Abstract
Background
Burnout is a public health problem with various health consequences, among which cardiovascular disease is the most investigated but still under debate. Our objective was to conduct a systematic review and meta-analysis on the influence of burnout on cardiovascular disease.
Methods
Studies reporting risk (odds ratio, relative risk, and hazard ratio) of cardiovascular disease following burnout were searched in PubMed, PsycINFO, Cochrane, Embase, and ScienceDirect. We performed a random-effect meta-analysis stratified by type of cardiovascular disease and searched for putative influencing variables. We performed sensitivity analyses using the most adjusted models and crude risks.
Results
We included 25 studies in the systematic review and 9 studies in the meta-analysis (4 cross-sectional, 4 cohort, and 1 case–control study) for a total of 26,916 participants. Burnout increased the risk of cardiovascular disease by 21% (OR = 1.21, 95% CI 1.03 to 1.39) using the most adjusted risks and by 27% (OR = 1.27, 95% CI 1.10 to 1.43) using crude risks. Using stratification by type of cardiovascular disease and the most adjusted risks, having experienced burnout significantly increased the risk of prehypertension by 85% (OR = 1.85, 95% CI 1.00 to 2.70) and cardiovascular disease-related hospitalization by 10% (OR = 1.10, 95% CI 1.02 to 1.18), whereas the risk increase for coronary heart disease (OR = 1.79, 95% CI 0.79 to 2.79) and myocardial infarction (OR = 1.78, 95% CI 0.85 to 2.71) was not significant. Results were also similar using crude odds ratio. The risk of cardiovascular disease after a burnout was not influenced by gender. Insufficient data precluded other meta-regressions.
Conclusions
Burnout seems to increase the risk of cardiovascular disease, despite the few retrieved studies and a causality weakened by cross-sectional studies. However, numerous studies focused on the pathophysiology of cardiovascular risk linked to burnout, which may help to build a preventive strategy in the workplace.
Keywords: mental health, burnout, cardiovascular disease, methodology, statistics
Introduction
Burnout is a public health problem (1). The term burnout was first used in 1969 by Harold B. Bradley (2). This term was taken up in 1974 by the psychoanalyst Herbert J. Freudenberger (3) and then in 1976 by the psychologist Christina Maslach (2). According to the World Health Organization, burnout is a syndrome combining a sense of exhaustion, cynicism or increased mental distance from work, and decreased work effectiveness, resulting from chronic stress at work that has not been successfully managed (4). Among the various health consequences of burnout, cardiovascular disease remains the most investigated and debated (5). Cardiovascular disease is the leading cause of death in the world, causing approximately 17.9 million deaths each year (6). However, cardiovascular disease promoted by burnout is not well known. Cardiovascular disease is a very diverse group of diseases, including diseases of the heart and blood vessels (7). Some studies (7, 8) investigated the pathophysiology of burnout, particularly the development of cardiovascular disease. Quantitative studies have limitations, in particular in their reporting of each type of cardiovascular disease. The calculation of risks seems heterogeneous between studies (9, 10). To date, no meta-analysis has specifically focused on the risk of cardiovascular disease following burnout exposure, putatively able to reconcile diverging literature. Individual risk factors for cardiovascular disease, such as age, gender, body mass index, smoking, physical activity, and lipid levels (11–13), were also not investigated specifically in the context of burnout.
Therefore, our objective is to perform a systematic review and meta-analysis on the influence of burnout on cardiovascular disease. A secondary objective is to compare the influence of burnout according to each cardiovascular disease and to study individual risk factors that influence the risk of cardiovascular disease due to burnout.
Methods
Literature search
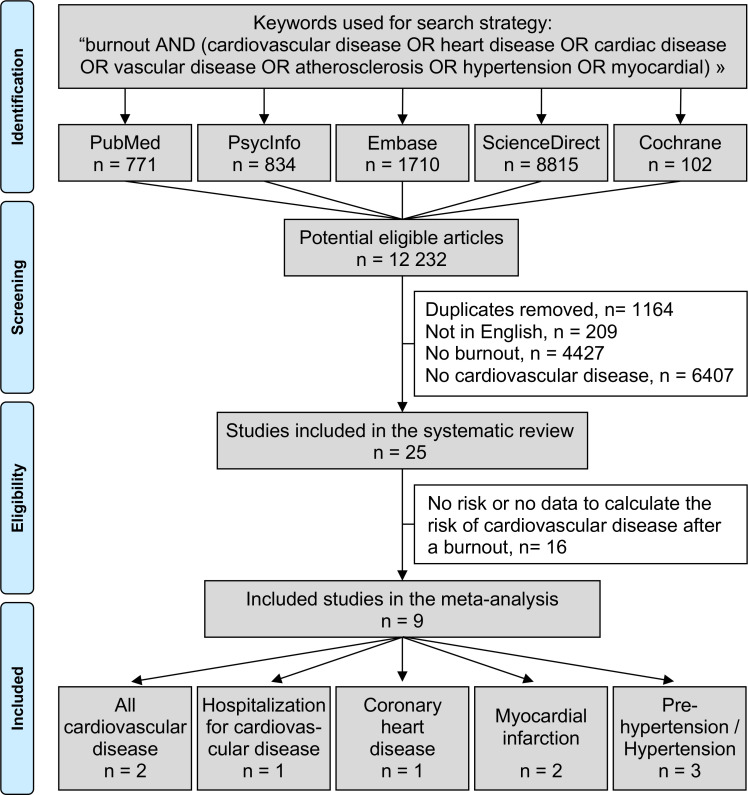
The following PICO (population, investigated condition, i.e., exposure, comparisons, and outcome) question was formulated: Are workers exposed to burnout at higher risk of cardiovascular disease, compared to workers not exposed to burnout? We reviewed all studies reporting the risk of having cardiovascular disease in relation with burnout. The PubMed, Cochrane Library, Embase, ScienceDirect, and PsycINFO databases were searched in July 2022 with the following keywords: burnout AND (cardiovascular disease OR heart disease OR cardiac disease OR vascular disease OR atherosclerosis OR hypertension OR myocardial) (details for the search strategy used within each database are available in Appendix 1 ). We limited our search to articles in adult workers and to those written in English. To be included in the systematic review, studies needed to describe our primary outcome variable, i.e., the influence of burnout on cardiovascular disease. Articles describing either an odds ratio, a relative risk, or a hazard ratio, or giving data to calculate the risk of cardiovascular disease following a burnout, were included in the meta-analysis. We included any type or diagnosis of cardiovascular disease including high blood pressure and atherosclerosis, but not dyslipidemia as we considered it more related to metabolic disease. For high blood pressure, we considered all cutoffs defined in retrieved articles. We also considered outcomes related to cardiovascular disease such as hospitalization for cardiovascular disease. References from all publications meeting the inclusion criteria were also searched manually to identify potential additional studies that were not found during the electronic search. In addition, we performed ancestry searches to locate other potentially eligible primary studies from previous reviews. Two authors (Awena John and Jean-Baptiste Bouillon-Minois) conducted the literature searches, reviewed the abstracts, and, based on the selection criteria, decided the suitability of the articles for inclusion and extracted the data. When necessary, disagreements were solved with a third author (Frédéric Dutheil) ( Figure 1 ). Then, all authors reviewed the eligible articles.
