Abstract
Background
Pseudoaneurysm formation sometimes complicates transplant nephrectomy. We report a case of bleeding from a pseudoaneurysm after transplantation nephrectomy that resulted in shock and emergency endovascular treatment.
Case presentation
A 56‐year‐old man underwent transplant nephrectomy 3 years and 9 months following transplantation for pyelonephritis‐related infection control. On postoperative day 7, he developed sudden pain in the lower abdomen and subsequently went into shock. A pseudoaneurysm at the anastomosis was detected, and urgent endovascular treatment was performed to stem the bleeding.
Conclusion
Vascular complications, including pseudoaneurysms, following transplant nephrectomy can be life‐threatening, and comprehensive awareness is needed in careful postoperative management.
Keywords: kidney transplant nephrectomy, pseudoaneurysm, transplant kidney infection, vascular complication, vascular reconstruction
Keynote message.
Kidney transplant nephrectomy with infection is associated with the risk of vascular complications and massive bleeding. Therefore, consideration of the vascular reconstruction method and being attentive to the risk of postoperative bleeding is important.
Abbreviations & Acronyms
- ADPKD
autosomal dominant polycystic kidney disease
- CRP
C‐reactive protein
- CT
computed tomography
- EIA
external iliac artery
- GSR
graft survival rate
- KT
kidney transplantation
- MRSA
methicillin‐resistant Staphylococcus aureus
- NA
not available
- TK
transplant kidney
- TN
transplant nephrectomy
- VC
vascular complication
Introduction
TN is commonly performed in patients with dysfunctional TKs with infection, pain, bleeding, graft malignancy, or anemia associated with inflammation. TN is sometimes complicated with life‐threatening pseudoaneurysms. Risk factors for VCs in TN have been reported to include infection, time to dialysis resumption, and chronic rejection. 1 , 2 , 3 Here, we describe a patient who had a good immediate post‐TN course but who developed bleeding from a pseudoaneurysm when abdominal pressure was applied, resulting in shock and emergency endovascular treatment.
Case presentation
A 52‐year‐old man who had undergone regular hemodialysis for 12 months for kidney failure secondary to ADPKD underwent ABO blood type‐incompatible living KT. The donor's three renal arteries were reconstructed to form two arteries, which were anastomosed with the recipient's EIA (Fig. 1a). Post‐KT, renal function did not improve, and a TK biopsy indicated acute tubular necrosis. Additional immunosuppressive drugs were administered, with minimal improvement. One month later, a nephrostomy tube was placed at the TK for stenosis at the uretero‐bladder anastomosis. At 10 months post‐KT, he developed recurrent pyelonephritis and was treated with antibiotics, but carbapenem‐resistant bacteria appeared among the causative organisms, and infection control was challenging. His kidney function continued to gradually deteriorate, and he was reintroduced to dialysis 17 months after KT. TN was performed 3 years and 9 months after KT because the patient requested re‐transplantation, and infection control was a priority. During surgery, the arteries around the transplanted kidney were resected as they appeared vulnerable owing to the effects of infection. The EIA was terminally anastomosed using a non‐infected artery (Fig. 1b–d). The central and distal sides of the EIA were sufficiently peeled off to perform tension‐free anastomoses. The patient was placed on bed rest until postoperative day 4 because of the high risk of postoperative VC. On postoperative day 7, when abdominal pressure was applied to defecate, the patient became aware of severe pain in the lower abdomen and subsequently went into shock. Emergency CT revealed a pseudoaneurysm at the anastomosis site and bleeding from the abdominal cavity into the pelvic cavity (Fig. 2a,b). Emergency endovascular treatment was performed, and the pseudoaneurysm disappeared after stenting (Fig. 2c,d). Postoperatively, red blood cell transfusion was performed until the hemoglobin levels stabilized. He was discharged 23 days after resection following CT confirmation that the hematoma had diminished in size and that there was no further source of infection. At 12 months post‐TN, our patient continued to progress without anemia or infection and was being prepared for re‐transplantation.
