Abstract
Background
Experiencing financial insecurity and being underserved is often associated with low health literacy, i.e., the ability to identify, obtain, interpret and act upon health information, which may result in poor health outcomes. Little is known about effective interventions for promoting health literacy among underserved populations. The objective of this systematic review is to summarize the literature on such interventions and identify characteristics that differentiate more effective interventions.
Methods
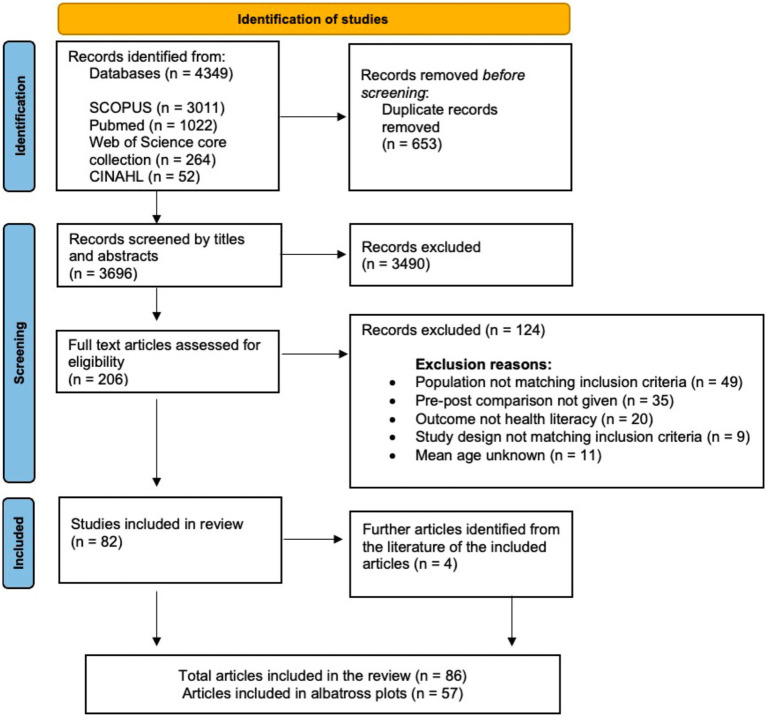
Following PRISMA guidelines we searched the databases SCOPUS, Pubmed, Web of Science core collection and CINAHL. We included primary studies with a quantitative study design and control groups testing interventions to increase health literacy or health knowledge in underserved populations between 18 and 65 years. Where possible, we converted effect sizes into Cohen’s d and compared mean differences of intervention and control groups. Albatross plots were created to summarize the results according to different health literacy and health knowledge outcomes.
Results
We screened 3,696 titles and abstracts and 206 full texts. In total, 86 articles were analyzed, of which 55 were summarized in seven albatross plots. The majority of the studies (n = 55) were conducted in the United States and had a randomized controlled study design (n = 44). More effective intervention approaches assessed needs of participants through focus group discussions prior to conducting the intervention, used bilingual educational materials, and included professionals fluent in the first languages of the study population as intervention deliverers. Additionally, the use of educational materials in video and text form, fotonovelas and interactive group education sessions with role playing exercises were observed to be effective.
Discussion
Although the outcomes addressed in the included studies were heterogeneous, effective intervention approaches were often culturally sensitive and developed tailored educational materials. Interventions aiming to promote health literacy in underserved populations should hence consider applying similar approaches.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=323801, PROSPERO registration ID: CRD42022323801.
Keywords: health literacy, socioeconomically disadvantaged, intervention strategies, multilingual education, face-to-face, albatross plots, systematic review
Introduction
Health literacy (HL) can be defined as a person’s “knowledge, motivation, and competences to access, understand, appraise and apply health information in order to make judgments and take decisions in everyday life concerning healthcare, disease prevention and health promotion” (1).
HL is an important resource when people engage with health-related information or the healthcare system. At the same time, low levels of HL are a risk factor for numerous health and health behavior outcomes. For example, individuals with low levels of HL suffer from higher mortality rates, have lower participation in cancer screening programs and show lower levels of preventive behaviors in general than those with higher HL (2–4).
Lower levels of HL are associated with difficulties taking medications as recommended [e.g., using non-standardized dosing tools (5), or recognizing all medications (6)]. Persons with low HL levels display more problems understanding health messages and more difficulties interpreting medication and nutrition labels (7–9).
This, however, does not necessarily imply individual deficits, but deficits in the way of how health-related information is presented or healthcare providers communicate (10).
HL levels are distributed unequally along social strata (11), and in particular population groups that face socioeconomic disadvantages1 are at high risk for low HL. This includes individuals with low educational attainment, unemployed people (see Footnote 1), people with a migration background, and in general people with a low socioeconomic status (12–15). In Europe, 74% of the group with a very low socioeconomic status show limited HL compared to 47% of the general population (11).
These studies indicate an urgent need to support and promote HL, especially in financially insecure and underserved populations. However, surprisingly little is known about effective interventions for promoting HL both in underserved populations and in general, and about potentially modifiable determinants of HL that could form the basis of interventions. A recent rapid review identified the following as potentially modifiable determinants of HL in working-age populations: providing accessible health information in digital and analog media, support in multiple and potentially simplified languages and health behaviors (16). However, it is not clear whether these strategies work with financially insecure and underserved populations.
There are several systematic reviews that summarize the effects of HL interventions on specific health outcomes or in specific populations (3, 17–19). However, there is a dearth of reviews on the effects of HL-focused interventions on actual HL outcomes (such as functional HL or mental health literacy). This is not only an academic issue, but crucial in order to understand which intervention features are most likely to promote HL. As HL is an important determinant of interactions with health services, health behaviors, and health outcomes (2–4), more knowledge on how to successfully intervene on HL is needed.
Although the definition of HL comprises the four dimensions accessing, understanding, appraising and applying health information, we also included health knowledge outcomes because this is a major part of HL and is decisive in implementing health promoting health behavior (20). This was highlighted during the COVID-19 pandemic, where health knowledge predicted protective behaviors, such as wearing masks, social distancing, and washing hands (21–23). Also, health knowledge might serve as a proxy for how well people access and understand health information.
This systematic review therefore aims to summarize existing interventions with the goal to identify effective strategies and techniques to promote HL (primary outcome) and health knowledge (secondary outcome) among working-age populations experiencing socioeconomic disadvantage.
The age group was chosen as we focused on people who could be potentially unemployed (in other words working-age populations) since under-employed people, unemployed people and especially long-term unemployed people often fulfill multiple risk factors for low HL such as financial insecurity, a migration history or limited literacy skills (24–26).
Methods
The systematic review was conducted in line with the PRISMA guidelines. The respective protocol was registered in May 2022 at PROSPERO (registration number: 323801).
Eligibility criteria and information sources
Four databases were searched in April 2022: SCOPUS (via Elsevier), Pubmed (via Ovid), Web of Science core collection and CINAHL (via EBSCO). The references of the included articles were searched for further relevant literature.
Inclusion criteria:
Quantitative study design including at least an intervention and a control group.
Primary or secondary outcome of the study has to be any kind of health literacy or health knowledge outcome.
Focusing on financially insecure and underserved working-age populations between 18 and 65 years including migrant populations (e.g., adults living in deprived areas, unemployed, low-income, poor, precarious employment status, undocumented legal status, low educational attainment, low literacy, low socioeconomic status).
Exclusion criteria:
Articles not reporting HL as an outcome.
