Abstract
Background
Worldwide there is an increasing demand for Hospital at Home as an alternative to hospital admission. Although there is a growing evidence base on the effectiveness and cost‐effectiveness of Hospital at Home, health service managers, health professionals and policy makers require evidence on how to implement and sustain these services on a wider scale.
Objectives
(1) To identify, appraise and synthesise qualitative research evidence on the factors that influence the implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home, from the perspective of multiple stakeholders, including policy makers, health service managers, health professionals, patients and patients’ caregivers.
(2) To explore how our synthesis findings relate to, and help to explain, the findings of the Cochrane intervention reviews of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home services.
Search methods
We searched MEDLINE, CINAHL, Global Index Medicus and Scopus until 17 November 2022. We also applied reference checking and citation searching to identify additional studies. We searched for studies in any language.
Selection criteria
We included qualitative studies and mixed‐methods studies with qualitative data collection and analysis methods examining the implementation of new or existing Hospital at Home services from the perspective of different stakeholders.
Data collection and analysis
Two authors independently selected the studies, extracted study characteristics and intervention components, assessed the methodological limitations using the Critical Appraisal Skills Checklist (CASP) and assessed the confidence in the findings using GRADE‐CERQual (Confidence in the Evidence from Reviews of Qualitative research). We applied thematic synthesis to synthesise the data across studies and identify factors that may influence the implementation of Hospital at Home.
Main results
From 7535 records identified from database searches and one identified from citation tracking, we included 52 qualitative studies exploring the implementation of Hospital at Home services (31 Early Discharge, 16 Admission Avoidance, 5 combined services), across 13 countries and from the perspectives of 662 service‐level staff (clinicians, managers), eight systems‐level staff (commissioners, insurers), 900 patients and 417 caregivers. Overall, we judged 40 studies as having minor methodological concerns and we judged 12 studies as having major concerns. Main concerns included data collection methods (e.g. not reporting a topic guide), data analysis methods (e.g. insufficient data to support findings) and not reporting ethical approval. Following synthesis, we identified 12 findings graded as high (n = 10) and moderate (n = 2) confidence and classified them into four themes: (1) development of stakeholder relationships and systems prior to implementation, (2) processes, resources and skills required for safe and effective implementation, (3) acceptability and caregiver impacts, and (4) sustainability of services.
Authors' conclusions
Implementing Admission Avoidance and Early Discharge Hospital at Home services requires early development of policies, stakeholder engagement, efficient admission processes, effective communication and a skilled workforce to safely and effectively implement person‐centred Hospital at Home, achieve acceptance by staff who refer patients to these services and ensure sustainability. Future research should focus on lower‐income country and rural settings, and the perspectives of systems‐level stakeholders, and explore the potential negative impact on caregivers, especially for Admission Avoidance Hospital at Home, as this service may become increasingly utilised to manage rising visits to emergency departments.
Keywords: Humans, Administrative Personnel, Checklist, Hospitalization, Hospitals, Patient Discharge
Plain language summary
Multiple perceptions about implementing hospital at home
Key messages
‐ When developing a Hospital at Home service, it is important to set up a straightforward process for healthcare professionals to refer patients. This includes producing clear guidelines that set out who the service is suitable for.
‐ Hospital at Home services need a trained workforce with skills to deliver safe and effective patient‐centred care in the home, with clear and consistent communication between staff, patients and caregivers.
‐ We propose a number of questions for use by healthcare professionals and managers when introducing new Hospital at Home services, or running existing services. The questions are intended to help plan for and implement Hospital at Home services and improve satisfaction and outcomes for staff, patients and caregivers.
What is Hospital at Home?
Hospital at Home provides hospital‐level care at home, for people who would otherwise be inpatients in hospital. One type of Hospital at Home is to avoid admission to hospital. This is called Admission Avoidance Hospital at Home. These services replace an admission to hospital, for people whose condition would normally need treatment in a hospital bed, for example for a flare‐up of a lung condition. Instead, a doctor can refer a patient they assess as being suitable to receive treatment for an illness in their own home (or the place where they usually live, including in residential care), for a limited time. Another type is called Early Discharge Hospital at Home. These services shorten the length of time people need to stay in hospital after being admitted as an inpatient, for example following surgery or treatment for an illness or condition. The care patients would usually receive from healthcare professionals in a hospital bed is instead provided in their home, and is not expected to compromise the quality of care.
What did we want to find out?
Our aim was to find out what is important when introducing, running and receiving care from Hospital at Home services. We wanted to explore a range of experiences of, and views on, Admission Avoidance and Early Discharge services. These might include things that managers want to know when planning to set up a Hospital at Home service, healthcare professionals’ views on working in a Hospital at Home service, what matters to patients who receive this type of care, or how family and caregivers experience Hospital at Home services for those they care for.
What did we do?
We searched for research that had explored experiences, attitudes or beliefs about Hospital at Home services from the perspectives of patients, caregivers, health professionals, managers and health funders. The studies addressed existing Hospital at Home services and those that were being set up, for people with a range of conditions, such as stroke, pneumonia or following surgery. The studies used interviews or focus groups to explore the views of people involved in delivering or receiving Hospital at Home services. We assessed and summarised the findings from each of the studies. We identified important findings across the studies, and then rated how confident we were in each finding. This confidence (or trust) depended on, for example, how much information relating to a particular finding had been provided in the studies.
What did we find?
We found 52 studies that explored Hospital at Home services, including 31 Early Discharge, 16 Admission Avoidance and five combined Early Discharge and Admission Avoidance services. These studies conducted interviews or focus groups with 662 healthcare staff, 900 patients, 417 caregivers and eight health funders.
In total, we identified 12 main findings after assessing all the studies. We grouped these findings as: (1) development of stakeholder relationships and systems prior to implementation, (2) processes, resources and skills required for safe and effective delivery, (3) acceptability and caregiver impacts and (4) sustainability of services. We are confident in most of our findings, but we are less confident in a few findings, mainly due to the small numbers of studies and interviews with health funders contributing to the review finding.
What are the limitations of the evidence?
All except one of the studies came from high‐income countries, and so our findings may not apply to low‐ and middle‐income countries. Some studies did not report all the information that might be useful. For example, services’ staffing and role types were not always included.
How up‐to‐date is this evidence?
The evidence is up‐to‐date to November 2022.
Summary of findings
Summary of findings 1. Summary of qualitative findings.
| Summary of review finding | GRADE‐CERQual assessment of confidence in the evidencea | Explanation of GRADE CERQual assessment | Studies contributing to the review finding |
| Theme 1. Development of stakeholder relationships and systems prior to implementation of Hospital at Home | |||
| Finding 1. Service level staff suggested early stakeholder engagement, including partnerships with third party service providers, were required to implement Hospital at Home. This was critical for implementing new services, overcoming regulatory requirements, building trust and ensuring referrals. | High | Minor concerns about adequacy. No or very minor concerns about methodological limitations, relevance and coherence. | Brody 2019; Chouliara 2014; Dinesen 2007; Fisher 2021; Gorbenko 2023; Hitch 2020; Kraut 2016; Lemelin 2007; Moule 2011; Sims 1997; Testa 2021 |
| Finding 2. For healthcare services planning to implement Hospital at Home, current systems need to integrate activity data and service costs. This allows healthcare services to collate total costs and savings to measure financial impact. This is important as policy makers, hospital executives and insurers from multiple‐payer settings require evidence about the financial impact of Hospital at Home to inform commissioning decisions. For multiple‐payer systems, financial impact and approval could be enhanced by including patients who contribute smaller financial benefits to the hospital if they are an inpatient. | Moderate | Moderate concerns about adequacy. Minor concerns about coherence. No or very minor concerns about methodological limitations and relevance. | Brody 2019; Chouliara 2014; Dismore 2019; Fisher 2021; Gorbenko 2023; Moule 2011 |
| Theme 2. Processes, resources and skills required to safely and effectively implement Hospital at Home | |||
| Finding 1. Safety concerns were expressed by all stakeholders, such as for patients going home alone in regard to pain management and their mobility, and staff expressed concern for their own safety due to home hazards, patient‐related factors and ergonomics. Patients were reassured about their safety with access to staff (including via phone) and equipment for safe monitoring. Timely delivery of appropriate equipment in the home alleviated some staff concerns. | High | Minor concerns about adequacy. No or very minor concerns about methodological limitations, relevance and coherence. | Dean 2007; Dismore 2019; Dow 2007b; Dubois 2001; Fisher 2021; Ko 2023; Kraut 2016; Kylén 2021; Lemelin 2007; Levine 2021; Lou 2017; Manning 2016; Nordin 2015; Sims 1997; Udesen 2022; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; Wallis 2022; Wang 2012; Wilson 2002 |
| Finding 2. Identifying patients using eligibility criteria and clinical judgement was challenging for referrers in the acute setting, especially in the start‐up phase of implementation. Services developed criteria to maintain responsiveness and manage capacity, and conducted teaching sessions to help acute staff to refer patients to Hospital at Home. Some services had concerns when staff were working at low capacity (not enough referrals), if staff were seeing patients that were either too ill, or did not need the higher level of care required for Hospital at Home. | High | Minor concerns about adequacy. No or very minor concerns about methodological limitations, relevance and coherence. | Andrade 2013; Brody 2019; Chouliara 2014; Dismore 2019; Fisher 2021; Gorbenko 2023; Kraut 2016; Lemelin 2007; Manning 2016; Moule 2011; Udesen 2022; Vaartio‐Rajalin 2020 |
| Finding 3. Leadership and co‐ordination from key champions, lead clinicians with medical responsibility and clinical accountability, managers with operational responsibility and other leaders were essential to provide high‐quality care. Hospital at Home managers, directors or co‐ordinators were responsible for creating a positive staff environment, ensuring protected time for training and clinical supervision, and facilitating service improvements. | Moderate | Minor concerns about adequacy and coherence. No or very minor concerns about methodological limitations and relevance. | Barnard 2016; Brody 2019; Crilly 2012; Dow 2007a; Fisher 2021; Hitch 2020; Karacaoglu 2021; Leung 2016; Sims 1997; Testa 2021; Udesen 2022 |
| Finding 4. A multidisciplinary skilled workforce was required to implement Hospital at Home, with collaboration between teams and professionals (e.g. via team meetings) a core feature. However, maintaining responsiveness was important, and the absence of a waiting list for admission to Hospital at Home allowed a service to respond to the demand for hospital care. Building rapport with external partners was challenging, and allied health professionals noted difficulties with their professional line of reporting and supervision. Some teams were frustrated by a lack of resource allocation, others recognised that the service was better staffed than usual care. Teams were also challenged to meet intensity targets and address workforce shortages. Multiple strategies could enhance capacity and responsiveness, such as securing more funding, training family members, adopting new technologies and implementing telehealth appointments. However, this could affect the provision of patient‐centred care. | High | Minor concerns about coherence. No or very minor concerns about adequacy, methodological limitations and relevance. | Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Cunliffe 2004; Dean 2007; Dinesen 2007; Dow 2007a; Fisher 2021; Gorbenko 2023; Hitch 2020; Karacaoglu 2021; Lemelin 2007; Moule 2011; O'Neill 2017; Papaioannou 2018; Rayner 2022; Sims 1997; Testa 2021; Udesen 2022; Vaartio‐Rajalin 2020; von Koch 2000 |
| Finding 5. Staff training, expansion of roles beyond usual scope of practice and rapid delivery of equipment or medical testing was essential to implement Hospital at Home. Expanding nurse roles increased capacity for acute medical care in the home and residential care. Expanding rehabilitation assistant roles increased capacity for rehabilitation in the home. The expansion of roles required appropriate governance structures and policy changes. | High | Minor concerns about coherence. No or very minor concerns about adequacy, methodological limitations and relevance. | Andrade 2013; Barnard 2016; Brody 2019; Cobley 2013; Crilly 2012; Cunliffe 2004; Dinesen 2007; Dismore 2019; Dubois 2001; Fisher 2021; Hitch 2020; Karacaoglu 2021; Lemelin 2007; Leung 2016; O'Neill 2017; Papaioannou 2018; Rayner 2022; Sims 1997; Testa 2021; Udesen 2022; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021 |
| Finding 6. Effective communication between staff, patients and caregivers, including documentation and sharing tailored information with patients, was essential to provide efficient and effective care and reassure patients that quality of care is maintained in Hospital at Home. Problems with communication were commonly encountered for patients (e.g. patient information was not tailored), caregivers (e.g. limited opportunities to discuss management with clinicians) and staff (e.g. absence of a shared electronic medical record hampering the sharing of information about patients, efficiency of the service and continuity of care). | High | Minor concerns about coherence. No or very minor concerns about adequacy, methodological limitations and relevance. | Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Cobley 2013; Collins 2016; Crilly 2012; Cunliffe 2004; Dean 2007; Dinesen 2007; Dinesen 2008; Dismore 2019; Dubois 2001; Fisher 2021; Gorbenko 2023; Jester 2003; Kimmel 2021; Ko 2023; Lemelin 2007; Leung 2016; Levine 2021; Mäkelä 2020; O'Neill 2017; Ranjbar 2015; Reid 2008; Rossinot 2019; Schofield 2006; Sims 1997; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; von Koch 2000; Wallis 2022; Wang 2012 |
| Finding 7. Health professionals required skills in delivering person‐centred care, shared decision‐making and tailoring care to achieve patient goals and patient satisfaction. Some caregivers were frustrated about their lack of involvement in decision‐making and care planning. Patients valued equal interactions and partnerships with the staff, and their ability to cater for their needs, and valued staff focussing on helping family members. | High | No or very minor concerns about adequacy, methodological limitations, relevance and coherence. | Andrade 2013; Chouliara 2014; Clarke 2010; Cobley 2013; Collins 2016; Cunliffe 2004; Dinesen 2007; Dow 2007a; Dow 2007b; Dubois 2001; Fisher 2021; Gorbenko 2023; Hitch 2020; Jester 2003; Karacaoglu 2021; Kimmel 2021; Ko 2023; Kylén 2021; Levine 2021; Lou 2017; Mäkelä 2020; Manning 2016; Nordin 2015; Papaioannou 2018; Ranjbar 2015; Reid 2008; Rossinot 2019; Schofield 2006; Udesen 2021; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; von Koch 2000; Wallis 2022; Wilson 2002 |
| Theme 3. Acceptance, perceived benefits and caregiver impacts from Hospital at Home | |||
| Finding 1. Patients, caregivers and service level staff believed Hospital at Home (including in residential care) was an appropriate alternative to hospital inpatient care, and facilitated optimal recovery and satisfaction with less risk of hospital‐acquired complications. Patients appreciated positive and competent staff who motivated them to reach their recovery goals. Sometimes the lack of caregiver support and 24‐hour supervision from hospital staff made some patients prefer to stay in hospital. | High | No or very minor concerns about adequacy, methodological limitations, relevance and coherence. | Andrade 2013; Barnard 2016; Cobley 2013; Cunliffe 2004; Dinesen 2008; Dow 2007a; Dow 2007b; Dubois 2001; Fisher 2021; Gorbenko 2023; Hitch 2020; Karacaoglu 2021; Kimmel 2021; Ko 2023; Kraut 2016; Lemelin 2007; Levine 2021; Lou 2017; Mäkelä 2020; Moule 2011; Nordin 2015; Papaioannou 2018; Ranjbar 2015; Rayner 2022; Rossinot 2019; Sims 1997; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; Wallis 2022; Wilson 2002 |
| Finding 2. Caregivers were impacted by Hospital at Home. This included disruption to their normal routines, work, energy and sleep. There were reports of stress and anxiety related to feeling untrained to provide patient support and monitoring and a lack of formal recognition and access to information. Some caregivers and patients were concerned about their privacy at home and the impact on the patient/caregiver relationship from being involved with care. | High | No or very minor concerns about adequacy, methodological limitations, relevance and coherence. | Andrade 2013; Brody 2019; Cobley 2013; Dinesen 2008; Dismore 2019; Dow 2007b; Dubois 2001; Fisher 2021; Hitch 2020; Jester 2003; Kimmel 2021; Ko 2023; Levine 2021; Lou 2017; Mäkelä 2020; Manning 2016; Nordin 2015; Reid 2008; Rossinot 2019; Sims 1997; Udesen 2021; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; Wallis 2022; Wilson 2002 |
| Theme 4. Sustainability of Hospital at Home | |||
| Finding 1. Staff and patients expressed concern that without widespread implementation and expansion, the perceived benefits of Hospital at Home to patients and the healthcare system would be limited. Health system benefits included long‐term financial savings from avoiding unnecessary hospitalisation, bed closures or reduced length of stay, plus increased hospital capacity with reduced waiting times. However, some patients were sceptical that Hospital at Home was more about saving money, and in multiple‐payer settings costs incurred by patients was a key factor when admitting patients to Hospital at Home. Peer institution success with Hospital at Home increased executive enthusiasm for Hospital at Home. Hospital at Home could showcase a hospital’s innovation and help sustain staff recruitment. However, staff recruitment may be more challenging in rural settings as excessive driving can affect staff satisfaction. | High | Minor concerns about adequacy. No or very minor concerns about methodological limitations, relevance and coherence. | Andrade 2013; Dow 2007b; Fisher 2021; Gorbenko 2023; Hitch 2020; Karacaoglu 2021; Ko 2023; Moule 2011; Papaioannou 2018; Rayner 2022; Sims 1997; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; Wallis 2022 |
aThe GRADE‐CERQual evidence profile for each finding is available in Appendix 1.
Background
Description of the topic
Two related 'Hospital at Home' services provide alternatives to traditional in‐hospital care: Admission Avoidance Hospital at Home and Early Discharge Hospital at Home. Admission Avoidance Hospital at Home avoids hospitalisation by providing acute or subacute treatment in a patient’s home or usual place of residence for a limited time, for a condition that would otherwise require a hospital admission (Edgar 2024). Eligible patients are typically referred from an emergency department, an acute assessment unit or directly from ambulance services; they can also be referred by community physicians and specialists to receive active treatment from healthcare professionals in their homes. Early Discharge Hospital at Home involves supporting patients to go home earlier than usual to receive acute care or subacute care in their homes for a limited time period (Caplan 2012; Goncalves‐Bradley 2017). Eligible patients are typically referred from acute inpatient care and provided active treatment from healthcare professionals in their homes, and therefore spend less time in hospital. This is a service that is more embedded in health systems due to the long‐term focus on reducing hospital length of stay. While this service can also include home‐based End‐of‐life Care services, which support people to die at home rather than in hospital (Sheppard 2021), End‐of‐life Care is not a focus of this qualitative evidence synthesis.
A Cochrane review of Admission Avoidance Hospital at Home included 20 randomised trials and 3100 participants with various conditions (e.g. older adults requiring admission to hospital following a stroke, with a diagnosis of dementia, or adults with chronic obstructive pulmonary disease or heart failure) (Edgar 2024). Compared to inpatient care, the review found that Admission Avoidance Hospital at Home probably makes little or no difference to patients' self‐reported health status, risk of death or likelihood of hospital readmission (moderate‐certainty evidence), probably reduces the likelihood of living in long‐term residential care at six months' follow‐up (moderate‐certainty evidence), may improve patient satisfaction (low‐certainty evidence) and may reduce healthcare costs (low‐certainty evidence) (Edgar 2024).
A Cochrane review of Early Discharge Hospital at Home included 32 randomised trials and 4746 patients with findings reported for various health conditions (e.g. stroke survivors, patients following elective surgery, older patients with various medical conditions such as chronic obstructive pulmonary disease) (Goncalves‐Bradley 2017). Compared to inpatient care, the review found that Early Discharge Hospital at Home probably reduces length of stay forpeople recovering from a stroke (about seven days), people following elective surgery (about four days) and older people with a medical condition ranging from half a day to 20 days (moderate‐certainty evidence). The evidence also showed that these services probably make little or no difference to the risk of death for people recovering from a stroke or older people with a mix of medical conditions (moderate‐certainty evidence), may make little or no difference to the risk of hospital re‐admission for people recovering from a stroke or elective surgery (low‐certainty evidence), and may decrease the risk of living in long‐term residential care for people recovering from a stroke and older people with a mix of medical conditions(low‐certainty evidence). The review also found that Early Discharge Hospital at Home may make little or no difference to caregiver burden for people recovering from stroke or elective orthopaedic surgery (low‐certainty evidence) and may slightly improve patient satisfaction for people recovering from stroke or elective surgery (low‐certainty evidence); we do not know if these services reduce healthcare costs across the various conditions because the certainty of this evidence is very low (Goncalves‐Bradley 2017).
Outcomes from these two Cochrane intervention reviews suggest that Hospital at Home services may provide either superior or similar outcomes compared to inpatient care. However, these reviews did not address how to implement these services. While health systems around the world vary with respect to financing (e.g. multiple‐ or single‐payer systems), policy objectives for Admission Avoidance Hospital at Home and Early Discharge Hospital at Home services are likely to be similar as they are expected to reduce demand for inpatient hospital beds, reduce costs and conserve health outcomes. This review seeks to understand the factors influencing their implementation. Here we use the term implementation to describe both the process by which these models of care are introduced to health systems and hospitals by policy makers, healthcare providers and governments through policy, guidelines and financing; and also the process by which these models of care are introduced and integrated into clinical practice by clinical leads and health professionals, how patient groups are selected for the services and how the services are experienced by patients and their caregivers.
How the intervention might work
To integrate potential findings of this qualitative evidence synthesis with the two Cochrane intervention reviews, we have developed a logic model (Figure 1). The purpose of a logic model is to outline the hypothesised causal pathway that links the intervention (e.g. Admission Avoidance Hospital at Home for eligible patients) with mediating factors that impact on the key outcomes (e.g. health status, healthcare utilisation, patient and caregiver satisfaction, admission to long‐term residential care, as reported in the Cochrane intervention reviews) (Baxter 2014).
1.
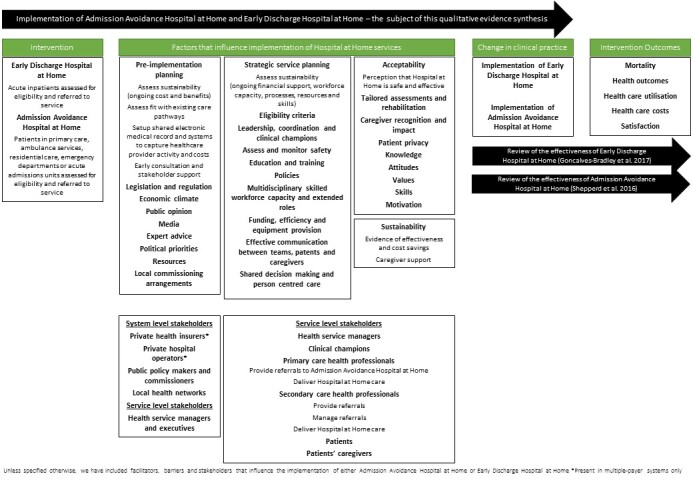
Updated logic model describing the factors that influence implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home.
As a preliminary step we integrated the findings of qualitative studies known to the review team into the draft logic model to suggest potential mediating factors and key stakeholders at the system, service and stakeholder level that may influence implementation of Hospital at Home services (Brody 2019; Buhagiar 2017; Dismore 2019; Gardner 2003; Gardner 2019; Kraut 2016; Lemelin 2007; Mäkelä 2018). This logic model suggests that the key stakeholders for successful implementation vary in multiple‐payer systems and single‐payer systems at the system level (e.g. private health insurers and public policy makers) but hold similar positions at the service level (e.g. health service managers and health professionals in primary and secondary care). This logic model was updated after this qualitative evidence synthesis, and we invited members of our stakeholder advisory panel to review the findings to ensure we include interpretations from a broader lens in the development of the logic model.
Why is it important to do this synthesis?
Countries around the world are dealing with an increasing demand for hospital‐level care by introducing services that provide health care in the home, as an alternative to hospital admission. Virtual wards are one such service that gained traction during the COVID‐19 pandemic by providing remote monitoring to people in their home (Norman 2023). Hospital at Home that provides a higher level of care, for example Admission Avoidance Hospital at Home, is another service that expanded during the pandemic. Although there is a growing evidence base on the effectiveness and cost of these services (Goncalves‐Bradley 2017; Sheppard 2022; Edgar 2024; Singh 2022), health service planners and practitioners require evidence on how to implement and sustain these services on a wider scale.
There is also substantial variation in the implementation of Hospital at Home services across different countries and healthcare settings. Across England, a single‐payer system, healthcare providers have implemented three different types of Hospital at Home services, each with varying functions. This includes Admission Avoidance Hospital at Home, Early Discharge Hospital at Home and Discharge to Assess (services that provide short‐term, funded support for patients to be discharged to their own home or a community setting, where longer‐term support needs are assessed) (Young 2009). This variation makes it difficult to assess how Hospital at Home services contribute to health care and ease the demand for hospital‐based care (NHS Benchmarking Network 2015). In Australian public hospitals (a single‐payer system), hospital in the home multi‐day admissions ranged from 25 admissions in Tasmania in 2017 to 2018 to 30,070 admissions in Victoria in the same year (Australian Institute of Health and Welfare 2019). Given the observed variation in implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home, and possibly variation in thresholds for admission to Hospital at Home across jurisdictions, there is a need to understand the factors that influence implementation of these models and how these may differ between healthcare settings (for example, high‐income versus low‐ and middle‐income countries; single‐payer systems versus multiple‐payer systems; urban versus regional or rural contexts; mechanisms of referral and boundaries with other health services; and the provision of social care and admission criteria). Where data permit, these factors will be explored in the qualitative evidence synthesis from the perspectives of multiple stakeholders.
A previous qualitative evidence synthesis including 16 studies examined perceptions of Hospital at Home among stakeholders with the main aim of identifying areas for improvement in this model of care (Chua 2022). Recommended improvements included more support for caregivers, including caregiver involvement in decision‐making, and better clinician training and use of technology to improve clinician collaboration and co‐ordination of Hospital at Home. Our qualitative evidence synthesis contributes new knowledge, as its focus is to explore factors affecting the implementation of these services, and it includes evidence for both acute and subacute care, applies GRADE CerQual to examine confidence in the findings, and applies rigorous Cochrane conduct and reporting methods including subgroup analyses. It also integrates with, and enhances, the findings of the two Cochrane intervention reviews (Goncalves‐Bradley 2017; Edgar 2024).
How this review might inform or supplement what is already known in this area
A qualitative exploration using a logic model to guide analysis facilitates the interpretation of the findings from the Cochrane intervention reviews by identifying the factors that hinder or support the implementation of these services. An assessment of the factors that influence the implementation of these services from the perspectives of people involved in the funding, commissioning and delivery of care (i.e. policy makers, managers, health professionals), and people receiving care (i.e. patients and caregivers), may also help to explain the reasons for variation in the implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home in different healthcare settings.
This qualitative evidence synthesis takes a global perspective. The findings will assist the implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home, and will be beneficial for a range of stakeholders, including policy makers and commissioners, health insurers, health service managers, health professionals, patients and patients' caregivers.
Objectives
To identify, appraise and synthesise qualitative research evidence on the factors that influence the implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home, from the perspective of multiple stakeholders, including policy makers, health service managers, health professionals, patients and patients’ caregivers.
To explore how our synthesis findings relate to, and help to explain, the findings of the Cochrane intervention reviews of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home services.
Methods
Design
This is a qualitative evidence synthesis of primary qualitative studies. Study reporting was guided by the Cochrane Effective Practice and Organisation of Care (EPOC) qualitative evidence synthesis template (Glenton 2020) and the 'enhancing transparency in reporting the synthesis of qualitative research' (ENTREQ) guidance (Tong 2012).
Criteria for considering studies for this review
Types of studies
We included primary studies that used qualitative methods for both data collection (such as focus group discussions or individual interviews) and data analysis (such as thematic analysis, framework analysis and grounded theory). We excluded studies that collected data using qualitative methods but did not analyse these data using qualitative analysis methods. As we expected to find sufficient qualitative studies that use qualitative methods for both data collection and data analysis, we excluded studies that collected data using open‐ended survey questions.
We included both published and unpublished studies, and studies published in any language. Mixed‐method studies were included where it was possible to extract the data that were collected and analysed using qualitative methods. We did not exclude studies based on our assessment of methodological limitations. We included studies regardless of whether they were conducted alongside studies of the effectiveness of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home (Goncalves‐Bradley 2017; Edgar 2024).
Topic of interest
The qualitative evidence synthesis includes qualitative studies that examine the implementation of new or existing Hospital at Home services (Admission Avoidance Hospital at Home or Early Discharge Hospital at Home) from the perspective of different stakeholders. This will allow exploration of factors influencing the implementation of Hospital at Home services that are being introduced compared with services that are already in place. We use the term 'implementation' to describe both the process by which these models of care are introduced to health systems and hospitals through policies and guidelines, and also the process by which these models of care are put into clinical practice by clinical leads and teams of health professionals for appropriate patients and accepted by patients and patients’ caregivers.
To ensure the focus of this qualitative evidence synthesis matches the focus of the corresponding Cochrane intervention reviews, we have used similar definitions and exclusion criteria (Goncalves‐Bradley 2017; Edgar 2024).
Types of interventions
Admission Avoidance Hospital at Home is a service that is established to avoid hospitalisation. It provides acute or subacute treatment in a patient’s home for a limited time, for a condition that would otherwise require a hospital admission (Edgar 2024). We included studies where patients are admitted to a Hospital at Home service from primary care in the community, ambulance services or from hospital emergency departments or acute admissions units.
Early Discharge Hospital at Home is a service that provides health care for patients discharged early from hospital. It provides acute or subacute treatment in a patient’s home for a limited time, for a condition that would otherwise require a hospital admission (Deloitte Access Economics 2011; Goncalves‐Bradley 2017). We included studies where patients are admitted to this service following an early discharge from hospital. We considered early discharge as defined by the authors of included studies as there is no consistent definition; the length of hospital admission prior to early discharge varies by health condition and varies across trials (Deloitte Access Economics 2011).
We included studies about Admission Avoidance Hospital at Home and Early Discharge Hospital at Home, where health professionals provide active acute or subacute treatment in a patient’s home or usual place of residence for a limited time and for a condition that would otherwise require a hospital admission. Typically, patients remain under the clinical responsibility of a hospital clinician while receiving Hospital at Home treatment, but we will also include studies where a patient’s general practitioner takes clinical responsibility. Health professionals that deliver Hospital at Home care can be hospital employees or employed through a service in the community (e.g. district nurses). For the purpose of this review, we define acute care as active, urgent, short‐term treatment in which the principal intent is to relieve symptoms of illness or injury, reduce the severity of an illness or injury, or protect against exacerbation or complication of an illness or injury that could threaten life or normal function (Independent Hospital Pricing Authority 2015; OECD 2011). We define subacute care as multidisciplinary care that is delivered by or informed by health professionals with specialist expertise and includes negotiated goals within a specified time frame that aim to optimise the patient’s functioning and quality of life (Independent Hospital Pricing Authority 2015; OECD 2011).
In line with these definitions, and with the exclusion criteria of the corresponding Cochrane intervention reviews, this review excluded studies that include patients not deemed to require acute or subacute care in a hospital setting. For example, we excluded from this review services that provide long‐term patient care, care in outpatient settings or after discharge from hospital, palliative care and self‐care by the patient in their home (Goncalves‐Bradley 2017; Edgar 2024). We additionally excluded studies that focus only on obstetric care, paediatric care, palliative care at home or mental health hospital at home (such as crisis‐resolution hospital at home) to ensure the focus of this qualitative evidence synthesis matches the focus of the corresponding Cochrane intervention reviews (Goncalves‐Bradley 2017; Edgar 2024). Studies that explore the implementation of Hospital at Home services for both adults (aged 18 years or older) and children will be included where data relating to adult Hospital at Home services are reported separately.
Types of participants
The review included the perspective of multiple stakeholders involved in Admission Avoidance Hospital at Home and Early Discharge Hospital at Home. Stakeholders' perspectives encompass their experiences, beliefs, perceptions and views relating to the implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home services.
At the system level, these stakeholders can include the following:
Policy makers and commissioners (or people in similar roles who make decisions about funding and policies for Admission Avoidance Hospital at Home and Early Discharge Hospital at Home).
Private health insurers (or people in similar roles in multiple‐payer systems who make decisions about funding and policies for Admission Avoidance Hospital at Home and Early Discharge Hospital at Home).
Private hospital operators (or people in multiple‐payer hospitals and hospital networks who make decisions about hospital policy and funding for Admission Avoidance Hospital at Home and Early Discharge Hospital at Home).
Local health networks (or people in single‐payer hospitals and hospital networks) who make decisions about hospital policy and funding for Admission Avoidance Hospital at Home and Early Discharge Hospital at Home.
At the service level, these stakeholders can include the following:
Health service managers (people in single‐payer or multiple‐payer hospitals who make decisions about policy and funding for patients’ care).
Clinical leads (health professionals who co‐ordinate and supervise teams of health professionals).
Clinical champions (health professionals who advocate for Admission Avoidance Hospital at Home and Early Discharge Hospital at Home to help with successful implementation).
Primary care health professionals (health professionals in the community that provide referrals to Admission Avoidance Hospital at Home; health professionals in the community who deliver Hospital at Home care).
Secondary care health professionals (health professionals in the hospital emergency department that provide referrals to Admission Avoidance Hospital at Home; health professionals in the hospital that provide referrals to Early Discharge Hospital at Home; health professionals in the hospital that manage referrals to Admission Avoidance Hospital at Home and Early Discharge Hospital at Home; health professionals in the hospital that deliver Hospital at Home care).
Adult patients (aged 18 years and older) with a disease or condition requiring an acute or subacute hospital admission, who are eligible for Admission Avoidance Hospital at Home or Early Discharge Hospital at Home. Patients requiring these services for the sole purpose of palliative care, obstetric care or mental health hospital at home are excluded from this review (see 'Types of interventions').
Patients’ caregivers (adults who would primarily provide assistance with activities of daily living, personal care and navigating services for the patient during the period of recovery) (Mäkelä 2020; Talley 2007).
Search methods for identification of studies
The Cochrane EPOC Information Specialist developed the search strategy for this review in consultation with the review authors (Noyes 2020).
Electronic searches
To identify primary studies, we searched the following databases to 17 November 2022:
MEDLINE, Ovid
CINAHL, EbscoHOST
Scopus, Elsevier
Global Index Medicus, WHO
We did not apply limits to language or publication date. Our search strategy combined known terms for Admission Avoidance Hospital at Home and Early Discharge Hospital at Home with a qualitative filter. Terms related to Admission Avoidance Hospital at Home and Early Discharge Hospital at Home were derived from a 'gold set' of known qualitative papers that the author team knew would be included in the qualitative evidence synthesis, as well as all terms used in included papers in the Cochrane intervention reviews (Goncalves‐Bradley 2017; Edgar 2024), and terms currently used in real‐world practice and evaluations (HITH Society Australasia 2019; World Hospital At Home Congress 2019). Our strategy favours specificity over sensitivity (Harris 2018). The search strategies are detailed in Appendix 2.
Searching other resources
Our search was supplemented by searching the reference list of relevant articles, and forward tracking the citations of studies included in the qualitative evidence synthesis and key references (the Cochrane intervention reviews and their included trials (Goncalves‐Bradley 2017; Edgar 2024)) using Scopus. Additionally, we approached experts in the field to request studies that might meet our inclusion criteria.
Selection of studies
Two review authors (JH, JW) independently screened the title and abstract of all records obtained from searching the literature, and coded them as ‘retrieve’ (potentially eligible or unclear) or ‘do not retrieve’ (not eligible). Two review authors (JH, JW, PM in various combinations) independently screened the full text of all retrieved articles, identified studies for inclusion and recorded the reasons for exclusion of ineligible studies. Any disagreement or uncertainty was resolved through discussion and, if needed, a third author (DOC, PM) adjudicated. Review authors who were authors on potentially eligible studies were not involved in assessing the eligibility of that study. Where necessary, we contacted study authors for further information.
We included a table listing studies that we excluded from our qualitative evidence synthesis at the full‐text stage, along with the main reasons for exclusion. Where the same study (i.e. using the same sample and methods) had been presented in different reports, we collated these reports so that each study, rather than each report, was the unit of interest in our qualitative evidence synthesis. Where the same Hospital at Home service was evaluated in different study reports (i.e. using different samples and methods), we considered these different studies, but noted that they assessed the implementation of the same service.
We used Covidence to screen and select studies, and we detailed the selection process to produce a Preferred Reporting Items of Systematic Reviews and Meta‐analysis (PRISMA) flow diagram (Liberati 2009).
Language translation
We included reports in any language. For titles and abstracts published in a language other than English, we used open source software (Google Translate) to determine whether the paper was potentially eligible for inclusion. If potentially eligible, we translated the full‐text report into English using the same open source software and, if this translation was insufficient, we planned to ask members of Cochrane networks or other networks that are fluent in that language to assist in assessing the full text of the paper for inclusion. If we were still unsure about the study's eligibility, we planned to include these in 'Studies awaiting classification' to ensure transparency in the review process.
Sampling of studies
Qualitative evidence syntheses aim for variation in concepts rather than an exhaustive sample, and large amounts of study data can impair the quality of the analysis. Once we identified all studies that were eligible for inclusion, we planned to assess whether their number or data richness would likely represent a problem for the analysis and planned to consider selecting a sample of studies.
If sampling was required, we planned to use purposeful sampling, which aims to limit data redundancy while ensuring optimal data richness and diversity. We planned to stratify studies by intervention type (Admission Avoidance Hospital at Home or Early Discharge Hospital at Home). For each intervention, we planned to then use a sampling frame to ensure representation by stakeholder group level (system level, local level), and geographic area (urban and regional or rural; low‐ and middle‐income countries and high‐income countries). Where we observed the potential for data redundancy (for example, multiple studies of patients in urban, high‐income country settings), we planned to assess the data richness of each study using a pilot data richness scale (Appendix 3) (Ames 2017). We planned to only include studies that provided a good amount and depth of qualitative data pertaining to factors that influence implementation (data richness score greater than three) (Cochrane EPOC 2017).
For this review, we did not consider sampling a subset of studies was necessary.
Data extraction
Two review authors (ET, JH, JW in various combinations) independently extracted data on study characteristics, using a standardised data collection form developed for this qualitative evidence synthesis. Any discrepancies were resolved by discussion or adjudication by a third author (PM). Review authors who were authors on an included study were not involved in data extraction for that study. For each study we recorded details, where available, on the following:
Intervention addressed (Admission Avoidance Hospital at Home; Early Discharge Hospital at Home) and whether the study is linked to an intervention trial.
Time since the intervention was implemented.
Study details (first author; corresponding author; year of evaluation; year of publication).
Research question and aims.
Geographic setting (country of programme; low‐ and middle‐income or high‐income country classification; urban, regional or rural location; multiple‐payer or single‐payer system; number of hospitals).
Participants (number; patient and caregiver characteristics (e.g. age, sex, clinical conditions), stakeholder's role or position (e.g. system level; private health insurer), service level (e.g. secondary care health professional)) and method of sampling participants.
Method of data collection (e.g. interview, focus group).
Method of data analysis (e.g. thematic analysis).
All text from the results sections of the included publications was extracted verbatim, including themes, sub‐themes, supporting quotes and conclusions (Thomas 2008).
To provide context for the qualitative findings, we used the Template for Intervention Description and Replication (TIDieR) framework to extract information on the Admission Avoidance Hospital at Home or Early Discharge Hospital at Home intervention that was the focus of the qualitative study (Hoffmann 2014). Where required, we extracted this information from the qualitative study or from a linked effectiveness trial.
What (materials): were any informational materials used?
What (procedures): is there a programme manager and, if so, what is their role? What are the patient eligibility criteria? Who refers patients to the programme and what is the admission pathway? On average, how many days do patients spend in acute care before being transferred to Hospital at Home? Is acute or subacute care provided to patients in the Hospital at Home service?
Who provided: who are patients under the care of while enroled in Hospital at Home? Who delivers Hospital at Home care, and are they employed through the hospital or are they from the community? Was training provided to the health professionals that refer to Hospital at Home services or deliver Hospital at Home services?
How and where was the Hospital at Home intervention delivered (e.g. 1:1 face‐to‐face in patients’ homes)?
When and how much: on average, how many days do patients spend in Hospital at Home, and how often do they receive treatment by a Hospital at Home health professional? How long has the programme been running?
Tailoring: was the intervention tailored to specific hospitals, health professionals or patients or patient groups and, if so, how?
Modifications: was the intervention modified during the study?
How well (planned and actual): did the intervention employ any strategies to improve fidelity, and was fidelity achieved?
Assessing the methodological limitations of included studies
Two review authors (ET, JH, JW in various combinations) independently assessed the methodological limitations of each included study using the Critical Appraisal Skills Programme (CASP) checklist (Critical Appraisal Skills Programme 2020). Any discrepancies were resolved by discussion or adjudication by a third author (DOC). The CASP tool uses a checklist of 10 questions, each of which includes multiple signalling questions to help users interpret the items (29 signalling questions in total). We summarised the findings of the CASP checklist in a 'Methodological limitations' table. Review authors who were authors on an included study were not involved in assessing the methodological limitations of that study.
Data analysis and synthesis
We used thematic synthesis to code the findings of included studies for factors that influence the implementation of Admission Avoidance Hospital at Home or Early Discharge Hospital at Home according to stakeholder perspectives. For example: system level (private health insurer) and service level (patient, health professional, health service manager). We used the approach recommended by Thomas and Harden including inductive line‐by‐line coding of extracted text and development of descriptive findings (Thomas 2008).
We reviewed each line of extracted text and developed codes based on the content and meaning of each extract. Existing codes were reviewed and revised as new codes were added. When all studies had been coded, all text related to each code was reviewed for consistency of coding across studies. Two review authors (JW, ET) independently coded an initial subset of studies and then met to discuss any discrepancies until consensus was reached. The remaining studies were coded by one author (ET or JW) and verified by a second author (ET or JW). Review authors who were authors on an included study were not involved in data analysis for that study.
We reviewed all codes for similarities and differences, and organised them into descriptive themes and findings relating to the factors that influence the implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home services. One author (JW) drafted a summary of the descriptive findings and these were discussed by the review team until consensus was reached. We managed the analysis using NVivo 12 software (NVivo). We decided to complete the first two steps of the Thomas and Harden method of thematic synthesis to develop descriptive findings. Whilst it would have been an option to undertake stage 3 to develop analytical themes with new theoretical insights using synthesised data from included studies, Thomas and Harden suggest that movement to the development of new theory and theoretical insights (stage 3) can also be achieved when integrating the findings from the QES with the results of the intervention effectiveness reviews. We therefore further developed the initial logic model as the mechanism for developing new theoretical insights (see section 'Results of integrating the review findings with the Cochrane intervention reviews of Early Discharge Hospital at Home and Admission Avoidance Hospital at Home').
To maximise the likelihood that our findings are transferable to real‐world practice (Marshall 2014), we invited our stakeholder advisory panel to review the qualitative evidence synthesis findings and revised logic model (NHMRC 2017). Articulating our findings through a logic model facilitated communication of the findings to stakeholders and identified strategies to improve the implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home services (Harris 2018). GD, policy maker from NSW Health, provided this stakeholder feedback, which was incorporated into the discussion.
Once we finished preparing the qualitative evidence synthesis findings, we examined each finding, and developed prompts for future implementers. These prompts are presented in the 'Implications for practice' section. They are not intended to be recommendations but are phrased as questions to help implementers consider the implications of the review findings within their context (i.e. to what extent are identified factors that influence the implementation of Hospital at Home services addressed).
Subgroup analyses
Where data permitted, we examined similarities and differences in the factors that influence the implementation of Hospital at Home services with regard to the following study characteristics:
Type of delivery model (Admission Avoidance Hospital at Home versus Early Discharge Hospital at Home)
Geographic setting (high‐income versus low‐ and middle‐income countries; single‐payer systems versus multiple‐payer systems; urban versus regional or rural contexts; services delivered in people’s homes versus residential care)
Presence of intervention components (mechanisms of referral; the provision of social care; admission criteria)
Patient populations where there is evidence that Hospital at Home services are effective (e.g. older adults requiring hospital admission, such as for chronic obstructive pulmonary disease; people recovering from stroke; people recovering from surgery), as informed by the Cochrane intervention reviews; patient populations identified as a priority for Hospital at Home services by policy makers
Assessment of confidence in review findings
Two review authors (JW, DOC) used the GRADE‐CERQual (Confidence in the Evidence from Reviews of Qualitative research) approach to independently assess our confidence in each finding (Lewin 2018). CERQual assesses confidence in the evidence, based on the following four key components:
Methodological limitations of the included studies: the extent to which there are concerns about the design or conduct of the primary study that contributed evidence to an individual review finding
Coherence of the review finding: an assessment of how clear and cogent the fit is between the data from the primary studies and a review finding that synthesises those data (by 'cogent', we mean well‐supported or compelling)
Adequacy of the data contributing to a review finding: an overall determination of the degree of richness and quality of data supporting a review finding
Relevance of the included studies to the review question: the extent to which the body of evidence from the primary studies supporting a review finding is applicable to the context (perspective or population, phenomenon of interest, setting) specified in the review question
We rated each domain as no or very minor concerns, minor concerns, moderate concerns or serious concerns. After assessing each of these four components, we made a judgement about the overall confidence in the evidence supporting the review finding. We judged confidence as high (i.e. highly likely that the review finding is a reasonable representation of the phenomenon of interest), moderate (i.e. likely that the finding is a reasonable representation of the phenomenon of interest), low (i.e. possible that the finding is a reasonable representation of the phenomenon of interest) or very low (i.e. unclear whether the finding is a reasonable representation of the phenomenon of interest). All findings started as 'high confidence' and were graded down if there were important concerns regarding any of the CERQual components. Where concerns in relation to a component are minor or moderate, it may not be necessary to rate down. However, if there are a number of such concerns, it may be appropriate to rate down by one level to represent two or more of these concerns. The final assessment was based on consensus amongst the review authors.
'Summary of qualitative findings' table and evidence profile
We present a summary of the findings and our assessments of confidence in these findings in a 'Summary of qualitative findings' table and detailed descriptions of our confidence assessment in an evidence profile.
Integrating the review findings with the Cochrane intervention reviews
We organised the findings from our QES (Harden 2018) to reflect the timeline for planning and implementing Hospital at Home services, categorising factors as those that facilitate implementation and those that may limit effectiveness. The findings of the qualitative evidence synthesis may inform subgroup analyses for future updates of the Cochrane intervention reviews, as well as the design of future trials aiming to implement Admission Avoidance Hospital at Home and Early Discharge Hospital at Home services.
Review author reflexivity
All review team members have prior experience with Hospital at Home, or an awareness that Hospital at Home services have either superior or similar effects compared to inpatient care but are potentially under‐utilised. Hence, all team members tend to view these services favourably. We approached the review with an awareness of this bias towards positively viewing Hospital at Home services, and endeavoured to keep an open and curious mind about the factors that influence the implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home.
We maintained a reflexive stance throughout all stages of this review process. All decisions or processes were conducted independently by at least two team members, who then discussed with each other and with the review team how their own backgrounds and positions may affect the analysis and interpretation of review findings. This allowed for regular opportunities to critically examine all decisions made and to counter our own biases. Members of this review team have clinical backgrounds (JW, DOC, RB, PM), qualitative research backgrounds (DOC, JW, SS, PM, RB), experience in writing Cochrane reviews (DOC, JW, JH, SS, RB) and experience in conducting research examining Hospital at Home (EG, JW, DOC, SS, PM, RB). Through our collective and individual experiences as clinicians, academics, researchers and policy makers, we anticipated that this review would reveal a combination of organisational, professional and individual factors that influence the implementation of Admission Avoidance Hospital at Home and Early Discharge Hospital at Home. As a team, we remained mindful of our presuppositions and supported each other to minimise the influence of these on our analysis or the interpretation of our findings. The lead author kept a reflexive journal throughout the review process and documented and reflected on progress and decisions made (Nowell 2017).
Results
Results of the search
We identified 7535 records through database searching up to 17 November 2022, plus one record via citation tracking. After 1688 duplicates were removed, we screened 5848 records, with 5656 records excluded based on titles and abstracts. We assessed 192 full‐text records for inclusion in this synthesis, with 123 records excluded due to incorrect study design (43 studies did not utilise qualitative methods in both data collection and analysis relating to service implementation) and incorrect intervention (80 studies were not assessing new or existing Hospital at Home services that were alternatives for acute or subacute care) (see Characteristics of excluded studies). In total, 52 studies (reported in 62 records) were included in the qualitative evidence synthesis, published from 1997 to 2022 and in three languages (English ‐ 49 studies, French ‐ two studies, Portuguese ‐ one study). Seven additional records are awaiting classification (see Characteristics of studies awaiting classification) (Figure 2).
2.

Study flow diagram
Description of the included studies
We included 52 studies in this review. A detailed description of the included studies is provided in the Characteristics of included studies table. A description of intervention components is included in Table 2, separated by intervention types of Early Discharge Hospital at Home for acute care, Early Discharge Hospital at Home for subacute care, Admission Avoidance Hospital at Home, and combined Early Discharge and Admission Avoidance Hospital at Home.
1. TIDieR table.
| Study ID | What (materials) | What (procedures) | Who provided | How | When and how much | Tailoring/modifications |
| Were any informational materials used? |
What are the patient eligibility criteria? Who refers patients to the programme and what is the admission pathway? On average, how many days do patients spend in acute care before being transferred to Hospital at Home? |
Is there a programme manager and, if so, what is their role? Who are patients under the care of while enrolled in Hospital at Home? Who delivers Hospital at Home care, and are they employed through the hospital or are they from the community? Was training provided to the health professionals that refer to Hospital at Home services or deliver hospital at home services? |
How and where was Hospital at Home intervention delivered? (e.g. 1:1 face‐to‐face in patient's home) What was the communication process? Was a phone service available? |
On average, how many days do patients spend in Hospital at Home, and how often do they receive treatment from a Hospital at Home health professional? What is the discharge or readmission process? |
Was the intervention tailored to specific hospitals, health professionals or patients or patient groups and, if so, how? Was the intervention modified during the study? |
|
| Early discharge (acute care) | ||||||
| Chevalier 2015 | Service: 'Hospitalisation at Home' service linked to 1 hospital (urology surgery unit) Materials: no information |
Eligibility: urology surgery for prostate cancer. Not taking anticoagulant therapy; with an adenoma prostate less than 80 cc; residing in the territory covered by the service, accompanied by a loved one immediately following surgery to return home. Admission process: during the first urological consultation, the surgeon offers the patient the service. Patients who agree are registered by the urology secretary who emails information on patient to the HAH admission service. Average time to surgery is 15 days. A HAH nurse co‐ordinator had a telephone consultation with the patient 1 week before the surgery to plan the stay. Number of days in acute bed: zero (less than 12 hours in hospital), returns home on the day of surgery. |
Programme manager: no information Medical responsibility: assume urology surgeon from hospital works in collaboration with the lead nurse co‐ordinators. Staff: nurses (including clinical lead nurse co‐ordinators), allied health professionals, social workers, assistant caregivers. All staff employed by the HAH service, which runs in collaboration with the hospital. Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home. Nurses were given a protocol to follow for nursing interventions to ensure HAH is safe and effective for the patients. One example included a protocol for withdrawal of urinary catheter depending on the colour of the urine. Communication process: the patient has the option of calling the HAH service or urology service with 24‐hour number |
HAH length of stay: 2 days HAH visits: visited by a nurse on day 1 and day 2 Discharge process: nurse sends by fax a summary of the treatments carried out to the surgeon on day of discharge |
No information |
| Clarke 2010 | Service: 'Early supported discharge' service linked to 1 hospital's chest clinic Materials: no information |
Eligibility: acute exacerbation of COPD. Resident in the local borough. Admission process: referral to the programme by their respiratory consultant or nursing staff from hospital. Patients had to give informed consent to receive the service. Number of days in acute bed: the programme aimed for discharge to HAH after 3.5 days (the average length of stay for COPD in that hospital was 9.5 days). Participants in this study spent between 2 and 9 days in hospital. |
Programme manager: no information Medical responsibility: no information Staff: 4 nurses with experience in respiratory care, based at a chest clinic attached to the acute care hospital. Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home. Home visits involved clinical assessment and checking that medication was being taken appropriately. Communication process: no information |
HAH length of stay: up to 2 weeks HAH visits: patients were visited at home daily for 3 days and then, as required, up to 2 weeks Discharge process: no information |
No information |
| Collins 2016 | Service: 'Early supported discharge' service linked to 1 hospital Materials: no information |
Eligibility: no information Admission process: patients are given the option of early supported discharge in hospital by hospital staff Number of days in acute bed: no information |
Programme manager: no information Medical responsibility: no information Staff: physiotherapists and occupational therapists. Unclear who they are employed under. Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Dean 2007 | Service: 'Early supported discharge Programme' linked to 1 hospital Materials: no information |
Eligibility: acute exacerbation of COPD Admission process: home care nurse in consult with physician may make the decision to admit. Nurses assess and educate patients suitable for supported discharge. Number of days in acute bed: no information |
Programme manager: no information Medical responsibility: medical staff employed through hospital Staff: nursing employed through hospital. Community team (primary care). Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: 14 days HAH visits: no information Discharge process: discharged to primary care after 14 days |
No information |
| Dinesen 2007 | Service: 'Home hospitalisation' service linked to one hospital. Same service as in Dinesen 2008. Materials: no information |
Eligibility: patients with heart failure, arrythmia and patients up for medicine adjustment. Heart patients were typically past the acute phase of their condition. At the time the patients were selected for home hospitalisation, they were able to walk around without dyspnoea. Admission process: no information Number of days in acute bed: 3 days typically |
Programme manager: no information Medical responsibility: cardiologist. Staff: home ‐ district nurses employed through community. Hospital ‐ nurses and doctors. Training: district nurses were trained in ECG recording and INR measurement techniques in order to carry out HAH duties |
HAH delivery: 1:1, face‐to‐face in the patient's home. Healthcare professionals at the hospital and district nurses enter data on blood pressure, pulse, weight and INR using a web‐portal to transmit patient data between home and hospital. When taking an ECG recording, district nurses also write a brief commentary about the patient's symptoms and transmit this information to the hospital. Communication process: the patients' GPs were informed by fax that their heart patient had been admitted to home hospitalisation. |
HAH length of stay: 3 days typically HAH visits: twice a day Discharge process: in case of emergency (anxiety, complications, etc.), the patient could at any time be re‐admitted to the hospital. Patients may also be instructed to return to the hospital after being assessed by their doctors or the visiting nurse. |
The design panel held a meeting to discuss the experiences and resolve the issues that occurred after the home hospitalisation of 3 patients. These issues included the adjustment and co‐ordination of workflows across sectors, comprehending written documentation by other healthcare professionals on the joint web‐portal as well as the difficulties on the part of the hospital staff to reach the district nurses on the phone. |
| Dinesen 2008 | Service: 'Home hospitalisation' service linked to 1 hospital. Same service as in Dinesen 2007. Materials: no information |
Eligibility: patients with heart failure, arrythmia and patients up for medicine adjustment. Heart patients were typically past the acute phase of their condition. At the time the patients were selected for home hospitalisation they were able to walk around without dyspnoea. Admission process: no information Number of days in acute bed: 3 days typically. (Of the 8 patients interviewed, average = 4.4 days, range 1 to 12.) |
Programme manager: no information Medical responsibility: cardiologist Staff: home ‐ district nurses employed through community. Hospital ‐ nurses and doctors. Training: district nurses were trained in ECG recording and INR measurement techniques in order to carry out HAH duties. |
HAH delivery: 1:1, face‐to‐face in the patient's home. Healthcare professionals at the hospital and district nurses enter data on blood pressure, pulse, weight, and INR using a web‐portal to transmit patient data between home and hospital. When taking an ECG recording, district nurses also write a brief commentary about the patient's symptoms and transmit this information to the hospital. Communication process: the patients' GPs were informed by fax that their heart patient had been admitted to home hospitalisation. |
HAH length of stay: 3 days typically. (Of the 8 patients interviewed, average = 3.8 days, range 1 to 6.) HAH visits: twice a day Discharge process: in case of emergency (anxiety, complications, etc.), the patient could at any time be re‐admitted to the hospital. Patients may also be instructed to return to the hospital after being assessed by their doctors or the visiting nurse. |
The design panel held a meeting to discuss the experiences and resolve the issues that occurred after the home hospitalisation of 3 patients. These issues included the adjustment and co‐ordination of workflows across sectors, comprehending written documentation by other healthcare professionals on the joint web‐portal as well as the difficulties on the part of the hospital staff to reach the district nurses on the phone. |
| Dismore 2019 | Service: nurse‐led 'respiratory specialist service' linked to 3 hospitals Materials: no information |
Eligibility: COPD exacerbation admitted to hospital. Identified as low mortality risk using the Dyspnoea, Eosinopenia, Consolidation, Acidaemia and atrial Fibrillation (DECAF Score 0 to 1). Age 35 years or older. 10 or more smoking pack‐years. Pre‐existing or admission obstructive spirometry. Exclusion: illness (other than COPD) likely to limit survival to less than 1 year. On long‐term ventilation. Has a coexistent secondary diagnosis necessitating admission. Assessed more than one overnight stay after admission or could not provide written informed consent (for trial). Admission process: after a brief inpatient assessment, all patients who met the entry criteria were offered participation. Patients could return home immediately provided the initial arterial pH was 7.35 or more and PaCO2 was 6 kPa or less. Patients with PaCO2 greater than 6 kPa without acidaemia could return home after 1 overnight stay in hospital, provided they were not deteriorating. Patients with acidaemia could return home the day that followed resolution of the acidaemia and, if initiated, once non‐invasive ventilation was complete. Number of days in acute bed: usually transferred to HAH within 24 hours of admission |
Programme manager: unclear Medical responsibility: respiratory consultant (remotely) Staff: respiratory specialist nurse (clinical lead), physiotherapist, psychologist, occupational therapist, social care worker. All employed through hospital. Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home.
Physiological parameters were monitored daily and blood sampling (including arterial blood gas analysis) taken as required. Oral and intravenous therapies, acute controlled oxygen therapy, physiotherapy, psychology, occupational therapy and formal social care were available at home. Communication process: an emergency contact number allowed patients to contact the team 24 hours a day, 7 days a week. |
HAH length of stay: median (IQR): 4 (2 to 5) days. HAH visits: once or twice daily by nurse under remote supervision of respiratory consultant. Unclear how often the other services are provided. Discharge process: the treatment period ended when the respiratory specialist nurse and consultant deemed that the patient was sufficiently well for discharge to the care of the GP. |
No information |
| Dubois 2001 | Service: 'Hospital‐at‐home care' service linked to 4 hospitals (urban and regional) Materials: care protocols developed by hospital physicians for each diagnosis and detailed the minimum care expected from the primary care physician and the home care team. E.g. frequency of home visits and monitoring. |
Eligibility: conditions: heart failure, community‐acquired pneumonia (CAP) and proximal deep venous thrombosis (DVT), lower back pain, IV‐antibiotherapy (IV‐A), chronic leg ulcers, palliative care, oncology, hip replacement Exclusion: psychogeriatric disorders. Patients had to be admitted to one of the participating hospitals for 1 or 2 days to undergo a medical check‐up. Written consent to be treated at home from the patient and family. Admission process: referred by hospital and decision to partake in programme made by patients, informal caregivers/family and primary care physician. Number of days in acute bed: ranged between 1 and 9 days for CAP patients, 1 and 6 days for TVP patients, and 1 and 36 days for IV‐A patients. Only 6 patients were transferred to HAH care during the day of their hospital admission (Day 1), and two‐thirds of HAH care patients were at home at Day 2 or 3 (CAP 69%, DVT 68%, IV‐A 62%). |
Programme manager: no information Medical responsibility: primary care physicians are advised by a hospital physician and team and they work together Staff: nursing care and home help were provided under the responsibility of a nurse from the home care programme Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home. Care protocols discussed between the hospital medical and nursing team and the health professionals directly involved in the care provided at the patients’ home. Communication process: no information |
HAH length of stay: 5 days average. Ranged 2 to 9 days for CAP, 1 to 18 days for IV‐A and 2 to 14 days for DVT. HAH visits: unclear how often they received treatment Discharge process: no information |
No information |
| Jester 2003 | Service: 'Hospital at home' linked to one specialist orthopaedic hospital Materials: no information |
Eligibility: primary diagnosis of OA and booked for hip or knee replacement. Patient agreed to be considered for early discharge into the service. Lived within the defined geographical area. No previous medical history of thromboembolic disease, insulin controlled diabetes, severe cardiac or respiratory disease. No history of dementia, depression or other mental health illness. Access to a telephone within their home. Co‐resident with an adult. Prepared to have the necessary equipment and adaptations made to their home to facilitate early discharge. Prepared to allow access to the service team. The patient’s GP must agree that the patient is suitable for early discharge into the service. Patients choose inpatient or HAH service. Admission process: no information Number of days in acute bed: 4 days (4th postoperative day compared to 12th day for usual care) |
Programme manager: no information Medical responsibility: orthopaedic consultant surgeon. Staff: nurses, physiotherapists employed by hospital Training: when the scheme was set up the team completed a short in‐house training course aiming to enhance multiskilling between nurses and therapists, hence minimising the need for duplication of visits by different healthcare professionals and to help transfer of specialist orthopaedic care into a community setting. |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: patients and carers were advised to contact the on‐call senior nurse at the inpatient centre if they required assistance outside these hours. The HAH team worked a 7‐day week from 08:00 to 20:00 and were contactable by mobile phone between visits. |
HAH length of stay: no information HAH visits: nursing and physiotherapy at least 1 daily Discharge process: no information |
No information |
| Karacaoglu 2021 | Services: 'Acute Care at Home service' based in a community hospital Materials: no information |
Eligibility: over 75 years with geriatric syndromes and either requiring assistance or managing independently with personal care and where support was required during their acute need (or following recovering of an acute condition) Admission process: referrals were received from a geriatric hospital ward once a geriatrician had ensured the patient was medically fit Number of days in acute bed: no information |
Programme manager: service was overseen by a team leader (non‐medical) Medical responsibility: whilst the service did not have exclusive use of a physician, it received professional support and clinical guidance from a consultant geriatrician (geriatrician) working on a discharging acute ward. Staff: advanced nurse practitioner, physiotherapist, occupational therapist, health care support workers, pharmacy technicians Training: focused on frequently utilised skill |
HAH delivery: assumed 1:1, face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: mean (range) 5.2 days (1 to 17) HAH visits: mean (range) 5 (1 to 21) visits. Discharge process: no information |
Operational modifications were required as unable to recruit a geriatrician, resulting in limited acute service admissions. E.g. the inpatient geriatrician had ensured the patient was medically fit. |
| Leung 2016 | Services: 'Home hospitalisation' linked to hospitals (number unclear) Materials: no information |
Eligibility: conditions requiring acute care Admission process: no information Number of days in acute bed: no information |
Programme manager: unclear Medical responsibility: general practitioner (medical lead for follow‐up) had the support of the co‐ordinating physician to ensure continuity of care; where the co‐ordinating physician is at the interface of the hospital teams and general practitioner Staff: nurses, nursing assistants, social workers, physiotherapists, occupational therapists, dieticians, psychologists, coordinating physicians Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home
Co‐ordinated medical and paramedical care Communication process: 24 hour, 7 day a week phone service |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Ranjbar 2015 | Service: 'COPD mobile care programme' based at 1 hospital Materials: no information |
Eligibility: COPD (mild exacerbation). Patients admitted to the medical and pulmonary wards at a university hospital. Ability to communicate in case of an acute worsening of the patients condition (including sufficient Swedish). Exclusions: severe exacerbation, comorbidity (those with acute severe dyspnoea, metabolic, or cardiovascular conditions) Admission process: referral by administrative team according to a screening sheet Number of days in acute bed: no information |
Programme manager: no information Medical responsibility: no information HAH staff: nurses, dieticians, physiotherapists or occupational therapists, all likely employed by hospital Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home. Nurse care includes assessing the patient’s clinical and medical status, inhalation technique and respiratory technique. The patient’s health, information on COPD, and self‐management of COPD are also discussed. If needed, nurses can also facilitate contact with dietitians, physiotherapists or occupational therapists. Communication process: days between visits patients are assessed by phone calls |
HAH length of stay: recommended 14 days HAH visits: nurse visits the patient before hospital discharge, followed by home visits every second day that last about 1 hour. Patients are allowed additional visits if needed. Mean length for this participant pool: 17 (range 7 to 34) days. Discharge process: patients are allowed to participate in the programme more than once, but participation on a regular basis is not recommended. Patients experiencing a worsening in symptoms are readmitted to the hospital. |
No information |
| Rossinot 2019 | Service: 'Hospital‐at‐home' service covering all Paris plus 3 districts of Paris with 20 bases linked to 37 hospitals Materials: no information |
Eligibility: patients suffering from severe, complex and progressive disease(s), but revisable depending on the evolution of their health condition. Examples include cancer, chronic disease, post‐fracture. The presence of at least one caregiver at home and the participation of the general practitioner are recommended before patients come back home, but are not mandatory. Patients may have one or more conditions, accompanied or not by poor social and financial backgrounds. Admission process: arrangements with hospitals and community‐based services are formalised by Hospital at Home and patients are transferred to the service after a medical prescription. Number of days in acute bed: no information |
Programme manager: hospital medical co‐ordinator Medical responsibility: general practitioner HAH staff: broadly includes nurses, assistant nurses, psychologists, physiotherapists. Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home
Medical and paramedical care Communication process: after‐hours phone service |
HAH length of stay: average is 25 days HAH visits: HAH services are available 24 hours a day and 7 days a week Discharge process: no information |
No information |
| Sims 1997 | Service: 'Going home service' linked to 1 hospital Materials: no information |
Eligibility: orthopaedic conditions Admission process: referrals mainly from orthopaedic unit of the main hospital in the region Number of days in acute bed: no information |
Programme manager: no information Medical responsibility: no information Staff: nurse co‐ordinator (clinical lead employed by hospital). Physiotherapist, occupational therapist, district nurses, healthcare support workers (HAH employees) Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home.
Intensive levels of medical, nursing, rehabilitative and social care. Healthcare support workers, under the supervision of and in consultation with the health professionals assisted in the delivery of care. Their tasks included washing and dressing the patient, taking the patient’s temperature, helping with household tasks. Communication process: no information |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Wang 2012 | Service: 'Hospital‐at‐home Programme' linked to 1 hospital Materials: no information |
Eligibility (trial): acute exacerbation of COPD. Inclusion criteria for implementation trial ‐ patients with acute exacerbation of COPD according to the definition adopted by the Global Initiative for Chronic Obstructive Lung Disease and needed hospital admission. Exclusion criteria from trial: life‐threatening respiratory failure; confusion; impaired consciousness; changes in chest x‐ray; comorbidities in need of further inpatient investigation or treatment Admission process: no information Number of days in acute bed: no information |
Programme manager: no information Medical responsibility: pulmonologist Staff: specialist nurse (employed by hospital) Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home.
The nurse evaluated the patients’ clinical status, essential clinical parameters, obtained blood samples for later analysis when needed, and assessed whether or not the patients could still be treated at home. The nurse could consult a pulmonologist in case of worsening of the patients’ symptoms. After the consultation, decisions were made on frequency of follow‐up, therapy changes or readmission to the hospital. Furthermore, the nurse invited the patient and his/her spouse to a dialogue, e.g. she asked how the patient felt and encouraged them to reflect on possible causes of the acute exacerbation and how to prevent it. Communication process: patients had the option to call the hospital at any time if they were concerned about their condition, especially regarding indications for readmission. |
HAH length of stay: 3 days HAH visits: 1‐hour visits from a nurse on each day Discharge process: no information |
No information |
| Early discharge (subacute care or rehabilitation) | ||||||
| Chouliara 2014 | Service: 2 'early supported discharge' services linked to separate hospitals' acute stroke units. Same services as in Cobley 2013. Materials: no information |
Eligibility: stroke. Barthel Index ≥ 14/20. Transfer independently or with assistance of one (± equipment). Sufficiently medically fit to be managed at home. Identified achievable rehabilitation goals. Admission process: patient referred by hospital staff from acute stroke unit Number of days in acute bed: no information |
Programme manager: no information Medical responsibility: physician Staff: nurse, mental health nurse (urban service only), physiotherapist, occupational therapist, speech therapist, social worker (urban service only), clinical psychologist (rural service only), assistant practitioner (urban service only), rehabilitation support worker. Staff who visit the home are employed though the HAH service. Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: 6 weeks general timeline HAH visits: all patients across both early supported discharge services received 1 to 2 visits per day for up to 6 weeks, for 7 days a week Discharge process: if needed, patients are referred on to community services for ongoing support and rehabilitation |
No information |
| Cobley 2013 | Service: 2 'early supported discharge' services linked to separate hospitals' acute stroke units. Same services as in Chouliara 2014. Materials: no information |
Eligibility: stroke. Barthel Index ≥ 14/20. Transfer independently or with assistance of one (± equipment). Sufficiently medically fit to be managed at home. Identified achievable rehabilitation goals. Admission process: patient referred by hospital staff from acute stroke unit Number of days in acute bed: unclear |
Programme manager: unclear Medical responsibility: physician Staff: nurse, mental health nurse (urban service only), physiotherapist, occupational therapist, speech therapist, social worker (urban service only), clinical psychologist (rural service only), assistant practitioner (urban service only), rehabilitation support worker. Staff who visit the home are employed through the HAH service. Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: 6 weeks general timeline HAH visits: all patients across both early supported discharge services received 1 to 2 visits per day for up to 6 weeks, for 7 days a week Discharge process: if needed, patients are referred on to community services for ongoing support and rehabilitation |
No information |
| Cunliffe 2004 | Service: 'Early discharge rehabilitation service' linked to 2 acute hospitals Materials: no information |
Eligibility (trial): medical and surgical patients. Aged 65 or above, reside within the Nottingham Health Authority boundary. Medically fit for discharge. Rehabilitation needs that could be met at home with a home‐based package of care and rehabilitation. Exclusion: people in need of constant or overnight care, those admitted from or discharged to institutional care Admission: referral by hospital staff Number of days in acute bed: no information |
Programme manager: no information Medical responsibility: general practitioner Staff: occupational therapists (2), physiotherapists (2), nurses (3), community care officer liaising with social services (1), rehabilitation assistants (7), secretarial support (1). Team employed by hospital. Training: rehabilitation assistants were care workers or auxiliary nurses who had been trained for this role during the pilot phase by the professional staff. |
HAH delivery: 1:1, face‐to‐face in the patient's home.
