Abstract
Objective:
The article studies the geographical features of the incidence of hypopharynx cancer (HPC) in Kazakhstan.
Methods:
The retrospective study was done for the period 2017-2021. Descriptive and analytical methods of ecoepidemiology were used. Crude (CR), age-specific (ASIR), age-standardized (ASR), equalized incidence rates and approximation were calculated. The dynamics of indicators was investigated using component analysis according to methodological recommendations. The method of drawing up a cartogram based on the determination of the standard deviation (σ) from the mean (x) was applied.
Result:
During the study period, 814 new cases of HPC were registered. The incidence rate decreased from 0.898 (2017) to 0.895 in 2021 and the overall decline was 0.003 per 100,000 population, including due to the age structure – ∑ΔA=+0.04, due to the risk of acquiring illness – ∑ΔR=−0.05 and their combined effect – ∑ΔRA=+0.01. The component analysis revealed that the increase in the number of patients with HPC was mainly due to the growth of the population (ΔP=+37.0%), changes in its age structure (ΔA=+106.1%) and changes associated with the risk of acquiring illness (ΔR=−133.4%). The cartograms were allocated according to the following criteria: low – up to 0.730/0000, average – from 0.73 to 1.180/0000, high – above 1.180/0000. The results of the spatial assessment showed the highest levels of HPC incidence in following regions: Atyrau (1.960/0000) and West Kazakhstan (1.580/0000).
Conclusion:
Thus, this is the first epidemiological study of HPC, which assessed the role of the influence of various factors, including demographic and risk of acquiring illness, on the dynamics of incidence, taking into account gender differences and geographical variability.
Key Words: hypopharynx cancer, incidence, component analysis, Kazakhstan
Introduction
Squamous cell carcinoma of the head and neck develops from the epithelium of the mucous membrane of the oral cavity, pharynx and larynx and is the most common malignant neoplasm of the head and neck. The hypopharynx’s position is inferior to the epiglottis and is bordered by the pharyngoepiglottic fold superiorly and the upper esophageal sphincter inferiorly. It refers to the portion of the pharynx where the cavity diverges anteriorly into the larynx and posteriorly into the esophagus (Emura et al., 2013). Hypopharyngeal cancer is characterized by poor prognosis, primarily attributed to its aggressive nature and late detection. Prognosis in hypopharyngeal cancer is significantly influenced by the disease stage. Patients diagnosed at an early stage (T1-T2) exhibit a 5-year survival rate of approximately 60%, in contrast to less than 25% for those with advanced tumors (T3-T4) or widespread nodal involvement (Sanders and Pathak, 2022).
Hypopharynx cancer (HPC) is not the most common type of head and neck cancer worldwide, affecting an estimated 84,254 patients worldwide in 2020 and leading to an estimated 38,599 deaths. The largest number of cases is registered in Asian countries (about 69% of all cases) (Ferlay et al., 2022). About two thirds of diagnosed cases of head and neck cancer are detected in developing countries (Sinard et al., 2014). Also, the largest number of cases of HPC is registered in countries with medium, high and very high human development index (Ferlay et al., 2022). The global incidence age standardised incidence rates of HPC is averaged at 0.9 per 100,000 (1.6 in men and 0.3 in women) (Ferlay et al., 2022).
HPC is a multifactorial disease (El Bedoui and Lefebvre, 2017). Major studies have been conducted to study the etiological factors of laryngeal cancer and it was assumed that, since the hypopharynx is anatomically related to the larynx, both of them are subject to similar risk factors (de Souza et al., 2011). Long-term exposure to tobacco (Mishra and Meherotra, 2014), tobacco products (Sapkota et al., 2007) and alcohol (Jayalekshmi et al., 2013) increases the risk of developing head and neck cancer (Marur and Forastiere, 2008), in particular HPC. Over the past decade, there has been an increase in cases of squamous cell carcinoma of the oropharynx and a decrease in cases of laryngeal and hypopharynx cancers. This trend is most likely associated with a decrease in cigarette smoking and the identification of exposure to high-risk oncogenic human papillomavirus (HPV) as a risk factor for head and neck cancer (Sturgis and Cinciripini, 2007; Gillison et al., 2012). At the same time, it has recently been said that the true incidence of HPV-associated cancers of the head and neck of the oral cavity, larynx and hypopharynx is only about 5% (Westra, 2015).
HPC in the early stages is often detected with the widespread use of narrow-band imaging (NBI) using magnifying endoscopy (Muto et al., 2010; Popek et al., 2019). Due to the widespread use of NBI with the help of magnifying endoscopy, it is easier to detect tumor recurrence and the appearance of new foci in the radiation field after chemoradiotherapy. NBI is an excellent follow-up method for subsequent screening of patients with HPC who have received chemoradiotherapy (Zabrodsky et al., 2014).
The purpose of this study is to conduct a spatio-temporal assessment of the incidence of HPC. This study will be the first in the Republic to highlight data on the trend of incidence of this pathology.
Materials and Methods
Cancer registration and patient recruitment
The cancer registry of the population of Kazakhstan covers considering the administrative-territorial division. New cases of HPC were extracted from the reporting forms of the Ministry of Health of the Republic of Kazakhstan (Form 7) from 2017 to 2021 using the International Disease Code 10, code C12-14.
Population denominators
The populace data was sourced from the Bureau of National Statistics, incorporating considerations of age and gender attributes along with administrative-territorial demarcations. (Bureau of National Statistics, 2022).
