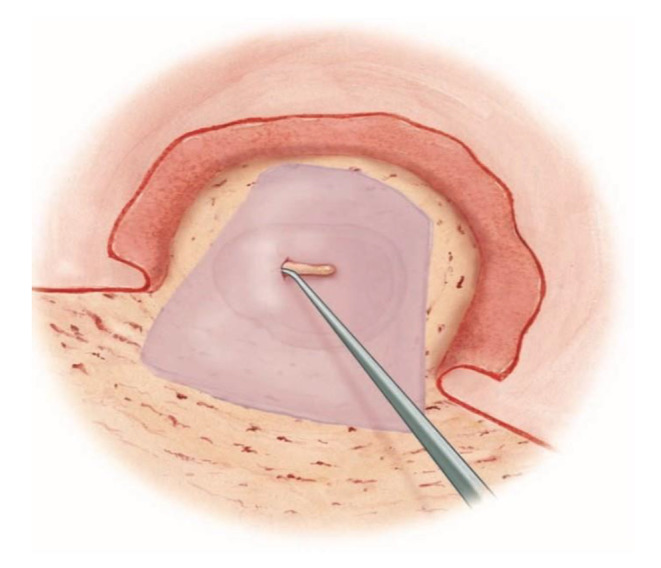
Tip of malleus passed through the buttonhole
Fig. 6.
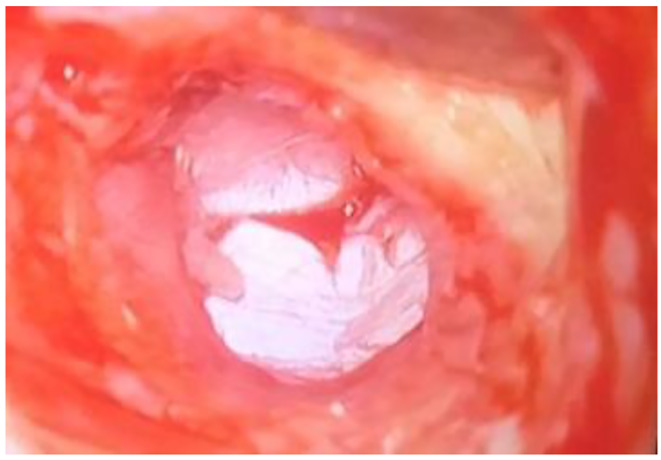
Closure of perforation after graft
Fig. 7.

Graft repositioned to cover the annulus
Results
60 patients with chronic otitis media with medium sized central perforation were enrolled.
The patients included in this study were of age 18 to 60 years (Table 1). Most common age group involved in the study were between 29 to 38 years (43.3%). (Chart 1)
Table 1.
Age distribution in two groups of patients studied
| Age group | Button hole(N = 30) | Percentage | Underlay | Percentage |
|---|---|---|---|---|
| 19–28 | 04 | 13.3% | 05 | 16.7% |
| 29–38 | 13 | 43.3% | 10 | 33.3% |
| 39–48 | 10 | 33.3% | 10 | 33.3% |
| 49–58 | 03 | 10% | 05 | 16.7% |
Chart 1.

Age distribution in two groups of patients studied
In our study in button hole technique there is equal distribution of male and female and in underlay technique there is a slight female preponderance. (Table 2, Chart 2).
Table 2.
Gender distribution in two groups of patients studied
| Gender | Buttonhole technique | Percentage | Underlay technique | Percentage |
|---|---|---|---|---|
| Female | 15 | 50% | 17 | 56.67% |
| Male | 15 | 50% | 13 | 43.33% |
| Total | 30 | 100% | 30 | 100% |
Chart 2.
