Abstract
Methylmalonic acidemia cblB type (MMA cblB) is an autosomal recessive inborn error of amino acid metabolism that results in impaired synthesis of adenosylcobalamin, a cofactor of methylmalonyl‐CoA mutase. It presents with episodes of coma, vomiting, hypotonia, metabolic acidosis, and hyperammonemia. End‐stage kidney disease is a long‐term complication. Treatments include vitamin B12 supplementation, L‐carnitine, and a low‐protein diet. Liver, kidney, or combined liver‐kidney transplantations are promising options, but they are not without complications. We report a patient suffering from MMA cblB who developed end‐stage kidney disease at 18 years of age. Kidney transplantation allowed him to recover normal kidney function and good metabolic control. Unfortunately, after two decades, he developed non‐Hodgkin lymphoma and severe chemotherapy toxicity which led to his death. The risk of lymphoproliferative diseases is known to increase after solid organ transplantation. However, in MMA, factors including mitochondrial dysfunction and oncometabolites, may further increase the risk of malignancy and drug toxicity. Our report highlights the importance of considering the increased risk of cancer in long‐term follow‐up of MMA cblB patients, especially after solid organ transplantation. Moreover, when chemotherapy is needed, the increased risk of toxicity and metabolic decompensation should be considered and monitored.
Keywords: chemotherapy toxicity, immunosuppression, kidney transplantation, methylmalonic acidemia, mitochondrial dysfunction, post‐transplant lymphoproliferative disorders
Synopsys.
Patients with methylmalonic acidemia have an increased risk of cancer, especially after solid organ transplantation, and increased susceptibility to chemotherapy toxicity.
1. INTRODUCTION
Methylmalonic acidemia cblB type (MMA cblB, OMIM 251110) is an autosomal recessive disease, due to variants in the MMAB gene (OMIM 607568) encoding the mitochondrial enzyme ATP:cobalamin adenosyltransferase, which converts cobalamin to adenosylcobalamin using ATP. Adenosylcobalamin is cofactor for methylmalonyl‐CoA mutase (MCM), which converts L‐methylmalonyl‐CoA into succinyl‐CoA that then enters the tricarboxylic acid cycle. 1 , 2
MMA cblB can present as early‐onset acute neonatal decompensation or as late‐onset symptoms including failure to thrive, anorexia, vomiting, and developmental delay. 3 , 4 The disease is included in the newborn screening panel in many countries, including Italy. 5 , 6 , 7
Management includes vitamin B12 supplementation (only for responsive patients), a low‐protein high‐energy diet, L‐carnitine supplementation, N‐carbamylglutamate, and antibiotics used intermittently to reduce propionate production by the gut flora. 3 , 8 , 9 , 10
Despite treatment, these patients can develop a variety of long‐term complications, including progressive renal disease (tubulointerstitial nephritis due to secondary mitochondrial disease), which commonly reaches end‐stage kidney disease during childhood or adolescence. 11 , 12 Liver, kidney, or combined liver‐kidney transplantations are considered an alternative to medical treatment. Kidney transplantation corrects renal failure and provides partial enzymatic activity. 13 , 14 , 15
A previous study by Brassier et al. demonstrated that kidney transplantation decreased urinary and plasma methylmalonic acid levels, reducing the number of metabolic decompensations and increasing the dietary protein allowance. However, the risk of metabolic decompensation is not entirely suppressed, presumably because enzymatic activity is insufficient in case of intercurrent diseases. 16 Moreover, these procedures are not without danger and entail severe challenges, such as the need for prolonged immunosuppression. Post‐transplant lymphoproliferative disorders (PTLD) represent one of the most feared and fatal complications following kidney transplantation, occurring in about 1% of patients. 17 Recent studies have evaluated specific short‐term complications of post‐transplantation immunosuppression in MMA patients, including acute/subacute neurological complications such as posterior reversible encephalopathy syndrome (PRES) 18 ; meanwhile, less is known about long‐term risks, such as malignancies. Furthermore, little is known about the management of malignancies in MMA patients and chemotherapy toxicity in the context of mitochondrial impairment and increased cellular oxidative stress.
