Abstract
Background and aims
Despite a huge body of evidence on the linkage between dietary intakes and pattern of sleeping, the findings are controversial. The current study aimed to summarize earlier findings on the association between adherence to Mediterranean diet (MD) and pattern of sleeping.
Methods
This study performed based on PRISMA guideline. Systematically search was applied in PubMed, Scopus and Google Scholar to find out relevant publications appeared up to February 2023. No restrictions on language and time of publication were applied. Duplicate citations were removed. We included observational studies which assessed MD as the main exposure and kind of sleep disorders as the main outcome.
Results
A total of 20 observational studies included. Out of these studies, two were cohort studies and 18 had a cross-sectional design. A total of 21,714 participants included. Usual dietary intakes were assessed using a validated Food Frequency Questionnaire, and a diet history questionnaire. Some studies did not report methods of measuring habitual dietary intakes. Adherence to MD was evaluated by KIDMED questionnaire, PREMED, alternate Mediterranean (aMed) questionnaire, MEDAS questionnaire, MedDietScore, MEDI-LITE score, modified Mediterranean Diet Score (mMDS), Mediterranean food pattern (MFP) and modified Mediterranean diet score (mMED). Pattern of sleeping was examined as sleep quality, sleep duration, sleep latency, sleep efficacy, sleepiness, sleep disturbance, taking a nap and some other sleep disorders.
Conclusion
In conclusion, findings of published studies highlighted the importance of consumption of MD for better sleep quality.
Keywords: Mediterranean diet, Sleep pattern, Sleep disorders, Sleep quality, Sleep hygiene, Sleep disturbance, Sleep, Dietary pattern
Intruduction
Sleep is an important physiological function to repair and clear tissue and brain [1]. World Health Organization expressed that 27% of the world’s population suffer from sleep disorders [2, 3]. Other sleep disorders include sleep-disordered breathing (SDB), parasomnias, narcolepsy, and restless leg syndrome [4]. As a common health problem in modern society, sleep disorder have a high incidence in the elderly population, which seriously affect the quality of life and physical and mental health [5]. There is a high prevalence of sleep disturbance worldwide as 7.8% of adults had severe sleep problems in the general population [6]. The prevalence of sleep disorder in older Iranian adults was reported as 48.9% [7]. Medical conditions, depression, anxiety, or cognitive dysfunction can occur along with sleep disorders [8]. These disorders can increase the risk of stroke [9, 10], migraine [11], neurodevelopmental disorders [12] and irritable bowel syndrome [13]. Despite the role of several factors in sleep quality, including age, sex, body weight and depression [14], dietary factors have received great attention recently. Consumption of fruit, vegetables, dairy products and various vitamins and minerals have been previously studied in this regard [15]. However, limited data are available abut theses specific dietary patterns. The Mediterranean diet (MD) is a diet based on high consumption of green leafy vegetables, fruits, fish, healthy fats mainly olive oil, legumes, whole grains, nuts and seeds, moderate intake of dairy products and wine consumption as well as low consumption of processed foods, confectionery and red meat [16, 17]. This diet is low in saturated fat and high in vegetable oils, which observed in Greece and Southern Italy during the 1960s [2]. The MD consists of antioxidants, anti-inflammatory micronutrients and n-3 fatty acids and is characterized by a high intake of monounsaturated fat and fiber [18].
The association between MD and various health-related outcomes has been previously studied [19]. For instance, some documents have shown that the high adherence to the MD can be associated with a lower incidence of chronic diseases and lower aging impairment [20] and frailty [21]. MD also can affect against platelet aggregation [22] and mental disorders including cognitive decline and cancer [23]. In fact, weight loss programs based on the MD, can decrease the lean tissue losses [24]. MD beneficial effects seem to be exerted in both populations of Mediterranean and non-Mediterranean areas [23].
Adherence to the Mediterranean diet has also been studied in relation to sleep patterns; however, findings were conflicting. For example, in a cohort study on the US women aged 20–76 y, adherence to the Mediterranean diet was associated with better sleep quality, higher sleep efficiency, and lower sleep disorders [25]. In contrast, van Egmond et al. in a study on 970 Swedish older men failed to see any significant association between adherence to the MD and self-reported sleep initiation and sleep maintenance problems [26]. Despite having several studies in this field, no systematic review has been conducted on the relationship between MD and sleep disorders. Overall, given the presence of conflicting results on the association between MD and sleep disorders, there is a need for a systematic review summarizing all available findings in this field. Considering above, we performed the current study to systematically review all available studies regard to the relationship between MD and sleep pattern.
Methods
Search strategy
This study performed based on PRISMA, protocol for reporting systematic reviews. We performed a comprehensive literature search in the online databases of PubMed, Scopus and Google Scholar up to January 2024. The key words which used for this search were as follows: “Mediterranean Diets” OR “diet” OR “Mediterranean dietary pattern” OR “Feeding Behavior” OR “dietary adherence” OR “dietary score” OR “Mediterranean score OR “MD score” OR “food pattern” OR “dietary habit” OR “Mediterranean dietary score” OR “Mediterranean” OR “dietary pattern” accompanied by “Sleep Disorders” or “insomnia” or “Sleep Wake Disorders” or “Sleep Disorders, Circadian Rhythm” or “Sleep” or “Sleep Deprivation” or “Sleep quality” or “Sleep disturbance” or “Sleep quality index” or “Sleep duration” or “Sleep impairment”. All keywords were based on MeSH and non-MeSH terms. All references of selected articles were also reviewed to find relevant missing publications.
