Summary
Background
Metformin for women with overweight or obesity during pregnancy has been evaluated in randomized trials to reduce adverse pregnancy and birth outcomes. The effect on longer‐term child health remains of interest.
Objectives
To evaluate the effect of in‐utero exposure to metformin on child health compared with no exposure.
Methods
We assessed children born to 513 women who participated in the Metformin in addition to dietary and lifestyle advice for pregnant women with overweight or obesity: the GRoW randomized trial, where women were randomized to receive either metformin or placebo during pregnancy. Child weight, height, anthropometry, diet, physical activity and neurodevelopment were assessed at six and 18 months and three to five years of age. The main outcome was BMI z‐score > 85th centile for age and sex.
Results
The number of children with BMI >85th centile was similar between treatment groups at all time points. At 18 months and three to five years of age, more than half of the children had a BMI z‐score > 85th centile, indicating a high risk of childhood obesity.
Conclusions
We did not show evidence of the benefit of metformin for children of women with overweight or obesity during pregnancy adding to the growing literature on the lack of effect of pregnancy interventions in reducing longer‐term risks of childhood obesity.
Keywords: child follow‐up, metformin, overweight and obesity, pregnancy intervention, randomized controlled trial
1. INTRODUCTION
Oral metformin, an insulin‐sensitizing agent, is commonly used during pregnancy for the management of gestational diabetes. 1 More recently, its use has been evaluated as a potential intervention to improve outcomes for women with overweight or obesity, either alone or as an adjunct therapy to dietary and lifestyle advice. However, there is little evidence to suggest that the use of metformin in the setting of maternal overweight and obesity reduces either the risk of maternal adverse health outcomes or the occurrence of high infant birth weight. 2
While there is some evidence that the use of metformin in pregnancy may impact pre‐pubescent childhood growth measures, 3 the longer‐term impact on health outcomes of children born to women with overweight or obesity remains to be determined. While some have suggested improvement in some early child cardiovascular measures following antenatal metformin, 4 this is not universal. 5 Furthermore, these follow‐up studies have been limited by the relatively small numbers of participants assessed, and a lack of focus on child anthropometric measures.
The Metformin in addition to dietary and lifestyle advice for pregnant women with overweight or obesity: the GRoW randomized trial evaluated the effect of metformin as an adjuvant therapy to dietary and lifestyle advice, involving 524 pregnant women with overweight or obesity. We reported that women who received metformin in addition to dietary and lifestyle advice were at similar risk of birth of a baby with birth weight greater than 4000 g when compared with women who received the dietary and lifestyle intervention alone but had significantly lower weekly gestational weight gain. 2 There were no other differences identified in maternal or infant health outcomes. 2 We now report the follow‐up of children born to women who participated in the GRoW randomized trial at six months, 18 months, and three to five years of age.
2. METHODS
We have previously reported the methods and clinical outcomes of the GRoW Randomized Trial 2 , 6 (ACTRN12612001277831). Briefly, participants with a singleton pregnancy, BMI of 25 kg/m2 or more, between 10 and 20 weeks gestation, were randomly allocated to daily metformin or placebo. Metformin was commenced at 500 mg and increased to 2000 mg over four weeks if tolerated. Women in the Placebo group were instructed to commence taking a single tablet, identical in taste and appearance to the metformin and increase to four tablets if tolerated. All women participating in the trial received a comprehensive dietary and lifestyle intervention as we have described previously. Approval to conduct these follow‐up assessments at six months, 18 months, and three to five years of age was provided by the Human Research Ethics Committee of the Women's and Children's Health Network. GRoW participants provided informed written consent for their child's participation at each follow‐up assessment. Assessments were conducted by a trained research assistant who remained blinded to the original treatment group allocation of the woman.
2.1. Primary and secondary outcomes
The primary outcome for each follow‐up time point was a child's BMI z‐score > 85th percentile for age and sex.
A range of secondary outcomes were obtained and included:
-
Infant and child Anthropometric Measurements:
We have established and validated methods of conducting anthropometric measurements in infants at six and 18 months of age, and children three to five years of age, as we have reported previously. 7 , 8 , 9 Information obtained included the infant's/child's length/height, weight, weight‐for‐length, and anthropometric measurements (arm, thigh, waist and hip circumferences; biceps, triceps, sub‐scapular, abdominal, supra‐iliac and thigh skin‐fold thickness).
Trained research assistants used Harpenden skin‐fold callipers to obtain skinfold thickness measurements, and received ongoing standardized training, again as we have reported previously. 10 Weight, length, BMI, weight‐for‐length, and head circumference measures were converted to z‐scores for age and gender, using WHO standards. 11 , 12
-
Infant Neurodevelopment:
The infant's or child's primary caregiver was asked to complete a structured age‐appropriate Ages and Stages Questionnaire (ASQ), 13 reporting five domains of development (communication, gross motor, fine motor, problem‐solving, and personal‐social skills), with possible responses including Yes, Sometimes, or No. A score in any one domain more than two SD below the mean was considered indicative of the need for further assessment and when identified, the primary caregiver was advised to seek additional medical advice. The ASQ has been validated against the Bayley Scales, 14 and in a paediatric population. 15
-
Infant feeding, child dietary intake and behaviour:
Six months: (breastfeeding, formula, or a combination of the two), as assessed by a questionnaire completed by the infant's primary caregiver.
18 months based on Growing Up in Australia: the Longitudinal Study of Australian Children 16 and three to five years: Child dietary intake, physical activity and sedentary behaviour, as in our previous studies, 7 , 8 and included duration of breast or formula feeding; introduction of solid foods; the number of servings of fruits, vegetables, and milk consumed daily; the consumption of red meat and processed meats per week; and consumption of non‐core foods, including salty snacks, fried potatoes, takeaway foods, soft drinks and other “extra” foods. 16 Caregivers were asked to estimate the hours per week spent playing outdoors, screen time and other sedentary behaviours, duration of overnight sleeping, and daytime sleeping. 16
Family food behaviours included whether family meals were eaten together, preparation of different meals for children, use of food to encourage behaviours, and use of a bottle at bedtime. 16
Three to five years: Caregivers were asked to complete the Child Eating Behaviour Questionnaire (CEBQ) to assess their child's enjoyment of food, emotional overeating, emotional undereating, satiety responsiveness, slowness in eating, desire to drink, food fussiness and food responsiveness. 17
2.2. Sample size
The sample size for the follow‐up assessments, done at three‐time points was fixed by the number of eligible women and infant pairs from the original GRoW trial, which was not designed or powered to detect differences in offspring outcomes. In the original GRoW trial, 524 women were randomized (261 metformin; 263 placebos) and 514 women‐infant pairs were included in the analysis (nine women experienced miscarriage or stillbirth, and one woman withdrew from the trial). One mother‐infant pair included in the original analysis was not eligible for follow‐up due to neonatal death. This resulted in 513 mother‐infant pairs (255 metformin; 258 placebos) eligible for follow‐up assessments.
The proportion of children three to five years old with BMI z‐score > 85th percentile in the Lifestyle Advice group of the LIMIT study (women with BMI ≥25.0 kg/m2 who received an antenatal diet and lifestyle intervention, 7 who were thus comparable with the Placebo group of the GRoW study) was 42%. With 513 children, there is 80% power (with a two‐sided alpha of 0.05) to detect an absolute reduction of 17% (from 42% to 25%) in the proportion of children with BMI z‐score > 85th percentile in the Metformin group compared with the Placebo group. For secondary continuous outcomes, the sample size of 513 children provides 80% power (with a two‐sided alpha of 0.05) to detect differences in means between the Metformin and Placebo groups of approximately 0.24 standard deviation (SD).
2.3. Statistical analysis
Data were analysed using intention to treat principles, according to the treatment group to which the woman was randomized in pregnancy. Missing data for anthropometric outcomes were imputed using the fully conditional specification (chained equations) method with data in wide form (one row per child, with repeated measures represented as separate variables). All imputation models included study centre, parity, maternal early pregnancy BMI (as a continuous measure), maternal age at trial entry, smoking status and quintile of relative socio‐economic disadvantage. Imputation models for outcomes other than z‐scores also included child sex and actual age at follow‐up assessment. Birth measures were included where appropriate as auxiliary variables, as well as earlier and/or later measures of each outcome. Imputation was performed with Stata Version 17. Imputed data were analysed using appropriate methods, with effects estimated for each imputation and then combined using Rubin's Rules. Child diet, sleep and behaviour outcomes were analysed using available data only, as there was no information available to enable sensible imputation for these outcomes.
Binary outcomes were analysed using log‐binomial regression (or log Poisson regression with robust variance in the case of convergence problems), and continuous outcomes were analysed using linear regression. All models for outcomes measured at multiple time points included a time‐by‐treatment interaction term to test for differential treatment effects across time, and Generalized Estimating Equations were used to account for correlation due to repeated measures. Separate estimates for each time point were derived, regardless of the significance of the interaction term. Estimates for binary outcomes are relative risks and 95% confidence intervals (Metformin vs. Placebo) at each time point, while estimates for continuous outcomes are differences in means (Metformin–Placebo) at each time point.
