Abstract
To study and analyse the variations in ethmoid roof anatomy and estimate the anatomical location and variations of AEA on CT scans. The study is conducted on 200 patients for detailed analysis of the olfactory fossa (OF) depth, supraorbital pneumatisation, and AEA location and distance from the skull base. In our study, Keros type II was predominant type seen followed by type I. Asymmetry was noted in 32/200 subjects (16%). The anterior ethmoidal artery (AEA) canal was seen in 341/400 sides (85.2%). We found Keros type II was the most common type in our study. We also found grade I anterior ethmoidal artery as the most common variant and the dangerous grade III anterior ethmoidal artery was least common type found in this study, and there was a significant association of Keros type II with increasing anterior ethmoidal artery grading.
Keywords: Ethmoid roof, Olfactory fossa, Anterior ethmoid artery, Anatomical variations, CT scan, Paranasal sinuses
Introduction
Endoscopic sinus surgery (ESS) is a known approach used to treat sinonasal pathologies. Most major complications of endoscopic sinus surgeries are related to the ethmoid bone. Properly analyzing variations of the ethmoid roof is essential, and therefore, preoperative computed tomography (CT) evaluation is necessary before ESS to minimize or avoid possible major complications [1–3]. The presence or absence of asymmetry in the ethmoid roof is significant for sinus surgeries [4]. However, there is a scarcity of data regarding the ethmoid roof, olfactory fossa (OF), and variations of the Anterior Ethmoidal Artery (AEA) in the Indian population. Preoperative knowledge about anatomy and its variations is crucial for surgeons to improve the safety profile of the procedure and plan the surgical approach accordingly to prevent expected complications [5, 6].
In this study, we aimed to determine the variations in the ethmoid roof, observe the location and grading of AEA on CT scans, and assess its variations among patients coming to a tertiary care hospital from multiple states in North India.
Material and Methods
The study is an institutional-based prospective cohort study, conducted on 200 patients referred by various clinical specialties for undergoing CT scan of paranasal sinuses (PNS) over a period of 23 months, from January 2021 to November 2022.
Inclusion Criteria
Individuals with age ≥ 18 years undergoing CT PNS for complaints like headache, nasal discharge, nasal blockage, ear pain, cough, etc.
Exclusion Criteria
Individuals < 18 years of age and/or having mental impairment unfit for radiological technique.
Individuals with a history of severe rhinosinusitis, sinonasal polyposis, tumors, congenital anomalies of the face, trauma to the anterior cranial fossa, or conditions involving bone destruction/remodeling.
Technique of Examination Scanner
All studies were performed using a 128-slice scanner (Ingenuity CT, Philips Healthcare, Best, The Netherlands).
Scans were performed in a supine position.
A scanogram was obtained.
Scan Range
The scan range extended from the upper level of frontal sinuses superiorly to the lower part of the maxilla inferiorly. The antero-posterior span of imaging was from the outer edge of the frontal bone anteriorly to the sphenoid bone posteriorly. This range was necessary to evaluate all the sinuses, including the ethmoid roof.
Scan Parameters
Tube Peak Voltage (kVp): 120kVp
Tube current–time product in milliampere-second (mAs): 200 mAs
Slice thickness: 1 mm • Increment: 0.5 mm
Pitch: 0.39 mm
Rotation time: 0.5 s
Field of View (FOV): 220 mm
Reconstruction: Standard
Window width: 2200 (bone scan)
Image Reconstruction and Post-processing
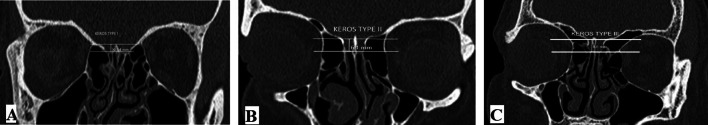
All images were transferred to workstations for post-processing. The depth of the olfactory fossa (for Keros Classification) was measured by drawing horizontal lines along the cribriform plate and at the medial ethmoid roof point. The vertical height of the lateral lamella (olfactory fossa depth) was measured between the two horizontal lines. A depth of 1–3 mm was categorized as Keros Type I, a depth of 4–7 mm as Type II, and ≥ 8 mm as Type III (Fig. 1A–C).
Fig. 1.
