Summary
As far as non-communicable disease is concerned, Japan is unique in showing a substantial decline in stroke mortality and the lowest and declining mortality from ischemic heart disease during the past half century, which contributed to the elongation of a 4-year average life expectancy, leading to top longevity in the world. However, several issues have remained in the prevention of cardiovascular disease with super-aging: i) how to manage the screening and lifestyle modification for both individuals with metabolic syndrome and those with non-overweight/ obesity plus metabolic risk factors, and ii) how to enhance the referral of very high-risk individuals screened at health checks to physicians for seeking treatment and examine whether an early clinical visit was associated with a lower risk of cardiovascular disease and total mortality. Health counseling is needed for both persons with metabolic syndrome and high-risk individuals with non-obese/overweight because the population attributable risk fraction of ischemic cardiovascular disease was similar for both high-risk individuals. Standardized counseling for very high-risk individuals accelerated clinical visits and reduced levels of risk factors. In health counseling, public health nurses were more effective in increasing clinic visits. Furthermore, the earlier clinic visit after the counseling suggested a lower risk of hospitalization for stroke, coronary heart disease, heart failure, and all-cause mortality. This article reviews these epidemiological findings for health practitioners and policymakers to perform further prevention and control for cardiovascular disease in Japan and other Asian and African countries with emerging cardiovascular burden and aging.
Keywords: metabolic syndrome, cardiovascular disease, prevention, referral, epidemiology, Japan
Introduction
A major component of non-communicable diseases is cardiovascular disease, primarily ischemic heart disease and stroke, and are the leading cause of mortality and a major cause of disability in the world (1,2). In Japan, the age-standardized mortality rate of stroke declined substantially from the highest level since 1965 and that of ischemic heart disease was the lowest level and continued to decline until recently; the mortality rate reached approximately two-times higher for stroke and one-fourth for ischemic heart disease in Japan compared to Western countries (3). That large decline in cardiovascular mortality contributed to a rise in the average life expectancy in Japan by 4 years (4). The average life expectancy in 2022 has become 81.5 years in men and 87.6 years in women leading the top longevity in the world (5).
The backgrounds for this health success are multifold, primarily due to the improvement of diets including reduction of sodium intake along with fresh foods due to improved transport systems and freezing technology under the sharp socioeconomic development between the 1960's and 1990's, and mandatory health screening for cardiovascular risk factors and health instructions, and referral to local physicians to seek treatment under the universal health coverage since 1980's (3). Previous articles reported that the improvement in lifestyles and cardiovascular risk factors were associated with declining trends for cardiovascular disease trends in Japan (6-8).
The community-based prevention programs are based on public health services and medical care under universal health coverage, aiming: i) the primordial and primary prevention of cardiovascular risk factors through environmental improvements and lifestyle modification for the general population, ii) secondary prevention of screening high-risk individuals, their lifestyle modification, if necessary referral to physicians for seeking medical treatment, and iii) tertiary prevention of early treatment for cardiovascular disease patients and their rehabilitation (3). The prevention programs of these components are feasible and effective in reducing the incidence of stroke (9) and ischemic heart disease (7,10) and attenuating an increment of medical cost compared to the reference communities (11,12).
In 2008, the Japanese government started a screening and education program for people aged 40-74 years focusing on metabolic syndrome to attenuate the burden of medical cost primarily for kidney hemodialysis (13) because diabetes, one of the major components of metabolic syndrome, had become the major cause of chronic kidney disease and kidney failure (14).
In spite of the health success in the prevention of cardiovascular disease in Japan, several issues have remained in the prevention of cardiovascular disease with super-aging such as an increasing trend for the number of patients with chronic heart failure, chronic kidney disease, and dementia (15). One of the major issues is how to manage the screening and control both for high-risk individuals with metabolic syndrome and those with non-overweight/obesity because the latter group numbers are over half of high-risk individuals with high glucose, high blood pressure, and dyslipidemia (16,17). The other is how to enhance the referral of very high-risk individuals screened at health checks to physicians to seek treatment and examine whether early clinical visits were associated with a lower risk of cardiovascular disease and total mortality because more than half of such high-risk people did not visit physicians (18). We conducted epidemiological studies to provide scientific evidence on the above issues (19,20). In addition, such preventive programs would help to make self-care interventions for health and well-being, i.e. the ability of individuals, families, and communities to promote health, prevent disease, maintain health, and cope with illness and disability with or without the support of a health worker (21).