We report the case of a patient with cblB MMA who developed non‐Hodgkin lymphoma more than 20 years after received a kidney transplantation, and experienced severe chemotherapy toxicity that led to his death.
2. CASE REPORT
The patient, an Italian male born in 1983 from non‐consanguineous parents, was diagnosed with MMA at the age of 1 month after an episode of severe ketoacidosis. Urinary organic acid analysis showed increased level of methylmalonic and methylcitric acids. Molecular examination revealed a homozygous variant of the MMAB gene (c.556C>T, p.R186W—courtesy of Professor MR Baumgartner, Zurich), confirming the diagnosis of cblB MMA. Both parents were carriers of this variant.
Despite the low‐protein diet (1–1.5 g/kg/day) and pharmacological therapy with L‐carnitine (100 mg/kg/die), he developed progressive kidney failure and required peritoneal dialysis at the age of 18 years. After 6 months of dialysis, he received a kidney transplantation from a deceased donor, with normalization of renal function (creatinine 1 mg/dL, eGFR according to Cockcroft‐Gault: 118.6 mL/m2). He was immunosuppressed with basiliximab, followed by steroids (withdrawn 1 year after transplantation), tacrolimus bid, and mycophenolate mofetil, modulated over time based on therapeutic drug monitoring and the health of the transplanted organ (tacrolimus 2.5–3 mg/day with serum levels ranging from 5 to 7 ng/mL, mycophenolate mofetil 500–750 mg/day). The immediate post‐transplantation course was complicated by two episodes of syncope followed by seizures. The patient was admitted to a local hospital and underwent an (unremarkable) CT scan, before being transferred to our center. Neurological examination at admission was normal. Brain MRI showed bilateral lesions in the tegmentum and pons, which were present also in diffusion weighted imaging, and were consistent with recent stroke‐like lesions. Antiepileptic treatment with oxcarbazepine resolved seizures, and was suspended after 10 years of treatment. Several episodes of tonsillitis occurred 5 years after transplantation, and the infection was resolved with radiofrequency treatments.
The patient continued a low protein diet (45 g/day) and carnitine supplementation (100 mg/kg/die) for management of the metabolic disease. Metabolic parameters improved greatly after transplantation, with reduced plasma MMA and increased urinary excretion (Table 1, Figure 1). The patient did not experience episodes of acute decompensation. He had normal academic achievement, autonomy, and socio‐professional integration. He earned a degree in biology and was employed as laboratory assistant.
TABLE 1.
Clinic and metabolic parameters over time.
| Protein intake | Therapy | Kidney function | Plasma MMA μmol/l (nv 0–2) a | Urine MMA mmol/mol crea (nv 0.1–5) a | Clinical features/complications | |
|---|---|---|---|---|---|---|
| 6 months pre‐kidney transplantation | 30 g/day | L‐carnitine 100 mg/kg | eGFR <15 mL/m2 | 1426.2 (244.5–4094.8) | 564.7 (145.2–934.3) | End stage renal disease |
| 6 months post‐kidney transplantation | 45 g/day | L‐carnitine 100 mg/kg, steroid, tacrolimus, mycophenolate mofetil | eGFR 118.6 mL/m2 | 488.31 (67–93.3) | 1830.4 (613.2–4332.9) | Seizures (tacrolimus toxicity) |
| Last 5 years | 45 g/day | L‐carnitine 100 mg/kg, tacrolimus, mycophenolate mofetil | eGFR 44.6 mL/m2 | 1806.68 (942.2–2802.7) | 5234.8 (2549.5–8529) | Progressive kidney disease, acidosis |
| Last 6 months | 45 g/day | L‐carnitine 100 mg/kg, tacrolimus, R‐CHOP | eGFR 21.4 mL/m2 | 3549.8 | 1830.3 | Non‐Hodgkin lymphoma, metabolic decompensation |
Abbreviation: MMA, methylmalonic acid.
Mean and range.
FIGURE 1.
