Abstract
Background
Gastric cancer is primarily treated by surgery; however, little is known about the changes in the intraperitoneal immune environment and the prognostic impact of surgery. Surgical stress and cancer-associated inflammation cause immune cells to mobilize into the abdominal cavity via numerous cytokines. One such cytokine, CX3CR1, has various immune-related functions that remain to be fully explained. We characterized the intraperitoneal immune environment by investigating CX3CR1+ cells in intraperitoneal lavage fluid during gastric cancer surgery.
Methods
Lavage fluid samples were obtained from a total of 41 patients who underwent gastrectomy. The relative expression of various genes was analyzed using quantitative real-time PCR. The association of each gene expression with clinicopathological features and surgical outcomes was examined. The fraction of CX3CR1+ cells was analyzed by flow cytometry. Cytokine profiles in lavage fluid samples were investigated using a cytometric beads array.
Results
CX3CR1high patients exhibited higher levels of perioperative inflammation in blood tests and more recurrences than CX3CR1low patients. CX3CR1high patients tended to exhibit higher pathological T and N stage than CX3CR1low patients. CX3CR1 was primarily expressed on myeloid-derived suppressor cells and tumor-associated macrophages. In particular, polymorphonuclear myeloid-derived suppressor cells were associated with perioperative inflammation, pathological N, and recurrences. These immunosuppressive cells were associated with a trend toward unfavorable prognosis. Moreover, CX3CR1 expression was correlated with programmed death–1 expression.
Conclusions
Our results suggest that CX3CR1+ cells are associated with an acute inflammatory response, tumor-promotion, and recurrence. CX3CR1 expression could be taken advantage of as a beneficial therapeutic target for improving immunosuppressive state in the future. In addition, analysis of intra-abdominal CX3CR1+ cells could be useful for characterizing the immune environment after gastric cancer surgery.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12957-024-03353-1.
Keywords: CX3CR1, Fractalkine receptor, Tumor-associated macrophage, Myeloid-derived suppressor cell, Programmed death 1, Intraperitoneal lavage fluid, Gastric cancer
Introduction
Gastric cancer is treated using a variety of strategies, including chemotherapy and immune therapy; however, surgery is a primary mode of treatment. Surgical treatment for gastric cancer is both difficult and highly invasive for patients.
The prognosis for patients who develop complications after gastric cancer surgery is often poor. One reason for poor prognosis is that residual cancer cells may proliferate due to a decline in host immunocompetence. We previously investigated the intra-peritoneal immune environment using intraperitoneal lavage fluid (ILF) from patients with gastric cancer and demonstrated that the number of inflammatory cells within the ILF differed according to the type of operative approach [1]. This suggested an increase in intraperitoneal granulocytes occurs during the invasive surgical procedure to treat gastric cancer. However, little is known about the changes in the intraperitoneal immune environment that occur due to surgery and their prognostic impact.
Inflammatory cells such as macrophages migrate, infiltrate, and accumulate under the influence of various cytokines and chemokines. One such chemokine, CX3CR1, which is a fractalkine receptor for CX3CL1 [2], reportedly exhibits multiple functions [3]. CX3CR1 is expressed by immune cells such as natural killer cells, lymphocytes, macrophages, and myeloid-derived suppressor cells (MDSCs) [4]. When CX3CR1 binds to CX3CL1, multiple pathways are activated that cause tumor and immune cells to migrate, invade, and metastasize, ultimately leading to angiogenesis [3, 5, 6]. In various types of cancer, including gastric cancer, reports suggest that CX3CR1 is a poor prognostic factor that promotes metastasis [3, 7]. In contrast, some studies have reported an association between CX3CR1+ lymphocytes and the effectiveness of immune checkpoint inhibitors [8–10]. We therefore investigated the characteristics and prognostic impact of CX3CR1+ cells in ILF from patients with gastric cancer.
Methods
Patients and Samples
This study included 41 patients with gastric cancer who underwent surgical operation that enabled us to collect ILF at Osaka City University (currently Osaka Metropolitan University, Osaka, Japan) between January 2020 and June 2021. Depending on the tumor location, the surgeon performed proximal, distal, or total gastrectomy with lymphadenectomy. Attending surgeons selected patients to undergo either laparoscopic (and robot-assisted) or open surgery. Regarding clinicopathological findings, the histological types were determined based on differentiated type (well differentiated/moderately differentiated)/undifferentiated (poorly differentiated). All pathological stages were recorded according to the TNM Classification of Gastric Cancer, 8th edition, published by the Union for International Cancer Control [11].
At the time of abdominal opening (designated ‘Opening’) or just before closing the abdominal wall (designated ‘Closure’), the abdominal cavity was irrigated using 500 mL of normal saline, and approximately 50 mL of lavage fluid was collected from the Douglas’ pouch. The obtained fluid was centrifuged at 300 × g for 10 min to pellet the cells. The cells were then resuspended in 1 mL of CELL BANKER (Nihon Zenyaku Kogyo Co. /Ltd.; cat. no. CB011) and stored at −80°C until further analysis.
This study was conducted according to the principles of the Declaration of Helsinki. All experimental procedures and follow-up were approved by the Osaka City University Ethics Committee (approval nos. 3138 and 4092). All patients provided written informed consent before enrollment.
Quantitative real-time PCR
Quantitative real-time PCR was conducted to analyze the relative expression of various genes in ILF. Total RNA was isolated from cryopreserved cells using an RNeasy Mini kit (QIAGEN, Hilden, Germany), and the RNA was used as a template for synthesis of complimentary DNA by reverse transcription using a High-Capacity cDNA Reverse Transcription kit (Invitrogen, Carlsbad, CA, USA) in accordance with the manufacturer’s instructions. We performed quantitative real-time PCR using the Taq-Man Gene Expression Assay (Thermo Fisher Scientific, Waltham, MA, USA). Other than CX3CR1 (Assay ID: Hs01922583_s1), MDSCs and tumor-associated macrophages (TAMs) were examined by assaying the relative expression of OLR1 (LOX-1; lectin-like oxidized low-density lipoprotein receptor 1, Assay ID: Hs01552593_m1) and CD163 (Assay ID: Hs00174705_m1). The relative expression of PDCD1 (PD-1; programmed death 1, Assay ID: Hs01550088_m1) was also examined for determining the exhausted status of immune cells and immune checkpoint molecules. Thermocycling was performed using a 7500 Fast Real-Time PCR System (Applied Biosystems, Foster City, CA, USA) as follows: initial incubation at 95°C for 10 min, followed by 40 cycles of 95°C for 15 s and 60°C for 1 min. The δδCt method was used to quantitate and analyze the expression of CX3CR1, OLR1, CD163, and PDCD1 relative to GAPDH as a control. The lowest expressed sample of each gene was designated the baseline sample to calculate the fold-change value. Receiver operating characteristic (ROC) curves were generated to determine cut-off values of gene expression, and patients were divided into two groups according to these values. ROC curves were based on 24-month relapse-free survival (RFS) for cut-off values of CX3CR1, OLR1, and CD163 expression and 24-month overall survival (OS) for cut-off values of PDCD1 expression (Supplementary Fig. 1).
