Abstract
Background
Improving patient flow in hospitals represents a worldwide healthcare challenge. The objective of this project was to depict the effectiveness of case management in improving patient flow in a tertiary hospital setting.
Methods
Quality improvement methods, including quantitative pre-Lean and post-Lean design, the Plan-Do-Check-Act concept, the Single Minute Exchange of Dies and the ‘demand and supply approach’ of the Institute of Healthcare Improvement, were adapted to examine and modify factors influencing hospital patient flow.
Results
This study (conducted from the last quarter of 2019 through September 2022) resulted in a remarkable improvement in patient flow, as evident from the reduction in average hospital length of stay (from 11.5 to 4.4 days) and average emergency department boarding time (from 11.9 to 1.2 hours) and the improvement of bed turnover rate (from 0.57 to 0.93), (p<0.001, p=0.017, p=0.038, respectively), with net cost savings of 123 130 192 million Saudi Riyals (US$32 821 239).
Conclusion
Implementing a well-structured case management programme can enhance care coordination, streamlilne transitions, boost patient outcomes, and increase revenues within hospital settings.
Keywords: Management; Continuous quality improvement; Efficiency, Organizational; Patient satisfaction
WHAT IS ALREADY KNOWN ON THIS TOPIC
Effective patient flow management within hospital settings plays a pivotal role in influencing the quality of care, staff workload and patient outcomes. This highlights the crucial need for structured and coordinated processes to elevate the overall experience and optimize the allocation of resources.
WHAT THIS STUDY ADDS
This work accentuates the vital significance of case management in enhancing patient flow, ultimately leading to improved healthcare outcomes, operational efficiency, and cost-effectiveness. Through streamlining patient care and optimizing transitions between healthcare services, it contributes to more effective and economic healthcare systems.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This study emphasizes the importance of sustainable improvement strategies in optimizing patient flow within hospital settings. It highlights the effectiveness of tailored interventions in case management programmes, in improving coordination of care, patient outcomes, and financial performance. Customizing interventions to fit the unique needs of each organization is crucial for successful implementation and the advancement of healthcare delivery practices.
Introduction
Patient flow is a crucial element of process management in hospitals. It describes the movement of patients through the different stages of required hospital care and considers whether they are subject to unnecessary delay.1 Optimising patient flow in hospitals ensures that patients receive the best available care while saving time, effort and costs.1 Failing to achieve hospital-wide patient flow puts patients at risk for suboptimal care and potential harm, as well as increasing hospital staff burden.2 Poor patient flow is especially apparent when incoming emergency department (ED) patients cannot be immediately admitted into the hospital due to a lack of available beds.3 When the supply cannot match the demand, patients experience lower quality of care and worse health outcomes.4 This paved the way for the integration of case management (CM) into healthcare.4
CM is a healthcare process where a professional helps the patient and their family navigate through a complicated set of services available within an organisation and their community to meet their healthcare needs in a cost-effective and coordinated manner.5 Knowledge of healthcare costs and resource utilisation has accustomed CM to challenge interventions with questionable effectiveness in the healthcare process.6 Case managers are the leaders in patient flow management; through working collaboratively with and coordinating care from all hospital departments, the case manager can identify and correct barriers to patient flow as they occur. This unique role positively impacts the quality of care and operational efficiency of the healthcare system.5 Yet, further studies are necessary to confirm the effectiveness of CM interventions.
Al Hada Armed Forces Hospital (Taif, Saudi Arabia) is a tertiary care hospital and one of nine Armed Forces hospitals in the Kingdom. With a capacity of 420 beds and 3000 staff, this acute facility provides extensive medical and nursing services, including open heart surgery and kidney transplants.7 Care is required for an average of a thousand patients per day. The CM department (comprising CM, bed management and discharge coordination divisions) was established at Al Hada Armed Forces Hospital in 2016 and was recognised by the Ministry of Defence Health Services (MODHS) in December 2019. An in-depth evaluation of the hospital patient flow parameters revealed notable inefficiencies. Therefore, this initiative was started in September 2019 and aimed at enhancing patient flow in the hospital, that is, facilitating timely and efficient patient movement throughout the hospital, ultimately enhancing overall operational efficiency. The specific objective was to shed light on the role of CM practices in making the intervention plan workable and effective. The secondary aim of the endeavour was to estimate the financial return of the new interventions.
Methods
Project team
A core team of stakeholders was assembled as a central part of setting up the project. This team comprised the director of the CM department, a continuous quality improvement and patient safety (CQI & PS) coach, a case manager or bed coordinator, representatives from medical administration, human resources (HR), materials management and other allied departments, as well as a nursing representative and the most responsible physician.
The project was launched in September 2019 by the MODHS, which is one of the strategic priorities at Al Hada Armed Forces Hospital. The project team established biweekly meetings for devising interventions, orchestrating implementation updates, refining strategies and overcoming obstacles arising along the way. In addition, daily and weekly huddles with hospital stakeholders and departmental champions were commenced. All introduced measures were communicated through visual management reporting systems to all hospital units.
Measures
Process measures
Percentage of compliance with multidisciplinary team review on the eighth day, percentage of early discharge planning for complex patients, percentage of patients discharged from the hospital units before 12:00, percentage of patients with documented preliminary discharge orders the night before discharge, median time (in min) until discharge, percentage of patients admitted to hospital units before 10:00, percentage of delayed admission (lasting >45 min), waiting time (in days) for elective admission and bed turnover rate (online supplemental table 1).
bmjoq-2023-002484supp001.pdf (90.2KB, pdf)
Primary outcome measures
Primary outcome measures include average hospital length of stay (LOS, in days), average ED boarding time (in hours) and patient experience (percentage) (online supplemental table 1).
Balancing measures
Balancing measures include mortality rate, hospital-acquired infection (HAI) rate and rate of hospital readmission within 30 days (online supplemental table 1).
Baseline data were available for the ED boarding time, the average LOS and the hospital readmission rate. Other measures were initiated at the start of the project (online supplemental table 1). Data for this project were retrieved from the patient census, reports from the bed management division and the admission office and patient flow indicators from the CQI & PS department. Shadowing8 was also used for collecting observational data. Patient experience data were collected quarterly via patient surveys throughout the intervention. The data were forwarded to Press Ganey,9 a third-party company assigned by the MODHS to collect and analyse patient feedback. The reports provided by Press Ganey were used to assess and track changes in patient experience throughout the entire intervention period.
For estimating study measures, data were retrieved weekly from the hospital management information system (WIPRO) and submitted to the CQI & PS department for analysis. All data were initially validated by the CQI & PS department to ensure accuracy and reliability. Subsequently, 10% of our data (through random sampling) was independently validated by other reviewers. If the results exceeded 90%, the data were considered valid. Moreover, the MODHS arranged multiple visits to our hospital to ensure the validity and reliability of the data collection. Continuous monitoring and evaluation were performed throughout the duration of the project, according to which decisions were made either to adapt, adjust or discard the intervention.
Return on investment (ROI) estimation
Estimation of the ROI10 was used to calculate the net financial gains throughout the project, taking into consideration all the resources invested and all the amounts gained through increased revenue, reduced cost or both. ROI is estimated as the ratio of two financial estimates of net financial returns from improvement action divided by the financial investment in the improvement project. When an ROI is ≥1, the returns generated by improvement actions are greater than or equal to the costs for development and implementation, representing a positive outcome. Conversely, an ROI <1 indicates a net loss from changes in quality and utilisation, reflecting a negative outcome. Cost savings are derived from the difference between returns and cost investment.
