Abstract
Questionnaires regarding the perceptions of chemotherapy and its impact on the quality of life (QoL) of their cat were received from owners of 31 cats treated for lymphoma between 2002 and 2006 with COP (cyclophosphamide, vincristine, prednisolone) chemotherapy. The QoL scores prior to the onset of cancer (mean 9.5, range 6–10) were significantly higher than the ratings given after the onset of cancer but before commencement of chemotherapy (mean 3.9, range 1–9.4). The QoL scores during chemotherapy (mean 6.3, range 1–10) were also significantly lower than prior to the onset of cancer, but significantly higher during treatment than prior to starting treatment. Adverse effects were experienced by 27 (87%) cats during the course of chemotherapy. Twenty-five (83%) of clients were happy they treated their cat and 27 owners (87%) would treat another cat. The results suggest that COP chemotherapy is perceived by owners to be tolerated by cats.
Haematopoietic tumours are frequently diagnosed in pet cats, comprising approximately a third of all feline neoplasia (Essex et al 1976). Lymphoma accounts for the majority, and its prevalence has been increasing since the 1970s (Louwerens et al 2005). Various chemotherapy regimes have been described for treatment of feline lymphoma (Mooney et al 1989, Mahoney et al 1995, Moore et al 1996, Kristal et al 2001). Recently, chemotherapy with cyclophosphamide, vincristine and prednisolone (COP) was found to result in remission rates and survival times comparable to or better than doxorubicin-based protocols (Teske et al 2002). A COP combination is the preferred protocol for feline lymphoma for many of the British oncologists (Hayes 2006, Blackwood 2007, Dobson 2007, Murphy 2007).
It is a common conception that cats may not tolerate chemotherapy well: predicted suffering, lack of cure and poor quality of life (QoL) are common reasons for electing for euthanasia rather than treatment for feline neoplasia (Slater et al 1996). Furthermore, most owners electing to pursue chemotherapy for feline lymphoma in a recent study felt apprehensive before treatment (Malik et al 2001).
The paucity of data evaluating QoL during chemotherapy for feline lymphoma may contribute to this conception. The lack of data is surprising; such information is paramount in the decision-making processes of clients. Only one study assessed owner's satisfaction with chemotherapy (a doxorubicin-based protocol): of 27 respondents, 58% and 31% found their cats' QoL satisfactory or somewhat satisfactory, respectively, refuting the general conception of intolerance (Malik et al 2001). However, assessment of QoL was not the primary aim of this extensive study. Thus, there was no determination of how owners assessed QoL, and no analysis of factors contributing to QoL categorisation. This study did not use Likert or linear analogue scales, which are applied for assessment in analogous human QoL assessments (Michel and Tannock 1998). Both scales are reliable and responsive to changes in clinical condition (Michel and Tannock 1998), and would provide more sensitive assessment of QoL than the three categories offered in the former study. Finally, doxorubicin is often responsible for the majority of toxicity experienced by cats treated with protocols including this drug (Malik et al 2001, Brønden et al 2003), so the QoL perceived by cat owners during COP chemotherapy might be superior.
It is recognised that owners lacking understanding of adverse effects before embarking on therapy for feline cancer are less satisfied with their decision for intervention (Slater et al 1996) and adverse effects may affect owner's perception of cats' QoL. Adverse effects reported with COP include gastrointestinal, dermatological and haematological toxicities (Moore et al 1996). Assessment of the importance of adverse effects is complex, particularly as there is no established methodology for documenting QoL for cats. Karnofsky's index, a tool for assessment of QoL in humans and recently modified for cats, largely focuses on changes in behaviour, taking into account more subtle changes in eating behaviour than simply anorexia and includes assessment of sleeping, comfort and socialisation (Hartmann and Kuffer 1998). There is no information regarding the impact of chemotherapy on such behaviours, which owners may consider important in their assessment QoL. Additionally, in humans, there is discrepancy between medical records of chemotherapy recipients documenting adverse effects and the effects reported independently by the patients themselves (Velikova et al 2001). Similarly, the incidence of adverse effects is underestimated in veterinary medical records (Mallery et al 1999). Prior knowledge of the expected prevalence and nature of adverse effects would aid clients in making a well-informed, satisfactory decision about treating their cat.
