Abstract
Practical relevance Blindness and behavioural changes occur relatively commonly in cats, either separately or in combination, causing devastating consequences for the cat and owner. Blindness can be caused by primary ophthalmic, metabolic or intracranial disease. Similarly behavioural changes may be the primary result of intracranial or systemic disease, but also occur secondarily to visual deficits or changes in interaction with the external environment (ie, non-medical problems). The anatomical pathways involved in vision are very close to those involved in behavioural regulation. It is, therefore, likely that a brain lesion (especially a forebrain lesion) that causes blindness will also cause behavioural abnormalities.
Clinical challenges In cases of partial or unilateral blindness, obvious visual deficits may not be apparent to the owner or clinician. Rather, the visual impairment may manifest more subtly as changes in behaviour, reluctance to jump or unwillingness to go outside. Similarly, behavioural problems may be episodic and, hence, a cat presenting with behavioural disturbances may appear clinically normal on evaluation. Behavioural changes are unlikely to be noticed unless marked and associated with bilateral blindness or advanced systemic illness.
Audience This article discusses these two major disorders separately, with the aim of highlighting for the clinician some of the important aspects of the general clinical and neurological examination that can be performed to identify these challenging cases.
BLINDNESS
Definitions
Traditionally blindness has been categorised as central or peripheral, although this terminology can cause confusion. For the purposes of this review, peripheral blindness is defined as that resulting from any lesion along the visual pathway shared with the pupillary light reflex (PLR) pathways. Central blindness, in contrast, results from a lesion in the visual pathway not shared with the PLR pathways.
Blindness can be partial or complete, unilateral or bilateral. The presentation depends on the aetiology and, as such, the ophthalmic and neurological examinations provide important clues as to the likely problem.
Peripheral blindness
Blindness due to a lesion rostral to the thalamus (ie, within the eye, cranial nerve II, optic chiasm or proximal optic tract).
Central blindness
Blindness due to a lesion caudal to the thalamus (ie, the forebrain including the distal optic tract, lateral geniculate nucleus, optic radiation or occipital cortex).
Clinical goals
The main goals for the clinician are to establish whether the blindness is the result of an ophthalmological or neurological disease; and, in the event of a suspected neurological condition, to localise the lesion accurately within the visual pathways. Having determined the neurological localisation, a list of possible causes for this localisation can be formulated. It is important then to proceed through a systematic investigation, selecting appropriate tests to diagnose the underlying condition; this will allow appropriate treatment to be implemented.
MULTIMEDIA
A video recording showing the abnormal behaviour and gait of a cat diagnosed with a left forebrain lesion is included in the online version of this article doi:10.1016/j.jfms.2011.09.007
Neuroanatomy
The pathways involved in the conscious perception of vision are outlined in Fig 1. Each cerebral hemisphere receives information from the contralateral visual field. The first neuron in the visual pathway is the bipolar cell of the retina, which receives impulses from the neuroepithelial cells of the retina (rods and cones). These synapse with a second neuron (ie, the retinal ganglion cells) and the axons of this neuron course in the optic nerve. In the cat, nasal (medial) retinal ganglion fibres (representing 65% of the retinal fibres) decussate at the optic chiasm, whereas temporal (lateral) retinal fibres (the remaining 35%) do not. 1 Therefore, a unilateral lesion will cause deficits of 35% and 65% in the visual fields of the ipsilateral and contralateral eye, respectively, although clinically this difference is not appreciable. Following the chiasm the ganglion fibres then course in the optic tract to the level of the thalamus and at this point the fibres follow one of two routes:
FIG 1.

The pathways for conscious perception of vision
Conscious perception of vision 80% of the optic fibres continue to the occipital cortex.
-
Reflex activity The remaining 20% of fibres are involved in two possible pathways:
Overlap of the visual fields (estimated at 75% in humans and approximately 50% in carnivores) 3 is the basis of binocular vision and depth perception. As a result of this overlap, we can only reliably test the function of the temporal visual fields (ie, nasal part of the retina).Parasympathetic pathway: these fibres are involved in the afferent arm of the PLR (see box below). In cats, the post-ganglionic fibres of the oculomotor nerve that form the efferent arm of the PLR are termed the ‘short ciliary fibres’. In dogs, this represents five to eight short ciliary nerves. In the cat, however, there are only two short ciliary nerves (ie, the malar and nasal). This anatomical difference may result in the characteristic ‘D’ shaped or ‘reverse D-shaped’ pupil seen in cats with lesions in only one of the two ciliary nerves. 2
Somatic motor responses: the remaining fibres synapse in the rostral colliculi of the midbrain where they are important in reflex movements of the head.