Strategy
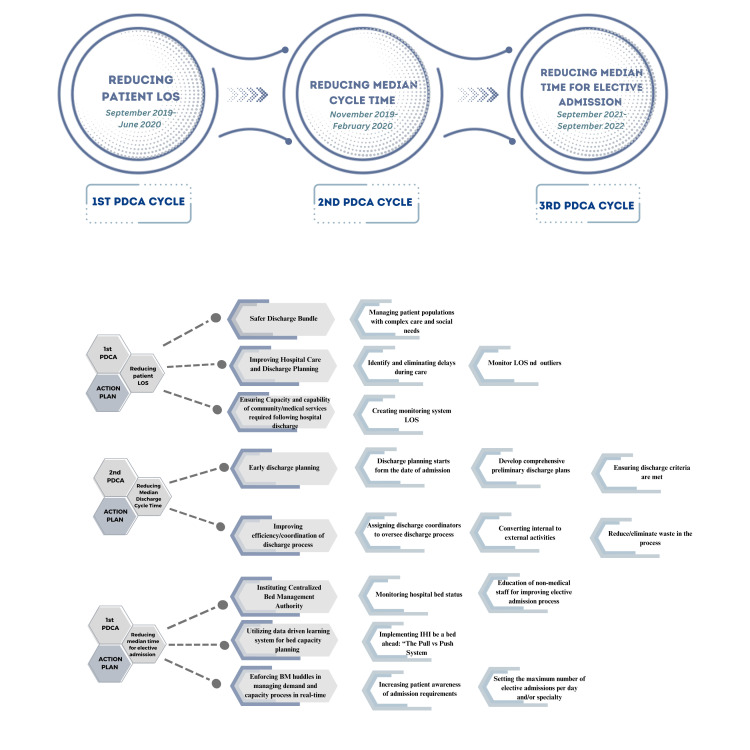
The improvement plan was introduced through a series of three Plan-Do-Check-Act (PDCA) cycles, each lasting from 3 to 9 months. The objectives of the three consecutive cycles were reducing patient LOS, reducing median discharge cycle time and reducing the median time for elective admission (figure 1). Most departments of the hospital were involved in the intervention. The inpatient wards (a total of 293 beds) were addressed. The nursery and critical care units were excluded since they have different performance indicator parameters. One pilot unit was chosen every cycle to check the effectiveness of the interventions.
Figure 1.
Outline of the objectives and approaches of the study. IHI, Institute for Healthcare Improvement; LOS, length of stay; PDCA, Plan-Do-Check-Act.
In the planning phase, the team applied the Donabedian approach11 to evaluate the structure, process and outcomes of healthcare quality and services (online supplemental file 1). The recommendations of the Institute for Healthcare Improvement (IHI)2 were adapted to improve patient flow across the hospital and modified throughout the intervention to best suit our hospital-specific situation.
First PDCA cycle
The first PDCA cycle started in September 2019. This cycle aimed at reducing the average hospital LOS through the implementation of actions that ensured that patient stays were needed or necessary according to clinical criteria for discharge and standardised LOS. The Male Medical I unit was selected as the pilot unit.
At the beginning of this cycle, the root causes for exceeding hospital LOS at Al Hada Armed Forces Hospital were identified. The top causes of prolonged stays were poor coordination of care, the unavailability of monitoring systems for LOS and the limited availability of the necessary supplies and equipment required before patient discharge.
Interventions applied during this cycle were influenced by the recommendations of the ‘Ensiab Project’.12 The interventions included the SAFER13 discharge bundle and the implementation of the RED to GREEN visual management system (based on the NHS RED and GREEN bed days).14 Flow improvement multidisciplinary teams (MDTs) were reinforced, led by a case manager for each hospital unit and daily morning MDT huddles were commenced. The objectives of MDT huddles were to monitor admission and discharge, and patient status (eg, requires moving, downgrading and discharging) and to timely identify challenges arising along the process. The IHI hospital inpatient waste identification tool15 was used to recognise waste along the process. The case manager also attended the morning patient round of the primary care team. This was an opportunity to communicate observed data, patient updates and emerging problems and to coordinate the required patient care (during hospital stay and after discharge). These data and problems were relayed to the project team for analysis.
The RED to GREEN visual management system increased the engagement of all medical staff in the project. Moreover, CM succeeded in establishing effective communication with stakeholders, which helped them understand the necessary changes and encouraged them to provide their input and to be actively engaged in the change process. This resulted in the gradual mitigation of the resistance of staff members towards the introduction of major changes to hospital processes.
To address patient transition following hospital discharge, the project team developed community/internal and external communication programmes to contact the necessary community services and healthcare facilities. These programmes covered other Armed Forces hospitals and Ministry of Health hospitals in the Taif Region, as well as home healthcare, rehabilitation and psychiatry facilities. Moreover, the need for a long-term care unit was highlighted by the project team and this has become a major strategic goal at Al Hada Armed Forces Hospital in the next 5 years.
Since standardised hospital LOSs for diagnosis-related groups (DRGs) for Al Hada Armed Forces Hospital were not available, the project requested benchmark LOSs for common diagnoses from each medical department. These standardised LOSs were created and integrated into the hospital management information system (WIPRO). This was an important step in the project that enabled the uploading of the patient data onto the system for monitoring and analysis. The hospital LOS was closely monitored. An ‘MDT Review for 7-day outliers’ form was dedicated to monitoring patients exceeding hospital LOS. Moreover, physicians had to document in Progress Notes or Physician Orders justifying the reason for keeping the patient in the hospital.
Many of the patients at Al Hada Armed Forces Hospital were geriatric with complex conditions and comorbidities, affecting the patient discharge process. These complex patient populations were managed through the efforts of case managers in coordinating patient care with social workers and other members of the interdisciplinary care team and involving family members in the process. Details of the intervention are displayed in table 1.
Table 1.
First PDCA cycle interventions aimed at reducing average hospital LOS
| Aim | Strategy | Action | Responsibility | Time frame |
| To reduce average hospital LOS | SAFER discharge bundle* | S—Senior review and board rounds are monitored as per hospital policy. | MRP case manager, discharge coordinator, nurses, social worke and home healthcare representative | September 2019–ongoing |
| A—All admitted patients have a consultant-approved care plan containing EDD and CCD. | ||||
| F—Flow of patients into, within and out of hospital, monitored by CM-led team.— | ||||
| E—Early discharges (potential and actual) identified and reviewed by the CM department. | ||||
| R—Review of all stranded patients by MDT. | ||||
| Improving hospital care and discharge planning | Attending morning rounds with the primary care team for patient status updates and progress. | Case manager or bed manager | September 2019–ongoing | |
| Communicating healthcare issues to a responsible physician and/or involved department to address problems and manage gaps in the process in a timely manner. | Case managers and primary care team | September 2019–ongoing | ||
| Relaying input on encountered problems to improve work efficiency. | BM director and case managers | September 2019–ongoing | ||
| Ensuring capacity or capability of community or medical services required following hospital discharge | Continuous monitoring of patients exceeding hospital LOS to identify the main community services required for the safe and timely discharge of patients. | BM division, CQI & PS department | September 2019–ongoing | |
| Developing community or internal and external communication programmes to support patient transition following discharge | BM division, medical administration and patient affairs | September 2019–ongoing | ||
| Identifying a long-term care unit as a major hospital strategic goal in the next 5 years. | Top management | September 2019–ongoing | ||
| Managing patient populations with complex care and social needs | Identifying patients with complex medical and social needs by the Case Manager upon admission. | Case manager | September 2019–ongoing | |
| Ensuring patients and family members are actively participating in the hospital discharge plan. | ||||
| Initiating separate rounds for complex patients, comprising all interdisciplinary team members. | ||||
| Identifying and eliminating delays during care | Using the IHI hospital inpatient waste identification tool to track delays. Managing delays in hospital services (eg, diagnostics, investigations and medical reviews). Seeking justification from the primary physician and/or involved departments for the delay in care, returning to the head of department and/or medical director in case of conflict. Using a RED to GREEN visual management system during rounds in all inpatient wards. | Case managers, bed managers, discharge coordinators and charge nurses | September 2019–ongoing | |
| Creating a monitoring system for LOS | Creating and implementing standardised hospital LOSs. | Medical administration, CQI & PS director and BM director | January 2020–ongoing | |
| Integrating standardised hospital LOSs into the hospital management information system (WIPRO). | CQI & PS director, BM division, ICT department director | January 2020–ongoing | ||
| Monitoring LOS and outliers | Monitoring hospital LOS for each admitted patient (as compared with standardised LOS). Monitoring and managing 7-day and 30-day outliers. | CM department, admitting clerk and ED nurses | January 2020–ongoing | |
| Quarterly meeting with the BU committee to assess results, address areas for improvement and realign goals and strategies. | BU committee, BM director, MDT representatives, DDC head | Quarterly | ||
| Activation of DDC (subcommittee of the BU committee) to facilitate discharge. | December 2020–ongoing |
*Adapted from the central policy of the medical services division.