The specific aims of the present study were to evaluate owners' perception of QoL during COP chemotherapy for feline lymphoma, to document adverse effects as reported by the owners, and to identify the factors influencing the owners' perception of QoL and satisfaction of their decision to treat.
Methods
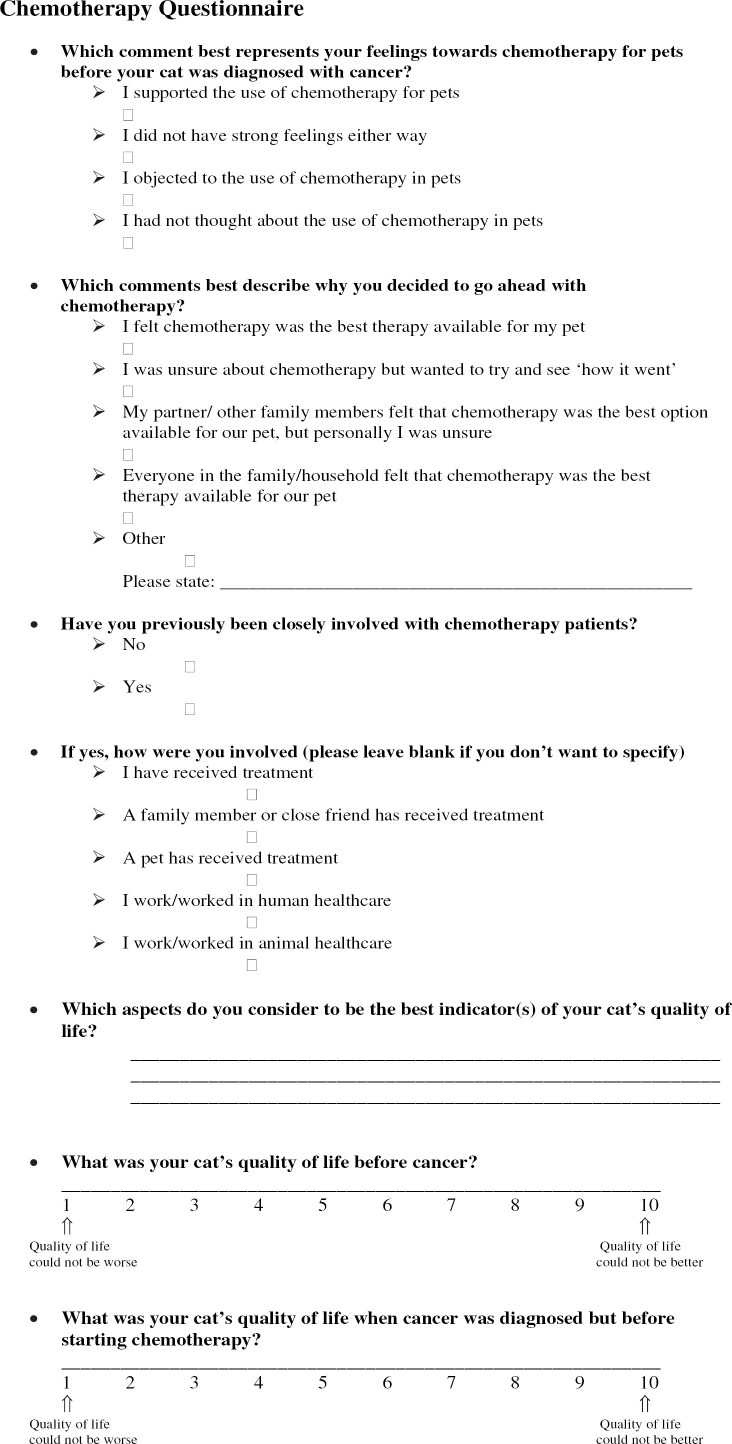
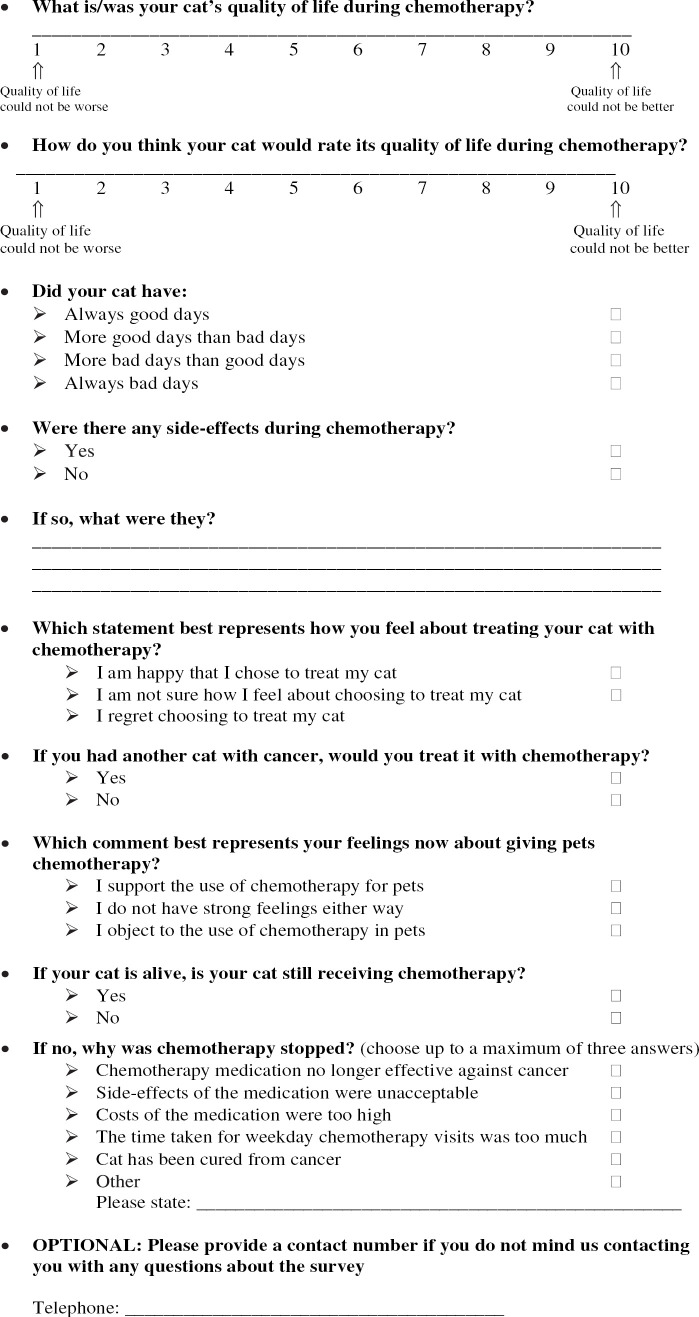
Records of cats diagnosed with lymphoma between 2002 and 2006 receiving chemotherapy treatment with a high-dose COP (intravenous cyclophosphamide, 250 mg/m2, every 3 weeks, intravenous vincristine, 0.75 mg/m2 weekly for 4 weeks then every 3 weeks, oral prednisolone, 40 mg/m2 daily for 7 days, then 20 mg/m2 every other day) at the Liverpool Small Animal Teaching Hospital (LUSATH) or with a COP-based protocol (oral cyclophosphamide, receiving 150 mg/m2 weekly; intravenous vincristine, 0.7 mg/m2, weekly for 4 weeks then every 4 weeks; oral prednisolone, 20–30 mg/m2 daily for 14 days, then every other day) at the Animal Health Trust (AHT) were reviewed. Cats were excluded from the study if they had not completed three or more treatment sessions or were never discharged from hospital. Signalment, anatomical classification of lymphoma and survival data were extracted from the records. A postal questionnaire (Fig 1) asked owners to comment on their perception of chemotherapy for pets before and after treatment of their cat, their prior experience of chemotherapy in humans and/or animals, and their initial reasons for selecting chemotherapy to treat their cat. Using a linear analogue scale, owners were asked to rate their cat's QoL on a scale of 1–10 (one being ‘quality of life could not be worse', 10 being ‘quality of life could not be better’) at three different times: pre-cancer, after diagnosis but before chemotherapy treatment, and during chemotherapy treatment. Owners were also asked to rate how they thought their cat perceived their own QoL, and to describe their cats' experience during chemotherapy as ‘all good days’, ‘more good than bad days', ‘more bad than good days’, or ‘all bad days’. Owners identified aspects they considered important to their cat's QoL, and complications of chemotherapy, in a written comment field. Owners were asked to comment on how they felt about treating their cat, and whether they would treat another cat. Finally, the owners were asked if their cat was alive. The owners were given the option of not completing the questionnaire. Follow-up telephone reminders were conducted by one of the authors (ST) if a response was not received.
