Abstract
Background
This systematic review and meta-analysis investigated the treatment for Achilles tendon rupture (ATR) associated with the lowest risk of rerupture in older patients.
Methods
Five databases were searched through September 2022 for studies published in the past 10 years analyzing operative and nonoperative ATR treatment. Studies were categorized as “nonelderly” if they reported only on patients aged 18–60 years. Studies that included at least 1 patient older than age 70 were categorized as “elderly inclusive.” Of 212 studies identified, 28 were eligible for inclusion. Of 2965 patients, 1165 were treated operatively: 429 (37%) from elderly-inclusive studies and 736 (63%) from nonelderly studies. Of the 1800 nonoperative patients 553 (31%) were from nonelderly studies and 1247 (69%) were from elderly-inclusive studies.
Results
For nonoperative treatment, the rate of rerupture was higher in nonelderly studies (83/1000 cases, 95% CI = 58, 113) than in elderly-inclusive studies (38/1000 cases, 95% CI = 22, 58; P<.001). For operative treatment no difference was found in the rate of rerupture between nonelderly studies (7/1000 cases, 95% CI = 0, 21) and elderly-inclusive studies (12/1000 cases, 95% CI = 0, 35; P<.78). Overall, operative treatment was associated with a rerupture rate of 1.5% (95% CI: 1.0%, 2.8%) (P<.001), which was lower than the 5% rate reported by other studies for nonoperative management (P<.001).
Conclusion
Older patients may benefit more than younger patients from nonoperative treatment of ATR. More studies are needed to determine the age at which rerupture rates decrease among nonoperatively treated patients.
Level of Evidence
3.
Keywords: Achilles tendon rupture, Elderly, Geriatric, Nonelderly, Nonoperative treatment, Operative repair, Rerupture rate
1. Introduction
Achilles tendon rupture (ATR) is a common injury that typically occurs during a sudden eccentric contraction of the gastrocnemius-soleus complex.1,2 This motion is frequently observed in sports such as basketball, which accounted for 48% of ATRs between August 2000 and December 2010 in the United States.2 Most ATRs occur in an area 2–6 cm from the tendon insertion site on the posterior calcaneus.1 Patients typically present with weak ankle plantarflexion and increased ankle dorsiflexion during eccentric contraction, potentially impairing their gait.1
ATR can be managed operatively or nonoperatively; it is unclear which treatment is preferable.3, 4, 5, 6 Some studies have shown a lower rate of tendon rerupture after operative treatment; however, this lower rate comes at the expense of increased risk for other complications, such as infection and sural nerve injury.7,8 Moreover, a difference in rerupture rates has not been found across all studies.3,5,6 It is also worth considering that operative treatment has not been associated with better overall outcomes compared with nonoperative treatment, which may explain the increasing popularity of nonoperative treatment.3, 4, 5, 6,9,10
Most ATRs occur during the 4th and 5th decades of life, with the second highest proportion occurring during the 6th to 8th decades of life.1 Most studies of ATR treatment exclude part, or all, of this older population—with many excluding patients older than 60 years. This exclusion is problematic considering that in the United States, between 2007 and 2011, 51% of patients older than 60 years who had ATR underwent operative treatment.11
Two studies found that older age was associated with higher complication rates, including rerupture, for both operative and nonoperative treatments.12,13 Yet a study comparing both treatment modalities and stratifying patients by age found no association between age and rerupture rate.11 Although one might be inclined to assume that older patients have worse tissue healing rates, and consequently higher rerupture rates, we could not find support for this notion in the literature.14,15 More data regarding treatment outcomes and complication rates for this age group are needed to support effective care.
In this meta-analysis, we compared rerupture rates after operative and nonoperative treatment in studies that included patients older than 70 years and those that included only patients aged 18–60 years. We also compared rerupture rates after operative and nonoperative treatments against a null hypothesis of a 5% rerupture rate, which has been reported by several meta-analyses of randomized controlled trials to be the lowest rate attainable through nonoperative treatment.3,7,8,16 Rerupture rates were also compared between the studies that included older patients against those that did not.
Considering that older age is a risk factor for acute ATR, we expected to find that operative treatment would be associated with a higher rerupture rate in elderly-inclusive studies than in nonelderly studies.17 Older age has also been associated with longer recovery times and a higher risk of postoperative complications, lending further support to this expectation.18,19 For nonoperative treatment, we expected to find a lower rerupture rate in elderly-inclusive studies than in nonelderly studies, given the decreased physical activity of many older individuals.20, 21, 22, 23
2. Methods
2.1. Ethical statement
This study used data from previously published studies and was therefore exempt from institutional review board approval. Patient consent was not required for this study given that all data were previously published.
2.2. Search strategy and study selection
The MEDLINE, Embase, Cochrane, CINAHL, and Web of Science databases were searched between July and September 2022 for systematic reviews, meta-analyses, randomized controlled trials (RCTs), prospective studies, and retrospective studies reporting operative and nonoperative ATR treatment outcomes. Search syntax is provided in Supplementary Tables.