Fig. 1.
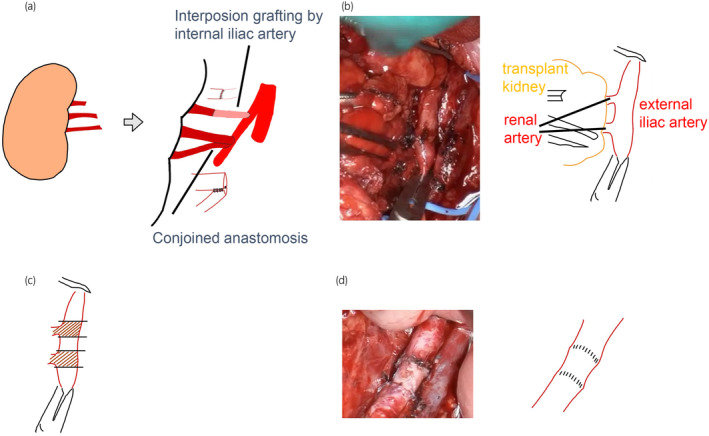
Illustration of operation techniques. (a) The transplanted kidney had three renal arteries, and the upper pole renal artery was short. The internal iliac artery was harvested as a graft and anastomosed end‐to‐end to the upper pole renal artery. Two main arteries were anastomosed and conjoined side‐to‐side. (b) The TK artery was very fragile and had severe adhesions to the surrounding area due to infection. Vascular suturing after severing the TK artery was extremely challenging. (c) The vessels were resected because the risk of VCs was high as the vessels had become fragile due to infection or other factors. (d) The uninfected EIA was used because of insufficient vessel length.
Fig. 2.
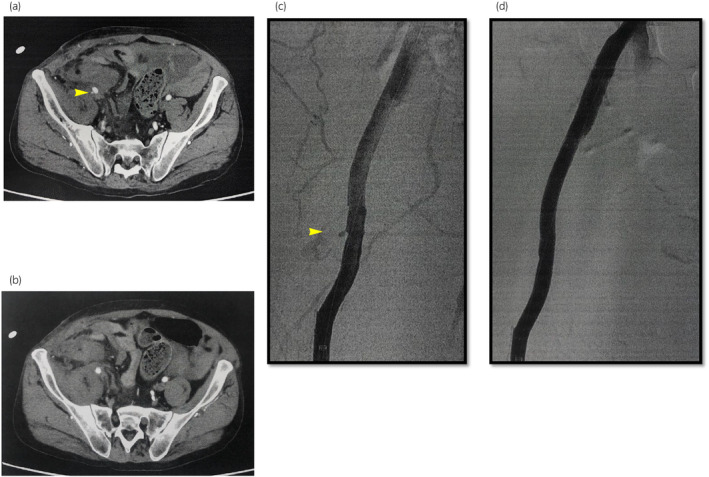
Contrast test to identify the bleeding site. (a) CT showing a pseudoaneurysm at the anastomosis of the EIA (b) The contrast material is also exposed to the abdominal cavity (c) Angiography showing the pseudoaneurysm (d) Covered stent placement (thickness, 8 mm; length, 10 cm).
Discussion
The British Transplantation Society reported indications for TN in 2014, and TN is used in many centers, 4 with decisions on whether to perform TN based on perceived benefits and risks. The indications, advantages, and disadvantages of TN are listed in Table 1. 5 , 6
Table 1.