Statistical analysis
The main method of this study was a retrospective study using descriptive and analytical methods of oncoepidemiology. Age-standardized rates (ASR) were calculated for eighteen different age groups (0-4, 5-9, …, 80-84, and 85+) using the world standard population proposed by WHO (Ahmad et al., 2001) with recommendations from the National Cancer Institute (National Cancer Institute, 2013).
The HPC incidence rates were calculated per 100,000 population. A retrospective study using descriptive and analytical methods of modern epidemiology were used. Incidence rates were used in the preparation of cartograms. A mapping method based on the determination of the standard deviation (σ) from the mean value (x) is employed (Igissinov, 1974). The extensive, crude rate (CR) and age-specific incidence rate (ASIR) are determined according to the generally accepted methodology used in sanitary statistics. The annual averages (M, P), mean error (m), Student criterion, 95% confidence interval (95% CI), and average annual upward/downward rates (T, %) were calculated (Merkov and Polyakov, 1974; Glanc, 1999; dos Santos Silva, 1999). Mean error in statistics usually refers to the average value of the differences between estimates and true values (Glanz, 1999). Student’s criterion, also known as t-test is used to compare the means of two groups, and is based on the difference in means divided by an estimate of the standard error of the difference (Glanz, 1999). In addition, we have determined the level of approximation (R2). The level of approximation in linear regression evaluates how close the linear model is to the original data. This indicator reflects how well the model matches the data and how accurately it predicts the values of the dependent variable based on the independent variables. Trends were determined using the least squares method, and the average annual growth rates were calculated using the geometric mean.
The dynamics of indicators was investigated using component analysis according to methodological recommendations (Dvoyrin and Aksel, 1987; Chissov et al., 2007). Component analysis of disease incidence is a methodology used in epidemiological studies to decompose changes in disease rates into components, aiming to identify the impact of various factors on disease dynamics in a specific population. This analysis allows for the separation of changes in disease incidence into several components, which can be as follows:
• Changes in population age structure (∑ΔA): Since the risk of various diseases can vary with age, changes in the population’s age structure (e.g., an increase in the proportion of older individuals) can influence the overall disease incidence.
• Changes in the risk of acquiring illness (∑ΔR): This component reflects alterations in the probability of developing a specific disease within the same age group. Causes of such changes may include modifications in environmental or social factors, lifestyle changes, vaccination efforts, etc.
• Combined influence of the age structure and the risk of acquiring illness (∑ΔAR): This component considers how the interplay between changes in population age structure and alterations in the risk of acquiring illness overall disease incidence.
Component analysis provides deeper insights into the factors influencing disease dynamics and helps identify those with the greatest impact. This analysis is a vital tool for developing and evaluating public health interventions and disease control strategies.
In this study, the component method also was employed to dissect the upsurge in the number of cases within the same population, but at different time periods. The analysis involved considering seven distinct components contributing to the increase in cases. The initial three components pertained to alterations in population size, its age structure, and the combined influence of these factors. The fourth component, representing the genuine increase in the number of patients, was solely attributed to variations in the indicator of the risk of acquiring illness. Subsequently, the next three components were associated with the risk of acquiring illness, population growth, changes in age structure, and the combined impact of all three factors. Consequently, the final four components were associated with an escalation in the risk of acquiring illness. The term “risk of acquiring illness” encompassed the entirety of these factors in the context of disease occurrence.
The following symbols and abbreviations were used in this article: AN – absolute number; ASIR – age specific incidence rate; ASP (ΔA) − the age structure of the population; ASR – age-standardized rate; END − the expected number of diseases; NHPC − the number of new HPC cases; PS (ΔP) − population size; RAI (ΔR) − risk of acquiring illness; R2 – level of approximation; SI − structural indexes; Р − the incidence; 0/0000 – per 100,000.
Ethics approval
Because this study involved the analysis of publicly available administrative data and did not involve contacting individuals, consideration and approval by an ethics review board was not required. At the same time, the submitted data is in accordance with the Law of the Republic of Kazakhstan No. 257-IV of March 19, 2010 “About State statistics” (http://adilet.zan.kz/rus/docs/Z100000257), the information in the summary report is confidential and can only be used for statistical purposes in accordance with the Principles of the World Medical Association (WMA, 2013).
Results
During the study period (2017-2021), 814 new cases of HPC were registered in the country (571 (70.1%) – in men, and 243 (29.9%) – in women). The greatest proportion of patients falls on the age of 55-69 years (55-59 years – 18.7%, 60-64 years – 18.2% and 65-69 years – 19.3%). The male and female populations exhibited distinct differences in the distribution of patients. The age group of 55-69 years showed the highest proportion of patients for both sexes, with males having the largest proportion within this age range. However, for the female population, the age group of 45-69 years showed the highest proportion of patients (Table 1).
Table 1.