Figure 1.
Search strategy.
Data extraction
The data collected included first author’s name, publication year, aims, outcomes of included articles, characteristics of studies (study design, periods of collection of data, and country), characteristics of the population (sample size, age, sex, and occupation), characteristics of burnout (scale used, method of calculation, and thresholds), characteristics of cardiovascular disease (type and criteria for diagnosis), and its associated risk (method of calculation, type of risk, and adjustment models).
Quality of assessment
We used the Newcastle–Ottawa Scale (NOS) to check the quality of included articles (14) ( Figure 2 ). The maximum score was 9 for cohort and 10 for cross-sectional studies. Additionally, we also used the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) for cohort and cross-sectional studies (15) ( Appendix 2 ).
Figure 2.
Methodological quality of included articles.
Statistical considerations
Statistical analysis was conducted using Stata software (v16, StataCorp, College Station, USA) (16–20). Extracted data were summarized for each study and reported as mean (standard deviation) and number (%) for continuous and categorical variables, respectively. We conducted random-effects meta-analysis (DerSimonian and Laird approach) (21) on the risk of cardiovascular disease following burnout using all odds ratio, relative risk, or hazard ratio (22–26). We stratified this meta-analysis on the type of cardiovascular disease (all cardiovascular disease, hospitalization for cardiovascular disease, coronary heart disease (CHD), myocardial infarction, and high blood pressure). We described our results by calculating the risk of cardiovascular disease after a burnout (21). Risks were centered at one if the risk of cardiovascular disease after a burnout did not differ from the risk of cardiovascular disease without having any burnout. Risk > 1 denoted an increased risk of cardiovascular disease, and hazard ratio < 1 reflected a decreased risk. We conducted a meta-analysis on the most adjusted models and on crude risks (sensitivity analyses) ( Figure 3 , Appendix 3 ). Statistical heterogeneity between studies was assessed using forest plots, confidence intervals, and I²: heterogeneity is considered low for I² <25%, modest for 25%–50%, and high for >50%. We also aimed to conduct sensitivity analysis by excluding studies not evenly distributed around the base of the metafunnel ( Appendix 4 ). We also proposed meta-regressions to investigate putative factors influencing the risk of cardiovascular disease following burnout exposure such as age, sex, occupation, or type of cardiovascular disease. Results were expressed as regression coefficients and 95% confidence intervals. Type I -error was fixed at α = 0.05.
Figure 3.
Summary of meta-analyses on the risk of cardiovascular disease after a burnout.
Results
An initial search produced 12,232 possible articles. Removal of duplicates and use of selection criteria reduced the number of articles reporting the influence of burnout on cardiovascular disease to 25 articles in the systematic review (5, 8–10, 27–47) and 9 were included in the meta-analysis (9, 10, 29, 36, 37, 41–44) ( Figure 1 ). The main characteristics of all studies are outlined in Table 1 and studies included in the meta-analyses are further described below. All articles were written in English.
Table 1.
Characteristics of included studies in the meta-analysis.
| Study | Country | Period of data collection | Design | Population | Burnout | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Sex, % men |
Age, years mean ± SD |
Occupational work | Measure | Risk | Adjustment | ||||
| Appels 1991 (9) | Netherland | 1979–1983 | Cohort | 3,210 | 100 | Burned out 52.3 ± 8.4 Controls 51.3 ± 8.6 |
64% blue collar workers | Maastricht Questionnaire | RR | Age, cholesterol, BP, smoking |
| Azfar 2021 (29) | Kyrgyzstan | Not precise | Cross-sectional | 694 | 43.5 | Mean age for six ethnic groups, from 34.3 ± 14.3 to 48.5 ± 15.7 | SMBQ | OR | Ethnicity, gender and BMI | |
| Honkonen 2005 (36) | Finland | 2000–2001 | Cross-sectional | 3,368 | 52.3 | 44.6± 8.6 | 30% blue collar 28% upper white collar 27% lower white collar 15% self-employed |
MBI-GS | OR | Sociodemographic, health behavior and depressive symptoms |
| Kitaoka 2009 (10) | Japan | 4–5 years | Cohort | 383 | 100 | 37.8 ± 11.6 | Middle managers | MBI-GS (Japanese Version) | OR | Age, alcohol, smoking, physical activity |
| Lin 2021 (37) | Taiwan | Not precise | Cross-sectional | 242 | 26.4 | 50.4±? | Workers in elderly welfare facilities | Copenhagen Burnout Inventory (Chinese Version) | OR | Age, sex, education, type of work shifts, nurse assistant work category, personal burnout, BMI |
| Sokejima 1998 (41) | Japan | 1990–1993 | Case–control | 526 | 100 | Burned out 55.5 ± 8.6 Controls 54.4 ± 8.3 |
51% managers and officials 15% professional and technical |
Burnout measure by Pines | OR | Age, occupational categories |
| Toker 2012 (42) | Israël | 2003–2010 | Cohort | 8,838 | 63 | CHD 53.5 ± 7.9 No CHD 44.9 ± 10.5 |
SMBM | HR | Age, sex, family history of CHD, smoking, subjective and objective workload, depression | |
| Toppinen-Tanner 2009 (43) | Finland | Not precise | Cohort | 7,897 | 76 | >18 | Forest industry employees | MBI-GS | HR | Age, sex, occupational status, physical environment, medication for hypertension and diabetes |
| Tsou 2020 (44) | Taiwan | 2018–2019 | Cross-sectional | 1,758 | 4.2 | Median 35.2 | Nurses | Chinese Burnout Inventory | OR | Sex, sleep time, alcohol, physical activity, fruit and vegetable intake |
MBI-GS, Maslach Burnout Inventory – General Survey; SMBM, Shirom Melamed Burnout Measure; SMBQ, Shirom Melamed Burnout Questionnaire; Burnout measure by Pines from (48).
Quality of articles
Using the NOS criteria for cross-sectional studies demonstrated a low risk of bias, except for sample representativeness and ascertainment of exposure ( Figure 2 ). NOS and STROBE evaluation for each included study are available in Appendix 2 .
Aims and outcomes of included articles
Six studies aimed to evaluate the association between burnout and the incidence or the prevalence of cardiovascular disease as a primary result (9, 10, 36, 37, 42, 43), while three studies evaluated this association as a secondary result (29, 41, 44). For one study (29), the main objective was to characterize different ethnic groups in Kyrgyzstan regarding cardiovascular disease and mental distress; for another study (41), it was to clarify the extent to which working hours affect the risk of acute myocardial infarction; and for the third study (44), it was to analyze the association between burnout and metabolic syndrome.
Study designs
Four studies were cross-sectional (29, 36, 37, 44), four were cohort studies (9, 10, 42, 43), and one was a case–control study. Cohort studies had a follow-up from 3.6 (42) to 10 (43) years on average. Five studies were conducted in Asia [Kyrgyzstan (29), Japan (10, 41), and Taiwan (37, 44)], three in Europe [Netherlands (9) and Finland (36, 43)], and one in Israel (42).
Recruitment of individuals
Recruitment procedures included individuals visiting polyclinics and healthcare centers (29, 41, 42), city employees (9), middle managers working on a manufacturing company (10), workers in public elderly welfare facilities (37), nurses working in a tertiary hospital (44), forest industry employees (43), and workers from the general population, i.e., any worker (36).