This article overviews the epidemiological findings on the above issues and provides clues for health practitioners' and policymakers' recommendations to enhance the prevention and control of cardiovascular disease and well-being in Japan and other Asian and African countries with emerging cardiovascular burdens and aging (22).
How to manage the screening and control both for high-risk individuals with metabolic syndrome and those with non-overweight/obesity?
The major strategy of nationwide programs on screening and lifestyle interventions is the reduction of abdominal obesity by lifestyle modification such as balanced diets and reduced alcohol consumption, smoking cessation, and enhanced physical activity, which are expected to control for high blood glucose, high blood pressure, and dyslipidemia (low HDL-cholesterol and/or high triglyceride levels) (9). Metabolic syndrome is defined as the presence of obesity/overweight as an essential component plus metabolic risk factors, which is different from the American criteria with obesity/overweight (one of the metabolic risk factors) (23). Thus, the Japanese program focuses on high-risk individuals with abdominal obesity/overweight, but not non-obese/ overweight ones with other metabolic risk factors, which may overlook the risk of non-obese/overweight individuals because over 60% or more of Japanese high-risk adults are the latter. Therefore, it is unclear whether the risk classification in the national program captures high-risk individuals who could benefit from lifestyle interventions, and it is necessary to examine how to manage the screening and control both for high-risk individuals with metabolic syndrome and those with non-overweight/obesity.
In a previous article described in detail (19), we examined the validity of risk classification to relate the classification with the risk of ischemic cardiovascular disease (ischemic heart disease and stroke) by a pooled analysis of 10 Japanese cohort studies on approximately 30,000 residents aged 40-79 years followed for a median of 9 years.
Metabolic syndrome is defined as the presence of high waist circumference of ≥ 85 cm in men and ≥ 90 cm in women and/or BMI of ≥ 25.0 kg/m2, an essential component plus one (probable metabolic syndrome) or two or more (definite metabolic syndrome) of the following: i) systolic blood pressure ≥ 130 mmHg, and/ or diastolic blood pressure ≥ 85 mmHg, or medication use; ii) triglyceride level ≥ 150 mg/dL and/or HDL-cholesterol level < 40 mg/dL; and iii) fasting glucose level ≥ 100 mg/dL, or non-fasting glucose level ≥ 140 mg/dL, or medication use. As shown in Table 1, the risk classification categories are information supply only (ISO), motivation-support intervention (MSI), and intensive support intervention (ISI) based on sex, age (40-64 and 65-75 years), current smoking status, and grade of metabolic syndrome (probable or definite). Current smoking is considered an additional risk factor when the number of the above risk factors, was counted one for high waist circumference ≥ 85 cm in men and ≥ 90 cm in women, and two for waist circumference < 85 cm in men and < 90 cm in women and BMI ≥ 25.0 kg/ m2. The ISI collapsed into the MSI for ages of 65-75 years.
Table 1. Risk classification in the national program of screening and lifestyle interventions for metabolic syndrome.