Pic showing Keros Classification for depth of Olfactory Fossa. A: Keros Type I (OF depth of 1–3 mm), B: Keros Type II (OF depth of 4–7 mm). C: Keros Type II (OF depth of ≥ 8 mm)
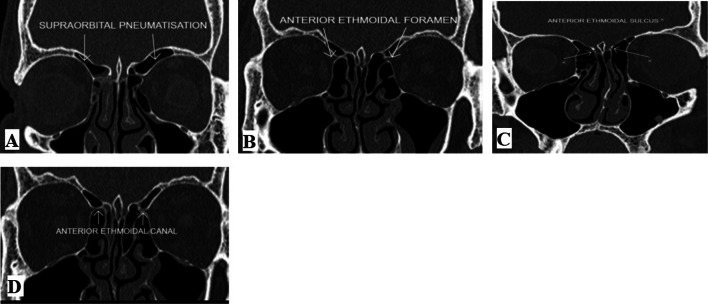
The CT images were evaluated on coronal and axial views for the presence of the supraorbital ethmoid cell (Fig. 2A). AEA was identified on the coronal view using the adjacent bony landmarks, namely the anterior ethmoidal foramen (Fig. 2B), anterior ethmoidal sulcus (Fig. 2C), and anterior ethmoidal canal (Fig. 2D). The Anterior Ethmoidal Foramen is a bony notch in the medial wall of the orbit. The Anterior Ethmoidal Sulcus is a bone sulcus on the lateral wall of the olfactory fossa, whereas the Anterior Ethmoidal Canal is a passage between the anterior ethmoidal foramen and anterior ethmoidal sulcus. Following the identification of AEA, the distance between AEA from the skull base was measured.
Fig. 2.
Pic showing Important Findings and Landmarks seen on CT scan of PNS. A: The CT PNS showing presence of supraorbital ethmoid cell. B: The CT PNS showing presence of Anterior Ethmoidal Foramen. C: The CT PNS showing presence of Anterior Ethmoidal Sulcus. D: The CT PNS showing presence of Anterior Ethmoidal Canal
Lannoy-Penisson et al. [7] categorized the AEA grade according to its location as follows:
Grade I—when it was found to be embedded in the skull base.
Grade II—when it courses under the skull base and seen as a protrusion at the skull base.
Grade III—when it travels freely at a distance from the skull base.
Statistical Analysis
The collected data were converted into a computer-based spreadsheet and analyzed. Categorical variables like Keros classification, gender, etc., were presented as proportions. Continuous variables were presented as mean and standard deviation. Appropriate statistical tests of significance like chi-square test (Fischer’s exact test, if required) were used to test the differences in other categorical measures, and t-test for differences in means. Significance was considered at levels for p-values less than 0.05.
Results
CT scans of PNS of 200 subjects were performed, and among these, 92 were females (46%) and 108 were males (54%). The mean age ± Standard deviation (SD) of the study group was 38.46 ± 13.75 years for females and 37.41 ± 16.04 years for males.
Comparison of Olfactory Fossa (OF) Depth with Gender (Table 1)
Table 1.
Comparison of Olfactory Fossa (OF) depth with Gender
| Sex | n | Mean ± Standard Deviation (in mm) | p value |
|---|---|---|---|
| OF DEPTH | |||
| Females | 184 | 4.760 ± 1.07 | 0.071 |
| Males | 216 | 4.949 ± 1.00 | |
The mean ± SD depth of OF in males (including both sides) was 4.949 ± 1.00 mm, and in females, it was 4.760 ± 1.07 mm. Statistically, no significant difference was present in the mean depth of the OF between males and females, with a p-value of 0.071.
Comparison of OF Depth with Side Distribution (Table 2)
Table 2.
Comparison of Olfactory Fossa (OF) depth with Side distribution
| Side | n | Mean ± Standard Deviation (in mm) | p value |
|---|---|---|---|
| OF DEPTH | |||
| Left | 200 | 4.830 ± 1.01 | 0.53 |
| Right | 200 | 4.895 ± 1.06 | |
The mean depth of the OF on the right side was 4.895 ± 1.06 mm, and the mean depth on the left side was 4.830 ± 1.01 mm. Using a sample t-test, the p-value was 0.53. Hence, no significant difference was seen between the mean depth of the OF on both sides.
Supraorbital Pneumatization
Supraorbital pneumatization was present in 28/400 (7%) in the study population.
