Abstract
Conscience is defined as the cornerstone of ethics and is considered a valuable asset. There is, however, little evidence about how Iranian nurses perceive conscience. The purpose of this study was to psychometrically evaluate the Persian version of the Perception of Conscience Questionnaire (PCQ) in Iranian nurses. In this cross-sectional and descriptive study, a psychometric evaluation of the PCQ was conducted on Iranian nurses in 2022. A total of 300 nurses participated in this study to validate the PCQ. At first, the initial translation and determination of face validity was done, and content validity was assessed using the Content Validity Index and Content Validity Ratio. Reliability was determined by intra-class correlation coefficient and Cronbach's alpha coefficient.
The construct validity of the PCQ was determined by exploratory factor analysis, which led to the extraction of five factors of warning signal, valuable asset, spiritual power, burden and conscience outcomes from the initial 14 factors of the questionnaire. Reliability of the whole questionnaire was calculated to be 0.80 using Cronbach's alpha. While an intra-class correlation coefficient of 0.58 indicated average stability, the five-factor construct of the PCQ showed good validity and reliability. Therefore, our findings proved that this tool is suitable for assessing Iranian nurses’ perception of conscience.
Key Words: Conscience, Ethics, Nurse, Psychometrics.
Introduction
Conscience is interpreted as the cornerstone of ethics; it affects the personal and professional lives of people, and is constantly present in everyday life. In the popular sense, conscience carries various concepts, including good, bad, sin, clear, unclear, and peace of mind or lack thereof (1). In related texts, it has been described as the inner voice that acts as our moral compass, or an integrated set of moral values, showing us how to be or how to act (1, 2). Throughout history, this concept has been the focus of religions, philosophy and science in various fields. For example, the concept of conscience can be found in many religions, a clear example being Islam, which refers to conscience as “nafs luwame or blamer” (3). In philosophy, conscience is a theoretical construct that is dependent on personal feelings and thoughts (4), and in its philosophical sense is an inner feeling or a vague sense of guilt about what has been done or should have been done (5). Finally, in psychology, Freud's inference about conscience is also interesting, since he introduces conscience as a superego that goes against a person and adjusts the demands of the institution and that person with external realities, and in case of mismatch, it causes neurosis and harm in individuals (6).
In the field of nursing, Cleary and Liss (citing Peplau) write that nurses should be at the forefront of ethics in providing care and practice a high level of ethics, goodness and honesty in patient care (7). According to research conducted on the role of conscience in nursing, conscience plays a significant part in guiding nurses' decision-making and their professional actions in the direction of goodness, honesty, truth and correctness. In this regard, in their study entitled "The Role of Conscience in Nursing", Jensen and Liddell showed that nurses consider conscience as an important factor in their professional practice and refer to it as a guiding force, a restraining mechanism and a source of sensitivity in nursing care (8). Therefore, according to what is stated in the texts, in nursing, conscience is defined as authority, a warning signal, a feeling and sensitivity, a valuable asset, a burden and a responsibility, an essence of nursing and a culture-dependent phenomenon (4, 8, 9). In nursing practice, conscience has been broadly considered as a basis for ethical affairs and ethical nursing care (10). The role of conscience in nursing is expressed in different ways, such as warning, a guide, a sensitivity elevator and a moral guide to the patient's needs (11, 12). Jodaki et al. also consider conscience as an existential command center that is associated with a tormented conscience and a sense of guilt if neglected, but one that brings a feeling of peace and satisfaction when applied in the care process (10).
Although philosophers believe conscience to be dependent on personal feelings and thoughts, and nurses consider it an inherent and valuable asset, in Iran there is little evidence of how nurses interpret conscience. Some nurses leave the profession based on how they perceive conscience, but some experience moral distress and manage the distress in different ways (4). Nurses’ views about the origin of conscience and its role, importance and place in nursing practice help researchers to understand the meaning of conscience and how to respond to the needs created by it. In general, the knowledge and understanding of conscience in the nursing community can help us understand feelings and behaviors related to troubled conscience and the resulting stress (1). However, research in this field is faced with many challenges due to the importance of this subject and the lack of a questionnaire with confirmed validity and reliability. Since this questionnaire has been designed and developed to assess the perception of conscience (1) and in order to utilize it within the nursing community of Iran, the researchers in this study decided that it should be adopted and psychometrically evaluated. Therefore, the present study was designed and implemented with the aim of adopting and psychometrically evaluating the Perception of Conscience Questionnaire to be used in the nursing community of Iran.
