Highlights
-
•
Patient experience and model of care is different in an MR-linac vs C-arm linac.
-
•
Patient reported anxiety in MR-linac was low.
-
•
Patients highly satisfied with their cancer care involving the MR-linac.
Keywords: MR-linac, Adaptive radiotherapy, Anxiety, Patient experience
Abstract
Purpose
An integrated magnetic resonance scanner and linear accelerator (MR-linac) was implemented with daily online adaptive radiation therapy (ART). This study evaluated patient-reported experiences with their overall hospital care as well as treatment in the MR-linac environment.
Methods
Patients pre-screened for MR eligibility and claustrophobia were referred to simulation on a 1.5 T MR-linac. Patient-reported experience measures were captured using two validated surveys. The 15-item MR-anxiety questionnaire (MR-AQ) was administered immediately after the first treatment to rate MR-related anxiety and relaxation. The 40-item satisfaction with cancer care questionnaire rating doctors, radiation therapists, the services and care organization and their outpatient experience was administered immediately after the last treatment using five-point Likert responses. Results were analyzed using descriptive statistics.
Results
205 patients were included in this analysis. Multiple sites were treated across the pelvis and abdomen with a median treatment time per fraction of 46 and 66 min respectively. Patients rated MR-related anxiety as “not at all” (87%), “somewhat” (11%), “moderately” (1%) and “very much so” (1%). Positive satisfaction responses ranged from 78 to 100% (median 93%) across all items. All radiation therapist-specific items were rated positively as 96–100%. The five lowest rated items (range 78–85%) were related to general provision of information, coordination, and communication. Overall hospital care was rated positively at 99%.
Conclusion
In this large, single-institution prospective cohort, all patients had low MR-related anxiety and completed treatment as planned despite lengthy ART treatments with the MR-linac. Patients overall were highly satisfied with their cancer care involving ART using an MR-linac.
Introduction
Radiotherapy linacs integrated with MR imaging (MR-linac) offer technological advances over conventional cone-beam CT-guided linacs, enabling improved soft tissue contrast, continuous intrafraction imaging and online adaptive radiotherapy (ART) [1], [2], [3]. The ability to define targets and organs-at-risk and account for their daily variations in position has allowed for dose-escalation and stereotactic treatment in the abdomen and pelvis which was previously limited with conventional treatment [4], [5], [6]. Although MR-guided online ART has now been shown to be clinically feasible and safe, it poses new burdens to patients and challenges to the team delivering high-quality care.
Compared to conventional linac delivery, online ART using MR-linac often requires patients to undergo lengthy treatments within a closed bore. This requires further consideration to manage patients’ control of pain, anxiety and claustrophobia. Discomfort during extended fractions can result in significant patient motion or in extreme cases failure to complete the radiotherapy course [7], [8], [9]. Few recent MR-linac studies have focused on physical patient comfort and reported general tolerability of the treatment position, but have focused less on MR-related anxiety [10], [11], [12]. Individualizing support and the provision of information for the MR-linac will ensure care with this advanced technology is patient-centered.
The model-of-care for online ART additionally differs from standard external-beam radiotherapy as daily treatment is often delivered by a small, consistent multi-disciplinary team of radiation therapists (RTT), medical physicists and radiation oncologists (RO). The impact on patient experiences of these substantial differences to conventional care merit further investigation. This study aimed to evaluate patient-reported outcomes and experience measures with the care they received during ART using MR-linac.
Materials and Methods
Clinical workflow with MR-linac
As part of standard care, RO assessed patients for MR safety, history of claustrophobia and suitability for MR-guided ART using a 1.5 T MR-linac (Unity, Elekta AB Stockholm, Sweden). Following the initial consultation, patients were scheduled for radiotherapy simulation and treatment on the MR-linac. Each patient received a 1-on-1 patient education session with an RTT via telephone one day prior to simulation. The information covered tumor-site specific procedures at simulation and treatment, patient preparation instructions and logistics of the hospital, such as parking and the check in process. Patients were encouraged to ask questions and guide the discussion.
Patients with upper abdominal targets first underwent kV fluoroscopy on a conventional linac to evaluate diaphragm breathing motion with an MR-compatible abdominal compression belt (Orfit Industries, Wijnegem, Belgium) [13]. Those with motion < 15 mm were eligible for MR-linac simulation (MRL-sim) while others were planned to be treated on a conventional linac with or without motion management (i.e., compression or active breath-hold device) [13].
For MRL-sim all patients were screened for MR safety by an RTT dual-certified in MR, in a dedicated area (American College of Radiology Zone II) prior to being brought into the Zone III and Zone IV areas of the MR-linac facility (Fig. 1). The duration of MRL-sim scans ranged from 2 to 3 min for high resolution imaging and from 2 to approximately 5 min when navigator-triggered exhale images were required for the upper abdomen [13]. The median length of time the patient was in the MRL room was 27 and 41 min for pelvic and abdominal targets respectively. All patients were positioned supine with hands on chest or by side. Immobilization included leg support for pelvic patients and an abdominal compression belt for abdominal patients (Fig. 2). MRL-sim included assessment to determine suitability of MR-guided ART such as patients' ability to lay on the treatment bed for extended time periods as well as target motion and visibility. This session was followed by CT- and multiphasic 3T MR-simulation when indicated for electronic densities and to aid in target delineation.