Pupillary light reflex
The PLR has an afferent (sensory) component and an efferent (motor) component, with no cerebral involvement. The afferent arm of this reflex shares some common pathways with the first part of the menace response (up to the level of the optic tract). Fibres involved in the PLR bypass the thalamus to terminate in the contralateral pretectal nucleus in the mesencephalon. The majority of these axons decussate to synapse on the ipsilateral parasympathetic nucleus of the oculomotor nerve (cranial nerve III). Pupillary constriction is, therefore, bilateral.

Clinical evaluation
Blindness can be caused by a lesion anywhere along the peripheral or central visual pathways. Therefore, a complete neurological and fundoscopic examination should be performed in every case to determine the localisation. 4 Assessment of the pathways outlined above for conscious perception of vision and the associated reflexes during the neurological examination allows the clinician to localise the blindness as central or peripheral.
Conscious perception of vision An assessment of conscious awareness of vision is made during the ‘hands-off’ neurological examination. 4 This involves observing the cat negotiating its way around an unusual environment (eg, the consulting room).
Abnormalities of behaviour and gait can also be detected in this manner. It is possible that unilateral blindness may go undetected and, in some cases, cats may be reluctant to move.
A normal PLR requires only the peripheral visual pathways to be intact and is not affected by a lesion involving the central visual pathways.
Therefore, visual placing can be used as an additional or alternative test.
Pupil size Pupillary size is valuable in localising a lesion (Fig 2). It is important to remember that cats can become easily stressed, causing increased sympathetic tone. This has the effect of dilating the pupils and reducing their normal response to light.
Pupillary light reflex The PLR should be evaluated alongside the menace response to determine whether the blindness is central or peripheral. A normal PLR requires only the peripheral visual pathways to be intact and is not affected by a lesion involving the central visual pathways.
Dazzle reflex This reflex theoretically evaluates the somatic motor response pathway, although in practice it can be very difficult to interpret and to obtain a useful clinical localisation. A bright light shone directly into the eye causes partial eyelid closure in the normal cat.
Menace Response This is a cortically mediated eyelid closure that occurs when a cat is confronted with a visual threat (see box). The menace response is a learned response and not a reflex. As such it may not become fully developed until 10–12 weeks of age in some cats and so testing in young patients may result in a false-negative result. If the menace response is not intact it is important to ensure that the facial and trigeminal nerves are functioning correctly. This is undertaken by touching the lateral and medial canthi of both eyelids. The result of this sensory stimulation should be a reflex closure of the ipsilateral eyelid. Absence of the palpebral reflex would suggest a trigeminal or facial nerve lesion.
Electroretinography Retinal function can be assessed using electroretinography to record the response of the retina to light stimulation. It may determine whether blindness is caused by retinal or post-retinal disease. The use of electroretinography is more common in dogs where ocular changes may be minimal despite overt retinal disease (eg, sudden acquired retinal degeneration syndrome). In cats, the majority of retinal diseases would cause visible ophthalmoscopic abnormalities and, hence, its use is limited.
FIG 2.
The effects of different visual pathway lesions on pupil size and light response. (A) Lesion of the ocular media, retina or optic nerve on the right side. The right pupil is mydriatic but may not be fully dilated due to consensual input from the left eye. Light stimulation of the left eye induces constriction of both pupils due to decussation at the chiasm and midbrain. Light stimulation of the right eye causes no change in the size of either pupil. (B) Lesion of the optic chiasm. Bilateral mydriasis is seen at rest. Both pupils are unresponsive to light. (C) Right-sided lesion of the optic tract. The pupils are normal in size at rest and constrict appropriately to light stimulation. (D) Lesion of the right visual cortex. The pupils are normal in size at rest and constrict appropriately to light stimulation
A normal menace response requires intact central and peripheral visual pathways.
Menace response
A normal menace response requires intact central and peripheral visual pathways, in addition to connections from the cerebrum to the brainstem and cerebellum. The pathway is initially the same as for the PLR (see box on page 864) up to the level of the optic chiasm. At this point the optic tract continues to the lateral geniculate nucleus and then on to the visual cortex (in the occipital lobe) via the optic radiation. It is assumed that the visual cortex projects to the motor cortex (ie, the frontal and parietal lobes). From here a cerebropontocerebellar pathway is postulated but the exact pathway is poorly understood. Fibres then exit the cerebellum via the rostral peduncle and synapse on the facial (VII) nucleus, stimulating the facial nerve and resulting in eyelid closure.

Localising the lesion
By combining the results of these tests it should be possible to accurately localise the lesion. For example, an abnormal PLR and menace response suggest the lesion lies within the pathways shared by these two tests. However, a normal PLR and abnormal menace response suggest a lesion within the visual pathways not shared by the PLR.