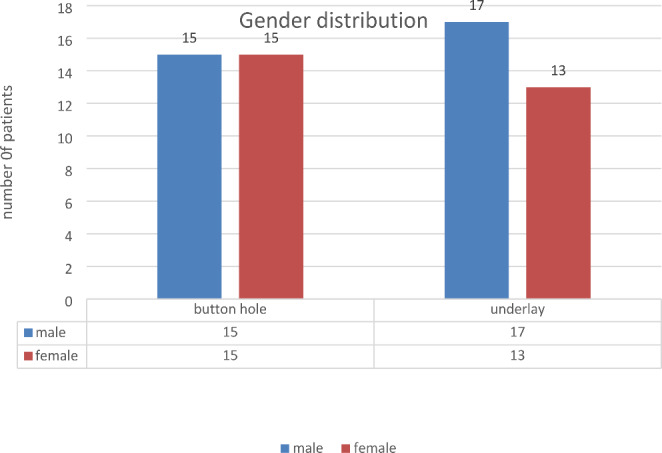
Gender distribution in two groups of patients studied
Table 3.
PTA distribution in two groups of patients studied
| Ab gap(PRE OP) | Button hole | Underlay |
|---|---|---|
| < 30dB HL | 10(16.7%) | 12(13.3%) |
| 30–40 dB | 20(83.3%) | 18(86.7%) |
| TOTAL | 30 | 30 |
In our study in both button hole technique and underlay technique there is equal distribution of right and left COM. (Chart 3). Patient’s hearing loss in decibels (pre-operative): Pre-operative Pure tone audiometry amongst the groups suggested that, in buttonhole tympanoplasty group 10 patients and in underlay tympanoplasty group 12 patients were having air bone gap < 30 dB.
Chart 3.
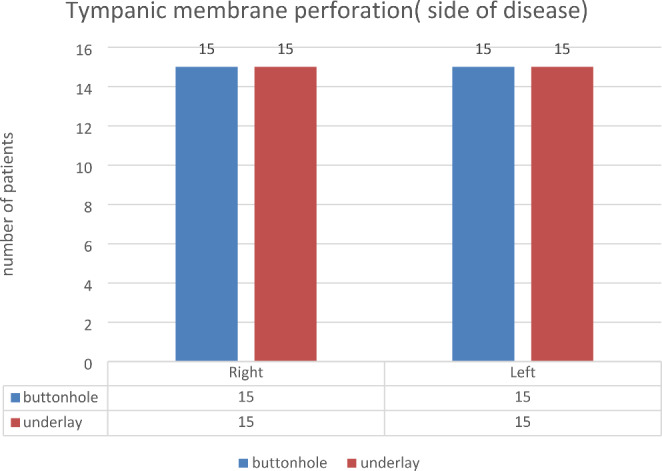
Tympanic membrane perforation distribution in two groups of patients studied
20 patients with 30–40 dB air bone gap belonged to the buttonhole tympanoplasty group and18 patients were from the underlay tympanoplasty. (Table 4).
Table 4.
Hearing gain in two groups of patients studied
| Hearing Gain | Buttonhole | Underlay |
|---|---|---|
| <=5 | 02 | 08 |
| 6–10 | 15 | 11 |
| > 10 | 13 | 11 |
| Total | 30 | 30 |
| Mean ± SD | 9.33 ± 3.24 | 8.20 ± 3.39 |
Audiometry done post operatively after 6 months showed that, in buttonhole technique group 29 out of 30 patients and in underlay technique all 30 patients were having air bone gap of < 30 dB.
30–40 dB hearing loss was seen in only one patient belonging to buttonhole technique group. (Chart 4). Post-operative audiometry was performed after 6 months duration. Hearing gain in two groups of patients studied, showed that 02 patient in buttonhole tympanoplasty and 08 patients in underlay tympanoplasty group had < = 5dB hearing improvement and 15 patients in buttonhole tympanoplasty group and 11 patients in underlay tympanoplasty group had hearing gain of between 5 and 10 dB, and > 10dB hearing gain was seen in 13 patients in buttonhole tympanoplasty group and 11 patients in underlay tympanoplasty group (Table No. 4).
Chart 4.