Hypopharynx Cancer in Kazakhstan, 2017-2021
| Age | All | Male | Female | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | Incidence | Number | Incidence | Number | Incidence | ||||||||||
| % | per 100,000 | Т, % | R2 | % | per 100,000 | Т, % | R2 | % | per 100,000 | Т, % | R2 | ||||
| ˂ 30 | 7 | 0.6 | 0.02±0.0 | −20.8 | 0.1782 | 4 | 0.7 | 0.02±0.0 | −39.2 | 0.3280 | 3 | 1.2 | 0.01±0.0 | −0.2 | 7E-06 |
| 30-34 | 14 | 1.7 | 0.2±0.0 | +28.2 | 0.6843 | 3 | 0.8 | 0.1±0.1 | +17.8 | 0.0286 | 11 | 4.5 | 0.3±0.1 | +31.3 | 0.2960 |
| 35-39 | 12 | 1.5 | 0.2±0.0 | +16.8 | 0.2693 | 5 | 1.5 | 0.2±0.1 | +38.8 | 0.4252 | 7 | 2.9 | 0.2±0.0 | +5.5 | 0.0500 |
| 40-44 | 37 | 4.5 | 0.6±0.1 | −20.4 | 0.6285 | 18 | 3.0 | 0.6±0.1 | −20.0 | 0.5639 | 19 | 7.8 | 0.6±0.2 | −20.8 | 0.5184 |
| 45-49 | 49 | 6.0 | 0.9±0.1 | +4.3 | 0.0925 | 21 | 5.8 | 0.8±0.2 | +42.5 | 0.8919 | 28 | 11.5 | 1.0±0.2 | −14.7 | 0.3288 |
| 50-54 | 80 | 9.8 | 1.6±0.1 | −6.1 | 0.5333 | 44 | 10.6 | 1.9±0.2 | +3.8 | 0.1254 | 36 | 14.8 | 1.3±0.2 | −17.8 | 0.7828 |
| 55-59 | 152 | 18.7 | 3.1±0.2 | −2.2 | 0.1285 | 99 | 15.2 | 4.4±0.4 | −3.7 | 0.1027 | 53 | 21.8 | 2.0±0.3 | +0.4 | 0.0006 |
| 60-64 | 148 | 18.2 | 3.8±0.3 | −6.8 | 0.4565 | 117 | 17.3 | 7.0±0.7 | −10.9 | 0.8852 | 31 | 12.8 | 1.4±0.3 | +8.7 | 0.1156 |
| 65-69 | 157 | 19.3 | 5.6±0.4 | +2.5 | 0.0910 | 130 | 15.2 | 11.6±1.2 | +4.5 | 0.1137 | 27 | 11.1 | 1.6±0.4 | −8.4 | 0.0643 |
| 70-74 | 83 | 10.2 | 5.0±0.7 | +3.9 | 0.0437 | 68 | 14.3 | 11.2±2.0 | +3.6 | 0.0248 | 15 | 6.2 | 1.4±0.3 | +8.7 | 0.0882 |
| 75-79 | 40 | 4.9 | 3.4±0.3 | +3.8 | 0.1042 | 34 | 10.6 | 8.8±1.6 | +3.7 | 0.0265 | 6 | 2.5 | 0.8±0.5 | +2.6 | 0.0009 |
| 80-84 | 30 | 3.7 | 3.4±0.7 | −16.1 | 0.4132 | 25 | 4.0 | 9.5±1.8 | −15.6 | 0.4505 | 5 | 2.1 | 0.8±0.5 | −14.1 | 0.0319 |
| 85+ | 5 | 0.6 | 1.2±0.6 | +10.2 | 0.0230 | 3 | 1.2 | 2.5±1.9 | +18.3 | 0.0291 | 2 | 0.8 | 0.6±0.4 | −0.3 | 1E-05 |
| Total | 814 | 100.0 | 0.9±0.0 | −0.8 | 0.0443 | 571 | 100.0 | 1.3±0.1 | +0.4 | 0.0048 | 243 | 100.0 | 0.5±0.0 | −3.6 | 0.2255 |
T, average annual upward/downward rates; R2, the value of the approximation confidence; CR, crude rate
The average age of patients with HPC in dynamics increased slightly from 60.3±0.8 years (95%CI=58.7-61.9) in 2017 to 61.2±0.8 years (95%CI=59.6-62.8), and average annual rate of growth made T=+0.3. The average age of patients was 61.2±0.3 years (95%CI=60.6-61.8). The average age of male patients was 63.3±0.2 years, while female patients had an average age of 56.3±0.7 years.
In both sexes, the age-specific incidence rates of HPC reached their highest point at 65-69 years (5.6±0.40/0000). Specifically, for the male population, the peak incidence rate was observed at 65-69 years (11.6±1.20/0000), while for the female population, it occurred at 55-59 years (2.0±0.30/0000) (Table 1).
HPC incidence rates exhibited diverse trends across age groups. The most notable annual average decreases were observed in the under 30 years age group (T=−20.8%) and the 40-44 years age group (T=−20.4%). Conversely, the most substantial upward trend was found in the 30-34 years age group (T=+28.2%). In the male population, trends in ASIR had a high level of approximation in such age groups as 40-44 years (T=−20.0%; R2=0.5639), 45-49 years (T=+42.5%; R2=0.8919) and 60-64 years (T=−10.9%; R2=0.8852). Among the female population, trends in ASIR had a high level of approximation only in two age groups: 40-44 years (T=−20.8%; R2=0.5184) and 60-64 years (T=−17.8%; R2=0.7828) (Table 1).
Different trends in age-related incidence rates in general affected the overall incidence rates, therefore, the overall incidence rate of HPC among the entire population of the country during the study period decreased very slightly, the total decline was −0.0030/0000 (Table 2) and depended on changes in the age structure of the population (∑ΔA=+0.040/0000), the risk of acquiring illness (∑ΔR=−0.050/0000) and the combined influence of the age structure and the risk of acquiring illness (∑ΔAR=+0.010/0000). At the same time, the average annual decline of the aligned indicator was T=−0.8%, and the approximation confidence value was low (R2=0.0443).
