Abstract
Background:
Previous studies have mainly focused on individual mental disorders, and there is no study addressing the total burden of mental disorders in the Middle East and North Africa (MENA).
Aims:
To evaluate the burden of mental disorders in the MENA region from 1990 to 2019.
Study Design:
A cross-sectional study.
Methods:
We utilized global burden of disease data to examine the burden of 12 mental disorders from 1990 to 2019 across age groups, genders, and the 21 MENA countries. We collected data on prevalence, incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years (DALY), including both crude and age-standardized rates per 100,000 people.
Results:
The DALY rate of mental disorders in MENA countries increased by 13.88% from 1,747.92 per 100,000 people in 1990 to 1990.5 per 100,000 people in 2019. The highest percentage increases in the DALY rates of mental disorders were observed for bulimia nervosa (35.69%), other mental health disorders (34.58%), and schizophrenia (33.02%) from 1990 to 2019. However, the DALY rates for idiopathic developmental intellectual disability (-26.48%), conduct disorder (-23.91%), attention-deficit/ hyperactivity disorder (-16.46%), and autism spectrum disorders (-4.12%) decreased in the MENA region from 1990 to 2019. In 2019, the highest DALY rates for idiopathic developmental intellectual disability, anxiety disorders, and major depressive disorder were observed in age groups ≤ 4 years, 5-19 years, and ≥ 20 years, respectively. The age-standardized DALY rate of mental disorders was the highest in Palestine (2,396.9 per 100,000), Iran (2,295.8 per 100,000), and Lebanon (2,126.0 per 100,000) compared with other MENA countries in 2019.
Conclusion:
There has been a slight increase in the burden of mental disorders in the MENA region between 1990 and 2019. National policies should prioritize evidence-based preventive measures and ensure accessible treatment options for mental health disorders in the population, especially in the MENA region.
INTRODUCTION
Mental disorders are among the top 10 causes of disability and disease burden worldwide, accounting for 970 million cases in 2019. Estimation provided by another study went beyond these values, indicating that on a global scale, these disorders comprise approximately 32.4% of years lived with disability (YLD) and 13.0% of disability-adjusted life-years (DALYs).1 Mental disorders are common in both genders, with an estimated lifetime risk of 37.66% and 32.05% in women and men, respectively.2 Mental disorders result in significant financial burdens, comprising direct expenses associated with diagnosis and treatment, as well as indirect expenses arising from the associated disability and mortality.3 On a global scale, poor mental health is associated with an approximate annual cost of $2.5 trillion.4 Considering the variations in the burden of mental disorders, it is essential to evaluate their epidemiology in different regions of the world. Such studies can serve as a foundation for future preventive measures to mitigate their associated burden.5
The Middle East and North Africa (MENA) region comprises 21 countries that share a range of common sociodemographic attributes.6 Considering these similarities, studying the epidemiology of mental disorders across these countries allows for a comparison of their experiences in addressing such conditions, thereby facilitating the sharing of these experiences to enhance mental health in the region.6,7 Some studies on the epidemiology of mental disorders have been published in recent years.6,8,9,10,11 However, these studies have mainly focused on individual disorders. To date, no study has investigated the total burden of mental disorders in the MENA region. As mental health services can be used for a variety of disorders,12 determining the total burden attributable to mental disorders can assist policymakers and healthcare providers in shaping their policies to improve the mental health of the population. Furthermore, no comparative study has been conducted on the burden of different mental disorders across demographic groups in the MENA region to determine the specific needs of each demographic group. Therefore, in this study, we evaluated the burden of mental disorders in the MENA region from 1990 to 2019.
MATERIALS AND METHODS
Data source
We used global burden of disease (GBD) data in our study, which was conducted by the Institute of Health Metrics and Evaluation to evaluate the burden and risk factors of diseases across 204 regions and territories of the world from 1990 to 2019. Further details about the methodological aspects of the GBD study have been reported elsewhere.13,14 The Ethics Committee of Tehran University of Medical Sciences approved the study protocol (approval number: IR.TUMS.MEDICINE.REC.1401.170).
Disorders
In this study, we included mental disorders from the GBD project, including schizophrenia, depressive disorders (major depressive disorders and dysthymia), bipolar disorder, anxiety disorders, eating disorders (anorexia nervosa and bulimia nervosa), autism spectrum disorders (ASD), attention-deficit/hyperactivity disorder (ADHD), conduct disorder, idiopathic developmental intellectual disability, and other mental disorders. The definition of conditions for mental disorders in GBD was mainly based on the International Classification of Diseases-10 and DSM-IV criteria.15
Indices
We retrieved data on the burden of mental disorders from 1990 to 2019 across age groups, genders, and MENA countries, including Algeria, Afghanistan, Egypt, Iran, Iraq, Jordan, Libya, Bahrain, Oman, Kuwait, Lebanon, Saudi Arabia, Morocco, Palestine, Qatar, Türkiye, Sudan, Tunisia, the United Arab Emirates (UAE), Yemen, and Syria. We obtained crude and age-standardized rates per 100,000 people for prevalence, incidence, mortality, years of life lost (YLL), YLD, and DALY.