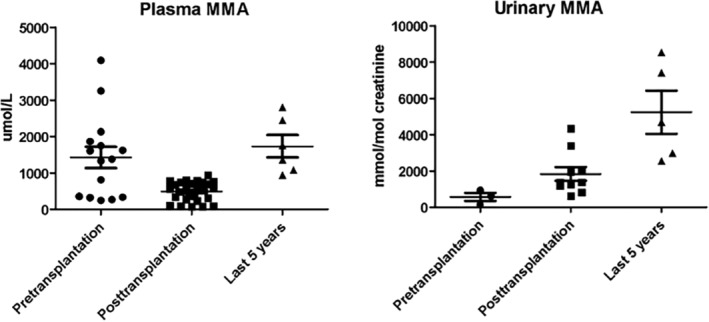
Plasma and urinary methylmalonic acid levels pre‐kidney transplantation and during short‐ and long‐term follow up. Plasma methylmalonic was greatly reduced after kidney transplantation, while urinary methylmalonic increased due to improved kidney function. Both parameters worsened during long‐term follow‐up.
After 10 years, kidney function progressively worsened (creatinine reached 2–2.2 mg/dL, eGFR 49.1–44.6 mL/m2, without proteinuria at the urine analysis); a renal biopsy was not performed. The patient had chronic acidosis (HCO3 − 15.9–18.2 mEq/L, nv 22.0–26.0; Base Excess – 12.2/−6.8 mEq/L, nv −5/+5) that required sodium bicarbonate supplementation (7.5 g/day in three doses). Metabolic parameters worsened (Table 1, Figure 1), with increase of plasma and urinary MMA, but he never developed acute ketoacidosis episodes. He continued immunosuppression with tacrolimus (serum level maintained between 5 and 7 ng/mL) and mycophenolate mofetil. In the same period, he had a chicken pox infection complicated by kerato‐uveitis of the right eye with severe decrease of visus. Treatment with oral valacyclovir led to progressive but partial restoration of visus; immunosuppressive therapy was unmodified.
At age 39, during routine follow‐up, abdominal ultrasound revealed a mass in the cecal region. Endoscopy revealed concentric stenosis with ulcers in the ascending colon. Histological examination revealed centrogerminative diffuse large B cell lymphoma (DLBCL). Immunohistochemistry was negative for bcl2 and myc. Immunostaining was negative for Human herpes virus 8 and in situ hybridization was negative for Epstein–Barr virus (EBV) RNA. Staging tests were performed. Abdominal CT scan showed a concentric parietal mass of the ascending colon, measuring 16 × 10 cm2 and involving the mesentery, with intense 18F‐FDG accumulation on PET (SUV max 18.38). There was no bone marrow or central nervous system involvement. Advanced stage (IV E gut IPI2) DLBCL was diagnosed. Serum E‐Barr virus DNA was negative as well. The patient was followed at a local hospital.
After diagnosis, mycophenolate mofetil was immediately discontinued and after 1 month the patient started chemotherapy according to the R‐CHOP protocol (2 cycles of rituximab +6 cycles of cyclophosphamide, vincristine, and doxorubicin). Urinary MMA was unchanged. After the second cycle, the patient developed severe pancytopenia and kidney failure (creatinine 4.58 mg/dL, eGFR 21.4 mL/m2), and was treated with transfusions of platelets and red blood cells and IV hydration. At the third cycle, the dosage of chemotherapy drugs was reduced (75%) but the patient presented again pancytopenia, fever, and kidney failure, treated with transfusions, antibiotics, and IV hydration. He also developed sensory neuropathy in the hands and feet attributed to vincristine. Despite the toxicity, restaging with PET‐TC scan showed marked both dimensional and metabolic response of the abdominal lesion (7 mm, SUV max 3.6). The IV cycle of chemotherapy was performed at reduced dosages.
