Abstract
Background:
Evidence is limited on nurse staffing in maternity units.
Purpose:
To estimate the relationship between hospital characteristics and adherence with Association of Women’s Health, Obstetric and Neonatal Nurses nurse staffing guidelines.
Methods:
We enrolled 3,471 registered nurses in a cross-sectional survey and obtained hospital characteristics from the 2018 American Hospital Association Annual Survey. We used mixed-effects linear regression models to estimate associations between hospital characteristics and staffing guideline adherence.
Findings:
Overall, nurses reported strong adherence to AWHONN staffing guidelines (rated frequently or always met by ≥ 80% of respondents) in their hospitals. Higher birth volume, having a neonatal intensive care unit, teaching status, and higher percentage of births paid by Medicaid were all associated with lower mean guideline adherence scores.
Discussion:
Important gaps in staffing were reported more frequently at hospitals serving patients more likely to have medical or obstetric complications, leaving the most vulnerable patients at risk.
Keywords: Nursing staff, hospital, Personnel staffing, Hospitals, Pregnancy, high risk, Workforce, Inpatients, Hospitals, teaching, Obstetric nursing
Introduction
There is a substantial amount of high-quality supportive evidence linking nurse staffing to inpatient morbidity and mortality (American Nurses Association [ANA], 2015, 2018, 2020; Association of Women’s Health, Obstetric, and Neonatal Nurses [AWHONN], 2022). Most of the research has focused on medical-surgical units and intensive care units in acute care hospitals. There has been very little attention to nurse staffing in inpatient maternity units (Lyndon et al., 2022a; Roth et al., 2020; Simpson et al., 2017; Simpson et al., 2020), although in the United States, childbirth is the most common reason for hospital inpatient stays with over 3.6 million births in 2021 (Hamilton et al., 2022) and the third most expensive inpatient condition (Liang et al., 2020). Maternal mortality rates in the United States have continued to rise each year in the United States and compare unfavorably to peer countries (United States Government Accountability Office [US GAO], 2022; Thoma & Declerq, 2022). While the COVID-19 pandemic exacerbated maternal mortality (Thoma & Declercq, 2022), the underlying high and increasing rates predate COVID-19: The US maternal mortality rate for 2021 was 32.2 deaths per 100,000 live births compared with a rate of 23.8 in 2020, 20.1 in 2019, and 17.4 in 2018 (Hoyert. 2022; US GAO, 2022). Approximately one-half of these deaths occur in the inpatient setting (Admon et al., 2022; Burgess et al., 2020) and disproportionately represent non-Hispanic Black women (Guglielminotti et al., 2021; Mogos et al., 2020; US GAO, 2022).
In 2010, AWHONN issued updated guidelines for nurse staffing in perinatal units. They had been previously published every 5 years by our physician colleagues in the Guidelines for Perinatal Care since 1983 (American Academy of Pediatrics & American College of Obstetricians and Gynecologists, 1983). There are specific recommended nurse-to-patient ratios for types of patients and clinical situations commonly encountered in the inpatient perinatal setting including during labor and birth (AWHONN, 2010). As part of the implementation process in 2011 and 2012, AWHONN organized a staffing project enrolling 183 hospitals in 43 states (Scheich & Bingham, 2015). Adherence to the updated staffing guidelines as reported by project hospitals ranged between 33% for 1-to-1 care women in labor receiving oxytocin (new standard in 2010) to 96% for 1-to-1 care for women during second stage labor (standard since 1983) (Scheich & Bingham, 2015). In a more recent study of 615 labor nurses from 67 hospitals in 3 states conducted in 2016 and 2017, we found substantial increases in adherence to the AWHONN guidelines for intrapartum nurse-to-patient ratios (Simpson et al., 2019). There were no nurse-to-patient ratios for which hospital adherence was below 60% and most were in the 70% to 90% range (Simpson et al., 2019). Adherence to 1-to-1 care for oxytocin doubled from 33% reported by Scheich and Bingham (2015) to 66% (Simpson et al., 2019). In both studies, large volume perinatal services (≥2000 birth per year: Scheich & Bingham, 2015; ≥2500 births per year: Simpson et al., 2019) reported significantly less adherence to the AWHONN (2010) nurse staffing guidelines when compared to hospitals with fewer births. Similar results have been noted in large volume neonatal intensive care units (NCIU). Profit et al. (2010) found nurses in large (> average daily census of 20 babies) NICUs had more patients (2.7 babies) than nurses in small NICUs (2.1 babies). Nurse staffing in large volume maternity services that is inconsistent with AWHONN (2010; 2022) nurse staffing standards may be a common practice that puts patients at risk for adverse events.
Purpose
The purpose of this study is to determine whether hospital characteristics such as birth volume and teaching status are associated with adherence to the AWHONN (2010) nurse staffing guidelines. Higher hospital birth volume is often associated with tertiary centers caring for high-risk maternity patients (American College of Obstetricians and Gynecologists et al., 2019; Friedman et al., 2016; Oot et al, 2021) and is frequently a characteristic of a teaching hospital with a high percentage of patients insured by Medicaid (Grover et al., 2014; Tikkanen et al., 2017). Many of these teaching hospitals are safety-net hospitals with poor financial resources (Colenda et al., 2022; Himmelstein et al., 2022). There is no consensus on definition of safety-net hospitals, however they are generally considered to provide care for higher percentages of patients covered by Medicaid, be teaching hospitals, have an NICU, and have a larger volume of births when compared to non-safety-net hospitals (Chatterjee et al., 2020; Hefner et al., 2021; Posescu et al., 2019), thus we chose these characteristics for this study. Based on recent data, maternity patients at highest risk for severe maternal morbidity more often give birth in teaching hospitals or safety-net hospitals and have Medicaid as their insurer (Fingar et al., 2018). These patients are the most vulnerable and are more likely to need more intensive nursing care based on their medical and psychosocial circumstances when compared to the general population of maternity patients. We aimed to determine whether hospitals with higher-risk maternity patients as identified by birth volume, percent of patients covered by Medicaid, presence of a NICU, and teaching status had less adequate nurse staffing when compared to hospitals with lower risk patients by evaluating nurse-reported adherence to the AWHONN (2010) nurse staffing guidelines.
Methods
Design, Participants, and Settings
The Labor RNs study was a large cross-sectional study designed to examine issues related to nurse staffing for labor and birth. We recruited registered nurses who worked in labor and birth units from hospitals in 37 US states selected in 2017 based on the projected feasibility of obtaining state data for future calculation of patient outcomes, as previously described (Lyndon et al., 2022a). Hospitals in target states that had more than 40 annual births in 2016 (n = 2,186) were invited to facilitate recruitment of nurses who worked in their labor and birth units. Nurse leaders for each unit were identified and contacted by email and/or telephone with information about the study.