| Non-obese/overweight | Information supply only (ISO) | Motivation-support intervention (MSI) | Intensive support intervention (ISI) |
|---|---|---|---|
| Waist < 85 cm for men, < 90 cm for women and BMI < 25 kg/m2, regardless of risk factors | Waist ≥ 85 cm in men, ≥ 90 cm in women and 0 risk factor OR | Waist ≥ 85 cm in men, ≥ 90 cm in women and 1 risk factor OR | Waist ≥ 85 cm in men, ≥ 90 cm in women and ≥ 2 risk factors OR |
| Waist < 85 cm for men, < 90 cm for women and BMI ≥ 25 kg/m2, and 0 risk factor | Waist < 85 cm in men, < 90 cm in women and BM ≥ 25 kg/m2, and 1 or 2 risk factors | Waist < 85 cm in men, < 90 cm in women and BMI ≥ 25 kg/m2, and ≥ 3 risk factors |
The criteria for referral to local physicians to seek medical treatment were defined as: i) hypertension: systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg or medication use; ii) dyslipidemia: triglyceride level ≥ 300 mg/dL, and/or HDL-cholesterol level < 35 mg/dL, and/or non-HDL-cholesterol ≥ 170 mg/dL, or medication use; and iii) diabetes: fasting glucose level ≥ 126 mg/dL, or non-fasting glucose level ≥ 200 mg/dL, or medication use. See the methods of incidence determination of ischemic heart disease and stroke in the previous report (19).
As shown in Figure 1, the risk of ischemic cardiovascular disease adjusted for age (years), area (community) and non-HDL cholesterol using the Cox proportional hazards model was 60% to 70% higher in middle-aged men and women who received ISI, and 30% higher in older women who received MSI, compared with non-obese/ overweight individuals: the corresponding hazard ratios (HRs) and their confidence intervals (CIs) were 1.60 (95% CI, 1.26-2.04), 1.71 (95% CI, 1.16-2.54), and 1.31 (95% CI, 1.01-1.69). The population attributable fractions in middle-aged men and women receiving ISI were 17.7% and 6.6%, respectively, while that in older women receiving MSI was 9.4%.
Figure 1.
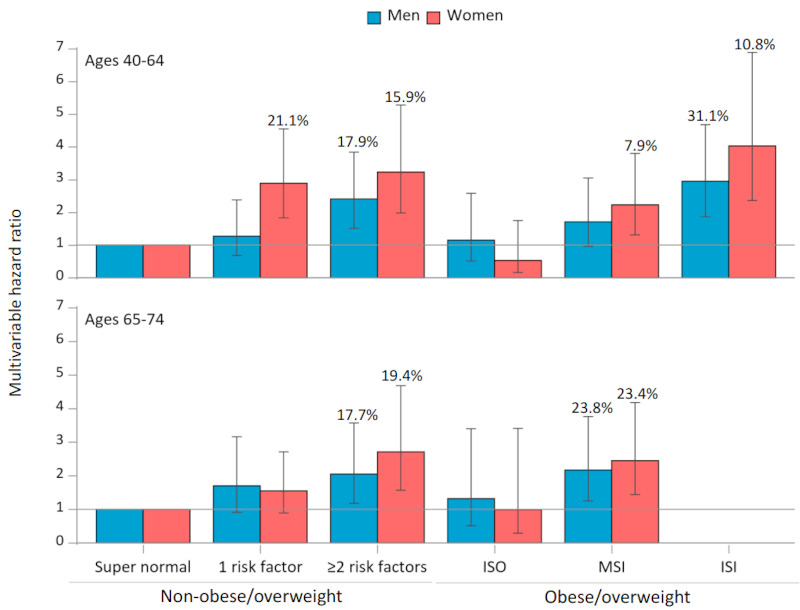
Age- and sex-specific multivariable hazard ratios of total cardiovascular disease according to the refined category of health intervention with non-obese/overweight subtypes for screened participants. Bar: 95% confidence interval. The number of percentages: population attributable risk. ISO: information supply only, MSI: motivation-support intervention, ISI: intensive support intervention. Data Source: modification from Reference 19.
Because the reference category included those with metabolic risk factors, we built a supernormal group (non-obese/overweight with no risk factor) as another reference. It was noteworthy that nonobese/overweight individuals with risk factors had similar hazard ratios and population-attributable risk fractions as individuals with metabolic syndrome (Figure 1). The middle-aged non-obese/overweight men and women with two or more risk factors and even middle-aged non-obese/ overweight women with only one risk factor had two to four times excess risk of cardiovascular disease, compared with the supernormal group. These findings justified the system for screening for both persons with metabolic syndrome and high-risk individuals with non-obese/overweight to conduct lifestyle interventions, and if needed, referral to local physicians in terms of risk stratification for cardiovascular disease.