Methods
This descriptive and cross-sectional study was conducted in 2022. In this study, the Perception of Conscience Questionnaire developed by Dahlqvist et al. in 2007 was psychometrically evaluated in Iranian nurses. The questionnaire consisted of 15 items in 6 factors: authority, warning signal, demanding sensitivity, asset at work, burden, and depending on culture. Each item had a 6-point Likert scale, ranging between 1 (No, totally disagree) and 6 (Yes, entirely agree).
Participants were asked to respond to each item based on their experience and views. No total sum could be calculated because the 15 items of the PCQ are analyzed separately (1). The questionnaire has been validated in Swedish health-care providers and nurses by Åhlin et al. in 2012 (13). The research community consisted of nurses working in hospitals affiliated to Mazandaran Universities of Medical Sciences. After obtaining permission from the ethics committee of Mazandaran University of Medical Sciences, participants were asked to fill out the questionnaire. To collect data, a demographic information form and a translated version of the 15-item PCQ developed by Dahlqvist et al. were used. The guidelines of the WHO were used for the translation and validation of the questionnaire. At first the questionnaire was translated into Farsi by two English language experts, then the translated versions were compared and the questions were adjusted one by one. After this stage, in order to compare and match the translated version with the original version of the tool, the Persian version was translated back into the original language by two people fluent in English. These people had not seen the questionnaire before and were not familiar with its content. After making sure that the translated version and the original version matched, the face validity of the questionnaire was determined. Inclusion criteria consisted of consenting to participate in the study, having a bachelor's degree or higher in nursing, and being occupied in the nursing profession. The convenience sampling method was used to select the samples and finally the questionnaire was completed by 300 nurses in 7 major hospitals in Mazandaran province.
Qualitative and quantitative methods were used to check the face validity of the questionnaire. For this purpose, the translated version was given to 10 nurses working in the hospitals of Mazandaran to evaluate the concepts and absence of ambiguities, and then the necessary corrections were made according to their comments. In order to determine the face validity of the questionnaire, the same 10 nurses were asked to rate the importance of items on a Likert scale, from not important (1) to very important (5). Then, the scores of the items were calculated by the formula “importance × frequency”, and an effect score higher than 1.5 for each item was considered desirable (14).
Both qualitative and quantitative methods were used to assess content validity. In the qualitative method, the questionnaire was given to ten members of the nursing faculty in Mazandaran universities of medical sciences. The faculty members were asked to use the appropriate concepts, put the phrases in their proper places, give points after qualitatively reviewing the questionnaire based on grammatical criteria, and finally provide an appropriate feedback. Then, their suggestions were considered in the questionnaire (15). The quantitative content validity of the tool was calculated using content validity ratio and content validity index for each item of the tool. The content validity ratio was used to examine the necessity of each item, and its purpose was to ensure that the best and most correct content had been selected. Therefore, the tool was given to ten faculty members who worked in the field of nursing and ethics and had at least 2 years of experience in school of nursing and midwifery, and they were asked to review the questionnaire based on a three-option Likert scale: not necessary (score 1), useful but not necessary (score 2) and necessary (score 3). According to the Lawshe table and the evaluation of the ten experts, a score of 0.62 and above was obtained for each item, which indicated that the item was important and necessary (16). The content validity index was also used to calculate the three characteristics of simplicity and fluency, relevance, and clarity or transparency of each item. Each of the items was evaluated in terms of relevance based on a Likert scale: not at all relevant (score 1), somewhat relevant (score 2), relatively relevant (score 3), and completely relevant (score 4). For two criteria, the experts evaluated each item in the same way based on a four-point Likert scale. Items with scores higher than 0.79 remained in the questionnaire, items with scores between 0.70 and 0.79 were considered questionable and had to be revised, and items with scores less than 0.70 were removed from the tool (17). The content validity index calculation formula was as follows:
