Abstract
Background and study aim
The development of a new cholangioscope, the SpyGlass™ Discover (Boston Scientific), has allowed the laparoscopic transcystic common bile duct exploration and stone clearance. The possibility of simultaneous treatment of choledocholithiasis during early laparoscopic cholecystectomy offers the opportunity to enormously reduce the time between acute cholecystitis diagnosis and the execution of cholecystectomy with better outcomes for patients. Furthermore, an altered anatomy of the gastrointestinal tract is not an obstacle to this technique. The aim of the study was to determine whether this new procedure is feasible, safe, and effective.
Patients and methods
The investigation employs a retrospective case series study including all consecutive patients with a diagnosis of common bile duct stones undergoing cholecystectomy and intraoperative laparoscopic common bile duct clearance using SpyGlass™ Discover at IRCCS Policlinico San Matteo in Pavia (Italy). Eighteen patients were included from May 2022 to May 2023.
Results
A complete clearance of the common bile duct was obtained in 88.9% of patients. The mean postoperative length of stay was 3 days. No major complications occurred. After a median follow-up of 8 months, no recurrence of biliary events or readmissions occurred.
Conclusion
This procedure has proven to be feasible, safe, and effective.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13017-023-00529-0.
Keywords: Case series, Choledochoscopy, Choledocholithiasis, Cholangioscopy, SpyGlass
Introduction
Common bile duct stones (CBDS) are present in 10–20% of patients with gallstones and in 5–15% of patients with acute calculous cholecystitis (ACC) [1].
In order to diagnose and treat biliary obstruction, endoscopic retrograde cholangiopancreatography (ERCP) stands as the gold standard [2]. However, ERCP is rarely used for diagnostic purposes, while second level examination, i.e., endoscopic ultrasound (EUS) or magnetic resonance cholangiopancreatography (MRCP), is often needed before ERCP for the diagnosis of CBDS. However, ERCP, EUS, and MRCP are costly and might not be readily available. The latter may cause ACC patients' surgical therapy to be delayed and decrease a favorable outcome [3–6]. Indeed, it is widely recognized and stated by international guidelines [1] that the best treatment for patients with ACC is early laparoscopic cholecystectomy (ELC). The definition of ELC is cholecystectomy performed as soon as possible from the moment of ACC diagnosis, preferably within 72 h following admission [3–6]. Among the reasons that make it challenging to achieve this aim (i.e., performing laparoscopic cholecystectomy as soon as possible) is the diagnosis of the presence of CBDS and their treatment by ERCP before performing laparoscopic cholecystectomy.
Recent pieces of research reported how simultaneous laparoscopic cholecystectomy and intraoperative ERCP stand as safer procedures for individuals with cholecystocholedocholithiasis. Such a joint procedure might facilitate intubation, decrease the need for additional stone removal operations, reduce hospital stays, and lessen postoperative problems, such as pancreatitis and stone residue [7]. However, in some cases, an altered anatomy of the gastrointestinal tract (e.g., after gastric, pancreatic, or biliary surgery) or a particular conformation of the duodenal papilla may prevent the papilla from being reached or intubated, making it impossible to perform ERCP. Furthermore, performing an intraoperative ERCP during cholecystectomy, especially in an emergency setting, is often burdened by major organizational and coordination issues among different specialists and the operating room.
In recent years, the development of a new cholangioscope, the SpyGlass™ Discover (Boston Scientific) [8–12] with an outer diameter of 3.5 mm, has allowed the laparoscopic transcystic CBD exploration and CBDS clearance. The possibility of simultaneous treatment of CBDS with SpyGlass™ Discover, after intraoperative cholangiography (IOC), during ELC offers the opportunity to enormously reduce the time between ACC diagnosis and the execution of ELC with better outcomes for these patients. Furthermore, an altered anatomy of the gastrointestinal tract is not an obstacle to this technique. The article presents a single-center case series including patients undergoing intraoperative laparoscopic transcystic treatment of CBDS using SpyGlass™ Discover during cholecystectomy.