Fig. 1.
MR-linac facility showing the American College of Radiology Zone II patient screening area (left) and Zone III console area (right).
Fig. 2.
Patient positioning for pelvic (left) and abdominal (right) treatments.
The daily MR-guided ART procedure included a team of 3 RTTs, 1 medical physicist, and 1 RO. Prior to the first treatment patients were re-screened by RTT dual-certified in MR and the process of daily adaption as well estimated treatment time was explained to the patient. Institutional workflows for the main sites treated in the pelvis and the upper abdomen have been detailed previously [13], [14]. Time of entry and exit of the MRL room was used to record overall times for both simulation and treatment. Other appointments and patient care while on treatment followed departmental standard of daily point of care assessments by the RTTs as well as weekly review with the RO.
Prospective research study
All patients ≥ 18 years of age treated with the MR-linac who provided informed consent were eligible for this single-institution, research ethics board-approved, observational study (ClinicalTrials.gov ID NCT04135794). Patients already enrolled on other interventional clinical trials involving RT were often not approached for the current study for pragmatic reasons. For research, two validated patient-reported measures were captured.
The MR-anxiety questionnaire (MR-AQ) asked patients to rate 15 anxiety statements as “not at all”, “somewhat”, “moderately” or “very much so” [15]. These can be further broken down into two subscales; items about anxiety symptoms (12 questions) and items about relaxation symptoms (3 questions) [15]. Each item was converted to a 4-point scale and summed per patient (range 15–60). Higher total scores indicate higher anxiety. MR-AQ was administered immediately after the first treatment. Per item scores, as well as total, anxiety- and relaxation-subscale scores were evaluated with descriptive statistics.
The satisfaction with outpatient cancer care questionnaire (EORTC PATSAT-C33 and OUT-PATSAT7) was administered immediately after the last treatment [16]. Patients rated 40-items using five-point Likert-type responses in terms of their experience with their doctors, RTTs, the services and care organization and their outpatient experience. The results were evaluated using descriptive statistics. “Excellent” plus “very good” responses per-item were considered positive. The lowest-scoring items were reported to identify opportunities to improve patient experience.
Subgroup differences in these patient reported outcomes and experiences were explored between patients treated for upper abdomen vs. pelvis targets, using unadjusted Wilcoxon rank-sum tests with p < 0.05 denoting a significant difference. These groups were chosen given their differences in radiotherapy immobilization (abdominal compression vs. none), and presumed medical care pathways as they were largely comprised of different tumor sites within each group (upper gastrointestinal vs. genitourinary cancers).
Results
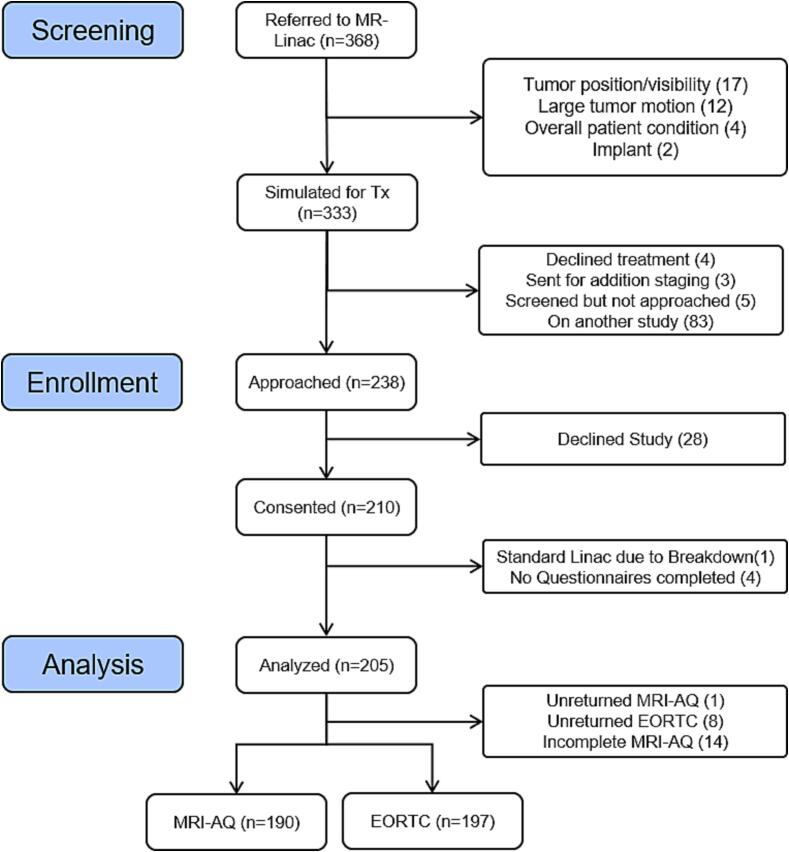
Between March 2019 and June 2023, 368 patients were referred for treatment with the MR-linac. The patient flow for clinical care and for research is shown in Fig. 3. Two patients failed MR-safety screening just prior to MRL-sim due to incompatible metal implants. Forty patients underwent MRL-sim but did not receive MR-linac treatment. This was most often due to difficult tumor position/visibility (n = 17) or large residual tumor motion with compression (n = 12), although four were unable to complete the simulation appointment due to their overall condition. Of these 4, one was unable to tolerate the abdominal compression belt, two could not lay still for the duration due to pain and coughing, and one had a large body habitus. Additionally, four ultimately declined radiotherapy altogether and three were deferred while completing additional staging.
