Abstract
Isocitrate dehydrogenase (IDH) enzymes catalyze the decarboxylation of isocitrate to alpha-ketoglutarate (αKG). IDH1/2 mutations preferentially convert αKG to R-2-hydroxyglutarate (R2HG), resulting in R2HG accumulation in tumor tissues. We investigated circulating 2-hydroxyglutate (2HG) as potential biomarkers for patients with IDH-mutant (IDHmt) cholangiocarcinoma (CCA).
R2HG and S-2-hydroxyglutarate (S2HG) levels in blood and tumor tissues were analyzed in a discovery cohort of patients with IDHmt glioma and CCA. Results were validated in cohorts of patients with CCA and clear-cell renal cell carcinoma.
The R2HG/S2HG ratio (rRS) was significantly elevated in tumor tissues, but not in blood for patients with IDHmt glioma, while circulating rRS was elevated in patients with IDHmt CCA. There were overlap distributions of circulating R2HG and total 2HG in patients with both IDHmt and wild-type (IDHwt) CCA, while there was minimal overlap in rRS values between patients with IDHmt and IDHwt CCA. Using the rRS cut-off value of 1.5, the sensitivity of rRS was 90% and specificity was 96.8%.
Circulating rRS is significantly increased in patients with IDHmt CCA compare with patients with IDHwt CCA. Circulating rRS is a sensitive and specific surrogate biomarker for IDH1/2 mutations in CCA. It can potentially be used as a tool for monitoring IDH-targeted therapy.
Introduction
Cholangiocarcinoma (CCA) is a heterogeneous group of hepatobiliary tumors that have a poor prognosis. Advanced CCA is traditionally subclassified by anatomic sites into intrahepatic cholangiocarcinoma (iCCA) and extrahepatic cholangiocarcinoma (eCCA). Recently, genomic advances have partially unveiled the complex molecular landscape of CCA, shedding new light on novel therapeutic opportunities and ushering in the era of precision oncology for 40%–55% of patients with CCA (1). Among these putatively actionable alterations, mutations in the isocitrate dehydrogenase (IDH1/2) genes are detected in 15% iCCA and <5% of eCCA (2–4). IDH1/2 mutations are also seen in other cancers including low-grade glioma (80%), acute myeloid leukemia (20%), and central chondrosarcoma (80%) (5, 6). The majority of IDH1 and IDH2 point mutations occur at residues arginine 132 (R132) or 172 (R172), respectively. IDH is an essential enzyme in the tricarboxylic acid cycle that catalyzes the decarboxylation of isocitrate to alpha-ketoglutarate (αKG) (6–8). However, IDH1/2 mutations preferentially convert αKG to R-2-hydroxyglutarate (R2HG) (9, 10). The aberrant R2HG production from IDH1/2 mutations results in R2HG accumulation, and its concentration in IDH-mutant (IDHmt) tumor tissues can reach 5–30 mmol/L, far higher than its physiologic concentrations(≈100 μmol/L) (11). Interestingly, the S-enantiomer (S2HG) concentrations remain low in both IDHmt and wild-type cancers.
Because 2HG is a membrane-diffusible small molecule, multiple attempts have been undertaken to explore the feasibility of circulating total 2-hydroxyglutarate (t2HG) or R2HG concentrations as alternative diagnostic tools for identifying IDH1/2 mutations in various IDHmt malignancies. Studies have demonstrated elevated levels of circulating t2HG and/or R2HG in IDHmt cancers, including CCA (12–20). We previously reported that tissue ratios of R2HG over S2HG (rRS) are a more sensitive biomarker for IDH1/2 mutations in patients with glioma than R2HG (21). In this study, we investigated circulating R2HG, t2HG, and rRS as potential biomarkers for IDH1/2 mutations in patients with CCA.
Materials and Methods
Tissue and blood samples were collected from patients who were participating in studies approved by the Research Ethics Board at University Health Network, Toronto, Canada. Written informed consent was obtained from each patient before biospecimen collection. These studies were conducted in accordance with the Declaration of Helsinki.