Articles not published in English or German.
Articles not reporting any statistical tests or pre-and post-results.
Articles where the full-text could not be accessed.
Articles not reporting the mean age of participants (excluded from the main analysis, but included in sensitivity analysis).
Search strategy
As recommended for systematic reviews, we used the PICO approach (Among working-age populations experiencing socioeconomic disadvantage (P) which health literacy interventions (I) compared to other or no such interventions (C) are effectively improving any health literacy and/or health knowledge outcome (O)?). The following search and MESH terms were used: “unemployed,” “redundant,” “unoccupied,” “refugees,” “low socioeconomic status,” “disadvantaged,” “deprived,” “low socioeconomic,” “poor,” “poverty,” “homeless,” “underprivileged,” “precarious employment status, “undocumented people,” “migrant,” “immigrant” (population); “intervention,” “health campaign,” “education” (intervention); “controlled study,” “controlled trial,” “control group,” “comparison group,” “reference group,” “experiment,” “quasi-experiment” (comparator); and “health literacy” or “health knowledge.” The search results were limited to adult populations by excluding the terms “children” “and adolescents.” Populations with a mean age of over 65 years were excluded during title/abstract and full-text screening. The search strategies for all searched databases can be found in Supplementary file 1.
Selection of studies
All articles identified from the searched databases were imported to the reference management software Endnote, where duplicates were removed. The remaining articles were then exported to the systematic review software Rayyan (27). Further duplicates missed during the initial deduplication were identified and removed in Rayyan before beginning the title and abstract screening. The title and abstract screening and full-text screening were done independently by two authors (FSZ & HS). All conflicts were resolved by discussion until a consensus was reached.
Data extraction
All data items were extracted twice by four authors independently in two-party teams (JK & FS and RH & HS) based on the extraction table devised a priori and presented in the study protocol (PROSPERO registration ID: CRD42022323801). The results of the extracted items were compared and conflicts were double-checked in the original article.
Among others, the following information was extracted: bibliographic information, study design, description of the intervention and control condition, definition of exact outcome, methods of outcome measurement, and effect estimator as reported in the article (Supplementary file 2).
Risk of bias analysis
Risk of bias was assessed independently by two authors (HS & JK) using the Risk of Bias tool (RoB) 2 of Cochrane for randomized controlled trials (RCT) (28) and the ROBINS-I for non-randomized controlled trials and quasi-experimental trials (29). Discrepancies in the assessments were discussed until resolved.
Data synthesis and analyses
Extracted study data were initially reviewed narratively. To begin with, we grouped the different relevant primary and secondary outcomes reported in the included studies in two categories as follows: (i) Health literacy: Functional health literacy and mental health literacy as primary outcomes; (ii) Health knowledge: cancer screening knowledge, child feeding knowledge, diabetes knowledge, food knowledge and HIV knowledge as secondary outcomes.
Due to heterogeneity in study outcomes, limitations in reporting, and variation in study designs, we refrained from conducting formal meta-analysis and used albatross plots to summarize findings. Albatross plots are a statistical visualization technique that can be used as an alternative to narrative reviews or to summarizing techniques such as vote counting in case of high heterogeneity of primary studies, as they allow comparing the approximate sizes of the effects and take into account the sample sizes of the primary studies as long as p-values are provided. In principle, albatross plots are scatter plots of study sample sizes against two-sided p-values and effect directions (in our case: favors HL intervention or favors control; (30)). Small two-sided p-values favoring the control group appear on the far left side of the panel, and small two-sided p-values favoring the HL intervention on the right side. Studies plotted close to the center have very small or non-significant effects. In addition, lines are added to the plot (albatross wings) that represent different levels of effect sizes (in our case: d values) based on the different alpha levels (0.05, 0.01 and 0.001) derived from primary study data. For a more detailed discussion of obtaining estimates for the effect size lines, see Harrison et al. (30).
For the comparison of different modes of delivery, we additionally indicated whether a study was conducted face-to-face or not by using different symbols in the plot.
We extracted sample sizes, p-values and effect sizes to summarize the intervention effects and to create seven albatross plots according to the different HL and health knowledge outcomes reported in the included studies. We compared mean differences (or differences between respondents giving correct and wrong answers in pre-and post-surveys for the intervention and control groups, respectively) to compute effect sizes. Where possible, all effect sizes reported in the studies (e.g., odds ratios, means of intervention and control groups, t values, etc.) were transformed into Cohen’s d. Only studies providing information regarding, sample size, p-values and effect sizes were included in the albatross plots. Effect sizes were calculated if not given insofar as mean, sample size and standard deviation were given. Sample sizes, p-values, and Cohen’s d of all included studies considered in the albatross plots are provided in Supplementary file 3. Albatross plots were created via Stata 17.0.
Sensitivity analysis
Sensitivity analysis was conducted by excluding articles that did not specifically report the study populations’ mean age or age range. Most of these excluded articles reported age group distributions of the study population.
Results
We screened 3,696 titles and abstracts and 206 full-texts. 82 articles met eligibility criteria and were included in the review. Four further articles were identified through hand-searching the literature of the included articles. Hence, in total, 86 articles were included in the main analyses, and 57 articles were included in albatross plots (Figure 1).
Figure 1.
PRISMA flow chart of the search process.
The main reasons for exclusion in the full-text phase were population not matching inclusion criteria (n = 49), no pre-post comparisons reported in the analyses (n = 28), no health knowledge outcome (n = 20), or the study design not matching the inclusion criteria (n = 9).
Study characteristics
The 86 studies included in the review were conducted in 20 different countries. The majority were conducted in the United States (n = 55), followed by China (n = 5), Taiwan (n = 4) and South Korea (n = 3).
51% of the included studies (n = 44) had a randomized controlled study design (of which 16 were cluster randomized controlled trials), while the remainder had a randomized or non-randomized quasi-experimental (n = 33), or another non-randomized controlled study design with a pre-post comparison (n = 9; Supplementary file 2).
All included studies were written in English and were published between 1990 and 2021. All study populations were working-age (18 to 65 years) and were potentially underserved or financially insecure. Mostly, the study populations were recruited from low-income neighborhoods and included migrants, young mothers, or clinical patients (with a low socioeconomic status) with pre-existing diseases such as diabetes and HIV. All in all, demographics of the study populations were roughly comparable (Supplementary file 2).
Health literacy outcomes and instruments
The included studies assessed a broad range of HL and health knowledge outcomes, including functional HL, mental health literacy, cancer screening knowledge, child feeding knowledge, diabetes knowledge, food knowledge, and HIV knowledge (Table 1; Supplementary files 2, 3).
Table 1.