Presence of Anterior Ethmoidal Artery (AEA) Canal on Right Side in Study Population
AEA canal was identified in 170 sides out of 200 with a presence of 85% on right side and it was not seen in remaining 30 sides.
Presence of AEA Canal on Left Side in Study Population
AEA canal was identified in 171 sides out of 200 with a presence of 85.5% on left side and it was not seen in remaining 29 sides (14.5%).
Association of Keros Type and Gender (Table 3)
Table 3.
Comparison of Gender distribution with Keros type
| KEROS TYPE | |||||||
|---|---|---|---|---|---|---|---|
| Sex | I | II | III | Total (n = 400) | Chi-square | p value | |
| Female | Frequency | 38 | 146 | 0 | 184 | 3.22 | 0.049 |
| Percentage | 20.70% | 79.30% | 0 | 100% | |||
| Male | Frequency | 30 | 186 | 0 | 216 | ||
| Percentage | 13.90% | 86.10% | 0 | 100% | |||
| Total | Frequency | 68 | 332 | 0 | 400 | ||
| Percentage | 17.00% | 83.00% | 0 | 100% | |||
Incidence of Keros Type II was predominant (83%) in our study, while Keros Type I was observed in only 17% in our study. On comparing Keros Type based on gender distribution, we found that Keros Type II was prevalent among males (86%) compared to females (79%). This difference was statistically significant (p-value = 0.049).
Comparison of Gender Distribution with Keros Type on Right Side (Table 4)
Table 4.
Comparison of Gender distribution with Keros type on RIGHT side
| KEROS TYPE | |||||||
|---|---|---|---|---|---|---|---|
| Sex | I | II | III | Total (n = 400) | Chi-square | p value | |
| Female | Frequency | 17 | 75 | 0 | 92 | 0.77 | 0.25 |
| Percentage | 18.50% | 81.50% | 0 | 100% | |||
| Male | Frequency | 15 | 93 | 0 | 108 | ||
| Percentage | 13.90% | 86.10% | 0 | 100% | |||
| Total | Frequency | 32 | 168 | 0 | 200 | ||
| Percentage | 16.00% | 84% | 0 | 100% | |||
Further comparison of gender distribution with Keros Type was done on the right side, and Keros Type II was found predominant in males (86.10%) compared to females (81.5%). However, the difference between sex and Keros Type on the right side was not statistically significant (p-value = 0.25).
Comparison of Gender Distribution with Keros Type on Left Side (Table 5)
Table 5.
Comparison of Gender distribution with Keros type on LEFT side
| KEROS TYPE | |||||||
|---|---|---|---|---|---|---|---|
| Sex | I | II | III | Total (n = 400) | Chi-square | p value | |
| Female | Frequency | 21 | 71 | 0 | 92 | 2.68 | 0.073 |
| Percentage | 22.80% | 77.20% | 0 | 100% | |||
| Male | Frequency | 15 | 93 | 0 | 108 | ||
| Percentage | 13.90% | 86.10% | 0 | 100% | |||
| Total | Frequency | 36 | 164 | 0 | 200 | ||
| Percentage | 18% | 82% | 0 | 100% | |||
We found that Keros Type II was predominant in our study, more in males (86.10%) compared to females (77.2%). However, the association between sex and Keros Type on the left side was not statistically significant (p-value = 0.073).
Association Between Keros Type and Side Distribution (Table 6)
Table 6.
Association of Keros type on side distribution
| KEROS TYPE | |||||||
|---|---|---|---|---|---|---|---|
| Side | I | II | III | Total (n = 400) | Chi-square | p value | |
| Left | Frequency | 36 | 164 | 0 | 200 | 0.28 | 0.35 |
| Percentage | 18% | 82% | 0 | 100% | |||
| Right | Frequency | 32 | 168 | 0 | 200 | ||
| Percentage | 16% | 84% | 0 | 100% | |||
| Total | Frequency | 68 | 332 | 0 | 400 | ||
| Percentage | 17% | 83% | 0 | 100% | |||
We found that Keros Type II was predominantly found in 84% on the right side and 82% on the left side, while Type I was found only in 16% on the right side and 18% on the left side. However, the association between Keros and side was not statistically significant (p-value = 0.35).
Association of Supraorbital Pneumatization with Keros Type (Table 7)
Table 7.