Figs 3 and 4 illustrate the processes involved in localising a unilateral and bilateral blindness.
FIG 3.
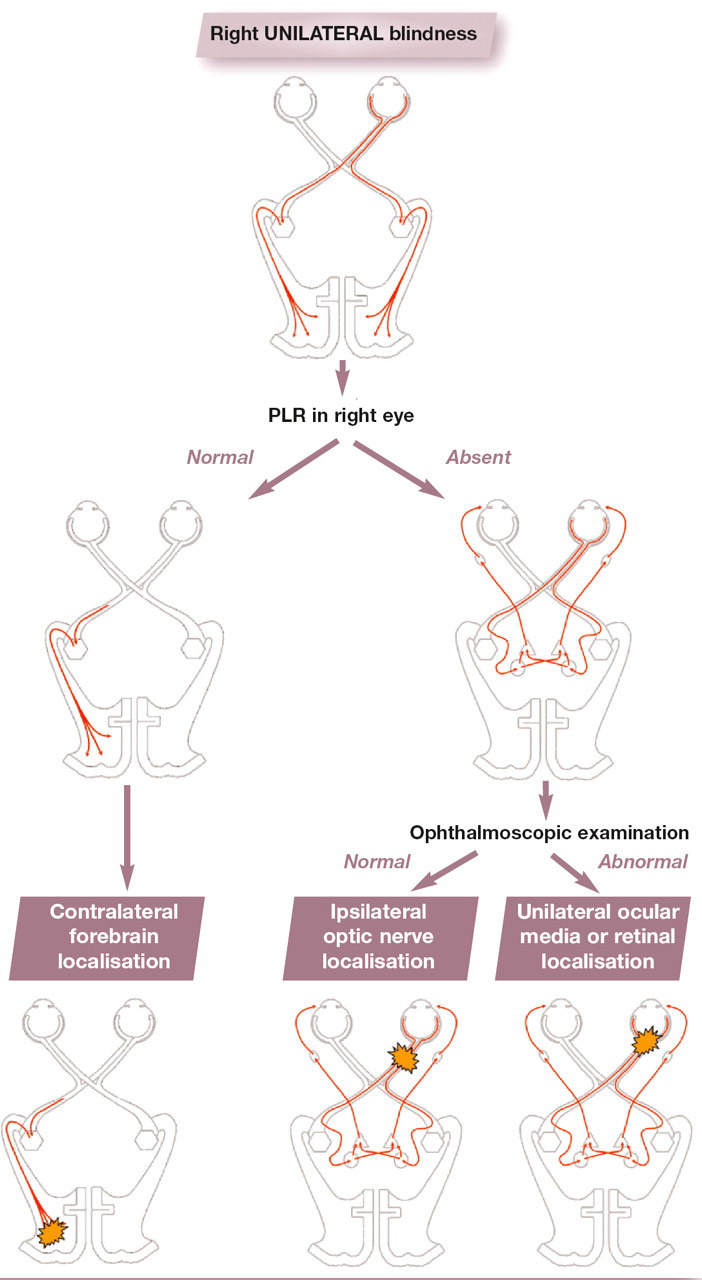
An approach to unilateral blindness using the PLR (pupillary light reflex) and ophthalmoscopic examination to determine lesion localisation
FIG 4.

An approach to bilateral blindness using the PLR and ophthalmoscopic examination to determine lesion localisation
Differential diagnosis
Having ascertained the location of the lesion the clinician must then determine the likely differential diagnoses. Table 1 lists diseases causing central and peripheral blindness in the cat, grouped by disease process using the ‘Vitamin D’ mnemonic. Thus the neurological localisation will help direct the clinical work-up, which, in turn, will further refine this list as possible causes for the blindness are investigated.
TABLE 1.
Neurological differential diagnoses for blindness grouped using the ‘Vitamin D’ mnemonic
| Disease process | Central blindness (ie, forebrain localisation) | Peripheral blindness (ie, retinal, optic nerve and optic chiasm localisation) |
|---|---|---|
|
| ||
| Vascular |
|
Ischaemic necrosis of the optic chiasm (secondary to feline ischaemic encephalopathy) Retinal detachment and/or haemorrhage secondary to arterial hypertension |
| Inflammatory | Infectious encephalitis (viral, protozoal, fungal, bacterial) |
|
| Traumatic | Head trauma | Trauma to the globes or orbits |
| Toxic |
|
Enrofloxacin toxicity (causing retinal degeneration) |
| Anomalous |
|
|
| Metabolic |
|
|
| Neoplastic | Primary or secondary brain tumour | Tumour of, or in vicinity of, optic chiasm (eg, meningioma, pituitary macroadenoma) Neoplasia of the optic nerve or compressing the optic nerve |
| Degenerative | Feline neuroaxonal dystrophy | |
Global brain ischaemia
Anaesthesia and cardiac arrest can cause cerebral hypoxia, which may result in blindness, 5 anisocoria 6 and seizures. 7 Magnetic resonance imaging may be helpful in identifying an underlying ischaemic encephalopathy, with the distribution of lesions reflecting areas with a particular susceptibility to hypoxia (eg, the occipital and parietal lobes, caudate nuclei and hippocampus). This is an uncommon complication of anaesthesia although it is an important cause of blindness in cats. Unfortunately very little is known regarding the prognosis in these cases. Of the reported cases, the majority of cats did not regain normal sight. However, published cases are limited in number and only reflect a referred population of patients, including those with unfavourable outcomes undergoing histopathological examination to achieve a definitive diagnosis. No specific treatment is required but time and supportive nursing care may allow some improvement.
