Abstract
Objective:
Compare the breast cancer mortality rate and the rate of mammograms with socioeconomic factors, in Brazilian´s Federative Units, during the period of 2015 to 2021.
Methods:
This is an ecological study, of a descriptive nature, which covers the 27 Brazilian federative units, using secondary data extracted from the DATASUS System. The information analyzed was mammography data, breast cancer mortality, demographic and economic data of the resident population and women over 20 years of age.
Results:
There is a direct relationship between mortality rate and mammograms rates in the Federative Units. The data obtained for Brazil presents a total of 133,048 deaths from breast cancer and 17,324,526 mammography exams in the period from 2015 to 2021. In other words, Brazil presents a standardized mortality rate value, 19.25 deaths per 100,000 women. Regarding the mammography rate, the value of the exam-specific mammography rate was 2,506.55 per 100,000 women. In relation to socioeconomic data by mortality rate group, higher mortality rates from breast cancer present higher rates in the variables: income rate by State (2,594.86), people with income (63.5), average percentage of women with more over 50 years old (29.5%), women with average years of education (6.64), white population (55.1%) and mammography exam rate (2873.20). When analysing the highest rates of mammography exam rates, higher rates are observed income rate by State (2,161.47), people with income (62.5%), average percentage of women over 50 years old (28.6%), women with an average number of years of education (5.8).
Conclusion:
Brazil has a high mortality rate due to breast cancer, when compared to other countries. The reasons are diverse, such as the modern, industrialized and populous lifestyle. The Federative Units with the highest mortality rate also have high rates of mammograms, that is, in the Federative Units with “better” sociodemographic conditions, the South and Southeast.
Key Words: Breast cancer, mammography, mortality rate
Introduction
Breast cancer is a public health problem both nationally and internationally, therefore it represents a high priority in the field of medical research (Anastasiadi et al., 2017). Among the types of cancer, breast cancer is the most common one in women in most countries, including Brazil (Kolak et al., 2017; Lei et al., 2021; Luo et al., 2022). Data indicate that 1 in 8 women will develop breast cancer throughout their lives (INCA, 2022).
In addition to being the most common neoplasm in females, breast cancer is the type of cancer responsible for the highest number of deaths worldwide, with an estimated 15% of cancer deaths in women globally (Ferreira et al., 2021). However, great advances in the treatment are being made (Harbeck and Gnant, 2017) and with this, the achieved survival rates are around 76.5% in 5 years (PAHO, 2020), whereas other authors such as Peres et al. (Peres et al.,2015) indicate 90% in 5 years. Despite that, 10% of women may still develop a recurrence, leading to death.
The improvement of diagnosis and treatment for breast cancer is constant, but the biological differentiation of individuals, the complexity of the tumor and exposure to numerous risk factors, consequently, results in a type of disease defined by a dynamic behavior and in continuous variation (Ferreira et al., 2021). From this, the annual incidence rate of breast cancer is around 60 per 100,000 women in Brazil (Ferreira et al., 2021).
Considering the Brazilian regions, generally, the highest incidence rates of breast cancer (Girianelli et al., 2014; INCA, 2022) are found in the South and Southeast, as well as in the Midwest. Regarding standardized breast cancer mortality rates, according to some studies (Girianelli et al., 2014; INCA, 2022) in Brazil, over 35 years of observation (between 1980 and 2016), the values changed from 9.2 deaths to 12.4 deaths per 100,000 women, which means an increase of 33.6%. When we analyze the breast cancer mortality rate by region, according to the Nation Institute of Cancer (2022) bulletin, the South, Southeast and Midwest have higher rates than others. Possibly, one of the reasons, as argued by Girianelli, Gamara and Silva (2014) is the presence of social and regional inequalities and the socio-demographic transformations experienced. These changes refer to dietary patterns, reproductive characteristics as well as the prevalence of cancer-related infections. Although developed countries, in recent decades, have been documenting a decrease in breast cancer mortality rates, this trend is associated with the reduction of hormone replacement therapy and the detection of preclinical cases by initial screening (Girianelli et al., 2014).
Among the ways of detection, an important tool against breast cancer is the mammography (Allemani et al., 2018; Kim et al., 2019). However, authors such as Gøtzsche (2015) and Miller (2003) highlight that mammography exams are a controversial topic. Furthermore, in Brazil, the Ministry of Health considers mammography examinations as early or late diagnosis and not as screening (Corrêa et al., 2017).
This exam is responsible for the diagnosis of clinically evident lesions and the detection of subclinical lesions, hence, the screening process (Lopes et al., 2015). Lesions detected by mammograms, in general, are smaller than those clinically identified (Miller et al., 2014), which means that with the mammography, breast cancer can be detected in early stages, helping in early treatment and consequently increasing the chance of cure. Smaller lesions confer a better prognosis (Barbosa et al., 2016; Cavalcante et al., 2021; Løberg et al., 2015). Thus, with early detection it is possible to reduce the number of mastectomies in relation to the number of breast-conserving surgeries (Barbosa et al., 2015; Cavalcante et al., 2021). In view of this, it has been argued that performing a mammogram reduces the mortality rate associated with breast cancer (Kim et al., 2019).
The increase in the mortality rate from breast cancer is not a recent topic, with studies by INCA (2022) and Girianelli, Gamara and Silva (2014) showing this trend when analyzing the period from 1980 to 2006. However, from 2008 and forward, there was an increase in the acquisition of mammography devices (Moura et al., 2020), so currently in Brazil, there are a total of 5,061 mammography devices, of which 4,844 are operational, and 2,171 are available to the Brazilian Public Healthcare System (SUS) (INCA, 2022). The coverage of mammograms in Brazil according to a study by Rodrigues et al. (2020) shows a possible difficulty for the population to access the mammography devices. Furthermore, it was discovered that, in the region of Goiás, the number of devices is sufficient; however, the number of tests performed is not. In the research by Lopes et al. (Lopes et al., 2015) in the State of Paraná, despite the number of mammography devices being above the recommended level, a tendency towards increased mortality from breast cancer was found, possibly due to poor distribution of devices, difficulties in accessing mammography devices by the population, or even late screening and diagnosis. Other authors (Rodrigues et al., 2020) comment on this inconsistency, since it is expected that the increase in mammograms will result in a reduction of the mortality rate and not the other way around. However, some authors (Barbosa et al., 2016; Fayer et al., 2020; Løberg et al., 2015; Luo et al., 2022) indicate that groups with lower socioeconomic conditions have shown high mortality from cancer due to a series of associated factors, such as, a lack of knowledge about the disease, late diagnosis of neoplasms that could be detected in the early stages through proper screening, greater difficulty in accessing diagnostic methods and adequate treatment. All this results in the arrival of patients in advanced stages of breast cancer, worsening the prognosis and presenting lower survival rates after diagnosis.