Association of Supraorbital pneumatisation with Keros Type
| KEROS TYPE | |||||||
|---|---|---|---|---|---|---|---|
| Supraorbital Pneumatization | I | II | III | Total (n = 400) | Chi-square | p value | |
| No | Frequency | 66 | 306 | 0 | 372 | 2.07 | 0.11 |
| Percentage | 17.70% | 82.30% | 0 | 100% | |||
| Yes | Frequency | 2 | 26 | 0 | 28 | ||
| Percentage | 7.10% | 92.90% | 0 | 100% | |||
| Total | Frequency | 68 | 332 | 0 | 400 | ||
| Percentage | 17.00% | 83.00% | 0 | 100% | |||
We found that Keros Type II was found in 92.9%, and Type I was found in only 7.1% of patients. However, the association was not statistically significant (p-value = 0.11).
Association of Supraorbital Pneumatization with Keros Type on the Right Side (Table 8)
Table 8.
Association of Supraorbital pneumatisation with Keros Type (Right Side)
| KEROS TYPE | |||||||
|---|---|---|---|---|---|---|---|
| Supraorbital Pneumatization | I | II | III | Total (n = 400) | Chi-square | p value | |
| No | Frequency | 30 | 156 | 0 | 186 | 0.33 | 0.61 |
| Percentage | 16.10% | 83.90% | 0 | 100% | |||
| Yes | Frequency | 2 | 12 | 0 | 14 | ||
| Percentage | 14.30% | 85.70% | 0 | 100% | |||
| Total | Frequency | 32 | 168 | 0 | 200 | ||
| Percentage | 16.00% | 84% | 0 | 100% | |||
We found that Keros Type II was more associated with supraorbital pneumatisation (85.70%) compared to Keros Type I. However, the association between Keros type and supraorbital pneumatisation was not statistically significant (p-value = 0.61).
Association of Supraorbital Pneumatization with Keros Type on the Left Side (Table 9)
Table 9.
Association of Supraorbital pneumatisation with Keros Type (Left Side)
| KEROS TYPE | |||||||
|---|---|---|---|---|---|---|---|
| Supraorbital Pneumatization | I | II | III | Total (n = 400) | Chi-square | p value | |
| No | Frequency | 36 | 150 | 0 | 186 | 3.30 | 0.056 |
| Percentage | 19.40% | 80.60% | 0 | 100% | |||
| Yes | Frequency | 0 | 14 | 0 | 14 | ||
| Percentage | 0% | 100% | 0 | 100% | |||
| Total | Frequency | 36 | 164 | 0 | 200 | ||
| Percentage | 18% | 82% | 0 | 100% | |||
| Percentage | 18% | 82% | 0 | 100% | |||
Further association between supraorbital pneumatisation with Keros Type on the Left side was studied and was found that Keros Type II was exclusively in those with supraorbital pneumatisation (100%), as compared to those without pneumatisation (80.6%). However, the association between Keros type and supraorbital pneumatisation was not statistically significant (p-value = 0.056).
Association Between Asymmetry and Gender
We found that the difference in OF depth between the right and left sides was ≥ 1 mm in 32 patients [16%] and < 1 mm in 168 (84%) patients. However, the association in OF depth difference (asymmetry) and gender was not statistically significant (p-value is 0.506).
Distance of AEA from the Skull Base and Respective Sides (Table 10)
Table 10.
Distance of anterior ethmoidal artery from the skull base and respective sides
| Side | AEA distance from skull base (in mm) | |
|---|---|---|
| Mean (in mm) | Standard Deviation (in mm) | |
| Right | 2.27 | 0.63 |
| Left | 2.18 | 0.49 |
The distance of AEA from the skull base on the respective side was studied, and the mean ± SD distance of AEA from the skull base was 2.27 mm ± 0.63 mm on the right side and 2.18 ± 0.49 mm on the left side.
Association of Sex and AEA Grade (Table 11)
Table 11.