Material and methods
Design
The present investigation stands as a retrospective case series study including all consecutive patients with a diagnosis of CBDS undergoing cholecystectomy and intraoperative laparoscopic CBD clearance using the cholangioscope SpyGlass™ Discover at IRCCS Policlinico San Matteo in Pavia (Italy). On a one-year horizon, from May 2022 to May 2023, 18 patients were included. The aim of the study was to determine whether this new procedure is feasible, safe, and effective.
Ethical considerations
Patients provided written informed consent. The study was carried out in line with the Helsinki Declaration. The ethics approval was not required for the collection, analysis, and publication of the retrospectively obtained and anonymized data for this case series.
Studied variables
Preoperative, intraoperative, and postoperative data were collected for all patients. Postoperative complications were defined with Clavien–Dindo grade. All patients were contacted by phone for follow-up.
Results
From May 2022 to May 2023, 18 patients with a diagnosis of CBDS underwent cholecystectomy and intraoperative laparoscopic CBD clearance using SpyGlass™ Discover at IRCCS Policlinico San Matteo in Pavia (Italy). The details of the patients and their clinical outcomes are reported in Table 1.
Table 1.
Characteristics and outcomes of patients undergoing common bile duct exploration and clearance with SpyGlass Discover
| No. | Age | Admission | Reason for admission | Preoperative attempt to ERCP | Preoperative imaging | Previous abdominal surgery | ASA | POSSUM-PS | Operative time (min) | Failure of cystic duct intubation | Complete clearance of CBD | ICU admission | Postoperative LOS | Total LOS | Postoperative complications | Clavien–Dindo grade | Need of postop ERCP |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 73 | Emergency | ACC with suspected CBDS | No | EUS | Yes | 2 | 20 | 240 | 0 | 1 | 0 | 3 | 11 | 0 | 0 | 0 |
| 2 | 75 | Emergency | ACC with suspected CBDS | No | CT | Yes | 2 | 21 | 300 | 0 | 1 | 0 | 3 | 15 | 0 | 0 | 0 |
| 3 | 71 | Emergency | ACC with suspected CBDS | No | US | No | 2 | 22 | 180 | 0 | 1 | 0 | 2 | 10 | 0 | 0 | 0 |
| 4 | 70 | Emergency | ACC with suspected CBDS | No | US | Yes | 2 | 32 | 180 | 0 | 1 | 0 | 5 | 9 | Biliary leak from drainage, spontaneously resolved | 1 | 0 |
| 5 | 51 | Emergency | AP with suspected CBDS | No | CT | Yes | 2 | 19 | 150 | 0 | 1 | 0 | 2 | 8 | 0 | 0 | 0 |
| 6 | 80 | Emergency | ACC with suspected CBDS | No | US | Yes | 2 | 24 | 240 | 0 | 1 | 0 | 2 | 5 | 0 | 0 | 0 |
| 7 | 85 | Emergency | ACC with suspected CBDS | No | MRCP | Yes | 2 | 17 | 180 | 0 | 1 | 0 | 4 | 8 | Asymptomatic rise of serum lipases, spontaneously resolved | 1 | 0 |
| 8 | 69 | Emergency | ACC with suspected CBDS | No | CT | Yes | 2 | 17 | 150 | 0 | 1 | 0 | 5 | 6 | 0 | 0 | 0 |
| 9 | 82 | Elective | CBDS | No | MRCP | Yes | 2 | 23 | 120 | 0 | 1 | 0 | 1 | 3 | 0 | 0 | 0 |
| 10 | 54 | Emergency | ACC with suspected CBDS | No | US | No | 2 | 15 | 210 | 0 | 1 | 0 | 8 | 15 | 0 | 0 | 0 |
| 11 | 65 | Emergency | ACC and AP with suspected CBDS | No | US | No | 2 | 16 | 150 | 0 | 1 | 0 | 1 | 13 | 0 | 0 | 0 |
| 12 | 84 | Emergency | ACC with suspected CBDS | No | US | Yes | 2 | 36 | 210 | 1 | 0 | 0 | 3 | 12 | 0 | 0 | 1 |
| 13 | 76 | Elective | CBDS | No | US | Yes | 2 | 18 | 150 | 0 | 1 | 0 | 2 | 5 | 0 | 0 | 0 |
| 14 | 85 | Emergency | ACC and AP with CBDS | No | TC | Yes | 2 | 19 | 210 | 0 | 1 | 0 | 2 | 8 | 0 | 0 | 0 |