Visits were for assessment or monitoring, the provision of rehabilitation therapies, or the provision of assistance and care. Medical care was given by the hospital team while in hospital and by the general practitioner when at home. All standard after‐care services were available, if required. Communication process: no information |
HAH length of stay: up to 4 weeks; average 12 days HAH visits: patients receive up to 4 visits per day, up to 7 days per week, between the hours of 8am and 10pm Discharge process: no information |
The package of care was tailored to individual needs |
| Dow 2007a | Service: 3 'Rehabilitation in the Home' (bed substitution) services linked to hospitals (number unknown). Same services as in Dow 2007b. Materials: no information |
Eligibility: rehabilitation clients with orthopaedic and neurological conditions. Medically stable. Able to benefit from rehabilitation. Home environment had to be assessed for suitability and safety for provision of the rehabilitation programme. Admission: referred from hospital‐based rehabilitation or acute wards and were often admitted to HAH on the day of discharge from hospital Number of days in acute bed: no information |
Programme manager: unclear Medical responsibility: unclear if medical rehabilitation consultant, geriatric medicine specialist or general practitioner (visits patient). Decisions about admission, duration of treatment and discharge from the programme were usually made at team meetings and then communicated to the client by a designated staff member. Staff: case manager. Home care staff included a district nurse, 'meals on wheels' staff, physiotherapists, occupational therapists, nurses, allied health assistants, speech pathologists, social workers, dieticians. All services were brokered by the home rehabilitation service likely not employed by the hospital. Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: case manager managed the administrative aspects of the client’s admission, communicated with the client’s general practitioner (in conjunction with the medical specialist) and communicated team decisions to the client and family. |
HAH length of stay: median days in RITH (range): 25 days (7 to 77) HAH visits: about 1 hour of therapy per day Discharge process: decision made at team meetings and then communicated to the client by a designated staff member |
No information |
| Dow 2007b | Service: 3 'Rehabilitation in the Home' (bed substitution) services linked to hospitals (number unknown). Same services as in Dow 2007a. Materials: no information |
Eligibility: rehabilitation clients with orthopaedic and neurological conditions. Medically stable. Able to benefit from rehabilitation. Home environment had to be assessed for suitability and safety for provision of the rehabilitation programme. Admission: referred from hospital‐based rehabilitation or acute wards and were often admitted to HAH on the day of discharge from hospital. Number of days in acute bed: no information |
Programme manager: no information Medical responsibility: unclear if medical rehabilitation consultant, geriatric medicine specialist or general practitioner (visits patient). Decisions about admission, duration of treatment and discharge from the programme were usually made at team meetings and then communicated to the client by a designated staff member. Staff: case manager. Home care staff included a district nurse, 'meals on wheels' staff, physiotherapists, occupational therapists, nurses, allied health assistants, speech pathologists, social workers, dieticians. All services were brokered by the home rehabilitation service likely not employed by the hospital. Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: case manager managed the administrative aspects of the client’s admission, communicated with the client’s general practitioner (in conjunction with the medical specialist) and communicated team decisions to the client and family. |
HAH length of stay: median days in RITH (range): 25 days (7 to 77) HAH visits: about 1 hour of therapy per day Discharge process: decision made at team meetings and then communicated to the client by a designated staff member |
No information |
| Fisher 2021 | Service: 6 'Early Supported Discharge' Services' linked to 6 sites Materials: no information |
Eligibility: stroke. Across the 6 services, criteria varied and were related to the wider stroke pathway, capacity and resources in the team, and the availability of services to take patients with more severe disability. Admission: some teams took referrals widely, including from GPs and by self‐referral, whereas other teams adhered rigidly to acute hospital referrals only. |
Programme manager: yes for some sites Medical responsibility: unclear Staff: multidisciplinary teams including OT, physios, speech and language therapists, assistant practitioners, clinical support workers, nurses, psychologists, social workers, dietitians, administrators, managers Training: staff training to deliver services varied across sites for nurses, therapists and rehab assistants. One service trained experienced rehab assistants to complete initial holistic assessments, which helped the service to work across a large rural geographical area and meet responsiveness targets. |
HAH delivery: all 1:1, face‐to‐face in the patient's home Communication process: all teams held weekly meetings and routinely collected data for audit and evaluation purposes |
HAH length of stay: mean 47 days (range 9 to 107 days) HAH visits: patients were seen within 24 hours and had a therapy assessment within 72 hours of admission to the team, although mechanisms for achieving these targets varied widely. Most services were 5 days a week, one service was 7 days a week. Discharge process: for one service, patients could be re‐referred to the service for further rehabilitation. For another site, could be re‐referred only if they had a new stroke. |
Models of operation were tailored to each service. |
| Hitch 2020 | Service: 'Early supported discharge' service linked to 1 hospital's inpatient rehabilitation ward Materials: accessible and specific information about the service model and pathway of care was provided to all stroke patients and carers |
Eligibility (trial): stroke. Medically stable post stroke. Considered suitable for safe home discharge. Able to be treated in the home environment and requiring intensive rehabilitation from at least 2 disciplines. Admission: patients were referred by the inpatient rehabilitation ward Number of days in acute bed: no information |
Programme manager: service co‐ordinator Medical responsibility: unclear, included general practitioners and rehabilitation consultant Staff: allied health clinicians, nurses, pharmacists, likely all employed through hospital Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home. Some services included telephone consultations. Communication process: the service team met on a weekly basis to co‐ordinate care provision. |
HAH length of stay: care was provided for 4 weeks, up to 5 days per week HAH visits: session frequency determined by individual patient needs Discharge process: all patients with ongoing rehabilitation needs at the time of discharge from the service were referred on to community‐based rehabilitation services. |
Session frequency determined by individual patient needs |
| Kimmel 2021 | ‘Better at Home service’ – a 3‐month pilot service linked to 1 hospital | Eligibility: participant or next of kin consent; participant having multidisciplinary rehabilitation goals; medically stable to be managed at home (with medical oversight and daily nursing); independent (with carer if available) to manage overnight as the service only provided visits between 8 am and 6 pm Admission: referrals from acute and subacute wards Number of days in acute bed: no information |
Programme manager: unclear Medical responsibility: unclear, included general physicians, rehabilitation specialists and geriatricians Staff: allied health and nursing, employed by the hospital Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: average 14 days HAH visits: at least daily contact with a health professional Discharge process: no information |
No information |
| Kraut 2016 | Service: 'Early supported discharge' services linked to metropolitan hospitals (number unclear) with acute stroke and rehabilitation units Materials: no information |
Eligibility: stroke. No further information. Admission: no information Number of days in acute bed: no information |
Programme manager: unclear Medical responsibility: unclear, included general physicians, rehabilitation specialists and geriatricians Staff: nurses, physiotherapists, occupational therapists, speech pathologists, likely employed by hospital Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Kylén 2021 | Service: 'Early supported discharge' services linked to 3 hospitals stroke units in 3 municipalities Materials: no information |
Eligibility: stroke. Eligibility unclear. Admission process: patients are offered the service if they meet the criteria set out by the stroke unit where they are hospitalised Number of days in acute bed: no information |
Programme manager: no information Medical responsibility: physician (stroke unit) Staff: physiotherapists, occupational therapists, speech and language therapists, physicians and nurses employed by hospital Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home. Multidisciplinary team providing stroke specialist rehabilitation. Communication process: no information |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Lou 2017 | Service: 'Early discharge' services (stroke teams) established at 3 regional hospitals, received referrals from 2 central hospitals with highly specialised stroke units and thrombolysis services Materials: no information |
Eligibility: mild‐to‐moderate stroke symptoms Admission process: no information Number of days in acute bed: 1 to 2 days; range 1 to 6 days |
Programme manager: no information Medical responsibility: no information Staff: nurses, physiotherapists, occupational therapists employed by regional hospital Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home and virtually via telephone Communication process: phone visits available |
HAH length of stay: unclear HAH visits: the stroke team visits each patient 2 to 7 days after discharge to evaluate the patient’s needs and to outline a rehabilitation plan, if needed. The stroke team usually makes 1 to 4 visits (by a physiotherapist, occupational therapist or nurse) to the patient’s home, depending upon the patient’s needs. Discharge process: patients who need further rehabilitation are referred to community‐based rehabilitation services. |
Tailored to patients ‐ based on individual assessments of each patient |
| Moule 2011 | Service: 'Early stroke discharge' service linked to 1 hospital Materials: no information |
Eligibility: stroke Admission process: no information Number of days in acute bed: no information |
Programme manager: a team manager rotated every 3 months across the senior clinical staff Medical responsibility: unclear Staff: occupational therapist (clinical lead), physiotherapists, speech and language therapists, dietitians, nurses. All employed through the hospital. External stakeholders from health and social care sector (not employed by hospital). Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Nordin 2015 | Service: 'Very early supported discharge' service linked to 1 hospital Materials: no information |
Eligibility (trial): stroke. > 18 years. Living within 30 minutes from the stroke unit. On day 2 National Institute of Health Stroke Scale (NIHSS; 0 to 116 points) and Barthel Index (BI) 50 to 99 points; MoCA index < 26 if BI = 100. Exclusion criteria: NIHSS > 16; BI < 50; life expectancy < 1 years (as with severe malignancy. Does not speak or communicate in Swedish prior to incidence. Admission process: early discharge planned at stroke unit meeting. The meeting included the stroke nurse co‐ordinator, health professionals, the patient and sometimes the next of kin participated. Referral by the stroke nurse from hospital stroke unit. Number of days in acute bed: 12 days. (Mean (SD) days in hospital 11.8 (6.7); median (IQR) days in hospital 10 (8 to 15.5)) |
Programme manager: no information Medical responsibility: no information Staff: nurse (clinical lead responsible for discharge planning, co‐ordination of rehabilitation and the contacts with primary health care), physiotherapist and occupational therapist ‐ all employed through hospital). Patients with need for speech therapy received in outpatient clinic. Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: maximum 4 weeks HAH visits: 2 to 4 team visits (stroke nurse, physiotherapist, occupational therapist) per week. Median of 11 visits (IQR 7 to 14) in total. Each visit lasted an average of about 1 hour. Discharge process: patient and the team decided the time to end the intervention within the 4‐week time frame. |
The intervention has a person‐centred approach, which is based on who the person is: their context, their history, their next of kin, their individual strengths and weaknesses. At initial meeting for admission to service, the patients’ needs and wishes were explored and their personal goals with rehabilitation were formulated and decided. |
| Reid 2008 | Service: 'Intermediate care service' linked to 1 hospital and work with clients in their homes and residential aged care facilities Materials: no information |
Eligibility: conditions at risk of leading to hospital admission or residential care. Aged 65 or over. At risk of admission into hospital or residential care. Medically stable and living at home. Admission process: no information Number of days in acute bed: no information |
Programme manager: no information Medical responsibility: unclear if general practitioner Staff: community team including nurses, physiotherapists, formal carers Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home or residential care and via telephone. Short‐term residential options are offered to those requiring 24‐hour care and/or high levels of dependency that cannot be managed in a home setting. Therapy, care and/or nursing care is provided to enable sufficient physical functioning and confidence to return or remain safely at home. Communication process: documentation remains with the client to allow communication between all parties involved in the rehabilitation process. |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| von Koch 2000 | Service: 'Early hospital discharge and continued home rehabilitation' based at a university hospital Materials: no information |
Eligibility: stroke. Patients admitted to Huddinge University Hospital with first or recurrent stroke. One week after onset had impaired motor capacity according to Lindmark Motor Capacity Assessment and/or dysphasia as per Reinvang Aphasia Test. Continent. Independent in feeding according to Katz ADL Index; had a Mini‐Mental State Examination score > 23. Admission process: 5 to 7 days after stroke, all eligible patients were invited to participate in the trial. Number of days in acute bed: 14 days |
Programme manager: no information Medical responsibility: no information Staff: case manager was either occupational therapist, physical therapist or speech therapist. Also consisted of 2 occupational therapists, 2 physical therapists and 1 speech and language therapist. They were regular staff who combined this home rehabilitation service with their usual clinical duties (employed by hospital). Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: case manager co‐ordinated the early discharge procedure, planned and made the necessary preparations for the early discharge, i.e. contacts with the family and/or home help service, adaptation of the patient’s home and ordering of assistive devices, and was the main provider of the services using the other members of the rehabilitation team on a consultative basis. |
HAH length of stay: average 14 weeks, ranged from 4 to 29 weeks after discharge, i.e. until 31 weeks after stroke HAH visits: average of 12 Discharge process: no information |
The intervention had a pragmatic approach, leaving decisions of frequency of visits, choice of activities and duration of the rehabilitation programme to the discretion of the individual case manager in collaboration with the patient and the patient’s family. The team held weekly meetings for co‐ordination of the rehabilitation service. |
| Wallis 2022 | Services:
Hospital at Home and Rehabilitation at Home Both linked to 1 private hospital (multiple‐payer) Materials: preadmission information sessions |
Eligibility: hip or knee replacement surgery (for study) Admission process: referred from acute surgical ward HAH ‐ patients remain admitted as acute patients Number of days in acute bed: HAH 2 days; RAH 4 to 5 days |
Programme manager: physician for HAH Medical responsibility: physician for HAH Staff: HAH ‐ physician, nurse and physiotherapist Staff: RAH ‐ physiotherapist, occupational therapist Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: no information |
Length of stay: HAH ‐ 2 to 3 days RAH ‐ 4 to 6 weeks Visits: HAH ‐ daily RAH ‐ weekly Discharge process: no information |
No information |
| Admission avoidance | ||||||
| Andrade 2013 | Service: 'Home care Programme' linked to 1 hospital's emergency department (1 of 9 services from 9 health districts) Materials: no information |
Eligibility: unclear ‐ deterioration of a clinical medical condition Admission process: referred from Emergency Care Unit |
Programme manager: no information Medical responsibility: physicians (clinical lead) Staff: physicians, nurses, nursing technicians, social workers. All employed through the hospital. Training: study results suggested weaknesses in the training of health professionals in HAH as training is predominantly hospital based. |
HAH delivery: 1:1 or 2:1 (a physician and nurse visited patient together), face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Barnard 2016 | Service: 'Hospital in the Nursing Home' service linked to 3 hospitals Materials: no information |
Eligibility: residents in aged care facilities Admission process: hospital staff attended residential aged care facilities to provide acute assessment and care for residents; and assessment of residents potentially needing emergency transfer. Hospital staff attend the aged care facilities and take a role in determining care requirements, level of required intervention and the establishment of a clinical plan. They also co‐ordinate services when residents did need to attend emergency department, and co‐ordinated inpatient services for residents if admitted to hospital. |
Programme manager: unclear. Assume directors of nursing at aged care facility Medical responsibility: no information Staff: nurses ‐ hospital, residential aged care and liaison officers Training: hospital staff provided training workshops for nursing staff from residential aged care |
HAH delivery: 1:1, face to face in the residential aged care facility Communication process: liaison officers liaised between hospital and residential aged care facilities to act as a point contact for both the hospital and residential aged care to ensure clear communication |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
The intervention was tailored to suit the needs of aged care facilities and their residents |
| Brody 2019 | Service: 'Hospital‐at‐Home Plus', a single home health agency linked to 1 hospital (Plus = 30‐day postacute period of transitional care) Materials: no information |
Eligibility: acute conditions including urinary tract infections, pneumonia, cellulitis, congestive heart failure, exacerbation of COPD and asthma, dehydration, deep vein thrombosis, diverticulitis, hyperglycaemia, hypertension Admission process: emergency department physicians referred patients to HAH. They were also accrued from observation units, outpatient offices, and home‐based primary care programme. |
Programme manager: administrative leaders mentioned, unclear Medical responsibility: physician employed at Mount Sinai Hospital (clinical lead) Staff: physicians, nurse practitioner, nurse, social worker, paramedics, phlebotomists, pharmacists. Some of these are employed by the hospital and others are employed externally by the state of New York, the Visiting Nurse Service of New York, or other companies. Training: HAH‐Plus physicians had to undergo minor training in order to have paramedicine control authority. Nurses employed with the Visiting Nurse Service of New York had to undergo training in order to perform more advanced medical care like placing IVs and performing infusions. |
HAH delivery: 1:1, face‐to‐face in the patient's home Communication process: no information |
HAH length of stay: no information HAH visits: variable, sometimes multiple visits per day Discharge process: following discharge there is a 30‐day post‐acute period of transitional care |
The implementation of the programme was tailored to Mount Sinai Hospital. Including the use of Visiting Nurse Service of New York, paramedics and other healthcare professionals, adapting their electronic health records to suit HAH, and training HAH‐Plus physicians. The home service is usually required to perform a 2‐hour assessment focused on functional and symptom status, and change its policy and implement without an assessment. |
| Cegarra‐Navarro 2010 | Service: 'hospital‐in‐the‐home unit' linked to 1 hospital Materials: every patient receives a written emergency plan that explains the 24‐hour telephone backup service |
Eligibility: stable medical condition that can be managed at home without unexpected emergency interventions. Availability of a carer at home. Appropriate standard of housing. Telephone connection. Patient consent. Admission process: no information on referral process. Patient retains status of a hospital inpatient throughout the period of HAH care. |
Programme manager: unit director Medical responsibility: 2 internal medicine physicians Staff: physicians, 4 nurses Training: no information |
HAH delivery: 1:1, face‐to‐face in the patient's home, with intravenous drugs administered by nurses Communication process: 24‐hour telephone backup service provided by a HAH nurse and director |
HAH length of stay: no information HAH visits: physician‐conducted virtual ward rounds every day. Daily home visits by nurse. Discharge process: formally discharged at the conclusion of HAH treatment. |
No information |
| Crilly 2012 | Service: 'Hospital in the Nursing Home' service linked to 1 major teaching hospital and 36 of 38 aged care facilities in the region Materials: referral forms developed for GPs, staff training and workshop materials |
Eligibility: conditions requiring acute care such as: respiratory, cellulitis, kidney/urinary tract, cardiac, abdominal/GI, viral/sepsis, other Admission process: referred by emergency staff and general practitioners. A lead nurse received referrals, determined appropriateness for admission. The lead nurse also liaises with and supports aged care nurses delivering the service and with patient's general practitioner about their capacity to provide care in the aged care facility. Mean (SD) hours in emergency department = 9.9 (0.7). |
Programme manager: yes, located in the hospital. Also a programme director located in the hospital emergency department Medical responsibility: programme manager (registered nurse) with acute care and community experience HAH staff: nurse (lead) based in the hospital, general practitioners (patient’s GP or after‐hours GP), aged care nursing staff Training: in the initial stages, a programme manager and director developed and organised workshops to upskill aged care staff and GPs, including promotion of service availability and referral process to hospital stakeholders (ED staff, ward staff, outpatient staff) and GP’s. Aged care nursing staff training comprised three main resources: a resource folder, DVDs and support/education from the programme manager. Each aged care facility was provided with a resource folder containing the referral form, contact names and numbers of hospital services and after‐hours GP services and protocol guidelines for clinical pathways for certain illness states (pneumonia, urinary sepsis, dehydration, palliative care, venous/arterial ulcers). The programme manager and director were involved in training aged care staff by leading a 2‐day workshop and liaising with staff to support resident management in the ACF. Registered and enroled Nurses working in aged care facilities were invited to attend a 2‐day workshop in work time. In its first year of operation, 2 such workshops were held with approximately 50 staff attending per workshop. Workshop content was determined by the programme manager and programme director, and overseen by content experts from a steering committee. The workshops included: an introduction to and overview of the service, the role of GPs and aged care staff, an overview of specific illness states (e.g. wounds, gastroenteritis), care updates (e.g. wound care, catheter care, subcutaneous infusion therapy, tracheostomy care, pain control) and special considerations (e.g. swallowing, last days of life, adult guardian, physiotherapy, cognitive failure). Content covered in the workshop was subsequently incorporated into a DVD that was distributed to each aged care facility. |
HAH delivery: 1:1 face‐to‐face in patient’s nursing homes Communication process: nurse lead developed individualised treatment plan for the patient in collaboration with patient’s general practitioner and aged care nursing staff, provided education, medication and equipment required for patient acute care in the aged care facility. Additional care might include wound dressing and observing subcutaneous fluid delivery. If required the nurse lead would provide individualised services and equipment or procedural in‐service for aged care staff receiving care of the patient when transferred from the hospital to the aged care facility. |
HAH length of stay: mean 9.6 days, median 5 days (range 1 to 78) HAH visits: daily by nurse lead and aged care nurses. Programme manager notified the GP and asked them to review the patient within 3 days (if prescribed antibiotics for example). Discharge process: no information |
No information |
| Gorbenko 2023 | Service: 14 new and pre‐existing US HAH Programmes. A waiver provided a fee‐for‐service payment for HAH care in Medicare for the first time. The waiver removed a hospital requirement to provide 24‐hour on‐site nursing. Materials: no information |
Eligibility and admission process: no information, variable across the 14 programmes | Programme manager/medical responsibility: no information, variable across the 14 programmes. Staff: includes (but may not be limited to) physician, advanced care provider, nursing or mobile integrated health provider, in‐home emergency services personnel Training: no information |
HAH delivery: 1:1 remotely or face‐to‐face in the patient’s home. | HAH length of stay: no information HAH visits: (requirement) at least 1 visit by a physician or advanced care provider (remote or in‐person), and at least 2 in‐person nursing or mobile health visits daily Discharge process: no information |
No information |
| Levine 2021 | Service: 'Home hospital' linked to 2 hospitals Materials: no information |
Eligibility (for trial): various acute conditions including cellulitis, heart failure, complicated urinary tract infection, pneumonia, COPD/asthma, other infection, chronic kidney disease, malignant pain, diabetes and its complications, gout flare, hypertensive urgency, previously diagnosed atrial fibrillation with rapid ventricular response, anticoagulation needs, or a patient who desires only medical management that requires inpatient admission, as determined by the emergency room team. Resides within either a 5‐mile or 20‐minute driving radius of emergency department. Has capacity to consent to study, > 18 years old, can identify a potential caregiver who agrees to stay with patient for first 24 hours of admission. Caregiver must be competent to call care team if a problem is evident to her/him. After 24 hours, this caregiver should be available for as‐needed spot checks on the patient. This criterion may be waived for highly competent patients at the patient and clinician's discretion. Exclusion criteria (for trial): undomiciled, no working heat (October to April), no working air conditioning if forecast > 80°F (June to September), or no running water. On methadone requiring daily pickup of medication. In police custody. Resides in facility that provides on‐site medical care (e.g. skilled nursing facility). Domestic violence screen positive. Acute delirium, as determined by the Confusion Assessment Method. Cannot establish peripheral access in emergency department (or access requires ultrasound guidance). Secondary condition: end‐stage renal disease, acute myocardial infarction, acute cerebral vascular accident, acute haemorrhage. Primary diagnosis requires multiple or routine administrations of intravenous narcotics for pain control. Cannot independently ambulate to bedside commode. As deemed by on‐call medical doctor, patient likely to require any of the following procedures: computed tomography, magnetic resonance imaging, endoscopic procedure, blood transfusion, cardiac stress test or surgery. High risk for clinical deterioration. Home hospital census is full (maximum 5 patients at any time). Admission process: Referred from emergency department. After the emergency physician decided to admit a patient, he or she would call the triage hospitalist as per usual protocol. If these physicians agreed that the patient met preliminary inclusion criteria, the home hospital team assessed the patient for eligibility, interest, and consent. |
Programme manager: no information Medical responsibility: general physician (clinical lead and home visits) Staff: physician, nurse, social worker, physiotherapist, occupational therapist, home health aide. All employed through the hospital. Training: all hospital‐based attending physicians received education on the trial and its inclusion criteria |
HAH delivery: 1:1, face‐to‐face in patients’ home. Doctors and nurses provided acute care services expected of a traditional hospital, including respiratory therapies (e.g. oxygen), intravenous medications, imaging studies, and continuous remote monitoring. Participants could receive medical meals and the services of a home health aide, social worker, physical therapist, and/or occupational therapist. All patients had continuous monitoring of temperature, heart rate, respiratory rate, telemetry, movement and falls via a small skin patch. Monitoring was performed through machine‐based algorithms, and clinical staff reviewed any alarms produced by these algorithms as part of their clinical care (delivered to their smartphone). Communication process: patients communicated with their home hospital team via telephone, video and short message service. |
HAH length of stay: no information HAH visits: at least 1 daily visit from an attending general physician and 2 daily visits from a registered nurse with additional visits performed as needed. The physician was available 24 hours a day for urgent issues and visits. Discharge process: Left to the discretion of the home hospital service. Follow‐up after discharge was by design no different than usual care. Urgent responses could occur in less than 20 min and a return to hospital could occur on a case‐by‐case basis. |
No information |
| Mäkelä 2020 | Service: 3 geriatrician‐led "Hospital at home" services (out of 9 participating in trial) linked to acute hospitals, including ambulance services Materials: no information |
Eligibility (for trial): acute medical conditions including falls, delirium, COPD, pulmonary disease, back pain, leg pain, cellulitis, abdominal pain, chest infection, heart failure. 65 years or older. Informed consent. Had been referred to a geriatrician‐led admission avoidance HAH service with CGA and would otherwise require hospital admission. Spoke English. Exclusion criteria (for trial): acute coronary syndrome. Required an acute surgical assessment. Suspected stroke. Receiving end‐of‐life care. Declined admission or were considered by the clinical staff to be too high risk for home‐based care (this could include an unsafe home environment). Lived in residential care setting. Admission process: referred to the trial by the on‐call attending physician of the hospital or one of their team members, emergency department or short stay staff, primary care physicians if recruited from home or ambulance service. Admissions are restricted to Monday to Friday in all but one site, from 0900 to early evening. A trained research nurse working with an attending geriatrician screened admissions to the assessment unit for potentially eligible participants. |
Programme manager: no information Medical responsibility: 2 sites ‐ geriatrician responsible for clinical governance, clinical reviews, supervised trainees, leads on service development, communication with the wider multidisciplinary team, orders investigations, referrals to other specialties and writing prescription. One site ‐ primary care physician had clinical responsibility, the attending geriatrician provided daily specialist advice and guidance, senior medical leadership of the HAH team, facilitated acute diagnostics, referrals to specialists and service development. Staff: geriatrician, nurse practitioners, physiotherapists, occupational therapists, social workers, pharmacists, primary care physicians and primary care team (employed through hospital or primary healthcare). In all but one site the usual primary care physicians and the primary care team are not involved in the delivery of health care during the CGA HAH episode of care. In two sites sessional primary care physicians were directly employed by CGA HAH. Training: training reported but unclear on details |
HAH delivery: 1:1, face‐to‐face in patients’ home. Included comprehensive geriatric assessment and direct access to elements of acute hospital‐based healthcare. Clinical team implements treatment and management recommendations, and if required refers to other services (e.g. older peoples’ mental health services, diagnostic services, social workers, dieticians, speech and language therapy, mental health services, pharmacy support and outpatient follow‐up). Patients have access to inpatient care, general practitioners and the primary healthcare team. The use of intravenous infusions, administration of medication via a pump and 24‐hour care is available in some sites. Nurse practitioners responsible for tasks that are similar to a junior doctor such as differential diagnosis, independent prescribers, request investigations, can take bloods for investigations, plus ECG monitoring, urinary catheterisation, post‐void bladder scanning, dressings to skin lesions, administer IV fluids and IV antibiotics, prescription of rehabilitation. Communication process: nurse practitioners liaise with home care or community teams for onward rehab/supported discharge; liaise with community teams and families. In most sites the community rehabilitation teams and district nurses remained involved in care, and have shared access to HAH electronic patient records. Emergency medical cover is available 24 hours a day. |
HAH length of stay: mean days (range): 6.8 days (1 to 19) for the patients interviewed HAH visits: care is delivered at least daily on weekdays by virtual wards Discharge process: no information |
No information |
| Manning 2016 | Service: 'Early response service' based in a community hospital and linked to a hospital's emergency department Materials: no information |
Eligibility: various acute conditions such as falls and fractures Admission process: referrals received from emergency departments. A nurse liaised with emergency staff. |
Programme manager: no information Clinical lead/responsibility: no information HAH staff: 6 nurses and 6 healthcare support workers. Plus access to a multidisciplinary team of physiotherapists, occupational therapists, a social worker, a speech therapist and the intermediate care consultant via ‘hot clinics’ (rapid access outpatient clinics) Training: no information |
HAH delivery: 1:1, face‐to‐face in patients’ home Communication process: no information |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Papaioannou 2018 | Service: 4 residential aged care homes 'intravenous service' linked to hospitals (number unclear) Materials: an education video for residents, family and aged care staff was created to introduce the study and provide information on the use of clinical pathways and procedures for implementing the service. Nursing staff used an IV therapy manual to implement the service. The manual included a description of their roles and responsibilities, nursing policies and procedures, a nursing checklist for IV therapy administration, monitoring, and discontinuation, troubleshooting issues that arise with IV therapy, prescription referral form and supply requisition form. |
Eligibility: respiratory or urinary tract infections requiring intravenous therapy for antibiotics or hydration Admission process: referred from emergency departments. Triage support provided by a nurse practitioner‐led outreach team to assist with assessment to identify residents most appropriate for this IV service. |
Programme manager: aged care director at each facility Medical responsibility: no information Staff: nurse practitioner (clinical lead), pharmacists, aged care staff employed through the aged care service Training: contracted nursing services provided training for IV therapy and monitoring (tubing changes, PICC dressing changes) including three visits in the first week, 2 visits in the second week and once a week thereafter at no charge. Extra visits if requested were paid for by the aged care service. This nursing training service was available 24/7 for consultation. In addition, if deemed appropriate by the aged care director, group education sessions on IV therapy administration were delivered by the contracted nursing service and available free of charge. Pharmacists were available through the aged care service contracted medical supply company to provide consultation support related to antibiotic use. Note: 3 of the homes did not have prior experience with in‐house intravenous therapy, and 1 home had very minimal experience with initiating intravenous therapy. |
HAH delivery: 1:1, face‐to‐face in patients’ long term aged care homes for intravenous therapy and monitoring Communication process: evidence‐based clinical pathways for the assessment and management of urinary tract infections and respiratory tract infections were put in place before starting the service. This was to facilitate decision‐making to either treat the residents with oral antibiotics or IV antibiotics within the aged care home or send the resident to the emergency department for further investigation and management. |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Rayner 2022 | Service: 2 hospital avoidance programmes for residential care, called Residential in Reach | Eligibility: nursing home resident who requires acute medical care Admission process: referred by the nursing homes |
Programme manager: nurse manager for one service Medical responsibility: Service 1 ‐ geriatrician‐led Service 2 ‐ nurse‐led Staff: clinical nurse specialists, geriatrician, registrars and geriatricians in training, nurse practitioner Training: no information |
HAH delivery: 1:1, face‐to‐face in nursing homes Communication process: no information |
HAH length of stay: no information HAH visits: Service 1 ‐ operated 5 days a week providing: telephone advice; nursing, medical and geriatrician review; diagnostic procedures Service 2 ‐ nurse‐led) operated 7 days a week providing telephone advice, nursing assessment and initiation of treatment. Residents were initially assessed by a clinical nurse specialist and referred to the Hospital in the Home (HITH) service or other specialist services within the larger health service, if they required further management. The HITH service provides hospital care in a person's home or other suitable location, with geriatrician assessment, and management. Discharge process: nurse or geriatrician decides if they need to be admitted to hospital |
No information |
| Schofield 2006 | Service: 'Acute respiratory assessment service' (nurse‐led outreach service) based in a university hospital's respiratory medicine department Materials: no information |
Eligibility (trial): patients with acute uncomplicated exacerbations of COPD Admission process: referred through personal or GP contact and after assessment in the service, experienced hospital admission through emergency department following GP referral or a direct call to the emergency ambulance service |
Programme manager: no information Medical responsibility: consultant respiratory physician Staff: physician, nurses providing outreach service and who are employed by hospital Training: no information |
HAH delivery: 1:1, face‐to‐face in patients' homes Communication process: no information |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Testa 2021 | Service: Aged Care Rapid Response Team linked to 43 residential care facilities Materials: no information |
Eligibility: older people at risk of hospitalisation Admission process: referrals made via telephone. ARRT staff (nurse/registrar) assess and triage the resident |
Programme manager: no information Medical responsibility: hospital‐based geriatrician Staff: hospital‐based geriatrician, an aged care community registrar and 2 clinical nurse consultants Training: the team did upskilling and were mostly senior staff |
HAH delivery: 1:1, face‐to‐face in patient's nursing home. Telehealth could be used to support the assessment and triage process. Communication process: no information |
HAH length of stay: no information HAH visits: usually occur within 24 hours. Services provided include: comprehensive geriatric assessment, treatment of acute infections, liaison with other services e.g. ambulance, mobile x‐ray and ultrasound, falls assessment, pain management and medication review Discharge process: no information |
No information |
| Udesen 2021 | Service: acute Team Odense linked to 1 hospital Materials: no information |
Eligibility: patients in need of short‐term treatment Admission process: most patients referred by GPs (42.2%), municipal staff (26.0%) or hospital staff (14.2%). The remaining patients were referred from the GP out‐of‐hours service, the Emergency Medical Dispatch Centre and others. |
Programme manager: no information Medical responsibility: nurse Staff: nurses employed by the hospital Training: no information |
HAH delivery: 1:1, face‐to‐face in patients' homes Communication process: general practitioners had an important role in this collaboration, as they were the primary contact point for Danish healthcare services that are free of charge. The option to call the service at any time while undergoing treatment |
HAH length of stay: median 1 day, min‐max 1 to 29 days. Mean length for intravenous therapy was 3.3 days. HAH visits: median 1 treatment, min‐max 1 to 45. The team possesses equipment that makes new and flexible solutions in patients’ homes possible (e.g. clinical nurse assessments with paraclinical samples and intravenous therapy). Discharge process: no information |
No information |
| Udesen 2022 | Service: emergency department‐based acute care service linked to 1 hospital Materials: no information |
Eligibility: nursing home residents in Odense Municipality requiring acute care Admission process: the service was activated by the emergency dispatch centre when an ambulance was requested from a nursing home. The first month of the implementation was a pilot period in which the service could be activated 24/7. When the service was not active, the ED consultants treated patients at the ED. Depending on the urgency of the incident, the acute care service was dispatched along with an ordinary ambulance. |
Programme manager: no information Medical responsibility: ED consultant Staff: acute care team, nurse Training: no information |
HAH delivery: 1:1, face‐to‐face in patient's nursing home Communication process: at the nursing homes, the ED consultants collaborated with the municipal acute care team and they performed acute evaluation and treatment on‐site in the nursing home residents’ homes |
HAH length of stay: no information HAH visits: the service operated on weekdays between 8 am and 4 pm. The diagnostic and treatment modalities included point‐of‐care blood sampling, acute ultrasound investigations and intravenous treatment. Discharge process: if the ED consultants felt as though hospital would be a more appropriate place to treat the patients, they were taken to hospital rather than being treated in the nursing home. |
No information |
| Wilson 2002 | Service: 'Hospital‐at‐Home admission avoidance scheme' linked to agency that allocates all acute medical admissions Materials: no information |
Eligibility (trial): acute conditions included chest infection, immobility, diarrhoea and vomiting, cerebrovascular accident, falls, urinary tract infection, acute exacerbation of chronic conditions such as Parkinson’s disease and multiple sclerosis).
Lived in the city of Leicester. Aged over 16 years old. Condition does not require specialist diagnostic investigation. Agreed to receiving HAH. Expected to be ready for discharge before 14 days. GP willing to accept medical responsibility. Required more than 4 hours’ nursing care a day. Admission process: referrals were made by the general practitioner and admitted directly to HAH. General practitioners contacted Bed Bureau (agency in Leicester allocates all acute medical admissions). Bed Bureau then contacted the HAH team, who assessed the patient in the usual way. If the patient was suitable, the HAH team contacted Bed Bureau staff, who randomised patients to HAH or usual hospital care. |
Programme manager: no information Medical responsibility: general practitioner Staff: nurse (clinical lead), physiotherapists, occupational therapists, generic health workers, cultural link worker Training: no information |
HAH delivery: 1:1, face‐to‐face in patients' homes Communication process: no information |
HAH length of stay: median 8 days (all patients discharged by 14 days) HAH visits: daily. Hours of care per day ranged from 4 to 24 hours. Discharge process: maximum length of stay is 14 days |
No information |
| Combined | ||||||
| Ko 2023 | Service: “NUHS@Home”, linked to an academic health institution and general hospital Materials: no information |
Eligibility: included patients who required ongoing hospitalisation. Singaporeans/permanent residents aged 21 years or older, and residence in the western part of Singapore (with predefined area codes). Excluded: (1) clinical criteria ‐ pregnant; on oxygen; acute psychosis or suicidal intent; needed negative pressure isolation; anticipated to deteriorate; planned endoscopy/blood transfusion/cardiac stress test/surgery/interventional radiology; required frequent drug monitoring; ongoing specialist review; required blood sugar monitoring for patients unable to self‐monitor; needed parenteral controlled drugs; and had acute myocardial infarction within the last 5 days. (2) social/functional/safety criteria, e.g. no access to telephone, no caregiver, COVID‐19, drug user Admission process: voluntary. Early discharge patients were identified by screening all patients admitted to the acute medical unit. Admission avoidance patients were identified by screening emergency department patients and referrals from the community nursing team or specialist outpatient clinics. Following discussion with the patients’ primary consultant physician, suitable patients were approached and reviewed by the HAH doctor to confirm that they met inclusion and exclusion criteria. Family members were contacted if patients did not have the capacity to give consent, or upon patient’s request. Number of days in acute bed: for early discharge ‐ median 2 days |
Programme manager: programme co‐ordinator Medical responsibility: HAH physician Staff: physician, nurse, pharmacist and programme coordinator. Hospital‐based clinicians collaborated with private on‐demand medical house‐call services that provided supplementary and after‐hour home visits. Training: no information |
HAH delivery: 1:1, face‐to‐face or videoconferencing in patients' homes or nursing home Communication process: after hours, the attending physician manned an on‐call phone |
HAH length of stay: mean (SD) was 4.5 (3.95) days HAH visits: all nursing and physician visits were performed by a private healthcare provider. A doctor reviewed patients by home visit or over videoconsultation at least once daily. Nurse visited patients on the same day to explain the programme details, care plan, vital signs monitoring and how to call the helpline for assistance. Nurses educated patients or their caregivers on how to use thermometers, blood pressure machines and pulse oximeters for monitoring, and how to receive teleconsultations if required. Intravenous therapy was delivered to patients via nursing home visits at a maximum of 3 times a day Physiotherapists and occupational therapists conducted home visits as clinically indicated Remote vital signs monitoring through a tablet and wireless blood pressure and oxygen meters. Where required, blood samples were drawn in the patient’s home and brought back to the hospital laboratory for processing. Discharge process: When patients fit conventional discharge criteria, they were discharged from the programme to the hospital’s existing post‐discharge transitional care programme. Patients who deteriorated were escalated to acute hospitals. |
No information |
| Lemelin 2007 | Service: 'Hospital in the Home' service linked to 1 hospital's inpatient unit and emergency department Materials: no information |
Eligibility: acute conditions ‐ COPD (32%), cellulitis (11%), diabetes (9%), congestive heart failure (9%). Other diagnoses included: nephritis, alcoholic cirrhosis of the liver, duodenal ulcer with haemorrhage, suspected C difficile enterocolitis, epilepsy, skull fracture and pneumonia. Eligibility (trial) Required acute but non‐critical hospital care. Safe physical and social home environments. Medically and psychiatrically stable. Medical conditions that were manageable within the service limits of the programme. Present minimal risk of needing care at night. Informal caregivers or caregiver networks available. Give consent to participate. Admission process: recruited from 14‐bed inpatient unit or directly from emergency department if they required hospital admission to the inpatient unit. Unclear who recruits them. Number of days in acute bed: average of 6.3 days |
Programme manager: no information Medical responsibility: hospital attending physician (reviewed care as required, throughout the care period) Staff: nurse practitioners (clinical lead, designated principal home care provider and direct care was provided by them almost exclusively, employed specifically for this programme from community. One was seconded from department of family medicine for the period of the study). Other providers also involved include family physicians, pharmacists and physiotherapists. Training: additional nurse practitioners were hired and trained for their role as home care provider; no information on training details. |
HAH delivery: 1:1, face‐to‐face in the patient's home and via telephone. Nurse practitioner performed a physical examination and initiated care provision including rehabilitative and supportive care, education, co‐ordination of services and counselling. Family physicians call group provided after hour coverage for patients as well as backup support to nurse practitioners. Communication process: the nurse practitioner maintained telephone contact until discharge. |
HAH length of stay: unclear HAH visits: daily visits from nurse practitioners immediately after patients transferred home Discharge process: patients were discharged from the service when the team agreed there was no further requirement for hospitalisation |
Provision of care was based on the patient's care needs and was determined in consultation with the family medicine resident, attending staff physician and other healthcare professionals at the time of transfer to the home. |
| O'Neill 2017 | Service: 'Hospital in the Home' service linked to one hospital's inpatient unit and emergency department Materials: staff training materials including policies, procedures, handbooks |
Eligibility: conditions requiring subacute care included urinary tract infection, chest pain, dyspnoea, constipation, delirium, dehydration, falls Admission process: no information Number of days in acute bed: no information |
Programme manager: unclear Medical responsibility: geriatrician assumed. Clinical champions also reported. Staff: specialist in‐reach team, nurses (clinical lead), nurse practitioner, wound specialist personal carers (nursing assistants). Unclear who they are employed through. Training: nursing staff training with access to advanced healthcare individuals or teams, clinical policies and procedures, Australian Medicines Handbook Aged Care Companion, advanced skills training via mandatory face‐to‐face workshops (urinary tract infection, chest pain, dyspnoea, constipation, delirium, dehydration, falls, palliative care). Certificates of clinical competence, learning portfolio records. Encouraged to use continuous learning (online webinars, downloadable Clinical Best Practices Sheets, e‐learning quick task demonstrations, quiz‐based learning assessments, video sessions). |
HAH delivery: 1:1, face‐to‐face in aged care facility Communication process: subacute care based on a traffic light system, whereby colour‐coded parameters were established on assessment documentation to determine a change in health status which then triggered further assessment and treatment. Includes advance care planning, early warning and decision‐support tools, diagnostic equipment, communication tool (Situation, Background, Assessment, Recommendation). |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Vaartio‐Rajalin 2020 | Service: 'Guy's and St Thomas @home service' linked to 2 hospitals. Same services as in Vaartio‐Rajalin 2021. Finland service: Materials: no information England service: Materials: no information |
Finland service: Eligibility: adults or older individuals with acute somatic health problems, including acute health problems linked to chronic somatic or mental health problems Admission: physicians refer patients from acute care unit, or hospital ward, or from a primary health centre, or elderly care service home. HAH nurse visits patients to assess if patient is suitable. Number of days in acute bed: no information England service: Eligibility: main conditions included heart failure, chronic obstructive pulmonary disease, pneumonia, cellulitis, urinary tract infections, resolving delirium, dehydration, hyperemesis, medication titration and blood monitoring. Admission process: referrals are taken directly from hospitals and community‐based health practitioners, including London ambulance service, district nurses and GPs. Number of days in acute bed: no information |
Finland service: Programme manager: unclear Medical responsibility: physicians (GPs or specialised physicians) Staff: registered nurses Training: no information England service: Programme manager: service leader ‐ unclear Medical responsibility: unclear Staff: administrative, physiotherapists, pharmacists, occupational therapists, social workers, drivers, matrons, clinical nurse specialists, registered nurses, nurse assistants Training: no information |
HAH delivery: 1:1, face‐to‐face in patient's home Communication process: no information |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
| Vaartio‐Rajalin 2021 | Service: 'Guy's and St Thomas @home service' linked to 2 hospitals. Same services as in Vaartio‐Rajalin 2020. Finland service: Materials: no information England service: Materials: no information |
Finland service: Eligibility: adults or older individuals with acute somatic health problems, including acute health problems linked to chronic somatic or mental health problems Admission: physicians refer patients from acute care unit, or hospital ward, or from a primary health centre, or elderly care service home. HAH nurse visits patients to assess if patient is suitable. Number of days in acute bed: no information England service: Eligibility: main conditions included heart failure, chronic obstructive pulmonary disease, pneumonia, cellulitis, urinary tract infections, resolving delirium, dehydration, hyperemesis, medication titration and blood monitoring. Admission process: referrals are taken directly from hospitals and community‐based health practitioners, including London ambulance service, district nurses and GPs. Number of days in acute bed: no information |
Finland service: Programme manager: no information Medical responsibility: physicians (GPs or specialised physicians) Staff: registered nurses Training: no information England service: Programme manager: service leader ‐ unclear Medical responsibility: no information Staff: administrative, physiotherapists, pharmacists, occupational therapists, social workers, drivers, matrons, clinical nurse specialists, registered nurses, nurse assistants Training: no information |
HAH delivery: 1:1, face‐to‐face in patient's home Communication process: no information |
HAH length of stay: no information HAH visits: no information Discharge process: no information |
No information |
ACF: aged care facility; ARRT: aged care rapid response team; BI: Barthel Index; CAP: community‐acquired pneumonia; CGA: comprehensive geriatric assessment; COPD: chronic obstructive pulmonary disease; DVT: deep venous thrombosis; ECG: electrocardiogram; ED: emergency department; GP: general practitioner; GI: gastrointestinal; HAH: Hospital at Home; INR: international normalised ratio; IQR: interquartile range; IV: intravenous; IV‐A: intravenous antibiotherapy; MoCA: Montreal Cognitive Assessment; NIHSS: National Institutes of Health Stroke Scale; OA: osteoarthritis; OT: occupational therapist; PICC: peripherally inserted central catheter; RAH: rehabilitation at home; RITH: rehabilitation in the home; SD: standard deviation; TVP: temporary transvenous pacing
Design
Forty‐three studies collected data using individual, group and/or joint interviews (Andrade 2013; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Clarke 2010; Cobley 2013; Collins 2016; Crilly 2012; Cunliffe 2004; Dean 2007; Dinesen 2008; Dismore 2019; Dow 2007b; Dubois 2001; Fisher 2021; Gorbenko 2023; Jester 2003; Karacaoglu 2021; Kimmel 2021; Ko 2023; Kraut 2016; Kylén 2021; Lemelin 2007; Levine 2021; Lou 2017; Mäkelä 2020; Manning 2016; Moule 2011; Nordin 2015; Papaioannou 2018; Ranjbar 2015; Rayner 2022; Reid 2008; Rossinot 2019; Schofield 2006; Sims 1997; Testa 2021; Udesen 2021; Vaartio‐Rajalin 2021; von Koch 2000; Wallis 2022; Wang 2012; Wilson 2002), three studies used focus groups (Barnard 2016; Leung 2016; O'Neill 2017), and six studies used both interviews and focus groups (Brody 2019; Dinesen 2007; Dow 2007a; Hitch 2020; Udesen 2022; Vaartio‐Rajalin 2020). Forty‐nine studies sampled participants purposively such as clinicians delivering the intervention, managers, commissioning staff and hospital staff referring into the service (Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Clarke 2010; Cobley 2013; Collins 2016; Crilly 2012; Cunliffe 2004; Dean 2007; Dinesen 2007; Dinesen 2008; Dismore 2019; Dow 2007a; Dow 2007b; Dubois 2001; Fisher 2021; Gorbenko 2023; Hitch 2020; Jester 2003; Karacaoglu 2021; Kimmel 2021; Ko 2023; Kraut 2016; Kylén 2021; Lemelin 2007; Leung 2016; Levine 2021; Lou 2017; Mäkelä 2020; Manning 2016; Moule 2011; O'Neill 2017; Papaioannou 2018; Ranjbar 2015; Rayner 2022; Reid 2008; Rossinot 2019; Schofield 2006; Sims 1997; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; von Koch 2000; Wallis 2022), and three studies used convenience samples or consecutive participants from a randomised controlled trial (Nordin 2015; Wang 2012; Wilson 2002).
Studies used multiple methods of analysis, with 48 studies using thematic and/or content analyses (Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Clarke 2010; Cobley 2013; Collins 2016; Crilly 2012; Cunliffe 2004; Dean 2007; Dismore 2019; Dow 2007a; Dow 2007b; Dubois 2001; Fisher 2021; Gorbenko 2023; Hitch 2020; Jester 2003; Karacaoglu 2021; Kimmel 2021; Ko 2023; Kraut 2016; Kylén 2021; Lemelin 2007; Leung 2016; Levine 2021; Lou 2017; Mäkelä 2020; Moule 2011; Nordin 2015; O'Neill 2017; Ranjbar 2015; Rayner 2022; Reid 2008; Rossinot 2019; Schofield 2006; Sims 1997; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; von Koch 2000; Wallis 2022; Wang 2012; Wilson 2002), seven studies used grounded theory (Chevalier 2015; Clarke 2010; Kimmel 2021; Leung 2016; Levine 2021; Reid 2008; Rossinot 2019); four studies used constant comparison (Clarke 2010; Cobley 2013; Cunliffe 2004; Levine 2021), one study used a naturalistic enquiry analysis (Papaioannou 2018), one a phenomenologic hermeneutic approach (Dinesen 2008), three studies used theory‐guided analyses including inter‐organisational theory (Dinesen 2007), normalisation process theory (Mäkelä 2020), and Kolcaba’s comfort theory (Manning 2016), and six studies applied theoretical frameworks or models including conceptual framework (Dinesen 2007), Consolidated Framework for Implementation Research (Hitch 2020) and Availability, Accessibility, Acceptability, and Quality of health services framework (Ranjbar 2015), Exploration, Preparation, Implementation, and Sustainment Framework (Gorbenko 2023), Donabedian’s model and the modified Andersen’s health behaviour model (Testa 2021) and the Theoretical Domains Framework (Wallis 2022).
Study participants
Service level
There were 662 staff (where numbers were reported) providing data in 30 studies (Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Crilly 2012; Cunliffe 2004; Dean 2007; Dinesen 2007; Dismore 2019; Dow 2007a; Dow 2007b; Fisher 2021; Gorbenko 2023; Hitch 2020; Karacaoglu 2021; Kraut 2016; Lemelin 2007; Leung 2016; Manning 2016; Moule 2011; O'Neill 2017; Papaioannou 2018; Rayner 2022; Sims 1997; Testa 2021; Udesen 2022; Vaartio‐Rajalin 2020; von Koch 2000). Staff from the hospital, home and residential care settings included nurses, nurse practitioners, allied health (e.g. physiotherapists), assistants, medical practitioners (e.g. hospital physicians, general practitioners), paramedics, service leads, managers and directors.
There were 900 patients (where numbers were reported) providing data in 28 studies (Clarke 2010; Cobley 2013; Collins 2016; Crilly 2012; Cunliffe 2004; Dean 2007; Dinesen 2008; Dismore 2019; Dow 2007a; Dubois 2001; Fisher 2021; Kimmel 2021; Ko 2023; Kraut 2016; Kylén 2021; Levine 2021; Lou 2017; Mäkelä 2020; Manning 2016; Nordin 2015; Ranjbar 2015; Rossinot 2019; Schofield 2006; Udesen 2021; Vaartio‐Rajalin 2021; Wallis 2022; Wang 2012; Wilson 2002); Patient participants either received the Hospital at Home service or were eligible to receive the service, but declined or were not admitted. Patient participants had specific conditions such as stroke (Cobley 2013; Collins 2016; Fisher 2021; Kraut 2016; Kylén 2021; Lou 2017; Nordin 2015), COPD (Clarke 2010; Dean 2007; Dismore 2019; Ranjbar 2015; Schofield 2006; Wang 2012), and heart conditions (Dinesen 2008), or had various conditions such as acute infections (Cunliffe 2004; Dow 2007a; Dubois 2001; Kimmel 2021; Ko 2023; Levine 2021; Mäkelä 2020; Manning 2016; Rossinot 2019; Udesen 2021; Vaartio‐Rajalin 2021; Wilson 2002). Some patient participants had specific procedures such as elective hip and knee replacements (Wallis 2022) or were residents from residential care homes (Crilly 2012).
There were 417 caregivers (where numbers were reported) providing data in 18 studies, including spouses, partners, siblings or other family members (Cobley 2013; Dinesen 2008; Dismore 2019; Dow 2007a; Dow 2007b; Jester 2003; Lou 2017; Mäkelä 2020; Papaioannou 2018; Reid 2008; Rossinot 2019; Schofield 2006; Vaartio‐Rajalin 2021; Wang 2012; Wilson 2002; Ko 2023; Udesen 2021; Wallis 2022).
Systems level
There were seven commissioners providing data (where numbers were reported) in three studies (Chouliara 2014; Fisher 2021; Moule 2011), and one executive leader of a private health insurer in one study (Brody 2019).
Setting
Fifty‐one studies were conducted in 13 high‐income countries including Australia (Barnard 2016; Crilly 2012; Dow 2007a; Dow 2007b; Hitch 2020; Kimmel 2021; Kraut 2016; O'Neill 2017; Rayner 2022; Testa 2021; Wallis 2022), Canada (Lemelin 2007; Papaioannou 2018), Denmark (Dinesen 2007; Dinesen 2008; Lou 2017; Udesen 2021; Udesen 2022), Finland (Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021), France (Chevalier 2015; Leung 2016; Rossinot 2019), Ireland (Collins 2016), Norway (Wang 2012), Singapore (Ko 2023), Spain (Cegarra‐Navarro 2010), Sweden (Kylén 2021; Nordin 2015; Ranjbar 2015; von Koch 2000), Switzerland (Dubois 2001), the USA (Brody 2019; Gorbenko 2023; Levine 2021) and the United Kingdom (Chouliara 2014; Cobley 2013; Clarke 2010; Cunliffe 2004; Dean 2007; Dismore 2019; Fisher 2021; Jester 2003; Karacaoglu 2021; Moule 2011; Mäkelä 2020; Manning 2016; Reid 2008; Schofield 2006; Sims 1997; Wilson 2002). One study was conducted in an upper middle‐income country ‐ Brazil (Andrade 2013).
Thirty‐seven studies were conducted in urban areas (Andrade 2013; Barnard 2016; Brody 2019; Chevalier 2015; Clarke 2010; Collins 2016; Crilly 2012; Cunliffe 2004; Dean 2007; Hitch 2020; Jester 2003; Karacaoglu 2021; Kimmel 2021; Ko 2023; Kraut 2016; Kylén 2021; Lemelin 2007; Leung 2016; Levine 2021; Manning 2016; Moule 2011; Nordin 2015; O'Neill 2017; Papaioannou 2018; Ranjbar 2015; Rayner 2022; Rossinot 2019; Schofield 2006; Sims 1997; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; von Koch 2000; Wallis 2022; Wang 2012; Wilson 2002), three studies in rural areas (Cegarra‐Navarro 2010; Lou 2017; Reid 2008), and 12 studies in both rural and urban areas (Chouliara 2014; Cobley 2013; Dinesen 2007; Dinesen 2008; Dismore 2019; Dow 2007a; Dow 2007b; Dubois 2001; Fisher 2021; Gorbenko 2023; Mäkelä 2020; Vaartio‐Rajalin 2021).
Forty‐five studies were conducted in single‐payer systems (Andrade 2013; Barnard 2016; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Clarke 2010; Cobley 2013; Collins 2016; Crilly 2012; Cunliffe 2004; Dean 2007; Dinesen 2007; Dinesen 2008; Dismore 2019; Dow 2007a; Dow 2007b; Fisher 2021; Hitch 2020; Jester 2003; Karacaoglu 2021; Kimmel 2021; Kraut 2016; Kylén 2021; Lemelin 2007; Leung 2016; Lou 2017; Mäkelä 2020; Manning 2016; Moule 2011; Nordin 2015; O'Neill 2017; Ranjbar 2015; Rayner 2022; Reid 2008; Rossinot 2019; Schofield 2006; Sims 1997; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; von Koch 2000; Wang 2012; Wilson 2002), and seven studies in multiple‐payer systems in the USA (Brody 2019; Gorbenko 2023; Levine 2021), Switzerland (Dubois 2001), Canada (Papaioannou 2018), Singapore (Ko 2023) and Australia (Wallis 2022).
Intervention
Thirty‐one studies reported on Early Discharge Hospital at Home services (Chevalier 2015; Chouliara 2014; Clarke 2010; Cobley 2013; Collins 2016; Cunliffe 2004; Dean 2007; Dinesen 2007; Dinesen 2008; Dismore 2019; Dow 2007a; Dow 2007b; Dubois 2001; Fisher 2021; Hitch 2020; Jester 2003; Karacaoglu 2021; Kimmel 2021; Kraut 2016; Kylén 2021; Leung 2016; Lou 2017; Moule 2011; Nordin 2015; Ranjbar 2015; Reid 2008; Rossinot 2019; Sims 1997; von Koch 2000; Wallis 2022; Wang 2012), 16 studies on Admission Avoidance Hospital at Home services (Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Crilly 2012; Gorbenko 2023; Levine 2021; Mäkelä 2020; Manning 2016; Papaioannou 2018; Rayner 2022; Schofield 2006; Testa 2021; Udesen 2021; Udesen 2022; Wilson 2002), and five studies on Combined Early Discharge and Admission Avoidance Hospital at Home services (Ko 2023; Lemelin 2007; O'Neill 2017; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021). Some studies reported on the same service: Chouliara 2014 and Cobley 2013, Dinesen 2007 and Dinesen 2008, and Dow 2007a and Dow 2007b reported on the same Early Discharge Hospital at Home services, while Vaartio‐Rajalin 2020 and Vaartio‐Rajalin 2021 reported on the same Combined Early Discharge and Admission Avoidance Hospital at Home service.
Early Discharge Hospital at Home services
Fifteen studies reported on acute care (Chevalier 2015; Clarke 2010; Collins 2016; Dean 2007; Dinesen 2007; Dinesen 2008; Dismore 2019; Dubois 2001; Jester 2003; Karacaoglu 2021; Leung 2016; Ranjbar 2015; Rossinot 2019; Sims 1997; Wang 2012) and 16 studies reported on subacute care (Chouliara 2014; Cobley 2013; Cunliffe 2004; Dow 2007a; Dow 2007b; Fisher 2021; Hitch 2020; Kimmel 2021; Kraut 2016; Kylén 2021; Lou 2017; Moule 2011; Nordin 2015; Reid 2008; von Koch 2000; Wallis 2022).
Acute care
Acute care was provided in 14 Early Discharge Hospital at Home services (15 studies) from seven countries including Denmark (Dinesen 2007; Dinesen 2008), Ireland (Collins 2016), France (Chevalier 2015; Leung 2016; Rossinot 2019), Norway (Wang 2012), Sweden (Ranjbar 2015), Switzerland (Dubois 2001) and the UK (Clarke 2010; Dean 2007; Dismore 2019; Jester 2003; Karacaoglu 2021; Sims 1997). Acute exacerbation of COPD was the most common single condition treated in five services (Clarke 2010; Dean 2007; Dismore 2019; Ranjbar 2015; Wang 2012). Treatment of post‐surgery orthopaedic conditions was provided in two services (Jester 2003; Sims 1997), heart conditions in one service (two studies: Dinesen 2007; Dinesen 2008), urology surgery in one (Chevalier 2015), pneumonia and deep vein thrombosis in one (Dubois 2001), complex/progressive diseases such as cancer in one (Rossinot 2019) and various acute conditions in two (Karacaoglu 2021; Leung 2016).
Medical responsibility generally resided with hospital‐based physicians, including a cardiologist (Dinesen 2007; Dinesen 2008), respiratory consultants (Dean 2007; Dismore 2019; Wang 2012), orthopaedic surgeon (Jester 2003) and urology surgeon (Chevalier 2015). In one study, clinical guidance was provided by a hospital‐based geriatrician (Karacaoglu 2021). A co‐ordinating physician was reported in one study (Leung 2016) and a medical co‐ordinator in one study (Rossinot 2019). General practitioners provided care in three services (Dubois 2001; Leung 2016; Rossinot 2019), with the general practitioner having sole medical responsibility in Rossinot 2019, and support of a hospital physician in Dubois 2001 and Leung 2016. Nursing care was provided in all services, including a specialist respiratory nurse (Dismore 2019; Wang 2012), a nurse co‐ordinator (Chevalier 2015; Sims 1997), and a district nurse (Dinesen 2007; Dinesen 2008). Allied health care was provided in eight services (Chevalier 2015; Dismore 2019; Jester 2003; Leung 2016; Ranjbar 2015; Rossinot 2019; Sims 1997; Wang 2012), including social care in three services (Chevalier 2015; Dismore 2019; Leung 2016) and healthcare support workers, in consultation with allied health professionals, assisted in the delivery of care in one (Sims 1997).
Delivery of care was provided one‐to‐one in a patient’s or caregiver's home in all services. Examples of Hospital at Home care for COPD included monitoring of arterial blood gases, intravenous therapy and oxygen therapy (Dismore 2019), evaluation of patient’s inhalation and respiratory technique (Ranjbar 2015), checking that medication was being taken appropriately (Clarke 2010), and advice on self‐management and prevention (Wang 2012). For orthopaedic conditions, examples of care in addition to medical, nursing, rehabilitative and social care, included washing and dressing the patient and helping with household tasks by support workers (Sims 1997). Telephone communication was available via Hospital at Home or hospital (Chevalier 2015; Jester 2003; Rossinot 2019; Wang 2012) or a dedicated 24‐hour emergency service (Dismore 2019; Leung 2016).
Referrals to the service were generally made by hospital medical staff, including a urology surgeon with assistance from their secretary (Chevalier 2015), respiratory consultant (Clarke 2010), geriatrician to ensure the patient was medically fit (Karacaoglu 2021) or administrative staff (Ranjbar 2015). For patients with COPD, eligibility criteria included an age cut‐off of 35 years or older and required a predictive tool score of low risk for mortality (Dismore 2019). For one service for various acute geriatric conditions, eligibility included an age cut‐off of 75 years or older (Karacaoglu 2021). The decision for Hospital at Home admission was reported to require approval of the patient, caregiver or primary care physician in three services (Collins 2016; Dubois 2001; Jester 2003). Hospital acute inpatient length of stay ranged from under 24 hours (Chevalier 2015; Dismore 2019) to about three days (Clarke 2010; Dinesen 2007; Wang 2012). Hospital at Home length of stay ranged from two days (Chevalier 2015) to 25 days (Rossinot 2019). A discharge summary of the treatments provided by Hospital at Home was sent to the urology surgeon on day of discharge (Chevalier 2015).
District nurses were trained in electrocardiogram (ECG) recording and international normalised ratio (INR) measurement techniques and used a web‐portal to transmit patient data between hospital and home, including ECG recordings and blood pressure (Dinesen 2007; Dinesen 2008). Nurses delivering postoperative care for urology surgery followed treatment protocols, such as for withdrawal of urinary catheters depending on the colour of the urine (Chevalier 2015), and primary care physicians and home care teams followed care protocols for various conditions developed by hospital physicians (Dubois 2001). Nurses and physiotherapists received in‐house training in delivery of orthopaedic care at home (Jester 2003).
Subacute care
Subacute care or rehabilitation was provided in 20 early discharge Hospital at Home services (16 studies) from four countries including Australia (Dow 2007a; Dow 2007b; Hitch 2020; Kraut 2016; Kimmel 2021; Wallis 2022), Denmark (Lou 2017), Sweden (Kylén 2021; Nordin 2015; von Koch 2000) and the UK (Chouliara 2014; Cobley 2013; Cunliffe 2004; Fisher 2021; Moule 2011; Reid 2008). Stroke was the most common single condition treated in 14 services (10 studies) (Chouliara 2014; Cobley 2013; Fisher 2021; Hitch 2020; Kraut 2016; Kylén 2021; Lou 2017; Moule 2011; Nordin 2015; von Koch 2000), and various conditions were treated in six services (six studies) (Cunliffe 2004; Dow 2007a; Dow 2007b; Kimmel 2021; Reid 2008; Wallis 2022).
Medical responsibility generally resided with hospital physicians and in four services (five studies) included stroke physicians, rehabilitation consultants and geriatricians (Chouliara 2014; Cobley 2013; Kraut 2016; Kylén 2021; Wallis 2022), and the involvement by general practitioners was unclear (Cunliffe 2004; Dow 2007a; Dow 2007b; Hitch 2020; Reid 2008). Nursing care was provided by 15 services (11 studies) (Chouliara 2014; Cobley 2013; Cunliffe 2004; Fisher 2021; Hitch 2020; Kimmel 2021; Kraut 2016; Kylén 2021; Lou 2017; Moule 2011; Wallis 2022), and a clinical lead nurse was reported in one service (Nordin 2015). Allied health care was provided in all 20 services, including a case manager as a co‐ordinator (Dow 2007a; Dow 2007b; von Koch 2000), occupational therapist as the clinical lead (Moule 2011), social care (Chouliara 2014; Cobley 2013; Cunliffe 2004; Dow 2007a; Dow 2007b; Fisher 2021) and rehabilitation assistants (Cunliffe 2004; Chouliara 2014; Cobley 2013; Dow 2007a; Dow 2007b; Fisher 2021).
Referrals to the service were generally made by hospital staff, such as staff from acute stroke units (Chouliara 2014; Cobley 2013; Fisher 2021; Kylén 2021; Nordin 2015), acute surgical wards (Wallis 2022), and other acute and subacute inpatient wards (Dow 2007a; Dow 2007b; Hitch 2020; Kimmel 2021), or not reported. Eligibility criteria with an age cut‐off included 18 years or older in one service (Nordin 2015) and 65 years or older in two services (Cunliffe 2004; Reid 2008). Eligibility criteria for rehabilitation patients included being medically stable and having rehabilitation goals (Kimmel 2021). Eligibility criteria for patients with stroke also included outcome, screening or predictive tools to guide admission to Hospital at Home such as the Barthel Index and Mini‐Mental State Examination scores (Chouliara 2014; Cobley 2013; Nordin 2015; von Koch 2000). Hospital inpatient length of stay ranged from two days (Lou 2017; Wallis 2022) to 14 days (von Koch 2000). Hospital at Home length of stay ranged from 12 days (Cunliffe 2004) to 14 weeks (von Koch 2000). Regarding discharge, patients needing further rehabilitation were referred on to community‐based services (Chouliara 2014; Cobley 2013; Hitch 2020; Lou 2017). Decisions about discharge were made in team meetings and then communicated to the patient (Dow 2007a; Dow 2007b) or in collaboration with the patient to decide the time to end the intervention within a four‐week time frame (Nordin 2015).
Training for rehabilitation assistants (care workers or auxiliary nurses) during the pilot phase by professional staff was reported in one study (Cunliffe 2004). Training of rehabilitation assistants to conduct initial holistic assessments was included in one service (Fisher 2021). Information about the service model and pathway of care was provided to all patients with stroke and caregivers in one study (Hitch 2020). Documentation remained with the patient to facilitate communication between everyone involved in rehabilitation care, reported in one study (Reid 2008).
Admission Avoidance Hospital at Home services
Acute care was provided by 30 Admission Avoidance Hospital at Home services (16 studies) from seven countries including Australia (Barnard 2016; Crilly 2012; Rayner 2022; Testa 2021), Brazil (Andrade 2013), Canada (Papaioannou 2018), Denmark (Udesen 2021; Udesen 2022), Spain (Cegarra‐Navarro 2010), the USA (Brody 2019; Gorbenko 2023; Levine 2021) and the UK (Mäkelä 2020; Manning 2016; Schofield 2006; Wilson 2002).
Admission avoidance for residents in residential care facilities was provided by seven services (six studies), including Australia (Barnard 2016; Crilly 2012; Rayner 2022; Testa 2021), Canada (Papaioannou 2018) and Denmark (Udesen 2022).
Various acute medical conditions such as cellulitis, heart failure and falls were treated in 14 services (Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Crilly 2012; Levine 2021; Mäkelä 2020; Manning 2016; Wilson 2002; Rayner 2022 (two services); Testa 2021; Udesen 2021; Udesen 2022), COPD in one service (Schofield 2006), and infections of the respiratory tract requiring intravenous therapy for antibiotics or hydration in one (Papaioannou 2018). One study including 14 services did not provide eligibility details (Gorbenko 2023).
Medical staff, such as geriatricians (Mäkelä 2020; Rayner 2022; Testa 2021), physicians (Andrade 2013; Brody 2019), respiratory physicians (Schofield 2006), internal medicine physicians (Cegarra‐Navarro 2010; Levine 2021), emergency department physicians (Udesen 2022) and general practitioners (Crilly 2012; Mäkelä 2020) provided input and medical responsibility. Nursing staff were included in all services, including nurse leads in four services (Papaioannou 2018; Rayner 2022; Udesen 2021; Wilson 2002), nurse practitioners in four (Brody 2019; Mäkelä 2020; Papaioannou 2018; Rayner 2022), clinical nurse consultants (Testa 2021), a registered nurse liaison officer who acted as a point contact for both the hospital and residential aged care facility (Barnard 2016) and nurse technician (Andrade 2013). Allied health care was included in six services (Andrade 2013; Brody 2019; Levine 2021; Mäkelä 2020; Manning 2016; Wilson 2002), with social care included in five services (Andrade 2013; Brody 2019; Levine 2021; Mäkelä 2020; Manning 2016) and pharmacy in one (Papaioannou 2018).
Delivery of care was provided one‐to‐one in a patient’s home or residential care facility. In the patient’s home, acute care services were similar to inpatient hospital care, including comprehensive geriatric assessment (Mäkelä 2020), oxygen therapy and intravenous medications (Cegarra‐Navarro 2010; Levine 2021; Mäkelä 2020; Udesen 2021). Telephone communication was available via Hospital at Home provision (Cegarra‐Navarro 2010; Levine 2021) or via emergency services for out‐of‐hours communication (Mäkelä 2020). In residential care, intravenous therapy, investigations (e.g. ultrasound, x‐ray), blood sampling and monitoring were also included (Crilly 2012; Papaioannou 2018; Testa 2021; Udesen 2022). A nurse developed an individualised treatment plan in collaboration with the patient’s general practitioner and aged care nursing staff and provided education, medication and equipment required for acute care in the aged care facility (Crilly 2012).
Twenty‐seven services were linked to hospital emergency departments, and three services in Australia were linked primarily to residential care facilities with their referrals received from the residential care facilities, primary care or ambulance services (Rayner 2022; Testa 2021). One emergency department‐based service treated patients in the residential care facility with referrals triggered when an ambulance was requested from a nursing home (Udesen 2022). Three services also reported referrals from primary care (Brody 2019; Mäkelä 2020; Udesen 2021; Wilson 2002), and two via ambulance service (Mäkelä 2020; Udesen 2021). Three services reported an age cut‐off, including 16 years or older (Wilson 2002), 18 years or older (Levine 2021) and 65 years or older (Mäkelä 2020). Hospital at Home length of stay was reported for one study with a median stay of one day and range of up to 29 days (Udesen 2021). An additional 30‐day post‐acute period of transitional care following discharge from Hospital at Home was reported for one service (Brody 2019), and follow‐up was left to the discretion of the service in another (Levine 2021).
Upskilling of residential care nurses was included in three services (Barnard 2016; Crilly 2012; Papaioannou 2018), with one service using contracted nursing services to provide training in intravenous (IV) therapy for antibiotics or hydration, and monitoring (tubing changes, dressing changes for peripherally inserted central catheters) as well as pharmacists to provide consultation support related to antibiotic use (Papaioannou 2018). A nurse lead promoted referral processes with general practitioners and hospital emergency staff (Crilly 2012). Physicians from a multiple‐payer service in the USA underwent brief training to have paramedicine control authority, and nurses underwent training in order to perform more advanced medical care, including placing IVs and performing infusions (Brody 2019). For three services involving residential care patients, resources were developed that supported implementation, including treatment protocols, clinical management guidelines, clinical pathways and referral forms (Barnard 2016; Crilly 2012; Papaioannou 2018). In one service, all patients received a written emergency plan explaining the 24‐hour telephone backup service (Cegarra‐Navarro 2010).
Combined Early Discharge and Admission Avoidance Hospital at Home services
Four combined services (five studies) were included from four countries, including Australia (O'Neill 2017), Canada (Lemelin 2007), Finland (Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021) and Singapore (Ko 2023). Acute medical conditions were treated in three services (four studies) (Ko 2023; Lemelin 2007; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021), and subacute care led by nurses for residents in a nursing home in another service (O'Neill 2017), although the conditions treated in O'Neill 2017 also included infections.
Medical responsibility was included in all services, such as geriatricians (O'Neill 2017), general practitioners (Lemelin 2007; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021), physicians (Ko 2023; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021), and a hospital physician with principal responsibility (Lemelin 2007). A programme co‐ordinator was reported in the fourth service (Ko 2023). Nursing care was included in all services, including nurse practitioners in two services (Lemelin 2007; O'Neill 2017), and allied health care in two services (three studies) (Lemelin 2007; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021), including social care in one service (two studies) (Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021).
Delivery of care was provided one‐to‐one in the patient’s home (Ko 2023; Lemelin 2007; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021) or residential care facility (Ko 2023; O'Neill 2017). Nurse practitioners initiated care delivery and maintained telephone contact until discharge, plus had back‐up from a family physicians' call group who also provided after‐hours coverage for patients in one service (Lemelin 2007). In a multiple‐payer service, an attending physician manned an on‐call phone (Ko 2023).
All services were linked to hospital emergency departments, and referrals to the service were from inpatient wards, emergency departments or primary care. Before admission, a Hospital at Home physician or nurse visited the patient to see if they were suitable for the service (Ko 2023; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021). Hospital acute inpatient length of stay was two days for early discharge patients in one service (Ko 2023), and six days for another (Lemelin 2007). Hospital at Home length of stay was 4.5 days in one service (Ko 2023).
One service implemented advanced skills training for aged care nurses via mandatory face‐to‐face workshops (e.g. urinary tract infections) including certification of clinical competence and continuous learning (e.g. online webinars) (O'Neill 2017). Additional nurse practitioners were hired and trained for their role as home care provider in another service (Lemelin 2007). A number of materials were used to support safe and effective care in one service, such as a traffic light system to monitor for deterioration, clinical guidelines, a communication tool (Situation, Background, Assessment, Recommendation) and diagnostic equipment (O'Neill 2017).
Patient populations and their health burden
Stroke was the most common condition, treated in 14 Early Discharge Hospital at Home services (10 studies: Chouliara 2014; Cobley 2013; Fisher 2021; Hitch 2020; Kraut 2016; Kylén 2021; Lou 2017; Moule 2011; Nordin 2015; von Koch 2000). Acute exacerbation of COPD was another common single condition treated in five Early Discharge Hospital at Home services (Clarke 2010; Dean 2007; Dismore 2019; Ranjbar 2015; Wang 2012) and one Admission Avoidance service (Schofield 2006). The remaining services included various acute medical or post‐surgical conditions, including treatment of heart conditions in one service (two studies: Dinesen 2007; Dinesen 2008).
For patients with stroke, findings highlighted the magnitude of the emotional and socioeconomic impact of living with the condition, with ongoing disability (Fisher 2021). Being at home reminded patients with stroke of what was missing and the considerable change in their lives in dealing with the consequences of their new condition, including persistent problems with fatigue, reading and writing, memory loss, mood swings, emotional security and reduced physical capacity that was ‘invisible to the outside world’ (Lou 2017; Nordin 2015). Patients with stroke were focused on rebuilding their physical and mental strength, reading abilities and energy levels in order to return to their pre‐stroke lives as quickly as possible (Fisher 2021; Nordin 2015). This included returning to work, going on holidays and participating in weddings (Nordin 2015), and wanting additional sources of support, such as psychological support, or support from peer support groups (Fisher 2021). Patients with stroke and their caregivers were concerned and frustrated about the future, including fear of a recurrent stroke and being able to recognise future stroke symptoms in order to get to hospital in a timely manner (Lou 2017; Nordin 2015). "I’ll do whatever it takes to improve. Just because I’m so determined and I want to get back on my feet as quickly as I can really." (Patient, Fisher 2021).
Patients with acute medical conditions also described difficulty at home such as reduced mobility and confidence (e.g. getting outdoors), pain, fatigue (especially patients with COPD after hospital stay due to an exacerbation of their condition), social problems such as loneliness and increased dependency upon their informal carers (Clarke 2010; Cunliffe 2004). Patients required ongoing physical and emotional support via community services such as physiotherapy and personal care (Kimmel 2021). Patients with heart conditions described increased awareness of their disease and symptoms as a result of being hospitalised at home, suggesting that they may be more likely to participate in future preventative testing and treatments (Dinesen 2008).
Methodological limitations of the studies
Table 3 reports the methodological limitations of included studies based on the Critical Appraisal Skills Program (CASP) assessment. Overall, 12 studies were assessed as having major concerns (Cunliffe 2004; Dean 2007; Dinesen 2007; Dubois 2001; Jester 2003; Karacaoglu 2021; Lemelin 2007; Leung 2016; Lou 2017; Manning 2016; Sims 1997; Wilson 2002) and 40 studies as having minor concerns (Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Clarke 2010; Cobley 2013; Collins 2016; Crilly 2012; Dinesen 2008; Dismore 2019; Dow 2007a; Dow 2007b; Fisher 2021; Gorbenko 2023; Hitch 2020; Kimmel 2021; Ko 2023; Kraut 2016; Kylén 2021; Levine 2021; Mäkelä 2020; Moule 2011; Nordin 2015; O'Neill 2017; Papaioannou 2018; Ranjbar 2015; Rayner 2022; Reid 2008; Rossinot 2019; Schofield 2006; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; von Koch 2000; Wallis 2022; Wang 2012).
2. Methodological limitations.
| Study |
Was there a clear statement of aims of the research? Is qualitative methodology appropriate? Was the research design appropriate to address the research aims? |
Was the recruitment strategy appropriate to the aims of the research? | Was the data collected in a way that addressed the research issue? | Has the relationship between researcher and participants been adequately considered? | Have ethical issues been taken into consideration? | Was the data analysis sufficiently rigorous? | Is there a clear statement of findings? | How valuable is the research? | Overall |
| Andrade 2013 | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Minor |
| Barnard 2016 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Brody 2019 | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Cegarra‐Navarro 2010 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Chevalier 2015 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Chouliara 2014 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Clarke 2010 | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Cobley 2013 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Collins 2016 | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Crilly 2012 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Cunliffe 2004 | Yes | No | No | No | No | No | Yes | No | Major |
| Dean 2007 | Yes | No | No | No | No | No | Yes | Yes | Major |
| Dinesen 2007 | Yes | No | No | No | No | Yes | Yes | Yes | Major |
| Dinesen 2008 | Yes | No | No | No | Yes | Yes | Yes | Yes | Minor |
| Dismore 2019 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Dow 2007a | Yes | Yes | Yes | No | No | No | Yes | Yes | Minor |
| Dow 2007b | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Dubois 2001 | Yes | No | No | Yes | No | No | Yes | Yes | Major |
| Fisher 2021 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Gorbenko 2023 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Minor |
| Hitch 2020 | Yes | No | No | No | Yes | Yes | Yes | Yes | Minor |
| Jester 2003 | Yes | No | No | No | No | No | Yes | No | Major |
| Karacaoglu 2021 | Yes | No | Yes | No | No | No | Yes | Yes | Major |
| Kimmel 2021 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Ko 2023 | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Minor |
| Kraut 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Kylén 2021 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Lemelin 2007 | Yes | No | No | No | No | No | No | Yes | Major |
| Leung 2016 | Yes | No | No | No | No | Yes | No | No | Major |
| Levine 2021 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Minor |
| Lou 2017 | Yes | No | Yes | No | Yes | No | Yes | Yes | Major |
| Mäkelä 2020 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor |
| Manning 2016 | Yes | Yes | No | No | No | Yes | No | Yes | Major |
| Moule 2011 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Nordin 2015 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| O'Neill 2017 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Papaioannou 2018 | Yes | Yes | No | No | No | Yes | Yes | Yes | Minor |
| Ranjbar 2015 | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Minor |
| Rayner 2022 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Reid 2008 | Yes | Yes | Yes | No | Yes | No | Yes | No | Minor |
| Rossinot 2019 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Schofield 2006 | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Sims 1997 | Yes | No | No | No | No | No | Yes | Yes | Major |
| Testa 2021 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Udesen 2021 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Udesen 2022 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Vaartio‐Rajalin 2020 | Yes | No | Yes | No | Yes | No | Yes | Yes | Minor |
| Vaartio‐Rajalin 2021 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| von Koch 2000 | Yes | No | Yes | No | No | Yes | Yes | Yes | Minor |
| Wallis 2022 | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Minor |
| Wang 2012 | Yes | Yes | No | No | Yes | Yes | Yes | No | Minor |
| Wilson 2002 | Yes | No | No | Yes | No | No | Yes | Yes | Major |
All studies clearly stated the aims of the research, utilised appropriate methodology, and the research design was appropriate for addressing the study aims. Key methodological limitations across studies included a lack of reporting on relationships between the researcher and participants, such as an examination of the researchers own role and potential bias in data collection in 45 studies (Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Clarke 2010; Cobley 2013; Collins 2016; Crilly 2012; Cunliffe 2004; Dean 2007; Dinesen 2007; Dinesen 2008; Dow 2007a; Dow 2007b; Fisher 2021; Hitch 2020; Jester 2003; Karacaoglu 2021; Kimmel 2021; Ko 2023; Kylén 2021; Lemelin 2007; Leung 2016; Lou 2017; Manning 2016; Moule 2011; Nordin 2015; O'Neill 2017; Papaioannou 2018; Ranjbar 2015; Rayner 2022; Reid 2008; Rossinot 2019; Schofield 2006; Sims 1997; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; von Koch 2000; Wallis 2022; Wang 2012); 19 studies did not discuss informed consent or whether ethics approval had been sought (Barnard 2016; Chevalier 2015; Chouliara 2014; Cunliffe 2004; Dean 2007; Dinesen 2007; Dow 2007a; Dubois 2001; Gorbenko 2023; Jester 2003; Karacaoglu 2021; Lemelin 2007; Leung 2016; Levine 2021; Manning 2016; Papaioannou 2018; Sims 1997; von Koch 2000; Wilson 2002); 15 studies did not report sufficient details on data collection, such as data saturation or use of a topic guide (Cunliffe 2004; Dean 2007; Dinesen 2007; Dinesen 2008; Dubois 2001; Hitch 2020; Jester 2003; Lemelin 2007; Leung 2016; Manning 2016; Papaioannou 2018; Ranjbar 2015; Sims 1997; Wang 2012; Wilson 2002); 14 studies did not report a sufficiently rigorous data analysis process, such as a description of the analysis process or present sufficient data to support findings (Andrade 2013; Cunliffe 2004; Dean 2007; Dow 2007a; Dubois 2001; Jester 2003; Karacaoglu 2021; Ko 2023; Lemelin 2007; Lou 2017; Reid 2008; Sims 1997; Vaartio‐Rajalin 2020; Wilson 2002).
Confidence in the review findings
Using GRADE‐CERQual, we assessed 10 findings as high confidence and two findings as moderate confidence (Table 1).
Key concerns were the adequacy of the data in six findings due to a small number of studies contributing to the review findings, including no data from low‐income countries. This included moderate concerns (one finding) and minor concerns (five findings). We had minor concerns about coherence of the data in five findings with some variation in findings across the studies. We had no or very minor concerns with methodological limitations and relevance contributing to the review findings for all findings. Our explanation of the GRADE‐CERQual assessment for each review finding is shown in the GRADE‐CERQual evidence profiles (Appendix 1).
Review findings
The findings were organised into four themes. In the first theme, we presented findings relevant to the development of stakeholder relationships and systems prior to the implementation of Hospital at Home. In the second theme, we presented findings about the processes, resources and skills required to safely and effectively implement Hospital at Home. In the third theme we presented findings relevant to acceptance and caregiver impacts from Hospital at Home. In the fourth theme we presented findings relevant to the sustainability of Hospital at Home.
After considering our sampling criteria, sampling was deemed not to be required, predominantly based on the number of studies. This was to reduce the risk of omitting findings from studies examining the implementation of Early Discharge or Admission Avoidance Hospital at Home. We explored any differences between Admission Avoidance Hospital at Home and Early Discharge Hospital at Home, geographic setting and patient populations under subgroup analyses. Summaries of each finding and their GRADE‐CERQual assessment are available in Appendix 1. Extracted data that exemplified each finding, including the study aim/s, intervention and conditions treated, and study participants are presented in Appendix 4.
Theme 1. Development of stakeholder relationships and systems prior to implementation of Hospital at Home
Implementation of Hospital at Home required early consultation with stakeholders. This included engagement with policy makers who require further evidence about the effectiveness and efficiency of Early Discharge Hospital at Home models and clarity on where they fit in the care pathway to inform commissioning decisions (Chouliara 2014; Fisher 2021).
"Three commissioners requested greater evidence as to whether Early Supported Discharge is the most efficient and effective way of providing rehabilitation and helping patients make the best of their recovery" (Study author, Chouliara 2014). "To be honest I am bit foggy about where early supported discharge sits alongside intermediate care and re‐enablement and how these are married up” (Commissioner,Chouliara 2014).
This finding applied across different services delivered in the home (Brody 2019; Hitch 2020; Moule 2011) and residential care (Testa 2021), including the development of relationships with third party providers that encouraged referrals and enhanced coverage of services (Chouliara 2014). One example included social care and community rehabilitation (such as rehabilitation for people recovering from a stroke) and was necessary to avoid tension between Hospital at Home and existing community specialist roles (Moule 2011).
“We’ve really endeavoured to build up a good relationship with the different organisations and I think the better that is, the better the team runs because you are getting referrals and good understanding” (Team lead, Chouliara 2014).
“When the service started, the health professionals delivering the service perceived that their specialism in stroke rehabilitation created tension between them and the Community Rehabilitation Team” (Study author, Moule 2011).
Engagement with, and active support from, hospital specialists (such as orthopaedics and cardiology) was critical for promotion of referrals to Hospital at Home services and, without this, a lack of confidence from acute hospital staff or teams could negatively impact referrals (Brody 2019; Chouliara 2014; Dinesen 2007; Kraut 2016; Lemelin 2007; Sims 1997). For example, hospital staff were concerned about reduced intensity of rehabilitation with Hospital at Home compared to hospital‐based care (Kraut 2016; Sims 1997).
"I am not sure there was enough 'buy in' from docs; there was subtle resistance to it. That changed over time as more of the attendings came to know us." (Nurse practitioner, Lemelin 2007).
For Hospital at Home services in fee‐for‐service settings, stakeholder engagement extended to funding agencies as the legal and regulatory environment could act as a barrier to the introduction of Hospital at Home (Brody 2019; Gorbenko 2023).
“Key to engage internal stakeholders including legal and regulatory compliance, as well as external partners, very early on in the process" (Study authors, Brody 2019).
In response to the COVID‐19 pandemic, the Centers for Medicare and Medicaid Services (CMS) in the USA approved payment for Acute Hospital at Home Care that did not require a constant nursing presence in the home. However, certain requirements needed to be met, such as two in‐person visits in the home by a nurse and a daily remote or in‐person visit by a physician. An interview study of the implementation of Acute Hospital at Home Care following CMS approval reported that key factors for successful implementation (defined as enrolling patients and improved coverage of services) included establishing new contracts and partnerships with external services already providing home health services, obtaining regulatory approval to deliver medications to a patient’s home, building electronic health record systems to replace outpatient systems, implementing service boundaries to ensure responsiveness for emergency staff if required and ensuring adequate staffing (Gorbenko 2023). After establishing the service, providing more services in‐house with staff employed by the hospital reduced costs and improved the efficiency of Hospital at Home (Gorbenko 2023).
"Both pre‐existing [Hospital at Home] and new programs described challenges implementing waiver components that in some cases delayed them from moving past the preparation stage to implementation" (Study authors, Gorbenko 2023).
Finding 1. Service level staff suggested early stakeholder engagement, including partnerships with third party service providers, was required to implement Hospital at Home. This was critical for implementing new services, overcoming regulatory requirements, building trust and ensuring referrals (high confidence).
Managers reported the inability to capture healthcare provider activity associated with Early Discharge Hospital at Home services within existing systems, and a need to pre‐emptively address this barrier before implementing Hospital at Home (Dismore 2019).
“If we are employing consultants, junior doctors, respiratory nurses, specialists nurses... and we are not having the patient in hospital so we are not getting the tariff for that... somebody has to pay the wage bill... and it’s about understanding that payment mechanism... then that becomes a lot easier for everybody because that is the kind of thing that will stop people moving forward” (Manager, Dismore 2019).
Healthcare service managers reported that the absence of a single billing and payment mechanism was a significant policy and operational barrier to implementing Admission Avoidance Hospital at Home in a multiple‐payer system (Brody 2019). This led to difficulty in signing up additional insurers (Brody 2019). For health services that are not free for patients at the point of delivery, a single billing and payment system was recommended whereby all bills are collated first by the hospital to prevent patients receiving bills from multiple providers and facilitate data capture on total costs and cost savings (Brody 2019).
Healthcare leaders that were not successful in enrolling patients in Hospital at Home struggled with how to calculate and measure financial impact, and financial executives were hesitant to invest until a clear benefit could be demonstrated (Gorbenko 2023). Healthcare leaders that were successful in enrolling patients in Hospital at Home made the business case at their health services by focusing on patients who contribute smaller margins to the hospital if they were admitted as an inpatient (Gorbenko 2023).
“That remains as probably our largest barrier is, I would say, the hospital financial folks are a little hesitant to really approve this because they're not quite sure how to fully calculate and measure financial impact of a program like this” (Healthcare leader, Gorbenko 2023).
Finding 2. For healthcare services planning to implement Hospital at Home, current systems need to integrate activity data and service costs. This allows healthcare services to collate total costs and savings to measure financial impact. This is important as policy makers, hospital executives and insurers from multiple‐payer settings require evidence about the financial impact of Hospital at Home to inform commissioning decisions. For multiple‐payer systems, financial impact and approval could be enhanced by including patients who contribute smaller financial benefits to the hospital if they were an inpatient (moderate confidence).
Theme 2. Processes, resources and skills required to safely and effectively implement Hospital at Home
Patients, caregivers and staff expressed concerns about aspects of safety related to Hospital at Home. Examples included living alone, pain management, restricted mobility (e.g. using their small living spaces), limited space for equipment, their ability to cope and risk of being readmitted (Dismore 2019; Kraut 2016; Kylén 2021; Wallis 2022). Staff also expressed concerns about delivering Hospital at Home due to home hazards, hygiene and risk of injury at work (Dow 2007a), with two staff members required when there was uncertainty around staff safety (e.g. for patients following stroke with alcoholism) (Fisher 2021).
“A common reason for declining participation was fear of being alone when unwell, even when offered (same day) social support" (Study author, Dismore 2019).
“Providing rehabilitation services at home meant that they were sometimes exposed to hazardous home environments, including aggressive dogs. They were also concerned about damaging their backs if they were required to transfer clients on their own or to work off low beds and chairs" (Study author, Dow 2007a).
Patients were reassured about their safety if they were independent with mobility when in hospital. They were also reassured if staff were available to deal with their concerns in person, by phone or via monitoring using technology (e.g. vital signs monitoring via skin patch) and could refer them back to the hospital without delay if necessary (Dean 2007; Dismore 2019; Fisher 2021; Ko 2023; Levine 2021; Lou 2017; Nordin 2015; Ranjbar 2015; Udesen 2021; Wang 2012; Wilson 2002).
"Feeling as if they 'could call [the care team] anytime' as reasons for feeling safe" (Study author, Levine 2021).
Finding 1. Safety concerns were expressed by all stakeholders, such as for patients going home alone in regard to pain management and their mobility, and staff expressed concern for their own safety due to home hazards, patient‐related factors and ergonomics. Patients were reassured about their safety with access to staff (including via phone) and equipment for safe monitoring. Timely delivery of appropriate equipment in the home alleviated some staff concerns (high confidence).
Referrers, such as emergency physicians and staff in acute hospital units, expressed difficulties in consistently identifying suitable patients for Hospital at Home. In part, this reflected a lack of explicit eligibility criteria for some patient populations, including residential care (Udesen 2022). For example, patients attending the emergency department with a range of conditions were challenging for emergency physicians' decision‐making about the suitability of referral and such decisions were time‐consuming (Brody 2019; Chouliara 2014). This required significant training and changes to clinical workflows, such as being able to hold a patient overnight for admission to Hospital at Home (Brody 2019). Other solutions included payment by the Hospital at Home service to existing emergency department physician assistants to work additional overnight shifts to identify potential patients for the service (Brody 2019). There was hesitancy among physicians to refer due to being unfamiliar with the criteria and referral process or due to misconceptions about referrals amongst hospital staff when the Hospital at Home service was being set up (Gorbenko 2023; Moule 2011).
“Misconceptions sometimes arose among ward staff, and the team members reported the need to educate others as to their role and function, and to make clear their criteria to ensure that appropriate patients were being referred to them” (Study author, Moule 2011).
To overcome this, Hospital at Home staff ran teaching sessions on hospital wards or in emergency departments to help staff reliably identify potentially eligible patients and comfortably refer patients (Gorbenko 2023; Moule 2011). However, physicians warned against applying overly restrictive criteria as a degree of clinical judgement was required (Dismore 2019). At times, this lack of clarity led to a delay in referring to Hospital at Home (Dismore 2019).
“It's getting that education piece to where the hospitalists and the emergency physicians are comfortable with referring that patient into this" (Healthcare leader, Gorbenko 2023).
Following referral to Hospital at Home, staff visited the patient to check their suitability for admission (Vaartio‐Rajalin 2020). However, nurse practitioners reported that, on occasions, patients were either too ill for Hospital at Home or did not require the higher level of healthcare provided by Hospital at Home (Lemelin 2007). Healthcare services implemented criteria to exclude certain groups of patients, such as patients with high levels of disability, as this could affect responsiveness of Hospital at Home and services were not able to provide the therapeutic intensity required to address the needs of patients with more severe disability (Fisher 2021). New services also limited admission to specific acute conditions, to target specific patients initially and to allow time to monitor the quality and safety of the intervention before expanding the criteria (Brody 2019; Vaartio‐Rajalin 2020). Sometimes this caused concern with staff working at low capacity for new services during the setup phase as the restrictive eligibility limited the number of patients that could be referred (Moule 2011).
“While some said that the care did not require the expertise of an advanced practice nurse and that their skill set was not optimally utilized in the HITH study, others felt that patients were too ill to be cared for by nurse practitioners outside the hospital" (Study authors, Lemelin 2007).
Finding 2. Identifying patients using eligibility criteria and clinical judgement was challenging for referrers in the acute setting, especially in the start‐up phase of implementation. Services developed criteria to maintain responsiveness and manage capacity, and conducted teaching sessions to help acute staff to refer patients to Hospital at Home. Some services had concerns when staff were working at low capacity (not enough referrals), or if staff were seeing patients that were either too ill, or did not need the higher level of care required for Hospital at Home (high confidence).
Successful implementation of Hospital at Home services included the role of a named clinical champion with clinical knowledge and accessibility as a single point of contact between services (Crilly 2012; Hitch 2020). Co‐ordination between and within services was considered essential to maintain high‐quality care (Brody 2019; Sims 1997). Services that focused on recovery from orthopaedic surgery or neurological conditions reported that co‐ordination was provided by a case manager (Dow 2007b). In another service, emergency department clinical nurse specialists facilitated fast tracking of residents through the emergency department with acute hospital care provided in their residential care facility (Testa 2021).
“I think if we didn’t have a coordinator, it would have fell apart. . . it’s important to have someone who is driving this process and that can be that main point of call to keep things moving along smoothly” (Staff, Dow 2007b).
“It was definitely from the top who drove it" (Residential care registered nurse, Crilly 2012).
Sole medical responsibility for patient care at one time was important to avoid confusion between medical staff in the hospital, Hospital at Home and primary care (Leung 2016; Udesen 2022). To maintain staff morale and quality of care, Hospital at Home managers required operational responsibility to ensure protected time for training and clinical supervision, and to encourage staff to share new ideas and facilitate growth to occur (Crilly 2012; Fisher 2021; Karacaoglu 2021). Health professionals who were champions of the service were also important for successful implementation, such as nurses in charge of inpatient wards, emergency departments or residential care facilities and who could facilitate referrals (Hitch 2020).
“She is really dynamic, very positive and you can see her passion for the whole project and wanting to drive it forward” (Heathcare support worker, Karacaoglu 2021).
Finding 3. Leadership and co‐ordination from key champions, lead clinicians with medical responsibility and clinical accountability, managers with operational responsibility and other leaders were essential to provide high‐quality care. Hospital at Home managers, directors or co‐ordinators were responsible for creating a positive staff environment, ensuring protected time for training and clinical supervision, and facilitating service improvements (moderate confidence).
Successful implementation of Hospital at Home services required funding of a skilled workforce. This included a registered nurse with experience of acute care to communicate at the point of admission to discharge with hospitals, Hospital at Home, residential care facilities if relevant, primary care, patients and carers. For example, a registered nurse acted as a ‘liaison officer’ to improve communication between the hospital, paramedics and residential aged care (Barnard 2016); a specialist stroke nurse enhanced communication with a medical consultant or general practitioner (Fisher 2021). Teamwork was enhanced by regular face‐to‐face meetings and staff rotations across teams to promote a better understanding of each team’s role, training, treatment protocols, processes and support (Chevalier 2015; Chouliara 2014; Fisher 2021; Moule 2011; Sims 1997; von Koch 2000). Following treatment protocols also ensured safe and effective acute medical care (Brody 2019; Chevalier 2015).
“Using the protocol of care made it possible to avoid individual practices not compliant and to respect the rules of good practice” (Study authors, Chevalier 2015).
Multidisciplinary collaborative working was a core feature of Hospital at Home services; at times the lack of integration with social care could undermine this (Moule 2011).
“It was set up with quite an expensive team of therapists and a nurse, but no actual social care input or anyone to carry out personal care, which meant that if the idea was that you take people out who’ve had a stroke earlier than they would otherwise, one would expect that in between the therapists visits they might need some degree of support, but that wasn’t available, that wasn’t thought about and put into the team” (External stakeholder from health and social care sector, Moule 2011).
Challenges existed for Hospital at Home services establishing collaboration with external partners (Brody 2019; Fisher 2021); physicians were frustrated with policy makers due to lack of resource allocation for their role (Vaartio‐Rajalin 2020). Tensions and opportunities arose from a blurring of professional boundaries due to the focus on multidisciplinary team working and task sharing (Moule 2011). This was expressed as a problem by allied health professionals as they utilised their professional manager for support (e.g. annual leave entitlements) and provided a workforce challenge for Hospital at Home managers (Moule 2011). Remote management and budgetary structures, and split roles across hospitals and community providers, could negatively impact on the quality of care by creating delays in care delivery (Moule 2011). Opportunities arose when team members offered unique skill sets such as information technology skills (Moule 2011). For residential care, collaboration between nursing home staff and the acute emergency service helped decision‐making (Udesen 2022). However, without sufficient nursing resources available in some residential care settings, unnecessary referrals or poor communication occurred with the Admission Avoidance service (Rayner 2022).
“Service participants reported instances of nursing home staff contacting them for advice but who were unable to adequately explain what was wrong with the resident and had not undertaken basic nursing assessments" (Study authors, Rayner 2022).