The findings may be useful for researchers, practitioners, and policymakers to construct preventive strategies, evaluation, practice guidelines, and health policies in countries or populations where the prevalence of obesity is not common as well as in Japan.
How to enhance the referral of very high-risk individuals screened to local physicians for seeking treatment and examine whether an early clinical visit was associated with a lower risk of cardiovascular disease and total mortality?
In 2008, a national program for health checks and counseling for people aged 40-74 years was enacted in Japan to screen for individuals with high blood pressure, high hemoglobin A1c or glucose, high low-density lipoprotein cholesterol levels, and proteinuria to reduce their risk through lifestyle modification and to refer very-high risk individuals to local physicians.
However, less than half of patients with untreated extremely severe hypertension (systolic and/or diastolic blood pressures 180/110 mmHg and over) screened via health checks did not visit physicians thereafter probably because of the lack of symptoms as well as insufficient health counseling following health checks. We thus test the effect of a community-based program to accelerate referral to local physicians for people at very high risk of cardiovascular disease using a parallel-arm, non-blinded, cluster randomized trial.
The trial was performed for forty-three municipalities (21 intervention and 22 usual care) to examine whether standardized health counseling for very high-risk individuals aged 40-74 years accelerates clinic visits (18,20). A total of 8,977 and 6,733 were allocated to the intervention and usual care groups, respectively, who were not under medical treatment but had high levels of blood pressure (systolic/diastolic 160/100 mmHg or more), hemoglobin A1c/glucose 7.0% or over/corresponding glucose levels or more), LDL-cholesterol (180 mg/dL or more for men), and/or proteinuria of 2+ or more who were expected to be at a 10-year risk of 15% (18). The usual care group was under the local counseling protocols.
For the intervention group, health counseling was provided primarily by a certified public health nurse and secondarily by a clinical nurse and a certified nutritionist based on the health belief model (24), and the detail of counseling was reported elsewhere (18,25). Briefly, a trained counselor explained how high blood pressure, hyperglycemia, and hyperlipidemia damage the brain, heart, and kidney vasculature and, if untreated, could lead to the occurrence of serious health problems, including stroke, heart attack, and renal failure (perceived susceptibility) using a progression flowchart of lifestyle-related diseases, the so-called "Where am I ?" chart (i.e., risky behaviors such as high salt intake and smoking leading to the development of metabolic risk factors, preclinical vascular disorders, ischemic heart disease and stroke, bedridden status, heart failure, dialysis, dementia, blindness, and necrosis of the extremities) (Figure 2), and emphasized that these diseases would harm the counselee and their family's life physically and economically (severity) using newly developed health education flyers. The counselor then provided information regarding the benefits of visiting a physician to seek treatment (benefits) and asked about barriers that prevent clinic visits (barriers). Accordingly, the counselee is expected to make their own decisions (self-efficacy) and take the appropriate action, such as seeing a physician to seek treatment (trigger to action). The above process is in line with self-care with the support of a health worker addressed by WHO (21).
Figure 2.