BM, bed management; BU, bed utilisation; CCD, clinical criteria for discharge; CM, case management; CQI & PS, continuous quality improvement & patient safety; DDC, difficult discharge committee; ED, emergency department; EDD, expected discharge date; ICT, information and communication technology; IHI, Institute for Healthcare Improvement; LOS, length of stay; MDT, multidisciplinary team; MRP, most responsible physician; OPD, outpatient department.
Second PDCA cycle
At the beginning of this cycle, there was an observable prolonged median discharge cycle time. Shadowing of a randomly selected discharge order showed that the time required for completing the discharge process was 225 min. This resulted in a bottleneck in hospital operations. Thus, the aim of this cycle was to reduce the mean discharge cycle time. The pilot unit during this cycle was the Orthopaedics Medical and Surgical unit.
Lean methodology was applied to test parameters involved in the discharge process and to evaluate the outcome of the interventions. Value stream mapping16 was used to trace patient flow throughout the discharge process, and Single-Minute Exchange of Dies17 was used to determine the activities negatively impacting the patient discharge process. Two main factors hindered the patient discharge process: remarkable variability in how the discharge process was carried out and the preparation of the discharge prescription. This was caused by the absence of a preliminary discharge order.
Steps for early planning of patient discharge were thus commenced, taking into consideration the criteria for medical readiness of discharge (medical and surgical cases) for Al Hada Armed Forces Hospital. A discharge coordinator participated in morning rounds to monitor and streamline the discharge process and to collect and report data. One of the main interventions in this cycle was to enforce the preparation or documentation of preliminary discharge orders the night before discharge. This provided time for informing patients and their relatives and for performing final activities (such as revising test results, nurse education, informing family members to arrange patient discharge or hospital transportation and completion of paperwork) to make timely discharge possible. The involvement of several departments (eg, physiotherapy, social workers and health educators) was mandatory during this phase.
Waste contributing to extended discharge cycle time was identified in waiting times (waiting for a physician to clear the patient for discharge and waiting for family members to fulfil patient discharge) and in unnecessary motion within the process (submission of prescriptions by nurses to the pharmacy department and acquisition of necessary medical supplies and devices by family members from the materials management department (MMD)). Several interventions were introduced. A paperless prescription system was implemented via the Hospital Management Information System (WIPRO), eliminating the need for nurses to physically submit prescriptions to the pharmacy department. This allowed for fast preparation and delivery of take-out medications. Additionally, acquiring supplies and medical equipment from the MMD became the responsibility of case managers upon requisition by the attending physician and was individually delivered to patients prior to discharge. To improve the early discharge of patients (before 12:00), case managers and discharge coordinators were involved in anticipating referrals to special facilities so that continuity of care could be guaranteed. Interventions are detailed in table 2.
Table 2.
Second PDCA cycle interventions aimed at reducing discharge cycle time
| Aim | Strategy | Action | Responsibility | Time frame |
| To reduce discharge cycle time | Early discharge planning | Starting discharge planning from the date of admission. | CM department | September 2019–ongoing |
| Ensuring timely patient referral (to physiotherapy, social worker, home healthcare and rehabilitation) as per treatment plan prior to discharge. | Case managers and discharge coordinators |
September 2019–ongoing | ||
| Developing comprehensive preliminary discharge plans to meet the ongoing medical and social needs of patients after discharge. Ensuring discharge criteria are met (preparing discharge summary, medications and OPD follow-up). Completing patient reassessment prior to discharge. |
MRP and case managers |
September 2019–ongoing | ||
| Enhancing communication among care team members and with patients and family members. Arranging MDT meetings with family members as needed. |
CM department | September 2019–ongoing | ||
| Improving efficiency and coordination of the discharge process | Studying discharge process using Lean methodology | CQI & PS department | November 2019 | |
Assigning a discharge coordinator to oversee the discharge process:
|
Discharge coordinators and MRPs |
September 2019–ongoing | ||
Converting internal to external activities:
|
Case managers, bed managers, discharge coordinators, nurses, MMD and MRP |
September 2019–ongoing | ||
Eliminating or reducing waste in the process:
|
Pharmacy department, MMD, OPD, medical administration and ICT department |
September 2019–ongoing | ||
| Patients for discharge are seen first in the morning rounds. | Medical administration and MRP | |||
| Final discharge order and medication prescription were finished before 9:00. | Medical administration and MRP |
CM, case management; CQI &PS, continuous quality improvement & patient safety; ED, emergency department; ICT, information and communication technology; MDT, multidisciplinary team; MMD, materials management department; MRP, most responsible physician; OPD, outpatient department.
During the COVID-19 pandemic, there were delays in the discharge process and prolongation of LOSs due to constant review of infectious disease protocols and re-swabbing for patient clearance and discharge. The CM department tackled this challenge by conducting a continuous review of the plan of care for each patient, providing care coordination to the responsible physician and following up and expediting laboratory test results.
Third PDCA cycle
The third PDCA cycle of the initiative commenced in September 2021, not immediately after the second cycle, due to the COVID-19 pandemic. Nevertheless, the interventions of the first and second cycles were sustained throughout the pandemic. The Male Surgical 1 unit was the pilot unit for this cycle.
At the beginning of this cycle, a prolonged median time for elective admission was observed (6 days). The main root causes of long admission times were a mismatch between demand and supply of inpatient beds, a lack of knowledge of non-medical staff regarding necessary medical terminology and diagnoses and a lack of awareness of patients regarding hospital preadmission requirements.
The main intervention was the establishment of a bed management division (following the CM department) to act as a centralised bed management authority that handles all admissions and transfers throughout the hospital. Moreover, the Admission Office, previously under the department of patient affairs, was transferred to the authority of the CM department, bringing both elective and emergency admissions under the purview of CM. Recruiting additional staff was necessary to support the new division. Internal hiring (ie, rehiring of existing staff) proved to be a cost-effective approach that also ensured staff retention.
Bed management monitored and analysed hospital-wide patient flow patterns to predict volume and seasonal variations. Furthermore, the IHI Be a Bed Ahead: ‘The Pull versus Push System’18 was implemented to address delays in patient movement between care points. In addition, daily morning bed management huddles were commenced, where bed managers monitored patient admissions and managed bed capacity and demand issues with the care team in real time.
Education of non-medical staff pertaining to medical terminology and hospital patient flow processes was necessary to improve the admission process time yet proved to be challenging. Nevertheless, the project team hired an admission office manager with a background in nursing and experience in CM or bed management, making the education programme possible. In addition, several interventions were implemented to improve patient and family member awareness of preadmission requirements. Details of the interventions of the third PDCA cycle are detailed in table 3.
Table 3.