The absence of a waiting list for admission to Hospital at Home was crucial if the service was to adequately respond to the demand for hospital care (Cunliffe 2004), but this risked underutilisation of the service. Services were also challenged to meet guideline targets with limited capacity to treat patients due to travel time. This was worse with workforce shortages (Gorbenko 2023; Karacaoglu 2021; Testa 2021), and when two team members were required to visit patients, which was necessary for some patients with stroke in residential care to prevent readmissions (Fisher 2021). Multiple strategies enhanced capacity and responsiveness including more funding, leasing staff from other services, staff training, training family members, encouraging self‐management, telehealth appointments and delaying admissions (Fisher 2021; Gorbenko 2023; Testa 2021). However, this could affect the provision of patient‐centred care (Fisher 2021). A time‐limited service, for example a maximum of 48 hours for people with COPD, could help keep the service focused on reducing reliance on hospital care (Dean 2007). Arguments against this included the need for flexibility to respond to the local healthcare setting and the varying health needs of the patient population, and that the timing and number of visits were decided in partnership between the staff and patient (Chouliara 2014; von Koch 2000).
“Capacity issues often meant that services relied on staff ‘walking the extra mile’ and maintaining momentum despite the difficulties to meet intensity targets. To quote one of the respondents, teams strived to ‘offer a champagne service on beer money" (Fisher 2021).
"The use of telehealth was noted to greatly increase the ARRT team’s capacity and response time. We’re doing so many video conferences … it’s allowed our capacity to build up because you don't need to go and do the reviews on site. Two [resident] reviews this morning already" (Clinical Nurse Consultant, Testa 2021).
Finding 4. A multidisciplinary skilled workforce was required to implement Hospital at Home, with collaboration between teams and professionals (e.g. via team meetings) a core feature. However, maintaining responsiveness was important, and the absence of a waiting list for admission to Hospital at Home allowed a service to respond to the demand for hospital care. Building rapport with external partners was challenging, and allied health professionals noted difficulties with their professional line of reporting and supervision. Some teams were frustrated by a lack of resource allocation; others recognised that the service was better staffed than usual care. Teams were also challenged to meet intensity targets and address workforce shortages. Multiple strategies could enhance capacity and responsiveness, such as securing more funding, training family members, adopting new technologies and implementing telehealth appointments. However, this could affect the provision of patient‐centred care (high confidence).
Healthcare services leaders reported the need to expand the roles of some healthcare providers (e.g. paramedics, nurses) to facilitate timely administration of medicines and tests as part of Admission Avoidance Hospital at Home services (Brody 2019). Expanding nurses’ roles, including catheter insertion and management of IV medications, was essential to increase the capacity for medical care in the home or residential care and could help avoid admissions (Crilly 2012; Papaioannou 2018; Rayner 2022; Udesen 2022). Also, expanding rehabilitation assistant roles to complete initial assessments and share therapy improved capacity and responsiveness targets for subacute rehabilitation by freeing up clinician time (Fisher 2021). However, some staff worried about the competencies of nursing home staff or rehabilitation assistants to support patients (Fisher 2021; Udesen 2022). Staff could not be employed to work in some Hospital at Home settings without additional training; this could be specific to the acute care provided (e.g. IV therapy) (Papaioannou 2018) or subacute care (e.g. for upskilling nursing staff via workshops and decision support tools) (O'Neill 2017).
“For nurses there was significant changes in operating practices with same‐day and multiple scheduled nursing visits per day, and training and policy change to allow home health nurses to place IVs and perform infusions. Substantial training of the home health nurses, some of whom had never placed IVs or performed infusions, and others who had not done so in years” (Study authors,Brody 2019).
There was an increased emphasis for staff involved with subacute care on learning ‘on the run’ (Hitch 2020), having increased support for junior staff to develop their self‐efficacy (Hitch 2020) and adapting clinicians’ behaviour via providing self‐management advice and reduced input allowing patients more responsibility for self‐management (von Koch 2000). Managers at one service discussed upskilling advanced nurse practitioners with appropriate governance structures due to limited ability to recruit a geriatrician (Karacaoglu 2021).
“With skilled advanced nurse practitioners or advanced nurse practitioners I think is as good a concept, as long as we make sure it is safe and there is clear governance structures within that… it doesn’t have to be a Geriatrician” (Management, Karacaoglu 2021).
General practitioners reported that they required training in how to manage more complex care needs (Leung 2016), as well as nurses perceiving to need a high level of competence when working alone with complex patients (O'Neill 2017). Rapid delivery of equipment and access to medical testing results was also considered essential for supporting delivery of Hospital at Home (Cunliffe 2004; Karacaoglu 2021; Vaartio‐Rajalin 2021). Problems could occur if the equipment was not suitable for use in patients’ homes and/or if alarms were frequent and unnecessary (e.g. from an intravenous pump) (Vaartio‐Rajalin 2021).
Finding 5. Staff training, expansion of roles beyond usual scope of practice and rapid delivery of equipment or medical testing was essential to implement Hospital at Home. Expanding nurse roles increased capacity for acute medical care in the home and residential care. Expanding rehabilitation assistant roles increased capacity for rehabilitation in the home. The expansion of roles required appropriate governance structures and policy changes (high confidence).
Effective methods of communication (this could be a landline in the patient’s home, contact details for the healthcare team or shared electronic medical record) could increase staff confidence, improve collaboration and teamwork and allay concerns about patient safety (Cegarra‐Navarro 2010; Dinesen 2007; Kimmel 2021; Ko 2023; O'Neill 2017; Ranjbar 2015; Udesen 2021; Wallis 2022).
“Having that information at hand [lap top computer] contributes to patient safety both directly and indirectly” … “because doctors can base decisions on the most up‐to‐date information, such as updated medical records” (Physician ‐ Internal medicine, Cegarra‐Navarro 2010).
"An electronic medical record allowed for synchronous communication between district nurses and hospital staff" (Study authors, Dinesen 2007).
Doctors and health professionals providing sufficient information and assurance to patients and caregivers about their suitability for the service helped manage expectations and allay fears about home safety (Wallis 2022). This included a doctor or paramedic managing family expectations to help avoid hospital admissions for residential care patients (Barnard 2016; Testa 2021). Patients and caregivers felt safe at home when they knew that nurses were in direct contact with hospital physicians or general practitioners (Udesen 2021). Practical information was also valued amongst clinicians, for example for locating a patient’s house and obtaining access (Vaartio‐Rajalin 2020).
Poor communication between teams was at risk outside usual working hours with the inability to contact other members of the team, and due to lack of a shared electronic health record and test results (Ko 2023). Duplication of assessments and documentation between hospital and Hospital at Home teams, a lack of a shared health record and inability to contact other members of the team was a source of frustration for staff and could lead to wasted resources in Hospital at Home services (Chouliara 2014; Fisher 2021). In one service, extra staff huddles were required to share patient information when physician and nursing notes were documented in separate electronic medical records (Gorbenko 2023). In another service, general practitioners experienced delays receiving electronic medical records from the emergency team, creating a barrier to continuity of patient care with faster handovers needed (Udesen 2022).
A related theme was the lack of patient involvement and absence of shared documents to facilitate care planning (Mäkelä 2020). Patients and caregivers expressed concern that they did not fully understand how Hospital at Home services work (Fisher 2021), and they required more than written information as it failed to address their needs (Wang 2012).
“There is something about smoking on every page [of the brochure], but I have never smoked” (Patient, Wang 2012).
Confidence in the service was hindered by inadequate communication between clinicians and patients when visits did not take place as planned, if service information was not received in a timely manner, if patients’ home environments were not adequately assessed, and patients had to repeat explanations of their health problems to different staff (Cobley 2013; Collins 2016). Transition between care settings could create problems; for example, discharge from Hospital at Home for patients with stroke could be delayed when social care input was not in place, and inadequate communication could lead to delayed re‐admission to hospital (Chouliara 2014; Dean 2007; Fisher 2021).
Finding 6. Effective communication between staff, patients and caregivers, including documentation and sharing tailored information with patients, was essential to provide efficient and effective care and reassure patients that quality of care is maintained in Hospital at Home. Problems with communication were commonly encountered by patients (e.g. patient information was not tailored), caregivers (e.g. limited opportunities to discuss management with clinicians) and staff (e.g. absence of a shared electronic medical record hampering the sharing of information about patients, efficiency of the service and continuity of care) (high confidence).
Patients and caregivers valued the opportunity to be involved in goal setting, care planning and decisions; some caregivers reported that they were not always included and expressed concern about a lack of consultation (Dow 2007b; Mäkelä 2020).
"No‐one told me beforehand or gave me any warning that he was going to be coming home” (Caregiver, Dow 2007b).
Some patients preferred a high frequency of visits, especially early on when anxiety was highest (Cobley 2013; Jester 2003; Ranjbar 2015). Subacute rehabilitation patients preferred more allied health than nursing or medical visits (Kimmel 2021; Wallis 2022). Some patients with chronic conditions, such as COPD, who were used to self‐managing their condition, considered home visits unnecessary (Clarke 2010), and other patients were overwhelmed with multiple visits from clinicians (Fisher 2021; Kimmel 2021).
For many patients, the home environment was considered more conducive to providing tailored rehabilitation, a higher level of autonomy and independence, and facilitating understanding of the discrepancies between the patient’s goals, environmental demands and caregiver behaviour (Karacaoglu 2021; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021). Findings indicated that these aspects could promote better partnerships between healthcare staff and patients (Andrade 2013; Collins 2016) and that a degree of flexibility was required to provide these services and adapt to the home environment. For example, patients appreciated the clinicians’ ability to adapt care to their unique needs and environments (Levine 2021), and staff might be required to wear ‘many hats’ to cater for patient needs and to focus on other members of the family by supporting caregivers in addition to the patient (Andrade 2013; Vaartio‐Rajalin 2020; Wilson 2002).
“You pick up on things, I think, when we go in to the home environment that would maybe not be picked up in the hospital…maybe move round their furniture, maybe different equipment that we could maybe be using in their own house that is maybe not in situ [in place] that would make their life easier” (Karacaoglu 2021).
Finding 7. Health professionals required skills in delivering person‐centred care, shared decision‐making and tailoring care to achieve patient goals and patient satisfaction. Some caregivers were frustrated about their lack of involvement in decision‐making and care planning. Patients valued equal interactions and partnerships with the staff, and their ability to cater for their needs and valued staff focussing on helping family members (high confidence).
Theme 3. Acceptance, perceived benefits and caregiver impacts from Hospital at Home
Patients, caregivers and healthcare staff from all Hospital at Home settings (including in residential care) believed Hospital at Home services achieved optimal health outcomes and satisfaction for patients (Cobley 2013; Cunliffe 2004; Dinesen 2008; Dow 2007b; Dubois 2001; Fisher 2021; Gorbenko 2023; Karacaoglu 2021; Kimmel 2021; Ko 2023; Kraut 2016; Lemelin 2007; Levine 2021; Lou 2017; Moule 2011; Nordin 2015; Papaioannou 2018; Ranjbar 2015; Rayner 2022; Rossinot 2019; Sims 1997; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; Wallis 2022; Wilson 2002). This was attributed to tailored assessments, advice and rehabilitation in a comfortable and familiar setting for patients and caregivers that facilitated more activity, better sleep, less risk of infections, faster functional recovery, saved trips to the hospital for caregivers, and avoided separating couples and families.
"It is more comfortable to be at home and I feel less ill. I can decide for myself how things should be. I get well faster at home" (Patient, Udesen 2021).
Patients assigned their progress to positive and competent staff who motivated them to reach their goals (Fisher 2021; Kimmel 2021), rather than adopt the ‘sick role’ in hospital (Ko 2023). Healthcare staff, including geriatricians, considered Hospital at Home to be more appropriate for patients with frailty or cognitive impairment as it enabled continuity in their usual routines and avoided confusion, as long as they had the required caregiver support (Ko 2023; Testa 2021; Udesen 2022). Hospital at Home was also perceived to improve equity and access for patients from low‐income and rural settings (Gorbenko 2023). Staff also felt it was more appropriate for people from culturally and linguistically diverse backgrounds who were not familiar with hospital systems (Dow 2007a).
“Staff saw RITH as being advantageous for carers who could be more involved in therapy without the stress of visiting the client in hospital. It was also seen as more appropriate for clients with cognitive impairment and people from culturally and linguistically diverse backgrounds who were not familiar with the Australian hospital system" (Study authors, Dow 2007a)
Specific to Admission Avoidance Hospital at Home, it was believed that the physical distancing prevented catching contagious diseases (Andrade 2013; Levine 2021). Also, nursing staff from residential care believed avoiding admission was less stressful for the family (Rayner 2022), and prevented poor outcomes associated with hospital care such as bed sores, falls, medication errors, confusion due to chemical restraints or being dissatisfied with negative labels such as ‘bed blockers’ by acute hospital staff (Barnard 2016; Papaioannou 2018). Sometimes staff perceived that patient homes were unsuitable (Kraut 2016) and some patients and caregivers felt obliged to agree to Hospital at Home as no other options were available (Rossinot 2019). For multiple‐payer services, a perceived lack of caregiver support at home and unceasing supervision for hospital stays made some patients and caregivers choose to remain in hospital (Ko 2023; Wallis 2022), and some patients undergoing elective surgery preferred to stay in hospital to rest from their daily lives (Wallis 2022).
“… I think the hospital [was] better. Because there will be nurses all down there [the hospital]. If I want to ask something, also can… my wife all make noise already, [asking me] why you cannot stay [in the] hospital" (Patient, Ko 2023).
Finding 1. Patients, caregivers and service level staff believed Hospital at Home (including in residential care) was an appropriate alternative to hospital inpatient care, and facilitated optimal recovery and satisfaction with less risk of hospital‐acquired complications. Patients appreciated positive and competent staff who motivated them to reach their recovery goals. Sometimes the lack of caregiver support and 24‐hour supervision from hospital staff made some patients prefer to stay in hospital (high confidence).
Several studies reported on the impact of caregivers and the crucial role they have in supporting care at home, the resources required to support caregivers in this role and the difficulties they experience in having respite from their caregiving responsibilities (Dow 2007b; Dubois 2001; Fisher 2021; Kimmel 2021; Ko 2023; Reid 2008; Rossinot 2019; Sims 1997; Udesen 2021). Caregivers appreciated the support they received from Hospital at Home staff, but also expressed concern about the nature and extent of support they needed to provide care (such as monitoring patient safety, personal care and exercise support) (Dow 2007b). Caregivers reported stress and disrupted sleep when they were not experienced and did not know how to help the patient (Ko 2023; Wallis 2022). Caregivers wanted to be involved in decisions when they felt the burden of care fell on them, but they felt ignored (Mäkelä 2020; Reid 2008). When a service did not formally identify the caregiver, this was an added strain to caregivers when staff expected them to perform a role (e.g. assist with personal care) as part of the team (Dow 2007b). Working caregivers had to balance caring tasks with work commitments, and preferred to work from home (Ko 2023).
"It is a new experience since I am not medically trained. So, there will be a situation where I don’t know what to do. So, I don’t want to judge the situation wrongly. A bit of stress for me" (Caregiver, Ko 2023).
Caregivers reported that without adequate support and training their role was demanding and could lead to exhaustion when combined with other responsibilities (Rossinot 2019). This was sometimes offset by caregivers avoiding hospital visits (Ko 2023; Udesen 2021). For some conditions, such as neurological conditions, the demands on caregivers could be substantial and patients expressed concern about being a burden (Dubois 2001; Fisher 2021; Rossinot 2019). Staff also highlighted the need to consider the willingness and readiness of caregivers to take on caring responsibility, especially for patients with severe disability (Fisher 2021). Despite these concerns, and with adequate support, patients and caregivers identified advantages of receiving healthcare in their home (Cobley 2013; Ko 2023). The absence of a caregiver living with the patient could be a source of anxiety that was sometimes dealt with by relying on other pre‐existing social networks (e.g. friends, neighbours) (Levine 2021; Mäkelä 2020). A patient’s relationship with close relatives, such as their spouse or child, could be negatively impacted by Hospital at Home, particularly when they had to become involved with personal care (Cobley 2013; Dinesen 2008; Lou 2017), including patients feeling like a burden to their families (Fisher 2021; Udesen 2021; Wallis 2022). A loss of patient privacy from staff (stranger) visits could be a concern for patients and caregivers (e.g. seeing their house untidy) (Dinesen 2008; Dismore 2019; Dubois 2001; Sims 1997; Vaartio‐Rajalin 2020).
"The patient's near‐ones can also become quite tired of having us in their homes for a long period of time, it is understandable… It disturbs their private life and private sphere" (Study authors,Vaartio‐Rajalin 2020).
Finding 2. Caregivers were impacted by Hospital at Home. This included disruption to their normal routines, work, energy and sleep. There were reports of stress and anxiety related to feeling untrained to provide patient support and monitoring, and a lack of formal recognition and access to information. Some caregivers and patients were concerned about their privacy at home and the impact on the patient/caregiver relationship from being involved with care (high confidence).
Theme 4. Sustainability of Hospital at Home
Patients, caregivers and healthcare staff from all settings were in favour of widespread implementation of Hospital at Home. This was due to perceived benefits of Hospital at Home (refer to category 3, finding 1) and the hospital system. System benefits included reduced demands on emergency departments and hospital wards, long‐term financial benefits from avoiding unnecessary hospitalisation, reduced length of stay, increased hospital capacity or bed closures, and ensuring ‘sicker’ patients were treated in hospital (Andrade 2013; Fisher 2021; Gorbenko 2023; Hitch 2020; Moule 2011; Papaioannou 2018; Sims 1997; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021). For established services, expanding the referral options to include more acute departments and primary care practices could improve the health system benefits (Karacaoglu 2021).
“It will be very slow until it feeds into the GP practices. We could take a lot of load from them if they meet us half way” (Karacaoglu 2021).
While dedicated funding was preferred, service level staff described that the funding of Hospital at Home for people following stroke was achieved by closing acute inpatient beds (Moule 2011). However, some patients were sceptical that Hospital at Home was more to do with saving the hospital money than benefiting patients (Dow 2007b). In multiple‐payer settings, cost and insurance were a factor when admitting patients (Ko 2023; Wallis 2022). In these settings, some patients and caregivers expected to be able to choose hospital or home‐based care without additional costs, as they had paid for insurance (Wallis 2022). Other patients and caregivers had to consider if they were willing to pay more for Hospital at Home than if they remained in hospital (Ko 2023; Wallis 2022).
“The main concern will be price, home care, the blood test, MRI, are we going to pay? How much is the cost? And how is the person going to pay? Cash or Medisave [government administered medical savings account]?” (Patient, Ko 2023).
Hospital leaders from multiple‐payer settings felt Hospital at Home programmes showcased a hospital’s innovation and described how the COVID‐19 pandemic shifted policy maker opinions and funding towards Hospital at Home by providing a fee‐for‐service payment for Hospital at Home for the first time (Gorbenko 2023). Hearing of peer institution success with Hospital at Home also increased executive enthusiasm for the programme (Gorbenko 2023). However, hospital leaders remained worried if some Hospital at Home services would remain funded post‐pandemic and wanted more data to support its cost‐effectiveness (Gorbenko 2023). Focus groups consisting of hospital physicians and nurses commented that it was easy to employ staff for Hospital at Home due to the positive perception of the role and service, despite its physical demands (Vaartio‐Rajalin 2020). Spending a lot of time driving affected staff satisfaction, especially for rural sites (Fisher 2021).
"Participants from programs that had been trying to implement Hospital at Home before the waiver described how the pandemic shifted leadership's opinions by demonstrating the 'value…and the success of providing care at home' (Study authors, Gorbenko 2023).
Finding 1. Staff and patients expressed concern that without widespread implementation and expansion, the perceived benefits of Hospital at Home to patients and the healthcare system would be limited. Health system benefits included long‐term financial savings from avoiding unnecessary hospitalisation, bed closures or reduced length of stay, plus increased hospital capacity with reduced waiting times. However, some patients were sceptical that Hospital at Home was more about saving money, and in multiple‐payer settings the costs incurred by a patient were a key factor when admitting patients to Hospital at Home. Peer institution success with Hospital at Home increased executive enthusiasm for Hospital at Home. Hospital at Home could showcase a hospital’s innovation and help sustain staff recruitment. However, staff recruitment may be more challenging in rural settings as excess driving can affect staff satisfaction (high confidence).
Subgroup analysis
Admission Avoidance versus Early Discharge Hospital at Home
Findings were broadly similar between Admission Avoidance and Early Discharge Hospital at Home services. There were similar safety concerns, such as acute hospital ward staff being reluctant to ‘let go’ of patients for early discharge due to safety concerns or risk of readmission (Chouliara 2014; Dinesen 2007). Likewise, emergency staff were reluctant to refer to admission avoidance services due to safety concerns (Brody 2019). Admission criteria also addressed safe home environments for both the patient and the home care staff for both services, such as requiring a working landline (Dean 2007), a caregiver (Lemelin 2007; Levine 2021) and the exclusion of medically unstable patients as well as people affected by drugs/alcohol (Vaartio‐Rajalin 2020). A referrer’s lack of knowledge of eligibility criteria hampered referrals to both Early Discharge and Admission Avoidance services. There was a need to educate hospital ward staff (if Early Discharge) or emergency staff (if Admission Avoidance) to help them identify when referral was appropriate (Brody 2019). Delays in service delivery, such as social care, were a frustration for referring staff from both Early Discharge and Admission Avoidance services, offsetting the benefits of the service (Chouliara 2014; Manning 2016). Leadership from programme managers, clinical champions and informal leaders, as well as the availability of a multidisciplinary workforce with regular team meetings, were required for successful and sustained implementation of both Early Discharge and Admission Avoidance Hospital at Home. Clinical responsibility for Early Discharge and Admission Avoidance Hospital at Home could include hospital physicians, general practitioners or both (Brody 2019; Dismore 2019; Dubois 2001). Intensified workloads were perceived for home care staff in Early Discharge services (Dow 2007b; Hitch 2020) and also for Admission Avoidance staff, particularly when managing complex, frail and medically vulnerable patients, including in the nursing home (O'Neill 2017). Communication concerns, such as no access to general practitioners after hours, or patients lacking comprehensible information, were a common source of frustration across both Early Discharge (Dean 2007) and Admission Avoidance services (Crilly 2012), while good communication was a source of confidence and efficiency for both services. The impacts of Early Discharge and Admission Avoidance services on caregivers were similar for both Early Discharge and Admission Avoidance services, with caregivers being required to perform additional tasks, but they benefited from reduced hospital visits. Reassurance from acute medical staff helped patients' and caregivers' decision‐making and relieved anxiety around Early Discharge or Admission Avoidance (Udesen 2022; Wallis 2022). Also, the importance of patient‐centred care and shared decision‐making, and a general acceptance that Hospital at Home leads to better recovery and less risk of hospital‐acquired complications, and should be implemented widely, were consistent across both services.
Geographic setting
Similar findings were identified between high‐income countries and the upper middle‐income country (Brazil, Andrade 2013), relating to factors that influence the implementation of Hospital at Home services. However, only one study was identified from an upper middle‐income country (Andrade 2013) and there were no studies from low‐income settings identified, so we are uncertain of the differences. Similar findings were also identified between urban and rural services. One exception may be the impact on staff satisfaction when providing Hospital at Home care to rural patients due to larger amounts of driving (Fisher 2021).
For multiple‐payer systems, service‐level staff perceived more communication challenges with establishing collaboration with external home care services such as physiotherapy and pharmacy (Brody 2019). Also, external services (e.g. physiotherapy, pharmacy) did not have access to documentation such as the patient’s chart, limiting written communication for the physiotherapist and order fulfilment for the pharmacy (Brody 2019). There may be other challenges due to the complexity of private health insurance and multiple payers. For example, no reimbursement in the multiple‐payer system was a major barrier to the implementation of Hospital at Home in the USA. In response to the COVID‐19 pandemic, a policy change facilitated implementation by providing a fee‐for‐service payment for Hospital at Home care in Medicare for the first time (Gorbenko 2023). Also, creating a single billing and payment system whereby all bills are required to be collated first by the hospital facilitated data capture on total costs and savings (Brody 2019). This helped sign up additional insurers and/or gain approval from hospital executives to facilitate implementation (Brody 2019; Gorbenko 2023).
For services provided to residents from residential care settings, the impact on caregivers may be less. At home, caregivers were more involved in monitoring and maintaining safety, particularly overnight (Mäkelä 2020). In home settings, some caregivers reported stress, exhaustion, both physical and mental, and feeling close to burnout (Ko 2023; Rossinot 2019), and some caregivers did not want the patient to receive care at home, so they could have relief from their caregiving duties (Vaartio‐Rajalin 2020).
Patient population
Different training requirements for the clinicians were required depending on the patient population. More advanced training of nurses to expand their scope of practice was required to deliver Hospital at Home interventions for patients with acute medical conditions (e.g. providing IV therapy for infections) and to achieve a greater capacity for medical care in a more efficient manner. For managing patients with more complex care needs, general practitioners requested training in complex care management (Leung 2016). For management of patients with subacute conditions (e.g. stroke rehabilitation) there was a greater focus on ‘learning on the run’ and coaching of junior staff (Hitch 2020), and also in‐house competency training for staff managing residents with subacute conditions in a nursing home (O'Neill 2017).
Results of integrating the review findings with the Cochrane intervention reviews of Early Discharge Hospital at Home and Admission Avoidance Hospital at Home
Of the 52 qualitative studies, four (Cunliffe 2004; Dismore 2019; Nordin 2015; von Koch 2000) were conducted alongside a randomised trial of Early Discharge Hospital at Home and three (Levine 2021; Mäkelä 2020; Wilson 2002) Admission Avoidance Hospital at Home. The Early Discharge Hospital at Home intervention review reported limited evidence of economic benefit through a reduction in hospital length of stay, or of improved health outcomes (Goncalves‐Bradley 2017). The recently updated Admission Avoidance Hospital at Home review reported that Admission Avoidance Hospital at Home, with the option of transfer to hospital, may provide an effective alternative to inpatient care for a select group of older people who have been referred for a hospital admission (Edgar 2024).
Our updated logic model is presented in Figure 1. We also organised the findings from our qualitative evidence synthesis to reflect the timeline for planning and implementing Hospital at Home services, categorising factors as those that support effective implementation (Figure 3) and those that might limit effectiveness (Figure 4). Prior to implementation, identifying how Hospital at Home services fit with existing care pathways, regulation, governance, budgets and existing workload will help to ensure that the services function as intended, ensure appropriate referrals and facilitate integration with existing services; early engagement with hospital and community healthcare staff can help with this. A recognised clinical champion, prompt delivery of equipment and assessment of patients using a clinical record that is shared by healthcare providers from different sectors facilitates the set‐up and delivery of Hospital at Home care and increases confidence in the service. A crucial element is training staff to equip them with the skills to adopt an extended role and support teamwork and task sharing, and the impact of these services on the existing workforce (Leary 2022). The benefits of receiving health care in the home are widely understood to support a faster recovery, but this could be undermined by a lack of support for carers who are involved in the provision of care and the risk that the demands for care might negatively impact on their relationship with the patient.
3.
Factors that support the effective implementation of Hospital at Home.
4.
Factors that limit the effective implementation of Hospital at Home.
Discussion
Summary of the main findings
Following synthesis of 52 qualitative studies exploring the implementation of Hospital at Home services (31 Early Discharge, 16 Admission Avoidance, five combined services), from the perspectives of clinicians, managers, commissioners, patients and caregivers, we graded 12 findings as high confidence (n = 10) and moderate confidence (n = 2). We classified the 12 findings into four themes: (1) development of stakeholder relationships and systems prior to implementation (two findings), (2) processes, resources and skills required for safe and effective implementation (seven findings), (3) acceptability and caregiver impacts (two findings) and (4) sustainability (one finding). For a summary of the main qualitative findings, see Table 1.
Comparison with other reviews and implications for the field
A previous qualitative evidence synthesis of 16 studies (including 11 studies included in our qualitative evidence synthesis) examined factors impacting on the quality and transferability of Hospital at Home services to develop and improve Hospital at Home (Chua 2022). There were similarities in findings related to the importance of patient‐centred care, support for caregivers, clinician training, communication, continuity of care, clinician collaboration and co‐ordination of care. However, our review extends these findings, for example by comparing findings between Admission Avoidance Hospital at Home and Early Discharge Hospital at Home and identifying similarities in factors affecting implementation between these two models of care, as well as similarities between diverse geographical settings such as high‐income countries versus upper middle‐income country, and between urban and rural settings.
A key difference identified in our review concerned the training requirements of staff depending on the patient population being cared for, such as acute versus subacute, or management of specific conditions (e.g. post‐surgical) versus a variety of conditions or complex conditions. For acute care, one key difference we identified related to the need for advanced training of nurses to deliver an admission avoidance service or early discharge service for patients with more acute conditions. Additional training in ECG recording and delivery of IV therapy was required for nursing staff managing acute conditions (Papaioannou 2018). Advanced training of nurses may improve efficiency and maximise capacity for acute medical care for Admission Avoidance Hospital at Home services and Early Discharge Hospital at Home services managing more acute conditions. For subacute care, upskilling of staff could be via in‐house workshops, or adapting the approach of allied health clinicians by delivering more self‐management advice (von Koch 2000), learning 'on the run' (Hitch 2020) and junior staff being supported by more experienced staff (Hitch 2020). For specific conditions, employing specialist nurses (e.g. respiratory nurses for managing exacerbations of COPD) or, for complex conditions, employing advanced practice nurses or experienced nurses, may mitigate the need for training. However, training of primary care GPs in managing complex conditions requires close attention to effectively deliver Hospital at Home (Leung 2016).
A key challenge to the implementation of Hospital at Home identified in our review concerned the admission and referral process. Unwillingness of patients and caregivers to be admitted to the service, and reluctance to refer from hospital physicians and acute hospital staff were barriers. These findings converged with the previous qualitative evidence synthesis (Chua 2022), and primary quantitative data indicating that 20% of patients declined Early Discharge Hospital at Home because they felt safer in hospital and 20% found it easier to remain in hospital (Levine 2022). This issue is particularly important as it relates to the sustainability of the service; if patients are not referred, if patients are not willing or if patients with a lower dependency than planned are referred, it is unlikely to be an alternative service for a hospital admission. Differences in opinion exist between hospital clinicians, suggesting that they may not embrace the idea of Hospital at Home depending on their own experience, attitudes and ‘ethos’ of care. We did not find this was limited to a particular specialism (e.g. cardiology versus gerontology). Early engagement of stakeholders, clinical champions and promotional work was identified as an enabler and is similar to a finding identified in another review investigating implementation of Mental Health Hospital at Home where engagement of psychiatrists during the early phase of implementation helped promote referrals (Towicz 2021).
Specific to conditions such as stroke, exacerbation of COPD and heart conditions, the negative impact of disease on patients and caregivers emerged and requires attention when discharging patients from Hospital at Home into the community. This finding converges with findings from a recent qualitative evidence synthesis (14 studies) exploring the experience of stroke patients receiving Early Discharge Hospital at Home (Connor 2022). Patients receiving Hospital at Home face an increased awareness of their condition that they need to confront, with ongoing impairments and disability such as reduced mobility and confidence (e.g. getting outdoors), pain and fatigue that is likely to require further testing and preventative treatments. While patients have a positive experience of Hospital at Home in an environment they perceive to optimise their rehabilitation, the transition to community care was difficult, suggesting that the negative impact of diseases following discharge from Hospital at Home requires attention.
Overall completeness and applicability of the evidence
Despite the inclusion of 52 studies, only two studies included the perspectives of systems‐level stakeholders (nine participants where reported). Despite limited views at the systems level, our findings shed light on the uncertainty that commissioners and policy makers have about the effectiveness and financial impact of Hospital at Home, and where these services fit within the context of other hospital‐ and community‐based care. Effectiveness reviews have highlighted the clear benefits to patients and hospital systems (Goncalves‐Bradley 2017; Edgar 2024). Therefore, our findings inform systems‐level stakeholders about the factors that need to be addressed to implement Hospital at Home services safely and effectively, and can also inform the development of clinical and health systems guidelines to guide evidence‐based decision‐making.
Studies were limited to 13 high‐income countries and one upper middle‐income country (Brazil), and most settings were single‐payer institutions. This has contributed to uncertainty about whether the current findings apply outside of these settings and the possibility of new findings as studies that include a broader range of settings and stakeholders are conducted.
Despite important differences regarding the function of Early Discharge versus Admission Avoidance Hospital at Home services, factors affecting the implementation of these two types of services were remarkably similar. Early engagement of stakeholders, particularly with regard to agreeing on patient eligibility for referrers for both Early Discharge and Admission Avoidance Hospital at Home was essential, as well as supporting delivery of safe and effective patient‐centred care via leadership, co‐ordination, staff training, collaboration, teamwork and supporting caregivers. The similarities in findings between these two models of care suggest that they may be extrapolated to guide the implementation of other care delivery services. For example, the implementation of doctor‐nurse substitution strategies in primary care (i.e. nurses deliver care usually delivered by doctors) requires leadership, access to resources such as trained staff and effective processes for referral (Karimi‐Shahanjarini 2019). Like our findings on Hospital at Home, doctor‐nurse substitution was also acceptable to patients, doctors and nurses once these factors were in place.
While the sharing of guidance and training for referrals was recommended to reduce uncertainty from referral sources, no studies in our qualitative evidence synthesis reported on the form this took. This is important because the sharing of guidance and training to enable access for referring clinicians to Hospital at Home teams, or other broader promotion strategies, will likely improve implementation of Hospital at Home across services and help with sustainability. No studies delved into the transferability of professionals' skills from other roles, or service types, for the Hospital at Home context. Provision of training and options for promotion affect staff retention and, in turn, the sustainability of services.
Limitations of the review
Including Hospital at Home services delivering acute and subacute services and classifying and comparing the different service delivery models was a strength. However, in some health systems (such as in the US), subacute care includes ongoing acute treatments for more medically stable patients. The search strategy was comprehensive, identifying 52 qualitative studies related to the implementation of Hospital at Home. Limitations include difficulties in ascertaining components of the service delivery models due to unclear or lack of reporting; this may have affected the classification of service models (e.g. Admission Avoidance, Early Discharge or combined), and when articles did not list the full staff complement and roles. This limited our ability to perform subgroup analyses related to the intervention components that may affect implementation. Overall, we acknowledge that there was less qualitative evidence relating to surgical care, with the majority of evidence pertaining to patients with medical conditions such as stroke and COPD, and no studies were identified from low‐income country settings.
While the majority of our findings (7/12) related to theme 2 (processes, resources and skills), some findings related to more than one finding and theme. For example, safety concerns of patients, caregivers and referring clinicians, such as reliance on patients and/or caregivers if there is no surveillance at night (theme 2, finding 1), related to eligibility criteria that required a caregiver to be present (theme 2, finding 2) and impacted the caregiver if they were expected to be involved in monitoring safety overnight (theme 3, finding 2). The finding on advanced training of nursing staff to prescribe and administer intravenous medications (theme 2, finding 5), might require policy and legislative changes in settings where nurses are not legally allowed to prescribe medications (theme 1, finding 1). This would affect the sustainability of Hospital at Home and might determine the degree to which Admission Avoidance Hospital at Home could be an alternative service for a hospital admission (theme 4, finding 1).
We did not incorporate implementation science frameworks or theory to guide the data collection, analysis and reporting of the findings, and we propose that this would be useful to explore in a future update of this qualitative evidence synthesis to assist in guiding future implementation and evidence‐to‐policy/practice translation efforts.
Authors' conclusions
Based on high confidence from 10 of 12 findings derived from 52 qualitative studies, implementing Hospital at Home requires early development of policies and stakeholder engagement, promotion of referral and admission processes to potential referrers, effective interdisciplinary communication and a skilled workforce to safely and effectively implement person‐centred care. This will help to achieve acceptance from patients, caregivers and health professionals delivering the service and sustainability of the service.
Implications for practice
Based on the findings of this qualitative evidence synthesis, a series of questions have been included to assist future implementers of Hospital at Home, including system funders, executive leaders and health professionals from public and private hospitals, including residential care facilities and primary care. They are intended to help implementers consider the findings of this qualitative evidence synthesis and apply them within their context. The importance of these questions will vary depending on the specific setting and conditions being managed.
Theme 1. Development of stakeholder relationships and systems prior to implementation of Hospital at Home
Finding 1. What promotional strategies exist for referring staff regarding patient eligibility and admission processes (e.g. staff from the emergency department, hospital physicians and specialists, primary care GPs, nurse unit mangers, allied health managers and new staff)? Do you need to engage with third party services to ensure sufficient coverage of home care? Health system funders may need clarity on the benefits and role of Hospital at Home. Do the health system funders in your setting understand the benefits of Hospital at Home, and where the models fit in the context of other health service delivery models (i.e. substituting for hospital inpatient care) and for whom?
Finding 2. Are there any regulatory changes required to deliver specific interventions (e.g. intravenous therapy or prescribing medications by nurses) that could maximise the capacity and sustainability of Hospital at Home? Can your service collate total costs and savings related to delivery of Hospital at Home (compared to inpatient care)? Are there any data collection and billing issues in Hospital at Home that need to be integrated into hospital database systems?
Theme 2. Processes, resources and skills required to safely and effectively implement Hospital at Home
Finding 1. Safety concerns will exist for patients (e.g. they may be worried about their safety at home without constant surveillance) and concerns for staff delivering the service (e.g. concerns about home hazards). What strategies have been implemented to make patients and caregivers feel safer with Hospital at Home? Are appropriate safety screening tools in place for home care staff?
Finding 2. Referrers in the acute setting and primary care are likely to have uncertainty regarding patient eligibility and referral processes. What strategies are in place to address this uncertainty?
Finding 3. Leadership and co‐ordination were essential. Is there a dedicated health service leader responsible for Hospital at Home and a single point of contact? Do you need to assign medical responsibility to avoid confusion between hospital and home care medical staff?
Finding 4. What multidisciplinary workforce is required? When and how will team meetings occur? What clinical supervision is in place for allied health staff delivering Hospital at Home? What financing and budgets are in place to maximise and sustain staff resource allocation and avoid delays in care delivery? Have you utilised the skills of the team members effectively? For Hospital at Home services delivering subacute care, has the service considered using therapy assistants delivering rehabilitation care in people’s homes rather than health professionals who could take an overview role to guide the rehabilitation? These questions are priorities for health systems that deal with workforce shortages and require dedicated training that goes beyond traditional training to overcome deficits in skills, such as working in a virtual care environment, and task sharing.
Finding 5. What staff training has been implemented? Assessing the need for staff training, including advanced training (e.g. IV therapy) or employing more experienced or skilled staff (e.g. nurse practitioners) in leadership roles may be critical to delivering safe and effective Hospital at Home care. This depends on the types of interventions required, i.e. acute versus subacute care.
Finding 6. What staff‐to‐staff documentation and communication processes are in place to ensure safe, effective care? Is patient communication and information individually tailored to the patients' needs and preferences?
Finding 7. Do your healthcare professionals have skills in patient‐centred care and shared decision‐making? Do referral and admission processes adopt a shared decision‐making model with patient and caregiver preferences considered when referring patients to Hospital at Home?
Theme 3. Acceptance, perceived benefits and caregiver impacts from Hospital at Home
Finding 1. Patients ultimately want optimal recovery. What processes are in place that measure patient acceptability?
Finding 2. It is likely some caregivers will be negatively impacted by Hospital at Home. Has the caregiver's role been defined, and recognised and discussed with patients and caregivers?
Theme 4. Sustainability of Hospital at Home
Finding 1. Are patients being referred to the service who would normally require inpatient admission?
Implications for future research
The following implications for research are based on our assessment of the qualitative studies included in this qualitive evidence synthesis, including our GRADE CERQual judgements and key findings, and aim to improve implementation of Hospital at Home for all key stakeholders. This complements a research agenda to help future Hospital at Home development based on a survey of attendees at the World Hospital at Home Congress in 2019 (Leff 2022).
Future qualitative researchers in the field of Hospital at Home should consider and be explicit about the components of their delivery model, such as specifying the full staff complements, roles and responsibilities, referral and discharge processes, promotional strategies used to ensure referrals and what training strategies were used to up‐skill staff. Better reporting of intervention components will make it easier to replicate the interventions and advance the evidence base. Qualitative researchers should also report a critical examination of their own perspectives on Hospital at Home and potential bias, including relationships between the researcher and participants that may have influenced the findings of their research, and ensure ethical approval is obtained. There should be Patient and Public Involvement and Engagement in future studies.
More primary qualitative research around factors affecting the implementation of Hospital at Home is needed in low‐ and middle‐income settings and rural settings, as well as the perspectives of stakeholders from multiple‐payer systems (e.g. insurers), and perspectives from systems‐level stakeholders (e.g. policy makers) in order to help improve confidence in the findings. Future researchers should also consider collecting data via observation of practice and receipt of care, in order to explore healthcare worker practice to complement the data about healthcare worker views and patient experiences identified from focus groups and one‐to‐one interviews.
A research priority is understanding the potential negative impact on caregivers from Admission Avoidance Hospital at Home. For example, the resources required to support caregivers, and their role in shared decision‐making. This will become increasingly important as countries implement hospital avoidance strategies to deal with the increased numbers attending the emergency department.
The negative impact of disease on patients and the home environment requires attention. Patients with stroke, COPD and various acute conditions described difficulty at home, such as reduced mobility and confidence (e.g. getting outdoors), pain, fatigue (especially COPD patients after a hospital stay due to an exacerbation of their condition), and this has implications for discharging patients to community services.
More research is needed around training and educating clinicians delivering Hospital at Home.
This review was started before the use of Hospital at Home became more of a focus due to the COVID‐19 pandemic. Future researchers should consider studying the implementation of Hospital at Home services in the context of the pandemic and post‐pandemic.
What's new
| Date | Event | Description |
|---|---|---|
| 12 March 2024 | Amended | Affiliation and email of contact author updated. |
History
Protocol first published: Issue 3, 2021 Review first published: Issue 3, 2024
Acknowledgements
This research is conducted by the authors for the National Health and Medical Research Council (NHMRC) Partnership Centre for Health System Sustainability (grant ID number: 9100002), administered by the Australian Institute of Health Innovation, Macquarie University. Along with the NHMRC, the funding partners in this research collaboration are: The Bupa Health Foundation, NSW Ministry of Health, Department of Health, WA and The University of Notre Dame Australia. Their generous support is gratefully acknowledged. While the NHMRC, The Bupa Health Foundation, NSW Ministry of Health, Department of Health, WA and The University of Notre Dame Australia have provided in‐kind and financial support for this research, they have not reviewed the content and are not responsible for any injury, loss or damage however arising from the use of, or reliance on, the information provided herein. The published material is solely the responsibility of the authors and does not reflect the views of the NHMRC or its funding partners.
The Norwegian Satellite of Cochrane Effective Practice and Organisation of Care (EPOC) receives funding from the Norwegian Agency for Development Co‐operation (Norad), via the Norwegian Institute of Public Health, to support review authors in the production of their reviews.
Editorial and peer reviewer contributions
The following people conducted the editorial process for this article:
Sign‐off Editor (final editorial decision): Jane Noyes, Centre for Health‐Related Research, Fron Heulog, Bangor University
Managing Editor (selected peer reviewers, provided editorial guidance to authors, edited the article): Sam Hinsley, Cochrane Central Editorial Service
Editorial Assistant (conducted editorial policy checks, collated peer reviewer comments and supported the editorial team): Leticia Rodrigues, Cochrane Central Editorial Service
Copy Editor (copy editing and production): Jenny Bellorini, Cochrane Central Production Service
Peer reviewers (provided comments and recommended an editorial decision): Jennifer Hilgart, Cochrane (methods), Yi Feng Lai 1) MOH Office for Healthcare Transformation, Singapore, 2) Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore, 3) School of Public Health, University of Illinois at Chicago, USA (clinical), Bruce Kinosian, MD, Division of Geriatric Medicine University of Pennsylvania (clinical), Professor Hanne Konradsen, Denmark (clinical) and Claire Jowett (consumer). One additional peer reviewer provided search peer review but chose not to be publicly acknowledged.
Appendices
Appendix 1. GRADE‐CERQual evidence profiles
| Review finding | Studies contributing to the review finding | Adequacy | Methodological limitations | Relevance | Coherence | CERQual assessment | Explanation of CERQual assessment |
| Theme 1. Development of stakeholder relationships and systems prior to implementation of Hospital at Home | |||||||
| Finding 1. Service‐level staff suggested that early stakeholder engagement, including partnerships with third party service providers, was required to implement Hospital at Home. This was critical for implementing new services, overcoming regulatory requirements, building trust and ensuring referrals. | Brody 2019; Chouliara 2014; Dinesen 2007; Fisher 2021; Gorbenko 2023; Hitch 2020; Kraut 2016; Lemelin 2007; Moule 2011; Sims 1997; Testa 2021 | Data from 11 studies (of 52 included) contributed to this finding. Minor concerns about data richness in one study. Covers high‐income countries, service‐ and systems‐level perspectives, Early Discharge and Admission Avoidance services and various conditions. Minor concerns related to small number of studies contributing to this finding and no data from low‐income countries. |
Strengths included clear aims (n = 11), appropriate methods (n = 11), research design (n = 11), presentation of findings (n = 10) and data analysis (n = 9), data collection (n = 7) and ethics (n = 6). Weaknesses included not reporting relationship between researcher and participant (n = 9), and concerns with reporting of recruitment method (n = 5). No or very minor concerns as there were 8 higher‐quality and 3 lesser‐quality studies contributing to the review finding. |
Contributes relevant data for the review question from 7 recent studies. No or very minor concerns, with some older studies contributing to this review finding. |
Good fit between data and review finding. No or very minor concerns. |
High | Minor concerns about adequacy. No or very minor concerns about methodological limitations, relevance and coherence. |
| Finding 2. For healthcare services planning to implement Hospital at Home, current systems need to integrate activity data and service costs. This allows healthcare services to collate total costs and savings to measure financial impact. This is important as policy makers, hospital executives and insurers from multiple‐payer settings require evidence about the financial impact of Hospital at Home to inform commissioning decisions. For multiple‐payer systems, financial impact and approval could be enhanced by including patients who contribute smaller financial benefits to the hospital if they were an inpatient. | Brody 2019; Chouliara 2014; Dismore 2019; Fisher 2021; Gorbenko 2023; Moule 2011 | Data from 6 studies (of 52 included) contributed to this finding. No concerns with data richness. Covers high‐income countries, service‐ and systems‐level perspectives, Early Discharge and Admission Avoidance services and various conditions. Moderate concerns related to small number of studies and systems‐level perspectives contributing to this finding and no data from low‐income countries. |
Strengths included clear aims (n = 6), appropriate methods (n = 6), research design (n = 6), data collection (n = 6), data analysis (n = 6), presentation of findings (n = 6), ethics (n = 4) and reporting of recruitment method (n = 4). Weaknesses included not reporting relationship between researcher and participant (n = 3). No or very minor concerns as there were 6 higher‐quality studies contributing to the review finding. |
Contributes relevant data for the review question from 5 recent studies. No or very minor concerns with 1 older study contributing to this review finding. |
Good fit between data and review finding. Minor concerns with some variation in findings across the studies. |
Moderate | Moderate concerns about adequacy. Minor concerns about coherence. No or very minor concerns about methodological limitations and relevance. |
| Theme 2. Processes, resources and skills required to safely and effectively implement Hospital at Home | |||||||
| Finding 1. Safety concerns were expressed by all stakeholders, such as for patients going home alone in regard to pain management and their mobility, and staff expressed concern for their own safety due to home hazards, patient‐related factors and ergonomics. Patients were reassured about their safety with access to staff (including via phone) and equipment for safe monitoring. Timely delivery of appropriate equipment in the home alleviated some staff concerns. | Dean 2007; Dismore 2019; Dow 2007b; Dubois 2001; Fisher 2021; Ko 2023; Kraut 2016; Kylén 2021; Lemelin 2007; Levine 2021; Lou 2017; Manning 2016; Nordin 2015; Sims 1997; Udesen 2021; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; Wallis 2022; Wang 2012; Wilson 2002 | Data from 20 studies (of 52 included) contributed to this finding. Minor concerns about data richness in 4 studies. Covers high‐income countries, service‐ and systems‐level perspectives, Early Discharge and Admission Avoidance services and various conditions. Minor concerns due to some thin data and no data from low‐income countries. |
Strengths included clear aims (n = 20), appropriate methods (n = 20), research design (n = 20), presentation of findings (n = 18), data collection (n = 13), ethics (n = 13), and data analysis (n = 12) and reporting of recruitment method (n = 12). Weaknesses included not reporting relationship between researcher and participant (n = 9). No or very minor concerns as there were 14 higher‐quality and six lesser‐quality studies contributing to the review finding. |
Contributes relevant data for the review question from 12 recent studies. No or very minor concerns, with some older studies contributing to this review finding. |
Good fit between data and review finding. No or very minor concerns. |
High | Minor concerns about adequacy. No or very minor concerns about methodological limitations, relevance and coherence. |
| Finding 2. Identifying patients using eligibility criteria and clinical judgement was challenging for referrers in the acute setting, especially in the start‐up phase of implementation. Services developed criteria to maintain responsiveness and manage capacity, and conducted teaching sessions to help acute staff to refer patients to Hospital at Home. Some services had concerns when staff were working at low capacity (not enough referrals), if staff were seeing patients that were either too ill, or did not need the higher level of care required for Hospital at Home. | Andrade 2013; Brody 2019; Chouliara 2014; Dismore 2019; Fisher 2021; Gorbenko 2023; Kraut 2016; Lemelin 2007; Manning 2016; Moule 2011; Udesen 2022; Vaartio‐Rajalin 2020 | Data from 12 studies (of 52 included) contributed to this finding. No concerns about data richness. Covers high‐income countries and one upper middle‐income country, service‐ and systems‐level perspectives, Early Discharge and Admission Avoidance services and various conditions. Minor concerns due to small number of studies contributing to this finding and no data from low‐income countries. |
Strengths included clear aims (n = 12), appropriate methods (n = 12), research design (n = 12), data collection (n = 10), ethics (n = 9), data analysis (n = 9), presentation of findings (n = 10) and recruitment method (n = 8). Weaknesses included not reporting relationship between researcher and participant (n = 7). No or very minor concerns as there were 10 higher‐quality and two lesser‐quality studies contributing to the review finding. |
Contributes relevant data for the review question from 10 recent studies. No or very minor concerns. |
Good fit between data and review finding. No or very minor concerns. |
High | Minor concerns about adequacy. No or very minor concerns about methodological limitations, relevance and coherence. |
| Finding 3. Leadership and co‐ordination from key champions, lead clinicians with medical responsibility and clinical accountability, managers with operational responsibility and other leaders were essential to provide high‐quality care. Hospital at Home managers, directors or co‐ordinators were responsible for creating a positive staff environment, ensuring protected time for training and clinical supervision, and facilitating service improvements. | Barnard 2016; Brody 2019; Crilly 2012; Dow 2007a; Fisher 2021; Hitch 2020; Karacaoglu 2021; Leung 2016; Sims 1997; Testa 2021; Udesen 2022 | Data from 11 studies (of 52 included) contributed to this finding. Minor concerns about data richness in one study. Covers high‐income countries, service, systems‐level perspectives, Early Discharge and Admission Avoidance services and various conditions. Minor concerns due to small number of studies contributing to this finding and no data from low‐income countries. |
Strengths included clear aims (n = 11), appropriate methods (n = 11), research design (n = 11), data collection (n = 8), data analysis (n = 8), presentation of findings (n = 10), recruitment method (n = 8) and ethics (n = 7). Weaknesses included not reporting relationship between researcher and participant (n = 7). No or very minor concerns as there were 8 higher‐quality and 3 lesser‐quality studies contributing to the review finding. |
Contributes relevant data for the review question from 7 recent studies. No or very minor concerns, with some older studies contributing to this review finding. |
Good fit between data and review finding. Minor concerns with variation in descriptions and explanations of the specific leadership (e.g. who, what, how etc). |
Moderate | Minor concerns about adequacy and coherence. No or very minor concerns about methodological limitations and relevance. |
| Finding 4. A multidisciplinary skilled workforce was required to implement Hospital at Home, with collaboration between teams and professionals (e.g. via team meetings) a core feature. However, maintaining responsiveness was important, and the absence of a waiting list for admission to Hospital at Home allowed a service to respond to the demand for hospital care. Building rapport with external partners was challenging, and allied health professionals noted difficulties with their professional line of reporting and supervision. Some teams were frustrated by a lack of resource allocation, others recognised that the service was better staffed than usual care. Teams were also challenged to meet intensity targets and address workforce shortages. Multiple strategies could enhance capacity and responsiveness, such as securing more funding, training family members, adopting new technologies and implementing telehealth appointments. However, this could affect the provision of patient‐centred care. | Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Cunliffe 2004; Dean 2007; Dinesen 2007; Dow 2007b; Fisher 2021; Gorbenko 2023; Hitch 2020; Karacaoglu 2021; Lemelin 2007; Moule 2011; O'Neill 2017; Papaioannou 2018; Rayner 2022; Sims 1997; Testa 2021; Udesen 2022; Vaartio‐Rajalin 2020; von Koch 2000 | Data from 24 studies (of 52 included) contributed to this finding. Minor concerns about data richness in 2 studies. Covers high‐income countries, and one upper middle‐income country, service‐ and systems‐level perspectives, early discharge and Admission Avoidance services and various conditions. No or very minor concerns with no data from low‐income countries. |
Strengths included clear aims (n = 24), appropriate methods (n = 24), research design (n = 24), presentation of findings (n = 23), data analysis (n = 17) and data collection (n = 17). Weaknesses included not reporting relationship between researcher and participant (n = 23), concerns with reporting of recruitment methods (n = 10) and ethics (n = 12). No or very minor concerns as there were 18 higher‐quality and 6 lesser‐quality studies contributing to the review finding. |
Contributes relevant data for the review question from 15 recent studies. No or very minor concerns, with some older studies contributing to this review finding. |
Good fit between data and review finding. Minor concerns with some variation in findings across the studies. |
High | Minor concerns about coherence. No or very minor concerns about adequacy, methodological limitations and relevance. |
| Finding 5. Staff training, expansion of roles beyond usual scope of practice and rapid delivery of equipment or medical testing was essential to implement Hospital at Home. Expanding nurse roles increased capacity for acute medical care in the home and residential care. Expanding rehabilitation assistant roles increased capacity for rehabilitation in the home. The expansion of roles required appropriate governance structures and policy change. | Andrade 2013; Barnard 2016; Brody 2019; Cobley 2013; Crilly 2012; Cunliffe 2004; Dinesen 2007; Dismore 2019; Dubois 2001; Fisher 2021; Hitch 2020; Karacaoglu 2021; Lemelin 2007; Leung 2016; O'Neill 2017; Papaioannou 2018; Rayner 2022; Sims 1997; Testa 2021; Udesen 2022; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021 | Data from 22 studies (of 52 included) contributed to this finding. Minor concerns about data richness in 2 studies. Covers high‐income countries and one upper middle‐income country, service‐ and systems‐level perspectives, early discharge and Admission Avoidance services and various conditions. No or very minor concerns with no data from low‐income countries. |
Strengths included clear aims (n = 22), appropriate methods (n = 22), research design (n = 22), presentation of findings (n = 20), and data analysis (n = 17) Weaknesses included not reporting relationship between researcher and participant (n = 20), concerns with reporting of recruitment methods (n = 8), ethics (n = 9) and data collection (n = 8). No or very minor concerns as there were 15 higher‐quality and seven lesser‐quality studies contributing to the review finding. |
Contributes relevant data for the review question from 16 recent studies. No or very minor concerns, with some older studies contributing to this review finding. |
Good fit between data and review finding. Minor concerns with some variation in findings across the studies. |
High | Minor concerns about coherence. No or very minor concerns about adequacy, methodological limitations and relevance. |
| Finding 6. Effective communication between staff, patients and caregivers, including documentation and sharing tailored information with patients, was essential to provide efficient and effective care and reassure patients that quality of care is maintained in Hospital at Home. Problems with communication were commonly encountered by patients (e.g. patient information was not tailored), caregivers (e.g. limited opportunities to discuss management with clinicians) and staff (e.g. absence of a shared electronic medical record hampering the sharing of information about patients, efficiency of the service and continuity of care). | Andrade 2013; Barnard 2016; Brody 2019; Cegarra‐Navarro 2010; Chevalier 2015; Chouliara 2014; Cobley 2013; Collins 2016; Crilly 2012; Cunliffe 2004; Dean 2007; Dinesen 2007; Dinesen 2008; Dismore 2019; Dubois 2001; Fisher 2021; Gorbenko 2023; Jester 2003; Kimmel 2021; Lemelin 2007; Leung 2016; Levine 2021; Mäkelä 2020; O'Neill 2017; Ranjbar 2015; Reid 2008; Rossinot 2019; Schofield 2006; Sims 1997; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; von Koch 2000; Wallis 2022; Wang 2012 | Data from 38 studies (of 52 included) contributed to this finding. Minor concerns about data richness in 3 studies. Covers high‐income countries, 1 upper middle income country, service‐ and systems‐level perspectives, Early Discharge and Admission Avoidance services and various conditions. No or very minor concerns with no data from low‐income countries. |
Strengths included clear aims (n = 38), appropriate methods (n = 38), research design (n = 38), presentation of findings (n = 36), data analysis (n = 27), data collection (n = 27) and ethics (n = 24). Weaknesses included not reporting relationship between researcher and participant (n = 34), and concerns with reporting of recruitment methods (n = 16). No or very minor concerns as there were 29 higher‐quality and nine lesser‐quality studies contributing to the review finding. |
Contributes relevant data for the review question from 24 recent studies. No or very minor concerns, with some older studies contributing to this review finding. |
Good fit between data and review finding. Minor concerns, with some variation in findings across the studies contributing to this finding. |
High | Minor concerns about coherence. No or very minor concerns about adequacy, methodological limitations and relevance. |
| Finding 7. Health professionals required skills in delivering person‐centred care, shared decision‐making and tailoring care to achieve patient goals and patient satisfaction. Some caregivers were frustrated about their lack of involvement in decision‐making and care planning. Patients valued equal interactions and partnerships with the staff, and their ability to cater for their needs and valued staff focussing on helping family members. | Andrade 2013; Chouliara 2014; Clarke 2010; Cobley 2013; Collins 2016; Cunliffe 2004; Dinesen 2007; Dow 2007a; Dow 2007b; Dubois 2001; Fisher 2021; Gorbenko 2023; Hitch 2020; Jester 2003; Karacaoglu 2021; Kimmel 2021; Ko 2023; Kylén 2021; Levine 2021; Lou 2017; Mäkelä 2020; Manning 2016; Nordin 2015; Papaioannou 2018; Ranjbar 2015; Reid 2008; Rossinot 2019; Schofield 2006; Udesen 2021; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; von Koch 2000; Wallis 2022; Wilson 2002 | Data from 34 studies (of 52 included) contributed to this finding. Minor concerns about data richness in 2 studies. Covers high‐income countries and one upper middle‐income country, service‐ and systems‐level perspectives, Early Discharge and Admission Avoidance services and various conditions. No or very minor concerns with no data from low‐income countries. |
Strengths included clear aims (n = 34), appropriate methods (n = 34), research design (n = 34), presentation of findings (n = 33), data analysis (n = 23), data collection (n = 25), ethics (n = 21) and recruitment methods (n = 21). Weaknesses included not reporting relationship between researcher and participant (n = 29). No or very minor concerns as there were 26 higher‐quality and 8 lesser‐quality studies contributing to the review finding. |
Contributes relevant data for the review question from 23 recent studies. No or very minor concerns, with some older studies contributing to this review finding. |
Good fit between data and review finding. No or very minor concerns. |
High | No or very minor concerns about adequacy, methodological limitations, relevance and coherence. |
| Theme 3. Acceptance, perceived benefits and caregiver impacts from Hospital at Home | |||||||
| Finding 1. Patients, caregivers and service‐level staff believed Hospital at Home (including in residential care) was an appropriate alternative to hospital inpatient care, and facilitated optimal recovery and satisfaction with less risk of hospital‐acquired complications. Patients appreciated positive and competent staff who motivated them to reach their recovery goals. Sometimes the lack of caregiver support and 24 hour supervision from hospital staff made some patients prefer to stay in hospital. | Andrade 2013; Barnard 2016; Cobley 2013; Cunliffe 2004; Dinesen 2008; Dow 2007a; Dow 2007b; Dubois 2001; Fisher 2021; Gorbenko 2023; Hitch 2020; Karacaoglu 2021; Kimmel 2021; Ko 2023; Kraut 2016; Lemelin 2007; Levine 2021; Lou 2017; Mäkelä 2020; Moule 2011; Nordin 2015; Papaioannou 2018; Ranjbar 2015; Rayner 2022; Rossinot 2019; Sims 1997; Testa 2021; Udesen 2021; Udesen 2022; Vaartio‐Rajalin 2020; Wallis 2022; Wilson 2002 | Data from 32 studies (of 52 included) contributed to this finding. Minor concerns about data richness in 3 studies. Covers high‐income countries, 1 upper middle‐income country, service‐ and systems‐level perspectives, Early Discharge and Admission Avoidance services and various conditions. No or very minor concerns with no data from low‐income countries. |
Strengths included clear aims (n = 32), appropriate methods (n = 32), research design (n = 32), presentation of findings (n = 31), data analysis (n = 21), data collection (n = 23), recruitment methods (n = 22) and ethics (n = 20). Weaknesses included not reporting relationship between researcher and participant (n = 26). No or very minor concerns as there were 25 higher‐quality and 7 lesser‐quality studies contributing to the review finding. |
Contributes relevant data from 23 recent studies. No or very minor concerns, with some older studies contributing to this review finding. |
Good fit between data and review finding. No or very minor concerns. |
High | No or very minor concerns about adequacy, methodological limitations, relevance and coherence. |
| Finding 2. Caregivers were impacted by Hospital at Home. This included disruption to their normal routines, work, energy and sleep. There were reports of stress and anxiety related to feeling untrained to provide patient support and monitoring and a lack of formal recognition and access to information. Some caregivers and patients were concerned about their privacy at home and the impact on the patient/caregiver relationship from being involved with care. | Andrade 2013; Brody 2019; Cobley 2013; Dinesen 2008; Dismore 2019; Dow 2007b; Dubois 2001; Fisher 2021; Hitch 2020; Jester 2003; Kimmel 2021; Ko 2023; Levine 2021; Lou 2017; Mäkelä 2020; Manning 2016; Nordin 2015; Reid 2008; Rossinot 2019; Sims 1997; Udesen 2021; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; Wallis 2022; Wilson 2002 | Data from 25 studies (of 52 included) contributed to this finding. Minor concerns about data richness in 3 studies. Covers high‐income countries, 1 upper middle income country, service‐ and systems‐level perspectives, Early Discharge and Admission Avoidance services and various conditions. No or very minor concerns with no data from low‐income countries. |
Strengths included clear aims (n = 25), appropriate methods (n = 25), research design (n = 25), presentation of findings (n = 24), data analysis (n = 16), data collection (n = 18), ethics (n = 19) and reporting of recruitment methods (n = 15). Weaknesses included not reporting relationship between researcher and participant (n = 20). No or very minor concerns as there were 19 higher‐quality and 6 lesser‐quality studies contributing to the review finding. |
Contributes relevant data from 18 recent studies. No or very minor concerns, with some older studies contributing to this review finding. |
Good fit between data and review finding. No or very minor concerns. |
High | No or very minor concerns about adequacy, methodological limitations, relevance and coherence. |
| Theme 4. Sustainability of Hospital at Home | |||||||
| Finding 1. Staff and patients expressed concern that without widespread implementation and expansion, the perceived benefits of Hospital at Home to patients and the healthcare system would be limited. Health system benefits included long‐term financial savings from avoiding unnecessary hospitalisation, bed closures or reduced length of stay, plus increased hospital capacity with reduced waiting times. However, some patients were sceptical that Hospital at Home was more about saving money, and in multiple‐payer settings, costs incurred by the patient were a key factor when admitting patients to Hospital at Home. Peer institution success with Hospital at Home increased executive enthusiasm for Hospital at Home. Hospital at Home could showcase a hospital’s innovation and help sustain staff recruitment. However, staff recruitment may be more challenging in rural settings as excessive driving can affect staff satisfaction. | Andrade 2013; Dow 2007b; Fisher 2021; Gorbenko 2023; Hitch 2020; Karacaoglu 2021; Ko 2023; Moule 2011; Papaioannou 2018; Rayner 2022; Sims 1997; Vaartio‐Rajalin 2020; Vaartio‐Rajalin 2021; Wallis 2022 | Data from 14 studies (of 52 included) contributed to this finding. Minor concerns about data richness in 1 study. Covers high‐income countries, 1 upper middle‐income country, service‐ and systems‐level perspectives, Early Discharge and Admission Avoidance services and various conditions. Minor concerns due to small number of studies contributing to this finding and no data from low‐income countries. |
Strengths included clear aims (n = 14), appropriate methods (n = 14), research design (n = 14), presentation of findings (n = 14), ethics (n = 10), data analysis (n = 9), data collection (n = 10) and recruitment methods (n = 9). Weaknesses included not reporting relationship between researcher and participant (n = 13). No or very minor concerns as there were 12 higher‐quality and 2 lesser‐quality studies contributing to the review finding. |
Contributes relevant data from 11 recent studies. No or very minor concerns, with some older studies contributing to this review finding. |
Good fit between data and review finding. No or very minor concerns. |
High | Minor concerns about adequacy. No or very minor concerns about methodological limitations, relevance and coherence. |
Appendix 2. Search strategies
MEDLINE search strategy
Ovid MEDLINE(R) ALL <1946 to November 15, 2022> (searched 17 November 2022)
| # | Query | Results |
| 1 | Hospital to Home Transition/ | 29 |
| 2 | exp Home Care Services/ | 50369 |
| 3 | exp Hospitalization/ or Hospitals/ | 371249 |
| 4 | 2 and 3 | 6305 |
| 5 | 1 or 4 | 6331 |
| 6 | (hospital* adj3 home).ti,ab,kf. | 10340 |
| 7 | (home care and (medical services or health services)).ti,ab,kf. | 862 |
| 8 | (home based adj (medical care or medical services or health services or health care or healthcare or care services or care program*)).ti,ab,kf. | 253 |
| 9 | home based program*.ti,ab,kf. | 514 |
| 10 | home ward.ti,ab,kf. | 48 |
| 11 | ((home or domiciliary) adj3 (rehab* or therap*)).ti,ab,kf. | 7772 |
| 12 | admission avoidance.ti,ab,kf. | 156 |
| 13 | avoid* admission*.ti,ab,kf. | 239 |
| 14 | (hospital* adj1 avoid*).ti,ab,kf. | 1530 |
| 15 | discharge home.ti,ab,kf. | 1668 |
| 16 | home discharge.ti,ab,kf. | 979 |
| 17 | early supported discharge.ti,ab,kf. | 190 |
| 18 | early discharge program*.ti,ab,kf. | 83 |
| 19 | (early discharge adj6 (home or hospital*)).ti,ab,kf. | 828 |
| 20 | or/5‐19 | 28162 |
| 21 | Qualitative Research/ | 77647 |
| 22 | Interviews as Topic/ | 66803 |
| 23 | (qualitative or interview* or themes or mixed method?).ti,ab,kf. | 667646 |
| 24 | or/21‐23 | 687880 |
| 25 | 20 and 24 | 3129 |
CINAHL search strategy
CINAHL 1980‐present, EbscoHost (searched 17 November 2022)
| # | Query | Results |
| S1 | (MH "Home Health Care+") and (MH "Hospitalization" or MH "Hospitals") | 2149 |
| S2 | (MH "Hospital to Home Transition" or MH "Early Patient Discharge") | 1109 |
| S3 | TI (hospital* N3 home) OR AB (hospital* N3 home) | 9053 |
| S4 | TI ( ("home care") and ("medical services" or "health services") ) OR AB ( ("home care") and ("medical services" or "health services") ) | 432 |
| S5 | TI (("home based") and ("medical care" or "medical services" or "health services" or "health care" or healthcare or "care services" or "care program*") ) OR AB (("home based") W1 ("medical care" or "medical services" or "health services" or "health care" or healthcare or "care services" or "care program*") ) | 398 |
| S6 | TI ("home based program*") OR AB ("home based program*") | 282 |
| S7 | TI ("home ward") OR AB ("home ward") | 37 |
| S8 | TI ( (home or domiciliary) and (rehab* or therap*) ) OR AB ( (home or domiciliary) N3 (rehab* or therap*) ) | 6483 |
| S9 | TI (( avoid* and (admission* or hospital*) ) OR AB ((avoid* N1 (admission* or hospital*) ) | 1873 |
| S10 | TI ("discharge home" or "home discharge") OR AB ("discharge home" or "home discharge") | 1403 |
| S11 | TI ("early supported discharge") OR AB ("early supported discharge") | 144 |
| S12 | TI ("early discharge program*") OR AB ("early discharge program*") | 60 |
| S13 | TI (( "early discharge" and (home or hospital*)) OR AB (( "early discharge" and (home or hospital*)) | 931 |
| S14 | TI (( "early patient discharge" and (home or hospital*) ) OR AB (( "early patient discharge" and (home or hospital*) ) | 11 |
| S15 | (MH "Qualitative Studies+") | 175170 |
| S16 | (MH "Interviews+") | 247210 |
| S17 | TI ( qualitative or interview* or themes or "mixed method" or "mixed methods" ) OR AB ( qualitative or interview* or themes or "mixed method" or "mixed methods" ) | 371120 |
| S18 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 | 21614 |
| S19 | S15 OR S16 OR S17 | 491600 |
| S20 | S18 AND S19 | 3728 |
| S21 | S20 [Limiters ‐ Exclude MEDLINE records] | 2090 |
Scopus, Elsevier
Searched 17 November 2022
| Query | Results |
| ( ( KEY ( "home care" AND ( hospitalization OR hospitalization ) ) ) OR ( TITLE‐ABS ( hospital* W/3 home ) ) OR ( TITLE‐ABS ( ( "home care" ) AND ( "medical services" OR "health services" ) ) ) OR ( TITLE‐ABS ( ( "home based" ) AND ( "medical care" OR "medical services" OR "health services" OR "health care" OR healthcare OR "care services" OR "care program*" ) ) ) OR ( TITLE‐ABS ( "home based program" OR "home based programs" OR "home based programme" OR "home based programmes" ) ) OR ( TITLE‐ABS ( "home ward" ) ) OR ( TITLE ( ( home OR domiciliary ) AND ( rehab* OR therap* ) ) ) OR ( ABS ( ( home OR domiciliary ) W/3 ( rehab* OR therap* ) ) ) OR ( TITLE ( avoid* AND ( admission* OR hospital* ) ) ) OR ( ABS ( avoid* W/1 ( admission* OR hospital* ) ) ) OR ( TITLE‐ABS ( "discharge home" OR "home discharge" ) ) OR ( TITLE‐ABS ( "early supported discharge" ) ) OR ( TITLE‐ABS ( "early discharge program" OR "early discharge programs" OR "early discharge programme" OR "early discharge programmes" ) ) OR ( TITLE ( "early discharge" AND ( home OR hospital* ) ) ) OR ( ABS ( "early discharge" W/3 ( home OR hospital* ) ) ) OR ( TITLE‐ABS ( "early patient discharge" AND ( home OR hospital* ) ) ) ) AND ( ( KEY ( "qualitative research" OR "qualitative study" ) ) OR ( TITLE‐ABS ( qualitative OR interview* OR themes OR "mixed method" OR "mixed methods" ) ) ) AND NOT INDEX ( medline ) | 1545 |
Global Index Medicus (GIM), WHO
Searched 17 November 2022
| Query | Results |
| ("admission avoidance" OR "early discharge" OR "early patient discharge" OR "early supported discharge" OR "discharge home" OR "home discharge" OR "discharge hospital" OR "hospital discharge" OR "home ward" OR "home hospital" OR "hospital at home" OR "hospital in the home" OR "home based hospitalization" OR "home based hospital" OR "hospital based home" OR "hospital to home" OR "hospital to the home" OR "home rehabilitation" OR "home therapy") [Title, abstract, subject] AND (qualitative OR interview* OR themes OR "mixed method" OR "mixed methods") [Title, abstract, subject] | 432 |
Appendix 3. Data richness scale
| Score | Measure |
| 1 | Very little qualitative data presented that relate to the synthesis objective. Those findings that are presented are fairly descriptive. |
| 2 | Some qualitative data presented that relate to the synthesis objective |
| 3 | A reasonable amount of qualitative data that relate to the synthesis objective |
| 4 | A good amount and depth of qualitative data that relate to the synthesis objective |
| 5 | A large amount and depth of qualitative data that relate in depth to the synthesis objective |
Adapted from Ames HMR, Glenton C, Lewin S. Parents' and informal caregivers' views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database of Systematic Reviews 2017, Issue 2. DOI: 10.1002/14651858.CD011787.pub2
Appendix 4. Findings tables with extracted data
Theme 1. Development of stakeholder relationships and systems prior to implementation of Hospital at Home
Finding 1. Service level staff suggested early stakeholder engagement, including partnerships with third party service providers, were required to implement Hospital at Home. This was critical for implementing new services, overcoming regulatory requirements, building trust and ensuring referrals (high confidence).
Early Discharge Hospital at Home
Commissioners reported needing evidence about the effectiveness and efficiency of Early Discharge Hospital at Home models versus traditional care for stroke patients and clarity on where Hospital at Home models fit in the stroke pathway to inform commissioning decisions (Chouliara 2014). External stakeholders from social care sectors thought it was important to consult with health and social care sectors to get social care implemented as part of hospital at home for stroke (Moule 2011). Hospital at home staff felt their specialism in stroke created tension between them and community rehabilitation teams, requiring early engagement with community rehabilitation services (Moule 2011). Hospital staff were concerned about a reduced intensity of rehabilitation (i.e. enough staff supervision) compared to hospital (Kraut 2016). Service level staff did not initially perceive the service as compatible with community‐based rehabilitation (Hitch 2020). There was a need for workforce consultations and benchmarking (Hitch 2020). Hospital staff reported that the concept of early discharge for orthopaedic conditions conflicted with traditional views about length of hospital stay that may impact referrals and felt there was a negative aspect of the service for patients around the service not being comparable to 24‐hour usual hospital care (Sims 1997). Acute hospital staff were sceptical, and wanted more understanding of the intervention in order to determine that the early supported discharge service is best for their stroke patient (Chouliara 2014). Service level staff perceived reluctance of acute hospital staff to hand over stroke patients, and a need to develop working relationships with acute staff was perceived as critical to the success of a service by increasing appropriate referrals (Chouliara 2014). Nurses and physicians were reluctant to ‘let go of’ heart patients for home hospitalisation until the relationship between the hospital and home nurses evolved from feelings of reservation to trust and respect and improved patient care (Dinesen 2007).
Admission Avoidance Hospital at Home
Systems and service level staff felt there was a need to develop internal and external partnerships, including with legal and regulatory compliance, well in advance of implementation in a multiple‐payer setting for various conditions (Brody 2019). This was important to address the lack of reach of Hospital at Home (Brody 2019; Gorbenko 2023) and examine how to gain buy‐in from potentially busy or sceptical referral sources (physicians) (Brody 2019). Relationships with other services and providers were seen by the team to encourage referral (Testa 2021).
Programme leaders felt certain regulations were unnecessary or did not improve safety, such as the requirement for two in‐person patient monitoring visits per day, and that clinical need should drive monitoring (Gorbenko 2023). To overcome this, the second visit was done by telehealth (Gorbenko 2023). Building electronic health record systems to replace outpatient systems was needed to meet regulatory requirements, and required support from informatic executives (Gorbenko 2023). Leaders identified the delivery of food a challenge (Gorbenko 2023). Also, delivering medications was a major implementation challenge with home healthcare nurses playing a critical role in medication delivery as a viable solution for addressing pharmacy challenges (Gorbenko 2023).
Combined Admission Avoidance and Early Discharge Hospital at Home
Nurse practitioners noted resistance and difficulties with getting buy‐in from medical staff that improved over time (Lemelin 2007).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Brody 2019, USA | Examine facilitators and barriers to implementation of Hospital at Home programme over its first year of operation to provide others with the opportunity to plan effectively for operationalisation | Admission Avoidance Hospital at Home for various acute conditions (This study focused on the first year of operation) |
Service level (staff) Systems level (executive leader) |
Icahn School of Medicine at Mount Sinai had developed partnerships with external vendors over years, and these and newer partnerships specific to HAH‐Plus both required significant lead time to complete contract negotiations and execution. Key to engage internal stakeholders including legal and regulatory compliance, as well as external partners, very early on in the process. It may not be possible to work with a single home health agency due to lack of coverage across an entire service area. |
| 2 | Chouliara 2014, England | Explore the perceptions of healthcare professionals and commissioners regarding the challenges and facilitators to implementation and perceived impact of early supported discharge services | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Study was conducted in the first year of implementation) |
Service level (staff) Systems level (commissioners) |
Commissioners argued that the current economic climate stresses the need for a more rigorous evaluation of the services’ outcomes. Three commissioners requested greater evidence as to whether Early Supported Discharge is the most efficient and effective way of providing rehabilitation and helping patients make the best of their recovery. Four commissioners underlined the need to clarify the position of Early Supported Discharge in the context of the stroke pathway. “To be honest I am bit foggy about where early supported discharge sits alongside intermediate care and re‐enablement and how these are married up”. (Commissioner) Hospital staff was perceived as occasionally reluctant to hand over patients to the Early Supported Discharge service as discussed by four team members in Site A. Participants agreed that the development of strong links with other services was critical to the success of early supported discharge. Their close working relationship with the acute service had facilitated the identification of appropriate patients: “We’ve really endeavoured to build up a good relationship with the different organisations and I think the better that is, the better the team runs because you are getting referrals and good understanding”. (Team lead) "Transfer between the services has improved and works in a much more seamless way”. (Service management) |
| 3 | Dinesen 2007, Denmark | Explore how the implementation of the concept ‘Home hospitalisation of heart patients’ by means of telehomecare technology influences the integration of clinical tasks across healthcare sectors | Early Discharge Hospital at Home for heart conditions | Service level (staff) | “From a nurse’s perspective it means ‘letting go of’ the patients at an earlier stage than we’re used to...” (Nurse) The relationship between the nurses at the hospital and the home (district nurses) evolved from feelings of reservation to trust and respect, and they made mutual adjustments to solve the clinical tasks "in the best way possible" to avoid patients being "kept hostage" between the two sectors. |
| 4 | Fisher 2021 | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service. (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery. |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
Achieving and maintaining good communication with commissioners was identified as an important parameter in developing an ESD service and establishing its position in the stroke care pathway. One team described liaising with commissioners as a time‐consuming and stressful exercise that could end fruitless as ‘they don’t speak the same language’; it resulted in ESD leads disengaging from the process because they felt that they had to prioritise their clinical work. As noted by a service manager, cultural differences between organisations reflected differences in their communication style; they thought that this characterised communication efforts between commissioners and clinicians and stressed the importance of ESD services tailoring their networking approach to effectively reach out to different stakeholders. "I think there are very, very many competing priorities for funding other than commissioners, what you have to do is make sure that you get the ear of the commissioner, establish your relationships and networks and never miss an opportunity and that’s very much an individual thing". |
| 5 | Gorbenko 2023, USA | Examine processes of uptake and implementation of the Acute Hospital Care at Home waiver (expansion) programme in a national sample. This included examining the barriers and facilitators of the waiver programme implementation across implementation stages and describing strategies used to address these barriers and/or best practices. | Admission Avoidance Hospital at Home | Service level (clinical leaders) | Both pre‐existing HaH and new programs described challenges implementing waiver components that in some cases delayed them from moving past the preparation stage to implementation. Programs varied in their response to the value of the requirement for two in‐person patient monitoring visits per day, with some feeling it was “not necessary” if patients were monitored remotely, and that clinical need should drive monitoring rather than “a requirement for billing.” One clinical director from a program that had yet to enroll felt that the two‐visit requirement did not improve patient safety while a clinical director from another non‐enrolling program felt it was reassuring for providers and patients to see patients twice per day, noting it was “okay and doable”. Other programs enrolling patients felt that they had been meeting these requirements. One clinical director explained that their pre‐waiver program included 4‐6 remote and one inperson visit each day, but ended up with two in‐person visits “90% of the time” due to patient need (for instance, administering antibiotics). "On days when we had two providers, one could do just televisits, and the other one might do the in‐person visits, which made more sense because to do both was logistically unworkable most of the time. So, on days when we had two providers available for visits, that's what we would do." “…we already had a contract with…emergency services, we just stayed with that territory.” One, there are certain services that the CMS waiver says that we have to be able to provide that we haven't done before, and so we're building that contract. The one that has been, honestly, the most challenging is food services. We have to, if patients…don't feel like they have adequate access to food, we have to be able to provide that and so finding someone who can do that and do it appropriately, that's been a little bit challenging.” Compared to inpatient settings where many service components are provided by the hospital, hospitals needed outside vendors to provide selected services in HaH. Both enroling and non‐enrolling HaHs believed it was advantageous to handle certain components (e.g. durable medical equipment) in‐house for financial, convenience and quality control reasons. Other services, such as mobile radiology, were better provided by vendors operating regularly in the home. Some programs described temporarily using vendors to comply with waiver requirements and begin enrolling patients as soon as possible, while planning to eventually move components in‐house. Others sought to build longer‐term vendor contracts. Enrolling and non‐enrolling programs also discussed the details and time needed to solidify vendor contracts, as a barrier to begin enrolling patients. Both enrolling and non‐enrolling programs found the requirement to respond to patients within 30 min for urgent clinical issues challenging. “That does geographically limit us to patients we would otherwise be willing to accept from a treatment and management perspective”. Geographical limitations affected both staffing and enrollment numbers. One multi‐hospital system considered moving the program “node” (the brick‐and‐mortar hospital, where HaH patients would go if needed) to a different site or creating a second “node” to capture more patients. Others relied on partnerships with community paramedics, and noted that this allowed them to expand their geographic reach. Among non‐enrolling programs, several participants identified pharmacy services as a major implementation challenge. Key challenges centered on: where medications would be prepared and dispersed (e.g., inpatient vs. ambulatory pharmacy), how many days of medication should be given to a patient, how and by whom medications are delivered, and how medications are documented and paid for. Medication safety was also a pressing issue across interviews, with one participant querying, “How do you manage chain of custody…?” Many participants discussed ongoing efforts within institutions to prevent medication errors and other risks to patient safety without burdening patients or providers. "Actually, the biggest part that was difficult for us was the pharmacy piece more than any other. Because along with it, we already have CMS approval and then we've got [state] approval…They're like, ‘You can't provide medications to a patient's home because you're an inpatient hospital.’…that's been the piece that's been the most difficult is to get other entities around this to understand that these are patients in the hospital…and still we are still waiting to admit our first patient.” Leaders of enrolling programs noted that they had implemented all required pharmacy components. Home healthcare nurses played a critical in medication delivery and, for several participants, provided the most viable solution for addressing pharmacy challenges. The most common approach was to have nursing staff deliver the medications directly to patients and to complete medication reconciliation at each visit. Most participants described building electronic health record (EHR) systems needed for patient care and billing as a priority but also a logistical and financial challenge. This was likened to building “an inpatient EHR [system] to be administered in an outpatient world” as “CMS was really clear this patient is inpatient”. HaH was to be a virtual unit of the hospital, not an outpatient service, while HaH programs that existed prior to the waiver often operated using outpatient records. EHR readiness varied starkly between enrolling and non‐enrolling programs. All but one non‐enrolling program described the EHR as a critical piece preventing them from enrolling patients, and two non‐enrolling programs reported that their HaH “go‐live” date was tied to the completion of the EHR. “…because this has to operate like an inpatient unit, but have transfer orders and charges in and out from vendors…we have homecare documentation system and it isn't even the same as our inpatient documentation system. So, we essentially had to rebuild everything to make sure that we've got the technology, the documentation system, the protocols really lined up with inpatient care versus ambulatory or homecare.” Support received from informatics executives. |
| 6 | Hitch 2020, Australia | Describe staff perceptions of the trial of an early supported discharge model of care for stroke survivors | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Implementation trial) |
Service level (staff) | Some staff reflected on the value of reviewing organisational data, workforce consultations and benchmarking against other services to inform the trial process. The relative priority of ESD within the organisation was understood by staff to interact with competing priorities, however they perceived a strong tension for change. ESD was not initially perceived as compatible with the community‐based rehabilitation context, with several participants describing feeling forced to choose between models of care rather than adopting a hybrid approach. These choices manifested themselves in changes to long‐held practices, which were particularly challenging for some of the smaller professions. While these changes were perceived as a positive opportunity to work in new ways by some, others found they challenged beliefs around the core business of community‐based rehabilitation. |
| 7 | Kraut 2016, Australia | Explore factors that indicated patient suitability and likelihood for referral and utilisation of early discharge rehabilitation at home | Early Discharge Hospital at Home for stroke (Rehabilitation at home) |
Service level (patients and staff) | Staff described a number of disadvantages that their patient could encounter, including a reduced intensity of rehabilitation compared with hospital. |
| 8 | Lemelin 2007, Canada | Evaluate the acceptance of a hospital at home programme managed and provided by nurse practitioners | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | "[There was] little opportunity to develop relationships with residents. I am not sure there was enough "buy in" from docs; there was subtle resistance to it. That changed over time as more of the attendings came to know us. Even though they rotate every two weeks, eventually they get to know you." (Nurse practitioner) |
| 9 | Moule 2011, England | Explore how the early stroke discharge team members and external stakeholders experienced the service implementation process | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (New service) |
Service level (staff) Systems level | For development of the model of care, operational matters, pathways, team composition and functioning, stakeholders from health and social care needed to be part of the development process. This approach may have helped to get social care implemented and the capacity of the team could be increased. (Stakeholders from health and social care) When the service started, the health professionals delivering the service perceived that their specialism in stroke rehabilitation created tension between them and the Community Rehabilitation Team. |
| 10 | Sims 1997, England | (1) Evaluate within the borough the practicality and acceptability of the 'Going Home Service' to patients and to staff employed in the service and in other services on which the scheme impinges (2) Establish the impact on informal carers |
Early Discharge Hospital at Home for orthopaedic conditions (New service) |
Service level (staff) |
Many respondents noted that the concept of early discharge conflicted with traditional views about length of hospitalisation held by clinical staff and patients. Staff thought that the three main disadvantages from the patients’ perspective were: … the service not being comparable to the 24‐hour specialist care available in hospital |
| 11 | Testa 2021 | Explore health professionals’ perspectives on the factors impacting Aged Care Rapid Response Team utilisation in the care of acutely unwell residential aged care facility residents | Admission Avoidance Hospital at Home (Acute, residential care) |
Service level (staff) |
"The development of good relationships with other services and providers was seen by the ARRT team to encourage referral to ARRT. This sentiment was echoed by participants external to the ARRT team. I personally think they're amazing. It’s a really good service. It ticks the boxes for getting the right patient, the right care, in the right place. And they're so easy to liaise with, and yeah just fantastic." (Extended Care Paramedic) |
Finding 2. For healthcare services planning to implement Hospital at Home, current systems need to integrate activity data and service costs. This allows healthcare services to collate total costs and savings to measure financial impact. This is important as policy makers, hospital executives and insurers from multiple‐payer settings require evidence about the financial impact of Hospital at Home to inform commissioning decisions. For multiple‐payer systems, financial impact and approval could be enhanced by including patients who contribute smaller financial benefits to the hospital if they were an inpatient (moderate confidence).