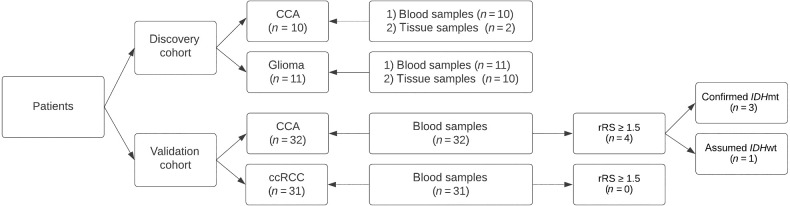
The study consisted of two cohorts of patients (Fig. 1). The discovery cohort comprised of patients with low-grade glioma or metastatic CCA. These patients were known to be IDHmt. The presence of IDH1/2 mutations was determined via either IHC for patients with glioma or next-generation sequencing for patients with CCA as a part of standard clinical care. Matched tissue and blood samples were collected where available from these patients.
Figure 1.
Study flow diagram. CCA: Cholangiocarcinoma; ccRCC: clear-cell renal cell carcinoma; 2HG: 2-Hydroxylutarate; rRS: ratio of R2HG/S2HG; IDHmt: IDH mutated; IDHwt: IDH wild type.
The validation cohort consisted of a second group of patients with metastatic CCA, whose blood samples were collected as a part of institutional biobanking initiatives. The mutational status of IDH1/2 in this group of patients with CCA was unknown except for one patient who was known to be IDHmt based on testing as part of routine clinical care. For patients who were suspected of harboring IDH1/2 mutations based on the elevated circulating rRS results, mutational analysis using circulating tumor DNA (ctDNA) was performed in a Clinical Laboratory Improvement Amendments–certified laboratory. In addition, a group of patients with clear-cell renal cell carcinoma (ccRCC) was included as a control group because IDH1/2 mutations have not been reported in the ccRCC population.
Tissue and blood samples collected were analyzed for R2HG and S2HG using a validated high-performance liquid chromatography (HPLC) tandem mass spectrometry method as reported previously (21).
Summary statistics were presented for R2HG, S2HG, t2HG, and rRS. The t2HG (t2HG = R2HG + S2HG) and rRS (rRS = R2HG/S2HG) values were calculated on the basis of measured levels of S2HG and R2HG. R2HG, S2HG, t2HG, and rRS were compared using t tests or one-way ANOVA between patients with glioma and CCA, between tissue and circulating 2HGs, or among cohorts using Prism (Version 9.5.1, GraphPad Software). Results were considered statistically significant if P ≤ 0.05.
Data availability
The data generated in this study are available upon request from the corresponding author.
Results
In the discovery cohort, a total of 21 patients with IDHmt tumors were included (glioma = 11, CCA = 10). Blood samples were available for all 21 patients, while sufficient tissue samples were available for 10 patients with glioma but only 2 patients with CCA. The validation cohort included 32 patients with CCA. There were no significant differences in demographic characteristics between patients with CCA enrolled in the discovery and validation cohorts (Table 1).
Table 1.
Characteristics of patients across cohorts.
| Characteristic | Discovery cohort | Validation cohort | ||
|---|---|---|---|---|
| Histology | Glioma | CCA | CCA | ccRCC |
| Number of patients | 11 | 10 | 32 | 31 |
| Sex, male (%) | 8 (73%) | 5 (50%) | 17(53%) | 26 (84%) |
| Age, years | ||||
| Median (range) | 42.0 (23.2–66.6) | 63.7 (48.0–78.9) | 64.5 (42.3–78.1) | 60 (30.0–81.0) |
Abbreviations: CCA: Cholangiocarcinoma; ccRCC: clear cell renal cell carcinoma.