Originally, we intended to compare only RCTs of geriatric patients with RCTs of individuals younger than 60 years, but this approach was not feasible because we were unable to find RCTs of only geriatric patients, and few studies included any geriatric patients. We then searched for retrospective studies with only geriatric patients, but this search also yielded very few results. Ultimately, the only way to perform this investigation given the available literature was to compare studies that included geriatric patients against studies that did not. Studies that included only patients aged 18 to 60 were categorized as “nonelderly” studies; studies that included at least 1 patient older than 70 were categorized as “elderly-inclusive” or “elderly” studies.
Our original search included studies published during the past 30 years, but given the recent changes in management of ATR, we decided to include studies published within the last 10 years (2012–2022) only. Studies published in languages other than English were excluded. Studies comparing 2 different operative treatments or 2 different nonoperative treatments were eligible for inclusion if the study determined there was no significant difference in patient outcomes. Operative treatments included open repair and percutaneous repair.
Duplicate studies were removed automatically using the Covidence data extraction tool (Veritas Health Innovation, Melbourne, Australia). Four reviewers (DA, JRG, RG, AV) independently screened titles and abstracts for relevance. Each publication was reviewed by at least 2 reviewers; a third reviewer was consulted if a consensus could not be reached regarding relevance. Studies deemed relevant underwent full-text review. Each publication was again reviewed by at least 2 reviewers; a third reviewer was consulted if a consensus could not be reached. Reasons for exclusion were documented, including wrong age range or no age range reported, out of publication date range, or no rerupture rate reported. We set no restrictions on the number of weeks between ATR and treatment, weightbearing status, or functional rehabilitation protocol.
After removal of duplicate studies, 212 records remained, of which, 69 were deemed potentially relevant and underwent full-text review (Supplementary Fig. 1). Ultimately, 28 publications were chosen for inclusion6,24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50 (Table 1), comprising 2965 patients, of whom 1165 (39%) were treated operatively and 1800 (61%) nonoperatively.
Table 1.
Studies of nonoperative and/or operative treatment of Achilles tendon rupture included in meta-analysis.
| First Author (Year) | N |
Age Range, years | |
|---|---|---|---|
| Patients (Treatment Group) | Reruptures (Treatment Gropup) | ||
| Myhrvold (2022) | 348 (O); 178 (N) | 2 (O); 11 (N) | 18–60 |
| Naskar (2022) | 39 (N) | 1 | 22–79 |
| Fischer (2021) | 47 (O); 29 (N) | 2 (O); 2 (N) | 21-–58 (O); 25–60 (N) |
| Nilsson (2021) | 35 (O); 41 (N) | 1 (O); 2 (N) | 25–81 (O); 27–76 (N) |
| Maempel (2020) | 140 (N) | 16 | 19–59 |
| Maempel (2020) | 33 (O); 31 (N) | 2 (O); 4 (N) | 21–59 |
| Mubark (2020) | 56 (N) | 3 | 27–81 |
| Yassin (2020) | 82 (N) | 2 | 21–91 |
| Yongliang (2020) | 36 (O) | 0 | 18–52 |
| Aujla (2019) | 442 (N) | 9 | 21–82 |
| Manent (2019) | 23 (O); 11 (N) | 0 (O); 0 (N) | 18–59 |
| Nam (2019) | 41 (O) | 0 | 19–52 |
| Ateschrang (2018) | 81 (O) | 4 | 24–76 |
| Haapasalo (2018) | 198 (N) | 11 | 22–88 |
| Reito (2018) | 210 (N) | 15 | 21–95 |
| Rungprai (2018) | 23 (O) | 0 | 20–50 |
| Lonzarić (2017) | 262 (O) | 3 | 21–83 |
| Aujla (2016) | 88 (N) | 1 | 27–80 |
| De la Fuente (2016) | 39 (O) | 2 | 20–55 |
| Renninger (2016) | 27 (O); 30 (N) | 1 (O); 2 (N) | 25–40 (O); 23–44 (N) |
| Cukelj (2015) | 60 (O); 30 (N) | 0 (O); 3 (N) | 25–40 |
| Korkmaz (2015) | 47 (N) | 7 | 32–42 |
| Barfod (2014) | 56 (N) | 5 | 26–56 |
| Jackson (2013) | 29 (O); 51 (N) | 1 (O); 2 (N) | 24–55 (O); 27–80 (N) |
| Jallageas (2013)a | 15 (O); 16 (O) | 0; 0 | 18–60; 19–71 |
| Bergkvist (2012) | 40 (N) | 4 | 18–86 |
| Hrnack (2012) | 15 (O) | 0 | 32–60 |
| Valente (2012) | 35 (O) | 0 | 21–83 |
N, nonoperative; O, operative.
All 31 patients in this study underwent operative treatment. Numbers are presented by age category.
2.3. Data extraction
Data were extracted by independent pairs of the 4 reviewers (DA, JRG, RG, AV) to a predetermined data extraction sheet. Characteristics extracted were as follows: authors, title, year of publication, age range, number of patients (operative, nonoperative, and combined), and rate of rerupture. For studies comparing treatments within the same category (e.g., open Achilles tendon repair vs. percutaneous Achilles tendon repair, both operative treatments), we pooled their data into their overall treatment category.