After a few days, the patient presented confusion, dyspnea, and tachypnea. At admission, blood tests showed severe metabolic acidosis with high lactic acid (pH 6.91, nv 7.35–7.45; HCO3 − 3.7 mEq/L, nv 22.0–26.0; Base Excess −28.9 mEq/L, nv −5/+5; Anion gap 47.6 mEq/L, nv 8–16; Lac 23.39 mmol/L nv 0.8–2.0), and hyperglycemia (glucose 367 mg/dL), treated with insulin and hemodiafiltration, with normalization within 24 h. Brain CT scan revealed symmetrical hypodense lesions of the caudate nuclei, typical of MMA. Chest CT showed a left basal consolidation, that, associated with leukocytosis (49.840/mm2) and increased CRP (19 mg/dL), led to diagnosis of pneumonia. Due to immunodepression status, patient was treated with meropenem, linezolid, and liposomal amphotericin B.
Despite the therapy, after 2 days he developed cardiorespiratory insufficiency for which he was admitted to the intensive care unit and mechanically ventilated. After 10 days, the course was complicated by pulmonary embolism, treated with anticoagulation. Suspected hypoxic/ischemic brain lesions prompted a CT scan, which revealed massive hemorrhage in the left basal ganglia, with edema and the presence of the “swirl sign” (indicator of active bleeding and predictor of poor outcome); similar hemorrhagic lesions were present in the caudate and lenticular nuclei of the right basal ganglia; hydrocephalus with blood inside the left lateral ventricle, third and fourth ventricle; severe edema enhanced by the compressive effect of the hemorrhages. The patient died the next day, 4 months after being diagnosed with lymphoma. No additional data regarding MMA values were available.
3. DISCUSSION
We report a case of non‐Hodgkin lymphoma (NHL) in the long‐term follow‐up of a patient with cblB MMA, after kidney transplantation.
In addition to the highest risk of cancer in kidney transplanted patients, compared to the general population, 19 several factors in patients with MMA may increase the risk of malignancy.
Case reports of liver and kidney cancer in MMA patients exist. Forny et al. described 5 cases of liver neoplasm in early onset MMA patients, including a cblB MMA patient. This latter required hemodialysis since 16 year‐old for stage 4 chronic kidney disease. After 6 years, she presented severe metabolic decompensation and passed away a few days later. A postmortem report confirmed hepatocellular carcinoma. Two other cases had chronic kidney disease before the development of liver tumors. One of them developed hepatoblastoma at the age of 11 years, 18 months after kidney transplantation. His neurological condition worsened, with bilateral pallidum lesions. During chemotherapy, plasma ammonia increased up to 150 μmol/L, as well as lactatemia (12.5 mmol/L) and glycemia. The patient died from toxicity within 3 weeks of initiating chemotherapy. 20 , 21 , 22 The last two cases presented early development of hepatoblastoma (4 and 19 months of age). One of them experienced very pronounced toxicity from chemotherapy, with severe metabolic acidosis and hyperglycemia. Finally, Potter et al. described a renal cell carcinoma in a 6‐year‐old patient with methylmalonic acidemia (MUT gene) and stage 4 chronic kidney disease. 23
These cases highlight some very important aspects in the management of patients with MMA: there may be a greater cancer risk, there seems to be an association with end‐stage renal disease (however, this may be linked to older age and more serious MMA disease in patients who develop cancer), and finally a greater susceptibility to the side effects of chemotherapy, including metabolic decompensation. Our patient also presented with these features. After kidney transplantation, his metabolic outcome was well‐controlled for 20 years. MMA levels increased progressively, but he did not experience episodes of metabolic decompensation requiring hospitalization. He followed a lacto‐vegetarian diet with a protein intake of 45 g/day. His kidney function was declining when he developed the cancer. Despite a good response to chemotherapy, he developed severe drug toxicity, comprising the most frequent side effects (cytopenia, fever, neuropathy), but also had a loss of metabolic balance with acidosis, and basal ganglia stroke which finally led to death. Unlike the previously reported cases above, he did not have a solid tumor, but a non‐Hodgkin lymphoma.