Association of Sex and anterior ethmoidal artery grade
| AEA Grade | |||||||
|---|---|---|---|---|---|---|---|
| Sex | I | II | III | Total (n = 341/400) | Chi-Square | p value | |
| Female | Frequency | 74 | 51 | 21 | 146 | 5.62 | 0.06 |
| Percentage | 50.7% | 34.9% | 14.4% | 100% | |||
| Male | Frequency | 83 | 64 | 48 | 195 | ||
| Percentage | 42.6% | 32.8% | 24.6% | 100% | |||
| Total | Frequency | 157 | 115 | 69 | 341 | ||
| Percentage | 46.1% | 33.7% | 20.2% | 100% | |||
Association of sex and AEA grading was studied, and grade I AEA was most commonly found in 157 sides out of 341 (46.1%), followed by grade II, which was reported in 115 sides (33.7%). AEA grade III was the least commonly found in only 69 sides (20.2%). However, the association between sex and AEA grade was not found to be statistically significant (p-value = 0.06).
Association of Sex with AEA Grade on the Right Side (Table 12)
Table 12.
Association of Sex and anterior ethmoidal artery grade on Right Side
| AEA Grade | |||||||
|---|---|---|---|---|---|---|---|
| Sex | I | II | III | Total | Chi-Square | p value | |
| Female | Frequency | 37 | 29 | 7 | 73 | 3.81 | 0.149 |
| Percentage | 50.7% | 39.7% | 9.6% | 100% | |||
| Male | Frequency | 44 | 33 | 20 | 97 | ||
| Percentage | 45.4% | 34% | 20.6% | 100% | |||
| Total | Frequency | 81 | 62 | 27 | 170 | ||
| Percentage | 47.6% | 36.5% | 15.9% | 100% | |||
Association of sex and AEA grading on the right side was studied, and grade I AEA was most commonly found (47.6%) followed by grade II AEA (36.5%) and grade III AEA (15.9%). Grade I AEA was seen more commonly in females (50.7%) compared to males (45.4%). However, the difference between sex and AEA grade was not statistically significant (p-value = 0.149).
Association of Sex with AEA Grade on the Left Side (Table 13)
Table 13.
Association of Sex and anterior ethmoidal artery grade on Left Side
| AEA Grade | |||||||
|---|---|---|---|---|---|---|---|
| Sex | I | II | III | Total | Chi-Square | p value | |
| Female | Frequency | 37 | 22 | 14 | 73 | 2.64 | 0.266 |
| Percentage | 50.7% | 30.1% | 19.2% | 100% | |||
| Male | Frequency | 39 | 31 | 28 | 98 | ||
| Percentage | 39.8% | 31.6% | 28.6% | 100% | |||
| Total | Frequency | 76 | 53 | 42 | 171 | ||
| Percentage | 44.4% | 31% | 24.6% | 100% | |||
Association of sex and AEA grading on the left side was studied, and grade I AEA was most commonly found (44.4%), followed by grade II AEA (31%) and grade III (24.6%). Grade I AEA was seen more commonly in females (50.7%) compared to males (39.8%). However, the difference between sex and AEA grade was not statistically significant (p-value = 0.266).
Association of AEA Grade and Side Distribution (Table 14)
Table 14.
Association of Anterior ethmoidal artery grade and Side distribution
| AEA Grade | |||||||
|---|---|---|---|---|---|---|---|
| Side | I | II | III | Total (n = 341/400) | Chi-Square | p value | |
| Left | Frequency | 76 | 53 | 42 | 171 | 4.122 | 0.127 |
| Percentage | 44.4% | 31% | 24.6% | 100% | |||
| Right | Frequency | 81 | 62 | 27 | 170 | ||
| Percentage | 47.6% | 36.5% | 15.9% | 100% | |||
| Total | Frequency | 157 | 115 | 69 | 341 | ||
| Percentage | 46% | 33% | 20.2% | 100% | |||
Association of AEA grade and side distribution was studied and found that Grade I AEA was most commonly found in 157/341 sides (46%). Grade II AEA was reported in 115/341 (33%), while grade III AEA was least commonly reported in 69/341 (20.2%). Grade I AEA was reported in 81/170 (47.6%) on the right side and 76/171 (44.4%) on the left side. Grade II AEA was reported in 62/170 (36.5%) on the right side and 53/171(31%) on the left side. Grade III AEA was reported in 27/170 (24.6%) on the right side and 42/171 (15.9%) on the left side. Grade III AEA was mildly higher on the left side compared to the right side, but the difference between the AEA grade and side was not statistically significant with a p-value = 0.12.
Association of Supraorbital Pneumatization with AEA Grade (n = 341/400) (Table 15)
Table 15.