Populations studied
Sample size ranged from 242 (37) to 8,838 (42). In total, 26,916 individuals were included in our meta-analysis.
Age was reported in all studies. Most of the studies (9, 10, 29, 36, 37, 41, 42) reported mean age. One study (44) reported age as a median, and one study (43) reported prevalence by age category.
Gender was reported in all studies. Overall, there were 43% of the sample were men (95% CI 20% to 66%), ranging from 26% (37) to 100% (9, 10, 41).
Other descriptive variables included body mass index (BMI) (10, 29, 36, 37, 41, 42), blood pressure (9, 10, 36, 37, 41–44), cholesterol (9, 10, 41, 42), occupational status (9, 36, 41, 43), work style (37, 42, 44), education level (29, 36, 37, 42), marital status (9, 29, 36), ethnicity (29), physical activity (10, 36, 42, 44), smoking habits (9, 10, 36, 41, 42, 44), and alcohol consumption (10, 36, 44), and two studies focused on family history of heart disease (41, 42). In addition, most studies (78%) conducted health examination to evaluate the risk of cardiovascular disease (9, 10, 36, 37, 41, 42, 44). The health examination included measurement of height (36, 41, 44), body weight (9, 36, 44), body circumference (10, 36), waist circumference (10, 44), electrocardiogram (ECG) (9, 36), spirometry (36), bioimpedance (36), heel bone density (36), blood test (10, 36), total cholesterol (9, 41), triglycerides, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol (42), fasting insulin and glucose tolerance (9, 42), and HbA1c and TSH (44) ( Table 1 ).
Measurements of burnout
All studies used self-administered questionnaires to assess burnout, but differed between studies except three studies (10, 36, 43) that used the Maslach Burnout Inventory – General Survey (MBI-GS) (49). The MBI-GS a 16-item questionnaire consisting of three subscales: exhaustion (five items), cynicism (five items), and lack of professional efficacy (six items), each item being scored on a seven-point scale ranging from 0 (“never”) to 6 (“daily”). One study used only four items for cynicism (10). Two studies (36, 43) calculated levels of burnout using a weighted sum: (0.4/5 × exhaustion + 0.3/5 × cynicism + 0.3/6 × lack of professional efficacy)/6 and considered burnout to be severe if the score is 3.50 to 6, mild if the score is 1.50 to 3.49, and no burnout is the score is 0 to 1.49. Despite not being written, the reference cited indicated that odds ratios for cardiovascular disease were calculated for the combination mild plus severe burnout. The third study (10) used previous data from their research team to divide each subscale into tertiles: burnout (yes/no) was considered for the combination of intense exhaustion (upper third) and either high cynicism (upper third) or low professional efficacy (lower third) or both. One study (29) used the Shirom Melamed Burnout Questionnaire (SMBQ) (38), which is an eight-item questionnaire, each item being scored on a seven-point scale from 1 (“almost never”) to 7 (“almost always”). Scores were summed and burnout was recorded as a dichotomous variable: high (uppermost quartile) and low (other quartiles). Another study (42) used the Shirom Melamed Burnout Measure (SMBM) (50), which is a 14-item questionnaire, also scored on a seven-point scale. Burnout was also recorded as a dichotomous variable: high (uppermost quintile) and low (other quintiles). One study (35) used the Chinese version of the Copenhagen Burnout Inventory (51), which is a 13-item questionnaire (items 1 to 6 for personal burnout and items 7 to 13 for work-related burnout), each item being scored on a five-point scale: 0 (“almost never”), 25 (“never”), 50 (“sometimes”), 75 (“often”), and 100 (“always”). Scores of items 7 to 13 were averaged, and work-related burnout was considered mild for a score <45, moderate for 50 to 69.9, and severe for ≥70. Odds ratios for cardiovascular disease were calculated for the combination moderate plus severe burnout (score >45). One study (44) used the Chinese occupational burnout inventory (52) that consists of three domains: psychological work demands, job control/personal accomplishment, and employment stability. After summing points for each domain, burnout (yes/no) was defined as high psychological work demands (upper tertile) plus low job control (lower tertile) plus low employment stability (lower tertile). The case–control study (41) used the “Burnout measure”, a 21-item questionnaire, developed by Pines (48), consisting of three subscales (physical, emotional, and mental exhaustion), with items being scored on a seven-point scale ranging from 1 (“never”) to 7 (“always”). Calculation of scores was not written but the reference cited (53) averaged scores of each item, and defined burnout as a dichotomous variable: burnout (average score >4) and no burnout (<4). A third category of “borderline” burnout was presented but not explained. We only considered odds ratio for burnout. The last study (9) added the question “Have you ever been burned out” (categorical answer: yes/no) to the Maastricht Questionnaire that addresses loss of energy, increased irritability, and demoralization, which was constructed to be an indicator of mental precursors to myocardial infarction (54). Prevalence of cardiovascular diseases by dimension of burnout (exhaustion, cynicism, and lack of professional efficacy) was reported in one study (44) and by severity per dimension in one study (36), and odds ratio per dimension of burnout was reported in one study (43).
Measurements of cardiovascular disease
All cardiovascular diseases were reported in two studies (29, 36). Diagnosis of cardiovascular disease was assessed using the question “Do you have any cardiovascular disease diagnosed by a doctor?” in one study (29), and using the Symptom Interview that was carried out in the first part of the health examination in the second study (36).
Hospitalization for cardiovascular disease was assessed in one study (43). Information on hospital admissions data was retrieved from the National Hospital Discharge Register, which is a complete, reliable source of illnesses that includes all hospital admissions with their causes.
CHD was assessed in one study (42). CHDs were defined as a composite of acute myocardial infarction, ischemic heart disease, and angina pectoris. Participants had to complete a self-report of medically diagnosed CHD.
Myocardial infarction was assessed in two studies (9, 41). One study (41) included patients admitted for a first attack of acute myocardial infarction. The other study (9) followed a cohort of patients with angina pectoris and retrieved those who had a myocardial infarction during the follow-up (54). In both studies, the diagnosis criteria for myocardial infarction were based on typical chest pain, electrocardiogram, and enzyme levels (55).
High blood pressure was reported in three studies: prehypertension was defined as systolic and diastolic blood pressure between 120/80 and 139/89 mmHg (37); ≥130/85 mmHg in the metabolic syndrome (44); and hypertension was defined as ≥140/90 mmHg (10, 37).
Meta-analysis on the risk of cardiovascular disease after burnout
Overall using the most adjusted risks, the overall risk of cardiovascular disease increased by 21% following burnout exposure (OR = 1.21, 95% CI 1.03 to 1.39). Using stratification by type of cardiovascular disease, having a burnout significantly increased the risk of cardiovascular disease-related hospitalization by 10% (1.10, 1.02 to 1.18) (43), and prehypertension by 85% (1.85, 1.00 to 2.70) (37, 44) ( Figure 3 , Appendix 3 ). Risks were not significant for CHD (1.79, 0.79 to 2.79) (42), myocardial infarction (1.78, 0.85 to 2.71) (9, 41), and hypertension (0.69, −0.07 to 1.45) (10, 37).
