Abstract
Introduction
Renal autotransplantation is considered a surgical procedure for extensive ureteral defects. Herein, we report a case of severe ureteral injury repaired by laparoscopic nephrectomy and renal autotransplantation with an iliac vein patch using bovine pericardium.
Case presentation
A 56‐year‐old woman who had previously undergone gynecological surgery complained of right‐sided abdominal pain. She was then later diagnosed with a right middle ureteral injury with a 5‐cm long defect. We performed retroperitoneal laparoscopic nephrectomy and renal autotransplantation. As the iliac vein was fragile, venous patching using bovine pericardium was performed. The patient's renal function was well preserved after surgery.
Conclusion
Laparoscopic nephrectomy and renal autotransplantation is an effective method for repairing severe ureteral injury with the preservation of renal function. A venous patch using bovine pericardium might be considered as a replacement for a fragile vein.
Keywords: laparoscopic nephrectomy, renal autotransplantation, venous patch
Abbreviations & Acronyms
- BP
bovine pericardium
- IVC
inferior vena cava
Keynote message.
Renal autotransplantation is an effective procedure for repairing severe ureteral defects with the preservation of renal function. A venous patch using bovine pericardium can be a useful reconstruction for fragile vein.
Introduction
Iatrogenic ureteral injury is one of the complications of abdominal and pelvic surgeries, and it is the most commonly reported complication in gynecological surgery. 1 Renal autotransplantation for ureteral injury may be the last but most useful resort for preserving renal function in selected cases. BP is used ubiquitously in vascular surgery. 2 Herein, we report a case of severe ureteral injury that was repaired with renal autotransplantation with a venous patch using BP.
Case presentation
A 56‐year‐old woman underwent open bilateral adnexectomy for a 20‐cm right ovary benign tumor. At 6 days after her surgery, she had right‐sided abdominal pain. Contrast‐enhanced computed tomography showed slight hydronephrosis and contrast‐medium accumulation in the right pelvis (Fig. 1a,b). Retrograde pyelography showed the contrast media leaking out of the right lower ureter (Fig. 2a). Given that a ureteral injury was suspected, percutaneous nephrostomy was performed. Antegrade pyelography showed a right ureteral interruption (Fig. 2b). The length of the ureteral defect was estimated to be 5 cm. She was referred to our hospital to undergo ureter repair surgery at 4 months after ovarian surgery. Her medical history included an open abdominal surgery for a uterine myoma. Blood examination revealed a low estimated glomerular filtration rate (eGFR: 47.2 mL/min/1.73 m2). We planned to perform renal autotransplantation because the injury site was in the middle ureter and the damaged area was long.
Fig. 1.
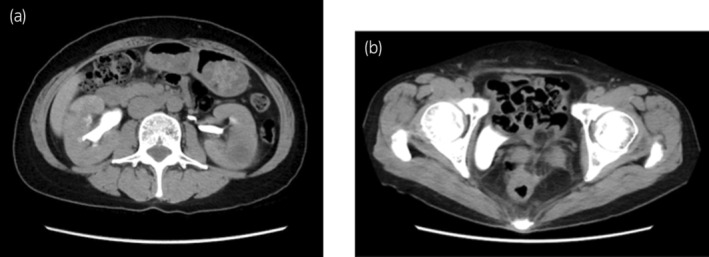
(a) Abdominal contrast CT shows slight hydronephrosis in the right kidney. (b) Contrast accumulation is observed on the right side of the pelvic cavity.
Fig. 2.
