Abstract
Introduction
Medical readiness is of paramount concern for active-duty military providers. Low volumes of complex trauma in military treatment facilities has driven the armed forces to embed surgeons in high-volume civilian centers to maintain clinical readiness. It is unclear what impact this strategy may have on patient outcomes in these centers. We sought to compare emergent trauma laparotomy (ETL) outcomes between active-duty Air Force Special Operations Surgical Team (SOST) general surgeons and civilian faculty at an American College of Surgeons verified level 1 trauma center with a well-established military-civilian partnership.
Methods
Retrospective review of a prospectively maintained, single-center database of ETL from 2019 to 2022 was performed. ETL was defined as laparotomy from trauma bay within 90 min of patient arrival. The primary outcome was to assess for all-cause mortality differences at multiple time points.
Results
514 ETL were performed during the study period. 22% (113 of 514) of patients were hypotensive (systolic blood pressure ≤90 mm Hg) on arrival. Six SOST surgeons performed 43 ETL compared with 471 ETL by civilian faculty. There were no differences in median ED length of stay (27 min vs 22 min; p=0.21), but operative duration was significantly longer for SOST surgeons (129 min vs 110 min; p=0.01). There were no differences in intraoperative (5% vs 2%; p=0.30), 6-hour (3% vs 5%; p=0.64), 24-hour (5% vs 5%; p=1.0), or in-hospital mortality rates (5% vs 8%; p=0.56) between SOST and civilian surgeons. SOST surgeons did not significantly impact the odds of 24-hour mortality on multivariable analysis (OR 0.78; 95% CI 0.10, 6.09).
Conclusion
Trauma-related mortality for patients undergoing ETL was not impacted by SOST surgeons when compared with their civilian counterparts. Military surgeons may benefit from the valuable clinical experience and mentorship of experienced civilian trauma surgeons at high volume trauma centers without creating a deficit in the quality of care provided.
Level of evidence
Level IV, therapeutic/care management.
Keywords: abdominal injuries, death, hemorrhage, Multiple Trauma
WHAT IS ALREADY KNOWN ON THIS TOPIC
Non-trauma fellowship trained military surgeons represent a large portion of the military’s surgical cadre; however, they are frequently stationed at medical centers who do not experience a high volume of trauma.
WHAT THIS STUDY ADDS
This study suggests that it is safe to embed military general surgeons at high volume, level 1 trauma centers without experiencing a deficit in care.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
These findings offer a new insight into optimizing surgical readiness for military providers at military-civilian partnerships.
Introduction
Partnerships between the military and civilian hospital systems have become increasingly recognized as an important tool for augmenting clinical practice and maintaining critical wartime medical skills necessary for military medical professionals.1–8 The importance of these partnerships spans across all branches of the military during both times of active combat and peacetime efforts.2 3 5 8–11 Moreover, expansion of these partnerships to include graduate medical education, as well as non-physician medical personnel, has increased the outreach of said programs and further augmented the capabilities of their respective civilian centers.9 10 Thus, military-civilian partnerships (MCPs) are believed to offer a dynamic and symbiotic relationship for all parties involved.8
The current training paradigm for the majority of active-duty military surgeons has largely been structured around military treatment facilities (MTFs) and military medical centers (MEDCENs). Although MTFs and MEDCENs support the military’s medical mission by providing healthcare to service members, their families, and retirees, concerns regarding decreasing surgical case volume and low surgical complexity pose a threat toward future surgical readiness.8 12–15 These concerns have been escalated during recent years, especially in the post-COVID-19 era, where staffing issues and referral patterns have driven a large portion of the surgical volume at MTFs and MEDCENs out to the civilian referral network.12 16–19 One proposed solution revolves around increasing the development of formalized MCPs in efforts to allow military healthcare professionals the opportunity to work at high volume civilian institutions where they have access to complex patient encounters to maintain readiness and proficiency for critical wartime tasks.3 8
Although MCPs offer a potential solution toward maintaining medical readiness, it is unclear what impact these partnerships may have on patient outcomes. This holds particularly true for trauma patients with increasing injury burden as centers offering a high volume of complex trauma patients would likely be the ideal institutions for MCPs.5 20 21 The emergent trauma laparotomy (ETL), with its associated complexity and high rate of mortality, is considered the signature procedure of the trauma surgeon. Both in combat and civilian scenarios, the ETL is likely the greatest potential impact an individual surgeon may have on limiting preventable death secondary to ongoing abdominopelvic hemorrhage. The documented rates of mortality after ETL varies widely between trauma centers and individual surgeons.22–25 As such, quantifying objective metrics from military surgeons working within these MCPs may provide valuable data for both the military and civilian institutions involved.
Our civilian institution represents a mature MCP that has been in place for the last 16 years for the US Air Force Special Operations Surgical Teams (SOST).10 Although this unique partnership allows SOST members to operate within a high-volume trauma center, it is unclear what impact SOST members may have on overall mortality in trauma patients requiring ETL. SOST surgeons have completed training in general surgery but traditionally have not received fellowship training. Although SOST members may have a robust experience with casualties in austere environments, differences in injury patterns and patient physiology may impact the outcomes in ETL for the civilian setting. Thus, we sought to analyze the outcomes of ETL in trauma patients between SOST surgeons and their civilian counterparts at our institution, paying particular attention to early mortality.