Indications, advantages, and disadvantages of TN
| Indications | Advantage | Disadvantage |
|---|---|---|
| Localizing symptoms (pain, infection, bleeding) that are resistant to medical therapy in a failed graft | Reduction in chronic rejection | Decreased GSR |
| To create space for re‐transplantation | Beneficial for survival on dialysis | Loss of residual kidney function |
| To enable complete withdrawal of immunosuppression | Prevention of graft intolerance syndrome | Difficulty in cross‐matching and longer waiting period for re‐transplant |
| Risk of graft rupture | Withdrawal of immunosuppressants | |
| Graft malignancy | Surgical complications | |
| Refractory anemia with raised CRP | ||
TN‐related complications such as bleeding, hematoma, and infection have been reported, with incidence rates ranging from 5% to 48%. 7 The incidence of VC has been reported to be 5.6%, with most reported cases being life‐threatening. 1 Risk factors include infection of the anastomotic site, 1 with the risk reported to be higher when TN is performed following 12 months of dialysis resumption. 2 Chronic rejection may also be a risk factor for pseudoaneurysm. 3 For our patient, underlying disease was also a risk factor for pseudoaneurysm, and patients with ADPKD are known to be prone to pseudoaneurysm during other common surgical procedures. 8 , 9 , 10 Table 2 lists the relevant studies identified following a PubMed search relating to VC after TN. Pseudoaneurysms are common in VC, and the risk of mortality is high. Prophylactic methods for VC include immediate vascular reconstruction through bypassing artificial vessels or the saphenous vein at the time of TN, whereas non‐immediate vascular reconstruction involves ligation of the EIA, followed by antibiotic treatment and two‐phase bypass surgery. 1 Eng et al. reported on two patients for whom artificial vessels or saphenous veins were used during TN. However, one patient died of MRSA wound infection and the other patient had a severe hemorrhage stemming from the site of the vein graft owing to MRSA infection. 1 Immediate vascular reconstruction is associated with VCs in cases where reconstruction occurs in the presence of local infection. Non‐immediate vascular reconstruction is performed when local infection has resolved; therefore, VCs are unlikely to occur. According to this report, ligation of the EIA without reconstruction at the time of TN is not uniformly associated with limb ischemia. 1 If the ipsilateral lower limb is deemed critically ischemic preoperatively, an extra‐anatomical bypass, such as a femoral‐femoral bypass graft employing antibiotics, is the preferred reconstruction method. However, this report appears not to have been updated as a search of more recent literature did not identify any reports on ligation of the EIA. Ligation of the EIA was not a treatment option at our hospital because of the risk of lower limb ischemia.
Table 2.
Indications, advantages and disadvantages of TN
| Author (references no.) | Patient no. | Indication for TN | VC | Interval between TN and diagnosis of VC | Clinical presentation | Treatment | Out come (post TN days) |
|---|---|---|---|---|---|---|---|
| Payne et al. 11 | 1 | Haemorrhage | EIA pseudoaneurysm post‐TN | 1 month | Wound haemorrhage | EIA ligation | Death (6 months) |
| Payne et al. 11 | 2 | Early graft failure | EIA pseudoaneurysm post‐TN | 6 weeks | Wound haemorrhage | EIA ligation | Death (1 month) |
| Payne et al. 11 | 3 | Acute rejection, sepsis | Fistula from iliac artery to appendix | 2 months | Intestinal haemorrhage | EIA ligation, resection of the appendix | Death |
| Brown et al. 12 | 4 | Acute rejection, sepsis | EIA bleeding post‐TN | 2 weeks | Wound haemorrhage | EIA ligation | Alive |