| 15 | 79 | Elective | AP with suspected CBDS | Yes, failure of major papilla intubation | MRCP | No | 2 | 15 | 120 | 0 | 1 | 0 | 2 | 5 | 0 | 0 | 0 |
| 16 | 83 | Emergency | AP with suspected CBDS | Yes, failure of major papilla intubation | US | Yes | 2 | 26 | 210 | 0 | 1 | 0 | 2 | 15 | 0 | 0 | 0 |
| 17 | 76 | Emergency | ACC with suspected CBDS | No | CT | No | 2 | 28 | 140 | 0 | 1 | 1 (for associated comorbidity) | 8 | 9 | 0 | 0 | 0 |
| 18 | 65 | Elective | CBDS | No | US | Yes | 2 | 14 | 210 | 0 | 0 | 0 | 3 | 3 | Biliary leak from drainage, spontaneously resolved | 1 | 1 |
ACC, acute calculous cholecystitis; AP, acute pancreatitis; CBDS, common bile duct stones; EUS, endoscopic ultrasonography; CT, computed tomography; MRCP, magnetic resonance cholangiopancreatography; CBD, common bile duct
The mean age of patients was 73.5 ± 10.1, and their mean POSSUM physiological score was 21.2. 77.8% of patients were admitted to the ward from the Emergency Department. 66.7% had a diagnosis of ACC, and the 27.8% of acute biliary pancreatitis. Four patients were admitted for an elective intervention for a diagnosis of CBDS and impossibility to perform ERCP. Three of them had a previous esophageal-gastric surgery, while one had an earlier failure of major papilla intubation. The diagnosis of CBDS was made with ultrasound (US) in 44.4% of patients, with CT scan in 27.8% and with EUS or MRCP in 22.2%, as reported in Table 2. In two patients (11.1%), an ERCP was attempted and failed for the impossibility of papilla intubation. In our series, the size of the main biliary duct stones (obtained from preoperative imaging) ranged from sludge to 1 cm.
Table 2.
Preoperative patients characteristics
| Characteristics | Mean ± SD Median (IQR) N (%) |
|
|---|---|---|
| Age (years) |
73.5 ± 10.1 75.5 (69.0–82.0) |
|
| Sex | Male | 11 (61.1) |
| Female | 7 (38.9) | |
| Hospital admission | Emergency | 14 (77.8) |
| Elective | 4 (22.2) | |
| Patients with ACC | 12 (66.7) | |
| Patients with AP | 5 (27.8) | |
| Imaging for CBDS diagnosis | Only US | 8 (44.4) |
| CT scan | 5 (27.8) | |
| MRCP | 3 (16.7) | |
| EUS | 1 (5.6) | |
| POSSUM-PS |
21.2 ± 6.1 19.5 (17.0–24.0) |
|
| PCR (mg/dl) |
7.1 ± 10.4 2.4 (0.9–8.3) |
|
| PCT (ng/mL) |
1.8 ± 1.7 1.3 (0.3–3.2) |
|
| Serum lipase (U/L) |
66.3 ± 62.9 36.0 (30.5–71.5) |
|
| Gamma-GT (mU/mL) |
137.8 ± 148.8 61.0 (29.5–217.0) |
|
| AP (UI/L) |
125.4 ± 48.6 114.0 (85.5–165.0) |
|
| Direct bilirubin (mg/dl) |
2.5 ± 2.1 0.9 (0.9–3.9) |
|
ACC, acute calculous cholecystitis; AP, acute pancreatitis; CBDS, common bile duct stones; US, ultrasonography; EUS, endoscopic ultrasonography; CT, computed tomography; MRCP, magnetic resonance cholangiopancreatography; POSSUM-PS, POSSUM physiological score; PCR, protein-c reactive; PCT, procalcitonin; gamma-GT, gamma-glutamyl transferase; AP, alkaline phosphatase
Laparoscopic cholecystectomy was performed in the American position. Laparoscopic access was performed by an optical 12mm umbilical trocar after Verres needle insufflation in Palmer point. In patients with previous surgeries, we entered the abdomen with an open technique and placed a 12-mm trocar at the umbilicus to insufflate the abdomen. Then, three more trocars were placed: an epigastric 12 mm and two 5-mm trocars in right flank (one on the right anterior axillary line and one in the midclavicular line), as highlighted in the following Fig. 1.