Flow cytometry
Flow cytometry was performed to determine the phenotypes of CX3CR1+ cells in ILF. Additional ILF samples (n=8) were collected by the same method for flow cytometry analyses. Red blood cells were lysed using RBC lysis buffer (eBioscience, San Diego, CA, USA), and the samples were washed with phosphate-buffered saline. Cells were subsequently saturated using BD Fetal Bovine Serum Stain Buffer (BD Biosciences) and incubated at 4°C for 30 min with the following antibodies to identify surface markers: BV421-labeled anti-CX3CR1 antibody (clone: 2A9-1: cat. no. 565800; BD biosciences). FITC-labeled anti-CD3 antibody (clone: UCHT1: cat. no. 555332; BD Biosciences) to detect T cells, and Alexa Fluor 488- labeled anti-FoxP3 antibody (clone: 25gD/C7: cat. no. 3270739; BD Biosciences) for regulatory T cells (Tregs). TAMs and monocytic MDSCs (M-MDSCs) were identified using PE-labeled anti-CD163 antibody (clone: GHI/61: cat. no. 556018; BD Biosciences) and BUV395-labeled anti-CD14 antibody (clone: MϕP9: cat. no. 563561; BD Biosciences). APC-labeled anti-LOX-1 antibody (clone: 15C4; cat. no. 358606; BioLegend) was primarily used to detect polymorphonuclear MDSCs (PMN-MDSCs). Dead cells were identified by staining with Fixable Viability Stain 780 (cat. no. 565388: BD Biosciences). Cells were permeabilized and fixed on ice for 20 min using Fixation/ Permeabilization Solution (BD Biosciences), and then they were washed with Perm/ Wash buffer (BD Biosciences) at 4°C for 30 min. A total of 3×104 events were collected using a BD LSRFortessaTM X-20 flow cytometer (BD Biosciences) with FACSDiva software (BD Biosciences). The resulting data were analyzed using FlowJo software, version 10 (Tree Star, Inc., Ashland, OR).
Cytometric bead array
To quantify multiple cytokines in ILF, we used the Cytometric Bead Array (cat. no. 558264, BD Biosciences), a flow cytometry application that enables the simultaneous measurement of the concentrations of multiple proteins in a small sample volume. We performed the procedure as per the manufacturer’s instructions. GM-CSF (cat. no. 558335), IFN-γ (cat. no. 558269), IL-4 (cat. no. 558272), IL-6 (cat. no. 558276), IL-10 (cat. no. 558274), IL-12p70 (cat. no. 558283), MCP-1 (cat. no. 558287), MIP-1α cat. no. 558325), TNF (cat. no. 558273), and VFGF (cat. no. 558336) were analyzed, as these proteins are commonly secreted by MDSCs and macrophages. All of the cytokine flexes were obtained from BD Biosciences. We analyzed 25 samples that contained confirmable and sufficient proteins using Closure samples. A total of 3×103 events were collected using a BD LSRFortessaTM X-20 flow cytometer (BD Biosciences) with FACSDiva software (BD Biosciences). Protein concentrations were determined using BD CBA Analysis Software, version 1.0.2 (BD Biosciences). Protein levels were compared between CX3CR1high and CX3CR1low samples using the cut-off value for CX3CR1.
Laboratory data
Laboratory data for before and after surgery were analyzed to identify any association with CX3CR1 expression. With regard to post-operative blood counts, complications other than surgical stress or cancer-associated inflammation, such as infection, can elevate inflammatory parameters. We then recorded the data on post-operative day (POD) 3, because systemic inflammation associated with surgical stress usually appears from POD 1 to 7, as we previously reported [1]. The neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were determined at the time of admission for surgery and on POD 3.
Statistical analysis
All statistical analyses were conducted using EZR [12], which is R with a modified version of R commander designed to add statistical functions frequently used in biostatistics. Fisher’s exact probability test was used to compare categorical variables. Continuous variables were compared using the Mann-Whitney U test. OS and RFS curves were compared using the Kaplan-Meier method, and the significance of differences in survival was assessed using the log-rank test. The date of surgery was set as the starting point for the measurement of OS and RFS. OS and RFS were defined based on the time of death and the time of death or recurrence, respectively. The correlogram and heatmap were generated using the web-based FaDA tool [13]. The correlogram was generated based on Spearman’s rank correlation coefficient. Hierarchical clustering in the heatmap was calculated using the average linkage method. P-values <0.05 were considered to indicate statistically significant differences.
Results
Association between CX3CR1, LOX-1, CD163, and PD-1 expression and clinical data before and after surgery
We analyzed the clinicopathological features of 41 patients with gastric cancer (Table 1). The mean age of the patients was 72 years (range, 43-89 years). The group included 31 men (75.6%) and 10 women (24.4%). The mean observation time was 18.2 months (range, 3-36 months).
Table 1.
Clinicopathological characteristics (n=41)
| Variables | N or median (range) | Variables | N or median (range) | |
|---|---|---|---|---|
| Age [years old] | 72 (43-89) | Hisological type | ||
| Sex | differentiated/ undifferentiated adenoca. | 22/ 19 | ||
| Male/ Female | 31/10 | Tumor Locationb | ||
| Body Mass Index [kg/m2] | 21.97 (16.59-33.58) | E/ U/ M/ L/ Other | 3/ 8/ 11/ 18/ 1 | |
| Other cancer history | 14 (34.1%) | pT categorya | ||
| cT-categorya | 1-2/ 3-4 | 16/ 25 | ||
| 1-2/ 3-4 | 13/ 28 | pN-categorya | ||
| cN-categorya | 0/ 1-3 | 19/ 22 | ||
| 0/ 1-3 | 20/ 21 | pStagea | ||
| cStagea | I-II/ III-IV | 26/ 15 | ||
| I-II/ III-IV | 21/ 20 | Ly | present/ absent | 18/ 23 |
| Comorbidities (present, %) | 35 (85.4%) | Vsss | present/ absent | 17/ 24 |
| Diabetes Mellitus | 14 (34.1%) | Surgical operation | ||
| Cardiac disease | 3 (7.31%) | Open/ Laparoscopy | 31/ 10 | |
| Renal disorder | 1 (2.44%) | TG/ DG+PGb | 14/ 27 | |
| Pulmonary disorder | 6 (14.6%) | Lymph nodes dissection (D1/ 1+/ 2) | 5/ 11/ 25 | |
| Hepatic disorder | 6 (14.6%) | Bleeding [mL] | 210 (5-1700) | |
| Operation time [min.] | 259 (106-607) | |||
| Anesthesia time [min.] | 294 (148-640) | |||
| Duration of hospitalization [days] | 13 (8-64) | |||
aTNM Classification of Gastric cancer, 8th ed
b Abbreviation: TG Total gastrectomy, DG Distal gastrectomy, PG Proximal gastrectomy
E Esophagogastoric, U Upper third gastric, M Middle third gastric, L Lower third gastric
We then examined the relative expression of CX3CR1 using Opening and Closure samples by quantitative RT-PCR. Based on the determined cut-off value, patients were divided into two groups (CX3CR1high or CX3CR1low). We also analyzed the association between CX3CR1 expression and various clinicopathological findings and operative outcomes (Table 2). In Opening samples, we did not find any association between these findings and CX3CR1 levels. In contrast, Closure samples exhibited significant differences between CX3CR1high and CX3CR1low patients. Although clinical Stage and patients’ comorbidities did not differ statistically in CX3CR1 levels, analysis of perioperative laboratory data indicated that CX3CR1high patients showed higher NLR, PLR, and C-reactive protein (CRP) levels than CX3CR1low patients. Moreover, there was a trend toward higher pathological T and N stage in the CX3CR1high group than the CX3CR1low group, though the difference was not statistically significant. In terms of operative outcomes, CX3CR1 expression was not affected by operative procedure or postoperative complications. Following clinical and pathological staging, CX3CR1high patients underwent more extensive lymphadenectomy and received more adjuvant chemotherapy than CX3CR1low patients without statistical differences. Also, the duration of hospitalization and recurrences after surgery differed significantly between the CX3CR1high and CX3CR1low groups.