Table 2 provides a clinical summary of the common conditions causing visual and behavioural disturbances in cats. A more extensive review of many of these diseases is found within the accompanying articles in this current neurologythemed issue of the Journal of Feline Medicine and Surgery, as well as in an earlier neurologythemed issue, published in May 2009 (vol 11, issue 5). One cause meriting brief discussion here is global brain ischaemia, as it has not been covered elsewhere.
TABLE 2.
Some of the more common intracranial causes of blindness and/or behavioural changes in cats
| Disease | Onset of clinical signs | MRI appearance and CSF changes | Therapy | Prognosis |
|---|---|---|---|---|
|
| ||||
| Vascular | ||||
| Cerebrovascular accidents | Peracute/acute * | Infarct: Intra-axial areas, with minimal mass effect, confined to a specific vascular territory, hyperintense on T2WI, delayed mild CE | Treat the underlying cause; otherwise supportive therapy | Good if no underlying cause identified |
| Haemorrhage: Intra- and/or extra-axial with mass effect, variable signal intensity and CE depending on the timing | Medical treatment; surgical therapy in the case of superficial compressive haematoma or failure of medical treatment | Fair to guarded, dependent on severity of clinical signs and response to therapy | ||
| Neoplastic | ||||
| Meningioma | Chronic | Intra-axial space-occupying lesion, hyperintense on T2WI, with homogeneous CE | Surgical removal and/or chemotherapy or radiotherapy | Fair |
| Lymphoma | Variable | Intra/extra-axial ill-defined lesions, with variable mass effect and signal intensity; CSF tap can reveal neoplastic cells | Chemotherapy; radiotherapy possible for a single lesion | Guarded/poor |
| Inflammatory/infectious | Subacute/acute | Meningeal/intra-axial single or multiple lesions, with variable mass effect and signal intensity; CSF usually confirms inflammatory aetiology | Immunosuppressive in case of sterile form of unknown aetiology | Guarded/fair |
| Traumatic | ||||
| Brain trauma | Peracute/acute * | Skull fracture, brain damage (contusion, laceration, etc) | Conservative (anti-oedema, antiepileptic, to decrease ICP) or surgical | Related to severity of presenting signs |
| Anomalous | ||||
| eg, Hydrocephalus | First weeks/months to first years of age | Hydrocephalus (dilation of ventricular system) | Conservative (decrease CSF production) or surgical (VPS) | Guarded/fair |
| Metabolic | ||||
| Thiamine deficiency | Acute/subacute | T2 hyperintensity of caudal colliculi, vestibular nuclei | Vitamin B1 supplementation | Good |
| Global brain ischaemia | Strictly related to anaesthesia | Bilateral and symmetrical T2 hyperintense lesions in the cerebral cortex | Supportive treatment | Related to severity of presenting signs |
| Hepatic encephalopathy | Subacute | Widened sulci, hyperintensity of lentiform nuclei on T1WI | Surgical correction of underlying hepatic disease when possible. Otherwise medical treatment (dietary management, lactulose, etc) | Guarded/fair |
Blindness and behavioural changes can sometimes have a belated onset. CE = contrast enhancement, ICP = intracranial pressure, VPS = ventriculoperitonealshunt
BEHAVIOURAL CHANGES
Definitions
Behavioural problems are becoming more frequently recognised in domestic animals, including dogs and cats. This is likely due to many factors, not least that dogs and cats live indoors in close contact with us, creating a denaturalisation of the animal's habits and increasing the owner's sensitivity in recognising abnormal behaviour. That said, differentiating between what is normal and abnormal in veterinary behavioural medicine can be challenging. In fact, behavioural changes can be vague and non-specific, with an owner's account of what constitutes abnormal behaviour being subjective and difficult to interpret.