Nurses were recruited between February 2018 and July 2019 via email invitation containing an electronic link to a 15-minute survey that included consent information on the landing page and was hosted on a secure Qualtrics server. Most of the nurse leaders sent the link to the survey via email to the nurses at their hospital. A smaller number of facilities provided email distribution lists for direct recruitment. These nurses received unique links and tailored reminders via Qualtrics. Six hospitals requested paper surveys and returned these to the study center via pre-addressed postage paid envelopes. Nurses selected their state and then their hospital from a pick list tailored to that state. The University of California San Francisco study center handled all recruitment, consent, and data collection and facilitating hospitals were thereby not engaged in human subjects activity. The institutional review boards at New York University and the University of California San Francisco approved the study. Where required by local hospital or system policy, we obtained local institutional review board approval as well.
Measures
A frequently used nurse staffing measure relies on nurse recall of the number of patients they were responsible for on the last shift worked (Aiken et al., 2002; Dierkes et al, 2022). However, the assignment for the last shift worked may or may not represent typical staffing for the nurses’ unit. The pattern of staffing is particularly important in labor and delivery, where patient assignments can vary widely depending on the type of patient, stage of labor, and changes in assignments throughout the shift. Shifting assignments in labor and delivery are common, especially in busier units. For example, the same nurse might care for two or three different patients in a 12-hour shift but be assigned 1-to-1 with each patient. Staffing in that scenario (1-to-1) would not be reflected accurately in the question about the number of patients the nurse had responsibility for during the shift (1-to-3). Therefore, we chose to assess the pattern of staffing more broadly as we have done in the past (Lyndon et al., 2022b; Simpson et al, 2019), rather than last shift worked.
We assessed the pattern of staffing via nurse’s report of the frequency with which the hospital in which the nurse was employed adhered to AWHONN (2010) staffing guidelines for labor, birth, and the immediate postpartum recovery period using 14 items with Likert-type response options: “rarely (1),” “occasionally (2),” “frequently (3),” “always (4),” and “not applicable” (Lyndon et al., 2022b). We had tested 19 items corresponding to each of the labor, birth, and recovery guidelines in prior research (Simpson et al., 2019) and for this study combined 5 detailed questions about specific types of high-risk patients into a single question to reduce redundancy. Nurses’ assessment of their hospitals’ quality of nursing care was assessed using a single question, “How would you describe the quality of nursing care delivered to patients in your unit?” with response options “poor (1),” “fair (2),” “good (3)” and “excellent (4).” This measure has been demonstrated to be a reliable quality indicator (McHugh & Stimpfel, 2012). Respondent demographics included age, years of experience (as an RN, as an RN working in labor and delivery, and working in this hospital), highest level of education, professional certifications, shift worked, full/part-time status, and role on the unit (staff nurse, charge nurse, nurse manager, clinical educator, clinical nurse specialist). Sex and race/ethnicity were also obtained in in accordance with federal guidelines. Hospital characteristics including annual birth volume, ownership type, obstetrics level, neonatal care level, teaching status, urban/rural status (metro, micro, rural), and status as a critical access hospital or sole community provider were obtained from the American Hospital Association (AHA) Annual Survey, 2018. Because AHA payer mix (% Medicaid discharges) was available for only 23 hospitals in our dataset, we computed payer mix from 2018 State Inpatient Data (SID) files, where available. We obtained SID from Arkansas, Arizona, California, Florida, Iowa, Kentucky, Massachusetts, Maryland, Minnesota, North Carolina, Nebraska, New Jersey, Nevada, Oregon, Utah, Vermont, Washington, Wisconsin, and West Virginia from the Hospital Cost and Utilization Project (HCUP) and from New York, Oklahoma, Pennsylvania, and Virginia from the individual states.
Data Analysis
Staffing responses were characterized using overall frequency of responses for each item, and for the outcome measure, an individual-level staffing score was created for each respondent by taking the mean of their individual response scores (Lyndon et al., 2022b). Respondent and hospital characteristics were summarized with descriptive statistics. Our previous categorization of annual birth volume (<500, 500–999, 1000–2499, and ≥ 2500) (Simpson et al.,, 2019) was a good fit for the current data and was retained for this analysis. Independent groups t-tests and Fischer’s Exact tests were used to compare the characteristics of sample hospitals to the remaining non-participating hospitals in the AHA dataset with more than 40 annual births.
To evaluate the relationship between nurse-reported adherence to AWHONN staffing guidelines and hospital characteristics, we conducted mixed-effects linear regressions with robust variance estimation of mean nurse staffing score on hospital characteristics, with the individual hospital as a random effect and each hospital characteristic as a fixed effect to account for the clustering of nurse respondents within hospitals. Bootstrapping was used to estimate standard errors and calculate confidence intervals for regression coefficients. Analyses were restricted to hospitals with at least 4 nurse respondents per prior research (Simpson et al., 2019). To ensure inclusion of very small hospitals, we also included hospitals with <4 surveys that met or exceeded the average hospital response rate of 35% (Lyndon et al., 2022a). Twenty-one hospitals returned fewer than 4 surveys, 2 of which were retained as they met the response rate criterion. To determine the necessity of a mixed model accounting for the clustering of nurses within hospitals, we calculated the intraclass correlation for the null model (containing only the clustering variable, hospital). This indicated that hospital clustering accounted for 44% of the variability in staffing ratings (ICC = .445, 95% CI = .39, .50), justifying the use of the mixed effects model.
Hospital characteristics with significant associations in the bivariate models were included in a multivariate mixed-effects model to determine independent predictors of mean nurse-reported staffing guideline adherence. We had 253 hospitals in our dataset with a valid number of nurse respondents for hospital level analysis. However, only 211 of these hospitals had complete AHA survey data on the selected hospital characteristics. In addition, 48 AHA identifiers were for “parent” hospitals, meaning the characteristics in the AHA survey covered more than one hospital under one identifier. Therefore, we conducted three sensitivity tests of the robustness of our findings: one using multiple imputation of missing hospital characteristics, one excluding “parent” hospitals, and one including only respondents who hold staff positions (who comprise more than 90% of the sample). We then tested association of staffing with nurse-reported quality of care in bivariate and multivariate mixed-effects models. For this second multivariate model, we included variables that were significant in the model of multivariate staffing on hospital characteristics. Lastly, the multivariate model was re-run including payer mix (percentage of births covered by Medicaid expressed in increments of 10%) for the subset of hospitals (160) for which the SID files were available. Given the potential correlation among hospital characteristics, we examined these predictors for collinearity. This examination indicted the set of hospital characteristics did not demonstrate problematic collinearity (VIF <10).