Summary of review findings.
| Interventions to promote health literacy among resource-limitedly disadvantaged populations | ||||
|---|---|---|---|---|
| Population: Financially insecurely disadvantaged populations between 18 and 65 years | ||||
| Outcomes | Comparison of studies | Total no. of participants (studies) | Risk of bias overall | |
| Studies that found significant improvements in health literacy or health knowledge (%) Risk of bias of individual studies |
Studies that did not find significant improvements in health literacy or health knowledge (%) Risk of bias of individual studies |
|||
| Functional health literacy | 2 (50%) (212 participants) - - |
2 (50%) (311 participants) o - |
563 (4 studies) |
High risk of bias in 3/4 studies |
| Mental health literacy | 3 (75%) (390 participants) o - - |
1 (25%) (20 participants) - |
410 (4 studies) |
High risk of bias in 3/4 studies |
| Cancer screening knowledge* | 3 (60%) 897 participants o - - |
2 (40%) 390 participants o - |
987 (4 studies) |
High risk of bias in 3/4 studies |
| Childfeeding knowledge* | 9 (60%) 6,810 participants - o - o - o - o - |
6 (40%) 3,044 participants - - o o o o |
8,007 (12 studies) |
High risk of bias in 6/12 studies |
| Diabetes knowledge | 1 (25%) 72 participants - |
3 (75%) 511 participants o + o |
583 (4 studies) |
High risk of bias in 1/4 studies |
| Food knowledge* | 10 (67%) 4,093 participants - - - o – o o + − 0 |
5 (33%) 1,023 participants - o o - o |
4,329 (12 studies) |
High risk of bias in 6/12 studies |
| HIV knowledge* | 12 (67%) 3,532 participants - o - - o - - - - - - - |
6 (33%) 2067 - o - - - - |
6,515 (17 studies) |
High risk of bias in 14/17 studies |
- High risk of bias, o Moderate risk of bias, + Low risk of bias. *Some studies included multiple outcomes and appear in both rows: Statistically significant health knowledge improvement and no statistically significant health knowledge improvement (Supplementary file 3). (Summary of risk of bias displayed in same order as studies labeled in Figures 2–8).
Mostly, self-developed tools were used to measure the respective outcomes. Some validated tools used in the included studies were the TOFHLA/S-TOFHLA for functional HL, (31–33) the HIV knowledge Questionnaire for HIV knowledge (34, 35) or the Food Frequency Questionnaire (36) (Supplementary files 2, 3).
Intervention effects by outcome and intervention strategies applied
Functional health literacy
We analyzed the results of four studies reporting functional HL (31–33, 37) (Figure 2). All studies included a face-to-face component and two studies showed a statistically significant improvement in functional HL scores (32, 33).
Figure 2.
Albatross plot—functional health literacy.
In both studies, Spanish-speaking adults received curriculums focusing on improving HL (32, 33). The curriculum included components based on theories of HL, adult learning principles and sociocultural theories of literacy and communication and was designed for adults with limited English language skills (32). In one of the studies, participants additionally received cardiovascular-specific content (33).
Mental health literacy
Four studies reporting mental health literacy outcomes were included (38–41) (Figure 3). Mental health literacy scores improved statistically significantly in three of these, all of which had a face-to-face component (38, 39, 41).
Figure 3.
Albatross plot—mental health literacy.
The interventions comprised mental health improvement services by bilingual gatekeepers following a multilingual mental health improvement guidebook developed by authors in eight different languages (38) or fotonovelas, a form of entertainment education aiming to promote depression and mental health literacy (39, 41). Both Unger et al. and Hernandez and Organista implemented the fotonovela “Secret Feelings” (42) which was presented in English and Spanish at a 4th grade reading level and describes the story of a Hispanic wife and mother who deals with depression and eventually decides to obtain counseling and medication. Using dialogs and photographs the fotonovela informs about depression symptoms and the use of antidepressants.
Cancer screening knowledge
We found four studies providing eight effect sizes and tests addressing knowledge about cancer screening (43–46) (Figure 4). In three of these tests, the intervention group scored significantly better than the control group (43, 45, 46). All significant tests were reported for face-to-face interventions, the one study without a face-to-face component yielded no significant effect (44).
Figure 4.
Albatross plot—cancer screening knowledge.
Effective intervention approaches to increase cancer screening knowledge incorporated bilingual gatekeepers delivering educational sessions consisting of informational handouts, message cards addressing barriers to screening, a short-animated video, in-class activities and informational brochures (43, 45). In another study, trained community health advisors, “consejeras” provided interactive educational sessions in their communities (46).
Child feeding knowledge
We analyzed 12 studies which provided 35 effect sizes regarding child feeding practices and maternal nutrition (47–58) (Figure 5). In 22 tests from 9 studies, participants from the intervention groups showed better knowledge scores compared to participants of the control groups (47, 50–55, 57, 58). In two tests an inverse association was shown with participants of the control groups showing better knowledge scores (54, 56). In the remaining outcomes, the intervention groups tended to score better, however, the improvements compared to the control groups were not statistically significant.
Figure 5.
Albatross plot – Child feeding knowledge.
Studies with a larger effect mostly had a face-to-face component.
Components of the intervention programs showing larger effects were bilingual educational materials in form of DVDs and booklets (47), bilingual video-based learning sessions with African-American mothers and mothers with Hispanic backgrounds talking about challenges and evidence-based methods while feeding their children (51), scripted messages developed based on focus group discussions which were delivered by nurses and at clinics or home visits (54), and a 6-month computer-based curriculum consisting of 12 modules implemented through weekly home visits in one-on-one educational sessions with parents (53). Using bilingual language materials was a key part of the described interventions above.
Diabetes knowledge
Four studies and five outcomes on diabetes knowledge (Figure 6) (59–62) were identified through our searches.
Figure 6.
Albatross plot—diabetes knowledge.
Intervention recipients tended to show better knowledge, however, only one (pilot) study resulted in statistically significant knowledge improvements (60). Here, participants received in-home educational and behavioral modification sessions by registered nurses addressing among other topics, symptoms awareness and appropriate treatments for diabetes. The education session was followed by biweekly support telephone sessions.
Food knowledge
12 studies and 30 effect sizes were analyzed related to food knowledge (36, 63–73) (Figure 7). In 20 tests from 10 studies, intervention recipients obtained better food knowledge scores compared to the control group (36, 63–65, 68–73). For one outcome, a negative association was shown, with the control group scoring higher than the intervention group (63). The remaining studies did not report significant intervention effects. Most studies with a positive intervention effect reported effect sizes above d = 0.25, partly above d = 0.5.
Figure 7.
Albatross plot—food knowledge.
Successful intervention designs incorporated children teaching their parents in their native language about safe food handling knowledge (72), used community settings such as churches to distribute bilingual educational materials, organized activities such as cooking demonstrations and taste testing, provided weekly motivational interviewing sessions by telephone (69), or conducted group education sessions using culturally adapted materials (70). Similarly, a multicomponent 12-week weight management program based on focus groups and designed to be culturally sensitive to Hispanic culture was effective. Nutrition classes were set up according to the needs of participants aiming to keep cooking their family recipes and providing advice on how to make them healthier. Another part of the intervention was exercise education and exercise classes including stretching, walking, cardio and kickboxing, some of which could easily be done at home (65).
HIV knowledge
We analyzed 17 studies and 24 effect sizes regarding HIV knowledge (34, 35, 74–88) (Figure 8). In 15 outcomes from 15 studies HIV knowledge of intervention receivers improved significantly compared to the control groups (34, 35, 74–81, 84–86, 88).
Figure 8.
Albatross plot—HIV knowledge.
A negative association was shown in two studies where the control group scored better (82, 89). In the remaining studies, there were some non-statistically significant improvements in the intervention groups.
Interventions with larger effects included 4-week educational sessions in video and text form (76), an intervention program delivered on a train and consisting of didactic presentation, role-playing, and group discussions (74) and an educational intervention using motivational interviewing strategies based on information-motivation behavioral skills model (35).
A key part of the interventions was the translation of intervention materials into the respective first language of the study participants, or intervention deliverers being fluent in the study participants’ first language (74, 76).