It is evident that there is such an inconsistency between the greater number of mammograms and high mortality rates, especially in developing countries (Barbosa et al., 2016; Løberg et al., 2015; Luo et al., 2022;). In regard to Brazil, this high number of mammograms possibly favors certain social strata, such as women with higher income, white and possessing higher education (Rodrigues et al., 2020). In view of all this, the present study aims to compare the breast cancer mortality rate and the rate of mammograms with sociodemographic and economic factors by the Brazilian Federative Units (UF) during the period of 2015 to 2021.
Materials and Methods
Design and Data Collection
This is an ecological study, using secondary data extracted from the DATASUS System – TABNET, from the Department of Informatics of SUS, which belongs to the Ministry of Health, and can be accessed through the website www2.datasus.gov.br/DATASUS/ index.php?area=02.
In addition, data on mammography were consulted from the link http://siab.datasus.gov.br/DATASUS/index.php?area=02 on “Health Care” and “Outpatient Production (SAI/SUS)”. To obtain data on mortality from breast cancer, we used the link http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sim/cnv/obt10uf.def under “vital stats” e “Mortality - 1996 to 2021, by ICD-10”, considering the Manual of International Statistical Classification of Diseases and Related Health Problems, in which breast cancer corresponds to the code C50. As for sociodemographic data, they were obtained through the link https://datasus.saude.gov.br/demograficas-e-socioeconomicas/ from “Demographic and Socioeconomic” and “Resident population”, also from DataSUS for the female population over 20 years of age by Federative Unit of Brazil.
Data Analisys
To calculate the gross mortality rate per 100,000 women, we divided the total number of deaths by the total population and multiplied by 100,000 women. The standardized mortality rate (SMR) was calculated from the observed deaths, divided by the expected deaths and multiplied by 100,000 women. The age groups were divided into 4 different groups (≤ 39 years, 40-59 years, 60-79 years and ≥ 80 years), and the age-standardized mortality rate was calculated by the direct method. Therefore, we performed the average mortality in the 7 years divided by the average of the female population, multiplied by 100,000. We also determined the respective 95% confidence intervals (95% CI) from the formula, TMP ± (1.96 X SE), where SE is the standard deviation. To determine the specific mammography rate, we determined the average number of mammograms performed in the Federative Units divided by the average of the female population in these 7 years and multiplied by 100,000 women. We computed the Comparative Mortality Ratio (CMR) to compare the rates. This index is interpreted as follows: CMR < 1 means that the observed mortality was lower than predicted, while values > 1 indicate that the mortality found was higher than predicted. For sociodemographic and economic data, the average rate and the percentage were calculated.
For the analysis of the descriptive data (proportions and averages) the Microsoft Excel program (2013 version) was used, for the Spearman correlation analysis and graph the R software (version 3.5) was used and the geographic distribution map was designed with the GQIS program (version 3.16).
Ethical Requests
The analyzed data come from secondary sources of public access, and without the possibility of individual identification of the information. Thus, in accordance with the recommendations in the National Health Council (CNS) resolution nº 466, of December 12, 2012, the ethical principles of research were respected, and this study was submitted to the Ethics Committee in Research involving human beings of Inga University Center (Maringá-Pr. Brazil), with CAAE (Certificate of Presentation for Ethical Appraisal) 51654021.4.0000.5220 and approved opinion number 4.997.733/2021.
Results
Descriptive Analysis
The data obtained for Brazil show a total of 133,048 deaths from breast cancer and 17,324,526 mammograms in the period from 2015 to 2021. The general result is that Brazil presents a standardized mortality rate (TMP) of 19.25 (95% CI 19.15-19.35) deaths per 100,000 women. As shown in Table 1, we can see that Rio de Janeiro represents the Federative Unit with the highest standardized mortality rate per 100,000 women (TMP=28.88; 95% CI 28.45-29.32). Amapá shows the lowest value (TMP=7.58; 95% CI 6.47-8.69). When mortality rates are observed according to age groups, we noticed that the Federative Units of the Southeast and South regions present values greater than 2, in the age group of 39 years and younger. The North region in this age group does not reach 2. In particular, Rio de Janeiro and the Federal District are the Units that showed the highest mortality rates in this age group. In the 40 to 59 age group, there are no great differences in the values of the rates between the Federative Units (FU), however, mainly the States of Rio de Janeiro and Sergipe showed high results in them compared to the others. In the age group of 60 to 79 years, the Southeast, South and Midwest regions show values above 70, while the North and Northeast are below this value. Specifically, the Federative Units of Rio de Janeiro, again, and the Federal District had the highest rates in this age group. And in those aged 80 years and over, the Southeast, South and Midwest regions have values above 150 and the other regions below that. The Federative Units Roraima and Federal District are the ones that obtained the best results within this range.
Table 1.