Fig. 1.
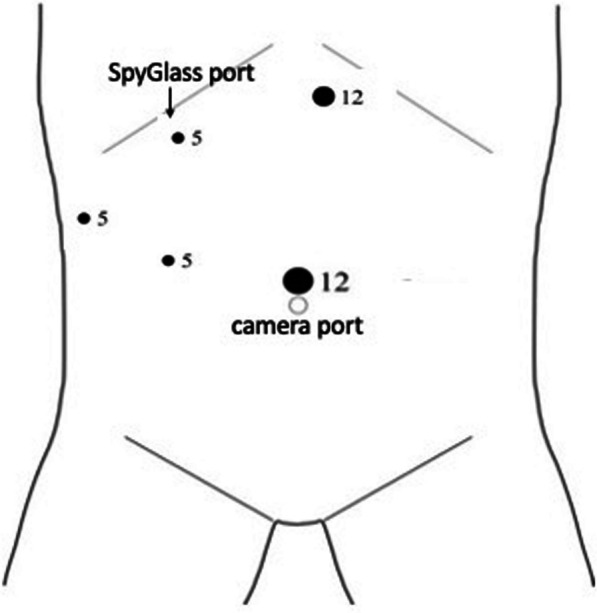
Trocar position
The cystic duct was isolated, and a transcystic intraoperative cholangiography (IOC) was performed to confirm the presence of CBDS. In case of CBDS confirmation, a fifth 5-mm trocar in the right hypochondrium was placed for cholangioscope SpyGlass™ Discover insertion. The cystic duct was intubated with the cholangioscope after positioning of the guide wire, and a cholangioscopy of the CBD was performed (Fig. 2A, B, Additional file 1: Video 1). In cases of very small or winding cystic duct, a complete cystic duct isolation and intubation of the duct more proximal to the CBD was necessary. The major papilla was passed, and the SpyGlass™ gently pushed up into the duodenum. Then, the SpyGlass™ was retracted in the CBD, and the stones removed with one of the following techniques, depending on the characteristics of the stones and the papilla:
In the case of sludge, it was pushed into duodenum through the papilla with pressure washing using the washing channel of the instrument;
In the case of small stones (smaller than cystic duct diameter), they were removed through the cystic duct using the basket (Additional file 1: Video 1);
In the case of big stones and of a permissive papilla, stones were pushed into the duodenum under direct vision through the papilla using the cholangioscope (Fig. 2C, D).
Fig. 2.