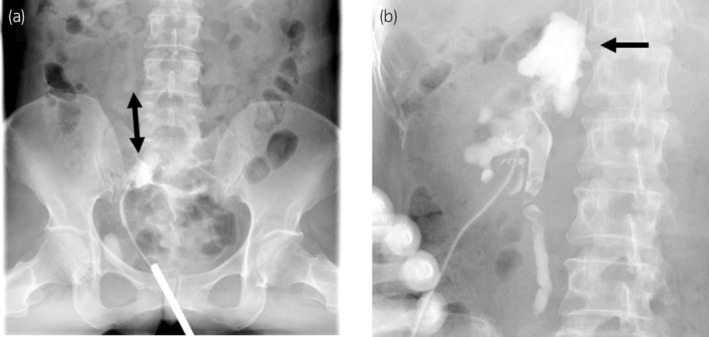
(a) Retrograde pyelography shows disconnection of the right ureter. The length of ureteral injury was expected to be 5 cm (arrows at both ends). (b) Antegrade pyelography shows dilation of the right pelvis and disconnection of the right ureter. Contrast leakage is observed due to injury of the renal pelvis during nephrostomy (single arrow).
First, we inserted the catheter in the right ureter by cystoscopy. To avoid intra‐abdominal adhesion, we dissected the retroperitoneal cavity through a Gibson incision. The iliac vessels were carefully dissected because of severe adhesions due to gynecological surgery and urinary leakage. The ureter's upper and lower ends were identified (Fig. 3). We considered the possibility of ureteroureteral anastomosis, but decided against it because of concerns about the risk of ureteral stricture after anastomosis. After changing to a lateral position, retroperitoneal laparoscopic nephrectomy was performed. Owing to the presence of severe adhesions around the kidney, a GelPort was placed on the Gibson incision and combined with a hand‐assisted approach. After the removal of the right kidney, it was promptly reflux‐cooled with a eurocholine solution. After trimming the vessels on ice slush, autotransplantation was performed. The internal iliac and renal arteries were anastomosed end‐to‐end. As the wall of the external iliac vein was very fragile, a venous patch using BP was performed by a vascular surgeon. A 4 × 2.5 cm pericardial patch was interposed to the external iliac vein and fixed at 4 points using 4‐0 Proline® with continuous sutures. Thereafter, we sutured the external iliac and renal veins on side‐to‐end anastomosis by 4‐0 Proline at the cephalad side of patch closure (Fig. 4a–d). We have chosen neoanastomosis of the urinary bladder due to the strong contusion of the remaining lower ureter. The total ischemic time was 5 h and 39 min. The amount of bleeding during the surgery was 1143 mL. The postoperative course was uneventful, and she was discharged at 10 days postoperatively. At 22 months after surgery, the renal function is well maintained (serum creatinine level, 0.72 mg/dL; eGFR, 64.4 mL/min per 1.73 m2).
Fig. 3.
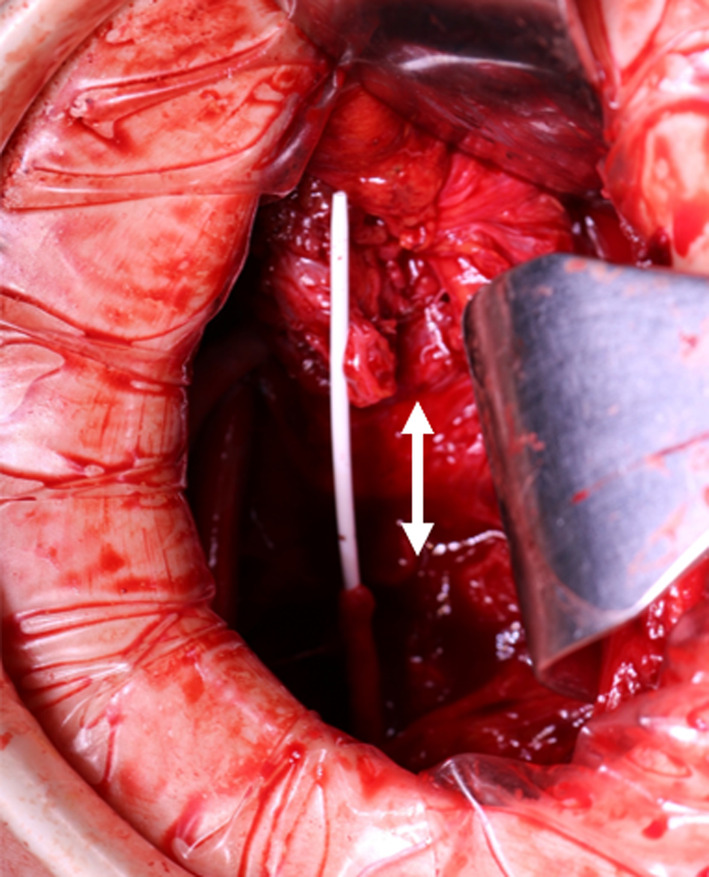
Intraoperative photograph. The upper side is cephalad. The distance between the lower ureter where the ureteral stent was placed and the upper ureter was approximately 5 cm (arrows at both ends).