The estimation of YLD was derived from systematic literature reviews, archived data sources, and survey data. In the GBD study, YLD was estimated by multiplying prevalence by disability weights associated with each disorder based on its severity. Disability weights ranged from 0 to 1, with higher values indicating greater severity.15
YLL for anorexia nervosa and bulimia nervosa was computed by multiplying cause-specific deaths by the expected remaining years of life at the time of death, determined by a normative life expectancy. The cause of death was specified based on verbal autopsy, police, cancer, vital registry and records, sibling history, and other census and survey data. DALYs were calculated by summing YLD and YLL values.15
We also retrieved sociodemographic index (SDI) values ranging from 0 to 1, with higher values indicative of better sociodemographic status. SDI is calculated based on the fertility rate of young individuals under 25 years, the mean educational years of those 15 years or older, and income per capita.
Statistical analysis
We used locally estimated scatterplot smoothing (LOESS) regression to examine the association between age-standardized DALY rates and SDI values across the MENA countries from 1990 to 2019. LOESS regression is a non-parametric smoothing technique employed to evaluate the relationship between two variables depicted in a scatterplot. This method assigns greater weight to values near the predicted values, producing a distinctive LOESS curve that effectively illustrates the predicted values corresponding to the given data points.16,17 We chose this method due to the complexity of the data, hypothesizing that the association between the DALY rate and SDI might not follow a linear pattern and could vary across different SDI values. We employed Python version 3.8 for data analysis, figure creation, and choropleth map generation.
RESULTS
The DALY rate of mental disorders in the MENA countries has increased by 13.88% from 1,747.92 per 100,000 people in 1990 to 1,990.5 per 100,000 people in 2019. The DALY rates of MDD (674.24 per 100,000), anxiety disorders (504.06 per 100,000), and bipolar disorders (168.13 per 100,000) were higher compared with other mental disorders in 2019 (Table 1). In 2019, the DALY rate of mental disorders was higher in females than in males (2,236.79 vs. 1,762.69 per 100,000 people). However, the DALY rates of schizophrenia, ASD, ADHD, conduct disorder, and idiopathic developmental intellectual disability were higher among males than females (Table 1).
Table 1. Burden of Mental Disorders Across Genders and Years in the Middle East and North Africa Countries.
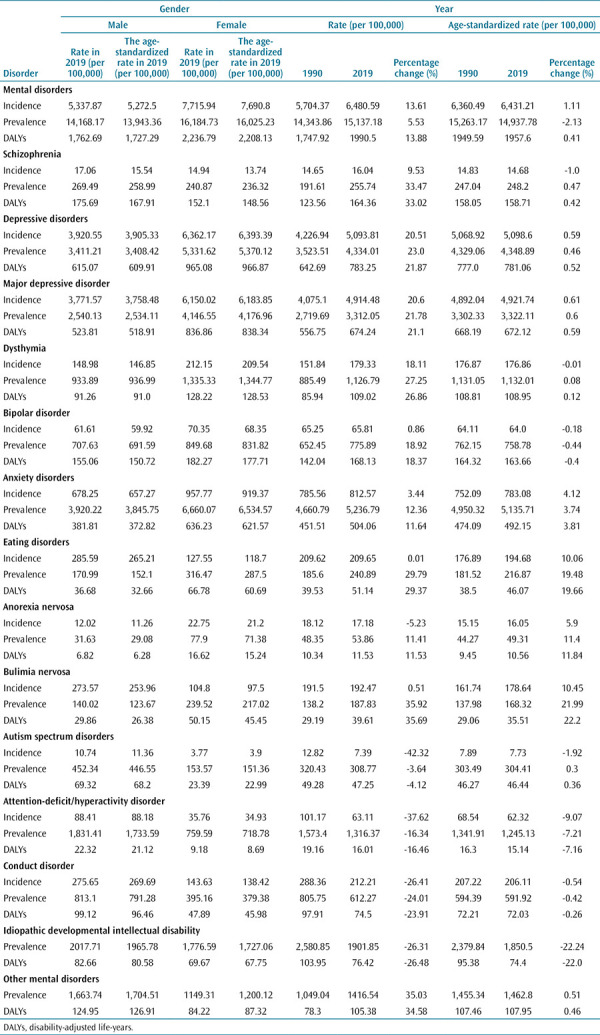
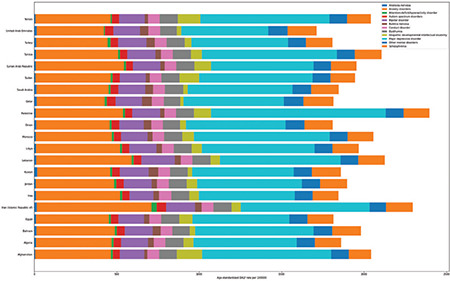
The highest percentage increases in the DALY rates of mental disorders from 1990 to 2019 were for bulimia nervosa (35.69%), other mental disorders (34.58), and schizophrenia (33.02%) (Figure 1). On the contrary, the DALY rates of idiopathic developmental intellectual disability (-26.48%), conduct disorder (-23.91%), ADHD (-16.46%), and ASD (-4.12%) decreased in the MENA region from 1990 to 2019.