After solid organ transplantation, the risk of developing lymphoproliferative disease (PTLD) is higher than that of the general population due to prolonged immunosuppression. 24 , 25 , 26 A recent review reports the follow‐up of 96 patients with MMA who underwent liver (n = 50), kidney (n = 8) or combined transplantation (n = 38) in the last 10 years. The median follow up was 2.5 years (0.2–12 years). Only 1 patient, a six‐year‐old MMA girl with MUT variants, developed a PTLD, occurring 1 year after liver‐kidney transplantation. She recovered with reduction of immunosuppression and rituximab, without requiring chemotherapy. 27 , 28 Conversely, in a long‐term follow‐up after liver transplantation of two cohorts of patients with propionic acidemia (12 and 14 patients, respectively), 4 developed PTLD (0.1–13.5 years after transplantation). 29 , 30 Longer follow‐up of transplanted MMA patients may reveal more cases of PTLD.
The occurrence of cancer in organic acidemias might be multifactorial. Mitochondrial dysfunction is a well‐recognized pathophysiological mechanism of MMA. Mitochondria are responsible for energy production but are also involved in cell proliferation and apoptosis (programmed cell death) and mitochondrial disorders have been associated with malignancies. 31
Mitochondrial impairment increases the production of reactive oxygen species ROS, also because MMA inhibits the transport of glutathione in mitochondria via a dicarboxylate carrier, resulting in redox imbalance and mitochondrial antioxidant defense exhaustion. 32 ROS plays a role in oncogenesis, causing DNA damage and activation of ROS‐dependent pro‐oncogenic signaling pathways. 22
Moreover, oncometabolites increase neoplastic vulnerability via their effect on key enzymes regulating metabolic pathways that facilitate cell survival or dedifferentiation. 33 Propionyl‐CoA is known to modify histone acetylation. 22 , 34 MMA induces SOX4 by activating autocrine TGFß signaling, resulting in transcriptional reprogramming of cancer cells that endows them with malignant properties such as invasiveness and metastatic potential. For example, MMA can induce a pro‐metastatic epithelial‐to‐mesenchymal transition‐like phenotype, with a decline in E‐cadherin and a concurrent increase in fibronectin and vimentin. 35 , 36
Several factors may increase the risk of PTLD. In early post‐transplantation onset PTLD, the induction therapy and the EBV infection are the most important. More than 50% of PTLD cases are EBV‐related, especially in case of EBV donor‐recipient mismatch. 17 Indeed, the role of anti‐thymocyte globulin induction therapy as a risk factor for PTLD is controversial. However, our patient was EBV negative at the onset of PTLD and induction was accomplished with basiliximab. By contrast, in patients with late‐onset PTLD the most important risk factors are patient age and the immune status. In particular, calcineurin inhibitors like tacrolimus are associated with an increased risk of PTLD. 37 Tacrolimus serum levels in our patient were consistently in the upper level of the target range, and may have resulted in excessive immunosuppression, as suggested by the documented infective episodes before PTLD onset. Therefore, the cumulative immunosuppression therapy may have increased the risk of PTLD.
Finally, our patient developed severe chemotherapy toxicity. Mitochondrial impairment can also explain the increased drug toxicity in MMA patients. Accordingly, our patient developed acidosis, high lactic acid, and basal ganglia stroke, secondary to mitochondrial impairment. This susceptibility should be considered in the chemotherapy plans of patients with organic acidemias.
In conclusion, our patient represents the first report of NHL in the long‐term follow‐up of a kidney transplanted patient with cblB‐MMA. Although prolonged post‐transplant immunosuppression is a risk factor for lymphoproliferative diseases, our patient presented lymphoma many years after the transplant, without a known infectious cause, and simultaneously with progressive renal and metabolic deterioration. Based on our experience, and previously described cases of cancer in patients with methylmalonic acidemia, we could speculate that oncogenesis could be the result of chemically induced damage stemming from the underlying metabolic disorder and longstanding kidney disease. More patients with long‐term follow‐up are necessary to appreciate the risk of malignancy in organic acidurias, especially after solid organ transplantation.
FUNDING INFORMATION
This research received no external funding.
CONFLICT OF INTEREST STATEMENT
The authors of this manuscript have no conflict of interest to disclose.
INFORMED CONSENT STATEMENT
Informed consent was obtained from the parents of the patient.