2.4. Primary outcome and statistical analysis
We defined the primary outcome as rerupture rate after operative or nonoperative treatment. We analyzed rerupture for both operative and nonoperative interventions. The first analysis examined within-group and between-group rerupture rates. Within-group analyses tested a null hypothesis of a 5% rerupture rate. The between-group analysis compared the rerupture rate between the operative and nonoperative interventions. To examine the association of age with rerupture, we stratified studies by age inclusivity (elderly vs nonelderly) and compared standardized rerupture rates per 1000 cases for operative and nonoperative treatments separately. Differences in mean age among elderly-inclusive studies and nonelderly studies were evaluated for significance using Welch's 2-sided t-test; standard deviations were calculated by using the range and mean.
In our final analysis, we used meta-regression to identify differences in rerupture rate accounting for age and intervention. We created 4 groups: 1) operative elderly, 2) nonoperative elderly, 3) operative nonelderly, and 4) nonoperative nonelderly. We used generalized linear mixed models, and all parameters were estimated via the restricted maximum likelihood approach. A continuity correction of 0.5 was applied in studies with zero cell frequencies, and the Clopper-Pearson confidence intervals were calculated for individual studies. Meta-analysis was performed using R statistical software, version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria) and Stata, version 18.1, software (StataCorp, College Station, TX, USA). Heterogeneity was evaluated by calculating the I2 index. I2 values of less than 25%, 26%–50%, 51%–75%, and 76%–100% were homogenous or had low, medium, and high heterogeneity levels, respectively. Given the clinical heterogeneity of the patient populations and the methodologic heterogeneity across different treatment options (e.g., open repair, percutaneous repair, functional weightbearing), a random effects model was used regardless of heterogeneity as recommended by Tufanaru et al.51 This process was then repeated for nonoperative interventions. P values < 0.05 were considered significant.
3. Results
The overall analysis of nonoperative intervention combined 19 studies with moderate heterogeneity (I2 = 54%). The nonoperative rerupture rate of 5.7%, (95% CI: 4.1%, 7.7%) was not significantly different than the standard of 5% (P = 0.40). For operative interventions, we combined 17 studies with moderate heterogeneity (I2 = 26%). The operative rerupture rate of 1.5% (95% CI: 1.0%, 2.8%) was less than the standard of 5% (P<.001).
Next, we conducted subgroup analysis and standardized the rerupture rate per 1000 cases. The overall rerupture rate was 33/1000 cases (95% CI: 21, 47), and study heterogeneity was medium-high (I2 = 61%). We found a lower rerupture rate after operative treatment of 9/1000 cases (95% CI: 1, 20) compared with 55/1000 cases (95% CI: 37, 75) after nonoperative treatment (P<.001; Fig. 1).
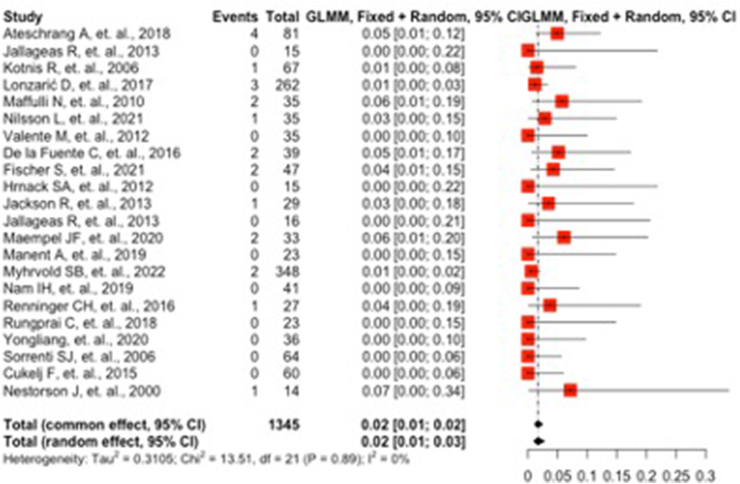
Fig. 1.
Forest plot showing the prevalence of Achilles tendon reruptures (number of reruptures per 1000 cases) after operative or nonoperative treatment.
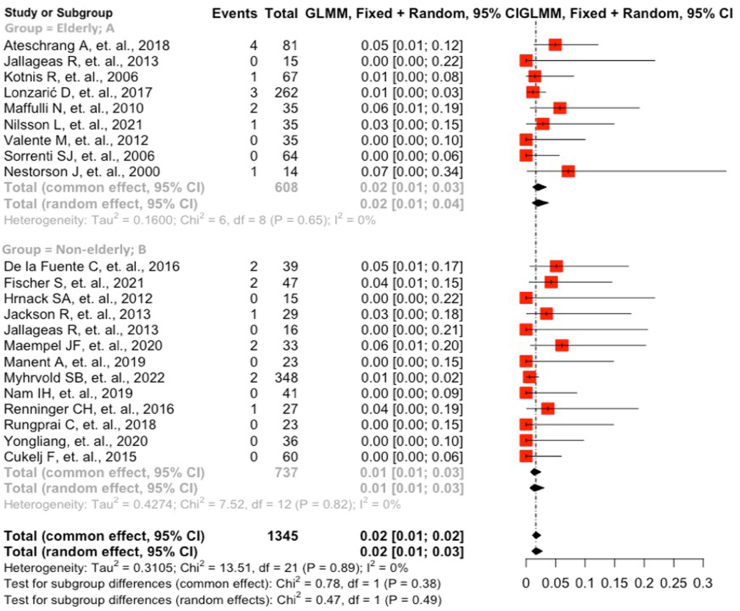
To analyze reruptures per 1000 cases of operative treatment, we used 5 elderly studies and 13 nonelderly. Study heterogeneity was moderate for both (I2 = 28% for elderly and 25% for nonelderly). Mean age in the elderly group (43 years) was higher than that in the nonelderly group (39 years) (P<.001). The overall rerupture rate was 8/1000 cases (95% CI: 1, 19), and rates did not differ between the elderly studies (12/1000 cases; 95% CI: 0, 35) and the nonelderly studies (7/1000 cases; 95% CI: 0, 21) (P<.78; Fig. 2).