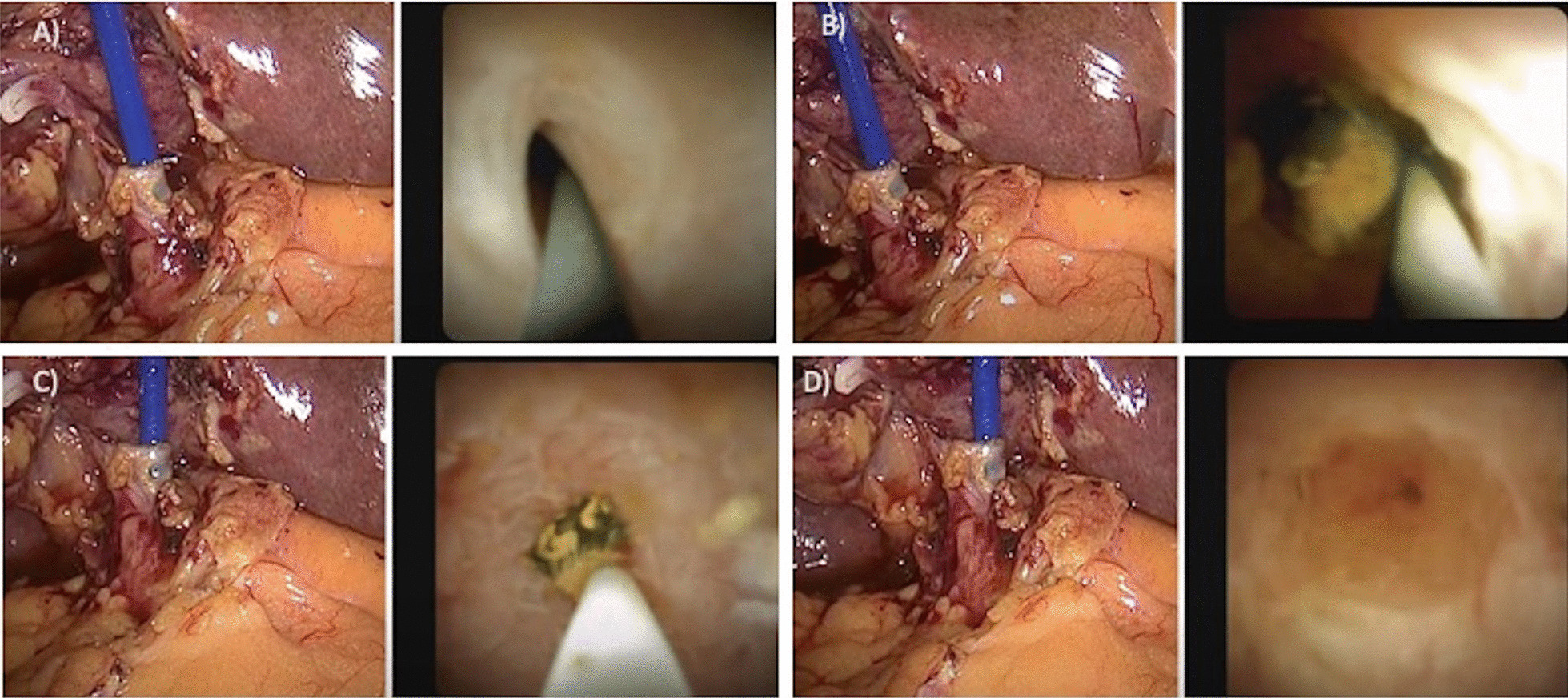
Laparoscopic cholangioscopy and common bile duct stones removal using SpyGlass™ Discover: A intubation of the cystic duct with the cholangioscope after positioning of guide wire; B cholangioscopy and common bile duct stones finding; C removal of stones, which are pushed beyond the duodenal papilla; D complete clearance of the common bile duct
After CBDS removal, a transcystic IOC was performed to confirm complete CBD clearance. The cystic duct was closed with Hemolock clip or with laparoscopic suture with PDS wire and the cholecystectomy completed. A drain was positioned under the liver and removed, if no biliary leak occurred, in second postoperative day.
We obtained a complete clearance of the CBD using the cholangioscope SpyGlass™ Discover in the 88.9% of patients. Two patients (11.1%) needed postoperative ERCP.
In one patient, we failed to intubate the cystic duct due to its small diameter, and a postoperative ERCP for CBDS removal was necessary.
In one patient with seven quite big stones in the CBD and a fibrotic papilla, we failed to pass it and reach the duodenum. Then, because we could not make the stones overcome the papilla, we removed five stones through the cystic duct using the basket. However, one stone was too large to pass the cystic duct, and we failed to reach a complete CBD clearance. This patient had a low-flow biliary leak from drainage on the first postoperative day, which spontaneously resolved. The patient underwent ERCP for residual CBDS removal. During the procedure, a transpapillary cholangiography was performed without biliary leak evidence.
The mean operative time was 186 min. No intraoperative complications occurred.