Behaviour can be defined as the product of the fine integration between an animal's internal (physiological/neurochemical, neuroanatomical and genetic components) and external environments and the extent to which these environments interact to produce long-term potentiation (cellular/molecular memory and learning). 8 Therefore, any changes in the internal and/or external environment of the cat can theoretically lead to abnormal behaviour.
For more practical (and didactic) purposes it is useful to differentiate between primary behavioural problems, which occur in the absence of concurrent medical conditions, and behavioural changes secondary to underlying disease, either neurological or non-neurological. In cats, in particular, it is not uncommon to observe abnormal behaviour as the sole manifestation of a neurological disease. Consequently, behavioural changes can sometimes be the only presenting sign to many owners.
In cats it is not uncommon to observe abnormal behaviour as the sole manifestation of a neurological disease.
Neuroanatomy
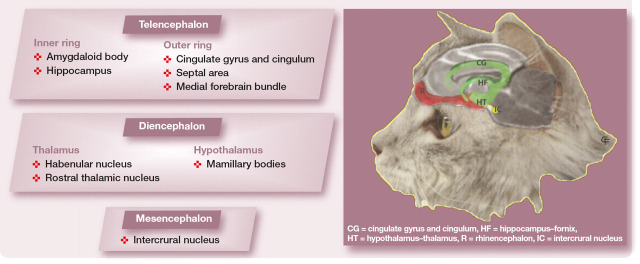
Before approaching the different situations that can potentially alter behaviour, it is important to consider the neuroanatomical structures that control behaviour in normal cats. These are all contained within the brain and are collectively known as the limbic system; limbus means border, and the limbic system refers to the anatomical arrangements of the telencephalic components of this system. 9 These components comprise two incomplete ring-like structures on the medial aspect of the cerebral hemispheres at their border with the diencephalon. The limbic system also has components in the diencephalon (thalamus and hypothalamus) and mesencephalon.
The intricacies and complexities of the limbic system are only partially understood. However, what is recognised is that the many areas that constitute the system, and the numerous connections that exist between them, mean that a lesion almost anywhere within the brain can affect the normal function of the limbic system, leading to abnormal behaviour. This system receives and assimilates impulses arriving from the olfactory, optic, auditory, exteroceptive (all the afferent impulses from the body surface) and interoceptive (all the afferent impulses from the viscera) sensory systems and then projects predominantly to the hypothalamus and caudal brainstem. In this way the limbic system controls the psychic and motor aspects of behaviour.
Learning, memory and emotions (eg, fear, anxiety and depression) are some of the functions regulated by the limbic system. Therefore, changes in a normal cat's habits and attitudes are likely to be seen with lesions in the forebrain, involving the limbic system components. Consequently, cats with limbic system disease may experience any number of the following signs: changes in personality, dementia, lethargy, listlessness, aggression, failure to recognise the owners or familiar environments, loss of learned habits, inappropriate house soiling, compulsive behaviours (eg, aimless pacing), restlessness, polyphagia, pica and anorexia.
Major Structures of the Limbic System
Common behavioural complaints
The most common behavioural problems in cats are inappropriate house soiling, aggression and changes in mentation/personality. 8,10,11 These signs are usually non-specific, occurring alone or in combination with other signs.
Some behavioural abnormalities may appear more obviously neurological. For example, seizures in cats, unlike dogs, are often of the ‘psychomotor’ type and the owner can misinterpret them as ‘compulsive behaviour’. Seizures may manifest as episodic aggression, disorientation, fear or anxiety; cats may suddenly hide or run in the absence of any specific trigger. A thorough history is very useful to establish the nature of such episodes. For instance, the paroxysmal nature of the event, combined with the possible presence of prodromal or post-ictal changes, is usually suggestive of a neurological condition. Video footage is frequently invaluable in such cases. A specific behavioural or paroxysmal disorder may only be triggered by particular environments or situations. The recognition of a behavioural abnormality is based purely on the owner's account and perception of the episode and so psychomotor seizures, for example, may go undiagnosed without the benefit of a video.
One field of particular interest currently comprises the compulsive disorders. 11
Compulsive disorders
Compulsive disorders are defined as repetitive or sustained abnormal behaviours performed out of context, and may constitute a neurological or non-neurological problem. They can be categorised as locomotory, oral or ingestive, aggressive, vocalisation or hallucinatory. Controversy surrounds their origin — that is, whether they represent seizures or are primary behavioural disturbances equivalent to the stereotypical behaviour of livestock and zoo animals and to the obsessive—compulsive disorders of humans. Manifestations in cats of compulsive disorders include agitation, circling, overgrooming (‘psychogenic dermatitis’), pica, self-directed aggression (eg, attacking the tail or ‘tail chasing’), persistent vocalising, avoiding imaginary objects and staring at shadows. However, a clear differentiation between compulsive disorders, pure behavioural disorders, seizures and other paroxysmal disorders mimicking seizures is generally challenging. Therefore, a detailed history and thorough physical and neurological examination are mandatory in order to achieve a definitive diagnosis.