Fig. 2.
Forest plot showing the prevalence of Achilles tendon reruptures (number of reruptures per 1000 cases) after operative treatment among elderly-inclusive studies (which included patients older than 70 years) and nonelderly studies (which included only patients aged 18–60 years).
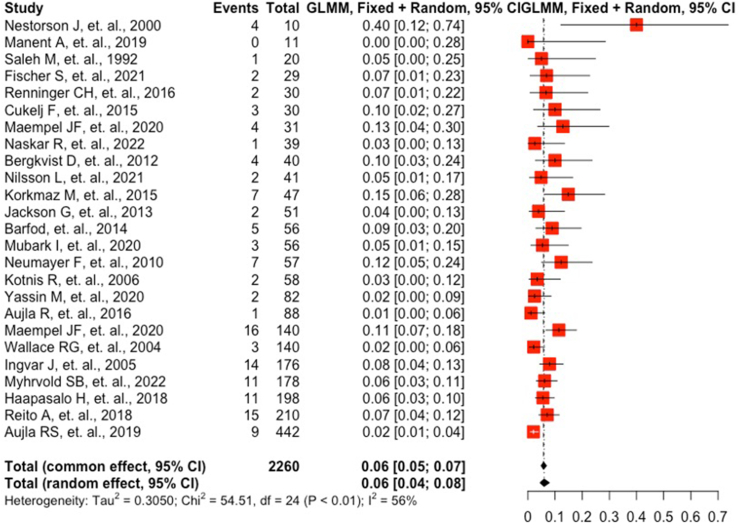
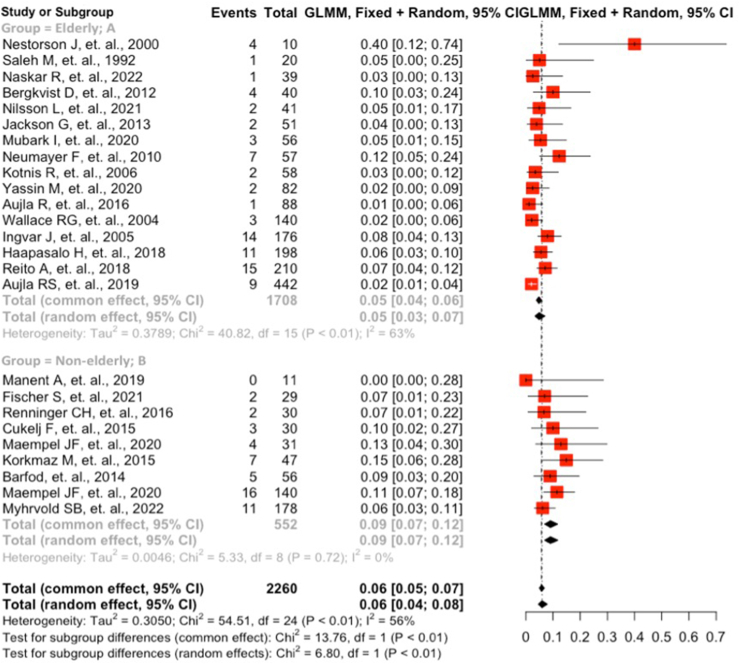
To analyze reruptures per 1000 cases of nonoperative treatment, we used 10 elderly and 9 nonelderly studies. Heterogeneity was medium-high in the elderly studies (I2 = 46%) and low in the nonelderly studies (I2 = 11%). Mean age in the elderly group (51 years) was older than in the nonelderly group (39 years) (P<.001). The overall rerupture rate was 55/1000 cases (95% CI: 37, 75). We found a higher rerupture rate of 83/1000 cases (95% CI: 58, 113) in the nonelderly studies versus 38/1000 cases (95% CI: 22, 58) in the elderly studies (P<.001; Fig. 3).
Fig. 3.
Forest plot showing the prevalence of Achilles tendon reruptures (number of reruptures per 1000 cases) after nonoperative treatment among elderly-inclusive studies (which included patients older than 70 years) and nonelderly studies (which included only patients aged 18–60 years).