Standardized Mortality Rate and Specific Mammography Rate per 100,000 Women in Brazil by Federation Unit from 2015 to 2021
| Region | UF | Standardized Mortality Rate*† | Specific Mammography Rate ‡ | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤ 39 years (CI 95%) |
40-59 years (CI 95%) |
60-79 years (CI 95%) |
≥ 80 years (CI 95%) |
Total (CI 95%) |
≤ 39 years (CI 95%) |
40-59 years (CI 95%) |
60-79 years (CI 95%) |
≥ 80 years (CI 95%) |
Total (CI 95%) |
|||||||||||||
| North | Acre | 1.2 (0.72-1.68) |
29.53 (24.18-34.88) |
53.33 (40.75-65.92) |
95.13 (51.18-139.08) |
8.98 (7.81-10.14) |
64.78 (61.25-68.32) |
8823.34 (8730.85-8915.84) |
6134.15 (5999.19-6269.12) |
628.93 (515.93-741.93) |
1744.01 (1727.77-1760.25) |
|||||||||||
| Amapá | 1.52 (0.96-2.07) |
26.42 (21.05-31.79) |
43.88 (30.61-57.15) |
122.23 (62.34-182.12) |
7.58 (6.47-8.69) |
12.96 (11.35-14.58) |
2612.64 (2559.24-2666.04) |
1651.61 (1570.19-1733.02) |
3300.23 (2989.02-3611.44) |
482.62 (473.78-491.46) |
||||||||||||
| Amazonas | 1.54 (1.29-1.78) |
30.77 (28.32-33.21) |
69.77 (63.09-76.45) |
136.83 (111.49-162.18) |
10.34 (9.78-10.91) |
27.14 (26.11-28.17) |
2962.99 (2938.99-2986.99) |
3247.3 (3201.72-3292.88) |
569.33 (517.63-621.02) |
650.97 (646.49-655.45) |
||||||||||||
| Para | 1.25 (1.09-1.40) |
25.39 (23.91-26.87) |
55.17 (51.47-58.88) |
140.17 (124.33-155.76) |
9.68 (9.30-10.05) |
61.34 (60.25-62.42) |
4317.21 (4297.94-4336.49) |
4421.78 (4388.60-4454.97) |
709.4 (674.02-744.77) |
1046.97 (1043.05-1050.88) |
||||||||||||
| Rondônia | 1.52 (1.15-1.89) |
25.23 (22.30-28.16) |
59.22 (50.82-67.62) |
174.41 (128.73-220.09) |
10.46 (9.62-11.30) |
27.69 (26.10-29.28) |
3531.67 (3496.36-3565.79%) |
3012.55 (2952.64-3072.45) |
267.84 (211.23-324.45) |
891.66 (883.90-899.42) |
||||||||||||
| Roraima | 1.44 (0.78-2.11) |
34.13 (26.92-41.35) |
76.55 (54.67-98.44) |
236.01 | 10.79 | 85 | 10130.03 | 11204.13 | 2165.76 | 2146.11 | ||||||||||||
| (123.82-348.21) | (9.16-12.42) | (79.88-90.12) | (10005.75-10254.31) | (10939.36-11468.90) | (1825.90-2505.63) | (2123.17-2169.05) | ||||||||||||||||
| Tocantins | 1.52 (1.12-1.92) |
28.3 (24.78-31.82) |
54.64 (46.52-62.75) |
132.73 (98.86-166.60) |
11.02 (10.09-11.95) |
78.85 (75.96-81.75) |
5706.91 (5656.90-5756.93) |
5033.72 (4955.80-5111.65) |
762.65 (681.47-843.84) |
1423.61 (1413.00-1434.21) |
||||||||||||
| North East | Alagoas | 1.41 (1.16-1.67) |
31.61 (29.25-33.96) |
61.2 (56.01-66.40) |
144.18 (124.14-164.21) |
13.36 (12.70-14.03) |
276.54 (272.98-280.11) |
13743.61 (13694.50-13792.72) |
12433.88 (12359.89-12507.87) |
1556.23 (1490.42-1622.04) |
3763.59 (3752.40-3774.78) |
|||||||||||
| Ceará | 2 (1.81-2.19) |
33.97 (32.51-35.43) |
63.45 (60.45-66.45) |
179.71 (168.11-191.31) |
16.84 (16.38-17.30) |
56.28 (55.27-57.29) |
5891.72 (5872.48-5910.95) |
5020.21 (4993.50-5046.92) |
539.9 (519.79-560.01) |
1674.02 (1669.43-1678.61) |
||||||||||||
| Bahía | 1.62 (1.49-1.74) |
30.56 (29.49-31.64) |
70.39 (67.68-73.09) |
212.16 (200.01-224.30) |
14.86 (14.53-15.19) |
83.67 (82.73-84.60) |
8883.71 (8865.39-8902.04) |
10070.34 (10038.01-10102.68) |
1135.12 (1107.03-1163.20) |
2552.59 (2548.22-2556.96) |
||||||||||||
| Maranhão | 1.08 (0.92-1.23) |
22.76 (21.26-24.26) |
41.79 (38.33-44.66) |
74.49 (63.98-84.04) |
8.37 (8.00-8.74) |
55 (54.50-56.71) |
5849.67 (5825.67-5873.67) |
4881.99 (4847.68-4916.30) |
739.75 (708.02-771.47) |
1366.96 (1362.21-1371.71) |
||||||||||||
| Paraíba | 1.53 (1.28-1.78) |
29.25 (27.25-31.25) |
62.78 (58.57-66.98) |
147.49 (132.62-162.36) |
16.02 (15.35-16.69) |
97.55 (95.54-99.55) |
10700.57 (10662.40-10738.75) |
8262.57 (8214.30-8310.85) |
987.58 (949.10-1026.05) |
3101.41 (3092.09-3110.72) |
||||||||||||
| Pernambuco | 1.82 (1.65-2.00) |
35.01 (33.61-36.42) |
81.24 (78.01-84.48) |
204.44 (191.96-216.93) |
19.29 (18.82-19.77) |
108.03 (106.66-109.41) |
12010.09 (11984.06-12036.11) |
12345.35 (12305.48-12385.22) |
1394.59 (1361.98-1427.20) |
3763.41 (3756.73-3770.10) |
||||||||||||
| Piauí | 1.76 (1.46-2.05) |
29.6 (27.34-31.87) |
57.88 (53.05-62.71) |
119.95 (102.52-137.38) |
13.66 (12.97-14.34) |
15.82 (14.94-16.69) |
3143.99 (3120.64-3167.33) |
2608.33 (2575.88-2640.77) |
243.19 (218.38-268.01) |
859.76 (854.32-865.19) |
||||||||||||
| Sergipe | 2.14 (1.75-2.53) |
36.42 (33.36-39.48) |
72.87 (65.89-79.84) |
194.28 (166.51-222.05) |
16.74 (15.82-17.66) |
141.85 (138.67-145.03) |
12987.73 (12929.93-13045.52) |
10293.3 (10210.37-10376.22) |
1335.15 (1262.35-1407.96) |
3471.14 (3457.85-3484.43) |
||||||||||||
| Rio Grande do Norte | 1.7 (1.41-1.99) |
31.81 (29.56-34.05) |
76.05 (70.77-81.33) |
165.17 (148.04-182.31) |
17.79 (17.02-18.56) |
133.9 (131.35-136.46) |
10284.93 (10244.54-10325.33) |
8310.48 (8255.32-8365.64) |
986.86 (944.98-1028.75) |
3014.24 (3004.23-3024.24) |