Sensitivity analyses and meta-regressions
We repeated an aforementioned meta-analysis using crude odds ratio and found similar results, i.e., an overall risk of cardiovascular disease following burnout exposure (OR = 1.32, 95% CI 1.19 to 1.44), as well as the risk of cardiovascular disease-related hospitalization (1.10, 1.02 to 1.18) and prehypertension (1.85, 1.00 to 2.70) ( Figure 3 , Appendix 3 ). Metafunnels analyzing for potential publication bias are presented in Appendix 4 ; however, excluding studies outside of metafunnels was deemed impossible because of the limited number of included studies.
The risk of cardiovascular disease after burnout was not influenced by gender (coefficient −0.007% men, 95% CI −0.071 to 0.056). Insufficient data precluded other meta-regressions.
Discussion
Despite the few numbers of studies and the fact that the causality is weakened by the cross-sectional design of some studies, the main finding was that burnout seems to increase the risk of cardiovascular disease. Insufficient data precluded further analyses of other risk factors. However, numerous studies focused on the pathophysiology of the cardiovascular risk linked to burnout.
Influence of burnout on cardiovascular disease: a public health issue
By the 1940s, cardiovascular disease became the number one cause of mortality among Americans, accounting for one in two deaths (56). Prevention and treatment were so poorly understood that most Americans accepted early death from heart disease as unavoidable (57). The Framingham study conducted in 1948 highlighted the importance of prevention in the occurrence of cardiovascular disease in individuals at high risk (57). A key component of this strategy was the ability to identify those most likely to have a future cardiovascular event, so that preventive interventions could be targeted (57). However, occupational risk factors were not evaluated or even reported in those historical studies. In 2004, the Interheart case–control study was the first large-scale study that also investigated occupational characteristics as risk factors for cardiovascular events. The study found that stress at work was involved in the occurrence of cardiovascular events (58). If stress at work has been studied for a long time, burnout is a more recent concept (59). The possibility that burnout may be a risk factor for the development of cardiovascular disease has been suggested in the 1990s (38), and the first prospective study using a valid measure of burnout was done in 2012, associating burnout with an increased risk of CHD (42). Despite the few numbers of studies and the fact that a causal relation could be extracted only from longitudinal studies, our meta-analysis seems in favor of an increased risk of cardiovascular disease following burnout, probably between 20% and 30%. Cardiovascular disease and burnout have both consequences on mental and physical health, as well as on work organization and economy (22, 23, 31–33, 37–40), increasing the numbers of sick leave and absenteeism (5). Interestingly, burnout also increases presenteeism, i.e., when people come to work even when sick, leading to a loss of productivity (5). In a vicious cycle, workers in burnout may not reach the desirable performance at work, which may lead to emotional exhaustion (60, 61). In addition to organizational and economic consequences for the companies, absenteeism or presenteeism related to burnout may represent the beginning of a social decline involving job loss and even permanent exclusion from the labor market (5).
Depending on individual risk factors
Age over 45 years old is a common risk factor for burnout and cardiovascular disease, while being a man is specifically a risk for cardiovascular disease (62), and being a woman specifically increases the risk of burnout (63). There are also risk factors related to occupation (44). Occupational factors that can both impact the risk of burnout and the risk of cardiovascular disease are heavy workload, long working hours, time pressure, low rewards, low autonomy (decision latitude), value conflict, and lack of clarity in goals (52). Those factors are considered common factors of stress. The more stressful the job, the higher the risk of burnout and cardiovascular disease (64). Preventing excessive work stress is a legal obligation in several countries, and promoting awareness of the link between stress and health among both employers and workers is an important component of workplace health promotion (65). Besides sociodemographic and occupational factors, lifestyle behaviors also play a role in the risk of burnout and cardiovascular disease (66). Smoking and alcohol negatively influence the incidence of both burnout and cardiovascular disease while physical activity reduces the risk of developing burnout or cardiovascular disease (42, 43). Interestingly, physical inactivity has been shown to be the only significant factor linked to stress, and it is commonly admitted that workplace health promotion should also encourage workers to exercise regularly (67). Specific ethnic characteristics also seem to influence the occurrence of burnout and cardiovascular disease, but the pathophysiology needs to be further explored (29). Besides putative genetic mechanisms related to ethnicity (68, 69), ethnic factors influencing the risk of burnout and cardiovascular disease could be better associated with common characteristics linked to family history, such as religious practices, geographical origins, or education (70–72). Indeed, despite the fact that, for example, having an Asian ethnicity has a lower risk of atherosclerosis (73), persistent ethnic and racial differences in all-cause and cardiovascular mortality are largely attributable to social determinants of health—i.e., poor social conditions are linked to mortality (74). At a state level, governments should act on systemic factors that shape health differences across racial and ethnic groups (74). Very interestingly, despite the fact that burnout seems ubiquitous, i.e., any worker could be in burnout, without evidence of a difference in burnout by ethnicity (75, 76), it has been shown in some articles that underrepresented minorities may have a lower prevalence of burnout (77, 78). A putative explanation could be because they form communities with stronger support groups, and also because the cultural diversity may be a protective factor from some working conditions (77, 78). To prevent burnout and cardiovascular disease, occupational health departments should consider relevant risk factors to identify high-risk groups for efficient preventive strategy (37).
Burnout and cardiovascular disease pathophysiological similarities
Interestingly, the pathophysiology of burnout also shares some similarities with the pathophysiology of cardiovascular disease, through neuroendocrine and inflammatory responses, as well as metabolic processes (79). The dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis has been demonstrated to play a major role in the pathophysiology of cardiovascular disease from historical studies (80–82). Interestingly, some studies suggest that burnout is also associated with dysregulation of the HPA axis (a key stress responsive endocrine system), proinflammatory cytokine levels, inflammation biomarkers, and higher allostatic load (8). Burnout is associated with functional disconnection between the amygdala and the anterior cingulate/medial prefrontal cortex (83). The HPA axis is the primary means through which humans mediate the response to stress (84). With prolonged chronic exposure to stress, the HPA axis negative feedback loop can be lost, rendering the mechanism dysfunctional (30). Repeated exposure to psychosocial stress results in exaggerated activation of both the HPA axis and the sympathetic nervous system (85). This maladaptive process has been implicated in the development of burnout (27) and in cardiovascular disease because it disrupts metabolic parameters such as lipids, hypertension, and type 2 diabetes (30). The hyperstimulation of the HPA axis because of chronic stress also increases cortisol secretion (44). High levels of cortisol further suppress the development of new neurons in the hippocampus. Then, without resolution, limbic brain structures begin to atrophy (86). Reduced activity of the parasympathetic nervous system increases the risk of CHD (87, 88). It has been suggested that parasympathetic nerve activity is decreased by weak stressors that do not increase sympathetic nerve activity (89). Even if the stressors encountered while working are weak, coronary risk could be increased by attenuated vagal tone (30, 90).