Table 2.
Component Analysis of the Hypopharynx Cancer Incidence Growth in Kazakhstan, 2017-2021
| Age group (i) | ASP | Growth (Si2−Si1) (3)−(2) |
Incidence | Incidence growth | |||||
|---|---|---|---|---|---|---|---|---|---|
| general (Pi2−Pi1) (6)−(5) | Including due to changes of | ||||||||
| 2017 (Si1) | 2021 (Si2) | 2017 (Pi1) | 2021 (Pi2) | Δ A (4)×(5) | Δ R (2)×(7) | Δ RA (4)×(7) | |||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Both sexes | |||||||||
| <30 | 0.5032 | 0.4917 | −0.0115 | 0.01 | 0.00 | +0.0 | −0.000 | −0.006 | +0.000 |
| 30-34 | 0.0826 | 0.0857 | +0.0030 | 0.13 | 0.31 | +0.2 | +0.000 | +0.014 | +0.001 |
| 35-39 | 0.0696 | 0.0726 | +0.0030 | 0.08 | 0.15 | +0.1 | +0.000 | +0.005 | +0.000 |
| 40-44 | 0.0636 | 0.0634 | −0.0002 | 0.96 | 0.42 | −0.5 | +0.000 | −0.034 | +0.000 |
| 45-49 | 0.0589 | 0.0581 | −0.0008 | 0.94 | 1.19 | +0.2 | −0.001 | +0.014 | +0.000 |
| 50-54 | 0.0568 | 0.0531 | −0.0037 | 1.95 | 1.50 | −0.5 | −0.007 | −0.026 | +0.002 |
| 55-59 | 0.0536 | 0.0526 | −0.0010 | 3.10 | 3.12 | +0.0 | −0.003 | +0.001 | +0.000 |
| 60-64 | 0.0393 | 0.0448 | +0.0055 | 4.79 | 3.19 | −1.6 | +0.026 | −0.063 | −0.009 |
| 65-69 | 0.0291 | 0.0314 | +0.0023 | 5.53 | 6.57 | +1.0 | +0.013 | +0.030 | +0.002 |
| 70-74 | 0.0139 | 0.0213 | +0.0074 | 3.59 | 5.46 | +1.9 | +0.027 | +0.026 | +0.014 |
| 75-79 | 0.0165 | 0.0098 | −0.0067 | 3.36 | 3.24 | −0.1 | −0.022 | −0.002 | +0.001 |
| 80-84 | 0.0081 | 0.0108 | +0.0027 | 3.43 | 1.96 | −1.5 | +0.009 | −0.012 | −0.004 |
| 85+ | 0.0047 | 0.0047 | +0.0000 | 0.00 | 0.00 | +0.0 | +0.000 | +0.000 | +0.000 |
| Total | ∑Si1=1.0 | ∑Si2=1.0 | P 1=0.90 | P 2=0.90 | −0.003 | ∑ΔA=+0.04 | ∑ΔR=−0.05 | ∑ΔRA=+0.01 | |
| Male* | |||||||||
| Total | ∑Si1=1.0 | ∑Si2=1.0 | P 1=1.20 | P 2=1.30 | +0.10 | ∑ΔA=+0.07 | ∑ΔR=+0.02 | ∑ΔRA=+0.01 | |
| Female* | |||||||||
| Total | ∑Si1=1.0 | ∑Si2=1.0 | P 1=0.61 | P 2=0.51 | −0.10 | ∑ΔA=+0.02 | ∑ΔR=−0.12 | ∑ΔRA=+0.01 | |
Δ A, the age structure of the population; ΔR, risk of acquiring illness; ΔRA, risk of acquiring illness and age structure of the population.; *The calculations were made in the same way as for the entire population.
In the male population of the republic, the crude incidence rates increased from 1.200/0000 (2017) to 1.300/0000 in 2021. The overall growth (+0.100/0000) depended on changes in the age structure of the population (∑ΔA=+0.070/0000) and the risk of acquiring illness (∑ΔR=+0.020/0000), and their combined effect was not pronounced (∑ΔRA=+0.010/0000) (Table 2). The average annual growth rate was T=+0.4% and the approximation value is R2=0.0048 (Table 1).
In the female population of the country, there was an overall decrease (−0.100/0000) in crude incidence rates from 0.610/0000 in 2017 to 0.510/0000 in 2021. This decline was influenced by changes in the age structure of the population (∑ΔA=+0.020/0000), a reduction in the risk of acquiring the illness (∑ΔR=−0.120/0000), and the combined effect of age structure and the risk of acquiring the illness (∑ΔRA=+0.010/0000) (T=−3.6; R2=0.2255) (Tables 1 and 2).
Further, we will consider the results of a component analysis of the dynamics of the number of patients with HPC in the whole population, in men and women (Tables 3 and 4). The results of the study show that the change in the number of patients with HPC in the republic was associated with the influence of the following factors:
Table 3.