||||||||||||
| Southeast | Espirito Santo | 2.12 (1.81-2.42) |
31.42 (29.42-33.41) |
78.55 (73.45-83.66) |
162.2 (144.88-179.51) |
18.32 (17.63-19.10) |
216.36 (213.24-219.47) |
13057.01 (13016.33-13097.70) |
15573.48 (15501.53-15645.42) |
1742.76 (1685.99-1799.52) |
4616.95 (4605.24-4628.65) |
|||||||||||
| Minas Gerais | 1.92 (1.79-2.04) |
27.5 (26.71-28.29) |
71.12 (69.17-73.06) |
155.44 (148.79-162.08) |
17.98 (17.67-18.30) |
146.39 (145.28-147.51) |
9424.49 (9409.83-9439.15) |
10659.5 (10635.69-10683.31) |
946.31 (929.91-962.71) |
3440.9 (3436.58-3445.22) |
||||||||||||
| Region | UF | Standardized Mortality Rate*† | Specific Mammography Rate ‡ | |||||||||||||||||||
| ≤ 39 years (CI 95%) |
40-59 years (CI 95%) |
60-79 years (CI 95%) |
≥ 80 years (CI 95%) |
Total (CI 95%) |
≤ 39 years (CI 95%) |
40-59 years (CI 95%) |
60-79 years (CI 95%) |
≥ 80 years (CI 95%) |
Total (CI 95%) |
|||||||||||||
| Southeast | Rio de Janeiro | 2.87 (2.70-3.05) |
38.92 (37.92-39.92) |
102.76 (100.37-105.16) |
203.8 (196.30-211.31) |
28.88 (28.45-29.32) |
50.62 (49.87-51.37) |
2140.79 (2133.39-2148.20) |
2370.77 (2359.28-2382.27) |
325.98 (316.49-335.47) |
873.75 (871.34-876.15) |
|||||||||||
| São Paulo | 2.28 (2.18-2.37) |
32.17 (31.59-32.74) |
90.82 (89.32-92.31) |
221.61 (216.16-227.06) |
22.99 (22.75-23.24) |
100.78 (100.14-101.42) |
4941.96 (4934.84-4949.08) |
5203.33 (5192.00-5214.66) |
789.43 (779.14-799.72) |
1841.27 (1839.11-1843.44) |
||||||||||||
| South | Paraná | 2.09 (1.91-2.27) |
29.85 (28.74-30.96) |
82.17 (79.27-85.07) |
203 (191.33-214.67) |
19.85 (19.40-20.29) |
430.83 (428.22-433.44) |
14753.81 (14729.10-14778.51) |
16391.13 (16350.16-16432.11) |
2440.2 (2399.74-2480.67) |
5548,81 (5541.31-5556.31) |
|||||||||||
| Santa Catarina | 2.2 (1.96-2.44) |
34.93 (33.37-36.49) |
95.81 (91.65-99.97) |
211.13 (195.88-226.38) |
22.6 (21.97-23.22) |
260.99 (258.33-263.65) |
13206.74 (13176.42-13237.07) |
14530.44 (14479.18-14581.71) |
1481.07 (1440.67-1521.47) |
4868.41 (4859.22-4877.59) |
||||||||||||
| Rio Grande do Sul | 2.16 (1.97-2.34) |
30.1 (29.04-31.16) |
92.37 (89.67-95.08) |
225.77 (216.17-235.37) |
25.97 (25.47-26.47) |
216.38 (214.49-218.27) |
7752.16 (7735.13-7769.20) |
7960.85 (7935.73-7985.96) |
915.5 (896.17-934.84) |
3160.67 (3155.11-3166.23) |
||||||||||||
| Midwest | DF | 2.46 (2.09-2.84) |
32.72 (30.29-35.15) |
100.22 (92.75-107.70) |
283.75 (249.77-317.72) |
19.08 (18.21-19.96) |
28.55 (27.27-29.84) |
1673.1 (1655.74-1690.46) |
2288.45 (2252.72-2324.19) |
304.92 (269.70-340.14) |
562.55 (557.79-567.31) |
|||||||||||
| Goiás | 2.18 (1.94-2.41) |
31.32 (29.77-32.87) |
86.19 (81.81-90.57) |
185.93 (168.32-203.55) |
17.69 (17.13-18.26) |
147.52 (145.56-149.49) |
7690.08 (7665.84-7714.32) |
7550.62 (7509.61-7591.64) |
1270.27 (1224.22-1316.31) |
2515.57 (2508.86-2522.27) |
||||||||||||
| Mato Grosso | 1.97 (1.65-2.29) |
29.27 (27.01-31.53) |
75.74 (69.23-82.26) |
176 (146.95-205.05) |
13.97 (13.25-14.69) |
111.09 (108.69-113.49) |
6772.28 (6737.90-6806.67) |
7286.25 (7222.23-7350.16) |
1268.18 (1190.20-1346.16) |
2005.61 (1996.99-2014.22) |
||||||||||||
| Mato Grosso do Sul | 1.7 (1.36-2.03) |
31.83 (29.32-34.34) |
87.14 (80.30-93.98) |
208.41 (180.93-235.88) |
18.06 (17.17-18.96) |
139.56 (136.55-142.58) |
10525.33 (10479.73-10570.92) |
9946.88 (9873.77-10019.98) |
1331.54 (1262.08-1400.99) |
3298.59 (3286.49-3310.69) |
||||||||||||
| Total | 1.98 (1.94-2.02) |
31.55 (31.27-31.83) |
81.78 (81.09-82.48) |
194.04 (191.52-196.66) |
19.25 (19.15-19.35) |
126.23 (125.91-126.56) |
7462.54 (7457.26-7465.83) |
8128.03 (8120.24-8135.81) |
943.25 (937.59-948.91) |
2506.55 (2505.37-2507.73) |
||||||||||||
† Crude and standardized death rate and CI confidence interval. ‡ Crude and specific mammography rates and CI confidence interval. Details on standardized mortality rate calculations are provided in the Methods section.
Regarding the mammography rates, according to Table 1 and considering the entire national territory, the value of the specific mammography rate (TME) was 2,506.55 (95% CI 2505.37-2507.73) per 100,000 women. Furthermore, we note that the highest TME was in the State of Paraná with 5,548.81 (95% CI 5541.31-5556.31) exams and the lowest was in Amapá with 482.62 exams (95% CI 473.78-491.46) per 100,000 women. The Southeast, South and Midwest regions are the ones with the highest rates of mammograms. By Federative Unit and age group, Paraná is the State that performs the most mammograms, as well as Alagoas in the age group of 39 years and younger, as well as 40 to 59 years. In the age group of 60 to 79 years, in addition to Paraná, Espírito Santo also has high rates. And in the group 80 years and older, Amapá has shown itself to be a State that has high rates of mammograms.