Figure 1.
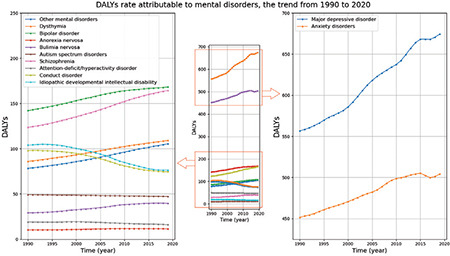
Trends in disability-adjusted life-years rates for mental disorders in the Middle East and North Africa region from 1990 to 2019.
DALYs, disability-adjusted life-years
The highest DALY rates of mental disorders in the MENA region in 2019 were observed in the 35-39 years age group, reaching 2,359.2 per 100,000 for males and 3,103.3 per 100,000 for females. The DALY rate of mental disorders was higher in females than males in the age group of ≥ 10 years. Conversely, in individuals younger than 10 years, the burden of mental disorders was higher in males than in females (Figure 2). In 2019, the highest DALY rates for mental disorders were observed in the age groups of ≤ 4 years, 5-19 years, and ≥ 20 years for idiopathic developmental intellectual disability, anxiety disorders, and MDD, respectively (Figure 3).
Figure 2.
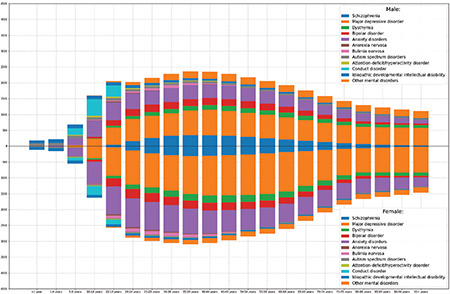
Disability-adjusted life-years rate of mental disorders in males and females across age groups in the Middle East and North Africa in 2019.
Figure 3.
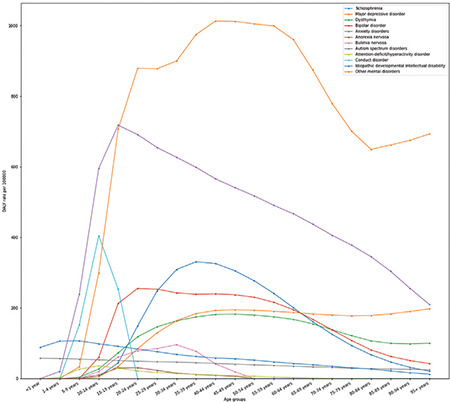
Disability-adjusted life-years rate attributable to mental disorders across age groups in the Middle East and North Africa in 2019.
The age-standardized DALY rate of mental disorders was the highest in Palestine (2,396.9 per 100,000), Iran (2,295.8 per 100,000), and Lebanon (2,126.0 per 100,000) compared with other MENA countries in 2019. In contrast, the age-standardized DALY rate was the lowest in the UAE (1,712.2 per 100,000), Türkiye (1,807.8 per 100,000), and Oman (1,809.5 per 100,000) (Figure 4).
Figure 4.
Age-standardized disability-adjusted life-years rate of mental disorders across the Middle East and North Africa countries in 2019.
The age-standardized DALY rate of depressive disorders was the highest in Palestine (1,168 per 100,000), Morocco (934.58 per 100,000), and Tunisia (930.15 per 100,000) in 2019. On the contrary, it was the lowest in the UAE (628.63 per 100,000), Iraq (690.87 per 100,000), and Türkiye (696.29 per 1000). The age-standardized DALY rate of eating disorders was the highest in Kuwait (74.05 per 100,000), Qatar (74.02 per 100,000), and the UAE (64.14 per 100,000) in 2019. In contrast, it was the lowest in Afghanistan (24.71 per 100,000), Yemen (26.06 per 100,000), and Sudan (30.94 per 100,000) (Figure 5 and Supplementary Figure 1).
Figure 5.