Findings
A total of 10,482 RNs were invited to participate across the 271 participating hospitals (median per hospital = 28, range 2 to 200). The median number of respondents who completed the survey per hospital was 10 (range = 2 to 65).
Response rate for participating hospitals was 35% with 3,471 nurses from 271 hospitals providing data for nurse-level aspects of this analysis (frequency of guideline adherence by item). Respondents were primarily female (86%, with 13.6% declining to state, 0.5% reporting male, and 0.1% reporting other gender), non-Hispanic (94.3%), and white (82.7%). Ten percent of respondents declined to report race. The remainder reported 2.2% Asian, 2.1% Black, 2% Multiracial, 0.6% American Indian or Alaska Native, and 0.2% Native Hawaiian or Other Pacific Islander. The majority of respondents held a bachelor’s degree or higher (2.6% diploma RN, 27% associate degree, 61.7% bachelor’s degree, 7.8% master’s degree, and 0.4% clinical, research, or other doctorate). Over 90% of respondents worked as staff nurses (63.9%) or in both staff and charge nurse roles (26.3%). Respondents worked mostly full-time (75.3%), day shift (53.3% days, 35% nights, 3.5% evenings, and 8.2% rotating shifts), and were highly experienced (mean 14.8 years as an RN; 12.3 years in labor and delivery; SD 11.6 and 10.6, respectively). Mean age of nurses in this sample was 40.7 years (range 21–73, SD 11.8). Characteristics of participating hospitals and comparison to 2,705 hospitals in the 2018 AHA Annual Survey with >40 births are presented in Table 1. Hospitals in the study sample had higher birth volumes and were more likely than other birth hospitals to have neonatal intensive care units but were otherwise similar.
Table 1.
Hospital Characteristics (AHA Annual Hospital Survey, 2018)
| Characteristic | Study sites (N = 271) | National (N = 2,705) | p | ||
|---|---|---|---|---|---|
|
| |||||
| Birth categories | n | % | n | % | 0.009 |
| <500 | 82 | 30.3% | 998 | 38.1% | |
| 500–999 | 62 | 22.9% | 574 | 21.9% | |
| 1000–2499 | 71 | 26.2% | 681 | 26.0% | |
| ≥2500 | 56 | 20.7% | 367 | 14.0% | |
| Ownership | n | % | n | % | 0.022 |
| Government | 47 | 17.3% | 531 | 19.6% | |
| Church Operated | 40 | 14.8% | 301 | 11.1% | |
| Other non-profit | 157 | 57.9% | 1449 | 53.6% | |
| Investor-owned | 27 | 10.0% | 424 | 15.7% | |
| Obstetrics Level | 0.114 | ||||
| Uncomplicated cases | 75 | 33.3% | 811 | 39.5% | |
| Most complicated cases | 82 | 36.4% | 731 | 35.6% | |
| All serious illnesses/abnormalities | 68 | 30.2% | 510 | 24.9% | |
| Neonatal Care | |||||
| Neonatal intensive care hospital | 112 | 48.1% | 789 | 36.1% | <.001 |
| Neonatal intermediate care hospital | 60 | 25.8% | 595 | 27.2% | 0.629 |
| Teaching Hospital | 146 | 53.9% | 1420 | 52.5% | 0.665 |
| Urban/Rural | 0.052 | ||||
| Metro | 190 | 70.1% | 1764 | 65.2% | |
| Micro | 55 | 20.3% | 535 | 19.8% | |
| Rural | 26 | 9.6% | 406 | 15.0% | |
| Critical Access Hospital | 38 | 14.0% | 460 | 17.0% | 0.21 |
| Sole Community Provider | 24 | 8.9% | 223 | 8.2% | 0.728 |
Note: Unequal variance t-test/Fisher’s Exact test. The range of annual births for hospitals in the sample was 49 to 14,334; the range for hospitals with at least 40 births in the American Hospital Association dataset was 40 to 16,829 at p = 0.002.
Overall, nurses reported strong adherence to AWHONN staffing guidelines (rated frequently or always met by ≥ 80% of respondents) in their hospitals (Figure 1), yet several guidelines were reported to be only rarely or occasionally met by 22.8–45.4% of respondents. Guideline adherence was reported to be high (>80%) for cervical ripening (1 nurse-to-2 patients, 83.9%), epidural initiation (1 nurse-to-1 patient, 84.1%), pushing during second stage labor (1-to-1 with continuous presence at the bedside, 93.3%); and birth (2 nurses per mother-baby dyad, 80.6%). Adherence was moderate (70% to 79%) for postpartum recovery (1 nurse per mother-baby dyad for at least 2 hours, 71.8%), category III fetal heart rate tracing (1 nurse-to-1 patient, 77.2 %), and mothers with high-risk conditions (1-to1, 72.6%).
Figure 1.