Both unadjusted and adjusted analyses were performed. Adjusted models included study centre, parity, maternal early pregnancy BMI, age at trial entry, smoking status and quintile of a relative socioeconomic disadvantage as covariates. Child outcomes other than z‐scores also included child sex and actual age at follow‐up.
Prespecified sensitivity analyses were carried out to test the robustness of the results to violations of the assumptions used in the main imputation model. Firstly, a complete case analysis (using only available data) was performed. Secondly, the primary outcome was re‐imputed under a range of Missing Not At Random (MNAR) assumptions: that having a BMI z‐score >85th percentile was (a) 1.5 times as likely, (b) 2 times as likely, (c) 0.66 times as likely, or (d) 0.5 times as likely as in the observed data, in one or both treatment groups. Secondly, the imputation of repeated‐measures outcomes was re‐performed using the ‘FCS‐jomo’ (a Fully Conditional Specification implementation of the Joint Multivariate‐Normal method for clustered data) method, which was specifically designed for longitudinal or clustered data.
3. RESULTS
There were 513 eligible children contributing data to the analyses (Figure 1). In total, 426 children (Metformin group n = 216; Placebo group n = 210) were assessed at six months of age; 382 children (Metformin group n = 195; Placebo group n = 187) at 18 months of age; and 304 children (Metformin group n = 157; Placebo group n = 147) at three to five years of age. This represents 83%, 74% and 59% of eligible children respectively. Baseline characteristics at the trial entry of women with infants and children included in this analysis were similar between treatment groups and similar to all women randomized into the study (Table 1).
FIGURE 1.
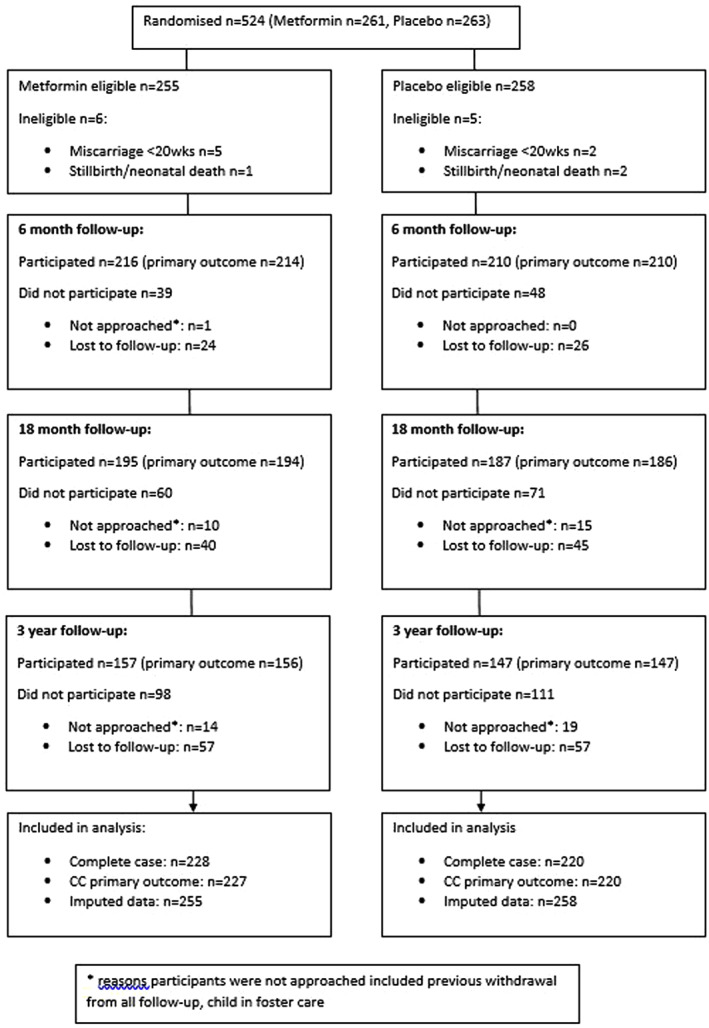
Participant flow at follow‐up assessments
TABLE 1.
Baseline maternal characteristics include all eligible randomized women and children who participated in any of the follow‐up studies
| Characteristic | Metformin n = 228 n (%) | Placebo n = 220 n (%) | Overall n = 448 n (%) |
|---|---|---|---|
| Maternal age years at trial entry a | 30.02 (5.51) | 30.21 (5.44) | 30.12 (5.47) |
| Study centre | |||
| WCH | 98 (42.98) | 93 (42.27) | 191 (42.63) |
| LMH | 105 (46.05) | 107 (48.64) | 212 (47.32) |
| FMC | 25 (10.96) | 20 (9.09) | 45 (10.04) |
| Primiparous at trial entry | 78 (34.21) | 81 (36.82) | 159 (35.49) |
| BMI (kg/m2) at trial entry b | 32.60 (28.68, 37.58) | 32.30 (29.17, 36.80) | 32.40 (28.90, 37.30) |
| BMI category | |||
| 25.0–29.9 | 74 (32.46) | 67 (30.45) | 141 (31.47) |
| 30.0–34.9 | 68 (29.82) | 75 (34.09) | 143 (31.92) |
| 35.0–39.9 | 50 (21.93) | 41 (18.64) | 91 (20.31) |
| 40.0+ | 36 (15.79) | 37 (16.82) | 73 (16.29) |
| Weight (kg) at trial entry a | 92.67 (19.54) | 91.98 (19.64) | 92.33 (19.57) |
| Height (cm) at trial entry a | 165.16 (6.86) | 164.85 (6.74) | 165.01 (6.79) |
| Smoking | |||
| No | 209 (91.67) | 186 (84.55) | 395 (88.17) |
| Yes | 18 (7.89) | 30 (13.64) | 48 (10.71) |
| Missing | 1 (0.44) | 4 (1.82) | 5 (1.12) |
| Ethnicity | |||
| Caucasian | 188 (82.46) | 189 (85.91) | 377 (84.15) |
| Asian | 4 (1.75) | 6 (2.73) | 10 (2.23) |
| Aboriginal/TSI | 6 (2.63) | 7 (3.18) | 13 (2.90) |
| Indian/Pak/Sri Lankan | 10 (4.39) | 6 (2.73) | 16 (3.57) |
| African | 6 (2.63) | 0 (0.00) | 6 (1.34) |
| Unknown | 4 (1.75) | 4 (1.82) | 8 (1.79) |
| Other | 10 (4.39) | 8 (3.64) | 18 (4.02) |
| IRSD c Quintile | |||
| Q1 (Most Disadvantaged) | 68 (29.82) | 76 (34.55) | 144 (32.14) |
| Q2 | 68 (29.82) | 66 (30.00) | 134 (29.91) |
| Q3 | 27 (11.84) | 25 (11.36) | 52 (11.61) |
| Q4 | 46 (20.18) | 40 (18.18) | 86 (19.20) |
| Q5 (Least Disadvantaged) | 19 (8.33) | 13 (5.91) | 32 (7.14) |
| Infant/child Sex | |||
| Male | 120 (52.63) | 131 (59.55) | 251 (56.03) |
| Female | 108 (47.37) | 89 (40.45) | 197 (43.97) |
| Age 6‐month follow‐up assessment b | 7.13 (6.44, 7.86) | 7.00 (6.34, 7.59) | 7.06 (6.37, 7.72) |
| Age 18‐month follow‐up assessment b | 19.18 (18.62, 19.92) | 19.15 (18.54, 19.84) | 19.16 (18.62, 19.87) |
| Age 3‐year follow‐up assessment b | 36.85 (35.99, 38.98) | 36.98 (35.93, 39.13) | 36.88 (35.96, 39.02) |
Mean and standard deviation.
Median and interquartile range.
Socioeconomic index as measured by SEIFA Index of Relative Socio‐economic Disadvantage (IRSD).
Child BMI z‐score > 85th centile was similar for children born to women who received metformin compared with women who received placebo at all of the time points measured, and the effect of treatment did not differ over time (Table 2). In both groups, the proportion of children with BMI z‐score > 85th centile increased over time from approximately one‐third of infants at six months of age, to at least half of children at 18 months, and three to five years of age.
TABLE 2.