Third PDCA cycle interventions aimed at reducing median time to elective admission
| Aim | Strategy | Action | Responsibility | Time frame |
| To reduce the median time to elective admission | Instituting a centralised bed management authority | Establishing BM as a division of the CM department. | August 2021 | |
| Moving admission office authority to the CM department to enable processing of all hospital admissions and transfers. | August 2021 | |||
| Initiating daily bed meetings to oversee bed placement of admitted and transferred patients and update or report hospital bed status. | Case managers, bed managers and discharge coordinators | August 2021–ongoing | ||
| Using data-driven learning systems for bed capacity planning | Using advanced data analytics coupled with expert physician knowledge to understand variation in bed capacity patterns. | BM division and admission office | August 2021–ongoing | |
| Predicting seasonal and volume variations to forecast changes in demand patterns. | BM division and admission office | August 2021–ongoing | ||
| Enforcing BM huddles and managing demand and capacity processes in real-time | Daily morning BM huddle | |||
| Each unit representative is given 1 min to communicate the current census, anticipated discharges, admissions and transfers within the hospital (and other major issues). | BM division | August 2021–ongoing | ||
| Meeting times are limited to 10–15 min. | ||||
| Using huddles to make decisions regarding cancellation of elective surgeries or procedures based on the demand of ED or other services. Managing issues surrounding gaps in communication and decision-making of the admission process. | ||||
| Monitoring hospital bed status | Tracing emergency and elective admissions all year round for early recognition of high census and capacity surges and expediting surge protocols. Updating hospital bed status to guarantee vacant beds for elective surgery admission. | BM division and admission office | August 2021–ongoing | |
| Implementing IHI Be a bed ahead: ‘The Pull versus Push’ system | Proactive management of admissions or transfers to facilitate the patient movement to next point of care. | BM division, nursing, administration and admission office | August 2021–ongoing | |
| Anticipating demand and having a bed ready in an inpatient unit into which a patient can be moved as soon as occurs. | ||||
| Increasing patient awareness of admission requirements | Providing information booklets for patients. Providing hospital-wide educational posters complemented with barcodes for direct access on mobile phones. Offering routine education by admission office personnel to patients prior to admission (including preadmission requirements, patient rights and responsibilities, and hospital information). Identifying cases scheduled for elective surgery to inform patients or family members of arriving early at the hospital for timely admission and proper preparation. Notifying patients via phone messages to ensure admission before 10:00. | BM division, admission office and OPD | August 2021–ongoing | |
| Education of non-medical staff to improve the elective admission process | Hiring an admission office manager with a nursing specialty and knowledge of the patient flow process to offer education to non-medical staff. Providing in-service education for admission office staff on medical terminology and routine workflow. Providing internet services to admission office staff to facilitate looking up unknown terminologies or diagnoses. | BM division and admission office | August 2021– ongoing | |
| Providing orientation by the BM division on the hospital patient flow process. | ||||
| Setting the maximum number of elective admissions per day and/or specialty | Screening of all additional cases per day from outpatient departments. | Medical administration, BM division, admission office, OR department | August 2021– ongoing | |
| Informing all heads of departments (through distributed memos) of the suggested total number of patients for elective surgeries per day or week to prevent overbooking resulting in cancellation of surgery. | ||||
BM, bed management; CM, case management; ED, emergency department; IHI, Institute for Healthcare Improvement; OPD, outpatient department; OR, operating room; PDCA, Plan-Do-Check-Act.
Results
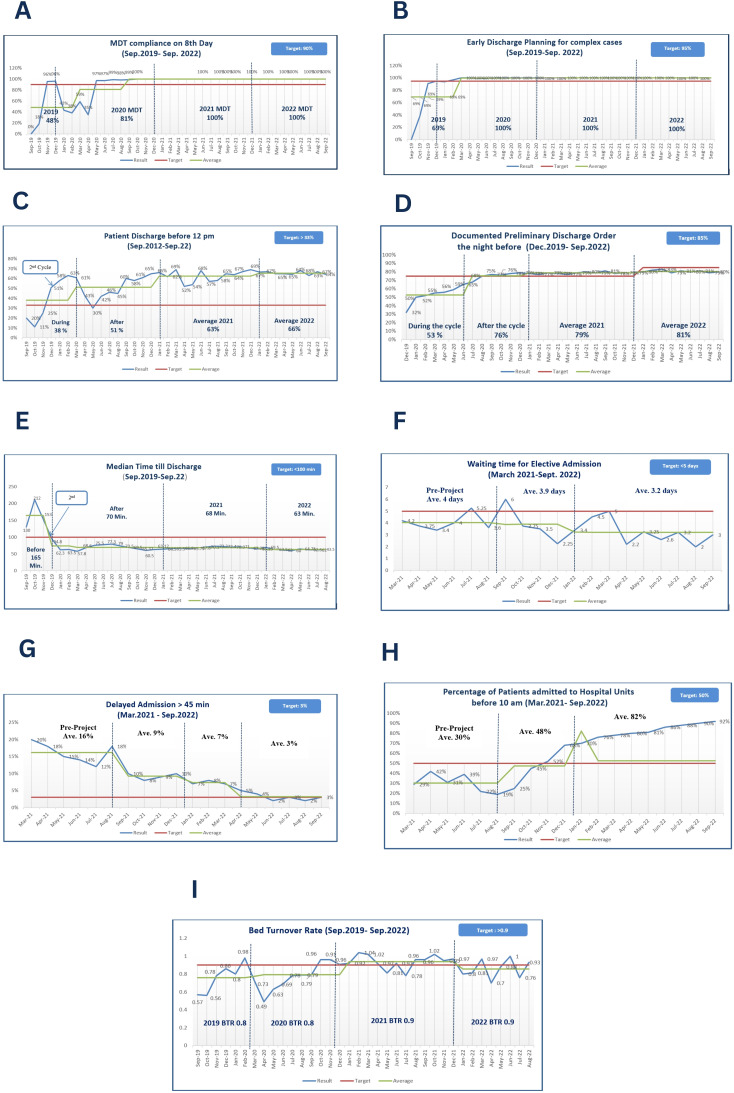
This project comprised three overlapping cycles of interventions starting in September 2019 through September 2022. The aim of the first PDCA cycle was to reduce the average hospital LOS. Regarding process measures used to evaluate these cycle interventions, the percentage of compliance with MDT review on the eighth day fluctuated throughout the first 12 months of the intervention, with the value exceeding the expected target beginning in April 2020. A 100% compliance was achieved in September 2020, and this compliance was sustained until the end of the project (p=0.009) (figure 2A, table 4). The percentage of early discharge planning for complex patients increased from a baseline of 0% at the beginning of the intervention to 100% in February 2020 and sustained at 100% until the end of the project; nevertheless, the change was not significant (figure 2B, table 4).
Figure 2.
Process measures. (A) MDT compliance on the eighth day (%). (B) Early initiation of discharge planning for complex cases (%). (C) Patients discharged from the hospital units before 12:00 (%). (D) Patients with documented preliminary discharge orders the night before discharge (%). (E) Median time (in minutes) until discharge from an inpatient setting. (F) Waiting time (in days) for elective admission. (G) Delayed admission (lasting >45 min) (%). (H) Patients admitted to hospital units before 10:00 (%). (I) Bed turnover rate. Ave., average; BTR, bed turnover rate; MDT, multidisciplinary team.
Table 4.
Project measures, baseline versus postintervention
| Measure | Type of measure | Value | P value | PDCA cycle |
Aim/impact | |
| Baseline | Postintervention | |||||
| Compliance with MDT review on the eighth day | Process | 0.0% | 100.0% | 0.009* | First | Reducing hospital LOS |
| Early discharge planning for complex patients | Process | 69.0% | 100.0% | 0.116 | First | Reducing hospital LOS |
| Patients discharged before 12:00 (%) | Process | 20.0% | 64.0% | 0.001* | Second | Reducing median discharge cycle time |
| Patients with documented preliminary discharge order the night before discharge | Process | 32.0% | 85.0% | 0.0018 | Second | Reducing median discharge cycle time |
| Median time until discharge | Process | 212.0 min | 61.5 min | 0.057 | Second | Reducing median discharge cycle time |
| Waiting time for elective admission | Process | 6.0 days | 3.0 days | 0.082 | Third | Reducing median time to elective admission |
| Delayed admissions (lasting >45 min) | Process | 10.0% | 3.0% | <0.001* | Third | Reducing median time to elective admission |
| Patients admitted to hospital units before 10:00 | Process | 19.0% | 92.0% | <0.001* | Third | Reducing median time to elective admission |
| Bed turnover rate | Process | 0.57 | 0.93 | 0.038* | First | Reducing hospital LOS |
| Average LOS | Outcome | 11.5 days | 4.4 days | <0.001* | First | Reducing hospital LOS |
| Second | Reducing median discharge cycle time | |||||
| Third | Reducing median time to elective admission | |||||
| ED Boarding time | Outcome | 11.9 hours | 1.2 hours | 0.017* | First | Reducing hospital LOS |
| Second | Reducing median discharge cycle time | |||||
| Third | Reducing median time to elective admission | |||||
| Patient experience Admission Discharge |
Outcome | 85.1% 83.5% |
83.5% 87.9% |
N/A N/A |
First | Reducing hospital LOS |
| Second | Reducing median discharge cycle time | |||||
| Third | Reducing median time to elective admission | |||||
| Hospital readmission within 30 days | Balancing | 7.5% | 0.0% | 0.065 | First | Reducing hospital LOS |
| Second | Reducing median discharge cycle time | |||||
| Third | Reducing median time to elective admission | |||||
| Hospital mortality rate | Balancing | 2.5% | 2.5% | 0.479 | First | Reducing hospital LOS |
| Second | Reducing median discharge cycle time | |||||
| Third | Reducing median time to elective admission | |||||
| Hospital-acquired infection rate | Balancing | 1.8% | 1.3% | 0.037* | First | Reducing hospital LOS |
| Second | Reducing median discharge cycle time | |||||
| Third | Reducing median time to elective admission | |||||
*Significant at p<0.05, t-test.