In our final analysis, we used meta-regression to identify differences in rerupture rate between operatively treated, nonoperatively treated, elderly, and nonelderly patients. We found medium study heterogeneity (I2 = 59%), with an overall rerupture rate of 32/1000 cases (95% CI: 20, 46). Subroup rerupture rates ranked from high to low were as follows: 1) nonelderly-nonoperative, 83/1000 cases (95% CI: 58, 113); 2) elderly-nonoperative, 38/1000 cases (95% CI: 22, 58); 3) elderly-operative, 12/1000 cases (95% CI: 0, 35); and 4) nonelderly-operative, 7/1000 cases (95% CI: 0, 21). Pairwise comparisons using a Bonferroni adjustment showed that the nonelderly-nonoperative group had a higher rerupture rate than the elderly-nonoperative group (P = 0.01), the elderly-operative group (P = 0.001), and the nonelderly-operative group (P<.001) (Fig. 4).
Fig. 4.
Forest plot showing the prevalence of Achilles tendon reruptures (number of reruptures per 1000 cases) after operative or nonoperative treatment for elderly-inclusive studies (which included patients older than 70 years) and nonelderly studies (which included only patients aged 18–60 years).
4. Discussion
Our results suggest that older patients may benefit more than younger patients from nonoperative treatment of ATR. This difference could potentially be attributed to the decline in physical activity observed with increased age, perhaps translating to greater adherence to nonweightbearing protocols and patients being less likely to rush physical therapy and consequently reinjure themselves.20, 21, 22, 23 We found no difference between the overall rate of rerupture after nonoperative treatment and the null hypothesis of a 5% rerupture rate, suggesting that our nonoperative rerupture rate was similar to those reported by previous studies.3,7,8,16 This finding served as a measure of internal validity and indicates that the nonoperative results were not simply attributable to methodological errors. The lowest rerupture rate (1.5%) occurred after operative treatment and was significantly lower than the standard 5% rate. This result was also expected given the existing evidence,7,8 providing a second measure of internal validity and indicating that the operative results were not attributable to methodological errors. With the data available, no difference could be detected in the rerupture rate between age groups after operative treatment, implying that age did not affect the operative repair of Achilles tendon rupture.
This study supports the results of Reito et al.44 and Wang et al.,11 who found that age alone was a poor predictor of rerupture, implying that the risk of effect modification from age is low. Therefore, studies investigating treatment of ATR should not routinely exclude older patients. Instead, future studies should include elderly patients, who are underrepresented in the current literature and warrant more direct outcome measurements.
The age range we specified was an attempt to ensure the elderly group was substantially older than the nonelderly group. Although the difference was significant, the clinical relevance of this difference is unclear.
This study has several limitations, the biggest of which is the indirect nature of our analysis; we compared the rerupture rate of elderly-inclusive studies with that of nonelderly studies rather than directly comparing the rerupture rate among elderly patients with that of nonelderly patients. This approach prevents us from conclusively establishing a relationship between ATR treatment outcomes and patient age. Second, because most studies excluded patients older than 60 years, the number of publications available for analysis was limited. We found no studies that included only geriatric patients; therefore, we were unable to perform direct analysis of the outcomes in that population. Third, there was an inherent bias in the literature, with nonoperative studies being more likely to include geriatric patients than operative studies. Even among the elderly-inclusive studies, the nonoperative subgroup had a older mean age (51 years) than the operative subgroup (43 years). This difference reflects the previous finding that elderly patients are more likely to receive nonoperative than operative treatment.12,15,52
Lastly, to increase generalizability, we did not control for postoperative physical therapy regimens or other nonoperative treatments. However, this omission may have limited the impact of “better” regimens, such as the functional rehabilitation protocol mentioned earlier. Therefore, our results may not accurately reflect a comparison between the 2 best treatment options currently available.
5. Conclusions
Clinical decisions regarding treatment of ATR are not based exclusively on risk of rerupture. The findings in this study provide further support for the use of operative treatments in younger patients and nonoperative treatments in older patients.
Guardian/patient's consent
This item is not applicable because this study was a review of anonymized data.
Ethical statement
This study was not subject to institutional review board approval because it was a review of anonymized data.
Funding statement
This work was supported by the National Institute on Aging, Medical Student Training in Aging Research Summer Program grant (grant number 2T35AG026758).
CRediT authorship contribution statement
Daniel Acevedo: Conceptualization, Methodology, Software, Investigation, Resources, Data curation, Writing – original draft, Writing – review & editing, Visualization, Supervision, Project administration, Funding acquisition. Jose R. Garcia: Investigation, Data curation, Writing – review & editing. Rajvarun S. Grewal: Investigation, Data curation, Writing – review & editing. Ashish Vankara: Investigation, Data curation, Writing – review & editing. Christopher J. Murdock: Methodology, Validation, Writing – review & editing, Visualization, Supervision. Patrick C. Hardigan: Formal analysis, Data curation, Writing – original draft, Visualization. Amiethab A. Aiyer: Conceptualization, Methodology, Validation, Writing – review & editing, Visualization, Supervision, Funding acquisition.
Declaration of competing interest
D Acevedo reports grants from the National Institute of Aging Medical Student Training in Aging Research Summer Program during the conduct of the study. AA Aiyer reports personal fees from Vilex and Smith & Nephew, outside the submitted work; is a board or committee member of the American Orthopaedic Foot and Ankle Society; receives publishing royalties, financial or material support from DeLee & Drez's Orthopaedic Sports Medicine (Elsevier) and Miller's Review of Orthopaedics (Elsevier); and is on the editorial or governing board of the Journal of Bone and Joint Surgery-British. The remaining authors have nothing to disclose.