Fig 1.
Chemotherapy questionnaire.
Data analysis
Data analysis was performed using SPSS 14.0 (SPSS 14.0 for Windows, SPSS, Inc.). Survival data obtained with Kaplan–Meier analysis was calculated from the start of chemotherapy until death. Cats lost to follow-up or alive at the completion of the questionnaire were censored from analysis. Associations were examined using Spearman's and Pearson's correlation coefficients, and Phi coefficient for categorical responses. Differences were explored using Mann–Whitney U tests, Wilcoxon test for related samples, and Kruskal–Wallis H test. A probability value of <0.05 was considered significant.
Results
Thirty-five of 42 cats that were receiving or had received COP chemotherapy for lymphoma met the study inclusion criteria. Thirty-one (89%) of the 35 owners completed the questionnaire. Twenty were from LUSATH (95% response rate), and 11 were from the AHT (79% response rate). Thirteen cats (42%) were alive at the time of the survey, with six (19% of total) still undergoing chemotherapy, and seven (23% of total) having completed chemotherapy and in remission. (Of the four owners who did not respond, contact was established with two, both of whom had cats that were alive and in remission. Although one owner was happy to participate in the survey and felt the experience to be positive, a questionnaire was not returned. The second owner declined to participate as she felt that her opinions were not yet established. Of the remaining two owners, one had emigrated without providing forwarding contact details and the other was not contactable by telephone or mail.)
Eight breeds were represented: 20 cats (65%) were of mixed breed (domestic short- or longhair). The remaining cats were Siamese (three), Oriental (two), Persian (two), Maine Coone (two), Burmese (one) and Devon Rex (one). Twenty cats (65%) were neutered males, nine (29%) were neutered females and two (6%) were entire females. The average age at diagnosis was 8 years (median 9 years, range 1–15 years). Seven cats (23%) had alimentary lymphoma without known other organ involvement, four cats (13%) had mediastinal lymphoma, one cat (3%) had mediastinal lymphoma with involvement of the prescapular lymph node, two cats (6%) had either multicentric or localised peripheral nodal lymphoma and 17 cats (55%) had extra-nodal lymphoma. Of the cats with extra-nodal lymphoma, five cats had nasal involvement, seven had renal involvement, two cats had alimentary lymphoma along with other extra-nodal forms, two cats had tracheal lymphoma, one cat had maxillary lymphoma, one cat had laryngeal lymphoma and one cat had retrobulbar lymphoma. Feline leukaemia (FeLV) and feline immunodeficiency viral status was known in 26 cats, with only one cat positive for each disease. Median survival time calculated for all 42 cats was 262 days (mean, 699 days, range, 1–1640 days). Median survival time for the 35 cats included in the study was 885 days (mean, 844 days, range, 30–1640 days), whereas median survival for the 31 cats for whom a questionnaire was returned was 885 days (mean, 854 days, range, 30–1640 days).
Prior experience of and attitude to chemotherapy
Prior to their cats developing cancer, 17 (55%) respondents had not previously thought about chemotherapy for pets/cats. Eleven (36%) had supported the idea of chemotherapy, and three (10%) had no strong feelings either way. No owner reported previously objecting to chemotherapy for pets.
Eighteen owners (58%) decided to treat their cat because the respondent/family thought chemotherapy was the best treatment for their pet; 11 (36%) said they had been unsure but wanted to try. Two (7%) owners had rehomed cats already receiving chemotherapy, so the decision had been made by the previous owner. No respondent selected that they were unsure although other family members wanted to try.
Nineteen (61%) cat owners reported no previous experience with chemotherapy. Of the 12 (39%) with prior experience, eight had a relative or friend who had had chemotherapy, four had worked in health care, two in animal health care, and three had previously experienced chemotherapy with another pet.