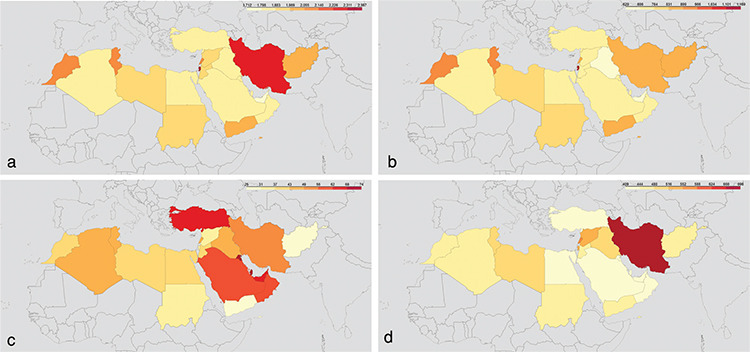
Age-standardized disability-adjusted life-years rate attributable to mental disorders across the Middle East and North Africa countries in 2019. (a) Mental disorders, (b) depressive disorders, (c) eating disorders, (d) anxiety disorders.
The association between SDI, age-standardized DALY rate, and SDI across MENA countries and years is shown in Figure 6, where the black lines indicate the predicted curve. There was a negative association between SDI and the age-standardized DALY rate of mental and depressive disorders. In contrast, there was a positive association between the age-standardized DALY rate of eating disorders and SDI (Figure 6 and Supplementary Figure 2).
Figure 6.
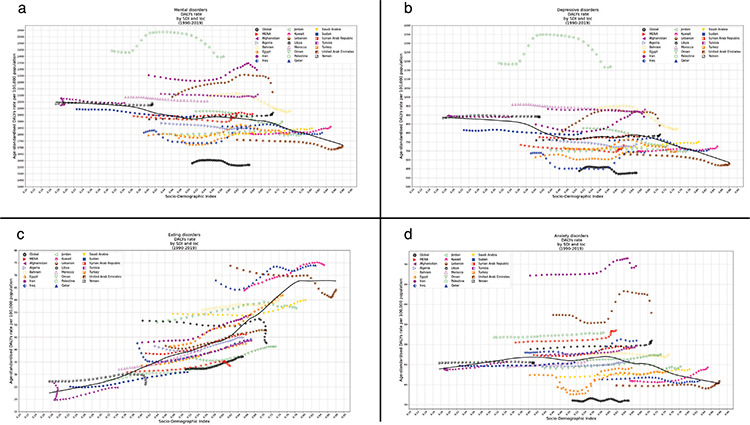
Association between age-standardized disability-adjusted life-years rate of mental disorders and sociodemographic index across the Middle East and North Africa countries and years. (a) Mental disorders, (b) depressive disorders, (c) eating disorders, (d) anxiety disorders.
DALYs, disability-adjusted life-years; SDI, sociodemographic index
DISCUSSION
In this article, we present, to the best of our knowledge, the most comprehensive assessment of trends in the burden of mental disorders in the MENA region from 1990 to 2019, highlighting the differences across demographic groups, regions, and years. Considering the population size and distribution structure change, the DALY rate of mental disorders has relatively increased from 1990 to 2019. Furthermore, we identified existing disparities in mental disorder DALY across regions, genders, and age groups.
We observed an increase in mental disorder DALY from 1990 to 2019 in the MENA region. Similarly, the global trend has also indicated an increase during the same period. From 1990 to 2019, there was a global increase in the burden of DALYs caused by mental disorders. The number of DALYs increased from 80.8 million to 125.3 million, and the proportion of global DALYs attributed to mental disorders increased from 3.1% to 4.9%.15 The demand for healthcare services is expected to increase with population growth. This is especially crucial in low-income and middle-income countries, where ensuring adequate treatment and care for the growing population is essential.18 Effective intervention options are available for mental disorders, which can alleviate the burden caused by these disorders.19 These interventions can help reduce the severity of symptoms, increase the likelihood of recovery, and decrease the risk of mortality.20,21 However, globally, there is a considerable lack of access to these services and insufficient resources allocated for their expansion. In addition, there are various barriers to receiving care, such as the perception of needing care and the stigma associated with mental health issues.22,23 Given the rising trend in the burden of mental disorders in the MENA region, coupled with limited insurance coverage, lack of services, and insufficient amenities,24,25 policymakers must ensure the provision of adequate facilities for the treatment and care of individuals with mental disorders. Moreover, given the prominent role of stigma as a barrier in MENA countries, increasing awareness about mental disorders in the region can mitigate stigma and promote greater utilization of healthcare facilities by individuals with mental disorders.25,26
In 2019, the DALY rates of MDD, anxiety disorders, and bipolar disorders were higher than those of other mental disorders in the MENA region. This finding is relatively consistent with the global burden of mental disorders, where depressive disorders, anxiety disorders, and schizophrenia had the highest DALY rates in 2019.15 According to the available data, there is compelling evidence indicating that experiences, such as childhood sexual abuse, intimate partner violence, being a victim of bullying, wars, and conflicts, have substantially contributed to the amplified load of depressive and anxiety disorders affecting individuals of all genders.27,28,29 The prevalence of intimate partner abuse in the Middle East is estimated to be around 26.3%, with psychological abuse being the most common type.30 Additionally, the MENA region is an area with the highest rates of armed conflict and war in the world.31 There is no study at the regional scale on the prevalence of childhood sexual abuse; however, studies conducted in Lebanon have indicated that the incidence of childhood sexual abuse ranges from 17% to 24%.32,33 Therefore, these factors may play crucial roles in the high prevalence of depressive and anxiety disorders in the region.