Component Analysis of the Hypopharynx Cancer Incidence in Dynamics in Kazakhstan, 2017-2021
| Age group (i) | NHC (nij) | PN (Nij) | Crude (Pij) | Standardized Pijc | END in 2021 (PijNi210-5) (6)×(5)×10-5 | ||||
|---|---|---|---|---|---|---|---|---|---|
| 2017 (j=1) | 2021 (j=2) | 2017 (j=1) |
2021 (j=2) |
2017 (j=1) |
2021 (j=2) |
2017 (j=1) |
2021 (j=2) |
||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Both sex | |||||||||
| <30 | 1 | 0 | 9077430 | 9283015 | 0.01 | 0.00 | 0.000 | 1.0 | |
| 30-34 | 2 | 5 | 1490787 | 1617067 | 0.13 | 0.31 | 0.026 | 2.2 | |
| 35-39 | 1 | 2 | 1255442 | 1370229 | 0.08 | 0.15 | 0.010 | 1.1 | |
| 40-44 | 11 | 5 | 1147710 | 1196696 | 0.96 | 0.42 | 0.027 | 11.5 | |
| 45-49 | 10 | 13 | 1061587 | 1096284 | 0.94 | 1.19 | 0.070 | 10.3 | |
| 50-54 | 20 | 15 | 1024469 | 1002632 | 1.95 | 1.50 | 0.085 | 19.6 | |
| 55-59 | 30 | 31 | 966855 | 992169 | 3.10 | 3.12 | 0.167 | 30.8 | |
| 60-64 | 34 | 27 | 709528 | 846439 | 4.79 | 3.19 | 0.125 | 40.6 | |
| 65-69 | 29 | 39 | 524698 | 593409 | 5.53 | 6.57 | 0.191 | 32.8 | |
| 70-74 | 9 | 22 | 250755 | 403052 | 3.59 | 5.46 | 0.076 | 14.5 | |
| 75-79 | 10 | 6 | 297457 | 185323 | 3.36 | 3.24 | 0.053 | 6.2 | |
| 80-84 | 5 | 4 | 145957 | 203846 | 3.43 | 1.96 | 0.016 | 7.0 | |
| 85+ | 0 | 0 | 85102 | 89391 | 0.00 | 0.00 | 0.000 | 0.0 | |
| Total | n 1=162 | n 2=169 | N 1=18037776 | N 2=18879552 | P 1=0.90 | P 2=0.90 | P 1 c=0.90 | P 2 c=0.85 | E(n 2 )=177 |
| Growth | |||||||||
| Male* | |||||||||
| Total | n 1=105 | n 2=119 | N 1=8729888 | N 2=9160399 | P 1=1.20 | P 2=1.30 | P 1 c=1.20 | P 2 c=1.22 | E(n 2 )=117 |
| Growth | |||||||||
| Female* | |||||||||
| Total | n 1=57 | n 2=50 | N 1=9307888 | N 2=9719153 | P 1=0.61 | P 2=0.51 | P 1 c=0.61 | P 2 c=0.49 | E(n 2 )=61 |
| Growth | |||||||||
END, the expected number of diseases; *, The calculations were made in the same way as for the entire population.
Table 4.
Influencing Components on the Number of Cases of Hypopharynx Cancer in Kazakhstan
| Components of growth in the number of cases due to: | Both sexes | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|---|
| AN | %, growth | AN | %, growth | AN | %, growth | ||||
| to (n2-n1) | to n1 | to (n2-n1) | to n1 | to (n2-n1) | to n1 | ||||
| 1. Growth PN. | 8 | +108.0 | +4.7 | 5 | +37.0 | +4.9 | 3 | +36.0 | +4.4 |
| 2. Changes ASP. | 7 | +106.1 | +4.6 | 6 | +44.1 | +5.9 | 1 | +21.0 | +2.6 |
| 3. Combined effect of changes in PN+ASP. | +0.3 | +5.0 | +0.2 | +0.3 | +2.2 | +0.3 | +0.1 | +0.9 | +0.1 |
| ∑1-3=+219.0 ∑1-3=+9.5 | ∑1-3=+83.2 ∑1-3=+11.1 | ∑1-3=+57.9 ∑1-3=+7.1 | |||||||
| 4. Change of RAI. | −9 | −133.4 | −5.8 | 2 | +10.8 | +1.4 | −11 | −160.4 | −19.7 |
| 5. Combined effect of changes of RAI+PN. | −0.4 | −6.2 | −0.3 | +0.1 | +0.5 | +0.1 | −0.5 | −7.1 | −0.9 |
| 6. Combined effect of changes of RAI+ASP. | +1.4 | +19.7 | +0.9 | +0.7 | +5.2 | +0.7 | +0.6 | +9.2 | +1.1 |
| 7. Combined effect of the changes RAI+PN+ASP. | +0.1 | +0.9 | +0.04 | 0.0 | +0.3 | +0.03 | +0.04 | +0.4 | +0.05 |
| ∑4-7=−119.0 ∑4-7=−5.1 | ∑4-7=+16.8 ∑4-7=+2.2 | ∑4-7=−157.9 ∑4-7=−19.4 | |||||||
| Total ∑1-7 | 7 | 100.0 | +4.3 | 14 | 100.0 | +13.3 | −7 | 100.0 | −12.3 |
AN, absolute number; PN, population number; ASP, age structure of the population; RAI, risk of acquiring illness.