Risk of bias analysis
We assessed the risk of bias in a variety of study designs using different tools. Due to poor reporting and lack of information provided, several studies were rated as low-quality studies. According to the RoB 2 from Cochrane, 11% (n = 3) of individually randomized controlled trials were given a low-risk rating, 32% (n = 9) were categorized as having some concerns and for 57% (n = 16) a high risk of bias was assessed. For cluster randomized controlled trials, 13% (n = 2) were rated as low-risk, 62% (n = 10) had some concerns and 25% (n = 4) were classified as high risk. While employing the ROBINS-I tool, 29% (n = 12) of quasi-experimental and non-randomized controlled trials were considered to have a moderate risk of bias, while 71% (n = 30) were assessed as having a serious or critical risk of bias (see Figure 9 and details in Supplementary file 4).
Figure 9.
Risk of bias analysis.
In an additional analysis, we assessed the included studies based on their risk of bias. We reran the albatross plots and compared effect sizes of studies with higher and lower risk of bias. Studies with a higher risk of bias more often showed larger effect sizes (details in Supplementary file 5).
Sensitivity analyses
11 articles not specifically reporting the study populations’ mean age or age range were analyzed separately and the results were compared to the main findings. Similar as in the main analysis most of the studies considered for the analysis were conducted in the United States (n = 4). Further studies were conducted in Australia, Bangladesh, China, Kenya, Nigeria, Netherlands and Turkey. Effective intervention approaches to improve health knowledge delivered educational programs via home visits (90), made use of different delivery modes including lectures, role-plays and interactive sessions (91) and incorporated bilingual gatekeepers as intervention deliverers (92) (Details in Supplementary file 6).
Discussion
Health literacy (HL) is distributed unequally. Underserved and financially insecure groups often report low levels of HL which in turn has a negative impact on their health and interactions with health services. Finding effective ways to improve HL in financially insecure and underserved populations is therefore of high public health relevance. To our knowledge, this is the first systematic review to assess the effects of interventions aiming to improve HL or health knowledge in working-age population groups experiencing socioeconomic disadvantage.
We found that successful intervention approaches (i.e., those that led to meaningful improvements in HL or health knowledge compared to the control groups) often incorporated a face-to-face component (31, 32, 35, 41, 51, 53–55, 60, 65, 69, 70, 72–74, 80) and often used culturally sensitive and multilingual materials with intervention deliverers being fluent in the first languages of the addressed populations, e.g., children of the study participants or bilingual gatekeepers (31, 32, 46, 47, 51, 65, 69, 70, 72).
Language support and health literacy
Language support in the majority language is also crucial for programs targeting non-native speakers. Effective studies for example implemented an English as a Second Language Curriculum combining HL content and English language instructions while using bilingual education material (32). Here, the intervention combined language-related content to improve English language proficiency through listening, reading and speaking exercises with health-literacy-related content to improve navigation of the participants within the healthcare system as well as numeracy skills and skills related to preventive practices.
The results of our review support the existing evidence on the role of language proficiency as a component of effective HL interventions. A 2018 review concluded that HL intervention approaches should be designed according to the specific needs of the target groups and use easy-to-understand language (93). An intervention (94) designed for unemployed minority or migrant women illustrates the important role of language proficiency for disadvantaged populations: Here, a key finding was that women from similar cultural and linguistic backgrounds were essential to approach and retain the target group in the intervention and consequently improve HL.
Similar strategies seemed to be effective in improving MHL and other health knowledge outcomes analyzed in the review. Successful MHL promotion interventions used a face-to-face component (38, 39, 41), easy-to-understand language, bilingual gatekeepers, or fotonovelas which not only reduced text but were also created according to the needs of the study populations and with relatable characters (39, 41). Further key parts of successful intervention strategies included multilingual intervention materials and in-home education sessions. Focus groups guiding the design of the intervention were important to address the specific needs of the target population (47, 51, 60, 65, 69).
Together with our review, these findings suggest that low-threshold communication of the intervention contents and addressing culture-specific aspects are essential if HL interventions in disadvantaged populations are to succeed.
Importance of face-to-face interventions
Interventions including face-to-face components seemed to be most effective in increasing HL and health knowledge. As virtually all alternatives to face-to-face delivery modes such as digital tools, self-help guides, etc. require resources and access (95–97), which in turn are distributed unequally across socioeconomic strata (96, 98), it is hardly surprising that face-to-face interventions are more effective in disadvantaged populations – alternatives could essentially be inaccessible. As digital literacy skills in particular are tied to socioeconomic factors such as higher education (99), this suggests that face-to-face components might be essential features for interventions that aim to be effective in underserved and financially insecure populations.
At the same time, low literacy needs to be distinguished from language proficiency. Migrant populations, e.g., might have high literacy skills in general but might not be language proficient in the majority language of their country of residence and accordingly score low on HL measures. In this case, online education materials might be useful as long as they are provided in the first language of the migrants. The literature suggests that online education can be as effective as face-to-face education in high-literate populations such as university students or health professionals (100, 101). This means that online interventions may be an option for high-literate migrant populations, but not for low-literate ones. At the same time, as our results suggest that face-to-face components might be more effective, language courses for migrant populations might be good settings for additional health literacy content.
Strengths and limitations
To our knowledge, this is one of the first systematic reviews to specifically focus on interventions on HL in financially insecure and underserved populations. Our search strategy was comprehensive, nevertheless, we may have missed relevant studies, for example, those that investigated health literacy intervention approaches in the context of complex interventions. The outcomes of the reviewed studies were heterogeneous and difficult to compare. Thus, no meta-analysis could be conducted, but albatross plots were created instead. Only few studies examined HL or MHL as primary outcome, therefore the results need to be interpreted with caution. However, comparing the results of the secondary outcomes (health knowledge outcomes) to the primary outcomes effective intervention approaches employed similar intervention strategies such as involving bilingual gatekeepers and using multilingual materials. It should also be noted that due to lack of information given, a significant number of studies were found to exhibit a serious risk of bias, even though many of them were RCTs. Clearly, more high-quality intervention studies on health literacy with a focus on underserved and financially insecure populations are required or at least study methods need to be described in more detail. Consequently, results of this systematic review need to be interpreted respectively, despite of the large number of studies included.
This review summarizes various articles and their key results to identify the best strategies for improving HL and health knowledge and filling the gap in the literature.
Still, more interventions are needed to identify effective ways of increasing all facets of HL (access, understand, appraise and apply health information) as measured by the HLS-EU-Q16 for, e.g., rather than functional HL only.
Conclusion and implications
This review found that effective HL intervention approaches were more likely to use face-to-face components and information matched to participants’ language skills and cultural backgrounds. Accordingly, future interventions should be designed face-to-face and according to the needs of the addressed population. Here, in particular, language proficiency and cultural aspects seem to be important. In practical terms, this could be ensured by involving target groups in needs assessments and intervention design, for example through focus group discussions before and throughout designing the intervention.
Furthermore, differentiating between low literacy and lack of language proficiency is crucial. While for example individuals with migration history might lack proficiency in the majority language, they might have high literacy levels in their first language and would therefore profit from native language health information, most likely regardless of the modality (brochures, video-based, face-to-face or not). For populations with low literacy however, written health information might not be suitable, and such information should be provided face-to-face or in visual formats. Depending on the composition of the respective target population, bilingual staff with fitting cultural backgrounds is important to approach and keep participants in intervention programs.