These findings indicate a decline in DALY rates for idiopathic developmental intellectual disability, conduct disorder, ADHD, and ASD in the MENA region between 1990 and 2019. The rise and development of prenatal genetic screening for hereditary causes of intellectual disabilities could be a plausible explanation for the reduced burden of these disorders in the MENA region in recent years.34,35 Our observation of a reduced burden of ASD in the MENA region contrasts with the global trend, where the burden of ASD has increased.36 The decreasing trend in the prevalence and incidence of ASD in MENA may be due to suboptimal case detection, lack of awareness about ASD, and stigma toward ASD.36,37 Similarly, the burden of conduct disorder has decreased in the MENA region, contrasting with the global trend.38 Further studies are needed to explore the potential reasons for this decline. Conversely, the highest increase in DALY rates for mental disorders during the same period was observed in patients with bulimia nervosa and schizophrenia, aligning with previous studies. In the MENA region, the rapid pace of urbanization has emerged as a significant risk factor that can substantially augment the disease burden of schizophrenia, as indicated by the DALYs associated with this mental health condition.39,40 Previous studies have also indicated a rising prevalence of eating disorders in the MENA region and Arab countries.41 Cultural shifts and the adoption of Western attitudes toward body shape and weight could be potential reasons for the increasing burden of eating disorders, including bulimia nervosa, in the region.42 Additionally, we discovered a positive association between SDI and age-standardized DALY rates in MENA countries. The economic growth and improvements in socioeconomic status, particularly in Arab countries, may also contribute to the increasing burden of eating disorders, including bulimia nervosa, in the region.43 Therefore, with the region’s ongoing economic growth, we may observe further increases in the burden of eating disorders in MENA. This necessitates additional attention from policymakers in the region.
Females are generally more susceptible to mental disorders than males.44 In addition, our study findings indicate that the DALY rate of mental disorders was higher in females than in males aged 10 years and above. Conversely, in individuals younger than 10 years, the burden of mental disorders was higher in males than in females. These results align with the global pattern observed in 2019. In 2019, depressive, anxiety, and eating disorders were more common in females, particularly among older age groups. Conversely, ADHD and ASD were more prevalent in males, especially among younger age groups.15 Evidence suggests that men and women experience different types of mental health problems. Women tend to have higher rates of internalizing disorders, such as depression and anxiety. In contrast, men are more likely to exhibit externalizing disorders, including substance abuse and antisocial behavior, which can have negative impacts on others.45,46 The burden of mental disorders was notably higher among adults aged 35-39, 40-44, and 30-34 years, encompassing both sexes, as they were within the working-age range. In a 2014 study conducted in Iran, it was observed that middle-aged women encounter challenges related to their mental health. The findings revealed two main themes: increased life concerns and physical and psychological tensions. The participants voiced concerns about how their multiple responsibilities affected their overall mental well-being.47 This alarming statistic raises serious concerns about the impact of mental disorders on the productivity and well-being of the working age population. Effective interventions and support systems are urgently needed to alleviate the burden of mental health issues in these crucial demographics.48,49 These findings emphasize the importance of considering gender and age disparities when addressing the burden of mental disorders. Tailoring interventions and providing targeted support based on these differences can improve mental health outcomes and ensure more effective and equitable mental health care for individuals of all ages and genders.
In 2019, the age-standardized DALY rate for mental disorders was notably higher in Palestine, Iran, and Lebanon compared to other MENA countries. Conversely, the UAE, Türkiye, and Oman had the lowest rates of age-standardized DALY. It is worth mentioning that Palestine, which has endured nearly five decades of conflict, bears the greatest burden related to mental disorders in the MENA region. Emotional and behavioral disorders were estimated to affect 54.4% of boys and 46.5% of girls aged 6 to 12 years in Palestine.50 A recent study conducted in 2022 revealed that countries, such as Egypt, Iran, and Türkiye, exhibited the highest percentages of anxiety disorder-related DALYs resulting from bullying victimization.6 The study also revealed that Iran had the highest percentage of DALYs related to MDD caused by intimate partner violence. Interestingly, Palestine exhibited the highest percentages of MDD-related DALYs attributed to childhood sexual abuse.6 Conversely, a higher socioeconomic status, including elevated income levels and improved access to education and healthcare, can significantly alleviate mental health burdens in countries, such as the UAE and Oman. This is because individuals with better socioeconomic conditions have greater employment opportunities, increased social support systems, and improved living standards, all of which positively impact their mental well-being. In addition, these individuals may have access to better mental healthcare services, such as therapy or counseling, which can help prevent, manage, or treat mental health issues effectively. As a result, the prevalence of mental health issues and their associated burdens can be lower in countries with higher socioeconomic status.18,51
We found mixed findings concerning the association between SDI and the burden of mental disorders in MENA countries. We found that the age-standardized DALY rate of eating disorders is positively correlated with SDI, which is consistent with previous studies. In a comparative study assessing the prevalence of eating disorders in both Western and non-Western countries, these disorders were more prevalent in Western nations. Concurrently, a rising trend in the prevalence of eating disorders has been identified in non-Western countries.52 Studies support this finding, highlighting that urbanization can indirectly impact the prevalence of eating disorders through economic, social, and environmental factors.53 However, there was an inverse association between the burden of depression and SDI, which contrasts with the previous studies. Previous studies have observed a positive correlation between the country’s GDP per capita and the risk of lifetime mood disorder.54 In another study, the prevalence of depression was higher in high- and upper-middle-income countries compared to low-middle- and low-income countries, based on World Bank criteria.55 Therefore, future studies are warranted to determine the underlying social, economic, and environmental factors contributing to the higher burden of depressive disorders in countries with lower SDI in the MENA region.