| Brown et al. 12 | 5 | Acute rejection | EIA bleeding post‐TN | 1 week | Abdominal pain, pulsatile mass | EIA ligation | Alive |
| Eng et al. 1 | 6 | Haemorrhage, sepsis | EIA pseudoaneurysm post‐TN | NA | NA | EIA ligation femoral‐femoral cross over grafting | Death (50 days) |
| Eng et al. 1 | 7 | Chronic rejection | EIA injury at TN | NA | NA | EIA ligation | Alive |
| Eng et al. 1 | 8 | Renal vein thrombosis, sepsis | EIA pseudoaneurysm and bleeding at TN | 0 days | NA | EIA ligation | Alive |
| Eng et al. 1 | 9 | Acute rejection, renal vein thrombosis | EIA injury at TN bleeding post‐TN | 21 days | NA | EIA ligation, saphenous vein grafting | Alive |
| Eng et al. 1 | 10 | Acute rejection | EIA bleeding post‐TN | NA | NA | EIA ligation femoral‐femoral cross over grafting | Alive |
| Eng et al. 1 | 11 | Chronic rejection | EIA injury at TN | NA | NA | EIA ligation | Death (3 days) |
| Eng et al. 1 | 12 | Haemorrhage, sepsis | EIA bleeding at TN | NA | NA | EIA ligation | Death (3 months) |
| Eng et al. 1 | 13 | Acute rejection, sepsis | EIA pseudoaneurysm post‐TN | 7 weeks | NA | Stent grafting | Alive |
| Eng et al. 1 | 14 | Chronic rejection | EIA pseudoaneurysm post‐TN | 6 months | NA | Stent grafting | Alive |
| Bracale et al. 3 | 15 | Chronic rejection | EIA pseudoaneurysm post‐TN | 37 months | Abdominal pain, pulsatile mass | EIA ligation, interposition grafting | Death (75 months) |
| Bracale et al. 3 | 16 | Renal vein thrombosis | EIA pseudoaneurysm post‐TN | 7 months | Asymptomatic | EIA ligation, interposition grafting | Alive |
| Bracale et al. 3 | 17 | Acute rejection | EIA pseudoaneurysm post‐TN | 71 days | Local discomfort, pulsatile mass | Stent grafting | Alive |
| Bracale et al. 3 | 18 | Renal arterial thrombosis | EIA pseudoaneurysm post‐TN | 6 months | Abdominal pain, anemia, fever, tender mass | EIA ligation, interposition grafting | Alive |
| Bracale et al. 3 | 19 | Chronic rejection | EIA pseudoaneurysm post‐TN | 5 months | Local pain, pulsatile mass | Stent grafting | Alive |
| Bracale et al. 3 | 20 | Acute rejection, sepsis | EIA pseudoaneurysm post‐TN | 13 days | Abdominal pain, fever, hypotension | EIA ligation femoral‐femoral cross over grafting | Alive |
| Siddiqui et al. 13 | 21 | Acute rejection, renal vein thrombosis | EIA bleeding post‐TN | 5 days | Abdominal pain | Stent grafting | Alive |
| Bracale et al. 14 | 22 | Early graft failure | EIA pseudoaneurysm post‐TN | 3 months | Abdominal pain, severe dyspnea, tachycardia | Stent grafting | Alive |
| Borges et al. 15 | 23 | Chronic rejection, sepsis | EIA pseudoaneurysm post‐TN | 1 year | Abdominal pain, pulsatile mass | Resection of the pseudoaneurysm and anastomosis between the common iliac artery and the Carrell patch | Alive |
In addition, care must be taken postoperatively as bleeding can occur a week after surgery, as in this case. A sufficient period of postoperative rest and thorough evaluation using imaging studies are necessary before discharge from the hospital.
Author contributions
Kuniaki Inoue: Writing – original draft. Shunta Hori: Conceptualization. Mitsuru Tomizawa: Conceptualization; writing – review and editing. Tatsuo Yoneda: Conceptualization; writing – review and editing. Yasushi Nakai: Conceptualization; writing – review and editing. Makito Miyake: Conceptualization; writing – review and editing. Nobumichi Tanaka: Project administration. Kiyohide Fujimoto: Project administration; supervision.
Conflict of interest
The authors declare no conflict of interest.
Approval of the research protocol by an Institutional Reviewer Board
Not applicable.
Informed consent
Consent to participate and for publication were acquired from the patient.
Registry and the Registration No. of the study/trial
Not applicable.