Acknowledgments
For editorial assistance, we thank Rachel Walden, MS, in the Editorial Services group of The Johns Hopkins Department of Orthopaedic Surgery. For preparing the search syntax and compiling database results, we thank Breck Turner, MS, of the Welch Medical Library at The Johns Hopkins School of Medicine.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2024.02.034.
Contributor Information
Daniel Acevedo, Email: acevedodaniel5100@gmail.com.
Jose R. Garcia, Email: jg2710@mynsu.nova.edu.
Rajvarun S. Grewal, Email: rajvarung@gmail.com.
Ashish Vankara, Email: avankar1@jhmi.edu.
Christopher J. Murdock, Email: cmurdoc5@jhmi.edu.
Patrick C. Hardigan, Email: patrick@nova.edu.
Amiethab A. Aiyer, Email: aaiyer2@jhmi.edu.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Pedowitz D., Kirwan G. Achilles tendon ruptures. Curr Rev Musculoskelet Med. 2013;6(4):285–293. doi: 10.1007/s12178-013-9185-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raikin S.M., Garras D.N., Krapchev P.V. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34(4):475–480. doi: 10.1177/1071100713477621. [DOI] [PubMed] [Google Scholar]
- 3.Soroceanu A., Sidhwa F., Aarabi S., Kaufman A., Glazebrook M. Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am. 2012;94(23):2136–2143. doi: 10.2106/JBJS.K.00917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ochen Y., Beks R.B., van Heijl M., et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364 doi: 10.1136/bmj.k5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holm C., Kjaer M., Eliasson P. Achilles tendon rupture--treatment and complications: a systematic review. Scand J Med Sci Sports. 2015;25(1):e1–e10. doi: 10.1111/sms.12209. [DOI] [PubMed] [Google Scholar]
- 6.Myhrvold S.B., Brouwer E.F., Andresen T.K.M., et al. Nonoperative or surgical treatment of acute Achilles' tendon rupture. NEJM. 2022;386(15):1409–1420. doi: 10.1056/NEJMoa2108447. [DOI] [PubMed] [Google Scholar]
- 7.Jiang N., Wang B., Chen A., Dong F., Yu B. Operative versus nonoperative treatment for acute Achilles tendon rupture: a meta-analysis based on current evidence. Int Orthop. 2012;36(4):765–773. doi: 10.1007/s00264-011-1431-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khan R.J., Carey Smith R.L. Surgical interventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev. 2010;9:CD003674. doi: 10.1002/14651858.CD003674.pub4. [DOI] [PubMed] [Google Scholar]
- 9.Egger A.C., Berkowitz M.J. Achilles tendon injuries. Curr Rev Musculoskelet Med. 2017;10(1):72–80. doi: 10.1007/s12178-017-9386-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ganestam A., Kallemose T., Troelsen A., Barfod K.W. Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. A nationwide registry study of 33,160 patients. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3730–3737. doi: 10.1007/s00167-015-3544-5. [DOI] [PubMed] [Google Scholar]
- 11.Wang D., Sandlin M.I., Cohen J.R., Lord E.L., Petrigliano F.A., SooHoo N.F. Operative versus nonoperative treatment of acute Achilles tendon rupture: an analysis of 12,570 patients in a large healthcare database. Foot Ankle Surg. 2015;21(4):250–253. doi: 10.1016/j.fas.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 12.Nestorson J., Movin T., Möller M., Karlsson J. Function after Achilles tendon rupture in the elderly: 25 patients older than 65 years followed for 3 years. Acta Orthop Scand. 2000;71(1):64–68. doi: 10.1080/00016470052943928. [DOI] [PubMed] [Google Scholar]
- 13.Stavenuiter X.J.R., Lubberts B., Prince R.M., Johnson A.H., DiGiovanni C.W., Guss D. Postoperative complications following repair of acute Achilles tendon rupture. Foot Ankle Int. 2019;40(6):679–686. doi: 10.1177/1071100719831371. [DOI] [PubMed] [Google Scholar]
- 14.Narici M.V., Maffulli N., Maganaris C.N. Ageing of human muscles and tendons. Disabil Rehabil. 2008;30(20-22):1548–1554. doi: 10.1080/09638280701831058. [DOI] [PubMed] [Google Scholar]
- 15.Maffulli N., Barrass V., Ewen S.W. Light microscopic histology of Achilles tendon ruptures. A comparison with unruptured tendons. Am J Sports Med. 2000;28(6):857–863. doi: 10.1177/03635465000280061401. [DOI] [PubMed] [Google Scholar]
- 16.Wilkins R., Bisson L.J. Operative versus nonoperative management of acute Achilles tendon ruptures: a quantitative systematic review of randomized controlled trials. Am J Sports Med. 2012;40(9):2154–2160. doi: 10.1177/0363546512453293. [DOI] [PubMed] [Google Scholar]
- 17.Kannus P., Natri A. Etiology and pathophysiology of tendon ruptures in sports. Scand J Med Sci Sports. 1997;7(2):107–112. doi: 10.1111/j.1600-0838.1997.tb00126.x. [DOI] [PubMed] [Google Scholar]