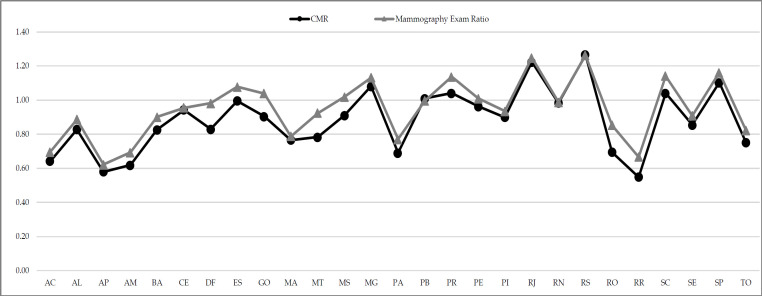
From the calculation of the comparison index of the standardized mortality ratio (CMR – Comparative Mortality Ratio), in Figure 1 we can observe it with the ratio of mammograms by Federative Unit of Brazil.
Figure 1.
Comparison of CMR and Ratio of Mammograms by Federation Unit from 2015 to 2021 (Acre-AC, Alagoas-AL, Amapá-AP, Amazonas-AM, Bahia-BA, Ceará-CE, Distrito Federal-DF, Goiás-GO, Maranhão-MA, Mato Grosso-MT, Mato Grosso do Sul-MS, Pará-PA, Pernambuco-PE, Piauí-PI, Rio Grande do Norte-RN, Rondônia-RO, Roraima-RR, Sergipe-SE, Tocantins-TO, Espírito Santo-ES, Minas Gerais-MG, Paraíba-PB, Paraná-PR, Rio de Janeiro-RJ, Rio Grande do Sul-RS, Santa Catarina-SC e São Paulo-SP)
We found, according to Figure 1, that most of the Federative Units, that is, 19 of them (Acre, Alagoas, Amapá, Amazonas, Bahia, Ceará, Federal District, Goiás, Maranhão, Mato Grosso, Mato Grosso do Sul, Pará, Pernambuco, Piauí, Rio Grande do Norte, Rondônia, Roraima, Sergipe and Tocantins) present ratios lower than 1, which means that the observed mortality was lower than expected. In contrast, the other Federative Units obtained values equal to or greater than 1 (Espírito Santo, Minas Gerais, Paraíba, Paraná, Rio de Janeiro, Rio Grande do Sul, Santa Catarina and São Paulo). If the value is higher, it indicates that there was a greater number of observed deaths than expected. Regarding the ratio of mammograms, the Federative Units such as Espírito Santo, Goiás, Minas Gerais, Mato Grosso do Sul, Paraíba, Paraná, Pernambuco, Rio de Janeiro, Rio Grande do Sul, Santa Catarina and São Paulo showed values greater than 1, so it can be said that more mammograms were performed than expected.
Comparative Analysis
To verify possible associations between the variables, we proceeded to divide the standardized mortality rate for breast cancer into three groups composed of nine Federal Units described below (see Table 2 and Figure 2).
Table 2.
Comparison of the 3 Mortality Rate Groups with Socio-Economic-Racial Data
| Sociodemographic and economic data | Group 1 | Group 2 | Group 3 |
|---|---|---|---|
| Avarege Rate of Lower Mortality | Average Rate of Intermediate Mortality |
Average Rate of Major Mortality |
|
| Average income rate by State (in reais R$) | 1,809.06 | 1,777.61 | 2,594.86 |
| Average percentage of households receiving “Bolsa Família” (%) | 25.4 | 22.7 | 7.9 |
| Average percentage of people with income (%) | 53.7 | 60.5 | 63.5 |
| Average vacancy rate | 8.54 | 8.13 | 6.71 |
| Average rate of the GINI* index of per capita household income | 0.63 | 0.6 | 0.58 |
| Average percentage of households that received LOAS (%) | 5.1 | 4.71 | 2.83 |
| Average percentage of women > 50 years old (%) | 19.71 | 25.95 | 29.3 |
| Average illiteracy rate (women > 60 years old) | 13.58 | 15.32 | 6.59 |
| Average years of schooling (women > 60 years old) | 4.81 | 5,01 | 6.64 |
| Average percentage of white population (%) | 21.99 | 30.62 | 55.01 |
| Average mammogram rate | 1,501.83 | 2,515.03 | 2,873.20 |
Footnote: own elaboration based on SIH-SUS data. LOAS (Organic Social Assistance Law- Brasil, 1993) is a right guaranteed to all low-income elderly people over 65 years of age. As well as people with disabilities of physical, intellectual or sensorial origin, also of low income and of any age. http://www.planalto.gov.br/ccivil_03/leis/l8742.htm *Gini index is an economic measure used to calculate the income inequality that exists among citizens of a territory, usually a country.
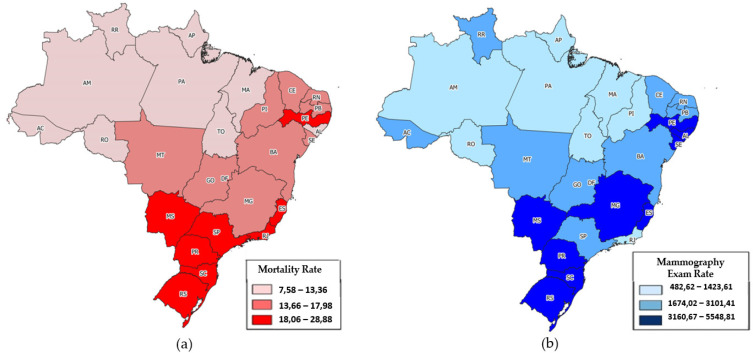
Figure 2.