Methods
We performed a retrospective review of a prospectively maintained, single center database of trauma patients requiring ETL from November 2019 to December 2022. Approval from the local Institutional Review Board was obtained for this project. Reporting of this study conforms to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. The institution serves a major metropolitan area as an American College of Surgeons (ACS) verified level 1 trauma center. The Division of Trauma and Acute Care Surgery employed 18 full-time faculty throughout the duration of the study period. The trauma service on average evaluated 5711 trauma activations with an average of 3512 trauma admissions annually during 2019–2022.
SOST composition
Six Air Force general surgeons were members of the embedded SOST teams during the study period. SOST units at the institution are composed of a general surgeon, anesthesiologist, emergency medicine physician, critical care nurse, surgical technician, and respiratory therapist.10 SOST teams are medically and tactically trained teams designed to be lightweight, mobile elements that can be rapidly deployed to provide life-saving resuscitation and surgical care far forward within the combat zone. Although their deployment tempo varies based on the operational needs worldwide, teams traditionally deploy on at least a biannual schedule and have various military-related training obligations, although they are not deployed. Although attached to their unit at our institution, SOST members serve as clinical assistant professors with weekday and overnight call requirements for the Division of Trauma and Acute Care Surgery on average 1–2 nights per month. None of the SOST surgeons attached to the division during the study period had fellowship training in surgical critical care or trauma surgery. Surgeons remained attached to the division during the study period for differing durations of time (in years, A: 0; B: 1; C: 3; D: 4; E: 4; F: 6). Similarly, surgeons had differing amounts of experience as military surgeons after residency prior to attachment with the division (in years, A: 3; B: 0; C: 3; D: 1; E: 0; F: 0).
SOST onboarding
Prior to working independently at the civilian trauma center, military general surgeons assigned to the SOST program undergo a 10-month long pipeline training program, encompassing military specific training, special operations specific battlefield surgical training, as well as an onboarding process review of case logs and trauma experience by the civilian institution. Onboarding time at the institution ranges between 3 and 6 months during which military surgeons function in a supervised junior attending role through various service lines covered by the Division of Trauma and Acute Care Surgery. Additionally, they complete a series of supervised trauma calls using the two in-house surgeon model for added supervision and mentorship until they are cleared by division leadership for independent call. Post-deployment surgeons underwent review and follow-up through the Joint Trauma System, at the unit level through the unit chief medical officer, and with the trauma medical director at the civilian institution. No formal re-onboarding was required after deployment with the civilian institution.
Patient eligibility and definitions
All trauma patients undergoing ETL from the trauma bay were eligible for inclusion. ETL was defined as a laparotomy for possible hemorrhage control directly from the trauma within 90 min of arrival. Those undergoing initial laparoscopy or endoscopy were excluded from analysis. Additionally, those requiring resuscitative thoracotomy due to traumatic arrest prior to ETL were excluded.
Information on patient demographics and injury characteristics were identified from the medical record. The arrival time to the trauma bay was used as the start time in time-based calculations. Time from emergency department (ED) arrival to departure was defined was ED time. Operation time was calculated as time from operation start to operation end. Mortality time was defined by the difference in time from ED arrival to time of death. Severe traumatic brain injury (TBI) was defined as an Abbreviated Injury Scale (AIS)-Head score ≥3.
Study characteristics
Patients were separated into two cohorts for comparison based on the initial operating surgeon. Those with ETL performed by an active-duty member of SOST were placed into the SOST cohort, whereas those with ETL performed by a civilian full-time faculty were placed into the CIV cohort. The main outcomes of interest were rates of mortality during operation and within 6 hours, 24 hours, and hospitalization. Intraoperative blood products transfused and rates of damage control laparotomy (DCL) were compared, as were median times in the ED and of operation. OR times of those with intraoperative death were excluded from analysis of overall median operative times. Similarly, those with intraoperative death were excluded from comparison of rates of DCL.
Data were presented as numerical values or proportions for categorical data and median (IQR) for continuous data, unless otherwise noted. Categorical data were compared by χ2 and Fisher’s exact tests where appropriate, whereas continuous data were compared with Mann-Whitney U tests. A multivariable logistic regression model was used to estimate ORs and associated 95% confidence intervals for SOST surgeon performance of operation on 24-hour mortality. Covariates were identified for inclusion in the model based on initial bivariate analysis with those variables having a p value ≤0.2 eligible for inclusion in the multivariable model. All data analysis was performed using SPSS V.26 (International Business Machines, New York, NY).