Table 2.
Association of CX3CR1 expression in intraperitoneal lavage fluid with clinicopathological data and operative outcomes
| CX3CR1 | |||||||
|---|---|---|---|---|---|---|---|
| Opening | Closure | ||||||
| low (n = 31 ) | high (n = 10) | P† | low (n = 17) | high (n = 24) | P† | ||
| Sex | Male/ Female | 24/ 7 | 7/ 3 | 0.683 | 11/ 6 | 20/ 4 | 0.270 |
| Age(years-old) | 72.0 (69.5-76.0) | 69.5 (65.3-77.3) | 0.438 | 69.6 (65.0-73.0) | 73.3 (69.0-78.3) | 0.295 | |
| Tumor size (mm) | 45.0 (30.0-80.5) | 42.5 (23.0-54.5) | 0.523 | 38.0 (30.0-50.0) | 50.0 (33.8-86.3) | 0.076 | |
| Comorbidities | absent/ present | 4/ 27 | 2/ 8 | 0.622 | 3/ 14 | 3/ 21 | 0.679 |
| Other cancer history | absent/ present | 18/ 13 | 9/ 1 | 0.123 | 12/ 5 | 15/ 9 | 0.742 |
| Preoperative NLR | 2.66 (1.92-3.39) | 1.98 (1.70-3.05) | 0.235 | 1.79 (1.64-3.29) | 2.75 (2.19-3.49) | 0.037* | |
| Postoperative NLR | 6.65 (4.47-9.01) | 6.65 (5.44-9.32) | 0.574 | 5.56 (3.81-6.65) | 7.38 (5.72-11.7) | 0.005* | |
| Preoperative PLR | 113 (70.1-137) | 78.1 (56.4-104) | 0.118 | 56.0 (51.2-101) | 124 (90.2-165) | <0.001* | |
| Postoperative PLR | 177 (128-236) | 183 (97.1-261) | 0.777 | 99.3 (79.0-174) | 191 (175-491) | <0.001* | |
| CRP POD3 | 12.1 (4.34-19.6) | 12.2 (9.92-21.3) | 0.649 | 6.29 (3.24-14.3) | 14.2 (10.1-23.8) | 0.010* | |
| cT stagea | T1-2/ 3-4 | 9/ 22 | 4/ 6 | 0.698 | 7/ 10 | 6/ 18 | 0.322 |
| cN stagea | N0/ 1-3 | 15/ 16 | 5/ 5 | 1 | 9/ 8 | 11/ 13 | 1 |
| cStagea | Stage I-II/ III-IV | 16/ 15 | 5/ 5 | 1 | 8/ 9 | 13/ 11 | 0.756 |
| Histological type | differentiated/ undifferentiated | 18/ 13 | 4/ 6 | 0.469 | 10/ 7 | 12/ 12 | 0.752 |
| pT stagea | T1-2/ 3-4 | 10/ 21 | 6/ 4 | 0.15 | 10/ 7 | 6/ 18 | 0.051 |
| pN number | 2.00 (0.00-3.00) | 0.00 (0.00-1.75) | 0.361 | 0.00 (0.00-3.00) | 2.00 (0.00-3.00) | 0.194 | |
| pN stagea | N0/ 1-3 | 13/ 18 | 6/ 4 | 0.469 | 11/ 6 | 8/ 16 | 0.062 |
| pStagea | Stage I-II/ III-IV | 20/ 11 | 7/ 3 | 1 | 13/ 4 | 14/ 10 | 0.321 |
| Lymphatic invasion | absent/ present | 16/ 15 | 7/ 3 | 0.467 | 12/ 5 | 11/ 13 | 0.201 |
| Venous invasion | absent/ present | 17/ 14 | 7/ 3 | 0.48 | 12/ 5 | 12/ 12 | 0.217 |
| Operative approach | open/ laparoscopic | 25/ 6 | 6/ 4 | 0.222 | 12/ 5 | 19/ 5 | 0.714 |
| Operative procedure | DG or PG/ TG | 19/ 12 | 8/ 2 | 0.447 | 13/ 4 | 14/ 10 | 0.321 |
| Lymphadenectomy | D1 or 1+/ D2 | 10/ 21 | 6/ 4 | 0.150 | 10/ 7 | 6/ 18 | 0.051 |
| Operative time (min) | 251 (213-289) | 300 (239-324) | 0.092 | 236 (219-306) | 261 (225-305) | 0.634 | |
| Anesthesia time (min) | 289 (246-322) | 314 (275-369) | 0.141 | 277 (265-331) | 296 (264-339) | 0.525 | |
| Bleeding (mL) | 200 (50-380) | 440 (35-844) | 0.370 | 80 (20-510) | 265 (73-410) | 0.283 | |
| Comlplications | absent/ present | 20/ 11 | 6/ 4 | 1 | 12/ 5 | 14/ 10 | 0.519 |
| Duration of hospitalization (days) | 13.0 (10-18.5) | 12.0 (11-18.3) | 0.867 | 11.0 (9-14) | 13.5 (11-21) | 0.039* | |
| Adjuvant chemotherapy | absent/ present | 13/ 18 | 6/ 4 | 0.469 | 11/ 6 | 8/ 16 | 0.062 |
| Recurrence | absent/ present | 23/ 8 | 5/ 5 | 0.241 | 15/ 2 | 13/ 11 | 0.039* |
| Recurrent style (local/ lymphatic/ hematogenous/ dissemination) | 0/ 2/ 3/ 5 | 1/ 0/ 1/ 2 | 0.566 | 0/ 0/ 0/ 2 | 1/ 2/ 4/ 5 | 0.692 | |
Data are expressed as median (interquarantile range) or the number
NLR Neutrophil-to-lymphocyte ratio, PLR Platelet-to-lymphocyte ratio, POD Post-operative day, DG Distal gastrectomy, PG Proximal gastrectomy, TG Total gastrectomy
†Fisher's exact probability test to categorical variables, Mann Whitney U test to continuous variables. p<0.05, statistically significant
aUICC-TNM Classification of Gastric Cancer, 8th ed
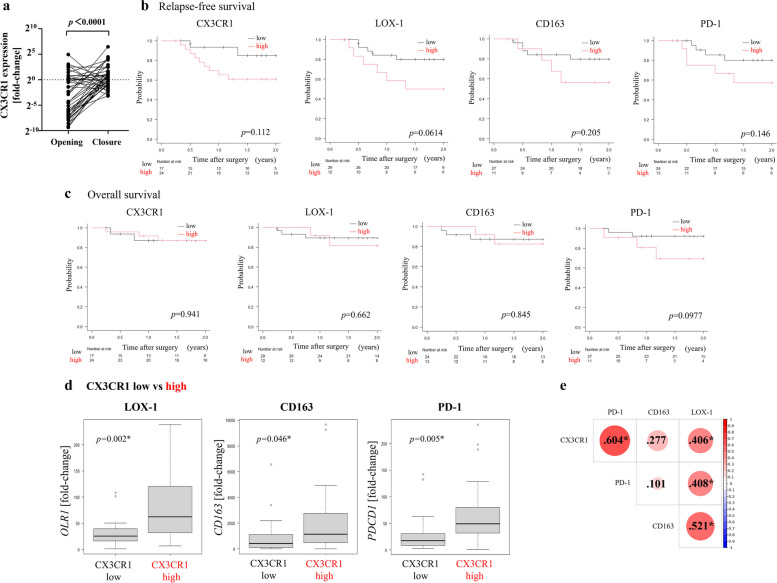
We analyzed the change of CX3CR1 expression in ILF before and after surgical maneuvers designating the cut-off sample as a baseline (Fig .1a). As a result, we found that CX3CR1 expression in a lot of ILF elevated through surgery (p<0.0001). Based on CX3CR1high or CX3CR1low at ‘Opening’ and ‘Closure’, we designated CX3CR1 changing groups as high-high, low-high, high-low, and low-low (Opening-Closure). We then analyzed their association with clinicopathological features and operative outcomes (Table 3). The low-high group showed relatively high preoperative inflammatory markers, whereas the high-low group had as low levels of those as the low-low group. The low-high group also had a trend toward higher pT stages and more recurrences, and underwent more extensive lymphadenectomy than CX3CR1low groups at ‘Closure’.We also examined LOX-1 (OLR1 gene) and CD163 (CD163 gene) expression in Closure ILF using quantitative real-time PCR. In addition, to identify immunosuppressive status and immune cell exhaustion, PD-1 (PDCD1 gene) expression was investigated. In Closure samples, sufficient