CVI = total number of evaluators/number of experts who gave a score of 3 or 4 to the target item
The construct validity of the questionnaire was measured using exploratory factor analysis. In factor analysis, a few factors are extracted from overlapping variables. The extracted factors do not interfere with each other and at the same time explain a clear and meaningful structure. According to the minimum sample size of 5 to 10 samples for each question and considering the fact that the current questionnaire had 15 items, the number of participants needed to be at least 200, taking into account a 15% possibility of inappropriate data and partial compilation of the tool. The KMO test was performed to confirm the appropriateness of sample size for exploratory factor analysis. A KMO of 0.6 to 0.7 was considered suitable, and 0.7 to 0.8 desirable (18). Extraction of the questionnaire factors was done by principal components analysis and scree plot, considering the eigenvalue. Factors with an eigenvalue greater than one were considered as factors of the studied concept. In the next step, the data rotation was done using the Varimax method, and by considering the amount of factor loading and the correlation between observations and components, the items related to each factor were determined (19). Also, confirmatory factor analysis was used to confirm the extracted construct in exploratory factor analysis. At this stage, goodness of fit indices of Chi-square, degree of freedom (df), root mean square error of approximation, goodness of fit index, approximation error variance estimates and other goodness indices were examined (20). The reliability of a questionnaire is confirmed if it gives the same results at different times. In this study, the reliability of the questionnaire and its internal consistency were investigated using Cronbach's alpha coefficient. An internal consistency higher than 0.7 was considered appropriate. Although a higher Cronbach's alpha coefficient implies better reliability of the questionnaire, large numbers also indicate a large number of questions that may be effective in answering the questionnaire. The pretest-posttest method was also used to check the stability of the questionnaire, and for this purpose, ten patients completed the questionnaire in two stages 14 days apart, and the stability of the questionnaire was evaluated by comparing the scores obtained from the first and the second stages.
Ethical Considerations
In order to comply with ethical codes, permission to conduct the research was obtained from Mazandaran University of Medical Sciences under the ethics code IR.MAZUMS.REC.1401.14697. Necessary explanations about the objectives of the study were given to the participants, both experts and nurses. The study method was explained to the participants and their informed consent was obtained before they began to fill in the questionnaire. All participants were also assured that their information would remain confidential. In general, the researchers remained loyal to the ethics code of Mazandaran University of Medical Sciences in the research process.
Results
The results of the data analysis showed that the number of nurses participating in this study was 300 and their mean age was 35.08 years (7.63). The mean of their work experience was 15.75 years, and 73% of them were married. In terms of education level, most (68%) had a bachelor’s degree.
The sample size adequacy index (KMO value of 0.82) and the significant Bartlett's sphericity test (P < 0.05) indicated that the sample size was sufficient to perform the factor analysis. The commonality of items was more than 0.4 for all items. The face and content validity of the questionnaire were confirmed based on the impact score of the item and the CVR results. According to the Lawshe table, the CVR score for each item was above the acceptable level, but item number 15 (conscience gives us wrong messages) obtained an unacceptable score (0.62) and was therefore removed.
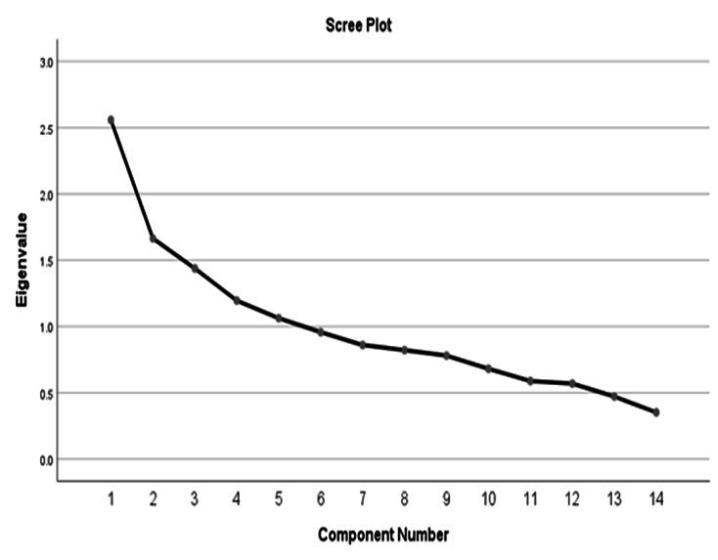
In the exploratory factor analysis, the eigenvalues were presented in a scree plot. The first five components had eigenvalues greater than one, but in the sixth and subsequent components, the eigenvalues dropped significantly. The sharp drop between components 1 to 5 and components 6 to 14 showed that the first 5 were the main factors, expressing 56.56% of the total variance (Figure 1). The variance explained by factors 1 to 5 were 13.99%, 12.61%, 11.71%, 9.23% and 9.002%, respectively (Table 1). The Varimax method was used to rotate the data.