Selection
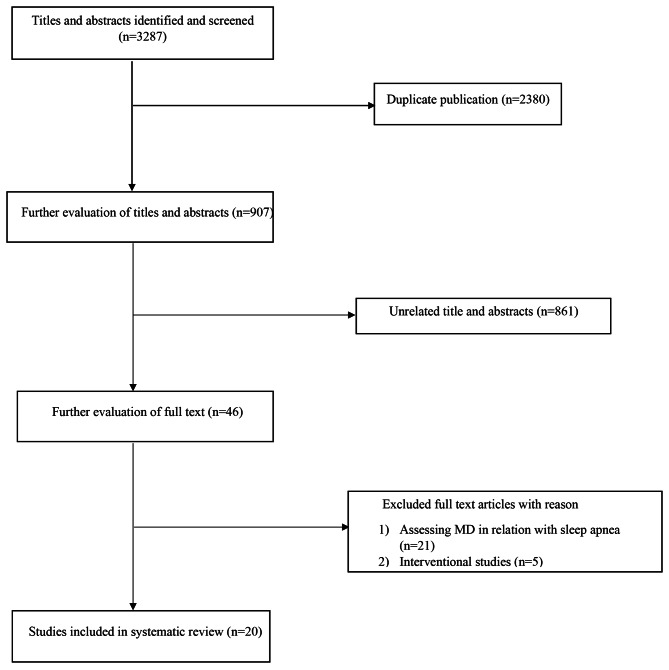
No restrictions on language and time of publications were applied. Duplicate citations were removed. Observational studies assessing the association between adherence to MD and sleep pattern were included in this systematic review. We included studies with the following criteria: (1) observational studies with prospective, case-control or cross-sectional design; (2) studies that considered adherence to MD as the main exposure; (3) those that had examined every kind of sleep disorders as the main outcome or as one of the outcomes. We excluded letters, comments, short communications, reviews, meta-analyses, ecological studies, and animal studies. A flow diagram of the study selection is shown in Fig. 1.
Fig. 1.
Flow chart of participation
Data abstraction
Required data from each eligible study were extracted by two independent investigators, and any disagreements were reconciled by discussion. The following information was extracted: name of the first author, publication year, individuals’ characteristics (mean age and sex), study design, sample size, method of assessment of exposure, type of study outcome, and method of outcome assessment.
Results
Totally, 3287 articles were found in our initial search; of them 2380 duplicate articles were excluded. After screening the remaining 907 records, 861 unrelated articles were also removed based on title and abstract assessment. Then, 46 articles remained for further evaluation of the full text. Out of those 46 studies, 21 studies were excluded due to assessing MD in relation to sleep apnea and other five studies were also excluded due to having interventional design. Finally, 20 articles were included in the current systematic review. All these studies had examined the association between MD and sleep disorders. Required information for each study has been given in Table 1. All included studies assessed in terms of demographic information as follow including study design, study location and date, exposure assessment, assessment of adherence to Mediterranean diet and outcome assessment.
Table 1.
Characteristics of included studies on the association between consumption of Mediterranean diet and pattern of sleeping
| Author | Gender | Study Design | Country | Age | Outcome Assessment | Exposure Assessment | Sample Size | Study Quality | Outcome | Result | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Zuraitkat et al. 2020 | female 100% | Cohort | USA | 20–76 y | PSQI a | FFQb /aMed score | 432 | Fair quality | Sleep onset latency | lower sleep onset latency | |
| Sleep efficiency | no association | ||||||||||
| Sleep disturbances | lower sleep disturbances | ||||||||||
| Godos et al. 2019 | female 58.5%, male 41.5% | cross sectional | Italy | over 18 y | PSQI | FFQ/Medi-lite score | 1936 | Good quality | Sleep quality | higher sleep quality | |
| Sleep latency | Lower sleep latency | ||||||||||
| Sleep duration | Lower shorter sleep duration | ||||||||||
| Habitual sleep efficacy | lower low sleep efficacy | ||||||||||
| Sleep disturbances | no association | ||||||||||
| Day time dysfunction | lower day dysfunction | ||||||||||
| Self-rated sleep quality | Higher sleep quality | ||||||||||
| need medication to sleep | no association | ||||||||||
| van Egmond et al. 2019 | females 53%, male 47% | cross sectional | Sweden | 71 ± 1 | questionnaires | food record/mMDS | 970 | Good quality | Sleep initiating problems | no association | |
| Sleep maintenance problems | no association | ||||||||||
| Mamalaki et al. 2018 | female 59.2%, male 40.8% | cross sectional | Greece | ≥ 65 y | questionnaires | FFQ / MedDietScore | 1639 | Good quality | Sleep duration | no association | |
| Sleep quality | lower trouble falling sleep, higher sleep adequacy | ||||||||||
| Flor-Alemany et al. 2020 | female 100% | cross sectional | Spain | 32.9 ± 4.6 | PSQI | FFQ /MFPc | 150 | Fair quality | Sleep quality | higher sleep quality during both the 16th and 34th | |
| Campanini et al. 2017 | female 51.4%, male 48.5% | Cohort | Spain | ≥ 60 y | questionnaires/ESSd | questionnaires/MEDASe | 1596 | Fair quality | indicator of Sleep quality | higher sleep quality | |
| Sleep duration | lower change in sleep duration | ||||||||||
| Castro-Diehl et al. 2018 | female 53.6%, male 46.4% | cross sectional | USA | 45–84 | WHIIRSf/Actigraphy | FFQ /aMed score | 2068 | Good quality | Insomnia | Lower insomnia by no change vs. decrease in a Med score | |
| Sleep duration | more likely to sleep 6–7 h/night (vs. <6 h/night) | ||||||||||
| Ferranti et al. 2016 | female 54.6%, male 45.5% | cross sectional | Italy | 11-14y | questionnaires/PDSSg | FFQ /KIDMED | 1586 | Good quality | sleep quality | higher total sleep time, week day sleep time | |