Child anthropometry outcomes at 6 months, 18 months and 3‐year follow‐up with time by intervention interaction term, unadjusted and adjusted treatment estimates
| Outcome | Metformin | Placebo | Unadjusted estimate (95% CI) | Unadjusted p | Adjusted estimate (95% CI) c | Adjusted p |
|---|---|---|---|---|---|---|
| BMI z‐score >85th Percentile a | 0.634* | 0.634* | ||||
| 6 Months | 0.33 (0.27, 0.40) | 0.28 (0.22, 0.34) | 1.19 (0.90, 1.59) | 0.223 | 1.19 (0.89, 1.58) | 0.236 |
| 18 Months | 0.56 (0.49, 0.63) | 0.52 (0.45, 0.59) | 1.08 (0.90, 1.31) | 0.400 | 1.08 (0.89, 1.31) | 0.426 |
| 3 Years | 0.50 (0.43, 0.58) | 0.49 (0.41, 0.57) | 1.03 (0.83, 1.28) | 0.795 | 1.03 (0.83, 1.27) | 0.822 |
| BMI z‐score >90th Percentile a | 0.160* | 0.160* | ||||
| 6 Months | 0.27 (0.21, 0.33) | 0.20 (0.15, 0.26) | 1.34 (0.95, 1.89) | 0.093 | 1.34 (0.95, 1.89) | 0.098 |
| 18 Months | 0.44 (0.37, 0.51) | 0.44 (0.37, 0.51) | 0.99 (0.79, 1.24) | 0.920 | 0.99 (0.78, 1.24) | 0.907 |
| 3 Years | 0.39 (0.31, 0.46) | 0.40 (0.33, 0.48) | 0.96 (0.73, 1.25) | 0.740 | 0.95 (0.73, 1.25) | 0.729 |
| Weight z‐score >85th Percentile a | 0.398* | 0.398* | ||||
| 6 Months | 0.29 (0.23, 0.35) | 0.24 (0.19, 0.30) | 1.18 (0.86, 1.63) | 0.301 | 1.18 (0.85, 1.62) | 0.321 |
| 18 Months | 0.46 (0.39, 0.53) | 0.46 (0.39, 0.53) | 1.00 (0.80, 1.24) | 0.972 | 0.99 (0.80, 1.23) | 0.933 |
| 3 Years | 0.38 (0.31, 0.45) | 0.41 (0.34, 0.49) | 0.93 (0.72, 1.21) | 0.592 | 0.93 (0.72, 1.20) | 0.560 |
| Weight z‐score >90th Percentile a | 0.182* | 0.182* | ||||
| 6 Months | 0.22 (0.17, 0.28) | 0.16 (0.11, 0.20) | 1.42 (0.95, 2.13) | 0.085 | 1.43 (0.96, 2.15) | 0.082 |
| 18 Months | 0.34 (0.27, 0.41) | 0.34 (0.27, 0.41) | 1.00 (0.76, 1.32) | 0.984 | 1.01 (0.76, 1.33) | 0.950 |
| 3 Years | 0.29 (0.23, 0.35) | 0.29 (0.22, 0.36) | 1.00 (0.72, 1.39) | 0.991 | 1.01 (0.73, 1.39) | 0.962 |
| Weight (kg) b , d | 0.084* | 0.117* | ||||
| 6 Months | 8.56 (8.40, 8.72) | 8.31 (8.15, 8.48) | 0.25 (0.02, 0.48) | 0.033 | 0.22 (−0.00, 0.44) | 0.051 |
| 18 Months | 12.25 (12.06, 12.44) | 12.21 (11.98, 12.44) | 0.04 (−0.26, 0.33) | 0.807 | 0.06 (−0.23, 0.35) | 0.672 |
| 3 Years | 16.10 (15.75, 16.45) | 16.36 (15.96, 16.76) | −0.26 (−0.78, 0.27) | 0.337 | −0.24 (−0.74, 0.26) | 0.345 |
| Length (cm) b , d | 0.667* | 0.888* | ||||
| 6 Months | 69.05 (68.62, 69.49) | 68.45 (68.02, 68.89) | 0.60 (−0.01, 1.21) | 0.053 | 0.53 (−0.00, 1.06) | 0.052 |
| 18 Months | 83.72 (83.24, 84.20) | 83.40 (82.85, 83.95) | 0.32 (−0.40, 1.05) | 0.385 | 0.42 (−0.25, 1.10) | 0.220 |
| 3 Years | 97.42 (96.72, 98.11) | 97.13 (96.41, 97.84) | 0.29 (−0.67, 1.25) | 0.554 | 0.36 (−0.49, 1.20) | 0.411 |
| Head Circumference (cm) b , d | 0.418* | 0.476* | ||||
| 6 Months | 44.32 (44.11, 44.53) | 44.12 (43.90, 44.33) | 0.20 (−0.09, 0.50) | 0.175 | 0.28 (0.02, 0.55) | 0.037 |
| 18 Months | 48.20 (47.98, 48.41) | 48.12 (47.88, 48.36) | 0.07 (−0.25, 0.40) | 0.649 | 0.18 (−0.12, 0.48) | 0.245 |
| 3 Years | 50.10 (49.85, 50.35) | 50.11 (49.84, 50.38) | −0.01 (−0.37, 0.35) | 0.965 | 0.09 (−0.26, 0.44) | 0.618 |
| Abdomen Circumference (cm) b , d | 0.053* | 0.066* | ||||
| 6 Months | 46.71 (46.25, 47.17) | 46.06 (45.53, 46.58) | 0.65 (−0.04, 1.34) | 0.064 | 0.61 (−0.07, 1.30) | 0.079 |
| 18 Months | 49.51 (49.01, 50.00) | 49.65 (49.09, 50.21) | −0.14 (−0.88, 0.60) | 0.708 | −0.12 (−0.85, 0.61) | 0.746 |
| 3 Years | 52.00 (51.38, 52.62) | 52.52 (51.77, 53.26) | −0.51 (−1.50, 0.47) | 0.306 | −0.51 (−1.48, 0.46) | 0.306 |
| Chest Circumference (cm) b , d | 0.143* | 0.180* | ||||
| 6 Months | 45.62 (45.30, 45.94) | 45.26 (44.88, 45.65) | 0.35 (−0.14, 0.85) | 0.163 | 0.38 (−0.11, 0.86) | 0.132 |
| 18 Months | 50.01 (49.66, 50.37) | 50.06 (49.65, 50.47) | −0.04 (−0.59, 0.50) | 0.875 | 0.03 (−0.51, 0.57) | 0.908 |
| 3 Years | 53.01 (52.53, 53.48) | 53.33 (52.79, 53.86) | −0.32 (−1.03, 0.39) | 0.373 | −0.26 (−0.93, 0.42) | 0.453 |
| Arm Circumference (cm) b , d | 0.012* | 0.013* | ||||
| 6 Months | 15.41 (15.24, 15.59) | 15.04 (14.85, 15.24) | 0.37 (0.11, 0.63) | 0.006 | 0.37 (0.11, 0.63) | 0.005 |
| 18 Months | 16.45 (16.28, 16.63) | 16.33 (16.13, 16.54) | 0.12 (−0.15, 0.39) | 0.380 | 0.14 (−0.13, 0.41) | 0.294 |
| 3 Years | 17.10 (16.89, 17.31) | 17.28 (17.00, 17.56) | −0.18 (−0.53, 0.17) | 0.308 | −0.16 (−0.50, 0.18) | 0.346 |
| Biceps Skin Fold (mm) b , d | 0.362* | 0.368* | ||||
| 6 Months | 7.03 (6.75, 7.32) | 7.05 (6.76, 7.33) | −0.01 (−0.42, 0.39) | 0.949 | −0.01 (−0.42, 0.39) | 0.951 |
| 18 Months | 6.65 (6.39, 6.91) | 6.80 (6.51, 7.08) | −0.14 (−0.51, 0.23) | 0.445 | −0.14 (−0.51, 0.24) | 0.470 |
| 3 Years | 6.95 (6.55, 7.35) | 7.42 (7.00, 7.84) | −0.47 (−1.04, 0.09) | 0.100 | −0.47 (−1.04, 0.10) | 0.107 |
| Triceps Skin Fold (mm) b , d | 0.178* | 0.177* | ||||
| 6 Months | 11.82 (11.43, 12.20) | 11.43 (11.05, 11.82) | 0.38 (−0.15, 0.91) | 0.161 | 0.34 (−0.20, 0.87) | 0.218 |
| 18 Months | 11.97 (11.49, 12.45) | 12.07 (11.66, 12.48) | −0.09 (−0.73, 0.54) | 0.771 | −0.14 (−0.77, 0.49) | 0.662 |
| 3 Years | 11.61 (11.08, 12.15) | 11.99 (11.39, 12.59) | −0.38 (−1.18, 0.43) | 0.357 | −0.42 (−1.23, 0.39) | 0.304 |
| Subscap Skin Fold (mm) b , d | 0.576* | 0.573* | ||||
| 6 Months | 7.45 (7.22, 7.69) | 7.42 (7.15, 7.69) | 0.03 (−0.33, 0.39) | 0.853 | −0.00 (−0.37, 0.37) | 0.992 |
| 18 Months | 7.03 (6.74, 7.32) | 7.03 (6.71, 7.36) | −0.01 (−0.45, 0.44) | 0.978 | −0.04 (−0.49, 0.40) | 0.846 |
| 3 Years | 6.81 (6.47, 7.15) | 7.10 (6.58, 7.63) | −0.29 (−0.94, 0.35) | 0.371 | −0.33 (−0.97, 0.31) | 0.307 |
| Supra Skin Fold (mm) b , d | 0.486* | 0.513* | ||||
| 6 Months | 8.29 (7.95, 8.64) | 7.90 (7.50, 8.29) | 0.40 (−0.14, 0.93) | 0.148 | 0.31 (−0.23, 0.85) | 0.254 |
| 18 Months | 7.56 (7.16, 7.95) | 7.53 (7.12, 7.93) | 0.03 (−0.53, 0.59) | 0.916 | −0.04 (−0.60, 0.53) | 0.896 |