Limitations
Our study has some limitations. Our meta-analysis inherits the limitations of each included study. First of all, the interpretation of causality may be limited. Cross-sectional studies (29, 36, 37, 44) showed associations between burnout and cardiovascular disease; however, prospective studies are more appropriate for investigating the possible consequences of burnout (5). In our meta-analysis, few studies were prospective (9, 10, 42, 43), and a causal relation could be extracted only from longitudinal studies. Moreover, they had a short follow-up that may have restricted the ability to observe the effects of burnout on cardiovascular disease. Then, only published articles were included in our meta-analysis; thus, our results were theoretically exposed to a publication bias (91). We also included only studies written in English; hence, results were theoretically exposed to a selection bias. There were also wide variability in study populations (30), with some studies not being representative of the general working population (29, 42, 43), especially because ethnic groups differed significantly in age, gender, and education (29). However, taken together, this wide variability population is in favor of the generalizability of our results. Our meta-analysis also had limitations in the measurement of both burnout and cardiovascular disease. Indeed, burnout scales differed between studies, rendering comparisons less precise, even if all studies had a control group with no burnout. Assessment of burnout has always been reported through self-administered questionnaires, which may have led to an over- or underestimation of burnout. However, assessing a mental state is obviously subjective (92–94). Some studies also assessed cardiovascular disease using self-reported questionnaire (29, 36, 42). Cardiovascular disease was very diverse and heterogenous, decreasing the level of proof of the overall results of our meta-analysis. Lastly, except for gender, there were not enough data to analyze the putative influencing factors of the effects of burnout on cardiovascular diseases. For example, no meta-regressions were made on severity and duration of burnout, as well as on occupational characteristics, because they were not reported.
Perspective of improvement for future studies
Considering that a causal link between burnout and cardiovascular disease is weakened by aforementioned limitations (particularly the inclusion of cross-sectional studies and the short follow-up for cohort studies), our meta-analysis also showed the need for further prospective studies with a long-term follow-up, using reliable records of cardiovascular disease as well as basic information such as details surrounding burnout (intensity and duration), sociodemographic factors (age, gender, marital status, and education level), occupational characteristics (job, occupational sector, and number of hours of work per week seniority), and lifestyle behavior (smoking, alcohol, physical activity, and nutrition/body mass index). Adjuvant measures should be assessed with reliable facility’s equipment (37). A long period of follow-up is needed because cardiovascular disease may occur several years after a burnout exposure, but a long period of follow-up is also needed to study the time effect itself for burnout to promote cardiovascular disease. To our knowledge, no study assessed the time period between burnout and cardiovascular disease, and associated influencing factors of this delay. Further studies should also use identical methods to measure burnout and to diagnose cardiovascular disease. All cardiovascular diseases should be considered, to assess disease-specific relationships.
Conclusion
Despite the few numbers of included studies and a causality weakened by the cross-sectional design of some studies, our meta-analysis seems to be in favor of an increased risk of cardiovascular disease following burnout, probably between 20% and 30%. However, numerous studies focused on the pathophysiology of cardiovascular risk linked to burnout. This better understanding may help to build a preventive and efficient strategy in the workplace. Future studies should be achieved through prospective studies with a long-term follow-up, which may also help to understand the chronology of development of cardiovascular disease following burnout.
Data availability statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.
Author contributions
AJ: Writing – original draft. J-BB-M: Writing – original draft. RB: Writing – review & editing. CP: Writing – review & editing. BC: Writing – review & editing. P-ML: Writing – review & editing. MZ: Writing – review & editing. UU: Writing – review & editing. JB: Writing – review & editing. FD: Writing – original draft.
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1326745/full#supplementary-material
Details for the search strategy used within each database.
Details for methodological quality of included articles (Methodological assessment of studies using STROBE criteria, Methodological assessment of studies using NOS criteria) and Checklists used for quality assessment of included studies (Newcastle-Ottawa Scale (NOS) for cross-sectional studies, Newcastle-Ottawa Scale (NOS) for cohort studies, Strengthening the Reporting of Observational studies in Epidemiology (STROBE) for cross-sectional and cohort studies)
Meta-analysis using the most adjusted and crude risk of cardiovascular disease after a burnout.
Metafunnels, based on data from the most adjusted and crude risk of cardiovascular disease after a burnout.Each dot represents a single study, with its corresponding risk (x axis) and its associated standard error of the risk (y-axis). Large high-powered studies are placed towards the top, and smaller low-powered studies towards the bottom. The plot should ideally resemble a pyramid or inverted funnel, with scatter due to sampling variation. Studies outside funnel plot are likely to present bias (94).
References
- 1. Friganović A, Selič P, Ilić B, Sedić B. Stress and burnout syndrome and their associations with coping and job satisfaction in critical care nurses: a literature review. Psychiatr Danub mars (2019) 31(Suppl 1):21−31. [PubMed] [Google Scholar]
- 2. Freudenberger HJ. Syndrome d’épuisement professionnel. 23:. [Google Scholar]
- 3. Freudenberger HJ. Staff burn-out. J Soc Issues (1974) 30(1):159−65. doi: 10.1111/j.1540-4560.1974.tb00706.x [DOI] [Google Scholar]
- 4. Burn-out an « occupational phenomenon »: International Classification of Diseases (2022). Available at: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases.
- 5. Salvagioni DAJ, Melanda FN, Mesas AE, González AD, Gabani FL, de Andrade SM. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PloS One [Internet] (2017) 12(10). doi: 10.1371/journal.pone.0185781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saheera S, Krishnamurthy P. Cardiovascular changes associated with hypertensive heart disease and aging. Cell Transplant (2020) 29:0963689720920830. doi: 10.1177/0963689720920830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maladies cardiovasculaires (2022). Available at: https://www.who.int/fr/health-topics/cardiovascular-diseases.