Regardless of individual literacy skills and language proficiency, all disadvantaged populations will profit from health services with low literacy requirements. Offering easy-to-understand, multilingual materials in places that are part of daily life, i.e., churches, sports clubs, mosques, barbers, and shopping centers, could be a way of reaching disadvantaged populations and increasing HL.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
HS: Conceptualization, Formal analysis, Investigation, Methodology, Software, Writing – original draft, Data curation, Writing – review & editing. FS-Z: Conceptualization, Data curation, Methodology, Software, Writing – review & editing. JK: Data curation, Methodology, Software, Writing – review & editing. RH: Data curation, Writing – review & editing. WH: Writing – review & editing. NB: Formal analysis, Writing – review & editing. TB: Project administration, Writing – review & editing. HZ: Conceptualization, Project administration, Writing – review & editing. BS: Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The systematic review was part of the project FORESIGHT funded by the German Federal Ministry of Health (Grant ZMVI1-2519FSB020).
Footnotes
1To promote inclusivity and avoid stigmas we have refrained in the following from using the terms “socially disadvantaged” and “socioeconomically disadvantaged,” opting instead for the expressions “financial insecurity” and “underserved.” Nevertheless, for the sake of article visibility, the original term is retained in the title and when referencing to the literature.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1332720/full#supplementary-material
References
- 1.Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. (2012) 12:80. doi: 10.1186/1471-2458-12-80, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bennett IM, Chen J, Soroui JS, White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med. (2009) 7:204–11. doi: 10.1370/afm.940, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fernandez DM, Larson JL, Zikmund-Fisher BJ. Associations between health literacy and preventive health behaviors among older adults: findings from the health and retirement study. BMC Public Health. (2016) 16:596. doi: 10.1186/s12889-016-3267-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howard DH, Sentell T, Gazmararian JA. Impact of health literacy on socioeconomic and racial differences in health in an elderly population. J Gen Intern Med. (2006) 21:857–61. doi: 10.1111/j.1525-1497.2006.00530.x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yin HS, Dreyer BP, Foltin G, van Schaick L, Mendelsohn AL. Association of low caregiver health literacy with reported use of nonstandardized dosing instruments and lack of knowledge of weight-based dosing. Ambul Pediatr. (2007) 7:292–8. doi: 10.1016/j.ambp.2007.04.004, PMID: [DOI] [PubMed] [Google Scholar]
- 6.Kripalani S, Henderson LE, Chiu EY, Robertson R, Kolm P, Jacobson TA. Predictors of medication self-management skill in a low-literacy population. J Gen Intern Med. (2006) 21:852–6. doi: 10.1111/j.1525-1497.2006.00536.x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis TC, Wolf MS, Bass PF, 3rd, Thompson JA, Tilson HH, Neuberger M, et al. Literacy and misunderstanding prescription drug labels. Ann Intern Med. (2006) 145:887–94. doi: 10.7326/0003-4819-145-12-200612190-00144, PMID: [DOI] [PubMed] [Google Scholar]
- 8.Rothman RL, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. (2006) 31:391–8. doi: 10.1016/j.amepre.2006.07.025 [DOI] [PubMed] [Google Scholar]
- 9.Wolf MS, Davis TC, Shrank W, Rapp DN, Bass PF, Connor UM, et al. To err is human: patient misinterpretations of prescription drug label instructions. Patient Educ Couns. (2007) 67:293–300. doi: 10.1016/j.pec.2007.03.024, PMID: [DOI] [PubMed] [Google Scholar]
- 10.Lancet T. Why is health literacy failing so many? Lancet. (2022) 400:1655. doi: 10.1016/S0140-6736(22)02301-7, PMID: [DOI] [PubMed] [Google Scholar]
- 11.Sørensen K, Pelikan JM, Röthlin F, Ganahl K, Slonska Z, Doyle G, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health. (2015) 25:1053–8. doi: 10.1093/eurpub/ckv043, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garcia-Codina O, Juvinyà-Canal D, Amil-Bujan P, Bertran-Noguer C, González-Mestre MA, Masachs-Fatjo E, et al. Determinants of health literacy in the general population: results of the Catalan health survey. BMC Public Health. (2019) 19:1122. doi: 10.1186/s12889-019-7381-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurrelmann K, Klinger J, Schaeffer D. Gesundheitskompetenz der Bevölkerung in Deutschland–Vergleich der Erhebungen 2014 und 2020. Bielefeld: Universität Bielefeld, Interdisziplinäres Zentrum für Gesundheitskompetenzforschung; (2020).
- 14.Schaeffer D, Berens EM, Vogt D. Gesundheitskompetenz der Bevölkerung in Deutschland. Dtsch Arztebl Int. (2017) 4:53–60. doi: 10.3238/arztebl.2017.0053 [DOI] [Google Scholar]
- 15.Svendsen MT, Bak CK, Sørensen K, Pelikan J, Riddersholm SJ, Skals RK, et al. Associations of health literacy with socioeconomic position, health risk behavior, and health status: a large national population-based survey among Danish adults. BMC Public Health. (2020) 20:565. doi: 10.1186/s12889-020-08498-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh H, Kolschen J, Samkange-Zeeb F, Brand T, Zeeb H, Schüz B. Modifiable predictors of health literacy in working-age adults - a rapid review and meta-analysis. BMC Public Health. (2022) 22:1450. doi: 10.1186/s12889-022-13851-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. (2011) 155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005, PMID: [DOI] [PubMed] [Google Scholar]
- 18.Pourrazavi S, Kouzekanani K, Bazargan-Hejazi S, Shaghaghi A, Hashemiparast M, Fathifar Z, et al. Theory-based E-health literacy interventions in older adults: a systematic review. Arch Public Heal. (2020) 78:72. doi: 10.1186/s13690-020-00455-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Walters R, Leslie SJ, Polson R, Cusack T, Gorely T. Establishing the efficacy of interventions to improve health literacy and health behaviours: a systematic review. BMC Public Health. (2020) 20:1040. doi: 10.1186/s12889-020-08991-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. (1984) 11:1–47. doi: 10.1177/109019818401100101, PMID: [DOI] [PubMed] [Google Scholar]
- 21.Duan Y, Shang B, Liang W, Lin Z, Hu C, Baker JS, et al. Predicting hand washing, mask wearing and social distancing behaviors among older adults during the covid-19 pandemic: an integrated social cognition model. BMC Geriatr. (2022) 22:91. doi: 10.1186/s12877-022-02785-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lv G, Yuan J, Hsieh S, Shao R, Li M. Knowledge and determinants of behavioral responses to the pandemic of COVID-19. Front Med. (2021) 8:8. doi: 10.3389/fmed.2021.673187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kebede Y, Yitayih Y, Birhanu Z, Mekonen S, Ambelu A. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. PloS One. (2020) 15:e0233744. doi: 10.1371/journal.pone.0233744, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Federal employment agency Germany . Long-term unemployment – Sociodemography. (2020). [Available from: https://statistik.arbeitsagentur.de/DE/Navigation/Statistiken/Interaktive-Angebote/Langzeitarbeitslosigkeit/Langzeitarbeitslosigkeit-Nav. html:jsessionid=9E0F8BB50126F383CCAE8BEF5501A8A7; Access date: 02.11.2023]