Results
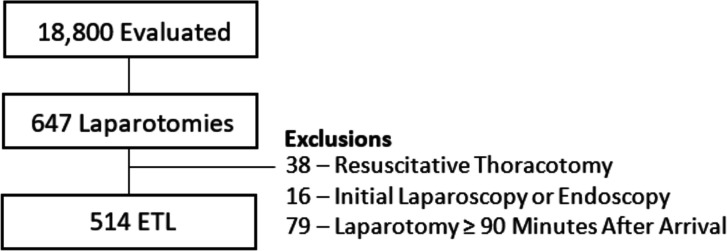
There were 18,800 trauma activations and 11,595 trauma admissions during the study period. A total of 647 laparotomies were performed in this time. Five hundred and fourteen (79.4%) were defined as ETL and included for final analysis (figure 1).
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram.
Overall, a majority of patients were male (82.7%) and were injured by penetrating mechanism of injury (71.8%). Most patients were transported directly from scene to the trauma bay (80.5%). Hypotension (systolic blood pressure (SBP) <90 mm Hg) was present on arrival in 22.0% of patients. A minority of patients (14.0%) had a concurrent traumatic brain injury (TBI), with an even smaller minority (8.9%) sustaining a severe TBI.
For patients undergoing ETL, the overall mortality rate for the entire cohort was 7.9% during the initial hospitalization. Mortality rates during initial operation were 2.5%, 3.3% within 6 hours, and 4.7% within 24 hours for the total patient cohort. DCL was used in 29.9% of patients overall.
SOST surgeons performed only 8.4% of ETL overall, with the rest being performed by the CIV cohort. The median number of ETLs performed by SOST members was 8 (4, 10) compared with the CIV cohort with a median 25 (12, 37). Overall, the range of ETL performed by SOST members was 2–12 and was 1–62 for civilian surgeons (online supplemental figure 1A,B). There were no differences in patient demographics, mechanism of injury, or presenting vital signs when comparing patients receiving ETL by either the SOST or CIV cohort (table 1). Patients in the CIV cohort had a significantly higher median INR (1.2 (1.06, 1.33) vs 1.1 (1.02, 1.26); p=0.03) when compared with patients in the SOST cohort. There were no other significant differences in presenting laboratory values. Similarly, there were no differences in injury severity or specific injuries managed at laparotomy between patients in the two cohorts (table 2).
Table 1.
Comparison of demographic and presentation characteristics of patients requiring emergent trauma laparotomy hospital mortality
| SOST (n=43) | Civilian (n=471) | P value† | |
| Demographics | |||
| Age | 31 (25, 42) | 32 (24, 45) | 0.73 |
| Gender | |||
| Male | 35 (81) | 390 (83) | 0.82 |
| Female | 8 (19) | 81 (17) | |
| Race | |||
| Caucasian | 17 (40) | 180 (38) | 0.96 |
| Black | 25 (58) | 276 (59) | |
| Hispanic | 1 (2) | 12 (3) | |
| Asian | 0 | 3 (1) | |
| Injury | |||
| Mechanism of Injury | |||
| Blunt | 12 (28) | 133 (28) | 0.96 |
| Penetrating | 31 (72) | 338 (72) | |
| Initial heart rate (bpm) | 102 (79, 122) | 100 (85, 120) | 0.85 |
| Initial SBP (mm Hg) | 115 (90, 145) | 118 (96, 140) | 0.80 |
| Hypotensive (initial SBP ≤90 mm Hg) | 13 (30) | 100 (21) | 0.17 |
| Lowest SBP (mm Hg) | 101 (82, 130) | 98 (77, 120) | 0.12 |
| Initial Glasgow Coma Scale Score | 15 (13, 15) | 15 (14, 15) | 0.22 |
| Direct from scene | 34 (79) | 38 (81) | 0.80 |
| Time in trauma bay (min) | 27 (16, 57) | 22 (14, 46) | 0.21 |
| REBOA | 3 (7) | 1 (0.2) | 0.002 |
| General laboratory | |||
| Lactate (mmol/L) | 3.3 (2.08, 5.95) | 4.0 (2.40, 7.00) | 0.24 |
| Serum creatinine (mg/dL) | 1.1 (0.90, 1.30) | 1.2 (1.00, 1.40) | 0.16 |
| Base excess (mEq/L) | −4.9 (–8.65, –1.75) | −4.7 (–8.95, –1.90) | 0.74 |
| Hemoglobin (g/dL) | 12.4 (11.20, 13.90) | 12.3 (10.90, 13.50) | 0.46 |
| Platelets (103/cm) | 219 (167, 295) | 227 (176, 281) | 0.87 |
| INR | 1.1 (1.02, 1.26) | 1.2 (1.06, 1.33) | 0.03 |
*Data shown as number (proportion) and median (IQR) for categorical and continuous variables, respectively.
†Data compared with Pearson χ2 or Fisher’s exact and Mann-Whitney U tests for categorical and continuous data, respectively.
INR, International Normalized Ratio; REBOA, resuscitative endovascular balloon occlusion of the aorta; SBP, systolic blood pressure; SOST, Special Operations Surgical Team.
Table 2.