| 3 Years | 8.22 (7.53, 8.91) | 8.29 (7.51, 9.08) | −0.07 (−1.14, 1.00) | 0.892 | −0.15 (−1.21, 0.91) | 0.787 |
| Abdomen Skin Fold (mm) b , d | 0.133* | 0.141* | ||||
| 6 Months | 9.12 (8.77, 9.46) | 8.87 (8.52, 9.21) | 0.25 (−0.24, 0.74) | 0.323 | 0.15 (−0.34, 0.65) | 0.544 |
| 18 Months | 8.23 (7.83, 8.63) | 8.38 (7.95, 8.80) | −0.15 (−0.72, 0.42) | 0.600 | −0.23 (−0.81, 0.34) | 0.426 |
| 3 Years | 8.81 (8.30, 9.32) | 9.36 (8.73, 9.99) | −0.55 (−1.37, 0.27) | 0.191 | −0.63 (−1.45, 0.18) | 0.129 |
| Thigh Skin Fold (mm) b , d | 0.508* | 0.497* | ||||
| 6 Months | 19.79 (19.27, 20.30) | 19.19 (18.64, 19.73) | 0.60 (−0.15, 1.35) | 0.118 | 0.52 (−0.22, 1.27) | 0.170 |
| 18 Months | 16.34 (15.77, 16.90) | 16.05 (15.46, 16.65) | 0.28 (−0.54, 1.10) | 0.501 | 0.19 (−0.63, 1.02) | 0.643 |
| 3 Years | 15.63 (14.76, 16.49) | 15.78 (14.85, 16.71) | −0.15 (−1.42, 1.12) | 0.815 | −0.24 (−1.50, 1.03) | 0.714 |
| BMI (kg/m2) b , d | 0.040* | 0.041* | ||||
| 6 Months | 17.92 (17.67, 18.17) | 17.69 (17.45, 17.94) | 0.23 (−0.12, 0.58) | 0.200 | 0.23 (−0.12, 0.58) | 0.200 |
| 18 Months | 17.46 (17.25, 17.67) | 17.52 (17.24, 17.79) | −0.05 (−0.39, 0.28) | 0.754 | −0.05 (−0.39, 0.29) | 0.770 |
| 3 Years | 16.93 (16.70, 17.16) | 17.23 (16.91, 17.55) | −0.30 (−0.69, 0.09) | 0.128 | −0.30 (−0.69, 0.09) | 0.134 |
| Weight for Length ratio b , d | 0.041* | 0.047* | ||||
| 6 Months | 0.12 (0.12, 0.13) | 0.12 (0.12, 0.12) | 0.00 (−0.00, 0.01) | 0.054 | 0.00 (−0.00, 0.01) | 0.061 |
| 18 Months | 0.15 (0.14, 0.15) | 0.15 (0.14, 0.15) | 0.00 (−0.00, 0.00) | 0.914 | 0.00 (−0.00, 0.00) | 0.809 |
| 3 Years | 0.16 (0.16, 0.17) | 0.17 (0.16, 0.17) | −0.00 (−0.01, 0.00) | 0.254 | −0.00 (−0.01, 0.00) | 0.260 |
| Sum of Skin Fold Thickness Measures (mm) b , d | 0.263* | 0.264* | ||||
| 6 Months | 63.38 (61.62, 65.13) | 61.78 (59.98, 63.59) | 1.59 (−0.95, 4.14) | 0.221 | 1.28 (−1.30, 3.85) | 0.331 |
| 18 Months | 57.74 (55.73, 59.75) | 57.73 (55.75, 59.70) | 0.02 (−2.79, 2.82) | 0.992 | −0.29 (−3.14, 2.57) | 0.844 |
| 3 Years | 58.02 (54.87, 61.17) | 59.98 (56.58, 63.37) | −1.95 (−6.26, 2.35) | 0.373 | −2.26 (−6.56, 2.04) | 0.303 |
| Fat Free Mass (kg) b , d | 0.120* | 0.166* | ||||
| 6 Months | 6.06 (5.90, 6.23) | 6.02 (5.84, 6.20) | 0.04 (−0.21, 0.29) | 0.746 | 0.06 (−0.18, 0.30) | 0.618 |
| 18 Months | 9.04 (8.74, 9.34) | 9.17 (8.88, 9.46) | −0.13 (−0.54, 0.28) | 0.535 | −0.06 (−0.45, 0.34) | 0.776 |
| 3 Years | 11.82 (11.41, 12.23) | 12.38 (11.94, 12.82) | −0.56 (−1.16, 0.03) | 0.063 | −0.50 (−1.07, 0.07) | 0.086 |
| Fat Mass (kg) b , d | 0.774* | 0.756* | ||||
| 6 Months | 2.54 (2.37, 2.70) | 2.36 (2.18, 2.54) | 0.18 (−0.06, 0.42) | 0.149 | 0.13 (−0.12, 0.37) | 0.317 |
| 18 Months | 3.22 (2.98, 3.46) | 2.91 (2.62, 3.20) | 0.31 (−0.04, 0.65) | 0.080 | 0.26 (−0.08, 0.61) | 0.137 |
| 3 Years | 4.26 (3.96, 4.56) | 4.12 (3.71, 4.52) | 0.14 (−0.36, 0.64) | 0.582 | 0.10 (−0.41, 0.60) | 0.706 |
| Percentage Fat Mass b , d | 0.813* | 0.825* | ||||
| 6 Months | 29.46 (27.95, 30.97) | 28.03 (26.38, 29.68) | 1.43 (−0.78, 3.64) | 0.205 | 1.10 (−1.10, 3.30) | 0.327 |
| 18 Months | 26.34 (24.62, 28.06) | 23.88 (21.92, 25.85) | 2.46 (−0.13, 5.04) | 0.063 | 2.08 (−0.48, 4.64) | 0.111 |
| 3 Years | 26.35 (24.79, 27.90) | 24.72 (23.17, 26.28) | 1.63 (−0.41, 3.67) | 0.118 | 1.26 (−0.79, 3.31) | 0.230 |
| Length z‐score b | 0.413* | 0.410* | ||||
| 6 Months | 0.18 (0.03, 0.33) | −0.02 (−0.19, 0.16) | 0.20 (−0.03, 0.43) | 0.094 | 0.18 (−0.05, 0.42) | 0.127 |
| 18 Months | 0.26 (0.11, 0.41) | 0.14 (−0.04, 0.33) | 0.12 (−0.12, 0.36) | 0.326 | 0.10 (−0.14, 0.34) | 0.398 |
| 3 Years | 0.10 (−0.05, 0.26) | 0.05 (−0.11, 0.21) | 0.05 (−0.17, 0.28) | 0.647 | 0.04 (−0.19, 0.26) | 0.751 |
| Weight z‐score b | 0.003* | 0.004* | ||||
| 6 Months | 0.46 (0.33, 0.60) | 0.19 (0.03, 0.36) | 0.27 (0.06, 0.48) | 0.012 | 0.25 (0.04, 0.46) | 0.021 |
| 18 Months | 0.93 (0.81, 1.06) | 0.84 (0.68, 1.00) | 0.09 (−0.10, 0.29) | 0.348 | 0.08 (−0.12, 0.28) | 0.444 |
| 3 Years | 0.75 (0.61, 0.89) | 0.83 (0.66, 1.01) | −0.08 (−0.31, 0.14) | 0.462 | −0.10 (−0.32, 0.12) | 0.371 |
| Weight for Length z‐score b | 0.022* | 0.023* | ||||
| 6 Months | 0.58 (0.42, 0.74) | 0.39 (0.22, 0.55) | 0.19 (−0.04, 0.42) | 0.098 | 0.17 (−0.06, 0.40) | 0.144 |
| 18 Months | 1.06 (0.92, 1.19) | 1.02 (0.85, 1.19) | 0.05 (−0.16, 0.26) | 0.654 | 0.03 (−0.18, 0.25) | 0.770 |
| 3 Years | 1.01 (0.84, 1.18) | 1.20 (1.00, 1.41) | −0.19 (−0.46, 0.07) | 0.156 | −0.21 (−0.47, 0.06) | 0.121 |
| BMI z‐score b | 0.026* | 0.028* | ||||
| 6 Months | 0.49 (0.32, 0.65) | 0.29 (0.13, 0.45) | 0.20 (−0.03, 0.43) | 0.096 | 0.18 (−0.05, 0.41) | 0.125 |
| 18 Months | 1.11 (0.97, 1.24) | 1.08 (0.90, 1.26) | 0.03 (−0.20, 0.26) | 0.808 | 0.02 (−0.21, 0.25) | 0.876 |
| 3 Years | 1.02 (0.87, 1.17) | 1.19 (0.99, 1.39) | −0.17 (−0.43, 0.08) | 0.189 | −0.18 (−0.44, 0.07) | 0.160 |
| Head Circumference z‐score b | 0.406* | 0.395* | ||||
| 6 Months | 0.63 (0.48, 0.77) | 0.48 (0.33, 0.63) | 0.15 (−0.06, 0.36) | 0.158 | 0.16 (−0.05, 0.36) | 0.140 |
| 18 Months | 0.82 (0.67, 0.97) | 0.73 (0.55, 0.90) | 0.09 (−0.14, 0.32) | 0.435 | 0.09 (−0.14, 0.32) | 0.421 |
| 3 Years | 0.64 (0.48, 0.80) | 0.63 (0.45, 0.81) | 0.01 (−0.23, 0.25) | 0.936 | 0.01 (−0.23, 0.25) | 0.918 |
| Systolic Blood Pressure b , d , e | 101.41 (99.76, 103.06) | 100.98 (98.78, 103.18) | 0.43 (−2.16, 3.02) | 0.746 | 0.91 (−1.74, 3.56) | 0.501 |
| Diastolic Blood Pressure b , d , e | 60.53 (58.86, 62.20) | 61.45 (59.12, 63.77) | −0.91 (−3.84, 2.01) | 0.540 | −0.66 (−3.60, 2.27) | 0.657 |
Binary outcome; descriptives are estimated proportion and 95% CI (combined across all imputations), and estimates are relative risk (95% CI), Metformin vs. Placebo. Adjusted models used log Poisson regression with robust variance estimation as the log‐binomial did not converge.