| sleep quantity | Lower insomnia | ||||||||||
| Adelantado-Renau et al. 2018 | girl 48%, boys 52% | cross sectional | Spain | 14-18y | PSQI/Wrist-worn accelerometer | KIDMEDh | 269 |
Fair quality |
Sleep quality | Higher sleep quality | |
| Sleep duration | no association | ||||||||||
| Muscogiuri et al. 2020 | females71.5%/male 28.5% | Cross sectional | Italy | 51.8 ± 15.7 y | PSQI | PREDIMED | 172 | Fair quality | Sleep quality | Higher sleep quality | |
| Boraita et al. 2020 | females 50%, males 50% | Cross sectional | Spain | 12–17 y | questionnaire | KIDMED | 761 | Good quality | Sleep duration | More sleep duration | |
| Rosi et al. 2020 | females 46%, males 54% | Cross sectional | Italy | 11–14 y | questionnaires/PDSS | KIDMED | 409 | Good quality | Sleep duration | adequate sleep duration | |
| Sleep quality | higher sleep quality | ||||||||||
| daytime sleepiness | Lower sleepiness | ||||||||||
| ÖZCAN1 et al. 2021 | females 31%, males 69% | Cross sectional | Turkey | 19–65 y | PSQI | MEDAS/quesstionnaries | 1053 | Good quality | Sleep quality | higher sleep quality | |
| Zaidalkilani et al. 2021 | female | Cross sectional | Jordan | 36 ± 10 y | AIS | Questionnarie/ PREDIMED | 917 | Good quality | Insomnia | Lower insomnia | |
| Gupta et al. 2021 | female 26%, male 74% | Cross sectional | Costa Rican | questionnaires | FFQ /aMed score | 2169 | Good quality | Sleep duration | Adequate sleep duration | ||
| inconsistent between weekday-weekend sleep | no association | ||||||||||
| take nap | no association | ||||||||||
| Bakırhan et al. 2022 | females 63%, males 37% | Cross sectional | Turkey | 19–64 y | PSQI | MEDAS | 250 | Good quality | Sleep quality | higher sleep quality | |
| Naja et al. 2022 | Females 81.5%, males 18.5% | Cross sectional | Emirates | 22 y | PSQI | KIDMED | 503 | Good quality | Sleep quality | better subjective sleep quality | |
| sleep latency | less sleep latency | ||||||||||
| sleep disturbance | less sleep disturbance | ||||||||||
| Sleep medication | No association | ||||||||||
| Sleep duration | No association | ||||||||||
| daytime dysfunction | less daytime dysfunction | ||||||||||
| Sleep efficacy | No association | ||||||||||
| Yaghtin et val. 2022 | female | Cross sectional | Iran | 12–18 y | ISI j | FFQ/mMED k | 733 | Good quality | Insomnia | Lower insomnia | |
| López-Gil et al. 2023 | Females 55.3%, males 44.7% | Cross sectional | Spain | 12–17 y | questionnaire | KIDMED | 847 | Good quality | Sleep duration | Higher sleep duration | |
| Mantzorou et al. 2023 | Females 48.4%, males 51.6% | Cross sectional | Greek | ≥ 65 y | PSQI | MedDietScore/FFQ | 3254 | Good quality | Sleep quality | Higher sleep quality | |
a. Pittsburgh Sleep Quality Index
b. Food Frequency Questionnaire
c. Mediterranean food pattern
d. Epworth Sleepiness Scale
e. Mediterranean Diet Adherence Screener
f. Women’s Health Initiative Insomnia Rating Scale
g. Parkinson’s disease sleep scale
h. Mediterranean Quality Index for children and teenagers
i. Athens Insomnia Scale
j. Iranian version of the Insomnia Severity Index
k. modified Mediterranean diet score
Demographic information of included studies
Study design
Totally, out of 20 included studies, two were cohort studies [25, 27] and eighteen had cross-sectional design [26, 28–36]. The duration of follow up for two cohort studies ranged from one year to 2.8 years [25, 27].
Participant characteristics
Included studies consisted 21,714 participants. Sample sizes across studies varied from 150 [31] to 3254 people [37]. Participants aged over 11 years old. All studies were on both gender, except for four articles that were performed on women [25, 31, 38, 39]. Five studies were on older adults (60–84 y) [26, 27, 29, 33, 37] and seven on young adolescents (11–15 y) [28–30, 35, 38, 40, 41]. All studies had assessed healthy people, except for of study of Castro-Diehl et al. [29] that had included atherosclerosis patients. One study had included pregnant women [31].
Study location and date
Out of 20 studies, two were carried out in the USA [25, 29], four in Italy [30, 32, 34, 35], five in Spain [27, 28, 31, 40, 41], two in Turkey [42, 43], two in Greece [33, 37] and one each in Sweden [26], Iran [38], Jordan [39], Emirate [44] and Costa Rica [36]. All studies were published between 2016 and 2023.
Exposure and outcome assessment
Exposure assessment
Evaluation of usual dietary intakes were done in the included studies as follow: nine studies used validated Food Frequency Questionnaire (FFQ) [25, 29–33, 36–38] to assay dietary intakes. Dietary records [26] and diet history [27] was in tow other studies. The remaining three studies did not report any data on the methods of measuring habitual dietary intakes [28, 34, 35, 39, 41–44].