1. Growth of population number ΔP=+108.0% (Male – ΔP=+37.0%; Female – ΔP=+36.0%).
2. Changes in the age structure of the population ΔA=+106.1% (Male – ΔA=+44.1%; Female – ΔA=+21.0%).
3. Combined effect of changes in population number and its age structure ΔPA=+5.0% (Male – ΔPA=+2.2%; Female – ΔPA=+0.9%).
4. Change in the risk of acquiring illness ΔR=−133.4% (Male – ΔR=+10.8%; Female – ΔR=−160.4%).
5. Combined effect of changes in the risk of acquiring illness and population number ΔPR=−6.2% (Male – ΔPR=+0.5%; Female – ΔPR=−7.1%).
6. Combined effect of changes in the risk of acquiring illness and age structure of the population ΔRA=+19.7% (Male – ΔRA=+5.2%; Female – ΔRA=+9.2%).
7. Combined effect of the changes in the risk of acquiring illness, population number and its age structure ΔRAP=+0.9% (Male – ΔRAP=+0.3%; Female – ΔRAP=+0.4%).
The overall increase in the absolute number of patients, considering both sexes, amounts to 7 or +4.3% compared to the initial number of patients.
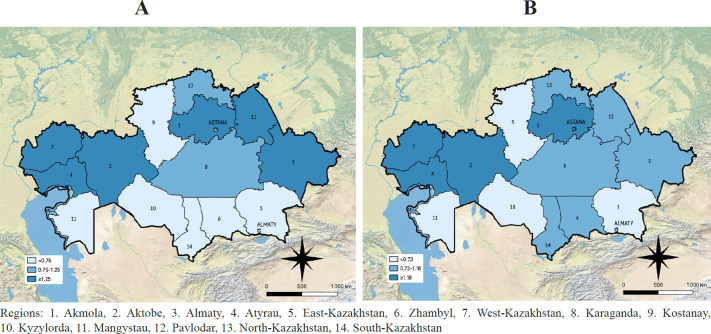
Based on the calculated average annual CR and ASR HPC indicators, the cartograms were compiled. The levels of HPC CR per 100,000 based on the following criteria were determined: low – up to 0.75, average – from 0.75 to 1.25, high – above 1.25. As a result, the following groups of regions were revealed (Figure 1 A):
Figure 1.
Cartogram of Hypopharynx Cancer Incidence in Kazakhstan (A – CR, B – ASR)
1. Regions with the lowest indicators (up to 0.75 per 100,000): Kostanay (0.37), Mangystau (0.50), Kyzylorda (0.53), Almaty (0.54), South Kazakhstan (0.56), Almaty city (0.57), Zhambyl (0.66).
2. Regions with average indicators (from 0.75 to 1.25 per 100,000): Astana city (0.84), Karaganda (0.91), North Kazakhstan (1.23).
3. Regions with high indicators (1.25 and above per 100,000): Aktobe (1.30), Pavlodar (1.33), East Kazakhstan (1.51), Atyrau (1.63), Akmola (1.76), West Kazakhstan (1.81).
The levels of HPC ASR per 100,000 population based on the following criteria were determined: low – up to 0.73, average – from 0.73 to 1.18, high – above 1.18. As a result, the following groups of regions were determined (Figure B):
1. Regions with the lowest indicators (up to 0.73 per 100,000): Kostanay (0.27), Almaty (0.53), Almaty city (0.55), Kyzylorda (0.60), Mangystau (0.61), Zhambyl (0.72).
2. Regions with average indicators (from 0.73 to 1.18 per 100,000): Karaganda (0.73), South Kazakhstan (0.80), North Kazakhstan (0.82), Pavlodar (1.03), East Kazakhstan (1.10).
3. Regions with high indicators (1.18 per 100,000 and above): Astana city (1.24), Aktobe (1.33), Akmola (1.37), West Kazakhstan (1.58), Atyrau (1.96).
Discussion
The incidence of hypopharynx cancer in Kazakhstan is generally decreasing. At the same time, according to the level of incidence, our country belongs to regions with a high incidence rate. In countries such as Madagascar (0.910/0000), Austria (0.880/0000) and Georgia (0.960/0000), the incidence rate was near that observed in our country.
Depending on the geographical location, the incidence of HPC among men and women varies greatly. In general, the incidence among men is 5 times higher than among women (Tangjaturonrasme et al., 2018). In Kazakhstan, the ratio was below the world average, namely 2.6:1. A similar indicator was found among patients in England (3:1) (Louie et al., 2015). In Kazakhstan, the incidence of HPC, as we see, has differences in relation to the sex of patients. Changes in the ratio of morbidity among men and women in the time curve indirectly reflect the local changing social habits of people at the regional level. Over the past five years, the incidence among men has a slight upward trend, and the incidence among women has a more pronounced rate of decline. At the same time, the level of approximation of the two indicators is very low. A similar trend was found in England, where the incidence also increased among men and decreased among women (Louie et al., 2015).
In Korea (Shin et al., 2013), France (Ligier et al., 2011), Italy (Associazione Italiana Registri Tumori, 2020) and North America (Kuo et al., 2014), the incidence of HPC is also decreasing. Trends in the incidence of HPC over time and in different countries strongly depend on the nature of tobacco use or the combined effect of tobacco and alcohol use. In this regard, it is necessary that the main potentially changeable factors, such as tobacco and alcohol consumption, be prevented through legislative measures and the promotion of a healthy lifestyle. On the other hand, the study of differences in geographical distribution and trends in the incidence of HPC in many countries is often problematic, since the presentation of available data is difficult due to its anatomical features, as well as the presence of late-stage tumors that are mistaken for laryngeal cancer, resulting in incorrect classification of the disease (Bradley, 2019).