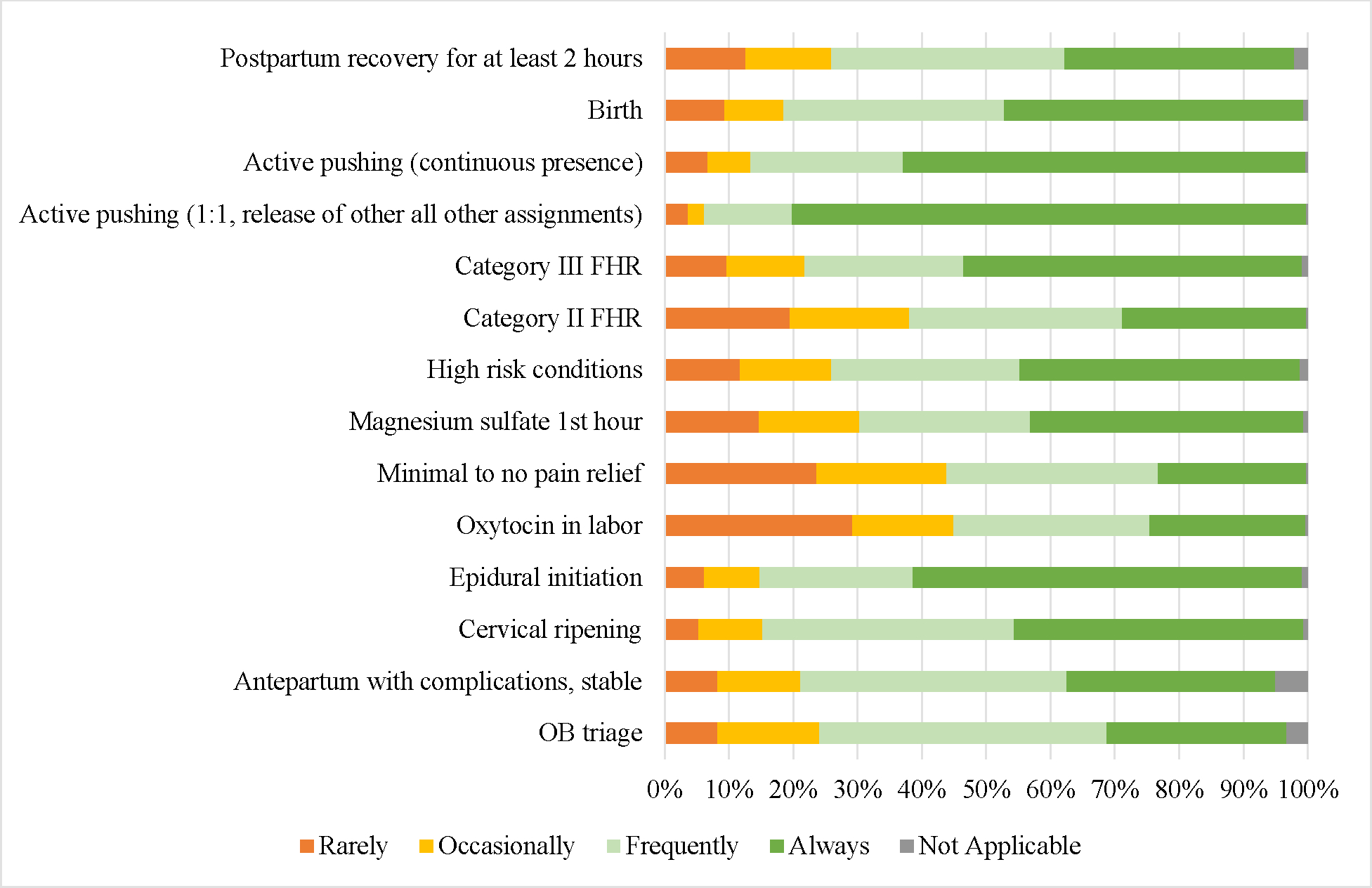
Frequency of Guideline Adherence
Guideline adherence was lowest for the following conditions: category II fetal heart rate tracing (1-to-1, 61.3%), women with minimal or no pain relief (1-to-1, 55.8%), and oxytocin administration in labor (1-to-1, 54.6%). Similarly, almost all nurses reported good or excellent quality of care (Excellent 57%, Good 37%, Fair 4.4%, Poor 0.2%).
Bivariate associations between hospital characteristics and mean nurse-reported adherence to staffing guidelines are shown in Table 2. In unadjusted analyses, higher birth volume, accepting all serious illnesses and abnormalities in obstetric cases, having a neonatal intensive care unit, and teaching status were all associated with lower mean guideline adherence scores, whereas location in micropolitan or rural core based statistical areas and designation as a critical access hospital were associated with higher mean guideline adherence scores. Hospital ownership and sole community provider status were not significantly associated with staffing guideline adherence.
Table 2.
Bivariate regressions of staffing on hospital characteristics
| AHA Hospital characteristics | Coefficient | 95% CI LL | 95% CI UL | p |
|---|---|---|---|---|
|
| ||||
| Births | ||||
| <500 | ref | ref | ref | ref |
| 500–999 | −0.164 | −0.324 | −0.004 | 0.044 |
| 1,000–2,499 | −0.296 | −0.442 | −0.149 | <.001 |
| ≥2,500 | −0.519 | −0.672 | −0.366 | <.001 |
| Ownership | ||||
| Government | ref | ref | ref | ref |
| Church | −0.049 | −0.260 | 0.162 | 0.648 |
| Other non-profit | −0.015 | −0.182 | 0.151 | 0.856 |
| Investor owned | −0.221 | −0.473 | 0.032 | 0.087 |
| Obstetrics Level | ||||
| Uncomplicated cases | ref | ref | ref | ref |
| Most complicated cases | −0.074 | −0.229 | 0.082 | 0.355 |
| All serious illnesses/abnormalities | −0.329 | −0.489 | −0.169 | <.001 |
| NICU Hospital a | −0.357 | −0.479 | −0.234 | <.001 |
| Neonatal intermediate hospital a | −0.182 | −0.327 | −0.037 | 0.014 |
| Teaching hospital a | −0.255 | −0.371 | −0.138 | <.001 |
| Core based statistical area | ||||
| Metro | ref | ref | ref | ref |
| Micro | 0.193 | 0.041 | 0.344 | 0.013 |
| Rural | 0.323 | 0.121 | 0.525 | 0.002 |
| Critical access hospital a | 0.286 | 0.110 | 0.462 | 0.001 |
| Sole community provider a | 0.086 | −0.129 | 0.301 | 0.434 |
ref = no
Bivariate regression also demonstrated an association between perceived quality of care and staffing guideline adherence [Good 0.33 (95% CI 0.27, 0.38, p<0.001)); Excellent 0.61 (95% CI 0.55, 0.67), p<0.001)], and payer mix (percentage of Medicaid births) and staffing [−0.43 (95% CI −0.58, −0.28), p<0.001].
In the adjusted analysis (Table 3), higher annual birth volume, neonatal intensive care status, and teaching status, were independent predictors of less staffing guideline compliance. Inclusion of hospital characteristics in the multivariable model of staffing on quality of care had minimal effect on the quality estimates. The full model explained 20.7% of the variance in staffing scores (R2 = .207). Quality of nursing care was significantly related to staffing. On average, Good and Excellent quality of care were associated with a .30- and .596-point increase in staffing guideline adherence compared to Poor/Fair quality of care (on a scale of 1–4). Significant differences in staffing ratings associated with hospital level characteristics were smaller. Staffing ratings decreased with increasing birth volume, with differences between higher birth volume hospitals associated with a range of .06 to .30 of a point decrease relative to the lowest category of birth volume (<500). Compared with non-teaching hospitals, teaching hospitals had on average a .10 point lower staffing ratings. Similarly, NICU hospitals had on average a .168 point lower rating on staffing than non-NICU hospitals. Neither hospitals’ obstetrics level or core based statistical area was significantly associated with staffing care in the multivariate model. Analysis was also conducted on a subset of hospitals (n = 160) for which SID files were available to examine the impact of percentage of births covered by Medicaid. Adding this to the model had little impact on other variables in the model (Table 4) and a higher percentage of births covered by Medicaid was significantly associated with reduced staffing guideline compliance, with a 10% increase in Medicaid covered births associated with a .04-point increase in staffing scores (range 1–4). Sensitivity analyses using multiple imputation (n=251 hospitals, not shown), excluding parent hospitals (n=163, not shown), excluding the top 5% of hospitals by number of respondents (not shown), and including only staff participants (not shown) generated comparable estimates of coefficients to the primary model.