ED, emergency department; LOS, length of stay; MDT, multidisciplinary team; PDCA, Plan-Do-Check-Act.
The second PDCA cycle was aimed at reducing discharge cycle time. To examine the impact of interventions, the following process measures were evaluated: percentage of patients discharged from the hospital units before 12:00, percentage of patients with documented preliminary discharge orders the night before discharge and median time until discharge. The baseline percentage of patients discharged before 12:00 was 20%. This measure rapidly increased, exceeding the expected target and reaching 63% in February 2020. It then plummeted between April 2020 and September 2020 due to the difficulty of attaining the interventions during the COVID-19 pandemic. The measure then gradually improved, from 30% in May 2019, exceeding the expected target in August 2020 (60%), and reaching 66% at the end of the initiative (p=0.001) (figure 2C, table 4). The percentage of patients with documented preliminary discharge orders the night before discharge started at a baseline of 32% and steadily increased to achieve the expected target in July 2020, and reaching 85% at the end of the initiative (p=0.001) (figure 2D, table 4). The baseline median time until discharge was estimated at 212 min in October 2019. This was rapidly decreased to 62.3 min in January 2020. The decrease was sustained until the end of the initiative, reaching 63 min at the end of the intervention. Yet, this 71% improvement was not statistically significant (figure 2E, table 4).
During the third PDCA cycle, reducing the median waiting time for elective admission was the main target of the interventions. Process measures examined for this cycle included waiting time for elective admission, the percentage of delayed admissions (lasting >45 min) and the percentage of patients admitted to hospital units before 10:00. The baseline measure of waiting time for elective admission was 6 days in September 2021. The median values fluctuated thereafter, showing increases and decreases still below the expected target level. By the end of the initiative, the median time was reduced by 50% (3 days in September 2022); nevertheless, the change was not statistically significant (figure 2F, table 4). Median delayed admission was estimated at 10% at baseline (September 2021). The measure gradually decreased, reaching 3% at the end of the initiative (p<0.001) (figure 2G, table 4). The percentage of patients admitted to hospital units before 10:00 started at a baseline value of 19% (September 2021). This measure gradually increased to 92% at the end of the initiative (p<0.001) (figure 2H, table 4).
Bed turnover rate, the process measure influenced by all project interventions, was initially estimated at 0.57 in September 2019. This gradually increased to 0.98 in February 2020, after which there was a rapid drop continuing until April 2020 due to the failure to sustain the interventions during the COVID-19 pandemic. The measure then gradually increased to 0.96 in October 2020, after which the increase was sustained, reaching 0.93 at the end of the initiative (p=0.038) (figure 2I, table 4).
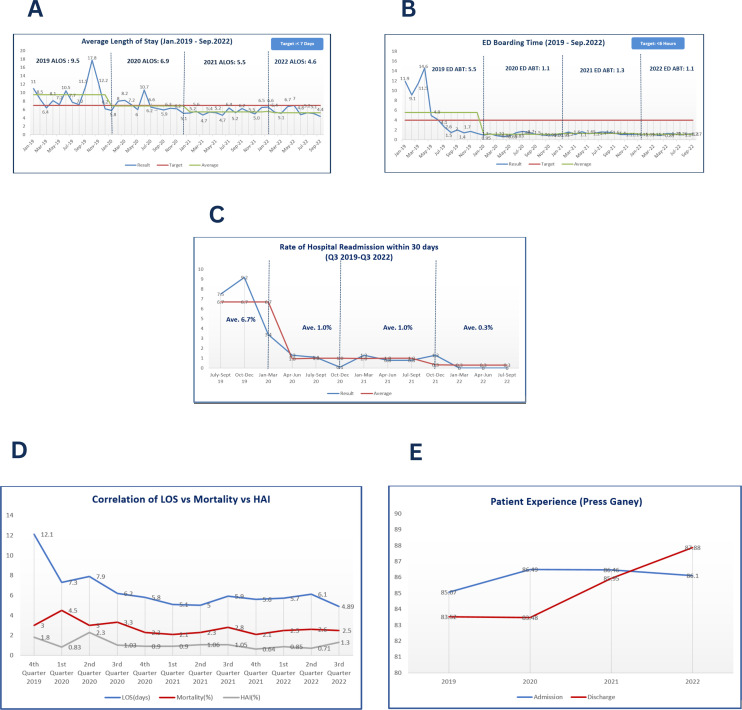
The outcome measures of this project were the average hospital LOS, the average ED boarding time, and patient experience. The baseline average hospital LOS was 11.5 in January 2019. The measure fluctuated remarkably until July 2020 (reaching 6.2), after which the measure was gradually reduced to 4.4 days at the end of the intervention (p<0.001) (figure 3A, table 4). The baseline average ED boarding time was 11.9 hours in January 2019. This rapidly dropped until July 2019, after which the reduction was sustained, reaching 1.2 hours at the end of the intervention (p=0.017) (figure 3B, table 4). Regarding patient experience, the domains of inpatient admission and discharge were specifically targeted. There was a gradual and sustainable improvement in patient experience of the admission process from a baseline of 85.1% in 2019 to 86.1% in 2022. Satisfaction with the discharge process increased from 83.5% at baseline in 2019 to 87.9% in 2022 (figure 3E, table 4).
Figure 3.
Outcome and balance measures (A) ALOS (in days). (B) ED boarding time (in min). (C) Rate of hospital readmission within 30 days. (D) Correlation of hospital LOS with mortality HAI rates. (E) Patient experience in the inpatient admission and discharge domains. Ave., average; ALOS, average length of stay; ED, emergency department; HAI, hospital-acquired infection; Q3, Quarter 3.
The balancing measures of the project were the hospital readmission rate within 30 days, the hospital mortality rate and the HAI rate. The hospital readmission rate was estimated at baseline in September 2019 (7.5%). This rapidly dropped to 1.2% in June 2020. The measure then gradually decreased to 0% in December 2021, with this value sustained to the end of the initiative. Nevertheless, this change was not statistically significant (figure 3C, table 4). Regarding mortality, the baseline measurement in the fourth quarter of 2019 was 2.5%, which increased to 4.5% in the first quarter of 2020. This was followed by a steady decrease to 2.5% at the end of the intervention, which was not correlated with hospital LOS. On the other hand, the HAI rate started at 1.8% at baseline in the fourth quarter of 2019. This declined in the first quarter of 2020, reaching 0.8%, followed by a rise to 2.3% in the second quarter of 2020. The HAI rate steadily decreased thereafter, reaching 1.3% at the end of the initiative, being correlated with hospital LOS (p=0.037) (figure 3D, table 4).
ROI estimation
ROI10 was estimated to determine the economic impact of the intervention. ROI was calculated as the ratio of two financial estimates of net financial returns from improvement action (cost reduction due to reducing hospital LOS) divided by the financial investment in the improvement project (internal hiring of staff for the bed management division). Cost savings were derived from the difference between returns (cost reduction resulting from reducing hospital LOS) and cost investment (internal hiring of staff for the bed management division).