Clinical work-up
Physical examination should rule out common feline non-neurological diseases that can result in behavioural disturbances, 8,10,11 such as renal insufficiency/failure, FLUTD, hyperthyroidism and diabetes mellitus (Table 3). For example:
TABLE 3.
Common behavioural changes and some of the more likely underlying diseases
| Behavioural complaint | Underlying disorder |
|---|---|
|
| |
| Inappropriate elimination | Degenerative/developmental: ectopic ureter Acquired: intraluminal obstruction — urolithiasis, polyps Metabolic/endocrine: diabetes mellitus, renal insufficiency/failure, hypercalcaemia, hypokalaemia, hyperadrenocorticism, hyperthyroidism, hypoadrenocorticism, hepatic insufficiency, primary polydipsia Inflammatory: prostatitis, vaginitis, cystitis/FLUTD |
| Aggression |
|
| Depression, sleepiness, listlessness |
|
| Abnormal cognition (eg, dementia, inability to learn, compulsive behaviour) |
|
| Non-specific fear and anxiety |
|
FLUTD = feline lower urinary tract disease, HE = hepatic encephalopathy
Inappropriate elimination Urolithiasis, cystitis, FLUTD, pyometra, diabetes mellitus and renal insufficiency/failure are common causes of inappropriate elimination in the cat.
Altered mentation Severe hepatic or uraemic encephalopathy, and thiamine or taurine deficiencies can cause varying degrees of mentation changes such as depression, listlessness and disorientation
Aggression Hyperthyroidism and pain (eg, due to arthritis) can result in aggressive behaviour. Hyperthyroidism has also been associated with manic behaviours and inappetence/anorexia. Recently, congenital hypothyroidism has been associated with mental retardation and seizures in two kittens, 12 although a definitive correlation between the thyroid hormone deficiency and the seizures could not be established. Deficiencies in thyroid hormone in children lead to abnormal brain development with concomitant deficits in behaviour, locomotor ability, speech, hearing and cognition. These functions may be partially caused by interactions between thyroid hormones, acetylcholine, nerve growth factor and hippocampal function. Hypertension, either primary or secondary to hyperthyroidism, renal failure or diabetes mellitus, can also cause behavioural changes such as disorientation, dullness and aggression.
Neurological examination
The neurological examination should focus primarily on evaluation of the intracranial component of the central nervous system. Neurological assessment in cats is not uncommonly limited by their non-cooperative nature. As a result, the ‘hands-off’ examination is very useful and may be the only thing we can rely on. 4
As mentioned, a cat with behavioural changes as a consequence of a lesion in the limbic system is very likely to experience forebrain signs (see box below). The following aspects of the neurological examination are, therefore, of particular importance:
Mentation This may be altered, resulting in varying degrees of depression and disorientation.
Gait evaluation Compulsive pacing, head pressing and/or circling may occur (see video clip, doi:10.1016/j.jfms.2011.09.007). The majority of cats with a forebrain lesion circle towards the affected side.
Postural reactions The hopping response is probably the most useful test of proprioception in cats but proprioceptive positioning can also be assessed. If the postural reactions are abnormal it is very likely that the cat has a neurological problem; however, a normal response does not rule out an underlying brain disorder.
Cranial nerve examination Vision may be affected partially or completely, unilaterally or bilaterally (see ‘Blindness’ section above). The menace response, despite not always being reliable in cats, is usually depressed, either with or without obvious visual deficits.
Forebrain lesions
Cats with unilateral or bilateral blindness may present initially with changes in behaviour (eg, reluctance to jump, unwillingness to go outside). The owner may not appreciate the visual deficits and interpret the associated clinical signs, such as depression and decreased activity, as being behavioural problems.
Further diagnostics
Should the physical and neurological examination reveal abnormalities suggestive of either a metabolic or intracranial disease, further tests must be done. Routine haematology, biochemistry and urinalysis are frequently sufficient in the case of metabolic disease, although further endocrine testing (eg, total serum thyroxine and thyroid-stimulating hormone, and ACTH stimulation test) may be necessary in selected cases. Where there is a suspicion of intracranial disease, brain MRI has become the imaging modality of choice. The advent of MRI has allowed detection of many brain disorders and is often complemented by cerebrospinal fluid analysis to further define an intracranial lesion.