Mapping of rates by Federative Unit. (a) Description of Standardized Mortality Rate by Federative Unit; (b) Description of Mammography Exam Rate by Federative Unit (Acre-AC, Alagoas-AL, Amapá-AP, Amazonas-AM, Bahia-BA, Ceará-CE, Distrito Federal-DF, Goiás-GO, Maranhão-MA, Mato Grosso-MT, Mato Grosso do Sul-MS, Pará-PA, Pernambuco-PE, Piauí-PI, Rio Grande do Norte-RN, Rondônia-RO, Roraima-RR, Sergipe-SE, Tocantins-TO, Espírito Santo-ES, Minas Gerais-MG, Paraíba-PB, Paraná-PR, Rio de Janeiro-RJ, Rio Grande do Sul-RS, Santa Catarina-SC e São Paul-SP)
• Group 1 composed of the Federative Units with the lowest mortality rates due to breast cancer (Amapá, Maranhão, Acre, Pará, Amazonas, Rondônia, Tocantins, Alagoas and Roraima).
• Group 2 composed of the Federative Units with an intermediate mortality rate (Piauí, Mato Grosso, Bahia, Paraíba, Sergipe, Ceará, Goiás, Rio Grande do Norte and Minas Gerais).
• Group 3 composed of the Federative Units with the highest mortality rate (Mato Grosso do Sul, Espírito Santo, Federal District, Pernambuco, Paraná, Santa Catarina, São Paulo, Rio Grande do Sul, Rio de Janeiro).
When we look at the sociodemographic and economic data by mortality rate group, as shown in Table 2 below, we note that group 3 (highest mortality rates from breast cancer) have higher rates in the variables: income rate by state, people with income, mean percentage of women over 50, mean years of schooling in women over 60, average percentage of white population, and average mammogram rate. On the other hand, group 1 (lower breast cancer mortality rates) shows higher rates in: families receiving Bolsa Família, unemployment rate, Gini index rate and rate of households that received LOAS. However, this group 1 had a lower rate of mammograms.
In other words, we can say that mortality from breast cancer increases with the percentage of women over 50 years of age and white, as well as with the number of years of study in this population. On the other hand, breast cancer mortality decreases: as the percentage of households receiving Bolsa Familia, or LOAS, increases; as the GINI index increases as the rate of unemployment and illiteracy is higher.
Based on the same line of reasoning for the average mortality rate groups, we performed the same procedure with the mammography test rate variable and the Federal Units. In this fashion, we also divided it into three groups composed of nine Federative Units described below:
• Group 1 composed of the Federative Units with the lowest rates of mammograms (Amapá, Federal District, Amazon, Piauí, Rio de Janeiro, Rondônia, Pará, Maranhão and Tocantins).
• Group 2 composed of the Federative Units with intermediate rates (Ceará, Acre, São Paulo, Mato Grosso, Roraima, Goiás, Bahia, Rio Grande do Norte and Paraíba).
• Group 3 composed of the Federative Units with the highest rates (Rio Grande do Sul, Mato Grosso do Sul, Minas Gerais, Sergipe, Pernambuco, Alagoas, Espírito Santo, Santa Catarina and Paraná).
According to Table 3, we observed that group 3 (higher average rate of mammograms) have higher rates in: Average income rate by State, average people with income, average percentage of women over 50 years old, average years of schooling in women over 60. On the other hand, group 1 (lower average rate of mammograms) showed a higher rate in the variables: average percentage of households receiving Bolsa Família , Average vacancy rate and Average illiteracy rate. However, this group 1 had lowest rates in Average percentage of women > 50 years old, Average years of schooling (women > 60 years old).
Table 3.
Comparison of 3 Groups of Mammogram Rates with Socioeconomic Data
| Sociodemographic and economic data | Group 1 (Lower) Average rate of Mammograms | Group 2 (Intermediate) Average rate of Mammograms |
Group 3 (Higher) Average rate of Mammograms |
|---|---|---|---|
| Average income rate by State (in reais R$) | 2,149.67 | 1,870.38 | 2,161.47 |
| Average percentage of households receiving Bolsa Família (%) | 56.7 | 38.2 | 38.6 |
| Average percentage of people with income (%) | 55.8 | 59.4 | 62.5 |
| Average vacancy rate | 51 | 40.4 | 42 |
| Average rate of the GINI* index of per capita household income | 0.52 | 0.53 | 0.5 |
| Average percentage of women > 50 years old (%) | 20.3 | 25.9 | 28.6 |
| Average illiteracy rate (women > 60 years old) | 30.5 | 27.9 | 22.6 |
| Average years of schooling (women > 60 years old) | 5.2 | 5.5 | 5.8 |
Source: Own elaboration based on SIH-SUS data. Footnote: *Gini index is an economic measure used to calculate the income inequality that exists among the citizens of a territory, usually a country.
In general, we observed that the mortality rate and sociodemographic variables have a significant direct correlation with the mammogram rate rho=.480, p=.010; and indirect significant correlation with illiteracy rho= -.579, p=.002 and Gini index rho= -.522, p=.005. With regards to the correlation with the mammogram rates, we did not obtain significant results.
Figure 2 shows the arrangement of the Federative Units according to mortality rates and mammography exam rate. In that, we noted that the Federative Units of Rio Grande do Sul, Santa Catarina, Paraná, Mato Grosso do Sul, Espírito Santo and Pernambuco have higher standardized mortality rates and a high rate of mammograms. All the North Federative Units, on the other hand, have low standardized mortality rates as well as low rates of mammograms, except for Roraima and Acre. The Federative Unit of Rio de Janeiro stands out for its high mortality rate and low rate of mammograms.
Discussion
From this study perspective, to compare the mortality rate, rate of mammograms and sociodemographic variables during the period from 2015 to 2021, once again, the results are unsettling, in which a direct and significant relationship is established between mortality rate and mammographies. The Federative Units that perform more mammograms have a higher mortality rate. This result may lead to the erroneous understanding that performing a mammogram is not beneficial. Although we can understand reality with these results, it is a complex relationship and there are several factors that interfere beyond the respective region (meaning Federative Unit). It should be noted that this study did not analyze the incidence of breast cancer. Although it is known that aging and population growth are the main drivers of the rapid increase in the burden of breast cancer, demographic transitions have also led to the increase in new cases of breast cancer in different ways both internationally and nationally. (Lei et al., 2021). In Nordic countries, the incidence of breast cancer has increased due to population growth and aging with values of 19% in Sweden, 59% in Iceland and almost 23% in China. Nevertheless, these same authors (Lei et al., 2021) claim that breast cancer was the leading cause of cancer death among women worldwide in 2020. They still claim that mortality in low-income countries such as Fiji, Jamaica, Samoa, Nigeria, Cameroon was higher than in high-income countries (eg South Korea, Australia, USA and the UK).