Fig. 3.
Patient flow diagram.
Two hundred and ten patients consented to the study and completed surveys from 205 patients were included in this analysis. No patients were withdrawn from the study after initial consent, although 4 patients failed to complete both questionnaires. Nineteen patients were of female (9 %) and 186 of male (91 %) biological sex, with a median age of 71 years (range 27–94 years). Treated sites were prostate (n = 119, 58 %), pancreas (n = 26, 13 %), liver (n = 19, 9 %), oligometastatic-lymph nodes (n = 26, 13 %), bone metastases (n = 7, 3 %), kidney (n = 4, 2 %) and other (n = 4, 2 %). Prescribed radiotherapy courses are in Table 1. The number of fractions ranged from 1 to 7 (median 6). The median (range) patient time on the MR-linac couch per fraction was 46 (31–113) and 66 (38–114) minutes for pelvis and upper abdominal treatments respectively.
Table 1.
Prescribed radiotherapy courses treated on MR-linac.
| Site | Dose/Fractionation (Number of patients) | |
|---|---|---|
| Prostate | 25–36.25 Gy/5 | (4) |
| 36–48 Gy/6 | (15) | |
| 42.7 Gy/7 | (93) | |
| 15 Gy/1 + 30 Gy/5 | (7) | |
| Pancreas | 42 Gy/3 | (1) |
| 30–45 Gy/5 | (25) | |
| Liver | 16–30 Gy/1 | (3) |
| 21–30 Gy/3 | (5) | |
| 27.5–45 Gy/5 | (11) | |
| Oligo LN | 30 Gy/3 | (12) |
| 30–40 Gy/5 | (14) | |
| Bone Mets | 30 Gy/3 | (2) |
| 35–50 Gy/5 | (5) | |
| Kidney | 35–40 Gy/5 | (4) |
| Other | 30–50 Gy/5 | (4) |
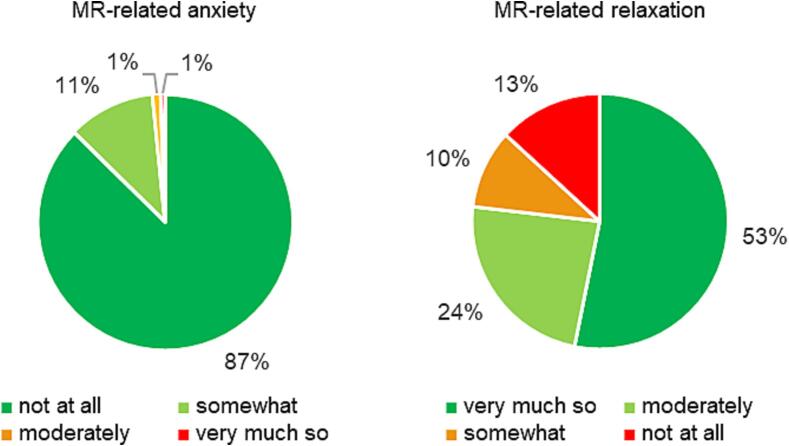
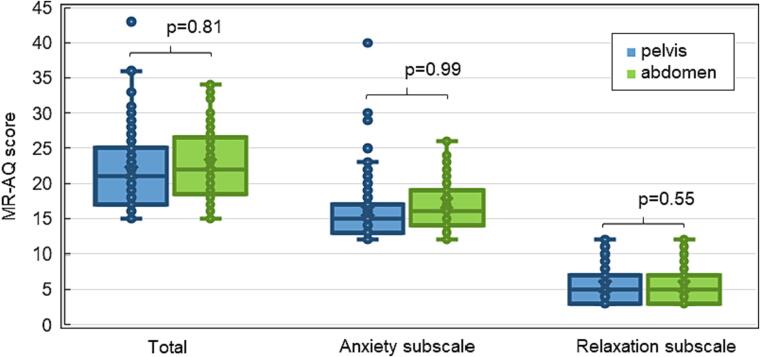
Of the 205 patients, 204 returned MR-AQ questionnaires; 14 were incomplete and were excluded from analysis. The median (inter-quartile range [IQR]) total MR-AQ score for all 190 patients included was 21(17–26), indicating a low level of MR-related anxiety overall. The full distribution of MR-AQ responses per item is shown in Appendix A. The median response for each patient was calculated per subscale. As seen in Fig. 4, the patients’ median MR-related anxiety was “not at all” (87 %). Only 1 % (n = 1) scored as “very much so” and this prostate patient also reported the only ‘very much so’ responses for ‘I panicked’, ‘I was afraid’, and ‘I found it hard to breathe’ but otherwise completed treatment without incident. Patients rated relaxation scores in a more distributed manner with 53 % “very much so”, 24 % “moderately”, 10 % “somewhat” and 13 % “not at all” being relaxed. The difference in total or subscale MR-AQ score were not statistically significant when comparing pelvis treatments to abdominal treatments using the compression belt (Fig. 5).