Comparison of injury characteristics of patients requiring emergent trauma laparotomy by hospital mortality
| SOST (n=43) | Civilian (n=471) | P value† | |
| Injury characteristics | |||
| Injury Severity Score (ISS) | 17 (10, 25) | 18 (10, 29) | 0.56 |
| ISS ≥15 | 25 (58) | 274 (58) | 1.0 |
| New ISS | 22 (13, 34) | 25 (14, 38) | 0.59 |
| AIS-Head | 0(0, 0) | 0(0, 0) | 0.70 |
| Any traumatic brain injury | 4 (9) | 42 (9) | 1.0 |
| Severe TBI (AIS-Head ≥3) | 7 (16) | 65 (14) | 0.65 |
| AIS-Chest | 2(0, 3) | 2(0, 3) | 0.59 |
| AIS-Abdomen | 3 (2, 4) | 3 (2, 4) | 0.25 |
| Operative injuries and management | |||
| Any solid organ injury | |||
| Liver | 14 (33) | 190 (40) | 0.32 |
| Spleen | 12 (28) | 133 (28) | 0.96 |
| Kidney | 4 (9) | 44 (9) | 1.0 |
| Pancreas | 4 (9) | 26 (6) | 0.30 |
| Hollow viscus | 27 (63) | 274 (58) | 0.56 |
| Major abdominal vascular injury | |||
| Named abdominal artery | 2 (5) | 20 (4) | 0.71 |
| Named abdominal vein | 3 (7) | 31 (7) | 0.76 |
| Pelvic fractures requiring preperitoneal packing | 0 | 7 (2) | 1.0 |
| Time of operation (min) | 129 (96, 173) | 110 (78, 150) | 0.01 |
| Concurrent thoracotomy | 1 (2) | 14 (3) | 1.0 |
| Concurrent sternotomy | 0 | 10 (2) | 1.0 |
| Damage control laparotomy | 12 (29) | 138 (30) | 0.89 |
| Utilization of backup attending | 5 (12) | 14 (3) | 0.01 |
| Mortality | |||
| Proportion of death within timeframe | |||
| Intraoperative | 2 (5) | 11 (2) | 0.30 |
| Within 6 hours | 2 (5) | 15 (3) | 0.64 |
| Within 24 hours | 2 (5) | 22 (5) | 1.0 |
| Hospitalization | 2 (5) | 39 (8) | 0.56 |
| Intraoperative resuscitation requirements | |||
| Crystalloid (mL) | 1500 (1000, 2000) | 1700 (2038, 2338) | 0.34 |
| Whole blood (units) | 0 (0, 3) | 1.5 (0, 2.75) | 0.24 |
| Red blood cells (units) | 0 (0, 2) | 0 (0, 2.5) | 0.50 |
| Plasma (units) | 0 (0, 2) | 0 (0, 3.25) | 0.98 |
| Platelets (units) | 0 (0, 0) | 0 (0, 0) | 0.96 |
| Cryoprecipitate (units) | 0 (0, 0) | 0 (0, 0) | 0.62 |
*Data shown as number (proportion) and median (IQR) for categorical and continuous variables, respectively.
†Data compared with Pearson χ2 or Fisher’s exact and Mann-Whitney U tests for categorical and continuous data, respectively.
AIS, Abbreviated Injury Scale score; TBI, traumatic brain injury.
tsaco-2023-001332supp001.pdf (42.3KB, pdf)
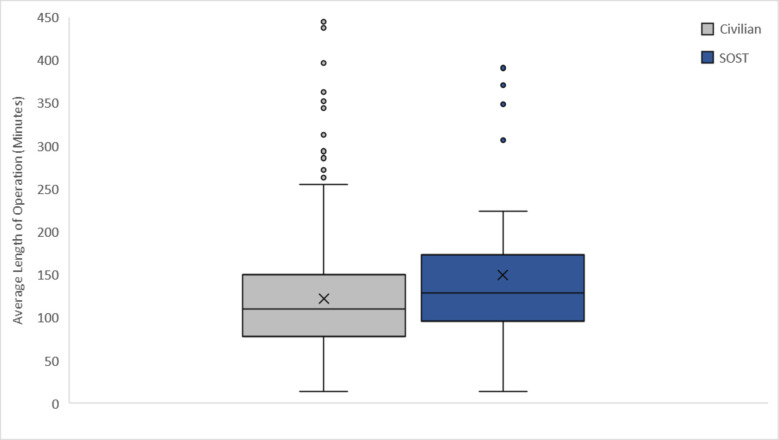
Although SOST surgeons were more likely to use resuscitative endovascular balloon occlusion of the aorta (REBOA) compared with the CIV cohort (7% vs 0.2%; p<0.01), time to the operating room was not significantly different between the two cohorts (27 min (16, 57) vs 22 min (14, 46); p=0.21) (figure 2). However, duration of operation was significantly longer in the SOST cohort (129 min (96, 173) vs 110 min (78, 150)); p=0.01). Rates of DCL were 29.2% overall with no differences between SOST and CIV surgeons (29% vs 30%; p=0.89). There was no difference in the frequency of fellow presence at the time of ETL when comparing SOST and CIV surgeons (70% vs 61%; p=0.26). SOST surgeons were significantly more likely to have the assistance of the backup attending surgeon during ETL compared with their civilian counterparts (12% vs 3%; p=0.01). Finally, intraoperative resuscitation and blood product requirements were found to be similar between the two cohorts assessed (table 2).