ACKNOWLEDGMENTS
We thank the parents of the patient for the support and the consent to publication of the data. We thank Richard Vernell, an independent medical writer, who provided medical writing support funded by Cometa A.S.M.M.E.—Associazione Studio Malattie Metaboliche Ereditarie—ONLUS.
Burlina AB, Burlina AP, Mignani R, et al. Non‐Hodgkin lymphoma in a kidney transplanted patient with methylmalonic acidemia: Metabolic susceptibility and the role of immunosuppression. JIMD Reports. 2024;65(2):56‐62. doi: 10.1002/jmd2.12411.
Communicating Editor: Georg Hoffmann
DATA AVAILABILITY STATEMENT
Data available on request due to privacy/ethical restrictions.
REFERENCES
- 1. Brasil S, Briso‐Montiano A, Gámez A, et al. New perspectives for pharmacological chaperoning treatment in methylmalonic aciduria cblB type. Biochim Biophys Acta Mol Basis Dis. 2018;1864(2):640‐648. doi: 10.1016/j.bbadis.2017.11.024 [DOI] [PubMed] [Google Scholar]
- 2. Forny P, Plessl T, Frei C, Bürer C, Froese DS, Baumgartner MR. Spectrum and characterization of Bi‐allelic variants in MMAB causing cblB‐type methylmalonic aciduria. Hum Genet. 2022;141(7):1253‐1267. doi: 10.1007/s00439-021-02398-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Baumgartner MR, Hörster F, Dionisi‐Vici C, et al. Proposed guidelines for the diagnosis and Management of Methylmalonic and Propionic Acidemia. Orphanet J Rare Dis. 2014;9(1):130. doi: 10.1186/s13023-014-0130-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bösch F, Landolt MA, Baumgartner MR, et al. Health‐related quality of life in paediatric patients with intoxication‐type inborn errors of metabolism: analysis of an international data set. J Inherit Metab Dis. 2021;44(1):215‐225. doi: 10.1002/jimd.12301 [DOI] [PubMed] [Google Scholar]
- 5. Ruoppolo M, Malvagia S, Boenzi S, et al. Expanded newborn screening in Italy using tandem mass spectrometry: two years of National Experience. IJNS. 2022;8(3):47. doi: 10.3390/ijns8030047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heringer J, Valayannopoulos V, Lund AM, et al. Impact of age at onset and newborn screening on outcome in organic acidurias. J Inher Metab Disea. 2016;39(3):341‐353. doi: 10.1007/s10545-015-9907-8 [DOI] [PubMed] [Google Scholar]
- 7. Heringer J, Valayannopoulos V, Lund AM, et al. Correction to: impact of age at onset and newborn screening on outcome in organic acidurias. J Inher Metab Dis. 2018;41(4):741‐742. doi: 10.1007/s10545-017-0116-5 [DOI] [PubMed] [Google Scholar]
- 8. Molema F, Gleich F, Burgard P, et al. Evaluation of dietary treatment and amino acid supplementation in organic acidurias and urea‐cycle disorders: on the basis of Information from a European multicenter registry. J Inher Metab Dis. 2019;42(6):1162‐1175. doi: 10.1002/jimd.12066 [DOI] [PubMed] [Google Scholar]
- 9. Burlina A, Bettocchi I, Biasucci G, et al. Long‐term use of Carglumic acid in methylmalonic aciduria, propionic aciduria and isovaleric aciduria in Italy: a qualitative survey. Eur Rev Med Pharmacol Sci. 2022. Jul;26(14):5136‐5143. doi: 10.26355/eurrev_202207_29302 [DOI] [PubMed] [Google Scholar]
- 10. Burlina A, Cazzorla C, Zanonato E, Viggiano E, Fasan I, Polo G. Clinical experience with N‐Carbamylglutamate in a single‐Centre cohort of patients with propionic and methylmalonic aciduria. Mol Genet Metab Rep. 2016;8:34‐40. doi: 10.1016/j.ymgmr.2016.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. De Baulny HO, Benoist JF, Rigal O, Touati G, Rabier D, Saudubray JM. Methylmalonic and propionic Acidaemias: management and outcome. J Inher Metab Dis. 2005;28(3):415‐423. doi: 10.1007/s10545-005-7056-1 [DOI] [PubMed] [Google Scholar]