Fig. 4.
Self-reported MR-related anxiety (MR-AQ) subscales (median rating per patient).
Fig. 5.
MR-related anxiety (overall and subscales) for patients treated with MR-linac to the pelvis or upper abdomen. Outliers are 1.5 times the inter-quartile range.
Patient experience questionnaires from 197 patients were analyzed. Positive satisfaction responses ranged from 78 to 100 % (median 93 %) across all items. Itemized responses are shown in Appendix B. The proportion of positive responses pooled from 10 questions related to the ROs was 95 % (range 91–95 %). The 7 questions about satisfaction with RTTs had the highest proportion of positive responses of any section at 99 % (range 96–100 %). The proportion of positive responses was lowest for the outpatient experience (7 questions) at 89 % (range 79–92 %). For 16 questions associated with services and care organization, responses were 92 % positive (range 78–99 %). The most favorable response in this section was 99 % for ‘How would you rate the care you received in this hospital?’.
Overall, the 5 questions with the lowest proportion of positive results (range 78–85 %) were for ‘The ease of access (parking, means of transport, etc.)?’, ‘The ease of communicating with the hospital services from home?’, ‘The information provided on the overall supportive services?’, ‘The information on who to contact if you are worried after you leave your hospital appointment?’ and ‘The information provided by doctors, nurses and other caregivers on things you could do to improve your health or prevent illness?’.
Questionnaire results were further compared between treatment sites in the pelvis versus the upper abdomen. Differences in positive satisfaction between groups were small overall (mean absolute difference 3.6 %, range 0–12 %). The largest per-item satisfaction difference was the information exchange with community care services (12 % lower for the pelvis group, p = 0.128). Of the 40 items only ‘the advice they gave you on managing your physical symptoms’ (p = 0.025), ‘the kindness and helpfulness of the technical, reception, laboratory personnel’ (p = 0.025) and ‘the waiting time for undergoing medical tests and/or treatments’ (p = 0.022) were significantly higher in patients with pelvis vs abdominal cancers.
Discussion
Recent studies have focused on patients’ physical MR-linac experience, such as feeling cold, nerve stimulation and noise with only a single question or two aimed at directly understanding anxiety [10], [11], [12]. This larger study aimed to move beyond the patient’s established acceptance of environmental factors related to the presence of the magnet (e.g., noise or temperature) and focus on several aspects of MR-related patient anxiety. This was also the aim of Barnes et al., who evaluated 170 patients across an international, multi-institution analysis using an MR-linac specific survey [17]. However, the strength of the current trial is the large prospective cohort of patients treated in a single institution, in a uniform manner. All patients included in this analysis were treated with the same online adaptive workflow in the same high-field MR-linac. Another strength is the evaluation of patient experience using a validated, widely available survey for outpatient cancer care that is not limited to use for MR-linac radiotherapy. This facilitates future comparisons to other technologies or models-of-care within radiotherapy, and other cancer treatment modalities. Unfortunately, previous radiotherapy studies using this tool failed to report item-specific, or section-specific results [16], [18], [19].
Despite potential concerns about the closed MR-linac environment, in this study 87 % of patients rated their MR-related anxiety as ‘not at all’ and only one patient as ‘very much so’, which is comparable to other reports [11], [17]. The low MR-AQ scores for both pelvic and abdominal patients suggests the restrictive feeling of the compression belt had little impact on anxiety. The question with the greatest incidence of high-anxiety response was ‘Self-control was required when going through the examination’ and may be linked to fear of moving while holding still in the treatment position for extended times. This contrasts with Barnes et al, who reported the poorest patient responses for ‘I needed more detailed information before my treatment’ [17].
The median treatment time of 47 min is similar to the 40–50 min diagnostic MR scans undergone by Ahlander et al’s patients [15]. Their study used the same MR-AQ and reported slightly higher scores for patients undergoing diagnostic MR of heart or spine. A subsequent study by Ahlander et al reported a 20.5 median MR-AQ score specifically for a 70 cm diagnostic MR bore size, which is the same as the current study of the MR-linac which also has a 70 cm bore [20]. In very rare instances, upper abdominal patients at our institution also took anxiolytic medications to aid in reducing breathing motion [13] although this would not explain the overall low prevalence of MR-related anxiety. Overall, low anxiety in the current study is likely due to a combination of upstream exposure to MR during diagnosis and staging and MRL-sim, and the referral process for MR-linac, given no patients had anxiety issues at the MR-linac.