Assessment of adherence to MD
Calculation of Mediterranean diet score was done by the following methods in the included studies: a validated 16 items KIDMED questionnaire was used in six studies [28, 30, 35, 40, 41, 44] and a 14 items validated PREMED Questionnaire was applied in two studies [34, 39]. Three studies mentioned a 10 items validated alternate Mediterranean (aMed) questionnaire [25, 29, 36]. In addition, three studies used 12 items validated MEDAS questionnaire [27, 42, 43]. The others used 11 items Med Diet Score [33, 37], 9 items MEDI-LITE score [32] and 8 items modified Mediterranean Diet Score (mMDS) [26, 38]. The study of Flor Alemany et al. had used Mediterranean food pattern (MFP) which was a validated questionnaire [31].
Outcome assessment
Sleep quality and quantity were separately considered as primary outcomes. In general, eleven studies assessed sleep quality [27, 28, 31–35, 37, 42–44], ten studies considered sleep duration [27–29, 32, 33, 35, 36, 40, 41, 44], three studies investigated sleepiness [30, 33, 35], four studies investigated sleep disturbances [25, 31, 32, 44], three studies examined taking nap [30, 33, 36] and three studies examined sleep efficacy and sleep latency [25, 32, 44]. All other sleep disorders that were assessed in two other studies were need medication to sleep [32, 44], day time dysfunction [32, 44], sleep initiating problems [26], sleep maintenance problems [26], not quiet sleep, awaken short of breath or with a headache, feel drowsy or sleepy during the day, trouble falling asleep, awaken during sleep and have trouble falling asleep, trouble staying awake during the day, snore during sleep, snoring and sleep adequacy [33], insomnia [29, 38, 39], inconsistent between weekday-weekend sleep [36] bed time and wake time on weekday and weekend, total sleep time, weekdays sleep time and weekend sleep time [30]. To examine sleep disorders, Pittsburgh Sleep Quality Index (PSQI), a 19 items validated questionnaire, was used by nine studies [25, 28, 31, 32, 34, 37, 43, 44], Women’s Health Insomnia Rating Scale (WHIIRS) and a five-items validated questionnaire, was used in the study of Castro-Diehl et al. [29]. Iranian version of the Insomnia Severity Index (ISI) and Athens Insomnia Scale (AIS( was used to assess insomnia in two studies [38, 39]. A validated self-report questionnaires and pediatric daytime sleepiness scale (PDSS) was used by two studies [30, 35]. An Epworth Sleepiness Scale (ESS), an eight items validated questionnaire, was used in the study of Campanini et al. [27] Some other questionnaires were used in the other eight remaining studies [26, 27, 30, 33, 35, 36, 40, 41]. Actigraphy [29] and Wrist-worn accelerometer [28] were used for sleep duration assessment in just two studies, which allowed for evaluation of sleep phenotype.
The association between MD and sleep disorders
Sleep disorders in relation to the adherence to the Mediterranean diet were investigated in different studies as follow:
Sleep quality
Sleep quality was reported in the most included studies. Mamalaki et al. [33] assessed sleep quality by examining following items: daytime sleepiness, sleep adequacy, sleep disturbance, trouble falling asleep, take naps, feel drowsy or sleepy during the day, trouble staying awake during the day, snoring, snore during sleep, awaken during sleep and have trouble falling asleep and awaken short of breath or with a headache. Ferranti et al. [30] reported the association of a component of sleep quality with MD and did not consider total sleep quality. Eleven studies that evaluated the association of MD with sleep quality reported a greater adherence to the MD in association with a better sleep quality [37, 42–44].
Sleep duration
Seven publications assessed MD in relation to sleep duration. Six studies reported a significant association between adherence to MD and sleep duration [27, 32, 35, 36, 40, 41]. While three studies reported no significant association between MD and duration of sleep [28, 33, 44]. Castro-Diehl et al. [29] compared moderate-high aMed score to a low aMed score across different categories of objectively measured sleep duration (< 6 h/night, 6–7 h/night, 7–8 h/night and > 8 h/night). They reached no significant association in total; however, participants with a moderate-high aMed score were more likely to sleep 6–7 h/night than those who had a low aMed score.
Sleep latency
Sleep latency was examined in three studies [25, 32, 44]. All of them had reported adherence to the MD was associated with a lower sleep latency.
Sleep efficacy
Based on three studies that assessed adherence to MD in relation to sleep efficacy, two of them reported no significant association [25, 44] and the other found a lower occurrence of low sleep efficacy by a greater adherence to MD [32].
Sleepiness
All three studies [30, 33, 35] that evaluated adherence to MD and sleepiness by PDSS [35] and self-report questionnaires [30, 33] reported an inverse association between sleepiness and MD.
Sleep disturbances
Four studies considered sleep disturbances as the outcome of interest. Zuraitkat et al. [25] and Naja et al. [44] found an inverse association between consumption of MD and sleep disturbances among women, however, no significant association was seen between sleep disturbances and MD in Godos et al. [32] and Mamalaki et al. [33] studies.
Taking a nap
All three studies that evaluated the association between adherence to MD and taking a nap reported no statistically significant associations [30, 33, 36].