- 8. Melamed S, Shirom A, Toker S, Berliner S, Shapira I. Burnout and risk of cardiovascular disease: Evidence, possible causal paths, and promising research directions. Psychol Bull (2006) 132(3):327−53. doi: 10.1037/0033-2909.132.3.327 [DOI] [PubMed] [Google Scholar]
- 9. Appels A, Schouten E. Burnout as a risk factor for coronary heart disease. Behav Med Wash DC (1991) 17(2):53−9. doi: 10.1080/08964289.1991.9935158 [DOI] [PubMed] [Google Scholar]
- 10. Kitaoka-Higashiguchi K, Morikawa Y, Miura K, Sakurai M, Ishizaki M, Kido T, et al. Burnout and risk factors for arteriosclerotic disease: follow-up study. J Occup Health (2009) 51(2):123−31. doi: 10.1539/joh.L8104 [DOI] [PubMed] [Google Scholar]
- 11. Fuchs FD, Whelton PK. HIGH BLOOD PRESSURE AND CARDIOVASCULAR DISEASE. Hypertens Dallas Tex 1979 (2020) 75(2):285−92. doi: 10.1161/HYPERTENSIONAHA.119.14240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jokinen E. Obesity and cardiovascular disease. Minerva Pediatr (2015) 67(1):25−32. [PubMed] [Google Scholar]
- 13. Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary behavior, exercise, and cardiovascular health. Circ Res (2019) 124(5):799−815. doi: 10.1161/CIRCRESAHA.118.312669 [DOI] [PubMed] [Google Scholar]
- 14. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol (2010) 25(9):603−5. doi: 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 15. Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Ann Intern Med (2007) 147(8). doi: 10.7326/0003-4819-147-8-200710160-00010-w1 [DOI] [PubMed] [Google Scholar]
- 16. Bouillon-Minois JB, Croizier C, Baker JS, Pereira B, Moustafa F, Outrey J, et al. Tranexamic acid in non-traumatic intracranial bleeding: a systematic review and meta-analysis. Sci Rep (2021) 11(1):15275. doi: 10.1038/s41598-021-94727-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bruet S, Butin M, Dutheil F. Systematic review of high-flow nasal cannula versus continuous positive airway pressure for primary support in preterm infants. Arch Dis Child Fetal Neonatal Ed (2022) 107(1):56−9. doi: 10.1136/archdischild-2020-321094 [DOI] [PubMed] [Google Scholar]
- 18. Dutheil F, Aubert C, Pereira B, Dambrun M, Moustafa F, Mermillod M, et al. Suicide among physicians and health-care workers: A systematic review and meta-analysis. PloS One (2019) 14(12):e0226361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dutheil F, Baker JS, Mermillod M, De Cesare M, Vidal A, Moustafa F, et al. Shift work, and particularly permanent night shifts, promote dyslipidaemia: A systematic review and meta-analysis. Atherosclerosis (2020) 313:156−69. doi: 10.1016/j.atherosclerosis.2020.08.015 [DOI] [PubMed] [Google Scholar]
- 20. Dutheil F, Comptour A, Mermillod M, Pereira B, Clinchamps M, Charkhabi M, et al. Letter to the Editor: Comment on « Maternal exposure to air pollution and risk of autism in children: A systematic review and meta-analysis ». Environ pollut Barking Essex 1987 (2020) 264:114724. doi: 10.1016/j.envpol.2020.114724 [DOI] [PubMed] [Google Scholar]
- 21. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials (1986) 7(3):177−88. doi: 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 22. Dutheil F, Comptour A, Morlon R, Mermillod M, Pereira B, Baker JS, et al. Autism spectrum disorder and air pollution: A systematic review and meta-analysis. Environ pollut Barking Essex 1987 (2021) 278:116856. doi: 10.1016/j.envpol.2021.116856 [DOI] [PubMed] [Google Scholar]
- 23. Dutheil F, Pélangeon S, Duclos M, Vorilhon P, Mermillod M, Baker JS, et al. Protective effect on mortality of active commuting to work: A systematic review and meta-analysis. Sports Med Auckl NZ (2020) 50(12):2237−50. doi: 10.1007/s40279-020-01354-0 [DOI] [PubMed] [Google Scholar]
- 24. Dutheil F, Zaragoza-Civale L, Pereira B, Mermillod M, Baker JS, Schmidt J, et al. Prostate cancer and asbestos: A systematic review and meta-analysis. Perm J (2020) 24. doi: 10.7812/TPP/19.086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lamat H, Sauvant-Rochat MP, Tauveron I, Bagheri R, Ugbolue UC, Maqdasi S, et al. Metabolic syndrome and pesticides: A systematic review and meta-analysis. Environ pollut Barking Essex 1987 (2022) 305:119288. doi: 10.1016/j.envpol.2022.119288 [DOI] [PubMed] [Google Scholar]
- 26. Mathieu S, Naughton G, Descatha A, Soubrier M, Dutheil F. Dupuytren’s Disease and exposure to vibration: Systematic review and Meta-analysis. Joint Bone Spine (2020) 87(3):203−7. doi: 10.1016/j.jbspin.2020.02.001 [DOI] [PubMed] [Google Scholar]
- 27. Romito BT, Okoro EN, Ringqvist JRB, Goff KL. Burnout and wellness: the anesthesiologist’s perspective. Am J Lifestyle Med (2021) 15(2):118−25. doi: 10.1177/1559827620911645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Alameri F, Aldaheri N, Almesmari S, Basaloum M, Albeshr NA, Simsekler MCE, et al. Burnout and cardiovascular risk in healthcare professionals during the COVID-19 pandemic. Front Psychiatry (2022) 13:867233. doi: 10.3389/fpsyt.2022.867233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Azfar HS, Dzhusupov KO, Orru H, Nordin S, Nordin M, Orru K. Cardiovascular disease and mental distress among ethnic groups in Kyrgyzstan. Front Public Health (2021) 9:489092. doi: 10.3389/fpubh.2021.489092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bayes A, Tavella G, Parker G. The biology of burnout: Causes and consequences. World J Biol Psychiatry (2021) 22(9):686−98. doi: 10.1080/15622975.2021.1907713 [DOI] [PubMed] [Google Scholar]
- 31. Chang BP, Gallos G, Wasson L, Edmondson D. The unique environmental influences of acute care settings on patient and physician well-being: A call to action. J Emerg Med (2018) 54(1):e19−21. doi: 10.1016/j.jemermed.2017.08.092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Clemow LP, Pickering TG, Davidson KW, Schwartz JE, Williams VP, Shaffer JA, et al. Stress management in the workplace for employees with hypertension: A randomized controlled trial. Transl Behav Med (2018) 8(5):761−70. doi: 10.1093/tbm/iby018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Denat Y, Gokce S, Gungor H, Zencir C, Akgullu C. Relationship of anxiety and burnout with extrasystoles in critical care nurses in Turkey. Pak J Med Sci (2016) 32(1):196−200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hallman T, Burell G, Setterlind S, Odén A, Lisspers J. Psychosocial risk factors for coronary heart disease, their importance compared with other risk factors and gender differences in sensitivity. J Cardiovasc Risk (2001) 8(1):39−49. doi: 10.1177/174182670100800106 [DOI] [PubMed] [Google Scholar]
- 35. Hallman T, Thomsson H, Burell G, Lisspers J, Setterlind S. Stress, burnout and coping: differences between women with coronary heart disease and healthy matched women. J Health Psychol (2003) 8(4):433−45. doi: 10.1177/13591053030084003 [DOI] [PubMed] [Google Scholar]
- 36. Honkonen T, Ahola K, Pertovaara M, Isometsä E, Kalimo R, Nykyri E, et al. The association between burnout and physical illness in the general population–results from the Finnish Health 2000 Study. J Psychosom Res (2006) 61(1):59−66. doi: 10.1016/j.jpsychores.2005.10.002 [DOI] [PubMed] [Google Scholar]
- 37. Lin PY, Chang CC, Tung CY, Chu WH, Tong FG. Risk factors of prehypertension and hypertension among workers at public elderly welfare facilities in Taiwan: A cross-sectional survey. Med (Baltimore) (2021) 100(8):e24885. doi: 10.1097/MD.0000000000024885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Melamed S, Kushnir T, Shirom A. Burnout and risk factors for cardiovascular diseases. Behav Med (1992) 18(2):53−60. doi: 10.1080/08964289.1992.9935172 [DOI] [PubMed] [Google Scholar]