Satisfaction with the RTTs was the highest of any section at 99 %. In fact, 6 of the 7 highest ranking questions were about the RTTs. These positive results could be due to the small team trained on the MR-linac, allowing the patients to see the same RTTs daily. This may change the way they perceive the time spent at the MR-linac as patients grow to know the RTT and what to expect. Additionally, patient education was done both prior to MRL-sim and first treatment, which has been shown to reduce anxiety and increase satisfaction [21]. The MR-linac experience also allows the patients to feel a more personalized touch with a private changing area, the experience of walking through the console area and seeing the entire team there to support them (Fig. 1) and being able to choose their own music to listen to during the procedure. A systematic review revealed that the quality of engagement with RTTs is one of the strongest predictors of overall satisfaction with radiotherapy [22].
The least positive responses were peripheral to the MR-linac experience and related to the patient's experience with logistics such as parking, which are seemingly unavoidable in a large city center. The second was rating the ease of communicating with the hospital services from home. New steps have already been implemented independently of this study to improve the patient experience in these areas, including an updated patient portal with messaging system and direct phone line to the treatment unit. The next lowest rated items were related to inter-departmental communication or referrals. This suggests a general satisfaction with the care received at the hospital but a desire for better after treatment care, support and follow-up.
Minor limitations of the current study include a lack of control group outside the MR-linac for comparison, and the possible patient selection bias given the referral pathways to MR-linac and effort towards patient education described above. As a result of our referral pathways, over 80 % of patients referred to MR-linac treatment have a diagnosis of prostate cancer whether referral is for primary or oligometastatic disease. This creates a limitation for our study as the potential population is primarily biologically male, in fact only 9 % of our participants were biologically female. Futhermore, MR-anxiety was assessed not at the patient’s first experience with the machine (MRL-sim) but after first treatment as it is assumed the longer MR-linac treatment would have higher anxiety than the relatively shorter MRL-sim session which may be an additional limitation. Future directions include comparing patient’s satisfaction across radiotherapy treatment platforms. Whiteside et al., reported no statistically significant difference between prostate patients treated on the MR-linac versus C-arm linac, but a larger study including a variety of treatment sites would be valuable [23]. Perhaps future efforts should develop care MR-linac pathways for patients with more substantial MR-related anxiety at baseline, in order to expand its benefits to more patients. Finally, our patient-centered outcomes captured using tools not specific to MR-linac may be crucial in evaluating other radiotherapy innovations and establishing value-based care [24].
Conclusion
In this large, single-institution prospective cohort, all patients had low MR-related anxiety and completed treatment as planned despite lengthy ART treatments with the MR-linac. A few opportunities to improve patient satisfaction were identified, largely around coordination between the radiation team with other care teams or resources. Overall, patients were highly satisfied with their cancer care involving ART on the MR-linac.
CRediT authorship contribution statement
Amanda Moreira: Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. Winnie Li: Investigation, Data curation, Writing – review & editing. Alejandro Berlin: Investigation, Writing – review & editing. Cathy Carpino-Rocca: Investigation, Data curation, Writing – review & editing. Peter Chung: Investigation, Writing – review & editing. Leigh Conroy: Investigation, Writing – review & editing. Jennifer Dang: Investigation, Data curation, Writing – review & editing. Laura A. Dawson: Investigation, Writing – review & editing. Rachel M. Glicksman: Investigation, Writing – review & editing. Ali Hosni: Investigation, Writing – review & editing. Harald Keller: Investigation, Writing – review & editing. Vickie Kong: Investigation, Data curation, Writing – review & editing. Patricia Lindsay: Investigation, Writing – review & editing. Andrea Shessel: Investigation, Data curation, Writing – review & editing. Teo Stanescu: Investigation, Writing – review & editing. Edward Taylor: Investigation, Writing – review & editing. Jeff Winter: Investigation, Writing – review & editing. Michael Yan: Investigation, Writing – review & editing. Daniel Letourneau: Conceptualization, Investigation, Methodology, Writing – review & editing. Michael Milosevic: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Writing – review & editing. Michael Velec: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was funded by the Radiation Medicine Program. The authors thank the clinical multidisciplinary MR-linac team and the study coordinators Edel Sexton and Melissa Bartolo-Rego for their support. Facility photos are from Kelvin Young Photography.
Appendix.
Appendix A. . Total MR-AQ distribution
| Item | Item score distribution (%) (Higher score will then indicate higher level of anxiety) |
|||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| *1. I felt that I controlled the situation | 50.5 | 23.2 | 11.6 | 14.7 |
| 2. I had palpitation | 92.6 | 5.8 | 0.5 | 1.1 |
| 3. I found it hard to breathe | 90.0 | 9.0 | 0.5 | 0.5 |
| 4. I was afraid | 87.9 | 9.5 | 2.1 | 0.5 |
| 5. I wanted to come out | 84.7 | 12.63 | 1.6 | 1.1 |
| 6. I panicked | 96.3 | 3.2 | 0.0 | 0.5 |
| *7. I felt relaxed | 46.8 | 24.7 | 15.3 | 13.2 |
| *8. I felt safe | 69.5 | 9.5 | 4.8 | 16.3 |
| 9. I worried in advance | 53.2 | 30.0 | 12.7 | 4.2 |
| *10. I felt calm | 50.5 | 20.5 | 11.1 | 17.9 |
| 11. I had to force myself to manage the situation | 72.1 | 18.4 | 6.8 | 2.6 |
| 12. Self-control was required when going through the examination | 54.7 | 20.0 | 13.7 | 11.6 |
| 13. I needed support and encouragement | 70.5 | 21.1 | 6.3 | 2.1 |
| 14. I wished to have someone with me | 87.9 | 8.4 | 1.1 | 2.6 |
| 15. I needed more detailed information | 76.3 | 16.3 | 3.7 | 3.7 |
| Total | 72.3 | 15.5 | 6.1 | 6.2 |
*Questions have been inverted.
