Abstract
Laparoscopy for intra-abdominal exploration and tissue sampling is useful in advanced ovarian cancers, in which it is presumed to be difficult to achieve complete tumour reduction in the initial surgery. This is a report of a case of suspected advanced ovarian cancer in a patient, who underwent laparoscopic screening and was later pathologically diagnosed with tuberculous peritonitis. A woman in her 50s visited her local doctor with constipation. Since imaging showed massive ascites she was referred for further evaluation. We initially suspected advanced ovarian cancer due to the presence of massive ascites and multiple peritoneal nodules. However, histopathological examination indicated that the nodules were tubercles, and the patient was subsequently diagnosed with tuberculous peritonitis. It is important to be aware that tuberculosis peritonitis can be misdiagnosed or mistaken for advanced ovarian cancer. Preoperative diagnosis of tuberculous peritonitis is often difficult. Tuberculous peritonitis should be considered if intraoperative findings show diffuse nodular disseminated lesions.
Keywords: Tuberculosis, Cancer - see Oncology
Background
Laparoscopy for intra-abdominal exploration and tissue sampling is useful in advanced ovarian cancers, in which it is presumed to be difficult to achieve complete tumour reduction in the initial surgery. In our hospital, in patients with massive ascites and intra-abdominal distention, complete resection cannot be expected during the initial surgery. Therefore, if the overall general health condition allows for the administration of general anaesthesia, an examination laparoscopy is performed as soon as possible, Here, we report a case of suspected advanced ovarian cancer in a patient, who underwent laparoscopic screening and was pathologically diagnosed with tuberculous peritonitis.
Case presentation
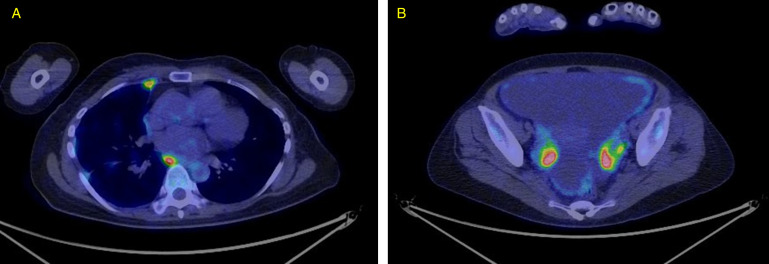
A woman in her 50s with two pregnancies and two deliveries (G2P2) visited her local doctor with constipation. Her height was 150 cm, weight was 53 kg and body mass index was 23.6 kg/m2. Vitals before treatment were blood pressure 131/79 mm Hg, heart rate 92 times/min, respiratory rate 22 times/min, Spo2 96% and body temperature 35.9°C. She had a history of acute right-sided empyema. She was diagnosed with bacterial empyema and was treated. No tuberculosis (TB) examination was performed. She did not have any risk factors for TB, such as diabetes, chronic renal failure, oral steroid use or smoking. She had no history of exposure to TB or travel. CT revealed massive ascites and positron emission tomography-CT showed abnormal uptake in the pleura, peritoneum, systemic lymph nodes and bilateral ovaries (figure 1A,B). In addition, the CA125 level was as high as 421 U/mL, and the patient was referred for a detailed examination. Transvaginal ultrasonography showed no obvious abnormalities in the uterus or bilateral adnexa; however, massive ascites was noted (figure 2).
Figure 1.
FDG, PET. PET-CT showed abnormal uptake in the pleura (A), and bilateral ovaries (B).
Figure 2.

Transvaginal ultrasonography. No obvious abnormalities in the uterus or bilateral adnexa; however, massive ascites was noted.