The reduction of hospital LOS at Al Hada Armed Forces Hospital resulted in net financial returns of 128 032 692 Saudi Riyals (SAR) (table 5), while the financial investment in the improvement action was estimated at 4 902 500 SAR (table 6). The net cost savings (ie, net financial returns−financial investment) were estimated at 123 130 192 SAR (US$32 821 239). Therefore, the ROI was estimated at 26.11.
Table 5.
Net financial returns due to the improvement plan
| Indicator | Year | ||
| 2020 | 2021 | 2022 | |
| Total number of beds | 220 | 283 | 293 |
| Bed occupancy rate (%) | 62.0 | 81.0 | 75.0 |
| Current bed use | 136 | 229 | 220 |
| Hospital LOS (days) before | 9.5 | 6.8 | 5.5 |
| Hospital LOS (days) after | 6.8 | 5.5 | 4.6 |
| Bed demand with new LOS | 98 | 185 | 184 |
| Gain in available beds | 39 | 44 | 36 |
| Daily bed cost (SAR) | 3000.0 | 3000.0 | 3000.0 |
| Daily operational efficiency (SAR) | 116 299 | 131 470 | 107 877 |
| Monthly operational efficiency (SAR) | 3 488 968 | 3 944 104 | 3 236 318 |
| Annual operational efficiency (SAR) | 41 867 621.0 | 47 329 253 | 38 835 818 |
| Net financial return | 128 032 692 SAR | ||
LOS, length of stay; SAR, Saudi Riyals.
Table 6.
Financial investment in the improvement action
| Internal hiring | September 2019–September 2020 | September 2020–September 2021 | September 2021–September 2022 | ||||||
| No. of staff | Monthly (SAR) | Annual (SAR) | No. of staff | Monthly (SAR) | Annual (SAR) | No. of staff | Monthly (SAR) | Annual (SAR) | |
| Saudi staff salary | 2 | 8000 | 192 000 | 2 | 8000 | 192 000 | 6 | 8000 | 576 000 |
| Non-Saudi staff salary | 5 | 13 000 | 780 000 | 9 | 13 000 | 1 404 000 | 11 | 13 000 | 1 716 000 |
| Initial training cost | 7 | 2500 | 17 500 | 4 | 2500 | 10 000 | 6 | 2500 | 15 000 |
| Annual cost (SAR) | 989 500 | 1 606 000 | 2 307 000 | ||||||
| Total financial investment | 4 902 500 SAR | ||||||||
SAR, Saudi Riyals.
Discussion
The Saudi population has grown exponentially in the last 20 years, leading to an increase in healthcare expenditure estimated at US$2.4 billion per year.19 Like most countries around the globe, Saudi Arabia experiences challenges in providing cost-effective healthcare services while ensuring the quality of care in its public facilities. Healthcare transformation is a central goal of Saudi Arabia’s Vision 2030.20 Saudi Arabia has opted to restructure its healthcare system through privatising public hospitals, a globally implemented solution for overcoming the financial burden of inefficient and unsatisfactory healthcare systems.21 Yet Vision 2030 sets the path for using innovation to enhance operational efficiency and financial sustainability in healthcare.20 Thus, the adoption of innovative CM approaches aligns with and contributes to Saudi’s Vision 2030.
The goal of this project was to streamline patient care, focusing on the role of CM as the main drive for the change package. The initiative started in September 2019 and was concluded in September 2022. The interventions were implemented via three overlapping PDCA cycles. All project measures (process, balancing and outcome) were continuously monitored. Hospital LOS has been established as a measure of the efficiency of healthcare.22 Unnecessarily long hospital stays are associated with poor patient outcomes, including hospital-acquired infections and increased mortality,23 as well as increased costs and negative patient experiences.24 Long patient LOSs reduce the operational efficiency of healthcare systems, burden the staff and increase the cost of unnecessary bed occupancy24 and the economic impact of adverse events.25 26 We used average hospital LOS as the major outcome measure of this initiative. The average hospital LOS for all causes across the Organisation for Economic Cooperation and Development countries was about 8 days. Turkey and Mexico had the shortest stays (about 4 days), whereas Japan and Korea had the longest stays (over 16 days).27
In the first PDCA cycle, CM focused on the coordination of patient care among all involved parties. One approach used in this project was enforcing the role of MDTs. MDTs make interprofessional education and collaboration possible.28 29 This collaboration allowed for problem-solving and decision-making in real-time. Moreover, the CM introduced measures to overcome the delayed transition of patients to other care or community settings, a well-known problem in healthcare that delays patient discharge and unnecessarily prolongs LOS.30 This was achieved by identifying patients with complex social and medical needs upon admission and by developing communication programmes addressing target care and community services. Proper transition of care has been shown to reduce hospital readmissions,31 which is in line with the reduction of the hospital readmission rate in our study.
Discharge planning is currently an important element in managing healthcare systems. Several authors have declared morning hours unsuitable for preparing the preliminary discharge order and this should ideally occur the day before discharge, when the patient has been tentatively identified as ready to leave.32 33 The planning of the discharge process was successfully tackled in the second PDCA cycle using several interventions. Discharge planning has been shown to be effective in reducing hospital LOSs,34 35 which is in line with our results.
Bed management was addressed in the third PDCA cycle. CM created a central bed management authority, moving all relevant hospital sections under its umbrella. This made the orchestration of all hospital admissions and transfers possible, with the aim of monitoring hospital beds and providing empty beds for elective and emergency admissions, to match demand and capacity. This resulted in a successful reduction of waiting times for elective admissions and the ED boarding time and increased hospital operational efficiency. The role of bed management in improving patient flow and hospital operational efficiency has been confirmed in several studies.36 37
The project team used internal hiring to recruit staff for the newly developed Bed Management Division. The advantages of internal hiring are multidimensional; short recruitment process, reduced recruitment costs, no need for advertising, and the fact that internal recruits are already familiar with the organisation’s culture and processes.38 In addition to achieving staff retention, this proved to be a rapid solution, which resulted in 315 000 SAR in estimated cost savings that would have otherwise been incurred in the external hiring of non-Saudi staff.
Being a tertiary care facility, Al Hada Armed Forces Hospital is the destination of complex patients with comorbidities requiring special diagnostics and treatment plans. CM and MDT approaches are the most common interventions used to address complexity in hospital settings, where complex patients are identified and engaged to prevent worsening health and improve health outcomes and patient satisfaction.29
Patients engaged in their own healthcare are believed to have better health outcomes and to be more satisfied with the service.39 40 But this is hard to achieve in an inpatient setting.39 Nevertheless, involving patients and their family members in discharge and admission planning (in the first and third PDCA cycles, respectively) proved to be an integral factor in the success of the improvement.
The importance of data-driven approaches for improving healthcare has been recently highlighted in the literature.30 From the beginning of the project, CM integrated data-driven approaches into its process. This facilitated data analysis, collaboration of care and decision-making, making the study interventions successful. This is in line with the results of several studies using data-driven approaches in comparable settings.30 32
Patient experience serves as a crucial outcome measure for assessing the effectiveness of hospital-wide patient flow improvements.41 This study followed patient satisfaction with admission and discharge processes, which has shown a steady increase over the period of the intervention.
Reducing average hospital LOS has been found to reduce mortality rates.42 However, this could not be demonstrated in our study. This could be explained by the complexity of the patient population at Al Hada Armed Forces Hospital. Moreover, increased mortality rates due to the COVID-19 pandemic further affected our findings. On the other hand, hospital LOS had a positive impact on the HAI rate in our study. This is consistent with the findings of various studies.43 44
The net cost savings of the initiative amounted to 123 million SAR over the 3 years of the project. The financial revenue generated by the project was exceptional, with an ROI of 26. According to the Agency for Healthcare Research and Quality,10 an ROI of 26 indicates that for every 1 SAR invested in the initiative, the hospital gained 26 SAR. This is in accordance with recent studies that have shown that managing patient flows through CM is not only beneficial to the patient but is also beneficial to the organisation.32 34 The literature is divided on the cost-effectiveness of CM,45 which is probably explained by the wide variability of CM approaches. Nevertheless, our interventions proved to be cost-effective in our hospital setting.