This study utilized data obtained from the estimates of GBD, and all the limitations inherent in GBD applied to this article. Although GBD provides an enhanced and reliable estimate of the GBD, it also has certain unavoidable limitations. One limitation, consistent with other GBD studies, is the heterogeneity in data collection methods, data sources, and quality. Each country has collected data with varying degrees of quality using various methods. The collapse of healthcare systems due to regional conflicts raises questions about the validity of data in some MENA countries. Second, our study did not consider substance use disorders.
To conclude, there has been a slight increase in the burden of mental disorders in the MENA region between 1990 and 2019. It is concerning that these conditions persistently present a notable health burden, chiefly because social inequality independently impacts mental disorders in specific populations. Our research findings strongly reinforce the perspective that mental conditions should be recognized as a central health challenge of the 21st century in the MENA region. Therefore, national policies must prioritize evidence-based preventive measures and ensure accessible treatment options for mental health disorders, especially in the MENA region.
Footnotes
Ethics Committee Approval: The ethics committee of Tehran University of Medical Sciences approved the study protocol (approval number: IR.TUMS.MEDICINE.REC.1401.170).
Data Sharing Statement: Raw data is publicly available from the GBD website (https://vizhub.healthdata.org/gbd-results/).
Authorship Contributions: Concept- A.N.A.; Design- M.E., A.N.A., S.R.D.; Supervision- M.E., A.N.A., A.H.M.; Fundings- M.E., A.N.A.; Data Collection or Processing- A.N.A., S.R.D.; Analysis or Interpretation- A.N.A., S.R.D.; Writing- A.N.A., F.G., S.T.K., S.S., H.N., S.R.D.; Critical Review- M.E., A.N.A., F.G., S.T.K., S.S., H.N., A.H.M., S.R.D.
Conflict of Interest: No conflict of interest was declared by the authors.
Funding: This study was supported by Tehran University of Medical Sciences (grant number: 57758).
References
- 1.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3:171–178. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 2.Pedersen CB, Mors O, Bertelsen A, et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014;71:573–581. doi: 10.1001/jamapsychiatry.2014.16. [DOI] [PubMed] [Google Scholar]
- 3.Trautmann S, Rehm J, Wittchen HU. The economic costs of mental disorders: Do our societies react appropriately to the burden of mental disorders? EMBO Rep. 2016;17:1245–1249. doi: 10.15252/embr.201642951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Lancet Global Health. Mental health matters. Lancet Glob Health. 2020;8:1352. doi: 10.1016/S2214-109X(20)30432-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barbui C, Gureje O, Patten SB, Puschner B, Thornicroft G. On the need for epidemiology in psychiatric sciences. Epidemiol Psychiatr Sci. 2020;29:e1. doi: 10.1017/S2045796019000507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moradinazar M, Mirzaei P, Moradivafa S, Saeedi M, Basiri M, Shakiba M. Epidemiological status of depressive disorders in the Middle East and North Africa from 1990 to 2019. Health Promot Perspect. 2022;12:301–309. doi: 10.34172/hpp.2022.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barry MM. Addressing the determinants of positive mental health: concepts, evidence and practice. International Journal of Mental Health Promotion. 2009;11:4–17. [Google Scholar]
- 8.Amini S, Bagheri P, Moradinazar M, Basiri M, Alimehr M, Ramazani Y. Epidemiological status of suicide in the Middle East and North Africa countries (MENA) from 1990 to 2017. Clin Epidemiol Glob Health. 2021;9:299–303. doi: 10.1016/j.cegh.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Safiri S, Noori M, Nejadghaderi SA, et al. Comparison of the burden of anorexia nervosa in the Middle East and North Africa region between 1990 and 2019. J Eat Disord. 2022;10:192. doi: 10.1186/s40337-022-00718-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Safiri S, Noori M, Nejadghaderi SA, et al. The estimated burden of bulimia nervosa in the Middle East and North Africa region, 1990-2019. Int J Eat Disord. 2023;56:394–406. doi: 10.1002/eat.23835. [DOI] [PubMed] [Google Scholar]
- 11.Safiri S, Mousavi SE, Nejadghaderi SA, et al. The Burden of Attention-Deficit Hyperactivity Disorder (ADHD) in the Middle East and North Africa Region, 1990 to 2019. J Atten Disord. 2023;27:1433–1447. doi: 10.1177/10870547231187161. [DOI] [PubMed] [Google Scholar]