Table 3.
Multivariate regression model of hospital level variables predicting staffing
| Coefficient | 95% CI LL | 95% CI UL | p | |
|---|---|---|---|---|
|
| ||||
| Nursing care quality | ||||
| Poor/Fair | ref | ref | ref | ref |
| Good | 0.306 | 0.216 | 0.397 | <.001 |
| Excellent | 0.593 | 0.499 | 0.686 | <.001 |
| AHA Hospital characteristics | ||||
| Births | ||||
| <500 | ref | ref | ref | ref |
| 500–999 | −0.062 | −0.145 | 0.020 | 0.14 |
| 1,000–2,499 | −0.145 | −0.244 | −0.045 | 0.004 |
| ≥2,500 | −0.302 | −0.408 | −0.196 | <.001 |
| Obstetrics Level | ||||
| Uncomplicated cases | ref | ref | ref | ref |
| Most complicated cases | 0.069 | −0.004 | 0.141 | 0.064 |
| All serious illnesses/abnormalities | 0.066 | −0.018 | 0.149 | 0.124 |
| NICU Hospital a | −0.168 | −0.240 | −0.096 | <.001 |
| Teaching hospital a | −0.103 | −0.163 | −0.042 | 0.001 |
| Core based statistical area | ||||
| Metro | ref | ref | ref | ref |
| Micro | −0.076 | −0.167 | 0.014 | 0.098 |
| Rural | 0.035 | −0.085 | 0.155 | 0.569 |
Note: Total N = 2,913, sites = 211
ref = no
Table 4.
Multivariate regression predicting staffing including payer mix
| Coefficient | 95% CI LL | 95% CI UL | p | |
|---|---|---|---|---|
|
| ||||
| Nursing care quality | ||||
| Poor/Fair | ref | ref | ref | ref |
| Good | 0.328 | 0.208 | 0.447 | <.001 |
| Excellent | 0.598 | 0.483 | 0.713 | <.001 |
| AHA Hospital characteristics | ||||
| Births | ||||
| <500 | ref | ref | ref | ref |
| 500–999 | −0.061 | −0.158 | 0.037 | 0.222 |
| 1,000–2,499 | −0.099 | −0.214 | 0.015 | 0.088 |
| ≥2,500 | −0.303 | −0.427 | −0.179 | <.001 |
| Obstetrics Level | ||||
| Uncomplicated cases | ref | ref | ref | ref |
| Most complicated cases | 0.068 | −0.024 | 0.160 | 0.148 |
| All serious illnesses/abnormalities | 0.093 | −0.004 | 0.189 | 0.061 |
| NICU Hospital a | −0.163 | −0.258 | −0.067 | 0.001 |
| Teaching hospital a | −0.127 | −0.194 | −0.061 | <.001 |
| Core based statistical area | ||||
| Metro | ref | ref | ref | ref |
| Micro | −0.034 | −0.131 | 0.064 | 0.501 |
| Rural | 0.049 | −0.093 | 0.190 | 0.502 |
| % of births covered by Medicaid | −0.044 | −0.063 | −0.026 | <.001 |
Note: Total N = 2,223, sites = 160 with % births covered by Medicaid computed from State Inpatient Data files.
ref = no
Discussion
The AWHONN nurse-to-patient staffing ratios for most aspects of labor are 1-to-1, birth is 2-to-1, and immediate postpartum recovery is 1–2 (AWHONN, 2010; 2022). Therefore, even small deviations in guideline adherence on a 1–4 scale represent situations where the nurses are substantively under-resourced. Such situations impair provision of safe, high quality care. Our findings that nurses who care for women giving birth at hospitals with a greater percentage of high-risk maternity patients are less likely to report nurse-to-patient ratios consistent with the AWHONN (2010) recommended nurse-to-patient ratios when compared to nurses in hospitals that care for lower risk women have significant policy implications for ongoing efforts to improve maternal outcomes and decrease risk of severe maternal morbidity and mortality in the United States. Over 50% of US maternal deaths occur in the inpatient setting (Admon et al., 2022; Burgess et al., 2020). The United States ranks unfavorably to other developed high-income countries in maternal mortality and morbidity with a disproportionate effect on minoritized women (Aspen Health Strategy Group, 2021; Fingar et al., 2018; Hoyert & Mininno, 2020; Hoyert, 2021; National Quality Forum, 2020; Oot et al., 2021; Society for Maternal-Fetal Medicine et al., 2021; Tikkanen et al., 2020; US GAO, 2022). This trend has worsened during the COVID-19 pandemic (Thoma & Declercq, 2022; US GAO, 2022). Women with high risk of severe maternal morbidity are more likely to give birth at a safety-net or teaching hospital and have Medicaid insurance (Fingar et al., 2018; Howell et al. 2016).
One cause of nurses in these types of hospitals having more patients than recommended for safe high-quality care may be poor reimbursement from Medicaid compared to commercial insurance for inpatient childbirth services, generating insufficient financial resources to support adequate nurse staffing (Himmelstein et al., 2022; National Academies of Sciences, Engineering, and Medicine, 2020). The nursing workforce is a large part of hospital budgets: one-third to one-half of the labor budget and approximately 17% to 25% of the total hospital budget (Begley et al., 2020). Using data from MarketScan commercial and Medicaid databases of births in the United States in 2010, reimbursement amounts to hospitals for vaginal and cesarean births were more than double for commercially insured patients when compared to Medicaid-insured patients (Truven, 2013). These disparities in reimbursement for birth between Medicaid and commercial insurance have persisted (National Academies of Sciences, Engineering, and Medicine, 2020). The higher the percentage of maternity patients insured by Medicaid, the greater the financial inequity among hospitals and the fiscal challenge to support safe staffing. As some hospitals struggle to control costs, it is important to consider that nurse staffing mandates such as the nurse-to-patient ratios in California can be protective against decreases in nurse staffing in times of economic challenges (Dierkes et al., 2022). Hospital administrators and maternity nurse leaders can use unit data to gain financial support for nurse staffing that is consistent with perinatal nurse staffing standards (AWHONN, 2010, 2022). Embedding the staffing standards into the electronic medical record (Jones & Hall, 2022) and meticulously collecting and reviewing data about patient characteristics, acuity, length of stay, and gaps in nurse staffing needs can be effective in increasing the nurse staffing budget to routinely reflect the standard nurse-to-patient ratios (Jones & Hall, 2022; Simpson, 2015).