After the first procedure that was performed in collaboration with endoscopists, all the following procedures were performed by a team of general surgeons only. The mean postoperative LOS was 3 days and the total mean LOS was 9 days. Three patients (16.6%) had minor postoperative complications (Clavien–Dindo 1): two patients had a low-flow biliary leak from drainage and one patient had an asymptomatic rise of serum lipase, all spontaneously resolved in 1–2 days. No major complications occurred (Table 3). After a median follow-up of 8 months (IQR 149–356 days), no new biliary events, post-discharge complications, or readmissions occurred.
Table 3.
Intraoperative and postoperative outcomes
| Characteristics | Mean ± SD Median (IQR) N (%) |
|---|---|
| Operative time (minutes) |
186.1 ± 47.2 180.0 (150.0–210.0) |
| Intraoperative complication | 0 (0.0) |
| Failure of cystic duct intubation | 1 (5.6) |
| Complete clearance of CBD | 16 (88.9) |
| Postoperative LOS (days) |
3.2 ± 2.1 2.5 (2.0–4.0) |
| Total LOS (days) |
8.9 ± 4.0 8.5 (5.0–12.0) |
| Postoperative minor complications (CD < 3) | 3 (16.7) |
| Postoperative major complications (CD ≥ 3) | 0 (0.0) |
| Need of postoperative ERCP | 2 (11.1) |
LOS, length of stay; CBD, common bile duct; CD, Clavien–Dindo
Discussion
The SpyGlass™ Digital Catheter is intended to provide direct visualization and guide optical and accessory devices for diagnostic and therapeutic applications during endoscopic procedures in the pancreaticobiliary system. It is specifically designed for the complete visualization of the extrahepatic biliary tree. The SpyGlass™ incorporates a perfusion channel to retain a good field of view and a greater optical resolution than traditional bile duct scopes. Additionally, it has a four-way angle which allows to easily visualize narrow and intricate ducts, such as the cystic and intrahepatic bile ducts [9]. The characteristics of SpyGlass™ Discover allows the percutaneous or laparoscopic transcystic exploration of CBD and the CBDS removal. Furthermore, SpyGlass™-guided electrohydraulic or laser lithotripsy can be used for difficult common bile duct stones not amenable to conventional endoscopic therapy.
Recently, there have been several reports regarding the peroral use of the SpyGlass™ DS for the diagnosis of indeterminate biliary stricture [8] and cystic duct neoplasm [9]. Furthermore, the use of SpyGlass™ technology for single-operator transpapillary [10] or percutaneous [11] cholangioscopy for removing difficult stones has been described too.
To our knowledge, this case series is the second and the largest published in the literature that includes patients undergoing intraoperative laparoscopic transcystic treatment of CBDS using SpyGlass™ Discover during cholecystectomy.
Up to now, only a series of four cases of patients undergoing intraoperative laparoscopic transcystic treatment of CBDS using SpyGlass™ Discover during cholecystectomy was reported by Kouli et al. with good outcomes [12].
Also a case of a patient with a huge stone in the CBD successfully treated with laparoscopic choledochotomy and cholangioscopy using SpyGlass™ Discover was reported by Palermo et al. [13]. However, probably for the huge diameter of the stone, the CBD exploration in this case was not performed with the transcystic technique.
There are many advantages of laparoscopic CBDS removal using SpyGlass™ Discover during cholecystectomy. First of all, the laparoscopic cholangioscopy is likely burdened with low risks due to the fact that it is not necessary to perform papillosphincterotomy. Our series confirms this low-risk profile, in particular, it showed no major complication after the procedure, no acute pancreatitis or post-procedural bleeding. Furthermore, this procedure is readily available, because the operation could be entirely performed by acute care surgeons or general surgeons during laparoscopic cholecystectomy, without needing endoscopic training. In patients with ACC with suspected CBDS, the opportunity to simultaneous treatment of CBDS during ELC, offers the possibility of enormously reducing the time between ACC diagnosis and the execution of ELC with better outcomes for these patients [3–6].
It should be noted that in our series, the total LOS is quite long, as, until recently, in our institution, the device was available only under special request due to the previous hospital’s administrative policy. Because the device is currently fully functional, we expect the preoperative time to be shorter. Indeed, most patients with ACC and associated CBDS are likely to receive ELC and simultaneous CBDS removal within 72h from admission.