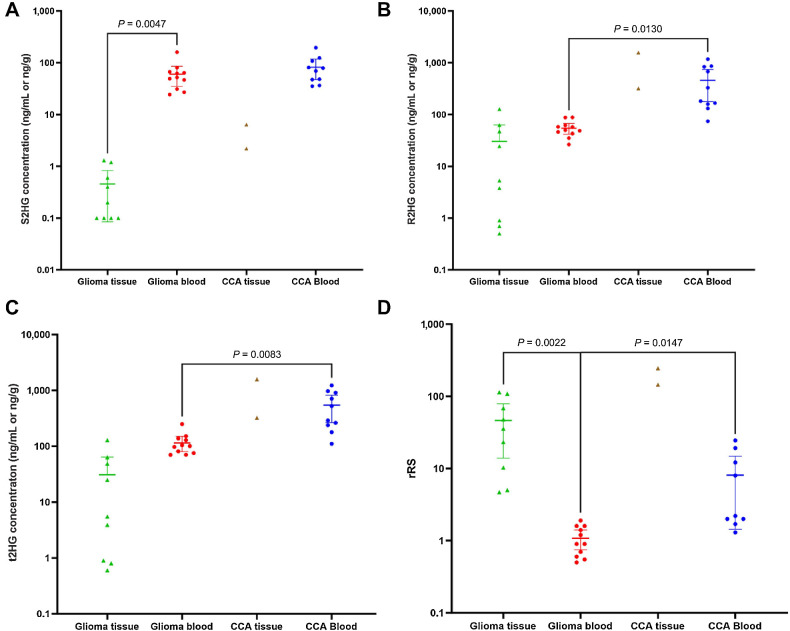
In patients with IDHmt glioma, S2HG levels were significantly lower in tumor tissues than in the blood, while R2HG levels were not statistically different (Table 2; Fig. 2). As a result, rRS was significantly higher in tumor tissue than in blood (46.4 ± 42.3 vs. 1.1 ± 0.5, P = 0.002). Because of limited tissue availability for patients with CCA, comparisons between tissue and blood 2HG levels were not performed. For 2 patients with CCA with sufficient tumor tissues for analysis, their tissue rRS levels were 144.8 and 244.9, respectively. Comparing patients with glioma and patients with CCA, circulating R2HG was significantly higher in patients with CCA while there was no difference seen in S2HG (Fig. 2). Consequently, circulating t2HG and rRS were significantly higher in patients with CCA than those in patients with glioma.
Table 2.
Tissue and circulating S2HG, R2HG, t2HG, and rRS mean levels for patients with glioma and CCA in the discovery cohort.
| Glioma | Cholangiocarcinoma | ||||
|---|---|---|---|---|---|
| Biomarkers | Serum (ng/mL) (n = 11) | Tissue (ng/g) (n = 10) | P value | Serum (ng/mL) (n = 10) | Tissue (ng/g) (n = 2) |
| S2HG | 60.3 ± 37.4 | 0.4 ± 0.5 | 0.005 | 82.3 ± 49.4 | 4.3 ± 3.0 |
| R2HG | 54.7 ± 19.3 | 30.3 ± 42.9 | NS | 458.8 ± 392.9 | 945.0 ± 883.9 |
| t2HG | 114.9 ± 52.1 | 30.7 ± 43.2 | NS | 541.0 ± 338.8 | 949.3 ± 886.9 |
| rRS | 1.1 ± 0.5 | 46.4 ± 42.3 | 0.002 | 7.6 ± 8.3 | 194.9 ± 70.8 |
Abbreviations: R2HG, R-2-hydroxyglutarate; rRS, ratio of R2HG/S2HG; S2HG, S-2-hydroxyglutarate; t2HG, total of R2HG+S2HG.
Figure 2.
S2HG (A), R2HG (B), t2HG (C), and rRS (D) in tissue and blood samples from the discovery cohort. S2HG: S-2-hydroxyglutarate; R2HG: R-2-hydroxyglutarate; t2HG: total of R2HG+S2HG; rRS: ratio of R2HG/S2HG. Y-axis is in logarithmic scale.
Among 32 patients with CCA in the validation cohort, 1 patient (Patient 460) was known to harbor IDH1R132C mutation (Table 3). Circulating 2HG analysis revealed additional 2 patients with abnormally high R2HG and rRS levels (Patients 376 and 468).
Table 3.
Circulating R2HG, S2HG, t2HG, and rRS for patients with CCA and ccRCC in the validation cohort.