levels of LOX-1, CD163, and PD-1 were obtained from 41, 37, and 38 patients, respectively. We evaluated whether the levels of LOX-1, CD163, and PD-1 had any effect on clinicopathological features and operative outcomes (Table 4). Patients were divided into two groups based on the aforementioned cut-off values (Supplementary Fig. 1). Neither CD163 nor PD-1 expression was significantly associated with clinicopathological findings or blood test parameters. However, the LOX-1high group had higher perioperative NLR and PLR, more extensive lymph node metastasis, and more extensive vascular invasion than the LOX-1low group. No significant differences were observed between perioperative outcomes and LOX-1, CD163, and PD-1 expression. LOX-1 expression was associated with postoperative recurrences significantly.
Fig. 1.
a The change of CX3CR1 expression through surgical maneuvers. b, c Comparison of relapse-free survival and overall survival based on levels of various molecules. P<0.05, statistically significant. b Relapse-free survival. c Overall survival. d Comparison of OLR1, CD163, and PDCD1 gene expression between CX3CR1high and CX3CR1low patients. *P<0.05, statistically significant. e Correlogram. Circle size indicates the degree of correlation. Figures in circles indicate correlation coefficients. Darker colors of circles indicate more-significant correlations. *P<0.05, statistically significant
Table 3.
Association of CX3CR1 dynamic change in intraperitoneal lavage fluid with clinicopathological data and operative outcomes
| CX3CR1 change 'Opening' to 'Closure' | ||||||
|---|---|---|---|---|---|---|
| high-high (n=5) | low-high (n=19) | high-low (n=5) | low-low (n=12) | P† | ||
| Sex | Male/ Female | 1/ 4 | 3/ 16 | 2/ 3 | 4/ 8 | 0.573 |
| Age(years-old) | 75.0 (67.0-78.0) | 72.0 (69.5-77.5) | 65.0 (57.0-72.0) | 71.5 (70.3-73.8) | 0.542 | |
| Tumor size (mm) | 56.0 (45.0-70.0) | 50.0 (32.5-87.5) | 38.0 (18.0-40.0) | 37.5 (30.0-56.3) | 0.258 | |
| Comorbidities | absent/ present | 1/ 4 | 2/ 17 | 1/ 4 | 2/ 10 | 0.913 |
| Other cancer history | absent/ present | 5/ 0 | 10/ 9 | 4/ 1 | 8/ 4 | 0.211 |
| Preoperative NLR | 2.20 (2.16-3.34) | 2.85 (2.28-3.52) | 1.69 (1.58-1.72) | 2.14 (1.75-3.30) | 0.123 | |
| Postoperative NLR | 7.43 (5.41-25.7) | 7.32 (5.83-10.1) | 5.88 (5.56-8.44) | 4.13 (3.54-6.14) | 0.025* | |
| Preoperative PLR | 111 (80.4-131) | 125 (93.7-178) | 53.5 (40.6-65.0) | 64.0 (51.2-115) | 0.004* | |
| Postoperative PLR | 186 (182-560) | 195 (173-399) | 89.7 (79.0-186) | 113 (83.8-167) | 0.010* | |
| CRP POD3 | 20.5 (10.1-23.2) | 13.9 (9.84-23.9) | 9.90 (8.35-14.3) | 4.34 (2.94-3.0) | 0.065 | |
| cT stagea | T1-2/ 3-4 | 2/ 3 | 4/ 15 | 2/ 3 | 5/ 7 | 0.601 |
| cN stagea | N0/ 1-3 | 3/ 2 | 15/ 4 | 4/ 1 | 9/ 3 | 0.842 |
| cStagea | Stage I-II/ III-IV | 2/ 3 | 11/ 8 | 3/ 2 | 5/ 7 | 0.757 |
| Histological type | differentiated/ undifferentiated | 1/ 4 | 11/ 8 | 3/ 2 | 7/ 5 | 0.457 |
| pT stagea | T1-2/ 3-4 | 2/ 3 | 4/ 15 | 4/ 1 | 6/ 6 | 0.082 |
| pN number | 1.0 (0.0-2.0) | 2.0 (0.0-3.0) | 0.0 (0.0-0.0) | 0.0 (0.0-3.25) | 0.498 | |
| pN stagea | N0/ 1-3 | 4/ 1 | 10/ 9 | 4/ 1 | 8/ 4 | 0.533 |
| pStagea | Stage I-II/ III-IV | 3/ 2 | 11/ 8 | 4/ 1 | 9/ 3 | 0.682 |
| Lymphatic invasion | absent/ present | 4/ 1 | 7/ 12 | 3/ 2 | 9/ 3 | 0.122 |
| Venous invasion | absent/ present | 3/ 2 | 9/ 10 | 4/ 1 | 8/ 4 | 0.521 |
| Operative approach | open/ laparoscopic | 2/ 3 | 3/ 16 | 2/ 3 | 3/ 9 | 0.555 |
| Operative procedure | DG or PG/ TG | 4/ 1 | 10/ 9 | 4/ 1 | 9/ 3 | 0.421 |
| Lymphadenectomy | D1 or 1+/ D2 | 3/ 2 | 3/ 16 | 3/ 2 | 7/ 5 | 0.045* |
| Operative time (min) | 294 (261-322) | 259 (213-286) | 306 (230-325) | 234 (211-283) | 0.353 | |
| Anesthesia time (min) | 321 (306-370) | 294 (246-324) | 339 (273-365) | 291 (248-333) | 0.469 | |
| Bleeding (mL) | 370 (50.0-615) | 230 (110-375) | 510 (20.0-920) | 70.0 (13.8-395) | 0.434 | |
| Comlplications | absent/ present | 3/ 2 | 11/ 8 | 3/ 2 | 9/ 3 | 0.803 |
| Duration of hospitalization (days) | 13 (11-20) | 14 (11.5-21.5) | 11 (11-13) | 10 (9.0-14) | 0.184 | |
| Adjuvant chemotherapy | absent/ present | 2/ 3 | 6/ 13 | 4/ 1 | 7/ 5 | 0.194 |
| Recurrence | absent/ present | 2/ 3 | 12/ 7 | 4/ 1 | 11/ 1 | 0.135 |
| Recurrent style (local/ lymphatic/ hematogenous/ dissemination) | 1/ 0/ 1/ 1 | 0/ 2/ 3/ 4 | 0/ 0/ 0/ 1 | 0/ 0/ 0/ 1 | 0.771 | |
Data are expressed as median (interquarantile range) or the number
NLR Neutrophil-to-lymphocyte ratio, PLR Platelet-to-lymphocyte ratio, POD Post-operative day, DG Distal gastrectomy, PG Proximal gastrectomy, TG Total gastrectomy
†Fisher's exact probability test to categorical variables, Mann Whitney U test to continuous variables. p<0.05, statistically significant
aUICC-TNM Classification of Gastric Cancer, 8th ed
Table 4.