Other sleep disorders
In addition to the disorders mentioned above, some other sleep disturbances were also examined in some studies. Needing medications to sleep and self-rated sleep quality [32] as well as sleep initiating problems and sleep maintenance problems [26] were also assessed in any other investigation. In general, only self-rated sleep quality was positively associated with MD. Other sleep outcomes were not associated with this dietary pattern. Mamalaki et al. [33] found no significant association between adherence to MD and some sleep disorders including: not quiet sleep, awaken short of breath or with a headache, feel drowsy or sleepy during the day, trouble falling asleep, awaken during sleep and have trouble falling asleep, trouble staying awake during the day, snore during sleep, snoring and sleep adequacy. However, they found lower occurrence of trouble falling sleep and higher sleep adequacy among those with the greatest adherence to MD than those with the lowest adherence. In the study of Castro-Diehl et al. [29], the association between three-levels (no change, decreased and increase) of change in aMed score was examined in relation to insomnia. No change in aMed score in almost a ten year period, compared with a decreased aMed score in this period, was associated with improved insomnia. Although a significant association was seen between adherence to MD with total sleep time and weekdays sleep time, no significant association was reported between sleep time on weekend and bed time or wake time on weekday and weekend with MD in study of Ferranti et al. [30].
Study quality
The quality of studies included in the current review was assessed using the Newcastle Ottawa Scale (NOS), designed for nonrandomized studies [45]. According to this scale, a maximum of 9 points awarded to each cohort study according to the following parameters: 4 points for selection of participants, 2 points for comparability, and 3 points for the assessment of outcomes. A maximum of 10 points awarded to each cross sectional study include: 5 points for selection of participants, 2 points for comparability, and 3 points for the assessment of outcomes. A study with score from 7 to 9 has high quality, 4–6, has high risk, and 0–3 has very high risk of bias. Based on NOS scoring, we found that 15 studies had high quality [26, 29, 30, 32, 33, 35, 36], four studies had a high risk of bias [25, 27, 28, 34] and one study [31] had a very high risk of bias.
Discussion
In this study, we summarized earlier studies about the adherence to MD and sleep quality. Summarizing previous findings, we found that adherence to MD might help sleeping better. Sleep disturbance can be linked to poor health outcomes and increase the risk of developing metabolic disease and cardiovascular events [46]. Nutrition can profoundly affect the hormones and inflammation which directly or indirectly contribute to good or bad sleep quality [47]. MD has long been studied in relation to several health related outcomes including sleep hygiene [47]. The MD was first defined as a diet with low saturated fats and high vegetable oils [48] with a particular focus on extra virgin olive oil. It contains high amounts of vegetables including leafy green vegetables, fruits, cereals, nuts and pulses/legumes, moderate intakes of fish and other meat, dairy products and red wine, and low intakes of eggs [47, 49]. It has been supposed that MD can increase the secretion of brain derived neurotrophic factors and improve total body antioxidant capacity [50]. Polyphenols intake in this dietary pattern can help explaining its Anti-inflammatory and antioxidant properties, through which it might affect learning and memorizing [51–53]. MD contains dietary sources of tryptophan, which is an amino acid that is associated with improving sleep quality [52]. Consumption of MD is accompanied with less sleep disorders because of its specific dietary components as high levels of very long-chain n-3 PUFAs [54] that might induce secretion of melatonin and serotonin with their fundamental role in better sleep quality which modulates circadian rhythm [50, 55]. MD can also improve adiposity and body weight, blood pressure, blood lipids, glucose metabolism and insulin sensitivity that may beneficially affect brain function, cognition, and mood which are also important to sleep [56, 57]. Moreover, it is considered that gut microbiota mediate sleep effects of the MD as some of them can promote higher production of SCFA and serotonin, and improve oxidative stress, inflammation, neurologic, and cognitive functions [58, 59]. In addition, olive oil favorably changed gut microbiota composition and metabolic function, maybe by increasing SCFA production [58].
We were not able to do a meta-analysis on these studies because of heterogeneity between studies in terms of reporting different effect sizes. In addition, the study design in included studies were different, which prohibited us again to derive a quantitative assessment of available literature. Most included studies, except for two, did not use actigraphy and Wrist-worn accelerometer to measure sleep quality, which are non-subjective method for assessment of sleep quality. Others had mostly used self-reported questionnaires to examine sleep quality, which are subject to recall and social biases. About assessing dietary pattern all studies had used self-reported questionnaires. Therefore, misclassification of study participants is unavoidable. The generalizability of our findings should be done cautiously because most included studies had examined a particular age group or had limited the analysis to one gender. Our quality assessment of included studies indicated that out of 12 studies, only seven studies had a high quality and the five remaining studies had a high risk or a very high risk of bias, which might further limits the reliability of findings in earlier studies in this regard.
In conclusion, most findings of published studies highlight the importance of consumption of MD for better sleep quality. Given the different forms of sleep pattern examined in the earlier studies, future large-scale, international, multicenter, population-based, epidemiological studies with samples from different areas like as other countries worldwide, urban, rural and island regions, are essential for more reliable conclusions. Clinical intervention studies to examine the effect of consumption of MD on sleep quality are needed. More animal studies can provide a better view of the mechanisms mediating the association between MD and sleep features. In addition, objective neurophysiological tools for sleep assessment (for example actigraphy, polysomnography) are suggested to widely use in feature studies. Moreover, other studies could examine the effects of meal timing and frequency, in the relation of the MD and sleep quality and quantity. Face-to-face interviews with validated questionnaire such as PSQI is recommended in future studies to reduce recall bias and to increase the validity of the responses. By further studies have been done on these desired variables, meta-analysis would be allowed to be performed. Therefore we can obtain more accurate information and make stronger recommendations for dietary pattern and sleep hygiene.
Acknowledgements
Not applicable.