- 12. Hörster F, Baumgartner MR, Viardot C, et al. Long‐term outcome in methylmalonic acidurias is influenced by the underlying defect (Mut0, Mut−, cblA, cblB). Pediatr Res. 2007;62(2):225‐230. doi: 10.1203/PDR.0b013e3180a0325f [DOI] [PubMed] [Google Scholar]
- 13. Leonard JV, Walter JH, McKiernan PJ. The Management of Organic Acidaemias: the role of transplantation. J Inher Metab Dis. 2001;24(2):309‐311. doi: 10.1023/A:1010395724012 [DOI] [PubMed] [Google Scholar]
- 14. Lubrano R, Elli M, Rossi M, et al. Renal transplant in methylmalonic acidemia: could it Be the best option?: report on a case at 10 years and review of the literature. Pediatr Nephrol. 2007;22(8):1209‐1214. doi: 10.1007/s00467-007-0460-z [DOI] [PubMed] [Google Scholar]
- 15. Mc Guire PJ, Lim‐Melia E, Diaz GA, et al. Combined liver‐kidney transplant for the management of methylmalonic aciduria: a case report and review of the literature. Mol Genet Metab. 2008;93(1):22‐29. doi: 10.1016/j.ymgme.2007.08.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brassier A, Boyer O, Valayannopoulos V, et al. Renal transplantation in 4 patients with methylmalonic aciduria: a cell therapy for metabolic disease. Mol Genet Metab. 2013;110(1–2):106‐110. doi: 10.1016/j.ymgme.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 17. Sprangers B, Riella LV, Dierickx D. Posttransplant lymphoproliferative disorder following kidney transplantation: a review. Am J Kidney Dis. 2021;78(2):272‐281. doi: 10.1053/j.ajkd.2021.01.015 [DOI] [PubMed] [Google Scholar]
- 18. Molema F, Williams M, Langendonk J, et al. Neurotoxicity including posterior reversible encephalopathy syndrome after initiation of calcineurin inhibitors in transplanted methylmalonic acidemia patients: two case reports and review of the literature. JIMD Rep. 2020;51(1):89‐104. doi: 10.1002/jmd2.12088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Au E, Wong G, Chapman JR. Cancer in kidney transplant recipients. Nat Rev Nephrol. 2018;14(8):508‐520. doi: 10.1038/s41581-018-0022-6 [DOI] [PubMed] [Google Scholar]
- 20. Cosson MA, Touati G, Lacaille F, et al. Liver hepatoblastoma and multiple OXPHOS deficiency in the follow‐up of a patient with methylmalonic aciduria. Mol Genet Metab. 2008;95(1–2):107‐109. doi: 10.1016/j.ymgme.2008.06.007 [DOI] [PubMed] [Google Scholar]
- 21. Chan R, Mascarenhas L, Boles RG, Kerkar N, Genyk Y, Venkatramani R. Hepatoblastoma in a patient with methylmalonic aciduria. Am J Med Genet. 2015;167(3):635‐638. doi: 10.1002/ajmg.a.36925 [DOI] [PubMed] [Google Scholar]
- 22. Forny P, Hochuli M, Rahman Y, et al. Liver neoplasms in methylmalonic aciduria: an emerging complication. J Inher Metab Dis. 2019;42(5):793‐802. doi: 10.1002/jimd.12143 [DOI] [PubMed] [Google Scholar]
- 23. Potter SL, Venkatramani R, Wenderfer S, et al. Renal cell carcinoma harboring somatic TSC2 mutations in a child with methylmalonic acidemia. Pediatr Blood Cancer. 2017;64(5):e26286. doi: 10.1002/pbc.26286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Caillard S, Lamy FX, Quelen C, et al. Epidemiology of posttransplant lymphoproliferative disorders in adult kidney and kidney pancreas recipients: report of the French registry and analysis of subgroups of lymphomas. Am J Transplant. 2012;12(3):682‐693. doi: 10.1111/j.1600-6143.2011.03896.x [DOI] [PubMed] [Google Scholar]