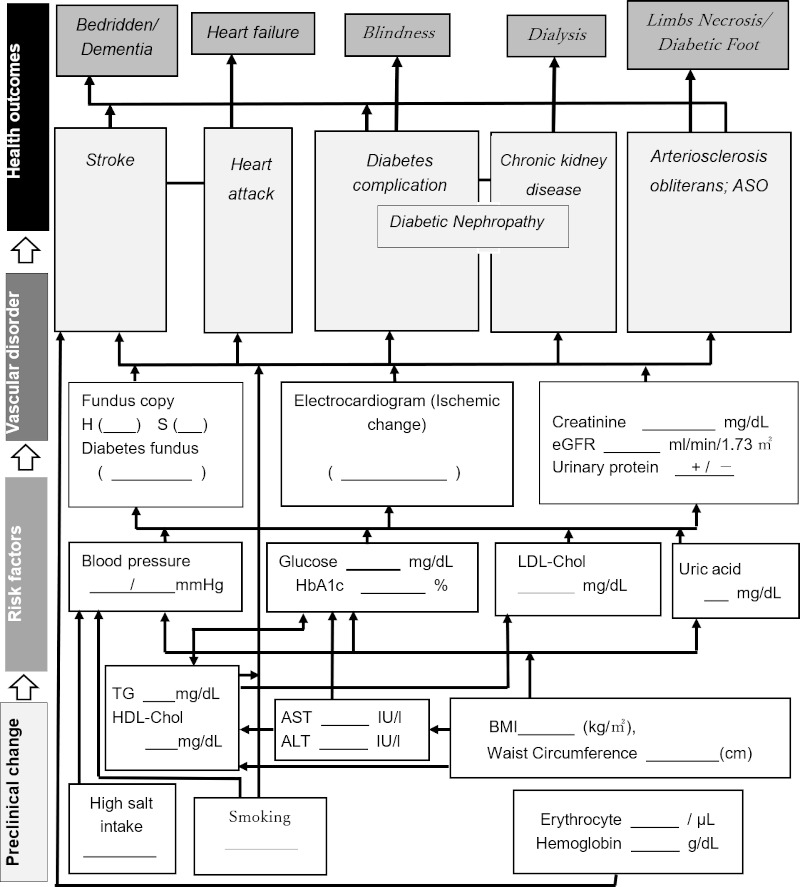
"Where am I?" Chart, a flow of disease progression. The underlined parts will be filled in by the data of each subject. Source: modified from Reference 18.
The counseling was provided three times (1-3, 4-6, and 7-9 months) after the health checks with the initial counseling primarily by home visits, secondarily through a face-to-face session at a municipal office or public health center, and tertiary telephonic counseling.
In results, the 12-month cumulative proportions of clinic visits after health checks were 58.1 (95% CI: 57.0-59.3) % vs.44.5 (43.2-45.8) %, with the probability ratio of clinic visits between the groups being 1.46 (1.24-1.72) for the total population (Figure 3), 1.48 (1.23-1.78) for hypertension, 1.34 (1.11-1.63) for diabetes, 1.67 (1.38-2.02) for dyslipidemia, and 1.25 (1.02-1.53) for proteinuria. The between-group differences between the baseline and 1-year surveys were −1.50 (−2.59, −0.41) mmHg for diastolic blood pressure in the hypertension group, −0.30% (−0.53%, −0.07%) for HbA1c in the diabetes group, −0.37 (−0.48, −0.27) mmol/L for LDL-cholesterol in the dyslipidemia group, and none for proteinuria. That trial demonstrated that standardized counseling after health checks for very high-risk individuals accelerated clinical visits and reduced levels of risk factors.
Figure 3.
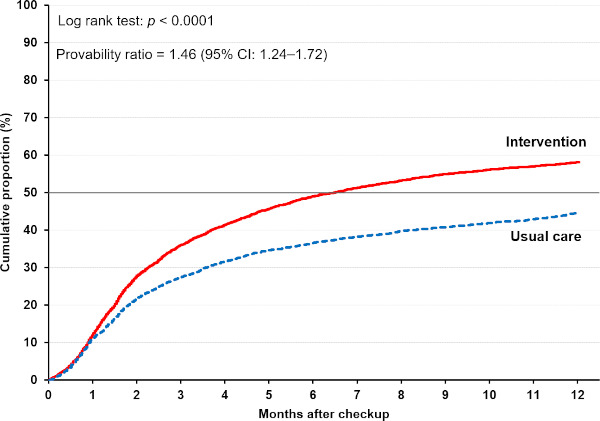
Cumulative proportions of clinic visits for participants in the intervention and usual care groups. Data Source: modified from Reference 20.