Relevance to clinicopathological characteristics and operative outcomes with LOX-1, CD163, and PD-1 expression
| LOX-1 | CD163 | PD-1 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Closure | Closure | Closure | ||||||||
| low (n = 29) | high (n = 12) | P† | low (n = 24) | high (n = 13) | P† | low (n=27) | high (n=11) | P† | ||
| Sex | Male/ Female | 22/ 7 | 9/ 3 | 1 | 18/ 6 | 10/ 3 | 1 | 22/ 5 | 8/ 3 | 0.667 |
| Age(years-old) | 71.0 (65.0-73.0) | 72.5 (69.0-78.3) | 0.295 | 72.0 (69.8-76.8) | 71.0 (67.0-73.0) | 0.202 | 71.0 (67.5-72.5) | 75.0 (72.0-79.0) | 0.032* | |
| Tumor size (mm) | 40.0 (30.0-65.0) | 50.0 (40.0-87.0) | 0.240 | 40.0 (28.0-61.3) | 45.0 (30.0-56.0) | 0.556 | 40.0 (27.5-62.5) | 45.0 (32.5-63.0) | 0.640 | |
| Comorbidities | absent/ present | 3/ 26 | 3/ 9 | 0.334 | 4/ 20 | 2/ 11 | 1 | 4/ 23 | 2/ 9 | 1 |
| Other cancer history | absent/ present | 20/ 9 | 7/ 5 | 0.719 | 16/ 8 | 8/ 5 | 1 | 17/ 10 | 8/ 3 | 0.714 |
| Preoperative NLR | 2.17 (1.79-2.97) | 3.23 (2.54-4.45) | 0.037* | 2.17 (1.79-3.01) | 3.12 (2.20-3.97) | 0.124 | 2.36 (1.76-3.31) | 2.24 (2.07-4.46) | 0.376 | |
| Postoperative NLR | 5.97 (4.28-8.33) | 8.48 (5.33-23.3) | 0.140 | 5.96 (4.53-8.54) | 6.91 (4.66-15.9) | 0.455 | 5.97 (4.32-8.63) | 7.43 (4.95-16.6) | 0.247 | |
| PreoperativePLR | 78.0 (53.6-124) | 132 (108-189) | 0.003* | 79.2 (54.2-128) | 123 (92.9-132) | 0.102 | 82.3 (53.9-129) | 111 (86.6-131) | 0.274 | |
| Postoperative PLR | 164 (90.8-203) | 201 (180-568) | 0.018* | 160 (90.5-207) | 186 (177-560) | 0.102 | 157 (90.2-252) | 186 (173-407) | 0.111 | |
| cT stagea | T1-2/ 3-4 | 11/ 18 | 2/ 10 | 0.276 | 10/ 14 | 2/ 11 | 0.149 | 10/ 17 | 3/ 8 | 0.714 |
| cN stagea | N0/ 1-3 | 16/ 13 | 4/ 8 | 0.306 | 13/ 11 | 6/ 7 | 0.737 | 12/ 15 | 7/ 4 | 0.476 |
| cStagea | Stage I-II/ III-IV | 17/ 12 | 4/ 8 | 0.181 | 14/ 10 | 6/ 7 | 0.512 | 14/ 13 | 6/ 5 | 1 |
| CRP POD3 | 11.5 (4.67-17.5) | 14.2 (7.12-23.3) | 0.547 | 11.37 (5.43-17.5) | 12.1 (3.24-23.2) | 0.987 | 12.2 (4.64-19.6) | 12.1 (10.7-21.9) | 0.394 | |
| Histological type | differentiated/ undifferentiated | 14/ 15 | 8/ 4 | 0.325 | 12/ 12 | 7/ 6 | 1 | 15/ 12 | 5/ 6 | 0.724 |
| pT stagea | T1-2/ 3-4 | 12/ 17 | 4/ 8 | 0.734 | 11/ 13 | 4/ 9 | 0.491 | 11/ 16 | 4/ 7 | 1 |
| pN number | 0.00 (0.00-3.00) | 2.50 (1.75-3.25) | 0.065 | 0.00 (0.00-4.25) | 2.00 (0.00-2.00) | 0.973 | 1.00 (0.00-3.00) | 1.00 (0.00-4.00) | 0.785 | |
| pN stagea | N0/ 1-3 | 17/ 12 | 2/ 10 | 0.019* | 13/ 11 | 5/ 8 | 0.495 | 13/ 14 | 5/ 6 | 1 |
| pStagea | Stage I-II/ III-IV | 20/ 9 | 7/ 5 | 0.719 | 17/ 7 | 9/ 4 | 1 | 19/ 8 | 6/ 5 | 0.457 |
| Lymphatic invasion | absent/ present | 19/ 10 | 4/ 8 | 0.087 | 14/ 10 | 8/ 5 | 0.460 | 15/ 12 | 7/ 4 | 0.729 |
| Venous invasion | absent/ present | 20/ 9 | 4/ 8 | 0.045* | 13/ 11 | 9/ 4 | 0.638 | 17/ 10 | 6/ 5 | 0.722 |
| Operative approach | open/ laparoscopic | 20/ 9 | 6/ 6 | 0.300 | 16/ 8 | 11/ 2 | 0.440 | 19/ 8 | 7/ 4 | 0.714 |
| Operative procedure | DG or PG/ TG | 20/ 9 | 7/ 5 | 0.719 | 19/ 5 | 6/ 7 | 0.067 | 7/ 20 | 2/ 9 | 1 |
| Lymphadenectomy | D1 or 1+/ D2 | 14/ 15 | 2/ 10 | 0.084 | 9/ 15 | 6/ 7 | 0.730 | 10/ 17 | 6/ 5 | 0.471 |
| Operative time (min) | 251 (223-309) | 264 (196-297) | 0.764 | 243 (214-303) | 268 (251-306) | 0.382 | 236 (213-304) | 267 (246-308) | 0.385 | |
| Anesthesia time (min) | 294 (268-352) | 292 (233-315) | 0.422 | 274 (250-333) | 312 (279-335) | 0.259 | 277 (250-322) | 306 (282-344) | 0.311 | |
| Bleeding (mL) | 140 (20-380) | 270 (142-651) | 0.105 | 100 (20-373) | 380 (150-750) | 0.0502 | 210 (45-470) | 150 (40-683) | 0.735 | |
| Complications | absent/ present | 20/ 9 | 6/ 6 | 0.300 | 17/ 7 | 8/ 5 | 0.716 | 17/ 10 | 7/ 4 | 1 |
| Duration of hospitalization (days) | 11.0 (10-18) | 14.0 (13-20) | 0.084 | 11.5 (10-14) | 14 (11-20) | 0.291 | 12.0 (10-18) | 13.0 (11-23) | 0.457 | |
| Adjuvant chemotherapy | absent/ present | 16/ 13 | 3/ 9 | 0.098 | 14/ 10 | 4/ 9 | 0.17 | 11/ 16 | 7/ 4 | 0.288 |
| Recurrence | absent/ present | 24/ 5 | 5/ 7 | 0.020* | 20/ 4 | 7/ 6 | 0.118 | 21/ 6 | 7/ 4 | 0.432 |
| Recurrent style (local/ lymphatic/ hematogenous/ dissemination) | 1/ 1/ 1/ 2 | 0/ 1/ 3/ 5 | 0.629 | 1/ 1/ 2/ 2 | 0/ 0/ 1/ 5 | 0.318 | 0/ 0/ 1/ 5 | 1/ 1/ 2/ 2 | 0.318 | |
Data are expressed as median (interquarantile range) or the number
NLR Neutrophil-to-lymphocyte ratio, PLR Platelet-to-lymphocyte ratio, POD Post-operative day, DG Distal gastrectomy, PG Proximal gastrectomy, TG Total gastrectomy
†Fisher's probability exact test to categorical variables, Mann Whitney U test to continuous variables. p<0.05, statistically significant
aUICC-TNM Classification of Gastric Cancer, 8th ed
Association between CX3CR1, LOX-1, CD163, and PD-1 expression and survival benefits
Prognostic impacts were examined based on the expression of CX3CR1, LOX-1, CD163, and PD-1 in ‘Closure’ ILF. (Fig. 1b, c). Although not statistically significant, all high-level CX3CR1, LOX-1, CD163, and PD-1 patients tended to have poorer RFS. With regard to OS, there were no significant differences between the high and low CX3CR1, LOX-1, CD163, and PD-1 expression groups.
Relationship between CX3CR1+ cell phenotype and LOX-1 and CD163