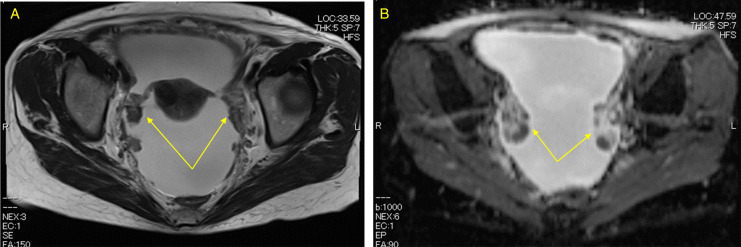
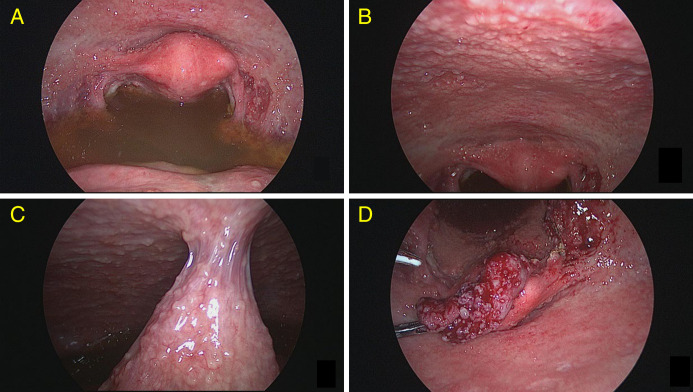
Blood tests showed a slight increase in CRP to 2.17 mg/dL and a slight decrease in the whited cell count to 2810x109/L. MRI showed thickening of the pelvic peritoneum and decreased diffusion in both ovaries (figure 3). Carcinomatous peritonitis secondary to ovarian cancer was suspected. On the fourth day after the initial visit, an examination laparoscopy was performed. Intraoperative findings showed massive ascites (figure 4A), small nodules diffusely disseminated over the uterus, bilateral adnexa and peritoneum (figure 4B), and fibrous adhesions between the peritoneum and small intestine (figure 4C). Carcinomatous peritonitis due to ovarian cancer was suspected, the right fallopian tube was excised as a histopathological sample for diagnostic purposes (figure 4D), and the surgery was completed. The operation time was 42 min, pneumoperitoneum time was 31 min and intraoperative bleeding was minimal.
Figure 3.
(A) MRI T2-weighted imaging. Thickening of the pelvic peritoneum (→). (B) MRI diffusion-weighted imaging. Decreased diffusivity of the bilateral ovaries (→).
Figure 4.
Laparoscopic findings. (A) Massive ascites. (B) Small nodules diffusely disseminated over the uterus, bilateral adnexa and peritoneum. (C) Fibrous adhesions between the peritoneum and the small intestine. (D) Right fallopian tube.
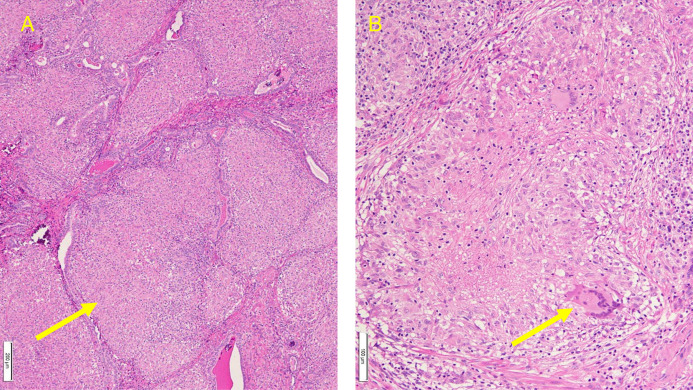
On the sixth postoperative day, histopathological examination with H&E staining revealed epithelioid granulomas (figure 5A) and Langhans giant cells (figure 5B) in the right fallopian tubal tissue, and the patient was diagnosed with TB. Adenosine deaminase (ADA) in the ascites was not tested because the histopathological diagnosis indicated a high possibility of TB. Sputum and ascitic fluid cultures did not show TB bacilli; however, a blood test performed after the pathological results were obtained was positive for T-SPOT.TB(T-SPOT), suggesting that the patient had a TB infection. The T-SPOT test is a test that diagnoses TB infection by stimulating peripheral blood with Mycobacterium TB-specific antigen and measuring the level of interferon-γ (IFN-γ) produced. The T-SPOT test will be positive if you are currently infected or have had a history of infection, so it is not possible to tell whether you are currently infected. Culture and PCR tests on sputum and ascites were negative, and TB gene and PCR tests on the removed fallopian tubes were negative. Although the T-SPOT was positive, it is unclear whether the patient is currently infected with TB. Therefore, we decided to perform diagnostic treatment for TB based on the pathological histology of the fallopian tubes.