| Characteristics | S2HG (ng/mL) | R2HG (ng/mL) | t2HG (ng/mL) | rRS |
|---|---|---|---|---|
| All patients with CCA (n = 32) | 166.1 ± 74.4 | 316.8 ± 625.1 | 482.9 ± 654.6 | 1.7 ± 2.9 |
| Mean ± SD (range) | (79.7–356) | (67.4—2,570) | (148.8–2,747) | (0.5–14.5) |
| CCA with IDH1R132C mutations (n = 3) | ||||
| Patient 376 | 242 | 2,290 | 2,532 | 9.5 |
| Patient 468 | 177 | 2,570 | 2,747 | 14.5 |
| Patient 460 | 324 | 1,730 | 2,054 | 5.3 |
| Mean ± SD (range) | 247.7 ± 73.7 | 2196.7 ± 427.7 | 2444.3 ± 354.7 | 9.8 ± 4.6 |
| (177–324) | (1,730–2,570) | (2,054–2,747) | (5.3–14.5) | |
| IDH wild-type CCA (n = 29) | ||||
| Mean ± SD (range) | 157.7 ± 70.4 | 122.3 ± 41.4 | 280 ±103 | 0.8 ± 0.2 |
| (79.7–356) | (67.4–226) | (148.8–538) | (0.5–1.6) | |
| All patients with ccRCC (n = 31) | 89.0 ± 70.9 | 60.2 ± 19.8 | 149.2 ± 85.4 | 0.8 ± 0.3 |
| Mean ± SD (range) | (35.1–365) | (34.7–124) | (72.1–451.2) | (0.2–1.5) |
Abbreviations: R2HG, R-2-hydroxyglutarate; rRS, ratio of R2HG/S2H; S2HG, S-2-hydroxyglutarate; t2HG, total of R2HG+S2HG.
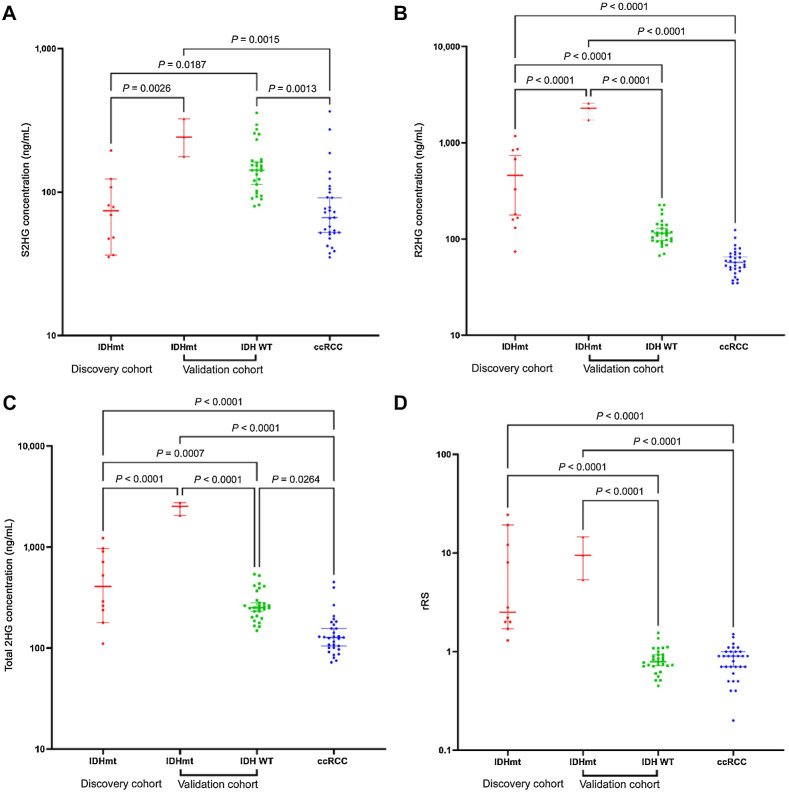
The distribution of S2HG, R2HG, and t2HG was wide in both patients with glioma and patients with CCA (Figs. 2 and 3). Although circulating R2HG and t2HG were significantly higher in patients with IDHmt CCA than those in IDHwt patients, there was considerable overlap in R2HG and t2HG concentrations in these patients. However, the circulating rRS distributed tightly around 0.8 ± 0.2 (range: 0.45–1.55) in IDHwt patients (Table 3). For the cohort of patients with ccRCC, the mean rRS was 0.8 ± 0.3, ranging from 0.2 to 1.5.
Figure 3.