Figure 2.
Box and whisker plot of average length of operation for SOST (Special Operations Surgical Team) and civilian surgeon cohorts.
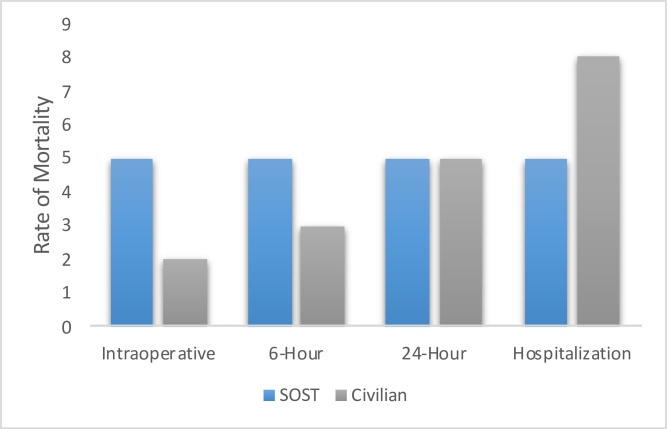
Mortality rates for the population requiring ETL overall were as follows: 2.5% intraoperative; 3.3% within 6 hours; 4.7% within 24 hours; 8.0% during hospitalization. There were no differences in mortality rates between SOST and CIV surgeons at any time point in initial bivariate analysis (figure 3). In the multivariable model adjusting for INR and the lowest ED SBP, performance of ETL by the SOST cohort had no association with risk of 24-hour mortality (OR 0.78; (0.10, 6.09)) (table 3). On review of the deaths in the SOST cohort, only one patient was identified as having possibility for performance improvement. The patient suffered a devastating injury to aorta, portal vein, and pancreas with intraoperative death who was determined to have anticipated mortality with opportunity for improvement. There were no apparent outliers among individual SOST surgeons in mortality after ETL (online supplemental table 4).
Figure 3.
Mortality rates for SOST (Special Operations Surgical Team) and CIV surgeon cohorts in patients requiring ETL (emergent trauma laparotomy).
Table 3.
Multivariable logistic regression analysis of risk factors for 24-hour mortality after emergent trauma laparotomy
| Variable | OR | 95% CI | |
| Lower | Upper | ||
| SOST surgeon | 0.78 | 0.10 | 6.09 |
| International Normalized Ratio (INR) | 2.61 | 1.60 | 4.28 |
| Lowest ED systolic blood pressure | 1.00 | 0.98 | 1.01 |
ED, emergency department; SOST, Special Operations Surgical Team.
tsaco-2023-001332supp002.pdf (86.4KB, pdf)
Discussion
The mature MCP at our institution offers SOST members the opportunity to maintain their medical skills in a high volume, level 1 civilian trauma center to assure readiness for their combat deployments.10 In this analysis comparing ETL outcomes between SOST surgeons and their civilian counterparts, we demonstrated that there was no difference in mortality outcomes or intraoperative blood product requirements between the surgeon cohorts studied. Although we did demonstrate that SOST surgeons displayed longer median operative times, the granularity of the data available for this assessment poses challenges to decipher the clinical relevancy of these findings. Although the clinical implications of the longer operative times remain unclear, we speculate that this may be due to a multitude of reasons to include lower case sample size, increased utilization of the backup attending surgeon, increased utilization of REBOA requiring intraoperative balloon management, as well as decreased overall experience level and operative volume. To our knowledge, however, this represents the first study of its kind comparing these objective metrics between military surgical personnel and civilian trauma surgeons within the same MCP.
There are currently a multitude of active MCPs throughout the USA that support Army, Air Force, and Navy surgeons.2 3 8–10 26–28 Recent data suggest that these programs may be beneficial in helping military surgeons obtain the knowledge, skills, and abilities (KSA) thresholds that the Military Health System has adopted to assess for readiness deficits.1–3 19 KSA metrics, which were designed to encompass the attributes required to be a proficient surgeon for critical wartime procedures, assign a point system to individual surgeon case volumes based on the level of complexity and scope of the procedure.19 Although scores greater than 14,000 per year suggest that a military surgeon is ready to effectively deploy, recent data suggest that only roughly 10% of military surgeons are meeting the aforementioned threshold.12 19 To date, however, KSAs are only officially tracked for surgeons working at MTFs and MEDCENs. Although our study did not specifically assess the individual KSA values assigned to each surgeon, a multitude of recently published studies have addressed this at various MCPs and concluded that MCPs offer a feasible way to successfully increase individual KSA values to promote surgical readiness.1–3
Our analysis further expands on prior MCP reports and offers an objective outcomes-based assessment of surgeons operating at a single center MCP by highlighting the utility and safety of incorporating military surgical teams into civilian institutions. The fully integrated nature of the MCP is not unique to our institution; however, our model is not ubiquitous to the various other current MCPs available.8–10 21 26 27 For instance, our model offers a program that fully integrates SOST surgeons into the Division of Trauma and Acute Care Surgery as attending faculty with an academic appointment as clinical assistant professors.10 Other MCP models encompass programs that allow military surgeons to act as volunteer clinical faculty and still retaining a significant portion of their clinical duties at their respective MTF or MEDCEN.1 3 Furthermore, other models offer a “just-in-time” concept where military medical teams will travel to a level 1 trauma center during their predeployment training to gain exposure and build team dynamics.3 Although these programs offer improvements within the current readiness structure, the institutional model here offers a multitude of unique opportunities to further support career development through mentorship, academic teaching of embedded military medics, residents and fellows, and access to a robust research infrastructure.10