In Brazil during the period of 2015 to 2021 obtained a mortality rate value of 19.25/100,000 women, higher than the results that Nogueira and Kluthcovsky (2022) presented of 13.84/100,000 women in 2018 and higher than the global average of 16.30/100,000 women. Such results, showed an increase of almost 55% when compared to the indexes presented by Girianelli, Gamarra and Azevedo (2014) in the period from 1980 to 2016. In addition, the Federative Units of the South and The Southeast are the ones with the highest mortality rates, corroborating the study by these authors (Girianelli et al., 2014), with the exception of the Midwest.
The highest mortality rate in the national territory is Rio de Janeiro. Authors such as Rodrigues et al., (2019) also confirm this result, with high mortality from breast cancer in this Federal Unit. Among the age groups of the mortality rate, it was observed that as women age, the data are higher. Thus, the age group of 80 and over was the one with the highest mortality rates, followed by those aged 60 to 79 years, in all Federative Units. And Rio de Janeiro and the Federal District are the Units that present the highest results among age groups. Nogueira and Kluthcovsky (2019) report that breast cancer is related to lifestyles in industrialized countries, and the associated factors are advanced age, especially from 50 years old.
With regards to mammogram rates, the Federative Unit of Paraná showed the highest one in Brazil, which goes according to the study by Lopes et al., (2015). Even though the State of Paraná has a number of mammography devices above the recommended level, these authors also found (Lopes et al., 2015) an increase in mortality from breast cancer, possibly due to poor distribution of devices, difficulties in population access to mammograms, or late screening and diagnosis. In addition to Paraná, the Units with the lowest rate of mammograms were Amapá, Distrito Federal and Piauí.
Another piece of data that corroborates the results is the analysis of the CMR. It was observed that most of the Federative Units of the South, Southeast and Midwest regions had more observed deaths than expected. And in the ratio of mammograms, most of the Federative Units were also from the South, Southeast and Midwest regions.
It is known that risk factors for breast cancer are linked to women having fewer children, breastfeeding less time, advanced age and obesity (Duarte et al., 2020; Medeiros et al., 2020). In the groups divided by high, medium and low mortality rates and sociodemographic and economic factors, it resulted that there is higher mortality in the Federative Units with “better” socioeconomic data. In other words, Units considered as “more developed”, with higher income, less need for State assistance in people´s healthcare, greater number of people with their own income, more years of study, lower illiteracy, higher proportion of women over 50 years and more mammograms (Barbosa et al., 2016). Higher mortality in FUs with a higher proportion of white women is due to the fact that the more “developed” states have a higher proportion of white people.
Likewise, we divided the groups into low, medium and high rates of mammograms and observed that higher rates of mammograms were associated with higher rates of income by State, people with income, average percentage of women aged 50 or more and with higher education. On the other hand, the group with the lowest rates of mammograms showed a higher rate of families receiving “Bolsa Família”, a higher rate of unemployment and a higher average of illiteracy. However, this group had a lower average percentage of women under 50 years of age and a lower average number of years of schooling. One possible explanation for this result is the difficulty in accessing the test, as stated by Rodrigues et al., (2019) and Lopes et al., (2015).
Analyzing all of these data, it seems to us that the greater number of mammograms is due to a higher incidence of breast cancer and greater financial conditions among the FUs to offer the exam. The higher incidence of death from breast cancer in more developed states would not be because the mammography cannot prevent deaths, but rather because states with better economic conditions have a higher incidence of breast cancer altogether and, consequently, higher mortality in itself, despite performing more mammograms. Another possibility that arises is that of a late access to screening and staging. The Ministry of Health suggests that screening with mammography in women aged 50 to 69 years should be carried out every two years (Medeiros et al., 2020). In addition, authors such as Lei et al., (2021) claim that Brazil has a very large geographical area, and the geographic variations in breast cancer mortality indicate an impairment in access to early screening and medical treatment, which would likely benefit from early detection by mammographic screening and improvements in treatment. However, weak medical infrastructure in many underdeveloped or developing countries has led to limited access to mammography. In Brazil, the same problem likely occurs, due to a series of factors, such as longer life expectancy, poor distribution of mammograms, thus favoring certain social strata, such as women with higher income, white and higher schooling (Fayer et al., 2020). Furthermore, in Brazil, Soares et al., (2015) also confirms this information and showed that deaths from breast cancer show geographic variations according to color. Authors such as Duarte et al., (2020) also present a study in the Minas Gerais Unit, where there was internal regional contrast, with high mortality from the disease in more urbanized and populous areas, which may be mainly related to factors of the industrialized lifestyle habits.
Another possibility of the global result of this study could be explained by what Medeiros et al., (2020) points out. The time between the diagnosis and the beginning of the first oncological treatment is long, in addition to considering that mammography exams in Brazil are resulting in late diagnosis of breast cancer. Sociodemographic, clinical and treatment-associated aspects interfere with time intervals. Probably identifying it early can help to promote actions for populations vulnerable to delay. This study has some limitations, such as the use of data from secondary sources that may present flaws or errors in the accounting of mortality data, however it is still a way of obtaining valuable information.
For the future, it is suggested that more variables would be included to verify the relationship between the mortality rate and the mammography, such as the time of diagnosis, the stage of the disease, eating habits and sedentary lifestyle. There is a direct relationship between the mortality and mammogram rates in the Federative Units of Brazil during the period of 2015 to 2021. Brazil has a high mortality rate from breast cancer when compared to other countries. The reasons are diverse, such as the modern, industrialized and populous lifestyle. The Federative Units with the highest mortality rate also have high rates of mammograms, that is, in the Federative Units with “better” sociodemographic conditions, the South and Southeast. There is still debate about the reason for the delay in performing mammographies.
Author Contribution Statement
Conceptualization, LS, IR and SMP; methodology, LS, IR, SMP, MDC and RP software, LS, IR, SMP, MDC and RP.; validation, LS,IR, SMP, MDC and RP; formal analysis, LS, IR, SMP, MDC, RP, CP and RRO; investigation, LS, IR, SMP, MDC, RP, CP and RRO; resources, IR, LS, SMP, MDC, RP, CP and RRO; data curation, LS, IR, SMP, MDC, RP, CP and RRO; writing—original draft preparation, LS, IR, SMP, MDC, RP, CP and RRO; writing-review and editing, LS, IR, SMP, MDC, RP, CP and RRO; supervision, SMP, MDC and RP; project administration, LS, IR, SMP, MDC and RP. All authors have read and agreed to the published version of the manuscript.