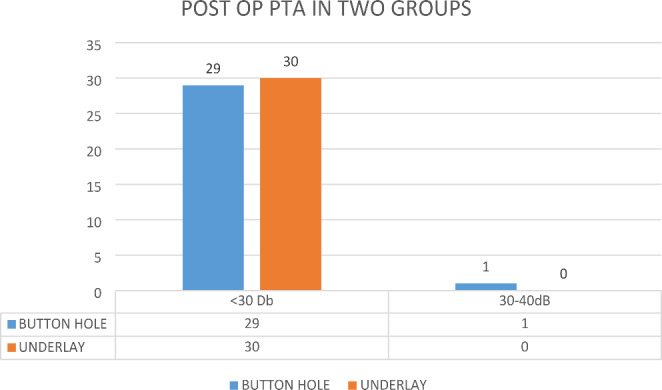
Post op PTA distribution in two groups of patient’s studied
Majority of patients had a hearing improvement between 5-10db, 15patients in buttonhole tympanoplasty and 11patients in underlay tympanoplasty group.
With regard to graft uptake 96.7% showed graft uptake in Buttonhole tympanoplasty group with one case of residual perforation and in underlay tympanoplasty the graft uptake was 93.3% with 2 cases of residual perforation and in 1 case there was medialisation of graft (Chart No 5). There was no intraoperative (bleeding, facial nerve palsy, chorda tympani nerve injury, wound hematoma) and postoperative complications (infections, bleeding, wound gaping, facial paralysis perichondritis, epithelial pearl formation, granulation tissue formation at the tympanomeatal flap or sensorineural hearing loss) noted in both the groups. Comparing both groups graft uptake was not statistically significant.
Chart 5.
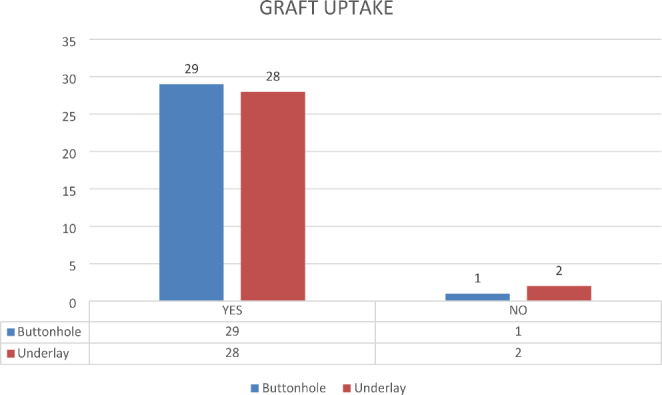
Graft uptake in two groups of patients studied
Statistical Methods
Student t test was used for the mean hearing improvement and to compare the mean of hearing gain between the two groups.
Chi-square/ Fisher Exact test has been used to find the significance of study parameters on categorical scale between two or more groups.
In Button hole tympanoplasty group the mean hearing gain was 9.3dB dB, and 8.17 dB in Underlay tympanoplasty group which was statistically significant (p < 0.05) but P value between group Button hole and Underlay tympanoplasty was not statistically significant (Tables 5 and 6).
Table 5.
Comparison of AB GAP Pre and Post 3 Months
| AB GAP | Pre | Post 3 Months | Difference | P Value |
|---|---|---|---|---|
| Button Hole | 32.43 ± 4.46 | 29.53 ± 3.7 | 2.90 ± 2.17 | 0.0001 |
| Underlay | 32.00 ± 4.56 | 29.43 ± 4.96 | 2.57 ± 1.28 | 0.0001 |
Table 6.
Comparison of AB GAP Pre and Post 6 Months
| AB GAP | Pre | Post 6 Months | Difference | P Value |
|---|---|---|---|---|
| Button Hole | 32.43 ± 4.46 | 23.13 ± 3.47 | 9.3 ± 3.24 | 0.0001 |
| Underlay | 32.00 ± 4.56 | 23.83 ± 3.87 | 8.17 ± 3.46 | 0.0001 |
Table 7.