The next question is what factors of health counselor's profession (public health nurse, clinical nurse, and nutritionist), their ages, and years of counseling experience for lifestyle-related diseases achieve the larger referral. Compared to nutritionists, the cumulative proportions of clinic visits at 3, 6, and 12 months were significantly higher for public health nurses, and intermediate for nutritionists, and tended to be higher for clinical nurses (Figure 4). The probability ratios (95% CIs) of clinic visits were 1.22 (1.11-1.35) for public health nurses and 1.04 (0.90-1.20) for nurses compared with nutritionists. After adjustment for participant and counselor characteristics, initial timing, mode, and number of counseling sessions. The corresponding probability ratios (95% CIs) were 1.16 (1.05-1.29) and 1.12 (0.95-1.31), respectively. The counselor's age and years of experience did not influence clinic visits of the target population. Public health nurses were more effective in increasing clinic visits among the target population, owing to their profession-specific competency focusing on disease prevention and health promotion (26).
Figure 4.
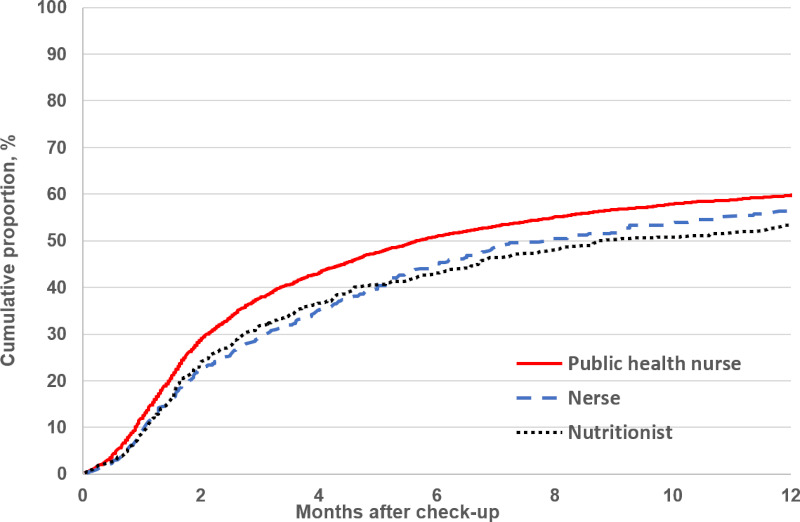
Cumulative proportions of clinic visits for participants according to health counselor's profession. Data Source: modified from Reference 25.
This trial did not report the effect of referral to physicians on the cumulative incidence of composite outcomes, i.e., hospitalization for stroke, myocardial infarction, unstable angina, chronic kidney disease, renal failure and dialysis, sudden cardiac death, and deaths from cardiovascular disease, chronic kidney disease, and renal failure) because of insufficient statistical power. Therefore, we examined the potential effect using a large observational cohort study of approximately 400 thousand very high-risk individuals (the same criteria as the above trial) from the health claims database of the Japan Health Insurance Association (27).
Our research team examined the associations between the timing of clinic visits during 12 months after health checks (early: < 3 months, intermediate: 4-6 months, late: 7-12 months, and none) and the risk of hospitalization for stroke, coronary heart disease, heart failure, or all-cause mortality.
During a median follow-up of 4.3 years, we found 15,860 composite outcomes of first hospitalization for stroke, coronary heart disease, heart failure, or all-cause mortality. Compared to very high-risk individuals without clinic visits after health checks, the adjusted hazard ratios (95% CIs) of a composite outcome were 0.78 (0.74, 0.81), 0.84 (0.78, 0.89), and 0.94 (0.89, 1.00) for early, intermediate, and late clinic visits, respectively. Similar associations were observed for hospitalization for stroke, coronary heart disease, heart failure, and all-cause mortality. The earlier clinic visit suggests lowering the risks of all individual endpoints.