Other fully integrated programs, such as the Army Military-Civilian Trauma Team Training (AMCT3), offer similar experiences to that of our institution; however, they are limited to surgeons who have been fellowship trained in Surgical Critical Care.26 27 SOST surgeons traditionally are comprised of non-fellowship trained general surgeons early in their careers. This represents a key difference between the various integrated MCPs. Ruggero et al recently described an MCP program that also used general surgeons within a major level 1 trauma center; however, this program fundamentally differed from our model in that the general surgeons described within their MCP act as fellow-level physicians.2 Similarly, Yonge et al described their experience in the Pacific Northwest, which used general surgeons at a non-academic level II center where they operated under the supervision of a staff surgeon.1 Despite being non-fellowship trained, SOST surgeons are expected to act in the same capacity as their civilian counterparts at our institution. This provides SOST surgeons enhanced opportunities akin to their combat deployments, with the ability to actively oversee and run acute trauma resuscitations, perform all indicated surgical procedures, and actively manage critically ill trauma patients during their hospital admission. Our data suggest that this unique structure is both safe and effective for patient care outcomes despite SOST surgeons not possessing prior formalized fellowship training. Similarly, not all civilian faculty have undergone advanced fellowship training, demonstrating that competence is learned through experience and not always reflected by credentials or diplomas.
It is likely that the volume of operative cases among the SOST surgeons was lower than their civilian counterparts for a variety of reasons. SOST surgeons maintain their military obligations, including overseas deployments, routine military training, and administrative tasks. On average, SOST surgeons have an enduring mission deployment between 4 and 6 months duration every 1–2 years, as well as short-notice alert mission taskings that typically last between 1 and 3 months at least once per year. Deployments and taskings required by SOST surgeons frequently vary in operative case volume and complexity depending on the operational environment present. Surgeons also are tasked with fulfilling other domestic and international military specific duties of varying lengths on a rotational basis several times per year. In addition to these competing time commitments, the SOST complement at the trauma center consists of three surgeons, who together function as one full-time equivalent (FTE) trauma surgeon. This FTE is split covering emergency general surgery and trauma call, further limiting the overall ETL case numbers per surgeon.
It is important to note that although our data suggest the safety of our integrated model, our model is that of a mature MCP that has been evolving during the past 16 years.10 Although SOST surgeons are fully credentialled attending surgeons, civilian in-house back-up is always available to offer support if needed. This system provides a safety net and mentorship when requested. In our analysis, SOST surgeons were more likely to use the backup attending than the CIV cohort (12% vs 3%; p=0.01), highlighting the culture of collaboration and mentorship built within our MCP. Moreover, our institution represents a major tertiary care medical facility within the Southeastern USA with a robust number of yearly trauma activations and admissions. As such, SOST surgeons are provided with the full armamentarium of surgical residents, surgical critical care fellows, and advanced practice providers to help manage and provide care for patients. We think this model offers a structured environment to allow for optimal growth and development of non-fellowship trained military surgeons as they prepare for future deployments.
Despite the promise that our institutional MCP has demonstrated, our study is not without its limitations, which should be considered when evaluating our findings. Our study intent was to demonstrate the overall safety of the program in hopes to provide an example for other MCPs to follow. In doing so, we sought to highlight that non-fellowship trained military surgeons can provide high level initial trauma care for critically ill patients. As such, we deliberately sought to limit our findings to early mortality data, intraoperative resuscitation requirements, and operative times in hopes to limit the confounding aspects that accompany post-surgical care. One such aspect includes the multitude of medical personnel helping to provide daily care to these patients. However, we recognize that additional outcomes, such as unplanned return to OR, may have been beneficial if available. We fully recognize that quality trauma care spans beyond the initial surgical procedures and is a direct effect of a highly functioning trauma system; however, we think that by having the right structure in place to support the development of the SOST surgeons, these data can help promote the expansion of current and future MCPs to allow more military general surgeons the opportunity to partake in these valuable programs. We think these data support the notion that well-designed MCPs can safely help non-fellowship trained military surgeons expand on their scope of practice, continue to develop their clinical skills, and increase their overall readiness level for future deployments.
Surgical readiness within the military healthcare system remains a critically important focus for all service branches. We think that designing creative ways to improve on the current readiness levels for military surgeons without compromising on the quality of care rendered should be the strategic goal of all MCPs to create a truly symbiotic relationship between the military and civilian institutions. Our data support a model for an MCP that allows for non-fellowship trained general surgeons to develop and maintain the high level of clinical proficiency needed for future operational missions. Future work identifying innovative ways to expand these capabilities to reach a wider audience of military personnel should be prioritized in order guarantee superior surgical care on the battlefield moving forward.