Figure 1.
Scree plot for determining the number of appropriate factors.
Table 1.
The determined variance for factors of the questionnaire.
| Factor |
Item
Number |
Item |
Factor
Loading |
Eigenvalue |
Variance
(%) |
|---|---|---|---|---|---|
| Warning Signal |
4 | Conscience warns us not to harm ourselves. | 0.686 | 1.195 | 13.992 |
| 5 | Conscience does not allow us to harm others. | 0.734 | 1.062 | ||
| 6 | Regardless of the thoughts and opinions of others, we must answer our inner call. |
0.392 | 0.957 | ||
| 7 | In my work environment, I express what my conscience tells me. |
0.710 | 0.860 | ||
| Valuable Asset | 1 | The call of conscience must be heard and understood. |
0.502 | 2.559 | 12.618 |
| 8 | In my work, I act according to the call of my conscience. |
0.816 | 0.821 | ||
| 9 | Ignoring the call of conscience weakens our conscience. |
0.773 | 0.780 | ||
| Spiritual Power |
3 | Ignoring the call of conscience is inevitable. | 0.403 | 1.438 | 11.714 |
| 13 | God speaks to us through conscience. | 0.775 | 0.472 | ||
| 14 | I grow as a person when I follow my conscience. |
0.633 | 0.352 | ||
| Burden | 11 | My conscience is very strict. | 0.782 | 0.588 | 9.239 |
| 12 | Our conscience expresses our social values. | 0.522 | 0.569 | ||
| Conscience Outcomes |
2 | Inner peace requires listening to the call of conscience. |
0.587 | 1.664 | 9.002 |
| 10 | I have to silence my conscience to work in the health-care system. |
0.711 | 0.681 |
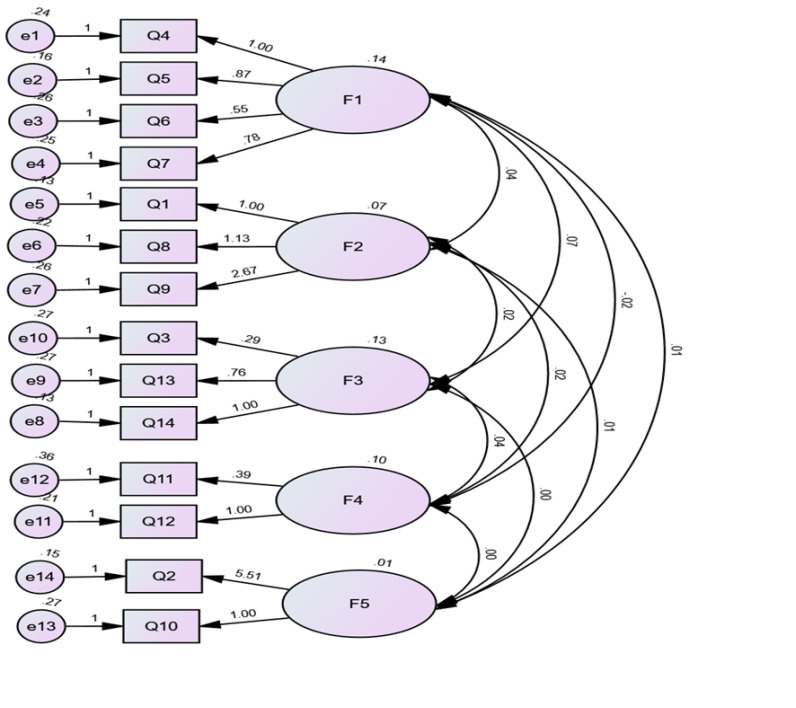
Also, according to the actual and recommended values of goodness indicators, the goodness of fit for the 14-item model of the original PCQ was found to be acceptable (Table2). The results showed that the CFA based on the five-factor model extracted from the EFA had an acceptable goodness of fit with the obtained data. The reliability of the whole instrument was 0.80 using Cronbach's alpha. To check the stability of the instrument, the intra-class correlation coefficient was calculated at 0.58, which indicated the average stability of the instrument. Figure 2 shows the standardized values of relationships between variables. If the factor loadings listed on the arrows were greater than 0.4, it would mean that the items were good indicators for the hidden variable (factor). If there was an item with a factor loading less than 0.4, it would be necessary to carefully remove that item and repeat the confirmatory factor analysis. Factor loadings greater than 0.4 were considered to have a significance level, with those greater than 0.5 indicating high significance. Of course, in the present study, after removing items 3 and 11, the model fit test could not be performed, and these items were not removed.