We compared the expression of LOX-1, CD163, and PD-1 between the CX3CR1high and CX3CR1low groups in ‘Closure’ ILF. (Fig. 1d). The CX3CR1high group had higher levels of all three molecules than the CX3CR1low group. A correlogram for all three molecules is shown in Fig. 1e. CX3CR1 level was significantly correlated with PD-1 and LOX-1 expression. In particular, LOX-1 expression exhibited significant correlations with the expression of CX3CR1, CD163, and PD-1.
Considering the tumor-promoting trend and high inflammation parameters in Closure CX3CR1high patients, we used flow cytometry to classify the phenotypes of CX3CR1+ cells. With regard to tumor-promoting or immunosuppressive cells, CX3CR1 is reportedly expressed by Tregs, MDSCs, and TAMs [3]; therefore, we analyzed CD3 expression in Tregs, CD14 and CD163 expression in M-MDSCs and TAMs, and LOX-1 expression in PMN-MDSCs. Representative contour plots are shown in Fig. 2a, b. Representative histograms of these molecules are shown in Fig. 2c and revealed that the presence of these molecules was associated with CX3CR1 expression. We then analyzed the proportion of CX3CR1+ cells in ILF (Fig. 2d). This analysis showed that CX3CR1+ cells rarely express CD3 (6%), whereas a large number of LOX-1+ PMN-MDSCs (44%) and CD163+ TAMs (38%) were present. We confirmed the Treg population using a FoxP3 antibody as shown in Fig. 2e and observed a similar trend to Fig. 2d (Fig. 2f; Tregs, 2.6%). With regard to the fraction of CD14+ cells among CX3CR1+ cells, CD163+ TAMs constituted approximately 70% of CD14+CX3CR1+ cells (Fig. 2g).
Fig. 2.
Flow cytometry analysis (n=8). a Representative contour plots of CD3 and LOX-1 positivity among CX3CR1+ cells. b Representative contour plots of CD14 and CD163 positivity among CX3CR1+ cells. c Representative histograms of CX3CR1+ cells classified by CD3, LOX-1, CD14, and CD163 positivity. d, e Bar graphs showing the mean and standard error. (d) Comparison of CD3, LOX-1, and CD163 positivity among CX3CR1+ cells. *P<0.05, statistically significant. NS, not significant. e Representative contour plots of FoxP3, LOX-1, and CD163 positivity among CX3CR1+ cells. f Comparison of FoxP3, LOX-1, and CD163 positivity among CX3CR1+ cells. *P<0.05, statistically significant. g Comparison of CD163 expression among CD14+CX3CR1+ cells. *P<0.05, statistically significant.
Cytokine levels within ILF
We used some Closure samples to analyze cytokine profiles and characterize local immune environment parameters such as promotion of inflammation and macrophage polarization. A total of 25 Closure samples contained sufficient protein for analysis, consisting of 17 CX3CR1high and 8 CX3CR1low samples. A heatmap showing the expression of 10 cytokines in these 25 samples is shown in Fig. 3a. The data indicated that compared with CX3CR1low samples, MDSCs and TAMs in CX3CR1high samples tended to secrete higher levels of various cytokines, including IL-4, IL-10, GM-CSF, and IFN-γ. We then compared the cytokine concentrations in detail between CX3CR1high and CX3CR1low samples (Fig. 3b). Both groups exhibited elevated levels of inflammatory proteins such as IL-6, MCP-1, MIP-1α, and VEGF, but the differences were not statistically significant. In addition, some CX3CR1high samples contained IL-4 and IL-10, whereas these proteins were rarely detected in CX3CR1low samples. Levels of GM-CSF, IFN-γ, IL-12p70, and TNF were also significantly higher in the CX3CR1high group than in the CX3CR1low group.
Fig. 3.
Cytokine profiles of Closure samples. a Heatmap. CX3CR1 group is divided into two subgroups: the high group is shown in dark blue, and the low group is shown in light blue. b Comparison of levels of various cytokines between the CX3CR1high and CX3CR1low groups. P<0.05, statistically significant.
Discussion
The results of the present study suggest that CX3CR1+ cells appearing in the abdominal cavity after gastric cancer surgery are associated with an acute inflammatory response and that these cells may originate from immunosuppressive macrophages and MDSCs. Our data also suggest that the presence of CX3CR1+ cells affect long-term prognosis. According to previous reports, the CX3CR1-CX3CL1 axis regulates the migration, invasion, and metastasis of tumor and immune cells [3, 5, 6]. This axis interacts with and recruits TAMs and MDSCs in tumor sites [3]; therefore, these cells express CX3CR1 in tumors, as observed in our study. These immune suppressive cells would affect the difference in the trend of pathological T and N stage, and CX3CR1high patients ended up receiving slightly more adjuvant chemotherapy and significantly relapsing more than CX3CR1low patients as shown in Table 2. With regard to recurrent styles, although there was no statistical significance, CX3CR1 expression was associated with the ease of relapse at any place including dissemination. We speculated that CX3CR1+ cells that have already circulated in patients affect hematogenous and lymphatic metastasis and they then migrate in the abdominal cavity by surgical procedure getting tumor cells to escape antitumor immunity to disseminate. We examined the phenotypes of CX3CR1+ cells in ILF using flow cytometry. In addition to MDSCs and TAMs, CX3CR1+ immunosuppressive cells are also thought to include Tregs. However, our results showed that LOX-1+ PMN-MDSCs and CD163+ TAMs are major CX3CR1+ cells but that T lymphocytes such as Tregs are rarely present. In other words, our data suggest that CX3CR1+ PMN-MDSCs and TAMs in particular exhibit immunosuppressive effects in the intraperitoneal immune microenvironment.