Circulating S2HG (A), R2HG (B), t2HG (C), and rRS (D) for patients with CCA in the discovery and validation cohorts. S2HG: S-2-hydroxyglutarate; R2HG: R-2-hydroxyglutarate; t2HG: total of R2HG+S2HG; rRS: ratio of R2HG/S2HG. Y-axis is in logarithmic scale.
rRS was significantly higher among patients with IDHmt CCA in both discovery and validation cohorts than that for patients with IDHwt CCA. In the discovery cohort, only 1 patient with IDHmt CCA had a rRS value lower than 1.5 (1.3), while only 1 IDHwt patient in the validation cohort had a rRS value higher than 1.5 (1.55). In addition to Patient 460, 2 patients with CCA in the validation cohort had rRS values above 1.5 (Table 3). Subsequent ctDNA analysis confirmed that both patients harbored IDH1R132C mutations. Using a cut-off rRS value of 1.5, the sensitivity of rRS for predicting IDH1/2 mutation status was 90%, and the specificity was 96.8%.
Discussion
CCA is characterized by overlapping, low-penetrance genomic alterations that span diverse signaling pathways (22). Identification of IDH1/2 mutations has enabled targeted therapy in a subset of patients with CCA. Numerous agents targeting IDHmt cancers, such as ivosidenib, vorasidenib, ceralasertib, olutasidenib, enasidenib, and BAY1436032, have either received regulatory approvals or are in various stages of clinical development (23–25). The ClarIDHy trial evaluated ivosidenib in patients with refractory IDHmt CCA (24). Ivosidenib provides a modest, but statistically significant improvement in progression-free survival of 1.3 months, compared with placebo (24).
Obtaining tumor tissue samples for molecular profiling remains a clinical challenge in patients with CCA. Some patients are diagnosed on the basis of bile duct brushing during endoscopic retrograde cholangiopancreatography. Even with core biopsies, there is a considerable failure rate in yielding sufficient tumor DNA content for accurate pathologic diagnosis or comprehensive molecular profiling (26, 27). This limitation can be attributed to the challenging characteristics of CCA, including its desmoplastic and necrotic nature, as well as the presence of intratumoral heterogeneity (28–30).
The intriguing aspect of IDHmt tumors is the aberrant production and accumulation of the circulating oncometabolite 2HG, specifically R2HG rather than S2HG (7, 9–11, 31). Under physiologic conditions, R2HG and S2HG exist at low but equal levels. Both are small molecules that can readily diffuse across cellular membranes (11). There has been a significant interest in the evaluation of circulating 2HG as a biomarker for IDH1/2 mutations in various hematologic and solid malignancies (12–20, 32). Janin and colleagues found that elevated serum 2HG concentrations reliably diagnosed IDHmt acute myeloid leukemia, achieving 100% sensitivity and 79% specificity when compared with wild-type cases (20). Lombardi and colleagues showed urinary 2HG concentrations were not elevated in patients with IDHmt glioma (13). Similarly, Capper and colleagues concluded that circulating 2HG were not elevated in patients with IDHmt glioma (14). For other solid tumors, circulating 2HG concentrations were reported to be a surrogate biomarker of IDHmt (12, 15, 16). In addition, circulating 2HG levels were shown to correlate with tumor burden in patients with IDHmt CCA (16).
One possible explanation for the high levels of circulating 2HG levels in IDHmt CCA, but not in patients with glioma, is due to the relative volumes of the circulatory system and brain tumor lesions. Any 2HG released from glioma lesions is diluted, making it harder to detect elevated 2HG in the peripheral blood of these patients.
We previously demonstrated that tissue rRS represents a highly sensitive and specific biomarker for IDH1/2 mutations in glioma, compared with R2HG or t2HG levels (21). The absolute levels of R2HG and/or t2HG are influenced by tumor volumes, cellularity and different point mutations in the IDH1/2 genes. These limitations can be mitigated by using S2HG as a readily available internal standard because R2HG and S2HG share the same physiochemical properties except chirality. As demonstrated in this study, there is considerable overlap of circulating R2HG or t2HG between patients with IDHwt and IDHmt CCA, while there is minimal overlap in rRS between patients with IDHwt and IDHmt CCA. Therefore, the circulating rRS could offer a more sensitive and specific biomarker for identifying IDH1/2 mutations in patients with CCA, particularly in cases where traditional tissue-based methods are not feasible or practical.