Table 2.
Actual and recommended values of goodness of fit indices.
| Goodness of Fit Indices | X2 df x2/df GFI AGFI CFI TLI RMSEA |
|---|---|
| Recommended Values | - - ≤ 3 ≥ 0.9 ≥ 0.9 ≥0.9 ≥ 0.9 ≤ 0.08 |
| Actual Values | 198.8 67 2.967 0.930 0.864 0.952 0.933 0.08 |
Figure 2.
Structural equation modeling, plot of standardized coefficients of path for the five-factor structure.
Other findings showed that the items of "In my work environment, I express what my conscience tells me" and "Regardless of the thoughts and opinions of others, we must respond to our inner voice" had been placed in the factors of "option" and "possession” in the original tool; in the present study, however, they were relocated to the factor of "warning signal", as they would have conveyed almost the same concept to the participants in this study. Also, items in the factors of "demanding sensitivity" and "culture-dependent" in the original study were relocated to other factors in the present study, and the researchers labeled them according to the concepts of each item.
Discussion
The findings showed high validity and reliability for the Persian version of the Perception of Conscience Questionnaire in Iranian Nurses. The original questionnaire was created by Dahlqvist et al. (2007) and included six factors (1, 13). In the study by Dahlqvist et al. (2007), perception of conscience included aspects such as authority, asset, warning signal, demanding sensitivity, burden and culture-dependent. In the present study, five factors were extracted, including warning signal, valuable asset, spiritual power, burden and conscience outcomes, which were labeled by the researchers with the help of experts who had experience in research on conscience. In this study, some items were relocated to different factors, generally due to the semantic and conceptual affinity of each question based on the cultural and religious background of the Iranian society. The factor that had the highest variance in the present study was "warning signal", while in the study by Dahlqvist et al. (2007), the highest variance was related to "authority" with a value of 19.2% (1). In Åhlin et al.'s study, as in Dahlqvist's study, six factors were extracted through principal component analysis, using Varimax rotation and an eigenvalue greater than 0.9, and the total variance of the instrument was equal to 63.19%, which was reported to be more than the present study; also, in Åhlin et al.'s study, the reliability of the tool was reported to be 0.70 using Cronbach's alpha test, but in the present study, it was 0.80 (13).
The first factor of the questionnaire in the present study is warning signal, which includes four items that rely on concepts aimed at protecting nurses from themselves and patients, and therefore nurses should be more sensitive to this issue. The warning signal of conscience can act as a guide for nurses in providing quality care and doing the right thing without caring about the opinion of others (10). A study by Nazari et al. also showed that the perception of conscience is a warning and protective signal against burnout in nurses (2). Also, in Lamb's study, conscience as a commander is dependent on culture and issues a warning signal that can be important in improving the quality of ethical care (4).