Acknowledgments
The authors would like to thank the patient for his important contributions.
References
- 1. Eng MM‐P, Power RE, Hickey DP, Little DM. Vascular complications of allograft nephrectomy. Eur. J. Vasc. Endovasc. Surg. 2006; 32: 212–216. [DOI] [PubMed] [Google Scholar]
- 2. Chowaniec Y, Luyckx F, Karam G et al. Transplant nephrectomy after graft failure: is it so risky? Impact on morbidity, mortality and alloimmunization. Int. Urol. Nephrol. 2018; 50: 1787–1793. [DOI] [PubMed] [Google Scholar]
- 3. Bracale UM, Carbone F, del Guercio L et al. External iliac artery pseudoaneurysm complicating renal transplantation. Interact. Cardiovasc. Thorac. Surg. 2009; 8: 654–660. [DOI] [PubMed] [Google Scholar]
- 4. Management of the failing kidney transplant British transplantation society guidelines. 2014. [Cited 20 Oct 2023]. Available from URL: https://bts.org.uk/wp‐content/uploads/2016/09/13_BTS_Failing_Graft‐1.pdf. [DOI] [PubMed]
- 5. Leal R, Pardinhas C, Martinho A, Sá HO, Figueiredo A, Alves R. Challenges in the management of the patient with a failing kidney graft: a narrative review. J. Clin. Med. 2022; 11: 1–13. 10.3390/jcm11206108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vlachopanos G, El Kossi M, Aziz D et al. Association of nephrectomy of the failed renal allograft with outcome of the future transplant: a systematic review. Exp. Clin. Transplant. 2021; 20: 1–11. [DOI] [PubMed] [Google Scholar]
- 7. Al Badaai G, Pernin V, Garrigue V et al. Renal graft intolerance syndrome in late graft failure patients: efficacy and safety of embolization as first‐line treatment compared to surgical removal. Transpl. Int. 2017; 30: 484–493. [DOI] [PubMed] [Google Scholar]
- 8. Joana BN, Filipe BR, Jose AL et al. Autosomal dominant polycystic kidney disease and coronary artery dissection or aneurysm: a systematic review. Renal Fail. 2016; 38: 493–502. [DOI] [PubMed] [Google Scholar]
- 9. Pirson Y. Extrarenal manifestations of autosomal dominant polycystic kidney disease. Adv. Chronic Kidney Dis. 2010; 17: 173–180. [DOI] [PubMed] [Google Scholar]
- 10. Infante B, Di Lorenzo A, Troise D et al. Iliac pseudoaneurysm, only a manifestation with more causes: a case report. J. Endovasc. Ther. 2021; 28: 642–645. [DOI] [PubMed] [Google Scholar]
- 11. Payne JE, Storey BG, Rogers JH, May J, Sheil AG. Serious arterial complications following removal of failed renal allografts. Med. J. Aust. 1971; 1: 274–275. [DOI] [PubMed] [Google Scholar]
- 12. Brown MW, Bradley JA, Hamilton DN. Ligation of the external iliac artery for post‐transplant nephrectomy bleeding. Postgrad. Med. J. 1982; 58: 378–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Siddiqui AC, Lew SQ, Sarin S, Venbrux AC. Emergency endovascular stenting of the right iliac artery in a patient with secondary haemorrhage following transplant nephrectomy. BMJ Case Rep. 2012; 2012: bcr0220125827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bracale UM, Porcellini M, del Guercio L, Bracale G. Embolization of a symptomatic pseudoaneurysm developing after transplant nephrectomy. Intern. Med. 2013; 52: 291–292. [DOI] [PubMed] [Google Scholar]
- 15. Borges L, Oliveira N, Dias E, Cássio I. Iliac artery pseudoaneurysm: a rare complication following allograft nephrectomy. BMJ Case Rep. 2014; 2014: bcr2013202596. [DOI] [PMC free article] [PubMed] [Google Scholar]