Appendix B. . Itemized satisfaction survey results
| Item | Item score distribution (%) |
|||||
|---|---|---|---|---|---|---|
| Fair | Poor | Good | Very Good | Excellent | N/A | |
| ABOUT YOUR RADIATION ONCOLOGIST 1. Their awareness of the care and treatment you received previously? |
0.0 | 0.5 | 2.0 | 18.9 | 70.9 | – |
| 2. The attention they gave to your physical symptoms? | 0.0 | 0.6 | 2.2 | 20.4 | 76.8 | 7.7 |
| 3. Their thoroughness in treating your physical symptoms? | 0.0 | 0.0 | 1.5 | 18.9 | 66.8 | 12.8 |
| 4. The information they gave you about your illness? | 0.0 | 1. | 5.1 | 15.3 | 75.5 | 2.6 |
| 5. The information they gave you about your medical tests and Treatment? | 0.0 | 0.0 | 5.1 | 17. | 76.6 | 1.0 |
| 6. The attention they gave to your opinion about the choice of your treatment (in case of possible choices)? | 0.0 | 1.0 | 5.1 | 16.8 | 67.3 | 9.7 |
| 7. The interest they showed in you as a person? | 0.0 | 1.0 | 5.1 | 14.7 | 79.2 | – |
| 8. The comfort and support they gave you? | 0.0 | 0.5 | 4.6 | 12.7 | 82.2 | – |
| 9. The frequency of their visits/consultations? | 0.0 | 0.0 | 9.8 | 24.2 | 66.0 | – |
| 10. The time they devoted to you? | 0.0 | 0.0 | 7.6 | 19.3 | 73.1 | – |
| ABOUT YOUR RADIATION THERAPISTS 11. The attention they gave to your physical comfort? |
0.0 | 0.0 | 1.0 | 6.6 | 91.4 | 1.0 |
| 12. The information they gave you about your care and treatment? | 0.0 | 0.0 | 1.0 | 15. | 82.7 | 0.5 |
| 13. The advice they gave you on managing your physical symptoms? | 0.0 | 0.5 | 3.0 | 13.7 | 76.6 | 6.1 |
| 14. The interest they showed in you as a person? | 0.0 | 0.0 | 1.0 | 9.1 | 89.8 | – |
| 15. The comfort and support they gave you? | 0.0 | 0.0 | 0.5 | 8.6 | 90.4 | 0.5 |
| 16. Their promptness in answering your specific requests? | 0.0 | 0.0 | 0.5 | 10.2 | 88.3 | 1.0 |
| 17. The time they devoted to you? | 0.0 | 0.0 | 0.0 | 11.2 | 88.8 | 0.0 |
| ABOUT THE SERVICES & CARE ORGANIZATION 18. The ease of recognizing the roles and responsibilities of the different caregivers (doctors, nurses, physiotherapists, psychologists, etc.) involved in your care? |
0.5 | 1.0 | 7.6 | 31.5 | 59.4 | – |
| 19. The exchange of information between the different caregivers (doctors, nurses, physiotherapists, psychologists, etc.)? | 0.0 | 0.5 | 8.2 | 27.7 | 63.6 | – |
| 20. The way doctors, nurses and other caregivers involved in your care seem to work together as a team? | 0.0 | 0.5 | 4.1 | 20.9 | 74.0 | 0.5 |
| 21. The exchange of information with other care services in the community (general practitioner, home care, nursing house, social services, etc.)? | 0.0 | 0.5 | 6.3 | 18.8 | 34.4 | 40.1 |
| 22. The kindness and helpfulness of the technical, reception, laboratory personnel, etc.? | 0.0 | 0.5 | 1.0 | 15.3 | 83.2 | – |
| 23. The information provided on the scheduling of medical tests, treatment or care? | 0.0 | 0.5 | 3.6 | 21.0 | 74.9 | – |
| 24. The information provided on the overall supportive services? | 2.7 | 1.1 | 12.3 | 28.3 | 55.6 | – |
| 25. The information provided by doctors, nurses and other caregivers on things you could do to improve your health or prevent illness? | 2.1 | 3.2 | 10.1 | 28.0 | 56.1 | 0.5 |
| 26. The waiting time for obtaining results of medical tests? | 0.5 | 0.5 | 6.2 | 16.1 | 66.8 | 9.8 |
| 27. The waiting time for undergoing medical tests and/or treatments? | 0.0 | 2.1 | 4.2 | 28.6 | 65.1 | – |
| 28. The privacy given when you were examined or treated? | 0.0 | 1.0 | 1.0 | 12.4 | 85.0 | 0.5 |
| 29. The opportunity for your family or those close to you to be involved in your care (talking to doctors, receiving disease and care information, etc.)? | 1.0 | 0.0 | 4.2 | 15.7 | 49.7 | 29.3 |
| 30. The ease of access (parking, means of transport, etc.)? | 3.1 | 5.2 | 14.1 | 29.7 | 47.9 | – |
| 31. The ease of finding your way to the different departments in the hospital? | 0.0 | 0.5 | 6.7 | 31.6 | 61.1 | – |
| 32. The environment of the building (cleanness, spaciousness, calmness, etc.)? | 0.0 | 0.0 | 3.1 | 165 | 80.4 | – |
| 33. How would you rate the care you received in this hospital? | 0.0 | 0.0 | 1.0 | 7.8 | 91.2 | – |