Author contributions
MF prepared the manuscript. MF and AA contributed in Table and figure preparation. AE reviewed and edited all part of manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Data availability
All data generated during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Reiter RJ, Sharma R, Cucielo MS, Tan DX, Rosales-Corral S, Gancitano G, et al. Brain washing and neural health: role of age, sleep, and the cerebrospinal fluid melatonin rhythm. Cell Mol Life Sci. 2023;80(4):88. doi: 10.1007/s00018-023-04736-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zaragoza-Martí A, Cabañero-Martínez MJ, Hurtado-Sánchez JA, Laguna-Pérez A, Ferrer-Cascales R. Evaluation of Mediterranean diet adherence scores: a systematic review. BMJ open. 2018;8(2). [DOI] [PMC free article] [PubMed]
- 3.Heath AC, Kendler KS, Eaves LJ, Martin NG. Evidence for genetic influences on sleep disturbance and sleep pattern in twins. Sleep. 1990;13(4):318–35. doi: 10.1093/sleep/13.4.318. [DOI] [PubMed] [Google Scholar]
- 4.Leung TN, Wong KL, Chan AKC, Li AM. Common childhood sleep problems and disorders. Curr Pediatr Reviews. 2024;20(1):27–42. doi: 10.2174/1573396318666220827102018. [DOI] [PubMed] [Google Scholar]
- 5.Tian Y, Li LM. [Epidemiological study of sleep disorder in the elderly]. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua. Liuxingbingxue Zazhi. 2017;38(7):988–92. doi: 10.3760/cma.j.issn.0254-6450.2017.07.028. [DOI] [PubMed] [Google Scholar]
- 6.Stubbs B, Vancampfort D, Thompson T, Veronese N, Carvalho AF, Solmi M, et al. Pain and severe sleep disturbance in the general population: primary data and meta-analysis from 240,820 people across 45 low- and middle-income countries. Gen Hosp Psychiatry. 2018;53:52–8. doi: 10.1016/j.genhosppsych.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Jalali R, Mohammadi M, Vaisi-Raygani A, Salari N. The prevalence of sleep disorders among Iranian older adults: a systematic review and meta-analysis. Curr Psychol. 2021:1–8.
- 8.Pearson O, Uglik-Marucha N, Miskowiak KW, Cairney SA, Rosenzweig I, Young AH et al. The relationship between sleep disturbance and cognitive impairment in mood disorders: a systematic review. J Affect Disord. 2023. [DOI] [PubMed]
- 9.McDermott M, Brown DL, Chervin RD. Sleep disorders and the risk of stroke. Expert Rev Neurother. 2018;18(7):523–31. doi: 10.1080/14737175.2018.1489239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu F, Zhou F, Zhang K, Wu T, Pan M, Wang X, et al. Effects of air pollution and residential greenness on sleep disorder: a 8-year nationwide cohort study. Environ Res. 2023;220:115177. doi: 10.1016/j.envres.2022.115177. [DOI] [PubMed] [Google Scholar]
- 11.Vgontzas A, Pavlović JM. Sleep disorders and Migraine: review of literature and potential pathophysiology mechanisms. Headache. 2018;58(7):1030–9. doi: 10.1111/head.13358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bruni O, Angriman M, Melegari MG, Ferri R. Pharmacotherapeutic management of sleep disorders in children with neurodevelopmental disorders. Expert Opin Pharmacother. 2019;20(18):2257–71. doi: 10.1080/14656566.2019.1674283. [DOI] [PubMed] [Google Scholar]
- 13.Wang B, Duan R, Duan L. Prevalence of sleep disorder in irritable bowel syndrome: a systematic review with meta-analysis. Saudi J Gastroenterology: Official J Saudi Gastroenterol Association. 2018;24(3):141–50. doi: 10.4103/sjg.SJG_603_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shim J, Kang SW. Behavioral factors related to Sleep Quality and Duration in adults. J Lifestyle Med. 2017;7(1):18–26. doi: 10.15280/jlm.2017.7.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13(1):3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Lopez-Garcia E, Rodriguez-Artalejo F, Li TY, Fung TT, Li S, Willett WC, et al. The Mediterranean-style dietary pattern and mortality among men and women with cardiovascular disease. Am J Clin Nutr. 2014;99(1):172–80. doi: 10.3945/ajcn.113.068106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manios Y, Detopoulou V, Visioli F, Galli C. Mediterranean diet as a nutrition education and dietary guide: misconceptions and the neglected role of locally consumed foods and wild green plants. Local Mediterranean food Plants Nutraceuticals. 2006;59:154–70. doi: 10.1159/000095212. [DOI] [PubMed] [Google Scholar]
- 18.Barrea L, Verde L, Annunziata G, Camajani E, Caprio M, Sojat A et al. Role of Mediterranean diet in endocrine diseases: a joint overview by the endocrinologist and the nutritionist. J Endocrinol Investig. 2023:1–17. [DOI] [PMC free article] [PubMed]
- 19.Barbaresko J, Koch M, Schulze MB, Nöthlings U. Dietary pattern analysis and biomarkers of low-grade inflammation: a systematic literature review. Nutr Rev. 2013;71(8):511–27. doi: 10.1111/nure.12035. [DOI] [PubMed] [Google Scholar]
- 20.Papadimitriou A, Foscolou A, Itsiopoulos C, Thodis A, Kouris-Blazos A, Brazionis L, et al. Adherence to the Mediterranean Diet and successful aging in greeks living in Greece and abroad: the epidemiological Mediterranean islands Study (MEDIS) Nutr Health. 2023;29(2):287–95. doi: 10.1177/02601060211072363. [DOI] [PubMed] [Google Scholar]
- 21.Dominguez LJ, Donat-Vargas C, Sayon-Orea C, Barberia-Latasa M, Veronese N, Rey-Garcia J, et al. Rationale of the association between Mediterranean diet and the risk of frailty in older adults and systematic review and meta-analysis. Exp Gerontol. 2023;177:112180. doi: 10.1016/j.exger.2023.112180. [DOI] [PubMed] [Google Scholar]