Although we prepared both Opening and Closure samples, CX3CR1 expression in Closure samples was associated with various blood parameters and a tumor-promoting status. This result suggests that surgery promotes the invasion of CX3CR1+ cells within the peritoneum and increased blood flow. In the peritoneum and omentum, immune cells aggregate to form a structure like a secondary lymphoid organ [14]. Surgery-related stress and cancer-associated inflammation reportedly induce immune cells to mobilize in the peritoneal cavity from the peritoneum or the omental immune structure [14, 15]. In this study, CX3CR1 expression did not differ statistically in operative outcomes as shown in Table 2. Without statistical significance, there were trends that CX3CR1high patients underwent more extensive lymphadenectomy and had more bleeding. In Table 3, the low-high group underwent more extensive lymphadenectomy than CX3CR1low groups at ‘Closure’. Lymphadenectomy and surgical bleeding might be associated with CX3CR1+ cell migration into the abdominal cavity. Relationships between CX3CR1 cell migration, bleeding, and lymphadenectomy would be proven by a larger study. As shown in Tables 2 and 3, the present study suggests that collecting ILF immediately after a surgical procedure is valid for investigating the intraperitoneal immune environment.
We examined the association between CX3CR1 expression and various blood count parameters. Perioperative blood count parameters such as the NLR and PLR are reportedly poor prognostic factors in gastric cancer [16, 17]. The NLR is reportedly an indicator of tumor-associated neutrophils, thereby linking to the association with poor prognosis [18]. The NLR is also related to surgical stress. We previously reported that more-invasive surgery leads to the release of more cytokines and the mobilization of more granulocytes into the peritoneum and blood [1]. Platelets also play a role in the inflammatory response and the development of pro-tumoral inflammation [19]. In this study, the CX3CR1high group exhibited elevated perioperative NLR and PLR. CX3CR1 expression was associated with not only postoperative parameters but also preoperative parameters, which were speculated to relate with cancer-associated inflammation caused by latent presence of many immunosuppressive cells. The proportion of LOX-1+ PMN-MDSCs among CX3CR1+ cells was also associated with NLR and PLR. Our results suggest that surgery-related stress and cancer-associated inflammation in particular are mediated by CX3CR1+ PMN-MDSCs. We also hypothesize that these cells are related to an unfavorable prognosis. As a promising monitor of acute inflammatory response, CX3CR1 expression may have advantages over NLR and PLR in predicting tumor-promotion status, possibility of unfavorable prognosis, and postoperative recurrence. We may be able to take advantage of CX3CR1+ immunosuppressive cells as a novel therapeutic target, unlike blood count parameters. CRP levels were highly elevated in the CX3CR1high group. Elevation of these inflammatory markers thus probably plays a role in the longer hospital stay of CX3CR1high patients after surgery than CX3CR1low patients due to the need for treatment of inflammation. CX3CR1+ cells in patients’ blood might tell us their circulation, but their examination is somewhat invasive.
We found CX3CR1+ PMN-MDSCs and TAMs in ILF, but these tumor-promoting cells reportedly interact with each other, as MDSCs promote TAM differentiation [20, 21], and interaction can differentiate PMN-MDSCs and M-MDSCs [22]. In our study, MDSCs and TAMs constituted a majority of CX3CR1+ cells and probably exhibited a bidirectional interaction. We therefore examined the cytokine profiles in peritoneal lavage fluids. The CX3CR1high group expressed higher levels of cytokines than the CX3CR1low group. Similar levels of inflammation-promoting cytokines were detected in samples from both groups. However, significantly higher levels of GM-CSF, IFN-γ, IL-4, and IL-10 released by MDSCs and TAMs were detected in the CX3CR1high group. These results support the hypothesis that a higher frequency of CX3CR1+ PMN-MDSCs and TAMs is associated with systemic tumor-promoting conditions. Although significantly higher levels of IL-12, which is typically released by M1-macrophages, were also detected in the CX3CR1high group, we speculate that interactions between subtypes of macrophages played a role in this result.
Our results also call attention to the relationship between PD-1 expression and CX3CR1+ cells. Previous studies reported that CX3CR1+CD8+ T cells are important in antitumor immunity and associated with the response to PD-1 therapy [8, 9]. In this study, CX3CR1 was expressed on immunosuppressive cells rather than antitumor immune cells. However, immunosuppressive cells such as MDSCs and TAMs upregulate Tregs and release various cytokines leading to suppressing T cell activation, inducing to tumor-progression, and upregulating PD-L1 of the tumor: they finally promote PD-1 expression and antitumor cell exhaustion [22, 23]. Our correlogram also revealed that CX3CR1 expression is correlated with PD-1 expression. In other words, ILF could be used to determine the exhaustion status of immune cells within the intraperitoneal immune environment. Characterizing the intraperitoneal condition could enable clinicians to predict the effectiveness of immune checkpoint inhibitors such as anti–PD-1 antibodies. CX3CR1 may also be a prognostic predictor and novel treatment target.
This study has several limitations. First, the number of eligible patients was small, and the observation period was short, so bias was likely. A more-extensive and longer-term study with a larger sample size is required to reinforce our results. Second, as this study primarily utilized quantitative real-time PCR and flow cytometry, we could not elucidate functional and mechanistic details. Further studies are also necessary in this regard.
Conclusions
In conclusion, CX3CR1 is expressed on immunosuppressive cells in ILF, including MDSCs and TAMs. These cells are associated with inflammatory parameters and tumor-promotion. CX3CR1+ cells could be taken advantage of as a novel therapeutic target in the future. In addition, analyses of the intraabdominal immune environment could be useful in the development of new therapeutic strategies to treat gastric cancer.
Supplementary Information
Acknowledgements
The authors thank FORTE Science Communications (https://www.forte-science.co.jp/) for English language editing.
Abbreviations
- ILF
intraperitoneal lavage fluid
- MDSC
myeloid-derived suppressor cell
- TAM
tumor-associated macrophage
- LOX-1
lectin-like oxidized low-density lipoprotein receptor 1
- PD-1
programmed death 1
- ROC
receiver operating characteristic (curve)
- RFS
relapse-free survival
- OS
overall survival
- Treg
regulatory T cell
- M-MDSC
monocytic MDSC
- PMN-MDSC
polymorphonuclear MDSC
- POD
post-operative day
- NLR
neutrophil-to-lymphocyte ratio
- PLR
platelet-to-lymphocyte ratio
- CRP
C-reactive protein
Authors’ contributions
SN acquired, analyzed, interpreted the data, and drafted the manuscript. MY and HT contributed substantially to the conception and design of the study, interpreted the data, and critically revised the manuscript. TM also acquired, analyzed, and interpreted the data. SD, YM, TTa, TTo, and SL acquired and analyzed the data. KM contributed to the study conception and design and critically revised the manuscript. All authors read and approved the final manuscript.