- 12.Wang PS, Aguilar-Gaxiola S, Alonso J, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370:841–850. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1562. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–150. doi: 10.1016/S2215-0366(21)00395-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cleveland WS, Devlin SJ. Locally weighted regression: an approach to regression analysis by local fitting. Journal of the American Statistical Association. 1988:596–610. [Google Scholar]
- 17.Jacoby WG. Loess: a nonparametric, graphical tool for depicting relationships between variables. Electoral Studies. 2000;19:577–613. [Google Scholar]
- 18.Hudson CG. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatry. 2005;75:3–18. doi: 10.1037/0002-9432.75.1.3. [DOI] [PubMed] [Google Scholar]
- 19.Reichenberg LW, Seligman L. Selecting effective treatments: A comprehensive, systematic guide to treating mental disorders: 5th ed. John Wiley & Sons. 2016. [Google Scholar]
- 20.Belvederi Murri M, Ekkekakis P, Magagnoli M, et al. Physical exercise in major depression: reducing the mortality gap while improving clinical outcomes. Front Psychiatry. 2019;9:762. doi: 10.3389/fpsyt.2018.00762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fusar-Poli P, McGorry PD, Kane JM. Improving outcomes of first-episode psychosis: an overview. World Psychiatry. 2017;16:251–265. doi: 10.1002/wps.20446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patel V, Chisholm D, Parikh R, et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Lancet. 2016;387:1672–1685. doi: 10.1016/S0140-6736(15)00390-6. [DOI] [PubMed] [Google Scholar]
- 23.Coombs NC, Meriwether WE, Caringi J, Newcomer SR. Barriers to healthcare access among U.S. adults with mental health challenges: A population-based study. SSM Popul Health. 2021;15:100847. doi: 10.1016/j.ssmph.2021.100847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nawaz R, Mahmood N, Al Mughairbi F, Khera G. Thought-Provoking Issues about Mental and Physical Health in the Middle East: An Overview. Remittances Review. 2023;8:2515–2525. [Google Scholar]
- 25.Pocock L. Mental health issues in the Middle East-an overview. Middle East J Psychiatry Alzheimers. 2017;8:10–15. [Google Scholar]
- 26.Sewilam AM, Watson AM, Kassem AM, et al. Suggested avenues to reduce the stigma of mental illness in the Middle East. Int J Soc Psychiatry. 2015;61:111–120. doi: 10.1177/0020764014537234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bauer NS, Herrenkohl TI, Lozano P, Rivara FP, Hill KG, Hawkins JD. Childhood bullying involvement and exposure to intimate partner violence. Pediatrics. 2006;118:235–242. doi: 10.1542/peds.2005-2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bell V, Méndez F, Martínez C, Palma PP, Bosch M. Characteristics of the Colombian armed conflict and the mental health of civilians living in active conflict zones. Confl Health. 2012;6:10. doi: 10.1186/1752-1505-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blanco C, Rubio J, Wall M, Wang S, Jiu CJ, Kendler KS. Risk factors for anxiety disorders: common and specific effects in a national sample. Depress Anxiety. 2014;31:756–764. doi: 10.1002/da.22247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moshtagh M, Amiri R, Sharafi S, Arab-Zozani M. Intimate partner violence in the Middle East region: a systematic review and meta-analysis. Trauma Violence Abuse. 2023;24:613–631. doi: 10.1177/15248380211036060. [DOI] [PubMed] [Google Scholar]
- 31.Sørli ME, Gleditsch NP, Strand H. Why is there so much conflict in the Middle East? J Conflict Resol. 2005;49:141–165. [Google Scholar]
- 32.Usta J, Farver J. Child sexual abuse in Lebanon during war and peace. Child Care Health Dev. 2010;36:361–368. doi: 10.1111/j.1365-2214.2010.01082.x. [DOI] [PubMed] [Google Scholar]
- 33.El Khoury C, Mutchler MG, Abi Ghanem C, et al. Sexual Violence in Childhood and Post-Childhood: The Experiences of Young Men Who Have Sex With Men in Beirut. J Interpers Violence. 2021;36:NP11198–NP11217. doi: 10.1177/0886260519880164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Acharya K. Prenatal testing for intellectual disability: misperceptions and reality with lessons from Down syndrome. Dev Disabil Res Rev. 2011;17:27–31. doi: 10.1002/ddrr.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verma IC, Puri RD. Global burden of genetic disease and the role of genetic screening. Semin Fetal Neonatal Med. 2015;20:354–363. doi: 10.1016/j.siny.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 36.Solmi M, Song M, Yon DK, et al. Incidence, prevalence, and global burden of autism spectrum disorder from 1990 to 2019 across 204 countries. Mol Psychiatry. 2022;27:4172–4180. doi: 10.1038/s41380-022-01630-7. [DOI] [PubMed] [Google Scholar]