Association of Supraorbital Pneumatization with Anterior ethmoidal artery grade (n = 341/400)
| AEA Grade | ||||||
|---|---|---|---|---|---|---|
| Supraorbital Pneumatization | I | II | III | Chi-square | p value | |
| No | Frequency | 146 | 108 | 65 | 0.154 | 0.926 |
| Percentage | 45.8% | 33.9% | 20.4% | |||
| Yes | Frequency | 11 | 07 | 04 | ||
| Percentage | 50% | 31.8% | 18.2% | |||
| Total | Frequency | 157 | 115 | 69 | ||
| Percentage | 46% | 33.7% | 20.2% | |||
Association of Supraorbital pneumatisation with AEA Grade was studied, and Supraorbital pneumatisation was found in 11/22 sides (50%) with grade I AEA, while observed in 7/22(31.8%) with grade II AEA and 4/22 (18.2%) in grade III. However, the association between supraorbital pneumatisation and AEA grade was not statistically significant (p-value = 0.92).
Association of Supraorbital Pneumatization with AEA Grade on the Right Side (Table 16)
Table 16.
Association of Supraorbital Pneumatization with Anterior ethmoidal artery grade on Right side
| AEA Grade | |||||
|---|---|---|---|---|---|
| Supraorbital Pneumatization | I | II | III | p value | |
| No | Frequency | 76 | 58 | 25 | 0.975 |
| Percentage | 47.8% | 36.5% | 15.7% | ||
| Yes | Frequency | 5 | 4 | 2 | |
| Percentage | 45.5% | 36.4% | 18.2% | ||
| Total | Frequency | 81 | 62 | 27 | |
| Percentage | 47.6% | 36.5% | 15.9% | ||
Association of Supraorbital pneumatisation with AEA grade on the right side was studied, and on the right side, 11 patients had supraorbital pneumatisation out of which grade I AEA was found in 5/11(45.5%), grade II AEA in 4/11(36.4%), while grade III AEA was observed in 2/11(18.2%). However, the association between supraorbital pneumatisation and AEA grade was not statistically significant (p-value = 0.97).
Association of Supraorbital Pneumatization with AEA Grade on the Left Side (Table. 17)
Table 17.
Association of Supraorbital Pneumatization with Anterior ethmoidal artery grade on Left side
| AEA Grade | |||||
|---|---|---|---|---|---|
| Supraorbital Pneumatization | I | II | III | p value | |
| No | Frequency | 70 | 50 | 0.77 | 0.77 |
| Percentage | 43.8% | 31.3% | 25% | ||
| Yes | Frequency | 6 | 3 | 2 | |
| Percentage | 54.5% | 27.3% | 18.2% | ||
| Total | Frequency | 76 | 53 | 42 | |
| Percentage | 44.4% | 31% | 24.6% | ||
Association of Supraorbital pneumatisation with AEA Grade on the Left Side was studied, and on the left side, 11 patients had supraorbital pneumatisation, out of which grade I AEA was found in 6/11(54.5%), grade II AEA in 3/11(27.3%) and grade III AEA was observed in 2/11(18.2%). However, the association between supraorbital pneumatisation and AEA grade was not statistically significant (p-value = 0.77).
Association Between Keros Classification and AEA grade (Table 18)
Table 18.
Association between Keros classification and Anterior Ethmoidal Artery grade
| AEA Grade | ||||||
|---|---|---|---|---|---|---|
| Keros Type | I | II | III | Total | p value | |
| I | Count | 43 | 19 | 4 | 66 | 0.001 |
| % within AEA grade | 27.4% | 16.5% | 5.8% | 19.4% | ||
| II | Count | 114 | 96 | 65 | 275 | |
| % within AEA grade | 72.6% | 83.5% | 94.2% | 80.6% | ||
| III | Count | 0 | 0 | 0 | 0 | |
| % within AEA grade | 0 | 0 | 0 | 0 | ||
| Total | Count | 157 | 115 | 69 | 341 | |
| % within AEA grade | 100% | 100% | 100% | 100% | ||
Association between Keros classification and AEA grade was studied, and it was found that Keros Type II became increasingly more common. It ranged from 72.6% in AEA grade I, 83.5% in AEA grade II, and 94.2% in AEA grade III. Hence, the association between Keros type II and increasing AEA grade was statistically significant with a p-value = 0.001.