Another advantage of this technique is the possibility to explore the CBD also in patients with altered gastrointestinal anatomy or in case of difficult access to the papilla (e.g., in the case of intradiverticular papilla). In our series, two patients with CBDS underwent successful laparoscopic CBDS removal after a failed ERCP due to the difficulty of papilla intubation.
The present series shows the safety and effectiveness of the intraoperative laparoscopic transcystic treatment of CBDS using SpyGlass™ Discover during cholecystectomy, reporting a success rate of 89% and no major complications.
The present study has evident limitations. First of all, this is a retrospective case series. The sample size is limited, and lacks a control group. However, this series represents one of the first pieces of evidence of the innovative application of SpyGlass™ Discover cholangioscope. Results are encouraging, and it emerges how the procedure is feasible, effective, and safe. The next step will be to compare the efficacy and risk profile of this procedure with ERCP followed by cholecystectomy. In this regard, the "INtraoperative Approach with eventual Clearance of Common bilE duct by SpyGlass™ Discover vs Sequential strategy in patients with acute calculus cholecystitis and Intermediate/high risk of common BiLE duct stone (INACCESSIBLE)" will soon begin in Italy. In this trial, patients with ACC with high/intermediate risk of CBDS, according to the score by Khoury et al. [14, 15], will be randomized to receive ERCP + ELC in two-stage procedures (control group) or simultaneous ELC + SpyGlass™ cholangioscopy and CBDS removal (study group).
Supplementary Information
Additional file 1: Video 1. Laparoscopic cholangioscopy and common bile duct stones removal using SpyGlass™ Discover.
Author contributions
PF, LC, and LA were involved in study conception; PF and LC performed manuscript conception and draft and contributed to important scientific knowledge; AP and FC helped in data collection; PF, LC, CMB, AP, AM, EC, FC, TM, MT, JV, AA, and LA critically revised the manuscript; all authors gave the final approval.
Funding
Dr Paola Fugazzola, Dr Francesca Calabretto, Dr Enrico Cicuttin, Prof Francesca Dal Mas, Dr Tommaso Dominioni, Dr Marcello Maestri, Dr Aurelio Mauro, Dr Alice Podestà, Dr Matteo Tomasoni, Dr Francesco Brucchi, Dr Jacopo Viganò, Prof Luca Ansaloni, Dr Andrea Anderloni, Prof Lorenzo Cobianchi have no conflicts of interest or financial ties to disclose.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author at reasonable request.
Declarations
Ethical approval
Patients provided written informed consent. The ethics approval was not required for the collection, analysis, and publication of the retrospectively obtained and anonymized data for this case series.
Consent for publication
Not applicable.
Competing interests
Dr. Paola Fugazzola, Dr. Francesca Calabretto, Dr. Enrico Cicuttin, Prof. Francesca Dal Mas, Dr. Tommaso Dominioni, Dr. Marcello Maestri, Dr. Aurelio Mauro, Dr. Alice Podestà, Dr. Matteo Tomasoni, Dr. Francesco Brucchi, Dr. Jacopo Viganò, Prof. Luca Ansaloni, Dr. Andrea Anderloni, and Prof. Lorenzo Cobianchi have no conflicts of interest or financial ties to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pisano M, Allievi N, Gurusamy K, Borzellino G, Cimbanassi S, Boerna D, et al. 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg. 2020;15(1):1–26. doi: 10.1186/s13017-020-00336-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adams MA, Hosmer AE, Wamsteker EJ, Anderson MA, Elta GH, Kubiliun NM, et al. Predicting the likelihood of a persistent bile duct stone in patients with suspected choledocholithiasis: accuracy of existing guidelines and the impact of laboratory trends. Gastrointest Endosc. 2015;82(1):88–93. doi: 10.1016/j.gie.2014.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brooks K, Scarborough J, Vaslef S, Shapiro M. No need to wait: an analysis of the timing of cholecystectomy during admission for acute cholecystitis using the American College of Surgeons National Surgical Quality Improvement Program database. Trauma Acute Care Surg. 2013;74(1):167–73; 173–4. 10.1097/TA.0b013e3182788b71. [DOI] [PubMed]