Fig. 4.
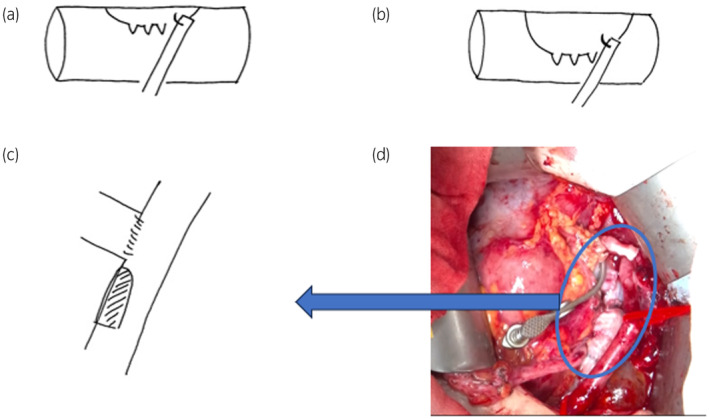
(a) When the needle was inserted into a blood vessel for vascular suture, it broke off due to fragile. (b) We trimmed the punctured area and sutured it again, but the hole expanded outside. (c) The external iliac vein was sutured with a pericardial patch. (d) The external iliac and renal veins were sutured with side‐to‐end anastomosis at the cephalic side of the patch closure. We patch closure of the iliac vein and suturing of the iliac and renal veins. The picture (c) is a simplified view in the blue circle.
Discussion
The repair of the urinary tract with renal preservation after a urinary injury is desired because ureteral injury occurs with preserved renal function. Conventional urinary tract repair methods for ureteral injury include ureteroureteral anastomosis, psoas hitch, and Boari flap. Renal autotransplantation is considered a last resort for the surgical treatment of extensive ureteral defects. 3 Hardy et al. utilized renal autotransplantation for the first time for a case of severe ureteral injury, and, now, it has become a valuable procedure for complex renal artery aneurysm and tumor. 4 An alternative to renal autotransplantation with extensive ureteral defect is ileal ureter substitutions. However, it could lead to complications, including hyperchloremic metabolic acidosis, anastomotic stenosis, and fistula formation.
In our case, renal autotransplantation was selected because the patient had several abdominal surgeries and extensive middle ureteral defects. Eisenberg et al. reported laparoscopic nephrectomy and autotransplantation for complex ureteral strictures in 15 patients. 5 The stricture length varied between 1 and 7 cm. No recurrence of stricture formation was noted (median follow‐up, 29 months). Hau et al. reported that autotransplantation is a safe and effective technique and should be taken into consideration for ureteral disease when alternative strategies are unsuitable. 6 The indications of autotransplantation included proximal ureteral injury secondary to ureteroscopic stone manipulation, ureteral injury secondary to laparoscopic retroperitoneal lymphadenectomy, or injury to the ureter after aortobifemoral bypass. Additionally, the creatinine levels improved at the 24‐month follow‐up, as in our case.