The incidence increases with age at the time of diagnosis in the range from 40 to 80 years (El Bedoui and Lefebvre, 2017). In our study, it was observed that the highest incidence of the disease in our country occurs between the fifth and eighth decades of life. As a result of the component analysis, we see that the incidence of HPC of the entire population is equally affected by both demographic indicators and the risk of acquiring illness. But considering separately the incidence among men and women, it was found that the increase in the incidence among the male population occurred mainly due to an increase in demographic indicators. On the contrary, the incidence among the female population tended to decrease due to a stronger reduction in the influence of risk of acquiring illness. Previously, studying the incidence of laryngeal cancer in Kazakhstan by component analysis, it was also found that the decrease in incidence is mainly due to a decrease in the influence of the risk of acquiring illness (Zatonskikh et al., 2016).
The incidence of HPC in Kazakhstan displays regional variations, with higher rates observed in the western and eastern regions and lower rates in the southern regions. The elevated incidence rates, particularly in certain areas, raise concerns as HPC carries a poor prognosis, ranking among the most unfavorable outcomes among all head and neck tumors. Often diagnosed at an advanced stage, HPC poses significant economic consequences, particularly in developing countries. Therefore, precise epidemiological investigations of the current and projected disease patterns are imperative to enhance diagnostic and treatment strategies.
Author Contribution Statement
DA, ZhT, DT – Collection and preparation of data, primary processing of the material and their verification. DA, DK, ZhT – Statistical processing and analysis of the material, writing the text of the article (material and methods, results). ZB, DA, GI – Writing the text of the article (introduction, discussion). AM, NI – Concept, design and control of the research, approval of the final version of the article. All authors approved the final version of the manuscript.
Acknowledgements
The authors greatly appreciate the contribution of the Ministry of Healthcare of the Republic of Kazakhstan to the current research by providing the data.
This study was not funded, it was performed within the framework of Darkhan Ahmedin’s dissertation, the topic of the dissertation was approved at the University Council of Astana Medical University.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Ahmad OE, Boschi-Pinto C, Lopez AD, et al. Age standardization of rates: a new who standard. GPE Discussion Paper Series: No.31 EIP/GPE/EBD. World Health Organization; 2001. [Google Scholar]
- Associazione Italiana Registri Tumori (AIRTUM) Cancer in Italy, Italian Association of Cancer Registries (cited 2022 Oct 24) 2020. Available from: https://www.registri-tumori.it/cms/pubblicazioni/i-numeri-del-cancro-italia-2020.
- Bradley PJ. Epidemiology of Hypopharyngeal Cancer. Adv Otorhinolaryngol. 2019;83:1–14. doi: 10.1159/000492299. [DOI] [PubMed] [Google Scholar]
- Bureau of National Statistics of the Agency for Strategic Planning and Reforms of the Republic of Kazakhstan. 2022. [(cited 2022 Oct 5)]. Available from official website of the: https://stat.gov.kz /
- Carvalho AL, Nishimoto IN, Califano JA, Kowalski LP. Trends in incidence and prognosis for head and neck cancer in the United States: a site-specific analysis of the SEER database. Int J Cancer. 2005;114:806–16. doi: 10.1002/ijc.20740. [DOI] [PubMed] [Google Scholar]
- Chissov V, Starinskiy V, Kovalev B. The organization of oncological service in Russia (methodical recommendations, manuals for doctors) Мoscow: 2007. p. p 663. (Russian) [Google Scholar]
- de Souza DL, Pérez MM, Curado MP. Gender differences in the incidence of laryngeal and hypopharyngeal cancers in Spain. Cancer Epidemiol. 2011;35:328–33. doi: 10.1016/j.canep.2011.02.003. [DOI] [PubMed] [Google Scholar]
- dos Santos Silva. Cancer epidemiology: principles and methods. Lyon, France: IARC; 1999. p. p 442. [Google Scholar]
- Dvoyrin VV, Aksel EM. Component analysis of the dynamics of malignant neoplasms: guidelines. Moscow: 1987. p. p 130. [Google Scholar]
- El Bedoui S, Lefebvre JL. Chapter 34 Management of Larynx and Hypopharyngeal Cancer in Otolaryngology Head and Neck Surgery, ed 2, 2017 . 2017. [(cited 2022 Oct 2)]. Available from: http://emedicine360.com/Jaypee.