- 4.Al-Mulhim AA. Timing of early laparoscopic cholecystectomy for acute cholecystitis. J Soc Laparoendosc Surg. 2008;12(3):282–287. [PMC free article] [PubMed] [Google Scholar]
- 5.Wiggins T, Markar SR, MacKenzie H, Faiz O, Mukherjee D, Khoo DE, et al. Optimum timing of emergency cholecystectomy for acute cholecystitis in England: population-based cohort study. Surg Endosc. 2019;33(8):2495–2502. doi: 10.1007/s00464-018-6537-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alore EA, Ward JL, Todd SR, Wilson CT, Gordy SD, Hoffman MK, et al. Ideal timing of early cholecystectomy for acute cholecystitis: an ACS-NSQIP review. Am J Surg. 2019;218(6):1084–1089. doi: 10.1016/j.amjsurg.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Liao Y, Cai Q, Zhang X, Li F. Single-stage intraoperative ERCP combined with laparoscopic cholecystectomy versus preoperative ERCP Followed by laparoscopic cholecystectomy in the management of cholecystocholedocholithiasis: a meta-analysis of randomized trials. Medicine (United States) 2022;101(10):E29002. doi: 10.1097/MD.0000000000029002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogura T, Imanishi M, Kurisu Y. Prospective evaluation of digital single-operator cholangioscope for diagnostic and therapeutic procedures (with videos) Digest Endosc. 2017;29:782–789. doi: 10.1111/den.12878. [DOI] [PubMed] [Google Scholar]
- 9.Matsuzawa H, Goto T, Shibuya T, Sato W, Chiba M, Takahashi K, et al. A preoperative diagnosis of advanced cystic duct carcinoma using SpyGlass DS cholangioscopy: a report of two cases. Intern Med. 2023;62(11):1617–1623. doi: 10.2169/internalmedicine.9732-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shin J, Oh C, Dong S. Single-operator cholangioscopy guided lithotripsy. Korean J Gastroenterol. 2022;80(4):163–168. doi: 10.4166/kjg.2022.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Colombi D, Bodini FC, Morelli N, Aragona G, Ciatti C, Maniscalco P, et al. Spyglass percutaneous transhepatic lithotripsy of symptomatic recurrent lithiasis of the intrahepatic bile duct with distal stenosis. Acta Biomed. 2022;93(1):1–5. doi: 10.23750/abm.v93i1.12338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kouli T, Gresz R, Khan J, Abdelwaheed S, Zino S. OGBN O06 sharing experience of SpyGlass TM discover and electrohydraulic lithotripsy in treating large bile duct stone through the trans-cystic approach during laparoscopic. Br J Surg. 2022;109(Supplement_9):10. doi: 10.1093/bjs/znac404.029. [DOI] [Google Scholar]
- 13.Palermo M, Fendrich I, Ronchi A, Obeid J, Gimenez M. Laparoscopic common bile duct exploration using a single-operator cholangioscope. J Laparoendosc Adv Surg Technol. 2020;30(9):989–992. doi: 10.1089/lap.2020.0534. [DOI] [PubMed] [Google Scholar]
- 14.Khoury T, Kadah A, Mari A, Kalisky I, Katz L, Mahamid M, et al. A validated score predicting common bile duct stone in patients hospitalized with acute calculus cholecystitis: a multi-center retrospective study. Surg Endosc. 2020;1:1. doi: 10.1007/s00464-020-07853-5. [DOI] [PubMed] [Google Scholar]
- 15.Fugazzola P, Cobianchi L, Dal Mas F, Cicuttin E, Dominioni T, Frassini S, et al. Prospective validation of the Israeli Score for the prediction of common bile duct stones in patients with acute calculous cholecystitis. Surg Endosc. 2023;37(11):8562–8569. doi: 10.1007/s00464-023-10442-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Video 1. Laparoscopic cholangioscopy and common bile duct stones removal using SpyGlass™ Discover.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author at reasonable request.