Figure 5.
(A) H&E staining ×40. Epithelioid granuloma (→). (B) H&E staining ×200 (→). Langhans giant cells (→).
After obtaining the pathological results, the patient was treated for TB at the department of respiratory medicine. Transvaginal ultrasonography performed 14 days after the start of treatment showed improvement in the ascites. As the TB drugs were effective, the patient was diagnosed with a very high possibility of tuberculous peritonitis, and oral anti-TB drugs (isoniazid, rifampicin, pyrazinamide and ethambutol) were administered for 9 months, and her symptoms improved.
Considering the possibility of aerosol infection in the operating room, the healthcare workers involved in the operation decided to follow up with blood tests. T-SPOT was confirmed to be negative twice, immediately after and 3 months later, and a follow-up was completed for all medical staff. Since the sputum culture for TB was negative, we did not follow up on TB in her family because no one in her family had symptoms such as cough or sputum.
Differential diagnosis
Tuberculous peritonitis is difficult to distinguish from advanced ovarian cancer preoperatively. We suspected advanced ovarian cancer in a patient, who underwent laparoscopic screening and was later pathologically diagnosed with tuberculous peritonitis. Culture and PCR tests on sputum and ascites were negative, and TB gene and PCR tests on the removed fallopian tubes were negative. Although the T-SPOT was positive, it is unclear whether the patient is currently infected with TB. Therefore, we decided to perform diagnostic treatment for TB based on the pathological histology of the fallopian tubes. As the TB drugs were effective, the patient was diagnosed with a very high possibility of tuberculous peritonitis.
Treatment
Isoniazid 300 mg/day, rifampicin 450 mg/day, pyrazinamide 1.5 g/day and ethambutol 750 mg/day were administered for 9 months.
Outcome and follow-up
After obtaining the pathological results, the patient was treated for TB at the department of respiratory medicine. Transvaginal ultrasonography performed 14 days after the start of treatment showed improvement in the ascites. Oral anti-TB drugs (isoniazid, rifampicin, pyrazinamide and ethambutol) continued for 9 months. 11 months after first treatment, she made a full recovery and is living with no deterioration in her quality of life.
Discussion
Among extrapulmonary TB, tuberculous peritonitis is extremely rare, accounting for 0.1%–0.7% of all TB cases.1 The routes of infection routes for tuberculous peritonitis are thought to include latent infected pulmonary foci that become active following a decrease in immunity and disseminate haematogenously to the peritoneum and continuous spread from adjacent intraperitoneal organs, such as the oviduct and small intestine.1 In this case, culture and PCR tests on sputum and ascites were negative, and TB gene and PCR tests on the removed fallopian tubes were negative. Although pulmonary empyema was not investigated for TB, it was not possible to identify the source of TB infection, whether pulmonary TB was haematogenously disseminated into the peritoneum, or intestinal TB was disseminated into the peritoneum. Therefore, the route of infection was presumed to be from latent infective foci. Tuberculous peritonitis is often misdiagnosed as advanced ovarian cancer and is diagnosed by the gynaecologist who performs the surgery.2 In advanced ovarian cancer, targeted chemotherapy for genetic mutations has been attempted in recent years. For difficult-to-resect advanced ovarian cancers, it is recommended to examine the peritoneal cavity via laparoscopy, perform an intra-abdominal biopsy, and submit for histopathological examination and genetic risk evaluation and germline and somatic testing.3 Therefore, there are more opportunities for laparoscopy in the field of obstetrics and gynaecology for suspected advanced ovarian cancer. Tuberculous peritonitis, which is difficult to distinguish from advanced ovarian cancer preoperatively, also exists. Tuberculous peritonitis is characterised by ascites, peritoneal thickening and increased fatty tissue density in the greater omentum on CT examination. Preoperative diagnostic imaging findings are similar to those of carcinoma-induced peritonitis and peritoneal cancer. Therefore, most cases of tuberculous peritonitis are diagnosed by tissue examination during laparoscopy or laparotomy, and the histological diagnostic rate is as high as 95%, especially when sufficient biopsy tissue is collected via laparoscopy.4 The positive rate of mycobacterial culture in ascites is 20%–50%,5 and the positive rate of PCR testing is reported to be approximately 60%–80%,6 making it difficult to bacteriologically prove TB with ascitic fluid. Tuberculous peritonitis has a mortality rate of 60% when the time from onset to diagnosis is >30 days.7 In this case, laparoscopy was performed 4 days after the first visit, and anti-TB drugs were initiated on the 13th day, leading to a favourable prognosis.