| ABOUT OUTPATIENT EXPERIENCE 1. The opportunity to see the same caregivers when you come to the outpatient clinic? |
0.5 | 0.0 | 9.1 | 27.8 | 62.6 | – |
| 2. The ease of arranging medical appointments at convenient times? | 0.6 | 1.1 | 6.7 | 28.9 | 62.8 | – |
| 3. The waiting time before obtaining a medical appointment? | 0.0 | 1.6 | 11.2 | 25.0 | 62.2 | – |
| 4. The ease of communicating with the hospital services from home? | 1.6 | 7.5 | 12.3 | 28.9 | 48.7 | – |
| 5. The information provided about what you should/ should not do after you leave your hospital appointment? | 1.1 | 1.1 | 12.0 | 28.3 | 57.6 | – |
| 6. The information on who to contact if you are worried after you leave your hospital appointment? | 1.6 | 2.7 | 11.8 | 27.3 | 56.7 | – |
| 7. The provision of follow-up by the different caregivers (doctors, nurses, physiotherapists, psychologists, etc.) after treatment? | 1.1 | 0.5 | 9.8 | 27.2 | 61.4 | – |
References
- 1.Bertelsen A.S., Schytte T., Møller P.K., Mahmood F., Riis H.L., Gottlieb K.L., et al. First clinical experiences with a high field 1.5 T mr linac. Acta Oncol. 2019;58(10):1352–1357. doi: 10.1080/0284186x.2019.1627417. [DOI] [PubMed] [Google Scholar]
- 2.Lagendijk J.J., Raaymakers B.W., Van den Berg C.A., Moerland M.A., Philippens M.E., van Vulpen M. MR guidance in radiotherapy. Phys Med Biol. 2014;59(21):R349–R369. doi: 10.1088/0031-9155/59/21/R349. [DOI] [PubMed] [Google Scholar]
- 3.Pollard J.M., Wen Z., Sadagopan R., Wang J., Ibbott G.S. The future of image-guided radiotherapy will be MR guided. Br J Radiol. 2017;90(1073):20160667. doi: 10.1259/bjr.20160667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall W.A., Paulson E., Li X.A., Erickson B., Schultz C., Tree A., et al. Magnetic resonance linear accelerator technology and adaptive radiation therapy: an overview for clinicians. CA Cancer J Clin. 2022;72(1):34–56. doi: 10.3322/caac.21707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bohoudi O., Bruynzeel A.M.E., Meijerink M.R., Senan S., Slotman B.J., Palacios M.A., et al. Identification of patients with locally advanced pancreatic cancer benefiting from plan adaptation in MR-guided radiation therapy. Radiother Oncol. 2019;132:16–22. doi: 10.1016/j.radonc.2018.11.019. [DOI] [PubMed] [Google Scholar]
- 6.Henke L., Kashani R., Robinson C., Curcuru A., DeWees T., Bradley J., et al. Phase I trial of stereotactic MR-guided online adaptive radiation therapy (SMART) for the treatment of oligometastatic or unresectable primary malignancies of the abdomen. Radiother Oncol. 2018;126(3):519–526. doi: 10.1016/j.radonc.2017.11.032. [DOI] [PubMed] [Google Scholar]
- 7.Purdie T.G., Bissonnette J.P., Franks K., Bezjak A., Payne D., Sie F., et al. Cone-beam computed tomography for on-line image guidance of lung stereotactic radiotherapy: localization, verification, and intrafraction tumor position. Int J Radiat Oncol Biol Phys. 2007;68(1):243–252. doi: 10.1016/j.ijrobp.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 8.Peguret N., Dahele M., Cuijpers J.P., Slotman B.J., Verbakel W.F. Frameless high dose rate stereotactic lung radiotherapy: intrafraction tumor position and delivery time. Radiother Oncol. 2013;107(3):419–422. doi: 10.1016/j.radonc.2013.04.019. [DOI] [PubMed] [Google Scholar]
- 9.Hoogeman M.S., Nuyttens J.J., Levendag P.C., Heijmen B.J. Time dependence of intrafraction patient motion assessed by repeat stereoscopic imaging. Int J Radiat Oncol Biol Phys. 2008;70(2):609–618. doi: 10.1016/j.ijrobp.2007.08.066. [DOI] [PubMed] [Google Scholar]
- 10.Tetar S., Bruynzeel A., Bakker R., Jeulink M., Slotman B.J., Oei S., et al. Patient-reported outcome measurements on the tolerance of magnetic resonance imaging-guided radiation therapy. Cureus. 2018;10(2):e2236. doi: 10.7759/cureus.2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klüter S., Katayama S., Spindeldreier C.K., Koerber S.A., Major G., Alber M., et al. First prospective clinical evaluation of feasibility and patient acceptance of magnetic resonance-guided radiotherapy in Germany. Strahlenther Onkol. 2020;196(8):691–698. doi: 10.1007/s00066-020-01578-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sayan M., Serbez I., Teymur B., Gur G., Zoto Mustafayev T., Gungor G., et al. Patient-reported tolerance of magnetic resonance-guided radiation therapy. Front Oncol. 