Indicators of QoL
Twenty-six owners submitted data regarding indicators of their cat's QoL; number of comments ranged from one to four. The most common indicator of QoL mentioned was appetite (24 owners, 92%). Playing (or having fun) was mentioned 14 (54%) times; being interactive 10 (38%) times, general demeanour eight (31%) times, and having energy six (23%) times. In addition, appearance, being able to get outdoors, being pain free, and being loving were mentioned three times each. Also mentioned were ‘natural behaviour’, and washing and sleeping (once each).
QoL score
Table 1 shows the owners' QoL ratings for their cats before cancer was diagnosed, after diagnosis but before treatment, and during treatment. It also shows the owners' perceptions of how their cat would rate their own QoL during treatment.
Table 1.
QoL ratings for cats by owners, rated on a scale of 1 (worst possible) to 10 (best possible)
| Rating of cats' QoL | Mean (SD) | Median | Minimum–maximum |
|---|---|---|---|
| Before cancer | 9.5 (0.99) | 10 | 6–10 |
| After diagnosis, pre-treatment | 3.9 (2.4) | 4 | 1–9.4 |
| During treatment | 6.3 (2.4) | 7 | 1–10 |
| Owners‘ perceptions of cats’ own rating during treatment | 6 (2.4) | 7 | 1–9 |
The QoL scores before the onset of cancer were significantly higher than the ratings given after diagnosis but prior to commencement of chemotherapy (Wilcoxon signed ranks test Z = −4.79, P < 0.0001). The QoL scores during chemotherapy were also significantly lower than prior to diagnosis (Wilcoxon Z = −4.64, P < 0.0001), but significantly higher during treatment than prior to treatment (Wilcoxon Z −3.41, P < 0.001). There was no significant difference between owners' ratings of their cats QoL and how they thought their cats would rate their own QoL (Wilcoxon Z = −1.72, P = 0.08).
Most owners (n = 19, 65%) reported that during chemotherapy their cats experienced more good days than bad days, and four (13%) reported that their cats had all good days. Six (19%) reported that cats had more bad days than good, and one reported that their cat had all bad days.
Alive status at the time of survey completion was significantly associated with better QoL rating during chemotherapy (Mann–Whitney U test: Z = −2.08, P = 0.037, two-tailed). Age of cat (Spearman's rho: −0.25, P = 0.21, two-tailed), QoL pre-chemotherapy (Spearman's rho: −0.07, P = 0.71, two-tailed), anatomical location of the tumour (Kruskal–Wallis test: χ2 3.54, df 3, P = 0.32), and breed (Kruskal–Wallis test: χ2 = 3.34, df = 7, P = 0.85) were not significantly associated with QoL rating.
Adverse effects during chemotherapy
Adverse effects were experienced by 27 (87%) cats (median two per cat) (Table 2). Hair loss was significantly associated with whisker loss (Phi = 0.41, P = 0.023), and loss of appetite was associated with lethargy (Phi = 0.44, P = 0.015). Hair loss was associated with a higher QoL rating (≥7) during chemotherapy (Phi = 0.49, P = 0.006). There was a non-significant association between loss of appetite and a lower QoL rating (<7) during chemotherapy (Phi = −0.32, P = 0.07). There was a non-significant association between experiencing hair loss and being alive at the study completion (Phi = −0.33, P = 0.07). Number of side effects was significantly related to number of bad days compared with number of good days (Spearman's rho = 0.38, P = 0.03).
Table 2.
Adverse effects reported during COP chemotherapy for feline lymphoma in 31 cats
| Adverse effect reported | Number of owners reporting effect (%) |
|---|---|
| Hair loss | 11 (35) |
| Loss of appetite | 9 (29) |
| Lethargy | 8 (26) |
| Vomiting | 7 (23) |
| Whisker loss | 5 (16) |
| Sleepiness | 5 (16) |
| Weight loss | 4 (13) |
| Stress | 1 (3) |
| Breathing difficulties | 1 (3) |
| Scared | 1 (3) |
| Constipation | 1 (3) |
| Incontinence | 1 (3) |
| Falling over | 1 (3) |
| Miserable | 1 (3) |
| Diarrhoea | 1 (3) |
| Urinary tract infection | 1 (3) |
Owners' assessment of their experience with chemotherapy
Twenty-five (81%) owners were happy that they treated their cat with chemotherapy, three (10%) were not sure and three (10%) felt regretful that they had chosen chemotherapy. Owners whose cats were now dead were less likely to report that they were happy that they had treated their cat (Phi = −0.42, P = 0.02), but were not more likely to regret treatment (Phi = 0.28, P = 0.12). Owners' feelings regarding their decision to treat their cat were associated with the number of side effects: regretful owners recorded a higher number of side effects (Spearman's rho = 0.38, P = 0.032). The length of time that had elapsed between the diagnosis and completing the survey was not significantly associated with QoL rating (Pearson's r = −0.27, P = 0.17). Twenty-seven owners (87%) would treat another cat with COP chemotherapy for lymphoma, and four (13%) would not.