Continuous outcomes; descriptives are estimated means and 95% CI (combined across all imputations), and estimates are differences in means (95% CI), Metformin–Placebo.
All adjusted models included study centre, parity (0 vs. 1+), age, BMI, smoking status and quintile of relative socioeconomic disadvantage.
Adjusted model for this outcome included child sex and actual age at follow‐up in addition to other covariates.
Measured at 3‐year follow‐up only; analysed using linear regression models.
p value for test of treatment by time interaction.
There was a trend within the secondary anthropometric outcomes for six‐month‐old infants suggesting infants of women who received metformin were slightly heavier, but this was not maintained at subsequent time points assessed (Table 2). Weight, length and BMI z‐scores were similar between groups and almost all greater than zero, indicating the infants of women with overweight and obesity are larger than the reference populations 11 (Table 2).
All other anthropometric measurements were similar between the two treatment groups at all‐time points with the exception of the head and arm circumference of infants at six months of age, which were significantly larger in the infants of women who received metformin. These differences did not persist at 18 months, or three to five years of age (Table 2). Blood pressure, measured at the three to five year follow‐up assessment only, was similar between the two treatment groups (Table 2).
Parent completed ASQs at six months, 18 months and three to five years of age were similar between the Metformin and Placebo groups (Table 3), across all domains with the exception of gross motor function. Infants of women who received metformin had slightly higher scores at 18 months of age compared with infants of women who received a placebo (Table 3). Again this difference was not evident either at six months or at three to five years of age and is likely a spurious result due to the large number of comparisons made.
TABLE 3.
Child neurodevelopment and 6 months, 18 months and 3 years of age
| Outcome | Metformin | Placebo | Unadjusted estimate (95% CI) | Unadjusted p | Adjusted estimate (95% CI) c | Adjusted p |
|---|---|---|---|---|---|---|
| Ages & Stages in Communication b | 0.635* | 0.829* | ||||
| 6 Months | 51.17 (10.36) | 51.74 (8.87) | −0.64 (−2.54, 1.25) | 0.507 | −0.34 (−2.29, 1.60) | 0.728 |
| 18 Months | 41.87 (14.04) | 41.79 (14.59) | −0.04 (−2.95, 2.87) | 0.979 | 0.13 (−2.83, 3.08) | 0.934 |
| 3 Years | 50.17 (10.99) | 51.28 (9.66) | −1.50 (−3.82,0.82) | 0.205 | −0.85 (−3.24, 1.54) | 0.488 |
| Ages & Stages in Gross Motor b | 0.875* | 0.910* | ||||
| 6 Months | 48.05 (11.56) | 46.93 (11.60) | 1.07 (−1.22, 3.36) | 0.361 | 1.24 (−1.08, 3.56) | 0.295 |
| 18 Months | 57.64 (6.26) | 56.09 (8.47) | 1.66 (0.13, 3.19) | 0.033 | 1.71 (0.17, 3.24) | 0.029 |
| 3 Years | 55.36 (7.17) | 54.20 (9.48) | 1.28 (−0.65,3.21) | 0.195 | 1.30 (−0.67, 3.27) | 0.197 |
| Ages & Stages in Fine Motor b | 0.970* | 0.951* | ||||
| 6 Months | 52.41 (9.71) | 51.54 (10.19) | 0.80 (−1.17, 2.77) | 0.427 | 0.76 (−1.26, 2.79) | 0.459 |
| 18 Months | 53.38 (7.45) | 52.77 (9.14) | 0.57 (−1.14, 2.29) | 0.512 | 0.56 (−1.20, 2.33) | 0.532 |
| 3 Years | 42.81 (15.12) | 42.59 (15.75) | 0.39 (−3.10,3.88) | 0.827 | 0.16 (−3.42, 3.75) | 0.929 |
| Ages & Stages in Problem Solving b | 0.464* | 0.584* | ||||
| 6 Months | 51.37 (9.74) | 51.90 (10.23) | −0.54 (−2.51, 1.43) | 0.593 | −0.40 (−2.45, 1.64) | 0.698 |
| 18 Months | 46.51 (10.32) | 45.75 (10.69) | 0.71 (−1.44, 2.85) | 0.519 | 0.82 (−1.40, 3.03) | 0.471 |
| 3 Years | 52.15 (10.11) | 51.42 (10.43) | 1.05 (−1.29,3.40) | 0.380 | 0.70 (−1.66, 3.07) | 0.560 |
| Ages & Stages in Personal Social b | 0.280* | 0.300* | ||||
| 6 Months | 49.01 (11.07) | 49.64 (11.10) | −0.58 (−2.78, 1.62) | 0.605 | −0.54 (−2.75, 1.68) | 0.636 |
| 18 Months | 50.00 (8.44) | 48.66 (9.84) | 1.33 (−0.54, 3.20) | 0.162 | 1.44 (−0.51, 3.38) | 0.148 |
| 3 Years | 51.69 (9.02) | 50.62 (9.60) | 1.26 (−0.86,3.38) | 0.245 | 1.07 (−1.11, 3.25) | 0.338 |
| Ages & Stages in Total Score b | 0.564* | 0.612* | ||||
| 6 Months | 252.01 (38.12) | 251.74 (39.60) | 0.01 (−7.66, 7.67) | 0.998 | 0.72 (−7.18, 8.62) | 0.859 |
| 18 Months | 249.40 (31.43) | 245.06 (37.41) | 4.22 (−2.73, 11.17) | 0.234 | 4.65 (−2.68, 11.97) | 0.214 |
| 3 Years | 252.19 (40.47) | 250.11 (42.53) | 2.91 (−6.41,12.24) | 0.540 | 2.39 (−7.32, 12.09) | 0.630 |
| Ages & Stages >1 Score Below Cutoff a | 0.591* | 0.620* | ||||
| 6 Months | 11/197 (5.58) | 12/192 (6.25) | 0.87 (0.40, 1.92) | 0.738 | 0.78 (0.34, 1.76) | 0.543 |
| 18 Months | 4/182 (2.20) | 9/179 (5.03) | 0.48 (0.16, 1.45) | 0.194 | 0.42 (0.14, 1.30) | 0.134 |
| 3 Years | 11/151 (7.28) | 16/137 (11.68) | 0.60 (0.28, 1.25) | 0.170 | 0.56 (0.27, 1.16) | 0.118 |
Binary outcome; descriptives are number and percentage, and estimates are relative risk (95% CI), Metformin vs. Placebo.
Continuous outcome; descriptives are mean and standard deviation, and estimates are difference in means (95% CI), Metformin–Placebo.
All adjusted models included study centre, parity, maternal age, early pregnancy BMI, smoking status and quintile of relative socioeconomic disadvantages as covariates.
p value for test of treatment by time interaction.
Breastfeeding occurrence and duration was similar for infants and children of women who received metformin compared with placebo (Table 4). The number of servings of fruit, vegetables and discretionary foods consumed was similar between treatment groups at 18 months and three to five years of age, as was the intake of energy and macronutrients (Table 4). Time spent outdoors and screen time were similar for infants and children across the two groups, at both 18 months, and three to five years of age (Table 4).
TABLE 4.