Conclusions
Health counseling after the health checks is necessary not only for both persons with metabolic syndrome but also for high-risk individuals with non-obese/overweight because the population attributable risk fraction of ischemic cardiovascular disease was similar for both high-risk individuals. A randomized trial demonstrated that standardized counseling based on a health-belief model for very high-risk individuals accelerated clinical visits and reduced levels of risk factors. In health counseling, public health nurses were more effective in increasing clinic visits probably because of their profession-specific competency focusing on disease prevention and health promotion. Furthermore, a large observational prospective study indicated that the earlier clinic visit after the counseling was associated with lower risks of hospitalization for stroke, coronary heart disease, heart failure, and all-cause mortality. These epidemiological findings may be useful for health practitioners and policymakers to enhance the prevention and control of cardiovascular disease and well-being in countries with emerging cardiovascular burdens and aging.
Funding
None.
Conflict of Interest
The author has no conflicts of interest to disclose.
References
- 1. World Health Organization: The top 10 causes of death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed December 1, 2023).
- 2. Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update from the GBD 2019 study. J Am Coll Cardiol. 2020; 76:2982-3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Iso H, Maruyama K, Yamagishi K. Chronic diseases and risk factor trends in Japan: Cardiovascular inequalities. In: Health in Japan: Social Epidemiology of Japan since the 1964 Tokyo Olympics (Brunner E, Cable N, Iso H, editors). Oxford University Press. 2020; pp163-178 [Google Scholar]
- 4. Ikeda N, Saito E, Kondo N, et al. What has made the population of Japan healthy? Lancet. 2011; 378:1094-1105. [DOI] [PubMed] [Google Scholar]
- 5. The Ministry of Health, Labour and Welfare. Life Table in 2021. https://www.mhlw.go.jp/toukei/saikin/hw/life/life21/index.html (accessed December 1, 2023). (in Japanese) .
- 6. Shimamoto T, Komachi Y, Inada H, Doi M, Iso H, Sato S, Kitamura A, Iida M, Konishi M, Nakanishi N. Trends for coronary heart disease and stroke and their risk factors in Japan. Circulation. 1989; 79:503-515. [DOI] [PubMed] [Google Scholar]
- 7. Iso H. Changes in coronary heart disease risk among Japanese. Circulation. 2008; 118:2725-2729. [DOI] [PubMed] [Google Scholar]
- 8. Iso H. Cardiovascular disease, a major global burden: Epidemiology of stroke and ischemic heart disease in Japan. Glob Health Med. 2021; 3:358-364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Iso H, Shimamoto T, Naito Y, Sato S, Kitamura A, Iida M, Konishi M, Jacobs DR Jr, Komachi Y. Effects of a long-term hypertension control program on stroke incidence and prevalence in a rural community in northeastern Japan. Stroke. 1998; 29:1510-1518. [DOI] [PubMed] [Google Scholar]
- 10. Kitamura A, Sato S, Kiyama M, Imano H, Iso H, Okada T, Ohira T, Tanigawa T, Yamagishi K, Nakamura M, Konishi M, Shimamoto T, Iida M, Komachi Y. Trends in the incidence of coronary heart disease and stroke and their risk factors in Japan, 1964 to 2003: The Akita-Osaka study. J Am Coll Cardiol. 2008; 52:71-79. [DOI] [PubMed] [Google Scholar]
- 11. Yamagishi K, Sato S, Kitamura A, Kiyama M, Okada T, Tanigawa T, Ohira T, Imano H, Kondo M, Okubo I, Ishikawa Y, Shimamoto T, Iso H; CIRCS Investigators. Cost-effectiveness and budget impact analyses of a long-term hypertension detection and control program for stroke prevention. J Hypertens. 2012; 30:1874-1879. [DOI] [PubMed] [Google Scholar]
- 12. Yamagishi K, Sankai T, Muraki I, Umesawa M, Cui R, Imano H, Kihara T, Noda H, Ikeda A, Ohira T, Tanigawa T, Kitamura A, Sato S, Kiyama M, Iso H. Trends in stroke, cardiovascular disease, and medical expenditure under a community-based long-term stroke prevention program. J Hypertens. 2023; 41:429-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kohro T, Furui Y, Mitsutake N, Fujii R, Morita H, Oku S, Ohe K, Nagai R. The Japanese National Health Screening and Intervention Program aimed at preventing worsening of the metabolic syndrome. Int Heart J. 2008; 49:193-203. [DOI] [PubMed] [Google Scholar]
- 14. Matsuzawa Y, Funahashi T, Nakamura T. Molecular mechanism of metabolic syndrome X: Contribution of adipocytokines, adipocyte-derived bioactive substances. Ann N Y Acad Sci. 1999; 892:146-154. [DOI] [PubMed] [Google Scholar]
- 15. The Ministry of Health, Labour and Welfare. Patient Survey in 2020. https://www.mhlw.go.jp/toukei/list/10-20.html (accessed December 1, 2023). (in Japanese) .