Discussion
This study found that the majority of owners were happy that they chose to treat their cat with COP chemotherapy and would choose to treat another cat with lymphoma. This was despite that the QoL during chemotherapy failed to completely return to pre-disease levels, suggesting that a small reduction in QoL is acceptable to owners. A similar ‘trade off’ is recognised in human oncology, where patients often prioritise the antineoplastic effects over toxicity and convenience (Gunnars et al 2001).
In veterinary medicine, where chemotherapy is frequently palliative, tolerating a decline in QoL may be less expected. However, the acceptance may be enhanced in patients with lymphoma, as the main alternative to chemotherapy is euthanasia. In addition, despite the fact that owners are informed of the palliative nature of treatment and expected survival times, 30% of owners overestimate their cats' life expectancy (Slater et al 1996), and this optimism may encourage owners that have embarked on therapy to accept a reduction in QoL. In the current study, the hope or actuality of long-term survival may have enhanced the owners' satisfaction with therapy, particularly in the individuals with living cats, and a positive correlation was found between a higher QoL rating and having a cat alive at the time of the survey response. A positive correlation was also observed between hair loss and a higher QoL rating, and as hair loss tends to occur later in therapy, these cats may represent the long-term survivors. Although it has been reported that up to 30% of cats with lymphoma may experience long-term survival (Malik et al 2001, Vail 2007) and seven (23%) cats in the current study were alive and in remission after completing chemotherapy, these still represent the minority of patients, and false optimism experienced by those owners whose cats were now dead would not be expected to produce a higher QoL rating. In addition, as data in the current study were derived using univariate analysis, it would be useful to investigate the relationship of adverse effects and QoL in future larger number studies with multivariate techniques, thus identifying potentially confounding variables.
The majority of cats experienced adverse effects during chemotherapy, but no cat was euthanased because of adverse effects. The rate of toxicity reported previously (29% or around 1/3) is less than that of the current study (87%) (Moore et al 1996, Teske et al 2002). This is probably due to the inclusion of adverse effects that are under-reported in conventional studies (such as lethargy) as the incidence of vomiting or diarrhoea (23% and 3%, respectively) is similar to previous reports (Moore et al 1996). Under-reporting may occur because the owners do not consider certain adverse effects to be worthy of report, or do not want to jeopardise their pet receiving therapy because of adverse effects they consider tolerable.
The current study did not allow allocation of relative weights of adverse effects, but the owner's rating of QoL allowed an indirect assessment. For instance, one of the more intolerable effects may be anorexia, as there was a trend for anorexia to be associated with lower QoL ratings, while good appetite was the most common indicator of good QoL. Unsurprisingly, feeling happy with the decision to treat was correlated with the number of adverse effects experienced. Understanding the nature and incidence of adverse effects influences satisfaction with the decision to treat (Slater et al 1996), so is important that owners are informed of all potential alterations to normal behaviour and not simply gastrointestinal, haematological and dermatological adverse effects. The current study assessed QoL as perceived by the owners, acting as proxy respondents. There are no validated direct or proxy survey instruments available for assessment of QoL in feline patients, and we have identified factors that contributed to owners perception of QoL. This provides critical information for future studies.