Early Discharge Hospital at Home
Managers reported the inability to capture healthcare provider activity associated with Hospital at Home services within existing systems (Dismore 2019), including nursing data (Fisher 2021), and a need to pre‐emptively address this barrier before implementing Hospital at Home (Dismore 2019).
Admission Avoidance Hospital at Home
Healthcare service managers reported that the absence of a single billing and payment mechanism was a significant policy and operational barrier to implementing Hospital at Home in a multiple‐payer system (Brody 2019). This barrier led to difficulty in signing up additional insurers (Brody 2019). A single billing and payment system, where all bills are collated first by the hospital, was perceived to prevent patients receiving bills from multiple providers and to facilitate data capture on total costs and cost savings (Brody 2019).
Healthcare leaders that were not successful in enroling patients in Hospital at Home struggled with how to calculate and measure financial impact and financial executives were hesitant to invest until a clear benefit could be demonstrated (Gorbenko 2023). Healthcare leaders that were successful in enrolling patients in Hospital at Home made the business case at their institutions, for instance, by focusing on patients who contribute smaller margins to the hospital (Gorbenko 2023).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Brody 2019, USA | Examine facilitators and barriers to implementation of Hospital at Home programme over its first year of operation to provide others the opportunity to plan effectively for operationalisation | Admission Avoidance Hospital at Home for various acute conditions (This study focused on the first year of operation) |
Service level (staff) Systems level (executive leader) |
"One of the most significant policy issues related to implementing HAH‐Plus is the absence of a method for assessing costs and cost savings, and thus how and how much organizations should be paid per case. This barrier led to difficulty in signing up additional insurers. When multiple partners are all billing vs. one to two superbills like in current hospitalizations, it becomes unwieldy both administratively and for patients/family. An additional barrier is the need to create a single unified billing and payment mechanism. A solution is to suppress bills from going directly to patients and have them collated into a single patient superbill similar to other bundled payment initiatives. " |
| 2 | Dismore 2019, England | Identify positive drivers and potential barriers to implementation of hospital at home for patients with exacerbation of COPD and low risk of death using the Dyspnoea, Eosinopenia, Consolidation, Acidaemia and atrial Fibrillation (DECAF) prognostic score and assist wider implementation | Early Discharge Hospital at Home for COPD (Implementation trial) |
Service level (patient, caregivers and staff) | An operational concern was the inability to capture activity within current payment systems. “Our work in trying to get the centre to change the way... we can record the data for hospital at home patients... perhaps by us doing that it would make it easier for other trusts to go down the hospital home route in the future” (Manager) “If we are employing consultants, junior doctors, respiratory nurses, specialists nurses... and we are not having the patient in hospital so we are not getting the tariff for that... somebody has to pay the wage bill... and it’s about understanding that payment mechanism... then that becomes a lot easier for everybody because that is the kind of thing that will stop people moving forward” (Manager) |
| 3 | Fisher 2021, UK | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service. (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery. |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
"A frequently raised issue was that nurses’ contribution was not captured by the SSNAP, leading to a big loss of information on ESD input: The nurses spend an awful lot of time with our patients and none of their data is captured." |
| 4 | Gorbenko 2023, USA | Examine processes of uptake and implementation of the Acute Hospital Care at Home waiver (expansion) programme in a national sample. This included examining the barriers and facilitators of the waiver programme implementation across implementation stages and describing strategies used to address these barriers and/or best practices. | Admission Avoidance Hospital at Home | Service level (clinical leaders) | Enroling programs had already made the business case for HaH at their institutions, for instance by focusing on HaH for patients who contribute smaller margins to the hospital. Non‐enroling program leaders struggled with how to “fully calculate and measure financial impact” and financial executives were hesitant to invest until a clear benefit could be demonstrated. |
Theme 2: Processes, resources and skills required to safely and effectively implement Hospital at Home
Finding 1. Safety concerns were expressed by all stakeholders, such as for patients going home alone in regard to pain management and their mobility, and staff expressed concern for their own safety due to home hazards, patient‐related factors and ergonomics. Patients were reassured about their safety with access to staff (including via phone) and equipment for safe monitoring. Timely delivery of appropriate equipment in the home alleviated some staff concerns (high confidence).
Early Discharge Hospital at Home
Staff perceived the ability for the patient and caregiver to ‘cope’ and the risk of readmission were important factors (Kraut 2016). Patients felt they needed to be ambulant before going home, which ranged from walking a few steps with minimal assistance to being ‘completely independent’ (Kraut 2016). When at home, patients experienced mobility problems with stairs, heavy doors and using their small living spaces (Kylén 2021).
Physicians had varying views around COPD patients' preference for the service, with some physicians believing patients feel safer in hospital, while other physicians disagreed (Dismore 2019). Hospital staff were concerned that the home environment may not be ideal for patient rehabilitation, with restricted mobility, lack of suitable equipment, and risk of re‐admission (Sims 1997). Staff expressed concern about alcoholism requiring two staff to visit patients due to uncertainty around safety (Fisher 2021). Staff also express concern about occupational health and safety due to hazardous home environments, including aggressive dogs, or damaging their backs if they were required to transfer patients from low beds and chairs (Dow 2007a).
Patients were fearful of problems occurring overnight when there was no monitoring or surveillance (Dubois 2001). COPD patients felt safe and reassured at home partly due to daily visits from the nurses and confidence in the skills of the clinicians (Dismore 2019). Patients perceived daily visits from a nurse contributed to feelings of safety (Wang 2012). Also having an inclusion criterion that there should be an outgoing call landline in the patient's house, so that a patient could call for assistance if their condition deteriorated, enhanced safety (Dean 2007). Visits from the team made stroke patients feel secure at home; the clinicians were expected to be experienced and competent in stroke rehabilitation and support them to complete daily activities (Nordin 2015). Stroke patients highly valued visits from staff, felt safe knowing someone would check on them, and perceived the staff as knowledgeable and experienced with stroke rehabilitation (Lou 2017). Subacute rehabilitation patients expressed multiple safety concerns about mobility, wound care, medications, causing damage to their new joint and not having a live‐in caregiver if something was to happen when they were alone (Wallis 2022).
Availability of caregivers for stroke patients was considered essential for patients who were not functionally independent (Kraut 2016) or had severe disability (Fisher 2021). When including complex strokes, staff noted increased workloads coincided with increased staff sickness, that caregivers struggled to cope, and increased risks of readmissions (Fisher 2021). Staff and patients agreed that caregiver presence made it easier for patients to receive hospital at home (Kraut 2016). Patients’ acceptance of and sense of security about early discharge and home rehabilitation were linked to living with their partner (Lou 2017). A common reason that COPD patients declined participation in Early Discharge Hospital at Home was a fear of being alone when unwell, despite being offered same‐day social support (Dismore 2019).
Admission Avoidance Hospital at Home
Nurses considered high levels of pain as an indicator for hospital stay and appreciated a rapid response in receiving equipment at home to make the home safe (Manning 2016). Patients reported the consistency of nursing provided comfort, but some were concerned about safety for those living alone or with more serious illness (Levine 2021). Patients felt safe at home by wearing a wireless skin patch for continuous vitals monitoring and having a physician available to contact (Levine 2021). Patients reported feeling safe with the presence of a caregiver, and because the team would be available and would refer to hospital if necessary and knowing when the staff would next arrive (Udesen 2021; Wilson 2002). Although not all patients felt the need to have a caregiver present to feel safe (Udesen 2021). Patients were also reassured by having a telephone number and the nurses’ encouragement to phone for any concerns (Wilson 2002). Patients and caregivers were concerned that diagnostics, equipment and medical care would not be available and, therefore, preferred hospital care (Wilson 2002).
Combined Admission Avoidance and Early Discharge Hospital at Home
Nurse practitioners perceived that patients experienced physical challenges such as having to prepare meals and difficulty accessing bathrooms (Lemelin 2007). Staff viewed the home as a challenge to staff safety, because of ergonomics and hygiene issues (Vaartio‐Rajalin 2020). Patients felt safe with more competent staff in this service and that they were less likely to encounter ‘students’ like they do in hospitals (Vaartio‐Rajalin 2021). Patients and caregivers were reassured with vital signs monitoring and accepting towards teleconsultation (Ko 2023).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Dean 2007, England | Evaluate the feasibility of a prospective hazard analysis when assessing quality and safety in a COPD early supported discharge care pathway | Early Discharge Hospital at Home for acute exacerbations of COPD | Service level (patients and staff) | One of the criteria for selection of patients for the supported discharge programme was that there should be an outgoing call landline in the patient's house so that a patient could call for assistance if their condition deteriorated. Hospital rules require that mobile phones are switched off when staff are on hospital premises so the usual route for patient to staff contact was not always available. |
| 2 | Dismore 2019, England | Identify positive drivers and potential barriers to implementation of Hospital at Home for patients with exacerbation of COPD and low risk of death using the Dyspnoea, Eosinopenia, Consolidation, Acidaemia and atrial Fibrillation (DECAF) prognostic score and assist wider implementation | Early Discharge Hospital at Home for COPD (Implementation trial) |
Service level (patients, caregivers and staff) | A common reason for declining participation in the RCT was fear of being alone when unwell, even when offered (same day) social support. The registered nurse stated that some patients were reluctant to accept social services because of perceived stigmatisation. Physicians’ preconceptions included the view that hospital care provides respite for carers and ensures patients feel safer. “The patient themselves may not be ready for it… I think they need to stay in hospital where they feel safer not because it is safer but basically they feel safer and also it gives a break (to) their carer." (Physician) Another physician disagreed, stating “That’s kind of often how people view patients with COPD that they want to come to hospital but actually it’s not true”. (Physician) Patients felt safe and reassured during HAH due to daily visits from the RSNs…confidence in the HAH clinical team and the availability of emergency services if return to hospital was needed. |
| 3 | Dow 2007b, Australia | Determine how the role of the carer in rehabilitation at home programmes is constructed | Early Discharge Hospital at Home for orthopaedic and neurological conditions (Rehabilitation at home) |
Service level (caregivers and staff) | One concern expressed by staff working in RITH programmes was their occupational health and safety. Providing rehabilitation services at home meant that they were sometimes exposed to hazardous home environments, including aggressive dogs. They were also concerned about damaging their backs if they were required to transfer clients on their own or to work off low beds and chairs. |
| 4 | Dubois 2001, Switzerland | Evaluate patients' satisfaction with Hospital at Home care | Early Discharge Hospital at Home for various conditions including community‐acquired pneumonia, intravenous anti‐biotherapy, deep venous thrombosis) (Pilot programme implemented 2 years prior) |
Service level (patients and staff) | The fear of problems arising at night, the lack of constant patient surveillance…. created anxiety and insecurity in some patients during H‐Hcare. |
| 5 | Fisher 2021 | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service. (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery. |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
Ensuring the safety of patients who had more severe disability was an important concern. One team questioned whether or not they would be able to provide the right equipment to support these patients at home. Relying on relatives to support patients with severe disability was risky and respondents highlighted the need to consider the willingness and readiness of patients’ spouses and families to assume caring responsibilities. "If anyone’s got a history of alcoholism we have to go out in twos because we just can’t predict it. That then makes it so much more complicated because we all manage our own diaries and just getting the right person at the right time to be able to double up with you is difficult." After a trialling period of accepting more complex strokes, staff observed that staff sickness rates increased dramatically. Staff working harder to maintain the quality of the service at the expense of their own health was suggested as a potential explanation. They get home and it’s actually the carers that really struggle and they just can’t cope, and that’s when accidents happen and they end up back in hospital, or infections and that sort of thing come on quite quickly. |
| 6 | Ko 2023, Singapore | Explore the experiences and perceptions of patients and their caregivers admitted to a Hospital at Home programme | Combined Admission Avoidance and Early Discharge Hospital at Home (Acute care) |
Service level (Patients and Caregivers) | Most participants felt assured with vital signs monitoring and accepting towards teleconsultation with their providers through video calls, voice calls, and texts. “…it’s better…The fact that he [the provider] video called me, I was more assured that oh, maybe it was nothing… it is not something that needed immediate attention.” (Patient) “…monitoring the vital signs was important, like knowing that the temperature and knowing that her heart rate and everything was normal. It gives us assurance.” (Caregiver) In contrast, several other participants highlighted issues with vital signs monitoring, including the discomfort of the wearable patch, and instability of transmission of readings. Despite these issues, most participants felt that the inconveniences were minor and acceptable. They were reassured through constant communication with the care team. “Once I go shower, the patch will not stick again… and you sweat so much, it will come out.” (Patient) “…I think initially they [care team] were still uncertain about whether it’s [VSM] functioning and whether the blood pressure data was being sent.… Yeah, I think there wasn’t real‐time feedback…so we are not sure whether it is sent over or not.” (LAR) |
| 7 | Kraut 2016, Australia | Explore factors that indicated patient suitability and likelihood for referral and utilisation of early discharge rehabilitation at home | Early Discharge Hospital at Home for stroke (Rehabilitation at home) |
Service level (patients and staff) | Safety for the patient, their family, and treating home visiting staff, and an identified ability for the patient and their carer to cope at home were the main factors considered with regard to patient suitability for referral to RITH. Possible readmission to hospital due to recurrence of illness [was considered]. Patients and staff generally reported there would be approval all round, "…the hospital wouldn’t send you home unless you could cope." However, the level of agreement between each patient and their treating health professional regarding the likelihood of them leaving hospital sooner with RITH varied. "Well, she’d virtually have to be independent to walk because we won’t be there at her beck and call, so she’d have to be able to get up, get out of the bed, go to the toilet and just do the basic things ... by herself." (Health professional). Staff opinion about the level of mobility required for discharge with RITH similarly varied according to the patient and their individual situation. All patients stated that they would need to be ambulant before going home, but for some this meant walking a few steps with minimal assistance while others wanted to be "completely independent". The level of support available at home together with personal expectations for recovery influenced patient opinion regarding level of mobility required for discharge with ESD. "I think I need to be able to stand for longer ... walk a bit better ... by myself ... I need my left hand working ... because right now, it’s not doing anything." (Patient) If a patient was not independently functioning, the presence and availability of family and/ or carers to assist was considered essential before ESD was considered. When asked about barriers and enablers, staff and patients agreed that the presence of family support would make it easier to go home with RITH. |
| 8 | Kylén 2021, Sweden | Explore how the environment was integrated in rehabilitation at home from the perspective of people post‐stroke, living in Sweden | Early Discharge Hospital at Home for stroke (Rehabilitation at home) |
Service level (Patients) | For some of the participants, it was difficult to predict the challenges of coming home from the hospital. When they had been asked about possible barriers in their home environments, they had responded that everything probably would work out just fine. However, when they returned home, it was not as easy as they thought, and many of them experienced problems. They also described barriers in the environment, such as stairs, heavy doors and small spaces, that limited their mobility and the possibility of using their living spaces. "Yes, they (the HCPs at the hospital) asked, and I said, “I feel so good at home; I can do it all”. And then when I got home, it was not like that. When you lie in your bed and just turn your head right and left, then you feel quite healthy, but when you get up, it was not so easy."(Patient) |
| 9 | Lemelin 2007, Canada | Evaluate the acceptance of a hospital at home programme managed and provided by nurse practitioners | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | They also perceived that, while patients felt more control over their personal health needs, they experienced some day‐to‐day physical challenges such as having to prepare meals, and difficulty accessing bathroom facilities. |
| 10 | Levine 2021, USA | Elucidate and explain patient perceptions of home hospital versus traditional hospital care to better describe the different perceptions of care in both settings | Admission Avoidance Hospital at Home for a variety of acute conditions | Service level (patients) | Feeling as if they: "could call [the care team] anytime" (patient) as reasons for feeling safe. “I was happy with him, you know, he was available any time that I called him and you know if he needs to come in for anything, he was more than happy. And [I was happy] that I have that kind of relationships with a physician to the point that you know I could reach out any time in the moment”. (Patient) Some home patients expressed doubts about the program’s safety in the case of more serious illness or in the case of a patient with less social support. “...[I] didn’t have the issue of different nurses on different shifts and on different days, so there was a continuity of care that was comforting”. (Patient) “I really like that they had me on the monitor so if anything was going on I had the capacity to call them and… they knew what my heart rate was, my respirations so they always had a pretty good check on my health. So I thought that was really comforting”. |
| 11 | Lou 2017, Denmark | Investigate how mild stroke patients and their partners experience and manage everyday life in a context of early discharge rehabilitation at home | Early Discharge Hospital at Home for stroke (mild) (Rehabilitation at home) |
Service level (patients and caregivers | “Well, first of all, I just didn’t feel that ill. And second, I knew Emma would be around. And that means a lot.. . a sense of security”. (Patient) Several patients remarked that going home to an empty house would have been a much more daunting prospect. All of the patients reported feeling safe and confident about going home, and only one partner, Ellen, voiced some concern over getting her husband, Frederik, home. She worried that he might have another stroke and about getting timely help, as they lived in a relatively remote area. However, she recognised with a smile that having him in the hospital would "also be a hassle". "In this process I’ve felt completely safe. Like, they didn’t just send me home and hope for the best; I knew someone would check up on me, that I was not alone". (Patient) Teams were very knowledgeable and experienced with stroke rehabilitation and that they were able to put themselves in the patient’s shoes. The participants highly valued visits from the ESD team. |
| 12 | Manning 2016, Wales | Explore how traditional and new models of care meet patients’ needs according to patient and staff experiences | Admission Avoidance Hospital at Home for various conditions (e.g. falls and fractures) | Service level (patients and staff) | Level of pain was a good indicator as to the reason for a hospital stay for orthopaedic patients. (Nurses) Rapid response of occupational therapy and physiotherapy providing equipment at home. (Nurse) Able to make home safe with equipment. (Nurse) |
| 13 | Nordin 2015, Sweden | Describe patients’ expectations of coming home very early after stroke with support and rehabilitation at home | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Clinical trial) |
Service level (patients) | “… it feels secure to know that they are coming home, that they, I know that on Tuesday that she’s coming at 10 am, or whatever time it is (appointed time). So I know that they are coming here (to my home).” (Patient) “It is sensible that people are coming who know what they are doing with this kind of stuff.” (Patient). |
| 14 | Sims 1997, England | (1) Evaluate within the borough the practicality and acceptability of the 'Going Home Service' to patients and to staff employed in the service and in other services on which the scheme impinges (2) Establish the impact on informal carers |
Early Discharge Hospital at Home for orthopaedic conditions (New service) |
Service level (staff) |
Prior to ESD implementation, anxieties were common amongst health professionals even though the concept of HAH isn't new. “There was concern (4) that the home environment may not always be ideal for patient rehabilitation; mobility could be restricted by the layout and by lack of aids and adaptations.” Prior to ESD implementation, consultant doctors had concerns about the provision of emergency cover in HAH. Staff thought that the three main disadvantages from the patients’ perspective were… the risk of re‐admission. |
| 15 | Udesen 2021, Denmark | Describe and explore patients’ and caregivers’ experiences with home treatment | Admission Avoidance Hospital at Home for acute conditions | Service level (patients and caregivers | The response time was an important factor in generating a sense of safety. Many of the patients and the caregivers expressed that it seemed reassuring when ATO arrived quickly. A caregiver said: ‘I thought they were competent. They provided us with safety when we needed urgent help. They came in a moment’. The option to call ATO at any time while undergoing treatment was expressed as being important in order to feel safe. One patient stated: ‘I felt very safe because they said that there were no stupid questions, and we could call them if we were in doubt about anything’. This view is supported by caregivers who were not aware of this possibility and experienced feeling unsafe in the periods between the visits from ATO. Importance of caregivers’ presence varied from one patient to the next and did not necessarily affect the feeling of safety when receiving treatment at home; many of the patients expressed that their caregivers’ presence was always nice. Again, it was not necessary for them to feel safe, as they perceived their treatment was well coordinated. Several of the patients who stated that caregivers made them feel safer mentioned that it was always a source of confidence to have another person by their side, as caregivers could talk and ask about additional information. One patient stated: ‘I can express myself well enough, but I think the acute care team was happy with the presence of my wife and the nursing assistant because they could help with additional information. They know me well and could explain my medical story’ Few patients expressed that caregiver presence was necessary to complete treatment at home. One patient said: ‘I probably would not have chosen to be home if he was not here because I was too ill to take care of myself’. Very few caregivers felt insecure in managing treatment and care at home. A caregiver explained: ‘He was very ill, and it would have been safer for him to be at the hospital’. In this context, patients without caregivers should be able to manage self‐ care, which is pointed out by several patients. ‘It was nice to have someone because I was feeling very ill’ ‘It was just antibiotic treatment, so there was not much to be involved in’ ‘It’s always nice when she’s there, but that was not what made me feel safe’ They provided us with safety when we needed urgent help. They came in a moment’ ‘I experienced them as truly competent, and they were not in doubt about what to do’ |
| 16 | Vaartio‐Rajalin 2020, Finland | Describe Hospital at Home staff's perceptions about Hospital at Home care, including work structures, processes and outcomes | Combined admission avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | The HAH staff also perceived that the home was a challenge to staff safety and taking care of one's own safety and work conditions were noted: "Our ergonomics is harder to maintain at the patient's home than in hospital, there can be very limited space and the level of hygiene can often be demanding at home…and there might be pets disturbing wound care or IV antibiotics". (Focus Group) |
| 17 | Vaartio‐Rajalin 2021, Finland | Describe how adult, non‐palliative patients and their spouses perceive person‐centredness in Hospital at Home care | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (patients and caregivers | “In HAH the nurses are experienced and competent, while at the hospital they are often very unexperienced or nursing students” (Patient) “In HAH the staff are more competent and you feel safe.” |
| 18 | Wang 2012, Norway | Explore COPD patients’ experiences of a limited early discharge hospital at home treatment programme | Early Discharge Hospital at Home for COPD | Service level (patients and caregivers | “It was safe, because I knew she was coming! If I did not feel 100% well, I knew that she was coming tomorrow to check me.” (Patient) |
| 19 | Wallis 2022, Australia | Explore patient and caregiver barriers and enablers and components of care that may increase acceptability of Hospital at Home | Early Discharge Hospital at Home for total hip or knee replacements (Subacute rehabilitation, multiple‐payer setting) |
Service level (patients and caregivers | Patients who received inpatient rehabilitation expressed multiple safety concerns if they had opted for home‐based care. This included concerns about mobility and personal care (e.g., fear of falling in the shower), managing household activities, managing stairs, wound care, taking medications or injections, causing damage to the new joint, and not having a live‐in caregiver if something was to happen when they were alone. |
| 20 | Wilson 2002, England | Compare hospital at home patient and carer satisfaction with hospital care. Explore which aspects of the two care options (Hospital at Home or hospital care) were particularly valued or caused concern |
Admission Avoidance Hospital at Home for acute medical conditions | Service level (patients and caregivers | "I’d got the knowledge that if I did need any help I could get it. They left me a telephone number, they really stressed that when they left, if you want any help don’t forget to ring us ..." (Patient) "[I was] confident they would know if I was very ill and that they would move me to hospital, that they would get the doctor." (Patient) "You felt calm, you knew somebody was coming, at ease. You’re not waiting for a nurse to come and help you to do things like you are in hospital." (Patient) "If there was something wrong with his heart he should be in hospital, where all the necessary equipment is." (Caregiver) "I needed a brain scan really, and he [the GP] couldn’t have one done in here on his own and if he got the results he’d probably not know what to look for ..." (Patient) "I wanted a second opinion because I was getting really worried about this ... In hospital at least she would have seen a doctor, and a doctor would have examined her and put her on medication." (Caregiver) |
Finding 2. Identifying patients using eligibility criteria and clinical judgement was challenging for referrers in the acute setting, especially in the start‐up phase of implementation. Services developed criteria to maintain responsiveness and manage capacity, and conducted teaching sessions to help acute staff to refer patients to Hospital at Home. Some services had concerns when staff were working at low capacity (not enough referrals), if staff were seeing patients that were either too ill, or did not need the higher level of care required for Hospital at Home (high confidence).
Early discharge hospital at home
Service level staff reported that misconceptions about the service from acute ward staff meant training was required to enable appropriate stroke patients to be referred to the service (Moule 2011), including having a trained nurse as a 'gatekeeper' (Fisher 2021). They also were concerned that the team were working at low capacity as they were limited in the cases they could accommodate due to restrictive eligibility (Moule 2011). Excluding patients with severe disability helped services to manage capacity and maintain responsiveness (Fisher 2021). Flexibility in use of the selection criteria was also necessary to manage cases when there were issues with the availability and quality of community rehabilitation services in the catchment area (Fisher 2021). Physicians believed that improving the appropriateness of referrals to the service for stroke patients required a balance of flexibility and specificity of the selection criteria (i.e. not overly restrictive) (Chouliara 2014). Consultants indicated that the timing of referral to the service was based on different factors including staff experience, knowledge, expectations and duration of the service, and inpatient rehabilitation waiting times (Chouliara 2014). At the beginning of the service implementation, hospital clinicians did not always trust predictive tools used to assist patient (COPD) selection for the service, which caused delays in returning home, but this improved with experience (Dismore 2019). Opinions varied as to when the service should be considered, from immediate arrival on the acute ward, to at least two weeks after their stroke depending on the amount of recovery in their condition (Kraut 2016).
Admission avoidance hospital at home
Emergency department physicians had difficulty identifying, screening and referring patients to the service, and were unclear or untrained (moonlighting staff) in which diagnoses were eligible to be safely treated in this setting (Brody 2019). Service‐level participants perceived that restricting eligibility for specific acute conditions or circumstances (e.g. patients were required to have a live‐in caregiver) allowed for intensive monitoring and modifications for quality and safety (Brody 2019). Hospital staff were frustrated if there were delays for medically fit patients being able to be discharged home when waiting for the social care services to become available (Manning 2016). In Brazil, a lack of knowledge about the function of the service, including eligibility criteria, hampered referrals to the service (Andrade 2013).
Service leaders identified that a manual process for identifying eligible patients in the electronic health record was time‐consuming and involved co‐ordination between hospitalists and Hospital at Home staff (Gorbenko 2023). They also reported hesitancy of physicians to refer patients to Hospital at Home due to being unfamiliar with the service or had concerns over the level of care their patients might need and their legal responsibility in making a referral “if there is a bad outcome” (Gorbenko 2023). This could be overcome with education to where hospitalists and emergency physicians become comfortable with referring patients into Hospital at Home (Gorbenko 2023).
For patients in residential care, the importance of creating consensus between ED service staff and general practitioners about who should decide if a service was needed was essential as it was sometimes used if a medical assessment was required (Udesen 2022). Also acute care nurses were challenged with whether the most appropriate solution was to keep the resident at the nursing home or to admit the patient to the hospital (Udesen 2022).
Combined Admission Avoidance and Early Discharge Hospital at Home
Nurse practitioners perceived they were either overqualified for the clinical role or felt that patients were too ill to be cared for by nurse practitioners outside the hospital, suggesting the wrong patients were referred (Lemelin 2007). Service‐level staff perceived that excluding patients with alcohol or drug problems was necessary for safety reasons (Vaartio‐Rajalin 2020).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Andrade 2013, Brazil | Understand the organisation of the health system from the perspective of professionals that provide home care services | Admission Avoidance Hospital at Home for various acute conditions | Service‐level (staff) | We have this problem, because everyone thinks that the Home Care Program is home visits, only for chronic patients. Lack of knowledge on the Home Care Program and its concept, its function, insertion into health services and on user admission criteria are factors that hinder effective insertion of the program in the Health System. The interviewed professional emphasize that this situation prevents actual consolidation of work in the system: People know that the Home Care Program exists, but no one knows how it works and who it's for, which type of patient it's for, and the requisites the patient must have to be included in the Home Care Program. Insertion of the Home Care Program in the system is still not appropriate. I think that it is mostly due to lack of information. difficulties mainly include lack of knowledge on the role of the Home Care Program, showing the need to overcome fragmented practice in the health care system. The construction and promotion of knowledge in relation to home care that can be implemented by the professionals of the Home Care Program is therefore necessary. |
| 2 | Brody 2019, USA | Examine facilitators and barriers to implementation of Hospital at Home programme over its first year of operation to provide others the opportunity to plan effectively for operationalisation | Admission Avoidance Hospital at Home for various acute conditions (This study focused on the first year of operation) |
Service level (staff) Systems level (Executive leader) |
Identifying, screening, and recruiting patients was a challenge in the start‐up phase of HAH‐Plus. Unclear what eligible diagnoses can be safely treated in this setting Unfeasible to ask ED physicians to remember when they could refer or to hold a patient overnight for admission to HAH‐Plus. Additionally, moonlighting physicians were not trained in how to refer. One benefit of starting the program slowly was that it allowed for intensive monitoring of quality and safety in the initial patients and developing an understanding of where potential for errors existed so that processes could be modified using continuous quality improvement principles. Criteria were updated to match advances in medical care that allowed for safe provision of care for a wider array of illness. E.g., Asthma. Eligibility was also expanded to patients who did not have an available caregiver. |
| 3 | Chouliara 2014, England | Explore the perceptions of healthcare professionals and commissioners regarding the challenges and facilitators to implementation and perceived impact of early supported discharge services | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Study was conducted in the first year of implementation) |
Service level (staff) Systems level (commissioners) |
“Just getting a bit more understanding of what the content is so that we can decide that Early Supported Discharge is in the best interests of the patient”. (Acute Stroke Unit Staff). "I think the criteria are good because they are not too defined or too loose; I think there are very few inappropriate people that come through". (Stroke Physician). In Site A, opinions varied with two respondents arguing that discussions with Early Supported Discharge services should be made “the minute patients arrive in the acute unit”. (Service level) Four others argued that the first two weeks after stroke is a very early stage for such decisions as “a lot of recovery will be happening while patients are still on the acute”. (Service level) |
| 4 | Dismore 2019, England | Identify positive drivers and potential barriers to implementation of hospital at home for patients with exacerbation of COPD and low risk of death using the Dyspnoea, Eosinopenia, Consolidation, Acidaemia and atrial Fibrillation (DECAF) prognostic score and assist wider implementation | Early Discharge Hospital at Home for COPD (Implementation trial) |
Service level (patient, caregivers and staff) | In the beginning predictive scores from DECAF may not be trusted. Early uncertainty with hospital at home selected by DECAF. Initially, some physicians expressed concern that, in their judgement, true risk for an individual patient was underestimated by DECAF. This led to delays in return home, which on occasion was unsettling for patients. “They have certain reservations, so you’ve got that conflict between their clinical impression and the predictive score… the simple score almost always outperforms clinical judgement, but clinicians don’t like to think that’s true”. (Physician) With experience, physicians became more confident using DECAF and the safety within HAH model of care: “As you get evidence suggesting it works and it’s safe you’re more confident in doing it”. (Physician). This was reflected in the wider HAH population as delayed return home was primarily an issue at the start of the trial. |
| 5 | Fisher 2021 | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
Adhering to selection criteria regarding disability levels helped the services to manage capacity and promote responsiveness. Services struggled to offer the therapeutic intensity that is required to address the needs of more severe patients, and attempting to cater for their needs could dilute the intensity of the service for the rest of the patients or reduce the flow of new patients into the service. Why would you take someone who was more dependent home, when you are going to have to rely on many more agencies to make sure that they get out there in a timely manner. You’ve got an ambulance crew that are prepared to take someone into the house because we have huge issues with transferring patients from the ambulance, to get them in to their homes again. So, that’s not just a decision that can be made by an ESD team providing it. It’s also about whether ambulance would support it, whether social services would support that, whether the carer’s want it. One team explained how they changed their model of service to improve responsiveness and further reduce hospital length of stay. Introducing two streams in the service allowed them to distinguish between mild to moderate patients with a straightforward discharge process and patients requiring more complex discharge planning. As a result, they managed to maintain the flow of patients from the hospital and free therapy time. Adding cognition to the eligibility criteria, however, was not considered the way forward because it could lead to the exclusion of patients who could benefit from the service, despite their cognitive problems. I feel that some bed managers don’t understand what is a stroke. They think that if you’re medically stable, you can go home. But apart from being medically stable, you should be rehabilitation stable as well. Cognitively, if the patient is not able to function, can’t remember how to make a cup of tea, turn off the faucet, take his or her medication, it’s not going to be safe. Flexibility in applying eligibility criteria ‐ The availability and quality of community rehabilitation services in the catchment area was a key factor influencing the level of flexibility demonstrated by the teams in the use of eligibility criteria. In one site, nurses had assumed the role of the ‘gatekeeper’ of the service by conducting the in‐reaching and initial screening of the patients. Their thorough medical assessment helped ensure that patients who fit the criteria were admitted to the service as opposed to patients with increased risk of re‐admission. |
| 6 | Gorbenko 2023, USA | Examine processes of uptake and implementation of the Acute Hospital Care at Home waiver (expansion) programme in a national sample. This included examining the barriers and facilitators of the waiver programme implementation across implementation stages and describing strategies used to address these barriers and/or best practices. | Admission Avoidance Hospital at Home | Service level (clinical leaders) | The majority of programs reported a manual process for identifying eligible patients in the EHR, which was often time‐ and labor‐intensive and involved coordination between hospitalists and HaH personnel. One clinical director at an enrolling program described this model as “push and pull…more of the pull approach”. Some programs described hesitancy among providers who were not familiar with HaH to refer patients. One non‐enrolling program reported that some physicians had concerns over “the level of care their patients might need” and their own responsibility in making a referral “if there is a bad outcome”. Once we found a team lead physician that was willing to test it out ‐well, first we were very conservative, so it's like how do you find perfect “patient” to bring into the home? But as this physician started to gain more experience and we're bringing sicker patients into the home. “It's getting that education piece to where the hospitalists and the Emergency physicians are comfortable with referring that patient into this." “We have to get them back down in the ED and do an H&P even though maybe the ED doc feels comfortable having done some enrollments. It's following the checklist no matter what, where right now, we have clinical judgement and the patient's engagement with us sort of dictating that. We understand why. We understand the consistency and why there is guardrail on this plan. It's going to be more oversight in our team, our coordinators to make sure every single piece gets done.” |
| 7 | Kraut 2016, Australia | Explore factors that indicated patient suitability and likelihood for referral and utilisation of early discharge rehabilitation at home | Early Discharge Hospital at Home for stroke (Rehabilitation at home) |
Service level (Patients and staff) | Consultants indicated that the timing of referral to RITH was dependent on a number of factors including: level of staff experience, the duration of RITH service intervention (linked with staff awareness of this), current inpatient rehabilitation waiting times and staff expectations. |
| 8 | Lemelin 2007, Canada | Evaluate the acceptance of a hospital at home programme managed and provided by nurse practitioners | Admission Avoidance and early discharge Hospital at Home for various acute conditions | Service level (staff) | Most nurse practitioners also felt that the nurse practitioner profession was not the most appropriate for this position. While some said that the care did not require the expertise of an advanced practice nurse and that their skill set was not optimally utilized in the HITH study, others felt that patients were too ill to be cared for by nurse practitioners outside the hospital. |
| 9 | Manning 2016, Wales | Explore how traditional and new models of care meet patients’ needs according to patient and staff experiences | Admission Avoidance Hospital at Home for various conditions (e.g. falls and fractures) | Service level (patients and staff) | Their frustration when the patient was medically fit but they had to wait for social care services to become available before being able to discharge a patient home. (Nurses) |
| 10 | Moule 2011, England | Explore how the early stroke discharge team members and external stakeholders experienced the service implementation process | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (New service) |
Service level (staff) Systems level | Within the hospital setting, the team needed to relate to the existing ward staff, both nursing and therapeutic. Because of the way in which the team had been created, misconceptions sometimes arose among ward staff, and the team members reported the need to educate others as to their role and function, and to make clear their criteria to ensure that appropriate patients were being referred to them. “We did quite a lot of teaching sessions on the wards to explain what we were and where we’d come from, and what our criteria were.” (Staff) Staff were concerned that the team were working to a lower than expected capacity and were limited in the cases they could accommodate.The team only ever had seven or eight patients. This arose because they couldn’t work with people in nursing homes, or who had existing packages of care. |
| 11 | Udesen 2022 | Explore different healthcare professionals’ perspectives on and experiences with the ED‐based acute care service | Admission Avoidance Hospital at Home (Emergency Department‐based Acute Care Service for residential care) |
Service level (staff) | Concerning the decision‐making, the acute care nurses explicitly discussed the ethical concerns, especially considering the choice of treatment. Sometimes the acute care nurses would be in doubt whether the most appropriate solution was to keep the resident at the nursing home or to admit him/her to the hospital. 'Very often it is speculative what the patients’ ailments are. You do not know, but you focus 100% on what is best for the patient. Then you very often conclude that it makes no sense to transfer the patient to the hospital because it has no consequences’ (Focus group). Few participants in the nursing home focus groups described the service as a supplemental medical service that could be used if a medical assessment was required at a nursing home. This notion was supported by a few GPs who had experienced nurses who insisted that the GP should request the ED‐based acute care service. One GP explained that it made no sense to activate the service if a firm decision regarding admission or non‐admission of the patient already had been made. This exemplifies the importance of creating consensus about who should decide if this service was needed. One GP said that he does not always agree with the ED consultants’ decisions about treatment at the nursing home. This notion, however, was not supported by the other GPs. |
| 13 | Vaartio‐Rajalin 2020, Finland | Describe Hospital at Home staff's perceptions about Hospital at Home care, including work structures, processes and outcomes | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | “We don't admit patients with alcohol or drug problems to HAH… They are untrustworthy when it comes to being at home [at a certain agreed‐upon time] and they usually have many friends under the influence of alcohol or drugs at home, too, which makes the care situation very unsafe.” (Focus group) |
Finding 3. Leadership and co‐ordination from key champions, lead clinicians with medical responsibility and clinical accountability, managers with operational responsibility and other leaders were essential to provide high‐quality care. Hospital at Home managers, directors or co‐ordinators were responsible for creating a positive staff environment, ensuring protected time for training and clinical supervision, and facilitating service improvements (moderate confidence).
Early Discharge Hospital at Home
For acute conditions, good managers were involved in all aspects of service development and created a positive team relationship where staff felt equally valued regardless of their position (Karacaoglu 2021). For stroke teams, staff perceived that good leadership included having protected time for clinical supervision and training for staff, and for staff to be involved in generating new ideas and developments (Fisher 2021; Karacaoglu 2021). The co‐ordinator was considered a clinical champion, with clinical knowledge and accessible as a single point of contact between services that was considered essential for the programme’s success (Hitch 2020). High levels of staff investment and investment from informal leaders (e.g. nurse unit managers) were also important for its success (Hitch 2020). For orthopaedic and neurological conditions, a case manager was essential to manage the administrative aspects of the patient’s admission and communication with staff, GP and patients/caregivers (Dow 2007a). For various conditions, GPs considered that sole medical responsibility for patient care at one time was important to avoid confusion with co‐ordinating doctors, hospital doctors and GPs (Leung 2016). For orthopaedic conditions, staff considered that organisation, communication, co‐ordination and planning were essential to maintain high‐quality care (Sims 1997).
Admission Avoidance Hospital at Home
For residential care facility for conditions requiring acute care, a program manager was perceived to be experienced, with a clinical background in acute care nursing and could communicate, negotiate and co‐ordinate care with relevant key stakeholders (aged care facility staff, GPs, hospital specialists and specialist services) (Crilly 2012). The development and expansion of the service was led by the key drivers of the service – a program manager and director (Crilly 2012). GPs and other staff considered the program manager’s role an essential role to avoid or facilitate admissions (Crilly 2012). Establishing medical responsibility for the patients after they had received treatment by the acute care service was important (Udesen 2022). The medical responsibility resided with hospital staff when the patient was in hospital, and if the patient was in a residential care facility, clinical responsibility resided with the GP (Crilly 2012). This process enabled the programme manager to communicate and co‐ordinate medical care (Crilly 2012). Directors of nursing (programme leaders) emphasised that the role of a liaison officer (a registered nurse employed to liaise between hospital and residential care facilities) improved communication between hospitals, paramedics and hospital in the nursing home (Barnard 2016). ED clinical nurse specialists facilitated fast tracking of residents through the ED and referred residents to other specialities such as Allied Health (Testa 2021).
Staff considered that if co‐ordination was not managed well, it would cause delays in care delivery and communication (Brody 2019). For this service, co‐ordination included distinct areas ‐ teamwork, documentation, service co‐ordination, timely provision of services, clear expectations and building workflows (Brody 2019).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Barnard 2016, Australia | Understand the experience of Directors of Nursing from residential aged care who either had support of the Hospital in the Nursing Home service, or did not. | Admission Avoidance Hospital at Home for various acute conditions (Aged care facility) |
Service level (staff) | Liaison officers facilitate continuity of care and discharge notice when patients return from hospital to the care home. Without a liasion officer the care home wouldn't receive discharge information. Having a HINH liasion officer also led to improved respect of care home staff from people such as paramedics, who may challenge their decision to transfer a patient to hospital. |
| 2 | Brody 2019, USA | Examine facilitators and barriers to implementation of Hospital at Home programme over its first year of operation to provide others the opportunity to plan effectively for operationalisation | Admission Avoidance Hospital at Home for various acute conditions (This study focused on the first year of operation) |
Service level (staff) Systems level (executive leader) |
This coordination fell under six distinct areas: teamwork, documentation, service coordination, timely provision of services, clear expectations, and building workflows. If they were not tightly managed, quality and safety would suffer due to care delivery or communication delays, or missing information. |
| 3 | Crilly 2012, Australia | Describe and evaluate the structures and processes involved in a ‘Hospital in the Nursing Home’ programme | Admission Avoidance Hospital at Home for conditions requiring acute care (Aged care facility) |
Service level (patients and staff) | The Hospital in the Nursing Home programme manager’s role involved coordinating care by liaising with and referring ACF residents to specialist services. This role was central to the operation of the programme in terms of referral and communication. The ability of the programme manager to communicate and negotiate care with relevant key stakeholders (ACF staff, GPs, hospital specialists and specialist services) to ensure that the residential care facility resident received the most appropriate care was identified. This process was done in collaboration with the ACF resident’s GP. This worked well as the programme manager had a background in both acute care nursing in the hospital and community‐based nursing and thus was not only aware of service options available, but had a pre‐established working relationship with some of the other service providers. By organizing and bringing together additional resources (such as allied health, pathology, specialist medical and nursing practitioners, as appropriate) the patients could receive some treatment in the residential care facility. Furthermore, the key elements and responsibilities of the programme manager’s role were evaluated as successful, as continuity of patient care could be provided from one healthcare provider to another. It was imperative that the programme manager was able to recognize when HINH services were not appropriate, when aspects of care were outside of the scope of practice of herself or the ACF, and when hospital admission was appropriate for the ACF resident. Thus, the programme manager’s role was formally designated as a nursing role. In terms of the nursing structures, the HINH programme manager (a Registered Nurse) was perceived to be experienced; with a background in acute care. This was felt to be fundamental to the role as the manager had to assess whether HINH or hospital admission was most appropriate. "Even though it is aged care, it is very, very important that they [the HINH programme manager] have an acute background. We’re not going out to nursing homes teaching nursing home staff how to do aged care. They’re already experts at that. All we’re doing is up‐skilling and supporting the acute care side." (HINH 2) GP’s found that when the programme manager provided additional assessment of an aged care facility resident at risk of hospital admission, this was beneficial. One GP stated that had it not been available, the resident would most certainly need to be transferred to hospital: “We can care more for our residents in the nursing homes with those added services”. (GP) The development and expansion of the HINH programme occurred with an integrated approach, led by key drivers of the service. The HINH programme manager and the HINH director were viewed by HINH staff to have a level of operational responsibility that could enable and facilitate growth to occur. One ACF nurse said: “it was definitely from the top who drove it”. (Nurse,residential care facility). There was an understanding that the clinical care of the ACF resident if in ED or hospital was by hospital staff, but when discharged from the ED or hospital back to the ACF, clinical responsibility resided with the GP. This meant that one main medical care provider had responsibility for patient care at one time, so confusion did not arise. This structure appeared to operate well during HINH programme operational hours because the HINH programme manager notified the GP and asked them to review the patient within 3 days (if discharged with antibiotics for example). |
| 4 | Dow 2007a, Australia | Make recommendations to the Victorian Government on best practice in rehabilitation at home | Early Discharge Hospital at Home for orthopaedic and neurological conditions (Rehabilitation at home) |
Service level (patients, caregivers and staff) | Case management was a feature of the bed substitution rehabilitation in the home programmes. A case manager’s role was to manage the administrative aspects of the client’s admission, communicate with the client’s general practitioner (in conjunction with the medical specialist) and communicate team decisions to the client and family. |
| 5 | Fisher 2021 | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
Clinical leads and managers were praised by their teams for creating a safe environment for staff to reflect on and acknowledge their limitations, while providing the opportunities to address knowledge gaps through further training. Despite capacity issues, time for supervision and training was protected in most teams; it was a way to promote staff retention and well‐being and cascade knowledge of evidence‐based standards through the team. Good leadership was linked to enabling staff members to engage in the running and development of the team. It was suggested that people perform better when they have ownership over aspects of the team function. Part of the leaders’ role was to keep the team informed about developments, share their vision and invite ideas. When introducing changes, some team leads stressed the importance of securing the team’s buy in and support to take things forward. Successful improvements happened collectively, with staff working in partnership to develop and implement a plan of action. |
| 6 | Hitch 2020, Australia | Describe staff perceptions of the trial of an early supported discharge model of care for stroke survivors | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Implementation trial) |
Service level (staff) | The hospital at home coordinator was identified as a key champion, with clinical knowledge, attendance at meetings, accessibility and acting as a single point of contact between services, contributing to the success of hospital at home. “I think if we didn’t have [REDACTED] or a coordinator, it would have fell apart. . . it’s important to have someone who is driving this process and that can be that main point of call to keep things moving along smoothly”. (focus group) High levels of staff investment were consistently identified as important by participants, and additional investment provided by management and informal ESD leaders (such as team leaders, managers, the steering committee, nurse unit managers and nurse practitioners) was also recognised within the service. |
| 7 | Karacaoglu 2021, UK | To understand staff views of implementing a Hospital at Home model in a Scottish care setting | Early Discharge Hospital at Home for various acute conditions | Service level (staff) | Participants described the presence of a positive team relationship where staff felt supported and valued regardless of their position: “Staff overall get on, it’s a great team. There is no like, you know, hierarchy or things like that. Everyone is treated as an equal” (HCSW). Strong team dynamic appeared to be facilitated by high satisfaction with management staff due to their personable qualities: “She is really dynamic, very positive and you can see her passion for the whole project and wanting to drive it forward” Management were described as transparent and involved staff in all aspects of service development, including decision making around patient care: “any changes with the patient, we have a meeting and discuss the patient and we’re asked for feedback once we’ve seen the patient so I do feel like we are really included” (HCSW). Staff reported high satisfaction with training received which focused on frequently utilised skills and in addition APs enrolled in a Master’s degree in Clinical Practice. Staff felt empowered by management to seek their own development opportunities: “Training wise everything is available to you…you just need to ask [name] or one of the senior members of staff” (HCSW). However, a tension existed between training uptake and sufficient staff available for service operation, particularly due to limited APs within the team: “…the other two [APs] have assignments due in tomorrow and have been off all week, so this has a massive effect on how many patients we can take into the service because there is only me here to assess them” (AP). |
| 8 | Leung 2016, France | Identify the incentives and barriers to the involvement of general practitioners in Hospital at Home | Early Discharge Hospital at Home for various acute conditions | Service level (staff) | According to general practitioners, teamwork with the coordinating doctor of the HAD was essential and necessary good communication and sharing of knowledge sessions for quality care. “Is it ourselves who coordinate everything or is it with the help of the coordinating doctor or the hospital doctor? In fact, very often, we do not know which role we have exactly in the HAD. What decisions to take?" "Do you always have to refer to the coordinating doctor? or to the hospital doctor? Or we take the decisions on ourselves?". (GP) |
| 9 | Sims 1997, England | (1) Evaluate within the borough the practicality and acceptability of the 'Going Home Service' to patients and to staff employed in the service and in other services on which the scheme impinges (2) Establish the impact on informal carers |
Early Discharge Hospital at Home for orthopaedic conditions (New service) |
Service level (staff) |
The majority of respondents considered good organisation, communication, co‐ordination and planning to be paramount in maintaining a good standard of care. |
| 10 | Testa 2021 | Explore health professionals’ perspectives on the factors impacting Aged Care Rapid Response Team utilisation in the care of acutely unwell residential aged care facility residents | Admission Avoidance Hospital at Home (Acute, residential care) |
Service level (staff) |
ARRT can facilitate the fast tracking of residents through the ED via the ED‐based Clinical Nurse Specialist, as well as refer residents to other specialities e.g. Allied Health. When I get the phone call from ARRT … I can just basically lookout for the patient as soon as they get on the screen. We can then kind of grab the medical team and say “Hey, let's quickly get someone on it”, you know, get them seen quickly, get them their scans happening, and then try and get them out quickly. So if someone didn't jump on board, they may sit in the [ambulance] bay for ‐ I don't know how many hours … Ido think that we can fast track them through [ED] to a degree. (ED‐based Clinical Nurse Specialist |
| 11 | Udesen 2022 | Explore different healthcare professionals’ perspectives on and experiences with the ED‐based acute care service | Admission Avoidance Hospital at Home (Emergency Department‐based Acute Care Service for residential care) |
Service level (staff) | All focus groups reported that patient responsibility was an important part to consider when bringing specialised care and treatment to nursing homes. Many participants discussed the importance of establishing who was responsible for the patients after they had received treatment by the acute care service. |
Finding 4. A multidisciplinary skilled workforce was required to implement Hospital at Home, with collaboration between teams and professionals (e.g. via team meetings) a core feature. However, maintaining responsiveness was important, and the absence of a waiting list for admission to Hospital at Home allowed a service to respond to the demand for hospital care. Building rapport with external partners was challenging, and allied health professionals noted difficulties with their professional line of reporting and supervision. Some teams were frustrated by a lack of resource allocation, others recognised that the service was better staffed than usual care. Teams were also challenged to meet intensity targets and address workforce shortages. Multiple strategies could enhance capacity and responsiveness, such as securing more funding, training family members, adopting new technologies and implementing telehealth appointments. However, this could affect the provision of patient‐centred care (high confidence).
Early Discharge Hospital at Home
Staff rotations or cross‐boundary working promoted a better understanding of each team’s role and assisted in more appropriate and timely referrals (Chouliara 2014; Fisher 2021). Weekly team meetings provided support and knowledge from each other (von Koch 2000). For orthopaedic conditions, staff valued daily team meetings in helping communication across the team (Sims 1997). For stroke, co‐location, team meetings and a ‘passion for stroke’ enabled teamwork, patient discussion and support (Fisher 2021; Moule 2011). However, communication with external partners did not have many opportunities to build up rapport (Fisher 2021). Allied healthcare professionals wanted to maintain their professional identity and be managed within their profession, making it challenging to lead the multidisciplinary service (Moule 2011). With management tasks being done within professional departments outside of Hospital at Home, no single person gave the team a sense of clear direction (Moule 2011). When implementing this service, the budget was not integrated, meaning that any changes to staffing required negotiation with several profession managers and the service needed to be fully integrated within the hospital system to ensure cover when needed (Moule 2011). For prostate cancer, staff described a collaborative team understanding each other’s role and a protocol helped aid teamwork, consistency of care and safety (Chevalier 2015). For COPD, the team was described as multidisciplinary, with an interdisciplinary approach (Dean 2007). For orthopaedic conditions, support workers worked well together in care delivery, and valued the health professional support from the multidisciplinary team (Sims 1997). For heart conditions, clinical decisions were shared across healthcare professionals involving the district nurse, the hospital nurse at hospital and doctors (Dinesen 2007). Staff perceived the absence of a waiting list was important to avoid delaying new admissions, as was the ability to provide a flexible number of visits depending on the patient’s presentation in order to expedite discharge and gain the patient’s confidence (Cunliffe 2004).
For stroke patients, staff expressed having rehabilitation assistants to deliver the repetitive everyday exercises allowed the highly skilled staff to focus on the more specialist elements of rehabilitation (Chouliara 2014). Providing a seven‐day service was uncommon with concerns around communication, responsiveness and reduced therapist input (Fisher 2021). Meeting intensity targets from clinical guidelines was challenging, especially when faced with staff shortages and limited capacity (Fisher 2021), and some patients could be held in the acute site until a slot became available, which unnecessarily prolonged their hospital length of stay (Fisher 2021). External stakeholders expressed that setting up the service with a balance of senior and support level workers may be more economical and provide greater capacity (Moule 2011). Stakeholders from social care expressed that the lack of involvement of social care undermined the team’s ability to provide holistic support for stroke patients (Moule 2011). For acute patients service, one service had difficulty recruiting a geriatrician, forcing the service to amend the eligibility criteria to more medically stable patients (Karacaoglu 2021). For stroke patients in residential care, double visits could be required, impacting on caseload and resources, with the focus on preventing readmission rather then reducing disability (Fisher 2021).
For orthopaedic and neurological conditions, staff perceived increased pressure when caring for frail and medically vulnerable patients (Dow 2007b). For stroke, most staff perceived there was an increased workload because they were managing an “inpatient caseload in an outpatient setting” (Hitch 2020). Staff recognised the service was better staffed than usual care services, and unique in providing both social care and rehabilitation in a co‐ordinated way (Cunliffe 2004). For acute medical and surgical patients, staff recognised the service was better staffed than usual care services, and unique in providing both social care and rehabilitation in a co‐ordinated way (Cunliffe 2004).
Agreement to deliver the COPD service in 48 hours helped a service achieve the primary aim of reduced hospital length of stay (Dean 2007). Commissioners felt there was a need to adapt components of the intervention to respond to the local healthcare setting and the variation in the stroke population and staff considered that a flexible length of intervention (i.e. the service could be extended or shortened), and a flexible frequency of visits, was important to avoid prolonging the service and delaying new admissions (Chouliara 2014). The timing and the number of visits were decided in partnership between the staff and patient and staff felt that patients realise once they are home that they do not need as many visits as they had first thought (von Koch 2000).
Admission Avoidance Hospital at Home
Nurses commented on the sharing of actions and responsibilities in care production at home for various acute conditions (Andrade 2013). For respiratory or urinary tract conditions (aged care facility), clinical decisions regarding the use of IV therapy were collaborative between staff (physicians, nurses, nurse practitioners, pharmacists) and staff could seek guidance when required (Papaioannou 2018). For a multiple‐payer system, service level staff perceived it was difficult establishing collaboration and teamwork with external partners (Brody 2019). Morning huddles with the team and external partners were developed to ensure service co‐ordination, team building and updates to care plans, and to ensure care needs were met (Brody 2019). Also, for working with an external pharmacy in a multiple‐payer system, a process was necessary to ensure each medication was faxed or electronically prescribed, received and delivered expediently for quality and safety purposes (Brody 2019). A physician expressed that the knowledge and experience gained from one patient are readily transferable to other similar patients, and this experience and knowledge can and should be shared with team members, and facilitated by hospital processes (Cegarra‐Navarro 2010).
Challenges around workforce shortages due to COVID‐19 and limited capacity to treat patients due to travel time were overcome by “leasing” staff from other home‐based programmes, using urban hubs where more staff were available, and providing teleheath appointments (Gorbenko 2023). For residential care, a small number of staff employed by the Admission Avoidance service restricted capacity that was amplified by the COVID‐19 pandemic (Testa 2021). Adopting telehealth expanded their capacity and staff considered expanding the service to weekends and after hours (Testa 2021).
Staff perceived increased pressure where nurses from the nursing home were caring for patients with subacute conditions that would be otherwise hospitalised plus their own usual caseload and responsibilities, and communication with the family and other members of the healthcare team also intensified (O'Neill 2017). Directors of nursing requested additional resources and funding to manage increased workloads for residential care staff (Barnard 2016). Directors of nursing also expressed a greater ability to assist anxious families with decision‐making as a result of multidisciplinary input (Barnard 2016). For residential care, collaboration between nursing home staff and acute emergency service helped decision‐making (Udesen 2022). More frequent use of the Residential in Reach programme occurred when the participating nursing home did not have sufficient nursing resources available and meant inappropriate referrals or communication with Admission Avoidance staff (Rayner 2022).
Combined Admission Avoidance and Early Discharge Hospital at Home
Nurse practitioners felt that the interdisciplinary team approach to care was beneficial to clients and important to establish (Lemelin 2007). Physicians were like consultants and available for nurses who were visiting the patient to make clinical decisions together (Vaartio‐Rajalin 2020). Physicians were frustrated with public policy makers' lack of understanding about their competencies and responsibilities in relation to resource allocation and resources (Vaartio‐Rajalin 2020).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Andrade 2013, Brazil | Understand the organisation of the health system from the perspective of professionals that provide home care services | Admission Avoidance Hospital at Home for various acute conditions | Service level (staff) | “The doctor who was with me had no doubt, he rolled up his sleeves, put on a glove and came in to do all the dressings with me and that without saying anything”. (Nurse) |
| 2 | Barnard 2016, Australia | Understand the experience of Directors of Nursing from residential aged care who either had support of the Hospital in the Nursing Home service, or did not | Admission Avoidance Hospital at Home for various acute conditions (Aged care facility) |
Service level (staff) | Directors of Nursing with Hospital in the Nursing Home support reported greater ability to assist families with decision making as a result of multidisciplinary input; sometimes averting transfer of residents to hospital: Participants referred to the high level of anxiety amongst families and commented that families are having a bad experience along the way. There is often disagreement in families as to how their loved one should be cared for during acute illness, and there can also be a hierarchy of information flow that needs to be navigated between family members. It all demands a lot of work from everyone to get best care. “I’ve found if they [a resident] get admitted, the liaison person rings us all the time. She informs us as to what’s happening. keeps us in the loop that way. Whereas in the past the person would just arrive back without any information.” (Director of Nursing) Directors of Nursing with Hospital in the Nursing Home support commented that there needs to be recognition that the extra work now sent our way needs extra resources and that we need extra funding to do the extra work. Directors of Nursing argued they were taking on more and more with less resource and that they were not costed to do basic stuff or resourced to provide high level care, and there is paperwork coming out of our ears. “We are doing more and getting less funding... more and more is coming back to us but give us the funding to do it.” (Director of Nursing) |
| 3 | Brody 2019, USA | Examine facilitators and barriers to implementation of Hospital at Home programme over its first year of operation to provide others with the opportunity to plan effectively for operationalisation | Admission Avoidance Hospital at Home for various acute conditions (This study focused on the first year of operation) |
Service level (staff) Systems level (Executive leader) |
When external partners are used teamwork was difficult. When multiple partners perform service delivery, with an often rotating group of staff within those partners, the nature of teamwork and ability to team‐build changes can be more challenging compared with a single organisation. Morning huddles with the HAH‐Plus team and external partners were developed to ensure service coordination and timeliness, team building, updates in the plan of care, and care needs were being met. Multiple informants noted that more time needed to be spent up front developing clear and specific protocols and workflows for initiation and provision of services. For instance, ensuring changes or initiation of new medications were confirmed and implemented by the appropriate pharmacy in a timely fashion and that the nurse, patient, and/or caregiver were aware of and performed those changes. Integrating pharmacy to ensure updated pharmacy orders were sent and filled properly. Because outside pharmacy partners were being used, a key work‐around had to be created to ensure each medication was faxed or electronically prescribed, received, and delivered expediently for quality and safety purposes. |
| 4 | Cegarra‐Navarro 2010, Spain | Examine the knowledge management practices of the Hospital at Home unit; to present a conceptual framework for hospital‐in‐the‐home units developed to guide learning | Admission Avoidance Hospital at Home for stable medical conditions | Service level (staff) | The doctor concluded that some of the lessons learnt from working with one patient are readily transferable to other similar patients. In doing so, practices include mentoring, teamwork, chat rooms, personal intranets, and opportunities for face‐to‐face conversations such as group dialogue or personal reflections on experiences and lessons learned. “The hospital should encourage teamwork or cross‐department specialist teams through organisational design”. (Physician ‐ Hospital at home) In addition, boundaries between work groups should be crossed without hierarchical barriers, restrictions or formalised structures. |
| 5 | Chevalier 2015, France | Understand the impacts 1 year from the implementation of a Hospital at Home service in partnership with a public hospital urology unit on professional practices in Hospital at Home by identifying the positive and negative impacts | Early Discharge Hospital at Home for urology surgery for prostate cancer | Service level (staff) | HAD appears as a team where everyone has a role that they knows and masters and where we also know the role of his colleague. We can therefore easily communicate because we know what one must do and what the other must do. The protocol makes it possible to work as a team. Treatment protocol helped with consistency of care and strengthened safety, despite some staff not trusting predictive scores. Using the protocol of care made it possible to avoid individual practices not compliant and to respect the rules of good practice. HAD professionals reported that the use of the treatment protocol was also reassuring for the patients. In fact, the patient is better informed about the seems to be part of his care path. Each speaker, in hospital environment as in HAD, has the same information. “It makes it possible to harmonize practices. Like that, the hospital practice and HAD hospital practice are fine be the same.” (Healthcare professional) Implementation of the treatment protocol made it possible to respond better to the continuity of between hospitalization with accommodation and HAD, in particularly on the transmission of information. |
| 6 | Chouliara 2014, England | Explore the perceptions of healthcare professionals and commissioners regarding the challenges and facilitators to implementation and perceived impact of early supported discharge services | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Study was conducted in the first year of implementation) |
Service level (staff) Systems level (commissioners) |
According to eight respondents, assigning rehabilitation assistants to deliver the repetitive everyday exercises allowed the highly skilled staff to focus on the more specialist elements of rehabilitation: “It’s about being able to break down the role and make sure that the right skilled person is doing the right part of the intervention”. (Team lead) The provision of specialist stroke care as critical for the successful rehabilitation of stroke patients in the community, maximising their recovery potential and facilitating the continuity of care across services. It was seen as a key component of the service, defining its identity and role. “Having the knowledge to deal with stroke patients is what sets the service aside from other community services”. (Acute stroke unit staff). Participation in meetings and common training events was seen as an effective way of developing and sustaining communication channels. Staff rotations across services promoted a better understanding of each team’s role, permitted the exchange of skills and knowledge and gave service users a sense of continuity along the pathway. “We could have some rotational element between staff so you can really share that sort of approach and the learning”. (Team lead) Regarding the length of the intervention, in Site B, it could be extended further than six weeks to compensate for the lack of stoke specialist community rehabilitation service in the region. Alternatively, the intervention could last only a few weeks to benefit milder spectrum patients. This flexible approach was endorsed by three respondents in Site A who argued that "sticking to the magic six‐week timeframe" could unnecessarily prolong the service and delay new admissions. "There is some reluctance to discharge someone even if they have achieved their goals… people may need us for a few days". (Service Management) A commissioner stressed the need to adapt hospital at home to the local healthcare context and variation in patient characteristics. A commissioner felt there was a need to adapt components of the intervention to respond to the local healthcare context and the variation in the stroke population: “No two stroke cases are ever going to be the same; our systems need to be reflective of that”. (Commissioner) |
| 7 | Cunliffe 2004, England | Assess the acceptability of the service and illuminate the relationship between process and outcome | Early Discharge Hospital at Home for acute medical and surgical patients | Service level (patients and staff) | Described a service, that they recognised was better staffed than usual after‐care services in which they had worked, and unusual in being able to provide both social care and rehabilitation in a coordinated way. The absence of a waiting list was important, and the ability to provide an intense input when needed (for example four visits a day). This required a flexible and problem‐solving approach, in which boundaries between professions were blurred. Gaining the patient’s confidence was crucial. So was ongoing assessment of their needs as this description of a package of care indicates. “Originally we put in 4 co‐worker type visits a day. One in the morning to help with wash and dressing and getting up, opening the curtains, emptying the commode, help with breakfast if she needs it. Sort of setting her up for the day and then at lunchtime when she has her main meal and to start with we’re doing that for her and now she’s doing most of that for herself. We were going in at teatime cause I didn’t even trust her to go through to the kitchen and make a sandwich she was so frail, she was struggling to stand from a chair first time we went. Now she is independent, making a hot drink, making a sandwich, so we are not going in at teatime anymore.” (Staff) |
| 8 | Dean 2007, England | Evaluate the feasibility of a prospective hazard analysis when assessing quality and safety in a COPD early supported discharge care pathway | Early discharge Hospital at Home for acute exacerbations of COPD | Service level (patients and staff) | All teams described themselves as "a multidisciplinary team" or "a multidisciplinary team with aspects of an interdisciplinary approach". Agreement to deliver service in 48 hours helped reduce the hospital length of stay for one service. One COPD supported discharge services provided by one site were not provided by the other. For example, one site had a service agreement with local authority service departments to provide a home care review within 48 hours of a request. The other site did not. This variation resulted in delayed admission to the supported discharge programme for one site and, as a consequence, one site was less equipped to deliver the programme's primary aim of reducing hospital length of stay. |
| 9 | Dinesen 2007, Denmark | Explore how the implementation of the concept ‘Home hospitalisation of heart patients’ by means of telehomecare technology influences the integration of clinical tasks across healthcare sectors | Early Discharge Hospital at Home for heart conditions | Service level (staff) | "Clinical decision‐making becomes a multidisciplinary decision‐making process involving the district nurse, the hospital nurse at hospital and doctors. This gives all of us the possibility to share data... We can also discuss observations and exchange suggestions for improvement of the care and treatment for the individual patient". |
| 10 | Dow 2007b, Australia | Make recommendations to the Victorian Government on best practice in rehabilitation at home | Early Discharge Hospital at Home for orthopaedic and neurological conditions (Rehabilitation at home) |
Service level (patients, caregivers, and staff) | RITH was one program that could provide a high level of post‐discharge support at home. Therefore, RITH programs were referred not only those people with conditions considered to be responsive to rehabilitation, but older frail people with a range of comorbidities. This placed additional pressure on the staff, and they acknowledged it caring for clients who were often frail and medically vulnerable. |
| 11 | Fisher 2021 | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
Respondents agreed that cross‐boundary working promoted an understanding of the ESD role and assisted in achieving appropriate and timely referrals: What I say to them is ‘Oh, I’m from ESD, do you know what we do?’. And I give them a leaflet and I say, ‘Come and spend some time with us’, but it’s about good relationships, communicating. I usually try and grab any new nurse that I don’t know and sometimes if they’ve got a good mentor the mentor will send them down. Co‐location with the acute team meant face‐to‐face interactions, shared IT and training events, or even supporting each other when at overcapacity. By contrast, communication with other referring hospitals was more strenuous because, other than speaking over the telephone, they did not have many opportunities to build up rapport in the same way. Regular MDT meetings with good attendance were thought to remediate breakdowns in team communication caused by increased workload and travelling. All teams agreed on the importance of safeguarding these meetings as essential to achieving clear communication between staff. It’s the one time in the week when everybody should come together to discuss the patient’s needs and their plans. In addition to formal meetings, most teams emphasised the value of opportunistic face‐to‐face interactions. Meeting colleagues at the end of the day helped staff combat feelings of isolation and loneliness that were related to being on the road most of the day. Clinical guidelines and the ESD consensus have identified the delivery of ESD by a co‐ordinated MDT that meet regularly and offer training opportunities as key to the delivery of an effective evidence based service. The NICE clinical guideline suggests that an ESD team should provide rehabilitation and care at the same intensity as they would if the person were to remain on a stroke unit, that is 45 minutes of each appropriate therapy every day. Against a background of staff shortages and reduced resources, teams were struggling to strike a balance between responding to an expanding list of referrals and offering the intensity required to achieve improvements in patient outcomes. In addition to the weekly MDT and wider meetings, some teams had introduced separate patch meetings to plan the visits for the following week. During these meetings, staff would collectively do their timetabling for the week to ensure that every patient was seen daily and that there were no overlaps. Having a stroke‐specialist nurse in the team allowed them to respond in a timely fashion to patients’ medication queries and address information gaps around medical issues. As noted by respondents, nurses were in a better position to identify when liaison with a stroke consultant or the GP was required. In addition to providing advice and reassurance to the MDT around medical issues, nurses’ presence in the team was perceived as a factor contributing to the development of an interdisciplinary skillset across the team, facilitating in this way the provision of holistic care and improving the efficiency of activities. In one site, participants described how the lack of a nurse in their team meant that they had to spend a lot of their time trying to secure nursing input from external services, such as district nurses, and the support that they would receive would not always be stroke specific. Capacity issues often meant that services relied on staff ‘walking the extra mile’ and maintaining momentum despite the difficulties to meet intensity targets. To quote one of the respondents, teams strived to ‘offer a champagne service on beer money’. Although their hard work helped them to meet patients’ needs, it also meant that services could become victims of their own success because senior managers and commissioners could maintain an unrealistic picture of the service’s capacity. It was suggested that thrombolysis patients tended to be of working age and required additional support, such as vocational rehabilitation. The teams felt the pressure to respond to the needs of these patients without, however, always having the resources to do so. "From a vocational rehab point of view, we’re not funded to provide vocational rehab but again, we’ll do it." In response to acute trust pressures, three teams saw higher‐intensity patients in care homes to teach the staff positioning, mouth care and communication. This was considered important because care home staff had a high turnover and needed this support to effectively handle these patients. Although the service’s input would be short term, there was an impact on caseload and resources because double visits could be required. The aim was to prevent re‐admissions and later complications rather than achieve improvements on disability. However, if we’ve got somebody that’s going into a nursing home or a care home, particularly if they’re really quite impaired so if they’re bed bound or if they’ve got a new communication impairment, we will put two people into the care home for a short period of time just to make sure that the care home know how to move somebody, and also so the family are aware, because there’s such a high turnover in the care home staff. Most teams did not provide a 7‐day service, mainly because of capacity issues. Concerns were voiced that 7‐day working reduced therapists’ time during the week, which, in turn, impeded communication with the MDT or other services and could negatively affect responsiveness. Where the service was provided, this was done either with reduced therapist input or with nonregistered staff doing the home visits or providing telephone cover. All of the services sought strategies to enhance the intensity of rehabilitation practice without further stretching their capacity. To achieve this, they offered relevant training to family members and care providers, implemented telerehabilitation and promoted a self‐management ethos. They envisaged to promote rehabilitation practice between sessions and empower patients and carers to effectively manage their recovery after discharge from the service. Teams perceived travel times to be an issue that had to be considered and managed, the impact was more pronounced in services covering rural and/or large catchment areas. The time required to reach their patients was identified by respondents as an important contextual influence, which could affect the number of patients they could see per day and the intensity of service that they could offer, especially against a background of reduced resources and stretched capacity. Respondents from services covering rural/large geographical areas noted that the complexity of their timetabling allowed little flexibility when arranging home visits for patients living remotely. This could mean reduced opportunities for rehabilitation provision tailored to patients’ needs, for instance arranging shorter and more frequent visits to manage patients’ fatigue. Adopting a flexible approach in how and who makes the first contact with patients was used strategically to improve responsiveness. Telephone contact was used by some teams at weekends to complete initial holistic assessments, enabling them to extend the service to 7 days. Teams had different approaches to managing the tension between capacity issues and meeting responsiveness targets (see all patients within 24 hrs) In some sites, patients could be held in the acute trust until a slot became available, which unnecessarily prolonged their hospital length of stay. When caseloads were full, some teams refused admissions completely and patients were discharged to the care of a non‐specialised rehabilitation service, for which waits could be long. Where other services did not exist, patients did not receive any rehabilitation at all. The urgency to see all patients within 24 hours was questioned by some respondents who felt that stroke survivors and their families could use more time at home to settle and identify their rehabilitation goals. |
| 12 | Gorbenko 2023, USA | Examine processes of uptake and implementation of the Acute Hospital Care at Home waiver (expansion) programme in a national sample. This included examining the barriers and facilitators of the waiver programme implementation across implementation stages and describing strategies used to address these barriers and/or best practices. | Admission Avoidance Hospital at Home | Service level (clinical leaders) | CMS requirements forced programs to adjust staffing and, in some cases, delay enrollment until staffing capacity could be met. Participants from both enrolling and non‐enrolling programs noted that in‐home visits were often time‐consuming, in part due to travel time, limiting staff capacity to only a few patients per day. The waiver also required new types of staff, e.g., acute care nursing staff. Programs made efforts to increase staff capacity across service areas by “leasing” staff from other homebased programs; focusing programs on urban hubs where more staff were available; and providing “hybrid” inperson/video appointments. Other programs noted contracted paramedic services an important bridge, although this varied by state. However, in some cases programs struggled with lack of available staff due to COVID‐19 burnout and turnover, and scope of practice regulations for acute care nursing, hospitalists and paramedics. |
| 13 | Hitch 2020, Australia | Describe staff perceptions of the trial of an early supported discharge model of care for stroke survivors | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Implementation trial) |
Service level (staff) | Diverse beliefs around the time commitment required by ESD were also evident, with consistent (but not universal) claims of increased workload made throughout this study. “I think that it certainly does add to the workload, both ours and our inpatient colleagues”. (Staff) “They (referrers) are having to spend a lot more time dedicated on these potential ESD clients to get everything done. . . that increase in workload has been stressful”. (Focus group) “Because basically, you’re trying to manage an inpatient caseload in an outpatient setting”. (Focus Group) |
| 14 | Karacaoglu 2021 | To understand staff views of implementing a Hospital at Home model in a Scottish care setting | Early Discharge Hospital at Home for various acute conditions | Service level (staff) | Operational modifications were required to address unexpected contextual challenges, in particular being unable to recruit a Geriatrician, resulting in limited acute service admissions. Consequently, the model shifted its focus from clinical care provision to enablement focused: “it has been away from that kind of disease focused management or very medical kind of modelling, particularly because we have no medic leading” (AP). Referrals were accepted from an acute geriatric hospital ward once a Geriatrician had ensured the patient was medically fit: “…we ended up going to a more of a rapid supported discharge type thing…at least then we would have control over the patients being medically stable so that we knew they would not be requiring huge amounts of our input that we couldn’t necessarily provide” (Management). The acuity of patients was limited by challenges in recruiting a Geriatrician. Potential options thought to address this were to build upon GP expertise and to increase skilled AP input: “we just keep the GP as a responsible clinician but they have input from PA’s [Physician Associates] or training GP, so we are exploring all of those possibilities at the minute. |
| 15 | Lemelin 2007, Canada | Evaluate the acceptance of a hospital at home programme managed and provided by nurse practitioners | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | Nurse practitioners felt that the interdisciplinary team approach to care was beneficial to clients and important to establish. |
| 16 | Moule 2011, England | Explore how the early stroke discharge team members and external stakeholders experienced the service implementation process | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (New service) |
Service level (staff) Systems level | Allied health staff utilised their professional line manager for clinical supervision, support, leave entitlement etc. This made it challenging for the leader of hospital at home (a rotating position) to manage the service. The lack of external management was an issue with no recognized hierarchy above it, with management tasks being done within professional departments outside of hospital at home and no single person gave the team a sense of clear direction. In the early stages of the project, the budget was not integrated, meaning that any reviewand alteration to the skills mix would require negotiation with several managers. Although the team needed to work as a truly multidisciplinary team with interdisciplinary practices and a clear identity, it was recognized that the team was not large enough to operate in isolation and needed to be fully integrated with other parts of the Trust for mutual provision of cover when needed. It was also clear that the team members offered a range of skills and expertise, not necessarily directly from the speciality, one example being the noted IT skills of a member of the team. “It was set up with quite an expensive team of therapists and a nurse, but no actual social care input or anyone to carry out personal care, which meant that if the idea was that you take people out who’ve had a stroke earlier than they would otherwise, one would expect that in between the therapists visits they might need some degree of support, but that wasn’t available, that wasn’t thought about and put into the team.” (External stakeholder from health and social care sector) This situation reflects the difficulties of working across health and social care boundaries in delivering the service and it was felt that: “With more health and social care type resources, they [the team] could get even more people home.” (External stakeholder from health and social care sector) “It would have been good to have had two healthcare assistants attached to intermediate care that could have provided hands‐on support sometimes for those people going home. This would increase the capacity of the team and may have widened the scope of referrals”. Being located in one physical spaceenabled the team to work well, talk about patients, and gain support. “It’s the passion for ‘stroke’ that’s done it.” (Staff) “Weekly staff meetings where we would talk through any day‐to‐day issues and concerns. We also had time‐tabling every week, where we would table patients and ensure that if we needed joint sessions, we could cover them. We also had our own multidisciplinary team meeting where we would talk about unified goals and, when we had seen the patient, come up with a joint plan.” (Staff) |
| 17 | O'Neill 2017, Australia | Examine nursing staff perceptions regarding their management of the deteriorating resident after the introduction of a hospital avoidance programme | Combined Admission Avoidance and Early Discharge Hospital at Home for conditions requiring subacute care (Aged care facility) |
Service level (staff) | While the nursing staff in this study preferred to avoid hospitalisation, they also recognised that keeping the residents in the facility required balancing subacute care with the demands of their daily responsibilities. Fewer transfers and faster turnaround from the hospital meant that nursing staff were caring for residents who may have otherwise been hospitalised. For the nursing assistants, subacute care often required frequent vital sign readings, one‐on‐one feeding, bathing, toileting and repositioning the resident every two hours. For the nurses, it meant focused attention on the needs of the resident, as well as possibly administering IV medications or frequent pain medication. Communication with the family and other members of the healthcare team also intensified when a resident’s health deteriorated. Thus, nursing staff had a lot to manage along with their daily routine care of other residents, as one staff member explained While the nursing staff in this study preferred to avoid hospitalisation, they also recognised that keeping the residents in the facility required balancing subacute care with the demands of their daily responsibilities. Moreover, there was recognition of the potential for providing emergency and subacute care to multiple residents simultaneously. |
| 18 | Papaioannou 2018, Canada | Describe the implementation of an intravenous service and assess the perceptions of residents, family caregivers and other relevant key informants | Admission Avoidance Hospital at Home for respiratory or urinary tract conditions (A pilot delivered in 4 residential care facilities, 3 multiple‐payer, 1 single‐payer) | Service level (caregivers and Staff) | “Having pharmacy as a key person to go to just even to talk things through, like here’s the situation, what do you think? And they were really very, I found they just would bring another perspective.” (Staff) “We have a nurse practitioner so we can call her any time, she can come in and assess and advise us if we have any question or anything.” (Staff) |
| 19 | Rayner 2022 | Understand what factors, including the service model, were associated with more frequent use of Residential in Reach services by nursing homes | Admission Avoidance Hospital at Home (2 'Residential in Reach' services for residential care patients) |
Service level (staff) | In some nursing homes that used the RiR services more frequently there were few or no RNs on a shift. There was a lack of skilled RNs working in participating nursing homes to assess and manage deteriorating residents. In addition to low numbers of RNs, a few participating nursing home staff reported being heavily dependent on agency staff to cover shifts. Service participants reported instances of nursing home staff contacting them for advice but who were unable to adequately explain what was wrong with the resident and had not undertaken basic nursing assessments. |
| 20 | Sims 1997, England | (1) Evaluate within the borough the practicality and acceptability of the 'Going Home Service' to patients and to staff employed in the service and in other services on which the scheme impinges (2) Establish the impact on informal carers |
Early Discharge Hospital at Home for orthopaedic conditions (New service) |
Service level (staff) |
“We all help each other out and if we need to know something we try to pool together to sort it out”. (Support Workers) Two support workers commented on how approachable the health care professionals were. The value of daily team meetings in helping communication across the team was mentioned. |
| 21 | Testa 2021 | Explore health professionals’ perspectives on the factors impacting Aged Care Rapid Response Team utilisation in the care of acutely unwell residential aged care facility residents | Admission Avoidance Hospital at Home (Acute, residential care) |
Service level (staff) |
The small number of staff employed by ARRT was seen to create some restriction in terms of achievement. This was particularly amplified by the COVID‐19 pandemic. We’re a small team. It would be great to have a bigger team. Something that we ‐ and I guess that’s another barrier, is if we had more geriatricians, more staff, more expertise in the field, Allied Health that worked directly with us, we might be able to achieve a lot of different things (AART Clinical Nurse Consultant). Health professionals external to the ARRT team expressed a desire for ARRT to extend its coverage to after hours and weekends. A lot of residential aged care patients do come in [to the ED] after hours, because they haven't got services like aged care rapid response after hours... [They] do tend to come quite regularly after hours, and we don't have that support then (ED‐based Clinical Nurse Specialist) Funding was sought to expand the ARRT team. As of October 2020, when interviews were conducted, ARRT was in the process of hiring additional medical, nursing and allied health staff. You know we're talking about our service, how good we are, we're giving them our figures and they're enhancing our staff at the moment because ofCOVID. We aren't a team that sat back and just let it happen. It's like no, we need this, we need that, we need this person in the position, we need this person in that position. We're not gonna just accept what you give us. (ARRT Clinical Nurse Consultant) The use of telehealth was noted to greatly increase the ARRT team’s capacity and response time. We’re doing so many video conferences … it’s allowed our capacity to build up because you don't need to go and do the reviews on site. Two [resident] reviews this morning already (ARRT Clinical Nurse Consultant) |
| 22 | Udesen 2022 | Explore different healthcare professionals’ perspectives on and experiences with the ED‐based acute care service | Admission Avoidance Hospital at Home (Emergency Department‐based Acute Care Service for residential care) |
Service level (staff) | In the two focus groups with the nursing home staff, the importance of collaboration with the acute care service was discussed. The collaboration made it possible for the nursing home staff to contribute useful information to the ED consultants’ decision‐making, and they felt appreciated and acknowledged for their insight to the residents. ‘It is very nice because different professionals stand together, and I feel heard and seen even though I am just a nursing home nurse. I really feel that I can contribute something’ [focus group]. The ED consultant portrayed it as an ‘eye‐opener’ as it increased his understanding of the nursing homes which made him understand the nursing staff’s thoughts and possibilities. The nursing home staff did express that they learned new things about treatment because they were supported by dialogues with the ED consultants. According to the respondents, all participants described that they had previously lacked the means to reduce unnecessary hospital admissions. The GPs explained that they often do not have the time to perform acute home visits before they have seen all their otherwise scheduled patients. Thus, it is considered a challenge when the nursing home staff calls concerning deteriorated residents. The GPs said that they sometimes have to admit the residents to a hospital without having seen them. This may result in unnecessary transfers and admissions. They [ED consultants] have the resources and opportunities to understand and manage these patients, setting the nursing home staff’s minds at ease and talk to relatives and staff about what would be the most appropriate solution’ (focus group). |
| 23 | Vaartio‐Rajalin 2020, Finland | Describe Hospital at Home staff's perceptions about Hospital at Home care, including work structures, processes and outcomes | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | Interprofessional care in hospital at home was perceived as collaborating for the patient's best. A complementary mix of competencies in a team and collaboration and communication were emphasized. “I see my role of [being] a physician as more like that of a consultant… the nurses discuss with me whether there is need to move the patient from HAH to hospital, or only to take some radiological analyses, blood samples… They make the clinical observations and situation analysis, I never visit the patient at home”. (Physician) “..nurses and physicians and we often make decisions together… the physician has to rely on the nurses' situation analysis and trust our professional competence when making decision.” (Focus group) “I wish public policy makers would understand the comprehensiveness of our competencies and responsibilities in relation to resource allocation and our wages.” (Physician) |
| 24 | von Koch 2000, Sweden | To describe the content and experience of a programme involving early hospital discharge and continued rehabilitation at home after stroke | Early Discharge Hospital at Home for stroke (Rehabilitation at home (Implementation trial) |
Service level (staff) | “We can discuss the patients and ventilate things, otherwise it would be difficult. You get advice, support and a few reminders. Sometimes I have deep thoughts about various things, and then the team provides a lot of good support.” (Staff) Initially the therapist underwent a learning process in adopting and implementing the philosophy of the home rehabilitation programme. In order to enable the patient to take an active part in the rehabilitation process the therapists had to modify their behaviour. As the patients assumed more responsibility the therapists came to realize that their part in the process had been altered to the extent that it was initially perceived as if they were not doing their job properly. In the beginning it did feel as if you did not do a whole lot. You didn’t do a lot of training. Now I understand that it all works out in the end, and the patient is satisfied. The timing and the number of visits were decided in partnership. The early hospital discharge was carefully prepared by the case manager according to the patient’s needs. The therapists reported that, initially, prior to discharge from the hospital, most patients believed they needed frequent home visits by the therapists. Once they were at home, however, the patients realized that frequent visits were not required – a realization reflected in longer and longer time intervals between visits until the final discharge from the programme. When it’s time for the early discharge from the hospital they want you to make frequent home visits, but once they’re at home they’re not so anxious any longer. The patient is also aware of the fact that the important thing is not the times when I come but what they themselves do between the home visits. |
Finding 5. Staff training, expansion of roles beyond usual scope of practice and rapid delivery of equipment or medical testing was essential to implement Hospital at Home. Expanding nurse roles increased capacity for acute medical care in the home and residential care. Expanding rehabilitation assistant roles increased capacity for rehabilitation in the home. The expansion of roles required appropriate governance structures and policy changes (high confidence).