- 25.Svendsen IW, Damgaard MB, Bak CK, Bøggild H, Torp-Pedersen C, Svendsen MT, et al. Employment status and health literacy in Denmark: a population-based study. Int J Public Health. (2021) 66:598083. doi: 10.3389/ijph.2021.598083, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Samkange-Zeeb F, Singh H, Lakeberg M, Kolschen J, Schüz B, Christianson L, et al. Health literacy needs among unemployed persons: collating evidence through triangulation of interview and scoping review data. Front Public Health. (2022) 10:10. doi: 10.3389/fpubh.2022.798797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ouzzani M, Hammady H, Fedorowicz Z, Rayyan AE,— a web and mobile app for systematic reviews. Systematic Reviews (2016) 5:210. doi: 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 29.Sterne J, Hernán M, Reeves B, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. (2016) 355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harrison S, Jones HE, Martin RM, Lewis SJ, Higgins JPT. The albatross plot: A novel graphical tool for presenting results of diversely reported studies in a systematic review. Res Synth Methods. (2017) 8, 281–9. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Soto Mas F, Jacobson HE, Olivárez A. Adult education and the health literacy of Hispanic immigrants in the United States. J Latinos Educ. (2017) 16:314–22. doi: 10.1080/15348431.2016.1247707 [DOI] [Google Scholar]
- 32.Soto Mas F, Ji M, Fuentes BO, Tinajero J. The health literacy and ESL study: a community-based intervention for spanish-speaking adults. J Health Commun. (2015) 20:369–76. doi: 10.1080/10810730.2014.965368, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Soto Mas F, Schmitt CL, Jacobson H, Myers OB. A cardiovascular health intervention for Spanish speakers: the health literacy and ESL curriculum. J Community Health. (2018) 43:717–24. doi: 10.1007/s10900-018-0475-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li X, Lin D, Wang B, Du H, Tain CC, Stanton B. Efficacy of theory-based hiv behavioral prevention among rural-to-urban migrants in China: a randomized controlled trial. AIDS Educ Prev. (2014) 26:296–316. doi: 10.1521/aeap.2014.26.4.296, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carey MP, Braaten LS, Maisto SA, Gleason JR, Forsyth AD, Durant LE, et al. Using information, motivational enhancement, and skills training to reduce the risk of HIV infection for low-income urban women: a second randomized clinical trial. Health Psychol. (2000) 19:3–11. doi: 10.1037/0278-6133.19.1.3, PMID: [DOI] [PubMed] [Google Scholar]
- 36.Havas S, Anliker J, Greenberg D, Block G, Block T, Blik C, et al. Final results of the Maryland WIC food for life program. Prev Med. (2003) 37:406–16. doi: 10.1016/S0091-7435(03)00160-9, PMID: [DOI] [PubMed] [Google Scholar]
- 37.Tsai TL, Lee SYD, Yu WR. Impact of a problem-based learning (PBL) health literacy program on immigrant Women's health literacy, health empowerment, navigation efficacy, and health care utilization. J Health Commun. (2018) 23:340–9. doi: 10.1080/10810730.2018.1445798, PMID: [DOI] [PubMed] [Google Scholar]
- 38.Choi YJ. Effects of a program to improve mental health literacy for married immigrant women in Korea. Arch Psychiatr Nurs. (2017) 31:394–8. doi: 10.1016/j.apnu.2017.04.012, PMID: [DOI] [PubMed] [Google Scholar]
- 39.Hernandez MY, Organista KC. Entertainment-education? A Fotonovela? A new strategy to improve depression literacy and help-seeking behaviors in at-risk immigrant Latinas. Am J Community Psychol. (2013) 52:224–35. doi: 10.1007/s10464-013-9587-1, PMID: [DOI] [PubMed] [Google Scholar]
- 40.Odom SE. Effects of an educational intervention on mothers of male children with attention deficit hyperactivity disorder. J Community Health Nurs. (1996) 13:207–20. doi: 10.1207/s15327655jchn1304_1 [DOI] [PubMed] [Google Scholar]
- 41.Unger JB, Cabassa LJ, Molina GB, Contreras S, Baron M. Evaluation of a fotonovela to increase depression knowledge and reduce stigma among hispanic adults. J Immigr Minor Health. (2012) 15:398–406. doi: 10.1007/s10903-012-9623-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cabassa LJ, Molina GB, Baron M. Depression fotonovela: development of a depression literacy tool for Latinos with limited English proficiency. Health Promot Pract. (2012) 13:747–54. doi: 10.1177/1524839910367578, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Calderón-Mora J, Byrd TL, Alomari A, Salaiz R, Dwivedi A, Mallawaarachchi I, et al. Group versus individual culturally tailored and theory-based education to promote cervical Cancer screening among the underserved Hispanics: a cluster randomized trial. Am J Health Promot. (2020) 34:15–24. doi: 10.1177/0890117119871004, PMID: [DOI] [PubMed] [Google Scholar]
- 44.Jibaja ML, Kingery P, Neff NE, Smith Q, Bowman J, Holcomb JD. Tailored, interactive soap operas for breast cancer education of high-risk Hispanic women. J Cancer Educ. (2000) 15:237–42. PMID: [DOI] [PubMed] [Google Scholar]
- 45.Luque JS, Tarasenko YN, Reyes-Garcia C, Alfonso ML, Suazo N, Rebing L, et al. Salud es Vida: a cervical Cancer screening intervention for rural Latina immigrant women. J Cancer Educ. (2016) 32:690–9. doi: 10.1007/s13187-015-0978-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Navarro AM, Raman R, McNicholas LJ, Loza O. Diffusion of cancer education information through a Latino community health advisor program. Prev Med. (2007) 45:135–8. doi: 10.1016/j.ypmed.2007.05.017, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cala Cala LF, Kelly CL, Ramos E, Van Vleet M, High P. Which mothers know that all babies cry? A randomized controlled trial of a child abuse prevention program for low-income new mothers. Clin Pediatr. (2020) 59:865–73. doi: 10.1177/0009922820922532, PMID: [DOI] [PubMed] [Google Scholar]
- 48.Campbell MK, Carbone E, Honess-Morreale L, Heisler-Mac Kinnon J, Demissie S, Farrell D. Randomized trial of a tailored nutrition education CD-ROM program for women receiving food assistance. J Nutr Educ Behav. (2004) 36:58–66. doi: 10.1016/S1499-4046(06)60134-6, PMID: [DOI] [PubMed] [Google Scholar]
- 49.Fitzgibbon ML, Stolley MR, Avellone ME, Sugerman S, Chavez N. Involving parents in Cancer risk reduction: a program for Hispanic American families. Health Psychol. (1996) 15:413–22. doi: 10.1037/0278-6133.15.6.413, PMID: [DOI] [PubMed] [Google Scholar]
- 50.Hoddinott J, Ahmed A, Karachiwalla NI, Roy S. Nutrition behaviour change communication causes sustained effects on IYCN knowledge in two cluster-randomised trials in Bangladesh. Matern Child Nutr. (2018) 14:e12498. doi: 10.1111/mcn.12498, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hughes SO, Power TG, Beck A, Betz D, Goodell LS, Hopwood V, et al. Short-term effects of an obesity prevention program among low-income Hispanic families with preschoolers. J Nutr Educ Behav. (2020) 52:224–39. doi: 10.1016/j.jneb.2019.12.001, PMID: [DOI] [PubMed] [Google Scholar]