QoL measurements were obtained using linear analogue scales to provide an accurate gauge of the relative changes in QoL from normal, through diagnosis and chemotherapy. Anchor points were provided (such as ‘could not be better’), but an absolute value, such as the mean rating during chemotherapy, cannot be definitively interpreted as good or bad. This is because the position on the scale is not standardised across the population and is only meaningful for the individual (Altman 1991). It seems likely that the perceived decline in QoL during chemotherapy was not sufficient for the owner to consider that their pet's QoL was poor or insufficient, and thus the positive perception of the decision to treat. Using similar QoL assessments a large range of other disease processes might result in a similar pattern of reduced QoL prior to treatment, and improved QoL after treatment, without a return to the perceived QoL prior to illness: no comparable data are available.
The median survival time of the surveyed population was 885 days. This exceeds the median survival (up to 654 days) previously reported for cats obtaining complete remission (Mooney et al 1989, Mahoney et al,1995, Kristal et al 2001, Teske et al 2002, Milner et al 2005). It is probable that the majority of the cats receiving less than three treatments, and thus excluded from the study, failed to respond to treatment. The study examined the remaining population of median and long-term survivors, and is comparable with previous populations of complete responders as it is likely that most of these cats obtained complete remission. Clearly, the present population may differ from previously reported populations due to differences in anatomical disease distribution and prevalence of FeLV in different geographical locations, and censorship. However, the present data concur with previous reports that a significant proportion of feline lymphoma patients can achieve long-term survival (Malik et al 2001, Teske et al 2002).
The study assessed the opinions of a referral clientele, and it may be argued that this highly motivated population may be more open-minded to treatment options for their pets. Conversely, however, this high commitment may also result in a high sensitivity to perceived distress. Secondly, due to the retrospective nature of the study, recall bias may have occurred. However, there was no correlation between length of time since diagnosis and QoL rating. Finally, data collection using postal questionnaires may suffer from non-respondent bias (Asch et al 1997). However, the high response rates obtained in the current study (>80%) minimises such bias (Sadura et al 1992, Asch et al 1997). In addition, follow-up telephone communication established that at least one of the two non-respondents with whom contact was possible was likely to be satisfied with their experience with chemotherapy, suggesting that the non-respondents were not necessarily a population that had negative feelings regarding their pet's treatment. It is likely the current results are a reasonable representation of a UK referral clientele.
Conclusions
The current study demonstrates that COP chemotherapy is perceived favourably by cat owners. Regardless of a perceived minor decline in their cat's QoL, 81% of clients were happy they treated their cat and 87% would treat another cat. While not perceived to detract greatly from the QoL during COP chemotherapy for feline lymphoma, it is important to recognise the high incidence of potentially minor adverse effects. Further work assessing QoL and adverse effects will allow continued improvement in the care of these patients.
Acknowledgements
The authors are grateful to staff of LUSATH and AHT, in particular Patricia Ibarrola, Daniel Batchelor and Alison Hayes, for assistance with case management, Jody Turner for AHT data retrieval, and to the numerous owners who submitted questionnaires for analysis.
References
- Altman D.G. Types of data. Altman D.G. Practical Statistics for Medical Research, 1991, Chapman and Hall: London, 10–18. [Google Scholar]
- Asch D.A., Jedrziewski M.K., Christakis N.A. Response rates to mail surveys published in medical journals, Journal of Clinical Epidemiology 50, 1997, 1129–1136. [DOI] [PubMed] [Google Scholar]
- Blackwood L. (2007) Personal communication.
- Brønden L.B., Rutterman G.R., Flagstad A., Teske E. Study of dog and cat owners' perceptions of medical treatment for cancer, Veterinary Record 152, 2003, 77–80. [DOI] [PubMed] [Google Scholar]
- Dobson J. (2007) Personal communication.