Child diet and behaviour
| Outcome | Metformin | Placebo | Unadjusted Estimate (95% CI) | Unadjusted p | Adjusted Estimate (95% CI) f | Adjusted p |
|---|---|---|---|---|---|---|
| Ever Breastfed a | 176/195 (90.26) | 176/190 (92.63) | 0.97 (0.79, 1.20) | 0.807 | 0.97 (0.78, 1.20) | 0.782 |
| Ever Given Infant Formula a | 134/181 (74.03) | 139/180 (77.22) | 0.96 (0.76, 1.22) | 0.728 | 0.95 (0.75, 1.21) | 0.692 |
| Breastfeeding Duration (mths) b | 8.96 (8.52) | 9.21 (8.35) | −0.25 (−2.02, 1.53) | 0.785 | −0.15 (−1.93, 1.63) | 0.869 |
| Serves Fruit/Day c , d | 0.781 | 0.628 | ||||
| 18 Months | N = 180 | N = 179 | ||||
| Does Not Eat | 2 (1.11) | 0 (0.00) | 1.15 (0.71, 1.86) | 0.574 | 1.05 (0.75, 1.72) | 0.842 |
| < 1/day | 7 (3.89) | 12 (6.70) | ||||
| 1/day | 32 (17.78) | 33 (18.44) | ||||
| 2+/day | 139 (77.22) | 134 (74.86) | ||||
| 3 Years | N = 146 | N = 137 | ||||
| Does Not Eat | 0 (0.00) | 3 (2.19) | 1.27 (0.77, 2.10) | 0.357 | 1.25 (0.75, 2.10) | 0.392 |
| < 1/day | 10 (6.85) | 9 (6.57) | ||||
| 1/day | 30 (20.55) | 32 (23.36) | ||||
| 2+/day | 106 (72.60) | 93 (67.88) | ||||
| Serves Vegetables/Day c , d | 0.757 | 0.920 | ||||
| 18 Months | N = 180 | N = 179 | ||||
| Does Not Eat | 1 (0.56) | 3 (1.68) | 0.87 (0.58, 1.29) | 0.482 | 0.83 (0.55, 1.25) | 0.369 |
| < 1/day | 18 (10.00) | 15 (8.38) | ||||
| 1/day | 63 (35.00) | 56 (31.28) | ||||
| 2+/day | 98 (54.44) | 105 (58.66) | ||||
| 3 Years | N = 146 | N = 137 | ||||
| Does Not Eat | 6 (4.11) | 11 (8.03) | 0.95 (0.61, 1.47) | 0.820 | 0.85 (0.55, 1.33) | 0.484 |
| < 1/day | 27 (18.49) | 18 (13.14) | ||||
| 1/day | 56 (38.36) | 52 (37.96) | ||||
| 2+/day | 57 (39.04) | 56 (40.88) | ||||
| Times/Week Extra Foods b , d | 0.992* | 0.986* | ||||
| 18mth | 6.70 (7.48) | 6.76 (6.58) | −0.06 (−1.51, 1.39) | 0.939 | 0.46 (−0.98, 1.91) | 0.529 |
| 3 yr | 11.83 (8.68) | 11.87 (7.79) | −0.05 (−1.96, 1.87) | 0.962 | 0.45 (−1.49, 2.38) | 0.652 |
| Hours/Week Outdoors b , d | 0.437* | 0.372* | ||||
| 18mth | 5.13 (3.43) | 4.71 (2.78) | 0.42 (−0.23, 1.06) | 0.204 | 0.55 (−0.13, 1.23) | 0.114 |
| 3 yr | 10.15 (7.51) | 10.44 (8.32) | −0.30 (−2.13, 1.54) | 0.753 | −0.28 (−2.19, 1.62) | 0.771 |
| Hours/Week Screen Time b , d | 0.164* | 0.170* | ||||
| 18mth | 0.50 (0.62) | 0.50 (0.77) | −0.00 (−0.15, 0.15) | 0.982 | −0.02 (−0.29, 0.25) | 0.901 |
| 3 yr | 9.84 (7.85) | 8.72 (5.65) | 1.12 (−0.45, 2.68) | 0.162 | 1.10 (−0.47, 2.67) | 0.168 |
| Total Energy (kJ) b , d , e | 4277.57 (1458.78) | 4351.41 (1484.86) | −73.85 (−418.38, 270.68) | 0.673 | 11.10 (−346.78, 368.98) | 0.951 |
| Total Fat (g) b , d , e | 35.27 (11.95) | 36.98 (14.25) | −1.71 (−4.78, 1.36) | 0.274 | −0.96 (−4.13, 2.20) | 0.548 |
| Fat as % Total Energy b , d , e | 31.16 (4.42) | 31.75 (3.92) | −0.58 (−1.56, 0.40) | 0.243 | −0.52 (−1.53, 0.50) | 0.314 |
| Saturated Fat (g) b , d , e | 15.48 (5.65) | 16.16 (6.97) | −0.68 (−2.16, 0.80) | 0.369 | −0.22 (−1.75, 1.31) | 0.776 |
| Fibre (g) b , d , e | 15.72 (6.87) | 15.49 (5.61) | 0.23 (−1.24, 1.71) | 0.755 | 0.20 (−1.34, 1.74) | 0.799 |
| Protein (g) b , d , e | 40.25 (13.70) | 41.80 (15.41) | −1.54 (−4.95, 1.87) | 0.374 | −1.05 (−4.54, 2.44) | 0.554 |
| Glycaemic Index b , d , e | 49.52 (3.91) | 49.19 (4.00) | 0.33 (−0.59, 1.26) | 0.482 | 0.32 (−0.63, 1.27) | 0.506 |
Binary outcome; descriptives are number and percentage, and estimates are relative risk (95% CI), Metformin vs. Placebo.
Continuous outcome; descriptives are mean and standard deviation, and estimates are difference in means (95% CI), Metformin–Placebo.
Ordinal outcome; descriptives are numbers and percentages in each category. Estimates are Odds Ratios (95% CI) from an ordinal logistic regression model and represent the relative odds of being in a lower‐ranked category vs. all higher‐ranked categories, in Metformin vs. Placebo, i.e., how much more likely children from the Metformin group are of being in a higher‐ranked category (lower consumption) compared to children from the Placebo group.
Adjusted model for this outcome included child sex and actual age at follow‐up in addition to other covariates.
Measured at 3‐year follow‐up only; analysed using linear regression models.
All adjusted models included study centre, parity, maternal age, early pregnancy BMI, smoking status and quintile of relative socioeconomic disadvantages as covariates.
p value for test of treatment by time interaction.
Eating behaviour as measured by the parent who completed CEBQ at three to five years of age was similar across both treatment groups for all domains except slowness of eating, where children of women who received metformin were assessed as slower at eating compared with children who received placebo (Table 5). The significance of this is unclear.
TABLE 5.
Child eating behaviour checklist
| Outcome | Metformin | Placebo | Unadjusted Estimate (95% CI) | Unadjusted p | Adjusted Estimate (95% CI) d | Adjusted p |
|---|---|---|---|---|---|---|
| CEBQ: Enjoyment of Food a , b , c | 3.59 (0.83) | 3.59 (0.89) | −0.00 (−0.20, 0.20) | 0.980 | −0.06 (−0.27, 0.14) | 0.546 |
| CEBQ: Emotional Over‐Eating a , b , c | 1.65 (0.60) | 1.66 (0.55) | −0.01 (−0.14, 0.13) | 0.892 | −0.03 (−0.17, 0.11) | 0.678 |
| CEBQ: Emotional Under‐Eating a , b , c | 2.97 (0.88) | 2.91 (0.96) | 0.06 (−0.16, 0.27) | 0.595 | 0.11 (−0.11, 0.34) | 0.313 |
| CEBQ: Satiety Responsiveness a , b , c | 3.14 (0.57) | 3.04 (0.59) | 0.10 (−0.04, 0.24) | 0.146 | 0.14 (0.00, 0.28) | 0.048 |
| CEBQ: Slowness in Eating a , b , c | 3.20 (0.67) | 3.04 (0.70) | 0.16 (−0.00, 0.32) | 0.051 | 0.19 (0.02, 0.36) | 0.025 |
| CEBQ: Desire to Drink a , b , c | 3.03 (1.05) | 2.86 (1.07) | 0.17 (−0.08, 0.42) | 0.173 | 0.20 (−0.06, 0.45) | 0.126 |
| CEBQ: Food Fussiness a , b , c | 3.08 (0.88) | 3.11 (1.00) | −0.03 (−0.25, 0.19) | 0.808 | 0.03 (−0.19, 0.25) | 0.795 |
| CEBQ: Food Responsiveness a , b , c | 2.41 (0.81) | 2.47 (0.81) | −0.06 (−0.25, 0.13) | 0.552 | −0.06 (−0.26, 0.13) | 0.515 |
Continuous outcome; descriptives are mean and standard deviation, and estimates are difference in means (95% CI), Metformin–Placebo.
Adjusted model for this outcome included child sex and actual age at follow‐up in addition to other covariates.
Measured at 3‐year follow‐up only; analysed using linear regression models.
All adjusted models included study centre, parity, maternal age, early pregnancy BMI, smoking status and quintile of relative socioeconomic disadvantages as covariates.
Results of sensitivity analyses were generally consistent with those of the main analysis. The estimates of treatment group comparisons in the raw data analysis, and for the primary outcome in the analysis of MNAR imputed data were consistent with the main analysis in all scenarios. The results of analyses on data imputed using ‘FCS‐jomo’ were likewise generally consistent with the results of the main imputation, but some of the statistically significant results for secondary outcomes at six months were not statistically significant in the FCS‐jomo imputed data (specifically head circumference, weight z‐score, and interaction p values).