The second factor is valuable asset, which covers three items. This factor refers to concepts such as understanding and acting on conscience and emphasizing conscience in the actions of nurses to prevent its weakening. In several studies, the concept of conscience has been referred to as a valuable asset that guides nurses toward the correct moral practice, while having a great impact on improving the quality of nursing care (9, 21). The results of a study by Lentz et al. showed that we should follow our conscience regardless of what others think, and this helps us make an ethical decision; they also stated that conscience is a value that helps people in ethical decision-making (22). In line with these findings, a study by Hasani et al. in Iran defined conscience as an intrinsic and internal asset that can be influenced by religion, culture and environment (23).
The third factor is spiritual power, which includes three items. This factor refers to concepts such as inner strength, God's relationship with man, and growth and development through conscience. In several studies, conscience has been considered as an internal force that is experienced from within and beyond (24, 25). In other studies, conscience has been defined as an internal force and a compass of moral action that guides the behavior and performance of humans. In caring for patients, conscience as a spiritual force can help to offer patients the best care possible and should be a moral guide for nurses (1, 5, 26).
The fourth factor is burden, which consists of two items. This factor refers to concepts such as strictness and social value. Although conscience can be considered as an asset, it can become a burden when taken too seriously. Also, in moral decision-making, conscience depends on our values and social context (1). Solms expresses from Freud's point of view that conscience as a floating anxiety that increases the burden and responsibility of people in life (27). When nurses follow their conscience to provide quality care, they have a positive view of it, but the conflict caused by conscience can lead to confusion and is associated with guilt (28). A study conducted by Yildirim et al. concluded that the understanding of conscience and the impact of conscience on the nurse-patient relationship can make nurses more sensitive to patient care and at the same time improve the quality of nursing care (29).
The fifth factor includes two items and is related to conscience outcomes. This factor refers to having the inner peace to listen to the call of conscience, and also not paying attention to conscience to be able to survive in the health-care system. Ignoring conscience and disobeying it leads to conflict and a guilty conscience. Studies have shown that these outcomes can lead to burnout and reduced quality of nursing care (26, 30, 31). In their study, Glasberg et al. pointed out that the tormented conscience helps morally sensitive people in making moral decisions, so that if a person cannot act based on his/her conscience, he/she will experience conflict and a sense of guilt (26). Also, ignoring one’s conscience leads to feelings of guilt and shame in nurses (4, 30). When people act against their conscience, they may suffer from severe pangs of conscience, or even claim that their conscience and sense of guilt are not important. Conscientious reactions at the time of taking action against one’s conscience can cause discomfort and guilt on the one hand, but improve and develop the conscience on the other (32, 33).
Conclusion
The results of the present study showed that the Persian version of the Perception of Conscience Questionnaire (PCQ) has acceptable validity and reliability, and the five-factors of the PCQ can satisfactorily measure the perception of conscience among Iranian nurses. Therefore, the PCQ can be used as a suitable tool for researchers and health policy-makers to evaluate nurses’ perception of conscience in order to promote nurses’ health and the overall quality of nursing care. This questionnaire can also measure the correlation between the perception of conscience and other concepts and variables in nurses and other health-care providers. In the end, it is suggested that a psychometric evaluation of the PCQ be done among other health-care providers, for instance physicians. Likewise, it is recommended to evaluate the relationship between the perception of conscience and other variables such as the quality of nursing care.
Acknowledgments
This article is based on the findings of a research project under the research code 14697 approved by Mazandaran University of Medical Sciences. We hereby thank and appreciate the participation and cooperation of the officials, faculty members and nurses who helped us in this research.
Notes:
Citation to this article:
Hasani SA, Nazari R, Shahsavari H, Ramim T, Jodaki K. Psychometric evaluation of the Persian version of the perception of conscience questionnaire in Iranian nurses. J Med Ethics Hist Med. 2023; 16: 16.
Conflict of Interests
The authors declare no conflicts of interest regarding the publication of this research project and paper.
Funding Statement
The study was supported with using the financial fund from the Mazandaran University of Medical Sciences.