- Essex M., Sliski A., Hardy W.D., Cotter S.M. The immune response to leukaemia virus and tumour associated antigens in cats, Cancer Research 36, 1976, 376–381. [PubMed] [Google Scholar]
- Gunnars B., Nygren P., Glimelius B. Assessment of quality of life during chemotherapy, Acta Oncologica 40, 2001, 175–184. [DOI] [PubMed] [Google Scholar]
- Hartmann K., Kuffer M. Karnofsky's score modified for cats, European Journal of Medical Research 3, 1998, 95–98. [PubMed] [Google Scholar]
- Hayes A. Feline lymphoma 1: principles of diagnosis and management, In Practice 28, 2006, 516–524. [Google Scholar]
- Kristal O., Lana S.E., Ogilvie O., Rand W.M., Cotter S.M., Moore A.S. Single agent chemotherapy with doxorubicin for feline lymphoma: a retrospective study of 19 cases (1994–1997), Journal of Veterinary Internal Medicine 15, 2001, 125–130. [DOI] [PubMed] [Google Scholar]
- Louwerens M., London C.A., Pedersen N.C., Lyons L.A. Feline lymphoma in the post-feline leukaemia virus era, Journal of Veterinary Internal Medicine 19, 2005, 329–335. [DOI] [PubMed] [Google Scholar]
- Mahoney O.M., Moore A.S., Cotter S.M., Engler S.J., Brown D., Pennick D.G. Alimentaty lymphoma in cats: 28 cases (1988–1993), Journal of the American Veterinary Medical Association 15, 1995, 1593–1598. [PubMed] [Google Scholar]
- Malik R., Gabor L.J., Foster S.F., McCorkell B.E., Canfield P.J. Therapy for Australian cats with lymphosarcoma, Australian Veterinary Journal 79, 2001, 808–817. [DOI] [PubMed] [Google Scholar]
- Mallery K.F., Freeman L.M., Harpster N.K., Rush J.E. Factors contributing to the decision for euthanasia of dogs with congestive heart failure, Journal of the American Veterinary Medical Association 214, 1999, 1201–1204. [PubMed] [Google Scholar]
- Michel M., Tannock I.F. Measuring health-related quality of life in clinical trials that evaluate the role of chemotherapy in cancer treatment, Canadian Medical Association Journal 158, 1998, 1727–1734. [PMC free article] [PubMed] [Google Scholar]
- Milner R.J., Peyton J., Cooke K., Fox L.E., Gallagher A., Gordon P., Hester J. Response rates and survival times for cats with lymphoma treated with the University of Wisconsin-Madison chemotherapy protocol: 38 cases (1996–2003), Journal of the American Veterinary Medical Association 7, 2005, 1118–1122. [DOI] [PubMed] [Google Scholar]
- Mooney S.C., Hayes A.A., MacEwen E.G., Matus R.E., Geary A., Shurgot B.A. Treatment and prognostic factors in lymphoma in cats: 103 cases (1977–1981), Journal of the American Veterinary Medical Association 194, 1989, 696–702. [PubMed] [Google Scholar]
- Moore A.S., Cotter S.M., Frimberger A.E., Wood C.A., Rand W.M., L'Heureux D.A. A comparison of doxorubicin and COP for maintenance of remission in cats with lymphoma, Journal of Veterinary Internal Medicine 10, 1996, 372–375. [DOI] [PubMed] [Google Scholar]
- Murphy S. (2007) Personal communication.
- Sadura A., Pater J., Osoba D., Levine M., Palmer M., Bennett K. Quality-of-life assessment: patient compliance with questionnaire completion, Journal of the National Cancer Institute 84, 1992, 1023–1026. [DOI] [PubMed] [Google Scholar]
- Slater M.R., Barton C.L., Rogers K.S., Peterson J.L., Harris C.K., Wallace K. Factors affecting treatment decisions and satisfaction of owners of cats with cancer, Journal of the American Veterinary Medical Association 208, 1996, 1248–1252. [PubMed] [Google Scholar]
- Teske E., Van Straten G., van Noort R., Ruttema G.R. Chemotherapy with Cyclophosphamide, Vincristine, and Prednisolone (COP) in cats with malignant lymphoma: new results with an old protocol, Journal of Veterinary Internal Medicine 16, 2002, 179–186. [DOI] [PubMed] [Google Scholar]
- Vail D.M. Hematopoietic tumors, feline lymphoma and leukemia. Withrow S.J., Vail D.M. Withrow and MacEwen's Small Animal Clinical Oncology, 4th edn, 2007, Elsevier: Philadelphia, 733–756. [Google Scholar]
- Velikova G., Wright P., Smith A.B., Stark D., Perren T., Brown J., Selby P. Self-reported quality of life of individual cancer patients: concordance of results with disease course and medical records, Journal of Clinical Oncology 19, 2001, 2064–2073. [DOI] [PubMed] [Google Scholar]