4. DISCUSSION
We have previously reported that metformin as an adjuvant therapy to a dietary and lifestyle intervention reduced weekly gestational weight gain compared with a dietary and lifestyle intervention alone in pregnant women with overweight and obesity (GRoW). 2 This modest impact on gestational weight gain did not have an effect on the proportion of infants or children with BMI >85th centile when assessed at six months, 18 months, or three to five years of age. Furthermore, we demonstrated little evidence of an effect following metformin administration during pregnancy on secondary infant and child anthropometric measurements, neurodevelopment, dietary intake, physical activity or eating behaviours. Despite the lack of differences observed between treatment groups, this cohort of children remains at high risk of overweight and obesity, with approximately half of children assessed having BMI above the 85th centile for age and sex, a figure almost double that observed in the general Australian childhood population. 18
We are aware of several randomized trials, which have investigated the effect of metformin on women with overweight or obesity during pregnancy. 19 , 20 , 21 , 22 , 23 To our knowledge, two of these trials have conducted and reported follow‐up of child participants at approximately three to five years of age. 4 , 5 In both of these follow‐up studies, only a small proportion of eligible children were assessed (151 of 393 (40%) 4 and 40 of 170 (24%) 5 ). Three trials, not reporting follow‐up, report different stages of recruitment to a single trial, 21 , 22 , 23 with uncertainty regarding adjustment for interim analyses.
Yang and colleagues evaluated a small subset of children (40 in total) from the EMPOWaR randomized trial at approximately five years of age. 5 There were no statistically significant differences identified between children who were exposed in‐utero to metformin (n = 19) and those who were not (n = 21) with regards to anthropometric measures. Furthermore, there were no significant differences identified in measures of cardiovascular function including blood pressure, arterial pulse wave velocity and central haemodynamics. 5
In contrast, Panagiotopoulou and colleagues report findings from the follow‐up of 151 children at approximately four years of age, 77 of whom were exposed to metformin during in‐utero development and 77 who were exposed to placebo. 4 While hip circumference measures were smaller in children exposed to metformin compared with those who were not, there were no other statistically significant differences identified across a range of anthropometric measures, raising the possibility of a chance finding. Children exposed to metformin also demonstrated small differences with lower central hemodynamic and cardiac diastolic indices compared with children exposed to placebo. 4 While statistically significant, these differences were of small magnitude and uncertain clinical significance.
Metformin has been used in pregnancy for women with polycystic ovary syndrome 24 and gestational diabetes, 25 with both trials reporting follow‐up of children after birth. 3 , 26 , 27 , 28 Children born to women who participated in the PREGMET Study were followed up at six months, four years, and five to 10 years of age. 26 , 27 At all‐time points assessed, children exposed in‐utero to metformin had higher BMI z‐scores compared with children born to women who received placebo. 26 , 27
The MIG randomized trial‐compared metformin with insulin for the treatment of women with gestational diabetes. 25 Assessments at two years of age identified children exposed to metformin to had larger subscapular skinfold thickness and mid‐upper arm circumference measures. 28 While the majority of anthropometric measures at seven to nine years of age were not different between the children born to women who received metformin and those who received insulin, children exposed to metformin demonstrated higher body weight and BMI, with a suggestion of increased adiposity measured by dual‐energy x‐ray absorptiometry. 3
Despite differences in the identified follow‐up studies with regard to the initial target populations and the pregnancy intervention provided, the magnitude of the effect of metformin on childhood anthropometric measures assessed at a variety of time points, appears modest in nature. Furthermore, where studies have reported statistically significant differences in childhood skinfold thickness and body circumference measures; these are inconsistent in time and specific site of measurement, raising the possibility of spurious findings of limited clinical significance.
In the recent past, there has been considerable research on pregnancy dietary and lifestyle interventions to ameliorate the impact of overweight, obesity and excess gestational weight gain on pregnancy, birth and long‐term maternal and child outcomes. 29 Findings from the infant and child follow‐up studies of these interventional studies have shown no effect on child adiposity outcomes between infants and children exposed to intervention in‐utero and those who were not. 7 , 8 , 9 , 30 , 31 , 32 The findings of these studies and studies of metformin during pregnancy highlight the likelihood that pregnancy interventions do not reduce the risk of childhood obesity and that we should focus effort on interventions prior to conception.
There are a number of strengths to our study, which to date represents the largest, most extensive, and most complete follow‐up assessment of children who were exposed to metformin in‐utero, at three‐time points in early childhood. Our assessments included 426 (83% of those eligible) infants or children at six months, 382 (74% of those eligible) at 18 months, and 304 (59% of those eligible) at three to five years of age.
Our trial methodology was robust, with accurate measurement of early pregnancy weight, height, and BMI; detailed maternal dietary and physical activity history; and consistent provision of the dietary and lifestyle intervention to all participants. Our follow‐up methods have adhered to a research quality protocol, with a standardized assessment of anthropometric measures, and consistent evaluation of childhood diet, physical activity, sedentary behaviour and sleep patterns, all of which are well‐recognized early life factors contributing to childhood overweight and obesity. 33
Our study does have some limitations, including that the follow‐up study has a sample size fixed by the initial randomized controlled trial, which was not designed or powered to detect differences in child BMI >85th percentile. In addition, there is potential selection bias. A smaller proportion of the total eligible randomized cohort at each time point was assessed and contributed data. However, baseline and clinical characteristics of women and children for whom data were available and who participated in the follow‐up study were similar between the two randomized treatment groups at each assessment point, and similar to the full randomized GRoW cohort.
We have undertaken robust statistical methods and imputation models at each of the assessment time point to address issues related to missing data, including analyses through multiple imputations for all children eligible for three to five year follow‐up. The imputation models used were robust, and additionally incorporated data available from the six and 18‐month childhood assessments. We conducted sensitivity analyses using data imputed under a range of MNAR scenarios, with our results consistent under a variety of plausible assumptions about the magnitude and direction of the difference between missing and observed data. On this basis, we consider our findings robust and valid and do not consider the risk of bias to be significant.
The retrospective collection of dietary intake and habits reliant on recall of women for their children has some limitations; however, there is no reason to expect that the ability to recall would differ for women by treatment group. Whilst we would caution against accepting these data as absolute, we are confident that the between‐group comparisons are robust.
Our findings show no evidence of any beneficial effects of in‐utero exposure to metformin among infants and children born to women with overweight or obesity, at any of the time points assessed at follow‐up. While the intervention resulted in a modest reduction in weekly gestational weight gain for women who received metformin, there was no longer‐term impact on child risk of obesity. However, this group of children remains at more than double the Australian risk of overweight and obesity in early childhood. Intervention during pregnancy may be too late to change the growth trajectory to improve child health and obesity risk, with future studies required to consider interventions to improve the overall health and wellbeing of women prior to pregnancy.
AUTHOR CONTRIBUTIONS
Jodie M. Dodd conceptualized the study with input from Andrea R. Deussen and Jennie Louise. Jennie Louise performed the statistical analysis. All authors contributed to the interpretation of the results. Andrea R. Deussen wrote the first draft. All authors contributed to critical revisions, approve the final version of the manuscript and were responsible for the decision to submit it for publication. All authors had access to the underlying data. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
ACKNOWLEDGEMENTS
We are indebted to the 524 women who participated in the GRoW randomized trial, and to the parents and children who contributed to the outcome data at six and eighteen months and three to five years of age. The following persons in Adelaide, South Australia participated in the follow‐up of the GRoW trial: Co‐ordinating Team—JM Dodd, A Deussen, J Louise, A Newman, A Jacobssen, C Sheppard, L Greenham, J Peters, L Williams, E Lyrtzis. Open access publishing facilitated by The University of Adelaide, as part of the Wiley ‐ The University of Adelaide agreement via the Council of Australian University Librarians.