The majority of previous studies on circulating 2HG only measured t2HG. We employed an analytic method that can quantitate R2HG and S2HG enantiomers separately, enabling the interpretation of rRS as a biomarker for IDH1/2 mutations in CCA. Our discovery cohort in this study is limited by the small number; however, the difference between tissue and serum 2HG levels in patients with glioma and the elevated circulating rRS in patients with IDHmt CCA are striking. Only 2 patients with CCA in the validation cohort were selected for subsequent ctDNA analysis. This decision was made based on the cost of performing ctDNA analysis.
Recent advances in ctDNA technology have revolutionized genomic analysis by eliminating the need for tumor tissue samples. However, the analysis of circulating 2HG has advantages as it requires a small volume of blood (<0.5 mL) and it can be completed within 30 minutes (33, 34). The cost is also a fraction of the cost of ctDNA analysis. The ClarIDHy trial demonstrated that ivosidenib inhibited 2HG production and reduced circulating 2HG levels in responding patients (35, 36). Hence, circulating 2HG analysis represents a cost-effective method for serially monitoring responses to IDHmt targeted therapies.
Our results show that circulating R2HG, t2HG, and rRS are elevated in patients with IDHmt CCA, and rRS is a sensitive and specific biomarker for IDHmt, consistent with the biology of IDH1/2 mutations. The potential of circulating rRS as a biomarker for response to IDH1/2 targeted therapies should be incorporated in future studies of IDHmt targeting agents.
Acknowledgments
Funding is provided through the generous support of the Princess Margaret Cancer Center Foundation.
Authors' Disclosures
G.M. O'Kane reports personal fees from AstraZeneca, Servier, MSD, Incyte; and grants and personal fees from Roche outside the submitted work. W.P. Mason reports personal fees from Merck; grants and personal fees from Servier and Novocure; grants from Hoffman La Roche; and personal fees from Ont Therapeutics outside the submitted work. A.R. Hansen reports grants from Roche, GSK, Janssen, AstraZeneca, Novartis, Boeringher-Ingelheim, and Genetech; grants and other support from Pfizer, Merck/MSD, Eisai outside the submitted work. R.C. Grant reports grants from Pfizer; personal fees from AstraZeneca, Eisai, Incyte, Knight Therapeutics, Guardant Health, and Ipsen outside the submitted work. J.J. Knox reports personal fees from AstraZeneca, Incyte; grants and personal fees from Roche and Ipsen outside the submitted work. E.X. Chen reports personal fees from AstraZeneca, Eisai, Ipsen, Merck, Roche, GSK and Bayer; grants from AstraZeneca, Roche, Merck, GSK, Novartis, Janssen, BMS, Mirati outside the submitted work. No disclosures were reported by the other authors.
Authors' Contributions
C.L Lee: Conceptualization, data curation, formal analysis, investigation, visualization, writing–original draft, writing–review and editing. G.M. O'Kane: Data curation, writing–review and editing. W.P. Mason: Data curation, writing–review and editing. W.-j. Zhang: Formal analysis, writing–review and editing. P. Spiliopoulou: Data curation, writing–review and editing. A.R. Hansen: Data curation, writing–review and editing. R.C. Grant: Data curation, writing–review and editing. J.J. Knox: Data curation, writing–review and editing. T.L. Stockley: Formal analysis, writing–review and editing. G. Zadeh: Data curation, writing–review and editing. E.X. Chen: Conceptualization, resources, data curation, supervision, funding acquisition, visualization, project administration, writing–review and editing.