References
- 1.Dahlqvist V, Eriksson S, Glasberg A-L, Lindahl E, Lü tzén K, Strandberg G, et al. Development of the perceptions of conscience questionnaire. Nurs Ethics. 2007;14(2):181–93. doi: 10.1177/0969733007073700. [DOI] [PubMed] [Google Scholar]
- 2.Nazari S, Norberg A, Strandberg G, Åhlin J, Ericson-Lidman E, Mazaheri M. Perceptions and stress of conscience in relation to burnout among nursing staff in older people care settings: a quantitative study. BMC Nurs. 2023;22(1):379. doi: 10.1186/s12912-023-01529-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdulwaly UC. [Pedoman Murajaah Al-Qur’an] Farha Pustaka; 2020. [Google Scholar]
- 4.Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood KW. Conscience, conscientious objection, and nursing: a concept analysis. Nursing Ethics. 2019;26(1):37–49. doi: 10.1177/0969733017700236. [DOI] [PubMed] [Google Scholar]
- 5.Rhodes R. Conscience, conscientious objections, and medicine. Theoretical Medicine and Bioethics. 2019;40:487–506. doi: 10.1007/s11017-019-09513-9. [DOI] [PubMed] [Google Scholar]
- 6.Nel M. Conscience: Phenomena and theories; In Hendrik G, Stoker. die Skriflig. 2019;53(1):12. [Google Scholar]
- 7.Cleary M, Lees D. The role of conscience in nursing practice. Issues in Mental Health Nursing. 2019;40(3):281–3. doi: 10.1080/01612840.2019.1548852. [DOI] [PubMed] [Google Scholar]
- 8.Jensen A, Lidell E. The influence of conscience in nursing. Nursing Ethics. 2009;16(1):31–42. doi: 10.1177/0969733008097988. [DOI] [PubMed] [Google Scholar]
- 9.Mazaheri M, Ericson Lidman E, Zargham Boroujeni A, OhlE n J, Norberg A. Clear conscience grounded in relations: Expressions of Persian-speaking nurses in Sweden. Nurs Ethics. 2017;24(3):349–361. doi: 10.1177/0969733015603442. [DOI] [PubMed] [Google Scholar]
- 10.Jodaki K, Esmaeili M, Cheraghi MA, Pashaeypoor S, Hoseini ASS. Clarifying the concept of conscience in nurses’ ethical performance in Iran: a concept analysis study. J Med Ethics Hist Med. 2021;14:14. doi: 10.18502/jmehm.v14i14.7669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saarnio R, Sarvimäki A, Laukkala H, Isola A. Stress of conscience among staff caring for older persons in Finland. Nursing ethics. 2012;19(1):104–15. doi: 10.1177/0969733011410094. [DOI] [PubMed] [Google Scholar]
- 12.Lamb C, Pesut B. Conscience and conscientious objection in nursing: a personalist bioethics approach. Nursing ethics. 2021;28(7-8):1319–28. doi: 10.1177/0969733021996037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahlin J, Ericson-Lidman E, Norberg A, Strandberg G. Revalidation of the perceptions of conscience questionnaire (PCQ) and the stress of conscience questionnaire (SCQ) Nursing Ethics. 2012;19(2):220–32. doi: 10.1177/0969733011419241. [DOI] [PubMed] [Google Scholar]
- 14.Zamanzadeh V, Ghahramanian A, Rassouli M, Abbaszadeh A, Alavi-Majd H, Nikanfar A-R. Design and implementation content validity study: development of an instrument for measuring patient-centered communication. Journal of Caring Sciences. 2015;4(2):165–78. doi: 10.15171/jcs.2015.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clark LA, Watson D. Constructing validity: New developments in creating objective measuring instruments. Psychological Assessment. 2019;31(12):1412. doi: 10.1037/pas0000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Almanasreh E, Moles R, Chen TF. Evaluation of methods used for estimating content validity. Research in Social and Administrative Pharmacy. 2019;15(2):214–21. doi: 10.1016/j.sapharm.2018.03.066. [DOI] [PubMed] [Google Scholar]
- 17.Shrotryia VK, Dhanda U. Content validity of assessment instrument for employee engagement. Sage Open. 2019;9(1) [Google Scholar]
- 18.Jackson DL, Voth J, Frey MP. A note on sample size and solution propriety for confirmatory factor analytic models. Structural Equation Modeling: A Multidisciplinary Journal. 2013;20(1):86–97. [Google Scholar]