- 37.Rafiei M, Nakhostin-Ansari A, Meshkat S, Khosravi A, Memari AH. Public awareness and stigma of autism spectrum disorder in Iran; An online survey. Res Dev Disabil. 2023;134:104441. doi: 10.1016/j.ridd.2023.104441. [DOI] [PubMed] [Google Scholar]
- 38.Wu J, Chen L, Li X, et al. Trends in the prevalence of conduct disorder from 1990 to 2019: Findings from the Global Burden of Disease Study 2019. Psychiatry Res. 2022;317:114907. doi: 10.1016/j.psychres.2022.114907. [DOI] [PubMed] [Google Scholar]
- 39.Sari D. Increasing Urbanisation and Pollution in the MENA Region: Causes of Conflicts? Security and Environment in the Mediterranean: Conceptualising Security and Environmental Conflicts. Springer. 2003:843–860. [Google Scholar]
- 40.Pedersen CB, Antonsen S, Timmermann A, et al. Urban-Rural Differences in Schizophrenia Risk: Multilevel Survival Analyses of Individual- and Neighborhood-Level Indicators, Urbanicity and Population Density in a Danish National Cohort Study. Schizophrenia Bulletin Open. 2022;3(1):sgab056. [Google Scholar]
- 41.Pike KM, Hoek HW, Dunne PE. Cultural trends and eating disorders. Curr Opin Psychiatry. 2014;27:436–442. doi: 10.1097/YCO.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 42.Miller MN, Pumariega AJ. Culture and eating disorders: A historical and cross-cultural review. Psychiatry. 2001;64:93–110. doi: 10.1521/psyc.64.2.93.18621. [DOI] [PubMed] [Google Scholar]
- 43.Ncube M, Anyanwu J, Hausken K. Inequality, economic growth and poverty in the Middle East and North Africa (MENA) African Development Review. 2014;26:435–453. [Google Scholar]
- 44.Kessler RC, Ustun TB. The WHO World Mental Health Surveys: Global perspectives on the epidemiology of mental disorders. New York: Cambridge University Press. 2008. [Google Scholar]
- 45.Afifi M. Gender differences in mental health. Singapore Med J. 2007;48:385–391. [PubMed] [Google Scholar]
- 46.Rosenfield S, Mouzon DM. Gender and Mental Health. 2013:277–296. [Google Scholar]
- 47.Sharifi K, Anoosheh M, Foroughan M, Kazemnejad A. Barriers to Middle-Aged Women’s Mental Health: A Qualitative Study. Iran Red Crescent Med. 2014. doi: 10.5812/ircmj.18882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hakulinen C, Komulainen K, Suokas K, et al. Socioeconomic position at the age of 30 and the later risk of a mental disorder: a nationwide population-based register study. J Epidemiol Community Health. 2023;77:298–304. doi: 10.1136/jech-2022-219674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li A, Wang D, Lin S, et al. Depression and Life Satisfaction Among Middle-Aged and Older Adults: Mediation Effect of Functional Disability. Front Psychol. 2021;12:755220. doi: 10.3389/fpsyg.2021.755220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Charara R, Forouzanfar M, Naghavi M, et al. The Burden of Mental Disorders in the Eastern Mediterranean Region, 1990-2013. PLoS One. 2017;12:e0169575. doi: 10.1371/journal.pone.0169575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reiss F, Meyrose AK, Otto C, Lampert T, Klasen F, Ravens-Sieberer U. Socioeconomic status, stressful life situations and mental health problems in children and adolescents: Results of the German BELLA cohort-study. PLoS One. 2019;14:e0213700. doi: 10.1371/journal.pone.0213700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Makino M, Tsuboi K, Dennerstein L. Prevalence of eating disorders: a comparison of Western and non-Western countries. MedGenMed. 2004;6:49. [PMC free article] [PubMed] [Google Scholar]
- 53.Gorrell S, Trainor C, Le Grange D. The impact of urbanization on risk for eating disorders. Curr Opin Psychiatry. 2019;32:242–247. doi: 10.1097/YCO.0000000000000497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hidaka BH. Depression as a disease of modernity: explanations for increasing prevalence. J Affect Disord. 2012;140:205–214. doi: 10.1016/j.jad.2011.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rai D, Zitko P, Jones K, Lynch J, Araya R. Country- and individual-level socioeconomic determinants of depression: multilevel cross-national comparison. Br J Psychiatry. 2013;202:195–203. doi: 10.1192/bjp.bp.112.112482. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