- Emura F, Baron TH, Gralnek IM. The pharynx: examination of an area too often ignored during upper endoscopy. Gastrointest Endosc. 2013;78:143–9. doi: 10.1016/j.gie.2013.02.021. [DOI] [PubMed] [Google Scholar]
- Ferlay J, Ervik M, Lam F, et al. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer ; 2022. [(cited 2022 Sep 30)]. Available from: https://gco.iarc.fr/today. [Google Scholar]
- Gillison ML, Broutian T, Pickard RK, et al. Prevalence of oral HPV infection in the United States, 2009-2010. JAMA. 2012;307:693–703. doi: 10.1001/jama.2012.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanc S. Biomedical statistics. Moscow, Practice: 1999. p. P 460. (Russian) [Google Scholar]
- Igissinov SI. Preparation and application method of cartograms in oncology. Healthcare Kazakhstan. 1974;2:69–71. [Google Scholar]
- Jayalekshmi PA, Nandakumar A, Akiba S, Gangadharan P, Koriyama C. Associations of tobacco use and alcohol drinking with laryngeal and hypopharyngeal cancer risks among men in Karunagappally, Kerala, India -Karunagappally cohort study. PLoS One. 2013;8:e73716. doi: 10.1371/journal.pone.0073716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo P, Chen MM, Decker RH, Yarbrough WG, Judson BL. Hypopharyngeal cancer incidence, treatment, and survival: temporal trends in the United States. Laryngoscope. 2014;124:2064–9. doi: 10.1002/lary.24651. [DOI] [PubMed] [Google Scholar]
- Ligier K, Belot A, Launoy G, et al. Descriptive epidemiology of upper aerodigestive tract cancers in France: incidence over 1980-2005 and projection to 2010. Oral Oncol. 2011;47:302–7. doi: 10.1016/j.oraloncology.2011.02.013. [DOI] [PubMed] [Google Scholar]
- Louie KS, Mehanna H, Sasieni P. Trends in head and neck cancers in England from 1995 to 2011 and projections up to 2025. Oral Oncol. 2015;51:341–8. doi: 10.1016/j.oraloncology.2015.01.002. [DOI] [PubMed] [Google Scholar]
- Marur S, Forastiere AA. Head and neck cancer: changing epidemiology, diagnosis, and treatment (published correction appears in Mayo Clin Proc. 2008 May;83(5):604. Mayo Clin Proc. 2008;83:489–501. doi: 10.4065/83.4.489. [DOI] [PubMed] [Google Scholar]
- Merkov AM, Polyakov LE. Sanitary statistics. Leningrad, Medicine; 1974. p. p 384. (Russian) [Google Scholar]
- Mishra A, Meherotra R. Head and neck cancer: global burden and regional trends in India. Asian Pac J Cancer Prev. 2014;15:537–50. doi: 10.7314/apjcp.2014.15.2.537. [DOI] [PubMed] [Google Scholar]
- Muto M, Minashi K, Yano T, et al. Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: a multicenter randomized controlled trial. J Clin Oncol. 2010;28:1566–72. doi: 10.1200/JCO.2009.25.4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. Recommendations on the use of the World Standard (WHO 2000-2025) (cited 2022 Sep 16) 2013. Available from: http://seer.cancer.gov/stdpopulations/world.who.html.
- Popek B, Bojanowska-Poźniak K, Tomasik B, et al. Clinical experience of narrow band imaging (NBI) usage in diagnosis of laryngeal lesions. Otolaryngol Pol. 2019;73:18–23. doi: 10.5604/01.3001.0013.3401. [DOI] [PubMed] [Google Scholar]
- Sanders O, Pathak S September 26, 2022, authors. StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. Hypopharyngeal Cancer. [PubMed] [Google Scholar]
- Sapkota A, Gajalakshmi V, Jetly DH, et al. Smokeless tobacco and increased risk of hypopharyngeal and laryngeal cancers: a multicentric case-control study from India. Int J Cancer. 2007;121:1793–8. doi: 10.1002/ijc.22832. [DOI] [PubMed] [Google Scholar]
- Shin A, Jung YS, Jung KW, et al. Trends of human papillomavirus-related head and neck cancers in Korea: national cancer registry data. Laryngoscope. 2013;123:30–7. doi: 10.1002/lary.24243. [DOI] [PubMed] [Google Scholar]
- Simard EP, Torre LA, Jemal A. International trends in head and neck cancer incidence rates: differences by country, sex and anatomic site. Oral Oncol. 2014;50:387–403. doi: 10.1016/j.oraloncology.2014.01.016. [DOI] [PubMed] [Google Scholar]
- Sturgis EM, Cinciripini PM. Trends in head and neck cancer incidence in relation to smoking prevalence: an emerging epidemic of human papillomavirus-associated cancers? Cancer. 2007;110:1429–35. doi: 10.1002/cncr.22963. [DOI] [PubMed] [Google Scholar]
- Tangjaturonrasme N, Vatanasapt P, Bychkov A. Epidemiology of head and neck cancer in Thailand. Asia Pac J Clin Oncol. 2018;14:16–22. doi: 10.1111/ajco.12757. [DOI] [PubMed] [Google Scholar]
- The Law of the Republic of Kazakhstan No. 257-IV of March 19, 2010 “About State statistics”. Available from: http://adilet.zan.kz/rus/docs/Z100000257.
- Westra WH. The pathology of HPV-related head and neck cancer: implications for the diagnostic pathologist. Semin Diagn Pathol. 2015;32:42–53. doi: 10.1053/j.semdp.2015.02.023. [DOI] [PubMed] [Google Scholar]
- WMA Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects. 2013. Available from: https://www.wma.net/ [PubMed]
- Zabrodsky M, Lukes P, Lukesova E, Boucek J, Plzak J. The role of narrow band imaging in the detection of recurrent laryngeal and hypopharyngeal cancer after curative radiotherapy. Biomed Res Int. 2014;2014:175398. doi: 10.1155/2014/175398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatonskikh V, Igissinov N, Igissinov S, et al. Component Analysis of Laryngeal Cancer Incidence Dynamics in Kazakhstan from 1999 to 2014. Asian Pac J Cancer Prev. 2016;17:4451–6. [PubMed] [Google Scholar]