References
- 1. Mody K, Kasi PM, Yang J, Surapaneni PK, Bekaii-Saab T, Ahn DH, et al. Circulating tumor DNA profiling of advanced biliary tract cancers. JCO Precis Oncol 2019;3:1–9. [DOI] [PubMed] [Google Scholar]
- 2. Javle M, Bekaii-Saab T, Jain A, Wang Y, Kelley RK, Wang K, et al. Biliary cancer: utility of next-generation sequencing for clinical management. Cancer 2016;122:3838–47. [DOI] [PubMed] [Google Scholar]
- 3. Ross JS, Wang K, Catenacci DVT, Chmielecki J, Ali SM, Elvin JA, et al. Comprehensive genomic profiling of biliary tract cancers to reveal tumor-specific differences and genomic alterations. J Clin Oncol 33:3s, 2015. (suppl; abstr 231). [Google Scholar]
- 4. Valle JW, Lamarca A, Goyal L, Barriuso J, Zhu AX. New horizons for precision medicine in biliary tract cancers. Cancer Discov 2017;7:943–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dang L, Jin S, Su SM. IDH mutations in glioma and acute myeloid leukemia. Trends Mol Med 2010;16:387–97. [DOI] [PubMed] [Google Scholar]
- 6. Dang L, Yen K, Attar EC. IDH mutations in cancer and progress toward development of targeted therapeutics. Ann Oncol 2016;27:599–608. [DOI] [PubMed] [Google Scholar]
- 7. Ward PS, Thompson CB. Metabolic reprogramming: a cancer hallmark even warburg did not anticipate. Cancer Cell 2012;21:297–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, et al. IDH1 and IDH2 mutations in gliomas. N Engl J Med 2009;360:765–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cairns RA, Mak TW. Oncogenic isocitrate dehydrogenase mutations: mechanisms, models, and clinical opportunities. Cancer Discov 2013;3:730–41. [DOI] [PubMed] [Google Scholar]
- 10. Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM, et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature 2009;462:739–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dang L, Su SSM. Isocitrate dehydrogenase mutation and (R)-2-hydroxyglutarate: from basic discovery to therapeutics development. Annu Rev Biochem 2017;86:305–31. [DOI] [PubMed] [Google Scholar]
- 12. Fathi AT, Sadrzadeh H, Comander AH, Higgins MJ, Bardia A, Perry A, et al. Isocitrate dehydrogenase 1 (IDH1) mutation in breast adenocarcinoma is associated with elevated levels of serum and urine 2-hydroxyglutarate. Oncologist 2014;19:602–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lombardi G, Corona G, Bellu L, Puppa AD, Pambuku A, Fiduccia P, et al. Diagnostic value of plasma and urinary 2-hydroxyglutarate to identify patients with isocitrate dehydrogenase-mutated glioma. Oncologist 2015;20:562–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Capper D, Simon M, Langhans CD, Okun JG, Tonn JC, Weller M, et al. 2-Hydroxyglutarate concentration in serum from patients with gliomas does not correlate with IDH1/2 mutation status or tumor size. Int J Cancer 2012;131:766–8. [DOI] [PubMed] [Google Scholar]
- 15. Delahousse J, Verlingue L, Broutin S, Legoupil C, Touat M, Doucet L, et al. Circulating oncometabolite D-2-hydroxyglutarate enantiomer is a surrogate marker of isocitrate dehydrogenase–mutated intrahepatic cholangiocarcinomas. Eur J Cancer 2018;90:83–91. [DOI] [PubMed] [Google Scholar]
- 16. Borger DR, Goyal L, Yau T, Poon RT, Ancukiewicz M, Deshpande V, et al. Circulating oncometabolite 2-hydroxyglutarate is a potential surrogate biomarker in patients with isocitrate dehydrogenase-mutant intrahepatic cholangiocarcinoma. Clin Cancer Res 2014;20:1884–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Watanabe T, Nobusawa S, Kleihues P, Ohgaki H. IDH1 mutations are early events in the development of astrocytomas and oligodendrogliomas. Am J Pathol 2009;174:1149–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gross S, Cairns RA, Minden MD, Driggers EM, Bittinger MA, Jang HG, et al. Cancer-associated metabolite 2-hydroxyglutarate accumulates in acute myelogenous leukemia with isocitrate dehydrogenase 1 and 2 mutations. J Exp Med 2010;207:339–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fallah-Rad N, Bedard PL, Siu LL, Kamel-Reid S, Chow H, Weijiang Z, et al. Association of isocitrate dehydorgenase-1 (IDH-1) mutations with elevated oncometabolite 2-hydroxyglutarate (2HG) in advanced colorectal cancer. J Clin Oncol 34:4s, 2016. (suppl; abstr 627). [Google Scholar]