Comparison of ABGAP Post 3 months and Post 6 Months
| AB GAP | Post 3 months | Post 6 Months | Difference | P Value |
|---|---|---|---|---|
| Button Hole | 29.53 ± 3.7 | 23.13 ± 3.47 | 6.40 ± 3.22 | 0.0001 |
| Underlay | 29.43 ± 4.96 | 23.83 ± 3.87 | 5.60± | 0.0001 |
Discussion
Tympanoplasty is a commonly performed procedure in COM. It is defined as a surgical procedure to eradicate disease in middle ear and to reconstruct the hearing mechanism with or without mastoid surgery and with or without tympanic membrane grafting. The study was conducted from Nov 2017 to May 2019 during which 60 cases of chronic otitis media (tubotympanic type) with medium sized perforation with moderate conductive hearing loss were included. All the 60 patients underwent Type 1 Tympanoplasty with post aural approach. Out of these, 30 patients underwent buttonhole type of Type 1 Tympanoplasty and other 30 patients underwent underlay type of type 1 tympanoplasty. Tympanoplasty was performed using temporalis fascia as the primary graft. Patients were followed up for a period of 6 months and were evaluated for graft uptake and hearing improvement.
In our study the mean age group of patients who had undergone button hole technique of tympanoplasty was 29–38 years and it was 29–48 years in patients who underwent underlay technique with the majority of patients in the age group of 3rd decade in both groups which is similar to the study by Shankar G et al. [4], a prospective study on 46 patients in the Department of ENT at a tertiary care hospital that had mean age in the 3rd decade.
In our study, in button hole technique there is equal distribution of male and female and in underlay technique there is a slight female preponderance which is comparable to the study by P. Packer a prospective study on various type of tympanoplasties wherein female preponderance was observed with male to female ratio was found to be 0.85: 1 [8].
In the past many techniques of grafting has been used. There have been many modifications and variations of the technique of tympanoplasty. In a retrospective study by Yigit O et al. [9], in Turkey a total of 104 patients underwent tympanoplasty via underlay technique in 46 patients and over underlay technique in 58 patients. In the first group the success rate was 91.5% and in second group the success rate was 94.4%.Study by Fiorina et al. [10], in Italy, 78 umbus anchored over-under myringoplasties were performed, graft uptake was obtained in 91% of cases with air-bone gap of 6.7 dB.
Compared to these studies graft uptake was comparable, in our study graft uptake was 96.7% in Buttonhole tympanoplasty and 93.3% by underlay method, as 1(3.3%) patient had a residual perforation in buttonhole tympanoplasty and 2(6.7%) patients in underlay tympanoplasty and 1 patient in underlay had medialisation of graft and none of the grafted ears in button hole technique exhibited medialisation, graft lateralization, or epithelial pearls. Comparing both the techniques for graft uptake our study showed no statistical significance.
All the patients were assessed by a pre-operative audiometric evaluation. Post-operative audiometry was done after months and the difference calculated.
In a prospective study by Shankar G et al. [4], a prospective study on 46 patients in the Department of ENT of a tertiary care hospital showed that buttonhole technique had significant air-bone closure (10–15 dB) on 6 month follow up. Study by Mehrada Rogha et al. [11], a prospective study done on 56 patients, 28 patients in Group A underwent buttonhole technique and 28 patients in Group B underwent overlay technique. Difference of air-bone gap in each group before and after surgery was 16.10dB in Group A and 15.78 in Group B. Improvement of hearing level was not significant between two surgical methods (p = 0.442).
In our study, in buttonhole tympanoplasty preoperative PTA was 32.43(+/-4.46) and postoperative PTA was 23.13(+/-3.24) with mean hearing gain of 9.3(± 3.24), and in underlay group the preoperative PTA was 32.04(+/-4.56) and post-operative PTA was 23.83(+/-3.87) with mean hearing gain of 8.17(± 3.46), which was statistically significant (p < 0.05). P value between button hole technique and underlay group was not statistically significant (p value 0.44) in terms of hearing gain.