Lessons learnt
The changes implemented in this project—the utilisation of case managers, bed managers, discharge coordinators and admission officers, coupled with modification of hospital-related processes and a patient or family-centred care approach have resulted in significant improvements in patient flow and a reduction in unnecessary hospital stays, with favourable financial outcomes. This model embodies the potential for sustainability and exportability.
The sustainability of these improvements relies on continuous implementation and refining of the roles and processes involved. This requires effective communication among the supervising body, including regular huddles, to timely identify and address challenges arising during the process. Ongoing training programmes and heightened awareness among healthcare professionals can help maintain the momentum and ensure long-term success in patient flow enhancements. The changes involved in this project can also be exportable. Establishing dedicated CM departments in each military hospital in Saudi Arabia can further solidify these changes and provide a framework for future improvements. Interinstitutional communication is necessary to discuss the specific strategies for transfer and the sustainability of the interventions. Additionally, highlighting positive financial impact and patient benefit can emphasise the value of these interventions and their potential replication in other healthcare settings.
In summary, the lessons learnt from this project underscore the importance of prioritising patient safety, optimising efficiency, improving accessibility and implementing sustainable solutions. By incorporating these lessons into future initiatives, healthcare organisations can strive for continuous improvement in patient care and operational efficiency.
Limitations
The first PDCA cycle of our initiative coincided with two ongoing projects, NO WAIT46 and the patient flow optimisation project47 of the CM department. Therefore, it is challenging to quantify the extent of change solely attributable to the interventions of this initiative. Assessing the impact of the intervention on hospital staff and their satisfaction with the change would have been a valuable addition to the work, but this was not addressed in the study. Additionally, we acknowledge the limited scope of the patient experience domain in this study, which focused on the inpatient domain encompassing admission and discharge processes. While these aspects are crucial for patient satisfaction and overall experience, other important domains of patient experience were not addressed. Further research and study should explore all satisfaction domains of the patient journey related to hospital LOS, such as communication with healthcare providers, involvement in treatment decisions, pain management, and overall care coordination.
It is important to note that although the findings of this study align with previous research, the context of each healthcare organisation may vary, and the specific interventions implemented may differ. Therefore, it is essential to consider the unique characteristics and needs of each organisation when designing and implementing CM interventions.
Conclusion
This project demonstrates that CM can improve patient flow in a hospital setting through the roles of case managers, bed managers, discharge coordinators and admission officers and through modifying hospital-related processes (admission/discharge planning, MDT huddles and others), with a positive financial impact due to a reduction of the costs of unnecessary inpatient stays. This project also demonstrates that a sustainable solution, rather than a short-term intervention, can be successfully implemented. The current intervention can serve as a reference point for future improvement projects dealing with patient flow in hospitals and how it contributes to quality improvement and patient benefit.
Due to the remarkable results of this improvement project, it was recommended that this set of interventions be disseminated to the MODHS and its satellites. The project team has begun professional training programmes across hospitals in the MODHS with the objectives of creating awareness about patient flow, teaching methods of improving patient flow and setting the groundwork for establishing CM departments in each hospital.
While challenges and limitations were encountered, the study has provided valuable insights into the complexities of optimising patient flow in a hospital setting. By addressing these challenges and building upon the successes of this project, hospitals can continue to improve patient care, resource utilisation, and overall operational efficiency. This research contributes to the body of knowledge on patient flow optimisation and provides a framework for future studies and implementations in other healthcare settings.
Acknowledgments
We would like to express our sincere thanks to our leader Dr. Ahmed Mohammed Al Amri, the CEO of the Health Services Directorate of Saudi Arabia, for his unlimited support and guidance in improving patient flow in our healthcare system. We like to extend our gratitude to Dr. Noura Alnowaiser, Executive Healthcare Quality Director, and Col. Dr. Yasser Alotaibi, Deputy Director of Quality improvement and Patient Safety at the Ministry of Defence Health Division, for guiding and supporting us in achieving our goals along this journey. Special thanks to Dr. Alia Ellawindy for her invaluable guidance and expertise throughout the study and publication. Finally, we would like to convey our heartfelt thanks to all medical and non-medical staff who helped make this whole process a great success.
Footnotes
Contributors: SAH is the main author and project team leader, guarantor of this work, accepts full responsibility for the work and/or conduct of the study, had access to the data and controlled the decision to publish. BA provided the ultimate leadership support for carrying out this study. LE research the cause of process variation, was involved in the selection and using the process improvement tools and aided in the analysis and interpretation of the results. FLB developed the research idea, was involved in designing the intervention along with the case management department and CQI & PS specialist. All authors discussed the results and prepared the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. NEJM Catalyst . What is patient flow?. NEJM Catalyst; 2018. 10.1056/CAT.18.0289 [DOI] [Google Scholar]
- 2. Rutherford PA, Anderson A, Kotagal UR, et al. Achieving hospital-wide patient flow (second edition). IHI white paper. Boston, Massachusetts: Institute for Healthcare Improvement, 2020. Available: www.ihi.org [Google Scholar]
- 3. Rojas-García A, Turner S, Pizzo E, et al. Impact and experiences of delayed discharge: a mixed-studies systemic review. Health Expect 2018;21:41–56. 10.1111/hex.12619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fraser K, Perez R. The evolution of case management and the professional case manager. In: Fraser K, Perez R, Latour C, eds. CMSA’s Integrated Case Management: a Manual for Case Managers by Case Managers. Springer Publishing Company, 2018: 1–20. 10.1891/9780826169518.0001 [DOI] [Google Scholar]
- 5. Giardino AP, De Jesus O. Case management. In: Statpearls [Internet]. Treasure Island (FL). Statpearls publishing, 2023. Available: https://www.ncbi.nlm.nih.gov/books/NBK562214/ [Google Scholar]
- 6. Proudlove N, Boaden R, Jorgensen J. Developing bed managers: the why and the how. J Nurs Manag 2007;15:34–42. 10.1111/j.1365-2934.2006.00632.x [DOI] [PubMed] [Google Scholar]
- 7. Daniels S, Ramey M. Healthcare economics and hospital case manager. in: the leader’s guide to hospital case management. In: Daniels S, Ramey M, eds. The Leader’s Guide to Hospital Case Management. Jones and Bartlett Publishers, 2005: 4–11. [Google Scholar]
- 8. McDonald S. Studying actions in context: a qualitative shadowing method for organizational research. Qual Res 2005;5:455–73. 10.1177/1468794105056923 [DOI] [Google Scholar]
- 9. PressGaney [Internet]. n.d. Available: https://www.pressganey.com/
- 10. AHRQ . Return on investment estimation. n.d. Available: https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/qitoolkit/combined/f1_combo_returnoninvestment.pdf
- 11. Panteli D, Quentin W, Busse R, et al. Understanding healthcare quality strategies: a five-lens framework. In: Busse R, Klazinga N, Panteli D, eds. Improving Healthcare Quality in Europe: Characteristics, Effectiveness and Implementation of Different Strategies. Copenhagen (Denmark): European Observatory on Health Systems and Policies.(Health Policy Series, No. 53, 2019: 2. Available: https://www.ncbi.nlm.nih.gov/books/NBK549261/ [PubMed] [Google Scholar]