- 20. Janin M, Mylonas E, Saada V, Micol JB, Renneville A, Quivoron C, et al. Serum 2-hydroxyglutarate production in IDH1 - and IDH2 -mutated de novo acute myeloid leukemia: a study by the acute leukemia french association group. J Clin Oncol 2014;32:297–305. [DOI] [PubMed] [Google Scholar]
- 21. Sim HW, Nejad R, Zhang W, Nassiri F, Mason W, Aldape KD, et al. Tissue 2-hydroxyglutarate as a biomarker for Isocitrate Dehydrogenase mutations in gliomas. Clin Cancer Res 2019;25:3366–73. [DOI] [PubMed] [Google Scholar]
- 22. Lamarca A, Barriuso J, McNamara MG, Valle JW. Molecular targeted therapies: ready for “prime time” in biliary tract cancer. J Hepatol 2020;73:170–85. [DOI] [PubMed] [Google Scholar]
- 23. Rizzo A, Ricci AD, Brandi G. IDH inhibitors in advanced cholangiocarcinoma: another arrow in the quiver? Cancer Treat Res Commun 2021;27:100356. [DOI] [PubMed] [Google Scholar]
- 24. Abou-Alfa GK, Macarulla T, Javle MM, Kelley RK, Lubner SJ, Adeva J, et al. Ivosidenib in IDH1-mutant, chemotherapy-refractory cholangiocarcinoma (ClarIDHy): a multicentre, randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol 2020;21:796–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mellinghoff IK, Van Den Bent MJ, Blumenthal DT, Touat M, Peters KB, Clarke J, et al. Vorasidenib in IDH1- or IDH2-mutant low-grade glioma. N Engl J Med 2023;389:589–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dong LQ, Shi Y, Ma LJ, Yang LX, Wang XY, Zhang S, et al. Spatial and temporal clonal evolution of intrahepatic cholangiocarcinoma. J Hepatol 2018;69:89–98. [DOI] [PubMed] [Google Scholar]
- 27. Walter D, Döring C, Feldhahn M, Battke F, Hartmann S, Winkelmann R, et al. Intratumoral heterogeneity of intrahepatic cholangiocarcinoma. Oncotarget 2017;8:14957–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Berchuck JE, Facchinetti F, DiToro DF, Baiev I, Majeed U, Reyes S, et al. The clinical landscape of cell-free DNA alterations in 1,671 patients with advanced biliary tract cancer. Ann Oncol 2022;33:1269–83. [DOI] [PubMed] [Google Scholar]
- 29. McGranahan N, Swanton C. Clonal heterogeneity and tumor evolution: past, present, and the future. Cell 2017;168:613–28. [DOI] [PubMed] [Google Scholar]
- 30. Lamarca A, Kapacee Z, Breeze M, Bell C, Belcher D, Staiger H, et al. Molecular profiling in daily clinical practice: practicalities in advanced cholangiocarcinoma and other biliary tract cancers. J Clin Med 2020;9:2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ward PS, Cross JR, Lu C, Weigert O, Abel-Wahab O, Levine RL, et al. Identification of additional IDH mutations associated with oncometabolite R(-)-2-hydroxyglutarate production. Oncogene 2012;31:2491–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Golub D, Iyengar N, Dogra S, Wong T, Bready D, Tang K, et al. Mutant isocitrate dehydrogenase inhibitors as targeted cancer therapeutics. Front Oncol 2019;9:417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kanamori M, Maekawa M, Shibahara I, Saito R, Chonan M, Shimada M, et al. Rapid detection of mutation in isocitrate dehydrogenase 1 and 2 genes using mass spectrometry. Brain Tumor Pathol 2018;35:90–6. [DOI] [PubMed] [Google Scholar]
- 34. Kalinina J, Ahn J, Devi NS, Wang L, Li Y, Olson JJ, et al. Selective detection of the D-enantiomer of 2-hydroxyglutarate in the CSF of glioma patients with mutated isocitrate dehydrogenase. Clin Cancer Res 2016;22:6256–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fan B, Mellinghoff IK, Wen PY, Lowery MA, Goyal L, Tap WD, et al. Clinical pharmacokinetics and pharmacodynamics of ivosidenib, an oral, targeted inhibitor of mutant IDH1, in patients with advanced solid tumors. Invest New Drugs 2020;38:433–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fan B, Abou-Alfa GK, Zhu AX, Pandya SS, Jia H, Yin F, et al. Pharmacokinetics/pharmacodynamics (PK/PD) of ivosidenib in patients with mutant IDH1 advanced cholangiocarcinoma from the phase III ClarIDHy study. J Clin Oncol 38:4s, 2020. (suppl; abstr 539). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated in this study are available upon request from the corresponding author.