Behavioural changes with a neurological origin
Some of the more common intracranial conditions that may potentially alter a cat's behaviour and/or vision are summarised in Table 2. A more extensive review of many of these diseases is found within the accompanying articles in this current neurology-themed issue of the Journal of Feline Medicine and Surgery, as well as in the earlier neurology-themed issue, published in May 2009 (vol 11, issue 5).
A disease process that is becoming more widely recognised and is the subject of ongoing research is cognitive dysfunction syndrome (CDS), which is briefly discussed below.
Cognitive dysfunction syndrome
CDS describes an age-related decline in cognitive abilities that is characterised by behavioural changes unattributable to other medical conditions. 13 This syndrome has also been described in dogs and shares many similarities with Alzheimer's disease in humans. It is generally accepted that cognitive and motor performance deteriorate with age in cats and a decline in visual and auditory ability has also been reported, especially in cats over 10 years of age. 13 The most commonly seen behavioural changes in cats with CDS include spatial or temporal disorientation, altered interaction with owners, changes in sleep—wake cycles and inappropriate urination, defecation and vocalisation. 13 These signs have been described by the acronym ‘DISHA’, which refers to ‘Disorientation’; ‘Interactions’ (eg, alterations in social interactions with people or other pets); ‘Sleep—wake cycle’ changes; ‘House soiling’ and deficits in other learned behaviours; and changes in ‘Activity’ levels (which could be a decrease in activity, or an increase in activity including repetitive behaviours and aimless wandering). 10,14
Cognitive dysfunction syndrome describes an age-related decline in cognitive abilities that is characterised by behavioural changes unattributable to other medical conditions — most commonly, spatial or temporal disorientation, altered interaction with owners, changes in sleep—wake cycles and inappropriate urination, defecation and vocalisation.
In a study evaluating 154 cats aged between 11 and 21 years, the overall percentage of cats displaying geriatric onset behavioural changes was 44% (67/154). Nineteen of these cats had concomitant medical conditions, leaving 36% (48/135) with behavioural changes not attributable to underlying disease. Fifty per cent (23/46) of cats aged over 15 years had signs consistent with CDS, whereas only 28% (25/89) of cats aged 11–14 years had behavioural abnormalities. The most common behavioural change seen in the 11- to 14-year old age group was an alteration in social interactions with people or other pets. 13
The pathophysiology of feline brain ageing still requires considerable study. It may involve a number of different mechanisms, occurring either alone or in combination. 13,14 Hypoxia (from primary vascular changes or arising secondarily to cardiac failure, systemic hypertension or anaemia), free radical production and extracellular β-amyloid deposition with senile plaque formation are all possible co-factors that lead to a reduction in the number of functioning neurons. Changes observed include generalised gliosis, degeneration of white matter, demyelination, neuroaxonal degeneration, a reduction in brain size, an increase in ventricular size and meningeal fibrosis (involving vascular and perivascular changes, with or without calcification). Moreover, functional changes including depletion of catecholamine neurotransmitters (norepinephrine, serotonin and dopamine), a decline in the cholinergic system, an increase in monoamine oxidase B activity and a reduction in endogenous antioxidants may also be involved. However, while the brains of older cats show many of these changes it is not yet clear which of them are directly associated with CDS.
Treatment of CDS
Treatment currently centres on diets enriched with antioxidants and other supportive compounds (eg, vitamin E, β-carotene, l-carnitine, omega-3 fatty acids) combined with environmental stimulation (eg, toys, company, interaction, food-hunting games) and drugs such as cholinesterase inhibitors, selegiline, propentofylline and non-steroidal anti-inflammatory medications. Preliminary results in cats, and evidence extrapolated from dogs, demonstrates a potential for dietary manipulation and environmental stimulation to improve the clinical signs and slow the decline associated with CDS. 13,14
In the absence of an obvious metabolic and/or neurological condition a primary behavioural problem should be suspected and treated.
Primary behavioural problems
In the absence of an obvious metabolic and/or neurological condition a primary behavioural problem should be suspected and treated. Specialists in veterinary behaviour are now widely available to provide pets with the best diagnostic approach and treatment options.
The therapeutic approach usually consists of behavioural corrective therapy combined, in difficult cases, with medical treatment. 15 The behavioural therapy is usually tailored to the individual family and patient's needs, and is based on subjective criteria such as historical behavioural information and specific situational details and other circumstances associated with the abnormal behaviour, as well as the medical history of the patient. This behavioural therapy requires close cooperation between the veterinarian and the owner, and the owner and the cat. It can, therefore, be very time-consuming and challenging.
In the past decade, knowledge of pharmacological management in veterinary behavioural medicine has expanded significantly in the light of developments in human behavioural medicine. The focus has been to understand how behavioural drugs can be used to reduce abnormal behaviours and help to manage underlying disease. Because there are so few drugs currently registered for behavioural disorders in veterinary medicine, veterinarians continue to rely on human-labelled drugs to treat these problems.
