Abstract
Pleomorphic adenoma is a benign tumor of salivary glands which is relatively rare among head & neck neoplasms. Parotid gland is the most common site of occurrence whereas submandibular gland is rarely affected. We present a case of a giant pleomorphic adenoma of submandibular gland.
Keywords: Pleomorphic adenoma, Submandibular gland, Tumours
Introduction
Salivary gland tumours are uncommon and comprise only 1–4% of head-face-neck tumours. Majority of the salivary gland tumours affect parotid gland with more than 70% of the cases. Submandibular gland is affected in 5–10% of the cases with pleomorphic adenoma being the most common tumour [1]. We present a case of a giant pleomorphic adenoma arising from submandibular gland in a 60 years old female, which was surgically excised with no recurrence on follow up till date.
Case Report
A 60-year-old female patient presented to our OPD with a 7- year history of swelling in right submandibular region. The swelling was insidious in onset, slow growing and painless. There was no dysphagia or respiratory distress. Patient did not have any comorbidities.
Examination – On inspection a firm, bosselated mass seen in right submandibular region ~ 15 cm × 10 cm × 10 cm in size (Fig. 1).
Fig. 1.
Mass on inspection
On palpation, mass was multilobulated, firm, non-tender & mobile with well-defined borders. Skin over the mass was mobile.
Oral cavity examination was within normal limits.
Indirect laryngoscopy and fiberoptic laryngoscopy were within normal limits.
Origin of the mass could not be ascertained on history and clinical examinations.
Coronal and Axial CT neck sections revealed a well-defined heterogeneous mass involving right submandibular gland with areas of calcification. The mass was ~ 14.3 (AP) cm ×9.8 (TR) cm × 10.1(CC) cm (Fig. 2).
Fig. 2.
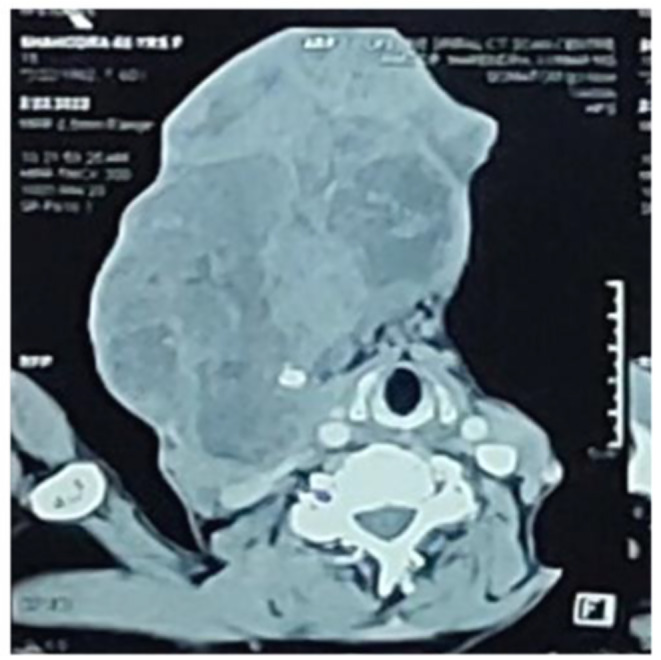
CT scan neck showing mass arising from right submandibular gland
FNAC suggested features of Pleomorphic adenoma with atypia of undetermined significance.
A provisional diagnosis of Pleomorphic adenoma of right submandibular gland was made and surgical excision planned.
Patient underwent complete excision of right submandibular gland through transcervical approach under general anesthesia. Internal jugular vein and Internal carotid artery identified and secured. Further dissection was done and the mass was removed completely. Surgical defect was closed primarily (Figs. 3 and 4).
Fig. 3.
Intraop picture
Fig. 4.

Postop picture
On gross examination, the tumor was lobulated, irregular, having well defined margins. Fat surrounding the tumor had multiple nodules. The cut surface showed areas of necrosis and cystic degeneration (Fig. 5).
Fig. 5.

Excised mass
Histopathology revealed biphasic tumor showing epithelial & mesenchymal components. Ductal epithelial cells arranged in form of cords & small tubules which are surrounded by myoepithelial cells. Adjacent area shows chondromyxoid matrix with interspersed myoepithelial cells. These findings were consistent with pleomorphic adenoma (Fig. 6).
Fig. 6.
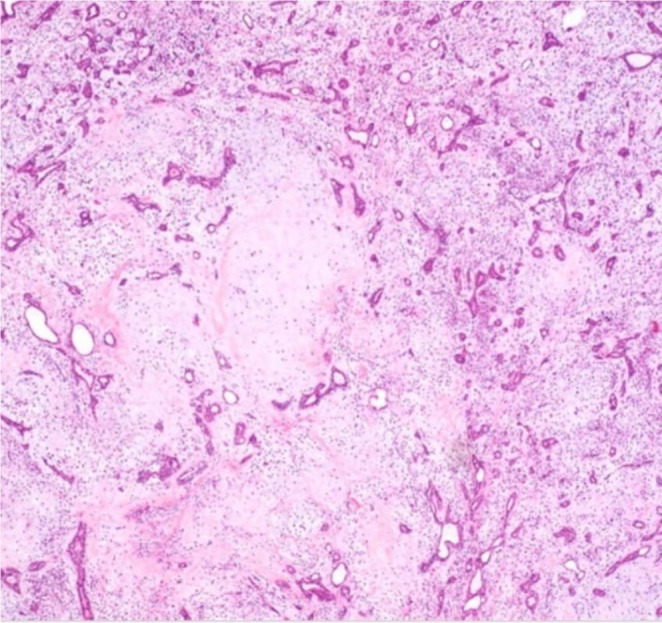
HPE
Thus, a definitive diagnosis of Pleomorphic adenoma of right submandibular salivary gland was made.