Acknowledgements
We thank CNPq and Capes for their support in the development and execution of this work.
Ethical Declaration
The analyzed data come from secondary sources of public access, and without the possibility of individual identification of the information. Thus, in accordance with the recommendations in the National Health Council (CNS) resolution nº 466, of December 12, 2012, the ethical principles of research were respected, and this study was submitted to the Ethics Committee in Research involving human beings of our Institution, with CAAE (Certificate of Presentation for Ethical Appraisal) 51654021.4.0000.5220 and approved opinion number 4.997.733/2021.
Conflict of Interest
The authors declare no conflict of interest.
References
- Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–75. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anastasiadi Z, Lianos GD, Ignatiadou E, Harissis HV, Mitsis M. Breast cancer in young women: an overview. Updates Surg. 2017;69:313–7. doi: 10.1007/s13304-017-0424-1. [DOI] [PubMed] [Google Scholar]
- Barbosa IR, Costa ICC, Bernal MM, Souza DLB. As iniquidades sociais e as disparidades na mortalidade por câncer relativo ao gênero. Rev Ciência Plural. 2015;1:79–86. [Google Scholar]
- Barbosa IR, Costa ICC, Bernal MM, Souza DLB. Desigualdades socioeconômicas e mortalidade por câncer: um estudo ecológico no Brasil. Rev Bras promoç Saúde. 2016;29:350–6. [Google Scholar]
- Cavalcante JAG, Batista LM, Assis TS. Câncer de mama: perfil epidemiológico e clínico em um hospital de referência na paraíba. SANARE. 2021;20:17–24. [Google Scholar]
- Corrêa CSL. Rastreamento do câncer de mama em Minas Gerais: avaliação a partir de dados dos sistemas de informações do Sistema Único de Saúde. Epidemiol Serv Saúde. 2017;26:481–92. doi: 10.5123/S1679-49742017000300006. [DOI] [PubMed] [Google Scholar]
- Duarte DAP, Nogueira MC, Magalhães MC, Bustamante-Teixeira MT. Iniquidade social e câncer de mama feminino: análise da mortalidade. Cad Saúde Colet. 2020;28:465–76. [Google Scholar]
- Fayer VA, Guerra MR, Nogueira MC, et al. Controle do câncer de mama no estado de São Paulo: uma avaliação do rastreamento mamográfico. Cad Saúde Colet. 2020;28:140–52. [Google Scholar]
- Ferreira MDC, Vale DB, Barros MBDA. Incidence and mortality from breast and cervical cancer in a Brazilian town. Rev Saude Publica. 2021;18:55–67. doi: 10.11606/s1518-8787.2021055003085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girianelli VR, Gamarra CJ, Azevedo GS. Disparities in cervical and breast cancer mortality in Brazil. Rev Saude Publica. 2014;48:459–67. doi: 10.1590/S0034-8910.2014048005214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harbeck B, Gnant M. Breast cancer. Lancet. 2017;389:1134–50. doi: 10.1016/S0140-6736(16)31891-8. [DOI] [PubMed] [Google Scholar]
- Kim G, Phillips J, Cole E, et al. Comparison of Contrast-Enhanced Mammography With Conventional Digital Mammography in Breast Cancer Screening: A Pilot Study. J Am Coll Radiol. 2019;16:1456–63. doi: 10.1016/j.jacr.2019.04.007. [DOI] [PubMed] [Google Scholar]
- Kolak A, Kamińska M, Sygit K, et al. Primary and secondary prevention of breast cancer. Ann Agric Environ Med. 2017;24:549–53. doi: 10.26444/aaem/75943. [DOI] [PubMed] [Google Scholar]
- Lei S, Zheng R, Zhang S, et al. Global patterns of breast cancer incidence and mortality: A population-based cancer registry data analysis from 2000 to 2020. Cancer Commun. 2021;4:1183–94. doi: 10.1002/cac2.12207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Løberg M, Lousdal ML, Bretthauer M, Kalager M. Benefits and harms of mammography screening. Breast Cancer Res. 2015;17:63–75. doi: 10.1186/s13058-015-0525-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes TCR, Gravena AAF, Dell Agnolo CM, et al. Prevalência E Fatores Associados à realização De Mamografia E Exame citopatológico. Rev Bras promoç Saúde. 2015;28:402–10. [Google Scholar]
- Luo C, Li N, Lu B, et al. Global and regional trends in incidence and mortality of female breast cancer and associated factors at national level in 2000 to 2019. Chin Med J. 2022;135:42–51. doi: 10.1097/CM9.0000000000001814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros GM, Gomes CTC, Alves NFE, et al. Fatores Associados ao Atraso entre o Diagnóstico e o Início do Tratamento de Câncer de Mama: um Estudo de Coorte com 204 130 Casos no Brasil. Rev Bras Cancerol. 2020;66:e–09979. [Google Scholar]
- Miller AB, Wall C, Baines CJ, et al. Twenty five years follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ. 2014;2014:348–66. doi: 10.1136/bmj.g366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moura LVM, Sousa SS, Ferreira DMD, et al. Avaliação da Cobertura do Exame Mamográfico de Rastreio do SUS e Mortalidade por Câncer de Mama no Nordeste Brasileiro. Braz J Hea Rev. 2020;3:9533–46. [Google Scholar]
- Nogueira LR, Kluthcovsky ACGC. Analysis of breast cancer mortality in Brazil and its regions, 2005 to 2019. RSD. 2022;9:e23211931628. [Google Scholar]
- PAHO. Pan American Health Organization. 2020. https://www.paho.org/en/topics/cancer .
- Peres VC, Veloso DL, Xavier RM, Salge AK, Guimarães JV. Câncer De Mama Em Mulheres: Recidiva E Sobrevida Em Cinco Anos. Enferm. 2015;24:740–7. [Google Scholar]
- Rodrigues DCN, Freitas-Junior R, Rahal RMS, et al. Difficult Access and Poor Productivity: Mammography Screening in Brazil. Asian Pac J Cancer Prev. 2019;20:1857–64. doi: 10.31557/APJCP.2019.20.6.1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soares LR, Gonzaga CM, Branquinho LW, et al. Mortalidade por câncer de mama feminino no Brasil de acordo com a cor. Rev Bras Ginecol Obstet. 2015;37:388–92. doi: 10.1590/SO100-720320150005319. [DOI] [PubMed] [Google Scholar]