- 12. Alotaibi Y, Alnowaiser N, Alamry A. Improving hospital flow ensiab project BMJ Open Qual 2021;10:e001505. 10.1136/bmjoq-2021-001505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. NHS improvement . SAFER patient flow bundle. 2021. Available: https://improvement.nhs.uk/resources/safer-patient-flow-bundleimplement/
- 14. Meo N, Paul E, Wilson C, et al. Introducing an electronic tracking tool into daily Multidisciplinary discharge rounds on a medicine service: a quality improvement project to reduce length of stay. BMJ Open Qual 2018;7:e000174. 10.1136/bmjoq-2017-000174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Resar RK, Griffin FA, Kabcenell A, et al. Hospital inpatient waste identification tool. IHI innovation series white paper. Cambridge, Massachusetts: Institute for Healthcare Improvement, 2011. Available: www.IHI.org [Google Scholar]
- 16. Marin-Garcia JA, Vidal-Carreras PI, Garcia-Sabater JJ. The role of value stream mapping in healthcare services: a Scoping review. Int J Environ Res Public Health 2021;18:951. 10.3390/ijerph18030951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bin Che Ani MN, Bin Shafei MSS. The effectiveness of the single minute exchange of die (SMED) technique for the productivity improvement. AMM 2013;465–466:1144–8. 10.4028/www.scientific.net/AMM.465-466.1144 Available: https://www.scientific.net/AMM.465-466 [DOI] [Google Scholar]
- 18. Optimizing patient flow: moving patients smoothly through acute care settings. IHI innovation series white paper. Boston: Institute for Healthcare Improvement; 2003. Available: www.IHI.org [Google Scholar]
- 19. Buswell G. The Healthcare system in Saudi Arabia. 2023. Available: https://www.expatica.com/sa/healthcare/healthcare-basics/healthcare-system-in-saudi-arabia-71162/
- 20. Alasiri AA, Mohammed V. Healthcare transformation in Saudi Arabia: an overview since the launch of vision 2030. Health Serv Insights 2022;15:11786329221121214. 10.1177/11786329221121214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. AlMubarak SH, Alfayez AS, Alanazi AT, et al. Autonomy, accountability, and competition: the optimization of the Saudi health care system. J Taibah Univ Sci 2021;16:144–51. 10.1016/j.jtumed.2020.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Marshall A, Vasilakis C, El-Darzi E. Length of stay-based patient flow models: recent developments and future directions. Health Care Manag Sci 2005;8:213–20. 10.1007/s10729-005-2012-z [DOI] [PubMed] [Google Scholar]
- 23. Marfil-Garza BA, Belaunzarán-Zamudio PF, Gulias-Herrero A, et al. Risk factors associated with prolonged hospital length-of-stay: 18-year retrospective study of hospitalizations in a tertiary healthcare center in Mexico. PLoS One 2018;13:e0207203. 10.1371/journal.pone.0207203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tipton K, Leas BF, Mull NK, et al. Interventions to Decrease Hospital Length of Stay. (Technical Brief, No. 40.) Introduction. Rockville (MD): Agency for Healthcare Research and Quality (US), 2021. Available: https://www.ncbi.nlm.nih.gov/books/NBK574438/ [PubMed] [Google Scholar]
- 25. Hoogervorst-Schilp J, Langelaan M, Spreeuwenberg P, et al. Excess length of stay and economic consequences of adverse events in Dutch hospital patients. BMC Health Serv Res 2015;15:531. 10.1186/s12913-015-1205-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Su LH, Chen IL, Tang YF, et al. Increased financial burdens and lengths of stay in patients with healthcare-associated infections due to multidrug-resistant bacteria in intensive care units: a propensity-matched case-control study. PLoS One 2020;15:e0233265. 10.1371/journal.pone.0233265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. OECD. Health at a Glance 2021: OECD Indicators. OECD Publishing, Paris: 2021. 10.1787/ae3016b9-en. [DOI] [Google Scholar]
- 28. Rubino L, Chassiakos YR, Freshman B. Collaboration across the disciplines in health care. Burlington: MA. Jones and Bartlett Publishers, 2010. [Google Scholar]
- 29. Perez R. Defining Healthcare complexity. In: Fraser K, Perez R, Latour C, eds. CMSA’s integrated case management: A manual for case managers by case managers. Springer Publishing Company, 2023: 3–8. 10.1891/9780826188342 [DOI] [Google Scholar]
- 30. Micallef A, Buttigieg SC, Tomaselli G, et al. Defining delayed discharges of Inpatients and their impact in acute hospital care: a scoping review. Int J Health Policy Manag 2022;11:103–11. 10.34172/ijhpm.2020.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kripalani S, Theobald CN, Anctil B, et al. Reducing hospital readmission rates: current strategies and future directions. Annu Rev Med 2014;65:471–85. 10.1146/annurev-med-022613-090415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McDermott CM, Venditti FJ. Implementing lean in knowledge work: implications from a study of the hospital discharge planning process. Oper Manag Res 2015;8:118–30. 10.1007/s12063-015-0103-7 [DOI] [Google Scholar]
- 33. Molla M, Warren DS, Stewart SL, et al. A lean six sigma quality improvement project improves timeliness of discharge from the hospital. Jt Comm J Qual Patient Saf 2018;44:401–12. 10.1016/j.jcjq.2018.02.006 [DOI] [PubMed] [Google Scholar]
- 34. Siddique SM, Tipton K, Leas B, et al. Interventions to reduce hospital length of stay in high-risk populations: a systematic review. JAMA Netw Open 2021;4:e2125846. 10.1001/jamanetworkopen.2021.25846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pellett C. Discharge planning: best practice in transitions of care. Br J Community Nurs 2016;21:542–8. 10.12968/bjcn.2016.21.11.542 [DOI] [PubMed] [Google Scholar]
- 36. Proudlove NC, Gordon K, Boaden R. Can good bed management solve the overcrowding in accident and emergency departments Emerg Med J 2003;20:149–55. 10.1136/emj.20.2.149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Manning L, Islam MS. A systematic review to identify the challenges to achieving effective patient flow in public hospitals. Health Planning & Management 2023;38:805–28. 10.1002/hpm.3626 Available: https://onlinelibrary.wiley.com/toc/10991751/38/3 [DOI] [PubMed] [Google Scholar]
- 38. Shuster L. Why internal recruitment can be a smart strategy for 2023 [online]. 2023. Available: https://www.forbes.com/sites/forbeshumanresourcescouncil/2023/02/22/why-internal-recruitment-can-be-a-smart-strategy-for-2023/?sh=27c5c14d12b6
- 39. Prey JE, Woollen J, Wilcox L, et al. Patient engagement in the inpatient setting: a systematic review. J Am Med Inform Assoc 2014;21:742–50. 10.1136/amiajnl-2013-002141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Marzban S, Najafi M, Agolli A, et al. Impact of patient engagement on healthcare quality: a scoping review. J Patient Exp 2022;9. 10.1177/23743735221125439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Oben P. Understanding the patient experience: a conceptual framework. J Patient Exp 2020;7:906–10. 10.1177/2374373520951672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lingsma HF, Bottle A, Middleton S, et al. Evaluation of hospital outcomes: the relation between length-of-stay, readmission, and mortality in a large International administrative database. BMC Health Serv Res 2018;18:116. 10.1186/s12913-018-2916-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hassan M, Tuckman HP, Patrick RH, et al. Hospital length of stay and probability of acquiring infection. Intl J of Pharm & Health Mrkt 2010;4:324–38. 10.1108/17506121011095182 [DOI] [Google Scholar]
- 44. Stewart S, Robertson C, Pan J, et al. Impact of healthcare-associated infection on length of stay. J Hosp Infect 2021;114:23–31. 10.1016/j.jhin.2021.02.026 [DOI] [PubMed] [Google Scholar]
- 45. Klaehn AK, Jaschke J, Freigang F, et al. Cost-effectiveness of case management: a systematic review. Am J Manag Care 2022;28:e271–9. 10.37765/ajmc.2022.89186 [DOI] [PubMed] [Google Scholar]
- 46. Elkholi A, Althobiti H, Al Nofeye J, et al. NO WAIT: new organized well-adapted immediate triage: a lean improvement project. BMJ Open Qual 2021;10:e01179. 10.1136/bmjoq-2020-001179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Alharbi S, Alasmari A, Hanafy E, et al. Reduction of hospital bed cost for inpatient overstay through optimization of patient flow. BMJ Open Qual 2023;12:e002142. 10.1136/bmjoq-2022-002142 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2023-002484supp001.pdf (90.2KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.