Intra-operative and post-operative periods were uneventful. Patient was on regular follow up for 2 years and no recurrence was seen.
Discussion
Pleomorphic adenoma is more predominant in women, which was the same in our case also.
Sporadic case reports of giant submandibular gland adenomas have been reported by Belli et al., Shultz et al. and Rognini et al. [2, 3]. Although they have reported such tumours in predominantly male sex, ours is a female patient Nerve compression was not found in reported cases and so is in our case.
Pleomorphic adenoma is an epithelial tumour of complex morphology, possessing epithelial and myoepithelial elements intermingled with mucoid, myxoid, or chondroid tissue arranged in a variety of patterns and embedded in a mucopolysaccharide stroma [4]. It is the commonest benign tumour of salivary glands [1] and accounts for 90% of all salivary gland tumours. The submandibular gland is the second most common site of PA after the parotid gland [5]. It is also the most frequent benign tumour arising in submandibular gland. The differential diagnosis of the submandibular mass can be basal cell adenoma, adenocarcinoma, mucoepidermoid carcinoma and lymphoma [6].
In children and in pregnant women, sonography is the first line of investigation. CT is the method of choice in patients suspicious for inflammatory disease or in patients with contraindication for MR imaging. However, MR imaging (MRI) is the method of choice for patients with palpable masses and a strong suspicion that the lesion is neoplastic [7]. We relied on CT scan in our case.
Song IH et al. demonstrated superiority of Core needle biopsy over FNAC for diagnosing salivary gland tumours in terms of adequacy (97.4% vs. 93.8%), sensitivity (88.2% vs. 58.2%), specificity (99.4% vs. 98.6%), PPV (97.8% vs. 88.9%), NPV (96.6% vs. 92.6%), and accurate tumour subtyping (88.3% vs. 70.7%) [8]. FNAC was used for cytopathologic evaluation in our case due to cost effectiveness of the procedure.
The incidence of malignant transformation in adenomas ranges from 1.9 to 23.3% [9]. The risk increases with a long history of appearance, recurrence, the advanced age of the patient, and location in the major salivary gland [10].
Recurrence of such tumours is possible especially if the surgical margins are involved, that is why it should be managed through complete excision of the tumour reaching completely free surgical margin [11].
Declarations
Informed Consent
Proper consent was taken from the patient for publishing her data and reports.
Conflict of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Spiro RH. Salivary Neoplasms: overview of a 35-year experience with 2,807 patients. Head Neck Surg. 1986;8:177–184. doi: 10.1002/hed.2890080309. [DOI] [PubMed] [Google Scholar]
- 2.Belli E, Marini Balestra F, Longo B. Giant pleomorphic adenoma of the submandibular gland. Case report. Minerva Stomatol. 2005;54:449–452. [PubMed] [Google Scholar]
- 3.Schulz T, Pauli R, Didzcuneit-Sandhop B. [Cervical giant Tumor in a 56-year-old female patient] HNO. 2010;58:159–161. doi: 10.1007/s00106-009-1954-8. [DOI] [PubMed] [Google Scholar]
- 4.Van der Wall I. Salivary gland Neoplasm. In: Prabhu SR, Wilson DF, Daftary DK, Johnson NW, editors. Oral Disease in the tropics. New York: Oxford University Press; 1992. pp. 478–486. [Google Scholar]
- 5.Laskawi R, Ellis M, Arglebe C, Schott A. Surgical management of benign tumors of the submandibular gland: a follow-up study. J Oral Maxillofac Surg. 1995;53:506–508. doi: 10.1016/0278-2391(95)90057-8. [DOI] [PubMed] [Google Scholar]
- 6.Illes RW, Brian MB. A review of the tumors of the salivary gland. Surg Gynecol Obstet. 1986;163:399–394. [PubMed] [Google Scholar]
- 7.Thoeny HC. Imaging of salivary gland tumours. Cancer Imaging. 2007;7(1):52–62. doi: 10.1102/1470-7330.2007.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Song IH, Song JS, Sung CO, Roh JL, Choi SH, Nam SY, Kim SY, Lee JH, Baek JH, Cho KJ. Accuracy of Core Needle Biopsy Versus Fine Needle Aspiration Cytology for diagnosing salivary gland tumors. J Pathol Transl Med. 2015;49(2):136–143. doi: 10.4132/jptm.2015.01.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perumal CJ, Meyer M, Mohamed A. A giant pleomorphic adenoma of the submandibular salivary gland: a case report Craniomaxillofac. Trauma Reconstr. 2012;5(3):185–188. doi: 10.1055/s-0032-1322530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yamamoto Y. Clinical signs and histology of carcinoma in pleomorphic adenoma. Otologia. 1994;87:1320–1324. [Google Scholar]
- 11.Abdelkhalek M, Elmetwally M, Mazy A, Gad M, Elsaid A, Awny S, Refky B, Abdallah A, Elalfy AF, Shokeir FA, Abdallah S, Elfeky A, Aboelamayem R, Hegazy MA. Gigantic submandibular pleomorphic adenoma: a rare case report. Int J Surg Case Rep. 2019;65:91–96. doi: 10.1016/j.ijscr.2019.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]