- 18.Lin H.S., Watts J.N., Peel N.M., Hubbard R.E. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr. 2016;16(1):157. doi: 10.1186/s12877-016-0329-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deiner S., Silverstein J.H. Long-term outcomes in elderly surgical patients. Mt Sinai J Med. 2012;79(1):95–106. doi: 10.1002/msj.21288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hallal P.C., Andersen L.B., Bull F.C., et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 21.Notthoff N., Reisch P., Gerstorf D. Individual characteristics and physical activity in older adults: a systematic review. Gerontology. 2017;63(5):443–459. doi: 10.1159/000475558. [DOI] [PubMed] [Google Scholar]
- 22.Ingram D.K. Age-related decline in physical activity: generalization to nonhumans. Med Sci Sports Exerc. 2000;32(9):1623–1629. doi: 10.1097/00005768-200009000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Sun F., Norman I.J., While A.E. Physical activity in older people: a systematic review. BMC Publ Health. 2013;13(1):449. doi: 10.1186/1471-2458-13-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ateschrang A., Körner D., Joisten K., et al. Incidence and risk factors for postoperative Achilles tendon calcifications after percutaneous repair. Arch Orthop Trauma Surg. 2018;138(2):203–210. doi: 10.1007/s00402-017-2829-1. [DOI] [PubMed] [Google Scholar]
- 25.Aujla R., Kumar A., Bhatia M. Non-surgical treatment of Achilles rupture: does duration in functional weight bearing orthosis matter? Foot Ankle Surg. 2016;22(4):254–258. doi: 10.1016/j.fas.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 26.Aujla R.S., Patel S., Jones A., Bhatia M. Non-operative functional treatment for acute Achilles tendon ruptures: the leicester Achilles management protocol (LAMP) Injury. 2019;50(4):995–999. doi: 10.1016/j.injury.2019.03.007. [DOI] [PubMed] [Google Scholar]
- 27.Barfod K.W., Bencke J., Lauridsen H.B., Ban I., Ebskov L., Troelsen A. Nonoperative dynamic treatment of acute Achilles tendon rupture: the influence of early weight-bearing on clinical outcome: a blinded, randomized controlled trial. J Bone Joint Surg Am. 2014;96(18):1497–1503. doi: 10.2106/JBJS.M.01273. [DOI] [PubMed] [Google Scholar]
- 28.Bergkvist D., Åström I., Josefsson P.O., Dahlberg L.E. Acute Achilles tendon rupture: a questionnaire follow-up of 487 patients. J Bone Joint Surg Am. 2012;94(13):1229–1233. doi: 10.2106/JBJS.J.01601. [DOI] [PubMed] [Google Scholar]
- 29.Cukelj F., Bandalovic A., Knezevic J., Pavic A., Pivalica B., Bakota B. Treatment of ruptured Achilles tendon: operative or non-operative procedure? Injury. 2015;46(Suppl 6):S137–S142. doi: 10.1016/j.injury.2015.10.070. [DOI] [PubMed] [Google Scholar]
- 30.De la Fuente C., Peña y Lillo R., Carreño G., Marambio H. Prospective randomized clinical trial of aggressive rehabilitation after acute Achilles tendon ruptures repaired with Dresden technique. Foot. 2016;26:15–22. doi: 10.1016/j.foot.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 31.Fischer S., Colcuc C., Gramlich Y., et al. Prospective randomized clinical trial of open operative, minimally invasive and conservative treatments of acute Achilles tendon tear. Arch Orthop Trauma Surg. 2021;141(5):751–760. doi: 10.1007/s00402-020-03461-z. [DOI] [PubMed] [Google Scholar]
- 32.Haapasalo H., Peltoniemi U., Laine H.J., Kannus P., Mattila V.M. Treatment of acute Achilles tendon rupture with a standardised protocol. Arch Orthop Trauma Surg. 2018;138(8):1089–1096. doi: 10.1007/s00402-018-2940-y. [DOI] [PubMed] [Google Scholar]
- 33.Hrnack S.A., Crates J.M., Barber F.A. Primary Achilles tendon repair with mini-dorsolateral incision technique and accelerated rehabilitation. Foot Ankle Int. 2012;33(10):848–851. doi: 10.3113/FAI.2012.0848. [DOI] [PubMed] [Google Scholar]
- 34.Jackson G., Sinclair V.F., McLaughlin C., Barrie J. Outcomes of functional weight-bearing rehabilitation of Achilles tendon ruptures. Orthopedics. 2013;36(8):e1053–e1059. doi: 10.3928/01477447-20130724-23. [DOI] [PubMed] [Google Scholar]
- 35.Jallageas R., Bordes J., Daviet J.C., Mabit C., Coste C. Evaluation of surgical treatment for ruptured Achilles tendon in 31 athletes. Orthop Traumatol Surg Res. 2013;99(5):577–584. doi: 10.1016/j.otsr.2013.03.024. [DOI] [PubMed] [Google Scholar]
- 36.Korkmaz M., Erkoc M.F., Yolcu S., Balbaloglu O., Öztemur Z., Karaaslan F. Weight bearing the same day versus non-weight bearing for 4 weeks in Achilles tendon rupture. J Orthop Sci. 2015;20(3):513–516. doi: 10.1007/s00776-015-0710-z. [DOI] [PubMed] [Google Scholar]