BP is used ubiquitously in vascular surgery, typically as a patch for arterial angioplasty, with excellent long‐term results. 7 In the urological field, there are several reports on the use of BP for venous reconstruction after resection of malignant tumor. 8 Particularly, the use of BP for inferior vena cava (IVC) reconstruction after IVC thrombectomy in renal cell carcinomas has been reported. 2 Our case is considered as the first to undergo renal autotransplantation with an external iliac vein patch using BP. BP has proven to be a suitable graft material in infected areas, and it can be used effectively for arterial reconstruction after removing infected grafts in vascular surgery. 9 , 10 Moreover, BP is biocompatible, derived from a biologic material fixed in glutaraldehyde, allowing for easy handling and resulting in low antigenicity. Routine anticoagulation is also not required after BP use. In our case, there were many adhesions around the iliac vessels due to a previous gynecological surgery, and the vascular wall of the external iliac vein was also fragile due to an infection. The long‐term result of using venous patches is uncertain and requires continued observation.
Conclusion
Renal autotransplantation is effective for repairing severe ureteral defects. A venous patch using BP might be used to replace the fragile vein.
Author contributions
Mizuki Hisano: Conceptualization; writing – original draft; writing – review and editing. Tomohiko Matsuura: Conceptualization; investigation. Junichi Koizumi: Conceptualization. Akito Ito: Conceptualization. Renpei Kato: Conceptualization. Shigekatsu Maekawa: Conceptualization. Mitsugu Kanehira: Conceptualization. Jun Sugimura: Conceptualization. Hajime Kin: Conceptualization. Wataru Obara: Supervision.
Conflict of interest
The authors declare no conflict of interest.
Informed consent
Not required by our institution.
Registry and the Registration No. of the study/trial
Not applicable.
Approval of the research protocol by an Institutional Review Board
Not required by our institution.
Acknowledgment
The authors would like to thank Enago (www.enago.jp) for the English language review.
References
- 1. Bašić D, Ignjatović I, Potić M. Iatrogenic ureteral trauma: a 16‐year single tertiary centre experience. Srp. Arh. Celok. Lek. 2015; 143: 162–168. [PubMed] [Google Scholar]
- 2. Smaldone MC, Cannon GM Jr, Hrebink RL. Resection of recurrent inferior vena cava tumor after radical nephrectomy for renal cell carcinoma. Urology 2006; 67: 1084.e5–1084.e7. [DOI] [PubMed] [Google Scholar]
- 3. Bodie B, Novick AC, Rose M, Straffon RA. Long‐term results with renal autotransplantation for ureteral replacement. J. Urol. 1986; 136: 1187–1189. [DOI] [PubMed] [Google Scholar]
- 4. Hardy JD. High ureteral injuries. Management by autotransplantation of the kidney. JAMA 1963; 184: 97–101. [DOI] [PubMed] [Google Scholar]
- 5. Eisenberg ML, Lee KL, Zumrutbas AE, Meng MV, Freise CE, Stoller ML. Long‐term outcomes and late complications of laparoscopic nephrectomy with renal autotransplantation. J. Urol. 2008; 179: 240–243. [DOI] [PubMed] [Google Scholar]
- 6. Hau HM, Bartels M, Tautenhahn HM et al. Renal autotransplantation a possibility in the treatment of complex renal vascular diseases and ureteric injuries. Ann. Transplant. 2012; 17: 21–27. [DOI] [PubMed] [Google Scholar]
- 7. Papakostas JC, Avgos S, Arnaoutoglou E et al. Use of the vascu‐guard bovine pericardium patch for arteriotomy closure in carotid endarterectomy. Early and long‐term results. Ann. Vasc. Surg. 2014; 28: 1213–1218. [DOI] [PubMed] [Google Scholar]
- 8. Coleman S, Kerr H, Krishnamurthi V et al. The use of bovine pericardium for complex urologic venous reconstruction. Urology 2014; 83: 495–497. [DOI] [PubMed] [Google Scholar]
- 9. D'Ambra L, Berti S, Feleppa C, Magistrelli P, Bonfante P, Falco E. Use of bovine pericardium graft for abdominal wall reconstruction in contaminated fields. World J. Gastrointest. Surg. 2012; 4: 171–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McMillan WD, Leville CD, Hile CN. Bovine pericardial patch repair in infected fields. J. Vasc. Surg. 2012; 55: 1712–1715. [DOI] [PubMed] [Google Scholar]


