Abstract
Catheter-related suppurative thrombophlebitis (CRST) is a complication of catheter-related bloodstream infection (CRBSI). The microbiology of CRST is similar with the microbiology of CRBSI, but Clostridium perfringens that causes gas gangrene is a rare pathogen of CRBSI and CRST. We present a case of catheter-related gas-forming suppurative thrombophlebitis due to Clostridium perfringens infection. Gas-forming thrombus around the catheter can be useful findings for the early diagnosis of catheter-related clostridial thrombophlebitis.
Keywords: Catheter-related bloodstream infection, Central line-associated bloodstream infection, Central venous catheter-related thrombosis, Clostridium perfringens, Gas-forming suppurative thrombophlebitis
Case presentation
A 78-year-old woman with diabetes mellitus was admitted to a hospital owing to a 3-month history of anorexia. Seven days before, a central venous catheter was inserted in the right femoral vein for total parenteral nutrition. She was referred to our hospital owing to a 2-day history of fever. Ultrasonography detected thrombus in the inferior vena cava. Further evaluation was performed by contrast-enhanced computed tomography (CECT). CECT revealed the presence of columnar gas in a thrombus around the catheter tip, extending from the right common iliac vein to the inferior vena cava (Figs. 1 and 2). Blood and removed catheter tip cultures were all positive for Clostridium perfringens. She received treatment with intravenous ampicillin-sulbactam for two weeks, followed by oral amoxicillin for two weeks. Anticoagulation therapy was continued for three months, and thrombus was dissolved. Recurrence was not observed following treatment.
Fig. 1.
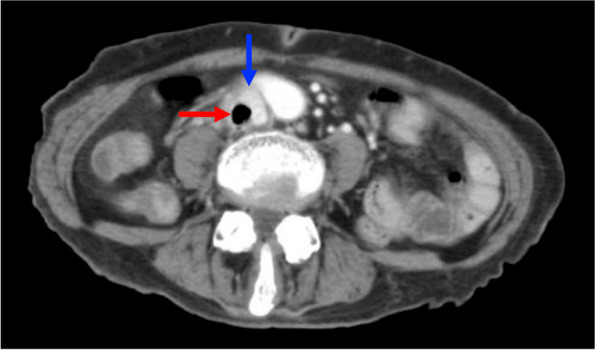
Axial contrast-enhanced computed tomography (CECT) showing round gas in a thrombus (red arrow) in the inferior vena cava (blue arrow)
Fig. 2.
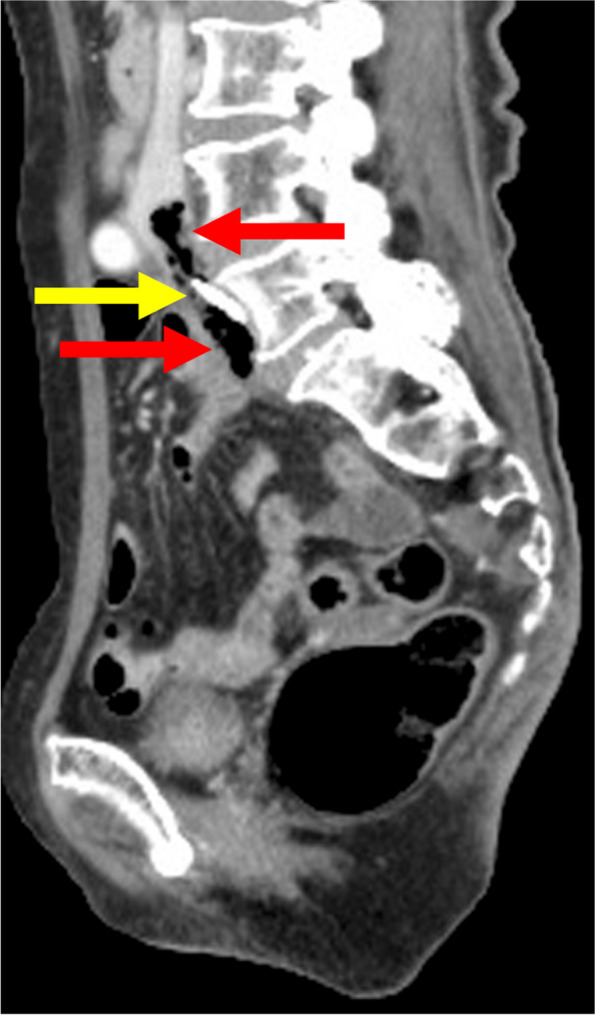
Sagittal CECT showing columnar gas (8.5 mm in diameter and 60 mm in length) in a thrombus (red arrows) and the central catheter tip in the right common iliac vein (yellow arrow)
Diagnosis
Catheter-related gas-forming suppurative thrombophlebitis due to Clostridium perfringens infection
The risk of catheter-related bloodstream infection (CRBSI) and catheter-related thrombosis was higher for femoral compared with subclavian and internal jugular [1]. Catheter-related suppurative thrombophlebitis (CRST) is a relatively uncommon complication of CRBSI [2], but should be ruled out [3]. The common pathogen is Staphylococcus aureus [2]. In the current case, Clostridium perfringens probably invaded the percutaneous tract or was carried hematogenously to the catheter because of bacterial translocation. Therefore, thrombus formation around the catheter was infected with Clostridium perfringens, resulting in quite rare form of central line-associated bloodstream infection, gas-forming suppurative thrombophlebitis. Our case highlights that gas-forming thrombus around the catheter can be useful findings that early diagnose catheter-related clostridial thrombophlebitis.
Acknowledgements
The authors thank Dr. Tetsuhiro Takei for his constructive comments on the manuscript.
Abbreviations
- CRST
Catheter-related suppurative thrombophlebitis
- CRBSI
Catheter-related bloodstream infection
- CECT
Contrast-enhanced computed tomography
Authors’ contributions
All authors contributed to the Image report design. The first draft of the manuscript as written by Yasuyoshi Miyamura. Takeshi Shimazaki, and Kunihiko Okada contributed to prepare Fig. 1–2 and commented on the manuscript. All authors read and approved the final manuscript.
Funding
This research received no specific fund from anywhere.
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Ethics approval is not required for de-identified single case report based on institutional policies.
Consent for publication
Consent for publication was obtained from patient’s family for publication of this study and accompanying images in accordance with the journal’s patient consent policy.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Arvaniti K, Lathyris D, Blot S, Apostolidou-Kiouti F, Koulenti D, Haidich AB. Cumulative evidence of randomized controlled and observational studies on catheter-related infection risk of Central Venous Catheter Insection Site in ICU Patients: a pairwise and netwok meta-analysis. Crit Care Med. 2017;45(4):e437–e448. doi: 10.1097/CCM.0000000000002092. [DOI] [PubMed] [Google Scholar]
- 2.Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O'Grady NP, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;49(1):1–45. doi: 10.1086/599376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaves F, Garnacho-Montero J, Del Pozo JL, Bouza E, Capdevila JA, de Cueto M, et al. Diagnosis and treatment of catheter-related bloodstream infection: Clinical guidelines of the Spanish Society of Infectious Diseases and Clinical Microbiology and (SEIMC) and the Spanish Society of Spanish Society of Intensive and Critical Care Medicine and Coronary Units (SEMICYUC) Med Intensiva (Engl Ed). 2018;42(1):5–36. doi: 10.1016/j.medin.2017.09.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.