Discussion
In the present study, the age of patients ranged from 18 to 80 years, with a mean age ± standard deviation (SD) of 37.93 ± 14.89 years. There was a slight male predominance (54% male and 46% female. The relative gender ratio in our study appears similar to earlier studies conducted by Moradi and Dalili [4], Thimmappa et al. [8].
In our study, Keros type II was the predominant type, observed in 83% of subjects, followed by type I, which was observed in only 17%. No Keros type III was seen in our study. This finding aligns with many previous studies conducted in India, where type II was found to be the most common type, except for Shama SA and Montaser M's study, where type I was the most common [9]. Type III Keros was the least common type in most studies, except for the study conducted by Erdogan et al. [10] in which type I was the least common.
We found a statistically significant association between sex and Keros type in our study (p-value = 0.049), similar to the study conducted by Babu et al. [11].
Asymmetry in the ethmoid roof results from the difference in depth of the olfactory fossa (OF) between the two sides. We noted asymmetry (OF depth difference ≥ 1 mm between the two sides) in 32 out of 200 subjects (16%). However, we did not find a statistically significant association (p-value = 0.506) between asymmetry and gender, similar to the studies conducted by Kaplanoglu et al. [1] and Souza et al. [12].
Important landmarks for the identification of the anterior ethmoidal artery (AEA) are the anterior ethmoidal foramen and anterior ethmoidal sulcus, which were observed in 100% of the cases in our study. However, we were able to identify the AEA canal in 341 out of 400 sides (85.2%). In a study conducted by Joshi et al., the AEA canal was observed in 97% of the cases [13].
In a study conducted by Abdulhadi et al. grade I AEA was the most common type observed in 42.5% of cases, which is very similar to our study where it accounted for 46.1% of cases. However, grade II was the least common type in their study, accounting for 20.2%, whereas grade III AEA was the least common in our study [14].
In our study, we observed that the percentage of Keros type II became increasingly more common with increasing AEA grade. It ranged from 72.6% in AEA grade I, 83.5% in AEA grade II, and 94.2% in AEA grade III. We found a statistically significant association (p-value = 0.001) between Keros type II and increasing AEA grade. Similar conclusions were also seen in studies conducted by Abdullah et al., where the percentage of Keros type II became increasingly common with increasing AEA grade, ranging from 39.4% in AEA grade I, 21.9% in AEA grade II, and 43.2% in AEA grade III [5].
The presence of supraorbital pneumatisation is important for surgeons as it causes the AEA to be located further below the skull base, increasing the risk of injuring the artery during surgery. In our study, supraorbital pneumatisation was seen in 28 out of 400 sides (7%), with the majority of cases (92.9%) seen in Keros type II. Type I was found in only 2 out of 28 sides (7.1%). However, no significant difference was observed with a p-value > 0.05. Supraorbital pneumatisation was most commonly seen with Keros type II on either side. To our knowledge, no previous study has been conducted comparing supraorbital pneumatisation with Keros type.
The mean distance of the AEA from the skull base was 2.7 ± 0.63 mm on the right side and 2.18 ± 0.49 mm on the left side. This measurement was calculated in subjects with the AEA away from the skull base (grade III) in our study. In a study conducted by Jabaz DF in 189 patients, the mean distance of the AEA from the skull base was 4 ± 1.5 mm on the right side and 4.02 ± 2.36 mm on the left side, which is not comparable to our study. The position of the AEA and the distance in relation to the skull base may show variation in a single subject between the two sides. Therefore, surgeons should be aware of such variations to prevent possible catastrophes [15].
Conclusion
In our study population, Keros type II was the most common type, which is relatively less dangerous compared to type III. No Keros type III was found in our study. We also found grade I anterior ethmoidal artery to be the most common variant in terms of location in relation to the skull base. The dangerous grade III anterior ethmoidal artery was the least common type found in this study.
We observed a very important finding where a significant association of Keros type II was seen with increasing anterior ethmoidal artery grading.
Knowledge and recognition of these variations prior to surgery help minimize the risk of injury to the artery and avoid complications.
Funding
The authors have not disclosed any funding.
Declarations
Conflict of interest
The authors have not disclosed any competing interests.