Preventable maternal morbidity and mortality are associated with delays in recognition of risk factors and in assessing clinical warning signs, providing accurate diagnoses, and escalation of care by implementing optimal treatment and coordinating care with the perinatal team (Bajaj et al., 2021; Society for Maternal-Fetal Medicine et al., 2021). Failure to rescue is a significant factor in excess maternal deaths among women of racial and ethnic minorities with severe maternal morbidity during birth hospitalization in the United States (Guglielminotti et al., 2021). Nurses report missing essential aspects of maternity care when they are short-staffed and being unable to give full attention to clinical needs of childbearing patients (Roth et al. 2020; Simpson et al., 2016, 2017, 2021). Clinicians perceive nurse staffing as an essential feature of a high-performing maternity service, one that has favorable outcomes based on risk-adjusted maternal morbidity metrics (Howell et al., 2022). There must be enough nurses to be able to recognize evolving maternal deterioration as per the AWHONN (2010, 2022) staffing standards for high-risk patients or patients are at risk for preventable adverse outcomes (Simpson, 2022a).
The Centers for Medicare and Medicaid Services (CMS) have indicated minimum nurse staffing regulations will be established for nursing homes to promote patient safety (White House, 2022). Hospital maternity services could benefit from similar rules for minimum nurse staffing consistent with AWHONN (2022) nurse staffing standards as part of CMS’s development of a new hospital designation to identify hospitals offering high-quality maternity care. CMS is requiring hospitals with maternity services to report several key quality measures to drive improvements in maternal health outcomes and maternal health equity (CMS, 2022). The precedent set for CMS’s requirements for minimal staffing in nursing homes should be extended to inpatient maternity care. Adequate nurse staffing is an indicator of the ability to provide quality nursing care. A change by CMS to require adherence to evidence-based nurse staffing standards as set per AWHONN and endorsed by multiple professional associations in the maternal-child field would likely be followed by other organizations such as the Joint Commission, which currently does not include nurse staffing in its acute-care hospital accreditation or its perinatal certification process (Simpson, 2022b).
Finally, at the individual hospital or hospital system level, providing safe staffing may be a crucial nursing recruitment and retention strategy in the context of the stresses the COVID-19 pandemic has placed on the healthcare workforce (French et al., 2022; Marufu et al., 2021; Schlak et al., 2022). Poorer nurse staffing has been associated with burnout and job dissatisfaction among nurses (Aiken et al., 2002; Shah et al, 2021). While the current exodus of nurses and other healthcare professionals from acute care is multifactorial (Schlak et al., 2022), providing safe staffing according to AWHONN (2022) standards might reduce, mitigate, or prevent burnout and turnover among perinatal nurses (Marufu et al., 2021).
Strengths and Limitations
Characteristics of participating hospitals and nurses are similar to those of hospitals and nurses in the United States, although they were more likely to have a higher birth volume and a NICU. Respondents represent a wide range of types of birthing hospitals in 34 states across the United States. Data about nurse staffing are based on self-report, however this methodology is commonly used in nurse staffing research. The response rate from labor nurses of 35% was reasonable for an electronic distribution method (Tourangeaue et al., 2013).
Conclusions
Better funding for teaching hospitals and safety-net hospitals caring for high-risk maternity patients such as higher disproportionate share payment and increased reimbursement for maternity care services more on par with commercial insurance may support better nurse staffing that is consistent with AWHONN (2010, 2022) nurse staffing standards. Policy changes such as CMS and hospital accrediting agencies adding nurse staffing as part of their evaluation process would be an effective way to advocate for safe nurse staffing to promote high-quality perinatal nursing care. Our results highlight the inequities in safe staffing for maternity patients based on hospital characteristics in the United States that may be one factor in less optimal maternal morbidity and mortality outcomes for the most vulnerable childbearing populations.
Acknowledgments
This project was supported by grant number R01HS025715 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. The Association for Women’s Health, Obstetric and Neonatal Nursing supported the development of the survey used in this study and provided non-financial support for study recruitment. This article draws on data published in Lyndon, et al. (2022).
Footnotes
Conflicts of Interest: None to report.
References
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, & Silber JH (2002). Hospital nurse staffing and patient mortality, nurse burnout and job satisfaction. JAMA, 288(16), 1987–1993. 10.1001/jama.288.16.1987 [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics & American College of Obstetricians and Gynecologists. (1983). Guidelines for perinatal care. American Academy of Pediatrics. [Google Scholar]
- American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine, Kilpatrick SJ, Menard MK, Zahn CM, & Callaghan WM (2019). Levels of maternal care (Obstetric Care Consensus No. 9). American Journal of Obstetrics and Gynecology, 221(6), B19–B30. 10.1016/j.ajog.2019.05.046 [DOI] [PubMed] [Google Scholar]
- American Nurses Association. (2015). Optimal nurse staffing to improve quality of care and patient outcomes: Executive summary. Silver Spring, MD. Author. https://www.nursingworld.org/~4ae116/globalassets/practiceandpolicy/advocacy/ana_optimal-nurse-staffing_white-paper-es_2015sep.pdf [Google Scholar]
- American Nurses Association. (2018). The business case for higher levels of nurse staffing in the hospital setting. Silver Spring, MD: Author. https://www.nursingworld.org/~4a58b1/globalassets/practiceandpolicy/nurse-staffing/ana-cost-calculator.pdf [Google Scholar]
- American Nurses Association. (2020). ANA’s principles for nurse staffing (3rd ed.). Silver Spring, MD: Author. https://www.nursingworld.org/practice-policy/nurse-staffing/staffing-principles/ [Google Scholar]
- Aspen Health Strategy Group. (2021). Reversing the U.S. maternal mortality crisis, 1–146. Washington, DC: The Aspen Institute. https://www.medicaidinnovation.org/_images/content/AHSG-Reversing_the_US_Maternal_Mortality_Crisis-Report_2021.pdf [Google Scholar]