- 25. Allen UD, Preiksaitis JK, AST Infectious Diseases Community of Practice . Post‐transplant lymphoproliferative disorders, Epstein‐Barr virus infection, and disease in solid organ transplantation: guidelines from the American Society of Transplantation infectious diseases community of practice. Clin Transplant. 2019;33(9):e13652. doi: 10.1111/ctr.13652 [DOI] [PubMed] [Google Scholar]
- 26. Montanari F, Orjuela‐Grimm M. Joining efforts for PTLD: lessons learned from comparing the approach and treatment strategies across the pediatric and adult age spectra. Curr Hematol Malig Rep. 2021;16(1):52‐60. doi: 10.1007/s11899-021-00606-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Siegel C, Arnon R, Florman S, Bucuvalas J, Oishi K. Nutritional management and biochemical outcomes during the immediate phase after liver transplant for methylmalonic acidemia. Nutrients. 2020;12(10):2976. doi: 10.3390/nu12102976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chakrapani A, Stojanovic J, Vara R, De Nictolis F, Spada M, Dionisi‐Vici C. Safety, efficacy, and timing of transplantation(s) in propionic and methylmalonic aciduria. J Inher Metab Dis. 2023;46(3):466‐481. doi: 10.1002/jimd.12613 [DOI] [PubMed] [Google Scholar]
- 29. Charbit‐Henrion F, Lacaille F, McKiernan P, et al. Early and late complications after liver transplantation for propionic acidemia in children: a two centers study. Am J Transplant. 2015;15(3):786‐791. doi: 10.1111/ajt.13027 [DOI] [PubMed] [Google Scholar]
- 30. Curnock R, Heaton ND, Vilca‐Melendez H, Dhawan A, Hadzic N, Vara R. Liver transplantation in children with propionic acidemia: medium‐term outcomes. Liver Transpl. 2020;26(3):419‐430. doi: 10.1002/lt.25679 [DOI] [PubMed] [Google Scholar]
- 31. Gasparre G, Porcelli AM, Lenaz G, Romeo G. Relevance of mitochondrial genetics and metabolism in cancer development. Cold Spring Harb Perspect Biol. 2013;5(2):a011411. doi: 10.1101/cshperspect.a011411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fontella FU, Pulrolnik V, Gassen E, et al. Propionic and L‐methylmalonic acids induce oxidative stress in brain of young rats. Neuroreport. 2000;11(3):541‐544. doi: 10.1097/00001756-200002280-00023 [DOI] [PubMed] [Google Scholar]
- 33. Erez A, DeBerardinis RJ. Metabolic dysregulation in monogenic disorders and cancer—finding method in madness. Nat Rev Cancer. 2015;15(7):440‐448. doi: 10.1038/nrc3949 [DOI] [PubMed] [Google Scholar]
- 34. Nguyen NHT, Morland C, Gonzalez SV, et al. Propionate increases neuronal histone acetylation, but is metabolized oxidatively by glia. Relevance for propionic acidemia: brain metabolism of propionate. J Neurochem. 2007;101(3):806‐814. doi: 10.1111/j.1471-4159.2006.04397.x [DOI] [PubMed] [Google Scholar]
- 35. Gomes AP, Ilter D, Low V, et al. Age‐induced accumulation of methylmalonic acid promotes tumour progression. Nature. 2020;585(7824):283‐287. doi: 10.1038/s41586-020-2630-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lee N, Kim D. Toxic metabolites and inborn errors of amino acid metabolism: what one informs about the other. Metabolites. 2022;12(6):527. doi: 10.3390/metabo12060527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Van Leeuwen MT, Grulich AE, Webster AC, et al. Immunosuppression and other risk factors for early and late non‐Hodgkin lymphoma after kidney transplantation. Blood. 2009;114(3):630‐637. doi: 10.1182/blood-2009-02-202507 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request due to privacy/ethical restrictions.