Footnotes
Contributors: PH, RDB, DL, and RU were responsible for study design. PH and RU were responsible for data acquisition. PH, RDB, NM, and DL were responsible for data interpretation. DL and PH were responsible for manuscript creating. DL, OR, NM, RU, RDB, and PH were responsible for manuscript edit and review. DL accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Yonge J, Schaetzel S, Paull J, Jensen G, Wallace J, O’Brien B, Pak G, Schreiber M, Glaser J. Optimizing combat readiness for military surgeons without trauma fellowship training: engaging the “voluntary faculty” model. J Trauma Acute Care Surg 2023;95:S31–5. 10.1097/TA.0000000000004040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ruggero JM, Farnand AW, Roach PB, Starr F, Tadlock MD, Bokhari F. Initial assessment of a regional military–civilian partnership on trauma surgery skills sustainment . Mil Med 2023;188:e2462–6. 10.1093/milmed/usac229 [DOI] [PubMed] [Google Scholar]
- 3. Lee JJ, Hall AB, Carr MJ, MacDonald AG, Edson TD, Tadlock MD. Integrated military and civilian partnerships are necessary for effective trauma-related training and skills sustainment during the inter-war period. J Trauma Acute Care Surg 2022;92:e57–76. 10.1097/TA.0000000000003477 [DOI] [PubMed] [Google Scholar]
- 4. Hall A, Qureshi I, Englert MZ, Davis E. Variability of value of trauma centers to general surgery combat casualty care skill sustainment. J Surg Educ 2021;78:1275–9. 10.1016/j.jsurg.2020.12.002 [DOI] [PubMed] [Google Scholar]
- 5. Knudson MM, Elster EA, Bailey JA, Johannigman JA, Bailey PV, Schwab CW, Kirk GG, Woodson JA. Military–civilian partnerships in training, sustaining, recruitment, retention, and readiness: proceedings from an exploratory first-steps meeting. J Am Coll Surg 2018;227:284–92. 10.1016/j.jamcollsurg.2018.04.030 [DOI] [PubMed] [Google Scholar]
- 6. Knudson MM, Elster EE, Woodson J, Kirk G, Turner P, Hoyt DB. A shared ethos: the military health system strategic partnership with the American College of Surgeons. J Am Coll Surg 2016;222:1251–5. 10.1016/j.jamcollsurg.2016.03.006 [DOI] [PubMed] [Google Scholar]
- 7. Martin MJ, Rasmussen TE, Margaret Knudson M, Elster E. Heeding the call: military-civilian partnerships as a foundation for enhanced mass casualty care in the United States. J Trauma Acute Care Surg 2018;85:1123–6. 10.1097/TA.0000000000002055 [DOI] [PubMed] [Google Scholar]
- 8. National Academies of Sciences E and Medicine . A national trauma care system: integrating military and civilian trauma systems to achieve zero preventable deaths after injury. National Academies Press, 2016. [PubMed] [Google Scholar]
- 9. Kilburn JP, Streit S, Degoes JJ, Andersen A, Gardner M, Fraser DR, Fildes J. The Las Vegas military-civilian partnership: an origin story and call to action. J Trauma Acute Care Surg 2022;93:S169–73. 10.1097/TA.0000000000003701 [DOI] [PubMed] [Google Scholar]
- 10. Rokayak OA, Lammers DT, Baird EW, Holcomb JB, Jansen JO, Cox DB, Winkler JP, Betzold RD, Manley NR, Northern DM, et al. The 16-year evolution of a military-civilian partnership: the University of Alabama at Birmingham experience. J Trauma Acute Care Surg 2023;95:S19–25. 10.1097/TA.0000000000004051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grabo DJ, Gurney JM, Parascandola L, Knudson MM. Military-civilian partnerships and the clinical readiness mission: A preliminary study from the military health system and the American college of Surgeons. J Trauma Acute Care Surg 2022;93:S16–21. 10.1097/TA.0000000000003704 [DOI] [PubMed] [Google Scholar]
- 12. Dalton MK, Remick KN, Mathias M, Trinh Q-D, Cooper Z, Elster EA, Weissman JS. Analysis of surgical volume in military medical treatment facilities and clinical combat readiness of US military Surgeons. JAMA Surg 2022;157:43–50. 10.1001/jamasurg.2021.5331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Edwards MJ, Edwards KD, White C, Shepps C, Shackelford S. Saving the military surgeon: maintaining critical clinical skills in a changing military and medical environment. J Am Coll Surg 2016;222:1258–64. 10.1016/j.jamcollsurg.2016.03.031 [DOI] [PubMed] [Google Scholar]
- 14. Edwards MJ, White CE, Remick KN, Edwards KD, Gross KR. Army general surgery’s crisis of conscience. J Am Coll Surg 2018;226:1190–4. 10.1016/j.jamcollsurg.2018.03.001 [DOI] [PubMed] [Google Scholar]