- Association of Women’s Health, Obstetric and Neonatal Nurses. (2010). Guidelines for professional registered nurse staffing for perinatal units. Washington, DC: Author. [Google Scholar]
- Association of Women’s Health, Obstetric and Neonatal Nurses. (2022). Standards for professional registered nurse staffing for perinatal units. Nursing for Women’s Health, 26(4), E1–E94. 10.1016/j.nwh.2022.02.00 [DOI] [PubMed] [Google Scholar]
- Begley R, Cipriano PF, & Nelson T, for the American Nurses Association, American Organization of Nursing Leadership and Health Care Financial Management Association. (2020). The business of caring: Promoting optimal allocation of nursing resources. Westchester, IL: Healthcare Financial Management Association. https://www.aonl.org/system/files/media/file/2020/01/Nursing%20allocation%20report%20FINAL_0.pdf [Google Scholar]
- Burgess APH, Dongarwar D, Spigel Z, Salihu HM, Moaddab A, Clark SL, Fox K (2020). Pregnancy-related mortality in the United States, 2003–2016: age, race, and place of death. American Journal of Obstetrics & Gynecology, 222(5), 489.e1–489.e8. 10.1016/j.ajog.2020.02.020. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid. (2022, April 18). CMS proposes policies to advance health equity and maternal health, support hospitals. Washington, DC. US Department of Health and Human Services. https://www.cms.gov/newsroom/press-releases/cms-proposes-policies-advance-health-equity-and-maternal-health-support-hospitals [Google Scholar]
- Chatterjee P, Sommers BD, & Maddox KEJ (2020). Essential but undefined-Reimagining how policymakers identify safety-net hospitals. New England Journal of Medicine, 383(27), 2593–2595. 10.1056/NEJMp2030228 [DOI] [PubMed] [Google Scholar]
- Dierkes A, Do D, Morin H, Rochman M, Sloane D, & McHugh M (2022). The impact of California’s staffing mandate and the economic recession on registered nurse staffing levels: A longitudinal analysis. Nursing Outlook, 70(2), 219–227. 10.1016/j.outlook.2021.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engineer LD, Winters BD, Weston CM, Zhang A, Sharma R, Bass E, Jones D, Rosen A, Yoon FB, Borzecki A, & Dy SM (2016). Hospital characteristics and the Agency for Healthcare Research and Quality Inpatient Quality Indicators: A systematic review. Journal of Healthcare Quality, 38(5), 304–13. 10.1097/JHQ.0000000000000015 [DOI] [PubMed] [Google Scholar]
- Fingar KF, Hambrick MM, Heslin KC, & Moore JE (2018, September). Trends and disparities in delivery hospitalizations involving severe maternal morbidity, 2006–2015. HCUP Statistical Brief No. 243, 1–21. Rockville, MD: Agency for Healthcare Research and Quality. www.hcup-us.ahrq.gov/reports/statbriefs/sb243-Severe-Maternal-Morbidity-Delivery-Trends-Disparities.pdf [PubMed] [Google Scholar]
- French R, Aiken LH, Fitzpatrick Rosenbaum KE, & Lasater KB (2022). Conditions of nursing practice in hospitals and nursing homes before COVID-19: Implications for policy action. Journal of Nursing Regulation. 13(1), p45–p53. 10.1016/S2155-8256(22)00033-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman AM, Ananth CV, Huang Y, D’Alton ME, & Wright JD (2016). Hospital delivery volume, severe obstetrical morbidity, and failure to rescue. American Journal of Obstetrics & Gynecology, 215(6), 795 e1–e14. 10.1016/j.ajog.2016.07.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover A Slavin PL, & Willson P (2014). The economics of academic medical centers. New England Journal of Medicine. 370(25), 2360–2362. 10.1056/NEJMp1403609 [DOI] [PubMed] [Google Scholar]
- Guglielminotti J, Wong CA, Friedman AM, & Li G (2021). Racial and ethnic disparities in death associated with severe maternal morbidity in the United States: Failure to rescue. Obstetrics & Gynecology, 137(5),791–800. 10.1097/AOG.0000000000004362 [DOI] [PubMed] [Google Scholar]
- Hamilton BE, Martin JA, & Osterman MJK (2022, May). Births: Provisional data for 2021. Vital Statistics Rapid Release, No. 20, 1–11. Hyattsville, MD: National Center for Health Statistics. 10.15620/cdc:116027. [DOI] [Google Scholar]
- Healthcare Cost and Utilization Project (HCUP). (2018). HCUP State Inpatient Databases (SID). Agency for Healthcare Research and Quality, Rockville, MD.www.hcup-us.ahrq.gov/sidoverview.jsp [PubMed] [Google Scholar]
- Hefner JL, Hogan TH, Opoku-Agyerman W, & Menachemi N (2021). Defining safety net hospitals in the health services research literature: A systematic review and critical appraisal. BMC Health Services Research, 21, 278. 10.1186/s12913-021-06292-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelstein G, Ceasar JN, & Himmelstein KE (2022). Hospitals that serve many Black patients have lower revenues and profits: Structural racism in hospital financing. Journal of General Internal Medicine, 5, 1–6. 10.1007/s11606-022-07562-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell EA, Egorova N, Balbierz A, Zeitlin J, & Hebert PL, (2016). Black-white differences in severe maternal morbidity and site of care. American. Journal of Obstetrics & Gynecology, 214(1), 122.e1–122.e7. 10.1016/j.ajog.2015.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell EA, Sofaer S, Balbierz A, Kheyfets A, Glazer KB, & Zetlin J (2022). Distinguishing high-performing from low-performing hospitals for severe maternal morbidity: A focus on quality and equity. Obstetrics & Gynecology, 139(6), 1061–1069. 10.1097/AOG.0000000000004806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyert DL (2021, April). Maternal mortality rates in the United States, 2019. NCHS Health E-Stats, 1–5. 10.15620/cdc:103855 [DOI] [Google Scholar]
- Hoyert DL, & Mininno AM (2020, January 30). Maternal mortality in the United States: Changes in coding, publication, and data release, 2018. National Vital Statistics Reports, 69(2), 1–18. Hyattsville, MD: National Center for Health Statistics. https://www.cdc.gov/nchs/data/nvsr/nvsr69/nvsr69-02-508.pdf [PubMed] [Google Scholar]
- Jones LW, & Hall VL (2022). Acuity-based staffing in labor and delivery using electronic health record data. MCN, The American Journal of Maternal Child Nursing, 47(5), 242–248. 10.1097/NMC.0000000000000838 [DOI] [PubMed] [Google Scholar]
- Liang L, Moore B, & Soni A (2020, July). National inpatient hospital costs: The most expensive conditions by payer, 2017. HCUP Statistical Brief No. 261, 1–19. Rockville, MD: Agency for Healthcare Research and Quality. www.hcup-us.ahrq.gov/reports/statbriefs/sb261-Most-Expensive-Hospital-Conditions-2017.pdf [PubMed] [Google Scholar]