Deussen AR, Louise J, Dodd JM. Childhood follow‐up of the GRoW randomized trial: Metformin in addition to dietary and lifestyle advice for pregnant women with overweight or obesity. Pediatric Obesity. 2023;18(1):e12974. doi: 10.1111/ijpo.12974
Funding information National Health and Medical Research Council, Grant/Award Numbers: APP1043181, APP1159338, APP1196133
REFERENCES
- 1. Wiernsperger NF, Bailey CJ. The antihyperglycaemic effect of metformin: therapeutic and cellular mechanisms. Drugs. 1999;58(Suppl 1):31‐39; discussion 75–82. doi: 10.2165/00003495-199958001-00009 [DOI] [PubMed] [Google Scholar]
- 2. Dodd JM, Louise J, Deussen AR, et al. Effect of metformin in addition to dietary and lifestyle advice for pregnant women who are overweight or obese: the GRoW randomised, double‐blind, placebo‐controlled trial. Lancet Diabetes Endocrinol. 2019;7(1):15‐24. doi: 10.1016/S2213-8587(18)30310-3 [DOI] [PubMed] [Google Scholar]
- 3. Rowan JA, Rush EC, Plank LD, et al. Metformin in gestational diabetes: the offspring follow‐up (MiG TOFU): body composition and metabolic outcomes at 7‐9 years of age. BMJ Open Diabetes Res Care. 2018;6(1):e000456. doi: 10.1136/bmjdrc-2017-000456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Panagiotopoulou O, Syngelaki A, Georgiopoulos G, et al. Metformin use in obese mothers is associated with improved cardiovascular profile in the offspring. Am J Obstet Gynecol. 2020;223(2):246 e1‐246 e10. doi: 10.1016/j.ajog.2020.01.054 [DOI] [PubMed] [Google Scholar]
- 5. Yang L, Lacey L, Whyte S, et al. Metformin in obese pregnancy has no adverse effects on cardiovascular risk in early childhood. J Dev Orig Health Dis. 2021;13(3):390‐394. doi: 10.1017/S2040174421000301 [DOI] [PubMed] [Google Scholar]
- 6. Dodd JM, Grivell RM, Deussen AR, Dekker G, Louise J, Hague W. Metformin and dietary advice to improve insulin sensitivity and promote gestational restriction of weight among pregnant women who are overweight or obese: the GRoW Randomised Trial. BMC Pregnancy Childbirth. 2016;16(1):359. doi: 10.1186/s12884-016-1161-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dodd JM, Deussen AR, Louise J. Effects of an antenatal dietary intervention in women with obesity or overweight on child outcomes at 3‐5 years of age: LIMIT randomised trial follow‐up. Int J Obes (Lond). 2020;44(7):1531‐1535. doi: 10.1038/s41366-020-0560-4 [DOI] [PubMed] [Google Scholar]
- 8. Dodd JM, Louise J, Deussen AR, et al. Prenatal diet and child growth at 18 months. Pediatrics. 2018;142(3) pii::e20180035. doi: 10.1542/peds.2018-0035 Epub 2018 Aug 8. [DOI] [PubMed] [Google Scholar]
- 9. Dodd JM, McPhee AJ, Deussen AR, et al. Effects of an antenatal dietary intervention in overweight and obese women on 6 month infant outcomes: follow‐up from the LIMIT randomised trial. Int J Obes (Lond). 2018;42(7):1326‐1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marfell‐Jones M, Olds T, Stewart A, Carter L. International standards for anthropometric assessment. International Society for the Advancement of Kinanthropometry; 2006.
- 11. World Health Organization . WHO Child Growth Standards: Length/Height‐for‐Age, Weight‐for‐Age, Weight‐for‐Length, Weight‐for‐Height, and Body Mass Index‐for‐Age. Methods Development WHO; 2008. Accessed 16 October, 2008. http://www.who.int/childgrowth/standards/technical_report/en/index.html [Google Scholar]
- 12. Freeman JV, Cole TJ, Chinn S, Jones PR, White EM, Preece MA. Cross sectional stature and weight reference curves for the UK, 1990. Arch Dis Child. 1995;73:17‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bricker D, Squires J, Mounts L. Ages and Stages Questionnaire: 12 Month: A Parent Completed Child Monitoring System. Paul H Brookes Publishing Co; 1995. [Google Scholar]
- 14. Squires J, Potter L, Bricker D. The ASQ User's Guide for the Ages and Stages Questionnaires: A Parent‐Completed, Child‐Monitoring System. Paul H Brookes Publishing Company; 1995. [Google Scholar]
- 15. Skellern CY, Rogers Y, O'Callaghan MJ. A parent‐completed developmental questionnaire: follow up of ex‐premature infants. J Paediatr Child Health. 2001;37(2):125‐129. doi: 10.1046/j.1440-1754.2001.00604.x [DOI] [PubMed] [Google Scholar]
- 16. International standards for anthropometric assessment. The International Society for the Advancement of Kinanthropometry; 2006. Australian Institute of Family Studies . Growing Up in Australia: The Longitudinal Study of Australian Children. http://www.aifs.gov.au/growingup/ [Google Scholar]
- 17. Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the children's eating behaviour questionnaire. J Child Psychol Psychiatry. 2001;42(7):963‐970. [DOI] [PubMed] [Google Scholar]
- 18. Australian Institute of Family Studies . 2020. Overweight and Obesity: an Interactive Insight. Cat. no. PHE 251. Canberra: AIHW. Accessed July 4, 2022. https://www.aihw.gov.au/reports/overweight-obesity/overweight-and-obesity-an-interactive-insight/contents/prevalence [Google Scholar]
- 19. Chiswick C, Reynolds RM, Denison F, et al. Effect of metformin on maternal and fetal outcomes in obese pregnant women (EMPOWaR): a randomised, double‐blind, placebo‐controlled trial. Lancet Diabetes Endocrinol. 2015;3(10):778‐786. doi: 10.1016/S2213-8587(15)00219-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Syngelaki A, Nicolaides KH, Balani J, et al. Metformin versus Placebo in Obese Pregnant Women without Diabetes Mellitus. N Engl J Med. 2016;374(5):434‐443. doi: 10.1056/NEJMoa1509819 [DOI] [PubMed] [Google Scholar]
- 21. Dienstmann G, Nascimento IBD, Sales WB, et al. No effect of a low dose of metformin on the lipid profile, body mass index and weight gain in pregnant women with obesity: A randomized trial. Obes Res Clin Pract. 2020;14(6):561‐565. doi: 10.1016/j.orcp.2020.09.005 [DOI] [PubMed] [Google Scholar]
- 22. Nascimento IBD, Sales WB, Dienstmann G, Souza MLR, Fleig R, Silva JC. Metformin for prevention of cesarean delivery and large‐for‐gestational‐age newborns in non‐diabetic obese pregnant women: a randomized clinical trial. Arch Endocrinol Metab May‐Jun. 2020;64(3):290‐297. doi: 10.20945/2359-3997000000251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sales WB, Nascimento IBD, Dienstmann G, Souza MLR, Silva GDD, Silva JC. Effectiveness of metformin in the prevention of gestational diabetes mellitus in obese pregnant women. Rev Bras Ginecol Obstet. 2018;40(4):180‐187. doi: 10.1055/s-0038-1642632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vanky E, Stridsklev S, Heimstad R, et al. Metformin versus placebo from first trimester to delivery in polycystic ovary syndrome: a randomized, controlled multicenter study. J Clin Endocrinol Metab. 2010;95(12):E448‐E455. doi: 10.1210/jc.2010-0853 [DOI] [PubMed] [Google Scholar]
- 25. Rowan JA, Hague WM, Gao W, Battin MR, Moore MP, Mi GTI. Metformin versus insulin for the treatment of gestational diabetes. N Engl J Med. 2008;358(19):2003‐2015. doi: 10.1056/NEJMoa0707193 [DOI] [PubMed] [Google Scholar]
- 26. Hanem LGE, Salvesen O, Madsen A, et al. Maternal PCOS status and metformin in pregnancy: Steroid hormones in 5‐10 years old children from the PregMet randomized controlled study. PLoS One. 2021;16(9):e0257186. doi: 10.1371/journal.pone.0257186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hanem LGE, Stridsklev S, Juliusson PB, et al. Metformin Use in PCOS Pregnancies Increases the Risk of Offspring Overweight at 4 Years of Age: Follow‐Up of Two RCTs. J Clin Endocrinol Metab. 2018;103(4):1612‐1621. doi: 10.1210/jc.2017-02419 [DOI] [PubMed] [Google Scholar]
- 28. Rowan JA, Rush EC, Obolonkin V, Battin M, Wouldes T, Hague WM. Metformin in gestational diabetes: the offspring follow‐up (MiG TOFU): body composition at 2 years of age. Diabetes Care. 2011;34(10):2279‐2284. doi: 10.2337/dc11-0660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. International Weight Management in Pregnancy Collaborative G . Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: meta‐analysis of individual participant data from randomised trials. BMJ. 2017;358:j3119. doi: 10.1136/bmj.j3119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hoffmann J, Gunther J, Stecher L, et al. Infant growth during the first year of life following a pregnancy lifestyle intervention in routine care‐Findings from the cluster‐randomised GeliS trial. Pediatr Obes. 2021;16(2):e12705. doi: 10.1111/ijpo.12705 [DOI] [PubMed] [Google Scholar]
- 31. Louise J, Poprzeczny AJ, Deussen AR, et al. The effects of dietary and lifestyle interventions among pregnant women with overweight or obesity on early childhood outcomes: an individual participant data meta‐analysis from randomised trials. BMC Med. 2021;19(1):128. doi: 10.1186/s12916-021-01995-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sandborg J, Henriksson P, Soderstrom E, et al. The effects of a lifestyle intervention (the HealthyMoms app) during pregnancy on infant body composition: Secondary outcome analysis from a randomized controlled trial. Pediatr Obes. 2022;17(6):e12894. doi: 10.1111/ijpo.12894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Reilly JJ, Armstrong J, Dorosty AR, et al. Early life risk factors for obesity in childhood. BMJ. 2005;330:1357. [DOI] [PMC free article] [PubMed] [Google Scholar]