- 52.Kim SS, Nguyen PH, Tran LM, Sanghvi T, Mahmud Z, Haque MR, et al. Large-scale social and behavior change communication interventions have sustained impacts on infant and young child feeding knowledge and practices: results of a 2-year follow-up study in Bangladesh. J Nutr. (2018) 148:1605–14. doi: 10.1093/jn/nxy147, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.LoRe D, Leung CYY, Brenner L, Suskind DL. Parent-directed intervention in promoting knowledge of pediatric nutrition and healthy lifestyle among low-SES families with toddlers: a randomized controlled trial. Child Care Health Dev. (2019) 45:518–22. doi: 10.1111/cch.12682, PMID: [DOI] [PubMed] [Google Scholar]
- 54.Monterrosa EC, Frongillo EA, de Cossío TG, Bonvecchio A, Villanueva MA, Thrasher JF, et al. Scripted messages delivered by nurses and radio changed beliefs, attitudes, intentions, and behaviors regarding infant and young child feeding in mexico. J Nutr. (2013) 143:915–22. doi: 10.3945/jn.112.169235, PMID: [DOI] [PubMed] [Google Scholar]
- 55.Rahman A, Iqbal Z, Roberts C, Husain N. Cluster randomized trial of a parent-based intervention to support early development of children in a low-income country. Child Care Health Dev. (2009) 35:56–62. doi: 10.1111/j.1365-2214.2008.00897.x, PMID: [DOI] [PubMed] [Google Scholar]
- 56.Scheinmann R, Chiasson MA, Hartel D, Rosenberg TJ. Evaluating a bilingual video to improve infant feeding knowledge and behavior among immigrant Latina mothers. J Community Health. (2009) 35:464–70. doi: 10.1007/s10900-009-9202-4 [DOI] [PubMed] [Google Scholar]
- 57.Singh A, Klemm RDW, Mundy G, Rana P, Pun B, Cunningham K. Improving maternal, infant and young child nutrition in Nepal via peer mobilization. Public Health Nutr. (2017) 21:796–806. doi: 10.1017/S1368980017002993, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang HH, Lin ML, Yang YM, Tsai HM, Huang JJ. The effects of group health education on childbearing knowledge, attitude, and behaviour among southeast Asian immigrant women in Taiwan. Midwifery. (2012) 28:754–9. doi: 10.1016/j.midw.2011.07.007, PMID: [DOI] [PubMed] [Google Scholar]
- 59.Frosch DL, Uy V, Ochoa S, Mangione CM. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Arch Intern Med. (2011) 171:2011–7. doi: 10.1001/archinternmed.2011.497 [DOI] [PubMed] [Google Scholar]
- 60.García A, Brown SA, Horner SD, Zuñiga J, Arheart KL. Home-based diabetes symptom self-management education for Mexican Americans with type 2 diabetes. Health Educ Res. (2015) 30:484–96. doi: 10.1093/her/cyv018, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gerber BS, Brodsky IG, Lawless KA, Smolin LI, Arozullah AM, Smith EV, et al. Implementation and evaluation of a low-literacy diabetes education computer multimedia application. Diabetes Care. (2005) 28:1574–80. doi: 10.2337/diacare.28.7.1574, PMID: [DOI] [PubMed] [Google Scholar]
- 62.Heisler M, Choi H, Palmisano G, Mase R, Richardson C, Fagerlin A, et al. Comparison of community health worker-led diabetes medication decision-making support for low-income latino and african american adults with diabetes using E-health tools versus print materials. Ann Intern Med. (2014) 161:S13–22. doi: 10.7326/M13-3012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Au LE, Whaley SE, Gurzo K, Meza M, Rosen NJ, Ritchie LD. Evaluation of online and in-person nutrition education related to salt knowledge and behaviors among special supplemental nutrition program for women, infants, and children participants. J Acad Nutr Diet. (2017) 117:1384–95. doi: 10.1016/j.jand.2016.12.013, PMID: [DOI] [PubMed] [Google Scholar]
- 64.Backman D, Scruggs V, Atiedu AV, Bowie S, Bye L, Dennis A, et al. Using a toolbox of tailored educational lessons to improve fruit, vegetable, and physical activity behaviors among African American women in California. J Nutr Educ Behav. (2011) 43:S75–85. doi: 10.1016/j.jneb.2011.02.004 [DOI] [PubMed] [Google Scholar]
- 65.Berry D, Colindres M, Sanchez-Lugo L, Sanchez M, Neal M, Smith-Miller C. Adapting, feasibility testing, and pilot testing a weight management intervention for recently immigrated Spanish-speaking women and their 2-to 4-year-old children. Hispanic Health Care Int (Springer Publishing Company, Inc). (2011) 9:186–93. doi: 10.1891/1540-4153.9.4.186 [DOI] [Google Scholar]
- 66.Bessems K, Linssen E, Lomme M, van Assema P. The effectiveness of the good affordable food intervention for adults with low socioeconomic status and small incomes. Int J Environ Res Public Health. (2020) 17:2535. doi: 10.3390/ijerph17072535, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gittelsohn J, Song HJ, Suratkar S, Kumar MB, Henry EG, Sharma S, et al. An urban food store intervention positively affects food-related psychosocial variables and food behaviors. Health Educ Behav. (2010) 37:390–402. doi: 10.1177/1090198109343886, PMID: [DOI] [PubMed] [Google Scholar]
- 68.Howard-Pitney B, Winkleby MA, Albright CL, Bruce B, Fortmann SP. The Stanford nutrition action program: a dietary fat intervention for low-literacy adults. Am J Public Health. (1997) 87:1971–6. doi: 10.2105/AJPH.87.12.1971, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hughes SC, Obayashi S. Faith-based intervention to increase fruit and vegetable intake among Koreans in the USA: a feasibility pilot. Public Health Nutr. (2016) 20:357–62. doi: 10.1017/S1368980016002354, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kjøllesdal MKR, Hjellset VT, Bjørge B, El Holmboe-Ottesen GM. Perceptions of risk factors for diabetes among Norwegian-Pakistani women participating in a culturally adapted intervention. Ethn Health. (2010) 16:279–97. doi: 10.1080/13557858.2011.573537 [DOI] [PubMed] [Google Scholar]
- 71.Nguyen PH, Frongillo EA, Sanghvi T, Wable G, Mahmud Z, Tran LM, et al. Engagement of husbands in a maternal nutrition program substantially contributed to greater intake of micronutrient supplements and dietary diversity during pregnancy: results of a cluster-randomized program evaluation in Bangladesh. J Nutr. (2018) 148:1352–63. doi: 10.1093/jn/nxy090, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ratnapradipa D, Quilliam D, Wier L, Rhodes DL. Food safety education: child-to-parent instruction in an immigrant population. J Environ Health. (2011) 73:70–5. PMID: [PubMed] [Google Scholar]
- 73.Tessaro I, Rye S, Parker L, Mangone C, McCrone S. Effectiveness of a nutrition intervention with rural low-income women. Am J Health Behav. (2007) 31:35–43. doi: 10.5993/AJHB.31.1.4 [DOI] [PubMed] [Google Scholar]
- 74.Bahromov M, Weine S. HIV prevention for migrants in transit: developing testing train. AIDS Educ Prev. (2011) 23:267–80. doi: 10.1521/aeap.2011.23.3.267, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bogale GW, Boer H, Seydel ER. Effects of a theory-based audio HIV/AIDS intervention for illiterate rural females in Amhara. Ethiopia AIDS Educ Prev. (2011) 23:25–37. doi: 10.1521/aeap.2011.23.1.25, PMID: [DOI] [PubMed] [Google Scholar]