- 39. Prosdócimo ACG, Lucina LB, Marcia O, Jobs PMJ, Schio NA, Baldanzi FF, et al. Prevalence of Burnout Syndrome in patients admitted with acute coronary syndrome. Arq Bras Cardiol (2015) 104(3):218−25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Smaardijk VR, Mommersteeg PMC, Kop WJ, Adlam D, Maas AHEM. Psychological and clinical characteristics of female patients with spontaneous coronary artery dissection. J Neth Soc Cardiol Neth Heart Found (2020) 28(9):485−91. doi: 10.1007/s12471-020-01437-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sokejima S, Kagamimori S. Working hours as a risk factor for acute myocardial infarction in Japan: case-control study. BMJ (1998) 317(7161):775−80. doi: 10.1136/bmj.317.7161.775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Toker S, Melamed S, Berliner S, Zeltser D, Shapira I. Burnout and risk of coronary heart disease: a prospective study of 8838 employees. Psychosom Med (2012) 74(8):840−7. doi: 10.1097/PSY.0b013e31826c3174 [DOI] [PubMed] [Google Scholar]
- 43. Toppinen-Tanner S, Ahola K, Koskinen A, Väänänen A. Burnout predicts hospitalization for mental and cardiovascular disorders: 10-year prospective results from industrial sector. Stress Health J Int Soc Investig Stress (2009) 25(4):287−96. doi: 10.1002/smi.1282 [DOI] [Google Scholar]
- 44. Tsou MT, Pai TP, Chiang TM, Huang WH, Lin HM, Lee SC. Burnout and metabolic syndrome among different departments of medical center nurses in Taiwan-Cross-sectional study and biomarker research. J Occup Health janv (2021) 63(1):e12188. doi: 10.1002/1348-9585.12188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. von Känel R, Princip M, Holzgang SA, Fuchs WJ, van Nuffel M, Pazhenkottil AP, et al. Relationship between job burnout and somatic diseases: a network analysis. Sci Rep (2020) 10(1):18438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zhang M, Loerbroks A, Li J. Job burnout predicts decline of health-related quality of life among employees with cardiovascular disease: A one-year follow-up study in female nurses. Gen Hosp Psychiatry (2018) 50:51−3. doi: 10.1016/j.genhosppsych.2017.10.004 [DOI] [PubMed] [Google Scholar]
- 47. Zhang M, Shi Y, Yang Y, Liu L, Xiao J, Guo T, et al. Burnout is associated with poor recovery of physical performance and low quality of life in patients after their first episode of acute coronary syndrome: A hospital-based prospective cohort study. Int J Cardiol (2017) 227:503−7. doi: 10.1016/j.ijcard.2016.10.114 [DOI] [PubMed] [Google Scholar]
- 48. Malach-Pines A. The burnout measure, short version. Int J Stress Manage (2005) 12(1):78−88. doi: 10.1037/1072-5245.12.1.78 [DOI] [Google Scholar]
- 49. Schaufeli WB, Leiter MP, Maslach C, Jackson SE. The MBI-General Survey. In: Maslach C, Jackson SE, Leiter MP, editors. Maslach Burnout Inventory Manual, 3rd ed. Palo Alto (Calif)7 Consulting Psychologist Press; (1996). p. 19–26. [Google Scholar]
- 50. Sassi N, Neveu JP. Traduction et validation d’une nouvelle mesure d’épuisement professionnel: Le shirom-melamed burnout measure. [Translation and validation of a new measurement of professional exhaustion: The Shirom-Melamed Burnout Measure.]. Can J Behav Sci Rev Can Sci Comport (2010) 42(3):177−84. [Google Scholar]
- 51. Yeh WY, Cheng Y, Chen CJ, Hu PY, Kristensen TS. Psychometric properties of the Chinese version of Copenhagen burnout inventory among employees in two companies in Taiwan. Int J Behav Med (2007) 14(3):126−33. doi: 10.1007/BF03000183 [DOI] [PubMed] [Google Scholar]
- 52. Yeh WY, Cheng Y, Chen MJ, Chiu AWH. Development and validation of an occupational burnout inventory. Taiwan J Public Health (2008) 27:349−64. [Google Scholar]
- 53. Imai H. Burnout and work environments of public health nurses involved in mental health care. Occup Environ Med (2004) 61(9):764−8. doi: 10.1136/oem.2003.009134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Appels A, Höppener P, Mulder P. A questionnaire to assess premonitory symptoms of myocardial infarction. Int J Cardiol (1987) 17(1):15−24. [DOI] [PubMed] [Google Scholar]
- 55. Appels A, Mulder P. Excess fatigue as a precursor of myocardial infarction. Eur Heart J (1988) 9(7). [DOI] [PubMed] [Google Scholar]
- 56. Kannel WB. Contribution of the framingham study to preventive cardiology. J Am Coll Cardiol (1990) 15(1):206−11. [DOI] [PubMed] [Google Scholar]
- 57. Mahmood SS, Levy D, Vasan RS, Wang TJ. The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Lancet Lond Engl (2014) 383(9921):999−1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet Lond Engl (2004) 364(9438):937−52. [DOI] [PubMed] [Google Scholar]
- 59. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry (2016) 15(2):103−11. doi: 10.1002/wps.20311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Aronsson G, Gustafsson K. Sickness presenteeism: prevalence, attendance-pressure factors, and an outline of a model for research. J Occup Environ Med (2005) 47(9):958−66. doi: 10.1097/01.jom.0000177219.75677.17 [DOI] [PubMed] [Google Scholar]
- 61. Wright TA, Cropanzano R. Emotional exhaustion as a predictor of job performance and voluntary turnover. J Appl Psychol (1998) 83(3):486−93. doi: 10.1037/0021-9010.83.3.486 [DOI] [PubMed] [Google Scholar]
- 62. Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, Shah K, et al. Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Dis (2019) 6(2):19. doi: 10.3390/jcdd6020019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Norlund S, Reuterwall C, Höög J, Lindahl B, Janlert U, Birgander LS. Burnout, working conditions and gender - results from the northern Sweden MONICA Study. BMC Public Health (2010) 10:326. doi: 10.1186/1471-2458-10-326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Mirmohammadi SJ, Taheri M, Mehrparvar AH, Heydari M, Saadati Kanafi A, Mostaghaci M. Occupational stress and cardiovascular risk factors in high-ranking government officials and office workers. Iran Red Crescent Med J (2014) 16(8):e11747. doi: 10.5812/ircmj.11747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kivimäki M, Kawachi I. Work stress as a risk factor for cardiovascular disease. Curr Cardiol Rep (2015) 17(9):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Lecca LI, Campagna M, Portoghese I, Galletta M, Mucci N, Meloni M, et al. Work related stress, well-being and cardiovascular risk among flight logistic workers: an observational study. Int J Environ Res Public Health (2018) 15(9):1952. doi: 10.3390/ijerph15091952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Chou LP, Tsai CC, Li CY, Hu SC. Prevalence of cardiovascular health and its relationship with job strain: a cross-sectional study in Taiwanese medical employees. BMJ Open (2016) 6(4):e010467. doi: 10.1136/bmjopen-2015-010467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Khan N, Palepu A, Dodek P, Salmon A, Leitch H, Ruzycki S, et al. Cross-sectional survey on physician burnout during the COVID-19 pandemic in Vancouver, Canada: the role of gender, ethnicity and sexual orientation. BMJ Open (2021) 11(5):e050380. doi: 10.1136/bmjopen-2021-050380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Garcia LC, Shanafelt TD, West CP, Sinsky CA, Trockel MT, Nedelec L, et al. Burnout, depression, career satisfaction, and work-life integration by physician race/ethnicity. JAMA Netw Open (2020) 3(8):e2012762. doi: 10.1001/jamanetworkopen.2020.12762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation (2018) 137(20):2166−78. doi: 10.1161/CIRCULATIONAHA.117.029652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Di Chiara T, Scaglione A, Corrao S, Argano C, Pinto A, Scaglione R. Education and hypertension: impact on global cardiovascular risk. Acta Cardiol (2017) 72(5):507−13. doi: 10.1080/00015385.2017.1297626 [DOI] [PubMed] [Google Scholar]