- 22.Nomikos T, Fragopoulou E, Antonopoulou S, Panagiotakos DB. Mediterranean diet and platelet-activating factor; a systematic review. Clin Biochem. 2018;60:1–10. doi: 10.1016/j.clinbiochem.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 23.Morze J, Danielewicz A, Przybyłowicz K, Zeng H, Hoffmann G, Schwingshackl L. An updated systematic review and meta-analysis on adherence to mediterranean diet and risk of cancer. Eur J Nutr. 2021;60:1561–86. doi: 10.1007/s00394-020-02346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Konieczna J, Ruiz-Canela M, Galmes-Panades AM, Abete I, Babio N, Fiol M, et al. An energy-reduced Mediterranean Diet, Physical Activity, and body composition: an interim subgroup analysis of the PREDIMED-Plus Randomized Clinical Trial. JAMA Netw Open. 2023;6(10):e2337994–e. doi: 10.1001/jamanetworkopen.2023.37994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zuraikat FM, Makarem N, St-Onge MP, Xi H, Akkapeddi A, Aggarwal B. A Mediterranean Dietary Pattern predicts Better Sleep Quality in US women from the American Heart Association Go Red for Women Strategically Focused Research Network. Nutrients. 2020;12(9). [DOI] [PMC free article] [PubMed]
- 26.van Egmond L, Tan X, Sjögren P, Cederholm T, Benedict C. Association between Healthy Dietary Patterns and self-reported sleep disturbances in older men: the ULSAM Study. Nutrients. 2019;11(5). [DOI] [PMC free article] [PubMed]
- 27.Campanini MZ, Guallar-Castillón P, Rodríguez-Artalejo F, Lopez-Garcia E. Mediterranean Diet and Changes in Sleep Duration and indicators of Sleep Quality in older adults. Sleep. 2017;40(3). [DOI] [PubMed]
- 28.Adelantado-Renau M, Beltran-Valls MR, Esteban-Cornejo I, Martínez-Vizcaíno V, Santaliestra-Pasías AM, Moliner-Urdiales D. The influence of adherence to the Mediterranean diet on academic performance is mediated by sleep quality in adolescents. Acta paediatrica (Oslo, Norway: 1992). 2019;108(2):339– 46. [DOI] [PubMed]
- 29.Castro-Diehl C, Wood AC, Redline S, Reid M, Johnson DA, Maras JE et al. Mediterranean diet pattern and sleep duration and insomnia symptoms in the multi-ethnic study of atherosclerosis. Sleep. 2018;41(11). [DOI] [PMC free article] [PubMed]
- 30.Ferranti R, Marventano S, Castellano S, Giogianni G, Nolfo F, Rametta S, et al. Sleep quality and duration is related with diet and obesity in young adolescent living in Sicily, Southern Italy. Sleep Sci (Sao Paulo Brazil) 2016;9(2):117–22. doi: 10.1016/j.slsci.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flor-Alemany M, Nestares T, Alemany-Arrebola I, Marín-Jiménez N, Borges-Cosic M, Aparicio VA. Influence of Dietary habits and Mediterranean Diet adherence on Sleep Quality during pregnancy. The GESTAFIT Project. Nutrients. 2020;12(11). [DOI] [PMC free article] [PubMed]
- 32.Godos J, Ferri R, Caraci F, Cosentino FII, Castellano S, Galvano F et al. Adherence to the Mediterranean Diet is Associated with Better Sleep Quality in Italian adults. Nutrients. 2019;11(5). [DOI] [PMC free article] [PubMed]
- 33.Mamalaki E, Anastasiou CA, Ntanasi E, Tsapanou A, Kosmidis MH, Dardiotis E, et al. Associations between the mediterranean diet and sleep in older adults: results from the hellenic longitudinal investigation of aging and diet study. Geriatr Gerontol Int. 2018;18(11):1543–8. doi: 10.1111/ggi.13521. [DOI] [PubMed] [Google Scholar]
- 34.Muscogiuri G, Barrea L, Aprano S, Framondi L, Di Matteo R, Laudisio D et al. Sleep Qual Obesity: Does Adherence Mediterranean Diet Matter? Nutrients. 2020;12(5). [DOI] [PMC free article] [PubMed]
- 35.Rosi A, Giopp F, Milioli G, Melegari G, Goldoni M, Parrino L et al. Weight status, adherence to the Mediterranean Diet, Physical Activity Level, and Sleep Behavior of Italian Junior High School adolescents. Nutrients. 2020;12(2). [DOI] [PMC free article] [PubMed]
- 36.Gupta K, Jansen EC, Campos H, Baylin A. Associations between sleep duration and Mediterranean diet score in Costa Rican adults. Appetite. 2021;170:105881. doi: 10.1016/j.appet.2021.105881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mantzorou M, Mentzelou M, Vasios GK, Kontogiorgis C, Antasouras G, Vadikolias K, et al. Mediterranean Diet adherence is Associated with Favorable Health-Related Quality of Life, Physical Activity, and Sleep Quality in a Community-Dwelling Greek Older Population. Antioxidants. 2023;12(5):983. doi: 10.3390/antiox12050983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yaghtin Z, Beigrezaei S, Yuzbashian E, Ghayour-Mobarhan M, Khayyatzadeh SS. A greater modified Mediterranean diet score is associated with lower insomnia score among adolescent girls: a cross-sectional study. BMC Nutr. 2022;8(1):60. doi: 10.1186/s40795-022-00553-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zaidalkilani AT, Alhaj OA, Serag El-Dine MF, Fekih-Romdhane F, AlRasheed MM, Jahrami HA, et al. Arab women adherence to the Mediterranean diet and insomnia. Medicina. 2021;58(1):17. doi: 10.3390/medicina58010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.López-Gil JF, Smith L, Victoria-Montesinos D, Gutiérrez-Espinoza H, Tárraga-López PJ, Mesas AE. Mediterranean dietary patterns related to sleep duration and sleep-related problems among adolescents: the EHDLA study. Nutrients. 2023;15(3):665. doi: 10.3390/nu15030665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boraita RJ, Alsina DA, Ibort EG, Torres JMD. Factors associated with adherence to a Mediterranean diet in adolescents from La Rioja (Spain) Br J Nutr. 2022;128(7):1425–32. doi: 10.1017/S0007114520003803. [DOI] [PubMed] [Google Scholar]
- 42.Bakırhan H, Pehlivan M, Özyürek F, Özkaya V, Yousefirad N. Diet, sleep and depression: does adherence to the mediterranean diet matter? JTSM-Journal Turkish Sleep Med. 2022.