- 37.Lonzarić D., Kruščić A., Dinevski D., Povalej Bržan P., Jesenšek Papež B. Primary surgical repair of acute Achilles tendon rupture: comparative results of three surgical techniques. Wien Klin Wochenschr. 2017;129(5-6):176–185. doi: 10.1007/s00508-016-1158-7. [DOI] [PubMed] [Google Scholar]
- 38.Maempel J.F., Clement N.D., Duckworth A.D., Keenan O.J.F., White T.O., Biant L.C. A randomized controlled trial comparing traditional plaster cast rehabilitation with functional walking boot rehabilitation for acute Achilles tendon ruptures. Am J Sports Med. 2020;48(11):2755–2764. doi: 10.1177/0363546520944905. [DOI] [PubMed] [Google Scholar]
- 39.Manent A., López L., Corominas H., et al. Acute Achilles tendon ruptures: efficacy of conservative and surgical (percutaneous, open) treatment-a randomized, controlled, clinical trial. J Foot Ankle Surg. 2019;58(6):1229–1234. doi: 10.1053/j.jfas.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 40.Mubark I, Abouelela A, Arya S, et al. Achilles tendon rupture: can the tendon gap on ultrasound scan predict the outcome of functional rehabilitation program? Cureus. 12(9):e10298. doi:10.7759/cureus.10298. [DOI] [PMC free article] [PubMed]
- 41.Nam I.H., Park Y.U., Cho J.H., Lee D.H., Min K.J. Comparison between early functional rehabilitation and cast immobilization after minimally invasive repair for an acute Achilles tendon rupture. J Foot Ankle Surg. 2019;58(4):628–631. doi: 10.1053/j.jfas.2018.12.024. [DOI] [PubMed] [Google Scholar]
- 42.Naskar R., Oliver L., Velazquez-Ruta P., Dhinsa B., Southgate C. Functional outcome of early weight bearing for acute Achilles tendon rupture treated conservatively in a weight-bearing orthosis. Foot Ankle Surg. 2022;28(5):595–602. doi: 10.1016/j.fas.2021.06.008. [DOI] [PubMed] [Google Scholar]
- 43.Nilsson L., Thorlund J.B., Kjær I.L., Kazlauskas A., Christensen M. Long-term follow-up after acute Achilles tendon rupture - does treatment strategy influence functional outcomes? Foot. 2021;47 doi: 10.1016/j.foot.2020.101769. [DOI] [PubMed] [Google Scholar]
- 44.Reito A., Logren H.L., Ahonen K., Nurmi H., Paloneva J. Risk factors for failed nonoperative treatment and rerupture in acute Achilles tendon rupture. Foot Ankle Int. 2018;39(6):694–703. doi: 10.1177/1071100717754042. [DOI] [PubMed] [Google Scholar]
- 45.Renninger C.H., Kuhn K., Fellars T., Youngblood S., Bellamy J. Operative and nonoperative management of Achilles tendon ruptures in active duty military population. Foot Ankle Int. 2016;37(3):269–273. doi: 10.1177/1071100715615322. [DOI] [PubMed] [Google Scholar]
- 46.Rungprai C., Phisitkul P. Outcomes and complications following endoscopically assisted percutaneous Achilles tendon repair. Arthroscopy. 2018;34(4):1262–1269. doi: 10.1016/j.arthro.2017.09.027. [DOI] [PubMed] [Google Scholar]
- 47.Valente M., Crucil M., Alecci V., Frezza G. Minimally invasive repair of acute Achilles tendon ruptures with Achillon device. Musculoskelet Surg. 2012;96(1):35–39. doi: 10.1007/s12306-011-0158-z. [DOI] [PubMed] [Google Scholar]
- 48.Yassin M., Myatt R., Thomas W., Gupta V., Hoque T., Mahadevan D. Does size of tendon gap affect patient-reported outcome following Achilles tendon rupture treated with functional rehabilitation? Bone Joint Lett J. 2020;102-B(11):1535–1541. doi: 10.1302/0301-620X.102B11.BJJ-2020-0908.R1. [DOI] [PubMed] [Google Scholar]
- 49.Yongliang Y., Honglei J., Wupeng Z., et al. Intraoperative ultrasonography assistance for minimally invasive repair of the acute Achilles tendon rupture. J Orthop Surg Res. 2020;15(1):258. doi: 10.1186/s13018-020-01776-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maempel J.F., Clement N.D., Wickramasinghe N.R., Duckworth A.D., Keating J.F. Operative repair of acute Achilles tendon rupture does not give superior patient-reported outcomes to nonoperative management. Bone Joint Lett J. 2020;102-B(7):933–940. doi: 10.1302/0301-620X.102B7.BJJ-2019-0783.R3. [DOI] [PubMed] [Google Scholar]
- 51.Tufanaru C., Munn Z., Stephenson M., Aromataris E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int J Evid Base Healthc. 2015;13(3):196–207. doi: 10.1097/XEB.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 52.Erickson B.J., Cvetanovich G.L., Nwachukwu B.U., et al. Trends in the management of Achilles tendon ruptures in the United States Medicare population, 2005-2011. Orthop J Sports Med. 2014;2(9) doi: 10.1177/2325967114549948. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.