- 76.Choi SY. Development of an educational program to prevent cervical cancer among immigrants in Korea. Asian Pac J Cancer Prev. (2013) 14:5345–9. doi: 10.7314/APJCP.2013.14.9.5345, PMID: [DOI] [PubMed] [Google Scholar]
- 77.Cianelli R, Ferrer L, Norr KF, Miner S, Irarrazabal L, Bernales M, et al. Mano a Mano-Mujer: An effective HIV prevention intervention for Chilean women. Health Care Women Int. (2012) 33:321–41. doi: 10.1080/07399332.2012.655388, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dancy BL, Marcantonio R, Norr K. The long-term effectiveness of an HIV prevention intervention for low-income African American women. AIDS Educ Prev. (2000) 12:113–25. PMID: [PubMed] [Google Scholar]
- 79.Flaskerud JH, Nyamathi AM. Effects of an AIDS education program on the knowledge, attitudes and practices of low income black and Latina women. J Community Health. (1990) 15:343–55. doi: 10.1007/BF01324297, PMID: [DOI] [PubMed] [Google Scholar]
- 80.Lawrence JSS, Wilson TE, Eldridge GD, Brasfield TL, O'Bannon RE. Community-based interventions to reduce low income, African American women's risk of sexually transmitted diseases: a randomized controlled trial of three theoretical models. Am J Community Psychol. (2001) 29:937–64. doi: 10.1023/A:1012919700096, PMID: [DOI] [PubMed] [Google Scholar]
- 81.Li N, Li X, Wang X, Shao J, Dou J. A cross-site intervention in Chinese rural migrants enhances HIV/AIDS knowledge, attitude and behavior. Int J Environ Res Public Health. (2014) 11:4528–43. doi: 10.3390/ijerph110404528, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nyamathi AM, Kington RS, Flaskerud J, Lewis C, Leake B, Gelberg L. Two-year follow-up of AIDS education programs for impoverished women. West J Nurs Res. (1999) 21:405–25. doi: 10.1177/01939459922043956, PMID: [DOI] [PubMed] [Google Scholar]
- 83.Nyamathi AM, Leake B, Flaskerud J, Lewis C, Bennett C. Outcomes of specialized and traditional AIDS counseling programs for impoverished women of color. Res Nurs Health. (1993) 16:11–21. doi: 10.1002/nur.4770160104, PMID: [DOI] [PubMed] [Google Scholar]
- 84.Pokharel P, Shettigar PG. Impact of counseling in knowledge, attitude and practice and association of nutritional status with CD4 count and opportunistic infections of HIV patients of Udupi. India Clin Nutrit ESPEN. (2019) 29:154–9. doi: 10.1016/j.clnesp.2018.11.001, PMID: [DOI] [PubMed] [Google Scholar]
- 85.Sanderson M, Khabele D, Brown CL, Harbi K, Alexander LR, Coker AL, et al. Results of a health education message intervention on HPV knowledge and receipt of follow-up care among Latinas infected with High-risk human papillomavirus. J Health Care Poor Underserved. (2015) 26:1440–55. doi: 10.1353/hpu.2015.0131, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Van Servellen G, Carpio F, Lopez M, Garcia-Teague L, Herrera G, Monterrosa F, et al. Program to enhance health literacy and treatment adherence in low-income HIV-infected Latino men and women. AIDS Patient Care & STDs. (2003) 17:581–94. doi: 10.1089/108729103322555971, PMID: [DOI] [PubMed] [Google Scholar]
- 87.van Servellen G, Nyamathi A, Carpio F, Pearce D, Garcia-Teague L, Herrera G, et al. Effects of a treatment adherence enhancement program on health literacy, patient-provider relationships, and adherence to HAART among low-income HIV-positive Spanish-speaking Latinos. AIDS Patient Care STDS. (2005) 19:745–59. doi: 10.1089/apc.2005.19.745, PMID: [DOI] [PubMed] [Google Scholar]
- 88.Zhang T, Tian X, Ma F, Yang Y, Yu F, Zhao Y, et al. Community based promotion on VCT acceptance among rural migrants in Shanghai, China. PloS One. (2013) 8:106. doi: 10.1371/journal.pone.0060106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nyamathi A, Stein JA, Schumann A, Tyler D. Latent variable assessment of outcomes in a nurse-managed intervention to increase latent tuberculosis treatment completion in homeless adults. Health Psychol. (2007) 26:68–76. doi: 10.1037/0278-6133.26.1.68, PMID: [DOI] [PubMed] [Google Scholar]
- 90.Özdil K, Karataş N, Zincir H. Low socioeconomic level and enterobius vermicularis: a interventional study to children and their mothers in home. Zoonoses Public Health. (2020) 67:882–91. doi: 10.1111/zph.12774, PMID: [DOI] [PubMed] [Google Scholar]
- 91.Tobin-West CI, Briggs N. Effectiveness of trained community volunteers in improving knowledge and management of childhood malaria in a rural area of Rivers state. Nigeria Niger J Clin Pract. (2021) 18:651–8. doi: 10.4103/1119-3077.158971 [DOI] [PubMed] [Google Scholar]
- 92.Mishra SI, Chavez LR, Magaña JR, Nava P, Burciaga Valdez R, Hubbell FA. Improving breast cancer control among Latinas: evaluation of a theory-based educational program. Health Educ Behav. (1998) 25:653–70. doi: 10.1177/109019819802500511, PMID: [DOI] [PubMed] [Google Scholar]
- 93.Visscher BB, Steunenberg B, Heijmans M, Hofstede JM, Devillé W, van der Heide I, et al. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health. (2018) 18:1414. doi: 10.1186/s12889-018-6331-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Reiter A, Hager I. Evaluierung-Gesundheit kommt nachhause - Mehr Wissen hilft. (2012). [Available from: https://fgoe.org/sites/fgoe.org/files/project-attachments/Gekona-Endbericht-2011-externe-Evaluierung-1.pdf; Accessdate: 02.11.2023]
- 95.Butcher CJ, Hussain W. Digital healthcare: the future. Future Healthc J. (2022) 9:113–7. doi: 10.7861/fhj.2022-0046, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Crawford A, Serhal E. Digital health equity and COVID-19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res. (2020) 22:e19361. doi: 10.2196/19361, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hege I, Tolks D, Kuhn S, Shiozawa T. Digital skills in healthcare. GMS. J Med Educ. (2020) 37:Doc63. doi: 10.3205/zma001356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Woolley KE, Bright D, Ayres T, Morgan F, Little K, Davies AR. Mapping inequities in digital health technology within the World Health Organization's European region using PROGRESS PLUS: scoping review. J Med Internet Res. (2023) 25:e44181. doi: 10.2196/44181, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.De Santis KK, Jahnel T, Sina E, Wienert J, Zeeb H. Digitization and health in Germany: cross-sectional Nationwide survey. JMIR Public Health Surveill. (2021) 7:e32951. doi: 10.2196/32951, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Maloney S, Haas R, Keating JL, Molloy E, Jolly B, Sims J, et al. Effectiveness of web-based versus face-to-face delivery of education in prescription of falls-prevention exercise to health professionals: randomized trial. J Med Internet Res. (2011) 13:e116. doi: 10.2196/jmir.1680, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Stevens GJ, Bienz T, Wali N, Condie J, Schismenos S. Online university education is the new normal: but is face-to-face better? Interactive Technol Smart Educ. (2021) 18:278–97. doi: 10.1108/ITSE-08-2020-0181 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.