- 15. Hall AB, Davis E, Vasquez M, Umberger J, Tadlock MD, Qureshi I, Walker A, Glaser J, McClendon H, Gurney JM. Current challenges in military trauma readiness: insufficient relevant surgical case volumes in military treatment facilities. J Trauma Acute Care Surg 2020;89:1054–60. 10.1097/TA.0000000000002871 [DOI] [PubMed] [Google Scholar]
- 16. Williams J, Francis A, Prey B, Conner J, Lammers D, Choi PM, Vicente D, Bingham J, McClellan J. Impact of COVID on surgical case volume at military treatment facilities with surgical residencies. Am J Surg 2023;225:897–902. 10.1016/j.amjsurg.2023.02.003 [DOI] [PubMed] [Google Scholar]
- 17. Schoenfeld AJ, Ho HT, Schoenfeld RJ, Coles C, Koehlmoos TP. Changes in surgical volume in military medical treatment facilities and military surgeon clinical combat readiness during the COVID-19 pandemic. Ann Surg Open 2023;4:e308. 10.1097/AS9.0000000000000308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. O’Reilly EB, Norris E, Ortiz-Pomales YT, Fox JP. A comparison of direct care at military medical treatment facilities with purchased care in plastic surgery operative volume. Plast Reconstr Surg Glob Open 2022;10:124–5. 10.1097/01.GOX.0000898976.03344.62 [DOI] [Google Scholar]
- 19. Holt DB, Hueman MT, Jaffin J, Sanchez M, Hamilton MA, Mabry CD, Bailey JA, Elster EA. Clinical readiness program: refocusing the military health system. Mil Med 2021;186:32–9. 10.1093/milmed/usaa385 [DOI] [PubMed] [Google Scholar]
- 20. Hall A, Qureshi I, Shackelford S, Glaser J, Bulger EM, Scalea T, Gurney J. Objective model to facilitate designation of military–civilian partnership hospitals for sustainment of military trauma readiness. Trauma Surg Acute Care Open 2019;4:e000274. 10.1136/tsaco-2018-000274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hight RA, Salcedo ES, Martin SP, Cocanour CS, Utter G, Galante JM. Level I academic trauma center integration as a model for sustaining combat surgical skills: the right surgeon in the right place for the right time. J Trauma Acute Care Surg 2015;78:1176–81. 10.1097/TA.0000000000000649 [DOI] [PubMed] [Google Scholar]
- 22. Hu P, Jansen JO, Uhlich R, Hashmi ZG, Gelbard RB, Kerby J, Cox D, Holcomb JB. It is time to look in the mirror: individual surgeon outcomes after emergent trauma laparotomy. J Trauma Acute Care Surg 2022;92:769–80. 10.1097/TA.0000000000003540 [DOI] [PubMed] [Google Scholar]
- 23. Harvin JA, Maxim T, Inaba K, Martinez-Aguilar MA, King DR, Choudhry AJ, Zielinski MD, Akinyeye S, Todd SR, Griffin RL, et al. Mortality following emergent trauma laparotomy: a multicenter, retrospective study. J Trauma Acute Care Surg 2017;83:464–8. 10.1097/TA.0000000000001619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tang A, Chehab M, Ditillo M, Asmar S, Khurrum M, Douglas M, Bible L, Kulvatunyou N, Joseph B. Regionalization of trauma care by operative experience: does the volume of emergent laparotomy matter J Trauma Acute Care Surg 2021;90:11–20. 10.1097/TA.0000000000002911 [DOI] [PubMed] [Google Scholar]
- 25. Joseph B, Azim A, Zangbar B, Bauman Z, OʼKeeffe T, Ibraheem K, Kulvatunyou N, Tang A, Latifi R, Rhee P. Improving mortality in trauma laparotomy through the evolution of damage control resuscitation: analysis of 1,030 consecutive trauma laparotomies. J Trauma Acute Care Surg 2017;82:328–33. 10.1097/TA.0000000000001273 [DOI] [PubMed] [Google Scholar]
- 26. Stinner DJ, Jahangir AA, Brown C, Bickett CR, Smith JP, Dennis BM. Building a sustainable Mil-Civ partnership to ensure a ready medical force: a single partnership site’s experience. J Trauma Acute Care Surg 2022;93:S174–8. 10.1097/TA.0000000000003632 [DOI] [PubMed] [Google Scholar]
- 27. Eckert MJ, Bonifacio AJ, Hardin RJ, Brown SR, King BT, Soliz BA, Barrigan CR, Johnson DL. The University of North Carolina at Chapel Hill and US army military-civilian medical partnership: a holistic approach to military medical readiness. J Am Coll Surg 2021;233:e126–7. 10.1016/j.jamcollsurg.2021.08.342 [DOI] [Google Scholar]
- 28. Eckert MJ, Hardin RD, Grado JR, Johnson DJ, Soliz BA, Brown SR. Military interprofessional healthcare teams: a model of what right looks like. J Am Coll Surg 2021;233:e125–6. 10.1016/j.jamcollsurg.2021.08.339 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tsaco-2023-001332supp001.pdf (42.3KB, pdf)
tsaco-2023-001332supp002.pdf (86.4KB, pdf)
Data Availability Statement
Data are available upon reasonable request.