Early Discharge Hospital at Home
Junior staff required increased support to develop self‐efficacy for treating stroke at home (Hitch 2020). Staff did not expect to have all the answers to patient questions and learning on the run and perceived the service aligned with organisational values, including an organisational commitment to innovation (Hitch 2020). Rehabilitation staff realised patients assumed more responsibility and self‐management, requiring modification of the therapist’s behaviour (i.e. less therapist input) (von Koch 2000). Home care nurses did not perceive themselves to have the same knowledge as hospital nurses for treating heart conditions, but patients did not know this and asked questions (Dinesen 2007). Hospital staff were concerned that the home staff might not have sufficient experience with orthopaedic patients and support workers would require additional training (Sims 1997). GP’s requested training for complex care in Hospital at Home (Leung 2016). One team introduced the term ‘nerapists’ as a reference to their staff's shared skillset and other services trained up rehabiliation assistants to complete initial assessments to improve capacity and responsiveness targets. (Fisher 2021). The success of this required effective delegation and experienced staff (Fisher 2021). One service discussed upskilling advanced nurse practitioners due to limited ability to recruit a geriatrician (Karacaoglu 2021).
Patients felt that nurses should be able to perform certain medical interventions (e.g. for IV drip) in Hospital at Home to avoid sending patients back to the hospital (Dubois 2001). Staff perceived that prompt access to equipment and other health professionals helped achieve rehabilitation objectives (Cunliffe 2004). COPD patients valued receiving oxygen equipment at home as it allowed better mobility (Dismore 2019). Stroke patients valued the timely delivery of equipment (Cobley 2013). Rapid access to blood test results and equipment provision was facilitated by newly developed pathways and teamwork (Karacaoglu 2021).
Admission Avoidance Hospital at Home
Healthcare services leaders reported the need to expand the roles of some healthcare providers (e.g. paramedics, nurses) to facilitate timely administration of medicines and tests as part of these services (Brody 2019). Provision of IV therapy in homes or residential care facilities by nurses required substantial training and support (Brody 2019; Papaioannou 2018). A workshop, education and increased acute care skills for nurses in a residential care facility was perceived to result in hospital avoidance for some residential care residents (Crilly 2012). For GPs, essential training included IV antibiotic prescribing for infections in residential care facilities (Papaioannou 2018). Staff considered Hospital at Home as a unique and innovative modality of health care, achieved through the creativity of health professionals to overcome the limitations of care in the residence, professional training and an expanded “toolbox” (Andrade 2013).
Directors of nursing at a residential care facility argued that additional facilities for medical care, such as on‐site X‐ray, blood transfusions, basic wound care and access to antibiotics would avoid unnecessary visits to hospital and increase capacity for medical treatment (Barnard 2016). Staff perceived that expanding the nursing scope of practice (e.g. such as providing IV therapy) achieved a greater capacity for medical care in residential care facilities and was considered an essential residential care role (Papaioannou 2018). Training and empowering nursing home nurses in acute care was perceived as helpful in reducing avoidable hospital admissions by effectively managing acutely unwell residents (Testa 2021). However, acute care nurses and nursing home nurses worried about the competencies at the nursing homes (Udesen 2022).
Combined Admission Avoidance and Early Discharge Hospital at Home
In a focus group of physicians and nurses, it was perceived it would be more efficient if nurses had limited rights to prescribe some medication (e.g. antibiotics for urinary tract infection), especially on weekends, rather than waiting until Monday (Vaartio‐Rajalin 2020). Nurses felt they required a high level of individual competence for clinical decision‐making as they were often working alone with complex patients (Vaartio‐Rajalin 2020). A subacute programme with structure and support was perceived to increase nursing staff and nursing assistants' confidence, skills and awareness of the role (O'Neill 2017). Nurse practitioners expressed concern that patients did not have immediate access to diagnostic testing and specialists that would be available in hospital (Lemelin 2007). Patients were concerned with equipment when it was unsuitable, when alarms went off regularly, limited their autonomy, if it was not designed for the patient, or it caused clutter (Vaartio‐Rajalin 2021).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Andrade 2013, Brazil | Understand the organisation of the health system from the perspective of professionals that provide home care services | Admission Avoidance Hospital at Home for various acute conditions | Service level (staff) | Professional training is a factor essential for proper team attention of health, which is essential for the adequate home care. Participants also revealed that the preparation process to act in the service includes courses that address not only aspects of everyday life at home, but also those who expand the “toolbox” for the unpredictable that home care keeps. “I took the urgency and emergency course, courses on clinical and traumatic emergencies; I took the care course for the frail elderly, I took the dressing course, I took the care for the elderly.” Health system assists patients in all aspects of healthcare in biopsychosocial factors, but training is more biomedical focussed with a predominance of teaching focused on hospital care. Innovation at work, achieved through the creativity of health professionals in the search for solutions to overcome the limitations of care in the residence. there is an understanding of AD as a unique and innovative modality of health care: “Because there is a lot of creativity for overcome the limitations of the physical environment”. It is reaffirmed that the innovative potential of home care if concretizes in the capacity of the teams in perceive and consider the different aspects experienced by users and their families in care production. So, they develop “Technological innovations of care and greater possibilities of carrying out work in team, which articulates and shares different knowledge and professional practices in projects therapeutic” with a view to expanding the autonomy for both users and users caregivers. |
| 2 | Barnard 2016, Australia | Understand the experience of Directors of Nursing from residential aged care who either had support of the Hospital in the Nursing Home service, or did not | Admission Avoidance Hospital at Home for various acute conditions (Aged care facility) |
Service level (staff) | Participants argued for additional assessment facilities within aged care facilities to care for residents, including access to mobile or on‐site X‐ray, on site blood transfusions, basic wound care [and] access to antibiotics. Transfer to ED was often for X‐rays for suspected fractures and both groups claimed X‐ray facilities were once the best thing for aged care. In fact, participants in both groups expressed despair at the number of people who come in [to hospital] just for an X‐ray. |
| 3 | Brody 2019, USA | Examine facilitators and barriers to implementation of Hospital at Home programme over its first year of operation to provide others the opportunity to plan effectively for operationalisation | Admission Avoidance Hospital at Home for various acute conditions (This study focused on the first year of operation) |
Service level (staff) Systems level (executive leader) |
In New York, only emergency medicine physicians can direct paramedics. Because HAH‐Plus physicians were not emergency medicine physicians, they would be unable to direct the paramedics, for instance to perform an electrocardiogram or administer intravenous (IV) medications such as furosemide. This restriction would make community paramedicine unworkable for HAH‐Plus By working with the New York City Regional Emergency Medical Services Advisory Committee, a limited paramedicine control authority for HAH‐Plus physicians, called “telemedicine physician”, that required a short training and restricted control solely to patients a physician has a prior professional relationship with, was created. For nurses there was significant changes in operating practices with same‐day and multiple scheduled nursing visits per day, and training and policy change to allow home health nurses to place IVs and perform infusions. Substantial training of the home health nurses, some of whom had never placed IVs or performed infusions, and others who had not done so in years. Substantial training required for home health nurses to perform IV’s and infusions. |
| 5 | Cobley 2013, England | Explore patients' and carers' perceptions of early supported discharge services during the early post‐discharge phase | Early Discharge Hospital at Home for stroke patients (Study was conducted in the first year of implementation) (Rehabilitation at home) |
Service level (patients and caregivers | There was a general consensus (10 of 19) among participants that the equipment provided was useful and delivered in a timely manner: "I’ve got that table and I’ve had two stools ... Then I’ve got a seat in the toilet and in the shower. Then they tried them all out before they signed me off anyway. Well ... I couldn’t do it without them". (Patient) "'We’ll probably get you a sock aid to help you put your socks on,’ but I didn’t get one". (Patient) |
| 6 | Crilly 2012, Australia | Describe and evaluate the structures and processes involved in a ‘Hospital in the Nursing Home’ programme | Admission Avoidance Hospital at Home for conditions requiring acute care (Aged care facility) |
Service level (patients and staff) | As a result of the workshop and on‐site education, the acute care skills of the aged care facility nurses developed. This resulted in hospital avoidance for some aged care residents. “It’s actually stopped us sending people to the hospital more regularly than we would have to … We can … provide all the care, we can do all the dressings. We can even do the swabs … we avoid … ambulance transfers and distress to the residents … and waiting down there [in ED]”. (Aged care Nurse) |
| 7 | Cunliffe 2004, England | Assess the acceptability of the service and illuminate the relationship between process and outcome | Early Discharge Hospital at Home for acute medical and surgical patients | Service level (patients and staff) | Prompt access to equipment and other professionals helped [Patients] achieve rehabilitation objectives. |
| 8 | Dinesen 2007, Denmark | Explore how the implementation of the concept ‘Home hospitalisation of heart patients’ by means of telehomecare technology influences the integration of clinical tasks across healthcare sectors | Early Discharge Hospital at Home for heart conditions | Service level (staff) | Hospital at home (district) nurses found that patients expected them to have in‐depth knowledge about their disease – The district nurses find that the patients expect them to have in‐depth domain knowledge of heart diseases and their treatment similar to hospitals nurses. "I’m happy to answer the patient’s questions about heart conditions, but I don’t have the same knowledge as the nurses at the hospital. It’s quite confusing, but the question is how much do I need to know?" and "It’s a new segment of patients, who in fact in some contexts are stronger on resources than some of the patients we normally deal with". (District Nurse) |
| 9 | Dismore 2019, England | Identify positive drivers and potential barriers to implementation of Hospital at Home for patients with exacerbation of COPD and low risk of death using the Dyspnoea, Eosinopenia, Consolidation, Acidaemia and atrial Fibrillation (DECAF) prognostic score and assist wider implementation | Early Discharge Hospital at Home for COPD (Implementation trial) |
Service level (patient, caregivers and staff) | Patients mentioned that the quality of the service was dependent on the skill of the attending RSN. This highlights the importance of adequate training and support. “The only concern I would have is that hospital at home is only as good as the nurses you’ve got on”. (Patient) "I couldn’t even walk up the ward... I only had this like little lead... I can go upstairs (at home)... it’s nice and I can get up and make myself a meal". (Patient) |
| 10 | Dubois 2001, Switzerland | Evaluate patients' satisfaction with Hospital at Home care | Early Discharge Hospital at Home for various conditions including community‐acquired pneumonia, intravenous anti biotherapy, deep venous thrombosis (Pilot programme implemented 2 years prior) |
Service level (patients) | Some said that nurses should be able to perform certain technical medical acts in H‐Hcare to avoid sending patients back to the hospital (e.g., for an IV drip). |
| 11 | Fisher 2021 | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
Respondents agreed that effective multidisciplinary working was enhanced by the blurring of professional divides and an interdisciplinary approach to the rehabilitation provision. Training was used to nurture interdisciplinary working because it helped staff understand each other’s work and feel comfortable with providing aspects of different roles. One team introduced the term ‘nerapists’ as a reference to their nurses’ and therapists’ shared skillset and approach to rehabilitation. Despite this, they emphasised the need to strike a balance between specialism and interdisciplinarity to avoid duplication and ensure that people are comfortable and confident with what they do without feeling ‘threatened’ by other disciplines. One service trained experienced RAs to complete initial holistic assessments, which helped the service to work across a large rural geographical area and meet their responsiveness targets. Respondents agreed that under the supervision of specialist staff, RAs had a key role in freeing time for therapy staff and maximising the service capacity and cost‐effectiveness. As noted by two teams, the success of this process depended on effective delegation. This related to registered staff’s experience and ability to effectively manage increased workload. Less‐experienced staff could be risk averse or lacked the confidence to judge the right time to hand over therapy tasks to RAs; as a result, patients’ length of stay in ESD could increase. Therapy input was shared between registered staff and RAs based on patient need. One team lead stressed the need to empower experienced RAs to handle difficult situations, escalating when they judged necessary, and encourage them to bring in new ideas that would benefit their patients . |
| 12 | Hitch 2020, Australia | Describe staff perceptions of the trial of an early supported discharge model of care for stroke survivors | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Implementation trial) |
Service level (staff) | ESD implementation was both congruent with, and challenging to, their existing rehabilitation practice knowledge. Referrers noted that Grade 1 staff required increased support in Phase 1 to develop self‐efficacy Staff noted ESD knowledge was not consistently developed for staff members joining the organisation mid‐trial. “When you’re starting something new you certainly don’t have all the answers . . . just starting and ironing things out as they went. . . That’s what I learnt through ESD, you had to just start, and then work it out as you go.” (Staff) Staff generally perceived ESD as aligning closely with organisational norms and values, particularly around the provision of best care and an organisational commitment to innovation |
| 13 | Karacaoglu 2021, UK | To understand staff views of implementing a Hospital at Home model in a Scottish care setting | Early Discharge Hospital at Home for various acute conditions | Service level (staff) | With skilled ANPs or APs I think is as good a concept, as long as we make sure it is safe and there is clear governance structures within that…it doesn’t have to be a Geriatrician” (Management). There was potential described for the responsible clinician to support in upskilling APs, along with formal training, ultimately leading to APs increasing their caseload responsibility safely: “because there is a confidence between the medic, could that be the Consultant or the GP with the team members, that there is less engagement between them as there is a confidence that has been built there so there is a need for a bit of supervision in there in checking but you are getting to know what that individual is doing” (Management). The presence of an MDT, in conjunction with newly developed pathways, led to reported efficiencies including rapid access to blood test results and equipment provision. |
| 14 | Lemelin 2007, Canada | Evaluate the acceptance of a Hospital at Home programme managed and provided by nurse practitioners | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | Nurse practitioners also highlighted some of the program drawbacks. They felt that clients in the HITH program did not have immediate access to diagnostic testing and specialists that would be available in a hospital environment. |
| 15 | Leung 2016, France | Identify the incentives and barriers to the involvement of general practitioners in Hospital at Home | Early Discharge Hospital at Home for various acute conditions | Service level (staff) | General practitioners were asking for a training on care in hospital at home and in particular on complex care. “I believe that we do not have the training for the HAD, the things have changed, and we do not have an update for knowledge". (GP) "I think that according to the criteria of mission in HAD, we can in fact have themes and from of these themes, do a training course three times a year: enteral nutrition, wounds…” (GP) |
| 16 | O'Neill 2017, Australia | Examine nursing staff perceptions regarding their management of the deteriorating resident after the introduction of a hospital avoidance programme | Combined Admission Avoidance and Early Discharge Hospital at Home for conditions requiring subacute care (Residential care facility) |
Service level (staff) | “I like it because it’s up‐skilling people and you know it’s not just relying on the RNs for everything that goes wrong, it’s up‐skilling all the staff, everyone is improving their skill level.” (staff) When a resident’s health deteriorates, nursing staff are under pressure to act quickly and correctly. Nursing staff who lack confidence in their assessment of the situation may hesitate and second‐guess their decisions, thus delaying treatment. The subacute programme, and the structure and support it provided, appeared to increase nursing staff confidence. “Well I think the sub‐acute program, workshop, that we’ve been having helps build your confidence,you know you’re doing the right thing, you know you’re thinking the right way. And you know you’re doing what everyone else, the management expects you to do, meeting expectations.” (Staff) |
| 17 | Papaioannou 2018, Canada | Describe the implementation of an intravenous service and assess the perceptions of residents, family caregivers and other relevant key informants | Admission Avoidance Hospital at Home for respiratory or urinary tract conditions (A pilot delivered in 4 residential care facilities, 3 multiple‐payer, 1 single‐payer) | Service level (caregivers and staff) | Successful implementation and administration of in‐home IV therapy was facilitated by access to training, and timely access to external nursing support. Both through the contracted nursing service, as well as outreach nurse practitioners, pharmacy consultation, and supply acquisition through the contracted medical supply company. "Raising the level of quality of training in care that is provided there, rather than being somewhat more sedate and kind of accepting that they’re not as skilled as other nurses, I think that would be very important to keep, to get their skills right up and put them up there with the rest." (staff) As many physiciansworking in aged care facilities are family physicians who maintain a primary care practice, they have minimal opportunities for prescribing IV antibiotics and thus require access to education on types of IV antibiotics, doses, and indications. Provision of IV therapy [by nurses] contributes to building capacity for medical treatment in aged care facilities. This service was credited with providing aged care facilities with more resources for medical care, and has expanded the nursing scope of practice, all of which has resulted in being better equipped for medical care. |
| 18 | Rayner 2022 | Understand what factors, including the service model, were associated with more frequent use of Residential in Reach services by nursing homes | Admission Avoidance Hospital at Home (2 'Residential in Reach' services for residential care patients) |
Service level (staff) | RNs had lost the clinical skills required to manage residents with complex care needs and deterioration, adding that they needed more education to increase their competence and improve their confidence. We have got quite a range of RNs with different backgrounds and different … and some of them have not done clinical skills like [catheter insertion and management of IV medications] for a long time (Nursing Home RN). Facility management are trying to change the policy to let RNs give IV antibiotics and deal with blocked catheters in the future (Nursing Home RN). We don't do IVs here, that is a policy, and no catheterization. We just ring "in‐ reach". (Nursing Home RN). We use RiR service if residents need IV antibiotics for cellulitis or a change of catheter. |
| 19 | Sims 1997, England | (1) Evaluate within the borough the practicality and acceptability of the 'Going Home Service' to patients and to staff employed in the service and in other services on which the scheme impinges (2) Establish the impact on informal carers |
Early Discharge Hospital at Home for orthopaedic conditions (New service) |
Service level (staff) |
Several of the hospital staff felt that Going Home Service staff might not have sufficient experience with orthopaedic patients to provide the necessary support. Staff training would be needed, especially for the support workers, to ensure that early discharge was successful. |
| 20 | Testa 2021 | Explore health professionals’ perspectives on the factors impacting Aged Care Rapid Response Team utilisation in the care of acutely unwell residential aged care facility residents | Admission Avoidance Hospital at Home (Acute, residential care) |
Service level (staff) |
Capability building of RAC staff is considered an important function of ARRT. Along with providing outreach services, capability building was perceived as helpful in reducing avoidable hospital admissions through empowering RAC staff to more effectively manage acutely unwell residents. Building up the capacity within the nursing staff. So that they can recognise deterioration early, that they feel more competent and confident they can manage more acutely unwell people. (ARRT Clinical Nurse Consultant) |
| 21 | Udesen 2022 | Explore different healthcare professionals’ perspectives on and experiences with the ED‐based acute care service | Admission Avoidance Hospital at Home (Emergency Department‐based Acute Care Service for residential care) |
Service level (staff) | ED consultants explained that they did not perform all the interventions at the nursing home because of limited possibilities. Sometimes the limited diagnostic possibilities made it challenging to assign diagnoses to the residents. The acute care nurses and some of the nursing home nurses discussed that they were worried about the competencies at the nursing homes. They questioned whether the nursing home assistants had the competencies to take care of residents who receive treatment initiated by the ED consultants: 'The patients become very complex, and their condition can quickly deteriorate. At the hospital, there is access to physicians and more nurses ... So, who is responsible for giving them some tools to support them in how to care for sick patients?’ (focus group) |
| 22 | Vaartio‐Rajalin 2020, Finland | Describe Hospital at Home staff's perceptions about Hospital at Home care, including work structures, processes and outcomes | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | "It would be useful to have this restricted right for nurses to prescribe some medication, often during weekends, it would be so easy to start a [course of] antibiotics against a urinary tract infection – which is so easy to diagnose – and not to have to wait until Monday." (Focus group) The participants emphasized the need for clinical skills, specialized nursing experience, seeing and analysing the whole patient situation and independent decision‐making, all connected to independent clinical decision‐making on the advanced level. They also stressed a proactive situation analysis, flexibility, creativity, advocacy skills and continuous learning, seen as a proactive and reactive professional attitude. Nurses also emphasised individual competence. “You are alone there during the home visit and make decisions alone… of course you can call your colleague, but it is really a huge responsibility we carry… It is not seen in our wage, in any way…There have been situations where we have saved the patient's life, it [does] not only [occur] in the ER or ICU….” "Sometimes it is really difficult to identify the actual address, where the patient is said to live… Or it is a tall building without an elevator, and you must carry up all your supplies… And during the wintertime when we can have up to 80 cm snow, you can't get near the building with your car… and all the fluids you have with you are too cold to be given immediately… (Focus group) |
| 23 | Vaartio‐Rajalin 2021, Finland | Describe how adult, non‐palliative patients and their spouses perceive person‐centredness in Hospital at Home care | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (patients and caregivers | “Our home is full of packages and boxes with syringes, catheters and so on, must they all be here? This doesn’t feel like home anymore”. (Patient) “The IV‐pole I have to walk with 6h every day, it really restricts my life ... And we had at first an IV‐infusion pump, but the alarm went off all the time, so I said I wouldn’t tolerate it anymore. These things should be made with us ... patients ... and for us.” (Patient) |
Finding 6. Effective communication between staff, patients and caregivers, including documentation and sharing tailored information with patients, was essential to provide efficient and effective care and reassure patients that quality of care is maintained in Hospital at Home. Problems with communication were commonly encountered for patients (e.g. patient information was not tailored), caregivers (e.g. limited opportunities to discuss management with clinicians) and staff (e.g. absence of a shared electronic medical record hampering the sharing of information about patients, efficiency of the service and continuity of care) (high confidence).
Early Discharge Hospital at Home
Nursing staff had difficulty communicating with primary care GPs via telephone as could only leave a message and faxing discharge summaries often failed to reach primary care (Dean 2007). Hospital staff reported similar issues due to the telephone hours of a GP and were frustrated trying to get in touch with district nurses (Dinesen 2007). Patients were frustrated when re‐explaining their care due to different staff and having to adapt to a new nurse and re‐establish a relationship (Dubois 2001). Ward staff were frustrated explaining the new service to patients and caregivers without adequate communication from the Hospital at Home service, creating stress and increased workload, and patient uncertainty (Sims 1997). For urology surgery, the staff felt communication and assurance by the physician (e.g. nurse will come if there is a problem) made patients feel safe (Chevalier 2015). Staff delivering the service were frustrated around duplication of assessments for stroke patients across services between hospital and home, with a need to improve sharing of information (Chouliara 2014). Acute hospitals and Hospital at Home services were rarely able to share electronic health records, hampering the sharing of patient information (Fisher 2021).
Heart patients valued being able to contact the hospital and community nurses at all hours (Dinesen 2008). Caregivers for hip and knee replacement patients valued being able to contact healthcare staff easily (Jester 2003). Acute medical and surgical patients had little knowledge about what care would be arranged for them (Cunliffe 2004). Caregivers appreciated good communication and being kept up‐to‐date with the patient’s progress (Reid 2008). COPD patients felt the written information failed to address their needs, however explanations from the nurse about disease management changed their everyday lives (Wang 2012). Before being admitted, COPD patients were sceptical about the service due to not knowing what it entailed, however, after receiving the right information, patients agreed to participate and were satisfied because they knew what to anticipate (Ranjbar 2015). Information and self‐management strategies were sometimes overwhelming due to COPD patients' poor health condition; however, advice and explanations of their disease made them feel less frightened and they valued the ease of contacting nurses and the doctor (Ranjbar 2015). Acute care patients and caregivers were reassured knowing nurses collaborated closely with the hospital physicians and the GPs (Udesen 2021). For subacute rehabilitation, patients appreciated being informed regarding the timing and purpose of clinician visits (Kimmel 2021). For elective joint replacement patients, receiving a recommendation from a specialist or general practitioner influenced their preferred choice of setting (Wallis 2022).
Stroke patients had limited knowledge, certainty or understanding of the service (Fisher 2021) and preferred more information regarding the aims, objectives and processes of the service (Collins 2016). Patients and caregivers were concerned about their limited understanding of stroke and its causes, secondary preventative measures, and lifestyle changes and inadequate provision and delivery of information (Cobley 2013). Patients and caregivers described how the written information failed to address their needs and preferred staff to talk them through what happened (stroke), why and what to expect, rather than just receiving information on pamphlets (Cobley 2013). Receiving stroke information was helpful, but a patient questioned why it was received well after their stroke (Cobley 2013). The competence of professionals who did not visit patients as planned was questioned, including a lack of explanation on care (Cobley 2013).
Service staff perceived that the process of securing social care input delayed stroke patients’ discharge, offsetting the effect of the service (Chouliara 2014; Fisher 2021). Hospital staff were confused about the re‐admission process and sometimes delayed re‐admissions (Dean 2007). Nursing staff had difficulty communicating with the hospital when attempting to arrange readmission from the service, resulting in patients not being re‐admitted (Dean 2007). Consultant doctors had concerns about emergency cover and a feasible readmission process from Hospital at Home nurse to ward nurse (Sims 1997). Delays in social care arrangements could prolong hospital length of stay or lead to unsafe discharges (Fisher 2021). A social worker liaising with both the acute and the Hospital at Home service permitted the allocation of targeted admission slots, ensuring that the patient was seen soon after their return home (Fisher 2021).
Admission Avoidance Hospital at Home
In a multiple‐payer service, external services (e.g. physiotherapy, pharmacy) did not have access to documentation such as the patient’s chart, limiting written communication and order fulfilment (Brody 2019). In one multiple‐payer service, physician and nursing notes were documented in separate electronic medical records, requiring twice‐daily staff huddles to share patient information (Gorbenko 2023). Hospital at Home physicians expressed concern that a breakdown of knowledge can easily occur during handovers when patients transition from hospital to home (Cegarra‐Navarro 2010). For this service, physicians and nurses felt laptop computers were an important tool for access to updated medical records and so that physicians could base clinical decisions on up‐to‐date information (Cegarra‐Navarro 2010). The team leader of this service recommended that the hospital should offer rewards to staff who reinforce both the culture and the behaviours needed for effective knowledge transfer (Cegarra‐Navarro 2010). Joint web‐based patient records allowed for synchronous communication between district nurses and hospital staff (Dinesen 2007). Nursing home staff that could talk directly with the ED consultants felt reassured (Udesen 2022). In a residential care facility, miscommunication between the GP and the service usually occurred after‐hours when the service did not operate (Crilly 2012).
Caregiver and patient observations and perceptions sometimes differed from healthcare staff observations and perceptions when they were shown to them (Mäkelä 2020). Patients and caregivers commented on the lack of documentation to support their own appraisal of change (Mäkelä 2020). Also, when copies of documentation summaries had been received by them, they were typically viewed as communication between staff that did not address their needs and the content (e.g. patient goals) was not comprehensible to them (Mäkelä 2020). Caregivers described limited opportunities to discuss with staff about management beyond the acute episode (Mäkelä 2020). There was a continuing pattern of fluctuating symptoms and functional capabilities, and caregivers described using their new knowledge and local doctors to avoid further emergency healthcare (Mäkelä 2020).
Prior to admission, caregivers used a triage and advice hotline to access immediate guidance (Mäkelä 2020). Patients valued prompt, clear and reliable information from nurses about what to expect at home and valued being able to call [the care team] anytime (Levine 2021). Patients and caregivers felt safe knowing the home nurses collaborated closely with the hospital and the GPs (Udesen 2021). Some COPD patients and caregivers had a very clear understanding of how they could use the service by making direct contact and believed the service was a speedy route to effective treatment (Schofield 2006). A doctor discussing the benefits and challenges of sending family members to hospital when it was not necessary helped keep residents in the nursing home and avoid hospital care (Barnard 2016). Similarly, an extended care paramedic's ability to communicate with the patient and family (to ally fears about avoiding hospital) and the GP facilitated admissions to the service (Testa 2021).
Staff perceived that the service was important for continuity of care while the patient is still unstable, however the absence of primary care after discharge may lead to worsening of the patient's health condition or readmission to hospital (Andrade 2013). Caregivers knowing how to contact district nursing and GPs following withdrawal of the acute service helped confidence and facilitated immediate post‐discharge care (Mäkelä 2020). GPs experienced delays receving shared patient data across electronic patient medical records and described this as a barrier to continuity in patient care (Udesen 2022).
Combined Admission Avoidance and Early Discharge Hospital at Home
Physicians expressed frustration around documentation systems not being improved and patients appreciated not having to re‐explain their situation to nurses (Vaartio‐Rajalin 2021). Patients felt secure with being able to contact the service (Vaartio‐Rajalin 2021) and receving assurance and prompt follow‐up from the care teams was important (Ko 2023). Patients felt communication between the hospital‐based care team and 3rd‐party providers could be improved to increase a sense of care continuity (Ko 2023). Nurses described how it can be difficult finding and accessing patients' homes as an example of poor communication (Vaartio‐Rajalin 2020). Caregivers were concerned about a lack of a precise and realistic information on the practical functioning of hospital at home leading to some feeling disappointed that the service provided was not the same as a ‘real hospital’ (Rossinot 2019). Most of the patients or caregivers did not know the service existed before it was presented (Rossinot 2019). Nurse practitioners voiced concerns over the continuity of care, when their involvement in patient care was limited to the few days of hospital at home (Lemelin 2007). Nurse practitioners addressed this transition by collaborating on the development of a common care plan with a community home care agency (Lemelin 2007).
In residential care facility, nurses and nursing assistants felt decision‐support tools improved their confidence with appropriate steps to take for managing deteriorating residents and a communication tool helped ensure that important information about a resident’s condition was relayed in an organised manner and resulted in closer collaboration and teamwork (O'Neill 2017).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Andrade 2013, Brazil | Understand the organisation of the health system from the perspective of professionals that provide home care services | Admission Avoidance Hospital at Home for various acute conditions | Service level (staff) | “Home care programs is important for this continuity while the patient is still unstable”. (Staff) The absence of primary care after discharge may lead to worsening of the patient's health condition or additional hospital stay, which causes suffering and emotional burden to the user and family members, and also overloads the Health System. |
| 2 | Barnard 2016, Australia | Understand the experience of Directors of Nursing from residential aged care who either had support of the Hospital in the Nursing Home service, or did not | Admission Avoidance Hospital at Home for various acute conditions (Aged care facility) |
Service level (staff) | HINH staff facilitated discussion of the benefits and challenges of sending family members to hospital when it was not necessary or was detrimental. “A doctor can come in and talk to the resident and the family member, very nicely worded, to tell them you’re being an idiot, you’re being ridiculous. We can say it but it doesn’t carry the weight”. (Director of Nursing) |
| 3 | Brody 2019, USA | Examine facilitators and barriers to implementation of the Hospital at Home programme over its first year of operation to provide others with the opportunity to plan effectively for operationalisation | Admission Avoidance Hospital at Home for various acute conditions (This study focused on the first year of operation) |
Service level (staff) Systems level (Executive leader) |
Other than some of the visiting nurses, no other members of the team (e.g., physical therapists, lab, pharmacy, durable medical equipment, oxygen, mobile phlebotomy, and radiology) had direct access to the patient’s chart, limiting written communication and real‐time order fulfillment. |
| 4 | Cegarra‐Navarro 2010 Spain | Examine the knowledge management practices of the Hospital at Home unit; to present a conceptual framework for hospital in the home units developed to guide learning | Admission Avoidance Hospital at Home for stable medical conditions | Service level (staff) | Information exchange important for safety and quality of care, sharing information with the right people. HAH physicians noted that breakdown of knowledge can easily occur during handovers when patients transition from hospital to home. Laptop computers are also bringing patient information to doctors at the patient’s home. “Having that information at hand contributes to patient safety both directly and indirectly” … “because doctors can base decisions on the most up‐to‐date information, such as updated medical records”. (Physician ‐ Internal medicine) In addition, the nurse asserted that access to laptop computers was reducing the time spent on manually retrieving patient records and saved hours each week frees up time for doctors to focus on their primary functions of diagnosis and treatment. The team leader suggested that the hospital should offer tangible rewards to those members who reinforce both the culture and the behaviours needed for effective knowledge transfer. |
| 5 | Chevalier 2015, France | Understand the impacts 1 year from the implementation of a Hospital at Home service in partnership with a public hospital urology unit on professional practices in Hospital at Home by identifying the positive and negative impacts | Early Discharge Hospital at Home for urology surgery for prostate cancer | Service level (staff) | Information and assurance make patients feel safe: The patient also feels safe suddenly because the secretary or the doctor, before he leaves the service hospitable, tells him he's going home but there is a nurse who will come if there is a problem. They explain that he can have some bleeding or something. And we, they us ask again to explain it. The patient integrates that well. And we have the same discourse between the service and us. |
| 6 | Chouliara 2014, England | Explore the perceptions of healthcare professionals and commissioners regarding the challenges and facilitators to implementation and perceived impact of early supported discharge services | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Study was conducted in the first year of implementation) |
Service level (staff) Systems level (commissioners) |
Eight interviewees also talked about the unnecessary duplication of assessments across services and stressed the need to improve data‐sharing practices between hospital and Early Supported Discharge teams. The process of securing social care input was presented by 11 respondents as "one of the biggest stumbling blocks" to patients’ timely discharge, offsetting the effect of ESD. |
| 7 | Cobley 2013, England | Explore patients' and carers' perceptions of early supported discharge services during the early post‐discharge phase | Early Discharge Hospital at Home for stroke patients (Study was conducted in the first year of implementation) (Rehabilitation at home) |
Service level (patients and caregivers | “I wouldn’t have a clue what was normal, what wasn’t normal ... who to ask for help and advice. I mean the internet’s okay, but it only takes it so far. Sometimes you need a person to put it into terms that you understand. Because it’s stressful when you don’t know what’s going on". (Patient) "You read the pamphlets, the leaflets and things, what to look for with strokes, but I mean the thing is, a lot of the things in there weren’t applicable". (Patient) "It would have been nice to have somebody sit down with me and say this is what’s happened, this is why it’s happened, this is what you can expect. Okay, so it is there in the leaflets but you just kind of flick through the leaflets". (Caregiver) "The information was good, but has come an awfully long time since my stroke". (Patient) |
| 8 | Collins 2016, Ireland | Explore the experiences of early supported discharge from the perspective of stroke survivors and how participants made sense of these experiences | Early Discharge Hospital at Home for stroke patients (Rehabilitation at home) |
Service level (patients) | “I don’t know how to describe it ... they [staff in the hospital] told me I’d get home; they told me about this ... then just in a couple of days I got home here.” (Patient) |
| 9 | Crilly 2012, Australia | Describe and evaluate the structures and processes involved in a ‘Hospital in the Nursing Home’ programme | Admission Avoidance Hospital at Home for conditions requiring acute care (Aged care facility) |
Service level (patients and staff) | Care home nurses served as a patient advocate, recognizing when Hospital in the Nursing Home would be best for the residents and communicating this with their GP. “The process of referral from ACF RNs involved some degree of tact in communicating with the GP and showing initiative in identifying that there was a problem and acting upon it. They served as a patient advocate, recognizing that hospital avoidance (with HINH intervention) appeared to be the most appropriate pathway for most ACF residents. These referral considerations are evident in the following quote: We have to ring the doctor [GP], that’s the first thing. We would say we have a wound that we would like … [HINH] to come and do it, is that OK? Because you don’t want to be stepping on the doctor’s toes. We’ve never had anybody [GP] say no”. (Nurse,residential care facility) Miscommunication between the GP and the HINH programme may have led to some ACF residents being transferred to the ED and others transferred back to the ACF with limited feedback or support. It should be noted that these downfalls usually occurred after‐hours when the HINH programme did not operate. |
| 10 | Cunliffe 2004, England | Assess the acceptability of the service and tilluminate the relationship between process and outcome | Early Discharge Hospital at Home for acute medical and surgical patients | Service level (patients and staff) | "No, nobody has said anything to me at all....Er they just come along and treat you like parcels of tea, sugar. (Patient) |
| 11 | Dean 2007, England | Evaluate the feasibility of a prospective hazard analysis when assessing quality and safety in a COPD early supported discharge care pathway | Early Discharge Hospital at Home for acute exacerbations of COPD | Service level (patients and staff) | Difficulty for COPD nursing staff to communicate with primary care GP’s, as line often busy, or doctor busy and could only leave a message. Faxed copies of discharge summaries failed to reach primary care because, in some city general practices, fax machines were switched off on afternoons when the practices are closed. There was confusion about this re‐admission process on various levels, particularly on the part of hospital staff who were not part of the supported discharge programme, for example in the acute admissions department, which sometimes resulted in delays in admission. Patients had experience of failing to be re‐admitted, having exercised their right to ask for re‐admission via the hospital bed bureau. Because bed bureau telephone lines were often engaged, nursing staff sometimes had difficulty in communicating with the bureau when attempting to arrange emergency admission from the community. |
| 12 | Dinesen 2007, Denmark | Explore how the implementation of the concept ‘Home hospitalisation of heart patients’ by means of telehomecare technology influences the integration of clinical tasks across healthcare sectors | Early Discharge Hospital at Home for heart conditions | Service level (staff) | Joint web‐based patient records allows for synchronous communication between district nurses and hospital staff. “The joint web journal is a necessary tool as part of the concept, if we are required to adjust the anticoagulant therapy on a daily basis. It helps to enhance security and enables us to coordinate tasks at the same time’’. (District nurse) District nurses find it stressful to meet the agreed deadlines with the hospital for data transmissions from the patient’s own home by 9:30 am. “In regard to time it’s difficult to send data and so on by 9 am. I also have to squeeze in administering insulin and eye drops. It’s difficult to coordinate things according to the hospital’s workflows”. (District nurse) Difficulty communicating between hospital and district nurse. The initial difficulty is the coordination of workflow between two organisations within a given timetable and framework (for example telephone hours of the GPs, and scheduled hours for blood‐sample taking at the hospital). “We at the hospital are frustrated because it’s extremely hard to be in touch with a district nurse – we have to call umpteen phone numbers before we happen to reach one. And when we call, we should have called before 1p.m., and then we have to call back again the next day”. (Hospital nurse) |
| 13 | Dinesen 2008, Wales | Understand the experiences and attitudes of patients and their spouses/partners with regard to the application of telehomecare technology as an option within home hospitalisation | Early Discharge Hospital at Home for heart conditions | Service level (patients and caregivers | Able to contact the hospital and community nurses at all hours. (Subtheme) |
| 14 | Dismore 2019, England | Identify positive drivers and potential barriers to implementation of Hospital at Home for patients with exacerbation of COPD and low risk of death using the Dyspnoea, Eosinopenia, Consolidation, Acidaemia and atrial Fibrillation (DECAF) prognostic score and assist wider implementation | Early Discharge Hospital at Home for COPD (Implementation trial) |
Service level (patient, caregivers and staff) | Patients felt safe and reassured during hospital at home due to …. the 24‐hour telephone support line… |
| 15 | Dubois 2001, Switzerland | Evaluate patients' satisfaction with Hospital at Home care | Early Discharge Hospital at Home for various conditions including community‐acquired pneumonia, intravenous anti‐biotherapy, deep venous thrombosis) (Pilot programme implemented 2 years prior) |
Service level (patients) | The competence of professionals who did not visit patients as planned was questioned. Critical comments were also expressed concerning lack of explanation on care…. Patients were frustrated when re‐explaining their care due to different staff. Explaining procedures, details of care, and so on to each new professional was regarded as a waste of time; moreover, it was felt that no one nurse could have a long‐range view of patients. Patients had to adapt to each new nurse and re‐establish a relationship. |
| 16 | Fisher 2021, UK | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
Unrealistic expectations of ESD were common, and often reflected gaps in information provision prior to discharge or even referrers’ lack of clarity around the intensity and length of the service. Respondents emphasised the need to be proactive, especially in the early days of the services’ development, as referrers may not fully understand the screening and referral process nor appreciate the quality of the service that patients would receive at home. Uncertainty related to the start of the service, what to expect and what it entailed, as well as what would happen when the ESD service was withdrawn. For the majority of participants the first time they were informed about ESD was at the hospital, either before or during their discharge, usually by the resident physiotherapist. Participants articulated that they were uncertain of what the services were and had only a brief idea of what it might involve (Patients). All teams recognised the need for timely, clear and constant information provision to both patients and families. This was important for addressing concerns about returning home and misconceptions about their recovery. Striking a balance in relation to information provision was also considered necessary to ensure that patients were not overwhelmed. Some teams discussed how they developed their information material to consider stroke‐related cognitive and language difficulties. In response to patient feedback, one service adapted their discharge letters to make them more accessible. As noted by a team lead, discharge from ESD services should be actively managed to avoid leaving patients and their families with a sense of ‘abandonment’ and to avoid an abrupt ending of the service. Timely communication was key to effectively preparing patients practically and emotionally for their discharge from ESD services. Establishing and maintaining communication with the carers was required to manage the delicate family dynamics that come as part of home‐based rehabilitation and to help carers to feel engaged in the rehabilitation. Early goal‐setting that involved the carers allowed patients and their families to have a clear understanding of what they were working towards and start the process of adjustment. Acute trusts and ESD services were rarely able to share electronic records, scan results or test results, which hampered the sharing of information about patients. Where good information technology facilities were in place, flexible working arrangements that allowed staff to return to the office only when necessary could further help to manage travel time and optimise resources. Staff were encouraged to start and finish their day with patients. Remote working helped to reduce travel time, but it could also mean that there were less opportunities for interaction and for the exchange of information, expertise and emotional support, all of which were deemed by respondents as particularly important in community working. Having access to the same electronic note systems was emphasised...being able to draw the right information would allow the social worker to identify areas of concern, develop a personalised and detailed care plan and observe patients’ progress. Delays in social care arrangements could prolong hospital length of stay or lead to unsafe discharges. ESD services admitting complex and more dependent stroke cases were the ones mainly affected. The problem was accentuated when effective communication channels between the ESD services and the referring teams were not in place and, as a result, ESD teams were not informed about the delays in a timely way. Having a social worker embedded in the pathway and liaising with both the acute and the ESD services streamlined discharge, as it permitted the allocation of targeted admission slots, ensuring that the patient was seen soon after their return home. Following discharge home, ESD services could be called to address issues arising from delays in social care input to prevent hospital re‐admissions. However, as noted by a social worker, it would be difficult for them to provide a quick and effective response to premature and unsafe discharges if they were not already familiar with the cases. They highlighted the importance of the timely involvement of a dedicated social worker who would follow patients and their families in their journey from the stroke unit into the community. |
| 17 | Gorbenko 2023, USA | Examine processes of uptake and implementation of the Acute Hospital Care at Home waiver (expansion) programme in a national sample. This included examining the barriers and facilitators of the waiver programme implementation across implementation stages and describing strategies used to address these barriers and/or best practices | Admission Avoidance Hospital at Home | Service level (clinical leaders) | “So, we'll hear complaints from patients, yes, or nurses…one of the things we do on our end that I know about is we have an incident reporting system. So, any time there's a system's issue like a delivery delay, an equipment problem, malfunction, a vendor problem, we can log that in our incident system. In one program, physician and nursing notes were documented in separate hospital and home health EHRs, requiring twice daily staff huddles to share information. As a solution to the interoperability issue, several programs reported adapting EHRs built for the COVID‐19 surge, for example, EHRs for virtual COVID units designed for non‐traditional settings such as field hospitals. |
| 18 | Jester 2003, England | Examine the experiences of informal carers looking after patients following early discharge to Hospital at Home | Early Discharge Hospital at Home for hip and knee replacements | Service level (caregivers) | Caregivers felt able to contact the hospital at home team easily. |
| 19 | Kimmel 2021, Australia | To evaluate the 3‐month pilot programme from the perspective of participants and identify themes or participant factors relating to the care received and involvement in decision‐making. This was to inform the development of bed substitution rehabilitation services in the future. | Early Discharge Hospital at Home (Subacute rehabilitation) |
Service level (patients) | Most participants reported feeling well informed regarding the time and purpose of clinician visits. They notified me every morning … rang up and said he was coming, you know, and an approximate time … they were fairly good if we had appointments or doing anything … |
| 20 | Ko 2023, Singapore | Explore the experiences and perceptions of patients and their caregivers admitted to a Hospital at Home programme | Combined Admission Avoidance and Early Discharge Hospital at Home, for acute conditions | Service level (patients and caregivers) | Assurance from the care teams was important... Participants were appreciative of receiving frequent calls and visits and having providers that were approachable, patient, and prompt in follow‐ups. While participants had positive experiences with the HaH care team, several others felt that the partnership and communication between the hospital‐based care team and 3rd‐party medical house‐call providers could be improved to increase a sense of care continuity. |
| 21 | Lemelin 2007, Canada | Evaluate the acceptance of a Hospital at Home programme managed and provided by nurse practitioners | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | Nurse practitioners voiced concerns over the continuity of care, when their involvement in patient care was limited to the few days of home hospitalization. "An ongoing problem in encounters with the health care system has been one of continuity of care. Patients are frequently expressing a sense of having been abandoned by a care provider that they have come to know." Over the course of the program, NPs worked to address these concerns and improve this transition by collaborating on the development of a common care plan with the community home care agency. |
| 22 | Leung 2016, Paris | Identify the incentives and barriers to the involvement of general practitioners in Hospital at Home | Early Discharge Hospital at Home for various acute conditions | Service level (staff) | "An ongoing problem in encounters with the health care system has been one of continuity of care. Patients are frequently expressing a sense of having been abandoned by a care provider that they have come to know.". (Nurse practitioner) |
| 23 | Levine 2021, USA | Elucidate and explain patient perceptions of home hospital versus traditional hospital care to better describe the different perceptions of care in both settings | Admission Avoidance Hospital at Home for a variety of acute conditions | Service level (patients) | “They [Nurses] were very informative about every step of the process of what I could expect, who was coming to get me, what was happening, what I could expect when we got to the house”. |
| 24 | Mäkelä 2020 | Explore the work of patients and caregivers at the time of an acute health event, the interface with health professionals in hospital and hospital at home and how their experiences related to the principles that underpin comprehensive geriatrician assessments | Admission Avoidance Hospital at Home for acute medical conditions | Service level (patients and caregivers |
“Nobody has asked me to actually walk. One of the pages, it says ‘Walk, out of 5’ and they’ve put ‘5 out of 5’, as though I could walk. Well, I can’t.” (Patient) “Mobilise independently to toilet in 2/52 with a stick...’ [Patient] was thrown by the numbers”. (Field notes) “It got so bad that I thought, ‘I’ll have to call a general practitioner’ but I couldn’t, because of the time in the morning. So I thought, ‘I’ve got a pendant [personal alarm], but I know what they’ll do, first is you go into hospital’. I had a big think and I asked one of the boys. Between us, we decided to ring 111. They rang me back, eventually. . . ‘We’ll have to send you a doctor’. The doctor came and says, ‘You have to go into hospital.” Others described a period of uncertainty over whether HAH input had finished or not. Patients and families often detected the end of an episode when the HAH folder had been removed from their home: "They didn’t tell me but I knew they’d come and got the folder". (Patient) Patients were willing to defer urgent decision‐making to family members, who described the challenges if a patient experienced fluctuating confusion. Although generally expressing a preference to remain at home, many patients later reflected on decisions by taking into account opinions of family members. “If it was a doctor saying ‘Do you want to go into hospital or do you want to stay at home?’ I would say, ‘Yes, I want to stay at home’. But if I was delirious then I wouldn’t mind my daughter or my son saying, ‘Take her into the hospital’. (Patient) Caregivers described limited opportunities for discussion with hospital or HAH staff on how to manage beyond the acute episode. “What I can do to change, if anything, the conditions of what mum’s living with”. (Caregiver ‐ son). Withdrawal of the acute service often meant continuing with a pattern of fluctuating symptoms and functional capabilities. Caregivers described adapting through their own knowledge and relational network to avoid further emergency healthcare. “After she’d been discharged out of [HAH] care a couple of weeks, she took another UTI [urinary tract infection]. But I’d taken a sample up to the doctors. . .I think it’s just me being a bit wary now, because you get to know little signs [of delirium starting]." (Caregiver ‐ daughter). “I’ve got the number for district nurses there...I know what to do if there’s anything happens, you know. Yeah, got all the numbers there, keep it handy". (Patient) "I’m very, very fortunate with my family doctor. She takes quite an interest in people and she could sort of fill in the gaps for me [after HAH discharge]". (Patient) “This [HAH] has been the best hospital experience from other times because there seems to be aftercare. . .normally you’d have to phone your doctor and go through whole loop again." (Caregiver ‐ daughter) |
| 25 | O'Neill 2017, Australia | Examine nursing staff perceptions regarding their management of the deteriorating resident after the introduction of a hospital avoidance programme | Combined Admission Avoidance and Early Discharge Hospital at Home for conditions requiring subacute care (Residential care facility) |
Service level (staff) | The subacute programme, especially the equipment and decision‐support tools, filled a gap by providing structure and support around the management of a deteriorating resident, or residents, as more than one resident may experience health problems at the same time. Participants said the decision‐support tools helped to improve their confidence around managing a deteriorating resident by providing guidance on the ‘appropriate steps to take. The decision‐support tools also included SBAR (Situation, Background, Assessment, Recommendation), a communication tool used to ensure that important information about a resident’s condition is relayed in an organised manner. The ‘process,’ which she says has resulted in closer collaboration and teamwork, which was further supported by another participant: “It [the program] helps everyone to work collaboratively.” (Nurse) “I think when we did order it [antibiotics] we definitely had to go to them [nursing staff] and kind of look at the care pathway and look at the process because it’s definitely something new that I think was easily accessible for the nursing staff when we did look at it and had a look at it together.” (Nursing assistant) |
| 26 | Ranjbar 2015, Sweden | Explore patients’ experiences of Sweden’s first COPD mobile care programme; and evaluate if a human rights‐based analysis could provide additional information on the patients’ experiences of the COPD mobile care programme | Early Discharge Hospital at Home for COPD | Service level (patients) | Several participants stated that they were initially sceptical about the programme due to being unaware of what it entailed. Lacking information about the programme at the time of discharge from hospital and feelings of too much occurring in connection with the discharge process were mentioned as reasons for scepticism. "The doctor asked me if I wanted to have it and I didn’t know what it was but I said yes immediately. Yes I did, because I thought that then someone will come home to me and then I will feel safe." (Patient) “The more you know, the safer you feel. You are not so frightened when you know what is what and get a proper explanation of this [disease].” (Patient) "If I had questions to the doctor, I could call them [the COPD mobile care nurses] and ask them to contact the doctor." (Patient) |
| 27 | Reid 2008, England | Explore informal carers’ experiences of an intermediate care service and how it met their needs | Early Discharge Hospital at Home for conditions at risk of leading to hospital admission or residential care (Rehabilitation at home) |
Service level (caregivers) | "...they kept us informed all the time … they explained to all of us and my mum what care she would be getting, how many times a day they would be coming in." (Caregiver) "when they felt she was ready to try at home that is when they started getting the ball rolling as they called it...they kept us informed all the time..." (Caregiver) |
| 28 | Rossinot 2019, France | Make an inventory of experiences of patients and family caregivers in Hospital at Home | Early Discharge Hospital at Home for a variety of conditions such as cancer, chronic disease and fracture | Service level (patients and caregivers) | “I didn’t know HAH existed”. (Patient) “A huge discovery! We didn’t know it!” (Caregiver) “HAH was sold to us as “hospital at home”. The same as a real hospital. I did really think it would be the same. But no. It is not the same.” (Caregiver) |
| 29 | Schofield 2006, Scotland | Explore care experiences and preferences with respondents and their families | Admission Avoidance Hospital at Home for COPD | Service level (patients and caregivers) | Some participants had a very clear understanding of how they could use the ARAS to optimum effect by making direct contact themselves. The husband carer below and his wife made consistent use of the ARAS and would only consider hospital as a last resort. He saw the ARAS as a speedy route to effective treatment. “..my wife would have been dead, that’s how badly she was, now to me that is a godsend that clinic, I can phone up any time and I can take my wife in ". (Caregiver) |
| 30 | Sims 1997, England | (1) Evaluate within the borough the practicality and acceptability of the 'Going Home Service' to patients and to staff employed in the service and in other services on which the scheme impinges (2) Establish the impact on informal carers |
Early Discharge Hospital at Home for orthopaedic conditions (New service) |
Service level (staff) |
Poor communication was mentioned by seven members of the Going Home Service team. This focused on communication between team members. As one interviewee stated: “I would like to feel more organised. If communication was better I think it would be better. If we all understood each other’s roles patients would be better informed”. Although they still approved of the concept, they viewed it more negatively since the Going Home Service had become operational. One ward member said: “In theory it’s a good idea, in practice we’re having difficulties. It’s a new culture and difficult to get across to patients and carers. It creates a lot of stress for the staff.” Three members of the ward staff were particularly concerned about what they saw as the failure to provide adequate information and the resultant increase in workload for ward staff. “I’ve found I’ve been quite stressed by patients and carers asking questions which should have been answered by the Going Home Service staff’. Staff thought that the three main disadvantages from the patients’ perspective were: poor communication leading to patient uncertainty about the service. Several people (4) saw early discharge as a benefit for patients, so long as patients’ preferences were accommodated, and they were adequately informed about the service. One ward staff member considered that such a policy had not been uniformly adopted. Prior to ESD implementation, hospital staff were concerned about the potential for increased re‐admissions and the process for this and wondered whether referrals from a Going Home Service nurse to a ward nurse would prove feasible. |
| 31 | Testa 2021 | Explore health professionals’ perspectives on the factors impacting Aged Care Rapid Response Team utilisation in the care of acutely unwell residential aged care facility residents | Admission Avoidance Hospital at Home (Acute, residential care) |
Service level (staff) |
A lot of the times we’ll go to [RACFs], they've got an advance care plan, but the family will try and override that … At the end of the day, the patient’s rights are there. But if they're not able to communicate those anymore. It's the ability of the paramedic to communicate well with the family, I think. Get them on board, discuss with them what really they want happening, adverse to what they think should happen. And you can get the GP onboard as well and have a little chat, and I think, allay the fears. Cause I think a lot of the time people just think, oh just take them to hospital, they'll be OK. But at the end of the day, the condition probably isn't going to change. (Extended Care Paramedic) Participants described the potential for tension between providing RACF‐based treatment for the resident and respecting the family’s wishes for hospital treatment. Families, I think, still see hospital is this gold standard of,care, and it is. But I think it's very hard sometimes to explain to families that [for] their loved ones … the outcome of the treatment of going into hospital may not necessarily change the position or change the condition for their family ‐ for their loved ones. So, it's managing those expectations. (ARRT Clinical Nurse Consultant) Participants reflected that communication and partnerships between the hospital and local RACFs was enhanced post‐COVID‐19. There's much more communication, and we're out there training them on PPE, and infection control measures, right now. |
| 32 | Udesen 2021, Denmark | Describe and explore patients’ and caregivers’ experiences with home treatment | Admission Avoidance Hospital at Home for acute conditions | Service level (patients and caregivers | Several of the patients and caregivers stated that ATO collaborated closely with the hospital and the GPs. Both groups said this created a sense of safety, as they knew that the acute nurses were in direct contact with hospital physicians or GPs. One patient said: ‘They had time to listen and made sure that we got answers to questions from the hospital physicians’. They cited sufficient information as being important for treatment at home. Several of the patients and caregivers stated that ATO’s base at the ED heightened their sense of safety because they had met the acute nurses at the ED before being discharged. One patient expressed this: ‘The nurse who told me about the treatment at home and who discharged me from the hospital was also one of those who came to my home. I was very happy to see a familiar face’. Many of the caregivers highlighted that the nurses spoke to them and the patients with dignity. One relative stated: ‘The way that she spoke to my father was really good. Some people do not have patience to talk with him’. The surroundings also made it possible to ask the nurses questions without feeling rushed. If the doctors think it’s safe, I’d rather be home…’ ‘It depends on how ill you are. If I’m not ill, I prefer to be at home’ |
| 33 | Udesen 2022 | Explore different healthcare professionals’ perspectives on and experiences with the ED‐based acute care service | Admission Avoidance Hospital at Home (Emergency Department‐based Acute Care Service for residential care) |
Service level (staff) | All nursing home staff found that it instilled security to talk directly with the ED consultants and that the acute care service arrived fast when called upon. All groups of participants discussed that this new initiative made it possible to base the decision‐making on complete patient pictures because the ED consultants had the time to get to understand the resident in his or her setting and to talk with the nursing home staff and the relatives. A few of the acute care nurses and nursing home nurses expressed that the communication could be improved. Some of them suggested that the open and extensive communication could be improved by aligning expectations on behalf of the patients for all caregivers. This could be obtained by increasing the communication between the nursing home staff, the ED consultants and the acute care nurses. The alignment should take place before the acute care nurse and the ED consultant left the nursing homes. Concerning the communication, the GPs discussed that it could be beneficial to have systematic and faster handovers from the ED to the GPs. They experienced delays when sharing data across electronic patient medical records. All participants described this as a barrier to continuity in patient care. |
| 34 | Vaartio‐Rajalin 2020, Finland | Describe Hospital at Home staff's perceptions about hospital at home care, including work structures, processes and outcomes | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | "Documentation is very important … for patient safety and care continuity and collaboration… it takes a lot of time, the structured documentation system and in addition we call each other quite often." (Physician ‐ Focus group) "Every time some development in HAH is discussed, the foremost principle is person‐centeredness, but when it comes to the realization of that development idea, there is no energy nor money to do anything about these problems hindering person centeredness… For example no‐one does anything to coordinate the documentation systems between units!" (Physician ‐ Focus group) "Sometimes it is really difficult to identify the actual address, where the patient is said to live… Or it is a tall building without an elevator, and you must carry up all your supplies… And during the wintertime when we can have up to 80 cm snow, you can't get near the building with your car… and all the fluids you have with you are too cold to be given immediate..." (Focus group) |
| 35 | Vaartio‐Rajalin 2021, Finland | Describe how adult, non‐palliative patients and their spouses perceive person‐centredness in Hospital at Home care | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (patients and caregivers | “I noticed that nurses had read about me before they came, they know my situation and me, I don’t have to explain it all every time.” (Patient) “With hospital‐at‐home I don’t need to feel anxious and think about who will visit me today and whether he/she can everything or not ... Never an abandoned feeling, the help is as near as the nearest telephone.” (Patient) |
| 36 | von Koch 2000, Sweden | To describe the content and experience of a programme involving early hospital discharge and continued rehabilitation at home after stroke | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Implementation trial) |
Service level (staff) | Staff perceived that the discontinuation of HAH was ultimately decided by the patient, within the time allowed. The discontinuation of the programme was well prepared by the partnership, and it was the patient who, within the time limits allowed, made the decision. A few patients considered themselves ready and ended the programme even though their therapists felt that there were more things that could have been accomplished. |
| 37 | Wallis 2022, Australia | Explore patient and caregiver barriers and enablers and components of care that may increase acceptability of Hospital at Home | Early Discharge Hospital at Home for total hip or knee replacements (Subacute rehabilitation, multiple‐payer setting) |
Service level (patients and caregivers | Receiving a recommendation from a specialist or general practitioner about their discharge destination was perceived as being helpful as doctors were experts and knew about their health circumstances. For some patients this allowed them to be open‐minded and their doctor’s advice influenced their preferred rehabilitation setting. |
| 38 | Wang 2012, Norway | Explore COPD patients’ experiences of a limited early discharge hospital at home treatment programme | Early Discharge Hospital at Home for COPD | Service level (patients and caregivers | “There is something about smoking on every page [of the brochure], but I have never smoked”. (Patient) One patient shared how he applied the advices: he had learned to relieve the breathlessness during an acute attack by hanging over the armchair in his living room. |
Finding 7. Health professionals required skills in delivering person‐centred care, shared decision‐making and tailoring care to achieve patient goals and patient satisfaction. Some caregivers were frustrated about their lack of involvement in decision‐making and care planning. Patients valued equal interactions and partnerships with the staff, and their ability to cater for their needs and valued staff focussing on helping family members (high confidence).
Early Discharge Hospital at Home
Stroke patients frequently commented on the benefits of receiving rehabilitation sessions and felt listened to and supported to recover as quickly as possible (Cobley 2013; Gorbenko 2023). However, waiting several days for the initial visit at home was disappointing (Cobley 2013). Caregivers of hip and knee replacement patients valued a high frequency of visits and staff were perceived as caring, helpful and friendly (Jester 2003). Acute medical and surgical patients valued frequent visits for care or rehabilitation soon after discharge when anxiety was at its greatest and recognised the care and rehabilitation interventions as being helpful, and the staff as being skilled (Cunliffe 2004). For acute patients, assessment of patients in their own home, as opposed to in hospital, was seen as more effective in identifying actual patient need and facilitated independent living (Karacaoglu 2021). For subacute rehabilitation, some patients felt that the service was protocol‐driven, lacked flexibility and preferred more allied health than nursing care, while some were overwhelmed by multiple clinician visits (Kimmel 2021). In a multiple‐payer setting, elective surgical patients also preferred more allied health support and less medical support (Wallis 2022), and wanted specific information about recovery and self‐management, including an emergency number if medical support required (Wallis 2022).
COPD patients valued the nurses' skills and knowledge, and the time they took to listen to patients’ concerns and take them seriously (Ranjbar 2015). However, some were critical of the high workloads of the nurses, and some wanted more frequent contact with nurses (Ranjbar 2015).
"Hurried" doctors and nurses were deplored, as was the time spent by professionals filling in papers (Dubois 2001). Timely visits were important if there was a problem; however, patients and caregivers were frustrated with inconsistent visits that were perceived to be random (Rossinot 2019). Caregivers described that the respect that the staff provided, a high level of responsiveness to needs, reliability and the co‐ordination of other stakeholders was valued (Reid 2008). A previous negative experience led to reluctance to use the service again (Reid 2008).
Team leaders considered how important it was to address the emotional and cognitive difficulties of stroke patients that may not have been expressed in hospital and to tailor the intervention to patients’ needs and priorities (Chouliara 2014). When there were delays in services, staff had to wear "many hats" to cater for patient needs (Fisher 2021). Staff expressed how decisions about care and discharge from the service were based on the interests, preferences and goals expressed by the patient (von Koch 2000). Their assessment at home achieved an understanding of discrepancies between patient goals, environmental demands and caregiver behaviour, enabling more tailored interventions and encouraging stroke patients to practise activities between visits and reflect on the achievements of their goals, which helped them return to activities and life (von Koch 2000). Staff perceived providing rehabilitation at home enabled meaningful goal‐setting and patient‐centred care (Hitch 2020). Staff perceived that they provided more individual care and treatment for the heart patients (Dinesen 2007). Staff described a “whole person” approach, considering physical, psychological, social and environmental influences on activity and responding to patients’ wishes to ensure realistic goals are set and achieved, irrespective of their professional background (Cunliffe 2004). Staff would also support a caregiver, such as when they had an emotional breakdown, and ensure support from the Stroke Association (London, UK) (Fisher 2021). Staff also recognised when daily home visits by healthcare professionals became overwhelming for patients and would tailor the service (Fisher 2021). Staff visits were also tapered off and directed towards self‐care in preparation for discharge (Fisher 2021).
Staff felt it was a deficiency of their service that they did not include caregivers in the care planning process (Dow 2007b). Caregivers perceived there was inadequate time for consultation about the patient’s needs and to prepare themselves to take on the care required, and some caregivers were confused about the service and frustrated at the lack of consultation and information provided to them about care planning and decisions to admit to the Hospital at Home service (Dow 2007b). Other caregivers felt their input into goal‐setting and care planning was highly valued, while others preferred the staff to make decisions around their care planning (Dow 2007a). Stroke patients described how the initial decision‐making was taken during a time of immense change in patients’ lives (Collins 2016). A stroke patient’s determination to get out of hospital and self‐manage was an enabler for Hospital at Home (Collins 2016). Some stroke patients were concerned about having "strangers" in their home and finding out things about them, but these "strangers" became familiar, and their visits became anticipated and valued (Collins 2016). Stroke patents reported having specific barriers to outdoor mobility that were not addressed in rehabilitation and patients were not asked about accessibility in environments that were important for them to visit (Kylén 2021). They also reported experiences of being informed rather than involved in the planning of rehabilitation at home (Kylén 2021). A few patients recovering from an acute bout of COPD refused the service and felt that receiving visits from staff was unnecessary because they could care for themselves (Clarke 2010).
Staff discussed how at home there is more of a partnership in discussing the stroke patient’s problems and together finding solutions for rehabilitation (von Koch 2000). Stroke patients felt that being visited at home promoted a more equal relationship between the patients/caregivers and the healthcare professionals because the visits occur on the patient’s "home ground" (Lou 2017).
Staff acted on behalf of the stroke patients between visits to retrieve information or convey messages (von Koch 2000).
Admission Avoidance Hospital at Home
COPD patients highly regarded the specialist clinical skills and one‐to‐one care in the home provided by the friendly and approachable nurses (Schofield 2006). Patients and caregivers appreciated undisturbed dialogues based on their individual needs (Udesen 2021). Caregivers viewed the staff from residential care settings to be professionally trained to provide IV therapy that helped them to avoid hospital admission (Papaioannou 2018).
Nurses perceived that achieving patient care goals required a multidisciplinary team effort and patients in the decision‐making process (Manning 2016). Patients felt that doctors were able to make sure that the services were tailored to their needs (Levine 2021). Patients with acute confusion were willing to defer urgent decision‐making to family caregivers, which caregivers found challenging (Mäkelä 2020). Patients and caregivers were concerned about the uncertainty around discharge from the service with decisions occurring away from their home (Mäkelä 2020). Staff perceived that care was centred towards patient autonomy and independence and reinforced person‐centred care and partnership (as opposed to a gap) between professionals and patients (Andrade 2013).
Leaders felt Hospital at Home was a unique opportunity to support the patient at home and work with the tools that they have at their disposal to help improve their health (Gorbenko 2023).
Clinicians also focussed on family members in need (Andrade 2013), and caregivers appreciated being looked after (Wilson 2002).
Combined Admission Avoidance and Early Discharge Hospital at Home
Patients perceived that the nurses actively worked to understand them as a patient, their background and condition (Vaartio‐Rajalin 2021). Staff support of self‐rehabilitation was important. Staff also perceived that the work in Hospital at Home is challenging in the introduction of certain issues into discussion, as the patient's family are always present (Vaartio‐Rajalin 2020). Patients and caregivers appreciated responsive and personalised communication from the nurses and doctors as required (Ko 2023).
Staff perceived that the home was seen as a place of equality and less hierarchical, and facilitated a deeper patient‐nurse relationship because it is easier for staff to fully concentrate on the patient (Vaartio‐Rajalin 2020). Patients perceived that their home enabled more participation and a more equal status in decision‐making (Vaartio‐Rajalin 2021). Staff perceived that intangible but necessary work involved co‐ordinating care not just for the patient, but for the caregiver and also pets (Vaartio‐Rajalin 2020).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Andrade 2013, Brazil | Understand the organisation of the health system from the perspective of professionals that provide home care services | Admission Avoidance Hospital at Home for various acute conditions | Service level (staff) | Care centred on search for the user's autonomy and independence. The testimonies presented reinforce the understanding of AD as a form of care that presupposes user‐centred care and your needs, distinguishing yourself from other modelling where there is a gap between professionals and users. “I don't focus solely on the patient that is registered in the Home Care Program because there can be a family member in need, an elderly person, for example, and we refer them to other locations. I can get a staple food basket at the extended care NGO. I can get diapers for them. Whatever they need most at that moment. And I make that connection in the team, too, I talk about the case and we refer them to other institutions.” (Staff) |
| 2 | Chouliara 2014, England | Explore the perceptions of healthcare professionals and commissioners regarding the challenges and facilitators to implementation and perceived impact of early supported discharge services | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Study was conducted in the first year of implementation) |
Service level (staff) Systems level (commissioners) |
Emotional issues could be addressed in a timely manner during Early Supported Discharge according to seven respondents who observed that emotional and cognitive difficulties may not be fully expressed before hospital discharge: "Even people that have minimal physical impairments can be really anxious because their whole life has changed". (Team Lead) According to 11 respondents, the home‐based model of rehabilitation offered therapists an ecologically valid appraisal of patients’ difficulties and, therefore, allowed tailoring the intervention to patients’ needs and priorities. “It is less about a body in a bed that needs a bit of fixing; to me, it feels more of a holistic service; just being in peoples’ houses, seeing what problems they actually have and adapting the service around that”. (Team Member) |
| 3 | Clarke 2010, England | Explore patients’ views of an early supported discharge service for COPD | Early Discharge Hospital at Home for COPD | Service level (patients) | “I can’t see any point because, er, as far what I can say, if I get my medications and if I’m looking after myself properly an that’s I,.. maybe a fortnight or once a month if they [respiratory nurses] want to come and see me and give me their advice I don’t mind.” (Patient – declined service) |
| 4 | Cobley 2013, England | Explore patients' and carers' perceptions of early supported discharge services during the early post‐discharge phase | Early Discharge Hospital at Home for stroke (Study was conducted in the first year of implementation) (Rehabilitation at home) |
Service level (patients and caregivers | "The team were encouraging and motivating and would take me on a walk to make sure I could get on a bus and that I was able to cross the road, things like that ..." (Patient) "It was a few days of me coming from hospital. I was left without any help at all from the Thursday to the Monday I sort of had to fend for myself ... I wished it could have started earlier than it did". (Patient) |
| 5 | Collins 2016, Ireland | Explore the experiences of early supported discharge from the perspective of stroke survivors and how participants made sense of these experiences | Early Discharge Hospital at Home for stroke (Rehabilitation at home) |
Service level (patients) | The initial decision to participate in the early supported discharge programme was taken during a time of immense change in participants’ lives. So, while participants understood that they would ‘get out’, they may not have fully understood the processes involved in early supported discharge. "To be quite honest with you, I don’t know how to describe it ... they [staff in the hospital] told me I’d get home; they told me about this ... then just in a couple of days I got home here". (Patient) "It suited me, it might not suit some people, but it definitely suited me because I wanted to get out of hospital and look after myself, basically." “Don’t want strangers in and don’t want them finding out stuff about me ...privacy would have been a big thing.”(Patient) "I looked forward to the camaraderie we had I missed them after it finished". (Patient) "We became friends, they were my friends while they were here." (Patient) ‘I missed them when they were finished.’ (Patient) |
| 6 | Cunliffe 2004, England | Assess the acceptability of the service and illuminate the relationship between process and outcome | Early Discharge Hospital at Home for acute medical and surgical patients | Service level (patients and staff) | They worked within an explicit team ethos in which physical, psychological, social and environmental issues were all legitimate areas for intervention, for all members of staff irrespective of their professional background. They were also explicit in the importance of the patient’s views and participation in rehabilitation, and felt that the home setting facilitated this style of practice. They reported a “whole person” approach, considering physical, psychological, social and environmental influences on activity. Rather than aiming to deliver pre‐specified interventions, they aimed to respond to patients’ wishes: “I'll sit down and ask what it is they're wanting to achieve. And then sometimes their goals are realistic and sometimes they're not and so if I think something is way off and we're not going to achieve it in a month then I'll possibly modify it sooner and healthier and then put it back to them and say: "Do you think this will possibly be more achievable?" And get them to keep feeding things back to me, so hopefully the goals are patient led rather than me led.” Patients were particularly complimentary about the ability of the service to provide frequent visits for care or rehabilitation soon after discharge when anxiety was at its greatest. Patients recognized the care and rehabilitation interventions as being helpful, and the staff as being skilled. Staff described a service that they recognised was better staffed than usual after‐care services in which they had worked, and unusual in being able to provide both social care and rehabilitation in a coordinated way. |
| 7 | Dinesen 2007, Denmark | Explore how the implementation of the concept ‘Home hospitalisation of heart patients’ by means of telehomecare technology influences the integration of clinical tasks across healthcare sectors | Early Discharge Hospital at Home for heart conditions | Service level (staff) | The healthcare professionals find that they can plan and carry out a more individual care and treatment plan for the patient: ‘‘In that the patient is observed both in the hospital and at home during his or her own everyday routines we are better equipped to give advice and guidance to meet the exact needs of the individual patient’’ |
| 8 | Dow 2007a, Australia | Make recommendations to the Victorian Government on best practice in rehabilitation at home | Early Discharge Hospital at Home for orthopaedic and neurological conditions (Rehabilitation at home) |
Service level (patients, caregivers, and staff) | “It was like 50:50. We did it together and we never felt that they’d taken over. We felt we were in control. We would listen to what they’d say and we’d make a plan accordingly”. (Caregiver) While other patients and caregivers felt that they did not have the knowledge, right or desire to set the direction of their rehabilitation and were “happy to go along with what they had in mind”. (Patient) |
| 9 | Dow 2007b, Australia | Determine how the role of the carer in rehabilitation at home programmes is constructed | Early Discharge Hospital at Home for orthopaedic and neurological conditions (Rehabilitation at home) |
Service level (caregivers and staff) | Carers were somewhat cynical about the extent to which discharge was in the best interests of the client. They perceived that discharge sometimes had more to do with the needs of the hospital than the patient. They also reported that discharge from hospital to home was not always adequately planned. There was inadequate time for consultation about the care recipient’s needs and to prepare themselves to take on the care required. "I don’t think we involve the family and the carers in the actual formulation of the decision about whether the person will go home or not. We make our recommendation then we inform, sometimes. Many staff believed that this lack of consult a shortcoming to get to know the carer and to properly include them in the care planning process." (Staff) “No‐one told me beforehand or gave me any warning that he was going to be coming home.” (Caregiver) |
| 10 | Dubois 2001, Switzerland | Evaluate patients' satisfaction with Hospital at Home care | Early Discharge Hospital at Home for various conditions including community‐acquired pneumonia, intravenous anti‐biotherapy, deep venous thrombosis) (Pilot programme implemented 2 years prior) |
Service level (Patients) | The relationship with nurses was highly valued "they know how to handle us." Some communication problems and unsatisfactory relationships with nurses did occur. The lack of support from hurried doctors and nurses, who often changed, was deplored; several patients felt they could not discuss their fears. Critical comments were also expressed concerning… time spent by professionals to fill in papers...Technical difficulties were not well tolerated by patients in H‐Hcare. |
| 11 | Gorbenko 2023, USA | Examine processes of uptake and implementation of the Acute Hospital Care at Home waiver (expansion) programme in a national sample. This included examining the barriers and facilitators of the waiver programme implementation across implementation stages and describing strategies used to address these barriers and/or best practices. | Admission Avoidance Hospital at Home | Service level (clinical leaders) | “…this is an opportunity to impact a little bit, the social determinants of health, where we're in a patient's setting where we can see the choices that they make…We're in their life and we have this really unique opportunity to work with the tools that they have at their disposal to help improve their care, not just, ‘Here's everything you need to do. Now, go home and do it.’” |
| 12 | Hitch 2020, Australia | Describe staff perceptions of the trial of an early supported discharge model of care for stroke survivors | Early Discharge Hospital at Home (Rehabilitation at home) (Implementation trial) |
Service level (staff) | Providing rehabilitation at home was also identified as a key aspect of ESD, which enabled meaningful goal setting and client centred practice. |
| 13 | Jester 2003, England | Examine the experiences of informal carers looking after patients following early discharge to hospital at home | Early Discharge Hospital at Home for hip and knee replacements | Service level (caregivers) | High frequency of visits by HAH team. (positive comments) The HaH staff should have visited more frequently. Staff were caring, helpful and friendly. |
| 14 | Fisher 2021, UK | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
Participants reported that they felt immediately supported by the team, and that they were given the needed time and attention in order to recover quicker. (Patients) For all participants it was paramount to return to their usual roles and routines as soon as possible. Working towards a set of personalised goals was highly valued and increased expectations of further recovery. Most of the participants felt that the time spent with the ESD therapists contributed to their overall recovery outcomes, because the ESD team focussed on their goals and kept reviewing their rehabilitation plan accordingly. (Patients) The participants felt listened to and emotionally supported by the ESD team. They appreciated that the therapists went over and above their “designated duty”, and apart from accommodating their physical rehabilitation needs they provided the stroke survivors with psychological support, which was essential to boost positive outcomes. (Patients) Guideline recommendations on intensity were treated with scepticism. Most respondents thought that they were logistically unrealistic or even inappropriate for their patient group and highlighted the need to provide rehabilitation intensity tailored to people’s needs (Staff). Gaps in the local stroke care pathway and slow response from other services, such as GPs, resulted in staff having to work with many different hats on to try and cater for patients’ needs. Sometimes we stay there for 1 hour and 30 minutes because of other issues. Sometimes a patient’s partner or wife has had an emotional breakdown, and we talk to them and phone the Stroke Association [London, UK] to provide carer support. Those things that we’re dealing, it’s not just the therapy. It’s about the whole, because our approach is holistic. Respondents also noted that registered nurses had a more holistic approach with their initial assessment of patients, touching effectively on sensitive issues, such as mood and incontinence: I think that’s part of the in‐reaching role is to make sure that they are medically OK. So possibly one of the strengths is two nurses who do the in‐reaching; we might be a little bit more forensic in terms of the medical side than maybe our therapy colleagues. So we’ll be looking at blood pressure, continence, medication, those sorts of things maybe and whether they’ve had all the correct investigations and sort of maybe a little bit more detail than maybe the therapists might be looking – have a different angle on it. Respondents referred to patients’ feedback, which suggested that some of them found daily home visits by health‐care professionals overwhelming, preferring some downtime and quality, uninterrupted time with family and friends. The need to consider and respect these requests was stressed with the view to providing a patient‐centred service, tailored to individual circumstances. In one site, staff were discouraged from seeing patients daily for 6 weeks; it was thought that this intensity could create psychological dependency and result in people feeling abandoned when discharged. In most sites, visits were the most intense initially and then tailed off, with patients being directed towards self‐care in preparation for discharge. |
| 15 | Karacaoglu 2021, UK | To understand staff views of implementing a Hospital at Home model in a Scottish care setting | Early Discharge Hospital at Home for various acute conditions | Service level (staff) | Characteristics that functioned well included assessment of patients in their own home, as opposed to in hospital, which was seen as more effective in identifying actual patient need and in turn allowed more appropriate adaptations to be put in place to facilitate independent living: “You pick up on things, I think, when we go in to the home environment that would maybe not be picked up in the hospital…maybe move round their furniture, maybe different equipment that we could maybe be using in their own house that is maybe not in situ [in place] that would make their life easier” (HCSW). In addition, participants described the ability to build a rapport with patients due to the small team size: “They all like continuity, they like the same person going in…they look forward to you coming” (HCSW). |
| 16 | Kimmel 2021, Australia | To evaluate the 3‐month pilot programme from the perspective of participants and identify themes or participant factors relating to the care received and involvement in decision‐making. This was to inform the development of bed substitution rehabilitation services in the future. | Early Discharge Hospital at Home (Subacute rehabilitation) |
Service level (patients) | Model of service delivery was not always modifiable to patients' perceived needs. Some patients felt that service was protocol‐driven and lacked flexibility. Despite satisfaction with the program, many participants commented that the services provided were not specific to their individual needs. Some participants felt that a nurse attending daily was unnecessary and they would have preferred more allied health intervention. Others felt overwhelmed by visits from multiple clinicians within a few hours on a single day. Many participants felt that the program was an extension of their hospital‐based care and did not feel that they were part of the decision‐making process; however, the majority did not feel that this had a negative impact on their care. |
| 17 | Ko 2023, Singapore | Explore the experiences and perceptions of patients and their caregivers admitted to a Hospital at Home programme | Combined Admission Avoidance and Early Discharge Hospital at Home, for acute conditions | Service level (patients and caregivers) | This program provided patients with a dedicated care team, which improved the perception of continuity of care. “…in the hospital at home, one nurse taking care of my condition. I got more attention from her and she would probably have a more understanding of my condition.” [Patient] “If they [the doctors] need[ed] to update me, they would just speak to me over the video call. So, it is very responsive…very personalized…not intrusive. (Caregiver) |
| 18 | Kylén 2021, Sweden | Explore how the environment was integrated in rehabilitation at home from the perspective of people post‐stroke, living in Sweden | Early Discharge Hospital at Home for stroke (Rehabilitation at home) |
Service level (patients) | When asked if someone had inquired about their home environment at the hospital before discharge, many participants said that the healthcare professionals had asked about potential barriers, such as if the home had stairs and/or elevators or if it was possible to enter the home without problems. They were also asked if they needed any assistive devices to manage everyday life but not about the accessibility in environments that were important for them to visit. Some participants reported having heavy front doors that were difficult to open or garbage facilities in multi‐ family housing that were difficult to use and indicated that these types of barriers were not considered in the rehabilitation, which limited the participants’ abilities to return to life as it was prior to the stroke. In general, the participants had experiences of being informed rather than involved in the planning of their continuous rehabilitation at home and integration of the environment. "...we had no planning, I was advised ... and received information from the start”. |
| 19 | Levine 2021, USA | Elucidate and explain patient perceptions of home hospital versus traditional hospital care to better describe the different perceptions of care in both settings | Admission Avoidance Hospital at Home for a variety of acute conditions | Service level (patients) | “The doctors were able to kind of think on their feet for me and kind of make sure that the services were a little bit tailored to my needs”. (Patient) |
| 20 | Lou 2017, Denmark | Investigate how mild stroke patients and their partners experience and manage everyday life in the context of early discharge rehabilitation at home | Early Discharge Hospital at Home for stroke (mild) (Rehabilitation at home) |
Service level (patients and caregivers | "It’s just more relaxed... Like, at the hospital I sit in the chair, right? At the patient side of the table. But at home it’s different. It’s my home ground so the roles are a bit different. She’s the visitor. That puts me more in control. In a way". (Patient) |
| 21 | Mäkelä 2020, UK | Explore the work of patients and caregivers at the time of an acute health event, the interface with health professionals in hospital and hospital at home and how their experiences related to the principles that underpin comprehensive geriatrician assessments | Admission Avoidance Hospital at Home for acute medical conditions | Service level (patients and caregivers |
Family members described the challenges if a patient experienced fluctuating confusion, having to negotiate with their relative about seeking hospital at home care before taking action on their behalf. Ambiguity about the timing of discharge from different visiting HAH staff suggested decision‐making occurring away from the home. Many described not knowing how long to expect HAH to be available or had not anticipated imminent discharge: "That just came out the blue". (Caregiver) |
| 22 | Manning 2016, Wales | Explore how traditional and new models of care meet patients’ needs according to patient and staff experiences | Admission Avoidance Hospital at Home for various conditions (e.g. falls and fractures) | Service level (patients and staff) | Able to achieve patient care goals by a multidisciplinary team effort and involving the patients in the decision‐making process. (Nurses) |
| 23 | Nordin 2015, Sweden | Describe patients’ expectations of coming home very early after stroke with support and rehabilitation at home | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Clinical trial) |
Service level (Patients) | “…we decided that on the first day that I was going to cook and she was going to be with me. How to get it to work and the like. // Make something myself, lunch or something. I’m going to try to do it myself, but they would be, she would be with me.” (Patient) “The first few days after I get home, they should be able to work out what I can’t manage to do, what I’m going to need help with”. (Patient) |
| 24 | Papaioannou 2018, Canada | Describe the implementation of an intravenous service and assess the perceptions of residents, family caregivers and other relevant key informants | Admission Avoidance Hospital at Home for respiratory or urinary tract conditions (A pilot delivered in 4 residential care facilities, 3 multiple‐payer, 1 single‐payer) | Service level (caregivers and staff) | LTCH nurses were perceived to be professionally trained and skilled to provide IV therapy and hypodermoclysis; as such, caregivers did not perceive the need for IV therapy as a priority reason for hospital transfer or admission. |
| 25 | Ranjbar 2015, Sweden | Explore patients’ experiences of Sweden’s first COPD mobile care programme and evaluate if a human rights‐based analysis could provide additional information on the patients’ experiences of the COPD mobile care programme | Early Discharge Hospital at Home for COPD | Service level (patients) | “They are competent because they know what they are doing, regarding the COPD. I know a little fraction but they know everything”. (Patient) “It was just like I had known her forever. No it was nothing, it was just like I had known them forever. So, it’s different people you can talk to, some you can’t talk to at all. So no, it was great, it was no problem”. (Patient) "They should have had more personnel in the beginning because when she came she had not much to do but in the end they had received so many patients so they had a shitload to do." (Patient) While a majority of participants were satisfied with the recommended length of stay, some wished for a longer stay or more frequent contact with nurses while in the programme. |
| 26 | Reid 2008, England | Explore informal carers’ experiences of an intermediate care service and how it met their needs | Early Discharge Hospital at Home for conditions at risk of leading to hospital admission or residential care (Rehabilitation at home) |
Service level (caregivers) | "They were really, really caring with her, she (ICS team member) did make her laugh and just give her a boost, confidence boost, and they involved her in having a wash and getting undressed. They encouraged her they did help her that way." (Caregiver) The process by which the decision was made over whether to accept or reject the residential service, was primarily influenced by previous experiences of residential care. Not surprisingly a previous negative experience led to reluctance to use the service again; but often the absence of a viable alternative to residential care meant that rejecting residential care was not possible. |
| 27 | Rossinot 2019, France | Make an inventory of experiences of patients and family caregivers in Hospital at Home | Early Discharge Hospital at Home for a variety of conditions such as cancer, chronic disease and fracture | Service level (patients and caregivers) | "There always is somebody who listens, who fastly comes if there is a problem… It’s an 'à la carte' service". (Patient) A patient was frustrated with inconsistent staff and schedules: “Everyday, there are different people. It is disturbing”. A caregiver was also frustrated: “there never was a permanent schedule. It is not easy. It is completely random. Some nurses prefer to start the day with my dad, other to finish by him. It depends”. |
| 28 | Schofield 2006, Scotland | Explore care experiences and preferences with respondents and their families | Admission Avoidance Hospital at Home for COPD | Service level (patients and caregivers) | Participants’ regard for the ARAS was overwhelming, and particular mention was made of its accessibility, ease of use, specialist clinical skills of the health professionals, and one to one care in the home by the friendly and approachable ARAS nurses. “Well, they’re not, eh shall we say officious and give an impression that they are in a hurry to go somewhere else. Concerned, as if they’re treating you, as if you are somebody special, not as if you’re just a number on their book”. (Patient) |
| 29 | Udesen 2021, Denmark | Describe and explore patients’ and caregivers’ experiences with home treatment | Admission Avoidance Hospital at Home for acute conditions | Service level (patients and caregivers | The home setting made it possible for the nurses to have undisturbed dialogues with patients and caregivers based on individual needs. |
| 30 | Vaartio‐Rajalin 2020, Finland | Describe Hospital at Home staff's perceptions about Hospital at Home care, including work structures, processes and outcomes | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | The tangible work that was coordinated for HAH patients included periodic, acute advanced nursing care, periodic care for long term illness linked to acute care needs, the monitoring of health and preventing of illness and the supporting of self‐rehabilitation. "This work in HAH is different...for example, because here the patients and their near‐ones are truly present all the time and have different challenges to meet and you must really think about how you introduce certain issues into discussion … That is really challenging … "(Focus group) The home context makes the care relationship different from the hospital ward, the home makes the patients equal with us nurses… less hierarchical… The care is given based on patient's terms. (Focus group) “During a home visit there is only the patient and the near‐one(s), no alarm calls from other patient rooms at the same time… You can fully concentrate on this specific patient and this situation and give your full attention…"(Focus group) The intangible but necessary work for the HAH patient consisted of coordinating care for the “whole patient,” being on call, documenting and reporting on patient safety and care continuity, advocating for the patient's best and testing new virtual methods for HAH care. It is so much more than to go into a patient's home and perform a task and come out… It is the whole situation, the whole patient is to be considered and coordinated… and the near‐ones…Before, during and after the actual home visit… To arrange consultations, to order blood samples or medicines… “We take the patient's near‐ones and dogs or cats into account, we show our respect for them by saying some words to near‐ones or clapping the pet... Or by taking the blood pressure also of the spouse, if they so wish”. |
| 31 | Vaartio‐Rajalin 2021, Finland | Describe how adult, non‐palliative patients and their spouses perceive person‐centredness in Hospital at Home care | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (Patients and caregivers | The hospital at home nurses were perceived to actively work to truly know and understand patients’ and spouses’ situations (i.e., their personal knowledge) and to recognize the intrinsic value of each patient and/or spouse by respecting their judicial and human rights to patient education and dignity, as well as the home environment. At home you have more equal status in decision‐making. “Participation ... and the contact with the one who is sick is closer and more intense in HAH care.” (Patient) |
| 32 | von Koch 2000, Sweden | To describe the content and experience of a programme involving early hospital discharge and continued rehabilitation at home after stroke | Early Discharge Hospital at Home for stroke (Rehabilitation at home (Implementation trial) |
Service level (staff) | Discontinuation of HAH was ultimately decided by the patient, within the time allowed. The discontinuation of the programme was well prepared by the partnership, and it was the patient who, within the time limits allowed, made the decision. A few patients considered themselves ready and ended the programme even though their therapists felt that there were more things that could have been accomplished. All therapists offered anecdotal evidences that decisions concerning what to do were based on the interests and goals expressed by the patient, as in this example cited by one of the speech and language therapists: “This man used to take a walk in order to place bets on the football games. Now he had problems writing his signature on the coupon and the goal for his walk had in some way lost its function. It was brought to my attention, and then I asked him if he wanted to practise writing his signature, something I would probably not have given priority to in a different situation. He wrote page after page practising his signature. He was very motivated.” In addition the therapists were observing and analysing the patient in his or her environment. In doing so the therapists achieved an understanding of discrepancies between the desires and abilities of the patient on the one hand and the environmental demands and expectations on the other. This implicit problem‐solving was concurrent with and enmeshed within the rehabilitation process. behaviour on the part of the spouses when communicating with patients with dysphasia, or their assisting more than required and desired by the patient are examples of problems that otherwise might have remained undetected. Examples of interventions used as a result of implicit problem solving were counselling, teaching, e.g. instructing the spouse how to assist the patient, and role modelling the desirable behaviour for spouses. Between the home visits the patients were encouraged to practise activities on their own. The patients were encouraged to devise solutions, to test them and to evaluate the outcome. Evaluation of the interventions applied included reminding the patient of their own previous ability, thus teaching the patient a strategy of reflecting on changes over time. You remember the way it was in the beginning. You couldn’t do this, you couldn’t do that. But now you can actually dress yourself and cook and do this and that. So you see, you’ve improved. It usually helps the patient to get on with his life. A very prominent theme characterizing the rehabilitation process was the partnership formed by the therapist and the patient, as illustrated in one of the interviews: In the hospital, this big institution where you are an authority in a white coat, the patient submits himself to you and wants you to help him and make him well. But at home I think it’s more like you discuss the patient’s problems and co‐operate with him to find solutions. One such theme was that activities between visits also could include the therapists acting on behalf of the patient in order to retrieve information or convey messages. “We act like a kind of an ombudsman for the patient. We make it easier for the patients and you assist them in finding the right authority for their problems”. |
| 33 | Wallis 2022, Australia | Explore patient and caregiver barriers and enablers, and components of care that may increase acceptability of hospital at home | Early Discharge Hospital at Home for total hip or knee replacements (Subacute rehabilitation, multiple‐payer setting) |
Service level (patients and caregivers | Patients and caregivers expressed the importance of specific information about recovery at home (e.g., expected recovery of pain and activity levels each week; extent to which the caregiver would need to look after the patient; rehabilitation‐at‐home schedules). Some patients and caregivers also wanted more information about ‘strong’ analgesics for managing pain overnight when the pain was perceived to be worse, and more practical instructions for self‐administering injections to prevent deep vein thrombosis. Patients and caregivers desired at least two home visits from clinicians in the first week following home discharge, with a higher number of sessions desired if patients were living alone and without caregiver support. Important components of care included provision of information and advice in response to patient and caregiver questions, observing how patients interacted in their home setting, and ensuring exercise performance was ‘absolutely right’, ‘customised’, and diverse with a range of exercises that were progressed incrementally. Patients believed routine home visits by doctors and/or nurses were not essential, providing there was an option for a doctor and/or nurse visit if required. This included a 24‐hour, 7 days‐a‐week direct line for medical advice and to arrange a home visit if required: “At three o’clock in the morning, [patient] was screaming in pain and I give her Palexia or something and about an hour later, she’s still screaming. What do I do? A direct line to the doctor to tell me what to do”. (Caregiver). |
| 34 | Wilson 2002, England | Compare Hospital at Home patient and carer satisfaction with hospital care. Explore which aspects of the two care options (hospital at home or hospital care) were particularly valued or caused concern. |
Admission Avoidance Hospital at Home for acute medical conditions | Service level (patients and caregivers | "They were marvellous, the home care nurses, they couldn’t have done more for him ... and they looked after me." (Caregiver) |
Theme 3. Acceptance, perceived benefits and caregiver impacts from Hospital at Home
Finding 1. Patients, caregivers and service level staff believed Hospital at Home (including in residential care) was an appropriate alternative to hospital inpatient care, and facilitated optimal recovery and satisfaction with less risk of hospital‐acquired complications. Patients appreciated positive and competent staff who motivated them to reach their recovery goals. Sometimes the lack of caregiver support and 24‐hour supervision from hospital staff made some patients prefer to stay in hospital (high confidence).