Behavioural drugs
Behavioural drugs act either as stimulators (agonists) or blockers (antagonists) of neurotransmitter receptors or as inhibitors of regulatory enzymes. Many of these drugs affect the monoamine neurotransmitters serotonin (5-hydroxytryptamine [5-HT]), norepinephrine (NE) and dopamine (DA), as well as acetylcholine (ACh), glutamate and gamma-aminobutyric acid (GABA) receptors, among others. Some of the most commonly used drugs are benzodiazepines, tricyclic antidepressants (eg, amitriptyline, imipramine), selective serotonin reuptake inhibitors (eg, fluoxetine) and monoamine oxidase inhibitors (eg, selegiline). Anticonvulsants can also be used for this purpose on occasion.
KEY POINTS
Blindness can be the result of central and peripheral pathway disorders; these disorders may be the consequence of metabolic, ophthalmic or neurological disease.
Behavioural changes can arise secondarily to sensory deficits (including visual, olfactory and auditory) or may result from metabolic, neurological or primary behavioural disease.
Anatomical structures involved in behaviour and vision are mainly located within the forebrain. Thus intracranial lesions will frequently affect both systems.
Video footage can help in the diagnosis of some of the more unusual behavioural and paroxysmal problems in cats.
Hypertension and hyperthyroidism are common systemic diseases causing derangements in behaviour and vision.
The prognosis for the resolution of blindness or behavioural changes is directly related to the underlying cause and available therapeutic options.
Biography

References
- 1. De Lahunta A, Glass E. Visual system. In: Veterinary neuroanatomy and clinical neurology. St Louis, Mosby: Saunders, 2009: 389–432. [Google Scholar]
- 2. Nell B, Suchy A. ‘D-shaped’ and ‘reverse-Dshaped’ pupil in a cat with lymphosarcoma. Vet Ophthalmol 1998; 1: 53–56. [DOI] [PubMed] [Google Scholar]
- 3. Sherman SM, Guillery RW, Kaas JH, et al. Behavioral, electrophysiological and morphological studies of binocular competition in the development of the geniculo-cortical pathways of cats. J Comp Neurol 1974; 158: 1–18. [DOI] [PubMed] [Google Scholar]
- 4. Garosi L. Neurological examination of the cat: how to get started. J Feline Med Surg 2009; 11: 340–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jurk IR, Thibodeau MS, Whitney K, et al. Acute vision loss after general anesthesia in a cat. Vet Ophthalmol 2001; 2: 155–58. [DOI] [PubMed] [Google Scholar]
- 6. Palmer AC, Walker RG. The neuropathological effects of cardiac arrest in animals: a study of five cases. J Small Anim Pract 1970; 11: 779–90. [DOI] [PubMed] [Google Scholar]
- 7. Panarello GL, Dewey CW, Barone G, et al. Magnetic resonance imaging of two suspected cases of global brain ischemia. J Vet Emerg Crit Care 2004; 14: 269–77. [Google Scholar]
- 8. Overall KL. Medical differentials with potential behavioral manifestations. Vet Clin North Am Small Anim Pract 2003; 33: 213–29. [DOI] [PubMed] [Google Scholar]
- 9. De Lahunta A, Glass E. Nonolfactory rhinencephalon: limbic system. In: Veterinary neuroanatomy and clinical neurology. St Louis, Mosby: Saunders, 2009: 448–53. [Google Scholar]
- 10. Seibert LM, Landsberg GM. Diagnosis and management of patients presenting with behavior problems. Vet Clin North Am Small Anim Pract 2008; 38: 937–950. [DOI] [PubMed] [Google Scholar]
- 11. Luescher AU. Diagnosis and management of compulsive disorders in dogs and cats. Vet Clin North Am Small Anim Pract 2003; 33: 253–67. [DOI] [PubMed] [Google Scholar]
- 12. Traas AM, Abbott BL, French A, Giger U. Congenital thyroid hypoplasia and seizures in 2 littermate kittens. J Vet Intern Med 2008; 22: 1427–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gunn-Moore D, Moffat K, Christie LA, et al. Cognitive dysfunction and the neurobiology of ageing in cats. J Small Anim Pract 2007; 48: 546–53. [DOI] [PubMed] [Google Scholar]
- 14. Landsberg G, Denenberg S, Araujo J. Cognitive dysfunction in cats: a syndrome we used to dismiss as ‘old age’. J Feline Med Surg 2010; 12: 837–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Simpson BS, Papich MG. Pharmacologic management in veterinary behavioral medicine. Vet Clin North Am Small Anim Pract 2003; 33: 365–404. [DOI] [PubMed] [Google Scholar]