According to a systematic review by Sanai and Bzeizi, ascites is the most common clinical finding in tuberculous peritonitis (73%), followed by abdominal pain (64.5%), weight loss (61%) and fever (59%).1 The sensitivity of ADA in ascites was as high as 94%, which was similar to that of laparoscopic findings and histopathology.1 Serum CA125 is a tumour marker of ovarian cancer; however, it is also increased in tuberculous peritonitis.2 Because the clinical symptoms and CA125 levels are elevated, it is often suspected as ovarian cancer. CA125 is also expressed in the peritoneum and pleura,8 we believe that it was elevated due to inflammation caused by tuberculous peritonitis. In cases with massive ascites, cytology and ADA levels of the ascitic fluid should be examined.
In general, in extrapulmonary TB, infectiousness can be considered negligible,9 but healthcare workers who come into unprotected contact with patients with TB are at risk of infection.10 As a guideline for TB infection control, surgeons and caregivers should wear N95 masks, strict air precautions should be taken and postoperative recovery should be performed in an air-conditioned room where appropriate precautions can be taken.10 In this case, carcinomatous peritonitis of ovarian cancer was suspected, and laparoscopy was not performed with tuberculous peritonitis in mind. Therefore, the medical personnel involved in the operating room were exposed to the risk of aerosol infection due to pneumoperitoneum. Therefore, even in cases in which ovarian cancer is suspected, tuberculous peritonitis should be considered for management. Liu Q et al reported that tuberculous peritoneal inflammation should be considered in patients with the following seven criteria: (1) young and socially poor, (2) history of menstrual abnormality and infertility, (3) clinical symptoms such as cough, weight loss, slight fever, night sweats, (4) ADA-positive ascites with significant lymphocytes and no malignant cells, (5) fever using long-term immunosuppressants, (6) history of treatment for TB and (7) abnormal chest CT or PET-CT with ascites, pelvic mass and elevated CA125.2 It is known that the uptake of Fluorodeoxyglucose(FDG) increases when the inflammatory response due to TB is high11 and there is a correlation between FDG accumulation and TB lesion size.12 In this case, it is expected that strong inflammation due to TB was occurring in the ovaries and pleura. No TB bacteria were detected in ascitic fluid or sputum culture, but laparoscopic findings revealed a large nodular lesion attached to the adnexa, so the right fallopian tube was removed. We believe that there is a relationship between nodule size and FDG uptake.
Although surgical tissue biopsy is important for the definitive diagnosis of tuberculous peritonitis, laparoscopic surgery with infection control measures considering TB peritonitis is important.
Patient’s perspective.