Early Discharge Hospital at Home
For stroke, staff were aware of the origin of the service and its supporting evidence, which was perceived to achieve good patient and service outcomes and closely aligned to their beliefs about best practice and early intervention (Hitch 2020). Staff generally perceived that the service met a patient’s need by returning home, which was perceived to be the optimal recovery environment (Hitch 2020). Staff were aware of the growing evidence base supporting Early Discharge Hospital at Home services and staff mentioned how patients were pleased to be at home (Moule 2011). Staff perceived that home was more comfortable for patients, facilitated context specific rehabilitation, and familiar surroundings and being closer to family and friends was an advantage (Kraut 2016). Staff also described disadvantages that their patient could encounter, including an unsuitable home environment that would make life difficult at home (Kraut 2016).
Stroke patients discussed how being at home would be better for them emotionally and physically with better recovery (Kraut 2016). Patients assigned their progress to the staff as they motivated them reach their goals (Fisher 2021). Patients highly valued recovery in their everyday surroundings, which was less stressful (Lou 2017). Patients described their home as a more private, individualised and focussed arena for rehabilitation, particularly for being able to ask questions of staff, and being able to walk around the house getting used to things that were in their homes (Cobley 2013). Being in their own surroundings provided access to their own things, being able to do what they want and to see their family again and facilitated daily activities and returning to everyday life (Nordin 2015).
For orthopaedic and neurological conditions, therapy in the home was perceived as a realistic environment, enabled a more realistic assessment of how well a patient and caregiver managed at home (Dow 2007a). It was seen as more appropriate for clients with cognitive impairment, and people from culturally and linguistically diverse backgrounds who were not familiar with the Australian hospital system (Dow 2007a). However, one caregiver did not want another ‘infection’ based on a previous infection while in hospital (Dow 2007b). For orthopaedic conditions, hospital and home staff perceived there were direct benefits to patients, fulfilling the patient’s preference for care at home, a faster recovery and improved quality of care (Sims 1997). For acute medical and surgical patients, staff felt that the home setting facilitated patient‐centred care (Cunliffe 2004). For subacute rehabilitation, participants primarily attributed satisfaction to the positive influence of being managed by staff in their home environment (Kimmel 2021). Acute care provided in the patients’ own home reduced concerns of hospital‐acquired infections (Karacaoglu 2021). In a multiple‐payer setting, patients undergoing elective joint replacement surgery perceived a lack of caregiver support and more intensive supervision and exercise sessions were a barrier to Hospital at Home (Wallis 2022). These patients and caregivers perceived their homes as familiar, comfortable and facilitating better sleep and recovery (Wallis 2022). The hospital was perceived as a risk for catching a contagious virus and akin to a prison (Wallis 2022). Despite this, some patients preferred hospital care for a rest from their usual daily lives (Wallis 2022). Patients and caregivers who had previously had joint replacement surgery preferred the same rehabilitation setting (inpatient or home) and sometimes the same clinician (Wallis 2022).
For treating pneumonia and deep venous thrombosis, home represented the flexibility of visits from family and friends, the comfort of a familiar bed, the choice of food, being able to maintain professional activities and financial saving (Dubois 2001). For COPD, patients considered the service as more convenient by avoiding admissions to hospital (Ranjbar 2015). For heart conditions, patients believed that Hospital at Home would shorten recovery periods, was mentally better and that they were free to pursue outdoor activities such as walking the dog (Dinesen 2008). For various conditions, patients and caregivers perceived better morale and satisfaction, and being at home increased the patients’ appetite (Rossinot 2019). In contrast, some patients and caregivers felt obliged to agree to Hospital at Home as no other options were available (Rossinot 2019).
Admission Avoidance Hospital at Home
For various medical conditions, patients found that being in their own surroundings was perceived to help them get better quicker with home being part of their therapy, and also important for couples that did not like to be separated (Wilson 2002). Being at home enabled patients to maintain their routines and be with their families, which was described as important (Udesen 2021). Home was perceived to allow better sleep in their own bed, improved social support from family and friends being able to visit much more easily, and more freedom to complete tasks and relax, and the physical distancing saved them from catching diseases (Levine 2021). Staff felt that patients would recover more quickly than if they were hospitalised, and reduce their risk of infection, and that they were well received by patients (Andrade 2013). For patients with acute confusion, patients described how the service had enabled continuity in their usual routines, in the familiar setting of their home (Mäkelä 2020). Hospital at Home was also perceived to improve equity and access for low‐income and rural patients (Gorbenko 2023).
In a residential care facility for various conditions, directors of nursing wanted to avoid hospital transfer for their residents due to the perceived negative view of hospital experiences (Barnard 2016). This included their residents being dozy on return from hospital due to chemical restraints, a perceived lack of care in hospital, and perceived negative language that hospital staff use to describe the residents (e.g. bed blockers) (Barnard 2016). For respiratory or urinary tract conditions (aged care facility), IV therapy within a residential care facility was valued as an opportunity to avoid hospital visits and admissions, better quality, and to avoid poor outcomes associated with hospital care (e.g. bed sores, confusion) (Papaioannou 2018). Staff believed it avoided care complications such as delirium, falls and medication errors (Testa 2021). Staff also perceived that it was less stress for the family and for the resident (Rayner 2022). Geriatricians believed the type of patient who would benefit most were those who were frail or had dementia (Testa 2021). Staff believed that patients at home were more mobile (Udesen 2022). Caregivers preferred the care in the nursing home due to a lower risk of poor outcomes, recovery being quicker than hospital care, being in a familiar environment and care providers being accustomed to their needs, better able to provide person‐centred care and better meals (Papaioannou 2018). Care in hospital was considered as less optimal because care providers are not familiar with the resident, and may not know potential safety risks, such as risk for falls (Papaioannou 2018).
Combined Admission Avoidance and Early Discharge Hospital at Home
For various conditions, staff perceived that patients recover sooner with less risk of infections, and the home facilitates functional recovery, better sleep and community outings (Vaartio‐Rajalin 2020). Nurse practitioners perceived that the quality of care was very high due to their advanced training, time with the patient, their specialist advice on management and caregiver support (Lemelin 2007). In a multiple‐payer setting, sometimes the perceived lack of caregiver support and unceasing supervision from hospital staff made some patients prefer staying in hospital (Ko 2023).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Andrade 2013, Brazil | Understand the organisation of the health system from the perspective of professionals that provide home care services | Admission Avoidance Hospital at Home for various acute conditions | Service level (staff) | “Patients get much better quickly than if they were hospitalized, not to mention the risk of infection." “You to be able to enter people's homes, we are very well received for that.” (Staff) |
| 2 | Barnard 2016, Australia | Understand the experience of Directors of Nursing from residential aged care who either had support of the Hospital in the Nursing Home service, or did not | Admission Avoidance Hospital at Home for various acute conditions (Aged care facility) |
Service level (staff) | Participants from both focus groups reported that they don’t like sending patients to hospital; not least of which was because of the view that residents are sent back far worse than when they went in. DONs claimed often hospitals won’t feed residents and that nobody gets showered in hospital now, unless families came to assist with the direct care. DONs expressed anger about the language of health care, noting that being viewed as a bed blocker was demeaning. Importantly, all DON’s expressed a view that they would rather keep their resident and often were not seeking to transfer them to hospital, especially since: the way they’ve been handled, talked about in front of...just add up to a really bad experience all the way through it. Residents it is claimed often return to a RAC disoriented and confused and heavily medicated from chemical restraints. DON’s commented that it was not unusual for a returning resident to be ‘‘very dozy’’ and that generally transferring was an overwhelming experience. |
| 3 | Cobley 2013, England | Explore patients' and carers' perceptions of early supported discharge services during the early post‐discharge phase | Early Discharge Hospital at Home for stroke (Study was conducted in the first year of implementation) (Rehabilitation at home) |
Service level (patients and caregivers | There was a consensus of preference among participants (15 of 19) for returning to their home environment as soon as possible: “Well, I was glad I was going home … I’m not saying the hospital was horrible, but I just didn’t like being in the hospital”. (Patient) Commonly, the home environment was described as a more private and individualized arena for rehabilitation: “If you’ve got any questions … you could ask them, whereas when you’re in a hospital, I feel that I can’t take up the people’s time because they haven’t really got time”. (Patient) |
| 4 | Cunliffe 2004, England | Assess the acceptability of the service and illuminate the relationship between process and outcome | Early Discharge Hospital at Home for acute medical and surgical patients | Service level (patients and staff) | They were also explicit in the importance of the patient’s views and participation in rehabilitation and felt that the home setting facilitated this style of practice. |
| 5 | Dinesen 2008, Wales | Understand the experiences and attitudes of patients and their spouses/partners with regard to the application of telehomecare technology as an option within home hospitalisation | Early Discharge Hospital at Home for heart conditions | Service level (patients and caregivers | "Mentally, it is three times better to be at home”. (Patient) Believe that home hospitalisation will shorten recuperation periods. (Patient) Free to pursue other activities, e.g. bicycle, walk, take the dog for a walk, etc. (Patient) |
| 6 | Dow 2007a, Australia | Make recommendations to the Victorian Government on best practice in rehabilitation at home | Early Discharge Hospital at Home for orthopaedic and neurological conditions (Rehabilitation at home) | Service level (patients, caregivers and staff) | “Well it would be an advantage him being at home because he’s in his own environment and he can learn around that instead of being in a hospital environment which is more routine ... well it’s better being at home than in hospital because you are in your own home, you’re doing your own thing.” (Health professional) Therapy in the home was seen as providing situation specific therapy in a realistic environment. It was seen as helpful in assisting clients in the adjustment from hospital to home, often reducing hospital length of stay. Staff were better able to identify motivators and barriers for therapy when working in the home and to assess more realistically how well the client and carer would manage, which was sometimes difficult to determine in hospital. RITH was seen as advantageous for clients who could not access centre‐based therapy and it gave clients more control over the direction, timing and duration of their therapy. Staff saw RITH as being advantageous for carers who could be more involved in therapy without the stress of visiting the client in hospital. It was also seen as more appropriate for clients with cognitive impairment and people from culturally and linguistically diverse backgrounds who were not familiar with the Australian hospital system. |
| 7 | Dow 2007b, Australia | Determine how the role of the carer in rehabilitation at home programmes is constructed | Early Discharge Hospital at Home for orthopaedic and neurological conditions (Rehabilitation at home) |
Service level (caregivers and staff) | [Caregiver] said that “They didn’t want a staph infection from the (hospital) in their ward”, referring to the fact that her husband had contracted a Staphylococcus infection while in another hospital. |
| 8 | Dubois 2001, Switzerland | Evaluate patients' satisfaction with Hospital at Home care | Early Discharge Hospital at Home for various conditions including community‐acquired pneumonia, intravenous anti biotherapy, deep venous thrombosis) (Pilot programme implemented 2 years prior) |
Service level (patients) | Positive aspects included the flexibility of scheduling, especially for visits from family and friends, as well as the comfort of a familiar bed and lodgings, the choice of food, the possibility of maintaining certain non‐physical professional activities, and financial saving. |
| 9 | Fisher 2021, UK | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
The home environment provides a familiar environment for stroke survivors to regain their independence, while returning to their usual routine and roles. Regardless of the participants’ uncertainty, all the respondents conveyed positive views of the service. They thought it was useful to have a continuous and prompt support available upon discharge from hospital: "The main benefit I think is the fact that it’s immediate. There’s not this gap between hospital and coming out" (Patient) Most of the interviewees (Patients) assigned their progress to the fact that the ESD team motivated them to work towards their recovery goals. Many participants were pleased to move from the hospital setting to the comfort of their own homes: “But you’re also in your own environment at home”. (Patient) |
| 10 | Gorbenko 2023, USA | Examine processes of uptake and implementation of the Acute Hospital Care at Home waiver (expansion) programme in a national sample. This included examining the barriers and facilitators of the waiver programme implementation across implementation stages and describing strategies used to address these barriers and/or best practices. | Admission Avoidance Hospital at Home | Service level (clinical leaders) | All participants discussed the many benefits to patients and families of receiving care at home, for example by giving providers an opportunity to assess social determinants including food security or hazards in the home. Our interviewees described how the HaH model positively impacted equity and access. They believed HaH benefited patients who normally lacked access to hospital level care, such as low‐income patients and those living in rural areas. |
| 11 | Hitch 2020, Australia | Describe staff perceptions of the trial of an early supported discharge model of care for stroke survivors | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Implementation trial) |
Service level (staff) | Participants were generally well aware of the origin of ESD and its supporting evidence, which was perceived to provide support for good patient and service outcomes. ESD was unequivocally perceived to have more advantages than other stroke rehabilitation programs (as indicated by the perceived disparity between ESD and standard practices). These advantages were perceived to come at no cost or disadvantage to patients, fulfilling both their and the service’s needs. “They have to get dressed, they have to get up and make their own cup of tea, they have to–you know, so it’s kind of forced rehab...” (Focus group). "It reduces bed days. . . so, that reduces risk of infections . . . risk of pressure injuries. . . demand on the ED department, just by having someone being able to move out of that bed sooner has allowed for other things to happen within the hospital". (Focus group) “It’s getting to people in an earlier part of their journey, when they are going to be making more spontaneous neuroplastic changes”. (Staff) “You’re seeing more of the things that you can actually do that will make a difference to that person’s life, rather than just the medical view”. (Focus Group) "Efficacy I know what intensive therapy looks like. . ... (but) they had to shift their thinking, because these clients were going to achieve their goals much quicker”. (Staff) |
| 12 | Karacaoglu 2021, UK | To understand staff views of implementing a Hospital at Home model in a Scottish care setting | Early Discharge Hospital at Home for various acute conditions | Service level (staff) | Care provided in patients’ own home reduced concerns of hospital acquired infections: “…the risks, they are exposed to more bugs and germs [in hospital], they are at a higher risk for their health” Staff received predominantly positive service feedback, in particular being able to receive care in their own home, with benefits including being able to have support networks close‐by: “At least when they are in their home environment they are in their comfort zone. Family, friends and all that have a lot easier access if they have those people round about them” |
| 13 | Kimmel 2021, Australia | To evaluate the 3‐month pilot programme from the perspective of participants and identify themes or participant factors relating to the care received and involvement in decision‐making. This was to inform the development of bed substitution rehabilitation services in the future. | Early Discharge Hospital at Home (Subacute rehabilitation) |
Service level (patients) | Most participants were very satisfied with the program, which was primarily attributed to the positive influence of being managed in their home environment. There were positive reflections on the knowledge and experience of the majority of the staff involved in the program, which contributed the high level of satisfaction. "I think it's so much better being at home, when your friends can come and visit you, so you're not bored all day, and you haven't got that horrible food … You're just in your own environment, your own home, and people visiting you … you know, people came around with food, I was very spoilt." |
| 14 | Ko 2023, Singapore | Explore the experiences and perceptions of patients and their caregivers admitted to a Hospital at Home programme | Combined Admission Avoidance and Early Discharge Hospital at Home, for acute conditions | Service level (patients and caregivers) | Participants shared positive HaH experiences, which included comfort, convenience, increased involvement in patient care, engagement with the care team, and perceived improved patient outcomes. “…comfort, it is intangible right. You can’t put dollars and cents into it…ability to sleep better right, you are close to the things that you are used to…watch TV…go onto the computer. Where else in the hospital, you can’t do all these.” (Patient) The perceived lack of caregiver support and round‐the‐clock direct supervision from the care team had made some patients prefer staying in a hospital ward. “…I think the hospital [was] better. Because there will be nurses all down there [the hospital]. If I want to ask something, also can…my wife all make noise already, [asking me] why you cannot stay [in the] hospital.” (Patient) Patients felt that being in a familiar environment at home allowed them to relinquish the “sick role” associated with hospital care, and to actively participate in their recovery. Patients reported better sleep, appetite, and mood, which they perceived to help with faster recovery. Several patients and caregivers perceived that HAH had improved the overall quality of care. For example, they described that HaH decreased their risk of contracting hospital‐acquired infections and reduced unnecessary admission to hospitals for elderly patients, especially those with recurring infections. Patients with dementia were able to recover in a familiar environment which reduced delirium. All the LARs perceived higher family satisfaction, in knowing that elderly patients were able to recover in a conducive environment. “[NUHS@Home provides a] more familiar environment, so she [dementia patient] feels less afraid and less confused…we rarely see her agitated at home, as compared to the hospital.” (Caregiver) |
| 15 | Kraut 2016, Australia | Explore factors that indicated patient suitability and likelihood for referral and utilisation of early discharge rehabilitation at home | Early Discharge Hospital at Home for stroke (Rehabilitation at home) |
Service level (patients and staff) | Most patients, and to a lesser degree staff, agreed that being at home in familiar surroundings and closer to family and friends was an advantage. Four patients discussed how being at home would be better for them mentally and emotionally. "Well it would be an advantage him being at home because he’s in his own environment and he can learn around that instead of being in a hospital environment which is more routine ... well it’s better being at home than in hospital because you are in your own home, you’re doing your own thing."(Staff ‐ Health professional) Staff described a number of disadvantages that their patient could encounter, including a reduced intensity of rehabilitation compared with hospital; possible readmission to hospital due to recurrence of illness; an unsuitable home environment that would make life difficult at home; and a reduced level of confidence away from the supportive hospital environment. |
| 16 | Lemelin 2007, Canada | Evaluate the acceptance of a hospital at home programme managed and provided by nurse practitioners | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) |
All NP respondents felt the patients received very good quality of care and that the program met (all or most of) the needs of their patients. NPs felt this was due to a combination of their advanced education; the amount of time the NPs were able to spend with each patient; and the information they provided on medications, chronic illness management, pain management, and caregiver support. "I think the quality of care was exceptionally high...” (Nurse practitioner) |
| 17 | Levine 2021, USA | Elucidate and explain patient perceptions of home hospital versus traditional hospital care to better describe the different perceptions of care in both settings | Admission Avoidance Hospital at Home for a variety of acute conditions | Service level (patients) | “It saves us from getting…any kind of disease from other people”. (Patient) “You know, I was sleeping in my own bed. You can’t top that”. (Patient) Home patients described their ability to do their daily activities: “I was able to do everything at home, you know like I tried to relax a little bit, but I was able to wash the dishes, do some laundry”. (Patient) “..and their ability to roam around their usual environment: “At least, I was here. I was not, you know, confined while I was at home, [I could] do what I wanted to do” (Patient). |
| 18 | Lou 2017, Denmark | Investigate how mild stroke patients and their partners experience and manage everyday life in the context of early discharge rehabilitation at home | Early Discharge Hospital at Home for stroke (mild) (Rehabilitation at home) |
Service level (patients and caregivers | They found it meaningful and valuable to practise and recover in their everyday surroundings. The couples reported that the home atmosphere was less stressful and that they were able to ask questions more freely: “It’s just more relaxed.. . Like, at the hospital I sit in the chair, right? At the patient side of the table. But at home it’s different. It’s my home ground so the roles are a bit different. She’s the visitor. That puts me more in control. In a way”. (Patient) |
| 19 | Mäkelä 2020, UK | Explore the work of patients and caregivers at the time of an acute health event, the interface with health professionals in hospital and Hospital at Home and how their experiences related to the principles that underpin comprehensive geriatrician assessments | Admission Avoidance Hospital at Home for acute medical conditions | Service level (patients and caregivers |
You’re in your own environment and people come in to check that you’re all right. I mean at least you can do what you want to do where in hospital you’re confined to a certain amount of space. (Patient) |
| 20 | Moule 2011, England | Explore how the early stroke discharge team members and external stakeholders experienced the service implementation process | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (New service) |
Service level (staff) Systems level | “It is more cost effective, with lower mortality, better outcomes and patient satisfaction.” (Staff) “Our patients’ general feedback was that they were just really pleased to be at home.” (Staff) |
| 21 | Nordin 2015, Sweden | Describe patients’ expectations of coming home very early after stroke with support and rehabilitation at home | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Clinical trial) |
Service level (Patients) | Being in a familiar environment was described as desirable. The participants longed to be in their own surroundings, to have access to their own things, and to see their family again. |
| 22 | Papaioannou 2018, Canada | Describe the implementation of an intravenous service and assess the perceptions of residents, family caregivers and other relevant key informants | Admission Avoidance Hospital at Home for respiratory or urinary tract conditions (A pilot delivered in 4 residential care facilities, 3 multiple‐payer, one single‐payer) | Service level (caregivers and staff) | “I think it helps the residents stay out of hospital, where the nurses there, even though they are skilled, we know the resident personally and know exactly what they require, what their day‐to‐day activities are so we know what to expect from them as they go through having the IV in.” (Staff) “Well when they go to the hospital it’s usually for the initial setup and starting the IV. Waiting long hours in the emergency, waiting long hours you know, just avoiding the transfer stress from going to the hospital, it takes a toll on some residents. So being within their home it’s much more beneficial for them.” (Staff) Care in a familiar environment and familiar care providers is valued and preferred over care in hospital. Caregivers valued their family member receiving medical care within the LTCH as the environment is familiar and care providers are accustomed with their needs. Care in hospital was considered as less optimal because care providers are not familiar with the resident and, as a consequence, may not understand what the resident is communicating to them, or they may not know potential safety risks, such as their risk for falls. It was perceived that, when care providers are familiar with the resident, they are better able to provide person‐centred care. “I think it also helped him maybe recover that much sooner or better or faster, [because] he’s not in the hospital because he likes the environment that he’s in and you know, the nurses there are, were catering to him because he had this IV and also you know, asking him if he wanted meals there and they came there and brought him meals and fed him and the food is much better there than in the hospital, so all of that obviously helps his recovery”. (Caregiver) |
| 23 | Ranjbar 2015, Sweden | Explore patients’ experiences of Sweden’s first COPD mobile care programme and evaluate if a human rights‐based analysis could provide additional information to the patients’ experiences of the COPD mobile care programme | Early Discharge Hospital at Home for COPD | Service level (patients) | "It was great because you know when you get ill you didn’t have to go to the hospital every time because they did much of the hospital’s [work] otherwise I would have had to go in". (Patient) |
| 24 | Rayner 2022 | Understand what factors, including the service model, were associated with more frequent use of Residential in Reach services by nursing homes | Admission Avoidance Hospital at Home (2 'Residential in Reach' services for residential care patients) |
Service level (staff) | The RiR services were highly regarded by all participants, especially as use of the service allows residents to be assessed and managed in the home. Instead of sending the resident to hospital In reach come. They do the assessment here, it's less stress for the family and for the resident. |
| 25 | Rossinot 2019, France | Make an inventory of experiences of patients and family caregivers in Hospital at Home | Early Discharge Hospital at Home for a variety of conditions such as cancer, chronic disease and fracture | Service level (patients and caregivers) | Hospital at home is linked to an improvement of morale and a good quality of care but necessitates the integration of heavy organizational constraints by caregivers and patients. “We eat a hundred times better at home than in the hospital”. (Patient) “My morale is better too.” (patient) “(Is it better for him to be treated at home?) Yes, for his morale.” (caregiver) |
| 26 | Sims 1997, England | (1) Evaluate within the borough the practicality and acceptability of the 'Going Home Service' to patients and to staff employed in the service and in other services on which the scheme impinges (2) Establish the impact on informal carers |
Early Discharge Hospital at Home for orthopaedic conditions (New service) |
Service level (staff) |
From across both staff sectors, nine interviewees suggested that the home environment encouraged faster rehabilitation and re‐integration into the community and 13 said the service promoted a speedier recovery. |
| 27 | Testa 2021 | Explore health professionals’ perspectives on the factors impacting Aged Care Rapid Response Team utilisation in the care of acutely unwell residential aged care facility residents | Admission Avoidance Hospital at Home (Acute, residential care) |
Service level (staff) |
When considering the risks and benefits of hospital transfer for unwell older RACF residents, participants recognised potential care complications for residents admitted to hospital. These care complications included delirium, falls and medication errors. The type of patient [who would benefit most from ARRT] would be someone who's frail, who has dementia. That would be an example of condition where it's better for them not to be in hospital if you can avoid it (Geriatrician). |
| 28 | Udesen 2021, Denmark | Describe and explore patients’ and caregivers’ experiences with home treatment | Admission Avoidance Hospital at Home for acute conditions | Service level (patients and caregivers | At home enabled them to maintain their routines and be with their families. Some patients also reported that they could take care of and socialise with their children, which they described as being significant and important. Most of the patients and caregivers expressed that treatment at home was more comfortable compared with hospitalisation or visiting a GP, and this was because of the familiar surroundings of their own homes: ‘It is more comfortable to be at home and I feel less ill. I can decide for myself how things should be. I get well faster at home’. (Patient) The patients and caregivers found the acute nurses to have high competencies and to act in a very professional manner. Most of the patients and caregivers explained that ATO was highly effective because the nurses managed to see their patients faster than GPs could and ATO does not have the same waiting procedures as the hospitals: 'It does not work well at the hospital. There was a lot of noise, waiting time, and no contact person. Nothing happened. It was good to come home to a follow up by the acute care team’ (Caregiver) |
| 29 | Udesen 2022 | Explore different healthcare professionals’ perspectives on and experiences with the ED‐based acute care service | Admission Avoidance Hospital at Home (Emergency Department‐based Acute Care Service for residential care) |
Service level (staff) | 'You will see if the patient is lying in bed. The patient often sits in a chair, drinking a cup of coffee ... At the ED, they would have been lying in a bed doing nothing’ (Focus group). The acute care service was not considered to be equivalent to hospital admission as there are limits to what can be provided outside the hospitals. The solution was described as an appropriate alternative. All of the focus group participants were very focused on which hospital‐related complications might be avoided by keeping the residents in the nursing homes: ‘ ...We can prevent hospital‐acquired infections, and we can prevent complications due to immobility and [keep them from] becoming confused when our demented residents are removed from their home’ (Focus group). Service increased the treatment efforts at the nursing homes resulting in overtreatment of the residents: ‘You have to be careful about what you initiate. Now it is acute conditions ... What can you assess and what is next? How much hospital do we want to bring to the nursing homes?’ (GP) The other five GPs disagreed and described that the alternative would have been patient transfers to the ED, and they explained that keeping the residents at the nursing homes was less intrusive for the residents than hospital admission because the residents avoided ED transfers, waiting hours at the ED and confusion. |
| 30 | Vaartio‐Rajalin 2020, Finland | Describe Hospital at Home staff's perceptions about Hospital at Home care, including work structures, processes and outcomes | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | Patients recover much sooner, don't get any bacteria like in the hospital. They rehabilitate themselves merely by doing ADL activities at home, they eat better, sleep better…They enjoy their normal life despite the health problem! They have a lot more social contacts, friends and relatives visit them at home rather than in the hospital…Some of them go to work, visit the theatre or cinema, take a trip somewhere… |
| 31 | Wallis 2022, Australia | Explore patient and caregiver barriers and enablers and components of care that may increase acceptability of Hospital at Home | Early Discharge Hospital at Home for total hip or knee replacements (Subacute rehabilitation, multiple‐payer setting) |
Service level (patients and caregivers | Patients described this setting [inpatient care] as more ‘official’, ‘disciplined’and ‘sensible’ representing potential barriers to home‐based care. This included the perception of more intensive supervision and exercise sessions, better facilities and equipment, ‘on‐tap’ medical care for careful monitoring, analgesia, and managing complications: “They probably wouldn’t supervise you that much because they’d only be here for half an hour.” (Patient) Some patients preferred inpatient rehabilitation to ‘receive a break’, ‘switch off’ from their usual daily lives and activities, and ‘relax’ knowing their meal would be provided, and they did not have to cook and clean, which would not be the case with home‐based care. Patients and caregivers perceived their homes in a positive way and the hospital in a negative way (even if patients preferred inpatient rehabilitation). Homes were perceived as familiar, relaxing, comfortable, allowing better sleep, more visitors, independence, control, solitude, and greater flexibility to develop their own routines. Hospital wards were perceived as noisy and busy places, akin to an ‘institution’ or a ‘prison’ that provided terrible food that did not meet their dietary requirements or cultural preferences. Hospitals had routines that made them go ‘stir crazy’, feel uptight, bored, and depressed, and provided group sessions that were the same for everyone. A few patients interviewed at the beginning of the Covid‐19 pandemic perceived the hospital was a place where there was a risk of catching the contagious virus. Patients who preferred home‐based care, perceived the home setting facilitated the ‘optimal recovery’, provided one‐on‐one rehabilitation attention, and psychological benefits resulting from being in their own home and from outdoor physical activity. Patients’ determination for an ‘optimal recovery’ included reaching milestones in the shortest possible time by performing their normal routines, activities, hobbies, and work. Patients and caregivers who had previously had joint replacement surgery preferred the same rehabilitation setting (and sometimes the same clinician). This gave them confidence in the knowledge that this service provided a safe and effective recovery. |
| 32 | Wilson 2002, England | Compare Hospital at Home patient and carer satisfaction with hospital care. Explore which aspects of the two care options (hospital at home or hospital care) were particularly valued or caused concern. | Admission Avoidance Hospital at Home for acute medical conditions | Service level (patients and caregivers | “I would always prefer to stay at home because I’ve got my own ways and my own ideas. Probably being at home works better than a drug ..." (Patient) "You’re in your own surroundings which helps you get better quicker." (Patient) The best thing about being in Hospital at Home was frequently described in broad terms as "being in your own home". |
Finding 2. Caregivers were impacted by Hospital at Home. This included disruption to their normal routines, work, energy and sleep. There were reports of stress and anxiety related to feeling untrained to provide patient support and monitoring and a lack of formal recognition and access to information. Some caregivers and patients were concerned about their privacy at home and the impact on the patient/caregiver relationship from being involved with care (high confidence).
Early Discharge Hospital at Home
Prior to implementation, staff thought the service might add an additional burden and anxiety for informal caregivers, although some felt a key advantage was that caregivers did not have to travel to hospital and received some respite while the service was in place (Sims 1997). Staff expected caregivers to provide assistance with domestic activities of daily living, monitor patient safety, support exercise regimes, and provide some assistance with personal care; however, the service had no formal processes for identification, recognition, inclusion or compensation for the carer (Dow 2007b). Staff highlighted the need to consider the willingness and readiness of caregivers to take on caring responsibility, especially for stroke patients with severe disability that was considered risky (Fisher 2021).
Patients who were more severely affected preferred not to overburden their caregivers, and before selecting Hospital at Home, took into account the inconveniences to informal caregivers, which was tiring and intolerable for some (Dubois 2001). However, caregivers avoided trips to the hospital, saving time and money, and some informal caregivers were less worried because they reasoned that if patients were at home, their illness was not so serious (Dubois 2001). Patients considered themselves a burden to their families and felt guilty (Rossinot 2019). Also, caregivers reported stress, exhaustion, both physical and mental, and feeling close to burnout (Rossinot 2019). For caregivers working full time, this was especially difficult and tiring because of their work and caregiving role, such as cooking and dealing with daily issues (Rossinot 2019). Caregivers had "no hesitation" because going home was the most satisfying solution (Rossinot 2019). Caregivers wanted to be involved in decisions when they felt the burden of care fell on them, but they felt ignored (Reid 2008).
Caregivers described that the therapy sessions for stroke patients allowed sufficient respite, while some caregivers felt the therapy time was not long enough for respite and felt housebound (Cobley 2013). Caregivers felt that the healthcare staff forget that the caregiver is looking after the stroke patient, which is demanding, and they felt thrown into the caregiving role without receiving adequate support or training (Cobley 2013). Also, caregivers reported doing tasks that were previously the responsibility of their partner, being more housebound, feeling exhausted and physically drained, and difficulty coping/feeling helpless with their partner’s emotional distress (Cobley 2013). Patients and caregivers relied on Hospital at Home staff for moral support (Rossinot 2019). Staff were concerned about stroke patients using the service with increased levels of dependence and that the service should extend support for caregivers (Hitch 2020). Caregivers described their role as “intimate, arduous and relentless” with all caregivers reported to provide some degree of help for the patient, such as assistance with hygiene, dressing and transfers (Dow 2007b). Caregivers felt “forced to take responsibility” and “insecure” when faced with their partners with heart conditions receiving hospital at home (Dinesen 2008) and patients felt confident to stay at home based on their physician’s assessment of their ability to stay at home (Dinesen 2008). Caregivers reported providing help for the patient following hip/knee replacement surgery, such as assistance with hygiene, dressing, transfers and overall responsibility (Jester 2003). Depending on relatives and neighbours for daily tasks was important for patients to feel emotionally secure at home (Nordin 2015). For subacute rehabilitation, patients felt that being at home was easier for their family, but many felt that they would not have managed at home without assistance from their caregiver (Kimmel 2021; Wallis 2022). For elective joint replacement patients, some from multiple‐payer settings did not want to burden their families or ask for their support and thought it was unrealistic (Wallis 2022).
Stroke patients had to adjust to a new relationship with their spouse. For example, one patient commented that their spouse became more of a carer than a wife (Cobley 2013). Caregivers considered it their role to nudge, challenge and support the patient in pursuing challenges at the right time (Lou 2017). However, female caregivers sometimes refrained from making comments and suggestions to the patients due to the importance of upholding their marital relationship rather than becoming the patient’s proxy therapist or mother (Lou 2017). Couples described how they adjusted in a positive manner – by adjusting their routines and divisions of labour at home (Lou 2017).
Heart patients and caregivers got on each other’s nerves due to a power imbalance (Dinesen 2008). Female caregivers appreciated being able to retain a mother/daughter relationship, rather than being expected to carry out personal care tasks (Reid 2008). COPD patients' personal relationship circumstances affected participation in hospital at home when a patient and spouse were divorcing, and they did not feel that their sold house would be conducive for recovery at home at this time (Dismore 2019). Caregivers wanted their home to be neat and tidy for the district nurse (Dinesen 2008). A COPD patient declined Hospital at Home because they were frightened that their house would not be tidy, and other patients were concerned that their caregivers might be frightened seeing/knowing they are unwell at home (Dismore 2019). Some patients mentioned a lack of intimacy related to a high frequency of nurse and doctor visits and tiredness (Dubois 2001). Staff highlighted a lack of privacy in the home as a disadvantage of the service (Sims 1997).
Admission Avoidance Hospital at Home
Staff described supporting caregivers with necessary resources to support care at home to avoid caregiver burnout (Andrade 2013). Staff perceived that patients were reluctant to receive hospital at home care, that some patients were sceptical, and some had caregivers that preferred the patient was hospitalised for respite from caregiving duties, and these barriers were sometimes addressed by offering additional home support (Brody 2019).
Caregivers valued the attention they received from Hospital at Home (Wilson 2002). Caregivers were more involved in monitoring and maintaining safety, particularly overnight (Mäkelä 2020). If patients did not want to be a burden to their families, they were prepared to accept help from other services (Manning 2016). Patients felt that being at home put less strain on their caregivers as they did not have to travel to hospital (Wilson 2002). Caregivers felt that although hospital would potentially relieve them from all their caring tasks, the upheaval of visiting the hospital, of being separated and not knowing what was happening to their relative while in hospital, was a less satisfactory option (Wilson 2002).
Caregiver availability to provide supervision was important (Mäkelä 2020). Patients living alone exhibited a determination to manage at home by relying on social connections such as neighbours, friends, private cleaners, formal carers, sheltered accommodation wardens, personal alarm responders and befrienders, and described diverse pre‐existing support networks (Mäkelä 2020). Others relied on family and tenants taking care of the daily tasks (Levine 2021).
Caregivers (spouses) emphasised the importance of Hospital at Home by not being separated from their partners (Wilson 2002).
Patients were worried about the house being clean (Levine 2021). Patients expressed feeling like a burden when they had to visit their GPs or the hospital, both to their caregivers and to healthcare professionals (Udesen 2021).
Combined Admission Avoidance and Early Discharge Hospital at Home
Caregivers described their role as an extension of their role as a spouse, including an assistant for activities of daily living, a person who helps them remember, a role as a social worker, nurse and patient advocate (Vaartio‐Rajalin 2021). Sometimes caregivers did not want the patient to receive care at home, so they could have relief from their caregiving duties (Vaartio‐Rajalin 2020). Staff perceived they had a balancing act of the patient’s and their caregivers’ preferences and physicians would call the caregivers to inform them and discuss the proposed Hospital at Home care plan (Vaartio‐Rajalin 2020). Caregivers reported stress and inability to sleep when they were not experienced and did not know how to help the patient (Ko 2023). Working caregivers preferred to work from home, and there were challenges such as taking unpaid time off to care for their loved ones (Ko 2023).
A perception of forced intimacy caused humiliation and burden on a relationship, such as when a child had to care for their parent and see them naked (Vaartio‐Rajalin 2021). Caregivers were concerned about the suffering sick relative, which impacted the relationship (Rossinot 2019). However, hardships also strengthened and reinforced relationships (Rossinot 2019; Vaartio‐Rajalin 2021).
Home care nurses from a combined service for acute conditions did not wear work uniforms and their cars did not have a logo to maintain the patient's privacy when visiting patients (Vaartio‐Rajalin 2020). Staff perceived that caregivers may feel tired of having staff in their homes, and experience an intrusion into their private lives, but with mixed feelings as they are also thankful for the care provided (Vaartio‐Rajalin 2020).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Andrade 2013, Brazil | Understand the organisation of the health system from the perspective of professionals that provide home care services | Admission Avoidance Hospital at Home for various acute conditions | Service level (staff) | Cost reduction for the System of Brazilian Health can occur simultaneously transferring work to families. What supportive services can be provided to patients to prevent or reduce risk of caregiver burnout during a home hospitalization? The home service seeks to minimize this situation by provide family members and patients with most the material resources necessary for care in the residence. |
| 2 | Brody 2019, USA | Examine facilitators and barriers to implementation of the Hospital at Home programme over its first year of operation to provide others the opportunity to plan effectively for operationalisation | Admission Avoidance Hospital at Home for various acute conditions (This study focused on the first year of operation) |
Service level (staff) Systems level (executive leader) |
One additional barrier was willingness of patients to accept HAH‐Plus care. Some patients were sceptical about HAH‐Plus, others had family who wanted them hospitalized so they could have respite from caregiving duties, and some did not want clinicians in their homes. These barriers were partially addressed through providing additional time‐limited aide services. |
| 3 | Cobley 2013, England | Explore patients' and carers' perceptions of early supported discharge services during the early post‐discharge phase | Early Discharge Hospital at Home for stroke patients (Study was conducted in the first year of implementation) (Rehabilitation at home) |
Service level (patients and caregivers | The therapeutic sessions between patient and the Early Supported Discharge (clinicians) team enabled them to engage in their own activities: “I could get on with the little jobs that wanted doing or I could just put my feet up and have a rest, so it made life a darn sight easier for me”. (Caregiver) On the contrary, two carers described feeling housebound as the team were "not with the patient long enough" to enable sufficient respite time for the carer. (Caregiver) Staff forget that the caregiver is looking after the patient which is demanding and they felt thrown into the caring role without receiving enough support from the staff. “I wasn’t physically shown the best way to support him ... it was all trial and error”. (Caregiver) Doing tasks that were previously the responsibility of their partner, being more house bound, feeling exhausted and physically drained, and difficulty coping/feeling helpless with their partners emotional distress. “His depression ... I just don’t know what to do. I can’t cope because I don’t know what to do to stop it. When he is continuously crying, it can be really wearing because you’re helpless”. (Caregiver) “I think the wife’s come more a carer than my wife now and she shouldn’t be”. |
| 4 | Dinesen 2008, Wales | Understand the experiences and attitudes of patients and their spouses/partners with regard to the application of telehomecare technology as an option within home hospitalisation | Early Discharge Hospital at Home for heart conditions | Service level (patients and caregivers | Caregivers felt “forced to take responsibility” and “insecure” when faced with their partners receiving hospital at home. Confidence in consultant doctor's assessment of ability to stay at home. (Patients) Was the dominant and controlling party, so patient, spouse/partner got on each other's nerves. Want the home to be neat and tidy before the district nurse comes. (Caregiver) |
| 5 | Dismore 2019, England | Identify positive drivers and potential barriers to implementation of Hospital at Home for patients with exacerbation of COPD and low risk of death using the Dyspnoea, Eosinopenia, Consolidation, Acidaemia and atrial Fibrillation (DECAF) prognostic score and assist wider implementation | Early Discharge Hospital at Home for COPD (Implementation trial) |
Service level (patient, caregivers and staff) | For some, personal circumstances affected participation: “My husband and I are divorcing and my house just having been sold the atmosphere at home wouldn’t be conducive in recuperating... but in the future... I would very much like to be involved”. (Patient – Declined service) “I thought people coming to my house, I cannot... I’m frightened that it wouldn’t be tidy”. (Patient ‐ declined service) “It’s frightening for them to see when you’re not well it’s not nice for my husband to sit and watch us when I’m bad”. (Patient) |
| 6 | Dow 2007b, Australia | Determine how the role of the carer in rehabilitation at home programmes is constructed | Early Discharge Hospital at Home for orthopaedic and neurological conditions (Rehabilitation at home) |
Service level (caregivers and staff) | The expectations that staff had of carers were consistent with the carers’ descriptions of their caring activities. Carers were mainly expected to provide assistance with domestic activities of daily living, such as cooking, cleaning and laundry, but they were also relied upon to monitor the client’s safety at home, follow‐through on therapeutic regimes, and to a lesser extent, provide assistance with personal care. (Staff) “A lot of encouragement and support, their OK [for the client] to come home, looking after the physical situation, providing the meals and the hotel‐type support.” (Staff regarding the programs expectations of caregivers) Other expectations were that the carer cooperate with the rehabilitation team’s care plan. Staff said they expected the carer “to work as part of the team” and “to be compliant, cooperative and amenable and if they’re not they are often labelled difficult, resistant and obstructive.” No services had formal processes of identification, recognition, inclusion or compensation for the carer. Staff saw RITH as being advantageous for carers who could be more involved in therapy without the stress of visiting the client in hospital. The work of caregivers was described as “intimate, arduous and relentless” with all caregivers reported to provide some degree of help for the patient such as assistance with hygiene, dressing and transfers. One carer described how showering and dressing her husband was a round‐the‐clock task: “It took nearly all day because he would wet himself and I would have to change him . . . It was all I did . . . (and at night) I’m up four or five times a night rushing to get a bottle for him. . . I don’t get a lot of rest of a night time.” |
| 7 | Dubois 2001, Switzerland | Evaluate patients' satisfaction with Hospital at Home care | Early Discharge Hospital at Home for various conditions including community acquired pneumonia, intravenous anti‐biotherapy, deep venous thrombosis) (Pilot programme implemented 2 years prior) |
Service level (patients) | When patients are more severely ill, they prefer to go to hospital to avoid overburdening their caregivers and to feel more secure. To the patients’ mind, fear and extra work because of H‐Hcare have affected many informal caregivers. More than a third thought that their caregivers had to support an unusual burden, particularly when patients were confined to bed. Being solicited more often was tiring for working husbands, wives, or aged spouses—H‐Hcare was intolerable for some caregivers. When having to choose the location of their next hospital stay, most patients will take into account the inconveniences to informal caregivers before selecting H‐Hcare. However, H‐Hcare also avoided trips to the hospital, which for several respondents represented a saving of time and money. Some informal caregivers were less worried because they reasoned that if patients were at home, their illness was not so serious. A lack of intimacy related to the frequent visits of nurses and doctors were mentioned. |
| 8 | Fisher 2021, UK | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
“It’s. it’s being a burden to my wife, because she’s having to do everything for me”. (Patient) Having a stable support system of their significant others eased their rehabilitation strain and enabled effective integration of their changed roles and lifestyles. Since family members were involved by the ESD team, they could effectively support the survivor during their exercise practice in‐between the sessions and follow their progress accordingly. 'They have involved my wife, but yeah. Yeah, they said that she can walk me round the block and my wife’s quite strict. She makes sure I do my exercise' (Patient). Relying on relatives to support patients with severe disability was risky and respondents highlighted the need to consider the willingness and readiness of patients’ spouses and families to assume caring responsibilities (Staff). |
| 9 | Hitch 2020, Australia | Describe staff perceptions of the trial of an early supported discharge model of care for stroke survivors | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Implementation trial) |
Service level (staff) | Participants expressed concerns about ESD’s ability to meet family needs in early recovery, particularly as patients are returning home with higher levels of dependence; “That’s the one piece of feedback I get from every single family member, I didn’t realise how hard this was going to be and I didn’t realise what it meant to be caring for them”. (Focus Group) A possible response suggested by staff was extending the ESD model beyond patients to support family and carers, who were acknowledged as key stakeholders. |
| 10 | Jester 2003, England | Examine the experiences of informal carers looking after patients following early discharge to hospital at home | Early Discharge Hospital at Home for hip and knee replacements | Service level (caregivers) | All caregivers provided some degree of help for the patient in terms of assistance with hygiene, dressing, transfers and overall responsibility. “I find it quite tiring and hard work”. |
| 11 | Kimmel 2021, Australia | To evaluate the 3‐month pilot programme from the perspective of participants and identify themes or participant factors relating to the care received and involvement in decision‐making. This was to inform the development of bed substitution rehabilitation services in the future. | Early Discharge Hospital at Home (Subacute rehabilitation) |
Service level (patients) | Family involvement and self motivation were important to facilitate recovery: "You really need back up support as well. As in I think you need a family member or a friend to be there as well … I'm lucky, I live with my husband, so he was at home for that duration" Most participants felt that being at home was easier for their family, but many felt that they would not have managed at home without assistance from their partner/carer. |
| 12 | Ko 2023, Singapore | Explore the experiences and perceptions of patients and their caregivers admitted to a Hospital at Home programme | Combined Admission Avoidance and Early Discharge Hospital at Home, for acute conditions | Service level (patients and caregivers) | Caregivers and LARs did not have to travel to visit their loved ones in the hospitals. This was especially appreciated by those with work commitments, or with limited mobility. Also, caregivers and LARs who opted for HaH were motivated by a sense of duty, by enabling their loved ones to recover comfortably at home. The availability of caregiver support was important for HaH. Furthermore, it was common for participants to employ live‐in domestic helpers that provided additional support for HaH patients. Nonetheless, some family members did express caregiver stress and disruption of daily routine during the HaH period. All participants expressed the importance of having caregiver support during the HaH period. It was common for caregiving duties to be distributed amongst multiple family members living in the same household. In cases where caregivers did not reside in the same household, they lived within proximity. Several participants expressed caregiver stress. Some were concerned that patients were not getting 24/7 direct clinical supervision, and immediate care may be delayed in the HaH care model. Some caregivers felt that they had to take responsibility to supervise the patient: '…it is a new experience since I am not medically trained. So, there will be a situation where I don’t know what to do. So, Idon’t want to judge the situation wrongly. A bit of stress for me.' “I can’t really sleep soundly, I would also be 3/4 awake, or half asleep…Have to be a bit more wary of her." (Caregiver) Frequent in‐person visits, up to three times a day, especially early in the morning and later at night, had inconvenienced and disrupted the families’ normal routines. Working caregivers preferred to work from home while patients were admitted to HaH. This presented additional challenges of work arrangements or taking time off to be at home. Sometimes, caregivers had to use unpaid time off to care for their loved ones: “Sometimes the doctors and nurse come, then they come and talk to me… then that means my work schedule need to be adjusted, because sometimes I have meetings.” (Caregiver) "I have to apply for leave, I need to take care of her [the patient] … there is a cost. Cost in the sense that when I apply leave [for work], I got [have] no pay.” (Caregiver) However, some working caregivers found it worthwhile to juggle work and caregiving responsibilities, especially if they perceived better care for their loved ones. “So physically, although I am working. Doctor call… nurse call… I’m the one who answer…Quite a lot of the time, I have to work halfway and answer [care providers’] calls. But the fact that he [the patient] is able to be home, to be in familiar environment, that’s more important than the inconvenience that I encountered to answer questions here and during working hours.” (Caregiver) Participants with flexible working arrangements were also more likely to juggle work and caregiving responsibilities. “…at home, they [my employers] can do like zoom call for my working day, while [I am] around with her [the patient] …I can…work from home via zoom.” (Caregiver) |
| 13 | Levine 2021, USA | Elucidate and explain patient perceptions of home hospital versus traditional hospital care to better describe the different perceptions of care in both settings | Admission Avoidance Hospital at Home for a variety of acute conditions | Service level (patients) | “I really have no difficulties at all and my families is close by. I don’t want to have to lift anything heavy… Uh, my son and his wife and granddaughter are close by. My wife was close by and we have our tenants, um, because we give him a little reduced in the rent. He takes care of all the snow shovelling and gardening so we don’t worry about that.” (Patient) “I was mostly worry about the house—being clean and you know like welcoming people. Physicians and nurses in my house and they have stuff organized and neat. That was my primary concern you know worry.” (Patient) |
| 14 | Lou 2017, Denmark | Investigate how mild stroke patients and their partners experience and manage everyday life in a context of early discharge rehabilitation at home | Early Discharge Hospital at Home for stroke (mild) (Rehabilitation at home) |
Service level (patients and caregivers | Generally, the partners considered it their role to nudge, challenge and support the patient in pursuing challenges at the right time. However, the partners (especially the women) recognised that they should not become the patient’s proxy therapist or "mother". The patients emphasised and valued their partners as anchors in the flow of everyday life: someone who notices if one is losing one’s grip, who cares when days are tough and with whom one can share concerns and considerations. The couples described how they adjusted their routines and made new divisions of labour at home. For example, before her stroke, Elin was solely responsible for most of the cleaning activities at home. However, because of Elin’s poststroke fatigue, Elin and her husband Ejnar redefined their division of labour so that they did the cleaning activities together. |
| 15 | Mäkelä 2020, UK | Explore the work of patients and caregivers at the time of an acute health event, the interface with health professionals in hospital and Hospital at Home and how their experiences related to the principles that underpin comprehensive geriatrician assessments | Admission Avoidance Hospital at Home for acute medical conditions | Service level (patients and caregivers |
“It’s like sleeping with one eye open, it’s almost like sleeping with one ear open”. The home setting may be significant for patients, if combined with family availability to provide supervision. "I’ve got a good cleaner and if there’s anything I just ask her to do it, and then [a friend of my son], he lives around the corner there, they were good friends for years and years, but he’s there if I need him". (Patient) |
| 16 | Manning 2016, Wales | Explore how traditional and new models of care meet patients’ needs according to patient and staff experiences | Admission Avoidance Hospital at Home for various conditions (e.g. falls and fractures) | Service level (patients and staff) | If patients did not want to be a burden to their families, they were prepared to accept help from other services. |
| 17 | Nordin 2015, Sweden | Describe patients’ expectations of coming home very early after stroke with support and rehabilitation at home | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Clinical trial) |
Service level (patients) | “… the computer, paying bills, my son made sure I did it (made sure the numbers were entered correctly), my son helps me”. (Patient) “… I’ve got a phone so I can keep in contact with the outside world. And the neighbours, I keep in contact with them as well, if anything happens. So that’s also a bit of comfort. And my daughter’s there now too, so that’s also a comfort”. (Patient) |
| 18 | Reid 2008, England | Explore informal carers’ experiences of an intermediate care service and how it met their needs | Early Discharge Hospital at Home for conditions at risk of leading to hospital admission or residential care (Rehabilitation at home) |
Service level (caregivers) | The impact on the carer of decisions made regarding the client was, in some cases, perceived to be largely ignored. Informal carers wanted to be involved especially when the burden of care fell on them rather than statutory services. Two female informal carers spoke about being placed under pressure by hospital staff to take over their parents care: "when that physio rung up and said can she come to your house. I said well yes but she has got to have like 24 hour (care), she couldn’t get dressed, there is no way I could pick her up." (Caregiver) Female informal carers appreciated not being expected to carry out personal care tasks and being able to retain a mother/daughter relationship rather than fulfilling a carer role. |
| 19 | Rossinot 2019, France | Make an inventory of experiences of patients and family caregivers in Hospital at Home | Early Discharge Hospital at Home for a variety of conditions such as cancer, chronic disease and fracture | Service level (patients and caregivers) | “They are here to lift up our mood a little... Talk...They listen... As it isn’t always easy, it feels good to have this staff... We know them, we talk... It enables us to vent when things are not going well...” (Caregiver) The majority of patients were aware of the difficulties faced by their caregiver and felt guilty about it, which lead to suffering. In this study patients considered themselves a “burden” or a “weight”. “I can feel I am a weight for her. I think I am a very heavy weight for her.” (Patient) “It might even be harder for him than it is for me, you see? To bear my mood swings, I think it is hard. I know I am sick, it is my problem. But for him it is difficult. It feels that way.” (Patient) Caregivers reported stress, exhaustion, both physical and mental, and feeling close to a burnout. For those working full time this was especially difficulty and tiring because of their work and caregiving role such as cooking, and dealing with daily issues. “I’m a multi‐functional maid. Almost madam’s slave.” (Caregiver) “We had no hesitation on HAH. It was clear that the most satisfying solution was him coming back home.” (Caregiver) The disease impacted the relationship where caregivers worry and suffer from the sight of their suffering sick relative. But sometimes the hardships reinforce the relationship. “Sometimes we fight. He became more capricious.” (Caregiver) “He is more thoughtful, he cares more, I think. Maybe he sometimes thinks I don’t take it enough upon myself.” (Patient) |
| 20 | Sims 1997, England | (1) Evaluate within the borough the practicality and acceptability of the 'Going Home Service' to patients and to staff employed in the service and in other services on which the scheme impinges (2) Establish the impact on informal carers |
Early Discharge Hospital at Home for orthopaedic conditions (New service) |
Service level (staff) |
Staff recognised that carers may experience increased anxiety and additional burden. Prior to ESD implementation, staff thought ESD would add an additional burden… for informal caregivers. The fact that carers had no need to make hospital visits and had some respite from care whilst the Going Home Service was in place were the main advantages identified for carers. (Staff) However, a new drawback, the lack of privacy in the home that the patients encountered, was also highlighted by eight people. …and 10 [mentioned] the invasion of privacy as factors to be considered. |
| 21 | Udesen 2021, Denmark | Describe and explore patients’ and caregivers’ experiences with home treatment | Admission Avoidance Hospital at Home for acute conditions | Service level (patients and caregivers | Many of the patients expressed that they often felt like they were a burden when they had to visit their GPs or the hospital, both to their caregivers and to healthcare professionals. 'I do not like to be a burden. In this way I feel that I am less burdensome’. Hospitalisation or visiting a GP seemed to be demanding for many of the patients and their caregivers due to transfer and waiting time at the hospital or at the GP’s office: ‘It’s easier for me at home. I do not like the hospital, so it was nice to have him at home. It would be difficult for me to get out to the hospital by bus’. (Caregiver) |
| 22 | Vaartio‐Rajalin 2020, Finland | Describe Hospital at Home staff's perceptions about Hospital at Home care, including work structures, processes and outcomes | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | The patient's near‐ones feel relief when their loved ones are at home and they know they can ask us, call us… But sometimes the near‐ones don't want the patient to receive care at home, because they are so tired of their official caretaker role and prioritize a short period of free time, when the patient is taken to the ward for care. Pre‐admission to HAH: Balancing between the patient's and his/her near ones' opinions and wishes. The patient is asked during the first evaluation visit upon referral to [HAH services] how he/ she manages at home, about his/her perception about their self‐care capacity and suitability of their home for HAH. "I [as a physician] nearly always call the patient's near one when we plan HAH care, to inform and to discuss… So that the idea gets their acceptance. And the nurses from the health care centre and from the hospital usually contact the near‐ones before the patient is given a referral to HAH care, during hospital discharge." (Focus group) “We don't have work uniforms with a large health and nursing care logo, because we want to maintain the patient's privacy while going in and out from his/her house… Same with the cars, we don't announce that we are from HAH…” (Focus group) "The patient's near‐ones can also become quite tired of having us in their homes for a long period of time, it is understandable… It disturbs their private life and private sphere…Yet the patients' near‐ones were found to have mixed feelings and were perceived to feel thankful, feel content and feel relief that care was organized in the home, but could also feel burdened and experience an intrusion into their private space." (Focus group) |
| 23 | Vaartio‐Rajalin 2021, Finland | Describe how adult, non‐palliative patients and their spouses perceive person‐centredness in Hospital at Home care | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (patients and caregivers | “I work three shifts, and after an evening shift here is then ... another evening shift waiting for me, at home”. An extension of the nonprofessional family caretaker role. An extension of the role as spouse. Role as an assistant for activities of daily living. Role as the person who helps them remember. A new role as social worker. A new role as nonprofessional nurse. A new role as patient advocate. Role as “saver of taxpayer/community resources.” A process that strengthens our relationship. A process that burdens our relationship. “All this ... that I was near death ... and that she is helping me now ...it has strengthened our relationship, we now talk much more than ever before, about the things we wouldn’t have talked about otherwise ...” (Patient) The forced intimacy caused humiliation and burden on a relationship, such as when a child had to care of their parent and see them naked. |
| 24 | Wallis 2022, Australia | Explore patient and caregiver barriers and enablers and components of care that may increase acceptability of Hospital at Home | Early Discharge Hospital at Home for total hip or knee replacements (Subacute rehabilitation, multiple‐payer setting) |
Service level (patients and caregivers | Patients who received inpatient rehabilitation did not feel comfortable asking family for support, expressed concerns about their caregiver being unreliable, giving up their own activities and hobbies, or keeping them awake at night. A few female patients interviewed before surgery also thought it would be too taxing or unrealistic for their husbands to be performing household tasks from making beds, gardening, and cooking: “You’re putting an enormous amount of pressure on the people around you who have to support you. I don’t want to punish the people around me.” (Patient) |
| 25 | Wilson 2002, England | Compare Hospital at Home patient and carer satisfaction with hospital care. Explore which aspects of the two care options (Hospital at Home or hospital care) were particularly valued or caused concern. |
Admission Avoidance Hospital at Home for acute medical conditions | Service level (patients and caregivers | “They were marvellous, the home care nurses, they couldn’t have done more for him ... and they looked after me.” (Caregiver) “If I’d been in hospital I would have been worrying about my husband because of his condition. Is he all right? How can he come and see me?... You can balance the two, of him doing it or having the trauma of going back and forth to hospital.” “I look at it this way; had my wife been in hospital, I’d still be doing the jobs at home and looking after the house and I’d still have to go to the hospital to visit her and the time I’ve spent in the hospital visiting her, I could rest at home.” "See how many years we’ve been married and done everything together ... we don’t want parting till the end now, do we? ... I mean I pray every night that we’ll both die together." (Caregiver) |
Theme 4. Sustainability of Hospital at Home
Finding 1. Staff and patients expressed concern that without widespread implementation and expansion, the perceived benefits of Hospital at Home to patients and the healthcare system would be limited. Health system benefits included long‐term financial savings from avoiding unnecessary hospitalisation, bed closures or reduced length of stay, plus increased hospital capacity with reduced waiting times. However, some patients were sceptical that Hospital at Home was more about saving money, and in multiple‐payer settings costs incurred by the patient were a key factor when admitting patients to Hospital at Home. Peer institution success with Hospital at Home increased executive enthusiasm for Hospital at Home. Hospital at Home could showcase a hospital’s innovation and help sustain staff recruitment. However, staff recruitment may be more challenging in rural settings as excessive driving can affect staff satisfaction (high confidence).
Early Discharge Hospital at Home
For stroke, staff reported a reduced the length of hospital stay and enabled the closure of hospital beds (Moule 2011). While dedicated funding was preferred, service‐level staff described how the funding of Hospital at Home for people following stroke was achieved by closing a number of acute care inpatient beds (Moule 2011). Staff felt that early discharge reduced bed days, reduced risk of infections and pressure injuries, reduced demand on the emergency department, reduced costs and benefited patients (Hitch 2020). For orthopaedic conditions, hospital and home staff perceived potential gains in terms of improved availability of acute beds and financial benefits (Sims 1997). For various acute conditions, existing services below capacity considered expanding referral options to include more acute departments and GP practices (Karacaoglu 2021).
For rural sites, spending a lot of time driving affected the job satisfaction and wellbeing of staff (Fisher 2021).
For orthopaedic and neurological conditions, caregivers were sometimes cynical of early discharge being more to do with hospital beds than patients’ best interests (Dow 2007b). In a multiple‐payer setting for elective joint replacement patients, some patients and caregivers expected their insurance payments to warrant their choice of hospital care, while a few patients expressed a willingness to pay for rehabilitation at home if their insurance did not cover it (Wallis 2022).
Admission Avoidance Hospital at Home
For various medical conditions, staff considered that the purpose was to reduce hospital admissions (dehospitalisation), highlighting the importance of reducing costs arising from unnecessary hospitalisation (Andrade 2013). In a residential care facility for various conditions, patients, caregivers, directors, nursing and medical staff were unanimously in favour of widespread implementation of this service across the region (Papaioannou 2018). Leaders from multiple‐payer settings described how Hospital at Home programmes showcased a hospital’s innovation and improved equity and access for low‐income and rural patients (Gorbenko 2023). Leaders felt that COVID‐19 shifted policy maker’s opinions towards Hospital at Home, but were worried whether the service would remain funded post pandemic and wanted more data to support its cost‐effectiveness (Gorbenko 2023). Hearing of peer institution success with Hospital at Home increased executive enthusiasm for the programme (Gorbenko 2023).
Combined Admission Avoidance and Early Discharge Hospital at Home
For various conditions, patients perceived economic benefits by ensuring the right patients were treated in hospital (i.e. sicker) (Vaartio‐Rajalin 2021). Staff perceived the benefits of not needing isolation rooms, saving costs for inpatients beds, and the importance of keeping patients out of hospital due to limited capacity (Vaartio‐Rajalin 2020). Staff also commented that it was easy to employ staff for Hospital at Home due to the positive perception of the role and service, despite its physical demands (Vaartio‐Rajalin 2020). In a multiple‐payer setting with a fee for service, the cost to the patient receiving Hospital at Home was a factor (Ko 2023). Some participants believed it should not exceed their cost for receiving hospital care and some were willing to pay additional costs to receive treatment in their own home (Ko 2023).
| # |
Study (Author year, country) |
Research aim/s | Intervention and conditions treated |
Participants (Systems, service, patient/caregiver level) |
Extracted data relevant to finding |
| 1 | Andrade 2013, Brazil | Understand the organisation of the health system from the perspective of professionals that provide home care services | Admission Avoidance Hospital at Home for various acute conditions | Service level (staff) | The interviewees expressed the PAD's “place” in reduction of hospital admissions, in the dehospitalization…and the economy itself even for the SUS system. (Staff) |
| 2 | Dow 2007b, Australia | Determine how the role of the carer in rehabilitation at home programmes is constructed | Early Discharge Hospital at Home for orthopaedic and neurological conditions (Rehabilitation at home) |
Service level (caregivers and staff) | [Caregiver] described her mother’s discharge as “getting rid of her out of hospital.” (Caregiver) |
| 3 | Fisher 2021, UK | (1) Explore patients' views and experiences of Early Supported Discharge services, including how stroke survivors’ expectations and understanding of Early Supported Discharge helped them make sense of their experiences, and shaped their engagement with the service (2) Explore staff views to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with Early Supported Discharge service delivery |
Early Discharge Hospital at Home for stroke | Service level (staff, patients) Systems level (commissioners) |
In sites that covered large geographical areas with high levels of rurality, when possible, staff treated patients who were based near their homes. However, despite the steps taken to reduce the burden of travelling, many respondents from across the six sites talked about how spending a big part of their day on the road affected their work–life balance and their physical and mental well‐being. Respondents also felt that the way that the national rates for mileage and car wear and tear were calculated placed staff who travelled a lot, and especially those in lower bandings, at a disadvantage. These issues affected staff morale and led to occasional resistance to work in areas that required a lot of travelling. Team leads tried to manage the situation by having staff or subteams rotate in covering geographical patches to share the burden of travelling and promote job satisfaction. |
| 4 | Hitch 2020, Australia | Describe staff perceptions of the trial of an early supported discharge model of care for stroke survivors | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (Implementation trial) |
Service level (staff) | “It reduces bed days. . . so, that reduces risk of infections . . . risk of pressure injuries. . . demand on the ED department, just by having someone being able to move out of that bed sooner has allowed for other things to happen within the hospital.” “We’re not trying to convince them to go down an option that suits us but it doesn’t suit them. . . like a double positive, like it seems to be financially better and actually better for the clients” “The cost of providing our service is less than if they were an inpatient so that’s good for the organisation. . . money kind of talks sometimes at higher levels more than other things” |
| 5 | Gorbenko 2023, USA | Examine processes of uptake and implementation of the Acute Hospital Care at Home waiver (expansion) programme in a national sample. This included examining the barriers and facilitators of the waiver programme implementation across implementation stages and describing strategies used to address these barriers and/or best practices. | Admission Avoidance Hospital at Home | Service level (clinical leaders) | Hearing of peer institution success with HaH increased executive enthusiasm for the program. Overall, participants believed the HaH model was valuable and were enthusiastic about implementation. Participants described multiple reasons for applying for the waiver. Demonstrating HaH financial value within their institutions was a top priority for programs, and the majority of participants expected HaH to have long‐term financial benefits. Other perceived benefits included expanding hospital capacity, improving cross‐operational dialogue and collaboration among hospital staff, and putting the hospital on the forefront of healthcare innovation. “There was that big article in New York Times about [health system name], about their Hospital‐at‐Home program. People and organizations around the country at the top of the C‐suite were seeing this and hearing this and saying, ‘How come we don't have a program like this?’ [We] were like, ‘We do. We've had it for years actually’. There is just so much support from our organization that we'd never had before…” One participant discussed HaH as a “safety valve” to manage COVID‐19 related capacity issues. Participants from programs that had been trying to implement HaH before the waiver described how the pandemic shifted leadership's opinions by demonstrating the “value…and the success of providing care at home” "I think that the pandemic has put a sense of this is temporary and we're doing this just to help with capacity for COVID surge…The only time limitedness to it is whether or not CMS is going to continue to fund for their subscribers and pay for the service post pandemic." …we talking about talking to other payors…about also covering it and getting some sort of bundled payment for these services. Everybody is looking to what can increase the effectiveness of hospitalization and decrease the cost and this might. The future of the waiver was a major concern for all programs. Some reported that this uncertainty affected their ability to hire staff and convince executive leaders at their institution that it is worth investing in this program. All agreed that, were the waiver to become permanent, it would help sustain their program and “pave the way for other payors]”. Several program leaders admitted they would struggle to sustain the program if the waiver went away, while others said they would continue regardless. This perception varied across leaders even at the same institution. All participants wanted to be able to show that the HaH adds value. Several participants believed the overall cost of HaH model is lower than brick‐and‐mortar admission and is therefore financially beneficial to both payers and hospitals although they noted the need for more data to support this. |
| 6 | Karacaoglu 2021, UK | To understand staff views of implementing a Hospital at Home model in a Scottish care setting. | Early Discharge Hospital at Home for various acute conditions | Service level (staff) | An expansion consideration described was to broaden the referral pathway to include acute departments and GP practices: “It will be very slow until it feeds into the GP practices. We could take a lot of load from them if they meet us half way” (HCSW) |
| 7 | Ko 2023, Singapore | Explore the experiences and perceptions of patients and their caregivers admitted to a Hospital at Home programme | Combined Admission Avoidance and Early Discharge Hospital at Home, for acute conditions | Service level (patients and caregivers) | Participants had differing views on the cost of HaH. Some participants felt that it should not exceed those of hospital stay since 24/7 in‐person care was not provided. Others were willing to pay more for the perceived better comfort and the attention they get from the care team. Nonetheless, the cost was a key factor when enrolling for HaH, and there was a consensus that HaH should be subsidised: “I’m willing to pay more than being hospitalized in the hospital…the convenience and the attention far outweighs that [the additional cost incurred].” (Caregiver) “The main concern will be price, home care, the blood test, MRI, are we going to pay? How much is the cost? And how is the person going to pay? Cash or Medisave [government administered medical savings account]?” (Patient) |
| 8 | Moule 2011, England | Explore how the early stroke discharge team members and external stakeholders experienced the service implementation process | Early Discharge Hospital at Home for stroke (Rehabilitation at home) (New service) |
Service level (staff) Systems level | Additionally, the team reported meeting aims to reduce the length of hospital stay. It was also recognized that the team had provided care in a secondary care setting that had enabled the closure of hospital beds. There was no new funding for the project, and the nature of the funding from acute care was thought to have influenced the way the project was conceived and developed. “The financing was based on the ten hospital beds closed.” (staff) |
| 9 | Papaioannou 2018, Canada | Describe the implementation of an intravenous service and assess the perceptions of residents, family caregivers and other relevant key informants | Admission Avoidance Hospital at Home for respiratory or urinary tract conditions (A pilot delivered in 4 residential care facilities, 3 multiple‐payer, 1 single‐payer) | Service level (caregivers and staff) | All of the interview participants (100%) were in favour of widespread implementation of this service across the region. |
| 10 | Rayner 2022 | Understand what factors, including the service model, were associated with more frequent use of Residential in Reach services by nursing homes | Admission Avoidance Hospital at Home (2 'Residential in Reach' services for residential care patients) |
Service level (staff) | Participating nursing home staff reported various instances when they had to use the RiR services because they could not get timely medical assistance and RiR service participants commented they were usually substituting GP care. Some GPs will not come; most of them because they work in their clinics. Some will say, "I'll come in tomorrow," if the resident can wait. "It takes a while for the GP to come if urgent (Nursing Home EN)." Access to medical care when residents deteriorate worsened afterhours, especially at weekends and nights, as most GPs simply do not work these hours and the RiR service was unavailable. Waiting for the locum to attend a rapidly deteriorating older person after hours was a major problem. ‘We can wait up to 6 h for a locum. It is unacceptable’. (RN) Many reported that locums did not assess the resident or consult the resident's medical records before making decisions and would often simply transfer a resident to acute care against their wishes to stay in the home. |
| 11 | Sims 1997, England | (1) Evaluate within the borough the practicality and acceptability of the 'Going Home Service' to patients and to staff employed in the service and in other services on which the scheme impinges (2) Establish the impact on informal carers |
Early Discharge Hospital at Home for orthopaedic conditions (New service) |
Service level (staff) |
Both groups of staff commented on the importance of early discharge in releasing hospital bed. For the health service, there were potential gains in terms of improved availability of acute beds and financial benefits. |
| 12 | Vaartio‐Rajalin 2020, Finland | Describe Hospital at Home staff's perceptions about Hospital at Home care, including work structures, processes and outcomes | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (staff) | Hospital at home does not automatically lead to economic benefit, but it shortens the care periods… There is no need for an isolation room and isolation staff, when we take care of those patients in their own homes. And ward patient [beds] are quite expensive, there not only nursing staff is needed but nutrition, cleaning, washing…If HAH did not exist, there would be many more patients in the hospital and [the hospital doesn't] have the resources to take care of those they have now, either! (Focus group) We don't have staff turnover and very few sick leaves though this can also be physically demanding work… We all the time have people wanting to work with us in HAH, never a problem to get substitutes….it also says something about HAH…(Focus group) |
| 13 | Vaartio‐Rajalin 2021, Finland | Describe how adult, non‐palliative patients and their spouses perceive person‐centredness in Hospital at Home care | Combined Admission Avoidance and Early Discharge Hospital at Home for various acute conditions | Service level (patients, caregivers and staff) | “This is also a matter of health economics, when I can be taken care of through hospital at home, the sicker people can use the hospital beds.” (Patient). |
| 14 | Wallis 2022, Australia | Explore patient and caregiver barriers and enablers and components of care that may increase acceptability of Hospital at Home | Early Discharge Hospital at Home for total hip or knee replacements | Service level (patients and caregivers | A few patients and caregivers expected their health insurer to cover their preferred setting, were ‘not impressed’ that home services depended on their level of insurance. A few patients also felt their insurance payments warranted inpatient rehabilitation, representing a potential barrier to home‐based care. A few patients and caregivers expressed a willingness to pay for rehabilitation‐at‐home and expressed satisfaction with hospital staff who advocated on their behalf for the insurance company to fund services at home serving as potential enablers for home‐based care. |
Footnotes
AART: Aged Care Rapid Response Team; ACF: aged care facility; AD: home care; ARAS: Acute Respiratory Assessment Service; ATO: Acute Team Odense; CMS: Centers for Medicare & Medicaid Services; COPD: chronic obstructive pulmonary disease; DON: director of nursing; ED: emergency department; EHR: electronic health record; ER: emergency room; ESD: Early Supported Discharge; DECAF: Dyspnoea, Eosinopenia, Consolidation, Acidaemia and atrial Fibrillation; GP: general practitioner; HCSW: healthcare support worker; H‐Hcare: Hospital at Home care; HAD: Home Hospitalisation; HAH: Hospital at Home; HCP: healthcare professional; HINH: hospital in the nursing home; MDT: multidisciplinary team; ISMMS: Icahn School of Medicine at Mount Sinai; ICS: intermediate care service; ICU: intensive care unit; IV: intravenous; LAR: legally acceptable representatives; LTCH: long‐term care home; NGO: non‐government organisation; PAD: home care programmes; RA: rehabilitation assistant; RAC: residential aged care; RACF: residential aged care facility; RCT: randomised controlled trial; RITH: rehabilitation in the home; RN: registered nurse; RSN: respiratory specialist nurse; SSNAP: Stroke National Audit Programme; UTI: urinary tract infection
Appendix 5. ENTREQ
| Number | Item | Guide and description | Evidence in manuscript |
| 1 | Aim | State the research question the synthesis addresses. | Section: Objectives |
| 2 | Synthesis methodology | Identify the synthesis methodology or theoretical framework which underpins the synthesis and describe the rationale for choice of methodology (e.g. meta‐ethnography, thematic synthesis, critical interpretive synthesis, grounded theory synthesis, realist synthesis, meta‐aggregation, meta‐study, framework synthesis). | Section: Methods
|
| 3 | Approach to searching | Indicate whether the search was pre‐planned (comprehensive search strategies to seek all available studies) or iterative (to seek all available concepts until the theoretical saturation is achieved). | Section: Methods ‐ Search methods for identification of studies.
|
| 4 | Inclusion criteria | Specify the inclusion/exclusion criteria (e.g. in terms of population, language, year limits, type of publication, study type). | Section: Methods ‐ Selection of studies. |
| 5 | Data sources | Describe the information sources used (e.g. electronic databases (MEDLINE, EMBASE, CINAHL, PsycINFO, Econlit), grey literature databases (digital thesis, policy reports), relevant organisational websites, experts, information specialists, generic web searches (Google Scholar) hand searching, reference lists) and when the searches conducted; provide the rationale for using the data sources. | Section: Methods ‐ Search methods for identification of studies. |
| 6 | Electronic Search strategy | Describe the literature search (e.g. provide electronic search strategies with population terms, clinical or health topic terms, experiential or social phenomena related terms, filters for qualitative research, and search limits). | Section: Methods ‐ Search methods for identification of studies. Section: Appendix 2. |
| 7 | Study screening methods | Describe the process of study screening and sifting (e.g. title, abstract and full text review, number of independent reviewers who screened studies). | Section: Methods – Selection of studies. |
| 8 | Study characteristics | Present the characteristics of the included studies (e.g. year of publication, country, population, number of participants, data collection, methodology, analysis, research questions). | Section: Results – Description of included studies. Section: Characteristics of included studies. Section: Table 1 – Tidier. |
| 9 | Study selection results | Identify the number of studies screened and provide reasons for study exclusion (e.g. for comprehensive searching, provide numbers of studies screened and reasons for exclusion indicated in a figure/flowchart; for iterative searching describe reasons for study exclusion and inclusion based on modifications to the research question and/or contribution to theory development). | Section: Results ‐ Results of the search. Section: Characteristics of excluded studies. Section: Figure 2 – Flow diagram. |
| 10 | Rationale for appraisal | Describe the rationale and approach used to appraise the included studies or selected findings (e.g. assessment of conduct (validity and robustness), assessment of reporting (transparency), assessment of content and utility of the findings). | Section: Methods ‐ Assessing the methodological limitations of included studies. |
| 11 | Appraisal items | State the tools, frameworks and criteria used to appraise the studies or selected findings (e.g. Existing tools: CASP, QARI, COREQ, Mays and Pope (Tong 2012); reviewer developed tools; describe the domains assessed: research team, study design, data analysis and interpretations, reporting). | Section: Methods ‐ Assessing the methodological limitations of included studies.
|
| 12 | Appraisal process | Indicate whether the appraisal was conducted independently by more than one reviewer and if consensus was required. | Section: Methods ‐ Assessing the methodological limitations of included studies. |
| 13 | Appraisal results | Present results of the quality assessment and indicate which articles, if any, were weighted/excluded based on the assessment and give the rationale. | Section: Results ‐ Methodological limitations of the studies. Section: Table 2 ‐ Methodological limitations. No articles were weighted/excluded based on the CASP assessment as per pre‐planned protocol. |
| 14 | Data extraction | Indicate which sections of the primary studies were analysed and how were the data extracted from the primary studies? (e.g. all text under the headings “results /conclusions” were extracted electronically and entered into computer software). | Section: Methods ‐ Data extraction.
|
| 15 | Software | State the computer software used, if any. | Section: Methods ‐ Data analysis and synthesis
|
| 16 | Number of reviewers | Identify who was involved in coding and analysis. | Section: Methods ‐ Data analysis and synthesis. |
| 17 | Coding | Describe the process for coding of data (e.g. line by line coding to search for concepts). | Section: Methods ‐ Data analysis and synthesis. |
| 18 | Study comparison | Describe how comparisons were made within and across studies (e.g. subsequent studies were coded into pre‐existing concepts, and new concepts were created when deemed necessary). | Section: Methods ‐ Data analysis and synthesis.