- 16. Iso H, Sato S, Kitamura A, Imano H, Kiyama M, Yamagishi K, Cui R, Tanigawa T, Shimamoto T. Metabolic syndrome and the risk of ischemic heart disease and stroke among Japanese men and women. Stroke. 2007; 38:1744-1751. [DOI] [PubMed] [Google Scholar]
- 17. Noda H, Iso H, Saito I, Konishi M, Inoue M, Tsugane S. The impact of the metabolic syndrome and its components on the incidence of ischemic heart disease and stroke: the Japan public health center-based study. Hypertens Res. 2009; 32:289-298. [DOI] [PubMed] [Google Scholar]
- 18. Noguchi M, Kojima S, Sairenchi T, Kinuta M, Yamakawa M, Nishizawa H, Takahara M, Imano H, Kitamura A, Yoshida T, Shintani A, Saito I, Yokoyama T, Shimomura I, Iso H. Japan Trial in High-Risk Individuals to Enhance Their Referral to Physicians (J-HARP)-A nurse-led, community-based prevention program of lifestyle-related disease. J Epidemiol. 2020; 30:194-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Iso H, Cui R, Takamoto I, et al. Risk classification for metabolic syndrome and the incidence of cardiovascular disease in Japan with low prevalence of obesity: A pooled analysis of 10 prospective cohort studies. J Am Heart Assoc. 2021; 10:e020760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Iso H, Noguchi M, Yokoyama T, Yoshida T, Saito I, Shintani A, Sairenchi T, Nishizawa H, Imano H, Kitamura A, Shimomura I. Effect of a community-based program to accelerate referral to physicians for individuals at high-risk of lifestyle-related diseases: A cluster randomized trial. J Atheroscler Thromb. 2023; 30:1389-1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. World Health Organization. Self-care interventions for health. https://www.who.int/news-room/fact-sheets/detail/self-care-health-interventions#:~:text=WHO%E2%80%99s%20definition%20of%20self-care%20is%20the%20ability%20of,or%20without%20the%20support%20of%20a%20health%20worker (accessed December 1, 2023).
- 22. Nakatani H. Population aging in Japan: policy transformation, sustainable development goals, universal health coverage, and social determinants of health. Glob Health Med. 2019; 1:3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009; 120:1640-1645. [DOI] [PubMed] [Google Scholar]
- 24. Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988; 15:175-183. [DOI] [PubMed] [Google Scholar]
- 25. Noguchi M, Kinuta M, Sairenchi T, Yamakawa M, Koide K, Katsura S, Matsuo K, Omote S, Imano H, Nishizawa H, Shimomura I, Iso H, On Behalf Of The J-Harp Research Group. Relationship between health counselor characteristics and counseling impact on individuals at high-risk for lifestyle-related disease: Sub-analysis of the J-HARP cluster-randomized controlled trial. Int J Environ Res Public Health. 2022; 19:6375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nigenda G, Magaña-Valladares L, Cooper K, Ruiz-Larios JA. Recent developments in public health nursing in the Americas. Int J Environ Res Public Health. 2010; 7:729-750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dong JY, Iso H, Muraki I, Tanaka M, Imano H. Timing of clinic visits after health checks and risk of hospitalization for cardiovascular events and all-cause death among the high-risk population. Atherosclerosis. 2023; 388:117409. [DOI] [PubMed] [Google Scholar]