I have been feeling bloated for several months and it was very painful. The doctor explained that there was a high possibility of cancerous peritonitis due to ovarian cancer, so we should conduct a examination laparoscopy as soon as possible. I was shocked when I was told that I might have ovarian cancer, but I was very relieved when I was told a week later that it was tuberculous peritonitis and could be treated. Currently, I am able to live my life without any symptoms, and I am glad that I was able to receive treatment right away. The doctor told me that this was a very rare case and that he would like me to report it for the future development of clinical medicine, and I readily agreed.
Learning points.
It is difficult to differentiate between tuberculous peritonitis and cancerous peritonitis.
Intraperitoneal observation using a laparoscopy and tissue biopsy is useful for diagnosing tuberculous peritonitis.
Tuberculous peritonitis should be considered if intraoperative findings show diffuse nodular disseminated lesions.
Acknowledgments
We would like to thank Editage (www.editage.jp) for English language editing.
Footnotes
Contributors: Authorship submitting author: MN corresponding author: HI Joint first authorship: AT collaborators (group authorship): MM. This paper was planned by HI and written by MN. The surgery was performed by MN and HI. The data were organised by MM. The paper was supervised and peer-reviewed by AT.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1. Sanai FM, Bzeizi KI. Systematic review: tuberculous peritonitis- presenting features, diagnostic strategies and treatment. Aliment Pharmacol Ther 2005;22:685–700. 10.1111/j.1365-2036.2005.02645.x [DOI] [PubMed] [Google Scholar]
- 2. Liu Q, Zhang Q, Guan Q, et al. Abdominopelvic tuberculosis mimicking advanced ovarian cancer and pelvic inflammatory disease: a series of 28 female cases. Arch Gynecol Obstet 2014;289:623–9. 10.1007/s00404-013-3034-2 [DOI] [PubMed] [Google Scholar]
- 3. Ovarian cancer, (version 5.2022). NCCN clinical practice guidelines in oncology;
- 4. Bhargava DK, Shriniwas P, Chopra P, et al. Peritoneal tuberculosis: laparoscopic patterns and its diagnostic accuracy. Am J Gastroenterol 1992;87:109–12. [PubMed] [Google Scholar]
- 5. Marshall JB. Tuberculosis of the gastrointestinal tract and peritoneum. Am J Gastroenterol 1993;88:989–99. [PubMed] [Google Scholar]
- 6. Sherman S, Rohwedder JJ, Ravikrishnan KP, et al. Tuberculous enteritis and peritonitis. report of 36 general hospital cases. Arch Intern Med 1980;140:506–8. [PubMed] [Google Scholar]
- 7. Chow KM, Chow VCY, Hung LCT, et al. Tuberculosis peritonitis-associated mortality is high among patients waiting for the results of mycobacterial culture of ascitic fluid samples. Clin Infect Dis 2002;35:409–13. 10.1086/341898 [DOI] [PubMed] [Google Scholar]
- 8. Charkhchi P, Cybulski C, Gronwald J, et al. CA125 and ovarian cancer: a comprehensive review. Cancers (Basel) 2020;12:3730. 10.3390/cancers12123730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dierkesmann R. Zur Frage der Infektiosität der Tuberkulose [the Infectiousness of tuberculosis]. Offentl Gesundheitswes 1990;52:501–5. [PubMed] [Google Scholar]
- 10. Jensen PA, Lambert LA, Iademarco MF, et al. Guidelines for preventing the transmission of mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep 2005;54:1–141. [PubMed] [Google Scholar]
- 11. Hara T, Kosaka N, Suzuki T, et al. Uptake rates of 18F-Fluorodeoxyglucose and 11C-choline in lung cancer and pulmonary tuberculosis: a positron emission tomography study. Chest 2003;124:893–901. 10.1378/chest.124.3.893 [DOI] [PubMed] [Google Scholar]
- 12. Sánchez-Montalvá A, Barios M, Salvador F, et al. Usefulness of FDG PET/CT in the management of tuberculosis. PLoS One 2019;14:e0221516. 10.1371/journal.pone.0221516 [DOI] [PMC free article] [PubMed] [Google Scholar]