Section: Methods – Subgroup analyses
|
| 19 | Derivation of themes | Explain whether the process of deriving the themes or constructs was inductive or deductive. | Section: Methods ‐ Data analysis and synthesis.
|
| 20 | Quotations | Provide quotations from the primary studies to illustrate themes/constructs and identify whether the quotations were participant quotations of the author’s interpretation. | Section: Review findings (text). Section: Appendix 4 – Findings tables with extracted data. |
| 21 | Synthesis output | Present rich, compelling and useful results that go beyond a summary of the primary studies (e.g. new interpretation, models of evidence, conceptual models, analytical framework, development of a new theory or construct). | Section: Figure 1, Figure 3 and 4.
|
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Andrade 2013.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Brazil (Belo Horizonte, urban) Income level: upper‐middle Services and hospitals: 'Home care program' linked to one hospital's emergency department (one of 9 programmes from 9 health districts) Payer system: single(National Health Service) |
|
| Aim | Understand the organisation of the health system from the perspective of professionals that provide home care services | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews Timing of data collection: May to June 2011 Timing of implementation: no information Data analysis: content analysis
|
|
| Participants |
Servicelevel (n = 7)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care) Description: a home care unit linked to a hospital emergency department provided care as an alternative for hospital admission. This unit represents an alternative to treat patients that are suffering from the deterioration of a clinical medical condition for which hospital admission is indicated but avoidable by means of home care. It is part of a health system that still also includes hospital admission if indicated. The service substitutes or complements existing services and is characterised as a set of actions for the promotion and protection of health, treatment of diseases and rehabilitation provided at home, in order to ensure continuity of care integrated to the Health System. Home care involves all healthcare services and represents efforts to change the organisation of health services in terms of centralising care for users in locations that are within their domain, considering that it seeks to overcome the healthcare provision model centred around hospital care, although hospitals are obviously essential in specific situations. Home care is one of the components of the Emergency Assistance Network and must be structured in a co‐ordinated manner, and integrated to the Health System. Patient eligibility: no information ‐ deterioration of a clinical medical condition Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: no information Declarations of interest: no information |
|
Barnard 2016.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Australia (Southeast Queensland, urban) Income level: high Services and hospitals: 'Hospital in the Nursing Home' linked to 3 hospitals Payer system: single |
|
| Aim | Understand the experience of directors of nursing from residential aged care either with or without the support of a hospital in the nursing home program | |
| Methods |
Sampling: purposive
Data collection: focus groups (n = 2), using semi‐structured questions Timing of data collection: no information Timing of implementation: no information Data analysis: content analysis
|
|
| Participants |
Servicelevel (n = 20)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care in residential aged care setting) Description: 3 hospitals partnered with residential aged care facilities in a care delivery model (Hospital in the Nursing Home) designed to reduce emergency transfers, decrease length of stay in emergency, increase available acute care beds, facilitate appropriate care intervention, effectively utilise existing health resources, and extend support to the residential care sector. Hospital staff attended residential aged care facilities to provide acute assessment and care for residents; and assessment of residents potentially needing emergency transfer. Hospital staff attend the aged care facilities and take a role in determining care requirements, level of required intervention and the establishment of a clinical plan. Hospital staff also provided training workshops for nursing staff from residential aged care, co‐ordinated services when residents did need to attend the emergency department, and co‐ordinated inpatient services for residents if admitted to hospital. Liaison officers (a registered nurse employed to liaise between tertiary and residential aged care facilities) act as a point contact for both the hospital and residential aged care to ensure clear communication. Patient eligibility: unclear ‐ conditions requiring acute care Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: no information Declarations of interest: no information |
|
Brody 2019.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): USA (New York, urban) Income level: high Services and hospitals: 'Hospital‐at‐Home Plus', a single home health agency linked to one hospital (Icahn School of Medicine at Mount Sinai Hospital) Payer system: multiple‐payer |
|
| Aim | Examine facilitators and barriers to implementation of Hospital at Home during first year of operation to provide others the opportunity to plan effectively for operationalisation | |
| Methods |
Sampling: purposive
Data collection
Timing of data collection: April to June 2015 Timing of implementation: November 2014 Data analysis: inductive thematic analysis
|
|
| Participants |
Servicelevel (n = 25)
Systemlevel (n = 1)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care) Description: in 2014, the Icahn School of Medicine at Mount Sinai Hospital was awarded a Health Care Innovation Award to implement Hospital at Home and an additional award to perform research on its implementation in a large academic health system. The programme included acute‐level care in the home provided as an alternative for hospital admission, plus a 30‐day postacute period of transitional care. The hospital had an existing home‐based primary care programme. The hospital initially partnered with a single home health agency. The emergency department was the most common entry point for recruiting patients; they were also accrued from observation units, outpatient offices, and the home‐based primary care programme. Because Hospital at Home blends components of inpatient and outpatient care, neither the inpatient nor outpatient electronic health record versions provided the necessary functionality, and a custom version was created on outpatient version. Implementing Hospital at Home required developing internal and external partnerships with skilled home health and aides, paramedicine and transport, lab and mobile radiology, phlebotomy, infusion pharmacy and medication delivery. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial:Federman 2018 Funding: The John A. Hartford Foundation provided the grant for the study. The implementation of HAH was funded by Centers for Medicare and Medicaid Services Innovation Award. Declarations of interest: authors declared none |
|
Cegarra‐Navarro 2010.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Spain (rural) Income level: high Services and hospitals: a 'Hospital in the Home unit' linked to 1 regional hospital Payer system: single |
|
| Aim | Examine the knowledge management practices of the hospital at home unit; present a conceptual framework for hospital at home units developed to guide learning within the context of home care services | |
| Methods |
Sampling: purposive
Data collection
Timing of data collection: March to May2009 Timing of implementation: April 1998 Data analysis: content analysis |
|
| Participants |
Servicelevel (n = 8)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care) Description: the service is based in a regional Spanish hospital with a capacity of 880 beds. Patients are visited, and intravenous drugs are administered by the Hospital at Home nursing team (4 nurses). Every patient receives a written emergency plan which explains the 24‐hour telephone backup service; this backup is provided by a Hospital at Home nurse and unit director. The Hospital at Home medical team (2 internal medicine doctors) undertake medical supervision while the patient is at home, and they undertake “ward rounds” every day. At the conclusion of treatment, the patient, who has retained the status of a hospital inpatient in every way throughout the period of Hospital at Home care, is formally discharged. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: the data from this research were taken from a research program supported by the Spanish Ministry of Education (Ref. ECO2008‐0641‐C02‐02), entitled 'Science Strategic Knowledge in the Sanitary Industry: An Application to Home Care Units'. Declarations of interest: no information |
|
Chevalier 2015.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): France (Paris, urban) Income level of country: high Services and hospitals: 'Hospitalisation at Home' (HAH) service linked to 1 hospital (urology surgery unit) Payer system: single |
|
| Aim | Understand the impacts 1 year from the implementation of a Hospital at Home service after urology outpatient surgery on professional practices in hospital at home by identifying the positive and negative impacts | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews
Timing of data collection: January to March 2014 Timing of implementation: November 2012 Data analysis: inductive thematic analysis, grounded theory
|
|
| Participants |
Servicelevel (n = 20)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (acute care) Description: a public hospital urology unit with 42 hospital beds partnered with a Hospital at Home service in France. During the first urological consultation (about 15 days before surgery), the surgeon offers the patient the service. For patients who agree, the urology secretary emailed information on patient to the Hospital at Home admission service to register the patient. A Hospital at Home nurse co‐ordinator had a telephone consultation with the patient a week before the surgery to plan the stay. On the day, the patient received outpatient surgery and returns home on the same day accompanied by a loved one. The patient returned home same day of surgery accompanied by a loved one (caregiver), and visited by a nurse on day 1 and day 2. Nurse intervention examples include withdrawal of urinary catheter depending on the colour of the urine. On the day of discharge from the service, the nurse sends by fax a summary of the treatments carried out to the surgeon. The patient has the option of calling the Hospital at Home service or urology service with 24‐hour number. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: no information Declarations of interest: reported no conflicts of interest |
|
Chouliara 2014.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (East Midlands, urban and semi‐rural) Income level: high Services and hospitals: 2 'Early Supported Discharge' services linked to separate hospitals with acute stroke units (1 city‐based and 1 semi‐rural hospital) Payer system: single |
|
| Aim | Explore the perceptions of healthcare professionals and commissioners regarding the challenges and facilitators to implementation and perceived impact of early supported discharge services | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews Timing of data collection: no information Timing of implementation: approximately 2011‐2012 (study was conducted in the first year of implementation) Data analysis: thematic analysis
|
|
| Participants |
Service level (n = 29)
Systems level (n = 6)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute care, rehabilitation) Description: 2 early supported discharge services. One service was based in the city with an acute stroke unit, specialist rehabilitation ward, plus a community stroke team for onward referrals. Another service was based in a semi‐rural town with acute stroke unit only. Patients are referred by hospital staff in the acute care stroke unit to the early supported discharge service where they are supported by a range of professionals in their recovery. All patients across both early supported discharge services received 1 to 2 visits per day for up to 6 weeks, for 7 days a week. For patient safety purposes, the Early Supported Discharge teams complete an access visit to ensure all necessary equipment is in place for the patient prior to hospital discharge. Following 6 weeks of Early Supported Discharge services, if needed, patients are referred on to appropriate community services for ongoing support and rehabilitation. Patient eligibility
Clinical team
|
|
| Notes |
Linked qualitative studies:Cobley 2013 (reports on the same service) Linked effectiveness trial: none Funding: This research was funded by the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care for Nottinghamshire, Derbyshire and Lincolnshire. Declarations of interest: authors declared none |
|
Clarke 2010.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (deprived inner‐city borough, urban) Income level: high Services and hospitals: Early Supported Discharge service linked to1 hospital Payer system: single‐payer |
|
| Aim | Explore patients’ views of an early supported discharge service for COPD | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews
Timing of data collection: January to June 2005 Timing of implementation: 2004 (after a 2‐year pilot scheme) Data analysis: thematic analysis,grounded theory, constant comparison
|
|
| Participants |
Service level (n = 23)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (acute care) Description: Hospital at Home service based at a chest clinic attached to the acute hospital. Discharge at 3.5 days (average length of stay for COPD at the time was 9.5 days). After discharge, patients were visited at home daily for 3 days by a nurse and then, as required, for up to 2 weeks. Home visits involved clinical assessment and checking that medication was being taken appropriately. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: Funding was obtained in part from the DH NHS R&D NCCRCD Programme (SJCT) and in part from the local NHS through a direct grant from the Strategic Health Authority. Declarations of interest: GW (an author) was employed by the NHS in the area during the period of the study. |
|
Cobley 2013.
| Study characteristics | ||
| Setting | Refer to included study Chouliara 2014 | |
| Aim | Explore patient and carer perceptions of early supported discharge services during the early post‐discharge phase | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews
Timing of data collection: no information Timing of implementation: approximately 2011‐2012 (study was conducted in the first year of implementation) Data analysis: thematic analysis, constant comparison
|
|
| Participants |
Service level (n = 42)
|
|
| Interventions | Refer to included study Chouliara 2014 | |
| Notes |
Linked qualitative study:Chouliara 2014 (reports on the same service) Linked effectiveness trial: none Funding: National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care for Nottinghamshire, Derbyshire and Lincolnshire. Declarations of interest: authors declared none |
|
Collins 2016.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Ireland (Galway, urban) Income level: high Services and hospitals: 'Early Supported Discharge' service linked to 1 large teaching hospital Payer system: single |
|
| Aim | Explore the experiences of early supported discharge from the perspective of stroke survivors and how participants made sense of these experiences | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews
Timing of data collection: August to December2012 (newly established service) Timing of implementation: unclear Data analysis: thematic analysis, interpretative, phenomenological
|
|
| Participants |
Service level (n = 4)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute, rehabilitation) Description: service based at a large teaching hospital. No further information Patient eligibility: stroke (no information on eligibility) Clinical team: unclear ‐ likely to include physiotherapists and occupational therapists |
|
| Notes |
Linked effectiveness trial: none Funding: no information Declarations of interest: authors declare none |
|
Crilly 2012.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Australia (Gold Coast, Queensland, urban) Income level: high Services and hospitals: 'Hospital in the Nursing Home' service linked to 1 major teaching hospital and 36 of 38 aged care facilities in the region Payer system: single |
|
| Aim | Describe and evaluate the structures and processes involved in a Hospital at Home (nursing home) programme | |
| Methods |
Sampling: purposive
Data collection
Timing of data collection: 2006 Timing of implementation: unclear ‐ initial pilot programme ran for 12 months and has continued Data analysis: content analysis
|
|
| Participants |
Service level (n = 19)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care, residential aged care) Description: based in a major public teaching hospital, with referrals from the emergency department. The service delivers acute care for aged care residents and provides advice and education to aged care staff and general practitioners. Service consists of 3 elements:
Initially, the programme operated from 08:00 to 16:30, Monday to Friday. Outside these hours, ACF residents were either admitted to a hospital ward for care continuation or admitted to the ED observation ward for HINH referral the next day. Initiated as a pilot project, the HINH programme was funded by the Queensland Aged Care Reform Unit (a publicly funded, state‐run service) for a period of 12 months. Queensland Health (the publicly funded state healthcare organisation) subsequently took over funding. As the ACF resident was receiving hospital‐type treatment in the ACF (i.e. care they otherwise would have received in hospital), the cost of HINH care was covered by the hospital (as it is funded by Queensland Health). Funding covered the costs of HINH setup: one full‐time programme manager, one mobile phone and overheads (e.g. office space and supplies). Time in kind was provided by the Hospital at Home programme director, and transport was via the HINH programme manager’s own vehicle. The Hospital at Home programme manager was a Registered Nurse with acute care and community experience (which meant no further training was required for the role). This experience led to the initial awareness of the service need and development of the HINH programme as guided by a steering committee. Steering committee members consisted of the Hospital Medical Director, a Data Support Services representative, the Nursing Director of Surgery and Critical Care, an ACF Nurse Unit Manager, a Nurse Unit Manager interested in aged care, the Deputy Director of Social Work, a GP who was the Chief Executive Officer of an after‐hours service and a GP with an interest in aged care. In the initial stages of implementation, an average day for the HINH programme manager might comprise the following: develop and organise workshops to be delivered to aged care staff and GPs, develop referral forms to be used by GPs, liaise with internal (hospital) stakeholders (e.g. ED staff, ward staff, outpatient staff) about service availability and referral process, sourcing potential clients from within the hospital, liaising with Aged Care Directors of Nursing to promote appropriate referrals from GPs, developing appropriate protocols and pathways for acute care (in collaboration with the programme director) and database development for data collection. Once the service was established, an average day for the HINH programme manager might comprise the following: daily review of clients currently admitted in the service, a review of referrals for new clients, follow‐up on these referrals (talking with GP, going to review the patient), determining appropriateness for HINH admission, developing individualised treatment plan for the patient in collaboration with patient’s GP and aged care nursing staff, providing education, medication and equipment required for patient acute care treatment for care to be delivered in the aged care facility. The Hospital at Home programme manager and programme director were actively involved in up‐skilling aged care staff by co‐leading a 2‐day workshop and liaising with aged care staff to support resident management in the ACF. Registered and Enrolled Nurses working in aged care were invited to attend a 2‐day workshop in work time. In its first year of operation, 2 such workshops were held with approximately 50 aged care staff attending per workshop. Workshop content was determined by the HINH programme manager and programme director, and overseen by content experts from the HINH steering committee. The workshops included: an introduction to and overview of the HINH service, the role of GPs and aged care staff, an overview of specific illness states (e.g. wounds, gastroenteritis), care updates (e.g. wound care, catheter care, subcutaneous infusion therapy, tracheostomy care, pain control) and special considerations (e.g. swallowing, last days of life, adult guardian, physiotherapy, cognitive failure) relevant to HINH services. Content covered in the workshop was subsequently incorporated into a DVD that was distributed to each aged care facility. The impact on workload as a result of Hospital at Home involvement by aged care staff was minimal. For each Hospital at Home patient, it would involve liaising with Hospital at Home programme manager and the resident’s GP as to the proposed care pathway and the capacity to provide and deliver some additional care in the aged care facility. The type of additional care delivered might include attending to wound dressing and observing subcutaneous fluid delivery. If required, the programme manager would provide individualised services and equipment or procedural in‐service for aged care staff receiving care of the patient when transferred from the hospital to the aged care facility. Patient eligibility: conditions requiring acute care such as respiratory, cellulitis, kidney/urinary tract, cardiac, abdominal/GI, viral/sepsis, other Clinical team
|
|
| Notes |
Linked effectiveness trial:Crilly 2010 Funding: Queensland Nursing Council and Australian Postgraduates Award Declarations of interest: no conflict of interest has been declared by the authors |
|
Cunliffe 2004.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (Nottingham, urban) Income level: high Services and hospitals: 'Early Discharge Rehabilitation Service' linked to 2 acute hospitals Payer system: single |
|
| Aim | Assess the acceptability of the service and to illuminate the relationship between process and outcome | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews Timing of data collection
Timing of implementation: 1998 (9‐month development phase before undertaking this implementation trial) Data analysis: thematic analysis, constant comparison
|
|
| Participants |
Service level (n = 31)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute, rehabilitation) Description: patients receive up to 4 visits per day, up to 7 days per week, between the hours of 8am and 10pm. Visits from the service could be for the purpose of assessment or monitoring, the provision of rehabilitation therapies, or the provision of assistance and care. The package of care could last up to 4 weeks and was tailored to individual needs. There were no doctors in the service ‐ medical care was given by the hospital team while in hospital and by the general practitioner when at home. Some patients, when assessed in hospital by the service team, were deemed not to require any further input. All standard after‐care services were available, if required. Patient eligibility (for implementation trial)
Clinical team
|
|
| Notes |
Linked effectiveness trial: effectiveness results included in the report Appendix 1 of Cunliffe 2004 included a description of study methods Funding: Nottingham Health Authority Declarations of interest: no information |
|
Dean 2007.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (Sheffield, urban) Income level: high Services and hospitals: 'Early Supported Discharge' programme linked to 1 hospital Payer system: single |
|
| Aim | Evaluate the feasibility of a prospective hazard analysis when assessing quality and safety in a COPD supported discharge care pathway | |
| Methods |
Sampling: purposive
Data collection
Timing of data collection: unclear Timing of implementation: unclear Data analysis: thematic analysis
|
|
| Participants |
Service level (n = 23)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (acute care) Description: provided specialist, hospital‐based, nursing care at home until the acute episode resolved (14‐day service), to reduce hospital length of stay Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: partial funding was provided by Sheffield Health and Social Care Research Consortium Declarations of interest: RL (author) is one of the clinicians providing the supported discharge service |
|
Dinesen 2007.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Denmark (Aalborg, urban) Income level: high Services and hospitals: 'Home hospitalisation' service linked to 1 hospital Payer system: unclear |
|
| Aim | Explore how the implementation of the concept ‘Home hospitalisation of heart patients’ by means of tele‐homecare technology influences the integration of clinical tasks across healthcare sectors
|
|
| Methods |
Sampling: purposive
Data collection
Timing of data collection: over 11 months, dates not specified Timing of implementation: unclear Data analysis: conceptual framework andinter‐organisational theory, etic and emic coding |
|
| Participants |
Service level (n = unknown as overlap of participants across the phases)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (acute care) Description: home hospitalisation service with joint responsibility between the district nurses and the hospital. The patients were admitted to the service for typically 3 days. Via a joint web‐portal, the healthcare professionals at the hospital and the district nurses could enter data via telehomecare on blood pressure, pulse, weight and INR. When the district nurse was taking an ECG recording, she could write a brief commentary about the patient's symptoms and transmit this information to the hospital. The staff at the hospital received the ECG recording in an email box. In case of emergency (anxiety, complications, etc.), the patient could at any time be re‐admitted to the hospital. Patient eligibility
Clinical team
|
|
| Notes |
Linked qualitative study:Dinesen 2008(reports on the same service) Linked effectiveness trial: none Funding: Spar Nord Fonden, Det Obelske Familiefond, Jyske Bank as well as by Aalborg University, Denmark Declarations of interest: no information |
|
Dinesen 2008.
| Study characteristics | ||
| Setting | Refer to Dinesen 2007 | |
| Aim | Understand the experiences and attitudes of patients and their spouses/partners with regard to the application of tele‐homecare technology as an option within home hospitalisation | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews and participant observation
Timing of data collection: over 11 months, dates not specified Timing of implementation: unclear Data analysis: phenomenologic hermeneutic approach
|
|
| Participants | Service level (n = 14)
|
|
| Interventions | Refer to Dinesen 2007 | |
| Notes |
Linked qualitative studies:Dinesen 2007 (reports on the same service) Linked effectiveness trial: none Funding: Spar Nord Fonden, Det Obelske Familiefond, Jyske Bank as well as by Aalborg University, Denmark Declarations of interest: no information |
|
Dismore 2019.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (North East ‐ North Shields, Ashington and Cramlington, urban and rural) Income level: high Services and hospitals: nurse‐led 'respiratory specialist service' linked to 3 hospitals Payer system: single (NHS) |
|
| Aim | Identify positive drivers and potential barriers to implementation of Hospital at Home for patients with exacerbation of COPD and low risk of death using the Dyspnoea, Eosinopenia, Consolidation, Acidaemia and atrial Fibrillation (DECAF) prognostic score and assist wider implementation | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews Timing of data collection: post‐discharge for patients and carers (dates not provided) Timing of implementation: April 2014 for 20 months (implementation trial) Data analysis: thematic‐construct analysis
|
|
| Participants |
Service level (n = 89)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (acute care) Description: the service treated patients at home supported by a nurse‐led respiratory specialist service, after a brief inpatient assessment. Patients were not regarded as sufficiently well for discharge. Patients returned home under the care of the hospital respiratory team, usually within 24 hours of admission. The treatment period ended when the respiratory specialist nurse and consultant deemed that the patient was sufficiently well for discharge to the care of the GP, typically after 5 days. Patients received once or twice daily visits from an RSN, under remote supervision from a respiratory consultant. An emergency contact number allowed patients to contact the team 24 hours a day, 7 days a week. Physiological parameters were monitored daily and blood sampling (including arterial blood gas analysis) taken as required. Oral and intravenous therapies, acute controlled oxygen therapy, physiotherapy, psychology, occupational therapy and formal social care were available at home. Patients could return home immediately provided the initial arterial pH was 7.35 or more and PaCO2 was 6 kPa or less. Patients with PaCO2 greater than 6 kPa without acidaemia could return home after one overnight stay in hospital, provided they were not deteriorating. Patients with acidaemia could return home the day that followed resolution of the acidaemia and, if initiated, once non‐invasive ventilation was complete. This ‘ABG management pathway’ was included as one of the minimisation indices. Return to hospital during HAH was not considered a readmission, but rather an increase in level of care. Patient eligibility (for trial)
Clinical team
|
|
| Notes |
Linked effectiveness trial:Echevarria 2018 Funding: NIHR Research for Patient Benefit and Northumbria Healthcare NHS Foundation Trust Teaching and Research Fellowship programmes. Declarations of interest: SCB reports grants from NIHR: Research for Patient Benefit programme, during the conduct of the study; HTA funding, grants from Philips Respironics, grants from Pzifer Open Air, personal fees from Pfizer and AztraZeneca outside the submitted work. AvW reports grants from NIHR: Research for Patient Benefit programme, during the conduct of the study. |
|
Dow 2007a.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Australia (Victoria, urban and rural) Income level: high Services and hospitals: 3 'Rehabilitation in the Home' (bed substitution) services linked to hospitals (number unknown) Payer system: single‐payer |
|
| Aim | Make recommendations to the Victorian Government on best practice in rehabilitation at home | |
| Methods |
Sampling: purposive
Data collection: individual or joint in‐depth interviews with patients and caregivers
Timing of data collection: patient and caregiver interviews conducted 3 months post discharge from service Timing of implementation: unclear (in Victoria programmes first established in 1995) Data analysis: content analysis |
|
| Participants |
Service level (n = 46+)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute care, rehabilitation) Description: bed substitution programmes that aimed to replicate hospital rehabilitation with a multidisciplinary team. Patients were most often referred from hospital‐based rehabilitation or acute wards and were often admitted on the day of discharge from hospital. Each programme provided just over 1 hour of therapy per day. The median length of stay was 25 days. A case manager’s role was to manage the administrative aspects of the client’s admission, communicate with the client’s general practitioner (in conjunction with the medical specialist) and communicate team decisions to the client and family. Decisions about admission, duration of treatment and discharge from the programme were usually made at these meetings and then communicated to the client by a designated staff member. Patient eligibility
Clinical team
|
|
| Notes |
Linked qualitative study:Dow 2007b (reports on the same service). Themes that were related solely to the 5 ambulatory care programmes that aimed to complement hospital care, and 1 hospital programme were not included in our analysis. Linked effectiveness trial: none Funding: commissioned and funded by the Victorian Department of Human Services. The studies were completed as part of one author’s doctoral study. Declarations of interest: authors declare none |
|
Dow 2007b.
| Study characteristics | ||
| Setting | Refer to Dow 2007a Services and hospitals: 1 'Rehabilitation in the Home' (bed substitution) service linked to 1 hospital (regional) |
|
| Aim | Determine how the role of the caregiver in rehabilitation at home programs is constructed | |
| Methods |
Sampling: purposive
Data collection
Timing of data collection: unclear Timing of implementation: unclear (in Victoria, programmes were first established in 1995) Data analysis: content and thematic analysis (caregiver interviews), thematic analysis (manager interviews) |
|
| Participants |
Service level (n = 47)
|
|
| Interventions | Refer to Dow 2007a | |
| Notes |
Linked qualitative study:Dow 2007a (reports on the same service) Linked effectiveness trial: none Funding: Commissioned and funded by the Victorian Department of Human Services. The studies were completed as part of one author’s doctoral study. Declarations of interest: authors declare none |
|
Dubois 2001.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Switzerland (Canton of Vaud, urban and rural) Income level: high Services and hospitals: 'Hospital at Home care' service linked to 4 hospitals (urban and regional) Payer system: multiple‐payer ‐ paper discusses how Switzerland health care is covered by public, private and out‐of‐pocket system |
|
| Aim | Evaluate patients' satisfaction with Hospital at Home care | |
| Methods |
Sampling: consecutive, convenience
Data collection
Timing of data collection: 6 weeks after receiving the service Timing of implementation: pilot programme implemented over 2 years from 1 July 1997 to 30 June 1999 Data analysis: deductive content analysis
|
|
| Participants |
Service level (n = 95)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (acute care) Description: patients were admitted to one of the participating hospitals for 1 or 2 days to undergo a medical check‐up. After presentation of the Hospital at Home care programme option to the patients, their family and their primary care physician, those who freely chose to be treated at home were transferred to the Hospital at Home care programme once written consent was obtained. Care follows a protocol drawn up by hospital physicians. Primary care physicians engaged in Hospital at Home are advised by a hospital team and they work together. Diagnosis‐specific protocols common to the participating health areas detailed the minimum care (e.g. frequency of home visits, monitoring, etc.) expected from the primary care physician and the home care team. Their application was discussed between the hospital medical and nursing team and those professionals directly involved in the care provided at the patients’ home. The length of stay inHospital at Home had to be short‐term. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: effectiveness results included in the report Funding: no information Declarations of interest: no information |
|
Fisher 2021.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (West and East Midlands, the East of England and the North of England; urban and rural) Income level: high Services and hospitals: 6 'Early Supported Discharge' services across 6 sites Payer system: single (NHS) |
|
| Aim |
|
|
| Methods |
Sampling:
Patient eligibility for interview
Staff eligibility for interview
Data collection
Timing of data collection
Timing of implementation:
Data analysis: thematic analysis (inductive and deductive)
|
|
| Participants |
Service level(n = 147)
Systems level (number not reported)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute) Description: early supported discharge (ESD) services across a large geographical area of England. The sites were labelled A–F, with site A being the most urban through to site F being the most rural. Sites A and B were hybrid services providing both an ESD service and a community rehabilitation service and some patients could be transferred from the ESD pathway to the community pathway. Sites A–C had the shortest length of stay, indicating closer adherence to the Early Supported Discharge model of an average stay of 6 weeks. Sites D–F were the most rural services. Each service had the flexibility to extend the length of stay of their patients if they deemed it appropriate. Site F ‐ It was decided that an ESD model would not work and that a broader supported discharge model taking a wider spectrum of strokes was deemed more appropriate. The variation in the way that services had been developed and configured met the needs of the local stroke pathways and geography. Models of operation were tailored to each service, with some teams taking referrals widely, including from GPs and by self‐referral, whereas other teams adhered rigidly to acute trust referrals only. There were some commonalities between the teams, including stated responsiveness times driven by national targets. Systems, processes and ways of working were configured to ensure that patients were seen within 24 hours and had a therapy assessment within 72 hours of admission to the team, although mechanisms for achieving these targets varied widely. All teams held weekly meetings and routinely collected data for audit and evaluation purposes over and above the nationally mandated data set. Patient eligibility: Eligibility criteria varied depending on the way that services were configured and were related to the wider stroke pathway, capacity and resources in the team, and the availability of other services to take patients with more severe disability. Patient length of stay varied from the recommended average of 6 weeks to 20 weeks. Clinical team: Multidisciplinary teams varied including OT, physio, speech and language therapist, assistant practitioners, clinical support workers, nurses, psychologists, social workers, dieticians, administrators, managers |
|
| Notes |
Linked effectiveness trial:Sheppard 2022 Funding: National Institute for Health Research (NIHR) Health Services Research and Delivery Declarations of interest: No potential conflict of interest was reported by the author(s). The views expressed are those of the authors and are not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. |
|
Gorbenko 2023.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): USA (all regions including Northeast, Midwest and South West, urban and rural) Income level: high Services and hospitals: study involved 14 new and pre‐existing US Hospital at Home programmes Payer system: multiple, including for‐profit status |
|
| Aim | Examine processes of uptake and implementation of the Acute Hospital Care at Home waiver (expansion) programme in a national sample using the Exploration, Preparation, Implementation, and Sustainment Framework. This included examining the barriers and facilitators of the waiver programme implementation across implementation stages and describing strategies used to address these barriers and/or best practices. | |
| Methods |
Sampling: purposive sampling to include 1 to 3 key personnel from each site
Data collection: individual and joint semi‐structured interviews via video conferencing
Timing of data collection: April to December 2021 Timing of implementation: unclear (study involved 14 new and pre‐existing US Hospital at Home programmes) Data analysis: iterative thematic coding and analysis using a combined inductive and deductive approach informed by the Exploration, Preparation, Implementation, and Sustainment Framework
|
|
| Participants |
Service level (n = 18)
Systems level (n = 0) |
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care) Description: across 14 programmes, Hospital at Home provided hospital‐level acute care in patients’ homes as an alternative for care traditionally provided in the hospital. With the waiver, the hospitals were no longer required to provide 24‐hour on‐site nursing, but programmes were otherwise required to adhere to all other hospital conditions of participant, including providing or contracting pharmacy, infusion, oxygen, transportation, food delivery, durable medical equipment, skill therapies and social work services; performing a history and physical exam in the hospital or emergency department; and making at least 1 visit by a physician or advanced care provider (remote or in‐person), and at least 2 in‐person nursing or mobile integrated health visits daily. Ten programmes had prior experience with any home‐based care (e.g. home health, home‐based medical care); 9 programmes had prior experience with Hospital at Home either before March 2020, when the COVID‐19 pandemic began (N = 5), or between March and November 2020 in response to the pandemic, but before the waiver was enacted (N = 4). As of 27 July 2022, 245 hospitals in 110 health systems in 36 states had obtained the waiver and CMS reported early positive outcomes. The waiver accelerated uptake of Hospital at Home by offering full diagnosis‐related group reimbursement through Medicare Fee‐for‐Service and non‐managed Medicaid beneficiaries. Patient eligibility: patients needed access to in‐home emergency services by personnel located within 30 minutes from their domicile Clinical team: includes (but may not be limited to) physician, advanced care provider, nursing or mobile integrated health provider, in‐home emergency services personnel |
|
| Notes |
Linked effectiveness trial: none Funding: The funding for this project was provided by The John A. Hartford Foundation. Declarations of interest: The authors have the following financial or personal conflicts to disclose: Dr. Leff serves as an adviser to Medically Home, Dispatch Health, Chartis Group, the Kenes 12 GORBENKO ET AL. Group, Patina Health, and MedZed. Dr. Leff's relationships have been reviewed and approved by Johns Hopkins University in accordance with its conflict‐of‐interest policy. Dr. Levine reports grants and co‐development from Biofourmis, a grant from IBM, and fees from the MetroHealth System. Dr. DeCherrie is a full‐time employee of Medically Home and has a voluntary appointment at the Icahn School of Medicine at Mount Sinai. Other authors have no conflicts to disclose. |
|
Hitch 2020.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Australia (Victoria, urban) Income level: high Services and hospitals: 'Early Supported Discharge' service linked to one hospital's inpatient rehabilitation ward (large teaching hospital) Payer system: single‐payer |
|
| Aim | Describe staff perceptions of the trial of an early supported discharge model of care for stroke survivors | |
| Methods |
Sampling: purposive
Data collection
Timing of data collection: 6 months after service implementation Timing of implementation: 2017 (implementation trial) Data analysis: thematic analysis using the Consolidated Framework for Implementation Research (CFIR) constructs as codes
|
|
| Participants |
Service level (n = 23)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute, rehabilitation) Description: an early supported discharge service was offered as part of services provided by a community rehabilitation team supported by a service co‐ordinator. Patients were referred by the inpatient rehabilitation ward. Care was provided for 4 weeks (up to 5 days per week), with session frequency determined by individual patient needs. Information about the new model and pathway of care was provided to all stroke survivors and caregivers, and the service team met on a weekly basis to co‐ordinate care provision. All patients with ongoing rehabilitation needs at the time of discharge from the service were referred on to community‐based rehabilitation services. Patient eligibility:
Clinical team
|
|
| Notes |
Linked effectiveness trial: effectiveness results included in the report Funding: none (declared in kind contributions from the healthcare organisation) Declarations of interest: no information |
|
Jester 2003.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (Birmingham, urban) Income level: high Services and hospitals: 'Hospital at Home' linked to 1 specialist orthopaedic hospital Payer system: unclear |
|
| Aim | Examine the experiences of informal carers looking after patients following early discharge to Hospital at Home | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews (part of mixed methods study) Timing of data collection: 6 months after service implementation Timing of implementation: unclear Data analysis: thematic analysis, quasi‐phenomenological design |
|
| Participants |
Service level (n = 21)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (acute care) Description: in a specialist orthopaedic hospital, patients were discharged early (day 4 compared to about day 12 for usual care) to the service. A member of the team met the patient at home and was visited at least once per day by either a Registered Nurse or physiotherapist whilst they remained in the scheme. The Hospital at Home team worked a 7‐day week from 08:00 to 20:00 and were contactable by mobile phone between visits. Patients and carers were advised to contact the on‐call senior nurse at the inpatient centre if they required assistance outside these hours. Medical responsibility for patients remained with the orthopaedic consultant surgeon at the inpatient area. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: effectiveness results included in the report Funding: no information Declarations of interest: no information |
|
Karacaoglu 2021.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Scotland, United Kingdom (Urban) Income level: high Services and hospitals: one service called 'Acute Care at Home' located at 1 community hospital (Aberdeen City Health and Social Care Partnership, Marischal College, Broad St, Aberdeen, UK) Payer system: single‐payer (NHS) |
|
| Aim | To understand staff views of implementing a Hospital at Home model in a Scottish care setting | |
| Methods |
Sampling: purposive
Data collection:
Timing of data collection: no information Timing of implementation: no information Data analysis: thematic analysis
|
|
| Participants |
Service level(n = 13)
Systems level (n = 0) |
|
| Interventions |
Type: Early Discharge Hospital at Home (acute) Description: The service was part of a transformation programme to redesign local services and the service predominantly utilised the early supported discharge pathway. Referrals were received from a Geriatric hospital ward and patients were typically in receipt of care for between 1 and 7 days, rather than remaining in hospital which would have occurred previously. The Acute Care at Home team provided rehabilitation support from nursing, physiotherapy and occupational therapy perspectives. The most frequently reported interventions that the AC@H team carried out included patient assessments, observations and reviews (35%), referrals and signposting to other services (24%), equipment provision (e.g. raised toilet seats, 16%) and personal care (11%). Patient eligibility: over 75 years with geriatric syndromes and either requiring assistance or managing independently with personal care and where support was required during their acute need (or following recovery from an acute condition). Clinical team: The multidisciplinary team were based in a community hospital and consisted of 1 x advanced nurse practitioner, 1 x physiotherapist, 1 x occupational therapist, 5 x health care support workers, 2 x pharmacy technicians and overseen by a team leader. Whilst the service did not have exclusive use of a physician, it received professional support and clinical guidance from a consultant geriatrician working on a discharging acute ward. |
|
| Notes |
Linked effectiveness trial: none Funding: the service was funded by Aberdeen City Health and Social Care Partnership’s Integrated Joint Board. Declarations of interest: the author declares no conflicts of interest. |
|
Kimmel 2021.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Melbourne, Australia (urban) Income level: high Services and hospitals: ‘Better at Home service’ – a 3‐month pilot service at 1 hospital (Alfred Health) Payer system: single |
|
| Aim | To evaluate the 3‐month pilot program from the perspective of participants and identify themes or participant factors relating to the care received and involvement in decision‐making. This was to inform the development of bed substitution rehabilitation services in the future. | |
| Methods |
Sampling: All participants were invited that were included in the pilot service, and 19/53 participants provided consent. Data collection: semi‐structured interviews performed by telephone where possible
Timing of data collection: 3 to 6 months following programme participation Timing of implementation: August to October 2018 Data analysis: iterative thematic analysis and grounded theory |
|
| Participants |
Service level (n = 19)
Systems level (n = 0) |
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute care) Description: The aim of the programme was to include patients who would otherwise have required an inpatient stay in subacute care. ‘Better at Home’ was commenced as a pilot to test the expansion of an existing home‐based service. The aim of this service was to improve the clinical capability and capacity of the service through the transition of admitted hospital (bed)‐based services to admitted home‐based services. The key principles included 1) home‐based rehabilitation for patients with the engagement of patient, carer and family; 2) at least daily contact from a health professional; and 3) goal‐directed, interdisciplinary and person‐centred care. The aim of the programme was to include patients who would otherwise have required an inpatient stay in subacute care, with the target patient cohort comprising those patients with orthopaedic or reconditioning needs. The model of care of Better at Home as a bed substitution model in Victoria requires that each patient receives a daily visit by a nurse and has access to therapy on an as‐needs basis. Patient eligibility:
Clinical team:
|
|
| Notes |
Linked effectiveness trial: none Funding: not reported Declarations of interest: no conflicts of interest to declare |
|
Ko 2023.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Singapore (Western Singapore, urban) Income level: high Services and hospitals: 'NUHS@Home' admitting patients from 2 tertiary public hospitals — a 1200‐bed academic health intuition and a 300‐bed general hospital Payer system: multiple ‐ as a pilot program patients who opted for Hospital at Home care had their bills completely subsidised by the hospital. Those who declined Hospital at Home would be provided standard care in the hospital, via usual hospital payment. |
|
| Aim | Explore the experiences and perceptions of patients and their caregivers admitted to a Hospital at Home programme | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews via telephone
Timing of data collection: February to August 2021 (6 weeks after discharge from Hospital at Home) Timing of implementation: not reported Data analysis: thematic analysis
|
|
| Participants |
Service level (n = 36)
Systems level (n = 0) |
|
| Interventions |
Type: Combined Early Discharge and Admission Avoidance Hospital at Home (acute care) Description: NUHS@Home is a Hospital at Home programme providing care through a multidisciplinary team, enabled by remote vital signs monitoring through a tablet and wireless blood pressure and oxygen meters. Hospital‐based clinicians collaborate with private on‐demand medical house‐call services that provided supplementary and after‐hour home visits. Patients were monitored through a biosensor adhesive vital patch for continuous heart rate and respiratory rate readings and Bluetooth‐connected blood pressure and oxygen devices. Patients were able to view these readings via a home‐placed tablet, synchronised to a clinical dashboard accessible by the care team. Patients who deteriorated were escalated to acute hospitals. Patient eligibility
Clinical team:
|
|
| Notes |
Linked effectiveness study: a prospective quasi‐experimental cohort study examining the effectiveness of a Hospital at Home programme in Singapore (Ko 2022b) Funding: evaluation grant from the Ministry of Health Office for Healthcare Transformation (MOHT) and a Health Services Research Grant from the National Medical Research Council Declarations of interest: authors declare no conflict of interest. The funder declared no commercial interest in this study and played no role in the design, analysis, interpretation of this qualitative data, or the writing of this paper. |
|
Kraut 2016.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Australia (Perth ‐ Western Australia, urban) Income level: high Services and hospitals: 'Early Supported Discharge' services linked to metropolitan hospitals (number unclear) with acute stroke and rehabilitation units Payer system: unclear |
|
| Aim | Explore factors that indicated patient suitability and likelihood for referral and utilisation of early discharge rehabilitation at home | |
| Methods |
Sampling: purposive and convenience
Data collection: individual, semi‐structured Interviews
Timing of data collection: no information Timing of implementation: no information Data analysis: inductive content analysis
|
|
| Participants |
Servicelevel (n = 29)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute, rehabilitation) Description: the service was linked to metropolitan hospitals with acute stroke and rehabilitation units. No further information. Patient eligibility: stroke (eligibility criteria not described) Clinical team
|
|
| Notes |
Linked effectiveness trial: effectiveness results included in the report Funding: no information Declarations of interest: at the time of this study the principal researcher was an employee of rehabilitation at home |
|
Kylén 2021.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Sweden (Southern region, urban) Income level: high Services and hospitals: 'Early Supported Discharge' services linked to 3 hospitals stroke units in 3 municipalities Payer system: single‐payer |
|
| Aim | Explore how the environment was integrated in rehabilitation at home from the perspective of people post‐stroke, living in Sweden | |
| Methods |
Sampling: purposive
Data collection: semi‐structured, individual interviews
Timing of data collection: August 2019 and January 2020, approximately 3 months after stroke onset Timing of implementation: no information Data analysis: inductive content analysis |
|
| Participants |
Service level (n = 17)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute, rehabilitation) Description: multidisciplinary team intervention aimed at facilitating discharge from hospital and providing stroke specialist rehabilitation at home Patient eligibility: no information Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: Formas, grant number 2015/389, the Swedish Stroke Association and Dalarna University Declarations of interest: the authors declared no conflicts of interest This study is part of a larger project (Kylén 2019) called Rehabilitation and Architecture (REARCH) aiming to increase the knowledge of how the environment can facilitate and/or hinder person‐centred rehabilitation at home. |
|
Lemelin 2007.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Canada (Ontario, urban) Income level: high Services and hospitals: 'Hospital in the Home' service linked to 1 hospital's inpatient unit and emergency department Payer system: single‐payer |
|
| Aim | Evaluate the acceptance of a Hospital at Home programme, managed and provided by nurse practitioners | |
| Methods |
Sampling: purposive Data collection: semi‐structured interviews Timing of data collection: August 2004 Timing of implementation: November 2003 to May 2005 (study period for the Hospital at Home programme) Data analysis: thematic analysis
|
|
| Participants |
Service level (n = 5)
|
|
| Interventions |
Type: Combined Early Discharge and Admission Avoidance Hospital at Home (acute care) Description: participants were recruited from the 14 bed inpatient unit of the Family Medicine Service (FMS) or directly from the emergency department.A lead programme nurse practitioner was seconded from the department of family medicine for the period of the study. Additional nurse practitioners were hired and trained for their role as home care provider. Almost exclusively, nurse practitioners provided rehabilitative and supportive care including education, co‐ordination of services and counselling. Family physicians call group provided after‐hour coverage for patients as well as backup support to nurse practitioners. Patients were referred from an inpatient unit of the Family Medicine Service (FMS) or directly from the emergency department. Immediately following each patient's transfer to the home, a nurse practitioner made a home visit, performed a physical examination and initiated care provision. The nurse practitioner continued to visit the patient daily and maintained telephone contact until discharge. The provision of care was based on the patient's care needs and was determined in consultation with the family medicine resident, attending staff physician and other health care professionals at the time of transfer to the home. Care was reviewed with the hospital medical team as required, throughout the care period. Patients were discharged from the service when the team agreed there was no further requirement for hospitalisation. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: effectiveness results included in the report Funding: J. W. McConnell Family Foundation for providing the base funding for the project & Ottawa CCAC for providing funding for the economic evaluation of the project. Declarations of interest: authors declared no conflicts of interest |
|
Leung 2016.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): France (Paris, urban) Income level: high Services and hospitals: 'Home Hospitalisation' linked to hospitals (number unclear) Payer system: unclear (assume single payer) |
|
| Aim | Identify the incentives and barriers to the involvement of general practitioners in the follow‐up of their patient in hospital at home | |
| Methods |
Sampling: purposive
Data collection: focus group, semi‐structured (2 hours) Timing of data collection: April 2015 Timing of implementation: 1991 Data analysis: thematic analysis, grounded theory
|
|
| Participants |
Service level (n = 12)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (acute care) Description: home hospitalisation, 24 hours, 7 days a week service at the patient's home, with co‐ordinated medical and paramedical care. In the absence of such a service, the patient would be hospitalised. The general practitioner (medical lead for follow‐up) had the support of the co‐ordinating physician to ensure continuity of care; where the co‐ordinating physician is at the interface of the hospital teams and general practitioner. Patient eligibility: conditions requiring acute care (no further information) Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: no information Declarations of interest: no information |
|
Levine 2021.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): USA (Boston, urban) Income level: high Services and hospitals: 'Home Hospital' linked to 2 hospitals (Brigham and Women’s Hospital ‐ an academic medical centre and Brigham and Women’s Faulkner Hospital ‐ affiliated community hospital) Payer system: multiple |
|
| Aim | Elucidate and explain patient perceptions of home hospital versus traditional hospital care to better describe the different perceptions of care in both settings | |
| Methods |
Sampling: purposive
Data collection: one‐to‐one or joint semi‐structured interviews conducted by telephone
Timing of data collection: October 2016 to March 2018 Timing of implementation: September 2016 (Implementation trial) Data analysis: thematic content analysis, constant comparison, grounded theory
|
|
| Participants |
Service level (n = 36)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care) Description: all patients received at least 1 daily visit from an attending general internist and 2 daily visits from a registered nurse (Partners HealthCare at Home), with additional visits performed as needed. Also tailored to patient need, participants could receive medical meals and the services of a home health aide, social worker, physical therapist, and/or occupational therapist. Home hospital could provide most of the acute care services expected of a traditional hospital, including respiratory therapies (e.g. oxygen), intravenous medications (Smiths Medical, St. Paul, MN), imaging studies and continuous monitoring (VitalConnect, San Jose, CA). No treatment pathways or algorithms were used. Monitoring was performed through machine‐based algorithms, and clinical staff reviewed any alarms produced by these algorithms as part of their clinical care. Participants communicated with their home hospital team via telephone, encrypted video, and encrypted short message service (Everbridge, Burlington, MA). The physician was available 24 hours a day for urgent issues and visits. Criteria for discharge were by design left to the discretion of the home hospital attending. Follow‐up after discharge was by design no different than usual care. Urgent responses could occur in less than 20 min and a return to hospital could occur on a case‐by‐case basis. Patient eligibility Inclusion criteria:
Exclusion criteria:
Clinical team
|
|
| Notes |
Linked effectiveness trial:Levine 2019 Funding: The study was supported by Brigham and Women’s Hospital President’s Fund. Declarations of interest: "none of the study’s commercial vendors participated in design, analysis, interpretation, preparation, review, or approval. Dr. Levine is a recipient of funding from Biofourmis for an investigator‐initiated study of machine learning warning scores for acutely ill patients, both traditionally and home hospitalized. Dr. Schnipper is a recipient of funding from Mallinckrodt Pharmaceuticals for an investigator‐initiated study of opioid‐related adverse drug events in post‐operative hospitalized patients. All other authors declare that they do not have a conflict of interest." |
|
Lou 2017.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Denmark (Horsens, rural) Income level: high Services and hospitals: 'Early Discharge Services' (stroke teams) established at 3 regional hospitals received referrals from 2 central hospitals with highly specialised stroke units and thrombolysis services Payer system: single |
|
| Aim | Investigate how mild stroke patients and their partners experience and manage everyday life in a context of early discharge rehabilitation at home | |
| Methods |
Sampling: purposive Data collection: individual, semi‐structured interviews
Timing of data collection: April to June 2015 Timing of implementation: 2012 Data analysis: thematic analysis
|
|
| Participants |
Service level (n = 40)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute, rehabilitation) Description: multidisciplinary service established at regional hospitals to support early discharge from acute stroke care from 2 central hospitals with highly specialised stroke units and thrombolysis services. The early discharge rehabilitation‐at‐home service delivered individualised, home‐based rehabilitation of patients with mild‐to‐moderate stroke symptoms. The stroke team visits each patient 2 to 7 days after discharge to evaluate the patient’s needs and to outline a rehabilitation plan, if needed. Based on individual assessments of each patient, the stroke team usually makes 1 to 4 visits (by a physiotherapist, occupational therapist or nurse) to the patient’s home, depending upon the patient’s needs. Those patients who need further professional rehabilitation are referred to community‐based rehabilitation services. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: Central Denmark Region’s health sciences research fund Declarations of interest: no information |
|
Manning 2016.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Wales (Cardiff, urban) Income level: high Services and hospitals: 'Early Response Service' based in a community hospital and linked to a hospital's emergency department Payer system: single |
|
| Aim | Explore how traditional and new models of care meet patients’ needs according to patient and staff experiences | |
| Methods |
Sampling: purposive
Data collection
Timing of data collection: 2011 Timing of implementation: August 2009 Data analysis: Kolcaba’s comfort theory and bio‐psycho‐social model
|
|
| Participants |
Service level (n = 20)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care) Description: an early response service was set up in a community hospital and was linked to a nearby accident and emergency department. The service was set up to prevent inappropriate hospital admissions and to facilitate discharge. The service had 6 nurses and 6 healthcare support workers. They had access to a multidisciplinary team of physiotherapists, occupational therapists, a social worker, a speech therapist and the intermediate care consultant via ‘hot clinics’ (rapid access outpatient clinics). The nurses’ role was to liaise with accident and emergency staff to offer a safe alternative to a hospital admission by looking after the patient in their own home. Patient eligibility: no information ‐ examples of patients includedfalls and fractures Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: study was undertaken as part of a professional doctorate in nursing in 2014 at a Welsh University. The author is a Florence Nightingale scholar; the foundation supports nurses with scholarships to enhance their education and practice. Declarations of interest: authors declared no conflict of interest |
|
Moule 2011.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (Bristol, urban) Income level: high Services and hospitals: 'Early Stroke Discharge' service linked to one hospital Payer system: single |
|
| Aim | Explore how the early stroke discharge team members and external stakeholders experienced the early supported discharge service implementation process | |
| Methods |
Sampling: purposive Data collection: individual, semi‐structured interviews
Timing of data collection: October 2009 and February 2010 Timing of implementation: no information (assume new service at time of interviews) Data analysis: thematic analysis |
|
| Participants |
Service level (n = 9)
Systems level (n = 1)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute, rehabilitation) Description: Early Stroke Discharge service bringing the time of discharge forward and providing a continuing rehabilitation period, commencing in hospital and continuing into the home and community Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness report:Cooke 2009 (unable to retrieve) Funding: the local Strategic Services Improvement Fund committee Declarations of interest: authors declared no conflicts of interest |
|
Mäkelä 2020.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England, Wales, Scotland and Northern Ireland (urban and semi‐rural) Income level: high Services and hospitals: 3 geriatrician‐led 'Hospital at Home' services (out of 9 participating in trial) linked to acute hospitals, including ambulance services Payer system: single |
|
| Aim | Explore the work of patients and caregivers at the time of an acute health event, the interface with health professionals in hospital and Hospital at Home and how their experiences relate to the principles that underpin comprehensive geriatrician assessments | |
| Methods |
Sampling: purposive
Data collection: individual and joint interviews, semi‐structured
Timing of data collection: June 2017 to July 2018 Timing of implementation: November 2014 to January 2020 Data analysis: content analysis guided by normalisation process theory |
|
| Participants |
Service level (n = 63)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care) Description: 3 geriatrician‐led services providing multidisciplinary healthcare at home for people who would otherwise be admitted to hospital. Included comprehensive geriatric assessment and direct access to elements of acute hospital‐based healthcare. Patient referral route is from primary care, hospital short stay acute medical assessment, the emergency room or ambulance service. They were referred to the trial by the on‐call attending physician of the hospital or one of their team members, emergency department staff or primary care physicians if recruited from home. A trained research nurse working with an attending geriatrician screened admissions to the assessment unit for potentially eligible participants. Clinical team implements treatment and management recommendations, and if required refers to other services (e.g. older peoples’ mental health services, diagnostic services, social workers, dieticians, speech and language therapy, mental health services, pharmacy support and outpatient follow‐up). Patients have access to inpatient care, general practitioners and the primary healthcare team. The use of intravenous infusions, administration of medication via a pump and 24‐hour care is available in some sites. Healthcare is provided 7 days a week, admissions are restricted to Monday to Friday in all but one site, from 0900 to early evening, and emergency medical cover is available 24 hours a day. Patient eligibility (for implementation study)
Clinical team
|
|
| Notes |
Linked effectiveness trial:Sheppard 2022 Funding: National Institute for Health Research (NIHR) Health Services Research and Delivery Declarations of interest: authors declare none |
|
Nordin 2015.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Sweden (Gothenburg, urban) Income level: high Services and hospitals: 'Very early supported discharge' service linked to 1 hospital's stroke unit (Sahlgrenska University Hospital) Payer system: single |
|
| Aim | Describe patients’ expectations of coming home very early after stroke with support and rehabilitation at home | |
| Methods |
Sampling: convenience/consecutive sampling
Data collection: Individual interviews
Timing of data collection: February 2012 to March 2014 Timing of implementation: August 2011 for patient screening (pilot study commenced in April 2010) Data analysis: content analysis
|
|
| Participants |
Service level (n = 10)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute, rehabilitation). Description: very early supported discharge service that began at the stroke unit with a meeting to make a plan for coming home. The meeting included the stroke nurse co‐ordinating the very early supported discharge service, health professionals, the patient and sometimes the next of kin participated. At this meeting, the patients’ needs and wishes were explored and their personal goals with rehabilitation were formulated and decided. If the patient and nurse have identified the need for home help service, the nurse also makes these contacts. After discharge from the stroke unit, the intervention comprised 2 to 4 visits (rehabilitation team ‐ stroke nurse, physiotherapist, occupational therapist) per week, for a maximum of 4 weeks. The patient and the team decided the time to end the intervention within this time frame. Speech and language therapy will be delivered if needed. Patient eligibility (for implementation trial)
Clinical team
|
|
| Notes |
Linked effectiveness trial:Rafsten 2019 Funding: financial support was received from the Swedish Research Council (VR 2012–3523), the Gothenburg Centre for Person‐Centred Care, the King Gustaf V’s and Queen Victoria’s Freemason Foundation, Renée Eanders foundation, the Foundation of the Swedish National Stroke Association, Hjalmar Swenson’s Research Foundation and Greta and Einar Asker’s Foundation. Declarations of interest: authors declared that they had no competing interests |
|
O'Neill 2017.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Australia (Queensland, urban) Income level: high Services and hospitals: 'Hospital Avoidance Subacute Program' based in a residential aged care facility linked to 1 hospital Payer system: unclear |
|
| Aim | Examine nursing staff perceptions regarding their management of the deteriorating resident after the introduction of a hospital avoidance programme | |
| Methods |
Sampling: purposive
Data collection: focus groups (n = 3)
Timing of data collection: conducted 14 to 15 months post implementation of service Timing of implementation: pilot programme introduced in early 2014 Data analysis: inductive thematic analysis |
|
| Participants |
Service level(n = 21)
|
|
| Interventions |
Type: Combined Early Discharge and Admission Avoidance Hospital at Home (subacute care, residential aged care) Description: hospital avoidance programme for residents in a 94‐bed nursing home to prevent unnecessary transfers to hospital, and to promote early discharge from hospital if a resident was transferred. The subacute care programme was based on a traffic light system, whereby colour‐coded parameters were established on assessment documentation to determine a change in health status which then triggered further assessment and treatment. Includes a combination of nursing staff advanced clinical skills training, advance care planning, early warning and decision‐support tools, diagnostic equipment, access to advanced healthcare individuals or teams and options for providing subacute care. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: first author received Australian Postgraduate Award Scholarship from Australian Government Department of Education and Training (project conducted in partial fulfilment of the PhD requirements). Paper sponsored by a $5000 bursary awarded from PresCare, Inc., an Australian aged care provider. Declarations of interest: none of the authors had any financial interest in this study |
|
Papaioannou 2018.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Canada (Ontario ‐ Hamilton‐Niagara region, urban) Income level: high Services and hospitals: 4 residential aged care homes 'intravenous service' linked to hospitals (number unclear) Payer system: single‐payer (1 public aged care home) and multiple‐payer (3 'for profit' aged care homes) |
|
| Aim | Describe the implementation of this in‐home IV therapy service and assess the perceptions of this service by residents, family caregivers and other relevant key informants | |
| Methods |
Sampling: purposive
Data collection: individual interviews, face‐to‐face or telephone
Timing of data collection: October 2015 to June 2016 (caregivers); July 2016 (staff) Timing of implementation: unclear, described as pilot so likely not long before qualitative study Data analysis: naturalistic enquiry inductive analysis
|
|
| Participants |
Service level (n = 16)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care, residential aged care) Description: 4 residential aged care homes developed an intravenous service for residents with respiratory or urinary tract infections. The services aimed to prevent unnecessary transfer to hospital and support timeless access to IV therapy within the aged care homes. Three of the homes did not have prior experience with in‐house intravenous therapy, and one home had very minimal experience with initiating intravenous therapy. In cases where residents were started on intravenous therapy in the emergency department, this service was an opportunity for residents to return home to complete their course of treatment rather than be admitted to hospital. Supportive resources were put in place prior to the start of the service, including evidence‐based clinical pathways for the assessment and management of urinary and respiratory tract infections, resident and family and staff education video, intravenous therapy manual, posters to explain the service to residents and families, triage support provided by a Nurse Practitioner Led Outreach Team to assist with assessment to identify residents most appropriate for this IV service, nursing training for intravenous therapy and monitoring (tubing changes, PICC dressing changes), timely access to medical supplies (intravenous pump, intravenous tubing and related supplies). Pharmacists were available to provide consultation support related to antibiotic use. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: effectiveness results included in the report Funding: study funded by the Hamilton Niagara Haldimand Brant Local Health Integration Network Emergency Services Steering Committee (ESSC). Postdoctoral fellowship support (Dr Afeez Abiola Hazzan) from The Hamilton Health Sciences Foundation for this study. Declarations of interest: authors declared that no conflicts of interest exist. Dr. O’Donnell, Ms Broadhurst, and Mr. Navare were employees of Medical Pharmacies Group Limited. |
|
Ranjbar 2015.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Sweden (Gothenburg, urban) Income level: high Services and hospitals: 'COPD Mobile Care Program' based at 1 hospital(Angered hospital) Payer system: single‐payer |
|
| Aim | Explore patients’ experiences of Sweden’s first COPD mobile care programme; and evaluate if a human rights‐based analysis could provide additional information to the patients’ experiences of the COPD mobile care programme | |
| Methods |
Sampling: convenience
Data collection: individual, semi‐structured interviews
Timing of data collection: March to April 2013 Timing of implementation: 2010 Data analysis: latent content analysis
|
|
| Participants |
Service level (n = 12)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute, rehabilitation) Description: a COPD mobile care programme at Angered hospital is an alternative to inpatient care but not equivalent to home care service or rehabilitation. The focus is to follow‐up patients in their homes after hospital admission. A team nurse visits the patient before hospital discharge, followed by home visits every second day that last about 1 hour during which the patient’s clinical and medical status, inhalation technique and respiratory technique are evaluated. The patient’s health, information on COPD, and self‐management of COPD are also discussed. If needed, nurses can also facilitate contact with dietitians, physiotherapists or occupational therapists. Nurses assess the patient by telephone on the days between home visits. The recommended length of stay in the programme is 14 days, during which patients are allowed additional visits if needed. Patients experiencing a worsening in symptoms are readmitted to the hospital. Patients are allowed to participate in the programme more than once, but participation on regular basis is not recommended. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: no funding Declarations of interest: authors declare no conflicts |
|
Rayner 2022.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Australia (Melbourne, urban) Income level: high Services and hospitals: 2 Residential in Reach services (Admission Avoidance). One was geriatrician‐led and located in outer eastern metropolitan Melbourne. One was nurse‐led and located in the inner north of metropolitan Melbourne. All nursing homes in the 2 health regions referred to the service. Payer system: single |
|
| Aim | Understand what factors, including the service model, were associated with more frequent use of Residential in Reach services by nursing homes | |
| Methods |
Sampling: purposive
Data collection: semi‐structured, in‐depth individual or small group interviews
Timing of data collection
Timing of implementation: since 2008 Data analysis: thematic analysis
|
|
| Participants |
Service level (n = 127)
Systems level (n = 0) |
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute, residential care) Description: This Residential in Reach service provides assessment and management of deterioration of acute conditions that would otherwise result in a hospital transfer, enabling residents to stay in familiar surroundings, often in line with their wishes. RiR services provide telephone advice, diagnostic testing, assessment and review, administration of intravenous fluids and antibiotics, wound, urinary catheter and percutaneous endoscopic gastrotomy tube management and palliative care. The two RiR services evaluated are part of Victorian health services and had a different model of service provision ‐ one was geriatrician‐led, the other was nurse‐led. Patient eligibility: nursing home resident who requires additional medical care Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: This research received no specific grant from any funding agency in the public, commercial, or not‐for‐ profit sectors. Declarations of interest: No conflict of interest has been declared by the author. |
|
Reid 2008.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (Halton, rural) Income level: high Services and hospitals: 'Intermediate Care Service' linked to 1 hospital and works with clients in their homes and residential aged care facilities Payer system: single‐payer |
|
| Aim | Explore informal carers’ experiences of an intermediate care service and how it met their needs | |
| Methods |
Sampling: purposive and snowball sampling
Data collection: individual, semi‐structured Interviews Timing of data collection: November 2003 to June 2005 Timing of implementation: unclear Data analysis: inductive, grounded theory and collaborative approach
|
|
| Participants |
Service level (n = 19)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute, rehabilitation, includes residential aged care) Description: short‐term rehabilitation (intermediate care service) for people who are medically stable and living at home. The service aims to avoid unnecessary hospital admission, facilitate hospital discharge, and improve levels of independence and prevent inappropriate residential or nursing home placement. Therapy, care and/or nursing care is provided to enable sufficient physical functioning and confidence to return or remain safely at home. The service uses a care management approach; and the care package documentation remains with the client to allow communication between all parties involved in the rehabilitation process. The multidisciplinary intermediate care service community team work with clients in their homes and/or in residential or nursing homes. Short‐term residential options are offered to those requiring 24‐hour care and /or high levels of dependency that cannot be managed in a home setting. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: not reported Declarations of interest: authors declared no conflicts |
|
Rossinot 2019.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): France (Paris, urban) Income level: high Services and hospitals: 'Hospital at Home' service covering 3 districts of Paris linked to 37 hospitals Payer system: single‐payer |
|
| Aim | Make an inventory of the experiences of patients and family caregivers in hospital at home | |
| Methods |
Sampling: purposive
Data collection: individual, semi‐structured interviews
Timing of data collection: March to May 2017 Timing of implementation: 1991 Data analysis: grounded theory
|
|
| Participants |
Service level (n = 19)
|
|
| Interventions |
Type: Combined Early Discharge and Admission Avoidance Hospital at Home (acute care) Description: Hospital at Homeservices implemented in 37 public hospitals located in Paris and suburbs, seeing 7 million patients yearly. Broadly, the services provide continuous and co‐ordinated medical and paramedical care that only a hospital facility can provide, in the patient’s home, for a limited period of time. The specific Hospital at Home service included adult medicine, as well as specialised obstetric and paediatric services, and a dedicated after‐hours service. Arrangements with hospitals and community‐based services are formalised by Hospital at Home and patients are transferred to the service after a medical prescription. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none No data related to obstetric and paediatric services were included in the study. Funding: study had no funding Declarations of interest: authors declared no competing interest |
|
Schofield 2006.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Scotland (Glasgow, urban) Income level: high Services and hospitals: 'Acute Respiratory Assessment Service' (nurse‐led outreach service) based in a university hospital's respiratory medicine department Payer system: single‐payer |
|
| Aim | Explore patients’ and families’ experience of care options (home/hospital) and preferences during acute uncomplicated exacerbations of COPD within an inner city area in Scotland | |
| Methods |
Sampling: purposive
Data collection: individual and joint, semi‐structured interviews (n = 30)
Timing of data collection: April 2002 to September 2003 Timing of implementation: established in the 1990s Data analysis: content analysis and analysis driven by the study objectives |
|
| Participants |
Service level (n = 40)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care) Description: an Acute Respiratory Assessment Service based in a large university hospital's department of respiratory medicine, supervised by a consultant respiratory physician and led by nurses who provided a specialist outreach service. Patients referred to the acute respiratory assessment service through personal or GP contact, or via the emergency department. After assessment in the respiratory service, patients were either treated in their home or admitted as inpatients direct to the respiratory ward. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: not reported Declarations of interest: not reported |
|
Sims 1997.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (London, urban) Income level: high Services and hospitals: 'Going Home Service' linked to 1 hospital Payer system: single |
|
| Aim | Evaluate the practicality and acceptability of the 'Going Home Service' to patients and to staff employed in the service and in other services on which the scheme impinges; and establish the impact on informal carers | |
| Methods |
Sampling: purposive Data collection: individual interviews
Timing of data collection: November 1994 to March 1995 (first interview, as the service came into operation) and approximately 10 months later (second interview, but not paired with the same participant in the first round) Timing of implementation: January 1995 Data analysis: content analysis |
|
| Participants |
Service level (n = 38)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (acute care) Description: "Early discharge scheme" generally described as providing intensive levels of medical, nursing, rehabilitative and social care within the patients’ own homes. Healthcare support workers, under the supervision of and in consultation with the health professionals on the Going Home Service, assisted in the delivery of care. Their tasks included: washing and dressing the patient; taking the patient’s temperature; helping with household tasks. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: no information Declarations of interest: no information |
|
Testa 2021.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Australia (Northern Sydney Local Health District, urban) Income level: high Services and hospitals: 'Aged Care Rapid Response Team' (Admission Avoidance) encompasses 43 local aged care facilities (3344 beds in total) and two public hospitals (a 720 bed and a 160 bed hospital) Payer system: single |
|
| Aim | Explore health professionals’ perspectives on the factors impacting Aged Care Rapid Response Team utilisation in the care of acutely unwell residential care facility residents | |
| Methods |
Sampling: purposive.
Data collection: semi‐structured interviews via Zoom video conferencing Timing of data collection: October 2020 Timing of implementation: established service. Unknown date. Data analysis: thematic analysis
|
|
| Participants |
Service level (n = 6)
Systems level (n = 0) |
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute, residential care) Description: the Aged Care Rapid Response Team supports home and RACF‐based management of older people at risk of hospitalisation, when appropriate, through the rapid delivery of outreach services to the Local Health District. The service reduces the number of avoidable emergency department presentations for older people who are acutely unwell and may provide an alternative to hospitalisation. Depending on the clinical need, the service offers virtual assessments and home visits to help people remain at home or in their Residential Aged Care Facility. Patient eligibility: older people at home or in aged care who are at risk of hospitalisation Clinical team
|
|
| Notes |
Linked effectiveness trial: none Funding: LT is supported by a Macquarie University Faculty of Medicine and Health Science Ph.D. Scholarship. Declarations of interest: The authors declared no competing interests. |
|
Udesen 2021.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Denmark (Odense, urban) Income level: high Services and hospitals: ‘Acute Team Odense’ at Odense University Hospital Payer system: single |
|
| Aim | Describe and explore patients’ and caregivers’ experiences with home treatment | |
| Methods |
Sampling: purposive
Data collection: qualitative interviews (part of mixed methods study)
Timing of data collection: 2018 to 2019 Timing of implementation: established in 2018 Data analysis: thematic analysis
|
|
| Participants |
Service level (n = 475)
Systems level (n = 0) |
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute) Description: ‘Acute Team Odense’ aim to prevent unnecessary hospitalisation and to provide treatment in the homes of adult patients (> 18 years) using fast response times and the more flexible application of competencies across sectors. Acute care teams are outpatient teams that provide acute nursing in patients’ own homes, whereas acute care units are organised as ‘acute beds’ located in care facilities. The acute care teams and units are specialised in identifying acute diseases and acute deterioration of chronic diseases as well as in performing specialised treatment previously performed at hospitals. The initiative offers a potential alternative to hospitalisation and supports a more flexible solution for patients and caregivers. The team (nurses) possesses equipment that makes new and flexible solutions in patients’ homes possible (e.g. clinical nurse assessments with paraclinical samples and intravenous therapy). To ensure continuous flow in relation to ATO’s capacity, only patients in need of short‐term treatment are discharged to ATO. ATO collaborates with GPs and municipal staff (nurses and nursing assistants), three departments at Odense University Hospital, the out‐of‐hours service and the Emergency Medical Dispatch Centre. The collaborating partners at Odense University Hospital include the Emergency Department, the Geriatric Department and the Palliative Team. The team is based in the ED to support close collaboration between sectors. Patient eligibility: to ensure continuous flow in relation to the team's capacity, only patients in need of short‐term treatment are discharged to ‘Acute Team Odense’. Clinical team: comprised of 20 nurses specialised in delivering acute nursing |
|
| Notes |
Linked effectiveness trial: none Funding: the research was supported by the Danish Health Authority (Award number: 4‐1214‐388/62) Declarations of interest: Danish Health Authority had no role in the design of the study; the data collection, analysis or interpretation; in writing the manuscript; or publication |
|
Udesen 2022.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Denmark (Odense, urban) Income level: high Services and hospitals: ‘Emergency Department‐based Acute Care Service’ based at Odense University Hospital Payer system: single |
|
| Aim | Explore different healthcare professionals’ perspectives on and experiences with the ED‐based acute care service | |
| Methods |
Sampling: purposive
Data collection: focus groups
Timing of data collection: March to April 2021 Timing of implementation: November 2020 Data analysis: thematic analysis, inductive
|
|
| Participants |
Service level (n = 28)
Systems level (n = 0) |
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute, residential care) Description: ‘Emergency department‐based acute care service’ maintained by consultants from an emergency department moving emergency care from the hospitals into nursing homes. ED‐based acute care service can be organised as an alternative to hospitalisation when the primary healthcare professionals have requested an ambulance. The new service provides acute on‐site evaluation and treatment to nursing home residents. The service is activated by the emergency dispatch centre when an ambulance is requested from a nursing home. The service operates on weekdays between 8 am and 4 pm. The first month of the implementation was a pilot period in which the service could be activated 24/7. When the service is not active, the ED consultants treat patients at the ED. Depending on the urgency of the incident, the acute care service is dispatched along with an ordinary ambulance. At the nursing homes, the ED consultants collaborate with the municipal acute care team, and they perform acute evaluation and treatment on‐site in the nursing home residents’ homes. The diagnostic and treatment modalities include point‐of‐care blood sampling, acute ultrasound investigations and intravenous treatment. Patient eligibility: nursing home residents in Odense Municipality requiring acute care Clinical team:
|
|
| Notes |
Linked effectiveness trial: none Funding: No funding reported for the specific project. SEJU is funded by grants from Østifterne, Region of Southern Denmark, Odense University Hospital and Odense Municipality. AL is funded by grants from Trygfonden. Declarations of interest: “None” reported. The donors of the grants had no role in the design of the study; the data collection, analysis, or interpretation; in writing the manuscript; or publication. |
|
Vaartio‐Rajalin 2020.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Finland (urban and rural) and England (London, urban) Income level: high Services and hospitals
Payer system: single‐payer |
|
| Aim | Describe Hospital at Home staff's perceptions about hospital at home care, including work structures, processes and outcomes | |
| Methods |
Sampling: purposive Data collection
Timing of data collection: February to May 2019 Timing of implementation: unclear (services were not newly established) Data analysis: inductive thematic content analysis |
|
| Participants |
Service level (n = 24, Finland)
Service level (n = 1, England)
|
|
| Interventions |
Finland service Type: Combined Early Discharge and Admission Avoidance Hospital at Home (acute care) Description: 3 Hospital at Home units. Two units offered Hospital at Home services during the day and evenings on weekdays and weekends in a rural setting (primary health care). One unit offered Hospital at Home services during the day, evening and overnight on weekdays and weekends in an urban setting (specialised health and nursing care). Patient eligibility:
Clinical team
England service Type: combined early discharge and admission avoidance hospital at home (acute care) Description: 1 Hospital at Home unit ‐ Guy's and St Thomas' @home service. A nurse‐led service that provides services in the London boroughs of Lambeth and Southwark. The catchment area of this service includes 2 major teaching hospitals (Guy's and St Thomas' and King's College Hospital). The Hospital at Home service was a 7‐day service operating 8am to 8pm when most visits carried out by multidisciplinary team and 8pm to 11pm the service has a limited nurse‐only team responsible for responding to urgent patient requests and the administration of intravenous medications. Referrals are taken directly from hospitals and community‐based health practitioners, including London ambulance service, district nurses and general practitioners (GPs). The service employs two clinical nurse specialists as a hospital‐based in‐reach team, and they work closely with ward and accident and emergency teams to identify patients suitable for early discharge. Patient eligibility
Clinical team
|
|
| Notes |
Linked qualitative study:Vaartio‐Rajalin 2021 (reports on the same service) Linked effectiveness trial: none Funding: Eschnerska Foundation, Turku, Finland Declarations of interest: reported as no conflicts of interest |
|
Vaartio‐Rajalin 2021.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Finland (urban and rural) Income level: high Services and hospitals
Payer system: single‐payer |
|
| Aim | Describe how adult, non‐palliative patients and their spouses perceive person‐centred Hospital at Home care | |
| Methods |
Sampling: purposive
Data collection: joint and individual telephone interviews
Timing of data collection: February to April 2019 Timing of implementation: unclear (service is not newly established) Data analysis: inductive thematic content analysis |
|
| Participants |
Service level (n = 45)
|
|
| Interventions | Refer to Vaartio‐Rajalin 2020 | |
| Notes |
Linked qualitative study: Vaartio‐Rajalin 2020 (reports on the same service) Linked effectiveness trial: none Funding: Eschnerska Foundation, Turku, Finland Declarations of interest: reported as no significant relationships with, or financial interest in, any commercial companies pertaining to this article |
|
von Koch 2000.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Sweden (Stockholm, urban) Income level: high Services and hospitals: 'Early Hospital Discharge and Continued Home Rehabilitation' based at a University Hospital (Huddinge University Hospital) Payer system: single |
|
| Aim | To describe the content and experience of a programme involving early hospital discharge and continued rehabilitation at home after stroke | |
| Methods |
Sampling: purposive Data collection: individual, semi‐structured Interviews
Timing of data collection: not reported Timing of implementation: 1993 to 1997 (implementation trial) Data analysis: thematic analysis |
|
| Participants |
Service level (n = 6)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (subacute care, rehabilitation) Description: all patients received initial care and rehabilitation in the stroke unit at the Department of Neurology. One therapist was assigned as case manager with the responsibility of co‐ordinating the early discharge procedure and the home rehabilitation programme and was the main provider of the services using the other members of the rehabilitation team on a consultative basis. The earlier hospital discharge than usual was aimed at coinciding with the patient’s attaining independence in toileting according to Katz ADL Index. The intervention had a pragmatic approach, leaving decisions of frequency of visits, choice of activities and duration of the rehabilitation programme to the discretion of the individual case manager in collaboration with the patient and the patient’s family. The team held weekly meetings for co‐ordination of the rehabilitation service. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial:Von Koch 2001 Funding: Swedish Medical Research Council; Swedish Association of the Neurologically Disabled; Swedish Stroke Association and Karolinska Institute Declarations of interest: no information |
|
Wallis 2022.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Australia (Melbourne, urban) Income level: high Services and hospitals: 'Hospital at Home' and 'Rehabilitation at Home' at 1 private hospital, with 2 acute sites Payer system: multiple |
|
| Aim | (i) Explore barriers and enablers to implementation of home‐based care, including theoretical explanations, and (ii) explore components of home‐based care that may increase its acceptability for privately insured patients | |
| Methods |
Sampling: purposive
Data collection: semi‐structured interviews, face‐to‐face or via telephone, one‐to‐one or in dyads
Timing of data collection: November 2019 to March 2020 Timing of implementation: Established. Timing not reported. Data analysis: Inductive thematic analysis
|
|
| Participants |
Service level (n = 45)
Systems level (n = 0) |
|
| Interventions |
Type: Early Discharge Hospital at Home (acute and subacute rehabilitation) Description Acute: Patients remain admitted as acute patients where they have a short acute inpatient stay (2 days) followed by daily home care from a physician, nurse and physiotherapist (all employed by the hospital) for a limited time (typically 2 to 3 days). These patients are then referred onto Rehabilitation at Home or outpatient physiotherapy following discharge. Subacute: Patients are discharged from acute care to the hospital's Rehabilitation at Home service with staff employed by the hospital or an external private home rehabilitation service. Rehabilitation at Home programmes are provided for about 4 to 6 weeks by allied health professionals and include negotiated goals aiming to optimise the patient’s functioning and quality of life, caregiver support and education. Patient eligibility: no information Clinical team Acute: physician, nurse, physiotherapist Subacute: physiotherapist, occupational therapist |
|
| Notes |
Linked effectiveness trial: none Funding: Authors received no specific funding for this work. Declarations of interest: Authors have declared no competing interests exist. |
|
Wang 2012.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): Norway (Oslo, urban) Income level: high Services and hospitals: 'Hospital at home' programme linked to 1 hospital Payer system: single |
|
| Aim | Explore COPD patients’ experiences of a limited early discharge hospital at home treatment programme | |
| Methods |
Sampling: consecutive participants in a randomised controlled trial
Data collection: individual and joint, semi‐structured Interviews
Timing of data collection: not reported Timing of implementation: dates of implementation trial not reported Data analysis: 4‐step method including: reading through whole transcripts and obtaining an overall impression; identifying themes and coding these under thematic headings; abstracting and condensing content within each thematic heading; summarising content within each thematic heading. |
|
| Participants |
Service level (n = 13)
|
|
| Interventions |
Type: Early Discharge Hospital at Home (acute care) Description: specialised hospital nurse visited the patients up to 1 hour daily over a period of 3 days after hospital discharge. As part of trial, within 36 hours the patients were allocated to the hospital at home or continued hospital treatment. The nurse evaluated the patients’ clinical status, essential clinical parameters, obtained blood samples for later analysis when needed, and assessed whether the patients could still be treated at home. The nurse could consult a pulmonologist in case of worsening of the patients’ symptoms. After the consultation, decisions were made on frequency of follow‐up, therapy changes or readmission to the hospital. Furthermore, the nurse invited the patient and his/her spouse to a dialogue, e.g. she asked how the patient felt and encouraged them to reflect on possible causes of the acute exacerbation and how to prevent it. During the 3‐day period the patients were allowed to call the hospital at any time if they were concerned about their condition, especially regarding indications for readmission. Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial: a trial investigating long‐term effects of a Hospital at Home programme was terminated after 1 year due to a slow inclusion rate. Funding: study was funded by The Research Council of Norway and the South‐Eastern Norway Regional Health Authority. Declarations of interest: authors declared they had no competing interests. |
|
Wilson 2002.