- 72. Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, et al. Burnout syndrome among medical residents: A systematic review and meta-analysis. PloS One (2018) 13(11):e0206840. doi: 10.1371/journal.pone.0206840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Mitchell C, Korcarz CE, Gepner AD, Kaufman JD, Post W, Tracy R, et al. Ultrasound carotid plaque features, cardiovascular disease risk factors and events: the multi-ethnic study of atherosclerosis. Atherosclerosis (2018) 276:195−202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Post WS, Watson KE, Hansen S, Folsom AR, Szklo M, Shea S, et al. Racial/ethnic differences in all-cause and cardiovascular disease mortality: the multi-ethnic study of atherosclerosis (MESA). Circulation (2022) 146(3):229−39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Lawrence JA, Davis BA, Corbette T, Hill EV, Williams DR, Reede JY. Racial/ethnic differences in burnout: a systematic review. J Racial Ethn Health Disparities (2022) 9(1):257−69. doi: 10.1007/s40615-020-00950-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Whitehead IO, Moffatt S, Jagger C, Hanratty B. A national study of burnout and spiritual health in UK general practitioners during the COVID-19 pandemic. PloS One (2022) 17(11):e0276739. doi: 10.1371/journal.pone.0276739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Eltorki Y, Abdallah O, Riaz S, Mahmoud S, Saad M, Ez-Eldeen N, et al. Burnout among pharmacy professionals in Qatar: A cross-sectional study. PloS One (2022) 17(5):e0267438. doi: 10.1371/journal.pone.0267438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Douglas M, Coman E, Eden AR, Abiola S, Grumbach K. Lower likelihood of burnout among family physicians from underrepresented racial-ethnic groups. Ann Fam Med (2021) 19(4):342−50. doi: 10.1370/afm.2696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Woda A, Picard P, Dutheil F. Dysfunctional stress responses in chronic pain. Psychoneuroendocrinology (2016) 71:127−35. doi: 10.1016/j.psyneuen.2016.05.017 [DOI] [PubMed] [Google Scholar]
- 80. Rosmond R, Björntorp P. The hypothalamic–pituitary–adrenal axis activity as a predictor of cardiovascular disease, type 2 diabetes and stroke. J Intern Med (2000) 247(2):188−97. doi: 10.1046/j.1365-2796.2000.00603.x [DOI] [PubMed] [Google Scholar]
- 81. Gardner MP, Lightman S, Sayer AA, Cooper C, Cooper R, Deeg D, et al. Dysregulation of the hypothalamic pituitary adrenal (HPA) axis and physical performance at older ages: An individual participant meta-analysis. Psychoneuroendocrinology (2013) 38(1):40−9. doi: 10.1016/j.psyneuen.2012.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Kumari M, Shipley M, Stafford M, Kivimaki M. Association of diurnal patterns in salivary cortisol with all-cause and cardiovascular mortality: findings from the whitehall II study. J Clin Endocrinol Metab (2011) 96(5):1478−85. doi: 10.1210/jc.2010-2137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Jovanovic H, Perski A, Berglund H, Savic I. Chronic stress is linked to 5-HT(1A) receptor changes and functional disintegration of the limbic networks. NeuroImage (2011) 55(3):1178−88. [DOI] [PubMed] [Google Scholar]
- 84. Smith SM, Vale WW. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues Clin Neurosci (2006) 8(4):383−95. doi: 10.31887/DCNS.2006.8.4/ssmith [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Orosz A, Federspiel A, Haisch S, Seeher C, Dierks T, Cattapan K. A biological perspective on differences and similarities between burnout and depression. Neurosci Biobehav Rev (2017) 73:112−22. doi: 10.1016/j.neubiorev.2016.12.005 [DOI] [PubMed] [Google Scholar]
- 86. Pretty J, Rogerson M, Barton J. Green mind theory: how brain-body-behaviour links into natural and social environments for healthy habits. Int J Environ Res Public Health (2017) 14(7):E706. doi: 10.3390/ijerph14070706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Hayano J, Sakakibara Y, Yamada M, Ohte N, Fujinami T, Yokoyama K, et al. Decreased magnitude of heart rate spectral components in coronary artery disease. Its relation to angiographic severity. Circulation (1990) 81(4):1217−24. [DOI] [PubMed] [Google Scholar]
- 88. Hayano J, Yamada A, Mukai S, Sakakibara Y, Yamada M, Ohte N, et al. Severity of coronary atherosclerosis correlates with the respiratory component of heart rate variability. Am Heart J (1991) 121(4 Pt 1):1070−9. doi: 10.1016/0002-8703(91)90664-4 [DOI] [PubMed] [Google Scholar]
- 89. Mukai S, Hayano J. Heart rate and blood pressure variabilities during graded head-up tilt. J Appl Physiol Bethesda Md 1985 (1995) 78(1):212−6. [DOI] [PubMed] [Google Scholar]
- 90. Shi Y, Jiang R, Zhu C, Zhang M, Cai H, Hu Z, et al. High job burnout predicts low heart rate variability in the working population after a first episode of acute coronary syndrome. Int J Environ Res Public Health (2021) 18(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Sterne JAC, Egger M, Smith GD. Investigating and dealing with publication and other biases in meta-analysis. BMJ (2001) 323(7304):101−5. doi: 10.1136/bmj.323.7304.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Clinchamps M, Auclair C, Prunet D, Pfabigan D, Lesage FX, Baker JS, et al. Burnout among hospital non-healthcare staff: influence of job demand-control-support, and effort-reward imbalance. J Occup Environ Med (2021) 63(1):e13−20. [DOI] [PubMed] [Google Scholar]
- 93. Dutheil F, Parreira LM, Eismann J, Lesage FX, Balayssac D, Lambert C, et al. Burnout in french general practitioners: A nationwide prospective study. Int J Environ Res Public Health (2021) 18(22):12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Sérole C, Auclair C, Prunet D, Charkhabi M, Lesage FX, Baker JS, et al. The forgotten health-care occupations at risk of burnout-A burnout, job demand-control-support, and effort-reward imbalance survey. J Occup Environ Med (2021) 63(7):e416−25. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Details for the search strategy used within each database.
Details for methodological quality of included articles (Methodological assessment of studies using STROBE criteria, Methodological assessment of studies using NOS criteria) and Checklists used for quality assessment of included studies (Newcastle-Ottawa Scale (NOS) for cross-sectional studies, Newcastle-Ottawa Scale (NOS) for cohort studies, Strengthening the Reporting of Observational studies in Epidemiology (STROBE) for cross-sectional and cohort studies)
Meta-analysis using the most adjusted and crude risk of cardiovascular disease after a burnout.
Metafunnels, based on data from the most adjusted and crude risk of cardiovascular disease after a burnout.Each dot represents a single study, with its corresponding risk (x axis) and its associated standard error of the risk (y-axis). Large high-powered studies are placed towards the top, and smaller low-powered studies towards the bottom. The plot should ideally resemble a pyramid or inverted funnel, with scatter due to sampling variation. Studies outside funnel plot are likely to present bias (94).
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.