Data reflects the experience of a single institution and might have been influenced by the expertise of the operating surgeon, in this case the principal investigator. Nevertheless, the strength of this study lies in its prospective nature, which allowed data to be accurately assessed without depending on patient recollection.
Conclusion
The results of tympanoplasty are measured in terms of success or failure of graft uptake and hearing improvement. Tympanoplasty is done by various techniques of underlay, overlay and interlay. The underlay technique has become popular over the years world over because of its distinctive advantages. In buttonhole tympanoplasty, the temporalis fascia is anchored to the handle of malleus through the buttonhole. In our study we are comparing buttonhole type of type 1 tympanoplasty with underlay type 1 tympanoplasty method.
Both techniques are good in terms of ease of graft placement, better graft uptake rate and audiological outcome and with no complications like lateralization of graft, epithelial pearl formation and anterior blunting.The advantages of button hole technique intraoperatively is that since the graft is anchored to the handle of malleus, all around movement of the graft is possible and postoperatively medialisation of graft is prevented.
Both techniques are good for chronic suppurative otitis media with medium sized central perforation with mild to moderate conductive hearing loss.
Funding
None.
Declarations
Conflict of interest
None declared.
Ethical Approval
Not required.
Informed consent
Taken.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Quinton Pathology and clinical course of the inflammatory diseases of the middle ear, Aina JG, Lloyd B, Dennis SP (2010) Glasscock-Shambaugh Surgery of the ear, 6th edn. USA: People’s Medical Publishing House, pp 427–428
- 2.Browning GG. Chronic otitis media. Browning GG. In: Merchant SN, Kelly G, Swan IR, Canter R, McKerrow WS, editors. Scott-brown’s otorhinolaryngology, head and neck Surgery. 7. Great Britain: edward arnold publishers ltd; 2008. pp. 3396–3439. [Google Scholar]
- 3.Aristides AS (2010) Tympanoplasty: tympanic membrane repair. In: Aina JG, Lloyd B, Dennis SP (eds) Glasscock-Shambaugh Surgery of the ear, 6th edn. USA: People’s Medical Publishing House, pp 465–488
- 4.Shankar G. A Narendranath A Buttonhole Tympanoplasty j Otolaryn. 2014;3(5):81–83. [Google Scholar]
- 5..Wallstein H (1952) Fusktionelle Operationen in Mittelohr Mit Hilfe Des Freien Spalt lappen transplantes. Arch Ohren Naseen-u-Kehlkoph, pp 161–242
- 6.Glasscock ME. Tympanic membrane grafting with fascia: overlay vs. undersurface technique. Laryngoscope 1973; 754 – 70., Taherinia A, Berjis N, Eshaghian A, Rogha M (2014) Comparison of tympanic membrane grafting medial or lateral to malleus handle. Advanced Biomedical Research. 3(1):56 [DOI] [PMC free article] [PubMed]
- 7.Gersdoff M, Gerard J- M.Management of tympanic membrane perforation:Special tympanoplasty techniques and problems,Atlas of middle ear surgeries,New York:Thieme;2011
- 8.Mackendrick PP. What’s best in myringoplasty: underlay or overlay. J Laryngol Otol. 1982;96:25–41. doi: 10.1017/S0022215100092203. [DOI] [PubMed] [Google Scholar]
- 9.Yigit O, Alkan S, Topuz E, Uslu B, Unsal O Dadas B.Short term evaluation of over – under myringoplasty technique.Eur Arch Otorhinolaryngol. 2005:262:400–403 [DOI] [PubMed]
- 10.Fiorino F, Barbieri F. Over – under ‘myringoplasty with umbus anchored graft. J Laryngology Otol. 2008;122:854–857. doi: 10.1017/S0022215108001874. [DOI] [PubMed] [Google Scholar]
- 11.Taherinia A, Berjis N, Eshaghian A, Rogha M. Comparison of tympanic membrane grafting medial or lateral to malleus handle. Adv Biomedical Res. 2014;3(1):56. doi: 10.4103/2277-9175.125804. [DOI] [PMC free article] [PubMed] [Google Scholar]