| Study characteristics | ||
| Setting |
Country (city or region, urban or rural population): England (Leicester, urban) Income level: high Services and hospitals: 'Hospital at Home Admission Avoidance Scheme' linked to agency that allocates all acute medical admissions Payer system: single‐payer |
|
| Aim | Compare Hospital at Home patient and carer satisfaction with hospital care; explore which aspects of the 2 care options (hospital at home or hospital care) were particularly valued or caused concern | |
| Methods |
Sampling: consecutive participants in a randomised controlled trial from both arms
Data collection: individual and joint, semi‐structured interviews (combined with caregivers)
Timing of data collection: not reported Timing of implementation: November 1995 to May 1996 (implementation trial) Data analysis: inductive, thematic analysis |
|
| Participants |
Service level (n = 67)
|
|
| Interventions |
Type: Admission Avoidance Hospital at Home (acute care) Description: a small, nurse‐led programme (Leicester Hospital at Home admission avoidance scheme) able to admit a maximum of 5 patients at any one time. Referrals were made by the general practitioner, who retains medical responsibility, by contacting Bed Bureau, the agency that in Leicester allocates all acute medical admissions. Bed Bureau then contacted the Hospital at Home team, who assessed the patient in the usual way. If the patient was suitable, the Hospital at Home team contacted Bed Bureau staff, who randomised patients to Hospital at Home or hospital care. Involved multidisciplinary care for 4 to 24 hours a day. Maximum length of stay was 14 days, and the hours of care provided each day ranged from four to 24 hours. Rapid access to equipment needed for home nursing, such as hospital beds, mattresses and commodes. Availability of a carer not essential (can be involved in care by negotiation if he or she wished). Patient eligibility
Clinical team
|
|
| Notes |
Linked effectiveness trial:Wilson 1999 and Wilson 2003 Funding: National Research and Development Programme, Primary‐Secondary Care Interface, NHS Executive, North Thames Declarations of interest: no information |
|
ACF: aged care facility; CMS: The Centers for Medicare & Medicaid Services; COPD: chronic obstructive pulmonary disease; ECG: electrocardiogram; ED: emergency department; ESD: Early Supported Discharge; FIM: Functional Independence Measure; GOLD: Global Initiative for Chronic Obstructive Lung Disease; GP: general practitioner; HINH: Hospital in the Nursing Home; INR: international normalised ratio; IQR: interquartile range; IV: intravenous; LAR: legally acceptable representative; MoCA: Montreal Cognitive Assessment; NHS: National Health Service (UK); OT: occupational therapy; PICC: peripherally inserted central catheter; RA: rehabilitation assistant; RAPT: Risk Assessment and Prediction Tool; SD: standard deviation; WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abildgaard Møller 2019 | Wrong intervention |
| Abrahams 1990 | Wrong design |
| Agbonyitor 2009 | Wrong intervention |
| Al‐Khashan 2011 | Wrong design |
| Alaei 2017 | Wrong intervention |
| Allen 2018 | Wrong intervention |
| Alves 2007 | Wrong intervention |
| Andrade 2013b | Wrong intervention: participants are not acute/subacute; they are not in admission avoidance or ESD situations (inputs seem to be from standard community‐based service) |
| Armstrong 2016 | Wrong intervention |
| Bai 2021 | Wrong design |
| Bamford 2011 | Wrong intervention |
| Barker 2006 | Wrong design |
| Barker 2021 | Wrong intervention |
| Barnacle‐Shaw 1998 | Wrong design |
| Bartu 1994 | Wrong design |
| Basinska 2021 | Wrong intervention |
| Basinska 2022 | Wrong intervention |
| Beech 2004 | Wrong design |
| Berg 2019 | Wrong intervention: no actual service reported |
| Bergkvist 2013 | Wrong design |
| Bergkvist 2018a | Wrong intervention: the descriptions indicate that treatment at home, following patients' haematopoietic stem cell transplantation, could be pre‐planned for selected patients as a routine service pathway (rather than as an 'early discharge service'). |
| Bergkvist 2018b | Wrong intervention ‐ see Bergkvist 2018b |
| Björkman 2010a | Wrong intervention |
| Björkman 2010b | Wrong intervention |
| Booth 2007 | Wrong intervention |
| Breier 1999 | Wrong intervention: insufficient information to know if the services met admission avoidance or ESD criteria. Also, there is insufficient information on the participants to be able to say that they had had acute or subacute presentations. |
| Burton 1998 | Wrong design |
| Cafazzo 2009 | Wrong intervention: reports on the development of a "remote patient monitoring system that facilitates the self‐care of patients undergoing nocturnal home hemodialysis" rather than examining the implementation of the HAH service itself, as required in the inclusion criteria. |
| Cameron 2022b | Wrong intervention |
| Carusone 2006a | Wrong intervention: describes a 'pathway' or guideline to standardise management of pneumonia and help prevent deterioration that might require hospitalisation, but there is no actual service, as such, attached to this. |
| Carusone 2006b | Wrong intervention ‐ refer to Carusone 2006a |
| Castro 2016 | Wrong intervention: relates to “the process of dehospitalization” (discharge) rather than Hospital at Home |
| Cegarra‐Navarro 2013 | Wrong design |
| Charron 2019 | Wrong intervention: related to day hospital admissions for transfusion procedures |
| Chee 2016 | Wrong intervention |
| Chen 2014 | Wrong intervention |
| Chen 2019 | Wrong intervention |
| Chen 2020 | Wrong intervention |
| Cherin 2020 | Wrong intervention |
| Christensen 2022 | Wrong intervention |
| Chua 2022 | Wrong intervention: this study sought stakeholder perceptions of potential Hospital at Home rather than actual defined services, as required in our selection criteria. |
| Closs 1995 | Wrong design |
| Coeugnet 2016 | Wrong design: some interview data collected but no qualitative analysis – "… the nurses verbalisations about their current emotions were transcribed and dichotomized as positive or negative emotions" (p112) |
| Cohen 2017 | Wrong intervention |
| Combes 2015 | Wrong intervention: related to dialysis down ‘in centre’ but not as admitted inpatient, i.e. in outpatient versus home |
| Conger 1995 | Wrong intervention |
| Cooper 1999 | Wrong design |
| Cox 2018 | Wrong intervention |
| de Rezende Ferreira 2021 | Wrong intervention |
| De Vliegher 2015 | Wrong intervention |
| Dempsey 2000 | Wrong design: qualitative data collection but no description of qualitative analysis |
| Donnelly 1999 | Wrong design: open‐ended questions and no no qualitative analysis methods |
| Duke 2012 | Wrong design |
| Elston 2022 | Wrong design |
| Ferguson 1989 | Wrong design |
| Fitzsimmons 2016 | Wrong intervention |
| Fried 1998 | Wrong intervention: it does not report on an actual service but instead seeks to "explore preferences for sites of care" in a more abstract and notional way, e.g. "it was difficult for some of the respondents to think abstractly about components of care" (p. 526) |
| Fried 1999 | Wrong design |
| Fried 2000 | Wrong design |
| Gache 2014 | Wrong intervention |
| Gardner 2003 | Wrong intervention: the article focused on “home infusion therapy” rather than acute admission avoidance or early supported discharge. Although it discussed this under the umbrella service “hospital in the home”, there is no description of case mix that would help with confirmation of meeting the review inclusion criteria. |
| Gorbenko 2021 | Wrong intervention |
| Guberman 2005 | Wrong intervention: some participants were receiving palliative care and data for different patient groups were not reported separately. |
| Guo 2022 | Wrong intervention |
| Gustafsson 2014 | Wrong intervention |
| Hall 2008 | Wrong intervention: evaluating patients' experiences of home and hospital chemotherapy ‐ comparing day care to home care |
| Heaney 2002 | Wrong design |
| Hoeman 1988 | Wrong intervention: discharge to home health agency (not acute or rehab admitted patients) |
| Horter 2014 | Wrong intervention |
| Hough 2020 | Wrong design |
| Huang 2022 | Wrong intervention |
| Hurley 2017 | Wrong intervention |
| Hynes 2012 | Wrong intervention: not about specific Hospital at Home service |
| Jaglal 2002 | Wrong design |
| Jang 2022 | Wrong intervention |
| Jimenez 2010 | Wrong design |
| Johannessen 2019 | Wrong intervention: describing co‐located beds that patients are managed in. Also, "patients should be stable enough to be examined and treated based on general practice methods." |
| Johnson 2001 | Wrong design |
| Juaton 2022 | Wrong intervention |
| King 2020 | Wrong design |
| Kjaerhauge Christiansen 2021 | Wrong intervention |
| Leonardsen 2018 | Wrong intervention ‐ see reason for Johannessen 2019 |
| Levine 2021b | Wrong intervention |
| Levine 2022 | Wrong design |
| Levinson 2021 | Wrong intervention |
| Lillebuen 2020 | Wrong intervention |
| Linqvist Leonardsen 2016 | Wrong intervention ‐ see reason for Johannessen 2019 |
| Luu 2021 | Wrong design |
| Marineau 2005 | Wrong intervention: intervention is telehealth rather than a Hospital at Home service where health professionals provide active acute or subacute treatment in a patient’s home, as required in the inclusion criteria. |
| Marineau 2007 | Wrong intervention ‐ see reason for Marineau 2005 |
| Martínez‐Caro 2013 | Wrong design: the authors describe undertaking surveys and then ‘another interview’ and then ‘another survey’ with hospital working groups. It is not possible to differentiate data collected using these different methods. |
| Mataure 2013 | Wrong intervention: related to the transition from inpatient hospital admission to community‐based care |
| McBride 2011 | Wrong intervention |
| Meyenfeldt 2022 | Wrong intervention |
| Misra‐Hebert 2021 | Wrong intervention |
| Montalto 1998 | Wrong design |
| Mooney 2003 | Wrong intervention |
| Murphy 2020 | Wrong design |
| Palmisano 2019 | Wrong design |
| Paryono 2022 | Wrong intervention |
| Randstrom 2014 | Wrong intervention: this sounds like 'standard' community‐based rehabilitation rather than Early Supported Discharge (e.g. refers to "exercise programmes soon after the older person’s homecoming from the hospital"). |
| Redmond 1994 | Wrong design |
| Ringsberg 2003 | Wrong intervention: this sounds like post‐discharge rehabilitation rather than Early Supported Discharge (e.g. might be in place of rehab in day units or outpatients, not just in place of hospital, as implied in the Introduction). |
| Rink 1998 | Wrong design |
| Roberts 2009 | Wrong intervention: does not report on actual service |
| Rochette 2021 | Wrong design |
| Rodgers 2019 | Wrong design |
| Rydmark Kersley 2021 | Wrong intervention |
| Sahin 2015 | Wrong design |
| Santamaria 2000 | Wrong design |
| Senillosa 2016 | Wrong design |
| Soerensen 2004 | Wrong intervention |
| Stephenson 2000 | Wrong intervention |
| Stuck 2017 | Wrong intervention: article is speculative, exploring referrers' views on home care as an alternative to admission, rather than implementation of an actual service |
| Taylor 2007 | Wrong design |
| Thorsén 2006 | Wrong design |
| van der Veen 2019 | Wrong intervention: it looks in a more general way at home‐based rehabilitation rather than specific services that can be identified as meeting the inclusion criteria (for example, could be addressing the "gap after institution‐based rehabilitation" (p. 3)). |
| Von Koch 2001 | Wrong design |
| Vrotsou 2023 | Wrong design |
| Watty 2003 | Wrong design |
| Wergeland 2022 | Wrong intervention: the service as described intends to reduce visits to the hospital (for people who could be outpatients at that stage) rather than avoiding or shortening an inpatient stay. |
| Wilson 2003 | Wrong design |
| Zakrajsek 2013 | Wrong intervention: exploring older adult care transitions from hospital to home (not Hospital at Home service) |
ESD: Early Supported Discharge; HAH: Hospital at Home
Characteristics of studies awaiting classification [ordered by study ID]
Akehurst 2017.
| Notes |
Reason: unable to retrieve full text Setting: UK Aim: What are the skills, knowledge and behaviours which staff need to work in integrated care to deliver high‐quality effective care for patients? How can current workforce development and planning approaches be improved and delivered? Methods: includes documentary analysis, semi‐structured interviews and focus groups Intervention: Early Discharge Hospital at Home ‐ a recovery at home service to facilitate early discharge and prevent re‐admission |
Dagsvik 2018.
| Notes |
Reason: unable to retrieve full text Setting: Norway Aim: to explore howworkforces from the primary healthcare services have experienced increased responsibility for somatic rehabilitation Methods: focus‐group interviews with 25 participants with professional backgrounds in nursing, healthcare practitioner, occupational therapy and physiotherapy. Analysis ‐ Systematic Text Condensation and applied Self‐determination Theory. Intervention: Early Discharge Hospital at Home (subacute or rehabilitation) |
Hayden‐Wright 2000.
| Notes |
Reason: unable to retrieve full text of thesis document Setting: UK Aim: no information Methods: no information Intervention: Admission Avoidance Hospital at Home |
O'Donovan 2019.
| Notes |
Reason: unable to retrieve full text Setting: Australia Aim: no information Methods: process mapping, root cause analysis and solutions sessions with stakeholders, as well as a semi‐structured phone interview with patients Intervention: Early Discharge Hospital at Home (acute care) The Acute Medical Ambulatory Centre was established with the goals of facilitating early discharge and preventing avoidable medical admissions. 12 months post its introduction, the service was inefficient and operating under capacity. A project aiming to improve the referral processes and increase the centre’s overall efficiency was undertaken. |
Sullivan 2022.
| Notes |
Reason: study protocol Setting: USA Aim: to systematically gather evidence from 12 Hospital at Home programmes and to develop a participatory approach to engage stakeholders, assess readiness, and develop/adapt implementation strategies and evaluation metrics Methods: qualitative interviews with key informants and document review Intervention: combined Admission Avoidance and Early Discharge Hospital at Home (acute care) The Department of Veterans Affairs Hospital at Home programme delivers patient‐centred, acute‐level hospital care at home. |
Valía‐Cotanda 2018.
| Notes |
Reason: unable to retrieve full text Setting: Spain Aim: no information Methods: no information Intervention: Admission Avoidance Hospital at Home (acute care) Includes the care of medical, social and psychological needs for older people aged 75 and above, who have been admitted to the hospital through the emergency department, and it starts after discharge from hospital to Hospital at Home. Programme aims: 1) reduce loneliness and increase social participation; 2) slow down progressive cognitive impairment. As part of the intervention, the following care pathways are designed in order to complement medical treatment and achieve the proposed aims: a motivational‐based care pathway developed by social workers. This care pathway is intended to motivate the patient to take part in the community, based on patient’s personal likes, being the ultimate goal to reduce loneliness. The planned structure for this care pathway is a monthly face‐to‐face interview and telephone follow‐up, in which the patient and the social worker check the accomplishment of a set of objectives and measures they have agreed upon. A cognitive impairment care pathway guided by psychologists. This care pathway is based on attention and memory training for those patients suffering from mild cognitive impairment. The training is delivered using a workbook including a set of exercises to train cognitive strategies. The planned structure for this care pathway is performed by a psychologist by means of a face‐to‐face interview and two telephone interviews per month. |
Yao 2022.
| Notes |
Reason: protocol Setting: USA Aim: no information Methods: a mixed‐methods study will be conducted with patients, clinicians and other staff to investigate their experience Intervention: combined Admission Avoidance and Early Discharge Hospital at Home (acute care) Mayo Clinic’s Advanced Care at Home including three hospitals in Phoenix, Arizona, Jacksonville, Florida and Eau Claire, Wisconsin. Acutely ill patients are those deemed by the emergency department or inpatient attending physicians as requiring acute inpatient care. |
Differences between protocol and review
In order to integrate findings from our qualitative evidence synthesis with findings from the Cochrane intervention reviews (Goncalves‐Bradley 2017; Edgar 2024), we organised the findings from our QES (Harden 2018) to reflect the timeline for planning and implementing Hospital at Home services, categorising factors as those that support effective implementation (Figure 3) and those that might limit effectiveness (Figure 4). No study authors were contacted for further information. We did not carry out the grey literature search using OpenGrey (www.opengrey.eu), Grey Literature Report (New York Academy of Medicine; www.greylit.org) or BASE (www.base‐search.net), or approach experts in the field for additional potentially eligible studies.
Contributions of authors
DOC, EG, JW and RB conceived the idea for the qualitative evidence synthesis. JW, JH, ET, PM and DOC contributed to study selection. JW, ET and JH assessed the methodological quality of studies. JW and ET undertook data analysis and presentation of initial themes. JW and DOC undertook Grade CERQual. JW and SS wrote the first draft of the manuscript, and DOC, JH, PM, ET, EG, GD and RB contributed to critically revising the drafts for important intellectual content. All authors approved the final version of the manuscript and agree to be accountable for its content.
Sources of support
Internal sources
-
School of Public Health & Preventive Medicine, Monash University, Australia
Jason Wallis, Denise O'Connor, Jia Xi Han and Rachelle Buchbinder draw a salary
-
NSW Health, Australia
Gary Disher draws a salary
-
London School of Hygiene and Tropical Medicine, UK
Petra Makela draws a salary
External sources
-
NHMRC Partnership Centre for Health System Sustainability, Australia
This research is conducted by Jason Wallis, Denise O'Connor, Emma Gearon and Rachelle Buchbinder (Cabrini Institute and Monash University) for the NHMRC Partnership Centre for Health System Sustainability (grant ID number: 9100002), administered by the Australian Institute of Health Innovation, Macquarie University. Along with the NHMRC, the funding partners in this research collaboration are: The Bupa Health Foundation, NSW Ministry of Health, Department of Health, WA and The University of Notre Dame Australia. Their generous support is gratefully acknowledged.
While the NHMRC, The Bupa Health Foundation, NSW Ministry of Health, Department of Health, WA and The University of Notre Dame Australia have provided in‐kind and financial support for this research, they have not reviewed the content and are not responsible for any injury, loss or damage however arising from the use of, or reliance on, the information provided herein. The published material is solely the responsibility of the authors and does not reflect the views of the NHMRC or its funding partners.
Declarations of interest
Sasha Shepperd: Co‐coordinating editor with Cochrane EPOC, but has not been involved in the editorial process of this qualitative evidence synthesis.
Jia Xi Han: Assistant Managing Editor with Cochrane EPOC, but has had no role in the editorial process of this qualitative evidence synthesis.
Evie Tripp: none known.
Gary Disher: none known.
Denise O'Connor: Editor with Cochrane EPOC and Cochrane Musculoskeletal, and director of the Australasian EPOC Satellite. All editorial decisions regarding this work were made independently by another editor.
Jason Wallis, Rachelle Buchbinder, Denise O’Connor, Emma Gearon and Petra Makela were involved in the conduct, analysis and publication of a study included in this QES. They were not involved in study eligibility decisions, data extraction, methodological assessment or GRADE‐CERQual assessments for that study.
Edited (no change to conclusions)
References
References to studies included in this review
Andrade 2013 {published data only}
- Andrade AM, Brito MJ, Silva KL, Montenegro LC, Cacador BS, Freitas LF. Organization of the health system from the perspective of home care professionals. Revista Gaúcha de Enfermagem 2013;34(2):111-7. [DOI] [PubMed] [Google Scholar]
- Andrade AM, Brito MJ, Silva KL, Von Randow RM, Montenegro LC. The home care job and its peculiarities: Impressing a new health care logic [Singularidades do trabalho na atenção domiciliar: imprimindo uma nova lógica em saúde / Peculiaridades de la atención domiciliaria: imprimiendo una nueva lógica en salud / The home care job and its peculiarities: impressing a new health care logic]. Rev. Pesqui. 2013;5(1):3383-93. [Google Scholar]
Barnard 2016 {published data only}
- Barnard A, Hou XY, Lukin B. Director of nursing experiences of a hospital in the nursing home program in South East Queensland. Collegian 2016;23(4):341-8. [PubMed] [Google Scholar]
Brody 2019 {published data only}
- Brody AA, Arbaje AI, DeCherrie LV, Federman AD, Leff B, Siu AL. Starting up a Hospital at Home program: facilitators and barriers to implementation. Journal of the American Geriatrics Society 2019;67(3):588-95. [DOI] [PubMed] [Google Scholar]
Cegarra‐Navarro 2010 {published data only}
- Cegarra-Navarro J-G, Wensley AKP, Sánchez-Polo M-T. An application of the Hospital-in-the-Home unlearning context. Social Work in Health Care 2010;49(10):895-918. [DOI] [PubMed] [Google Scholar]
- Cegarra-Navarro JG, Cepeda-Carrión G. How to implement a knowledge management program in hospital-in-the-home units. Leadership in Health Services 2010;23(1):46-56. [Google Scholar]
Chevalier 2015 {published data only}
- Chevalier LB, Marquestaut O, Lukacs B, Stampa M. Impact on professional practices of a care protocol implemented between usual hospital care and hospital at home [Impacts sur les pratiques professionnelles d’un protocolede soins mis en place entre l’hospitalisation avec hébergementet l’hospitalisation à domicile]. Sante Publique 2015;27(2):205-11. [PubMed] [Google Scholar]
Chouliara 2014 {published data only}
- Chouliara N, Fisher RJ, Kerr M, Walker MF. Implementing evidence-based stroke Early Supported Discharge services: a qualitative study of challenges, facilitators and impact. Clinical Rehabilitation 2014;28(4):370-7. [DOI] [PubMed] [Google Scholar]
Clarke 2010 {published data only}
- Clarke A, Sohanpal R, Wilson G, Taylor S. Patients' perceptions of early supported discharge for chronic obstructive pulmonary disease: a qualitative study. Quality and Safety in Health Care 2010;19(2):95-8. [DOI] [PubMed] [Google Scholar]
Cobley 2013 {published data only}
- Cobley CS, Fisher RJ, Chouliara N, Kerr M, Walker MF. A qualitative study exploring patients’ and carers’ experiences of Early Supported Discharge services after stroke. Clinical Rehabilitation 2013;27(8):750-7. [DOI] [PubMed] [Google Scholar]
Collins 2016 {published data only}
- Collins G, Breen C, Walsh T, McGrath M. An exploration of the experience of early supported discharge from the perspective of stroke survivors. International Journal of Therapy and Rehabilitation 2016;23(5):207-14. [Google Scholar]
Crilly 2012 {published data only}
- Crilly J, Chaboyer W, Wallis M. A structure and process evaluation of an Australian hospital admission avoidance programme for aged care facility residents. Journal of Advanced Nursing 2012;68(2):322-34. [DOI] [PubMed] [Google Scholar]
Cunliffe 2004 {published data only}
- Cunliffe AL, Gladman JR, Husbands SL, Miller P, Dewey M E, Harwood RH. Sooner and healthier: a randomised controlled trial and interview study of an early discharge rehabilitation service for older people. Age and Ageing 2004;33(3):246-52. [DOI] [PubMed] [Google Scholar]
Dean 2007 {published data only}
- Dean JE, Hutchinson A, Escoto KH, Lawson R. Using a multi-method, user centred, prospective hazard analysis to assess care quality and patient safety in a care pathway. BMC Health Services Research 2007;7(89):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dinesen 2007 {published data only}
- Dinesen B, Gustafsson J, Nøhr C, Andersen SK, Sejersen H, Toft E. Implementation of the concept of home hospitalisation for heart patients by means of telehomecare technology: Integration of clinical tasks. International Journal of Integrated Care 2007;7:1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dinesen 2008 {published data only}
- Dinesen B, Nøhr C, Andersen SK, Sejersen H, Toft E. Under surveillance, yet looked after: telehomecare as viewed by patients and their spouse/partners. European Journal of Cardiovascular Nursing 2008;7(3):239–46. [DOI] [PubMed] [Google Scholar]
Dismore 2019 {published data only}
- Dismore LL, Echevarria C, Wersch A, Gibson J, Bourke S. What are the positive drivers and potential barriers to implementation of hospital at home selected by low-risk DECAF score in the UK: a qualitative study embedded within a randomised controlled trial. BMJ Open 2019;9(4):e0266092019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dow 2007a {published data only}
- Dow B, Black K, Bremner F, Fearn M. A comparison of a hospital-based and two home-based rehabilitation programmes. Disability and Rehabilitation 2007;29(8):635-41. [DOI] [PubMed] [Google Scholar]
Dow 2007b {published data only}
- Dow B, McDonald J. The invisible contract: shifting care from the hospital to the home. Australian Health Review 2007;31(2):193-202. [DOI] [PubMed] [Google Scholar]
Dubois 2001 {published data only}
- Dubois A, Santos-Eggimann B. Evaluation of patients' satisfaction with hospital-at-home care. Evaluation & The Health Professions 2001;24(1):84-98. [DOI] [PubMed] [Google Scholar]
Fisher 2021 {published data only}
- Cameron TM, Koller K, Byrne A, Chouliara N, Robinson T, Langhorne P, et al. A qualitative study exploring how stroke survivors’ expectations and understanding of stroke Early Supported Discharge shaped their experience and engagement with the service. Disability & Rehabilitation 2023;45(16):2604-11. [DOI] [PubMed] [Google Scholar]
- Fisher R, Chouliara N, Byrne A, Lewis S, Langhorne P, Robinson T, et al. What is the impact of large-scale implementation of stroke Early Supported Discharge? A mixed methods realist evaluation study protocol. Implementation Science 2019;14(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher RJ, Chouliara N, Byrne A, Cameron T, Lewis S, Langhorne P, et al. Large-scale implementation of stroke early supported discharge: the WISE realist mixed-methods study. NIHR Journals Library. Health Services and Delivery Research 2021;9(22). [PubMed]
Gorbenko 2023 {published data only}
- Gorbenko K, Baim-Lance A, Franzosa E, Wurtz H, Schiller G, Masse S, et al. A national qualitative study of Hospital-at-Home implementation under the CMS Acute Hospital Care at Home waiver. Journal of the American Geriatrics Society 2023;71(1):245-58. [DOI: 10.1111/jgs.18071] [DOI] [PubMed] [Google Scholar]
Hitch 2020 {published data only}
- Hitch D, Leech K, Neale S, Malcolm A. Evaluating the implementation of an early supported discharge (ESD) program for stroke survivors: a mixed methods longitudinal case study. PLOS One 2020;15(6):e0235055. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jester 2003 {published data only}
- Jester R, Hicks C. Using cost-effectiveness analysis to compare Hospital at Homeand in-patient interventions. Part 1. Journal of Clinical Nursing 2003;12:13-9. [DOI] [PubMed] [Google Scholar]
- Jester R. Early discharge to hospital at home: should it be a matter of choice? Journal of Orthopaedic Nursing 2003;7(2):64-9. [Google Scholar]
Karacaoglu 2021 {published data only}
- Karacaoglu K, Leask, CF. Staff views of a hospital at home model implemented in a Scottish care setting. AIMS Public Health 2021;8(3):467-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kimmel 2021 {published data only}
- Kimmel LA, Burge A, Watterson D, Wolters C, Holland A, Reed M, et al. Substituting inpatient rehabilitation beds for home-based multidisciplinary rehabilitation: a qualitative study of patient perceptions. Australasian Journal on Ageing 2021;40(3):275-82. [DOI] [PubMed] [Google Scholar]
Ko 2023 {published data only}
- Ko SQ, Chua CMS, Koh SH, Lim YW, Shorey S. Experiences of patients and their caregivers admitted to a Hospital-at-Home program in Singapore: a descriptive qualitative study. Journal of General Internal Medicine 2023;38(3):691-8. [DOI: 10.1007/s11606-022-07765-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kraut 2016 {published data only}
- Kraut J, Singer B, Singer K. Clinician and client views of utilising early supported discharge services. International Journal of Therapy and Rehabilitation 2016;23(10):464-71. [Google Scholar]
Kylén 2021 {published data only}
- Kylén M, Ytterberg C, Koch L, Elf M. How is the environment integrated into post-stroke rehabilitation? A qualitative study among community-dwelling persons with stroke who receive home rehabilitation in Sweden. Health & Social Care in the Community 2021;00:1-11. [DOI] [PubMed] [Google Scholar]
Lemelin 2007 {published data only}
- Lemelin J, Hogg WE, Dahrouge S, Armstrong CD, Martin C M, Zhang W, et al. Patient, informal caregiver and care provider acceptance of a hospital in the home program in Ontario, Canada. BMC Health Services Research 2007;7:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leung 2016 {published data only}
- Leung I, Casalino E, Pateron D, Grateau G, Garandeau E, Stampa M. Participation of general practitioners in the management of their "hospital at home" patients [Participation des médecins généralistes dans les prisesen charge de leurs patients en hospitalisation à domicile]. Sante Publique 2016;28(4):499-504. [PubMed] [Google Scholar]
Levine 2021 {published data only}
- Levine DM, Pian J, Mahendrakumar K, Patel A, Saenz A, Schnipper JL. Hospital-level care at home for acutely ill adults:a qualitative evaluation of a randomized controlled trial. Journal of General Internal Medicine 2021;36(7):1965-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lou 2017 {published data only}
- Lou S, Carstensen K, Møldrup M, Shahla S, Zakharia E, Nielsen CP. Early supported discharge following mild stroke: a qualitative study of patients' and their partners' experiences of rehabilitation at home. Scandinavian Journal of Caring Sciences 2017;31(2):302-11. [DOI] [PubMed] [Google Scholar]
Mäkelä 2020 {published data only}
- Gardner M, Shepperd S, Godfrey M, Mäkelä P, Tsiachristas A, Singh-Mehta A, et al. Comprehensive geriatric assessment in hospital and hospital-at-home settings: a mixed-methods study. Health Services and Delivery Research 2019;7:1-236. [PubMed] [Google Scholar]
- Makela P, Godfrey M, Cradduck-Bamford A, Ellis G, Shepperd S. A protocol for the process evaluation of a multi-centre randomised trial to compare the effectiveness of geriatrician-led admission avoidance hospital at home versus inpatient admission. Trials 2018;19:569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mäkelä P, Stott D, Godfrey M, Ellis G, Schiff R, Shepperd S. The work of older people and their informal caregivers in managing an acute health event in a hospital at home or hospital inpatient setting. Age & Ageing 2020;49:856-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepperd S, Cradduck-Bamford A, Butler C, Ellis G, Godfrey M, Gray A, et al. A multi-centre randomised trial to compare the effectiveness of geriatrician-led admission avoidance hospital at home versus inpatient admission. Trials 2017;18:491. [DOI] [PMC free article] [PubMed] [Google Scholar]
Manning 2016 {published data only}
- Manning SN. A multiple case study of patient journeys in Wales from A&E to a hospital ward or home. British Journal of Community Nursing 2016;21(10):509-17. [DOI] [PubMed] [Google Scholar]
Moule 2011 {published data only}
- Moule P, Young P, Glogowska M, Weare J. Early Stroke Discharge Team: a participatory evaluation. International Journal of Therapy & Rehabilitation 2011;18(6):319-28. [Google Scholar]
Nordin 2015 {published data only}
- Nordin A, Sunnerhagen KS, Axelsson AB. Patients' expectations of coming home with Very Early Supported Discharge and home rehabilitation after stroke - an interview study. BMC Neurology 2015;15:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunnerhagen KS, Danielsson A, Rafsten L, Bjorkdahl A, Axelsson AB, Nordin A, et al. Gothenburg very early supported discharge study (GOTVED) NCT01622205: a block randomized trial with superiority design of very early supported discharge for patients with stroke. BMC Neurology 2013;13:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Neill 2017 {published data only}
- O'Neill BJ, Dwyer T, Reid‐Searl K, Parkinson L. Managing the deteriorating nursing home resident after the introduction of a hospital avoidance programme: a nursing perspective. Scandinavian Journal of Caring Sciences 2017;31(2):312-22. [DOI] [PubMed] [Google Scholar]
Papaioannou 2018 {published data only}
- Papaioannou A, Abiola Hazzan A, Ioannidis G, O’Donnell D, Broadhurst D, Navare H, et al. Building capacity in long-term care: Supporting homes to provide intravenous therapy. Canadian Geriatrics Journal 2018;21(4):310-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ranjbar 2015 {published data only}
- Ranjbar V, Hjalmarsson A, Ascher H, Ekberg-Jansson A. Chronic obstructive pulmonary disease mobile care: a participant-focussed and human rights-based evaluation. Health Services Management Research 2015;28(3-4):58-66. [Google Scholar]
Rayner 2022 {published data only}
- Rayner JA, Fetherstonhaugh D. What factors influence nursing home use of hospital avoidance programs? An interview study. Journal of Advanced Nursing 2022;78(2):510-22. [DOI] [PubMed] [Google Scholar]
Reid 2008 {published data only}
- Reid GA, Hulme C. The impact of intermediate care: the carer’s perspective. International Journal of Therapy and Rehabilitation 2008;15(11):500-6. [Google Scholar]
Rossinot 2019 {published data only}
- Rossinot H, Marquestaut O, Stampa M. The experience of patients and family caregivers during hospital-at-home in France. BMC Health Services Research 2019;19(1):470. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schofield 2006 {published data only}
- Schofield I, Knussen C, Tolson D. A mixed method study to compare use and experience of hospital care and a nurse-led acute respiratory assessment service offering home care to people with an acute exacerbation of chronic obstructive pulmonary disease. International Journal of Nursing Studies 2006;43(4):465-76. [DOI] [PubMed] [Google Scholar]
Sims 1997 {published data only}
- Sims J, Rink E, Walker R, Pickard L. The introduction of a hospital at home service: a staff perspective. Journal of Interprofessional Care 1997;11(2):217-24. [Google Scholar]
Testa 2021 {published data only}
- Testa L, Ryder T, Braithwaite J, Mitchell RJ. Factors impacting hospital avoidance program utilisation in the care of acutely unwell residential aged care facility residents. BMC Health Services Research 2021;12(1):599. [DOI] [PMC free article] [PubMed] [Google Scholar]
Udesen 2021 {published data only}
- Udesen SEJ, Nielsen DS, Andersen N, Ostervang C, Lassen AT. Municipal acute care teams as a flexible solution for the treatment of acutely ill patients at-home: a mixed-method study of patients' and caregivers' experiences with an acute care team. BMJ Open 2021;11(8):e049945. [DOI] [PMC free article] [PubMed] [Google Scholar]
Udesen 2022 {published data only}
- Udesen SEJ, Nielsen DS, Andersen N, Rasmussen C-H, Mikkelsen S, Braband M, et al. Healthcare professionals' experience with emergency department-based acute care performed within nursing homes. Age & Ageing 2022;51:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vaartio‐Rajalin 2020 {published data only}
- Vaartio-Rajalin H, Ngoni K, Fagerström L. Balancing between extremes—Work in hospital-at-home. Nursing Open 2020;7(1):398-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vaartio‐Rajalin 2021 {published data only}
- Vaartio-Rajalin H, Fagerström L, Santamäki-Fischer R. “They know me and my situation"— patients’ and spouses’ perceptions of person-centered care in hospital-at-home care. Holistic Nursing Practice 2021;35(6):332-43. [DOI] [PubMed] [Google Scholar]
von Koch 2000 {published data only}
- Koch L, Holmqvist LW, Wottrich AW, Tham K, Pedro-Cuesta J. Rehabilitation at home after stroke: a descriptive study of an individualized intervention. Clinical Rehabilitation 2000;14(6):574-83. [DOI] [PubMed] [Google Scholar]
- Koch L, Wottrich AW, Holmqvist LW. Rehabilitation in the home versus the hospital: the importance of context. Disabililty and Rehabilitation 1998;20(10):367-72. [DOI] [PubMed] [Google Scholar]
Wallis 2022 {published data only}
- Wallis JA, Gearon E, Naylor J, Young K, Zayontz S, Risbey P, et al. Barriers, enablers and acceptability of home-based care following elective total knee or hip replacement at a private hospital: a qualitative study of patient and caregiver perspectives. PLOS One 2022;17(8):e0273405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2012 {published data only}
- Wang Y, Haugen T, Steihaug S, Werner A. Patients with acute exacerbation of chronic obstructive pulmonary disease feel safe when treated at home: a qualitative study. BMC Pulmonary Medicine 2012;12:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2002 {published data only}
- Wilson A, Wynn A, Parker H. Patient and carer satisfaction with 'hospital at home': quantitative and qualitative results from a randomised controlled trial. British Journal of General Practice 2002;52(474):9-13. [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Abildgaard Møller 2019 {published data only}
- Abildgaard Møller L, Delmar C. The role of home nurses, tasks and responsibilities in coherence patient transitions from hospital to primary sector [Hjemmesygeplejerskers rolle, opgaver og ansvar i sammenhængende patientovergange fra hospital til primærsektor]. Nordisk Sygeplejeforskning/Nordic Nursing Research 2019;9(2):156-65. [Google Scholar]
Abrahams 1990 {published data only}
- Abrahams R, Hernandez W, Capitman J, Leutz W. Current problems and future options for Medicare's home health system: an exploratory survey of home health agencies. Pride Institute Journal of Long Term Home Health Care 1990;9(1):32-42. [PubMed] [Google Scholar]
Agbonyitor 2009 {published data only}
- Agbonyitor M. Home-based care for people living with HIV/AIDS in Plateau State, Nigeria: findings from qualitative study. Global Public Health 2009;4(3):303-12. [DOI] [PubMed] [Google Scholar]
Alaei 2017 {published data only}
- Alaei S, Alhani F, Navipour H. Role of counselling and nursing care services centres in reducing work loads of hospitals: a qualitative study. Koomesh 2017;19(2):475-83. [Google Scholar]
Al‐Khashan 2011 {published data only}
- Al-Khashan H, Mishriky A, Selim M, El Sheikh A, Binsaeed A. Home caregivers' satisfaction with the services provided by Riyadh Military Hospital's home support program. Annals of Saudi Medicine 2011;31(6):591-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Allen 2018 {published data only}
- Allen J, Hutchinson AM, Brown R, Livingston PM. User experience and care for older people transitioning from hospital to home: patients’ and carers’ perspectives. Health Expectations 2018;21(2):518-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alves 2007 {published data only}
- Alves M, Tavares Araújo M, Moreira Santana D, Loureiro Vieira D. Nurse's work in a company of Home Care from Belo Horizonte, Brazil [Trabalho do enfermeiro em uma empresa de Home Care de Belo Horizonte, Brasil]. Investigación y Educación en Enfermería 2007;25(2):96-106. [Google Scholar]
Andrade 2013b {published data only}
- Andrade AM. Structuring the health care network from the perspective of professionals, users and household care [Estruturação da rede de atenção à saúde na perspectiva de profissionais, usuários e cuidadores da atenção domiciliar]. Federal University of Minas Gerais 2013.
Armstrong 2016 {published data only}
- Armstrong JJ, Sims-Gould J, Stolee P. Allocation of rehabilitation services for older adults in the Ontario home care system. Physiotherapy Canada 2016;68(4):346-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bai 2021 {published data only}
- Bai M, Ge H, Yao N, Chen T, Wu PH. Home health care delivery models in China: an exploratory comparative study [探索中的居家医疗服务模式比较研究]. Chinese General Practice 2021;24(19):2379-84. [Google Scholar]
Bamford 2011 {published data only}
- Bamford KB, Desai M, Aruede MJ, Lawson W, Jacklin A, Franklin BD. Patients' views and experience of intravenous and oral antimicrobial therapy: room for change. Injury 2011;42(Suppl 5):S24-7. [DOI] [PubMed] [Google Scholar]
Barker 2006 {published data only}
- Barker KL, Reilly KA, Lowe CM, Beard DJ. Patient satisfaction with accelerated discharge following unilateral knee replacement. International Journal of Therapy & Rehabilitation 2006;13(6):247-53. [Google Scholar]
Barker 2021 {published data only}
- Barker RE, Brighton LJ, Maddocks M, Nolan CM, Patel S, Walsh JA, et al. Integrating home-based exercise training with a hospital at home service for patients hospitalised with acute exacerbations of copd: developing the model using accelerated experience-based co-design. International Journal of Chronic Obstructive Pulmonary Disease 2021;16:1035-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barnacle‐Shaw 1998 {published data only}
- Barnacle-Shaw J, Chapman T, Jones S. Rehabilitation at home following early discharge after hip surgery. British Journal of Therapy and Rehabilitation 1998;5(5):232-7. [Google Scholar]
Bartu 1994 {published data only}
- Bartu A, Saunders W. Domiciliary detoxification: a cost effective alternative to inpatient treatment. Australian Journal of Advanced Nursing 1994;11(4):12-8. [PubMed] [Google Scholar]
Basinska 2021 {published data only}
- Basinska K, Künzler-Heule P, Guerbaai, RA, Zúñiga F, Simon M, Wellens NIH, et al. Residents' and relatives' experiences of acute situations: a qualitative study to inform a care model. Gerontologist 2021;61(7):1041-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Basinska 2022 {published data only}
- Basinska K, Zuniga F, Simon M, De Geest S, Guerbaai RA, Wellens NIH, et al. Implementation of a complex intervention to reduce hospitalizations from nursing homes: a mixed-method evaluation of implementation processes and outcomes. BMC Geriatrics 2022;22(1):196. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beech 2004 {published data only}
- Beech R, Russell W, Little R, Sherlow-Jones S. An evaluation of a multidisciplinary team for intermediate care at home. International Journal of Integrated Care 2004;4:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berg 2019 {published data only}
- Berg U, Berg M, Rolfson O, Erichsen-Andersson A. Fast-track program of elective joint replacement in hip and knee—patients' experiences of the clinical pathway and care process. Journal of Orthopaedic Surgery & Research 2019;14:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergkvist 2013 {published data only}
- Bergkvist K, Larsen J, Johansson UB, Mattsson J, Svahn BM. Hospital care or home care after allogeneic hematopoietic stem cell transplantation--patients' experiences of care and support. European Journal of Oncology Nursing 2013;17(4):389-95. [DOI] [PubMed] [Google Scholar]
Bergkvist 2018a {published data only}
- Bergkvist K, Larsen J, Johansson U-B, Mattsson J, Fossum B. Family members’ life situation and experiences of different caring organisations during allogeneic haematopoietic stem cells transplantation—a qualitative study. European Journal of Cancer Care 2018;27(1):e12610. [DOI] [PubMed] [Google Scholar]
Bergkvist 2018b {published data only}
- Bergkvist K, Fossum B, Johansson UB, Mattsson J, Larsen J. Patients’ experiences of different care settings and a new life situation after allogeneic haematopoietic stem cell transplantation. European Journal of Cancer Care 2018;27(1):e12672. [DOI] [PubMed] [Google Scholar]
Björkman 2010a {published data only}
- Björkman RK, Asplund K, Svedlund M, Paulson M. Activity and participation in home rehabilitation - older people's and family members' perspectives. Journal of Clinical Nursing 2010;19(Suppl 1):70-92. [DOI] [PubMed] [Google Scholar]
Björkman 2010b {published data only}
- Björkman RK, Wengler Y, Asplund K, Svedlund M. Multidisciplinary team's promoting a rehabilitative approach among older people in home care. Journal of Clinical Nursing 2010;19(Suppl 1):70-92. [Google Scholar]
Booth 2007 {published data only}
- Booth S, Kendall M. Benefits and challenges of providing transitional rehabilitation services to people with spinal cord injury from regional, rural and remote locations. Australian Journal of Rural Health 2007;15(3):172-8. [DOI] [PubMed] [Google Scholar]
Breier 1999 {published data only}
- Breier SJ. Home intravenous therapy down under. Journal of Intravenous Nursing 1999;22(4):187-93. [PubMed] [Google Scholar]
Burton 1998 {published data only}
- Burton LC, Leff B, Harper M, Ghoshtagore I, Steinwachs DA, Greenough WB, et al. Acceptability to patients of a home hospital. Journal of American Geriatrics Society 1998;46(5):605-9. [DOI] [PubMed] [Google Scholar]
Cafazzo 2009 {published data only}
- Cafazzo JA, Leonard K, Easty AC, Rossos PG, Chan CT. The user-centered approach in the development of a complex hospital-at-home intervention. Advances in Information Technology and Communication in Health 2009;143:328-33. [PubMed] [Google Scholar]
Cameron 2022b {published data only}
- Cameron TM, Walker MF, Fisher RJ. A qualitative study exploring the lives and caring practices of young carers of stroke survivors. International Journal of Environmental Research & Public Health 2022;19(7):3941. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carusone 2006a {published data only}
- Carusone SC, Loeb M, Lohfeld L. Pneumonia care and the nursing home: a qualitative descriptive study of resident and family member perspectives. BMC Geriatrics 2006;6(2):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carusone 2006b {published data only}
- Carusone SC, Loeb M, Lohfeld L. A clinical pathway for treating pneumonia in the nursing home: Part I: The nursing perspective. American Medical Directors Association 2006;7(5):271-8. [DOI] [PubMed] [Google Scholar]
Castro 2016 {published data only}
- Castro WS. Dehospitalisation in a general public hospital of Minas General: start of home care [A desospitalização de um hospital público geral de Minas Gerais: início da atenção domiciliar]. Federal University of Minas Gerais Nursing School 2016.
Cegarra‐Navarro 2013 {published data only}
- Cegarra-Navarro J-G, Cepeda Carrión G. Implementing telemedicine technologies through an unlearning context in a homecare setting. Behaviour & Information Technology 2013;32(1):80-90. [Google Scholar]
Charron 2019 {published data only}
- Charron J, Gouezec H, Bajeux E. Home blood transfusion in France: benefits and development terms [Transfusion à domicile: intérêt et conditions de développement dansle contexte Français]. Clinical and Biological Transfusion 2019;26(4):304-8. [DOI] [PubMed] [Google Scholar]
Chee 2016 {published data only}
- Chee S, Neo AY, Chen LS, Seah EY, Li CL, Aung NL, et al. Understanding factors influencing the choice of discharge destination by older patients post total lower limb replacement: a qualitative study. Proceedings of Singapore Healthcare 2016;25(1):43-9. [Google Scholar]
Chen 2014 {published data only}
- Chen AW, Koh YT, Leong SW, Ng LW, Lee PS, Koh GC. Post community hospital discharge rehabilitation attendance: self-perceived barriers and participation over time. Annals of the Academy of Medicine 2014;43(3):136-44. [PubMed] [Google Scholar]
Chen 2019 {published data only}
- Chen H, Walabyeki J, Johnson M, Boland E, Seymour J, Macleod U. An integrated understanding of the complex drivers of emergency presentations and admissions in cancer patients: qualitative modelling of secondary-care health professionals' experiences and views. PLOS One 2019;14(5):e0216430. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2020 {published data only}
- Chen Y, Chen Y, Zheng K, Dodakian L, See J, Zhou R, et al. A qualitative study on user acceptance of a home-based stroke telerehabilitation system. Topics in Stroke Rehabilitation 2020;27(2):81-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cherin 2020 {published data only}
- Cherin P, Pindi Sala T, Clerson P, Dokhan A, Fardini Y, Duracinsky M, et al. Recovering autonomy is a key advantage of home-based immunoglobulin therapy in patients with myositis: a qualitative research study. Medicine 2020;99(7):e19012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Christensen 2022 {published data only}
- Christensen HM, Pietersen PI, Laursen CB, Wittrock D, Nadim G, Jorgensen G, et al. Patients’ perspectives on point-of-care diagnostics and treatment by emergency medical technicians in acute COPD exacerbations: a qualitative study. Scandinavian Journal of Trauma, Resuscitation & Emergency Medicine 2022;30(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chua 2022 {published data only}
- Chua CMS, Ko SQ, Lai YF, Lim YW, Shorey S. Perceptions of stakeholders toward "Hospital at Home" program in Singapore: a descriptive qualitative study. Journal of Patient Safety 2022;18(3):e606-12. [DOI] [PubMed] [Google Scholar]
Closs 1995 {published data only}
- Closs SJ, Stewart LS, Brand E, Currie CT. A scheme of early supported discharge for elderly trauma patients: the views of patients, carers and community staff. British Journal of Occupational Therapy 1995;58(9):373-76. [Google Scholar]
Coeugnet 2016 {published data only}
- Coeugnet S, Forrierre J, Naveteur J, Dubreucq C, Anceaux F. Time pressure and regulations on hospital-in-the-home (HITH) nurses: an on-the-road study. Applied Ergonomics 2016;54:110-9. [DOI] [PubMed] [Google Scholar]
Cohen 2017 {published data only}
- Cohen AB, Knobf MT, Fried TR. Avoiding hospitalizations from nursing homes for potentially burdensome care: results of a qualitative study. JAMA Internal Medicine 2017;177(1):137-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Combes 2015 {published data only}
- Combes G, Allen K, Sein K, Girling A, Lilford R. Taking hospital treatments home: a mixed methods case study looking at the barriers and success factors for home dialysis treatment and the influence of a target on uptake rates. Implementation Science 2015;10:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Conger 1995 {published data only}
- Conger CO. Recreating life: a grounded theory of caregiver and care recipient relationship development in acute home care. University of Utah 1995.
Cooper 1999 {published data only}
- Cooper G. Hospital in the home in Victoria: factors influencing allocation decisions. Australian Journal of Primary Health - Interchange 1999;5(1):60-9. [Google Scholar]
Cox 2018 {published data only}
- Cox M, O'Connor C, Biggs K, Hind D, Bortolami O, Franklin M, et al. The feasibility of early pulmonary rehabilitation and activity after COPD exacerbations: external pilot randomised controlled trial, qualitative case study and exploratory economic evaluation. Health Technology Assessment 2018;22(11):1-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dempsey 2000 {published data only}
- Dempsey J. The appropriateness of admissions and the influences on a decision to admit. Journal of Quality in Clinical Practice 2000;20(2-3):95-9. [DOI] [PubMed] [Google Scholar]
de Rezende Ferreira 2021 {published data only}
- Rezende Ferreira SI, Teston EF, De Andrade GKS, Giacon-Arruda BCC, Sato DM, Almeida RGDS. Challenges for the home hospitalization of the elderly from the family perspective. Revista Baiana de Enfermagem 2021;35:e42249. [Google Scholar]
De Vliegher 2015 {published data only}
- De Vliegher K, Aertgeerts B, Declercq A, Milisen K, Sermeus W, Moons P. Shifting care from hospital to home: a qualitative study. Primary Health Care 2015;25(9):26-33. [Google Scholar]
Donnelly 1999 {published data only}
- Donnelly M, Dempster M. A home from hospital service for older people. The Ulster Medical Journal 1999;68(2):78-83. [PMC free article] [PubMed] [Google Scholar]
Duke 2012 {published data only}
- Duke M, Botti M, Hunter S. Effectiveness of pain management in hospital in the home programs. Clinical Journal of Pain 2012;28(3):187-94. [DOI] [PubMed] [Google Scholar]
Elston 2022 {published data only}
- Elston J, Gradinger F, Asthana S, Fox M, Dawson L, Butler D, et al. Impact of ‘enhanced’ intermediate care integrating acute, primary and community care and the voluntary sector in Torbay and South Devon, UK. International Journal of Integrated Care 2022;22(1):14,1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferguson 1989 {published data only}
- Ferguson G. The hospital at home: interest in New Brunswick's experiment is growing. Canadian Medical Association Journal 1989;141:1087-9. [PMC free article] [PubMed] [Google Scholar]
Fitzsimmons 2016 {published data only}
- Fitzsimmons DA, Thompson J, Bentley CL, Mountain GA. Comparison of patient perceptions of telehealth-supported and specialist nursing interventions for early stage COPD: a qualitative study. BMC Health Services Research 2016;16(1):420. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fried 1998 {published data only}
- Fried TR, Doorn C, Tinetti ME, Drickamer MA. Older persons' preferences for site of treatment in acute illness. Journal of General Internal Medicine 1998;13(8):522-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fried 1999 {published data only}
- Fried TR, Doorn C, O'Leary JR, Tinetti ME, Drickamer MA. Older persons' perceptions of home and hospital as sites of treatment for acute illness. American Journal of Medicine 1999;107(4):317-23. [DOI] [PubMed] [Google Scholar]
Fried 2000 {published data only}
- Fried TR, Doorn C, O'Leary JR, Tinetti ME, Drickamer MA. Older person's preferences for home vs hospital care in the treatment of acute illness. Archives of Internal Medicine 2000;160(10):1501-6. [DOI] [PubMed] [Google Scholar]
Gache 2014 {published data only}
- Gache K, Leleu H, Nitenberg G, Woimant F, Ferrua M, Minvielle E. Main barriers to effective implementation of stroke care pathways in France: a qualitative study. BMC Health Services Research 2014;14:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gardner 2003 {published data only}
- Gardner G, Gardner A, Morley G, Watson DA. Managing intravenous medications in the non-hospital setting: an ethnographic investigation. Journal of Infusion Nursing 2003;26(4):227-33. [DOI] [PubMed] [Google Scholar]
Gorbenko 2021 {published data only}
- Gorbenko K, Franzosa E, Masse S, Brody AA, Sheehan O, Kinosian B, et al. “I felt useless”: a qualitative examination of COVID-19’s impact on home-based primary care providers in New York. Home Health Care Services Quarterly 2021;40(2):121-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guberman 2005 {published data only}
- Guberman N, Gagnon É, Côté D, Gilbert C, Thivièrge N, Tremblay M. How the trivialization of the demands of high-tech care in the home is turning family members into para-medical personnel. Journal of Family Issues 2005;26(2):247-72. [Google Scholar]
Guo 2022 {published data only}
- Guo M, Kong M, Shi W, Wang M, Yang H. Listening to COVID-19 survivors: what they need after early discharge from hospital - a qualitative study. International Journal of Qualitative Studies on Health and Well-being 222;17(1):2030001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gustafsson 2014 {published data only}
- Gustafsson LA, Hodson TJ, Fleming JM, Hoyle MF. The impact of STRENGTH on the expected and actual transition to home experience. Disability and Rehabilitation 2014;36(26):2244-51. [DOI] [PubMed] [Google Scholar]
Hall 2008 {published data only}
- Hall M, Lloyd H. Evaluating patients' experiences of home and hospital chemotherapy. Cancer Nursing Practice 2008;7(1):35-8. [Google Scholar]
Heaney 2002 {published data only}
- Heaney C, Lim K, Lydall-Smith S, Dorevitch M. Unassigned geriatric evaluation and management program: preventing sub-acute hospital admissions. Australian Health Review 2002;25(6):191-7. [DOI] [PubMed] [Google Scholar]
Hoeman 1988 {published data only}
- Hoeman SP. A system designed for paradox: hospital home health nursing in the United States. Recent Advances in Nursing 1988;20:92-104. [Google Scholar]
Horter 2014 {published data only}
- Horter S, Stringer B, Reynolds L, Shoaib M, Kasozi S, Casas EC, et al. "Home is where the patient is": a qualitative analysis of a patient-centred model of care for multi-drug resistant tuberculosis. BMC Health Services Research 2014;14:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hough 2020 {published data only}
- Hough P, Gleeson S, Shkuratova N, Coker F, Williams C. Introducing a clinically effective allied health rapid discharge team within a complex aged subacute in-patient cohort on a cost recovery basis: The Supported Patient c entred Early Discharge (SPeED) initiative. Australian Health Review 2020;44:931–4. [DOI] [PubMed] [Google Scholar]
Huang 2022 {published data only}
- Huang Y, Hu J, Mao B, Ni P, Shou Y, Hou L, Xie T. Perspectives on the process of negative pressure wound therapy at home in patients with chronic wound: a qualitative descriptive study. International Journal of Lower Extremity Wounds 2022;21(4):384-96. [DOI] [PubMed] [Google Scholar]
Hurley 2017 {published data only}
- Hurley EM, McHugh S, Carrroll A, White B, Normand C. A protocol to evaluate the effectiveness of a nationwide Acute Medicine programme: examining what works, for whom, how, and in what circumstances. International Journal of Integrated Care 2017;17(5):A209. [Google Scholar]
Hynes 2012 {published data only}
- Hynes G, Stokes A, McCarron M. Informal care-giving in advanced chronic obstructive pulmonary disease: lay knowledge and experience. Journal of Clinical Nursing 2012;21(7-8):1068-77. [DOI] [PubMed] [Google Scholar]
Jaglal 2002 {published data only}
- Jaglal SB, Santaguida L, Kreder H, Naglie G, Coyte PC, Scott J, et al. The At Home Early Discharge (AHEAD) program for hip fracture patients: results of a pilot study. Physiotherapy Canada 2002;54(2):102-9. [Google Scholar]
Jang 2022 {published data only}
- Jang H, Kim S, Kim D, Park M, Rhue S, Lee C, et al. “It's a part of the patient”: the experiences of patients with cancer undergoing home-based chemotherapy from patients' and nurses' perspectives. Asia-Pacific Journal of Oncology Nursing 2022;9(8):100072. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jimenez 2010 {published data only}
- Jimenez S, Aguilo S, Gil V, Antolin A, Prieto S, Bragulat E, et al. Psychosocial factors determine patients' acceptance of emergency department discharge directly to hospital-at-home care [Los factores psicosociales determinan la aceptacio ´nde la hospitalizacio ´n a domicilio directamente desde el servicio de urgencias]. Gaceta Sanitaria 2010;24(4):303-8. [DOI] [PubMed] [Google Scholar]
Johannessen 2019 {published data only}
- Johannessen A-K, Steihaug S. Municipal acute units as part of the clinical pathway for older patients. International Journal of Integrated Care 2019;19(4):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnson 2001 {published data only}
- Johnson MK, Flanigan U, Fuld J, Irwin A, Stewart C, Stevenson RD. Hospital at home services for acute exacerbation of chronic obstructive pulmonary disease: a survey of British practice. Health Bulletin 2001;59(3):163-70. [PubMed] [Google Scholar]
Juaton 2022 {published data only}
- Juaton M, Cusack L, Schultz T. Healthcare workers’ experiences of transitioning natalizumab infusions from hospital services to an in-home setting: a qualitative study. Australian Journal of Advanced Nursing 2022;39(1):18-26. [Google Scholar]
King 2020 {published data only}
- King R, Seeger T, Wang M, Li Pi Shan R, McGovern C, Knox J, et al. Early supported discharge for neurorehabilitation following acquired brain injury. Frontiers in Neurology 2020;11:596526. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kjaerhauge Christiansen 2021 {published data only}
- Kjaerhauge Christiansen L, Rasmussen AM, Mouritzen HS, Ostervig Buus AS, Gronkjaer M. Quickly home again: patients' experiences of early discharge after minor stroke. Scandinavian Journal of Caring Sciences 2021;35(4):1187-95. [DOI] [PubMed] [Google Scholar]
Leonardsen 2018 {published data only}
- Leonardsen A-C, Del Busso L, Grøndahl VA, Jelsness-Jørgensen L-P. Handovers in primary healthcare in Norway: a qualitative study of general practitioners' collaborative experiences. Health & Social Care in the Community 2018;26(1):e173-8. [DOI] [PubMed] [Google Scholar]
Levine 2021b {published data only}
- Levine DM, Desai MP, Ross J, Como N, Anne Gill E. Rural perceptions of acute care at home: a qualitative analysis. Journal of Rural Health 2021;37(2):353-61. [DOI] [PubMed] [Google Scholar]
Levine 2022 {published data only}
- Levine DM, Paz M, Burke K, Schnipper JL. Predictors and reasons why patients decline to participate in home hospital: a mixed methods analysis of a randomized controlled trial. Journal of General Internal Medicine 2022;37(2):327-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levinson 2021 {published data only}
- Levinson R, Salas L, Zanca JM. The experience of using a hospital bed alternative at home among individuals with spinal cord injury: a case series. Journal of Spinal Cord Medicine 2021;46(2):204-14. [DOI: 10.1080/10790268.2021.1937454] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lillebuen 2020 {published data only}
- Lillebuen L, Schick-Makaroff K, Thompson S, Molzahn A. Facilitators and barriers to care in rural emergency departments in Alberta for patients on peritoneal dialysis (PD): an interpretive descriptive study. Canadian Journal of Kidney Health and Disease 2020;7:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Linqvist Leonardsen 2016 {published data only}
- Linqvist Leonardsen A-C, Del Busso L, Abrahamsen Grøndahl V, Ghanima W, Barach P, Jelsness-Jørgensen L-P. A qualitative study of patient experiences of decentralized acute healthcare services. Scandinavian Journal of Primary Health Care 2016;34(3):317-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Luu 2021 {published data only}
- Luu P, Vimont A, Leleu H, Mace V, Mondschein T, Haushalter E, et al. Evaluation of the PRADO home discharge support programme for orthopaedic surgery in 2018. Orthopaedics & Traumatology: Surgery & Research 2022;108:1-6. [DOI: 10.1016/j.otsr.2021.102923] [DOI] [PubMed] [Google Scholar]
Marineau 2005 {published data only}
- Marineau ML. Exploring the lived experience of individuals with acute infections transitioning in the home with support by an advanced practice nurse using telehealth. University of Hawai'i at Manoa PhD thesis 2005.
Marineau 2007 {published data only}
- Marineau ML. Telehealth advance practice nursing: the lived experiences of individuals with acute infections transitioning in the home. Nursing Forum 2007;42(4):196-208. [DOI] [PubMed] [Google Scholar]
Martínez‐Caro 2013 {published data only}
- Martínez-Caro E, Cegarra-Navarro JG, Solano-Lorente M. An extension of the technology acceptance model in hospital-in-the-home units. In: Handbook of Research on ICTs and Management Systems for Improving Efficiency in Healthcare and Social Care. IGI Global, 2013:1191-207. [Google Scholar]
Mataure 2013 {published data only}
- Mataure P, Thupayagale-Tshweneagae GB. Expectations of clients enrolled in a community and home-based care programme: Insights from Zimbabwe. Africa Journal of Nursing & Midwifery 2013;15(1):149-62. [Google Scholar]
McBride 2011 {published data only}
- McBride SE, Beer JM, Mitzner TL, Rogers WA. Challenges for home health care providers: a needs assessment. Physical and Occupational Therapy in Geriatrics 2011;29(1):5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Meyenfeldt 2022 {published data only}
- Meyenfeldt EMV, Nassau F, Betue CTI, Barberio L, Schreurs WH, Marres GMH, et al. Implementing an enhanced recovery after thoracic surgery programme in the Netherlands: a qualitative study investigating facilitators and barriers for implementation. BMJ Open 2022;12(1):e051513. [DOI] [PMC free article] [PubMed] [Google Scholar]
Misra‐Hebert 2021 {published data only}
- Misra-Hebert AD, Rothberg MB, Fox J, Ji X, Hu B, Milinovich A, et al. Healthcare utilization and patient and provider experience with a home visit program for patients discharged from the hospital at high risk for readmission. Healthcare 2021;9(1):100518. [DOI] [PMC free article] [PubMed] [Google Scholar]
Montalto 1998 {published data only}
- Montalto M, Karabatsos G. General practitioner involvement in hospital in the home: the hospital's view. Australian Family Physician 1998;27(9):811-5. [PubMed] [Google Scholar]
Mooney 2003 {published data only}
- Mooney J, Boxer E. Keeping heart failure patients at home. Australian Journal of Advanced Nursing 2003;21(1):8-13. [Google Scholar]
Murphy 2020 {published data only}
- Murphy P, Harradine D, Hewitt M. Evaluation of an early discharge from hospital scheme focusing on patients' housing needs: The ASSIST Project. Health & Social Care in the Community 2020;28(5):1544-50. [DOI] [PubMed] [Google Scholar]
Palmisano 2019 {published data only}
- Palmisano M, Nicolì LA, Calò D, Marseglia C. “Home Hospitalization”: skills and knowledge of nurses (the case of “Città della Salute e della Scienza” hospital in Turin) [“Ospedale a Domicilio”: competenze e conoscenze dell’infermiere (Esperienza dell’AOU Città della Salute e Scienza di Torino)]. Professioni Infermieristiche 2019;72(4):29-34. [Google Scholar]
Paryono 2022 {published data only}
- Paryono P, Ar Rochmah M, Setyopranoto I, Trisnantoro L. Postacute-stroke management problems in home care service: a qualitative single-centered study in Yogyakarta, Indonesia. Journal of Neurosciences in Rural Practice 2022;13(1):50-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Randstrom 2014 {published data only}
- Randstrom KB, Wengler Y, Asplund K, Svedlund M. Working with 'hands-off' support: a qualitative study of multidisciplinary teams' experiences of home rehabilitation for older people. International Journal of Older People Nursing 2014;9(1):25-33. [DOI] [PubMed] [Google Scholar]
Redmond 1994 {published data only}
- Redmond K. The hospital in the home. The Lamp 1994;51(4):21. [PubMed] [Google Scholar]
Ringsberg 2003 {published data only}
- Ringsberg KC, Holmgren B. Home rehabilitation of stroke patients from the perspective of the patients and their relatives. Nordisk Fysioterapi 2003;7(3):21-31. [Google Scholar]
Rink 1998 {published data only}
- Rink E, Sims J, Walker R, Pickard L. Hospital care at home: An evaluation of a scheme for orthopaedic patients. Health and Social Care in the Community 1998;6(3):158-63. [DOI] [PubMed] [Google Scholar]
Roberts 2009 {published data only}
- Roberts CM, Seiger A, Ingham J. Patient views on three key service areas within hospital COPD care. Health Education Journal 2009;68(1):26-33. [Google Scholar]
Rochette 2021 {published data only}
- Rochette A, Dugas A, Morissette-Gravel A-S. Inclusion of relatives in stroke rehabilitation: perception of quality of services they received in the context of early supported discharged (ESD), in- and out-patient services. Topics in Stroke Rehabilitation 2021;28(2):142-52. [DOI] [PubMed] [Google Scholar]
Rodgers 2019 {published data only}
- Rodgers H, Howel D, Bhattarai N, Cant R, Drummond A Ford GA. Evaluation of an extended stroke rehabilitation service (EXTRAS): a randomized controlled trial and economic analysis. Stroke 2019;50(12):3561-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rydmark Kersley 2021 {published data only}
- Rydmark Kersley A, Bertero C. Women's experiences of an enhanced recovery after surgery program: a qualitative study. Nursing & Health Sciences 2021;23(1):263-72. [DOI] [PubMed] [Google Scholar]
Sahin 2015 {published data only}
- Sahin E, Matta A. A contribution to operations management-related issues and models for home care structures. International Journal of Logistics: Research and Applications 2015;18(4):355-85. [Google Scholar]
Santamaria 2000 {published data only}
- Santamaria N, McKenzie M. The carers of hospital in the home patients focus on clinical processes, procedures and the prediction of deterioration. Australian Journal of Advanced Nursing 2000;17(4):16-20. [PubMed] [Google Scholar]
Senillosa 2016 {published data only}
- Senillosa M, González PM. The role of home-care in treating patients [El papel de la internación domiciliaria en el cuidado del enfermo]. Salud(i)Ciencia 2016;21(8):863-66. [Google Scholar]
Soerensen 2004 {published data only}
- Soerensen AA, Mendes IA, Hayashida M. Homecare: a study on its implementation in a private health system [Atendimento domiciliar: análise de um serviço privado]. Rev Rene Fortaleza 2004;5(2):86-92. [Google Scholar]
Stephenson 2000 {published data only}
- Stephenson S, Wiles R. Advantages and disadvantages of the home setting for therapy: views of patients and therapists. British Journal of Occupational Therapy 2000;63(2):59-64. [Google Scholar]
Stuck 2017 {published data only}
- Stuck A, Crowley C, Martinez T, Wittgrove A, Brennan JJ, Chan TC, et al. Perspectives on home-based healthcare as an alternative to hospital admission after emergency treatment. Western Journal of Emergency Medicine 2017;18(4):761-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 2007 {published data only}
- Taylor S, Eldridge S, Chang YM, Sohanpal R, Clarke A. Evaluating hospital at home and early discharge schemes for patients with an acute exacerbation of COPD. Chronic Respiratory Disease 2007;4(1):33-43. [DOI] [PubMed] [Google Scholar]
Thorsén 2006 {published data only}
- Thorsén AM, Holmqvist LW, Koch L. Early supported discharge and continued rehabilitation at home after stroke: 5-year follow-up of resource use. Journal of Stroke and Cerebrovascular Diseases 2006;15(4):139-43. [DOI] [PubMed] [Google Scholar]
van der Veen 2019 {published data only}
- Veen DJ, Dopp CM, Siemonsma PC, Nijhuis-van der Sanden MW, Swart BJ, Steultjens EM. Factors influencing the implementation of home-based stroke rehabilitation: professionals' perspective. PLOS One 2010;14(7):e0220226. [DOI] [PMC free article] [PubMed] [Google Scholar]
Von Koch 2001 {published data only}
- Von Koch L, Holmqvist LW. Early supported discharge and continued rehabilitation at home after stroke. Physical Therapy Reviews 2001;6(2):119-40. [Google Scholar]
Vrotsou 2023 {published data only}
- Vrotsou K, Orive-Calzada M, Gonzalez N, Vergara I, Pascual-Fernandez N, Guerra-Lopez C, et al. Factors associated with the hospital at home workload: a Delphi consensus study [Factores relacionados con la carga de trabajo en hospitalización a domicilio: estudio de consenso Delphi]. Journal of Healthcare Quality Research 2023;38:233-44. [DOI: 10.1016/j.jhqr.2022.09.001] [DOI] [PubMed] [Google Scholar]
Watty 2003 {published data only}
- Watty K, White MA, Matthews JP, Buchanan L, Clarke JL, Sulkowski AJ, et al, . There's no place like home: a prospective evaluation of chemotherapy in the home. Australian Journal of Cancer Nursing 2003;4(1):18-21. [Google Scholar]
Wergeland 2022 {published data only}
- Wergeland D, Harsten K, Klarare A, Steindal SA. Hospital nurses' experiences of assessing health status changes in stem-cell transplanted patients in home care: a qualitative study. Journal of Clinical Nursing 2022;31(21-2):3190-9. [DOI] [PubMed] [Google Scholar]
Wilson 2003 {published data only}
- Wilson A, Parker H, Wynn A, Spiers N. Performance of hospital-at-home after a randomised controlled trial. Journal of Health Services Research & Policy 2003;8(3):160-4. [DOI] [PubMed] [Google Scholar]
Zakrajsek 2013 {published data only}
- Zakrajsek AG, Schuster E, Guenther D, Lorenz K. Exploring older adult care transitions from hospital to home: a participatory action research project. Physical and Occupational Therapy in Geriatrics 2013;31(4):328-44. [Google Scholar]
References to studies awaiting assessment
Akehurst 2017 {published data only}
- Akehurst J, Giles K, Stronge P. Building workforce capacity and capability for integrated working. International Journal of Integrated Care 2017;17(5):A231. [DOI: ] [Google Scholar]
Dagsvik 2018 {published data only}
- Dagsvik G, Abildsnes E, Thygesen E. Norwegian municipal rehabilitation services in transition. International Journal of Integrated Care 2018;18(S2):A291. [DOI: ] [Google Scholar]
Hayden‐Wright 2000 {published data only}
- Hayden-Wright C. Admission avoidance: an investigation into the change of practice associated with it [sic] implementation [Thesis]. Cambridge (UK): Homerton College, School of Health Studies, 2000. [Google Scholar]
O'Donovan 2019 {published data only}
- O'Donovan C, Wright S, Towler S, Furness E. Streamlining referral processes at a tertiary acute medical ambulatory centre. Age and Ageing 2019;48:iii17-iii65. [DOI: 10.1093/ageing/afz103.32] [DOI] [Google Scholar]
Sullivan 2022 {published data only}
- Sullivan JL, Yousefi‑Nooraie R, D’Arcy D, Levine A, Zimmerman L, Shin MH, et al. Hospital in home: evaluating need and readiness for implementation (HENRI) in the Department of Veterans Affairs: protocol for a mixed‑methods evaluation and participatory implementation planning study. Implementation Science Communications 2022;3:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Valía‐Cotanda 2018 {published data only}
- Valía-Cotanda E, Gil-Salmerón A, Alhambra-Borrás T, Garcés-Ferrer J. Integrated care for elderly receiving hospital-at-home care: designing an innovative home-based programme. International Journal of Integrated Care 2018;18(S2):A367. [DOI: ] [Google Scholar]
Yao 2022 {published data only}
- Yao X, Paulson M, Maniaci MJ, Dunn AN, Nelson CR, Behnken EM, et al. Effect of hospital‑at‑home vs. traditional brick‑and‑mortar hospital care in acutely ill adults: study protocol for a pragmatic randomized controlled trial. Trials 2022;23:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Ames 2017
- Ames HM, Glenton C, Lewin S. Parents' and informal caregivers' views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database of Systematic Reviews 2017, Issue 2. Art. No: CD011787. [DOI: 10.1002/14651858.CD011787.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Australian Institute of Health and Welfare 2019
- Australian Institute of Health and Welfare. Admitted patient care 2017–18: Australian hospital statistics. Health services series no. 90. Cat. no. HSE 225. Table S5.26: Separations with hospital-in-the-home care, public and private hospitals, states and territories, 2017–18 2019.
Baxter 2014
- Baxter SK, Blank L, Woods HB, Payne N, Rimmer M, Goyder E. Using logic model methods in systematic review synthesis: describing complex pathways in referral management interventions. BMC Medical Research Methodology 2014;14:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brody 2019
- Brody AA, Arbaje AI, DeCherrie LV, Federman AD, Leff B, Siu AL. Starting up a hospital at home program: facilitators and barriers to implementation. Journal of the American Geriatric Society 2019;67(3):588-95. [DOI] [PubMed] [Google Scholar]
Buhagiar 2017
- Buhagiar MA, Naylor JM, Simpson G, Harris IA, Kohler F. Understanding consumer and clinician preferences and decision making for rehabilitation following arthroplasty in the private sector. BMC Health Services Research 2017;17(1):415. [DOI] [PMC free article] [PubMed] [Google Scholar]
Caplan 2012
- Caplan GA, Sulaiman NS, Mangin DA, Aimonino Ricauda N, Wilson AD, Barclay L. A meta-analysis of "hospital in the home". Medical Journal of Australia 2012;197(9):512-9. [DOI] [PubMed] [Google Scholar]
Chua 2022
- Chua CM, Ko SQ, Lai YF, Lim YW, Shorey S. Perceptions of hospital-at-home among stakeholders: a meta-synthesis. Journal of General Internal Medicine 2022;37(3):637-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cochrane EPOC 2017
- Cochrane Effective Practice and Organisation of Care (EPOC). EPOC Qualitative Evidence Syntheses guidance on when to sample and how to develop a purposive sampling frame. EPOC Resources for review authors, 2017. epoc.cochrane.org/epoc-resources-review-authors.
Connor 2022
- Connor EO, Dolan E, Horgan F, Robinson K, Galvin R. Experiences of early supported discharge services following stroke: a qualitative evidence synthesis. Age and Ageing 2022;51(Suppl 2):afac124.012. [Google Scholar]
Cooke 2009
- Cooke R, Ellis H, Fafiolu R, Highfield E, Robinson C. Early supported discharge team from stroke. Interim report. University Hospitals. Bristol NHS Foundation Trust 2009.
Crilly 2010
- Crilly J, Chaboyer W, Wallis M, Thalib L, Polit D. An outcomes evaluation of an Australian Hospital in the Nursing Home admission avoidance programme. Journal of Clinical Nursing 2010;20:1178-87. [DOI] [PubMed] [Google Scholar]
Critical Appraisal Skills Programme 2020
- Critical Skills Appraisal Programme. CASP (Systematic Review) Checklist. www.casp-uk.net (accessed 7 November 2020).
Deloitte Access Economics 2011
- Deloitte Access Economics. Economic analysis of Hospital in the Home (HiTH). Hospital in the Home Society of Australasia 2011.
Dismore 2019
- Dismore LL, Echevarria C, Wersch A, Gibson J, Bourke S. What are the positive drivers and potential barriers to implementation of hospital at home selected by low-risk DECAF score in the UK: a qualitative study embedded within a randomised controlled trial. BMJ Open 2019;9(4):e026609. [DOI] [PMC free article] [PubMed] [Google Scholar]
Echevarria 2018
- Echevarria C, Gray J, Hartley T, Steer J, Miller J, Simpson AJ, et al. Home treatment of COPD exacerbation selected by DECAF score: a non-inferiority, randomised controlled trial and economic evaluation. Thorax 2018;73:713-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edgar 2024
- Edgar K, Iliffe S, Doll HA, Clarke MJ, Gonçalves-Bradley DC, Wong E, et al. Admission avoidance hospital at home. Cochrane Database of Systematic Reviews 2024, Issue 3. Art. No: CD007491. [DOI: 10.1002/14651858.CD007491.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Federman 2018
- Federman AD, Soones T, DeCherrie LV, Leff B, Siu AL. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Internal Medicine 2018;178(8):1033-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gardner 2003
- Gardner G, Gardner A, Morley G, Watson DA. Managing intravenous medications in the non-hospital setting: an ethnographic investigation. Journal of Infusion Nursing 2003;26(4):227-33. [DOI] [PubMed] [Google Scholar]
Gardner 2019
- Gardner M, Shepperd S, Godfrey M, Mäkelä P, Tsiachristas A, Singh-Mehta A, et al. Comprehensive geriatric assessment in hospital and hospital-at-home settings: a mixed-methods study. Health Services and Delivery Research 2019;7(10):1-206. [PubMed] [Google Scholar]
Glenton 2020
- Glenton C, Bohren MA, Downe S, Paulsen EJ, Lewin S, on behalf of Effective Practice and Organisation of Care (EPOC). EPOC Qualitative Evidence Synthesis: Protocol and review template. Version 1.1. EPOC Resources for review authors. Oslo: Norwegian Institute of Public Health; 2020. Available at: http://epoc.cochrane.org/epoc-specific-resources-review-authors.
Goncalves‐Bradley 2017
- Goncalves-Bradley DC, Iliffe S, Doll HA, Broad J, Gladman J, Langhorne P, et al. Early discharge hospital at home. Cochrane Database of Systematic Reviews 2017, Issue 6. Art. No: CD000356. [DOI: 10.1002/14651858.CD000356.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harden 2018
- Harden A, Thomas J, Cargo M, Harris J, Pantoja T, Flemming K, et al. Cochrane qualitative and implementation methods group guidance series-paper 5: methods for integrating qualitative and implementation evidence within intervention effectiveness reviews. Journal of Clinical Epidemiology 2018;97:70-8. [DOI: doi: 10.1016/j.jclinepi.2017.11.029. Epub 2017 Dec 11. PMID: 29242095.] [DOI] [PubMed] [Google Scholar]
Harris 2018
- Harris JL, Booth A, Cargo M, Hannes K, Harden A, Flemming K, et al. Cochrane Qualitative and Implementation Methods Group guidance series-paper 2: methods for question formulation, searching, and protocol development for qualitative evidence synthesis. Journal of Clinical Epidemiology 2018;97:39-48. [DOI] [PubMed] [Google Scholar]
HITH Society Australasia 2019
- HITH Society Australasia Ltd. Hospital in the home service register. www.hithsociety.org.au (accessed 10 September 2020).
Hoffmann 2014
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. [DOI] [PubMed] [Google Scholar]
Independent Hospital Pricing Authority 2015
- Independent Hospital Pricing Authority (IHPA). Admitted hospital care types: guide for use. www.ihpa.gov.au/publications/admitted-hospital-care-types (accessed 5 October 2020).
Karimi‐Shahanjarini 2019
- Karimi-Shahanjarini A, Shakibazadeh E, Rashidian A, Hajimiri K, Glenton C, Noyes J, et al. Barriers and facilitators to the implementation of doctor-nurse substitution strategies in primary care: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2019, Issue 4. Art. No: CD010412. [DOI: 10.1002/14651858.CD010412.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ko 2022b
- Ko SQ, Goh J, Tay YK, Nashi N, Hooi BM, Luo N, et al. Treating acutely ill patients at home: data from Singapore. Annals of the Academy of Medicine, Singapore 2022;51(7):392-9. [PubMed] [Google Scholar]
Kraut 2016
- Kraut JC, Singer BJ, Singer KP. Clinician and client views of utilising early supported discharge services. International Journal of Therapy and Rehabilitation 2016;23(10):464-71. [Google Scholar]
Kylén 2019
- Kylén M, Koch L, Pessah-Rasmussen H, Marcheschi E, Ytterberg C, Heylighen A, et al. The importance of the built environment in person-centred rehabilitation at home: study protocol. International Journal of Environmental Research and Public Health 2019;16(13):2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leary 2022
- Leary A. Saved bed days: the ultimate currency. BMJ 2022;378:1-2. [DOI: ] [DOI] [PubMed] [Google Scholar]
Leff 2022
- Leff B, DeCherrie LV, Montalto M, Levine DM. A research agenda for hospital at home. Journal of the American Geriatrics Society 2022;70(4):1060-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lemelin 2007
- Lemelin J, Hogg WE, Dahrouge S, Armstrong CD, Martin CM, Zhang W, et al. Patient, informal caregiver and care provider acceptance of a hospital in the home program in Ontario, Canada. BMC Health Services Research 2007;7:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levine 2019
- Levine DM, Ouchi K, Blanchfield B, Saenz A, Burke K, Paz M, et al. Hospital-level care at home for acutely ill adults. Annals of Internal Medicine 2019;172(2):77-85. [DOI] [PubMed] [Google Scholar]
Levine 2022
- Levine DM, Paz M, Burke K, Schnipper JL. Predictors and reasons why patients decline to participate in home hospital: a mixed methods analysis of a randomized controlled trial. Journal of General Internal Medicine 2022;37(2):327-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2018
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implementation Science 2018;13 Suppl 1:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Annals of Internal Medicine 2009;151(4):W65-94. [DOI] [PubMed] [Google Scholar]
Marshall 2014
- Marshall MN. Bridging the ivory towers and the swampy lowlands; increasing the impact of health services research on quality improvement. International Journal for Quality in Health Care 2014;26(1):1-5. [DOI] [PubMed] [Google Scholar]
Mäkelä 2018
- Mäkelä P, Godfrey M, Cradduck-Bamford A, Ellis G, Shepperd S. A protocol for the process evaluation of a multi-centre randomised trial to compare the effectiveness of geriatrician-led admission avoidance hospital at home versus inpatient admission. Trials 2018;19(1):569. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mäkelä 2020
- Mäkelä P, Stott D, Godfrey M, Ellis G, Schiff R, Shepperd S. The work of older people and their informal caregivers in managing an acute health event in a hospital at home or hospital inpatient setting. Age and Ageing 2020;49(5):856-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
NHMRC 2017
- NHMRC Partnership Centre for Health System Sustainability. Advisory groups. www.healthsystemsustainability.com.au/people-and-partners/advisory-groups/ (accessed 17 February 2020).
NHS Benchmarking Network 2015
- NHS Benchmarking Network. National Audit of Intermediate Care Summary Report 2015. static1.squarespace.com/static/58d8d0ffe4fcb5ad94cde63e/t/58f08efae3df28353c5563f3/1492160300426/naic-report-2015.pdf (accessed 29 August 2020).
Norman 2023
- Norman G, Bennett P, Vardy ER. Virtual wards: a rapid evidence synthesis and implications for the care of older people. Age and Ageing 2022;52:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nowell 2017
- Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. International Journal of Qualitative Methods 2017;16(1):1609406917733847. [Google Scholar]
Noyes 2020
- Noyes J, Booth A, Cargo M, Flemming K, Harden A, Harris J, et al. Chapter 21: Qualitative evidence. In Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020), Cochrane, 2020. Available from www.training.cochrane.org/handbook (accessed 5 November 2020).
NVivo [Computer program]
- NVivo. Version 12. Melbourne: QSR International Ptd Ltd, 2020.
OECD 2011
- OECD. Classification of Health Care Functions (ICHA-HC). In: A System of Health Accounts. 2011 edition. Paris: OECD Publishing, 2011. [Google Scholar]
Rafsten 2019
- Rafsten L, Danielsson A, Nordin A, Björkdahl A, Lundgren-Nilsson A, Larsson MEH, et al. Gothenburg very early supported discharge study (GOTVED): a randomised controlled trial investigating anxiety and overall disability in the first year after stroke. BMC Neurology 2019;19(277):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sheppard 2021
- Shepperd S, Gonçalves-Bradley DC, Straus SE, Wee B. Hospital at home: home‐based end‐of‐life care. Cochrane Database of Systematic Reviews 2021, Issue 3. Art. No: CD009231. [DOI: 10.1002/14651858.CD009231.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sheppard 2022
- Shepperd S, Butler C, Cradduck-Bamford A, Ellis G, Gray A, Hemsley A, et al. Is comprehensive geriatric assessment admission avoidance hospital at home an alternative to hospital admission for older persons? A randomised trial. Annals of Internal Medicine 2021;174(7):889-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2022
- Singh S, Gray A, Shepperd S, Stott DJ, Ellis G, Hemsley A, et al. Is comprehensive geriatric assessment hospital at home a cost-effective alternative to hospital admission for older people? Age and Ageing 2022;51(1):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Talley 2007
- Talley RC, Crews JE. Framing the public health of caregiving. American Journal of Public Health 2007;97(2):224-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2008
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology 2008;8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tong 2012
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Medical Research Methodology 2012;12:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
Towicz 2021
- Towicz M, Yang WX, Moylan S, Tindall R, Berk M. Hospital-in-the-home as a model for mental health care delivery: a narrative review. Psychiatric Services 2021;72(12):1415-27. [DOI] [PubMed] [Google Scholar]
Von Koch 2001
- Von Koch L, Holmqvist LW. Early supported discharge and continued rehabilitation at home after stroke. Physical Therapy Reviews 2001;6:119-40. [Google Scholar]
Wilson 1999
- Wilson A, Parker H, Wynn A, Jagger C, Spiers N, Jones J et al. Randomised controlled trial of effectiveness of Leicester hospital at home scheme compared with hospital care. BMJ 1999;319(7224):1542–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
World Hospital At Home Congress 2019
- World Hospital At Home Congress. Scientific program. whahc2019.kenes.com/2019/programme-(2)/programme.html (accessed 11 August 2020).
Young 2009
- Young J. The development of intermediate care services in England. Archives of Gerontology and Geriatrics 2009;49:S21-5. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Gearon 2021
- Gearon E, O'Connor D, Wallis JA, Han JX, Shepperd S, Makela P, et al. Factors influencing the implementation of early discharge hospital at home and admission avoidance hospital at home: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2021, Issue 3. Art. No: CD014765. [DOI: 10.1002/14651858.CD014765] [DOI] [PMC free article] [PubMed] [Google Scholar]