2020;10:1782. doi: 10.3389/fonc.2020.01782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stanescu T., Shessel A., Carpino-Rocca C., Taylor E., Semeniuk O., Li W., et al. MRI-guided online adaptive stereotactic body radiation therapy of liver and pancreas tumors on an MR-linac system. Cancers (Basel) 2022;14(3):716. doi: 10.3390/cancers14030716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li W., Padayachee J., Navarro I., Winter J., Dang J., Raman S., et al. Practice-based training strategy for therapist-driven prostate MR-linac adaptive radiotherapy. Tech Innov Patient Support Radiat Oncol. 2023;13(27) doi: 10.1016/j.tipsro.2023.100212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahlander B.M., Årestedt K., Engvall J., Maret E., Ericsson E. Development and validation of a questionnaire evaluating patient anxiety during magnetic resonance imaging: the magnetic resonance imaging-anxiety questionnaire (MRI-AQ) J Adv Nurs. 2016;72(6):1368–1380. doi: 10.1111/jan.12917. [DOI] [PubMed] [Google Scholar]
- 16.Brédart A., Anota A., Young T., Tomaszewski K.A., Arraras J.I., De Albuquerque M., et al. EORTC quality of life group. phase III study of the European Organisation for Research and Treatment of Cancer satisfaction with cancer care core questionnaire (EORTC PATSAT-C33) and specific complementary outpatient module (EORTC OUT-PATSAT7) Eur J Cancer Care (Engl) 2018;27(1) doi: 10.1111/ecc.12786. [DOI] [PubMed] [Google Scholar]
- 17.Barnes H., Alexander S., Bower L., Ehlers J., Gani C., Herbert T., et al. Development and results of a patient-reported treatment experience questionnaire on a 1.5 T MR-linac. clin transl. Radiat Oncol. 2021;30(31–37) doi: 10.1016/j.ctro.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thery L., Anota A., Waechter L., Laouisset C., Marchal T., Burnod A., et al. Palliative care in day-hospital for advanced cancer patients: a study protocol for a multicentre randomized controlled trial. BMC Palliat Care. 2021;20(1):61. doi: 10.1186/s12904-021-00754-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krug D., Vonthein R., Illen A., Olbrich D., Barkhausen J., Richter J., et al. Metastases-directed radiotherapy in addition to standard systemic therapy in patients with oligometastatic breast cancer: study protocol for a randomized controlled multi-national and multi-center clinical trial (OLIGOMA) Clin Transl Radiat Oncol. 2021;28:90–96. doi: 10.1016/j.ctro.2021.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahlander B.M., Engvall J., Ericsson E. Anxiety during magnetic resonance imaging of the spine in relation to scanner design and size. Radiography (Lond) 2020;26(2):110–116. doi: 10.1016/j.radi.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Halkett G., O’Connor M., Jefford M., Aranda S., Merchant S., Spry N., et al. RT prepare: a radiation therapist-delivered intervention reduces psychological distress in women with breast cancer referred for radiotherapy. Br J Cancer. 2018;118:1549–1558. doi: 10.1038/s41416-018-0112-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O'Neill A., Hughes C., McClure P., Rainey C., McLaughlin L., McFadden S. Patient engagement with radiation therapists: patient perspectives, challenges, and opportunities. A systematic review Radiography (Lond) 2023 May;29(Suppl 1):S128–S136. doi: 10.1016/j.radi.2023.02.022. [DOI] [PubMed] [Google Scholar]
- 23.Whiteside L., Nelder C., Pitt E., Hodgson C., Choudhury A., Eccles C. Comparing patient acceptability of MR-guided radiotherapy to conventional CBCT on two Elekta systems: a questionnaire-based survey. J Radiother Pract. 2023;22:E50. doi: 10.1017/S146039692200020. [DOI] [Google Scholar]
- 24.Vandemaele M., Aznar M., Blanchard P., Borras J.M., Leech M., Aggarwal A., et al. A systematic literature review of definitions and classification systems for radiotherapy innovation: a first step towards building a value-based assessment tool for radiation oncology. Radiother Oncol. 2023;183 doi: 10.1016/j.radonc.2023.109602. [DOI] [PubMed] [Google Scholar]