Funding
No funding was received.
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The study was conducted according to the principles of the Declaration of Helsinki. Approval of the research protocol by the Institutional Review Board/Informed Consent: All experimental procedures after 2013 were approved by the Osaka City University Ethics Committee (approval nos. 3138 and 4092), and all patients provided informed consent for collection and analysis of their specimens before enrollment.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yoshii M, Tanaka H, Ohira M, Muguruma K, Lee T, Sakurai K, Kubo N, Maeda K, Hirakawa K. Regulation of neutrophil infiltration into peritoneal cavity by laparoscopic gastrectomy. Hepatogastroenterology. 2015;62:546–550. [PubMed] [Google Scholar]
- 2.Combadiere C, Salzwedel K, Smith ED, Tiffany HL, Berger EA, Murphy PM. Identification of CX3CR1. A chemotactic receptor for the human CX3C chemokine fractalkine and a fusion coreceptor for HIV-1. J Biol Chem. 1998;273:23799–23804. doi: 10.1074/jbc.273.37.23799. [DOI] [PubMed] [Google Scholar]
- 3.Korbecki J, Simińska D, Kojder K, Grochans S, Gutowska I, Chlubek D, Baranowska-Bosiacka I. Fractalkine/CX3CL1 in Neoplastic Processes. Int J Mol Sci. 2020;21:3723. doi: 10.3390/ijms21103723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Imai T, Hieshima K, Haskell C, Baba M, Nagira M, Nishimura M, Kakizaki M, Takagi S, Nomiyama H, Schall TJ, Yoshie O. Identification and Molecular Characterization of Fractalkine Receptor CX<sub>3</sub>CR1, which Mediates Both Leukocyte Migration and Adhesion. Cell. 1997;91:521–530. doi: 10.1016/S0092-8674(00)80438-9. [DOI] [PubMed] [Google Scholar]
- 5.Schmall A, Al-tamari HM, Herold S, Kampschulte M, Weigert A, Wietelmann A, Vipotnik N, Grimminger F, Seeger W, Pullamsetti SS, Savai R. Macrophage and Cancer Cell Cross-talk via CCR2 and CX3CR1 Is a Fundamental Mechanism Driving Lung Cancer. American Journal of Respiratory and Critical Care Medicine. 2014;191:437–447. doi: 10.1164/rccm.201406-1137OC. [DOI] [PubMed] [Google Scholar]
- 6.Ma X, Wang M, Yin T, Zhao Y, Wei X. Myeloid-Derived Suppressor Cells Promote Metastasis in Breast Cancer After the Stress of Operative Removal of the Primary Cancer. Front Oncol. 2019;9:855. doi: 10.3389/fonc.2019.00855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wei LM, Cao S, Yu WD, Liu YL, Wang JT. Overexpression of CX3CR1 is associated with cellular metastasis, proliferation and survival in gastric cancer. Oncol Rep. 2015;33:615–624. doi: 10.3892/or.2014.3645. [DOI] [PubMed] [Google Scholar]
- 8.Yamauchi T, Hoki T, Oba T, Jain V, Chen H, Attwood K, Battaglia S, George S, Chatta G, Puzanov I, Morrison C, Odunsi K, Segal BH, Dy GK, Ernstoff MS, Ito F. T-cell CX3CR1 expression as a dynamic blood-based biomarker of response to immune checkpoint inhibitors. Nat Commun. 2021;12:1402. doi: 10.1038/s41467-021-21619-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamauchi T, Hoki T, Oba T, Saito H, Attwood K, Sabel MS, Chang AE, Odunsi K, Ito F. CX3CR1-CD8+ T cells are critical in antitumor efficacy but functionally suppressed in the tumor microenvironment. JCI Insight. 2020;5:e133920. doi: 10.1172/jci.insight.133920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yan Y, Cao S, Liu X, Harrington SM, Bindeman WE, Adjei AA, Jang JS, Jen J, Li Y, Chanana P, Mansfield AS, Park SS, Markovic SN, Dronca RS, Dong H. CX3CR1 identifies PD-1 therapy-responsive CD8+ T cells that withstand chemotherapy during cancer chemoimmunotherapy. JCI Insight. 2018;3:e97828. doi: 10.1172/jci.insight.97828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brierley JD, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. Wiley Blackwell; Oxford, UK. 2017
- 12.Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone marrow transplantation. 2013;48:452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Danger R, Moiteaux Q, Feseha Y, Geffard E, Ramstein G, Brouard S. FaDA: A web application for regular laboratory data analyses. PLoS One. 2021;16:e0261083. doi: 10.1371/journal.pone.0261083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okabe Y. Immune Niche Within the Peritoneal Cavity. Curr Top Microbiol Immunol. 2021;434:123–134. doi: 10.1007/978-3-030-86016-5_6. [DOI] [PubMed] [Google Scholar]
- 15.Schurink B, Cleypool CGJ, Bleys R. A rapid and simple method for visualizing milky spots in large fixed tissue samples of the human greater omentum. Biotech Histochem. 2019;94:429–434. doi: 10.1080/10520295.2019.1583375. [DOI] [PubMed] [Google Scholar]
- 16.Mellor KL, Powell A, Lewis WG. Systematic Review and Meta-Analysis of the Prognostic Significance of Neutrophil-Lymphocyte Ratio (NLR) After R0 Gastrectomy for Cancer. J Gastrointest Cancer. 2018;49:237–244. doi: 10.1007/s12029-018-0127-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schiefer S, Wirsik NM, Kalkum E, Seide SE, Nienhüser H, Müller B, Billeter A, Büchler MW, Schmidt T, Probst P. Systematic Review of Prognostic Role of Blood Cell Ratios in Patients with Gastric Cancer Undergoing Surgery. Diagnostics (Basel). 2022;12:593. doi: 10.3390/diagnostics12030593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cupp MA, Cariolou M, Tzoulaki I, Aune D, Evangelou E, Berlanga-Taylor AJ. Neutrophil to lymphocyte ratio and cancer prognosis: an umbrella review of systematic reviews and meta-analyses of observational studies. BMC Med. 2020;18:360. doi: 10.1186/s12916-020-01817-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yamamoto T, Kawada K, Obama K. Inflammation-Related Biomarkers for the Prediction of Prognosis in Colorectal Cancer Patients. Int J Mol Sci. 2021;22:8002. doi: 10.3390/ijms22158002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nature Reviews Immunology. 2009;9:162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang Y, Li C, Liu T, Dai X, Bazhin AV. Myeloid-Derived Suppressor Cells in Tumors: From Mechanisms to Antigen Specificity and Microenvironmental Regulation. Front Immunol. 2020;11:1371. doi: 10.3389/fimmu.2020.01371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Veglia F, Sanseviero E, Gabrilovich DI. Myeloid-derived suppressor cells in the era of increasing myeloid cell diversity. Nat Rev Immunol. 2021;21(8):485–98 [DOI] [PMC free article] [PubMed]
- 23.Qin R, Ren W, Ya G, Wang B, He J, Ren S, Jiang L, Zhao S. Role of chemokines in the crosstalk between tumor and tumor-associated macrophages. Clin Exp Med. 2023;23(5):1359–73. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.