Ethical Approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation and with the Ethical approval. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki Declaration of 1975, as revised in 2008, and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kaplanoglu H, Kaplanoglu V, Dilli A, Toprak U, Hekimoglu B. An analysis of the anatomic variations of paranasal sinuses and ethmoid roof using computed tomography. Eurasian J Med. 2013;45:115–125. doi: 10.5152/eajm.2013.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kainz J, Stammberger H. The roof of the anterior ethmoid: a locus minoris resistentiae in the skull base. Laryngol Rhinol Otol. 1988;67:142–149. doi: 10.1055/s-2007-998473. [DOI] [PubMed] [Google Scholar]
- 3.Jacob TG, Kaul JM. Morphology of the olfactory fossa—a new look. J Anatomic Soc India. 2014;63:30–35. doi: 10.1016/j.jasi.2014.04.006. [DOI] [Google Scholar]
- 4.Moradi M, Dalili B. Variations of ethmoid roof in the Iranian population—a cross sectional study. Iran J Otorhinolaryngol. 2020;32:169–173. doi: 10.22038/ijorl.2019.37340.2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdullah B, Lim EH, Husain S, Snidvongs K, Wang Y. Anatomical variations of anterior ethmoidal artery and their significance in endoscopic sinus surgery: a systematic review. Surg RadiolAnat. 2019;41:491–499. doi: 10.1007/s00276-018-2165-3. [DOI] [PubMed] [Google Scholar]
- 6.Amarnath S, Kumar P. Study of variants of anterior ethmoidal artery on computed tomography of paranasal sinuses. Int J Otorhinolaryngol Head Neck Surg. 2019;5:19–23. doi: 10.18203/issn.2454-5929.ijohns20185106. [DOI] [Google Scholar]
- 7.Lannoy-Penisson L, Schultz P, Riehm S, Atallah I, Veillon F, Debry C. The anterior ethmoidal artery: radio-anatomical comparison and its application in endonasal surgery. Acta otolaryngologica. 2007;127:618–622. doi: 10.1080/00016480600987826. [DOI] [PubMed] [Google Scholar]
- 8.Thimmappa TD, Amith P, Nagaraja M, Harsha KN, Gangadhar KS, Azeem A. Anatomical variations of sinonasal region: a CT scan study. Int J Res Med Sci. 2014;2:1441–1445. doi: 10.5455/2320-6012.ijrms20141137. [DOI] [Google Scholar]
- 9.Shama SAM, Montaser M. Variations of the height of the ethmoid roof among Egyptian adult population: MDCT study. The Egy J Radiol and Nucl Med. 2015;46:929–936. doi: 10.1016/j.ejrnm.2015.07.013. [DOI] [Google Scholar]
- 10.Erdogan S, Keskin IG, Topdag M, Ozturk M, Sari F, Mutlu F. Ethmoid roof radiology; analysis of lateral lamella of cribriform plate. Otolaryngol Pol. 2015;69:53–57. doi: 10.5604/00306657.1184543. [DOI] [PubMed] [Google Scholar]
- 11.Babu AC, Nair MR, Kuriakose AM. Olfactory fossa depth: CT analysis of 1200 patients. Ind J Radioland Imag. 2018;28:395–400. doi: 10.4103/ijri.IJRI_119_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Souza SA, Souza MM, Idagawa M, Wolosker ÂM, Ajzen SA. Computed tomography assessment of the ethmoid roof: a relevant region at risk in endoscopic sinus surgery. Radiol Bras. 2008;41:143–147. doi: 10.1590/S0100-39842008000300003. [DOI] [Google Scholar]
- 13.Joshi AA, Shah KD, Bradoo RA. Radiological correlation between the anterior ethmoidal artery and the supraorbital ethmoid cell. Ind J Otolaryngol Head Neck Surg. 2010;62:299–303. doi: 10.1007/s12070-010-0088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdulhadi BN, Shyaa AI, Altamimi L. Computed tomography assessment of the ethmoid roof based on Keros classification in Iraqi patients undergoing functional endoscopic sinus surgery. J Ideas Health. 2021;4:365–370. doi: 10.47108/jidhealth.Vol4.Iss2.120. [DOI] [Google Scholar]
- 15.Jabaz DF. Computerized tomography profile of the olfactory fossa based on keros classification and the anterior ethmoid artery location to the skull base. Al-Qadisiyah Med J. 2022;18:26–36. [Google Scholar]