- 43.ÖZCAN BA, YEŞİLKAYA B, YILMAZ HÖ, GÜNAL AM, ÖZDEMİR AA. Effects of adherence to the Mediterranean diet on depression, anxiety, and sleep quality during the Covid-19 pandemic in Turkey. Int J Innovative Res Reviews. 2021;5(2):39–44. [Google Scholar]
- 44.Naja F, Hasan H, Khadem SH, Buanq MA, Al-Mulla HK, Aljassmi AK, et al. Adherence to the Mediterranean diet and its association with sleep quality and chronotype among youth: a cross-sectional study. Front Nutr. 2022;8:805955. doi: 10.3389/fnut.2021.805955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45. doi: 10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Larcher S, Benhamou PY, Pépin JL, Borel AL. Sleep habits and diabetes. Diabetes Metab. 2015;41(4):263–71. doi: 10.1016/j.diabet.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 47.Zhao M, Tuo H, Wang S, Zhao L. The effects of Dietary Nutrition on Sleep and Sleep disorders. Mediat Inflamm. 2020;2020:3142874. doi: 10.1155/2020/3142874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martínez-González MA, Sánchez-Villegas A. The emerging role of Mediterranean diets in cardiovascular epidemiology: monounsaturated fats, olive oil, red wine or the whole pattern? Eur J Epidemiol. 2004;19(1):9–13. doi: 10.1023/B:EJEP.0000013351.60227.7b. [DOI] [PubMed] [Google Scholar]
- 49.Davis C, Bryan J, Hodgson J, Murphy K. Definition of the Mediterranean Diet; a literature review. Nutrients. 2015;7(11):9139–53. doi: 10.3390/nu7115459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hibbeln JR, Ferguson TA, Blasbalg TL. Omega-3 fatty acid deficiencies in neurodevelopment, aggression and autonomic dysregulation: opportunities for intervention. Int Rev Psychiatry (Abingdon) 2006;18(2):107–18. doi: 10.1080/09540260600582967. [DOI] [PubMed] [Google Scholar]
- 51.Silva AR, Moraes BPT, Gonçalves-de-Albuquerque CF. Mediterranean Diet: lipids, inflammation, and Malaria infection. Int J Mol Sci. 2020;21(12). [DOI] [PMC free article] [PubMed]
- 52.Martínez-Rodríguez A, Rubio-Arias J, Ramos-Campo DJ, Reche-García C, Leyva-Vela B, Nadal-Nicolás Y. Psychological and Sleep effects of Tryptophan and Magnesium-Enriched Mediterranean Diet in Women with Fibromyalgia. Int J Environ Res Public Health. 2020;17(7). [DOI] [PMC free article] [PubMed]
- 53.Wang YB, Page AJ, Gill TK, Melaku YA. The association between diet quality, plant-based diets, systemic inflammation, and mortality risk: findings from NHANES. Eur J Nutr. 2023;1:15. doi: 10.1007/s00394-023-03191-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Murphy RA, Tintle N, Harris WS, Darvishian M, Marklund M, Virtanen JK et al. Omega-3 and omega-6 polyunsaturated fatty acid biomarkers and sleep: a pooled analysis of cohort studies on behalf of the Fatty Acids and Outcomes Research Consortium (FORCE). The American journal of clinical nutrition. 2021. [DOI] [PMC free article] [PubMed]
- 55.Catalá A. The function of very long chain polyunsaturated fatty acids in the pineal gland. Biochim Biophys Acta. 2010;1801(2):95–9. doi: 10.1016/j.bbalip.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 56.Scoditti E, Tumolo MR, Garbarino S. Mediterranean diet on sleep: a health alliance. Nutrients. 2022;14(14):2998. doi: 10.3390/nu14142998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.von Deneen KM, Garstka MA. Neuroimaging perspective in targeted treatment for type 2 diabetes melitus and sleep disorders. Intell Med. 2022;2(04):209–20. doi: 10.1016/j.imed.2022.05.003. [DOI] [Google Scholar]
- 58.Lippolis T, Cofano M, Caponio GR, De Nunzio V, Notarnicola M. Bioaccessibility and bioavailability of diet polyphenols and their modulation of gut microbiota. Int J Mol Sci. 2023;24(4):3813. doi: 10.3390/ijms24043813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Han D, Wu Y, Lu D, Pang J, Hu J, Zhang X, et al. Polyphenol-rich diet mediates interplay between macrophage-neutrophil and gut microbiota to alleviate intestinal inflammation. Cell Death Dis. 2023;14(10):656. doi: 10.1038/s41419-023-06190-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated during this study are included in this published article.