- 19.Safdari R, Yu P, Khenarinezhad S, Ghazanfari Savadkoohi E, Javanmard Z, Yousefi A, Barzegari S. Validity and reliability of the Persian version of the patient readiness to engage in health information technology (PRE-HIT) instrument. BMC Primary Care. 2022;23(1):50. doi: 10.1186/s12875-022-01665-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barzegari S, Arpaci I, Hasani A, Zabihi A, Nazari R. Psychometric properties of the Persian COVID19 phobia scale. Journal of Nursing and Midwifery Sciences. 2022;9(3):205. [Google Scholar]
- 21.Juthberg C, Sundin K. Registered nurses’ and nurse assistants’ lived experience of troubled conscience in their work in elderly care-a phenomenological hermeneutic study. International Journal of Nursing Studies. 2010;47(1):20–9. doi: 10.1016/j.ijnurstu.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 22.Lentz LM, Smith-MacDonald L, Malloy D, Carleton RN, Bremault-Phillips S. Compromised conscience: a scoping review of moral injury among firefighters, paramedics, and police officers. Front Psychol. 2021;12:639781. doi: 10.3389/fpsyg.2021.639781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hasani P, Jalali R, Abedsaeedi Z. Nurses’ experience of the perception of nursing conscience: a phenomenological study. Iranian Journal of Nursing Research. 2013;8(3):1–9. [Google Scholar]
- 24.Posey D. The inner Voice. Journal of Christian Nursing. 2023;40(2):133. doi: 10.1097/CNJ.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 25.Houen A. On inner voice, free indirect style, and lyric. Textual Practice. 2021;35(6):1037–63. [Google Scholar]
- 26.Glasberg A-L, Eriksson S, Dahlqvist V, Lindahl E, Strandberg G, Söderberg A, et al. Development and initial validation of the stress of conscience questionnaire. Nurs Ethics. 2006;13(6):633–48. doi: 10.1177/0969733006069698. [DOI] [PubMed] [Google Scholar]
- 27.Solms M. Extracts from the revised standard edition of Freud’s complete psychological works. The International Journal of Psychoanalysis. 2018;99(1):11–57. doi: 10.1080/00207578.2017.1408306. [DOI] [PubMed] [Google Scholar]
- 28.Ford NJ, Austin W. Conflicts of conscience in the neonatal intensive care unit: perspectives of Alberta. Nursing ethics. 2018;25(8):992–1003. doi: 10.1177/0969733016684547. [DOI] [PubMed] [Google Scholar]
- 29.Yildirim G, Kaya N, Altunbas N. Relationship between nurses' perceptions of conscience and perceptions of individualized nursing care: a cross‐sectional study. Perspectives in Psychiatric Care. 2022;58(4):1564–75. doi: 10.1111/ppc.12964. [DOI] [PubMed] [Google Scholar]
- 30.Munkeby H, Bratberg G, Devik SA. Meanings of troubled conscience in nursing homes: nurses’ lived experience. Nursing ethics. 2023;30(1):20–31. doi: 10.1177/09697330221117261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ahlin J, Ericson‐Lidman E, Norberg A, Strandberg G. A comparison of assessments and relationships of stress of conscience, perceptions of conscience, burnout and social support between healthcare personnel working at two different organizations for care of older people. Scandinavian journal of caring sciences. 2015;29(2):277–87. doi: 10.1111/scs.12161. [DOI] [PubMed] [Google Scholar]
- 32.Backman A, Sjogren K, Lövheim H, Lindkvist M, Edvardsson D. The influence of nursing home managers’ leadership on person-centred care and stress of conscience: a cross-sectional study. BMC nursing. 2021;20(1):1–8. doi: 10.1186/s12912-021-00718-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jasemi M, Aazami S, Hemmati maslak pak M, Habibzadeh H, Esmaeili Zabihi R. Factors affecting conscience-based nursing practices: a qualitative study. Nursing ethics. 2019;26(5):1350–60. doi: 10.1177/0969733018761173. [DOI] [PubMed] [Google Scholar]