- Lyndon A, Simpson KR, Spetz J, Zhong J, Gay CL, Fletcher J, & Landstrom GL (2022a). Nurse-reported staffing guidelines and exclusive breast milk feeding. Nursing Research, Advance online publication (September 2022). 10.1097/NNR.0000000000000620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyndon A, Simpson KR, Spetz J, Fletcher J, Gay CL, Landstrom GL (2022b). Psychometric properties of the perinatal missed care survey and missed care during labor and birth. Applied Nursing Research, 63, 151516. 10.1016/j.apnr.2021.151516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marufu TC, Collins A, Vargas L, Gillespie L, Almghairbi D (2021). Factors influencing retention among hospital nurses: Systematic review. British Journal of Nursing, 30(5), 302–308. 10.12968/bjon.2021.30.5.302 [DOI] [PubMed] [Google Scholar]
- McHugh MD, & Stimpfel AW (2012). Nurse reported quality of care: a measure of hospital quality. Research in Nursing & Health, 35(6), 566–575. 10.1002/nur.21503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2020). Birth settings in America: Outcomes, quality, access, and choice. Washington, DC: The National Academies Press. 10.17226/25636 [DOI] [PubMed] [Google Scholar]
- National Quality Forum. (2020, November). Maternal morbidity and mortality environmental scan. 1–95. Washington, DC: Author. https://www.qualityforum.org/Publications/2020/11/Maternal_Morbidity_and_Mortality_Environmental_Scan.aspx [Google Scholar]
- Oot A, Huennekens K, Yee L, & Feinglass J (2021). Trends and risk markers for severe maternal morbidity and other obstetric complications. Journal of Women’s Health, 30(7), 964–971. 10.1089/jwh.2020.8821 [DOI] [PubMed] [Google Scholar]
- Popescu I, Fingar KR, Cutler E, Guo J, & Jiang HJ (2019). Comparison of 3 safety-net hospital definitions and association with hospital characteristics, JAMA Network Open, 2(8), e198577. 10.1001/jamanetworkopen.2019.8577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Profit J, Petersen LA, McCormick MC, Escobar GJ, Coleman-Phox K Zheng Z, Pietz K, & Zupancic JA,F (2010). Patient-to-nurse ratios and outcomes of moderately preterm infants. Pediatrics, 125(2), 320–326. 10.1542/peds.2008-3140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth C, Brewer MA, Bay RC, & Gosselin KP (2020). Nurses’ experiences of “being swamped” in the clinical setting and association with adherence to AWHONN nurse staffing guidelines. MCN The American Journal of Maternal Child Nursing, 45(5), 271–271. 10.1097/NMC.0000000000000643 [DOI] [PubMed] [Google Scholar]
- Scheich B & Bingham D (2015). Key findings from the AWHONN perinatal staffing data collaborative. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 44(2), 317–328. 10.1111/1552-6909.12548 [DOI] [PubMed] [Google Scholar]
- Schlak AE, Rosa WE, Rushton CH, Poghosyan L, Root MC, & McHugh MD (2022). An expanded institutional- and national-level blueprint to address nurse burnout and moral suffering amid the evolving pandemic. Nursing management, 53(1), 16–27. 10.1097/01.NUMA.0000805032.15402.b3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson KR (2015). Predicting nurse staffing needs for a labor and birth unit in a large-volume perinatal service. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 44(2), 329–338. 10.1111/1552-6909.12549 [DOI] [PubMed] [Google Scholar]
- Simpson KR (2022a). Nurse staffing, missed care, and risk of patient mortality. MCN, The American Journal of Maternal Child Nursing, 47(2), 115. 10.1097/NMC.0000000000000800 [DOI] [PubMed] [Google Scholar]
- Simpson KR (2022b). Why isn’t nurse staffing evaluated as part of hospital accreditation and quality designations? MCN, The American Journal of Maternal Child Nursing, 48(1), Advance online publication (October 2022). 10.1097/NMC.0000000000000871 [DOI] [PubMed] [Google Scholar]
- Simpson KR, & Lyndon A (2017). Consequences of delayed, unfinished, or missed nursing care during labor and birth. Journal of Perinatal & Neonatal Nursing, 31(1), 32–40. 10.1097/jpn.0000000000000203 [DOI] [PubMed] [Google Scholar]
- Simpson KR, Lyndon A, & Ruhl C (2016). Consequences of inadequate staffing include missed care, potential failure to rescue, and job stress and dissatisfaction. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 45(4), 481–490. 10.1016/j.jogn.2016.02.011 [DOI] [PubMed] [Google Scholar]
- Simpson KR, Lyndon A, Spetz J, Gay CL, Landstrom GL (2019). Adherence to the AWHONN staffing guidelines as perceived by labor nurses. Nursing for Women’s Health, 23(3), 217–223. 10.1016/j.nwh.2019.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson KR, Roth C, Hering SL, Landstrom GL, Lyndon A, Tinsley JM, Zimmerman J, & Hill CM (2021). AWHONN members’ recommendations on what to include in the updated standards for professional registered nurse staffing for perinatal units. Nursing for Women’s Health, 25(5), 329–336. 10.1016/j.nwh.2021.08.001 [DOI] [PubMed] [Google Scholar]
- Society for Maternal-Fetal Medicine, Lappen JR, Pettker CM, & Louis JM (2021). Assessing the risk of maternal morbidity and mortality (Consult Series No. 54). American Journal of Obstetrics & Gynecology, 224(4), B2–B15. 10.1016/j.ajog.2020.12.006 [DOI] [PubMed] [Google Scholar]
- Thoma ME & Declercq ER (2022). All-cause maternal mortality in the US before vs during the COVID-19 pandemic. JAMA Network Open, 5(6), e2219133. 10.1001/jamanetworkopen.2022.19133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tikkanen R, Gunja MZ, FitzGerald M, & Zephyrin L (2020, November 18). Maternal mortality and maternity care in the United States compared to 10 other developed countries (Issue Briefs). Washington, DC: The Commonwealth Fund. 10.26099/411v-9255 [DOI] [Google Scholar]
- Tikkanen RS, Woolhandler S, Himmelstein DU, Kressin NR, Hanchate A, Lin M, McCormick D, & Lassar K (2017). Hospital payer and racial/ethnic mix at private academic medical centers in Boston and New York City. International Journal of Health Services. 47(3), 460–476. 10.1177/0020731416689549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tourangeau R, Couper MP, & Couper MP (2013). Science of web surveys. New York, NY: Oxford University Press. [Google Scholar]
- Truven Health Analytics. (2013). The cost of having a baby in the United States. Ann Arbor, MI: Author. https://www.nationalpartnership.org/our-work/resources/health-care/maternity/archive/the-cost-of-having-a-baby-in-the-us.pdf [Google Scholar]
- United States Government Accountability Office. (2022. October 19). Maternal health outcomes worsened and disparities persisted during the pandemic (Report to Congressional Addressees). https://www.gao.gov/products/gao-23-105871
- White House. (2022, February 28). Protecting seniors and people with disabilities by improving safety and quality of care in the nation’s nursing homes. (Fact Sheet). Washington, DC: Author. https://www.whitehouse.gov/briefing-room/statements-releases/2022/02/28/fact-sheet-protecting-seniors-and-people-with-disabilities-by-improving-safety-and-quality-of-care-in-the-nations-nursing-homes/ [Google Scholar]


